The Unseen Burden: Epidemiology, Diagnosis, and Control of Intestinal Protozoan Infections
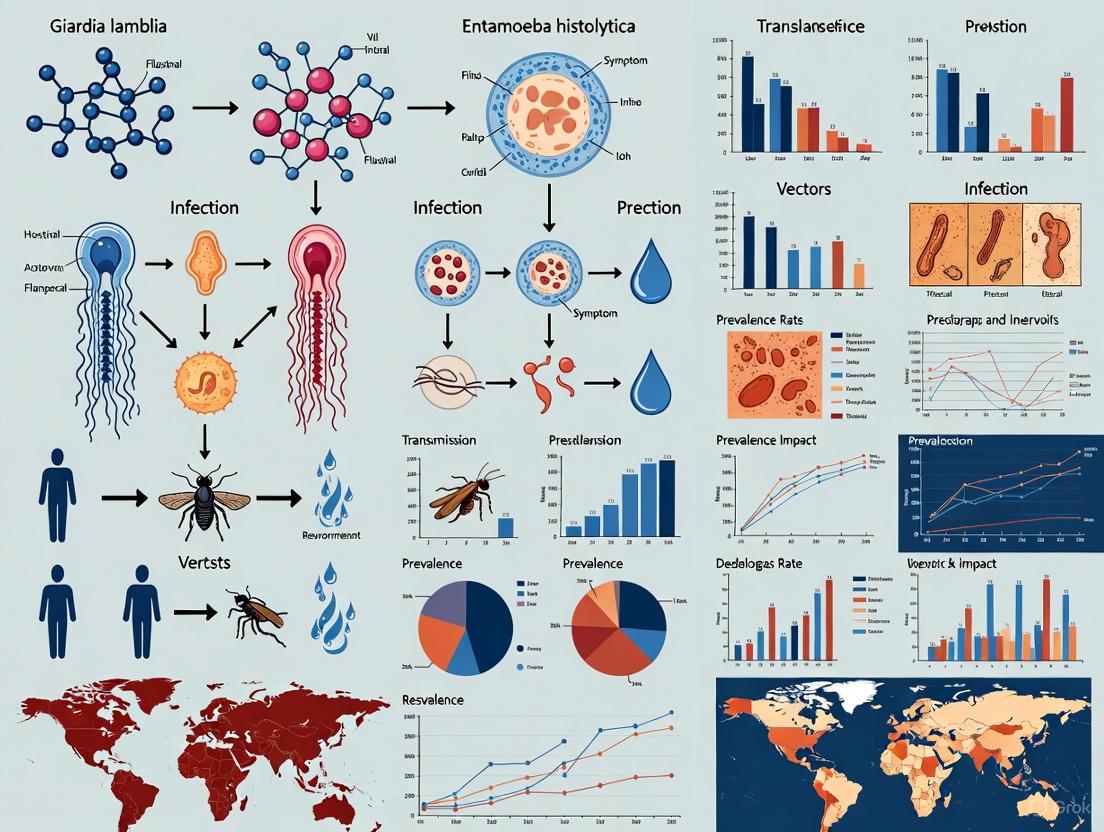
This article provides a comprehensive analysis of the epidemiology of intestinal protozoan infections, focusing on the major pathogens Entamoeba histolytica, Giardia lamblia, and Cryptosporidium spp.
The Unseen Burden: Epidemiology, Diagnosis, and Control of Intestinal Protozoan Infections
Abstract
This article provides a comprehensive analysis of the epidemiology of intestinal protozoan infections, focusing on the major pathogens Entamoeba histolytica, Giardia lamblia, and Cryptosporidium spp. It synthesizes current data on global and regional prevalence, identifies key socioeconomic and environmental risk factors, and evaluates the strengths and limitations of conventional and advanced diagnostic methodologies. Furthermore, it examines the challenges in the current therapeutic landscape, including drug resistance, and explores future directions for drug discovery and public health intervention. Tailored for researchers, scientists, and drug development professionals, this review aims to bridge epidemiological insights with practical applications for improved disease control and drug development strategies.
Global Burden and Risk Factors: Mapping the Impact of Intestinal Protozoa
Intestinal protozoan infections (IPIs) represent a significant and persistent global health challenge, particularly in resource-limited settings. These infections, primarily caused by Entamoeba histolytica, Giardia lamblia, and Cryptosporidium parvum, contribute substantially to the global burden of diarrheal diseases, which remain a leading cause of mortality and morbidity worldwide [1] [2]. The World Health Organization identifies diarrhea as the third leading cause of death among children under five years, with approximately 443,832 annual fatalities [1]. Understanding the current epidemiological landscape of IPIs is fundamental for developing targeted interventions, guiding drug development initiatives, and shaping public health policy. This systematic review synthesizes recent data on the global prevalence and incidence of intestinal protozoan infections, framing the findings within the broader context of epidemiological research and therapeutic development.
The clinical manifestations of IPIs range from asymptomatic carriage to severe diarrheal illness with potential for long-term sequelae. Amebiasis, caused by E. histolytica, is characterized by symptoms including abdominal pain, bloody diarrhea, fever, and in severe cases, liver abscesses [3]. Giardiasis typically presents with watery diarrhea, abdominal pain, flatulence, and weight loss, while cryptosporidiosis manifests with watery diarrhea accompanied by stomach cramps, nausea, and vomiting, with particular severity in immunocompromised individuals [4] [3]. The transmission of these pathogens occurs predominantly through the fecal-oral route, with contamination of food and water serving as major vehicles for dissemination [5]. Despite their significant public health impact, IPIs have historically been neglected in drug discovery efforts, with few therapeutic advances in recent decades and growing concerns about drug resistance [1] [2].
Global Epidemiology of Intestinal Protozoan Infections
Intestinal protozoan infections impose a substantial disease burden worldwide, disproportionately affecting populations in tropical and subtropical regions with inadequate sanitation infrastructure. Current estimates indicate that approximately 3.5 billion people are affected by IPIs globally, with around 450 million people currently suffering from active infections [6] [3]. These infections are responsible for nearly 1.7 billion episodes of diarrhea annually, contributing significantly to global morbidity and mortality statistics [5]. The disability-adjusted life years (DALYs) attributed to these infections are considerable, with amebiasis alone responsible for more than 55,000 deaths and 2.2 million DALYs, while cryptosporidiosis accounts for approximately 100,000 deaths and 8.4 million DALYs [2].
The geographical distribution of IPIs reflects complex interactions between environmental factors, socioeconomic conditions, and public health infrastructure. Developing countries in tropical regions bear the greatest disease burden, with prevalence rates often exceeding 25% in certain populations [6]. The parasites exhibit a global distribution, but the highest concentrations are found in areas of Central and South America, Africa, and Asia, with prevalence rates reaching up to 25% in some heavily indebted poor countries [3]. This unequal distribution highlights the role of socioeconomic determinants in disease transmission and the critical need for targeted interventions in high-burden regions.
Regional Variations in Prevalence
Significant geographical heterogeneity exists in the prevalence of intestinal protozoan infections, with notable variations between and within world regions. A recent meta-analysis focusing on Malaysia reported an overall pooled prevalence of 24% (95% CI: 0.17-0.29) for IPIs in the country [4]. Subgroup analysis revealed considerable regional variation within Malaysia, with Kelantan and Perak states reporting the highest prevalence rates of 39% and 29% respectively, while Selangor and Kuala Lumpur reported substantially lower rates of 13.6% [4]. These variations likely reflect differences in infrastructure, sanitation practices, and socioeconomic factors across regions.
In Sub-Saharan Africa, prevalence rates are notably elevated. A recent health facility-based cross-sectional study conducted in Simada, northwest Ethiopia, documented a strikingly high prevalence of 57.1% among individuals visiting a health center [7]. Occupational factors significantly influenced risk, with farmers (AOR = 8.0), secondary school students (AOR = 3.1), and merchants (AOR = 4.7) demonstrating higher likelihood of infection [7]. Similarly, a study among school children in Zeita village, Central Ethiopia, found an overall IPI prevalence of 46.8%, with E. histolytica (25.2%), G. lamblia (19.3%), and C. parvum (2.5%) identified as the predominant pathogens [8]. These figures substantially exceed global averages and underscore the disproportionate burden borne by particular regions and populations.
Table 1: Regional Prevalence of Intestinal Protozoan Infections
| Region/Country | Prevalence (%) | Predominant Pathogens | Population Studied | Citation |
|---|---|---|---|---|
| Global Estimate | ~24% (pooled) | Entamoeba spp., Giardia lamblia, Cryptosporidium spp. | General population | [4] |
| Ethiopia (Simada) | 57.1% | Not specified | Health center visitors | [7] |
| Ethiopia (Zeita) | 46.8% | E. histolytica (25.2%), G. lamblia (19.3%) | School children | [8] |
| Malaysia | 24% | Entamoeba spp. (18%), G. lamblia (11%) | General population | [4] |
| Kelantan, Malaysia | 39% | Entamoeba spp. | General population | [4] |
| Selangor/Kuala Lumpur, Malaysia | 13.6% | Entamoeba spp. | General population | [4] |
Prevalence in Specific Populations
The risk of intestinal protozoan infections is not uniformly distributed within populations, with certain demographic groups experiencing disproportionately high infection rates. Indigenous communities consistently demonstrate elevated prevalence rates, with a meta-analysis in Malaysia reporting a 27% prevalence among indigenous populations compared to 23% in local communities from rural areas [4]. This disparity likely reflects differences in access to healthcare, sanitation infrastructure, and educational resources.
School-aged children represent another vulnerable population, with studies consistently reporting high infection rates in this demographic. Research among school children in Central Ethiopia revealed that factors including parental occupation (P = 0.028), sources of drinking water (P = 0.001), water handling practices (P = 0.027), consumption of raw vegetables (P = 0.001), and latrine availability significantly influenced infection risk [8]. Interestingly, this study found no significant association between gender and IPI prevalence (P = 0.54), suggesting environmental and behavioral factors outweigh biological sex as determinants of infection [8].
Immunocompromised individuals, particularly those with HIV/AIDS, also face elevated risk and disease severity. Studies in Malaysia have documented increased rates of cryptosporidiosis among intravenous drug users with HIV-positive status, highlighting the intersection of parasitic infections with other health challenges [4]. Prison inmates with HIV-positive status showed slightly higher IPI prevalence (27.5%) compared to HIV-negative inmates (25.8%) [4], emphasizing the need for targeted screening and prevention in institutional settings.
Pathogen-Specific Epidemiology and Risk Factors
Distribution of Major Pathogenic Species
The relative prevalence of specific protozoan pathogens varies geographically and among different population groups. According to a comprehensive meta-analysis of studies in Malaysia, Entamoeba species demonstrate the highest prevalence at 18% (95% CI: 0.12-0.24), followed by G. lamblia at 11% (95% CI: 0.08-0.14), and Cryptosporidium species at 9% (95% CI: 0.03-0.14) [4]. This distribution pattern reflects the biological characteristics and transmission dynamics of each pathogen, with Entamoeba species potentially benefiting from greater environmental persistence and multiple transmission routes.
The prevalence of specific pathogens also shows considerable variation across studies and settings. In research conducted among Ethiopian school children, E. histolytica was identified as the most prevalent pathogen (25.2%), followed by G. lamblia (19.3%) and C. parvum (2.5%) [8]. The relatively low detection of Cryptosporidium in this study may reflect methodological limitations, as specialized staining techniques are required for optimal identification of this pathogen [8]. These findings underscore the importance of diagnostic approach in determining pathogen-specific prevalence rates and the value of multiplex detection methods in surveillance studies.
Table 2: Prevalence of Specific Intestinal Protozoan Pathogens
| Pathogen | Global Prevalence Estimates | Clinical Manifestations | High-Risk Populations | Citation |
|---|---|---|---|---|
| Entamoeba histolytica | 18% (Malaysia meta-analysis); 25.2% (Ethiopian children) | Amebic dysentery, liver abscess | School children, indigenous communities | [4] [8] |
| Giardia lamblia | 11% (Malaysia meta-analysis); 19.3% (Ethiopian children) | Watery diarrhea, malabsorption, weight loss | Children, travelers, immunocompromised | [4] [8] |
| Cryptosporidium parvum | 9% (Malaysia meta-analysis); 2.5% (Ethiopian children) | Profuse watery diarrhea, particularly severe in immunocompromised | HIV+ individuals, children | [4] [8] |
| Intestinal protozoa collectively | 450 million current infections globally | Diarrhea, abdominal pain, malnutrition | Children in developing countries | [6] [3] |
Environmental Contamination and Transmission Dynamics
Environmental reservoirs play a crucial role in the transmission and persistence of intestinal protozoan infections. A global systematic review and meta-analysis of vegetable and fruit contamination found a pooled prevalence of intestinal protozoan parasites of 20% (16-24%) in vegetables and 13% (8-20%) in fruits [5]. Contamination occurs primarily through irrigation with contaminated water, fertilization with untreated manure, and improper handling during harvesting and transportation. The analysis included 189 articles with 202 datasets, examining 45,495 vegetable samples and 5,113 fruit samples, providing comprehensive insights into this transmission route [5].
The risk of foodborne transmission is influenced by agricultural practices, hygiene standards, and environmental conditions. The meta-analysis revealed that low-income countries reported significantly higher prevalence of protozoan contamination in vegetables and fruits compared to high-income countries [5]. This disparity reflects differences in regulatory frameworks, sanitation infrastructure, and agricultural practices between economic contexts. Geographical factors also influenced contamination rates, with the African region reporting the highest prevalence (25%), followed by the Eastern Mediterranean region (24%) [5]. These findings highlight the importance of food safety interventions within broader IPI control strategies.
Socioeconomic and Behavioral Determinants
Risk factor analyses consistently identify socioeconomic status and hygiene behaviors as critical determinants of IPI transmission. A meta-analysis of ten risk factors in Malaysia found significantly elevated pooled prevalence (38-52%) among children under 15 years, males, individuals with low income or no formal education, and those exposed to untreated water, poor sanitation, or unhygienic practices [4]. These findings align with studies from Ethiopia identifying low income (AOR = 3.3) and failure to wash hands before meals (AOR = 12.4) as significant predictors of infection [7].
The association between poverty and IPI risk reflects multiple pathways, including inadequate sanitation infrastructure, limited access to clean water, crowded living conditions, and educational barriers. In the Ethiopian study, participants with no habit of handwashing before meals had more than 12 times higher odds of IPIs compared to those with consistent handwashing practices [7]. Similarly, improper water handling practices and consumption of raw vegetables significantly increased infection risk among school children [8]. These findings underscore the potential of integrated interventions addressing water, sanitation, and hygiene (WASH) alongside educational components to reduce IPI transmission.
Research Methodologies and Diagnostic Approaches
Epidemiological Study Designs
Robust epidemiological investigation of intestinal protozoan infections requires careful consideration of study design and methodology. Cross-sectional studies represent the most common approach for estimating prevalence, providing snapshot assessments of infection rates at specific timepoints. The studies cited in this review employed health facility-based [7] and community-based [8] cross-sectional designs, each offering distinct advantages for different research questions. Health facility-based designs facilitate sample collection and diagnostic procedures but may introduce selection bias, while community-based designs enhance representativeness at the cost of operational complexity.
Systematic reviews and meta-analyses have emerged as powerful tools for synthesizing evidence across multiple studies and generating pooled prevalence estimates. The Malaysia meta-analysis followed PRISMA guidelines, conducted comprehensive searches across five databases (Scopus, Google Scholar, Web of Science, PubMed, and Cochrane Library), and employed a random effects model to account for heterogeneity [4]. This approach identified 103 potentially relevant articles, with 49 studies meeting inclusion criteria after duplicate removal and eligibility screening [4]. The high statistical heterogeneity observed (I² = 98.94%, P < 0.001) reflects substantial variability across included studies, necessitating careful interpretation of pooled estimates [4].
Laboratory Diagnostic Techniques
Accurate diagnosis of intestinal protozoan infections requires appropriate laboratory methods with sufficient sensitivity and specificity. Basic microscopic techniques, including direct wet mount examination and formol-ether concentration methods, remain widely used in resource-limited settings [7] [8]. While cost-effective and technically accessible, these approaches have limitations in sensitivity and ability to differentiate between pathogenic and non-pathogenic species.
Advanced diagnostic methods improve detection capabilities but require greater technical and financial resources. The Modified Ziehl-Neelsen (MZN) staining technique enables identification of Cryptosporidium oocysts, which are often missed in routine microscopy [8]. Immunoassays detecting parasite-specific antigens offer enhanced sensitivity and specificity, while molecular approaches such as real-time polymerase chain reaction (PCR) provide the highest sensitivity and enable species differentiation [3]. The optimal diagnostic approach depends on available resources, technical expertise, and specific clinical or research objectives, with many settings benefiting from a combination of methods.
Diagram 1: Diagnostic Workflow for Intestinal Protozoan Infections. This flowchart illustrates the sequential approach to laboratory diagnosis of IPIs, from sample collection to final identification, highlighting both basic and advanced methodological pathways.
Quality Assessment and Statistical Analysis
Methodological rigor in IPI research requires careful attention to quality assessment and appropriate statistical approaches. The Malaysia meta-analysis utilized Cochrane's Q and I² statistics to quantify heterogeneity, with I² values >75% indicating high heterogeneity [4]. Random-effects models were employed to account for this variability, and publication bias was assessed using funnel plots and Egger's test [4]. Similar approaches were applied in a global meta-analysis of IPIs in colorectal cancer patients, which included 70 studies and assessed quality using the Newcastle-Ottawa Scale [9].
Sample size considerations are particularly important in IPI research, as inadequate power may limit the ability to detect significant associations. The Ethiopian school-based study initially calculated a sample size of 422 using a single population proportion formula but ultimately collected data from 280 respondents due to school absenteeism during the COVID-19 pandemic [8]. Such methodological adaptations highlight the practical challenges of conducting field research in resource-limited settings while underscoring the importance of transparent reporting of limitations.
Research Reagents and Materials
Table 3: Essential Research Reagents for Intestinal Protozoan Infection Studies
| Reagent/Material | Application | Specific Function | Examples/References |
|---|---|---|---|
| Formol-ether | Stool concentration | Preserves parasites and removes debris | Used in concentration techniques [7] [8] |
| Modified Ziehl-Neelsen stain | Cryptosporidium detection | Acid-fast staining of oocysts | Identification of C. parvum [8] |
| Specific antigens | Immunoassays | Detection of parasite-specific proteins | EIA for E. histolytica, Giardia [3] |
| PCR primers/probes | Molecular detection | Amplification of parasite DNA | Real-time PCR assays [3] |
| Culture media | Parasite isolation | Support growth of trophozoites | Axenic culture for E. histolytica [1] |
| Microscopy reagents | Stool examination | Visualization of parasites | Iodine, saline for wet mounts [8] |
Implications for Public Health and Drug Development
Public Health Interventions
The high prevalence rates documented across multiple regions underscore the urgent need for enhanced public health interventions targeting intestinal protozoan infections. The significant association between WASH indicators and infection risk supports continued investment in water sanitation infrastructure and hygiene education programs [7] [8]. The identification of specific high-risk populations, including school children, indigenous communities, and agricultural workers, enables targeting of limited resources to maximize impact [7] [4].
Food safety interventions represent another critical component of comprehensive IPI control. The substantial contamination rates documented in vegetables and fruits (20% and 13% respectively) highlight the importance of measures to prevent contamination throughout the production and distribution chain [5]. These include treatment of irrigation water, proper composting of manure, and education for food handlers regarding hygienic practices. Regulatory frameworks governing food safety should incorporate specific standards for parasitic contamination, particularly in high-prevalence regions.
Drug Development and Therapeutic Considerations
The current therapeutic landscape for intestinal protozoan infections remains inadequate, with few advances in recent decades and growing concerns about drug resistance. Metronidazole, the most common drug used for treating invasive amebiasis and giardiasis, has been in use for over 60 years, with efficacy limitations and significant side effects including nausea, vomiting, and potential resistance [1] [2]. Treatment failures in giardiasis occur in up to 20% of cases, rising to 40.2% in some settings [2]. Similarly, nitazoxanide, the only treatment option for cryptosporidiosis, demonstrates variable efficacy (56-80%) and is not effective for immunocompromised patients [2].
Promising drug development approaches include target-based screening, drug repurposing, and natural product discovery. Auranofin, an anti-rheumatic compound, has shown efficacy against Giardia and Entamoeba in clinical trials, inhibiting parasite thioredoxin reductase [1] [2]. Azidothymidine (AZT), an antiretroviral drug, also exhibits inhibitory activity against Giardia [1]. High-throughput screening approaches have identified novel compound classes with anti-protozoal activity, including chalcone derivatives with efficacy against Giardia [2]. These developments represent potential advances in the therapeutic arsenal against IPIs, though translation to clinical practice remains challenging.
Diagram 2: Drug Development Pipeline for IPIs. This workflow outlines the major pathways for discovering and developing new therapeutic agents against intestinal protozoan parasites, from initial approach selection through clinical development.
Intestinal protozoan infections remain a significant global health challenge, with recent systematic reviews documenting pooled prevalence rates of approximately 24% in endemic regions and rates exceeding 50% in some high-risk populations [7] [4]. The substantial geographical and demographic heterogeneity in infection rates reflects complex interactions between pathogen biology, environmental factors, and socioeconomic determinants. The high prevalence of protozoan contamination in vegetables and fruits (20%) underscores the importance of food safety interventions within comprehensive control strategies [5].
From a research perspective, methodological standardization would enhance comparability across studies, particularly regarding diagnostic approaches and risk factor assessment. The high statistical heterogeneity observed in meta-analyses (I² > 98%) highlights the substantial variability in current evidence and the need for more standardized methodologies [4]. Future research should prioritize high-quality epidemiological studies in underrepresented regions, development of improved diagnostic tools suitable for resource-limited settings, and investigation of the long-term health consequences of chronic protozoan infections.
Therapeutic development for IPIs has lagged behind other infectious diseases, with heavy reliance on decades-old drugs and emerging resistance patterns [1] [2]. Recent advances in parasite genomics, chemical biology, and drug repurposing offer promising avenues for therapeutic innovation. Translating these discoveries to clinical practice will require enhanced collaboration between academic researchers, pharmaceutical companies, and public health agencies, with particular attention to ensuring accessibility and affordability in high-burden populations. Through integrated approaches addressing both environmental transmission and therapeutic limitations, substantial progress can be made toward reducing the global burden of intestinal protozoan infections.
Intestinal protozoan infections (IPIs) represent a significant global health challenge, with a distribution pattern that highlights profound disparities between tropical and developed regions. This whitepaper provides a comparative analysis of the endemicity of IPIs, drawing on recent meta-analytical data and longitudinal cohort studies. It examines the prevalence rates, key risk factors, and species distribution of major protozoans—including Entamoeba spp., Giardia lamblia, and Cryptosporidium spp.—across different geographical and socioeconomic contexts. The paper details standardized methodologies for epidemiological surveillance and laboratory diagnosis, supported by data visualization and a catalog of essential research reagents. The analysis confirms that poverty, inadequate sanitation, and limited access to healthcare are the primary drivers of the high IPI burden in tropical regions, underscoring the need for targeted interventions and robust research capabilities.
The global distribution of intestinal protozoan infections (IPIs) serves as a stark indicator of the health inequities between tropical and developed regions. These infections, caused by pathogens such as Entamoeba histolytica, Giardia lamblia, and Cryptosporidium spp., are predominantly faecal-oral in transmission, making them intensely sensitive to environmental and socioeconomic conditions [10]. In tropical and subtropical regions, IPIs are a pervasive public health challenge, disproportionately affecting vulnerable populations, including school-aged children, indigenous communities, and low-income households [11] [4]. In contrast, developed regions typically report IPIs as sporadic cases, often associated with travel, localized outbreaks, or immunocompromised individuals [12]. The persistence of high IPI prevalence in tropical areas is intrinsically linked to factors such as poverty, inadequate water and sanitation infrastructure, and climatic conditions favorable to pathogen transmission [10] [7]. This document synthesizes current evidence to delineate the hotspots of IPI endemicity, compare the underlying risk factors, and equip researchers with the methodological frameworks for continued investigation into these neglected tropical diseases.
Comparative Analysis of Endemicity Patterns
Quantitative data from recent systematic reviews and cohort studies reveal distinct patterns of IPI endemicity. The following tables summarize key prevalence rates and risk factor associations, providing a clear comparison between different regional contexts.
Table 1: Global and Regional Prevalence of Intestinal Protozoan Infections
| Region/Country | Overall IPI Prevalence | Prevalence of Entamoeba spp. | Prevalence of G. lamblia | Prevalence of Cryptosporidium spp. | Population Studied |
|---|---|---|---|---|---|
| Malaysia (National Average) | 24% (95% CI: 17.0–29.0) [4] | 18% (95% CI: 12–24) [4] | 11% (95% CI: 8–14) [4] | 9% (95% CI: 3–14) [4] | General Patient Population |
| Malaysia (Indigenous Communities) | 27% [4] | - | - | - | Indigenous Groups |
| Malaysia (Rural Communities) | 23% [4] | - | - | - | Rural Dwellers |
| Eswatini (Manzini & Lubombo) | 42.2% (2022) [11] | Predominant [11] | - | - | Schoolchildren (2022 Cohort) |
| Ethiopia (Simada District) | 57.1% [7] | - | - | - | Health Center Visitors |
| Developed Regions (United States) | - | - | - | - | Sporadic/Imported Cases [12] |
Table 2: Key Risk Factors and Associated Measures of Effect for IPIs
| Risk Factor | Population/Setting | Measure of Effect (Adjusted Odds Ratio, aOR) | Significance |
|---|---|---|---|
| Single Employed Parent | Schoolchildren, Eswatini [11] | aOR = 3.97 (95% CI: 1.48–10.64) | p=0.006 |
| No Handwashing Before Meals | Simada, Ethiopia [7] | aOR = 12.4 (95% CI: 5.6–27.6) | Significant |
| Low Income | Simada, Ethiopia [7] | aOR = 3.3 (95% CI: 1.6–7.0) | Significant |
| Occupational Group (e.g., Farmer) | Simada, Ethiopia [7] | aOR = 8.0 (95% CI: 8.2–28.5) | Significant |
| Untreated Water, Poor Sanitation | Malaysia (Meta-Analysis) [4] | Pooled Prevalence: 38-52% | Significant |
The data demonstrates that IPI prevalence in tropical regions is substantially higher than the sporadic cases typically encountered in developed nations. Sub-national variations are also critical; for instance, in Malaysia, the state of Kelantan has a prevalence of 39%, compared to 13.6% in Selangor and Kuala Lumpur [4]. Longitudinal data from Eswatini shows remarkable persistence of IPIs, with an overall prevalence of 43.0% in 2019 and 42.2% in 2022, despite the disruptions of the COVID-19 pandemic [11]. This stability suggests deeply entrenched environmental and socioeconomic drivers. Furthermore, the species composition can shift over time, as observed in Eswatini where Giardia intestinalis infections declined while Blastocystis hominis increased [11], highlighting the dynamic nature of parasitic ecology.
Regional Case Studies
The Malaysian Context: A Meta-Analytical Perspective
Malaysia presents a compelling case study of a rapidly developing nation where IPIs remain a significant burden, particularly among its most vulnerable populations. A comprehensive meta-analysis of 49 studies revealed a national pooled IPI prevalence of 24% [4] [13]. The primary pathogens identified were Entamoeba spp. (18%), G. lamblia (11%), and Cryptosporidium spp. (9%). The highest disease burden was concentrated in indigenous communities (27%) and rural areas (23%), with significant regional disparities observed [4]. Key risk factors identified through meta-analysis include being a child under 15 years of age, male gender, low income, lack of formal education, and exposure to untreated water and poor sanitation [4]. These factors collectively underscore the role of socioeconomic development and infrastructure in determining disease patterns.
Sub-Saharan Africa: Longitudinal Insights from Eswatini
A prospective cohort study in Eswatini followed 128 schoolchildren from 2019 to 2022, providing valuable longitudinal data on IPI trends [11]. The study found that protozoan infections predominated, while helminth infections remained low (<2.5%). A critical finding was the significant association between socioeconomic status and infection risk: children with only one employed parent had nearly four times higher odds of infection (aOR = 3.97) and over four times higher odds of pathogenic protozoan infection (aOR = 4.33) in 2022 [11]. While handwashing before meals was a protective factor in 2019 (aOR = 0.10), this association was not significant in 2022, potentially indicating behavioral shifts during the pandemic. This case highlights how household-level socioeconomic pressures can be a more significant determinant of infection risk than individual hygiene practices in high-burden settings.
Experimental and Surveillance Methodologies
Robust epidemiological and laboratory protocols are fundamental to characterizing IPI endemicity. The following section details standardized methodologies cited in recent literature.
Cross-Sectional Survey Design and Sample Collection
Cross-sectional surveys are a cornerstone of IPI surveillance. The study in Simada, Ethiopia, provides a representative protocol [7].
- Participant Recruitment: A health facility-based cross-sectional study can be employed, recruiting participants who visit a central health clinic over a defined period (e.g., February to April 2023).
- Data Collection: A standardized, pre-tested questionnaire administered via interview collects data on socio-demographics (age, occupation, income), hygiene behaviors (handwashing habits, water source), and household environmental factors.
- Sample Collection and Transport: Each participant provides a fresh stool sample in a wide-mouthed, clean, leak-proof container. Samples are labeled with unique identifiers and transported in cool boxes to the parasitology laboratory for processing, ideally on the same day.
Laboratory Diagnostic Techniques
Accurate diagnosis is critical for surveillance and research. The following techniques are widely used, often in combination.
- Direct Wet Mount Microscopy: A small amount of stool is emulsified with a drop of saline (0.85% NaCl) and/or iodine on a microscope slide and examined under x10 and x40 objectives for motile trophozoites, cysts, oocysts, and helminth eggs. This method is rapid but has low sensitivity [7].
- Formol-Ether Concentration Technique (FECT): This sedimentation method increases the yield of parasites. An emulsified stool sample is filtered into a tube and mixed with formalin (to preserve) and ether (to dissolve fats and debris). The mixture is centrifuged, and the sediment is examined microscopically. This was a key method used in the Ethiopian study [7].
- Merthiolate-Iodine-Formaldehyde (MIF) Staining and Concentration: Used in the Eswatini cohort, the MIF method involves staining and fixing stool samples, which allows for the identification of eggs, cysts, and trophozoites, improving morphological differentiation [11].
- Molecular Methods (PCR): Molecular approaches, such as real-time polymerase chain reaction (PCR), offer superior sensitivity and specificity, and can differentiate between pathogenic and non-pathogenic species (e.g., E. histolytica vs. E. dispar). While not used in all field studies, they are considered the gold standard in research settings [3].
Diagram: Integrated Workflow for IPI Surveillance and Research. This diagram outlines the sequential and parallel processes in a comprehensive IPI study, from population definition to public health action, highlighting the integrated role of different diagnostic techniques. FECT: Formol-Ether Concentration Technique; MIF: Merthiolate-Iodine-Formaldehyde.
The Scientist's Toolkit: Research Reagent Solutions
A standardized set of reagents and materials is essential for conducting field and laboratory research on IPIs. The following table details key items and their applications based on the methodologies described in the search results.
Table 3: Essential Research Reagents and Materials for IPI Investigation
| Reagent/Material | Function/Application | Example Protocol/Note |
|---|---|---|
| Merthiolate-Iodine-Formaldehyde (MIF) Solution | Staining and preservation of parasitic elements (cysts, eggs, trophozoites) in stool samples for microscopic examination. | Used in the Eswatini cohort study [11]. Compatible with commercial kits (e.g., Para Quick). |
| Formalin (10% Buffered) | Primary fixative and preservative for stool samples, killing pathogens and stabilizing morphology for concentration techniques and biobanking. | Used in Formol-Ether Concentration Technique (FECT) [7]. |
| Diethyl Ether | Used in FECT to dissolve dietary fats and debris, clearing the sample and concentrating parasitic elements in the sediment. | Added to the formalin-fixed sample prior to centrifugation [7]. |
| Saline (0.85% NaCl) | Isotonic solution for creating direct wet mounts to observe motile trophozoites and for initial sample emulsification. | Used for initial microscopic screening [7]. |
| Lugol's Iodine Solution | Stains glycogen and nuclei of protozoan cysts, enhancing microscopic visualization and identification. | Applied in wet mount or as part of staining procedures like MIF. |
| DNA Extraction Kits (Stool-specific) | Isolation of high-quality genomic DNA from complex stool matrices for subsequent molecular assays. | Critical step prior to PCR. |
| PCR Master Mix & Species-Specific Primers/Probes | Amplification and detection of parasite-specific DNA sequences for highly sensitive and specific identification and differentiation. | Enables detection of pathogens like C. parvum and differentiation of E. histolytica from E. dispar [3]. |
Pathogen Transmission and Host Interaction Pathways
Understanding the life cycles and host interactions of intestinal protozoa is vital for developing effective interventions. The following diagram illustrates the key pathways from environmental transmission to disease outcome.
Diagram: IPI Transmission and Disease Pathway. This diagram maps the progression from underlying socioeconomic and environmental drivers, through faecal-oral transmission and pathogen-specific mechanisms, to acute and chronic health outcomes. Key risk factors from the analysis (poverty, poor sanitation) are shown as primary drivers.
