Standardizing Sample Collection and Storage: 2025 Best Practices for Research and Drug Development
This guide provides a comprehensive framework for standardizing sample collection and storage, critical for ensuring data integrity and reproducibility in biomedical research and drug development.
Standardizing Sample Collection and Storage: 2025 Best Practices for Research and Drug Development
Abstract
This guide provides a comprehensive framework for standardizing sample collection and storage, critical for ensuring data integrity and reproducibility in biomedical research and drug development. It covers foundational principles from global regulations and biobanking guidelines, details methodological workflows for handling diverse biological specimens, offers troubleshooting strategies for common pre-analytical errors, and outlines validation techniques for quality assurance. Aimed at researchers, scientists, and drug development professionals, this article synthesizes current best practices to enhance operational efficiency, facilitate cross-institutional collaboration, and uphold sample quality from collection to disposal.
The Pillars of Quality: Understanding Why Standardization is Non-Negotiable
FAQs on Data Quality in Research
Q1: What do the core data quality attributes mean in the context of sample management?
In sample management, quality attributes are specific, measurable standards that ensure the integrity and usability of research specimens and their associated data.
- Accuracy: The degree to which sample data (e.g., donor ID, collection time, volume) correctly describes the real-world specimen. An inaccurate patient identifier can link a test result to the wrong individual, compromising the entire study [1].
- Completeness: The extent to which all required data for a specimen is present. This includes mandatory fields in a database, such as patient consent status, sample type, and collection date. Incomplete data can render a sample useless for analysis [1] [2].
- Consistency: Ensures that sample information is non-conflicting when stored or used across different systems or time points. For example, a sample's collection date should be the same in the lab's database and the clinical record [1].
- Timeliness: Reflects how current and up-to-date the sample data is, and whether the data is available when needed. This also applies to the sample itself; for instance, a blood sample that is not processed and frozen within the required time window may degrade, making its data untimely [1] [3].
- Usability: The fitness of a sample and its data for its intended research purpose. This overarching attribute is achieved when all other quality dimensions are met, ensuring the specimen can be confidently used in analysis [4].
Q2: A sample's data seems correct, but the result from its analysis appears to be an outlier. How can I troubleshoot this?
Do not trust a single data point at face value [5]. We recommend a systematic investigation focusing on the sample's journey and data authenticity.
- 1. Verify Pre-Analytical Variables: Review the sample's chain of custody. A significant portion of errors occur during the pre-analytical phase [6]. Check:
- Collection Technique: Was the correct vacuum tube used? Was it inverted properly to mix with additives? Poor technique can cause hemolysis or microclots, altering results [3].
- Storage Conditions: Was the sample stored at the correct temperature before analysis? Deviations can degrade samples [2] [7].
- Sample Handling: Was the sample centrifuged at the correct speed and duration? Was there a delay in processing? [3]
- 2. Audit Data Authenticity and Consistency: Cross-reference the sample's data with other records.
- Compare the participant's data from this time point with their data from previous visits. Are the values consistent with their baseline? [5]
- Check for inconsistencies between what was documented (e.g., "sample collected") and the supporting evidence (e.g., exact collection time on the tube label matches the worksheet) [5].
- 3. Check for Confounding Factors: Consider the study design.
Q3: Our team frequently encounters "Quantity Not Sufficient" (QNS) errors and mislabeled tubes. What are the best practices to prevent these issues?
These common problems are often rooted in protocol deviations and can be minimized with strict procedures and checklists.
To Prevent QNS Errors:
- Know Volume Requirements: Always consult the test requirements and central lab manual prior to collection to know the minimum volume needed [3] [2].
- Use Proper Equipment: Ensure you are using the correct tube type that is designed to draw the required volume [3].
- Verify Fill Levels: Before processing, check that tubes have been filled to the appropriate level [3].
To Prevent Labelling Errors:
- The Two-Identifier Rule: Label all primary containers with at least two patient identifiers (e.g., full name and date of birth, or study ID number) at the time of collection [3] [6].
- Bedside Labeling: Label tubes immediately after drawing them, in the presence of the patient [6].
- Leverage Technology: Implement barcode wristbands and bedside barcode printing systems. One study showed this reduced specimen labeling errors by 62% [6].
- Pre-Prepare Labels: For studies with multiple patients, prepare labels in advance to reduce the risk of applying the wrong label under time pressure [2].
Troubleshooting Guide: Common Sample Collection Issues
| Problem | Potential Impact on Research | Corrective & Preventive Actions |
|---|---|---|
| Incorrect Collection Tube Used [2] | Invalid Results: Additives (e.g., anticoagulants) in the wrong tube can alter chemistry or invalidate tests. Sample Loss. | Corrective: Discard sample and recollect using proper tube. Preventive: Keep a color-coded tube guide at each phlebotomy station; review the Central Lab Manual before starting [2]. |
| Hemolyzed Sample [3] | Inaccurate Analysis: Spilled intracellular components can falsely elevate potassium, LDH, AST, and other analytes. | Corrective: Recollect the sample. Preventive: Use appropriate needle gauge (21-22G); avoid vigorous shaking; allow alcohol to dry before venipuncture; ensure proper clotting before centrifugation [3]. |
| Improper Storage Conditions [2] [7] | Sample Degradation: Loss of analyte stability, death of cells in culture, bacterial overgrowth. Irreversible Damage. | Corrective: If stability is unknown, assume degradation and recollect. Preventive: Clearly mark storage zones (ambient, refrigerated, frozen); use continuous temperature monitoring with alerts; implement backup power systems [7] [6]. |
| Use of Expired Collection Kits [2] | Unreliable Results: Evacuated tubes may lose vacuum; preservatives or additives may degrade. | Corrective: Recollect using a kit with a valid expiration date. Preventive: Implement a first-in-first-out (FIFO) inventory system; perform regular audits of lab kits and discard expired supplies [2] [7]. |
| Missing or Incomplete Data [2] | Breach of Protocol: Compromises chain of custody, risks sample exclusion from analysis. Introduces Bias. | Corrective: Attempt to recover data from source documents. Preventive: Use a Lab Information Management System (LIMS) to enforce required fields; ensure "if it's not documented, it didn't happen" is a core lab principle [7]. |
Quality Attribute Metrics for Experimental Protocols
To standardize the assessment of sample quality, the following metrics should be tracked and reported in study protocols.
Table 1: Metrics for Core Quality Attributes
| Quality Attribute | Metric to Measure | Calculation Method | Target Threshold |
|---|---|---|---|
| Completeness | Percentage of mandatory fields populated for all samples. | (Number of samples with fully populated mandatory fields / Total number of samples) * 100 [1] | >98% |
| Uniqueness | Rate of duplicate or misidentified samples. | (Number of samples with duplicate identifiers / Total number of samples) * 100 [1] | <0.1% |
| Timeliness | Percentage of samples processed within the required time window. | (Number of samples processed within protocol-specified time / Total number of samples) * 100 [1] | >95% |
| Accuracy | Percentage of data points that match verifiable source documents. | (Number of verified correct data points / Total number of data points checked) * 100 [1] | >99% |
| Consistency | Percentage of sample records that match across different systems (e.g., LIMS vs. EHR). | (Number of perfectly matched records / Total number of records checked) * 100 [1] | >99.5% |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials for Standardized Sample Collection & Storage
| Item | Function & Importance in Standardization |
|---|---|
| EDTA Tubes (e.g., Lavender Top) | Prevents coagulation by chelating calcium. Critical for hematology tests like CBCs, as it preserves cellular morphology. The correct fill volume and immediate inversion are essential for data accuracy [3]. |
| Serum Separator Tubes (SSTs/Gel-Barrier) | Contains a clot activator and a gel barrier. After centrifugation, the gel forms a stable barrier between serum and cells, which is critical for obtaining high-quality, non-hemolyzed serum for chemistry tests [3]. |
| Cryogenic Vials | Designed for safe storage of samples in liquid nitrogen or -80°C freezers. Their integrity is critical for long-term biobanking, preventing sample degradation and ensuring data validity in longitudinal studies [7]. |
| Chain of Custody Forms (Digital or Paper) | Documents every individual who has handled a sample from collection to analysis. Critical for maintaining sample integrity, audit trails, and meeting regulatory compliance standards in clinical trials [7] [6]. |
| Lab Information Management System (LIMS) | A software platform that centralizes sample data, tracks location, manages storage conditions, and automates workflows. Critical for scaling operations, ensuring consistency, and providing real-time quality control [7]. |
Sample Integrity Assessment Workflow
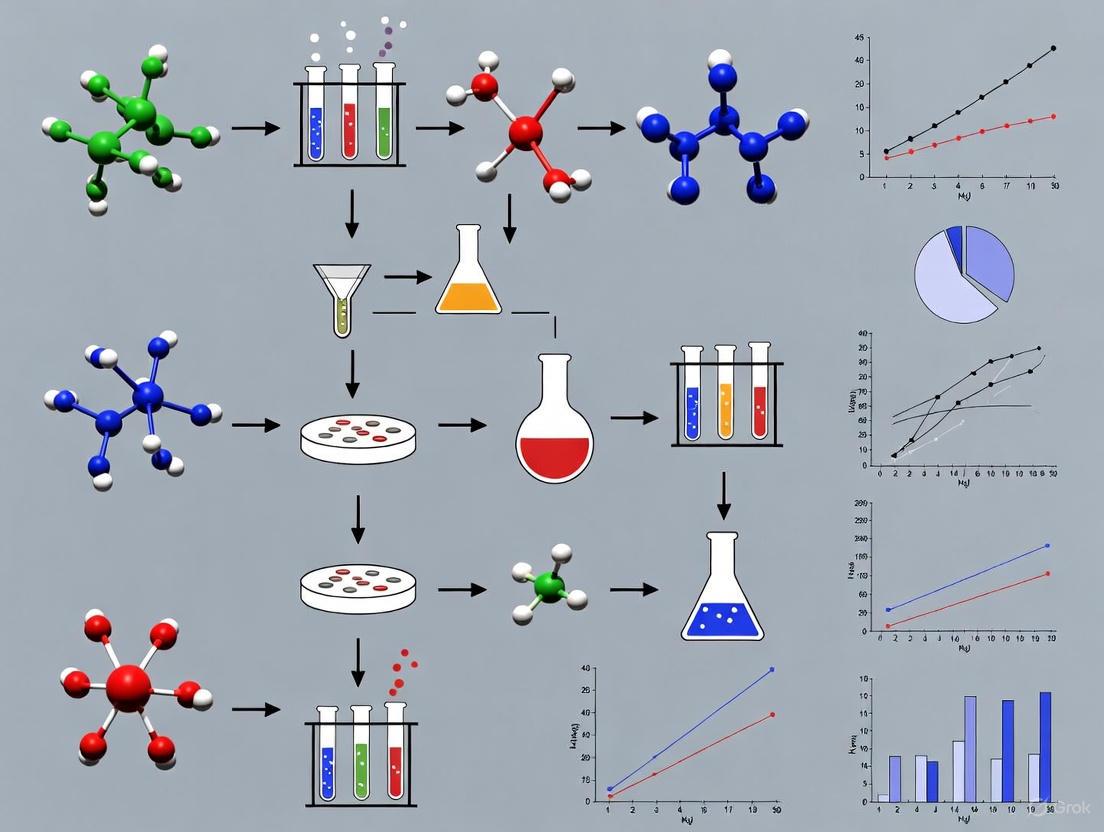
The following diagram maps the logical workflow for assessing and ensuring sample integrity against the core quality dimensions from collection through to analysis.
Six Dimensions for Qualitative Data Assessment
When analyzing observational or usability data from experimental protocols (e.g., technician feedback, participant responses), apply these six dimensions to separate surface impressions from real insights [5].
This technical support center provides troubleshooting guides and FAQs to help researchers, scientists, and drug development professionals navigate the complex regulatory environment governing sample collection, storage, and data handling. This content is framed within the broader thesis on the standardization of sample collection and storage research.
Frequently Asked Questions (FAQs)
Q1: Our research institute operates across multiple US states. Which data privacy laws are most critical for us to comply with in 2025?
The US has no single national privacy law, creating a complex patchwork of state-level regulations [8]. For 2025, compliance with the following new and updated laws is critical [9] [10]:
- New Jersey Personal Data Privacy Act: Effective January 15, 2025, it requires data protection assessments before high-risk data processing and has specific rules for minors' data [10].
- Delaware, Iowa, Nebraska, and New Hampshire Laws: All effective January 1, 2025, each with variations in consumer rights and cure periods [9] [10].
- Minnesota Consumer Data Privacy Act: Effective July 31, 2025, it grants consumers unique rights to question profiling results and may implicitly require a Chief Privacy Officer [9] [10].
- Maryland Personal Data Protection Law: Effective October 1, 2025, it features stricter data minimization requirements and a complete ban on selling sensitive data [9] [10].
- Tennessee Information Protection Act: Effective July 1, 2025, it offers an affirmative defense for businesses following recognized privacy frameworks [9] [10].
Table: Key 2025 State Privacy Law Dates and Provisions
| State | Effective Date | Key Feature | Cure Period |
|---|---|---|---|
| Delaware | January 1, 2025 [10] | Entity-level GLBA exemption [10] | 60-day, expires Dec 31, 2025 [10] |
| New Hampshire | January 1, 2025 [10] | Universal opt-out mechanism support [10] | 60-day, expires Dec 31, 2025 [10] |
| New Jersey | January 15, 2025 [10] | Mandatory pre-processing data protection assessments [10] | 30-day, until July 15, 2026 [10] |
| Minnesota | July 31, 2025 [9] | Right to explanation of profiling [10] | 30-day, until Jan 31, 2026 [10] |
| Maryland | October 1, 2025 [9] | "Strictly necessary" data collection standard [10] | 60-day, until April 1, 2027 [10] |
Q2: What are the core GxP standards we must follow for sample integrity in clinical research and biobanking?
GxP is a collective term for "Good Practice" quality guidelines that ensure product quality, data integrity, and patient safety throughout the product lifecycle [11] [12]. The core domains are [13] [11]:
- Good Laboratory Practice (GLP): Ensures the uniformity, consistency, reliability, reproducibility, quality, and integrity of non-clinical safety tests in research labs [13].
- Good Clinical Practice (GCP): An international ethical and scientific quality standard for designing, conducting, recording, and reporting trials that involve human subjects [13] [11].
- Good Manufacturing Practice (GMP): Governs the manufacturing and quality assurance of products, covering issues like cleanliness, record-keeping, and personnel qualifications [13] [11].
- Good Distribution Practice (GDP): The minimum standard for wholesale distributors to ensure that the quality and integrity of medicines are maintained throughout the supply chain [13].
Q3: We are implementing an automated sample storage system. How can we ensure it meets GxP data integrity requirements?
Automated sample storage systems are critical for modern biobanking and research, with the global market projected to grow from USD 1.3 billion in 2024 to USD 3.6 billion by 2034 [14]. To ensure GxP compliance [13] [12]:
- Implement Robust Data Governance: Establish comprehensive data governance policies, including data classification, access controls, and regular audits.
- Ensure System Validation: Follow a defined software development lifecycle (SDLC) process and validate all computerized systems.
- Maintain Audit Trails: Implement secure, computer-generated, time-stamped audit trails to independently record user actions.
- Apply ALCOA+ Principles: Ensure all data is Attributable, Legible, Contemporaneous, Original, and Accurate (ALCOA), plus complete, consistent, enduring, and available.
- Integrate with LIMS: Ensure your automated storage seamlessly integrates with Laboratory Information Management Systems (LIMS) for efficient sample tracking and metadata management [14].
Table: The Scientist's Toolkit: Essential GxP Compliance Solutions
| Tool / Solution | Function in Research & Compliance |
|---|---|
| Integrated Compliance Platforms | End-to-end digital systems combining various tools for real-time GxP monitoring and documentation [12]. |
| Automated Sample Storage System | Robotic systems providing secure, traceable, temperature-controlled storage for biological samples, minimizing human error [14]. |
| Laboratory Information Management System (LIMS) | Software for tracking sample metadata, automating retrieval, and providing real-time inventory updates [14]. |
| Blockchain Technology | Provides an immutable, transparent ledger for tracking data and samples throughout the product lifecycle, enhancing auditability [12]. |
| RFID & 2D Barcode Tracking | Advanced labeling technologies for real-time sample identification, minimizing manual intervention and enhancing traceability [14]. |
Troubleshooting Common Compliance Issues
Issue 1: Data Breach or Integrity Failure During a Clinical Trial
Problem: A data integrity failure or potential breach is identified, risking GCP non-compliance and invalidation of trial data.
Solution:
- Immediate Action: Isolate affected systems and conduct a root cause analysis following GCP protocols for documentation and reporting [13].
- Remediation: Implement enhanced cybersecurity controls. In 2025, 90% of life sciences organizations are increasing such investments [12].
- Long-term Prevention: Adopt AI and machine learning to automate routine compliance checks and monitor for deviations in real-time [12].
Issue 2: Sample Integrity Compromise in Biobank
Problem: A breach in sample integrity is detected, potentially due to temperature excursion or misidentification in storage.
Solution:
- Immediate Action: Quarantine affected samples and document the event per GLP guidelines. Use the system's audit trail to trace all actions on the samples [13].
- Remediation: Validate and utilize the automated storage system's real-time environmental monitoring and alert functions. Systems integrated with AI can predict maintenance needs to prevent such failures [14].
- Long-term Prevention: Ensure your automated storage system meets GMP/GDP requirements for equipment calibration and maintenance, and that it integrates with LIMS for full sample traceability [13] [14].
The following workflow outlines the integrated compliance path for managing samples and data, connecting the key regulatory and operational steps discussed.
Issue 3: Inability to Fulfill a Consumer Data Deletion Request
Problem: A research participant from California requests the deletion of their data, but the data is part of a longitudinal study and cannot be simply removed without compromising research integrity.
Solution:
- Assessment: Determine if your organization qualifies as a "business" under laws like the CCPA and if an exemption applies (e.g., for research conducted in the public interest) [8].
- Action: If no exemption applies, comply with the request using verified processes. For data brokers, the California "Delete Act" requires a single, accessible deletion mechanism by January 1, 2026 [8].
- Prevention: Update privacy notices and consent forms to clearly explain data usage in research and the rights applicable to participants.
This technical support center provides troubleshooting guides and frequently asked questions (FAQs) to help researchers, scientists, and drug development professionals navigate the challenges of sample management within the context of standardizing collection and storage research.
Troubleshooting Guides
Guide 1: Addressing Sample Degradation Issues
Sample degradation compromises data integrity. This guide helps identify and rectify common causes.
| Problem | Possible Root Cause | Recommended Action | Preventive Measures |
|---|---|---|---|
| Unexpected analyte degradation | Incorrect or fluctuating storage temperature [15] | Check temperature monitoring system and data loggers; implement corrective actions per SOP [15]. | Validate analyte stability for all storage conditions; use storage units with continuous monitoring and alarm systems [15]. |
| Poor sample quality upon analysis | Inconsistent processing or handling post-collection [16] | Review processing protocols (centrifugation time/force, temperature) for consistency [15]. | Use standardized protocols, smart tubes, and train staff on new preparation techniques [16]. |
| Compromised sample integrity after transport | Temperature excursion during shipment [16] | Inspect packaging and data loggers upon receipt; document deviation [15]. | Use qualified carriers, validated packaging (e.g., dry shippers), and ship with temperature data loggers [16] [15]. |
Guide 2: Resolving Sample Identification and Traceability Errors
Unambiguous sample identification is critical for data credibility. Troubleshoot identification issues using this guide.
| Problem | Possible Root Cause | Recommended Action | Preventive Measures |
|---|---|---|---|
| Unreadable or lost sample labels | Handwritten labels; labels incompatible with storage conditions (e.g., liquid nitrogen) [16] | Reconcile samples against shipment inventory and protocol information; use a unique identifier [15]. | Move away from handwritten labels; use pre-printed barcodes, QR codes, or RFID chips with storage-compatible materials [16]. |
| Gaps in chain of custody | Lack of a robust electronic tracking system [15] | Reconstruct sample movement from paper records and lab notebooks; report discrepancy [15]. | Implement a Laboratory Information Management System (LIMS) compliant with 21 CFR Part 11 to maintain audit trails [16] [15]. |
| Mismatch between sample and data | Human error during manual data entry or sample logging [16] | Halt analysis and verify all sample identifiers against the electronic inventory [15]. | Automate data capture with barcode scanners; split samples into multiple aliquots shipped separately to preserve one set [16] [15]. |
Frequently Asked Questions (FAQs)
Sample Collection & Consent
Q: What are the key consent requirements for collecting biological specimens for future research? A: When obtaining consent, it must be clear to participants that they can refuse permission for future research use without it affecting their participation in the current study or their healthcare. Participants should also be informed that they can change their mind and withdraw permission at a future date. For research involving minors, permission must be obtained from a parent or guardian, and the child, upon becoming an adult, must have the right to rescind that permission. It is recommended that consent for future use be incorporated into the main study consent form rather than being a separate document [17].
Q: Is additional consent needed to use previously collected, identifiable biological specimens for a new study? A: Yes. If an investigator plans to use already collected identifiable biological specimens for research not defined in the original protocol, they must consult with their IRB. If the IRB finds the existing consent is insufficient, then new consent must be obtained or waived by the IRB [17].
Sample Storage & Handling
Q: What are the industry-standard storage temperatures, and how should they be documented? A: To avoid confusion from slight variations in temperature settings (e.g., a freezer set to -70°C vs. -80°C), it is recommended to move away from specific temperatures and adopt standard terminology with defined ranges. The suggested terms are "room temperature," "refrigerator," "freezer," and "ultra-freezer." All storage units must have continuous temperature monitoring with alert systems for excursions [15].
Q: What are the best practices for ensuring sample integrity during long-term storage? A: Best practices include [16] [15]:
- Secure, Access-Controlled Facilities: Limit access to authorized personnel using badges, codes, or biometrics.
- 24/7 Monitoring: Implement monitoring and warning systems for storage units, with contingency plans for equipment failure.
- Disaster Recovery Plan: Have a plan for power outages or unit failures.
- LIMS: Use a Laboratory Information Management System for real-time inventory tracking and location status.
- Sample Splitting: Split samples into multiple sets (e.g., Set 1 and Set 2) and store them in different units to mitigate risk.
Sample Transport & Logistics
Q: What regulations govern the transportation of biological samples? A: Transporting biological samples is a demanding process that requires adherence to international regulations. Key standards include [16]:
- IATA: International Air Transport Association regulations for air transport.
- ADR: European Agreement concerning the International Carriage of Dangerous Goods by Road.
- MOTs (CFR 173.6): Materials of Trade standards for road transport in the US. Biological samples are classified as dangerous goods, either Category A (UN2814/UN2900) or Category B (UN3373), each with specific packaging requirements.
Q: What should I check when receiving a sample shipment? A: Upon receipt [15]:
- Inspect the packaging for damage.
- Verify that the required shipping conditions were maintained (e.g., sufficient dry ice remains).
- Check the samples against the shipment inventory for discrepancies.
- Log the samples into your facility's tracking system (e.g., LIMS) and move them to appropriate storage conditions immediately. Any deviations must be reported to the shipping facility and responsible personnel.
Essential Workflows in Sample Management
The following diagram illustrates the complete lifecycle of a biological sample, from collection to final disposal, highlighting key decision points and pathways.
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials and systems used in effective sample management.
| Item | Function & Purpose |
|---|---|
| LIMS (Laboratory Information Management System) | A robust electronic system for managing sample data, inventory, chain of custody, and audit trails, often compliant with 21 CFR Part 11 [16] [15]. |
| Standardized Collection Tubes | Tubes with appropriate anticoagulants or preservatives (e.g., smart tubes, microtainers) to ensure sample stability at the point of collection [16] [15]. |
| Barcode/QR Code/RFID Labels | For unambiguous sample identification from collection onwards, replacing error-prone handwritten labels and enabling efficient tracking [16]. |
| Temperature-Monitored Storage Units | Refrigerators, freezers, and ultra-freezers with continuous monitoring and alarm systems to maintain sample integrity [15]. |
| Validated Shipping Containers | Packaging such as dry shippers that maintain required temperature conditions during transport, complying with IATA/ADR regulations [16] [15]. |
| Temperature Data Loggers | Devices included in shipments or storage to monitor and record conditions, providing evidence of stability maintenance [15]. |
| Chain of Custody Documentation | Paper or electronic records that track every handler, location, and storage condition change throughout a sample's life [15]. |
The Critical Role of Standardization in Multi-Center Studies and Biobanking
Why is a standardized organizational structure non-negotiable in multi-center studies?
A well-defined organizational structure is fundamental to the success of a multi-center study. It ensures adequate communication, monitoring, and coordination across all participating sites, which is critical for maintaining protocol adherence and data integrity [18].
The following structure is commonly recommended:
- Steering Committee: Composed of principal investigators from major participating clinical centers, this committee is responsible for designing the protocol, approving changes, and dealing with operational problems [18].
- Coordinating Center: This center performs critical functions including preparing the manual of operations, developing data collection forms, randomizing patients, and data analysis. Its most important role is monitoring data quality and participation levels across all clinical units [18].