The comparative analysis of regional hotspots for intestinal protozoan infections underscores a persistent and significant public health burden in tropical regions, directly linked to socioeconomic disparities. The high prevalence rates reported in countries like Malaysia, Eswatini, and Ethiopia—often exceeding 20% and reaching over 50% in specific districts—stand in stark contrast to the situation in developed nations [11] [4] [7]. The evidence clearly identifies poverty, inadequate sanitation, lack of access to clean water, and low education levels as the fundamental drivers of this endemicity. For researchers and drug development professionals, addressing this challenge requires a multi-faceted approach. This includes implementing robust surveillance using standardized protocols, developing and deploying point-of-care diagnostics, and pursuing new therapeutic agents. Furthermore, the findings advocate for integrated control strategies that extend beyond the health sector, encompassing improvements in water, sanitation, and hygiene (WASH) infrastructure and targeted health education. Sustained research efforts and evidence-based interventions are critical to reducing the disproportionate burden of these neglected infections and achieving global health equity.
The epidemiology of intestinal protozoan infections represents a significant field of study within global public health, particularly in resource-limited settings. These infections, caused by pathogenic protozoa such as Giardia duodenalis, Entamoeba histolytica, and Cryptosporidium spp., contribute substantially to the global burden of gastrointestinal diseases, especially among vulnerable populations in developing regions [14] [15]. The World Health Organization estimates that approximately 450 million people suffer from these infections, with disproportionate impacts on children in low- and middle-income countries where sanitation infrastructure and healthcare access remain limited [16] [13].
The transmission dynamics of intestinal protozoa are intricately linked to socioeconomic conditions, with poverty serving as a fundamental determinant of infection risk. These pathogens primarily spread through the fecal-oral route via contaminated water, food, environmental surfaces, and direct person-to-person contact [17] [18]. Consequently, populations experiencing inadequate water sanitation, poor hygiene practices, and limited education face elevated exposure risks, creating persistent cycles of infection and retransmission within communities [15] [19].
This technical guide examines the complex interrelationships between socioeconomic determinants and intestinal protozoan infection rates, with particular focus on poverty, educational attainment, and sanitation infrastructure. Through systematic analysis of current epidemiological data and research methodologies, this review aims to provide researchers and public health professionals with evidence-based insights to inform targeted intervention strategies and drug development priorities for high-risk populations.
Socioeconomic Determinants and Epidemiological Patterns
Poverty and Economic Status
Economic disadvantage consistently demonstrates a strong correlation with increased prevalence of intestinal protozoan infections across multiple geographical regions. Low income directly constrains access to essential resources including safe water, sanitary facilities, and healthcare services, thereby creating favorable conditions for parasite transmission and persistence.
Table 1: Economic Status and Protozoan Infection Rates
| Region | Economic Indicator | Infection Rate/Association | Primary Protozoa Identified |
|---|---|---|---|
| Egypt | Low socioeconomic status | RR = 2.4 (95% CI: 1.8-3.2) [19] | Entamoeba spp., Giardia duodenalis |
| MENA Region | Low income | Generally associated with higher parasitic infection rates [14] | Giardia lamblia, Blastocystis hominis |
| Eastern Tigrai, Ethiopia | Using well water (poverty proxy) | Significant risk factor (p<0.05) [15] | E. histolytica/dispar, G. duodenalis |
| Malaysia | Low income | 38-52% higher prevalence [13] | Entamoeba spp., Giardia lamblia |
| Ethiopia (University students) | Pocket money ≤347 Birr/month | Increased risk (AOR = 0.20 for higher income) [18] | E. histolytica/E. dispar |
The relationship between poverty and infection risk manifests through multiple pathways. In Egypt, a comprehensive meta-analysis revealed that children from low socioeconomic households had 2.4 times higher risk of intestinal parasitic infections compared to their more affluent counterparts [19]. Similarly, in the MENA region, low income was generally associated with higher rates of parasitic infections, particularly in Egypt, Palestine, Lebanon, and Iran [14]. The economic barrier extends beyond household resources to community-level infrastructure, as demonstrated in Eastern Tigrai, Ethiopia, where using well water as a drinking source – a marker of limited municipal water access – emerged as a significant risk factor for protozoan infections [15].
Educational Attainment
Education level, particularly maternal education, serves as a powerful determinant of intestinal protozoan infection risk through its influence on health knowledge, hygiene practices, and healthcare-seeking behaviors.
Table 2: Educational Factors and Infection Associations
| Region | Educational Factor | Association with Infection | Statistical Measure |
|---|---|---|---|
| Egypt | Low maternal education | RR = 1.62 [19] | Risk Ratio |
| MENA Region | Lower education levels | Higher infection rates (Egypt, Iran, Qatar) [14] | Significant association |
| Ethiopia (University students) | Educated father | Lower risk (AOR = 0.62, 95% CI: 0.12-0.86) [18] | Adjusted Odds Ratio |
| Sanandaj City, Iran | Parental education | No significant association [20] | P>0.05 |
| Malaysia | No formal education | 38-52% higher prevalence [13] | Pooled prevalence |
The protective effect of education demonstrates variability across different cultural and regional contexts. In Egypt, low maternal education was associated with a 1.62 times higher risk of intestinal parasitic infections in children [19]. Similarly, in the MENA region, individuals with lower education levels generally showed higher infection rates, though some studies reported no significant association, indicating potential mediating factors such as community-level health education programs or environmental conditions [14]. The relationship between paternal education and infection risk among Ethiopian university students further underscores the intergenerational educational influence on health outcomes, with students having educated fathers demonstrating significantly lower infection rates [18].
Sanitation and Hygiene Infrastructure
Water, sanitation, and hygiene (WASH) conditions represent critical environmental determinants of intestinal protozoan transmission, with inadequate infrastructure consistently associated with elevated infection prevalence across multiple studies.
Table 3: Sanitation and Hygiene-Related Risk Factors
| Risk Factor | Region | Associated Measure | Protozoa Involved |
|---|---|---|---|
| Poor handwashing after toilet use | Jalalabad, Afghanistan | AOR = 5.37 (95% CI: 2.34-12.31) [17] | Giardia lamblia, E. histolytica |
| Poor handwashing before eating | Jalalabad, Afghanistan | AOR = 6.65 (95% CI: 3.89-11.37) [17] | Giardia lamblia, E. histolytica |
| Unwashed raw vegetable consumption | Jalalabad, Afghanistan | AOR = 28.83 (95% CI: 5.50-151.03) [17] | Giardia lamblia, E. histolytica |
| Not having home latrine | Eastern Tigrai, Ethiopia | Significant risk factor (p<0.05) [15] | E. histolytica/dispar, G. duodenalis |
| Untreated water exposure | Malaysia | 38-52% higher prevalence [13] | Entamoeba spp., Giardia |
The impact of inadequate sanitation manifests most dramatically in conflict-affected and humanitarian settings. In Jalalabad, Afghanistan, researchers documented striking risk elevations associated with poor hygiene practices, including a 28.83-fold increased infection risk among children consuming unwashed raw vegetables and 6.65-fold higher risk among those with inadequate handwashing before eating [17]. The absence of home latrines in Eastern Tigrai, Ethiopia, significantly increased protozoan infection risk, highlighting the importance of basic sanitation infrastructure in interrupting fecal-oral transmission cycles [15]. These findings collectively underscore the fundamental role of WASH interventions in comprehensive protozoan infection control strategies.
Research Methodologies and Protocols
Field Study Design and Epidemiological Assessment
Conducting robust epidemiological research on socioeconomic determinants and intestinal protozoan infections requires meticulous study design and standardized protocols to ensure data comparability across different populations and regions.
Cross-sectional Survey Protocol: The predominant study design for investigating socioeconomic determinants of intestinal protozoan infections is the cross-sectional survey, which provides prevalence estimates at a specific point in time [20] [17] [15]. The standardized protocol includes:
- Stratified Random Sampling: Implement multistage stratified random sampling to ensure representative population coverage across diverse socioeconomic strata [17]. Administrative zones serve as primary stratification units, followed by random selection of schools or communities within each zone.
- Standardized Questionnaire Administration: Administer pre-tested, structured questionnaires to collect demographic and socioeconomic data [17] [15]. Key variables include household income, parental education and occupation, water source, sanitation facilities, housing conditions, and hygiene behaviors.
- Sample Size Calculation: Determine minimum sample sizes using single-proportion formula with 95% confidence level, 80% power, and 4-5% margin of error [17] [15]. Account for potential non-response rates by oversampling by 10%.
- Ethical Considerations: Obtain ethical approval from institutional review boards and secure informed consent from all participants or guardians [17]. Maintain confidentiality of participant data through anonymization and secure storage.
Cohort Study Design: Longitudinal cohort studies provide valuable insights into causal relationships between socioeconomic factors and infection incidence [19]. Implementation includes:
- Baseline Assessment: Document socioeconomic status and potential confounders before follow-up period.
- Regular Follow-up: Conduct repeated stool examinations and symptom assessments at predetermined intervals (typically 3-6 months).
- Incidence Calculation: Track new infections among initially negative participants to calculate incidence rates across different socioeconomic strata.
Laboratory Diagnostic Techniques
Accurate parasite identification and quantification are essential for reliable assessment of infection prevalence and intensity. Standardized laboratory protocols ensure comparability across studies.
Stool Sample Collection and Processing Protocol:
- Sample Collection: Distribute labeled, leak-proof containers to participants with instructions to collect approximately 2g of fresh stool [17] [15]. For liquid stools, collect 5-6mL samples. Ensure samples are processed within 30-60 minutes of collection or preserved appropriately.
- Macroscopic Examination: Document stool consistency, color, presence of mucus or blood before microscopic analysis [16].
- Direct Wet Mount Preparation:
- Prepare normal saline (0.9%) and Lugol's iodine solutions
- Emulsify rice grain-sized stool sample in saline on microscope slide
- Apply coverslip and examine systematically under 10x and 40x objectives
- Repeat procedure with iodine solution for cyst identification [16]
- Formalin-Ether Concentration Technique:
- Modified Acid-Fast Staining: For identification of Cryptosporidium spp. and Cyclospora cayetanensis:
- Prepare thin stool smears on microscope slides
- Fix with methanol for 3 minutes
- Flood with carbol fuchsin for 15 minutes
- Decolorize with acid-alcohol for 30 seconds
- Counterstain with methylene blue for 1 minute
- Examine under 100x oil immersion objective [16]
Quality Control Measures: Implement rigorous quality control procedures including:
- Parallel examination of samples by two trained microscopists
- Regular proficiency testing with known positive and negative samples
- Random re-examination of 10% of samples by senior technologist
- Calibration and maintenance of laboratory equipment [17] [15]
Data Analysis and Statistical Approaches
Robust statistical analysis is crucial for elucidating relationships between socioeconomic variables and infection outcomes while controlling for potential confounders.
Primary Analytical Framework:
- Prevalence Calculation: Compute overall and species-specific prevalence rates with 95% confidence intervals using the formula: Number positive/Total examined × 100 [17] [19].
- Bivariate Analysis: Conduct initial screening of associations between socioeconomic factors and infection status using Chi-square tests for categorical variables and t-tests for continuous variables [15].
- Multivariable Logistic Regression: Construct models to identify independent socioeconomic predictors while controlling for confounding variables [17] [19]. Include variables with p<0.20 from bivariate analysis in initial models, using backward elimination to retain significant predictors (p<0.05) in final models.
- Measures of Association: Report adjusted odds ratios (AORs) with 95% confidence intervals for significant predictors in final models [17].
Advanced Analytical Techniques:
- Meta-Analysis Methods: For systematic reviews, employ random-effects models using inverse variance weighting to calculate pooled prevalence estimates and risk ratios [19] [13]. Assess heterogeneity using I² statistic, with values >75% indicating substantial heterogeneity.
- Meta-Regression Analysis: Examine temporal trends in prevalence using meta-regression with publication year as continuous variable [19].
- Sensitivity Analysis: Evaluate robustness of findings using leave-one-out approach to determine if results are unduly influenced by individual studies [19].
Visualizing Transmission Pathways and Determinants
The complex relationships between socioeconomic determinants and intestinal protozoan infection risk can be visualized through a comprehensive transmission pathway diagram.
Figure 1: Socioeconomic Determinants of Intestinal Protozoan Infection Transmission Pathways. This diagram illustrates the complex pathways through which poverty, limited education, and inadequate sanitation infrastructure contribute to increased exposure and susceptibility to intestinal protozoan infections, ultimately leading to adverse health outcomes.
Research Reagents and Materials
Table 4: Essential Research Reagents for Protozoan Infection Studies
| Reagent/Material | Application | Technical Specifications | Research Context |
|---|---|---|---|
| Formalin (10%) | Stool preservation and concentration procedures | 100mL formaldehyde (37-40%) in 900mL distilled water; neutral buffered [17] [15] | Fixation of parasites for morphological preservation during transport and storage |
| Ethyl Acetate | Parasite concentration via formalin-ether technique | Laboratory grade, ≥99.5% purity [17] [15] | Lipid extraction and debris clarification in concentration methods |
| Carbol Fuchsin | Acid-fast staining of Cryptosporidium and Cyclospora | Basic fuchsin (0.3%), phenol (5%) in ethanol (10%) [16] | Differentiation of acid-fast intestinal protozoa from non-acid-fast organisms |
| Lugol's Iodine Solution | Staining of protozoan cysts for microscopy | Iodine (5%), potassium iodide (10%) in distilled water [16] | Enhanced visualization of internal cyst structures including nuclei and glycogen vacuoles |
| Microscope Slides and Coverslips | Preparation of wet mounts and stained smears | Pre-cleaned glass slides (75x25mm); #1 thickness coverslips (22x22mm) [17] | Standardized preparation for microscopic examination at 100x-400x magnification |
| Centrifuge | Parasite concentration procedures | Standard clinical centrifuge with 15mL tube capacity; adjustable 500-2000xg [15] | Sedimentation of parasites during formalin-ether concentration technique |
Discussion and Research Implications
The synthesized evidence demonstrates consistent and strong associations between socioeconomic determinants and intestinal protozoan infection rates across diverse geographical and cultural contexts. The interrelationships between poverty, education, and sanitation create complex pathways that perpetuate disproportionate disease burdens among disadvantaged populations.
Public Health and Research Implications
The epidemiological patterns observed across multiple studies highlight several critical considerations for public health interventions and future research directions. First, the consistent association between poverty and infection risk underscores the necessity of poverty alleviation as a fundamental component of parasitic disease control [14] [19]. Second, the variable protective effects of education across different regions suggest the importance of contextualized health education programs that address specific local knowledge gaps and behavioral practices [14] [18]. Third, the dramatic risk elevations associated with inadequate sanitation infrastructure emphasize the imperative of WASH investments as foundational public health measures [17] [15].
From a research perspective, several methodological considerations emerge. The heterogeneity in socioeconomic metrics across studies complicates direct comparisons and meta-analyses, highlighting the need for standardized socioeconomic indicators in parasitological research [14] [19]. Additionally, the complex interrelationships between different socioeconomic determinants necessitate multivariate analytical approaches that can elucidate independent effects while accounting for potential confounding [17] [19]. Future research should also prioritize longitudinal designs to establish temporal relationships and causal pathways between socioeconomic factors and infection risk.
Methodological Considerations and Limitations
Current research on socioeconomic determinants of intestinal protozoan infections faces several methodological challenges. The cross-sectional design predominant in existing literature provides valuable prevalence estimates but limits causal inference regarding socioeconomic risk factors [20] [17] [15]. The heterogeneity in socioeconomic measurement across studies complicates comparative analyses and meta-analytic approaches [14] [19]. Additionally, diagnostic sensitivity varies considerably between direct wet mount and concentration techniques, potentially underestimating true prevalence, particularly for low-intensity infections [17] [16].
Regional research gaps also present limitations, with disproportionate representation from certain endemic areas and underrepresentation of others [14] [19] [13]. Furthermore, many studies focus primarily on children or specific subpopulations, limiting generalizability to broader community contexts. Future research should address these limitations through standardized socioeconomic metrics, optimized diagnostic approaches incorporating molecular methods where feasible, and expanded geographical coverage to include underrepresented endemic regions.
This technical review establishes robust evidence linking socioeconomic determinants—particularly poverty, limited education, and inadequate sanitation—to increased risk of intestinal protozoan infections. The synthesized data demonstrate that economically disadvantaged populations face substantially elevated infection risks, with low income associated with 2.4-fold higher infection rates in Egypt [19], and specific hygiene-related practices showing even more dramatic risk elevations in high-transmission settings like Afghanistan [17].
The relationships between these determinants operate through complex pathways involving constrained resources, limited health knowledge, and inadequate infrastructure that collectively increase exposure frequency and decrease protective behaviors. Effective intervention strategies must address these interconnected determinants through multidimensional approaches that combine poverty alleviation, educational investment, and sanitation infrastructure development.
For researchers and drug development professionals, these findings highlight the importance of considering socioeconomic context in clinical trial design, intervention development, and public health programming. Future research should prioritize standardized socioeconomic metrics, longitudinal designs to establish causal pathways, and intervention studies that address multiple determinants simultaneously. Through integrated approaches that address both biological and social determinants of health, substantial progress can be made toward reducing the disproportionate burden of intestinal protozoan infections among vulnerable populations worldwide.
Intestinal protozoan infections, primarily caused by Entamoeba histolytica, Giardia lamblia, and Cryptosporidium species, represent a significant global health burden, disproportionately affecting specific population groups. These infections are transmitted via the fecal-oral route through contaminated food, water, or direct contact, causing symptoms ranging from self-limiting diarrhea to severe, life-threatening complications [21] [22] [13]. Current global estimates indicate approximately 3.5 billion people are affected, with around 450 million individuals currently symptomatic [21] [22]. This technical review examines the epidemiological evidence defining children, immunocompromised individuals, and Indigenous communities as high-risk populations, analyzes the biological and socioeconomic factors driving vulnerability, and outlines essential research methodologies for advancing evidence-based interventions within public health frameworks.
Epidemiological Profile of Major Intestinal Protozoa
The three primary protozoan pathogens responsible for the majority of intestinal infections demonstrate distinct geographical distributions and clinical manifestations, yet collectively contribute to substantial disease burden across vulnerable populations.
Table 1: Characteristics of Major Intestinal Protozoan Pathogens
| Pathogen | Disease | Key Clinical Manifestations | At-Risk Populations | Global Burden |
|---|---|---|---|---|
| Entamoeba histolytica | Amoebiasis | Abdominal pain, bloody diarrhea, fever, liver abscesses | Children, Indigenous communities | 50 million annual cases; 100,000 deaths [21] [22] |
| Giardia lamblia | Giardiasis | Watery diarrhea, abdominal pain, flatulence, weight loss | Children in tropical regions | ~200 million annual infections [21] [22] |
| Cryptosporidium spp. | Cryptosporidiosis | Watery diarrhea, stomach cramps, nausea, vomiting | Immunocompromised individuals, children | Prevalence: 13% (India), 7.3% (Thailand) in children [21] [22] |
Vulnerability Analysis of High-Risk Populations
Pediatric Vulnerability
Children, particularly those under five years of age, bear a disproportionate burden of intestinal protozoan infections due to a combination of immunological, behavioral, and environmental factors. In Malaysia, diarrheal diseases remain a leading cause of mortality in children under 5, with a reported mortality rate of 0.8% in 2019 [21] [22]. A recent systematic review and meta-analysis of intestinal protozoal infections in Malaysia identified children under 15 years as having significantly higher pooled prevalence rates, between 38% and 52%, with the highest burden observed among indigenous pediatric populations [13].
The increased susceptibility in children stems from several key factors:
- Immature immune systems: Developing adaptive immunity limits capacity to combat protozoan pathogens effectively
- Behavioral factors: Poor hand hygiene practices and frequent hand-to-mouth contact increase ingestion of infectious cysts
- Environmental exposure: Higher likelihood of contact with contaminated soil and water during play
- Nutritional status: Pre-existing malnutrition compromises intestinal barrier function and immune competence
Immunocompromised Individuals
Immunocompromised patients, particularly those with HIV/AIDS, organ transplants, or immunosuppressive therapy, experience more severe and prolonged manifestations of intestinal protozoan infections. Cryptosporidiosis demonstrates particularly aggressive courses in immunocompromised hosts, with potential for chronic, life-threatening diarrhea and extra-intestinal dissemination [13].
Malaysian studies have documented the heightened vulnerability in immunocompromised populations:
- HIV-positive inmates demonstrated 27.5% prevalence of intestinal parasitic infections compared to 25.8% in HIV-negative inmates [13]
- Intravenous drug users with HIV showed increased rates of cryptosporidiosis, though often asymptomatic [13]
- The clinical severity of infection correlates with degree of immunosuppression, particularly CD4+ T-cell counts in HIV patients
The pathophysiological mechanisms underlying increased severity in immunocompromised hosts include:
- Defective cell-mediated immunity: Crucial for controlling intracellular protozoa like Cryptosporidium
- Reduced IgA secretion: Compromises mucosal barrier function in the gastrointestinal tract
- Dysregulated inflammatory responses: May lead to excessive tissue damage or inadequate pathogen clearance
Indigenous Communities
Indigenous populations globally experience disproportionate burdens of intestinal protozoan infections, driven by historical, socioeconomic, and structural determinants of health. The COVID-19 pandemic highlighted persistent health inequities, with Native Americans experiencing 2.1-times higher mortality compared to White Americans [23]. Similar disparities exist for other infectious diseases, reflecting systemic factors rather than biological susceptibility.
Table 2: Documented Health Disparities in Indigenous Populations
| Health Indicator | Indigenous Population | Comparison Population | Disparity Measure |
|---|---|---|---|
| COVID-19 mortality | Native Americans | White Americans | 2.1-times higher [23] |
| Influenza hospitalization | First Nations (Canada) | General Canadian population | 4-5-times higher [23] |
| RSV hospitalization | Inuit infants (Nunavut) | Temperate region infants | 484 vs. 27 per 1,000 [23] |
| Invasive infection ICU admissions | Indigenous children (Australia) | Non-Indigenous children | 47.6 vs. ~17.3 per 100,000 [24] |
The structural determinants driving these disparities include:
- Inadequate infrastructure: Lack of access to clean water and sanitation facilities in many Indigenous communities
- Household crowding: Facilitates fecal-oral transmission of pathogens
- Poverty and food insecurity: Higher prevalence of underlying comorbidities that worsen infection outcomes
- Historical trauma and systemic discrimination: Creates barriers to healthcare access and undermines trust in health systems
- Underfunded health services: Limited capacity for prevention, diagnosis, and treatment
In Malaysia, studies documented a 27% prevalence of intestinal protozoan infections in indigenous communities, compared to 23% in local rural communities [13]. Subnational analysis revealed the highest prevalence in Kelantan state (39%), followed by Perak (29%), with urban centers like Selangor and Kuala Lumpur reporting lower rates (13.6%) [13].
Research Methodologies and Experimental Protocols
Systematic Review and Meta-Analysis Protocol
Recent comprehensive reviews have established rigorous methodologies for synthesizing epidemiological data on intestinal protozoan infections [21] [22] [13]. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) framework provides standardized guidelines for conducting and reporting systematic reviews in this field.
Table 3: Key Methodological Components for Systematic Reviews of Intestinal Protozoan Infections
| Component | Specifications | Application Examples |
|---|---|---|
| Search Strategy | Multi-database search (PubMed/MEDLINE, Scopus, Web of Science, Google Scholar, Cochrane); No language restrictions; Inclusion of grey literature | Search terms: medical subject headings (MeSH) + free-text for giardiasis, cryptosporidiosis, amoebiasis, prevalence, epidemiology, risk factors [21] [22] |
| Eligibility Criteria | Studies with original data; Human subjects; Specific diagnostic methods; Defined timeframes (e.g., 2010-2024) | Exclusion of case reports, reviews; Focus on E. histolytica, G. lamblia, Cryptosporidium spp. [21] [22] [13] |
| Risk of Bias Assessment | Joanna Briggs Institute tools; Newcastle-Ottawa Scale | Evaluation of selection, detection, and reporting biases in included studies [21] [22] |
| Data Synthesis | Random effects model; Pooled prevalence with 95% CI; Subgroup analysis; Meta-regression | Calculation of overall prevalence; Analysis by region, population, diagnostic method [13] |
The following workflow diagram illustrates the systematic review process:
Diagnostic Methodologies
Accurate diagnosis of intestinal protozoan infections requires appropriate methodological selection based on clinical context, available resources, and research objectives. The following diagram illustrates the diagnostic workflow:
Table 4: Diagnostic Methods for Intestinal Protozoan Infections
| Method | Principles | Advantages | Limitations | Applications |
|---|---|---|---|---|
| Microscopy | Direct visualization of cysts/trophozoites in stool samples | Low cost; Widely available; Can detect multiple parasites | Low sensitivity; Requires expertise; Cannot differentiate species | Initial screening; Resource-limited settings [21] [22] |
| Immunoassays | Detection of parasite-specific antigens in stool | Higher sensitivity than microscopy; Rapid tests available | Species-specific; Limited multiplexing | Outbreak investigations; Clinical diagnostics [21] [22] |
| Molecular Methods (PCR, qPCR) | Amplification of parasite-specific DNA sequences | High sensitivity and specificity; Species differentiation; Quantification possible | Higher cost; Technical expertise required; Equipment needs | Research; Surveillance; Species confirmation [21] [22] [13] |
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents for Intestinal Protozoan Research
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Stool Preservation Solutions | 10% Formalin, Sodium acetate-acetic acid-formalin (SAF), Polyvinyl alcohol (PVA) | Maintain parasite morphology for microscopy; Preserve nucleic acids for molecular assays | Choice affects downstream applications; Formalin-fixed samples suitable for microscopy and PCR [21] [22] |
| DNA/RNA Extraction Kits | Commercial kits with bead-beating steps (mechanical disruption) | Break cyst walls to release nucleic acids; Purify DNA/RNA for molecular assays | Mechanical disruption crucial for efficient extraction; Inhibitor removal essential for clinical samples [21] [22] [13] |
| PCR Master Mixes | Multiplex real-time PCR kits; Conventional PCR reagents | Simultaneous detection of multiple pathogens; Species differentiation; Quantification | Multiplexing requires careful primer/probe design; Include internal controls to detect inhibition [21] [22] [13] |
| Primary Antibodies | Species-specific monoclonal antibodies (e.g., anti-Giardia cyst wall protein) | Immunofluorescence; ELISA development; Histological detection | Commercial availability varies by species; Cross-reactivity testing required [21] [22] |
| Reference Genomic DNA | ATCC reference strains for each protozoan species | Positive controls for molecular assays; Assay validation; Quality control | Essential for validating in-house PCR assays; Confirms specificity and sensitivity [21] [22] [13] |
The epidemiological evidence clearly identifies children, immunocompromised individuals, and Indigenous communities as disproportionately affected by intestinal protozoan infections. Biological factors, including immune status and developmental stage, interact with socioeconomic determinants, such as poverty, inadequate sanitation, and limited healthcare access, to create intersecting vulnerabilities. The pooled prevalence of 24% identified in the Malaysian systematic review underscores the substantial disease burden in endemic regions, with even higher rates (27%) documented among Indigenous populations [13]. Addressing these disparities requires multifaceted approaches combining improved diagnostic methodologies, targeted public health interventions, and research that specifically addresses the structural determinants of health in vulnerable communities. Future research priorities should include development of point-of-care diagnostics, implementation research on effective intervention delivery, and community-engaged studies that prioritize Indigenous knowledge and self-determination in research partnerships.
Intestinal protozoan infections represent a significant global health burden, affecting billions of individuals worldwide and causing substantial morbidity and mortality, particularly in vulnerable populations and resource-limited settings [3] [4]. The transmission dynamics of these pathogens are complex, involving multiple interconnected pathways including waterborne, foodborne, and zoonotic routes. Understanding these dynamics is fundamental to developing effective public health interventions, diagnostic approaches, and therapeutic strategies. This technical guide provides an in-depth examination of the transmission mechanisms, epidemiological patterns, and laboratory methodologies relevant to major intestinal protozoa, with a specific focus on Entamoeba histolytica, Giardia lamblia (also known as G. duodenalis or G. intestinalis), and Cryptosporidium species [3] [25]. These pathogens collectively contribute to a substantial portion of the global intestinal protozoal infection burden, with an estimated 3.5 billion people affected and approximately 450 million currently experiencing active infections [3] [4]. The epidemiological significance of these parasites extends beyond their prevalence, as they are responsible for severe diarrheal diseases, nutritional deficiencies, and impaired cognitive development in children, creating a cycle of disease and poverty that disproportionately affects developing regions [4] [25].
Major Pathogens and Clinical Manifestations
The clinical presentation of intestinal protozoal infections varies significantly based on the causative organism, infectious dose, and host immune status. Entamoeba histolytica, the causative agent of amoebiasis, invades the intestinal mucosa leading to characteristic symptoms such as abdominal pain, bloody diarrhea (dysentery), fever, and in severe cases, liver abscesses [3] [25]. The organism's ability to form flask-shaped ulcers in the colonic mucosa and disseminate to extra-intestinal sites represents a significant virulence mechanism that distinguishes it from non-pathogenic amoeba species [25]. Giardia lamblia causes giardiasis, which typically presents with abundant, foul-smelling, watery diarrhea, abdominal pain, flatulence, and weight loss without invasive disease [3] [25]. The parasite attaches to the intestinal epithelium without tissue invasion, but induces malabsorption and nutrient deficiency through mechanisms that remain partially understood [25].
Cryptosporidium species, particularly C. parvum and C. hominis, cause cryptosporidiosis, which manifests as watery diarrhea accompanied by stomach cramps, nausea, vomiting, and fever [3] [4]. This pathogen poses a particularly severe threat to immunocompromised individuals, including those with HIV/AIDS, where infections can become chronic, life-threatening, and refractory to treatment [4]. The parasite's unique intracellular but extracytoplasmic localization within host epithelial cells contributes to its resistance to many conventional antiprotozoal therapies and enables robust environmental transmission through highly resistant oocysts [25].
Table 1: Major Intestinal Protozoan Pathogens and Clinical Features
| Pathogen | Disease | Primary Symptoms | Severe Complications | High-Risk Populations |
|---|---|---|---|---|
| Entamoeba histolytica | Amoebiasis | Bloody diarrhea, abdominal pain, fever | Liver abscess, amoeboma, perforation | All age groups, tropical regions |
| Giardia lamblia | Giardiasis | Watery diarrhea, abdominal pain, flatulence, weight loss | Malabsorption syndrome, chronic diarrhea | Children, travelers, immunocompromised |
| Cryptosporidium spp. | Cryptosporidiosis | Watery diarrhea, stomach cramps, nausea, vomiting | Protracted diarrhea, biliary involvement | HIV/AIDS, young children |
| Toxoplasma gondii | Toxoplasmosis | Often asymptomatic, flu-like symptoms | Congenital defects, encephalitis in immunocompromised | Fetus, HIV/AIDS, transplant recipients |
The differential diagnosis of these infections is challenging because most enteric pathogens cause similar symptomatology, leading to potential misidentification without proper laboratory confirmation [3] [4]. Multiple infectious agents can cause acute gastroenteritis, and contamination may originate from food, water, the environment, or animals, further complicating epidemiological analysis and outbreak investigations [4]. The severity of disease ultimately depends on the immune status of affected individuals, with immunocompromised patients experiencing more severe and protracted illnesses [3].
Transmission Pathways and Epidemiology
Waterborne Transmission
Waterborne transmission represents a predominant pathway for the global dissemination of intestinal protozoan pathogens, particularly Giardia and Cryptosporidium [26]. These organisms produce environmentally resistant cysts (for Giardia and Entamoeba) or oocysts (for Cryptosporidium) that can survive for extended periods in water and are highly resistant to conventional water treatment methods, including chlorine-based disinfection [26]. A comprehensive review of global waterborne protozoan outbreaks from 2017 to 2020 identified 251 outbreaks worldwide, with the majority (57.77%) occurring in the Americas, followed by Europe (29.48%), Oceania (11.16%), and Asia (1.59%) [26]. The disproportionate representation of developed countries in these statistics reflects their advanced diagnostic capabilities and surveillance systems rather than actual higher incidence, highlighting significant surveillance bias and underreporting in resource-limited regions [26].
Recreational water venues, including swimming pools, water parks, and interactive fountains, have emerged as significant transmission vehicles in developed countries, primarily due to inadequate disinfection and contamination events [26]. The robust nature of protozoan cysts and oocysts enables their survival in properly chlorinated water, facilitating point-source outbreaks that can affect numerous individuals simultaneously. Additionally, drinking water contamination continues to pose a substantial threat, particularly in regions with compromised water treatment infrastructure or agricultural runoff that introduces zoonotic strains into water sources [26]. The traditional water treatment processes, including coagulation, sedimentation, filtration, and disinfection, have demonstrated variable efficacy against protozoan parasites, with filtration representing the most reliable barrier against these pathogens [26].
Foodborne Transmission
Foodborne transmission of intestinal protozoa occurs through the contamination of raw or ready-to-eat foods with infective cysts or oocysts, typically via contact with contaminated water, soil, or infected food handlers practicing poor personal hygiene [3] [4]. Fresh produce, including leafy greens, berries, and herbs, represents a particularly high-risk commodity due to potential contamination at multiple points along the production chain, from irrigation with contaminated water to processing and preparation [4]. The robust nature of protozoan transmission stages enables their survival on food surfaces and resistance to various food preservation methods, including refrigeration and mild disinfectants.
Foodborne outbreaks often prove challenging to investigate and attribute to specific protozoan pathogens due to several factors: the relatively low infectious doses required for some species (as few as 10-100 cysts for Giardia); the prolonged incubation periods that complicate traceback investigations; and the limited implementation of protozoan testing in routine food safety monitoring programs [4]. Molecular typing methods have enhanced our ability to link clinical, food, and environmental isolates during outbreak investigations, providing valuable insights into transmission chains and contamination sources.
Zoonotic and Environmental Transmission
Zoonotic transmission represents a significant pathway for several intestinal protozoa, particularly Cryptosporidium and Giardia, which infect a broad range of animal hosts in addition to humans [27] [28]. Cattle have been identified as important reservoirs for zoonotic Cryptosporidium and Giardia species and genotypes, establishing these animals as significant sources of human-infectious strains [27]. A recent study conducted in Kazakhstan demonstrated high prevalence rates of Cryptosporidium spp. (49.2%) in calves aged 1-30 days, with a subsequent dramatic decline in older animals, highlighting age-dependent susceptibility and the potential for environmental contamination from agricultural operations [27]. Similarly, Giardia spp. infections were detected in 5.2% of the youngest calves, with more even distribution across age groups [27].
Companion animals also contribute to zoonotic transmission cycles, with dogs and cats serving as reservoirs for several protozoan pathogens [28]. In the United States, where over 77 million dogs and 93 million cats share households with humans, pets play a significant role in the epidemiology of zoonotic parasites [28]. Toxoplasma gondii, with a seroprevalence ranging from 18-80% in U.S. cats depending on geographic location, represents a particularly important zoonotic threat, especially to pregnant women and immunocompromised individuals [28]. Cats serve as definitive hosts for T. gondii, shedding millions of oocysts following primary infection and contaminating soil, water, and agricultural products [28].
Table 2: Global Prevalence and Outbreak Patterns of Major Intestinal Protozoa
| Pathogen | Global Burden | Regional Prevalence Variations | Dominant Transmission Routes | Notable Outbreak Settings |
|---|---|---|---|---|
| Entamoeba histolytica | 50 million invasive cases annually, 100,000 deaths [3] | Up to 25% in low-income countries [4] | Waterborne, foodborne, person-to-person | Areas with poor sanitation, institutions |
| Giardia lamblia | ~200 million cases annually [3] | 1.1-2.1% in children in temperate countries; higher in tropics [3] | Waterborne, foodborne, zoonotic | Childcare centers, recreational water venues |
| Cryptosporidium spp. | Leading cause of waterborne outbreaks [26] | 4.3% in developed countries, 10.4% in developing nations [27] | Waterborne, zoonotic, person-to-person | Recreational water facilities, contaminated drinking water |
| Toxoplasma gondii | ~30-40% global seroprevalence in cats [28] | 9% seroprevalence in US (6-49 year olds) [28] | Foodborne (undercooked meat), environmental oocysts | Community outbreaks linked to environmental contamination |
Environmental factors significantly influence transmission dynamics, with climate, seasonality, and sanitation infrastructure serving as important determinants of infection risk [27] [26]. The persistence of protozoan cysts and oocysts in the environment is enhanced under cool, moist conditions, while extreme temperatures and desiccation can reduce viability. Seasonal variations in infection rates have been documented for several protozoa, often corresponding to rainfall patterns that influence both water contamination levels and human water-use behaviors [27].
Diagnostic Methodologies and Laboratory Protocols
Specimen Collection and Processing
The accurate diagnosis of intestinal protozoal infections begins with proper specimen collection, handling, and processing. Fresh stool specimens represent the primary sample type for diagnosing most intestinal protozoa, with collection protocols requiring careful attention to timing, preservation, and transport conditions to maintain parasite viability and morphological integrity [25]. Multiple specimens collected over several days are often necessary to maximize detection sensitivity due to the intermittent shedding characteristic of many protozoan species [25]. Preserved stool specimens in fixatives such as sodium acetate-acetic acid-formalin (SAF) or polyvinyl alcohol (PVA) are essential for maintaining morphological features for microscopic identification and enabling batch testing in clinical laboratories [25].
Concentration techniques represent a critical step in diagnostic protocols for intestinal protozoa, significantly enhancing detection sensitivity by increasing the number of organisms available for examination. The two primary concentration methods employed in clinical laboratories are flotation techniques and sedimentation procedures [27] [25]. Flotation methods, including zinc sulfate (ZnSO₄) and sucrose solutions, exploit the lower specific gravity of protozoan cysts and oocysts compared to the flotation medium, causing them to rise to the surface where they can be collected for examination [27]. Sedimentation techniques, such as formalin-ethyl acetate concentration, rely on centrifugation to concentrate parasites in the sediment while removing debris through ethyl acetate extraction [25]. Each method offers distinct advantages for different protozoan species, with flotation techniques particularly effective for Giardia and Cryptosporidium, while sedimentation methods preserve the morphological details critical for Entamoeba identification [25].
Microscopic Examination
Microscopic examination remains a cornerstone of intestinal protozoan diagnosis, providing a cost-effective method for parasite detection and morphological identification that is accessible to laboratories with limited resources [25]. Both direct wet mounts and permanently stained smears are essential components of comprehensive parasitological examination [25]. Direct wet mounts prepared from fresh or concentrated stool specimens enable detection of motile trophozoites (for E. histolytica and Giardia) and provide initial information about cyst and oocyst morphology [25]. The addition of iodine to wet mounts enhances internal structural details, facilitating species identification based on characteristic features such as nuclear number and position, inclusion bodies, and overall cyst size and shape [25].
Permanent staining with trichrome or iron-hematoxylin provides superior morphological detail for species identification and represents an essential procedure for differentiating Entamoeba histolytica from non-pathogenic amoeba species [25]. These staining techniques highlight nuclear characteristics, including chromatin pattern, karyosome position, and nuclear size, which represent critical diagnostic features for amoeba identification [25]. For Cryptosporidium and other coccidian parasites, modified acid-fast staining demonstrates variable staining characteristics (pink to red against a blue or green background) that facilitate detection and differentiation from other stool components [25]. Despite its utility, microscopic examination requires substantial expertise, exhibits inter-technologist variability, and has limited sensitivity for low-level infections, necessitating complementary diagnostic approaches in many clinical scenarios [25].
Immunological and Molecular Detection Methods
Immunoassay techniques have significantly advanced the diagnosis of intestinal protozoal infections by providing improved sensitivity and specificity compared to microscopic methods alone [3]. Enzyme immunoassays (EIAs) and direct fluorescent antibody (DFA) tests targeting parasite-specific antigens have become established methods for detecting Giardia, Cryptosporidium, and Entamoeba histolytica in stool specimens [25]. DFA tests combine highly specific fluorescent-labeled antibodies with morphological assessment, offering excellent sensitivity and specificity for Giardia and Cryptosporidium while providing a permanent record for quality assurance [25]. Rapid cartridge-style immunochromatographic assays provide point-of-care testing capabilities with minimal training requirements, making them valuable in resource-limited settings and outbreak investigations [25].
Molecular methods based on nucleic acid amplification techniques, particularly polymerase chain reaction (PCR) and multiplexed panels, represent the current gold standard for sensitive and specific detection and differentiation of intestinal protozoa [3] [25]. Real-time PCR assays offer exceptional sensitivity, species-specific identification, and quantification capabilities, while requiring only a single stool sample for testing multiple pathogens [3]. Multiplex PCR panels allow simultaneous detection of numerous gastrointestinal pathogens from a single specimen, significantly streamlining the diagnostic process for patients with diarrheal illness [25]. The high sensitivity of molecular methods is particularly valuable for detecting low-level infections, identifying pathogens in convalescent patients with minimal parasite shedding, and conducting epidemiological studies to understand true community prevalence [3]. Molecular techniques also enable genotype discrimination, providing valuable information for outbreak investigations and understanding transmission dynamics between human and animal reservoirs [27].
Diagram 1: Comprehensive diagnostic workflow for intestinal protozoan infections demonstrating the integration of traditional and modern detection methodologies.
Research Reagent Solutions and Experimental Tools
Advancing research on transmission dynamics of intestinal protozoa requires specialized reagents and experimental tools that enable precise detection, characterization, and investigation of these pathogens. The following table summarizes essential research reagents and their applications in studying waterborne, foodborne, and zoonotic transmission pathways.
Table 3: Essential Research Reagents for Studying Protozoan Transmission Dynamics
| Reagent/Category | Specific Examples | Research Applications | Function in Experimental Protocols |
|---|---|---|---|
| Nucleic Acid Extraction Kits | ZR BashingBead Lysis Tubes, Chemagic DNA Blood 400 Kit H96 [29] | DNA isolation from stool, water, food, and vectors | Mechanical and chemical lysis for downstream molecular detection and genotyping |
| Molecular Detection Reagents | qPCR master mixes, primers targeting parasite-specific genes (satellite DNA, mini-exon, 18S rRNA) [29] | Pathogen detection and quantification in clinical, environmental samples | Amplification and quantification of parasite DNA; determination of parasitic load |
| Genotyping Reagents | Oxford Nanopore Ligation Sequencing Kits, barcoding primers [29] | Strain typing, transmission tracking, phylogenetic analysis | Next-generation sequencing for DTU identification and outbreak strain discrimination |
| Immunological Reagents | Fluorescent-labeled antibodies, EIA kits for cyst wall antigens [25] | Species-specific detection in clinical and environmental samples | Immunofluorescence microscopy; high-throughput screening of water/food samples |
| Culture Media | Axenic media for in vitro parasite propagation [25] | Isolation, virulence studies, drug screening | Maintenance of parasite stocks; generation of biological material for experiments |
| Filtration Systems | Water sampling filters, concentration devices [26] | Environmental surveillance, water testing | Capture and concentration of cysts/oocysts from large water volumes |
| Staining Reagents | Trichrome, modified acid-fast stains, fluorescent vital dyes [25] | Microscopic identification, viability assessment | Morphological differentiation; determination of infectivity in environmental samples |
The development and application of these research tools have significantly advanced our understanding of protozoan transmission dynamics. Molecular detection reagents, particularly those designed for quantitative PCR, enable not only sensitive pathogen detection but also quantification of parasitic load, which correlates with transmission potential and disease severity [29]. Genotyping reagents facilitate discrimination of discrete typing units (DTUs) and strains, providing critical information for tracking outbreak sources, understanding zoonotic transmission, and identifying imported versus locally acquired infections [29]. The integration of these tools into multidisciplinary research approaches has enabled significant advances in characterizing transmission networks and identifying critical control points for intervention.
The transmission dynamics of intestinal protozoan parasites through waterborne, foodborne, and zoonotic pathways represent a complex interplay between pathogen biology, environmental factors, and human behaviors. The robust nature of protozoan cysts and oocysts enables their persistence in various environments and resistance to conventional control measures, facilitating their global distribution and substantial public health impact [26]. Understanding these transmission pathways is essential for developing evidence-based interventions that effectively reduce the burden of intestinal protozoal infections in human populations. Current research priorities include enhancing detection methods for environmental surveillance, elucidating the mechanisms of zoonotic transmission, developing more effective water treatment technologies, and integrating molecular typing into public health surveillance systems to better understand and interrupt transmission networks. As climate change, urbanization, and agricultural intensification continue to alter environmental conditions and human-parasite interactions, ongoing investigation into the transmission dynamics of intestinal protozoa will remain critical for protecting global public health.
From Microscopy to Molecular Assays: A Toolkit for Protozoan Detection and Surveillance
Within the epidemiology of intestinal protozoan infections, accurate diagnosis is the cornerstone of effective disease surveillance, outbreak control, and drug development. Despite advancements in molecular and immunodiagnostic methods, conventional techniques based on microscopy and staining remain the operational backbone in both routine laboratories and field studies, particularly in resource-limited settings where the burden of these infections is highest [30] [31]. These techniques provide a direct, relatively inexpensive, and immediate method for detecting parasitic elements. This whitepaper provides an in-depth technical assessment of these conventional methods, detailing their protocols, performance characteristics, and enduring utility in epidemiological research and public health.
The Role of Conventional Diagnostics in Epidemiological Workflows
In the context of epidemiological research, the primary objectives of diagnostic testing are to accurately identify the causative agent, determine prevalence, monitor transmission dynamics, and evaluate the impact of interventions. The workflow for diagnosing intestinal protozoa typically begins with microscopic examination of stool specimens, which can be performed using a variety of preparation and staining techniques depending on the target organism and the goals of the survey [30] [32].
The diagram below illustrates the pivotal role of conventional diagnostics within a broader epidemiological research framework.
Critical Staining Techniques and Their Diagnostic Utility
A variety of stains are employed to enhance the visualization and differentiation of intestinal protozoa. Each stain has distinct advantages and is suited for specific parasites. The table below provides a comparative overview of key staining techniques and their applications for major pathogenic protozoa.
Table 1: Staining Techniques for Key Intestinal Protozoa
| Organism | Recommended Stains & Techniques | Key Morphological Features | Diagnostic Utility & Notes |
|---|---|---|---|
| Entamoeba histolytica | Wet mount, Trichrome, Periodic Acid-Schiff (PAS) [32] | Trophozoite: 10-60 µm; Cyst: 10-20 µm. Trophozoites may contain ingested RBCs [32]. | Trichrome is standard for permanent stains. PAS is used in tissue biopsies. Cannot be morphologically distinguished from E. dispar without additional tests [30]. |
| Giardia duodenalis | Wet mount, Trichrome, Hematoxylin, Lugol's Iodine, ELISA [32] | Trophozoite: 9-21 µm; Cyst: 7-12 µm. Characteristic falling-leaf motility of trophozoites in wet mounts [32]. | Direct wet mount is preferred for initial screening. ELISA for antigen detection is now common, with 92-98% sensitivity and 87-100% specificity [32]. |
| Cryptosporidium spp. | Modified Acid-Fast, Auramine-Rhodamine [30] [32] | Oocysts: 2-5 µm. Stain bright red with Modified Acid-Fast against a blue/green background; may appear as "ghost" cells [30]. | Sensitivity of a single modified acid-fast stain is low (~54.8%); multiple specimens improve yield [30]. |
| Cyclospora cayetanensis | Modified Acid-Fast, Wet mount [32] | Oocysts: 8-10 µm. Autofluoresce under UV light [32]. | Differentiated from Cryptosporidium by larger size. |
| Cystoisospora belli | Wet mount, Modified Acid-Fast [32] | Oocysts: 30x12 µm [32]. | - |
| Microsporidia | Modified Trichrome, Fluorescence Methods [33] [32] | Spores: 1-2 µm. Very small, can be misinterpreted as fecal debris [32]. | Modified trichrome is the primary screening method. Fluorescence brighteners enhance detection [33]. |
| Dientamoeba fragilis | Iron Hematoxylin, Trichrome [32] | Trophozoite: 7-12 µm. No cystic stage [32]. | Examination of permanently stained slides from fresh or preserved specimens is essential. |
Detailed Experimental Protocols for Key Techniques
For researchers and laboratory professionals, standardized protocols are vital for ensuring consistent and comparable results across studies. The following section provides detailed methodologies for critical diagnostic procedures.
Direct Wet Mount Examination
The direct wet mount is a fundamental, rapid technique for observing motile trophozoites and parasitic structures.
- Principle: To identify motile trophozoites and cysts in near-native state, providing immediate diagnostic clues [32].
- Materials: Fresh stool specimen, physiological saline (0.85% NaCl), Lugol's iodine solution, microscope slides, coverslips, compound microscope.
- Procedure:
- Saline Mount: Place a drop of physiological saline on one end of a clean microscope slide. Emulsify a small portion of stool (about 2 mg) in the saline. Apply a coverslip.
- Iodine Mount: Place a drop of Lugol's iodine on the other end of the same slide. Emulsify a separate portion of the same stool sample in the iodine. Apply a coverslip.
- Examination: Systematically scan the entire area under the coverslip using the 10x objective. Switch to the 40x objective for detailed observation of morphology. Examine the saline mount first for motility, then the iodine mount to observe nuclear detail and confirm cyst identification.
- Technical Notes: The entire preparation must be examined within 30-60 minutes of collection to observe trophozoite motility and prevent disintegration. Lugol's iodine stains glycogen masses and nuclei but kills trophozoites [32].
Formalin-Ethyl Acetate Sedimentation Technique (FECT)
This concentration method increases the sensitivity of detection by removing debris and concentrating parasitic elements.
- Principle: To separate and concentrate parasitic cysts, oocysts, and eggs from fecal debris using formalin fixation and ethyl acetate extraction [34].
- Materials: 10% formalin, ethyl acetate, centrifuge tubes, centrifuge, applicator sticks, gauze or strainers, iodine stain.
- Procedure:
- Emulsification: Emulsify 1-2 g of stool in 3-4 mL of 10% formalin in a centrifuge tube. For formed stools, let it stand for 30 minutes for fixation.
- Filtration and Sedimentation: Filter the suspension through gauze into a new centrifuge tube. Add 3-4 mL of ethyl acetate, cap the tube, and shake vigorously for 30 seconds.
- Centrifugation: Centrifuge at 500 x g for 10 minutes. Four layers will form: a sediment containing parasites, a formalin layer, a plug of debris, and an ethyl acetate layer at the top.
- Examination: Loosen the debris plug with an applicator stick and decant the top three layers. Use the sediment to prepare wet mounts or stained smears for microscopic examination [34].
Permanent Staining with Trichrome Stain
Permanent staining is essential for the definitive identification of protozoa, especially at higher magnifications.
- Principle: To differentially stain internal structures of protozoan trophozoites and cysts for detailed morphological examination and archival purposes [32].
- Materials: Schaudinn's fixative, Trichrome stain, 70% and 90% ethanol, acid-alcohol, xylene, mounting medium, microscope slides.
- Procedure:
- Smear Preparation: Prepare a thin smear of fresh or polyvinyl alcohol (PVA)-preserved stool on a slide and allow it to air dry.
- Fixation: Place the smear in Schaudinn's fixative for a minimum of 30 minutes.
- Staining:
- Hydrate through 70% ethanol (5 min) and iodine-alcohol (1 min).
- Rinse in 70% ethanol (1 min) and then 50% ethanol (1 min).
- Stain in Trichrome working solution for 7-10 minutes.
- Rinse in acid-alcohol for 1-3 seconds.
- Dehydrate rapidly through 95% ethanol, absolute ethanol, and xylene (2-3 dips each).
- Mounting: Mount with a coverslip using a synthetic resin.
- Interpretation: Cytoplasm appears blue-green to purple. Nuclei, chromatoid bodies, and ingested RBCs are stained red or purplish. Background debris appears green [32].
Performance and Limitations in Epidemiological Context
While indispensable, conventional microscopic techniques have well-documented limitations that researchers must account for in study design and data interpretation.
- Sensitivity and Specificity: The sensitivity of microscopy is variable and often suboptimal. For example, the sensitivity of a permanent stained smear for Giardia can be as low as 66.4%, and a single modified acid-fast stain for Cryptosporidium has a sensitivity of approximately 54.8% [30]. Specificity is compromised by the inability to distinguish morphologically identical species (e.g., pathogenic E. histolytica from non-pathogenic E. dispar) without additional tests [30].
- Operator Dependency: The accuracy of microscopy is heavily reliant on the skill and experience of the examiner. Proficiency requires extensive training, and maintaining competency is challenging, especially in non-endemic areas with low positive rates [35] [31].
- Impact on Epidemiological Data: These limitations can lead to underestimation of true prevalence, misclassification of etiological agents in diarrheal studies, and an incomplete picture of the diversity of intestinal protozoa in a population [30].
The Research Toolkit: Essential Reagents and Materials
Successful diagnosis and research rely on a suite of core reagents and materials. The following table details these essential components.
Table 2: Key Research Reagent Solutions for Conventional Parasitology
| Reagent/Material | Function | Specific Application Examples |
|---|---|---|
| 10% Formalin | Universal fixative and preservative for protozoan cysts and helminth eggs. Preserves morphology for concentration techniques [34]. | Used as the base solution in the Formalin-Ethyl Acetate Concentration Technique (FECT). |
| Polyvinyl Alcohol (PVA) | Preservative that both fixes the specimen and provides a adhesive medium for attaching stool to slides for permanent staining [32]. | Preferred for preparing smears for trichrome and other permanent stains, especially for trophozoites. |
| Schaudinn's Fixative | A mercuric-chloride-based fixative used to preserve the morphology of trophozoites and cysts prior to staining. | Critical pre-treatment step for high-quality trichrome staining [32]. |
| Trichrome Stain | A polychrome stain for permanent smears that differentially colors cytoplasm, nuclei, and inclusions. | Definitive identification of intestinal protozoa like Entamoeba histolytica and Giardia duodenalis [32]. |
| Modified Acid-Fast Stain | Stains the acid-fast cell wall of certain coccidian parasites. | Detection of Cryptosporidium spp., Cyclospora cayetanensis, and Cystoisospora belli oocysts [30] [32]. |
| Merthiolate-Iodine-Formalin (MIF) | Combined fixative, preservative, and stain. Useful for field surveys. | A single-solution solution for collecting, preserving, and initially examining stool specimens [34]. |
The Evolving Diagnostic Landscape: Conventional Methods and Novel Technologies
The field of parasitology diagnostics is evolving, with conventional methods now being complemented and enhanced by new technologies. Immunoassays and molecular techniques offer higher sensitivity and specificity for certain pathogens [30] [31]. Furthermore, artificial intelligence (AI) is emerging as a powerful tool to augment microscopy.
- Integration with Molecular Diagnostics: Polymerase chain reaction (PCR) is highly effective for speciating parasites (e.g., distinguishing E. histolytica from E. dispar), determining assemblages, and detecting low-intensity infections missed by microscopy [30]. However, its cost and technical requirements often relegate it to a confirmatory role in epidemiological surveys.
- Augmentation with Artificial Intelligence: Deep-learning models are being developed to automate the detection and classification of parasites in microscopic images. Studies have validated models like YOLOv8 and DINOv2, which can achieve high accuracy (>94-98% agreement with technologists) and even detect more organisms than human experts in some cases [35] [34]. This technology holds promise for reducing labor, improving standardization, and mitigating the challenges of operator dependency in large-scale studies. The following diagram conceptualizes this integrated diagnostic workflow.
Microscopy and staining remain vital tools in the epidemiological study of intestinal protozoan infections. Their simplicity, low cost, and immediate results ensure their continued relevance, particularly in field settings and resource-limited regions that bear the greatest disease burden. A critical understanding of their protocols, performance characteristics, and limitations is essential for researchers to design robust studies, accurately interpret data, and make informed decisions about when to integrate more advanced diagnostic methods. As the field progresses, the hybridization of conventional microscopy with AI-driven image analysis presents a promising pathway to enhance diagnostic accuracy, efficiency, and scalability for global public health initiatives.
The epidemiology of intestinal protozoan infections represents a significant global health challenge, particularly in tropical and subtropical regions where they contribute substantially to morbidity and mortality [36]. Accurate diagnosis is the cornerstone of effective disease management, surveillance, and control strategies. For decades, microscopic examination of stool specimens has been the traditional mainstay for diagnosing parasites like Entamoeba histolytica, Giardia duodenalis, and Cryptosporidium spp. [36]. However, this method presents important limitations, including labor-intensiveness, dependence on skilled microscopists, and insufficient sensitivity and specificity to reliably distinguish between pathogenic and non-pathogenic species [36] [37].
The evolution of immunodiagnostic technologies has revolutionized the detection of intestinal protozoa. Techniques such as Enzyme-Linked Immunosorbent Assay (ELISA), Rapid Diagnostic Tests (RDTs), and various antigen detection platforms have emerged as powerful alternatives, offering enhanced sensitivity, specificity, and operational efficiency [36] [38]. These advances are particularly crucial within epidemiological research, enabling more accurate prevalence studies, improved outbreak investigations, and better assessment of intervention effectiveness. This technical guide examines current immunodiagnostic methods, their applications in research, and the experimental protocols that underpin their use in the study of intestinal protozoan infections.
Technical Principles of Immunodiagnostic Methods
Immunodiagnostic methods for intestinal protozoa operate on the principle of detecting parasite-specific antigens in stool samples using monoclonal or polyclonal antibodies. The fundamental reaction involves antigen-antibody binding, which is then visualized through various signaling systems [38].
A key challenge in intestinal protozoan diagnosis is species differentiation. For example, the pathogenic E. histolytica is morphologically identical to the non-pathogenic E. dispar, necessitating detection methods that can distinguish between them at the molecular level [36] [37]. This is typically achieved by targeting species-specific antigens, such as the galactose-inhibitable adherence lectin for E. histolytica [36] [38].
The following diagram illustrates the core logical relationship and workflow selection for immunodiagnosis of intestinal protozoa:
Core Immunodiagnostic Platforms
Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA provides a robust platform for high-throughput detection of protozoan antigens in fecal samples. The technique is particularly valuable in research settings and large-scale epidemiological studies where batch processing is required [36] [38].
Key Characteristics:
- Format: Typically microplate-based for processing multiple samples simultaneously
- Sample Requirements: Fresh, frozen, or preserved stool samples (formalin, SAF); not suitable for concentrated or PVA-treated samples [38]
- Detection Capability: Specific antigens for Giardia, Cryptosporidium, and E. histolytica
- Performance: Reported sensitivity of 94-100% and specificity of 100% for giardiasis; 93-100% sensitivity for cryptosporidiosis [38]
Commercial ELISA kits for E. histolytica specifically target the galactose-inhibitable adherence lectin, enabling differentiation from non-pathogenic E. dispar [36] [38]. This specificity is crucial for accurate epidemiological mapping of true amebiasis prevalence.
Rapid Diagnostic Tests (RDTs) and Immunochromatographic Tests (ICT)
RDTs have transformed point-of-care testing for intestinal protozoa, offering rapid results without requiring sophisticated equipment or extensive technical expertise [39]. These lateral flow immunoassays are particularly valuable in resource-limited settings and for field studies.
Key Characteristics:
- Format: Dipstick or cassette format with visual readout
- Time to Result: 15-20 minutes
- Detection Capability: Often multiplexed for simultaneous detection of Giardia, Cryptosporidium, and sometimes E. histolytica [39] [38]
- Performance: Variable sensitivity (89.2% for Giardia in one evaluation); may have reduced sensitivity for low cyst counts or unusual Cryptosporidium species [39]
The operational simplicity of RDTs makes them ideal for prevalence surveys and rapid screening in outbreak situations, though their performance characteristics must be validated for the specific population and parasite strains under investigation [39].
Direct Fluorescent Antibody (DFA) Testing
DFA testing is considered a reference method for detecting Giardia and Cryptosporidium, combining immunological specificity with morphological confirmation [38].
Key Characteristics:
- Format: Microscopy-based with fluorescein-labeled monoclonal antibodies
- Sample Requirements: Concentrated or unconcentrated fecal samples
- Performance: Approximately 99% sensitivity and 100% specificity for cryptosporidiosis [38]
- Additional Value: Enables quantification of cysts and oocysts, supporting epidemiologic and control studies [38]
Performance Comparison of Immunodiagnostic Methods
The table below summarizes the performance characteristics of major immunodiagnostic platforms for key intestinal protozoa:
Table 1: Performance Characteristics of Immunodiagnostic Methods for Intestinal Protozoa
| Method | Target Protozoa | Sensitivity | Specificity | Time to Result | Throughput | Key Differentiating Capability |
|---|---|---|---|---|---|---|
| ELISA | Giardia duodenalis | 94-100% [38] | 100% [38] | 2-3 hours | High (batch) | Detects specific soluble antigens |
| Cryptosporidium spp. | 93-100% [38] | ~100% [38] | 2-3 hours | High (batch) | Detects specific surface antigens | |
| E. histolytica | 80-94% [36] | High | 2-3 hours | High (batch) | Differentiates from E. dispar via Gal/GalNAc lectin detection [36] | |
| RDT/ICT | Giardia duodenalis | 89.2% [39] | 99.3% [39] | 15-20 min | Low (single) | Rapid field deployment |
| Cryptosporidium spp. | Variable by species [39] | High [38] | 15-20 min | Low (single) | Rapid field deployment | |
| E. histolytica | Not specified | Not specified | 15-20 min | Low (single) | Some tests differentiate E. histolytica from E. dispar [38] | |
| DFA | Giardia duodenalis | ~100% [38] | 100% [38] | 1-2 hours | Moderate | Gold standard; enables quantification [38] |
| Cryptosporidium spp. | 99% [38] | 100% [38] | 1-2 hours | Moderate | Gold standard; enables quantification [38] |
Research Reagent Solutions
The table below outlines essential research reagents and their applications in immunodiagnostic development and implementation:
Table 2: Key Research Reagent Solutions for Protozoan Immunodiagnostics
| Reagent/Category | Specific Examples | Function/Application in Research |
|---|---|---|
| Bacterial Immunoglobulin-Binding Proteins | Protein A (SpA), Protein G (SpG), Protein L (SpL) [40] | Serological assays; antibody purification; diagnostic test development with broad immunoglobulin binding capacity |
| Monoclonal Antibodies | Anti-Gal/GalNAc lectin (E. histolytica) [36] | Specific detection of pathogenic E. histolytica; differentiation from non-pathogenic species |
| Anti-Giardia cyst wall protein [38] | Detection of Giardia cysts in DFA, ELISA, and RDT formats | |
| Anti-Cryptosporidium oocyst surface antigen [38] | Detection of Cryptosporidium oocysts in various assay formats | |
| Commercial Kits | TechLab E. histolytica II [38] | Specific detection of E. histolytica in stool specimens |
| Merifluor Cryptosporidium/Giardia [38] | Gold standard DFA detection for both parasites | |
| Crypto/Giardia K-SeT [39] | Rapid immunochromatographic test for simultaneous detection | |
| Signal Detection Systems | Fluorescein isothiocyanate (FITC) [38] | Fluorescent labeling for DFA tests |
| Enzyme substrates (HRP, AP) [36] | Colorimetric or chemiluminescent detection in ELISA | |
| Colloidal gold [39] | Visual signal in lateral flow RDTs |
Experimental Protocols for Key Assays
ELISA Protocol for Giardia and Cryptosporidium Antigen Detection
Principle: This protocol details the detection of Giardia- or Cryptosporidium-specific antigens in stool samples using a sandwich ELISA format [38].
Materials:
- Commercial ELISA kit (e.g., ProSpecT, TechLab Giardia II, Crypto CELISA)
- Fresh or preserved stool sample (avoid PVA-treated samples)
- Microplate washer and reader
- Incubator set at specified temperature
Procedure:
- Sample Preparation: Emulsify 100-500 mg of stool in provided dilution buffer. Centrifuge at high speed (e.g., 14,000 × g) for 2-5 minutes to clarify [37].
- Plate Setup: Add 100 μL of sample supernatant, positive control, and negative control to appropriate wells of the antibody-coated microplate.
- Incubation: Cover plate and incubate at room temperature or 37°C for 60 minutes.
- Washing: Wash plate 3-5 times with wash buffer to remove unbound material.
- Detection Antibody: Add 100 μL of enzyme-conjugated detection antibody to each well. Incubate for 30-60 minutes.
- Washing: Repeat washing step as above.
- Substrate Addition: Add 100 μL of enzyme substrate (e.g., TMB for HRP) to each well. Incubate for 10-30 minutes in the dark.
- Stop Solution: Add stop solution (e.g., sulfuric acid) to terminate reaction.
- Reading: Measure absorbance at appropriate wavelength (e.g., 450 nm) within 30 minutes.
Interpretation: Calculate cutoff value per manufacturer's instructions. Samples with absorbance above cutoff are considered positive.
Immunochromatographic Test (RDT) Protocol
Principle: This protocol describes the use of a rapid immunochromatographic test for simultaneous detection of Giardia and Cryptosporidium antigens (e.g., Crypto/Giardia K-SeT) [39].
Materials:
- Commercial duplex RDT kit
- Fresh stool sample
- Timer
Procedure:
- Sample Preparation:
- For formed stool: Use provided sampling device to collect standardized fecal inoculum (~10 mg) and transfer to dilution tube.
- For liquid stool: Pipette 80 μL directly into dilution tube [39].
- Extraction: Add extraction buffer, mix thoroughly, and wait for specified extraction time (typically 1-5 minutes).
- Test Application: Apply extracted sample to sample well of test device using provided dropper.
- Development: Wait for specified development time (15-20 minutes).
- Reading: Observe control and test lines. Control line must appear for valid test.
Interpretation:
- Positive Giardia: Control line plus Giardia test line
- Positive Cryptosporidium: Control line plus Cryptosporidium test line
- Positive for both: Control line plus both test lines
- Negative: Control line only
- Invalid: No control line
Direct Fluorescent Antibody (DFA) Protocol
Principle: This protocol details the DFA method for simultaneous detection and quantification of Giardia cysts and Cryptosporidium oocysts (e.g., Merifluor kit) [38].
Materials:
- Commercial DFA kit containing FITC-labeled monoclonal antibodies
- Stool sample (fresh or preserved)
- Microscope slides and coverslips
- Fluorescence microscope with appropriate filters
- Centrifuge
Procedure:
- Sample Preparation: Filter or concentrate stool sample if necessary. Prepare 1:10-1:50 dilution in PBS or kit buffer.
- Slide Preparation: Apply 10-50 μL of sample to microscope slide. Air dry.
- Fixation: Fix with methanol or according to kit instructions for 5-10 minutes.
- Staining: Apply FITC-labeled monoclonal antibody mixture. Incubate in humidified chamber for 30 minutes at 37°C or room temperature.