- Advisory Committee: Comprising independent experts not contributing data to the study, this committee reviews study design, adjudicates controversies, and evaluates interim data for trends that might necessitate early study termination [18].
- Central Observers/Labs: These are essential for ensuring consistent performance and interpretation of specific laboratory tests or diagnostic findings across all centers, eliminating inter-institutional variation [18].
What are the most critical pre-analytical variables to control in biobanking?
The quality of biospecimens can be severely compromised by pre-analytical variables, especially for sensitive genomic, proteomic, and metabolomic analyses [19]. Controlling these factors is vital for providing robust and reliable samples for research.
Table: Key Pre-analytical Variables and Their Impacts
| Variable | Potential Impact on Sample Quality |
|---|---|
| Warm and Cold Ischemia | Can degrade biomolecules and alter protein phosphorylation states [19]. |
| Freeze-Thaw Cycles | Can cause protein denaturation, degradation, and loss of nucleic acid integrity [19]. |
| Type of Stabilizing Solution | Inappropriate solutions can inhibit downstream analytical techniques or fail to preserve target molecules [19]. |
| Time to Processing | Delays can lead to glycolysis in blood samples, altering metabolite levels, or RNA degradation in tissues [20]. |
| Storage Temperature Fluctuations | Can accelerate sample degradation and reduce long-term viability [20]. |
The international standard ISO 20387:2018 for biobanking requires that processes for collecting, processing, and preserving biological material are defined and controlled to ensure fitness for the intended research purpose [19] [21] [22].
Our multi-center study is experiencing protocol deviations. How can we improve adherence?
Protocol deviations often stem from an overly complex or ambiguous protocol. To improve adherence, focus on simplification, clarity, and centralized monitoring.
- Simplify and Focus the Protocol: A protocol that tries to answer too many questions can become impracticably heavy, leading to poor adherence and patient withdrawals. Focus on a primary, carefully identified objective [18].
- Ensure Unanimous Agreement: All principal investigators on the steering committee must reach unanimity on the final protocol. A majority decision is insufficient where professional ethics and scientific conviction are concerned [18].
- Leverage Your Coordinating Center: The coordinating center should monitor data for quality and periodically edit and analyze it. It is also responsible for detecting major drops in participation level at any clinical unit, allowing for timely intervention [18].
- Use Digital Management Tools: Modern technology platforms can streamline multisite management by providing real-time insights into site progress, enabling seamless document exchange, and ensuring workflow standardization across all sites [23].
What quality control procedures must our biobank implement according to international standards?
ISO 20387:2018 specifies that a biobank must define, document, and implement quality control (QC) procedures for its processes and data [22]. The biobank must define a minimum set of QC procedures to be performed on the biological material and associated data [22].
Table: ISO 20387 Quality Control Requirements
| Focus Area | QC Requirements |
|---|---|
| Processes | Establish procedures specifying QC activities throughout all biobanking processes. Define QC criteria corresponding to predefined specifications to demonstrate fitness for purpose [22]. |
| Data | Define the type and frequency of QC performed on data, focusing on accuracy, completeness, and consistency [22]. |
| Biosafety & Biosecurity | Implement procedures to ensure compliance with biosafety (preventing unintentional exposure/release) and biosecurity (preventing loss, theft, or misuse) [22]. |
How should we handle the return of individual research results from a biobank?
The return of individual research results (IRR) is a complex issue. Before offering results, a biobank must overcome significant practical challenges related to quality, validity, and operations [24].
- Analytical Validity and Quality Control: Research tests must be repeated using a clinical standard methodology in a CLIA-certified or similarly accredited laboratory to ensure analytical validity. Research labs and biobanks typically lack this certification [24].
- Sample Tracking and Identity Confirmation: Rigorous quality-assurance procedures are needed to ensure the sample tested actually came from the correct participant. The risk of misidentification may be higher in a research setting than in a clinical lab [24].
- Clinical Validity and Utility: Even if a result is analytically valid, its clinical significance (clinical validity) and actionability (clinical utility) must be well-established. Returning results of unknown significance can cause unnecessary harm and anxiety [24].
- Operational Burden and Informed Consent: The process of re-contacting participants, providing appropriate counseling, and managing the resulting healthcare inquiries requires significant resources and should be anticipated in the original informed consent process [24] [22].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Reagents for Standardized Biospecimen Processing
| Reagent / Material | Critical Function |
|---|---|
| Viral Transport Medium | Used with nasopharyngeal swabs to maintain virus viability for isolation and RT-PCR analysis [20]. |
| EDTA Tubes | Anticoagulant for collecting whole blood for peripheral blood mononuclear cell (PBMC) isolation, used for virus isolation [20]. |
| Standardized Filter Paper | For collecting dried blood spots (DBS); must be high-quality (e.g., Whatman 903) and marked with circles for standardized blood deposition [20]. |
| Sterile Transport Medium / PBS | For resuspending urine sediment pellets or nasopharyngeal samples to preserve specimens during storage and shipment [20]. |
| Cryogenic Labels | Designed to withstand long-term storage in liquid nitrogen vapor or ultra-low freezers without degrading or detaching, ensuring sample identity [25]. |
What are the key statistical reporting guidelines we must follow for publication?
Adherence to standardized reporting guidelines is crucial for the transparency, reproducibility, and reliability of published biomedical research [26].
The following workflow outlines the selection of key guidelines:
Key statistical elements to report, as per the SAMPL (Statistical Analyses and Methods in the Published Literature) guidelines, include [26]:
- Randomization: Report the specific method used (e.g., computer-generated random numbers). Do not use the term loosely [26].
- Blinding and Allocation Concealment: Clearly distinguish between blinding (who was unaware of the treatment) and allocation concealment (the method, e.g., sealed envelopes, used to prevent foreknowledge of group assignment) [26].
- Sample-Size Estimation: Report all parameters used in the calculation (e.g., estimates, alpha, power), the source of these estimates, and the formula or software used [26].
- Statistical Analysis: Describe the appropriateness of each statistical test used, the software package, how outlying data and missing data were handled, and clearly distinguish between pre-specified primary analyses and post-hoc exploratory analyses [26].
From Theory to Practice: A Step-by-Step Guide to Standardized Protocols
This technical support article provides the foundational knowledge and practical tools to design a robust pre-collection plan, ensuring the integrity of your samples from the moment they are obtained.
Troubleshooting Guide: Common Pre-Collection & Sample Handling Issues
Q: My coagulation samples are frequently rejected by the lab for being "clotted" or "under-filled." What is the root cause and how can I prevent this?
A: This typically indicates an issue with the blood-to-anticoagulant ratio or improper mixing [27].
- Prevention: Ensure light blue-top (sodium citrate) tubes are filled to the proper vacuum level [27]. Immediately after venipuncture, invert the tube gently 3 to 6 times using complete end-over-end inversions to ensure adequate mixing and prevent clotting [27] [28].
Q: When drawing blood from an indwelling catheter, my coagulation results are inconsistent. What could be contaminating the sample?
A: Contamination from heparin, saline, or tissue fluids is a common risk with catheters [27] [28].
- Prevention: Flush the line with 5 mL of saline and discard the first 5 mL of blood or six dead space volumes of the catheter before collecting the sample for coagulation testing [27]. For winged collection sets, discard the first tube (neutral or citrate) before filling the coagulation tube [28].
Q: My plasma samples were rejected for having high platelet counts despite centrifugation. How can I ensure Platelet-Poor Plasma (PPP)?
A: A single centrifugation step may be insufficient. Incomplete platelet removal affects tests like Lupus and Heparin Assays [28].
- Prevention: Implement a double centrifugation protocol [27] [28]. After the first centrifugation, transfer the plasma to a new plastic tube using a plastic pipette, and re-centrifuge the sample. When transferring the plasma a second time, take care not to include any residual platelets [28].
Q: How should I handle sample transport and storage to avoid activation of coagulation factors?
A: Improper temperature is a key risk.
- Prevention: Transport samples at room temperature (15–25°C) and keep the tube vertical [28]. Do not transport on ice or in a refrigerated state (2-8°C), as this can cause cold activation of some factors [28]. Process or freeze plasma within 4 hours of collection for most tests [27] [28].
Pre-Collection Planning Checklist
A successful collection begins long before the sample is taken. Use this checklist to ensure all planning aspects are covered.
- Define Clear Objectives: Determine what you need to learn from the data to guide the entire collection strategy [29].
- Describe Sampling Procedures: Document the sample volume to be collected, required anticoagulant, collection and storage containers, and processing details (e.g., centrifugation time, force, temperature) in the study protocol or laboratory manual [15].
- Establish Sample Labeling Protocol: Use a unique identifier for all samples. Avoid handwritten labels. Minimum information should include protocol number, subject number, visit/time, matrix, and the unique ID [15].
- Plan for Sample Splitting: If sample volume permits, split the sample into two portions (e.g., Set 1 and Set 2) to provide a backup aliquot [15].
- Develop a Chain of Custody Plan: Maintain a record of the sample's location and storage conditions throughout its entire life cycle, ideally using a Laboratory Information Management System (LIMS) [15].
- Validate Equipment and Methods: Conduct pilot tests to identify potential issues and refine data collection methods before full-scale implementation [29].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and their functions for proper sample collection in coagulation and general bioanalysis.
| Item | Function & Application |
|---|---|
| Light Blue-Top Vacutainer Tube (3.2% Sodium Citrate) | The standard collection tube for plasma-based coagulation testing. It maintains the blood-to-anticoagulant ratio at nine parts blood to one part citrate for accurate results [27]. |
| Plastic Transfer Pipettes | Used for transferring plasma after centrifugation. Plastic is recommended to minimize the risk of activating the coagulation cascade [27]. |
| Non-Activating Plastic Centrifuge Tubes | Essential for storing plasma after processing. These tubes ensure that the plasma does not come into contact with activating surfaces, preserving sample integrity [28]. |
| ZL6 Data Logger / ZENTRA Cloud | While specific to environmental data, this illustrates the importance of real-time data collection and monitoring. For sample management, this translates to temperature monitoring systems for storage units to ensure analyte stability [30] [15]. |
| TEROS Borehole Installation Tool | While used for soil sensor installation, it exemplifies the critical nature of proper installation tools for accuracy. In a lab context, this underscores the need for validated tools and precise techniques, such as using the correct needle gauge (19-22 gauge) for venipuncture to prevent hemolysis [30] [28]. |
Standardized Protocols & Data Tables
Sample Collection & Handling Parameters
Adhering to standardized parameters is critical for maintaining sample integrity. The tables below summarize key requirements.
Table 1: Sample Collection Specifications
| Parameter | Recommendation | Potential Risk of Non-Compliance |
|---|---|---|
| Needle Gauge | 19-22 gauge (23 gauge acceptable for pediatric/compromised veins) [28] | Hemolysis, sample contamination [28] |
| Tourniquet Time | Release immediately when first tube starts to fill (<1 minute) [28] | Hemolysis, activation of fibrinolysis, acidosis [28] |
| Tube Mixing | 3-6 complete end-over-end inversions immediately after collection [27] [28] | Improper anticoagulant mixing, sample clotting, microclots [27] [28] |
| Sample Stability (Room Temp) | 4 hours for most routine tests [28] | Activation of coagulation factors, false results [28] |
Table 2: Centrifugation & Storage Specifications
| Parameter | Recommendation | Potential Risk of Non-Compliance |
|---|---|---|
| Centrifugation (Standard) | 1500 g, 15 minutes, room temperature [28] | Platelet contamination, false results in Lupus/Heparin assays [28] |
| Plasma Processing Time | Within 4 hours of collection (except protimes) [27] | Degradation of analytes, loss of sample viability [27] |
| Frozen Storage (-20°C) | Maximum 2 weeks [28] | Analyte instability, loss of data integrity [28] |
| Frozen Storage (-70°C) | 6 months to 12 months [28] | Analyte instability, loss of data integrity [28] |
Experimental Workflow for Standardized Plasma Sample Collection
The following diagram illustrates the critical path from patient to analysis, highlighting key decision points to ensure sample quality and standardization.
Key Best Practices for Standardization
- Define Clear Objectives: The foundation of any successful collection is a clear understanding of what you need to learn from the data. This guides the entire strategy, from sample volume to analysis methods [29].
- Document Everything: Sample collection procedures must be explicitly described in the study protocol or a laboratory manual. This includes the volume of the sample to be collected, the required anticoagulant, collection and storage containers, and labeling requirements with a unique identifier [15].
- Maintain Chain of Custody: A record of the sample's location and storage conditions must be maintained throughout its entire life cycle—from collection to disposal. This is critical for proving sample integrity and is best managed using a Laboratory Information Management System (LIMS) where available [15].