- Washing: Rinse slide gently with PBS or wash buffer to remove unbound antibody.
- Mounting: Apply mounting medium and coverslip.
- Examination: Examine using fluorescence microscope at 200-400× magnification.
Interpretation:
- Giardia cysts: Apple-green fluorescence, oval shape, 8-12 μm
- Cryptosporidium oocysts: Apple-green fluorescence, spherical, 4-6 μm
- Report as positive if structures with appropriate morphology and fluorescence are observed
Technological Innovations and Emerging Applications
High-Throughput Bead-Based Antigen Detection
Recent advances in immunoassay technology include the development of high-throughput bead-based antigen detection systems. These multiplex immunoassays enable simultaneous detection of multiple parasitic antigens and are particularly valuable for large-scale surveillance studies [41].
Principle: The technology uses microscopic beads conjugated with capture antibodies for different targets. Following antigen binding, detection is achieved using fluorescent reporter systems, with analysis via flow-based instrumentation [41].
Research Applications:
- Large-scale epidemiologic surveys
- Validation of RDT performance in field studies
- Detection of low-density infections in elimination settings
- Simultaneous monitoring of multiple pathogens
This approach was successfully integrated into school-based malaria surveys in Senegal, demonstrating utility for parasitic disease surveillance and highlighting its potential application for intestinal protozoa [41].
Engineering Chimeric Proteins for Enhanced Detection
Innovations in protein engineering have led to the development of chimeric immunoglobulin-binding proteins that enhance diagnostic capabilities [40].
Principle: By fusing protein domains from different bacterial sources (e.g., Protein A, G, L), researchers have created recombinant proteins with optimized binding characteristics for various immunoglobulin classes and subclasses [40].
Research Applications:
- Improved sensitivity in serological assays
- Enhanced antibody purification processes
- Development of broad-spectrum detection systems
- Creation of novel immunodiagnostic platforms with superior performance characteristics
These engineered proteins represent the next generation of immunodiagnostic tools, with potential applications in both human and veterinary parasitology [40].
Immunodiagnostic methods have fundamentally transformed the epidemiological study of intestinal protozoan infections. ELISA, rapid tests, and antigen detection platforms provide researchers with powerful tools for accurate parasite detection, species differentiation, and large-scale surveillance. While each platform offers distinct advantages and limitations, their collective development has addressed critical gaps in diagnostic capabilities, particularly in resource-limited settings where the burden of intestinal protozoa is highest.
The continued evolution of these technologies—including high-throughput multiplex assays, engineered binding proteins, and increasingly sophisticated rapid tests—promises to further enhance our understanding of protozoan disease epidemiology. These advances will support more effective control strategies and contribute to global efforts to reduce the health burden of intestinal protozoan infections. As the field progresses, the integration of immunodiagnostic methods with molecular techniques will likely provide the most comprehensive approach to understanding and combating these persistent pathogens.
The epidemiology of intestinal protozoan infections has been revolutionized by the adoption of molecular diagnostics, which provide unparalleled resolution for species identification and outbreak tracing. Conventional microscopy, while useful for initial detection, lacks the sensitivity and specificity required for distinguishing between morphologically identical but genetically distinct strains of pathogens. Molecular tools, particularly polymerase chain reaction (PCR) and advanced genotyping techniques, overcome these limitations by targeting unique genetic sequences. Within the context of intestinal protozoa, these methods are critical for understanding transmission dynamics, identifying zoonotic potential, and implementing targeted public health interventions. The World Health Organization recognizes the burden of diarrheal diseases caused by protozoan parasites, highlighting the necessity for advanced diagnostic capabilities in both developed and developing regions [42].
The transition to molecular methods represents a paradigm shift in parasitology and epidemiological research. These techniques enable researchers to detect low levels of infection, identify mixed assemblages, and track the sources of outbreaks with precision that was previously unattainable. For intestinal protozoa such as Giardia lamblia, Cryptosporidium spp., and Blastocystis, molecular characterization has revealed extensive genetic diversity that correlates with clinical outcomes and transmission patterns. This technical guide provides an in-depth examination of PCR and genotyping methodologies, their applications in intestinal protozoan research, and detailed protocols for implementation in laboratory settings, framed within the broader context of epidemiological investigation and public health response.
Core Molecular Techniques and Their Applications
Polymerase Chain Reaction (PCR) and Its Variations
PCR serves as the foundational technology for molecular detection and characterization of intestinal protozoa. This enzyme-driven process amplifies specific DNA sequences, enabling the detection of pathogens present in minute quantities within clinical samples. In epidemiological research, several PCR variations have been developed to address different diagnostic challenges:
Conventional PCR: Utilizes a single round of amplification with primers targeting conserved genetic regions. This method provides basic detection capabilities and is often used for initial screening of samples. In a study of HIV/AIDS patients, conventional PCR effectively detected Blastocystis and microsporidia, demonstrating its utility in vulnerable populations [43].
Nested PCR: Employs two successive amplification reactions with two sets of primers, significantly enhancing sensitivity and specificity. The first reaction uses outer primers to amplify a larger target region, while the second reaction uses inner primers that bind within the first amplicon. This method is particularly valuable for detecting low-abundance pathogens and was successfully employed for identifying Cryptosporidium spp. and G. intestinalis in HIV/AIDS patients, where infection burden can vary considerably [43].
Real-Time PCR (qPCR): Monitors amplification in real-time using fluorescent markers, combining detection with quantification. This method provides superior sensitivity and allows for the determination of parasite load, which can correlate with disease severity. Furthermore, real-time PCR enables genotyping through the use of assemblage-specific primers and melting curve analysis. A recent study on Giardia lamblia demonstrated that real-time PCR with primers targeting the tpi and gdh genes achieved 100% and 96% amplification rates respectively in microscopy-positive samples, far surpassing conventional detection methods [42].
Genotyping Methodologies
Genotyping builds upon PCR amplification to differentiate between genetically distinct strains or assemblages of the same parasite species. This level of discrimination is crucial for understanding transmission patterns, host specificity, and virulence factors:
Single-Locus Genotyping: Relies on sequence variation within a single genetic marker. Common targets for intestinal protozoa include the tpi (triosephosphate isomerase), gdh (glutamate dehydrogenase), and bg (β-giardin) genes. For example, a study on Giardia lamblia used tpi and gdh genes to differentiate assemblages A and B, revealing that mixed assemblages A&B were most prevalent (46%), followed by assemblage B (32%) and assemblage A (22%) [42].
Multilocus Genotyping (MLG): Analyzes multiple genetic loci to provide higher resolution and overcome potential misclassification that can occur with single-locus approaches. MLG is particularly important for detecting mixed infections and understanding recombination events. The combination of tpi, gdh, and bg genes has been adopted to improve classification reliability and detect sub-assemblage diversity [42].
Multilocus Sequence Typing (MLST): Extends MLG by sequencing multiple housekeeping genes to create highly discriminatory strain types. This approach is valuable for tracking transmission pathways during outbreak investigations and for population genetic studies of intestinal protozoa.
Experimental Data and Findings in Intestinal Protozoan Research
Molecular tools have generated significant quantitative data on the prevalence and genetic diversity of intestinal protozoa across different populations. The tables below summarize key findings from recent studies, demonstrating the power of these techniques in epidemiological research.
Table 1: Prevalence of Intestinal Protozoa in HIV/AIDS Patients vs. Control Group Using Molecular Detection
| Parasite | HIV/AIDS Patients (n=100) | Control Group (n=50) | P-value |
|---|---|---|---|
| Blastocystis | 22% | 8% | 0.029 |
| Microsporidia | 17% | 6% | 0.013 |
| Cryptosporidium spp. | 12% | 2% | 0.009 |
| G. intestinalis | 11% | 0% | 0.001 |
| Multiple Parasitism | 12% | 0% | N/A |
Source: Adapted from [43]
Table 2: Distribution of G. lamblia Assemblages Based on Different Genetic Markers
| Assemblage | tpi Gene (n=50) | gdh Gene (n=48) |
|---|---|---|
| Mixed A&B | 46% | 42% |
| Assemblage B | 32% | 36% |
| Assemblage A | 22% | 18% |
| Amplification Success | 100% | 96% |
Source: Adapted from [42]
Table 3: Association Between G. lamblia Assemblage Distribution and Epidemiological Factors
| Factor | Association with Assemblage | Statistical Significance |
|---|---|---|
| Age | Significant association | P < 0.05 |
| Residence | Significant association | P < 0.05 |
| Animal Contact | Significant association | P < 0.05 |
| Gender | No significant association | P = 0.276 |
| Water Source | No significant association | Not significant |
| Clinical Symptoms | No significant association | Not significant |
Source: Adapted from [42]
The data reveal several important patterns. HIV/AIDS patients show significantly higher prevalence of all intestinal protozoa compared to healthy controls, with multiple parasitism occurring exclusively in the immunocompromised group [43]. For Giardia lamblia, mixed assemblages A&B represent the most common infection pattern, challenging previous assumptions about single assemblage dominance [42]. The association of certain assemblages with specific epidemiological factors like age, residence, and animal contact provides insights into potential transmission pathways and risk factors.
Detailed Experimental Protocols
Sample Collection and DNA Extraction
Proper sample collection and processing are critical for successful molecular analysis:
Sample Collection: Collect stool samples from patients presenting with gastrointestinal symptoms. Preserve samples immediately in appropriate preservatives (e.g., 10% formalin or specific nucleic acid preservation buffers) to prevent DNA degradation. In the referenced Giardia study, 332 stool samples were collected from outpatients aged 2-16 years presenting with diarrhea [42].
Microscopic Examination: Perform initial screening using the formalin-ethyl acetate sedimentation method to concentrate parasites and confirm presence through morphological identification. Re-examine negative samples on consecutive days to minimize false negatives. Individuals who remain negative across all examinations are considered confirmed negative [42].
DNA Extraction: Use commercial DNA extraction kits specifically designed for stool samples, such as the QIAamp Fast DNA Stool Mini Kit. These kits effectively remove PCR inhibitors commonly found in fecal material. Assess DNA quantity and quality using spectrophotometry (e.g., NanoDrop 2000), with 260/280 and 260/230 absorbance ratios near 1.8 indicating high-quality DNA. Store extracted DNA at -20°C until PCR analysis [42].
Real-Time PCR for Detection and Genotyping
The following protocol details the real-time PCR method used for Giardia lamblia detection and genotyping:
- Primer Design: Select assemblage-specific primers targeting established genetic markers. For Giardia lamblia, the tpi and gdh genes provide reliable discrimination between assemblages A and B [42].
Table 4: Primer Sequences for G. lamblia Genotyping
| Gene | Primer Sequence | Amplified Products (bp) |
|---|---|---|
| tpi A | Forward: 5ʹ-TCGTCATTGCCCCTTCCGCC-3ʹReverse: 3ʹ-CAGTTGAGGATAGCAGCG-5ʹ | 77 |
| tpi B | Forward: 5ʹ- GATGAACGCAAGGCCAATAA -3ʹReverse: 3ʹ- -AAGAAGGAGATTGGAGAATC -5ʹ | 77 |
| gdh A | Forward: 5ʹ- CCGGCAACGTTGCCCAGTTT -3ʹReverse: 3ʹ- TCCGAGTTCAAGGACAAGT -5ʹ | 180 |
| gdh B | Forward: 5ʹ- CGTATTGGCGTCGGCGGT -3ʹReverse: 3ʹ- CTATCAGACCAGAGGCCACA -5ʹ | 133 |
Source: Adapted from [42]
PCR Reaction Setup: Prepare reactions in a 20 µl volume containing:
- 10 µl Maxima SYBR Green PCR Master Mix
- 2 µl primer mix (MGX Genotyping Assay)
- Extracted DNA containing 500 ng of template
- Nuclease-free water to final volume
Amplification Parameters: Use the following thermal profile on a Rotor-Gene PCR system:
- Initial hold: 50°C for 2 minutes
- Initial denaturation: 95°C for 10 minutes
- 40-45 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing: 59°C for 30 seconds
- Extension: 72°C for 30 seconds
Controls: Include known Giardia-positive DNA sample and nuclease-free distilled water as positive and negative controls, respectively, in each run to ensure assay validity [42].
Data Analysis and Interpretation
Statistical Analysis: Perform data analysis using statistical software such as IBM SPSS. Express qualitative variables as frequencies and percentages, with statistical significance set at P ≤ 0.05. Use Chi-square test for comparisons between groups, employing Monte Carlo test for nonparametric conditions when appropriate [42].
Genotype Assignment: For real-time PCR, analyze amplification curves and melting temperatures to assign assemblages. Samples amplifying with both assemblage A and B primers indicate mixed infections. Consider a sample positive if it shows exponential amplification above the threshold and demonstrates the expected melting temperature for the specific assemblage.
Phylogenetic Analysis: For sequence-based genotyping, perform multiple sequence alignment and construct phylogenetic trees to visualize genetic relationships between isolates. This analysis helps identify clusters and potential transmission networks.
Workflow Visualization
Molecular Workflow for Protozoan Detection and Genotyping
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents for Molecular Detection and Genotyping
| Reagent/Kit | Function | Application Example |
|---|---|---|
| QIAamp Fast DNA Stool Mini Kit | DNA extraction from stool samples | Efficiently extracts high-quality DNA while removing PCR inhibitors present in fecal material [42] |
| Maxima SYBR Green PCR Master Mix | Real-time PCR amplification | Provides fluorescence-based detection of amplified DNA in real-time PCR assays [42] |
| Assemblage-Specific Primers (tpi, gdh) | Target amplification and differentiation | Enables discrimination between Giardia assemblages A and B through gene-specific amplification [42] |
| NanoDrop 2000 Spectrophotometer | Nucleic acid quantification and quality assessment | Determines DNA concentration and purity through absorbance ratios at 260/280 and 260/230 nm [42] |
| Formalin-Ethyl Acetate Solution | Stool processing and parasite concentration | Sedimentation method for microscopic examination and sample preservation before DNA extraction [42] |
Implications for Public Health and Future Directions
Molecular tools for PCR and genotyping have transformed our approach to intestinal protozoan infections, providing insights that directly impact public health interventions. The ability to identify specific assemblages and their associations with epidemiological factors enables targeted control measures. For instance, the finding that mixed Giardia assemblages are most prevalent suggests complex transmission patterns requiring multifaceted intervention strategies [42]. Similarly, the high prevalence of multiple parasitic infections in HIV/AIDS patients underscores the need for comprehensive screening protocols in immunocompromised populations [43].
Future developments in molecular epidemiology will likely focus on point-of-care applications, multiplexed detection platforms, and whole-genome sequencing for ultimate resolution. The integration of molecular data with geographical information systems and temporal tracking will further enhance outbreak investigation capabilities. As these technologies become more accessible and cost-effective, their implementation in resource-limited settings will be crucial for global control of intestinal protozoan infections, ultimately reducing the significant burden of diarrheal diseases worldwide.
Intestinal protozoan infections, including those caused by Entamoeba histolytica, Giardia lamblia, and Cryptosporidium spp., represent a significant global health burden, particularly in tropical regions and areas with limited resources. These pathogens are primarily transmitted via the fecal-oral route through contaminated food, water, or direct contact, causing symptoms ranging from mild abdominal discomfort to severe dysentery, malnutrition, and even death [3]. Effective surveillance programs are fundamental to understanding disease burden, identifying risk factors, detecting outbreaks, and evaluating control interventions. Such programs enable public health officials to allocate resources efficiently and implement targeted measures to reduce transmission within communities.
The design of surveillance systems must account for the complex epidemiology of these pathogens, including variations in prevalence across geographic regions, populations, and seasons. In Malaysia, for example, the pooled prevalence of intestinal protozoal infections has been estimated at 24%, with significant regional variation from 13.6% in Selangor and Kuala Lumpur to 39% in Kelantan [44]. This heterogeneity underscores the need for surveillance systems that can capture local epidemiological patterns while enabling data comparison across regions. Furthermore, surveillance data must be visualized and communicated effectively to support public health decision-making, requiring appropriate graphical representations and analytical tools [45] [46].
Epidemiological Framework and Burden Assessment
Prevalence and Distribution Patterns
Understanding the geographical and demographic distribution of intestinal protozoan infections is crucial for designing targeted surveillance programs. Meta-analytical data from Malaysia reveals a pooled prevalence of 24% (95% CI: 0.17-0.29) for intestinal protozoan infections, with significant heterogeneity across regions (I² = 98.94%) [44]. This high heterogeneity reflects substantial variations in environmental conditions, socioeconomic factors, and public health infrastructure across different study populations.
Table 1: Prevalence of Major Intestinal Protozoa in Malaysia Based on Meta-Analysis
| Pathogen | Pooled Prevalence | 95% Confidence Interval | Clinical Manifestations |
|---|---|---|---|
| Entamoeba spp. | 18% | 0.12 - 0.24 | Amoebiasis: bloody diarrhea, abdominal pain, potential liver abscesses |
| Giardia lamblia | 11% | 0.08 - 0.14 | Giardiasis: watery diarrhea, abdominal pain, flatulence, weight loss |
| Cryptosporidium spp. | 9% | 0.03 - 0.14 | Cryptosporidiosis: watery diarrhea, stomach cramps, nausea, vomiting |
The highest disease burden falls disproportionately on vulnerable populations, with indigenous communities showing a prevalence of 27%, followed by rural populations at 23% [44]. Children under 15 years bear a particularly high burden, reflecting both behavioral factors and immunological susceptibility. This population distribution pattern should guide surveillance system design to ensure adequate representation of high-risk groups through appropriate sampling strategies.
Risk Factor Identification
Surveillance programs must incorporate systematic assessment of risk factors to enable targeted interventions. Meta-analyses have identified several significant predictors of infection, with pooled prevalence rates between 38% and 52% associated with specific risk factors [44]. The major risk factors include:
- Socioeconomic factors: Low income and no formal education
- Environmental exposures: Untreated water sources and poor sanitation
- Demographic characteristics: Male gender and age under 15 years
- Hygiene practices: Unhygienic personal and food handling practices
These risk factors interact in complex ways, creating distinct transmission patterns across different settings. Surveillance systems should capture data on these variables to identify high-risk populations and prioritize interventions. The systematic collection of risk factor information enables public health officials to move beyond descriptive epidemiology to analytical approaches that can identify root causes of transmission.
Surveillance System Design
Core Components and Infrastructure
Effective surveillance for intestinal protozoan infections requires infrastructure that integrates multiple components into a cohesive system. The core elements include:
- Case definitions: Standardized clinical and laboratory criteria for confirming cases
- Laboratory networks: Coordinated diagnostic facilities with quality assurance
- Data management systems: Electronic platforms for data collection, storage, and analysis
- Reporting mechanisms: Clear pathways for timely information flow from healthcare facilities to public health authorities
- Feedback loops: Regular dissemination of analyzed data to stakeholders
Surveillance systems can be designed as passive, active, or sentinel systems depending on program objectives and available resources. Passive surveillance, which relies on routine reporting from healthcare facilities, is most common but may underestimate true disease incidence. Active surveillance, involving regular outreach to identify cases, provides more complete data but requires substantially more resources. Sentinel surveillance monitoring specific sites or populations offers a compromise, providing high-quality data from representative locations.
Diagnostic Methods in Surveillance
The choice of diagnostic methods significantly influences surveillance data quality, affecting both sensitivity and specificity. Surveillance programs must select methods based on program objectives, resource constraints, and required data granularity.
Table 2: Diagnostic Methods for Intestinal Protozoan Infections in Surveillance
| Method | Sensitivity Range | Advantages | Limitations | Best Use in Surveillance |
|---|---|---|---|---|
| Microscopy (O&P) | 20-90% [47] | Low cost, detects multiple parasites simultaneously | Labor-intensive, requires expertise, cannot differentiate morphologically identical species | Baseline surveys in resource-limited settings |
| Immunoassays | 85-100% [47] | Rapid, technically simpler, high throughput | Limited to specific pathogens, variable sensitivity between products | Outbreak investigations, routine screening |
| qPCR/Molecular | >95% [48] | Highest sensitivity and specificity, species differentiation, quantification | Higher cost, requires specialized equipment and training | Precision surveillance, drug efficacy studies, outbreak tracing |
Molecular methods such as real-time PCR (qPCR) have emerged as powerful tools for surveillance, providing species-level differentiation critical for understanding transmission dynamics. For example, qPCR can distinguish pathogenic E. histolytica from non-pathogenic E. dispar, which is impossible with conventional microscopy [48]. Recent advances have also enabled the development of multiplex qPCR assays that detect multiple pathogens simultaneously, such as Entamoeba dispar + Entamoeba histolytica and Cryptosporidium spp. + Chilomastix mesnili in duplex reactions [48]. These molecular approaches enhance surveillance efficiency but require laboratory infrastructure and technical expertise that may not be universally available.
Data Management and Visualization
Data Collection and Management
Robust data management forms the foundation of effective surveillance systems. Standardized data collection instruments should capture demographic, clinical, laboratory, and risk factor information in structured formats amenable to analysis. Key considerations include:
- Minimum data sets: Define essential elements including unique identifiers, demographic information, symptom profiles, exposure history, laboratory results, and outcome data
- Data quality assurance: Implement validation rules, duplicate checks, and audit trails
- Data integration: Develop mechanisms to combine surveillance data with complementary information sources (environmental, meteorological, socioeconomic)
- Privacy protection: Ensure appropriate safeguards for personal health information
Electronic data capture systems, ranging from simple mobile applications to complex web-based platforms, can improve data quality and timeliness. These systems should be designed with end-users in mind, incorporating feedback from frontline healthcare workers who collect and report surveillance data.
Visualization for Epidemiological Intelligence
Data visualization transforms surveillance data into actionable intelligence, enabling public health officials to quickly identify patterns, trends, and anomalies. Effective visualization requires selecting appropriate graphical representations based on the type of data and analytical objectives [46] [49].
Table 3: Data Visualization Methods for Surveillance Data
| Visualization Type | Best Use Cases | Epidemiological Application | Key Considerations |
|---|---|---|---|
| Line graphs | Displaying trends over time | Monitoring incidence rates, evaluating interventions over time | Maintain consistent time intervals, avoid too many lines |
| Bar charts | Comparing categories or groups | Comparing prevalence across regions, demographic groups | Use natural order for categories, avoid scale breaks |
| Histograms | Showing distribution of continuous variables | Age distribution of cases, incubation periods | Select appropriate bin sizes to avoid misleading patterns |
| Scatter plots | Exploring relationships between variables | Correlation between risk factors and infection rates | Can show correlation but not necessarily causation |
| Maps | Displaying geographic distribution | Identifying disease hotspots, clustering patterns | Use appropriate base maps and scaling methods |
Geographic Information Systems (GIS) have become increasingly important in surveillance, allowing integration of spatial data to identify clustering, predict spread, and target resources. During the 2013 cyclosporiasis outbreak in the United States, spatial analysis played a crucial role in identifying the source of infection [47]. Similarly, social network analysis can visualize transmission pathways in outbreak settings, while phylogenetic trees based on molecular data can reveal relationships between isolates [45].
Diagram 1: Surveillance data flow from collection to public health action
Laboratory Methods and Protocols
Stool Sample Collection and Preservation
Proper specimen collection and preservation are critical for accurate laboratory diagnosis. Multiple stool specimens (typically three collected every other day) significantly increase diagnostic yield, with one study showing a 22.7% increase in detection for E. histolytica, 11.3% for Giardia, and 31.1% for D. fragilis when three specimens were examined compared to one [47]. Specimens should be collected before antimicrobial administration or contrast radiography, as these can interfere with detection.
Preservation methods must be appropriate for intended diagnostic tests:
- Formalin-based fixatives: Suitable for concentration procedures and permanent staining
- Polyvinyl alcohol (PVA): Preserves parasite morphology for stained smears
- Molecular transport media: Maintains nucleic acid integrity for PCR-based methods
- Refrigeration: Short-term preservation at 2-8°C if processing within 24 hours
Surveillance programs should establish standardized protocols for specimen collection, labeling, transport, and storage to ensure sample quality and result reliability.
Molecular Detection Protocol
Molecular methods, particularly real-time PCR (qPCR), offer high sensitivity and specificity for surveillance applications. The following protocol adapts recently published methods for detecting major intestinal protozoa [48]:
Sample Processing:
- Homogenize 0.5-1.0 g stool sample in phosphate-buffered saline
- Extract DNA using commercial stool DNA extraction kits
- Elute DNA in 50-100 μL elution buffer
- Quantify DNA concentration using spectrophotometry and adjust to working concentration
qPCR Reaction Setup:
- Reaction volume: 10 μL total volume
- Reaction mix: 5 μL master mix, 0.5-1.0 μL each primer (final concentration 0.5 μM), 0.25-0.5 μL probe (final concentration 0.1-0.25 μM), 2-3 μL template DNA, nuclease-free water to volume
- Thermal cycling conditions: 95°C for 3 minutes, followed by 45 cycles of 95°C for 15 seconds and 60°C for 30 seconds
- Duplex reactions: Combine Entamoeba dispar (FAM-labeled) + Entamoeba histolytica (HEX-labeled); Cryptosporidium spp. (FAM-labeled) + Chilomastix mesnili (HEX-labeled)
Quality Control:
- Include negative controls (nuclease-free water) and positive controls (plasmid DNA with target sequence) in each run
- Monitor amplification curves and cycle threshold (Ct) values
- Establish cutoff values based on validation studies
This protocol enables efficient detection of multiple pathogens in surveillance specimens, with the reduced reaction volume decreasing reagent costs—an important consideration for large-scale surveillance programs.
Diagram 2: Molecular detection workflow for surveillance applications
Implementation Considerations
Resource-Limited Settings
Surveillance programs in resource-constrained environments face particular challenges, including limited laboratory infrastructure, shortages of trained personnel, and budgetary constraints. Implementation strategies for these settings include:
- Phased implementation: Begin with sentinel surveillance before expanding to comprehensive systems
- Diagnostic algorithms: Combine cost-effective methods (e.g., antigen tests) with referral of samples for molecular confirmation
- Capacity building: Train local healthcare workers in specimen collection, basic diagnostics, and data reporting
- Leveraged infrastructure: Utilize existing programs (e.g., integrated disease surveillance) to maximize resources
The retirement of experienced technologists and inadequate training of new staff in parasitology represents a significant challenge for maintaining microscopy proficiency [47]. To address this, some laboratories have developed affiliations with organizations that conduct parasitology surveillance in regions of disease endemicity, such as the Walter Reed Army Institute of Research, Naval Medical Research Unit, Joint Pathology Center, and CDC DPDx laboratories [47]. These partnerships provide access to positive specimens for teaching and proficiency testing.
Evaluation and Quality Assurance
Surveillance systems require continuous evaluation to ensure data quality and utility. The CDC guidelines recommend assessing surveillance systems based on:
- Simplicity: Structure and ease of operation
- Flexibility: Adaptability to changing needs or conditions
- Data quality: Completeness and validity of collected information
- Sensitivity: Ability to detect cases and outbreaks
- Timeliness: Speed between steps in the surveillance process
- Stability: Reliability and availability of the system
- Acceptability: Willingness of participants to engage with the system
Quality assurance programs should include regular proficiency testing for laboratory diagnosis, data quality audits, and systematic feedback from stakeholders. Molecular methods require particular attention to quality control, including validation of primers and probes, monitoring for inhibition, and standardization across participating laboratories.
Research Reagent Solutions
Table 4: Essential Research Reagents for Protozoan Infection Surveillance
| Reagent Category | Specific Examples | Application in Surveillance | Technical Notes |
|---|---|---|---|
| Primer/Probe Sets | E. histolytica 18S rRNA, Cryptosporidium COWP gene, Giardia β-giardin gene | Species-specific detection and differentiation by qPCR | Validate specificity against local strains; check for cross-reactivity |
| Plasmid Controls | Recombinant plasmids containing target sequences (ampicillin/kanamycin resistance) | Quantification standards, quality control, assay validation | Create dilution series for limit of detection studies |
| DNA Extraction Kits | Commercial stool DNA extraction kits | Nucleic acid purification for molecular assays | Include inhibition controls; optimize for difficult specimens |
| Master Mixes | TaqMan-based reactions with UNG contamination control | qPCR amplification | Scale reaction volumes (10μL) to reduce costs in high-throughput surveillance |
| Immunoassays | TechLab Giardia II, Remel ProSpecT Cryptosporidium, Meridian Merifluor | Rapid detection in field settings or resource-limited laboratories | Assess lot-to-lot variability; follow manufacturer storage requirements |
| Microscopy Reagents | Formalin-ethyl acetate concentration, trichrome staining, modified acid-fast staining | Primary detection in basic laboratories, morphological confirmation | Maintain consistent staining protocols across surveillance sites |
The development and validation of reagents for emerging targets represents an active area of research. For example, the first molecular detection of Chilomastix mesnili by qPCR was recently reported using newly designed primers and probes targeting the small ribosomal subunit [48]. Such advances expand the capacity of surveillance systems to monitor both pathogenic and indicator organisms that signal fecal contamination.
Effective surveillance programs for intestinal protozoan infections require careful integration of epidemiological principles, laboratory methods, data management, and visualization techniques. The high prevalence of these infections in many regions, coupled with their significant health burden, underscores the importance of robust surveillance systems that can guide public health interventions. Current evidence indicates prevalence rates up to 24% in some populations, with particularly high burden among children, indigenous communities, and rural populations [44].
Future directions in surveillance include the expanded use of molecular methods for precise pathogen identification, development of point-of-care tests for field use, and implementation of data visualization tools that enhance pattern recognition and decision support [45]. The integration of genomic data with traditional epidemiological information promises to transform surveillance from descriptive monitoring to predictive analytics capable of anticipating and preventing outbreaks. As surveillance systems evolve, their crucial role in reducing the burden of intestinal protozoan infections will continue to expand, contributing to global efforts to achieve health equity and reduce disparities in parasitic disease burden.
Integrating Diagnostic Data for Public Health Decision-Making
The effective management and integration of diagnostic data are fundamental to addressing persistent public health challenges, particularly the burden of intestinal protozoal infections (IPI). These infections, caused by pathogens such as Entamoeba spp., Giardia lamblia, and Cryptosporidium spp., remain a significant global health concern, especially in developing regions. In Malaysia specifically, a recent systematic review and meta-analysis revealed a substantial pooled prevalence of 24% for these infections, with certain states like Kelantan reporting rates as high as 39% [4] [13]. The fight against these diseases is hindered by fragmented health information systems and disparate data sources, which prevent a unified view of the epidemiological landscape [50]. This whitepaper provides a technical guide for researchers, scientists, and drug development professionals on frameworks and methodologies for integrating diverse diagnostic data streams. By leveraging advanced data equity principles, artificial intelligence (AI), and interoperable systems, public health decision-makers can transform raw data into actionable intelligence, enabling targeted interventions and efficient resource allocation to reduce the impact of IPI.
Epidemiological Context: The Burden of Intestinal Protozoal Infections
A clear understanding of the prevalence and distribution of IPI is the first critical step in formulating an effective public health response. The following table summarizes key quantitative findings from a recent meta-analysis in Malaysia, illustrating the scope of the problem and highlighting vulnerable populations [4] [13].
Table 1: Prevalence and Risk Factors of Intestinal Protozoal Infections in Malaysia
| Epidemiological Factor | Detailed Finding | Pooled Prevalence (95% CI) |
|---|---|---|
| Overall IPI Prevalence | Combined prevalence of Entamoeba spp., G. lamblia, & Cryptosporidium spp. | 24% (0.17 - 0.29) |
| Pathogen-Specific Prevalence | Entamoeba spp. | 18% (0.12 - 0.24) |
| Giardia lamblia | 11% (0.08 - 0.14) | |
| Cryptosporidium spp. | 9% (0.03 - 0.14) | |
| Regional Variation (States) | Kelantan | 39% |
| Perak | 29% | |
| Selangor & Kuala Lumpur | 13.6% | |
| Population Subgroups | Indigenous Communities | 27% |
| Local Rural Communities | 23% | |
| Key Risk Factors | Children under 15, low income, no formal education, exposure to untreated water, poor sanitation, unhygienic practices | 38% - 52% |
This data underscores the disproportionate impact on marginalized groups, including indigenous communities and children, and highlights the critical influence of socioeconomic and environmental determinants [4] [13]. This level of detailed, stratified information is only possible through the systematic aggregation and analysis of diagnostic data from across the health system.
A Framework for Integrated Diagnostic Data Systems
Integrating diagnostic data for public health requires a structured approach that ensures data from various sources can be seamlessly combined, analyzed, and interpreted. The core of this approach involves addressing data interoperability and applying a lens of data equity to prevent the exacerbation of existing health disparities [50].
Key Technical Components
- Interoperability and Breaking Down Data Silos: Diagnostic data for IPI often resides in disconnected systems, including electronic health records (EHRs), laboratory information management systems (LIMS), and public health surveillance databases. Leveraging frameworks like the Trusted Exchange Framework and Common Agreement (TEFCA) can facilitate secure health information exchange between these systems. The goal is to create a unified platform that integrates clinical data with broader Social Determinants of Health (SDOH) data, such as water quality and sanitation access, which are critical risk factors for IPI [50].
- Applying a Data Equity Lens: Data equity involves implementing "fair data practices that respect and promote human rights, opportunity and dignity" [50]. In the context of IPI, this means:
- Ensuring diagnostic data collection includes diverse and vulnerable populations, such as indigenous communities, to avoid biased models and interventions.
- Using culturally sensitive methodologies and involving communities in data governance.
- Addressing biases in AI and machine learning models, which can perpetuate disparities if trained on non-representative data [50].
Promising Initiatives and Models
Real-world examples demonstrate the feasibility and impact of such integration. The Colorado Social Health Information Exchange (CoSHIE) is a pioneering statewide initiative that provides a secure, centralized platform for sharing data between healthcare providers and social service organizations [50]. A similar model adapted for IPI control could allow a clinician to not only diagnose a Cryptosporidium infection but also automatically trigger a referral to a social service agency to address the patient's lack of access to clean water, thereby tackling the root cause of the infection.
Experimental Protocols for Data Collection and Management
Robust public health decision-making depends on the quality of the underlying data. The following section outlines detailed methodologies for generating reliable quantitative data on IPI, from systematic literature reviews to primary data management.
Protocol 1: Systematic Review and Meta-Analysis of IPI Prevalence
This protocol is designed to synthesize existing epidemiological evidence, as demonstrated in the Malaysian study [4] [13].
- Objective: To estimate the pooled prevalence of intestinal protozoal infections and identify associated risk factors in a defined population.
- Eligibility Criteria:
- Population: Human patients in the target region (e.g., Malaysia).
- Intervention/Exposure: Diagnosis of IPI (Entamoeba spp., G. lamblia, Cryptosporidium spp.).
- Comparator: Non-infected individuals.
- Outcomes: Prevalence rates, risk factor odds ratios.
- Study Types: Primary observational studies (cross-sectional, cohort, case-control).
- Information Sources: A comprehensive search of electronic databases including PubMed/MEDLINE, Scopus, Web of Science, and Google Scholar. The reference lists of retrieved articles should also be hand-searched.
- Search Strategy: Using medical subject headings (MeSH) and keywords combined with Boolean operators (AND/OR). Example: ("intestinal protozoal infections" OR "amoebiasis" OR "giardiasis" OR "cryptosporidiosis") AND ("prevalence" OR "risk factors") AND "[Country/Region]" [4] [13].
- Study Selection and Data Extraction: The process should follow the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Data extracted from included studies will include: first author, publication year, study region, sample size, diagnostic methods, and number of positive cases for each protozoan.
- Data Synthesis and Analysis: Pooled prevalence estimates should be calculated using a random-effects model to account for heterogeneity between studies. Results are presented as proportions with 95% confidence intervals (CI). Heterogeneity can be assessed using the I² statistic, where a value greater than 75% indicates high heterogeneity. Subgroup analyses based on region, population, and detection methods should be conducted [4] [13].
Protocol 2: Primary Data Management and Quality Assurance
Once primary data is collected, it must be rigorously managed to ensure its quality and integrity for analysis [51].
- Objective: To transform raw, collected data into a clean, analysis-ready dataset.
- Procedure:
- Data Cleaning: The dataset must be checked for and corrected prior to analysis.
- Checking for Duplications: Identify and remove identical copies of data from repeated submissions.
- Handling Missing Data: Determine the extent and pattern of missingness using statistical tests like Little's Missing Completely at Random (MCAR) test. Decide on inclusion/exclusion thresholds for incomplete records (e.g., exclude questionnaires with <50% completion) and consider advanced imputation methods if data is not missing at random [51].
- Checking for Anomalies: Run descriptive statistics to identify values outside expected ranges (e.g., a value of 6 on a 1-5 Likert scale). These anomalies must be investigated and corrected.
- Data Analysis:
- Descriptive Analysis: Begin with frequencies, means, medians, and standard deviations to summarize the socio-demographic and clinical characteristics of the sample.
- Assessing Normality: Test the normality of the distribution of continuous variables using measures of skewness and kurtosis (values of ±2 generally indicate normality) or statistical tests like the Shapiro-Wilk test. This determines whether parametric or non-parametric inferential tests should be used [51].
- Inferential Analysis: Employ statistical tests (e.g., chi-squared tests, logistic regression) to analyse relationships between risk factors and IPI outcomes, based on the study hypotheses and data type.
- Interpretation and Presentation:
- Report both statistically significant and non-significant findings transparently.
- Avoid selective reporting and correct for multiplicity (e.g., using the Bonferroni correction) when multiple comparisons are made [51].
- Data Cleaning: The dataset must be checked for and corrected prior to analysis.
The workflow for this quantitative data management process is visualized below.
Diagram 1: Quantitative data management workflow from collection to findings.
Visualizing the Data Integration Pathway
The following diagram maps the logical pathway from fragmented diagnostic data sources to integrated public health intelligence, specifically for IPI surveillance and control. This process relies heavily on the principles of interoperability and data equity discussed in Section 3.
Diagram 2: Diagnostic data integration pathway for public health action.
The Researcher's Toolkit: Essential Reagents and Materials
The following table details key research reagents and solutions essential for conducting laboratory-based studies and developing diagnostic assays for intestinal protozoal infections.
Table 2: Key Research Reagent Solutions for Intestinal Protozoan Infection Studies
| Research Reagent / Solution | Primary Function and Application |
|---|---|
| Multiplex PCR Assays | Molecular detection and simultaneous differentiation of multiple protozoan pathogens (Entamoeba histolytica, G. lamblia, Cryptosporidium spp.) from a single stool sample. Crucial for rapid epidemiological analysis and detecting resistance mutations [52]. |
| Antigen Detection Kits (ELISA/EIA) | Immunoassay-based detection of protozoan-specific antigens (e.g., G. lamblia CWP1, E. histolytica Gal/GalNAc) in stool samples. Used for high-throughput screening and clinical diagnosis. |
| Microscopy Stains (e.g., Trichrome, Iodine) | Staining of stool smears for the morphological identification and visualization of cysts and trophozoites under light microscopy. A foundational, though less specific, diagnostic method. |
| Fecal DNA/RNA Extraction Kits | Isolation of high-purity, amplification-ready nucleic acids from complex and inhibitory stool matrices. This is a critical first step for all molecular diagnostic applications. |
| Real-Time PCR (qPCR) Probes & Master Mixes | Quantitative detection and genotyping of protozoan DNA with high sensitivity and specificity. Used for determining pathogen load and in antimicrobial resistance (AMR) research. |
| Axenic Culture Media | In vitro cultivation and propagation of specific protozoan strains (e.g., E. histolytica) for downstream applications like drug sensitivity testing, genomic studies, and antigen production. |
| Recombinant Antigens & Antibodies | Key reagents for developing and calibrating immunoassays, and for researching host-pathogen interactions and pathogen biology. |
The integration of diagnostic data is not merely a technical exercise but a strategic imperative for modern public health. In the fight against intestinal protozoal infections, which are deeply intertwined with poverty and inequity, a unified data ecosystem is the most powerful tool for understanding disease dynamics, targeting interventions, and ultimately reducing the burden on vulnerable populations. By adopting the frameworks, protocols, and tools outlined in this guide—with a steadfast commitment to interoperability, data equity, and rigorous data management—researchers and public health professionals can transform disparate data points into coherent, actionable intelligence. This will pave the way for more precise, effective, and equitable public health decision-making, moving us closer to the goal of controlling and preventing intestinal protozoal infections worldwide.
Overcoming Diagnostic Limitations and Therapeutic Failures in Protozoal Diseases
Intestinal protozoan infections (IPIs), caused by pathogens such as Giardia duodenalis, Entamoeba histolytica, and Cryptosporidium spp., represent a significant global health burden, affecting approximately 3.5 billion people annually and causing an estimated 1.7 billion episodes of diarrheal disease [53] [54]. The accurate detection of these parasites is fundamental to epidemiological surveillance, yet remains hampered by the persistent limitations of conventional diagnostic methods. Microscopic examination, while widely used as a reference standard, is constrained by significant issues with sensitivity, specificity, and operator dependency [53] [54] [55]. These diagnostic pitfalls impede accurate prevalence estimation, obscure true disease burden, and ultimately compromise the development of effective public health interventions. This technical guide examines the core limitations of traditional diagnostics within epidemiological research contexts and details the advanced methodologies overcoming these challenges.
Quantitative Evidence: Documenting Diagnostic Limitations
The performance disparities between diagnostic methods have been quantitatively demonstrated in recent multicenter studies. The following tables summarize key performance metrics and study characteristics, providing a comparative analysis for researchers.
Table 1: Performance Characteristics of Molecular vs. Conventional Methods for Protozoan Detection
| Parasite | Method | Sensitivity (%) | Specificity (%) | Notes | Study |
|---|---|---|---|---|---|
| Multiple Protozoa | Allplex GI-Parasite Assay (Multiplex RT-PCR) | 97.2-100 | 99.2-100 | Performance for E. histolytica, G. duodenalis, D. fragilis, Cryptosporidium spp. | [37] |
| Giardia duodenalis | Commercial & In-House RT-PCR | High | High | Complete agreement between PCR methods; performance similar to microscopy | [53] [54] |
| Cryptosporidium spp. | Commercial & In-House RT-PCR | Limited | High | Limited sensitivity likely from inadequate DNA extraction from oocysts | [53] [54] |
| Entamoeba histolytica | Molecular Assays (PCR) | Critical for accurate diagnosis | Critical for accurate diagnosis | Microscopy cannot differentiate from non-pathogenic E. dispar | [53] [54] |
| Dientamoeba fragilis | Commercial & In-House RT-PCR | Inconsistent | High | Detection remains inconsistent across studies | [53] [37] [54] |
Table 2: Summary of Recent Comparative Studies on Protozoan Diagnostics
| Study Focus | Sample Size & Design | Key Findings on Diagnostic Pitfalls | Reference |
|---|---|---|---|
| Comparative PCR Analysis | 355 stool samples (18 Italian labs); compared commercial/in-house RT-PCR vs. microscopy | Molecular methods are promising but require standardization of sample collection, storage, and DNA extraction. | [53] [54] |
| Multiplex Assay Evaluation | 368 samples (12 Italian labs); evaluated Allplex GI-Parasite Assay vs. conventional methods | The multiplex RT-PCR kit exhibited excellent performance for common enteric protozoa. | [37] |
| Meta-analysis of Prevalence | 49 included studies; systematic review in Malaysia | Pooled prevalence of IPIs was 24%; high heterogeneity (I² > 98%) reflects diagnostic method variability. | [4] |
| Metagenomic/ Metatranscriptomic Sequencing | 1,067 diarrheal samples; compared sequencing to standard diagnostics | Metatranscriptomics showed strong correlation with gold-standard diagnostics for most pathogens and superior sensitivity over metagenomics for some. | [56] |
Experimental Protocols for Advanced Detection
To address the documented shortcomings of microscopy, researchers are adopting standardized molecular and sequencing protocols. The following sections detail key methodologies cited in contemporary literature.
Multicenter Protocol for Molecular Test Evaluation
A 2025 multicenter study involving 18 Italian laboratories established a protocol for comparing molecular and conventional diagnostics [53] [54].
- Sample Collection and Storage: A total of 355 consecutive stool samples were collected over six months. Of these, 230 were fresh samples, and 125 were preserved in Para-Pak media. All samples were examined by conventional microscopy (the reference method) per WHO and CDC guidelines. Fresh samples were stained with Giemsa, while fixed samples were processed using the formalin-ethyl acetate (FEA) concentration technique. After examination, samples were promptly frozen at -20°C [54].
- DNA Extraction: For molecular analysis, a 350 µL volume of Stool Transport and Recovery Buffer (S.T.A.R. Buffer; Roche) was mixed with approximately 1 µL of fecal sample using a sterile loop. After incubation at room temperature for 5 minutes and centrifugation at 2000 rpm for 2 minutes, 250 µL of supernatant was collected. An internal extraction control (50 µL) was added, and DNA was extracted using the MagNA Pure 96 DNA and Viral NA Small Volume Kit on the MagNA Pure 96 System (Roche), a fully automated platform for nucleic acid preparation [54].
- In-House RT-PCR Amplification: Each 25 µL reaction mixture contained 5 µL of extracted DNA, 12.5 µL of 2× TaqMan Fast Universal PCR Master Mix (Thermo Fisher Scientific), 2.5 µL of a primer and probe mix, and sterile water. Amplification was performed on an ABI 7900HT Fast Real-Time PCR System using the cycling regimen: 1 cycle of 95°C for 10 min; followed by 45 cycles of 95°C for 15 s and 60°C for 1 min. Each run included positive controls and negative (water) controls [54].
- Commercial RT-PCR: The commercial AusDiagnostics RT-PCR test was used in parallel according to the manufacturer's instructions [53].
Metatranscriptomic Sequencing for Pathogen Detection
A large-scale 2025 study (INTEGRATE) on 1,067 diarrheal samples established a protocol for metatranscriptomic sequencing, which demonstrated high diagnostic correlation [56].
- Sample Processing and Nucleic Acid Extraction: Stool samples were divided into aliquots. One part was used for traditional diagnostic methods, while the other was designated for sequencing. Total RNA was extracted from the clinical sample aliquot. The extracted RNA was treated with DNase to eliminate genomic DNA contamination [56].
- rRNA Depletion and Library Preparation: The purified total RNA underwent ribosomal RNA (rRNA) depletion using the NEBNext rRNA Depletion Kit (Bacteria) to enrich for pathogen and host mRNA transcripts. Strand-specific RNA-Seq libraries were then prepared from the rRNA-depleted RNA using the NEBNext Ultra Directional RNA Library Prep Kit for Illumina, which includes a reverse transcription step to convert RNA into complementary DNA (cDNA) [56].
- Sequencing and Bioinformatics: The final libraries were sequenced using paired-end, 150-bp sequencing on an Illumina HiSeq 4000, yielding an average of 34 million filtered reads per sample. Quality-controlled reads were processed using the MetaWRAP pipeline. Taxonomic assignment of RNA reads was performed with Kraken2 (v2.1.2) using a custom database encompassing RefSeq complete genomes and proteins for archaea, bacteria, fungi, viruses, and protozoa [56].
Antigen Detection via Immunochromatographic Test (ICT)
While molecular methods are highly sensitive, immunological methods offer rapid, user-friendly alternatives. A typical protocol for a rapid immunochromatographic test (ICT) is outlined below [57].
- Sample Preparation: A small amount of fresh or unpreserved stool sample (e.g., 100-200 mg) is emulsified in the provided extraction buffer vial. The mixture is vortexed and allowed to settle [57].
- Test Procedure: The supernatant is transferred to a test tube. The test strip, which contains immobilized monoclonal antibodies against target protozoan antigens (e.g., Giardia duodenalis cell wall proteins or Cryptosporidium spp. oocyst surface epitopes), is placed into the supernatant. The liquid migrates up the strip via capillary action [57].
- Result Interpretation: After a specified incubation time (typically 10-15 minutes), the appearance of a colored test line, in addition to the control line, indicates a positive result. The test is considered invalid if the control line does not appear. These tests are quick and do not require specialized equipment but may have lower sensitivity compared to molecular methods [57].
The Researcher's Toolkit: Essential Reagents and Kits
Table 3: Key Research Reagent Solutions for Protozoan Diagnosis
| Reagent / Kit Name | Function / Target | Brief Description & Research Application |
|---|---|---|
| Allplex GI-Parasite Assay (Seegene) | Multiplex RT-PCR detection | Simultaneously detects G. duodenalis, D. fragilis, E. histolytica, B. hominis, C. cayetanensis, Cryptosporidium spp. Validated on Bio-Rad CFX96 systems [37]. |
| AusDiagnostics RT-PCR (R-Biopharm Group) | Multiplex RT-PCR detection | Commercial PCR test for G. duodenalis, Cryptosporidium spp., E. histolytica, D. fragilis. Used in multicenter comparative studies [53] [54]. |
| MagNA Pure 96 System (Roche) | Automated Nucleic Acid Extraction | Utilizes magnetic bead technology with the MagNA Pure 96 DNA and Viral NA Small Volume Kit for standardized, high-throughput DNA extraction from stool [54]. |
| S.T.A.R. Buffer (Roche) | Stool Transport and Recovery | Stabilizes nucleic acids in stool specimens before DNA extraction, helping to overcome PCR inhibitors present in feces [54]. |
| NEBNext rRNA Depletion Kit (Bacteria) | Ribosomal RNA Depletion | Critical for metatranscriptomic studies; removes abundant bacterial rRNA to enable sequencing of less abundant pathogen and host transcripts [56]. |
| Monoclonal Antibodies (various) | Antigen Detection (ELISA, ICT, DFA) | Target-specific proteins (e.g., Giardia cyst wall, Cryptosporidium oocyst surface). Used in immunodiagnostic platforms for rapid detection, though may lack species differentiation [57]. |
Visualizing Diagnostic Pathways and Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the core diagnostic pathways and experimental workflows for detecting intestinal protozoa.
Diagnostic Method Evolution and Pitfalls
Molecular Detection Workflow
The epidemiological research landscape for intestinal protozoan infections is undergoing a paradigm shift, moving away from operator-dependent, low-sensitivity microscopy toward precise molecular and sequencing technologies. Quantitative evidence from recent multicenter studies confirms that molecular methods, including multiplex RT-PCR and metatranscriptomics, directly address the critical pitfalls of traditional diagnostics by offering superior sensitivity, specificity, and standardization [53] [37] [56]. The adoption of detailed, standardized protocols for these advanced methods is crucial for generating reliable, comparable prevalence data and for accurately defining the true global burden of these infections. For the research community, embracing these tools and the accompanying experimental rigor is foundational to strengthening public health surveillance, validating new drug targets, and ultimately controlling the transmission of intestinal protozoa.
The epidemiology of intestinal protozoan infections is significantly complicated by the emergence and spread of drug-resistant parasites. Giardia duodenalis and Entamoeba histolytica, responsible for giardiasis and amebiasis respectively, represent major global health burdens, particularly in developing regions with inadequate sanitation. Therapeutic failure against these parasites has been increasingly documented, threatening disease control programs and patient outcomes. This whitepaper examines the current understanding of resistance mechanisms in these parasites, framed within the context of epidemiological trends and the pressing need for novel therapeutic strategies. The growing challenge of nitroimidazole-refractory giardiasis, particularly in specific geographical hotspots, and emerging insights into amebic resistance mechanisms underscore the necessity for continued research into parasite biology and resistance detection methods [58] [59].
Epidemiological Context of Resistance
Geographical Distribution of Drug-Refractory Giardiasis
The prevalence of drug-refractory infections varies significantly by geographic region, indicating potential differences in drug pressure or circulating parasite strains. A comprehensive study in Stockholm, Sweden, analyzing 4,285 giardiasis cases from 2008–2020, found that 2.4% (102 cases) were nitroimidazole-refractory. The burden was disproportionately associated with travel to the Indian subcontinent. Among cases acquired in India, 12% (64/545) were refractory to nitroimidazole treatment, and this percentage increased significantly over the study period, from 8.5% during 2008–June 2014 to 17.2% during July 2014–2020 [58].
Table 1: Prevalence of Nitroimidazole-Refractory Giardiasis by Region of Acquisition (Sweden, 2008-2020)
| Region of Acquisition | Total Cases | Refractory Cases | Refractory Prevalence |
|---|---|---|---|
| India | 545 | 64 | 12.0% |
| Asia (excluding India) | 792 | 9 | 1.1% |
| Africa | 1,115 | 17 | 1.5% |
| Europe | 1,247 | 11 | 0.9% |
| Americas | 349 | 1 | 0.3% |
| Sweden (domestic) | 881 | 5 | 0.6% |
This data highlights India as a notable hotspot for refractory giardiasis, with prevalence more than 10 times higher than in other world regions [58]. The reasons for this high prevalence are not fully understood but may include high drug pressure from frequent use of 5-nitroimidazoles. Interestingly, neighboring Pakistan with similar living conditions showed much lower prevalence (approximately 1%), suggesting complex regional factors at play [58].
Global Burden and Risk Factors for Entamoeba Infections
The global burden of Entamoeba infection-associated diseases (EIADs) remains substantial, with an age-standardized disability-adjusted life year (DALY) rate of 36.77 per 100,000 in 2019. Although this rate has declined significantly over the past 30 years, it remains disproportionately high among children under 5 years (257.43/100,000) and in low sociodemographic index (SDI) regions (100.47/100,000). Concerningly, high-income regions like North America and Australia have experienced increasing trends in EIAD burden among adults and the elderly [60].
Risk factors significantly associated with Entamoeba infection include low economic status, untreated drinking water, consumption of raw vegetables, and poor handwashing habits before meals [61]. Molecular epidemiological studies have revealed complex species distributions, with E. dispar and E. moshkovskii frequently detected in both asymptomatic and symptomatic intestinal infections, though E. histolytica remains the primary species associated with invasive extra-intestinal disease [61] [62].
Mechanisms of Drug Resistance in Giardia
Nitroimidazole Resistance and Extracellular Vesicle-Mediated Adaptation
Nitroimidazoles (metronidazole, tinidazole) are first-line treatments for giardiasis. Their activation requires reduction by parasite enzymes, particularly pyruvate:ferredoxin oxidoreductase (PFOR), which generates reactive nitro-radicals that cause cytotoxic damage. Resistance is associated with reduced drug activation and efficient nitro-radical scavenging.
A groundbreaking 2025 study revealed that small extracellular vesicles (sEVs) serve as key mediators of phenotypic adaptation to drug stress in Giardia. sEVs derived from metronidazole-resistant clones can transfer resistance traits to drug-susceptible parasites by modifying the expression of enzymes involved in metronidazole metabolism and reducing production of reactive oxygen species (ROS) in recipient parasites. This transfer efficiency and phenotypic impact demonstrate genotype-specific variation, highlighting a novel communication mechanism that may facilitate the spread of drug resistance phenotypes within parasite populations [63].
The following diagram illustrates this sEV-mediated mechanism of resistance adaptation:
Experimental Protocol for sEV-Mediated Resistance Transfer
Objective: To investigate the role of small extracellular vesicles (sEVs) in mediating metronidazole resistance transfer between Giardia lamblia clones.
Methodology:
- Parasite Culture and sEV Isolation: Maintain metronidazole-resistant and wild-type susceptible Giardia clones in axenic culture. Isolate sEVs from resistant clone supernatants via differential ultracentrifugation (100,000 × g for 2 hours).
- sEV Characterization: Determine sEV size distribution and concentration using nanoparticle tracking analysis. Confirm presence of sEV markers (e.g., tetraspanins) by western blot.
- Co-culture Experiments: Incubate susceptible parasites with sEVs derived from resistant clones (50 μg/mL) for 24 hours. Include controls with no sEVs and sEVs from susceptible clones.
- Drug Sensitivity Assessment: Expose sEV-treated and control parasites to metronidazole (0-50 μM) for 48 hours. Assess viability using ATP-based assays and measure IC50 values.
- Molecular Analysis: Quantify expression of metronidazole metabolism enzymes (PFOR, nitroreductases) and ROS production in recipient parasites using qRT-PCR and fluorescent probes, respectively.
Expected Outcomes: sEVs from resistant clones should increase the metronidazole IC50 in susceptible parasites, correlate with altered expression of drug metabolism enzymes, and reduce ROS accumulation upon drug exposure [63].
Mechanisms of Drug Resistance in Entamoeba
Mutator Strain Approach for Elucidating Resistance Mechanisms
A novel "mutator" strain of Entamoeba histolytica was developed to accelerate the identification of drug resistance mechanisms. This strain expresses a proofreading-deficient, error-prone DNA polymerase δ mutant under a tetracycline-regulatable promoter, resulting in a approximately 60-fold higher mutation rate than wild-type parasites. After 66 weeks of cultivation, this mutator strain accumulated sufficient mutations to enable isolation of highly miltefosine-resistant clones [59].
Whole-genome sequencing of miltefosine-resistant clones identified shared mutations in three candidate genes. Of particular significance was a mutation in P4-ATPase (EHI096620N417K), a homolog of proteins previously implicated in miltefosine resistance in Leishmania and Saccharomyces. Researchers further demonstrated that exogenous expression of both EHI096620N417K (P4-ATPase) and EHI_035500N182I (kinase) was sufficient to confer miltefosine resistance in susceptible strains, confirming their role in the resistance phenotype [59].
The experimental workflow for generating and analyzing drug-resistant mutants using this system is illustrated below:
Complement Resistance Through Trogocytosis
Beyond drug resistance, Entamoeba histolytica employs a sophisticated mechanism to evade host immune responses through trogocytosis - the ingestion of bite-sized pieces of host cells. After performing trogocytosis on human cells, amoebae display human proteins on their surface, including negative regulators of complement activation such as CD46 and CD55. This acquisition provides protection against complement-mediated lysis, enabling bloodstream dissemination and extra-intestinal invasion [64].
Experimental evidence demonstrates that amoebae which have performed trogocytosis become resistant to lysis not only by human serum but also by mouse serum, indicating cross-species protection. Furthermore, exogenous expression of human CD46 or CD55 in amoebae was sufficient to confer resistance to mouse serum, confirming that display of these human complement regulators protects against complement activation across species barriers [64].
Research Tools and Methodologies
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Studying Resistance Mechanisms
| Reagent/Cell Line | Specific Application | Function/Utility in Resistance Research |
|---|---|---|
| E. histolytica Mutator Strain | Generation of drug-resistant mutants | Accelerates identification of resistance genes through enhanced mutation rate [59] |
| Giardia Clonal Populations (Resistant & Sensitive) | sEV transfer experiments | Enable study of horizontal resistance transfer and genotype-specific effects [63] |
| Tetracycline-Inducible System | Regulation of mutator gene expression | Allows controlled induction of high mutation rates [59] |
| Anti-CD46/Anti-CD55 Antibodies | Complement resistance studies | Confirm surface display of host complement regulators after trogocytosis [64] |
| C3-Depleted Serum | Complement pathway analysis | Determines complement dependence in serum resistance assays [64] |
| Metronidazole-Resistant Giardia sEVs | Resistance transfer studies | Investigate vesicle-mediated phenotypic adaptation [63] |
Molecular Detection of Entamoeba Species
Accurate species discrimination is crucial for epidemiological studies and understanding species-specific resistance patterns. A multiplex PCR protocol targeting the 18S rRNA gene enables differential detection of E. histolytica, E. dispar, and E. moshkovskii:
Primer Sequences:
- ENTAF: 5'-GAG CAC AGC ATG AGC GAA AT-3' (conserved forward primer)
- EhR: 5'-GAT CTA GAA CTC ACA CTT ATG T-3' (E. histolytica-specific, 166 bp product)
- EdR: 5'-CAC CAC TCC CTA CTA TTA DC-3' (E. dispar-specific, 752 bp product)
- EmR: 5'-TGA GCC CCA GAG GAG ACA T-3' (E. moshkovskii-specific, 580 bp product)
Protocol: DNA extraction from stool samples or cultures followed by PCR amplification with all four primers. Products are separated by agarose gel electrophoresis for species identification based on amplicon size. This method has proven effective in field studies, revealing unexpectedly high rates of E. moshkovskii in asymptomatic populations [62].
The challenge of drug resistance in Giardia and Entamoeba requires multifaceted research approaches spanning molecular parasitology, epidemiology, and drug discovery. The emergence of nitroimidazole-refractory giardiasis in specific geographic hotspots underscores the need for ongoing surveillance and region-specific treatment guidelines. Novel mechanisms such as sEV-mediated resistance transfer in Giardia and trogocytosis-based complement evasion in Entamoeba reveal sophisticated parasite strategies that complicate therapeutic interventions.
Innovative tools like the E. histolytica mutator strain provide powerful platforms for elucidating resistance mechanisms and identifying potential drug targets. Future research should focus on validating these findings in clinical isolates, developing point-of-care diagnostic tools for resistance detection, and exploring combination therapies that target multiple resistance pathways simultaneously. As the epidemiology of these infections continues to evolve, particularly with the changing burden in high-SDI regions, sustained research investment is crucial for maintaining effective control of these significant parasitic diseases.
Within the epidemiology of intestinal protozoan infections (IPIs) research, a critical public health challenge extends beyond the high prevalence of these diseases to the significant limitations of the therapeutic arsenal used to combat them. IPIs, caused by pathogens such as Giardia lamblia, Entamoeba histolytica, and Cryptosporidium spp., affect over a billion people globally, with a pooled prevalence of 24% reported in some endemic regions like Malaysia [44]. These infections disproportionately impact vulnerable populations, including children, immunocompromised individuals, and those in resource-limited settings, leading to substantial morbidity and mortality [65] [1]. Despite their global burden, the drug development pipeline for intestinal protozoa has been largely stagnant for decades. The current pharmacopeia is dominated by a limited number of drug classes, primarily nitroimidazoles such as metronidazole, which has been the first-line treatment for giardiasis and amoebiasis for over 60 years [1]. The efficacy of these established therapeutics is increasingly compromised by emerging drug resistance, significant adverse effects, and treatment failures in vulnerable patient populations. This whitepaper examines the primary limitations of current therapeutics for intestinal protozoan infections, analyzes the molecular mechanisms underpinning these shortcomings, and outlines essential methodological approaches for advancing drug discovery in this neglected field of research.
Major Therapeutic Limitations by Pathogen
The clinical management of major intestinal protozoan infections is challenged by a combination of drug-related toxicity, increasing treatment failures, and a sparse pipeline of novel therapeutic agents. The tables below summarize the key drugs, their limitations, and the associated molecular mechanisms for the principal intestinal protozoa.
Table 1: Current Treatment Regimens and Primary Limitations for Major Intestinal Protozoa
| Parasite | Primary Drugs | Major Limitations | Clinical Consequences |
|---|---|---|---|
| Giardia lamblia | Metronidazole, Tinidazole, Albendazole [1] | Emerging resistance, Neurological & GI toxicity, Treatment failures (~40-60% efficacy in some cases) [1] | Refractory infections, prolonged morbidity, especially in children [1] |
| Entamoeba histolytica | Metronidazole (invasive) + Luminal agents (Paromomycin/Diloxanide) [1] | Side effects (nausea, vomiting), Complex combination therapy required, No clear resistance but clinical failures occur [66] [1] | Incomplete eradication, risk of relapse and transmission [1] |
| Cryptosporidium spp. | Nitazoxanide [66] [1] | Limited efficacy in immunocompromised patients, Modest effect in malnourished children [66] | Persistent, life-threatening diarrhea in HIV/AIDS and malnourished children [65] [66] |
| Cyclospora cayetanensis | Trimethoprim-Sulfamethoxazole (TMP-SMX) [1] | High allergy prevalence, No alternative for pregnant women, Emerging resistance [1] | Treatment challenges in allergic individuals and specific patient populations [1] |
Table 2: Molecular Mechanisms of Drug Action and Resistance
| Drug/Drug Class | Primary Molecular Target | Mechanisms of Resistance |
|---|---|---|
| Nitroimidazoles (Metronidazole) | Activated by parasite ferredoxins; causes DNA fragmentation and cell cycle arrest [1] | Reduced drug activation via downregulation of pyruvate:ferredoxin oxidoreductase (PFOR) and nitroreductase activity; enhanced DNA repair [1] |
| Benzimidazoles (Albendazole) | Binds to β-tubulin, disrupting microtubule polymerization and causing cell cycle arrest [1] | Mutations in β-tubulin gene reducing drug binding affinity [1] |
| Nitazoxanide | Inhibits PFOR enzyme and nitroreductase; disrupts plasma membrane potential [1] | Mechanisms not fully elucidated; suspected overlap with nitroimidazole resistance pathways [1] |
| Paromomycin | Binds to 30S ribosomal subunit, inhibiting protein synthesis [1] | Reduced drug uptake; target site modifications [1] |
Mechanisms of Drug Failure and Resistance
Side Effect Profiles and Toxicity
The toxicity of current antiprotozoal drugs presents a significant barrier to effective treatment. Metronidazole, the most widely used drug, is associated with neurological side effects (headache, dizziness), gastrointestinal distress (nausea, metallic taste), and potential genotoxicity [1]. Its prolonged use, often required for refractory infections, increases the risk of adverse events. Furthermore, the therapeutic regimen for amoebiasis highlights the complexity of treatment, wherein a combination of tissue-active (metronidazole) and luminal agents (paromomycin or diloxanide furoate) is required for complete eradication of the parasite [1]. This multi-drug approach increases the pill burden and the potential for cumulative side effects, compromising patient compliance and treatment completion.
Clinical and Molecular Drug Resistance
Drug resistance is a growing concern, most notably in Giardia lamblia. Resistance to metronidazole, the cornerstone of giardiasis treatment for decades, has become a major clinical issue, with numerous reports of refractory infections [1]. The molecular mechanisms are multifaceted, involving the downregulation of key enzymes like pyruvate:ferredoxin oxidoreductase (PFOR) and nitroreductases responsible for activating the pro-drug within the parasite [1]. This reduced activation diminishes the cytotoxic effects of the drug. Additionally, mutations in the β-tubulin gene confer resistance to albendazole, a second-line agent, further limiting treatment options [1]. For Cryptosporidium, the problem is not classical resistance but intrinsic treatment failure, as the first-line drug nitazoxanide shows significantly reduced efficacy in immunocompromised individuals, a key risk group for severe disease [66].
Diagram 1: Molecular Mechanisms of Drug Action and Resistance in Giardia. The diagram illustrates how metronidazole and albendazole exert their effects and how parasite resistance mechanisms (red) disrupt these processes.
Experimental Protocols for Investigating Therapeutic Limitations
To advance the development of novel therapeutics, robust experimental methodologies are required to evaluate drug efficacy, resistance, and mode of action. The following protocols represent standard and advanced approaches in the field.
Protocol 1: In Vitro Drug Susceptibility and Resistance Induction
This protocol is used to determine the baseline sensitivity of parasite isolates to antiprotozoal compounds and to investigate mechanisms of resistance.