- Plan for the Entire Lifecycle: Pre-collection planning must encompass more than just the draw. Consider and document procedures for processing, temporary storage at the collection site, shipment to the analytical laboratory, and final storage or disposal [15].
- Implement Quality Controls: A quality control process should be in place at the collection site to ensure documented procedures are followed. Any discrepancies must be reported immediately [15].
In the fields of biomedical research and drug development, the integrity of experimental data is fundamentally dependent on the quality of the collected samples. Standardization of sample collection and storage is not merely a procedural formality but a critical scientific prerequisite. The emergence of research on extracellular vesicles and RNA, for instance, has highlighted that technical standardization is of central importance because the influence of disparate isolation and analysis techniques on downstream results remains unclear [31].
Aseptic technique is a set of strict procedures that healthcare providers and researchers use to prevent the spread of germs that cause infection [32]. According to the Centers for Disease Control and Prevention (CDC), over 2 million patients in America contract a healthcare-associated infection annually, underscoring the vital importance of these infection control measures [33]. In laboratory and clinical settings, consistent application of aseptic techniques protects both the sample integrity and the personnel, ensuring that research outcomes are reliable, reproducible, and uncontaminated by external variables.
Fundamental Principles of Aseptic Technique
Defining Aseptic vs. Sterile vs. Clean
Understanding the distinction between related terms is crucial for proper technique implementation:
- Clean: This refers to items free from dirt, stains, and other debris, but not sterile. An unused glove from a box is clean but not sterile, meaning it still has some microorganisms [32]. Clean techniques focus on reducing the overall number of germs but do not completely eliminate them.
- Aseptic: This refers to a stricter standard of infection control aimed at eliminating pathogens completely. Providers wear sterile gloves rather than clean gloves and use sterile drapes and instruments to create a barrier against contamination [32].
- Sterile: This term describes an absolute state of being free from all living microorganisms. Healthcare providers usually use "aseptic" to describe techniques and procedures and "sterile" to describe settings and instruments. For example, a provider uses aseptic techniques to create a sterile environment [32].
In laboratory practice, the difference is subtle but vital: sterilization creates the contamination-free zone, while aseptic technique maintains it [34].
Core Elements of Aseptic Technique
Aseptic techniques rely on four fundamental elements [32]:
- Tool and Patient/Subject Preparation: All tools or instruments must be sterilized, typically using methods like steam sterilization (autoclaving). For human patients, providers apply antiseptic to the skin to reduce germs.
- Barriers: The use of masks, gowns, and gloves creates a protective barrier that prevents cross-contamination.
- Contact Guidelines: Personnel must follow strict sterile-to-sterile contact rules, meaning they wear sterile protective gear and only touch sterile items.
- Environmental Controls: This involves measures to reduce germs in the environment, such as keeping doors closed during surgical procedures or using laminar flow hoods.
Proper Use of Personal Protective Equipment (PPE)
PPE forms an immediate protective barrier between the personnel and the hazardous agent, protecting both the researcher and the sample [35].
Essential PPE Components
- Gloves: Gloves protect both patients and healthcare personnel from exposure to infectious material that may be carried on the hands [33]. In a cell culture lab, gloves should be changed when contaminated and disposed of properly [35].
- Lab Coats or Gowns: A clean lab coat should be worn to prevent contamination from street clothes [34]. For higher-risk procedures, a sterile fluid-resistant gown may be necessary.
- Eye Protection: Safety glasses or goggles protect eyes from chemical splashes and accidental aerosols [35].
- Masks/Respirators: Masks are used for droplet precautions, while fit-tested N-95 respirators are required for airborne precautions [33].
PPE Donning and Doffing Sequence
The order of putting on (donning) and removing (doffing) PPE is critical to prevent self-contamination. The following diagram illustrates the proper workflow:
Sterile Equipment and Work Area Management
Instrument Sterilization
Instruments must be sterilized before they are used for aseptic procedures. The most common method is steam sterilization in an autoclave [32]. After use, instruments first need to be cleaned using a sterile brush in sterile water (not saline) to remove organic material [36]. It is important to note that briefly immersing instruments in alcohol is not an effective means of sterilization [36].
Maintaining a Sterile Work Area
A major requirement is maintaining an aseptic work area restricted to cell culture work [35].
- Biosafety Cabinet (BSC): The primary tool for cell culture work, a BSC creates a sterile working environment by continuously filtering air through a HEPA filter [34]. It should be turned on for at least 15 minutes before use to allow airflow stabilization [34].
- Work Surface Disinfection: Before and after work, the interior surfaces of the BSC must be thoroughly wiped with 70% ethanol [35] [34].
- Workflow Management: All necessary materials should be arranged strategically within the hood before beginning, keeping items at least six inches from the front grille to avoid disrupting airflow [34]. The work surface should be uncluttered and not used as a storage area [35].
Troubleshooting Guides for Common Aseptic Technique Issues
Contamination Identification and Resolution
| Contamination Type | Visual Signs | Common Sources | Corrective Actions |
|---|---|---|---|
| Bacterial | Cloudy, turbid culture medium; tiny, shimmering specks under microscope [34]. | Non-sterile reagents, contaminated surfaces, improper glove technique [35]. | Quarantine and discard culture. Review hand hygiene and surface disinfection. Use fresh, aliquoted reagents [34]. |
| Fungal/Yeast | Fuzzy, off-white/black surface growth; small, refractile spheres in medium [34]. | Airborne spores, skin contact with plate, unclean incubators [35]. | Discard culture. Clean incubators and BSC thoroughly. Ensure all plates are stored in sterile re-sealable bags [35]. |
| Mycoplasma | No visible turbidity; subtle effects on cell growth/metabolism [34]. | Fetal bovine serum, cross-contamination from infected cultures [34]. | Quarantine and discard culture. Regular testing of cell stocks and reagents is essential [34]. |
| Cross-Contamination | Unusual cell morphology or growth patterns [35]. | Using same pipette for different cell lines, unsterile equipment [35]. | Use a sterile pipette only once. Have dedicated media and reagents for each cell line [35]. |
Procedural Failures
| Problem | Potential Cause | Prevention Strategy |
|---|---|---|
| Consistent contamination in all cultures | Contaminated common reagent or media [35]. | Aliquot reagents into smaller, single-use volumes. Test new lots of reagents before full use [34]. |
| Sporadic contamination | Breach in personal technique, disrupted airflow in BSC [34]. | Minimize rapid arm movements in BSC. Do not talk, sing, or whistle during procedures [35]. |
| Contamination after successful subculture | Unsterile equipment or surface [35]. | Ensure thorough disinfection of work surfaces with 70% ethanol before and after work [35] [34]. |
| Ineffective instrument sterilization | Reliance on alcohol immersion instead of validated methods [36]. | Use autoclaving for initial sterilization. For batch procedures, use a hot bead sterilizer between samples [36]. |
Frequently Asked Questions (FAQs)
Q1: What is the most critical step of aseptic technique for cell culture? While all steps are important, the most critical element is the consistent use of the biosafety cabinet and the meticulous disinfection of all surfaces and materials with 70% ethanol before starting work. This establishes and maintains the sterile field [34].
Q2: Is it necessary to flame the neck of a bottle during aseptic procedures? Yes, flaming the neck of a sterile bottle or flask is a crucial step in proper aseptic technique. The heat creates an upward convection current of sterile air, preventing airborne microorganisms from entering the container while it is open [34]. Note that flaming is not recommended inside a modern biosafety cabinet as it disrupts laminar airflow [35].
Q3: How do I know if my cell culture is contaminated? Visible signs include a cloudy or turbid appearance of the medium (bacteria), fuzzy spots or growth on the surface (fungi), or an unusual change in medium pH. For insidious contaminants like mycoplasma, which do not cause visible changes, regular testing is required [34].
Q4: Why is 70% ethanol the preferred disinfectant instead of 100%? 70% ethanol is more effective for microbial control because the presence of water slows evaporation, allowing for longer contact time and better penetration through the microbial cell wall.
Q5: Can I wear sterile gloves for multiple procedures? No. Gloves should be changed between procedures, when moving from a contaminated to a clean body site on a patient, and after touching potentially contaminated surfaces or equipment [33] [35].
Aseptic Technique Workflow: From Preparation to Execution
The following diagram provides a comprehensive overview of the key stages and decision points in a standardized aseptic collection procedure, integrating PPE use, workspace management, and sterile handling.
Essential Research Reagent Solutions and Materials
The following table details key materials and their functions essential for maintaining asepsis in a research setting.
| Item | Function | Key Consideration |
|---|---|---|
| 70% Ethanol | Gold standard for surface disinfection of work areas and equipment [35] [34]. | More effective than 100% ethanol due to better microbial penetration. |
| Sterile Disposable Pipettes | For manipulating liquids without introducing contaminants [35]. | Use each pipette only once to avoid cross-contamination. |
| Autoclave | Provides steam sterilization for instruments, glassware, and solutions [32]. | Validate sterilization cycles regularly. Use indicators to confirm sterility. |
| Biosafety Cabinet (BSC) | Provides a HEPA-filtered sterile work environment for procedures [35] [34]. | Must be certified annually. Run for 15+ minutes to purge airborne particles. |
| Personal Protective Equipment (PPE) | Forms a barrier against shed skin, dirt, and microbes from the researcher [35]. | Includes gloves, lab coats, and safety glasses. Change gloves frequently. |
| Sterile Culture Vessels/Media | Sterile consumables for cell growth and manipulation. | Ensure integrity of packaging. Discard if packaging is damaged. |
| Hot Bead Sterilizer | For decontaminating microsurgical instrument tips between animals in batch procedures [36]. | Follow manufacturer's instructions for exposure time. Not a substitute for initial autoclaving. |
FAQs and Troubleshooting Guides
This section addresses common challenges researchers face when implementing and using barcode and QR code systems in the laboratory.
FAQ 1: How do I choose between a 1D barcode and a 2D code for my samples?
The choice depends on your data requirements and the physical space available on your labware [37].
- Solution: The following table outlines the key differences to guide your selection:
| Feature | 1D Barcodes (e.g., Code 128, Code 39) | 2D Barcodes (e.g., Data Matrix, QR Code) |
|---|---|---|
| Data Capacity | Limited (typically 20-25 characters) [38] | High (up to 7,089 numeric characters) [38] |
| Data Type | Primarily numbers and letters [37] | Alphanumeric, binary, URLs, and more [38] [37] |
| Space Required | Requires more horizontal space | Stores more data in a compact area [37] |
| Common Uses | Labeling lab equipment, general inventory [37] | Small vials, sample tubes, linking to detailed digital records [37] |
FAQ 2: My scanner cannot read the barcodes on my samples. What is wrong?
This is a common issue often related to the quality of the printed code or the scanning environment [37].
- Troubleshooting Guide:
- Check the Quiet Zone: Ensure there is a clear, unobstructed margin around the barcode. This "quiet zone" is essential for the scanner to distinguish the code from its surroundings [38] [37].
- Verify Contrast: The code must have high contrast between the foreground and background (e.g., black on white). Avoid color combinations that blend together, as this is a frequent cause of scan failures [39] [37].
- Assess for Damage: Look for smudging, tearing, or fading on the label. If the code is physically damaged, it may not be scannable [37].
- Confirm Size and Density: If the code is too small or has too much information encoded in a small space, scanners may fail to read it. Ensure the code is printed at a sufficient size for your scanner [39].
FAQ 3: What is a serialized QR code, and why would I use it for sample management?
A serialized QR code is a unique code on each individual sample, containing a unique identifier string in its embedded URL [40].
- Solution: Serialization is critical for unit-level traceability, which is a cornerstone of standardization. It allows you to:
- Track Individual Samples: Follow a single sample's journey from collection through analysis, which is vital for audits and reproducibility [40].
- Prevent Counterfeiting: Authenticate unique samples, as a code scanned multiple times in disparate locations can indicate a counterfeit [40].
- Manage Data Precisely: Associate specific data, like experimental conditions or patient information, with one specific sample rather than a batch [40].
FAQ 4: The data linked to my QR code needs to be updated. Can I change it without reprinting all my labels?
Yes, this is a key advantage of using QR codes for sample labeling.
- Solution: If the QR code encodes a URL that points to a digital record, you can update the information on the webpage or database entry that the URL leads to without ever changing the physical label [40]. This ensures that users scanning the code will always access the most current information, which is crucial for long-term sample storage [41].
FAQ 5: How can I ensure my barcoded labels will withstand harsh lab environments (e.g., freezers, liquid nitrogen, solvents)?
Label durability is a non-negotiable aspect of reliable sample management.
- Solution: The longevity of your labels depends on the materials used [37].
- Label Material: Choose durable label materials designed to withstand your laboratory's specific conditions, including exposure to extreme temperatures, moisture, and chemicals [37].