- Parasite Culture: Maintain axenic cultures of target protozoa (e.g., Giardia trophozoites) in appropriate medium (e.g., TYI-S-33) at 37°C [1].
- Drug Preparation: Prepare serial dilutions of the test drug (e.g., metronidazole, albendazole) in culture-compatible solvent (e.g., DMSO), ensuring final solvent concentration is non-toxic (<0.1%).
- IC50 Determination: Inoculate 96-well plates with log-phase trophozoites. Incubate with drug dilutions for 24-48 hours. Assess viability using colorimetric (e.g., MTT) or fluorometric assays. Calculate the half-maximal inhibitory concentration (IC50) using non-linear regression analysis.
- Resistance Induction: Subject parasites to progressively increasing sub-lethal concentrations of the drug over multiple generations (e.g., 3-6 months). Islect resistant clones via limiting dilution.
- Resistance Mechanism Analysis:
- Genomics: Sequence the whole genome or candidate genes (e.g., β-tubulin for albendazole) of resistant versus susceptible lines to identify mutations [1].
- Transcriptomics: Perform RNA-Seq to analyze differentially expressed genes, focusing on drug activation pathways (e.g., PFOR, nitroreductases) and efflux pumps [1].
- Functional Assays: Measure enzyme activity (e.g., nitroreductase) and intracellular drug accumulation in resistant clones.
Protocol 2: Assessment of Compound Efficacy in Animal Models
Animal models are critical for evaluating drug efficacy and pharmacokinetics in a whole-organism context.
- Infection Model: Use immunocompetent or immunodeficient (for Cryptosporidium) rodent models (e.g., mice, gerbils). Infect animals orally with infectious stages (cysts, oocysts). Confirm establishment of infection by monitoring fecal shedding of parasites via microscopy or PCR.
- Treatment Groups: Randomize infected animals into groups (n=5-10): vehicle control, positive control (standard drug), and experimental compound(s) at multiple doses.
- Drug Administration: Initiate treatment post-infection confirmation. Administer compounds orally or via IP injection for 5-10 days. Record clinical signs (weight, diarrhea) daily.
- Outcome Measures:
- Primary: Quantify parasite burden in feces throughout treatment and in intestinal tissues at endpoint (e.g., by qPCR or histology).
- Secondary: Assess pathological changes (villous atrophy, inflammation) in intestinal sections (ileum, cecum) via H&E staining [65].
- Pharmacokinetics: In separate studies, measure plasma and intestinal drug concentrations over time to determine exposure profiles.
- Data Analysis: Compare parasite reduction and clinical improvement between groups using appropriate statistical tests (e.g., ANOVA). The effective dose (ED50) is calculated from the dose-response curve.
Diagram 2: Experimental Workflow for Antiprotozoal Drug Discovery. This flowchart outlines the key stages in the preclinical development of new therapeutics, from initial screening to candidate selection.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential reagents and their applications in researching intestinal protozoa and evaluating new therapeutics.
Table 3: Key Research Reagents for Investigating Antiprotozoal Therapeutics
| Research Reagent | Function and Application | Key Utility in Drug Discovery |
|---|---|---|
| Axenic Culture Media (e.g., TYI-S-33) | Supports in vitro growth of parasites like Giardia and Entamoeba trophozoites without contaminants [1]. | Essential for high-throughput in vitro drug screening and maintaining laboratory strains. |
| Modified Acid-Fast Staining Kits | Differentiates and identifies acid-fast oocysts of Cryptosporidium spp. and Cyclospora cayetanensis in stool samples [16]. | Critical for diagnosing infection in animal models and clinical trials; assessing parasite burden. |
| Species-Specific PCR & qPCR Assays | Detects and differentiates parasite species (e.g., E. histolytica from E. dispar) and quantifies parasite load [65] [44]. | Gold standard for sensitive quantification of infection intensity in vitro and in vivo. |
| Recombinant Parasite Enzymes (e.g., PFOR, Nitroreductase) | Purified proteins involved in key metabolic pathways and drug activation [1]. | Used for high-throughput target-based screening and mechanistic studies of drug action/resistance. |
| Anti-Tubulin Antibodies | Label microtubules in parasite cytoskeleton for immunofluorescence microscopy. | Visualize the cytological effects of benzimidazole drugs and confirm target engagement. |
| NOD/SCID Mouse Model | Immunodeficient rodents susceptible to chronic Cryptosporidium infection [66]. | Vital for evaluating drug efficacy against cryptosporidiosis in an immunocompromised host. |
The limitations of current therapeutics for intestinal protozoan infections—encompassing significant side effects, emerging drug resistance, and a high rate of treatment failure in vulnerable populations—represent a critical obstacle in the epidemiological control of these widespread diseases. The heavy reliance on a few aging drug classes, particularly nitroimidazoles, is clinically unsustainable. Overcoming these challenges requires a multi-faceted research strategy. Future efforts must prioritize drug repurposing (e.g., auranofin, azidothymidine) to accelerate the availability of new chemical entities, and target-based drug discovery leveraged from genomic data to identify novel, parasite-specific pathways [1]. Furthermore, exploring adjunct therapies, such as probiotics to modulate the gut microbiota and potentially improve treatment outcomes, presents a promising avenue [67]. Strengthening the drug discovery pipeline through increased funding, enhanced epidemiological surveillance of resistance, and the application of advanced molecular tools is imperative to develop the next generation of safe, effective, and accessible antiprotozoal drugs.
Intestinal protozoan infections, including Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, constitute a significant global public health burden, particularly in resource-limited settings. These pathogens are primarily transmitted via the fecal-oral route through contaminated water, food, soil, and fomites, causing substantial gastrointestinal morbidity, malnutrition, and mortality worldwide [68] [69]. The epidemiology of these infections is intrinsically linked to inadequate water, sanitation, and hygiene (WASH) infrastructure, with an estimated 2.5 billion people lacking access to improved sanitation facilities [69]. This technical guide examines the evidence for WASH interventions in controlling intestinal protozoan infections, providing epidemiologists and public health researchers with a critical analysis of intervention efficacy, methodological approaches for evaluation, and strategic frameworks for optimizing integrated control programs.
Epidemiological Burden of Intestinal Protozoan Infections
The global burden of intestinal protozoan infections is substantial, though precise quantification remains challenging due to diagnostic limitations and surveillance gaps. Cryptosporidium spp. and E. histolytica were responsible for an estimated 8.4 million and 2.2 million disability-adjusted life years (DALYs), respectively, according to the Global Burden of Disease Study 2010 [69]. Giardiasis has an estimated prevalence of 2-3% in high-income countries and 20-30% in developing countries [69]. A recent meta-analysis of studies in Malaysia found an overall pooled prevalence of intestinal protozoal infections of 24%, with Entamoeba spp. being most prevalent (18%), followed by G. lamblia (11%) and Cryptosporidium spp. (9%) [44]. Significant disparities in prevalence exist across populations, with marginalized groups such as indigenous communities and people experiencing homelessness bearing a disproportionate burden [70] [44].
Transmission Pathways and Risk Factors
The classic "F-diagram" (feces, fluids, fingers, fomites, flies) illustrates the multiple transmission pathways for enteric protozoa, with WASH interventions serving as critical barriers at multiple points in this transmission cycle [71]. Key risk factors identified through meta-analyses include:
- Exposure to untreated water (pooled prevalence of 38-52% in exposed groups) [44]
- Poor sanitation facilities (open defecation associated with 38% increased risk) [70] [72]
- Suboptimal hygiene practices (limited handwashing with soap) [71]
- Low socioeconomic status and educational attainment [44]
- Residence in informal settlements or rural areas with limited infrastructure [71]
Molecular epidemiological studies have identified diverse transmission patterns, including anthroponotic transmission (person-to-person), waterborne outbreaks, and zoonotic transmission for some protozoa like Giardia [69].
Evaluating WASH Intervention Efficacy: Experimental Evidence
Randomized Controlled Trials
The WASH Benefits Bangladesh trial, a cluster-randomized controlled trial, provides robust evidence on the effects of individual and combined WASH interventions on childhood protozoan infections. After approximately 2.5 years of intervention implementation among 5,551 pregnant women in rural Bangladesh, the trial measured effects on Giardia, Cryptosporidium, and E. histolytica prevalence using multiplex real-time PCR of child stool samples [68].
Table 1: Effect of WASH Interventions on Giardia Infection Prevalence from the WASH Benefits Bangladesh Trial [68]
| Intervention Arm | Prevalence (%) | Prevalence Ratio (PR) | 95% Confidence Interval |
|---|---|---|---|
| Control | 35.5 | Reference | Reference |
| Sanitation | 26.5 | 0.75 | 0.64–0.88 |
| Handwashing | 28.2 | 0.80 | 0.66–0.96 |
| Combined WSH | 29.7 | 0.83 | 0.72–0.96 |
| Nutrition + WSH | 26.7 | 0.75 | 0.64–0.88 |
| Water Treatment | No significant effect | - | - |
| Nutrition Alone | No significant effect | - | - |
The trial demonstrated that individual handwashing and sanitation interventions significantly reduced childhood Giardia infections, with prevalence ratios of 0.80 and 0.75, respectively [68]. Interestingly, combined WSH interventions provided no additional benefit over individual interventions, suggesting potential overlap in their mechanisms of protection or ceiling effects in this context. Water treatment and nutrition interventions alone showed no significant effect on protozoan infections [68]. The low prevalence of E. histolytica and Cryptosporidium (<2%) in this setting resulted in imprecise effect estimates for these species [68].
Quasi-Experimental Studies
A quasi-experimental study among the Karen hill tribe in northern Thailand evaluated an integrated intervention program combining mass drug administration (MDA) with albendazole and WASH education [73]. The study involved 691 residents across two villages, with one village receiving the combined intervention and the other serving as a control (receiving MDA only).
Table 2: Effect of Integrated MDA and WASH Education on Intestinal Parasitic Infection (IPI) Prevalence in Northern Thailand [73]
| Time Point | Intervention Group Prevalence | Control Group Prevalence | P-value |
|---|---|---|---|
| Baseline | 36.0% (123/342) | 36.8% (96/261) | - |
| 3-month follow-up | 23.6% | No significant change | 0.002 |
| 6-month follow-up | 23.1% | No significant change | 0.002 |
The intervention group showed a significant reduction in overall IPI prevalence from 36.0% to 23.1% at 6 months, while the control group showed no significant changes despite receiving MDA [73]. The intervention group also demonstrated significant improvements in knowledge, attitudes, and practices (KAP) scores related to parasite prevention and control. This study highlights that MDA alone is insufficient for sustained control of intestinal parasitic infections due to rapid reinfection, and that integrating WASH education can significantly reduce reinfection rates in endemic populations [73].
Methodological Approaches for WASH Intervention Evaluation
Experimental Protocols and Diagnostic Methods
Cluster-Randomized Trial Methodology (based on WASH Benefits Bangladesh Trial [68]):
- Cluster Identification and Randomization: Identify geographical clusters (8 neighboring compounds with eligible pregnant women) separated by minimum 1-km buffers to prevent spillover. Randomize matched clusters to intervention arms using computer-generated random numbers.
- Intervention Components:
- Water: Provide chlorine-treated drinking water and safe storage vessels with spigots to index households.
- Sanitation: Distribute child potties and sani-scoop hoes for fecal disposal, and install double-pit latrines with hygienic water seals for all compound households.
- Handwashing: Install handwashing stations with soapy water near latrines and kitchens.
- Combined Arms: Implement integrated WSH or WSH plus nutrition interventions.
- Implementation: Train local community health promoters to support intervention adherence. Maintain >80% adherence through regular monitoring.
- Outcome Measurement: Collect stool samples from children after approximately 2.5 years of intervention. Process samples using multiplex real-time PCR for simultaneous detection of Giardia, Cryptosporidium, and E. histolytica.
- Statistical Analysis: Employ intention-to-treat analysis using targeted maximum likelihood estimation (TMLE) to estimate prevalence ratios and prevalence differences, adjusting for potential informative censoring.
Molecular Detection Protocol [68]:
- DNA Extraction: Extract genomic DNA from stool samples using commercial kits with appropriate quality controls.
- Multiplex Real-Time PCR: Perform simultaneous detection of multiple protozoan pathogens using species-specific primers and probes.
- Quantification: Use cycle threshold (Ct) values to estimate infection intensity, with Ct=40 imputed for non-detects.
- Quality Assurance: Include positive and negative controls in each run, with blinded sample analysis to prevent measurement bias.
Mechanistic Modeling Approaches
Mathematical models provide valuable tools for generalizing RCT findings and exploring counterfactual intervention scenarios. A recent analysis of the WASH Benefits Bangladesh trial developed a compartmental transmission model to evaluate how six WASH factors impact intervention effectiveness [74]:
- Preexisting WASH conditions (proportion with pre-existing WASH infrastructure)
- Disease transmission potential (baseline prevalence and reproduction number R₀)
- Intervention compliance (fidelity and adherence)
- Intervenable fraction (proportion of transmission along addressable pathways)
- Intervention efficacy (effectiveness in reducing transmission)
- Community coverage (proportion of population receiving interventions)
This modeling approach revealed that increasing community coverage had the greatest impact on intervention effectiveness, with median increases of 34.0 and 45.5 percentage points in the WSH and WSHN arms when increasing coverage to 20% [74]. The effect of community coverage depended on how much transmission occurred along pathways not modified by the interventions. Individual interventions had complementary but not synergistic effects when combined [74].
Conceptual Frameworks and Visualizations
WASH Intervention Mechanisms in Protozoan Infection Control
Cluster-Randomized Trial Evaluation Workflow
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for WASH Intervention Studies
| Reagent/Material | Application | Technical Specifications | Evidence Source |
|---|---|---|---|
| Multiplex Real-Time PCR Kits | Simultaneous detection of multiple protozoan pathogens | Species-specific primers/probes for Giardia, Cryptosporidium, E. histolytica; internal controls | [68] |
| DNA Extraction Kits | Isolation of pathogen DNA from stool samples | Optimized for difficult samples; inhibitors removal; quality control measures | [68] |
| Chlorine-based Water Treatment | Point-of-use water disinfection | Sodium hypochlorite solutions; safe storage containers with spigots | [68] [74] |
| Improved Sanitation Facilities | Fecal containment and safe disposal | Double-pit pour-flush latrines with water seals; child potties | [68] [73] |
| Handwashing Stations | Hygiene behavior promotion | Soapy water containers; designated stations near latrines/kitchens | [68] [73] |
| Stool Collection Kits | Sample acquisition and preservation | Standardized containers; transport media; cold chain maintenance | [68] [73] |
| Structured Questionnaires | KAP assessment and covariate data collection | Validated instruments; local language adaptation; digital data capture | [70] [73] |
Discussion and Strategic Recommendations
The evidence synthesized in this review indicates that WASH interventions can significantly reduce intestinal protozoan infections, but their effectiveness depends critically on implementation context, specific pathogens targeted, and intervention design. Several key insights emerge for optimizing control strategies:
Intervention Selection and Targeting
- Sanitation and handwashing interventions demonstrate more consistent efficacy against Giardia compared to water treatment alone [68]. This may reflect the importance of direct fecal-oral transmission pathways for this pathogen, which are better interrupted by sanitation and hygiene measures.
- Combined interventions may not provide additive benefits over single interventions in all settings, potentially due to overlapping mechanisms of protection or implementation constraints [68]. This suggests the importance of context-specific intervention selection rather than presuming combination approaches are always superior.
- Interventions should be prioritized for high-risk populations, including indigenous communities, people experiencing homelessness, and residents of informal settlements where WASH access is most limited [70] [44].
Implementation Considerations
- Community coverage appears to be a critical determinant of intervention effectiveness, with modeling studies suggesting coverage thresholds of at least 20% for meaningful impact [74]. This highlights the importance of population-level coverage rather than only household-level adoption.
- Behavioral components (knowledge, attitudes, practices) are essential for sustained effectiveness, as demonstrated by the success of integrated MDA and WASH education programs in reducing reinfection rates [73].
- Intervention fidelity and adherence must be maintained at >80% levels to achieve significant effects, requiring robust community engagement and ongoing support [68].
Research Gaps and Future Directions
Future research should address several critical knowledge gaps:
- Pathogen-specific intervention effects require further elucidation, particularly for Cryptosporidium and E. histolytica, which were underpowered in previous trials [68].
- Optimal intervention sequencing and combinations need evaluation across diverse epidemiological contexts.
- Novel implementation strategies that enhance coverage and adherence in hard-to-reach populations warrant development and testing.
- Long-term sustainability of WASH intervention effects remains inadequately documented, particularly after external support ends.
WASH interventions represent essential tools for controlling intestinal protozoan infections, with compelling evidence supporting the efficacy of sanitation and handwashing interventions against Giardia infections. The optimization of these interventions requires careful consideration of local epidemiology, transmission pathways, and social context. Integrated approaches that combine WASH improvements with behavioral change communication and, where appropriate, pharmacological interventions, offer the most promising strategy for sustainable control. Future research should prioritize the development of targeted, cost-effective interventions that achieve high community coverage and address the specific needs of vulnerable populations. As the field advances, mechanistic modeling and molecular epidemiological tools will play increasingly important roles in refining intervention strategies and accelerating progress toward the control and elimination of intestinal protozoan infections.
Novel Drug Targets and Repurposing Efforts in the Pipeline
Intestinal protozoan infections, including giardiasis, amoebiasis, cryptosporidiosis, and cyclosporiasis, present a substantial global health burden, particularly in tropical regions and among vulnerable populations. Entamoeba histolytica, Giardia lamblia, Cryptosporidium species, and Cyclospora cayetanensis are among the primary pathogens responsible for severe diarrheal illnesses, contributing significantly to morbidity and mortality in children and immunocompromised individuals [44] [75] [1]. The epidemiology of these infections reveals a troubling prevalence, with a recent meta-analysis in Malaysia reporting an overall pooled prevalence of 24% for intestinal protozoal infections, with Entamoeba spp. (18%) and G. lamblia (11%) being most common [44]. Risk factors such as inadequate sanitation, limited access to clean water, low socioeconomic status, and poor hygiene practices perpetuate transmission cycles [44] [75].
The current therapeutic landscape for intestinal protozoan infections faces multiple challenges, including limited drug efficacy, emerging drug resistance, and problematic side effects. Metronidazole, the primary treatment for giardiasis and amoebiasis, demonstrates reduced efficacy against resistant strains and presents toxicity concerns [76] [1]. Similarly, nitazoxanide, the only FDA-approved drug for cryptosporidiosis, shows limited effectiveness in immunocompromised patients [77] [76]. These limitations underscore the urgent need for novel therapeutic approaches targeting innovative molecular pathways and exploring drug repurposing strategies to accelerate the development of effective treatments.
Emerging Novel Drug Targets
Calcium-Dependent Protein Kinase 1 (CDPK1) in Cryptosporidium
Cryptosporidium stands out among the top diarrheal pathogens with no effective treatments or vaccines, causing over 50,000 annual deaths in children under five and posing particular risks to immunocompromised adults [77]. An essential enzyme for Cryptosporidium survival, CDPK1 (Calcium dependent protein kinase 1), has emerged as a promising drug target. Research demonstrates that silencing CDPK1 significantly reduces parasite growth, establishing it as a validated target for therapeutic intervention [77].
CDPK1 exhibits structural features distinct from human kinase enzymes, presenting opportunities for selective inhibitor design that can target the parasite without harming host tissues [77]. Current drug discovery efforts led by the University of Houston are focusing on designing drug candidates with enterohepatic recycling properties, enabling them to remain in the system longer by being absorbed through the liver and then redirected to the intestine. Additionally, researchers are engineering these compounds for gastrointestinal (GI)-targeting to minimize systemic exposure and directly deliver drugs to the site of Cryptosporidium infections [77]. Success in demonstrating GI-targeting would represent a significant advancement not only for cryptosporidiosis but also for drug design strategies targeting other GI conditions, including colonic cancers and inflammatory bowel diseases.
Cysteine Proteases in Entamoeba histolytica and Giardia lamblia
Cysteine proteases play crucial roles in the pathogenesis of several intestinal protozoa, facilitating tissue invasion, nutrient acquisition, and immune evasion. In E. histolytica, these enzymes degrade extracellular matrix components and disrupt host immune responses, making them attractive molecular targets for drug development [1].
Recent computational studies investigating Fowlerpain-1 (FWP1), a papain-like cysteine protease in Naegleria fowleri, have provided structural insights applicable to intestinal protozoa. Research utilizing AlphaFold2-Multimer modeling and molecular dynamics simulations has identified stable interaction interfaces between proteases and endogenous inhibitors like stefins [78]. These studies revealed two conserved motifs (PG and QVVAG) as critical mediators of active-site recognition, identifying a concave binding pocket with both hydrophobic and polar characteristics suitable for high-affinity ligand binding [78]. These findings support the structural hypothesis for selective protease inhibition and identify stefins as promising scaffolds for developing structure-guided therapeutics targeting protozoan cysteine proteases.
Thioredoxin Reductase in Multiple Protozoa
The thioredoxin system, essential for maintaining redox homeostasis in parasitic protozoa, represents another promising target pathway. Thioredoxin reductase, an enzyme involved in reactive oxygen species detoxification, has been validated as a vulnerable target in E. histolytica, G. lamblia, and Cryptosporidium parvum [76].
High-throughput screening campaigns against E. histolytica identified auranofin, an FDA-approved anti-rheumatic drug, as a potent inhibitor of thioredoxin reductase. Auranofin demonstrated a half-maximal effective concentration (EC~50~) 10-fold better in vitro than metronidazole (0.5 μM vs. 5 μM) against E. histolytica [76]. Importantly, auranofin maintained efficacy against metronidazole-resistant Giardia strains, with no significant difference in EC~50~ between metronidazole-sensitive parental isolates and their metronidazole-resistant isogenic derivative lines [76]. This cross-species activity highlights the potential of targeting conserved essential pathways across multiple protozoan parasites.
Table 1: Promising Novel Drug Targets for Intestinal Protozoan Infections
| Drug Target | Parasite | Biological Function | Therapeutic Approach | Development Status |
|---|---|---|---|---|
| CDPK1 | Cryptosporidium spp. | Calcium-dependent signaling for survival | Selective kinase inhibitors; GI-targeted drugs | Preclinical development |
| Cysteine Proteases | E. histolytica, G. lamblia | Tissue invasion, immune evasion | Stefins as scaffold for inhibitors | Computational modeling |
| Thioredoxin Reductase | E. histolytica, G. lamblia, C. parvum | Redox homeostasis, oxidative stress defense | Auranofin repurposing | Clinical trial phase IIa for giardiasis |
| β-tubulin | G. lamblia | Cytoskeleton formation, cell division | Albendazole derivatives | Clinical use with emerging resistance |
| Pyruvate:Ferredoxin Oxidoreductase (PFOR) | G. lamblia, Cryptosporidium spp. | Energy metabolism | Nitazoxanide and derivatives | FDA-approved with limitations |
Drug Repurposing Strategies and Candidates
Auranofin for Giardiasis and Amoebiasis
Drug repurposing represents a promising strategy for accelerating the development of antiprotozoal therapies by leveraging compounds with established safety profiles. Auranofin, a gold-containing compound approved for rheumatoid arthritis, has demonstrated remarkable efficacy against multiple intestinal protozoa. Clinical trial phase IIa (NCT02736968) revealed that auranofin significantly decreases parasite load of G. lamblia and effectively clears metronidazole-resistant infections [1].
Auranofin's multivalent activity against various protozoa stems from its inhibition of thioredoxin reductase, disrupting the parasite's antioxidant defense system. Beyond its activity against trophozoites, auranofin exhibits cysticidal activity, effectively killing Entamoeba invadens cysts within 72 hours - a significant advantage over metronidazole which lacks efficacy against cysts [76]. This comprehensive antiparasitic activity, combined with its established safety record and potential for cost-effective production, positions auranofin as a promising therapeutic alternative, particularly in resource-limited settings where metronidazole resistance is emerging.
Medicines for Malaria Venture (MMV) Pathogen Box Compounds
The MMV Pathogen Box, a collection of bioactive compounds with antiparasitic potential, has yielded promising candidates for drug repurposing against protozoan infections. Screening of this compound library identified several molecules with significant activity against Toxoplasma gondii, offering potential for application against intestinal protozoa with similar biological pathways [79].
Three MMV Pathogen Box compounds - MMV675968, MMV022478, and MMV021013 - demonstrated potent anti-Toxoplasma activity in both human trophoblastic cells (BeWo) and third-trimester placental villous explants [79]. At non-toxic concentrations, these compounds irreversibly inhibited parasite proliferation and interfered with early stages of the lytic cycle, including adhesion and infection. Morphological analysis revealed that treated tachyzoites exhibited membrane disruption, cytoplasmic degradation, and organelle disorganization [79]. Among these candidates, MMV021013 stands out as particularly promising due to its favorable pharmacokinetic properties, including predicted gastrointestinal absorption and blood-brain barrier permeability, with no predicted mutagenic, tumorigenic, irritant, or reproductive effects [79].
Additional Repurposing Candidates
Several other drug repurposing candidates show promise for treating intestinal protozoan infections:
Azidothymidine (AZT), an antiretroviral drug, exhibits inhibitory activity against G. lamblia by targeting the enzyme triosephosphate isomerase (TimGi). AZT directly binds to TimGi and induces conformational changes that disrupt enzyme function [1]. This interaction between AZT and TimGi highlights the potential of targeting glycolytic enzymes in anaerobic protozoa, which depend heavily on glycolysis for energy production.
Nitroxoline, an antibiotic used for urinary tract infections, has demonstrated potent antitrypanosomal activity and may have applications against intestinal protozoa. Studies show that nitroxoline exhibits significantly greater efficacy than benznidazole against both epimastigote and intracellular amastigote forms of Trypanosoma cruzi [78], suggesting potential cross-reactivity against other protozoan pathogens.
Curcumin and curcumin nanoemulsion (CR-NE) have emerged as promising therapeutic agents for cyclosporiasis. In murine models, CR-NE demonstrated superior efficacy compared to trimethoprim-sulfamethoxazole (TMP-SMX), the current standard treatment [1]. The anti-protozoal activity of curcumin appears to involve regulation of transcription pathways, induction of cellular death through activation of intracellular calcium release, and mitochondrial membrane depolarization.
Table 2: Promising Repurposed Drug Candidates for Intestinal Protozoan Infections
| Drug Candidate | Original Indication | Target Protozoa | Mechanism of Action | Development Status |
|---|---|---|---|---|
| Auranofin | Rheumatoid arthritis | E. histolytica, G. lamblia, C. parvum | Thioredoxin reductase inhibition | Phase IIa clinical trial for giardiasis |
| MMV021013 | Antiparasitic screening | T. gondii (potential for intestinal protozoa) | Interferes with early lytic cycle | Preclinical testing |
| Azidothymidine (AZT) | HIV/AIDS | G. lamblia | Binds triosephosphate isomerase | Experimental validation |
| Nitroxoline | Urinary tract infections | T. cruzi (potential cross-reactivity) | Under investigation for mechanism | Experimental validation |
| Curcumin nanoemulsion | Anti-inflammatory | C. cayetanensis | Induces apoptosis, mitochondrial disruption | Murine models |
Experimental Models and Methodologies
In Vitro Screening Platforms
Robust in vitro screening methodologies form the foundation of antiprotozoal drug discovery. For anaerobic intestinal parasites like E. histolytica and G. lamblia, researchers have developed specialized high-throughput screening (HTS) platforms that maintain oxygen-free environments to mimic natural habitats [76]. These automated systems enable rapid evaluation of compound libraries against both parasites using similar assay conditions, significantly accelerating the discovery timeline.
For Cryptosporidium species, in vitro models typically employ human colorectal adenocarcinoma cells (HCT-8), which originate from the ileocecal region corresponding to the site of human infection [76]. These infection models facilitate quantitative assessment of compound efficacy through various methods, including real-time PCR quantification of parasite burden using C. parvum heat shock protein 70 (Hsp70)-specific primers [76]. Standardized protocols involve treating infected cells with compound concentrations typically ranging from 1-20 μM for 48 hours, with efficacy determined by comparing parasite burden between treated and untreated wells.
Advanced Phenotypic Screening Assays
Innovative phenotypic screening approaches have been developed specifically for protozoan parasites. For Toxoplasma gondii, researchers employ sophisticated screening protocols using human trophoblastic cells (BeWo) and third-trimester placental villous explants to evaluate compound effects on the parasite's lytic cycle, including adhesion, invasion, and intracellular proliferation [79]. These comprehensive assessments include evaluation of compound toxicity, irreversible inhibition of parasite proliferation, morphological alterations through electron microscopy, and impact on host immune responses through cytokine quantification.
For Plasmodium species, which serve as models for protozoan research, advanced transmission-blocking platforms have been established using transgenic NF54/iGP1_RE9Hulg8 parasites engineered to conditionally produce large numbers of stage V gametocytes expressing a red-shifted firefly luciferase viability reporter [80]. This innovative system enables both in vitro screening and in vivo assessment of gametocyte killing and clearance kinetics through whole animal bioluminescence imaging in humanized mouse models, providing a comprehensive platform for evaluating transmission-blocking drug efficacy.
Diagram 1: Drug Discovery Workflow for Intestinal Protozoan Infections. This diagram illustrates the integrated experimental pipeline from initial screening to lead candidate identification.
Target Validation and Mechanism of Action Studies
Comprehensive target validation represents a critical step in the drug discovery pipeline. For kinase targets like CDPK1 in Cryptosporidium, researchers employ structural biology approaches to identify unique features that enable selective inhibitor design [77]. Advanced techniques including X-ray crystallography and comparative genomics help identify parasite-specific structural features that can be exploited for selective targeting.
For characterizing compound mechanism of action, researchers utilize diverse methodologies including:
- Molecular docking studies to predict interactions between compounds and potential molecular targets [78]
- Molecular dynamics simulations to assess binding stability and conformational changes [78]
- Gene expression profiling to identify transcriptional changes induced by compound treatment
- Metabolomic approaches to detect alterations in parasite metabolic pathways
- Resistance selection studies to identify potential target pathways
These integrated approaches facilitate the translation of hit compounds to lead candidates with defined molecular targets and mechanisms of action.
Research Reagent Solutions
Table 3: Essential Research Reagents for Antiprotozoal Drug Discovery
| Reagent/Cell Line | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Cell Lines | HCT-8 (human colorectal adenocarcinoma) | Cryptosporidium in vitro culture | From ileocecal region, corresponds to infection site |
| Cell Lines | BeWo (human trophoblastic) | Toxoplasma invasion and proliferation studies | Maternal-fetal interface model |
| Animal Models | Humanized NODscidIL2Rγ^null^ mice | Plasmodium transmission-blocking studies | Supports P. falciparum gametocytes |
| Animal Models | Hamster model | Amebic liver abscess studies | For in vivo efficacy testing |
| Compound Libraries | MMV Pathogen Box, Malaria Box | High-throughput screening | Bioactive compounds with antiparasitic activity |
| Compound Libraries | FDA-approved drug libraries | Drug repurposing screens | Compounds with known safety profiles |
| Reporter Parasites | NF54/iGP1_RE9Hulg8 P. falciparum | Transmission-blocking drug assessment | Express red-shifted firefly luciferase |
| Detection Assays | Real-time PCR (C. parvum Hsp70) | Parasite burden quantification | Enables precise quantification of infection |
| Detection Assays | Luciferase reporter assays | Viability assessment for transgenic parasites | Enables high-throughput screening |
The pipeline for novel drug targets and repurposing efforts against intestinal protozoan infections has expanded significantly, driven by advances in molecular parasitology, screening technologies, and structural biology. Promising targets like CDPK1 in Cryptosporidium and cysteine proteases in E. histolytica offer opportunities for selective therapeutic intervention, while drug repurposing candidates such as auranofin and MMV Pathogen Box compounds provide accelerated paths to clinical application.
The ongoing challenges of drug resistance and limited treatment options for vulnerable populations underscore the imperative for sustained investment in protozoan drug discovery. Integration of innovative screening platforms, robust validation methodologies, and collaborative frameworks between academic institutions, pharmaceutical companies, and global health organizations will be essential to translate these promising approaches into effective therapies that reduce the substantial global burden of intestinal protozoan infections.
Future directions should emphasize combination therapies targeting multiple parasitic pathways simultaneously, development of formulations with improved gastrointestinal targeting, and application of artificial intelligence-assisted drug design to optimize lead compounds. With concerted effort and strategic investment, the coming decade promises significant advances in the therapeutic arsenal against these neglected tropical diseases.
Validating Epidemiological Trends and Comparative Analysis of Control Measures
Meta-analysis of prevalence studies is a powerful epidemiological tool for synthesizing population-level estimates of disease burden, particularly for conditions such as intestinal protozoan infections. The process of validating the pooled prevalence estimate and quantifying, interpreting, and managing heterogeneity is fundamental to the reliability and interpretation of these findings. This technical guide provides an in-depth examination of these core components, framed within the context of intestinal protozoan infections research. It offers researchers and drug development professionals a detailed framework for conducting robust meta-analyses, including structured protocols for statistical validation, graphical workflows for investigating heterogeneity, and a comprehensive toolkit of essential methodological reagents. By adhering to these guidelines, scientists can enhance the rigor of their evidence synthesis, leading to more accurate public health interventions and resource allocation for parasitic disease control.