- Printing Technology: For applications with high wear and tear, consider laser etching the code directly onto the sample container, as this provides a permanent and durable mark [40].
The Scientist's Toolkit: Essential Materials for Implementation
The following table details key solutions and materials required for implementing a robust sample labeling system.
| Item | Function |
|---|---|
| Barcode/QR Code Generator Software | Creates the unique barcode or QR code images. Enterprise-grade solutions can generate serialized codes at scale via APIs or web tools [40]. |
| Thermal Transfer Printer | Prints high-resolution, durable labels that are resistant to smudging and fading, which is critical for data integrity [37]. |
| Durable Label Materials | Synthetic labels (e.g., polyester, polypropylene) withstand exposure to extreme temperatures, moisture, and chemical spills [37]. |
| Barcode Scanner | An electronic device that reads the barcodes. Can be handheld or integrated into an automated workflow (inline scanning) [40] [37]. |
| Laboratory Information Management System (LIMS) | The central software database that associates the unique identifier from each barcode with all sample metadata, enabling full traceability [40] [37]. |
| Inline Scanning System | Automated scanning hardware used on production or packaging lines to activate and verify codes and associate individual samples with their larger containers (aggregation) [40]. |
Experimental Protocol: Workflow for Implementing a Serialized QR Code System
This protocol provides a detailed methodology for implementing a unit-level sample tracking system using serialized QR codes, a key procedure for standardizing sample collection and storage research.
1. Experimental Design and Code Generation Define the data structure for your unique identifiers. Use an enterprise QR code generator to create a unique QR code for each sample via a programmatic interface (API) or web tool. The embedded URL in each code should contain a unique serial number [40].
2. Label Printing and Affixing Select a printer that supports variable data printing (VDP), such as a digital printer, as each label will be unique [40]. Use high-quality, durable label material suitable for your sample storage conditions (e.g., cryogenic-resistant labels for freezer storage) [37]. Affix labels consistently to sample containers, ensuring they are secure and easy to scan.
3. Sample Registration (Activation) Scan each sample's QR code in the laboratory to "activate" it within your database (e.g., LIMS). This links the physical sample to its digital record and is essential for billing and preventing unauthorized use of labels [40].
4. Data Association and Aggregation In the digital record, log all relevant sample metadata (e.g., collection date, donor/patient ID, experimental conditions). For larger studies, implement an aggregation process: scan the serialized codes of individual samples and associate them with the QR or barcode on the box, crate, or pallet in which they are placed. This allows for tracking at the logistical unit level [40].
5. Quality Control and Verification Implement a QC step to verify that all codes are scannable and correctly associated in the database. Use scanners to confirm data integrity upon sample retrieval or at any point in the experimental workflow [37].
The logical workflow for this protocol is as follows:
Troubleshooting Guides
Dried Blood Spot (DBS) Collection and Analysis
Problem: Low antibody recovery or false negative results from DBS elution.
- Potential Cause 1: Incomplete elution of analytes from the filter paper.
- Solution: Ensure the DBS punch is fully submerged in the elution buffer and shaken for a sufficient duration. One protocol specifies shaking at 240 rpm for one hour at room temperature [42].
- Potential Cause 2: Incorrect blood volume spotted or uneven saturation.
- Solution: Apply blood to fill the entire pre-printed circle on the DBS card (approximately 50 μL per spot) and ensure no white areas are visible before punching [42].
- Potential Cause 3: Inadequate drying or improper storage leading to sample degradation.
- Solution: Dry spots for at least 3 hours at room temperature. Store dried cards in sealed plastic pouches with desiccant sachets at -20°C to prevent moisture damage and analyte degradation [43].
Problem: High sample variability in quantitative DBS analysis.
- Potential Cause 1: Variable extracted blood volume due to differences in hematocrit or punch location.
- Solution: For methods requiring high precision, use a predefined punch from the center of a fully saturated spot and consider hematocrit assessment. Some methods use two ¼-inch diameter punches for analysis [42].
General Sample Storage and Quality Control
Problem: Unstable biomarker measurements in stored samples.
- Potential Cause 1: Suboptimal storage temperature or conditions.
- Solution: Implement a formal biobanking system. Store plasma/serum at -70°C or lower [43] [44]. For DBS, follow consistent drying and desiccant-packaged storage at -20°C [43].
- Potential Cause 2: Lack of quality control measures across multiple samples or batches.
- Solution: Establish a Quality Management System (QMS) for the biorepository. This includes standardized procedures for sample collection, processing, storage, and incident management to ensure data reproducibility and scientific credibility [44].
Frequently Asked Questions (FAQs)
Q1: What are the key advantages of using Dried Blood Spots (DBS) over venous blood collection in large-scale studies? DBS sampling offers several key advantages [43] [45]:
- Minimally Invasive: Utilizes finger- or heel-prick collection, reducing participant discomfort.
- Logistically Simpler: Does not require trained phlebotomists for collection.
- Easier Transport and Storage: DBS cards are stable at ambient temperatures during shipping and require less freezer space, as they can be stored at -20°C compared to the -70°C often required for plasma/serum [43]. The United States Postal Service considers them a Nonregulated Infectious Material [45].
Q2: How does the performance of DBS compare to plasma for serological assays like SARS-CoV-2 antibody detection? Studies demonstrate a strong correlation between DBS and plasma/serum. One study found a correlation of r=0.935 for IgG against the Receptor Binding Domain (RBD) and r=0.965 for IgG against the full-length spike protein of SARS-CoV-2 [43]. Another study using an EUA-approved immunoassay reported a 98.1% categorical agreement between self-collected DBS and venous serum, with a correlation (R) of 0.9600 [42].
Q3: What are critical pre-analytical factors to control when collecting DBS samples?
- Drying Time: Dry spots for a minimum of 3 hours at room temperature before storage [43] [42].
- Storage Conditions: Store dried cards in sealed plastic bags with desiccant to protect from atmospheric humidity [43].
- Card Integrity: Use high-quality filter cards and check for correct, adequate blood spotting to ensure sample integrity [43].
Q4: Why is standardization critical in extracellular vesicle (EV) research from biofluids like plasma? EV research faces challenges due to the heterogeneity of vesicles and the variety of methods used for their isolation and analysis. Standardization of specimen handling, isolation techniques, and analysis is crucial to facilitate comparison of results between different studies and laboratories, and to ensure the validity of potential biomarkers [31].
Table 1: Correlation between Dried Blood Spot (DBS) and Plasma/Serum Samples for SARS-CoV-2 IgG Detection
| Specimen Comparison | Target Antigen | Correlation Coefficient (r or R) | Categorical Agreement | Citation |
|---|---|---|---|---|
| DBS vs. Plasma | RBD | r = 0.935 | - | [43] |
| DBS vs. Plasma | Full-length Spike | r = 0.965 | - | [43] |
| Self-collected DBS vs. Serum | Spike (Roche Elecsys) | R = 0.9600 | 98.1% | [42] |
| Professionally collected DBS vs. Serum | Spike (Roche Elecsys) | R = 0.9888 | 100.0% | [42] |
Table 2: Analytical Performance of a Representative DBS Assay for SARS-CoV-2 Antibodies
| Performance Parameter | Value | Citation |
|---|---|---|
| Limit of Blank (LOB) | 0.111 U/mL | [42] |
| Limit of Detection (LOD) | 0.180 U/mL | [42] |
| Assay Imprecision (Pooled Standard Deviation) | 0.0419 U/mL (Lot 1), 0.0346 U/mL (Lot 2) | [42] |
Experimental Protocols
- Punch: Using a ¼-inch (6.35 mm) diameter punch, take two punches from saturated areas of the DBS card.
- Elute: Place punches into a 16x75 mm polypropylene tube and submerge in 150 µL of universal diluent.
- Shake: Place tubes on a microplate shaker at 240 rpm for one hour at room temperature.
- Separate: Squeeze out remnant solution from the punches and discard them. The resulting extract (~100 µL) is ready for analysis.
- Collection: Sterilize the fingertip and lance with a single-use lancet. Wipe away the first drop of blood and apply subsequent drops to a filter card to fill 2-4 spots.
- Dry: Allow the blood spots to dry for 3 hours at room temperature.
- Store: Place the dried card in a plastic pouch with a silica gel desiccant sachet. Store at -20°C until analysis.
Workflow and Relationship Diagrams
DBS Sample Journey
Specimen Analysis Correlation
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for DBS-based Serology
| Item | Function/Description | Citation |
|---|---|---|
| Filter Paper Cards | Specially designed paper (e.g., Whatman 903, Eastern Business Forms 903) for absorbing and preserving a standardized volume of blood. | [42] [45] |
| High-Flow Lancets | Contact-activated devices for minimally invasive finger-prick blood collection. | [42] |
| Universal Diluent | A buffer solution used to submerge and elute analytes from the DBS punch back into a liquid phase for analysis. | [42] |
| Silica Gel Desiccant | Sachets placed with dried cards in storage pouches to absorb atmospheric moisture and prevent sample degradation. | [43] |
| Plastic Specimen Pouches | Sealable bags for storing dried cards, protecting them from physical damage and environmental contamination. | [43] [42] |
Your technical guide to resolving data traceability and sample integrity issues in the research laboratory.
This technical support center provides troubleshooting guides and FAQs for researchers and scientists implementing Laboratory Information Management Systems (LIMS) to maintain a robust chain of custody (CoC) within the context of standardizing sample collection and storage research.
Frequently Asked Questions (FAQs)
What is the core function of a Chain of Custody in research? The core function of a Chain of Custody is to provide a chronological, documented trail that ensures sample integrity and data traceability from collection through to final disposition. It documents who handled a sample, when, for what purpose, and under what conditions, making data legally defensible and scientifically credible [46] [47].
Our lab is using spreadsheets for sample tracking. When is it time to switch to a LIMS? You should consider a LIMS if you recognize three or more of these signs: your team wastes significant time searching for information [48]; you experience frequent manual data entry errors [49] [48]; preparing for audits is a major headache [48]; you lack real-time visibility into your lab's workflow status [48]; or you have difficulty complying with standards like ISO/IEC 17025 [48].
What are the most common pitfalls when implementing a CoC with a new LIMS? Common pitfalls include inadequate staff training leading to procedural errors, overcomplicated procedures that staff bypass, poor technology integration with existing instruments, and insufficient quality control like regular audits of the CoC process [46].
How does a LIMS enhance compliance with standards like ISO/IEC 17025? A LIMS facilitates compliance by centralizing documentation, ensuring data integrity through immutable audit trails, and automating quality control checks. It provides the framework for complete traceability, which is a fundamental requirement for ISO/IEC 17025 accreditation [50] [48].
What is the difference between a Chain of Custody and an Audit Trail? A Chain of Custody specifically tracks the physical and custodial journey of a sample—its location, handling, and transfers [47]. An Audit Trail is a detailed, timestamped record of every action and change made to the data within the LIMS, providing a transparent history of data modifications [47].
Troubleshooting Guides
Issue 1: Frequent Sample Tracking Errors
Problem: Samples are frequently mislabeled, misplaced, or their current status in the workflow is unknown, leading to testing delays and potential mix-ups.
Diagnosis: This indicates a reliance on error-prone manual tracking methods (e.g., paper logs, spreadsheets) and a lack of unique, scannable identifiers for samples [49].
Solution:
- Implement Unique Barcoding: Use the LIMS to generate and print a unique barcode for each sample at accessioning [49] [46] [51].
- Scan at Every Transfer: Enforce a procedure where staff must scan the sample barcode at every stage—storage, transfer, analysis, and disposal [46] [51].
- Leverage Real-Time Dashboard: Use the LIMS dashboard to view the real-time status and location of all samples, which automatically updates with each scan [48].
Prevention: Incorporate barcode label training into standard onboarding [46]. Run regular audits of the sample tracking logs to ensure scanning compliance.
Issue 2: Inadmissible Data or Broken Chain of Custody
Problem: During an audit or data review, the history of a sample cannot be fully produced, or the records are incomplete, challenging the validity of your results.
Diagnosis: The chain of custody documentation has gaps. This is often due to manual logbook entries that are lost or incomplete, or a process that allows sample handling outside of the documented system [47].
Solution:
- Verify Automated Audit Trails: Ensure your LIMS is configured to automatically log every user action with a timestamp and secure user ID [50] [47]. This creates an immutable record.
- Reconstruct the Path: Use the LIMS audit trail to reconstruct the sample's full custody path and identify the exact point of failure [50].
- Enforce Role-Based Access: Configure role-based access controls in the LIMS to prevent unauthorized handling of samples and data [50].
Prevention: Lead a culture of integrity where following CoC procedures is non-negotiable [50]. Establish a clear SOP that no sample should be handled without logging the action in the LIMS first.
Issue 3: Inefficient Workflows and Slow Turnaround
Problem: Sample processing is slower than expected, workflows are inconsistent between technicians, and staff are overloaded with administrative tasks.
Diagnosis: Workflows are not standardized or automated, leading to reliance on manual interventions, data re-entry, and constant status checks [48].
Solution:
- Map and Configure Workflows: Document your "as-is" sample testing workflows, then configure them within the LIMS to create a standardized "to-be" process [52].
- Automate Assignments and Alerts: Use the LIMS to automatically assign analytical tasks to technicians and trigger alerts when quality control checks fail or when a step is overdue [50] [49].
- Integrate Instruments: Connect analytical instruments to the LIMS to allow for automated data capture, eliminating manual transcription errors [53] [52].
Prevention: Adopt a phased rollout of new automated workflows and gather user feedback for continuous improvement [53] [52].
Issue 4: Failed Audit Due to Inadequate Traceability
Problem: An auditor cannot verify the integrity of your data or the path of a critical sample, resulting in a compliance finding.
Diagnosis: The laboratory cannot promptly produce a complete, unbroken record of sample custody and data history, often due to disjointed records and a lack of system-wide traceability [48].
Solution:
- Generate Pre-Built Reports: Utilize the LIMS reporting module to generate chain of custody and audit trail reports for any sample or date range on demand [48].
- Centralize Documentation: Use the LIMS to store and manage all relevant SOPs, instrument calibration records, and personnel qualifications in a single, audit-ready location [48] [52].
- Demonstrate Data Integrity: Show the auditor the enforced user authentication and the immutable, timestamped audit trail for all data modifications [50].
Prevention: Conduct regular internal audits using the same report generation process to identify and correct gaps before an external audit [50] [46].
Experimental Protocols & Methodologies
Standardized Workflow for Chain of Custody Integrity
The following methodology details the implementation of a LIMS-supported CoC protocol to ensure standardization in sample collection and storage research.
Procedure:
- Sample Collection & Accessioning:
- Upon receipt, create a sample record in the LIMS.
- Action: The system automatically generates a unique identifier and a corresponding barcode label. Print and affix this label to the sample container [49] [46].
- Documentation: The LIMS record captures collector information, date/time of receipt, and initial sample condition.
Secure Storage & Monitoring:
- Action: Scan the sample barcode and the barcode of its assigned storage location (e.g., freezer shelf) [49] [51]. The LIMS automatically updates the sample's location.
- Integration: For critical storage, link IoT-enabled monitors (e.g., for temperature) to the LIMS. The system will automatically log environmental conditions and trigger alerts for any deviations [50].
Analysis & Data Capture:
- Action: When retrieving the sample for analysis, scan its barcode. The LIMS will present the authorized testing workflow.
- Data Integrity: Upon analysis, directly import instrument results into the sample's record via system integration to prevent transcription errors [49] [52]. All actions are automatically recorded in the audit trail.
Final Disposition & Archiving:
- Action: For disposal or long-term archiving, perform a final barcode scan and select the appropriate disposition action in the LIMS [51].
- Documentation: The LIMS records the date, time, and authorizing user, finalizing the sample's lifecycle with a complete and unbroken chain of custody.
The Scientist's Toolkit: Research Reagent & Material Solutions
The following materials are essential for establishing and maintaining a robust chain of custody protocol.
| Item | Function in Chain of Custody |
|---|---|
| Barcode Labels & Scanner | Creates a unique, machine-readable identity for each sample, enabling fast, error-free logging of its movement and status at every stage [49] [46]. |
| Tamper-Evident Seals | Provides physical evidence of unauthorized access to sample containers, crucial for maintaining sample integrity, especially in forensic or legally sensitive research [51]. |
| Certified Reference Materials | Used to calibrate instruments and validate analytical methods, ensuring the accuracy and defensibility of the test results linked to the sample in the LIMS [51]. |
| Temperature Monitoring Devices | IoT-enabled sensors that continuously log storage conditions (e.g., temperature, humidity). They can be integrated with the LIMS to automatically record and alert deviations that could compromise sample stability [50]. |
| Role-Based Access Control System | A fundamental feature of a LIMS that restricts system functions and data access based on user roles, preventing unauthorized handling and ensuring accountability [50] [51]. |
Data Presentation: LIMS Impact on Laboratory Operations
The quantitative benefits of implementing a LIMS for chain of custody and data management are demonstrated in the following metrics from industry reports.
Table 1: Operational Improvements from LIMS Implementation
| Performance Indicator | Reported Improvement | Source / Context |
|---|---|---|
| Data Entry Errors | Reduction of up to 80%-90% | [49] [48] |
| Sample Throughput / Workload | Capability to double | [48] |
| Report Turnaround Time | 50% increase in speed for Certificate of Analysis (CoA) generation | [53] |
| Setup Time for New Systems | 30% reduction using pre-configured templates | [53] |
Troubleshooting Guide: Common Temperature Excursions
Problem 1: Temperature Excursion During Transit
- Symptoms: Data logger shows temperature spikes/drops outside required range; product stability may be compromised.
- Immediate Actions:
- Isolate Affected Shipment: Move to appropriate temperature-controlled environment immediately upon receipt [54].
- Document the Excursion: Record the duration, magnitude of temperature deviation, and time of occurrence from your data logger [55].
- Assess Product Impact: Consult the product's Stability Profile to determine if the excursion falls within acceptable tolerances [55].
- Preventive Solutions:
- Validate Packaging: Pre-condition Phase Change Materials (PCMs) and use validated thermal shipping configurations for specific duration and ambient conditions [55].
- Use Real-Time Alerts: Implement IoT-enabled loggers that send immediate notifications when temperatures deviate, allowing for proactive intervention [56] [57].
Problem 2: Inconsistent Temperatures in Storage Unit
- Symptoms: Temperature mapping reveals hot or cold spots; varying readings between different sensors.
- Immediate Actions:
- Preventive Solutions:
- Regular Mapping: Conduct formal temperature mapping seasonally (at least 2-3 times per year) and after any equipment maintenance or room layout changes [54].
- Install Automated Monitoring: Use continuous monitoring systems with sensors placed in previously identified critical areas for constant oversight [58] [59].
Problem 3: Condensation or Frost on Stored Samples
- Symptoms: Moisture buildup on packaging or samples; ice formation in frozen units.
- Immediate Actions:
- Preventive Solutions:
- Transition Samples: Allow samples acclimated to room temperature to cool in a refrigerated area before placing in long-term frozen storage to reduce frost buildup.
- Use Climate-Controlled Storage: For humidity-sensitive materials, specify climate-controlled storage which regulates both temperature and humidity [54].
Frequently Asked Questions (FAQs)
Q1: What is the critical difference between "Cold Chain" and "Cool Chain"?
- The Cold Chain is the broader term for a temperature-controlled supply chain for products that require freezing or refrigeration [55]. The Cool Chain is a specific subset for products requiring a narrow 2°C to 8°C range, essential for many biological products and pharmaceuticals [55].
Q2: What does "Controlled Room Temperature" specifically mean?
- Controlled Room Temperature is a defined range, typically 15°C to 25°C (59°F to 77°F) [55]. It is not merely "room temperature" but a stable, monitored environment for products that do not need refrigeration but must avoid extremes [60] [55].
Q3: How should we respond to a temperature excursion for a material without a defined stability profile?
- Isolate the material and consult the supplier or literature for stability data. If no information exists, assume the material is compromised and do not use it for critical experiments. Conduct a small-scale viability test if possible, but err on the side of caution to protect research integrity [55].
Q4: What is the purpose of "Preconditioning" in passive shipping systems?
- Preconditioning is the process of bringing refrigerant packs (like gel packs or PCMs) to the precise required temperature before packing the shipment. This ensures the system starts at its designed thermal capacity and maintains the correct temperature for the intended duration [55].
Q5: What are the key regulatory frameworks governing temperature-controlled shipments?
- Key regulations include:
- Good Distribution Practices (GDP): Guidelines for the proper distribution of pharmaceuticals [57] [61].
- IATA Temperature Control Regulations (TCR): Specific rules for shipping temperature-sensitive goods by air [62].
- Food Safety Modernization Act (FSMA): U.S. law focusing on the safe transportation of food products [57] [61].
Standardized Temperature Ranges
The following table defines the standard temperature ranges used for classifying and handling temperature-sensitive research materials.
| Category | Temperature Range | Common Applications & Examples |
|---|---|---|
| Cryogenic | Below -150°C to -195.8°C [60] [55] | Storage and shipment of stem cells, genetic materials, and sensitive biological samples using liquid nitrogen [61] [55]. |
| Deep Frozen | Below -30°C ( -22°F) [61] | Specialized medical samples, certain biologics [61]. |
| Frozen | -20°C to -15°C [55] | Many vaccines, biological samples, frozen foods [57] [55]. |
| Refrigerated | 2°C to 8°C (36°F to 46°F) [57] [61] [55] | Vaccines, biologics, many pharmaceuticals, fresh produce [57] [61]. |
| Controlled Room Temperature | 15°C to 25°C (59°F to 77°F) [55] | Some pharmaceuticals, chemicals, and products that must avoid temperature extremes [60] [55]. |
| Cool/Ambient | 8°C to 25°C (46°F to 77°F) [57] | Flowers, snacks, and less temperature-sensitive chemicals [57]. |
Experimental Protocol: Validating a Passive Shipping Configuration
This protocol outlines the methodology for testing and validating a passive insulated shipper to ensure it maintains the required temperature range for a specified duration.
1.0 Objective To empirically verify that a specific passive shipping system (insulated container + refrigerants) can maintain a payload within 2°C to 8°C for a minimum of 48 hours under simulated summer conditions.
2.0 Materials and Equipment (Research Reagent Solutions)
| Item | Function |
|---|---|
| Validated Temperature Data Loggers (≥3 per test) | To continuously record temperature inside the package. Use high-accuracy, calibrated devices [59]. |
| Insulated Shipper | The container being validated (e.g., expanded polystyrene, polyurethane). |
| Phase Change Materials (PCMs) or Gel Packs | Refrigerants that absorb/release heat at specific temperatures to maintain a stable thermal environment [56] [61]. |
| Thermal Chamber/Environmental Chamber | To expose the test package to a controlled, elevated ambient temperature (e.g., +35°C or +40°C) [55]. |
| Dummy Payload | A simulated product with thermal mass and properties equivalent to the actual shipment contents. |
3.0 Methodology
- Preconditioning: Activate the PCMs or gel packs by conditioning them to the specified starting temperature (e.g., freeze at -20°C or refrigerate at +5°C) for at least 24 hours [55].
- Assembly:
- Place the preconditioned PCMs/gel packs into the shipper according to the manufacturer's configuration.
- Place the dummy payload and at least three pre-activated data loggers into the primary payload area. Position loggers to monitor the most vulnerable locations (top, center, bottom).
- Thermal Challenge:
- Close and seal the shipper.
- Place the assembled unit in a thermal chamber pre-set to the challenge temperature (e.g., +35°C).
- Maintain the chamber temperature for the entire test duration (48 hours or more).
- Data Collection:
- Upon completion of the test period, retrieve the shipper and immediately download data from the loggers.
- The validation is successful if all data loggers show the payload temperature remained within the 2°C to 8°C range for the entire 48 hours.
4.0 Documentation
- The validation report must include a temperature graph from all loggers, details of the packaging configuration, and a statement of pass/fail against the acceptance criteria [55].
Cold Chain Workflow
The diagram below illustrates the critical control points in a temperature-controlled logistics workflow, from storage to final delivery.
Cold Chain Integrity Pathway
The Scientist's Toolkit: Essential Materials for Temperature-Controlled Logistics
| Tool/Material | Function |
|---|---|
| Phase Change Materials (PCMs) | Substances that absorb/release heat at specific temperatures to maintain a stable thermal environment inside a package, often more precise than gel packs [56] [61]. |
| IoT-Enabled Data Loggers | Devices that track and transmit temperature and location data in real-time, allowing for immediate intervention during excursions [56] [57]. |
| Insulated Shippers | Containers with high thermal resistance that minimize heat transfer between the internal payload and the external environment [61] [55]. |
| Dry Ice | Solid carbon dioxide (-78.5°C) used as a cooling agent for shipping products requiring ultra-low or cryogenic temperatures [61] [55]. |
| Thermal Pallet Covers | Large insulated covers used to protect palletized goods from temperature fluctuations during temporary storage or airport tarmac delays [60]. |
| Validation Protocol | A formal document detailing the test methodology for proving that a packaging system maintains required temperatures under specific conditions [55]. |
Beyond the Basics: Identifying Pitfalls and Implementing Proactive Solutions
Troubleshooting Guides
Guide 1: Troubleshooting Hemolysed Samples
Problem: Sample shows pink/red plasma after centrifugation, indicating hemolysis. Question: What are the primary causes and solutions for in vitro hemolysis during blood collection?