In infectious disease epidemiology, understanding the true burden of a condition is the first step toward effective control and prevention. Intestinal protozoan infections, caused by parasites such as Entamoeba histolytica, Giardia lamblia, and Cryptosporidium spp., represent a significant global health challenge, particularly in resource-limited settings. Individual prevalence studies provide snapshots of this burden in specific locations and populations. However, a meta-analysis synthesizes these disparate estimates to produce a single pooled prevalence figure, offering a more precise and generalizable understanding of the disease landscape. For instance, a recent meta-analysis on intestinal protozoal infections in Malaysia found an overall pooled prevalence of 24%, with Entamoeba spp. being the most common at 18% [44]. Such a figure is far more informative for policymakers than a collection of variable individual study estimates.
The validity of this pooled estimate, however, is not a given. It is contingent upon a rigorous process of statistical validation and a nuanced interpretation of heterogeneity—the statistical variation in observed effects across the included studies. Heterogeneity is not merely a statistical nuisance; it is an inevitable feature of meta-analyses that, when properly investigated, can reveal valuable insights into sociodemographic, geographical, and methodological sources of variation in disease prevalence [81]. This guide details the protocols for validating pooled estimates and navigating the complexity of heterogeneity, using examples from the field of intestinal protozoan research to illustrate key concepts.
Core Concepts: Pooled Prevalence and Heterogeneity
The Pooled Prevalence Estimate
The pooled prevalence estimate is the weighted average of the prevalence figures from the individual studies included in the meta-analysis. The weights are typically inverse-variance, meaning that studies providing more precise estimates (with narrower confidence intervals) contribute more to the final pooled result. This estimate is almost always derived using a random-effects model, which explicitly assumes that the true underlying prevalence may vary from study to study. This model is more appropriate than a fixed-effect model for prevalence meta-analyses, where clinical and methodological diversity is expected. The result is reported as a point estimate with a 95% confidence interval (CI). For example, a meta-analysis of chronic widespread pain reported a pooled prevalence of 10.6% (95% CI: 8.6-12.9) [82].
Understanding and Quantifying Heterogeneity
Heterogeneity refers to the variability in study outcomes beyond what would be expected by chance alone. In meta-analysis, it is quantified using several key statistics:
- I² Statistic: This describes the percentage of total variation across studies that is due to heterogeneity rather than chance. It is a widely used, standardized measure. An I² of 0% indicates no observed heterogeneity, while values of 25%, 50%, and 75% are typically interpreted as low, moderate, and high, respectively. Crucially, in meta-analyses of prevalence, I² values are frequently very high (a median of 96.9% was observed in one sample), and should be interpreted with caution as they can be influenced by the number of studies and the extremity of the pooled estimate [83].
- τ² (Tau-squared): This estimates the variance of the true effects across studies. It is measured on the same scale as the effect measure (e.g., for a logit-transformed prevalence), making it less directly interpretable than I², but more absolute.
- Prediction Interval: While the 95% CI expresses the uncertainty around the average prevalence, the 95% prediction interval estimates the range within which the true prevalence of a future, similar study would be expected to fall. It is a more useful measure for appreciating the practical implications of heterogeneity and is calculated as:
pooled mean ± t-value * √(τ² + SE²)[81].
Table 1: Key Statistical Measures in a Prevalence Meta-Analysis
| Measure | Definition | Interpretation | Example from Literature |
|---|---|---|---|
| Pooled Prevalence | Weighted average prevalence across studies. | The best single estimate of the average disease burden. | 24% overall pooled prevalence for intestinal protozoan infections in Malaysia [44]. |
| 95% Confidence Interval (CI) | Range of plausible values for the average prevalence. | A narrow CI indicates higher precision in the pooled estimate. | 10.6% (95% CI: 8.6-12.9) for chronic widespread pain [82]. |
| I² Statistic | Percentage of total variability due to heterogeneity. | High values are common in prevalence meta-analyses and require careful investigation. | I² = 98.94% in a meta-analysis of intestinal protozoan infections, indicating very high heterogeneity [44]. |
| τ² (Tau-squared) | Estimated variance of the true prevalence across studies. | A higher τ² indicates greater dispersion of true study effects. | Not always reported, but essential for understanding the absolute amount of heterogeneity. |
| 95% Prediction Interval | Range for the expected prevalence in a new study. | Provides a more realistic expectation of the variation in the real world. | If pooled prevalence is 10% and τ is large, a 95% PI might be 2% to 25%. |
Experimental Protocols for Validation and Investigation
Protocol 1: Validating the Pooled Estimate
A robust pooled estimate is not just a number generated by software; it is a conclusion validated through multiple sensitivity analyses.
- Primary Analysis: Calculate the pooled prevalence using a random-effects model with a double arcsine transformation. This transformation stabilizes the variances of study-specific prevalence estimates, which is particularly important when prevalences are close to 0% or 100%, preventing studies with extreme estimates from being over-weighted [82].
- Risk of Bias Assessment: Use a validated tool (e.g., the QUADAS-2 for diagnostic studies, or domains from the Quality in Prognosis Studies tool) to assess the methodological quality of each included study. Stratify studies as having "low" versus "moderate/high" risk of bias.
- Sensitivity Analysis - Risk of Bias: Re-calculate the pooled prevalence using only studies judged to be at a low risk of bias. Compare this estimate to the primary analysis. A stable estimate increases confidence in the result. For example, in the chronic widespread pain meta-analysis, the pooled prevalence increased from 10.6% to 11.8% when only low-risk studies were considered [82].
- Sensitivity Analysis - Influence Analysis: Iteratively remove one study at a time and re-run the meta-analysis to determine if any single study is exerting a disproportionate influence on the pooled result.
Protocol 2: Investigating Heterogeneity
When high heterogeneity (e.g., I² > 75%) is identified, pre-planned subgroup analyses and meta-regression should be employed to explore its sources.
- Pre-specify Hypotheses: Before analyzing the data, hypothesize potential sources of heterogeneity (e.g., geographical region, patient age, diagnostic method).
- Subgroup Analysis: Stratify the studies based on these categorical variables and calculate pooled estimates for each subgroup. Differences between subgroups can explain heterogeneity.
- Meta-Regression: Use meta-regression to investigate the association between continuous or multiple study-level variables (e.g., mean age of participants, year of publication) and the prevalence estimate. This statistically tests whether a specific covariate can explain some of the between-study variance (τ²).
Visualization of Workflows and Relationships
Meta-Analysis Workflow for Prevalence Studies
This diagram outlines the core sequential process for conducting and validating a meta-analysis of prevalence, from literature search to final interpretation.
Heterogeneity Investigation Pathway
This diagram details the logical decision process for responding to and interpreting high heterogeneity in a meta-analysis.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key methodological "reagents" essential for conducting a rigorous meta-analysis of prevalence.
Table 2: Essential Methodological Reagents for a Prevalence Meta-Analysis
| Research 'Reagent' | Function / Application | Technical Specifications & Examples |
|---|---|---|
| Systematic Search Protocol | To identify all relevant, unbiased evidence for the research question. | A pre-registered strategy (e.g., on PROSPERO) combining keywords and database-specific subject terms for the disease (e.g., "intestinal protozoan", "giardiasis") and study design ("prevalence", "cross-sectional study") [82] [44]. |
| Data Extraction Form | To consistently capture key data from each included study. | A standardized electronic form capturing population demographics, sample size, number of cases, case definition (e.g., ACR criteria, PCR-confirmed), diagnostic method, and geographical data [82]. |
| Statistical Software & Packages | To perform complex meta-analytical calculations and generate visualizations. | R (with packages meta, metafor), Stata ( metan command), or dedicated add-ins like MetaXL for Microsoft Excel [82]. |
| Risk of Bias Assessment Tool | To methodologically appraise the quality and limitations of included studies. | Tools specific to study design, such as the JBI Critical Appraisal Checklist for Prevalence Studies or relevant domains from the QUIPS (Quality In Prognosis Studies) tool [82]. |
| Data Transformation Formula | To stabilize variances for pooling prevalence data, especially near 0% or 100%. | The Double Arcsine Transformation is recommended. The final pooled result and its confidence interval are then back-transformed to the original prevalence scale for interpretation [82]. |
The meta-analysis of prevalence studies provides a powerful, quantitative summary of disease burden, but its validity hinges on a rigorous and transparent process. Researchers must move beyond simply calculating a pooled estimate and a high I² value. By employing sensitivity analyses to validate the estimate, using prediction intervals to convey the implications of heterogeneity, and proactively investigating sources of variation through subgroup analysis and meta-regression, scientists can produce more reliable and informative results. In the context of intestinal protozoan infections, this rigorous approach is indispensable for generating the evidence base needed to guide effective public health policy, target interventions to high-risk populations, and ultimately reduce the global burden of these parasitic diseases.
Intestinal protozoan infections (IPIs), caused by pathogens such as Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, represent a significant global health burden, particularly in tropical and subtropical regions [36]. These infections are a leading cause of diarrheal diseases, affecting approximately 3.5 billion people annually worldwide [84] [3]. Accurate diagnosis is fundamental to epidemiological research, effective patient management, and the development of control strategies. However, the diagnosis of intestinal protozoa presents considerable challenges due to the diversity of pathogens, varying technological resources across regions, and limitations inherent in all current diagnostic methods [36].
This technical guide provides a data-driven analysis of the diagnostic methods for intestinal protozoa, focusing on their comparative efficacy within epidemiological research. We synthesize recent multicenter study data, systematic reviews, and meta-analyses to evaluate traditional and advanced diagnostic platforms. The objective is to offer researchers, scientists, and drug development professionals a comprehensive resource for selecting appropriate diagnostic methodologies based on performance characteristics, operational requirements, and research goals.
Current Diagnostic Landscape and Performance Metrics
The diagnostic landscape for intestinal protozoa is diverse, encompassing conventional techniques, immunodiagnostic methods, and molecular assays. Each platform offers distinct advantages and limitations, which must be carefully considered within the context of the research objectives and available resources [36].
Conventional Microscopy
Microscopic examination of stool specimens remains the most widely used diagnostic method, particularly in resource-limited settings [84] [36]. As a reference standard, it offers the advantages of low cost and the ability to detect a broad range of parasites not targeted by specific molecular tests [84].
However, microscopy has significant limitations. Its sensitivity and specificity are highly dependent on the skill of the microscopist and the quality of the sample [84] [36]. Furthermore, it cannot differentiate between morphologically identical species, such as pathogenic E. histolytica and non-pathogenic E. dispar [84]. The sensitivity of microscopy for detecting Cryptosporidium spp. with modified acid-fast staining is only 54.8%, and for G. duodenalis using a permanent stained smear, it is approximately 66.4% [36].
Immunodiagnostic Methods
Immunodiagnostic techniques, including enzyme-linked immunosorbent assay (ELISA), rapid enzyme immunoassay (EIA), and immunochromatographic tests (ICT), detect parasite-specific antigens or host antibodies [36]. These methods are generally inexpensive, user-friendly, and provide rapid results, making them suitable for rapid screening [84] [36].
A key advancement is the development of antigen-detection tests that use monoclonal antibodies against the E. histolytica adhesin Gal/GalNAc lectin, allowing for differentiation from E. dispar [36]. However, the sensitivity of these antigen-detection tests ranges from 80% to 94% compared to polymerase chain reaction (PCR), and some require fresh or unpreserved fecal samples [36]. Immunofluorescence microscopy offers higher sensitivity and specificity than traditional microscopy but is more expensive and requires expert personnel [84].
Molecular Diagnostics
Molecular methods, particularly real-time PCR (RT-PCR), are gaining traction in non-endemic areas with low parasitic prevalence due to their enhanced sensitivity and specificity [84]. These methods are especially valuable for genetic characterization, epidemiological investigations, and detecting low pathogen loads [85] [36].
Multiplex PCR panels can simultaneously detect multiple pathogens (viruses, bacteria, and parasites) in a single stool sample, providing results in hours rather than days [85]. A 2025 multicenter study in Italy demonstrated complete agreement between a commercial RT-PCR test (AusDiagnostics) and an in-house RT-PCR assay for detecting G. duodenalis, with both methods showing high sensitivity and specificity comparable to microscopy [84].
A significant technical challenge for molecular detection of protozoa is the robust wall structure of these organisms, which can complicate DNA extraction from parasite oocysts [84]. The performance of molecular assays is also influenced by sample preservation, with PCR results from preserved stool samples often being better than those from fresh samples due to superior DNA preservation [84].
Table 1: Comparative Analysis of Diagnostic Methods for Key Intestinal Protozoa
| Diagnostic Method | Target Protozoa | Sensitivity & Specificity | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Microscopy | Broad spectrum | Variable; low sensitivity for Cryptosporidium (~55%) [36] | Low cost; detects multiple parasites [84] | Cannot differentiate pathogenic species [84] |
| Immunoassay (Antigen Detection) | E. histolytica, Giardia, Cryptosporidium | Sensitivity: 80-94% vs. PCR for E. histolytica [36] | Rapid; user-friendly; differentiates E. histolytica from E. dispar [36] | Requires fresh/unpreserved samples (some tests) [36] |
| In-house RT-PCR | G. duodenalis, Cryptosporidium spp., E. histolytica, D. fragilis | High agreement with commercial PCR for Giardia [84] | High sensitivity/specificity; customizable [84] | Requires standardization and validation [84] |
| Commercial Multiplex PCR Panels | Comprehensive pathogen panels | High sensitivity/specificity [85] | Detects co-infections; rapid turnaround [85] | High cost; may detect organisms of uncertain significance [85] |
Data-Driven Insights from Recent Studies
Recent multicenter trials and meta-analyses provide robust, quantitative insights into the performance and epidemiological context of these diagnostic methods.
Multicenter Molecular Method Evaluation
A 2025 multicentre study across 18 Italian laboratories compared a commercial RT-PCR test (AusDiagnostics) and an in-house RT-PCR assay against traditional microscopy for identifying infections with G. duodenalis, Cryptosporidium spp., E. histolytica, and Dientamoeba fragilis [84].
The study analyzed 355 stool samples (230 fresh, 125 preserved). The data showed complete agreement between the AusDiagnostics and in-house PCR methods for detecting G. duodenalis, with both demonstrating high sensitivity and specificity similar to conventional microscopy. For Cryptosporidium spp. and D. fragilis detection, both molecular methods showed high specificity but limited sensitivity, which was likely attributable to inadequate DNA extraction from the parasite [84].
A critical finding was that molecular assays were essential for the accurate diagnosis of E. histolytica, as they can differentiate it from non-pathogenic look-alikes. Overall, PCR results from preserved stool samples were superior to those from fresh samples, underscoring the importance of sample preservation for molecular diagnostics [84].
Epidemiological Context and Risk Factors
A 2025 systematic review and meta-analysis focusing on Malaysia estimated the overall pooled prevalence of IPIs at 24% (95% CI: 0.17–0.29) [44]. Among the specific protozoa identified, Entamoeba spp. had the highest prevalence at 18% (95% CI: 0.12–0.24), followed by G. lamblia at 11% (95% CI: 0.08–0.14) and Cryptosporidium spp. at 9% (95% CI: 0.03–0.14) [44]. This high prevalence underscores the substantial disease burden in many regions.
Subgroup analysis revealed significant regional variation, with Kelantan state having the highest prevalence (39%) and Selangor and Kuala Lumpur reporting the lowest (13.6%) [44]. The analysis of ten risk factors found that pooled prevalence was significantly higher (38–52%) in children under 15, males, individuals with low income or no formal education, and those exposed to untreated water, poor sanitation, or unhygienic practices [44]. A study from Ethiopia corroborated these findings, identifying mother/guardian illiteracy, absence of a functional toilet, handwashing without soap, and frequent contact with animals as significant risk factors [75].
Table 2: Pooled Prevalence and Associated Risk Factors for IPIs (Malaysia Meta-Analysis 2025)
| Epidemiological Measure | Finding | Significance/Notes |
|---|---|---|
| Overall Pooled Prevalence | 24% (95% CI: 17.0–29.0) [44] | I² = 98.94%, (P < 0.001); indicates high heterogeneity [44] |
| Protozoa-Specific Prevalence | ||
| ➝ Entamoeba spp. | 18% (95% CI: 0.12–0.24) [44] | Highest burden among the three protozoa studied [44] |
| ➝ Giardia lamblia | 11% (95% CI: 0.08–0.14) [44] | Significant cause of diarrheal disease [44] |
| ➝ Cryptosporidium spp. | 9% (95% CI: 0.03–0.14) [44] | Particularly severe in immunocompromised individuals [44] |
| Key Associated Risk Factors | Children under 15, male gender, low income/no formal education, untreated water, poor sanitation, unhygienic practices [44] | Pooled prevalence 38%–52% in groups with these risk factors [44] |
Experimental Protocols for Diagnostic Evaluation
For researchers aiming to validate or compare diagnostic methods, the following protocols, derived from recent studies, provide a robust framework.
Protocol 1: Multicenter Comparison of Molecular and Microscopic Methods
This protocol is adapted from the 2025 Italian multicentre study [84].
- Sample Collection and Preparation: Collect stool samples systematically. Divide each sample: one portion for immediate microscopic examination and another for molecular testing. For molecular analysis, preserve a portion in appropriate media like Para-Pak or S.T.A.R. Buffer. Store samples at -20°C until processing [84].
- Microscopic Examination: Perform conventional microscopy on fresh samples using Giemsa stain. Examine fixed samples using the formalin-ethyl acetate (FEA) concentration technique. All examinations should adhere to WHO and CDC guidelines [84].
- Automated Nucleic Acid Extraction: Use the MagNA Pure 96 System with the MagNA Pure 96 DNA and Viral NA Small Volume Kit. Prior to extraction, mix 350 µl of S.T.A.R. buffer with approximately 1 µl of each fecal sample using a sterile loop. Incubate for 5 minutes at room temperature and centrifuge at 2000 rpm for 2 minutes. Transfer 250 µl of supernatant to a fresh tube and combine with 50 µl of an internal extraction control before loading onto the automated system [84].
- In-house RT-PCR Amplification: Prepare a reaction mixture containing 5 µl of extracted DNA, 12.5 µl of 2× TaqMan Fast Universal PCR Master Mix, 2.5 µl of primers and probe mix, and sterile water to a final volume of 25 µl. Perform multiplex tandem PCR using a standard thermocycler program [84].
- Commercial PCR Testing: Process extracted DNA alongside the in-house assay using a commercial RT-PCR kit, such as the AusDiagnostics test, strictly following the manufacturer's instructions [84].
- Data Analysis: Compare results from all three methods (microscopy, in-house PCR, commercial PCR). Calculate percent agreement, sensitivity, and specificity for each target parasite, using a composite reference standard or latent class analysis to account for the lack of a perfect gold standard [84].
Protocol 2: Systematic Review and Meta-Analysis of Prevalence and Risk Factors
This protocol is based on a 2025 study protocol for a systematic review in Malaysia [3].
- Eligibility Criteria: Define inclusion criteria: studies involving human patients, using validated diagnostic methods (microscopy, molecular techniques, or immunoassays), and reporting data on infections caused by E. histolytica, G. lamblia, and/or C. parvum. Exclude case reports, reviews, and studies without original data [3].
- Information Sources and Search Strategy: Conduct comprehensive searches in electronic databases such as PubMed/MEDLINE, Scopus, ProQuest, Web of Science, and Google Scholar. Use a combination of Medical Subject Headings (MeSH) and free-text terms for the three search components: intestinal protozoal infection, prevalence, and risk factors/detection methods. There should be no language restrictions, and the reference lists of identified papers should be manually searched [3].
- Study Selection and Data Extraction: Follow the PRISMA guidelines. Use a two-stage screening process: first based on titles and abstracts, then on full-text assessment. Use a standardized, piloted data extraction form to record study characteristics (author, year, location), participant details, diagnostic methods used, and outcome data (prevalence figures, odds ratios for risk factors) [3].
- Risk of Bias Assessment: Assess the quality of included studies using appropriate tools, such as the Joanna Briggs Institute tools or the Newcastle-Ottawa Scale [3].
- Data Synthesis and Analysis: Perform a meta-analysis using a random-effects model to estimate pooled prevalence with 95% confidence intervals. Conduct subgroup analyses based on geographic region, diagnostic method, and target population to explore heterogeneity. Use the I² statistic to quantify statistical heterogeneity. Use meta-regression to investigate specific sources of heterogeneity. Assess publication bias using funnel plots and statistical tests like Egger's test [3].
Workflow Visualization
The following diagram illustrates the integrated diagnostic and research pathway for intestinal protozoan infections, synthesizing the methodologies discussed in this guide.
Integrated Diagnostic Pathway for IPI Research
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for conducting research on the diagnosis of intestinal protozoa.
Table 3: Essential Research Reagents for Diagnostic Studies of Intestinal Protozoa
| Reagent/Material | Specific Example | Research Function | Key Considerations |
|---|---|---|---|
| Stool Transport & Preservation Media | S.T.A.R. Buffer (Roche), Para-Pak Media [84] | Preserves nucleic acids for molecular studies; maintains parasite morphology for microscopy. | Choice affects DNA yield; preserved samples often give better PCR results than fresh [84]. |
| Nucleic Acid Extraction Kit | MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche) [84] | Automated, high-throughput nucleic acid purification. | Critical for breaking down robust parasite walls; includes internal extraction controls [84]. |
| PCR Master Mix | TaqMan Fast Universal PCR Master Mix (Thermo Fisher) [84] | Provides enzymes, dNTPs, and optimized buffer for qPCR amplification. | Enables sensitive multiplex tandem PCR detection [84]. |
| Primers & Probe Mix | In-house designed or commercial sets [84] | Target-specific sequences for pathogen identification. | Design is critical for specificity; must differentiate pathogenic/non-pathogenic species [36]. |
| Commercial Multiplex PCR Panel | AusDiagnostics GI pathogen panel [84] [85] | Simultaneously detects a broad panel of pathogens from one sample. | Ideal for syndromic testing; can identify co-infections missed by targeted tests [85]. |
| Staining Reagents | Giemsa stain, Modified Acid-Fast stain [84] [36] | Enhances microscopic visibility of parasites and their structures. | Sensitivity is variable (e.g., ~55% for Cryptosporidium with acid-fast) [36]. |
| Immunoassay Kits | EIA/ELISA kits for antigen detection [36] | Detects parasite-specific antigens in stool samples. | Useful for rapid screening; sensitivity 80-94% vs. PCR for E. histolytica [36]. |
| Concentration Reagents | Formalin-Ethyl Acetate (FEA) [84] | Concentrates parasites from a larger stool volume into a sediment. | Increases the sensitivity of microscopic examination [84]. |
Evaluating the Impact of Public Health Interventions Across Different Settings
Intestinal protozoan infections (IPIs) remain a major global public health concern, particularly in low- and middle-income countries where sanitation and hygiene are inadequate. It is estimated that nearly 3.5 billion people are affected by intestinal protozoal infections worldwide, with approximately 450 million individuals currently experiencing active infections [3]. Parasites such as Giardia lamblia, Entamoeba histolytica, and Cryptosporidium parvum contribute substantially to the global disease burden, causing symptoms including watery diarrhea, abdominal pain, fever, and in severe cases, malnutrition and impaired cognitive development [3] [86].
The transmission of these protozoa occurs primarily via the fecal-oral route through various modes including human-to-human contact, zoonotic transmission, and waterborne or foodborne spread [3]. Schoolchildren and under-five children are among the most vulnerable groups, with recent studies revealing alarmingly high prevalence rates. A 2023 study in Jalalabad, Afghanistan, found a 48.8% prevalence of intestinal parasitic infections among schoolchildren, with Giardia lamblia (35.8%) and Entamoeba histolytica (34.3%) being the most frequently detected protozoa [87]. Similarly, a 2023 study in the Borena district of central Ethiopia found that 31.1% of under-five children with diarrhea were infected with intestinal protozoans, primarily G. lamblia (18.7%) and E. histolytica (14.2%) [86].
The substantial burden of these infections, coupled with their disproportionate impact on vulnerable populations in resource-limited settings, underscores the critical need for effective public health interventions. This technical guide provides researchers, scientists, and drug development professionals with a comprehensive framework for evaluating the impact of interventions targeting intestinal protozoan infections across diverse settings.
Methodological Framework for Intervention Evaluation
Core Evaluation Disciplines and Definitions
Evaluating public health interventions encompasses several overlapping disciplines with nuanced distinctions. Understanding these frameworks is essential for designing appropriate evaluation strategies [88].
Table 1: Disciplines in Public Health Intervention Evaluation
| Discipline | Definition | Type of Knowledge | Primary Focus |
|---|---|---|---|
| Implementation Science | Assesses the extent to which efficacious health interventions can be effectively integrated within real-world public health and clinical service systems [88]. | Widely applicable | Integration of evidence-based interventions into service systems |
| Impact Evaluation | Assesses the efficacy and effectiveness of an intervention in terms of intended and unintended health, social, and economic outcomes; involves the explicit statement of a counterfactual [88]. | Widely applicable | Causal effects of interventions under ideal or real-world conditions |
| Program Evaluation | Assesses the processes and outcomes of a program with the intent of furthering its improvement [88]. | Program-specific | Program improvement and decision-making for specific implementations |
| Comparative Effectiveness Research | Assesses which treatment works best for whom, and under what circumstances, and considers health as well as economic outcomes [88]. | Widely applicable, clinical focus | Comparison of alternative treatments or interventions |
Evaluation Study Designs
Robust evaluation methodologies are essential for generating credible evidence about intervention effectiveness. The choice of study design depends on the evaluation questions, resources, and context.
Current Epidemiological Landscape and Risk Factors
Understanding the epidemiological context and modifiable risk factors is essential for designing targeted interventions and evaluating their potential impact.
Prevalence and Distribution of Intestinal Protozoan Infections
Recent studies across diverse geographical settings demonstrate varying prevalence rates of intestinal protozoan infections, reflecting differences in sanitation, hygiene, and socioeconomic conditions.
Table 2: Recent Prevalence Studies of Intestinal Protozoan Infections (2023-2025)
| Location | Study Population | Sample Size | Overall IPI Prevalence | G. lamblia | E. histolytica | Other Parasites | Reference |
|---|---|---|---|---|---|---|---|
| Jalalabad, Afghanistan | Schoolchildren (6-15 years) | 603 | 48.8% | 35.8% | 34.3% | H. nana (22.5%), A. lumbricoides (5.3%) [87] | [87] |
| Borena District, Ethiopia | Under-five children with diarrhea | 380 | 31.1% | 18.7% | 14.2% | E. vermicularis (0.8%), A. lumbricoides (0.5%) [86] | [86] |
| Malaysia (Systematic Review Protocol) | General population | Multiple studies | Pending (Analysis to conclude 2025) | Pending | Pending | C. parvum included in review [3] | [3] |
Modifiable Risk Factors for Intestinal Protozoan Infections
Identifying and addressing modifiable risk factors is crucial for developing effective interventions. Recent multivariate analyses have identified several significant factors associated with intestinal protozoan infections.
Table 3: Adjusted Odds Ratios for Significant Risk Factors for IPIs
| Risk Factor Category | Specific Factor | Population | Adjusted Odds Ratio (AOR) | 95% Confidence Interval | Reference |
|---|---|---|---|---|---|
| Hygiene Practices | Poor handwashing before eating | Schoolchildren, Afghanistan | 6.65 | 3.89–11.37 | [87] |
| Poor handwashing after toilet use | Schoolchildren, Afghanistan | 5.37 | 2.34–12.31 | [87] | |
| Hand washing with water alone (vs. soap/ash) | Under-five children, Ethiopia | 3.05 | 1.20–7.75 | [86] | |
| Never washing hands upon returning home | Schoolchildren, Afghanistan | 4.52 | 2.66–7.67 | [87] | |
| Environmental Sanitation | Absence of functional toilet in household | Under-five children, Ethiopia | 1.95 | 1.20–3.19 | [86] |
| Consumption of unwashed raw vegetables/fruits | Schoolchildren, Afghanistan | 28.83 | 5.50–151.03 | [87] | |
| Socioeconomic Factors | Maternal illiteracy | Under-five children, Ethiopia | 2.80 | 1.67–4.71 | [86] |
| Older age (13-15 years) | Schoolchildren, Afghanistan | 3.22 | 1.70–6.10 | [87] | |
| Behavioral Factors | Frequent contact with domestic animals | Under-five children, Ethiopia | 2.10 | 1.24–3.57 | [86] |
| Frequent street food consumption | Schoolchildren, Afghanistan | 2.45 | 1.30–4.58 | [87] | |
| Personal Hygiene | Poor nail hygiene | Schoolchildren, Afghanistan | 5.11 | 2.16–12.11 | [87] |
Experimental Protocols and Diagnostic Methodologies
Standardized Laboratory Protocols for IPI Detection
Accurate parasitological diagnosis is essential for both surveillance and evaluation of interventions. The following protocol summarizes standardized methodologies used in recent high-quality studies.
Stool Sample Collection and Processing
Sample Collection: Study participants are provided with clean, dry, wide-mouthed leak-proof containers. For children, special pediatric collection containers with spoons may be used. Instructions should emphasize avoiding contamination with water or urine [87] [86].
Transport and Storage: Samples should be transported to the laboratory within 2 hours of collection if possible. When delays are anticipated, samples should be refrigerated at 4°C or preserved in 10% formalin or sodium acetate-acetic acid-formalin (SAF) for longer preservation [87].
Macroscopic Examination: Upon receipt, samples are examined for consistency (formed, soft, watery), color, and the presence of blood or mucus, which should be documented [86].
Microscopic Examination Techniques
Direct Wet Mount Preparation:
- Emulsify a small portion of stool (approximately 2 mg) in a drop of physiological saline (0.85% NaCl) on a microscope slide
- Prepare a second preparation in a drop of Lugol's iodine solution
- Apply coverslips (22 × 22 mm) to both preparations
- Examine systematically under microscope at 10× and 40× objectives
- Scan entire coverslip area, documenting all parasitic elements observed [86]
Formalin-Ether Concentration Technique (Richie's Method):
- Emulsify 1 g of stool in 10 mL of 10% formalin in a centrifuge tube
- Strain through double-layered gauze or a sieve into a clean tube
- Add 3 mL of ethyl acetate, stopper the tube, and shake vigorously for 30 seconds
- Centrifuge at 500 × g for 2 minutes
- Loosen the fatty debris plug from the side of the tube and decant the supernatant
- Examine the sediment after resuspending in a small amount of formalin or saline [87] [86]
Quality Control: A minimum of 10% of samples should be re-examined by a second experienced microscopist to ensure consistency and accuracy of results.
Molecular Detection Protocols
While microscopy remains the field standard, molecular methods offer enhanced sensitivity and specificity for evaluation studies requiring precise speciation and quantification.
DNA Extraction Protocol:
- Use commercial stool DNA extraction kits following manufacturer's instructions
- Include appropriate positive and negative controls in each extraction batch
- Quantify DNA concentration using spectrophotometry or fluorometry
- Store extracted DNA at -20°C until analysis [3]
Multiplex PCR Protocol:
- Design species-specific primers for target protozoa (G. lamblia, E. histolytica, C. parvum)
- Optimize reaction conditions to ensure specific amplification
- Include appropriate controls in each run (positive, negative, inhibition)
- Analyze amplification products using gel electrophoresis or real-time detection systems [3]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Research Reagent Solutions for IPI Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Sample Collection & Transport | Clean, dry, wide-mouthed containers; 10% formalin; SAF fixative | Maintain sample integrity during transport | Formalized samples are suitable for concentration techniques but not for wet mounts [86] |
| Microscopy Reagents | Physiological saline (0.85% NaCl); Lugol's iodine solution; Methanol; Giemsa stain | Enable morphological identification of parasites | Iodine staining helps visualize nuclear details of cysts; permanent staining aids in species differentiation [87] |
| Concentration Reagents | 10% formalin; Ethyl acetate; Ether; Triton X-100 | Increase detection sensitivity by concentrating parasitic elements | Formalin-ether concentration is considered the gold standard for intestinal parasite concentration [87] |
| Molecular Biology Kits | Commercial stool DNA extraction kits; PCR master mixes; Species-specific primers and probes; Agarose | Enable sensitive and specific detection and differentiation of protozoan species | Multiplex PCR allows simultaneous detection of multiple pathogens in a single reaction [3] |
| Quality Control Materials | Known positive control samples; Negative control samples; External quality assessment panels | Ensure accuracy and reliability of laboratory results | Participation in external quality assurance programs is essential for maintaining laboratory competency [86] |
Implementation and Evaluation Framework
Intervention Strategies and Their Evaluation Metrics
Effective interventions targeting intestinal protozoan infections employ multi-faceted approaches. The logical framework below illustrates the pathway from interventions to intended outcomes and appropriate evaluation metrics.
Data Presentation and Statistical Analysis
Guidelines for Effective Table Design in Intervention Studies
Proper data presentation is crucial for transparent reporting of intervention effects. Table 1 in scientific papers should be designed to illuminate potential threats to internal and external validity [89].
Key Considerations for Table 1 Design:
- Columns: Include stratification by exposure status (for cohort studies) or disease status (for case-control studies) to allow assessment of potential confounding
- Rows: Include all key study variables, potential confounders, and selection variables to inform about residual confounding or selection bias
- Cells: Present descriptive statistics appropriate to variable type (n (%) for categorical variables; mean (SD) or median (IQR) for continuous variables) [89]
Avoid reliance on p-values for assessing confounding, as statistical significance does not necessarily indicate meaningful differences or confounding. Instead, focus on the magnitude of differences and their potential clinical or public health relevance [89].