In vitro hemolysis, the rupture of red blood cells after collection, is a major cause of sample rejection and can alter test results for potassium, phosphate, magnesium, aspartate aminotransferase, and lactate dehydrogenase [63]. Over 98% of hemolysis identified in laboratory samples is due to in vitro rupture of cells [63].
- Probable Cause 1: Traumatic venipuncture or incorrect needle size.
- Solution: Use an appropriately sized needle (19-22 gauge is recommended for coagulation samples to ensure blood flows quickly and evenly) and avoid probing the vein [64] [63].
- Probable Cause 2: Forcing blood from a syringe through a needle.
- Solution: If using a syringe, transfer blood gently without a needle attached and apply minimal vacuum [63].
- Probable Cause 3: Vigorous handling or shaking of collection tubes.
- Solution: Gently invert tubes according to the manufacturer's instructions immediately after collection. Never shake tubes [64] [63].
- Verification Protocol: Document the venipuncture technique, needle gauge, and tube handling procedures. Visually inspect plasma post-centrifugation.
Guide 2: Troubleshooting Clotted Samples
Problem: Blood has clotted in the collection tube, making it unsuitable for analysis. Question: Why is a sample clotted, and how can this be prevented, especially in sodium citrate tubes?
Clotted samples are particularly common in neonatal and pediatric settings [64]. For sodium citrate tubes, clotting is often due to an incorrect ratio of blood to anticoagulant.
- Probable Cause 1: Underfilled blue-top sodium citrate tube.
- Solution: Ensure the vacuum tube is filled to at least 90% of its capacity to maintain the critical 9:1 blood-to-anticoagulant ratio. Do not combine two partially filled tubes [64].
- Probable Cause 2: Inadequate or delayed mixing after collection.
- Solution: Gently mix the tube with the anticoagulant immediately and thoroughly after collection [64].
- Probable Cause 3: Traumatic venipuncture releasing tissue factor.
- Solution: Avoid probing the vein with the needle, as this causes vascular injury and may initiate clotting [64].
- Verification Protocol: Visually check for clots before processing. Confirm tube fill volume and mixing practices.
Guide 3: Troubleshooting Sample Processing Delays
Problem: Delays between sample collection and processing/analysis. Question: What are the impacts of processing delays, and how can they be mitigated?
Processing delays can compromise sample integrity. For coagulation testing, delays can affect platelet activity and test results.
- Probable Cause 1: Long transport times to the laboratory or between sites.
- Solution: Implement and follow written procedures for maximum allowable time from collection to processing and plasma freezing [64].
- Probable Cause 2: Inefficient sample tracking and workflow.
- Solution: Use a digital sample tracking system to monitor a sample's location and status in real-time, reducing the risk of misplacement and delays [65].
- Probable Cause 3: Improper temporary storage conditions before processing.
- Solution: Define and validate acceptable temporary storage conditions (e.g., room temperature) for different sample types. Consider using sample stabilizers that allow for room-temperature storage and handling [66].
- Verification Protocol: Record the time of collection, receipt, and processing for all samples. Audit workflows for bottlenecks.
Frequently Asked Questions (FAQs)
FAQ 1: What is the recommended order of draw for sample collection to prevent cross-contamination? Following the correct order of draw is critical to prevent cross-contamination between samples, especially from anticoagulants like EDTA [63]. A typical recommended order is provided in the table below.
FAQ 2: Why is centrifugation critical for coagulation samples, and what are the specific requirements? Coagulation testing requires platelet-poor plasma, defined as a platelet count of <10,000/µL, which is essential for obtaining accurate frozen plasma aliquots [64]. Centrifugation must not be performed in refrigerated centrifuges, and the procedure must be validated for each centrifuge model to ensure the correct speed (RPM/g-force) is achieved [64].
FAQ 3: Beyond hemolysis and clotting, what other pre-analytical variables significantly impact test results? Several other factors are important, including patient posture, fasting status, circadian rhythms, and medications or supplements like biotin [63]. Patient posture can affect analyte concentrations by up to 10%, and biotin can interfere with immunoassays, requiring a 1-week washout before testing [63].
FAQ 4: How common are pre-analytical errors? Errors during the pre-analytical phase are very common, accounting for 46% to 68% of all errors in the testing cycle [63]. One estimate specific to coagulation samples suggests pre-analytical errors occur in as many as 5% of all blood collections [64].
The table below summarizes key quantitative data related to pre-analytical variables.
Table 1: Key Pre-analytical Specifications and Error Rates
| Variable | Specification / Rate | Impact / Note |
|---|---|---|
| Pre-analytical Errors | 46-68% of all testing errors [63] | Most common phase for errors. |
| Coagulation Sample Errors | ~5% of collections [64] | Varies by medical discipline. |
| Needle Gauge | 19-22 gauge [64] | Ensures proper blood flow. |
| Sodium Citrate Fill Volume | ≥90% [64] | Critical for 9:1 blood-to-anticoagulant ratio. |
| Platelet-Poor Plasma | <10,000/µL [64] | Required for coagulation testing. |
| Biotin Washout Period | ≥1 week [63] | Prevents immunoassay interference. |
Experimental Protocols
Protocol 1: Method Comparison for Point-of-Care Hemoglobin Testing
This protocol is adapted from a 2025 study evaluating a point-of-care hemoglobinometer in feline samples, demonstrating a method comparison approach applicable to evaluating new pre-analytical techniques or devices [67].
Objective: To evaluate the agreement, accuracy, and precision of a point-of-care device (HemoCue Hb 201+) against a reference laboratory analyzer (ADVIA 2120) and assess the impact of potential interferents [67].
Materials:
- Blood samples in EDTA tubes.
- HemoCue Hb 201+ analyzer and its microcuvettes.
- Reference hematology analyzer (e.g., ADVIA 2120).
- Pipette (20 µL) and hydrophobic surface (e.g., Parafilm).
Methodology:
- Sample Collection: Collect venous blood into EDTA tubes. Record the venipuncture site [67].
- Reference Analysis: Measure the hemoglobin concentration using the reference laboratory analyzer first [67].
- Point-of-Care Analysis:
- After reference analysis, gently invert the EDTA tube 8-10 times [67].
- Using a pipette, collect three 15 µL aliquots and eject each onto a hydrophobic surface [67].
- Aspirate each drop into a microcuvette and insert it into the HemoCue analyzer within 10 seconds of aspiration. Record the result of each replicate [67].
- Data Analysis:
- Assess agreement and systematic bias using statistical methods like Passing-Bablok regression and Bland-Altman analysis [67].
- Calculate precision between replicate measurements using the intraclass correlation coefficient (ICC) [67].
- Compare the performance of the device in the presence of potential interferents (e.g., lipemia, azotemia) using statistical tests like the Wilcoxon rank-sum test [67].
Protocol 2: Validation of Centrifugation Procedures for Coagulation Samples
Objective: To establish and validate a standardized centrifugation protocol to consistently generate platelet-poor plasma (<10,000/µL platelets) for coagulation assays.
Materials:
- Sodium citrate blood samples.
- Laboratory centrifuge(s).
- Hemocytometer or hematology analyzer for platelet counting.
Methodology:
- Procedure Definition: Define the proposed centrifugation steps, including speed (RPM/g-force), duration, and temperature (e.g., room temperature, not refrigerated) [64].
- Sample Processing: Centrifuge a set of samples using the defined procedure.
- Quality Control:
- After centrifugation, carefully remove the plasma supernatant.
- Determine the platelet count in the plasma using a hemocytometer or a hematology analyzer [64].
- Validation Criteria: The procedure is considered validated only if the platelet count in the plasma is consistently below the target of 10,000/µL across multiple sample runs and using different centrifuges in the laboratory [64].
- Documentation: Create written procedures for the validated protocol to be followed by all personnel.
Workflow and Relationship Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Managing Pre-analytical Variables
| Item | Function |
|---|---|
| Stabilized Blood Collection Tubes | Tubes with preservatives that stabilize nucleic acids (e.g., cfDNA, cfRNA) or cells, enabling room-temperature storage and transport, thus mitigating pre-analytical variables associated with processing delays and temperature control [66]. |
| Standardized Sodium Citrate Tubes (3.2%) | Blue-top tubes containing 3.2% sodium citrate as an anticoagulant. They require a precise 9:1 blood-to-anticoagulant ratio for accurate coagulation testing [64]. |
| Polypropylene Secondary Tubes | Non-activating plastic tubes used for aliquoting plasma for coagulation assays. Materials like polystyrene can activate the coagulation cascade and should be avoided [64]. |
| HemoCue Hb 201+ System | A point-of-care hemoglobinometer that requires only a 10 μL blood drop, providing results within 60 seconds. This can reduce iatrogenic blood loss from frequent testing [67]. |
| Barcoded Tube Labels & Tracking Software | Standardized labels and integrated digital systems (e.g., QISS LAB) to prevent misidentification, track samples across the workflow, and maintain chain of custody, addressing common challenges like mislabeling and sample loss [65]. |
Within the critical framework of standardizing sample collection and storage research, maintaining sample integrity is a foundational requirement for reproducible science. For researchers and drug development professionals, sample degradation poses a significant risk to data validity, potentially compromising diagnostic accuracy, therapeutic efficacy studies, and fundamental research outcomes. This guide addresses two prevalent challenges—managing light-sensitive samples and preventing damage from repeated freeze-thaw cycles—by providing targeted troubleshooting and evidence-based protocols to safeguard your valuable samples.
FAQ: Understanding Sample Degradation
What are the primary mechanisms of sample degradation during freeze-thaw cycles?
Repeated freezing and thawing damages samples through several physical and biochemical mechanisms [68]:
- Ice Crystal Formation: Rapid freezing leads to ice crystal formation that can pierce and rupture cell membranes and organelle structures. Slow cooling, while reducing crystals, creates an osmotic imbalance that also causes cell rupture [68].
- Freeze Concentration: As ice forms, salts, proteins, and other solutes in the buffer become concentrated in the remaining liquid, creating a stressful environment that can denature proteins and destabilize biomolecules [68].
- Oxidative Stress: The freeze-thaw process can generate reactive oxygen species (ROS), leading to oxidative damage such as DNA double-strand breaks (indicated by phosphorylated H2AX) and lipid peroxidation [68].
Why are some samples sensitive to light, and what are the consequences?
Light-sensitive samples, such as those containing certain vitamins, neurotransmitters, or photosensitive chemicals, can undergo photodegradation. When exposed to light, especially ultraviolet wavelengths, the energy absorbed can break chemical bonds, alter molecular structures, and form reactive species. This leads to:
- Loss of analyte activity or function.
- Formation of degradation products that interfere with assays.
- Inconsistent and unreliable experimental results due to uncontrolled variable introduction [69].
How does sample type influence its sensitivity to freeze-thaw cycles?
Biomolecule stability during freeze-thaw varies significantly. Peer-reviewed research provides the following insights [70]:
| Biomolecule | Impact of Repeated Freeze-Thaw Cycles | Key Findings |
|---|---|---|
| RNA | High Impact | Integrity is significantly degraded; impact varies by tissue type. Gene expression results are altered, particularly when measured by absolute quantification [70]. |
| Protein | Low to Moderate Impact | No obvious degradation observed after multiple cycles. However, functional assays (e.g., kinetics) may be affected by protein unfolding [70] [68]. |
| DNA | Low Impact | No obvious degradation observed after multiple cycles. However, minor damage can affect downstream PCR [70] [68]. |
What are the best practices for aliquoting samples to prevent freeze-thaw degradation?
The core best practice is to divide samples into single-use aliquots immediately after processing [68]. This prevents the need to repeatedly thaw and refreeze the main stock.
- Volume: Aliquot a volume that is typically used in a single experiment or assay.
- Containers: Use sterile, low-protein-binding vials or cryotubes.
- Documentation: Label each aliquot clearly with a unique identifier and track the number of freeze-thaw cycles for each vial in your Laboratory Information Management System (LIMS) [7].
Beyond aliquoting, what additives can protect samples during freezing?
Cryoprotectants are essential additives that mitigate freezing damage. The two main classes are [68]:
| Cryoprotectant Type | Examples | Mechanism of Action |
|---|---|---|
| Intracellular (Penetrating) | DMSO, Glycerol, Ethylene Glycol | Penetrate the cell membrane to prevent intracellular ice crystal formation, thereby reducing membrane rupture. |
| Extracellular (Non-Penetrating) | Sucrose, Dextrose, Polyvinylpyrrolidone | Remain outside the cell, reducing the hyperosmotic stress and concentration of solutes during freezing. |
Troubleshooting Guides
Problem 1: Unexpected Results from a Previously Stable Sample
This is a common issue often traced back to cumulative, unseen sample degradation.