Statistical Analysis Plan for Intervention Studies
A pre-specified statistical analysis plan should include:
- Primary Analysis: Intention-to-treat analysis comparing primary outcomes between intervention and control groups
- Effect Measures: Calculation of prevalence ratios, incidence rate ratios, or odds ratios with 95% confidence intervals
- Multivariable Analysis: Adjustment for pre-specified potential confounders identified in the causal framework
- Subgroup Analyses: Assessment of intervention effects across different population subgroups (e.g., age, gender, socioeconomic status)
- Process Evaluation: Assessment of intervention fidelity, reach, and implementation barriers
The evaluation of public health interventions for intestinal protozoan infections requires methodologically rigorous approaches that account for complex transmission dynamics and diverse socioeconomic contexts. The high prevalence rates observed across recent studies in Afghanistan [87] and Ethiopia [86], coupled with identified modifiable risk factors, highlight both the urgent need for effective interventions and the potential for substantial public health impact.
Successful intervention evaluation depends on appropriate study designs, accurate diagnostic methods, and comprehensive analytical approaches that consider both efficacy and implementation factors. As the field advances, integration of molecular diagnostics, geospatial analysis, and implementation science frameworks will enhance our ability to develop and evaluate interventions that are not only effective but also feasible, scalable, and sustainable across diverse settings.
Future directions should include more robust cost-effectiveness analyses, assessment of combination interventions addressing multiple transmission pathways simultaneously, and tailored approaches for specific high-risk populations. Through rigorous evaluation methodologies, researchers and public health professionals can generate the evidence needed to optimize interventions and reduce the substantial global burden of intestinal protozoan infections.
Evaluating the comparative efficacy of antiparasitic drugs is a cornerstone of epidemiological research and clinical management for intestinal protozoan infections. This process relies on a multifaceted approach, integrating data from controlled clinical trials, real-world treatment outcomes, and advanced experimental models. For researchers and drug development professionals, understanding the methodologies for collecting and analyzing this data is paramount for developing effective public health interventions and guiding therapeutic choices. This guide provides a technical framework for this critical analysis, detailing core experimental protocols, data quantification methods, and the essential toolkit required for robust drug efficacy research.
A primary challenge in this field is the varied landscape of evidence. A 2025 meta-epidemiological study found no systematic difference in effect sizes between single-arm interventional trials and single-arm observational cohort studies, but noted that both designs exhibit high levels of between-study heterogeneity (median I²: 54.8 for trials, 77.2 for cohorts) [90]. This highlights the inherent variability in study outcomes and the necessity of rigorous, standardized protocols to generate reliable, comparable data on drug performance.
Quantitative Efficacy Data from Clinical and Preclinical Studies
The comparative efficacy of therapeutic interventions is ultimately quantified through key performance indicators such as cure rates, parasite reduction, and safety profiles. The following tables summarize quantitative findings from recent clinical and preclinical studies.
Table 1: Clinical Treatment Outcomes for Parasitic Infections
| Infection / Patient Group | Therapeutic Regimen | Outcome Measure | Efficacy Result | Study Details |
|---|---|---|---|---|
| Visceral Leishmaniasis (Pediatric, Ethiopia) [91] | SSG & PM (First-line) | Clinical Cure Rate | 77.5% | Retrospective cohort (n=200); Poor outcomes: 22.5% (partial response, death, relapse) |
| Intestinal Protozoa (Disabled Patients, Türkiye) [16] | Not Specified | Infection Prevalence | 41% | Case-control (n=200 patients); Control group prevalence: 9% (p=0.001) |
| Spina Bifida Subgroup [16] | Not Specified | Infection Prevalence | 83.3% | Subgroup analysis; Highest risk category |
Table 2: Preclinical Efficacy of a Novel Nano-formulation Against Trichinellosis [92]
| Treatment Group | Efficacy: Intestinal Phase | Efficacy: Muscular Phase | Key Findings |
|---|---|---|---|
| NTZ-loaded ZnO NPs | >97% | >97% | Highest efficacy; profound amelioration of biomarkers |
| Nitazoxanide (NTZ) alone | Not Specified | Lower comparable efficiency | Safe profile but lower efficacy |
| Gold Standard (Albendazole) | Not Specified | Low effectiveness on larval stage | Poor bioavailability, bone marrow suppression |
Experimental Protocols for Efficacy Evaluation
A critical component of generating reliable efficacy data is the implementation of standardized, detailed experimental protocols. The methodologies below are adapted from recent high-impact studies.
Protocol 1: Clinical Cohort Study for Treatment Outcomes
This protocol is designed for evaluating drug efficacy in a hospital or clinical setting, based on a study of visceral leishmaniasis in pediatric patients [91].
- Study Design: A retrospective cohort study analyzes existing patient records to determine treatment outcomes.
- Population and Setting: The study focuses on pediatric patients (≤15 years) admitted to a specialized hospital ward. For the referenced study, 222 admissions were reviewed, with 200 complete records meeting the inclusion criteria [91].
- Data Collection: Researchers extract data on patient demographics, clinical presentations, specific treatment regimens administered, and treatment outcomes from medical records.
- Operational Definitions: Outcomes must be clearly defined. For example:
- Clinical Cure: Absence of clinical features of infection after a full treatment course, confirmed by clinical assessment and/or negative parasitological tests [91].
- Poor Treatment Outcome: An aggregate of partial response, death, or relapse.
- Statistical Analysis: Data are analyzed using statistical software (e.g., SPSS). Logistic regression is used to identify factors (e.g., age, immunocompetence, adherence to guidelines) independently associated with treatment outcomes, with a statistical significance threshold of p < 0.05 [91].
Protocol 2: Preclinical Trial of a Novel Nano-formulation
This protocol describes the in vivo evaluation of a new drug formulation, as demonstrated in a murine model of trichinellosis [92].
- Animal Model and Infection: Laboratory mice (e.g., Swiss Albino) are orally infected with a specific dose of parasites (e.g., 250 T. spiralis larvae).
- Treatment Groups: Mice are randomly assigned to groups receiving different interventions:
- The experimental formulation (e.g., NTZ-loaded ZnO NPs)
- The standard drug (e.g., Albendazole)
- The active drug alone (e.g., Nitazoxanide)
- The nanoparticle carrier alone (e.g., blank ZnO NPs)
- A control (e.g., placebo)
- Parasitological Assessment: This is the primary efficacy measure. The number of adult worms in the intestine and the number of encapsulated larvae in muscle tissues are counted after treatment to calculate drug efficacy for each phase of the life cycle [92].
- Supplementary Assessments: To provide a comprehensive efficacy and safety profile:
- Biochemical: Measure markers of tissue damage and oxidative stress (e.g., creatine kinase, malondialdehyde).
- Immunological: Quantify cytokine levels (e.g., interleukins) to assess immune response modulation.
- Histopathological: Examine tissue sections for structural damage and inflammation restoration [92].
Workflow Diagram: Experimental Protocol for Preclinical Drug Efficacy
The following diagram visualizes the key stages of the preclinical trial protocol for evaluating a novel anti-parasitic formulation.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of the experimental protocols requires a suite of reliable research reagents and materials. The following table details essential items and their functions in antiparasitic drug efficacy research.
Table 3: Essential Research Reagents and Materials for Antiparasitic Drug Evaluation
| Reagent / Material | Primary Function in Research | Example Application / Note |
|---|---|---|
| Nitazoxanide-loaded ZnO NPs | Novel nano-formulation to enhance drug solubility, tissue penetration, and efficacy. | Used to treat murine trichinellosis; showed >97% efficacy in both intestinal and muscular phases [92]. |
| Transmission Electron Microscopy (TEM) | Characterizes the size, shape, and morphology of nano-formulations. | Confirmed uniform spherical/hexagonal shapes of ZnO NPs (30-80 nm) [92]. |
| Fourier Transform Infrared (FTIR) Spectroscopy | Verifies chemical composition and successful drug loading in nano-formulations. | Identified characteristic functional groups and metal-oxygen bonds in NPs [92]. |
| Liposomal Amphotericin B (L-Amb) | First-line drug for visceral leishmaniasis; targets the parasite's cell membrane. | Preferred for immunocompromised patients; use limited by cost and need for inpatient care [91]. |
| Sodium Stibogluconate (SSG) & Paromomycin (PM) | Combination therapy used as first-line treatment for VL in East Africa. | Explored to improve efficacy and reduce drug resistance [91]. |
| Modified Acid-Fast Staining Kits | Specific staining for detecting oocysts of Cryptosporidium spp. and Cyclospora cayetanensis in stool samples. | Critical for accurate diagnosis in epidemiological studies [16]. |
| rK39 Immunochromatographic Test | Rapid diagnostic test for detecting antibodies against Leishmania infection. | Used for serological confirmation of visceral leishmaniasis [91]. |
| ELISA Kits for Cytokines (e.g., IL-2, IL-4) | Quantifies levels of specific cytokines to assess the host's immune response modulation by the drug. | Revealed profound amelioration of immunological markers in treated mice [92]. |
| Biochemical Assay Kits (CK, ALT, AST, MDA, NO) | Measures markers of tissue damage (e.g., muscle, liver) and oxidative stress. | Assessed drug safety and restorative effects in preclinical models [92]. |
Mechanistic Insights and Workflow Visualization
Understanding how a drug works at a molecular level is crucial for explaining its efficacy and for the rational development of next-generation therapeutics.
Mechanism of Fexinidazole Against Trypanosomes
A 2025 study on fexinidazole, the first oral monotherapy for Human African Trypanosomiasis, provided the first comprehensive analysis of its mechanism of action [93]. The research demonstrated that the drug's trypanocidal activity is primarily due to the induction of DNA damage within the parasite. The treatment causes an accumulation of DNA lesions and significantly inhibits DNA synthesis, ultimately leading to parasite death. The study also highlighted the relationship between nitroaromatic drug treatments, DNA damage formation, and the activation of reactive oxygen species (ROS), a process essential for parasitic cell proliferation [93].
Workflow Diagram: Drug Mechanism of Action Analysis
The following diagram outlines the key investigative process for elucidating a drug's mechanism of action, based on the fexinidazole study.
The comparative analysis of antiparasitic drug efficacy is a complex but essential discipline, powered by integrating data from well-designed clinical studies, controlled preclinical models, and deep mechanistic investigations. The presented frameworks for quantitative assessment, experimental protocols, and essential research tools provide a foundation for robust research. Future advances will depend on overcoming challenges such as high heterogeneity in single-arm studies, the spread of drug resistance, and the limited efficacy of existing drugs against all life stages of parasites. The integration of novel approaches, such as nano-formulations to improve drug delivery and genetic tools to unravel resistance mechanisms, will be critical in developing the next generation of antiparasitic therapies.
Within epidemiological research on intestinal protozoan infections, quantifying the economic and health burden is fundamental for guiding public health policy, securing research funding, and prioritizing drug development initiatives. The Disability-Adjusted Life Year (DALY) has emerged as a dominant metric for measuring the overall burden of disease, combining both fatal and non-fatal health losses into a single, comparable figure [94]. One DALY represents the loss of the equivalent of one year of full health [95]. For protozoal intestinal diseases, which are a significant global health concern causing an estimated 450 million illnesses annually, accurately validating the Cost of Illness (COI) and DALYs is a critical skill for researchers and health economists [4] [96]. These metrics move beyond simple incidence or mortality rates to capture the full impact of conditions like giardiasis, cryptosporidiosis, and amoebiasis, which are often marked by debilitating acute symptoms and long-term sequelae such as growth faltering in children and post-infectious functional gastrointestinal disorders [97] [4]. This guide provides a technical framework for the calculation, application, and validation of these essential metrics within the specific context of intestinal protozoan infections.
Conceptual Foundations and Calculation of DALYs
Core Components of the DALY Metric
The DALY is a societal measure of disease burden, calculated by summing two core components: the Years of Life Lost (YLL) due to premature mortality and the Years Lived with Disability (YLD) [94]. The formula is expressed as:
DALY = YLL + YLD
This composite metric provides a more complete picture of a disease's impact than mortality data alone, as it accounts for both the loss of life and the reduction in quality of life due to illness or disability.
- Years of Life Lost (YLL): This component quantifies the burden of premature death by calculating the difference between the actual age at death and a standard life expectancy for that age. It is calculated as YLL = N × L, where
Nis the number of deaths, andLis the standard life expectancy at the age of death [98] [94]. For intestinal protozoan infections, which can be fatal in vulnerable populations such as children, the elderly, and the immunocompromised, YLL constitutes a significant portion of the total burden [97]. - Years Lived with Disability (YLD): This component quantifies the burden of living with a disease or its consequences. It incorporates the incidence of the condition, its average duration, and a disability weight (DW) that reflects the severity of the health loss. The calculation is YLD = I × DW × L, where
Iis the number of incident cases,DWis the disability weight, andLis the average duration of the case until remission or death [98] [94].
Disability Weights and Their Critical Role
The disability weight (DW) is a value between 0 (representing perfect health) and 1 (representing a health state equivalent to death) that reflects the severity of a specific disease or disability state [94]. These weights are central to the YLD calculation and are typically derived from large-scale population surveys or expert opinion, though the methodology has been a subject of debate [98]. For intestinal protozoan infections, the disability weight captures the pain, discomfort, functional impairment, and social stigma associated with acute and chronic symptoms like severe diarrhea, abdominal pain, and malnutrition. The specific DW assigned to a condition like "infectious diarrhea" or "moderate abdominal pain" is applied to all incident cases in the population for the duration of the illness to estimate the total non-fatal burden.
Table: Disability Weight Examples for Conditions Relevant to Intestinal Protozoa
| Health State | Disability Weight (DW) 2004 | Disability Weight (DW) 2010 | Notes |
|---|---|---|---|
| Diarrheal diseases | Varies by severity | Varies by severity | Weights are typically stratified as mild, moderate, or severe. |
| Moderate abdominal pain | Information missing | Information missing | Often a co-morbidity in burden calculations for enteric infections. |
| Lower back pain | 0.061 | 0.032-0.037 | Provided as a reference for a non-fatal, chronic condition. |
| Amputation of finger | 0.102 | 0.030 | Provided as a reference for a permanent, non-fatal disability. |
Methodologies for Calculating and Validating DALYs
Data Sourcing and Integration
Robust DALY estimation requires integrating data from multiple sources to ensure accuracy and comprehensiveness.
- Incidence and Prevalence Data: Utilize high-quality, population-based surveillance systems, cohort studies, and systematic reviews to obtain reliable estimates of the number of new and existing cases of specific intestinal protozoan infections. For example, a meta-analysis in Malaysia found an overall pooled prevalence of intestinal protozoal infections of 24%, with Entamoeba spp. (18%) and Giardia lamblia (11%) being most common [4].
- Mortality Data: Source data from national vital registration systems, verbal autopsies, and cause-of-death models from the Global Burden of Disease (GBD) study. It is crucial to correctly attribute deaths to the underlying cause, such as diarrhea or its complications, caused by a specific protozoan pathogen [97].
- Disability Weights: Use the most recent and context-appropriate disability weights published by the GBD study. Researchers must map the specific health states associated with the intestinal protozoan infection (e.g., acute watery diarrhea, persistent diarrhea) to the standardized weights provided by the GBD collaborators [94].
- Duration of Illness: Derive estimates for the average duration of illness (
Lin the YLD formula) from clinical cohort studies, treatment trials, and longitudinal surveys. For chronic or recurrent infections, this parameter must account for the long-term nature of the disease.
Analytical Protocols and Computational Steps
The following protocol outlines the key steps for calculating the burden of a specific intestinal protozoan infection, such as giardiasis, in a defined population.
Step 1: Define the Population and Timeframe Clearly specify the population of interest (e.g., a national population, children under 5, a specific region) and the time period for the analysis (e.g., the calendar year 2021).
Step 2: Calculate Years of Life Lost (YLL)
- Obtain the number of deaths (
N) attributed to the specific protozoan infection in the target population and timeframe. - For each death, determine the standard life expectancy (
L) at the age of death, using a reference life table (e.g., from the GBD study). - Sum the years of life lost across all deaths to obtain the total YLL. YLL = Σ (N × L)
Step 3: Calculate Years Lived with Disability (YLD)
- Obtain the number of new incident cases (
I) of the infection in the target population and timeframe. - Identify the appropriate disability weight (
DW) for the health state associated with the infection (e.g., "moderate-to-severe infectious diarrhea"). - Determine the average duration of the illness (
L) in years. For an acute episode of giardiasis lasting 15 days, the duration would be 15/365 = ~0.041 years. - Calculate the total YLD. YLD = I × DW × L
Step 4: Calculate Total DALYs Sum the YLL and YLD to obtain the total disease burden in DALYs for the population. DALYs = YLL + YLD
Step 5: Disaggregate and Validate Results Disaggregate DALY estimates by age and sex to identify vulnerable sub-populations, a common practice in burden of disease studies [97]. Validate results by comparing them with previous estimates, checking for internal consistency, and conducting uncertainty analyses around key input parameters (e.g., incidence, mortality, DW).
Table: Global Burden of Enteric Infections (1990-2021) - A Model for Protozoan Burden Context
| Metric | 1990 (Age-Standardized Rate per 100,000) | 2021 (Age-Standardized Rate per 100,000) | Rate Change (1990-2021) |
|---|---|---|---|
| Prevalence | 1043.56 | 879.58 | -0.18 |
| Incidence | 65466.27 | 57721.08 | -0.12 |
| Deaths | 60.58 | 17.83 | -0.73 |
| DALYs | 3337.13 | 1020.15 | -0.72 |
This table, adapted from GBD 2021 data on all enteric infections, shows the general trend of decreasing burden, against which disease-specific protozoan burdens can be compared [97].
Conducting robust burden of disease studies requires a suite of methodological tools and data resources.
Table: Key Research Reagent Solutions for DALY Estimation
| Reagent/Resource | Function in Burden of Disease Research | Example/Specification |
|---|---|---|
| GBD Results Tool | Primary data source for extracting pre-calculated DALYs, YLLs, YLDs, and associated uncertainty intervals for a vast array of diseases and injuries, including enteric infections. | Institute for Health Metrics and Evaluation (IHME) [97] |
| Disability Weight (DW) Catalog | Provides the essential severity weights for specific health states required for the YLD calculation. | GBD Study Disability Weights Library |
| Socio-demographic Index (SDI) | A composite indicator of development status used to analyze how disease burden correlates with income per capita, educational attainment, and fertility. | GBD Socio-demographic Index [97] |
| Statistical Analysis Software | Used for data management, decomposition analysis, modeling, and visualization of burden estimates. | R (with ggplot2 package), Python, Stata [97] |
| Uncertainty Analysis Framework | A methodological tool to quantify and propagate the uncertainty inherent in input data (e.g., incidence, mortality) through to the final DALY estimate. | Bayesian statistical models, Monte Carlo simulation |
Critical Analysis and Limitations of the DALY Framework
While DALYs are a powerful tool, researchers must be aware of their methodological limitations and controversies to critically evaluate and validate burden estimates.
- Methodological Concerns and Arbitrary Assumptions: Critics have noted that the conceptual and technical basis for DALYs can be flawed, with assumptions and value judgments that are "open to serious question" [98]. The construction of the YLD formula is theoretically grounded in the Time Trade-Off (TTO) technique, which lacks a rigorous mathematical or economic theory foundation, leading some to view it as arbitrarily defined [98].
- Inconsistency and Non-Reproducibility: The DALY synthetic indicator has been associated with inconsistent and non-reproducible results, which can lead to flawed public health rankings and decision-making [98]. The disability weights, in particular, have been a source of inconsistency, as they may be derived from the preferences of "independent experts" rather than from direct surveys of patients actually living with the condition [98].
- Neglect of Socioeconomic Context: Standard DALY calculations may not fully capture how socioeconomic status (SES) modulates disease burden. A scoping review in the MENA region found that low income was associated with higher rates of parasitic infections, and the relationship between education level and infection was complex and divergent across studies [14]. This suggests that a simple DALY estimate may mask significant health inequities.
Application to Intestinal Protozoan Infections and Future Directions
Applying the DALY framework to intestinal protozoan infections reveals a significant global health burden, disproportionately affecting vulnerable populations. Research indicates that regions with low socioeconomic status and poor WASH (Water, Sanitation, and Hygiene) infrastructure bear the highest burden [14] [99]. For instance, a meta-analysis in Malaysia identified that the highest prevalence of intestinal protozoal infections was associated with factors like low income, no formal education, and exposure to untreated water [4]. From a global perspective, enteric infections at large remain a leading cause of health loss, particularly in low and low-middle SDI regions [97].
Future research and validation efforts should focus on:
- Refining Disability Weights: Developing more nuanced weights that capture the full spectrum of illness for protozoan infections, including post-infectious complications and cognitive impacts.
- Integrating a One Health Approach: As called for in research on protozoan pathogens in Kenya, future burden estimates should more fully incorporate data on environmental reservoirs and animal hosts to capture the complete transmission dynamics of zoonotic protozoa like Cryptosporidium and Giardia [99].
- Conducting Localized Burden Studies: Global estimates can mask local outbreaks and regional variations. There is a need for high-resolution, sub-national burden studies to inform targeted control programs, especially given the disparities identified in studies within the MENA region and Malaysia [14] [4].
- Linking Burden to Economic Cost: Beyond DALYs, comprehensive Cost of Illness studies that translate the DALY burden into monetary terms by factoring in direct medical costs and indirect productivity losses are essential for making a compelling economic argument for increased investment in drug development and public health interventions.
Conclusion
The epidemiology of intestinal protozoan infections reveals a significant and persistent global health challenge, disproportionately affecting vulnerable populations in resource-limited settings. Key takeaways include the confirmed high prevalence of these infections, the critical influence of socioeconomic and environmental risk factors, and the ongoing evolution of diagnostic technologies from microscopy to molecular tools. However, major hurdles remain, including the limitations of current chemotherapies and emerging drug resistance. Future efforts must be directed toward the discovery and development of novel anti-protozoal agents, the validation and widespread implementation of cost-effective, high-sensitivity diagnostic tools, and the strengthening of integrated public health measures that address the root causes of transmission. For biomedical and clinical research, this underscores the urgent need for translational studies that bridge epidemiological data with drug discovery and the development of evidence-based, localized control programs.
References
- 1. Perspectives on the Drug Discovery of Intestinal Protozoan ... [https://www.intechopen.com/chapters/1189194]
- 2. Editorial: Drug Development for Parasite-Induced Diarrheal ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.00577/full]
- 3. Epidemiological Characteristics of Intestinal Protozoal ... [https://www.researchprotocols.org/2025/1/e66350]
- 4. Prevalence and risk factors of intestinal protozoal infections ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425333/]
- 5. Global prevalence of intestinal protozoan contamination in ... [https://www.sciencedirect.com/science/article/pii/S0956713521007945]
- 6. Drug Development to Protozoan Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3103878/]
- 7. Prevalence of intestinal protozoan infections and ... [https://www.sciencedirect.com/science/article/pii/S221339842400246X]
- 8. Prevalence of Intestinal Protozoan Parasites and Associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8639259/]
- 9. Global prevalence and correlation of intestinal parasitic ... [https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-025-04144-y]
- 10. Tropical diseases and the gastrointestinal tract [https://www.frontiersin.org/journals/tropical-diseases/articles/10.3389/fitd.2025.1612952/full]
- 11. Comparative Analysis of Intestinal Parasitic Infections and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360875/]
- 12. The Landscape of Parasitic Infections in the United States [https://www.sciencedirect.com/science/article/pii/S0893395223001229]
- 13. Prevalence and risk factors of intestinal protozoal infections ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0332218]
- 14. a scoping review in the Middle East and North African region [https://pmc.ncbi.nlm.nih.gov/articles/PMC12414970/]
- 15. More Than Half Prevalence of Protozoan Parasitic Infections ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6954853/]
- 16. Frequency of Intestinal Protozoa in Patients Receiving ... [https://www.turkiyeparazitolderg.org/articles/frequency-of-intestinal-protozoa-in-patients-receiving-treatment-at-van-special-physioactive-special-education-and-rehabilitation-center/doi/tpd.galenos.2025.69875]
- 17. Prevalence and associated factors of intestinal parasitic ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11847-w]
- 18. Prevalence of feco-oral transmitted protozoan infections and ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-019-4095-z]
- 19. Prevalence and risk factors of intestinal parasitic infections ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150492/]
- 20. Prevalence of Intestinal Protozoa Infections and Associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5522686/]
- 21. Characteristics of Epidemiological ... Intestinal Protozoal Infections [https://www.researchprotocols.org/2025/1/e66350/]
- 22. Characteristics of Epidemiological ... Intestinal Protozoal Infections [https://pmc.ncbi.nlm.nih.gov/articles/PMC12008696/]
- 23. Infectious diseases in Indigenous populations in North America [https://pmc.ncbi.nlm.nih.gov/articles/PMC10156139/]
- 24. The burden of invasive infections in critically ill Indigenous ... [https://www.mja.com.au/journal/2017/206/2/burden-invasive-infections-critically-ill-indigenous-children-australia]
- 25. Practical Guidance for Clinical Microbiology Laboratories [https://pmc.ncbi.nlm.nih.gov/articles/PMC5740970/]
- 26. Waterborne protozoan outbreaks: An update on the global, ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969721056394]
- 27. Prevalence and infestation dynamics of intestinal protozoa ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533579/]
- 28. Transmission and Epidemiology of Zoonotic Protozoal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3553666/]
- 29. Characterizing the transmission dynamics of Trypanosoma ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06917-6]
- 30. Methods of Common Diagnostic : Current and... Intestinal Protozoa [https://pmc.ncbi.nlm.nih.gov/articles/PMC9606991/]
- 31. Parasitic diagnosis: A journey from basic microscopy to cutting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617590/]
- 32. Diseases Workup: Laboratory Studies, Imaging... Intestinal Protozoal [https://emedicine.medscape.com/article/999282-workup]
- 33. Microsporidiosis - Infectious Diseases - MSD Manual Professional... [https://www.msdmanuals.com/professional/infectious-diseases/intestinal-protozoa-and-microsporidia/microsporidiosis]
- 34. Performance validation of deep-learning-based approach in ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06878-w]
- 35. Detection of protozoan and helminth parasites in concentrated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607898/]
- 36. Diagnostic Methods of Common Intestinal Protozoa [https://www.mdpi.com/2414-6366/7/10/253]
- 37. Evaluation of Allplex™ GI-Parasite Assay—A Multiplex Real ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390207/]
- 38. Stool Specimens – Detection of Parasite Antigens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/antigendetection.html]
- 39. Rapid diagnostic tests relying on antigen detection from ... [https://www.sciencedirect.com/science/article/abs/pii/S0732889318302487]
- 40. Advancements in Immunology and Microbiology Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11357253/]
- 41. RDT performance through high-throughput bead-based ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1598280/full]
- 42. Molecular detection and genotyping of Giardia lamblia in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617593/]
- 43. Molecular detection of intestinal protozoa and ... [https://pubmed.ncbi.nlm.nih.gov/40848374/]
- 44. Prevalence and risk factors of intestinal protozoal infections ... [https://pubmed.ncbi.nlm.nih.gov/40934249/]
- 45. Visualization and Analytics Tools for Infectious Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5734643/]
- 46. Descriptive statistics and data visualization - Epidemiology [https://fiveable.me/epidemiology/unit-11/descriptive-statistics-data-visualization/study-guide/0Qv6LseuDSfCjboA]
- 47. Detection of Intestinal Protozoa in the Clinical Laboratory - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3957779/]
- 48. Implementation of real-time PCR assays for diagnosing ... [https://link.springer.com/article/10.1007/s00436-025-08483-3]
- 49. Principles of Epidemiology: Lesson 4, Section 4 [https://archive.cdc.gov/www_cdc_gov/csels/dsepd/ss1978/lesson4/section4.html]
- 50. The Role of Data in Public Health and Health Innovation [https://www.jmir.org/2025/1/e78794]
- 51. Quantitative Data Quality Assurance, Analysis and Presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056448/]
- 52. What are the 2025 Trends in Diagnostics? [https://www.hartmannyoung.com/resources/blog/what-are-the-2025-trends-in-diagnostics-/]
- 53. Comparative analysis of commercial and "In-House" molecular tests for... [https://pubmed.ncbi.nlm.nih.gov/40751255/]
- 54. Comparative analysis of commercial and “In-House” molecular tests for... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 55. Epidemiology and clinical features of intestinal protozoan ... [https://www.sciencedirect.com/science/article/abs/pii/S1477893921001484]
- 56. Enhancing infectious intestinal disease diagnosis through ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01478-w]
- 57. Immunological Methods of Common Intestinal Protozoa [https://encyclopedia.pub/entry/28740]
- 58. Prevalence of Nitroimidazole-Refractory Giardiasis ... [https://wwwnc.cdc.gov/eid/article/31/6/25-0076_article]
- 59. Entamoeba histolytica "mutator" strain with a high rate of ... [https://pubmed.ncbi.nlm.nih.gov/40503832/]
- 60. Global burden and trends of the Entamoeba infection ... [https://www.sciencedirect.com/science/article/pii/S0001706X23000530]
- 61. Epidemiology of clinically relevant Entamoeba spp. (E. ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8448324/]
- 62. First Description of Entamoeba moshkovskii in a Rural Area ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0140302]
- 63. Genotype-Specific Small EVs Released by Giardia lamblia ... [https://pubmed.ncbi.nlm.nih.gov/40888009/]
- 64. Cross-species protection suggests Entamoeba histolytica ... [https://pubmed.ncbi.nlm.nih.gov/40741974/]
- 65. Intestinal Parasitic Infections in 2023 - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10284646/]
- 66. Therapy of intestinal protozoa [https://www.sciencedirect.com/science/article/abs/pii/S1471492203002435]
- 67. Parasites and Microbiota: Dual Interactions ... [https://www.mdpi.com/2076-2607/12/10/2076]
- 68. Effects of Water, Sanitation, Handwashing, and Nutritional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6206106/]
- 69. Effect of sanitation and water treatment on intestinal ... [https://www.sciencedirect.com/science/article/abs/pii/S1473309915003497]
- 70. Water, sanitation, and hygiene access among people who ... [https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-024-02163-x]
- 71. Can water, sanitation and hygiene help eliminate stunting? [https://pmc.ncbi.nlm.nih.gov/articles/PMC5084825/]
- 72. Water, sanitation and hygiene insecurity predict abscess ... [https://www.sciencedirect.com/science/article/pii/S0955395924001701]
- 73. The impact of an integrated intervention program combining ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-024-06611-z]
- 74. Understanding the Effectiveness of Water, Sanitation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11661469/]
- 75. Intestinal protozoa infections and associated factors among ... [https://www.sciencedirect.com/science/article/pii/S2405673125000017]
- 76. Reprofiled drug targets ancient protozoans - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3555889/]
- 77. University of Houston Professor Awarded $3.9M To Fight ... [https://www.uh.edu/news-events/stories/2025/october/10072025-cuny-parasites-enzymes-nih.php]
- 78. Recent Advancements in the Development of Antiprotozoal ... [https://www.mdpi.com/journal/pharmaceuticals/special_issues/7C9W2XIDFR]
- 79. Novel drug candidates targeting Toxoplasma gondii in ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1673462/full]
- 80. An all-in-one pipeline for the in vitro discovery and in vivo ... [https://www.nature.com/articles/s41467-025-62014-3]
- 81. Heterogeneity in meta-analyses: an unavoidable challenge worth exploring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326561/]
- 82. A systematic review and meta-analysis of the prevalence of chronic widespread pain in the general population - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4711387/]
- 83. Meta-analysis of prevalence: I2 statistic and how to deal with heterogeneity - PubMed [https://pubmed.ncbi.nlm.nih.gov/35088937/]
- 84. Comparative analysis of commercial and “In-House ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317615/]
- 85. Aditum | 1309 | [https://aditum.org/journals/clinical-medical-case-reports-and-case-series/current-issue/1309]
- 86. Intestinal protozoa infections and associated factors among ... [https://pubmed.ncbi.nlm.nih.gov/40008242/]
- 87. Prevalence and associated factors of intestinal parasitic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551352/]
- 88. Evaluating Public Health Interventions: 1. Examples, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4695951/]
- 89. Who is in this study, anyway? Guidelines for a useful Table 1 [https://pmc.ncbi.nlm.nih.gov/articles/PMC6773463/]
- 90. Single‐arm interventional versus observational studies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11795979/]
- 91. Visceral leishmaniasis treatment outcome and associated ... [https://www.frontiersin.org/journals/tropical-diseases/articles/10.3389/fitd.2025.1566971/full]
- 92. Promising therapeutic efficacy of nitazoxanide-loaded zinc ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274003/]
- 93. Analysis of Newest Drug Against a Deadly Parasite Infection ... [https://news.stonybrook.edu/newsroom/press-release/medical/analysis-of-newest-drug-against-a-deadly-parasite-infection-may-help-advance-treatments/]
- 94. Disability-adjusted life year [https://en.wikipedia.org/wiki/Disability-adjusted_life_year]
- 95. Global health estimates: Leading causes of DALYs [https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/global-health-estimates-leading-causes-of-dalys]
- 96. Global impact of parasitic infections and the importance ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1546195/full]
- 97. Global burden, subtype, risk factors and etiological analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11965617/]
- 98. Unraveling the limitations of disability-adjusted life years ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11525889/]
- 99. Prevalence and Risk Factors of Waterborne ... [https://weekly.chinacdc.cn/en/article/doi/10.46234/ccdcw2025.014]