Investigation and Resolution Steps:
Audit the Sample History: Check the sample's chain of custody and storage records.
- Freeze-Thaw Count: Determine how many times the sample has been thawed and re-frozen. The maximum tolerated cycles depend on the analyte [70].
- Light Exposure: Review if the sample was exposed to light during handling or analysis. Implement the use of amber or opaque vials for all storage and handling steps [71].
- Storage Temperature Logs: Verify that storage freezers and refrigerators have maintained their target temperatures without excursions. Ensure monitoring systems with alerts are in place [72].
Run Quality Control Assays:
- For RNA, check the RNA Integrity Number (RIN) using a bioanalyzer. Degradation is a key risk [70].
- For proteins, use techniques like SDS-PAGE to look for smearing or unexpected bands indicating breakdown.
- Always include control samples of known quality with each batch of analysis for comparison [71].
Review and Update SOPs:
- Ensure Standard Operating Procedures (SOPs) explicitly detail handling practices for light-sensitive and temperature-critical samples, including the use of specific cryoprotectants and light-blocking containers [72].
Problem 2: Despite Aliquoting, Sample Activity is Lost After Thawing
If degradation occurs even in single-use aliquots, the freezing or thawing process itself may be flawed.
Investigation and Resolution Steps:
Optimize the Thawing Protocol:
Re-evaluate Your Cryoprotectant:
Implement Redundant Storage:
- Split your aliquots and store them in separate freezers or, ideally, an off-site backup facility. This protects against catastrophic loss from equipment failure [72].
Experimental Protocols
Protocol 1: Systematic Evaluation of Freeze-Thaw Cycle Impact on Biomolecule Integrity
This protocol provides a methodology to empirically determine the stability of your specific samples, supporting the standardization of storage practices.
1. Objective: To quantify the degradation of DNA, RNA, or protein in a specific sample matrix (e.g., plasma, tissue homogenate) across multiple controlled freeze-thaw cycles.
2. Experimental Design:
- Sample Preparation: Pool a large volume of your sample matrix and split it into multiple identical aliquots.
- Control Group: A set of aliquots that is analyzed immediately without freezing (Baseline, T0).
- Test Groups: The remaining aliquots are subjected to 1, 3, 5, and 10 complete freeze-thaw cycles.
- Freezing: Snap-freeze aliquots in a consistent manner (e.g., liquid nitrogen or -80°C freezer).
- Thawing: Thaw groups consistently using either the "on ice" or "room temperature" method to compare these conditions [70].
3. Data Collection and Analysis:
- Quantitative Analysis: Use appropriate assays (e.g., qPCR for DNA/RNA, Bradford/BCA for protein concentration) to measure yield and integrity after each cycle.
- Integrity Assessment: Analyze RNA integrity with a bioanalyzer (RIN) or protein integrity with SDS-PAGE/Western Blot.
- Statistical Analysis: Compare results from each cycle group to the baseline control to determine the point of significant degradation.
The following workflow outlines the experimental procedure:
Protocol 2: Validating a Light Protection Workflow for Photosensitive Analytes
This protocol establishes a standardized procedure to ensure light-sensitive analytes are protected throughout an experiment.
1. Objective: To confirm that implemented light-protection measures effectively prevent the photodegradation of a target analyte.
2. Experimental Design:
- Sample Preparation: Split a homogeneous sample into two sets.
- Control Group (Light-Protected): Wrapped in aluminum foil or stored in amber vials. All processing steps are performed under minimal or yellow/red safelight conditions.
- Test Group (Light-Exposed): Intentionally exposed to standard laboratory lighting (including UV-containing ambient light) for defined durations during handling and storage.
- Storage: Both groups are stored under otherwise identical conditions (e.g., -80°C).
3. Data Collection and Analysis:
- Quantitative Analysis: Measure the concentration of the target analyte in both groups at various time points.
- Degradation Product Analysis: Use chromatography (e.g., HPLC) to detect and quantify the formation of any light-induced degradation products.
- Functional Assay: If applicable, perform a functional assay (e.g., enzyme activity) to compare the activity between the two groups.
The logical relationship of the validation procedure is as follows:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are critical for implementing the strategies discussed in this guide.
| Item | Specific Function | Application Notes |
|---|---|---|
| DMSO (Dimethyl Sulfoxide) | Intracellular cryoprotectant; prevents ice crystal formation. | Common concentration 5-10%. Cytotoxic at room temperature; remove post-thaw for cell cultures [68]. |
| Glycerol | Intracellular cryoprotectant; reduces freezing point. | Often used at 5-20%. Less toxic than DMSO for some applications [68]. |
| Sucrose | Extracellular cryoprotectant; buffers osmotic pressure. | Used as a non-penetrating agent to stabilize proteins and membranes [68]. |
| Amber/Opaque Vials | Blocks light exposure to prevent photodegradation. | Essential for storage of all light-sensitive samples (e.g., vitamins, riboflavin) [71] [69]. |
| RNA Stabilization Reagents | (e.g., RNAlater) Immediately inactivate RNases upon sample collection. | Preserves RNA integrity in tissues and cells before nucleic acid extraction [71]. |
| Protease Inhibitor Cocktails | Prevent protein degradation by inhibiting proteases. | Added to lysis buffers and sample solutions during protein isolation [73]. |
| Barcoded Cryogenic Vials | Enable unique sample identification and tracking in a LIMS. | Critical for maintaining chain of custody and preventing handling errors [7] [72]. |
Table of Contents
- Understanding Temperature Excursions and Their Impact
- Developing a Standard Operating Procedure for Excursion Response
- Troubleshooting Guides and FAQs
- Experimental Protocols for Excursion Impact Assessment
- The Scientist's Toolkit: Essential Research Reagents and Materials
Understanding Temperature Excursions and Their Impact
A temperature excursion is defined as an event in which a time–temperature-sensitive product is exposed to temperatures outside its prescribed storage or transport range [74] [75]. In the context of biomedical research, this "product" can include biological samples, reagents, and experimental drugs. Industry analysis suggests that up to 20% of temperature-sensitive healthcare products are damaged during transit due to poor cold chain management, highlighting the prevalence of this issue [74] [75].
The impact on research integrity can be severe, potentially compromising the stability, potency, and overall integrity of biological materials [74]. For example, a 2025 study on blood-based biomarkers for Alzheimer's disease found that pre-analytical variations like storage and centrifugation delays significantly impact biomarker levels [76]. The table below summarizes the sensitivity of various biomarkers to temperature excursions, based on empirical findings.
Table 1: Sensitivity of Neurological Blood-Based Biomarkers to Pre-analytical Variations [76]
| Biomarker | Sensitivity to Temperature Excursions and Delays | Key Findings |
|---|---|---|
| Amyloid-beta (Aβ42, Aβ40) | High | Most sensitive; levels decline by >10% under storage and centrifugation delays, more steeply at room temperature (RT) vs. 2°C–8°C. |
| Neurofilament Light (NfL) | Medium | Levels increase by >10% upon storage at RT or -20°C. |
| Glial Fibrillary Acidic Protein (GFAP) | Medium | Levels increase by >10% upon storage at RT or -20°C. |
| Phosphorylated Tau (pTau) | Low (Highly Stable) | pTau isoforms (especially pTau217) demonstrate high stability across most pre-analytical variations. |
Developing a Standard Operating Procedure for Excursion Response
A robust SOP is the cornerstone of an effective excursion management plan. It ensures a consistent, defensible, and rapid response, which is crucial for both research validity and regulatory compliance [74] [75]. The following workflow outlines the key stages of a comprehensive response procedure.
The core components of a comprehensive SOP should include [74] [75]:
- Immediate Quarantine: Physically isolate the affected samples or materials to prevent their unintended use in experiments.
- Detailed Recording: Document the exact time, duration, magnitude of the temperature deviation, and handling conditions.
- Notification Protocol: Define clear escalation paths to immediately alert the Quality Assurance (QA) unit, principal investigator, and senior management.
- Impact Assessment: Base the decision to release, recondition, or reject the material on scientific evidence, such as stability data and excursion studies [74]. This is critical for maintaining research standardization.
- Root Cause Analysis (RCA): Investigate whether the failure was due to equipment malfunction, packaging failure, human error, or an external factor like a transportation delay [74] [75].
- Corrective and Preventive Actions (CAPA): Implement measures to prevent recurrence, which may include equipment repair, SOP updates, staff retraining, or improving packaging protocols [74] [75].
Troubleshooting Guides and FAQs
Q1: We experienced a brief power outage, and our -80°C freezer temperature rose to -65°C for 45 minutes. What should we do with the biological samples inside? A1: Immediately quarantine the samples and label them as "Under Investigation." Consult any available stability data for the specific analytes stored within (e.g., refer to Table 1). For sensitive biomarkers like Amyloid-beta, even short excursions can be detrimental [76]. The final decision to use or discard the samples should be documented along with the justification, as part of your laboratory's quality management system [44].
Q2: A shipment of research blood samples arrived at our lab 6 hours later than scheduled, and the temperature logger shows a 2-hour excursion to 25°C. How do we assess the impact? A2: This is a common pre-analytical challenge. Follow these steps:
- Quarantine & Log: Isolate the shipment and record all data from the logger.
- Assess Sample Type: Determine the stability of your target analytes. As shown in Table 1, plasma Aβ42 and Aβ40 are highly sensitive to such delays at room temperature, while pTau217 is more stable [76].
- Run Quality Controls: If possible, perform a quality control assay on a subset of samples to check the integrity of key biomarkers.
- Document & CAPA: Document the event and its resolution. A CAPA might involve revising the shipping protocol to require colder PCMs or a different courier [74] [77].
Q3: Our laboratory refrigerator door was left ajar overnight, causing a temperature excursion to 10°C. How can we prevent this from happening again? A3: This is typically addressed through CAPA. Corrective actions include servicing the refrigerator and calibrating its thermostat. Preventive actions are key [74] [75]:
- Training: Reinforce SOPs for all staff regarding proper door closure.
- Technology: Invest in real-time temperature monitoring systems with audible door-open alerts and SMS/email notifications for excursions [77].
- Procedure: Implement a daily check-off sheet for laboratory equipment.
Experimental Protocols for Excursion Impact Assessment
For novel analytes with unknown stability, conducting a structured excursion impact study is essential for standardizing research protocols and making evidence-based decisions after an incident.
Objective: To determine the stability of a target analyte (e.g., a specific protein or nucleic acid) under defined temperature excursion conditions.
Methodology:
- Sample Preparation: Split a large, homogeneous pool of the biological sample (e.g., plasma, serum, tissue homogenate) into multiple aliquots.
- Control Group: Immediately freeze a set of aliquots at the recommended long-term storage temperature (e.g., -80°C). These serve as baseline controls.
- Excursion Simulation: Expose the remaining aliquots to different temperature conditions (e.g., Room Temperature: 25°C, Refrigerated: 4°C, Freezer: -20°C) for varying durations (e.g., 2, 6, 24 hours).
- Analysis: After the excursion period, analyze all aliquots (including controls) using your standard assay (e.g., ELISA, Simoa, PCR). Measure the concentration or activity of the target analyte.
- Data Interpretation: Compare the results from the excursion samples to the baseline controls. A significant change (e.g., >10% deviation) indicates susceptibility to the tested conditions [76].
The workflow for this experiment is designed to systematically test stability.
The Scientist's Toolkit: Essential Research Reagents and Materials
Proper management of temperature-sensitive materials is fundamental to standardization. The following table details key items and their handling requirements.
Table 2: Key Research Reagent Solutions and Sample Handling Specifications
| Item / Material | Function in Research | Typical Storage Temp. | Critical Handling Notes |
|---|---|---|---|
| Blood Collection Tubes | Sample acquisition for biomarker analysis | Varies by type | Primary collection tube type can alter biomarker levels by >10%; must be standardized [76]. |
| Plasma/Serum Samples | Source material for biomarker measurement (e.g., Aβ, pTau, NfL) | -80°C for long term | Plasma Aβ42/Aβ40 are highly sensitive to delays in processing/freezing; pTau217 is more stable [76]. |
| Enzymes (e.g., Restriction Enzymes, Polymerases) | Catalyzing biochemical reactions | -20°C | Frequent short temperature excursions during use can reduce activity over time. |
| Reference Standards & Calibrators | Quantification and calibration of assays | As specified by mfr. | Integrity is paramount; excursions can invalidate entire assay runs and standard curves. |
| Phase Change Materials (PCMs) | Thermal buffer for shipping/storing samples | Conditioned to target temp | Validated packaging systems using PCMs are critical for mitigating excursion risks during transport [74] [77]. |
| Real-Time Data Loggers | Monitoring temperature during storage/transport | N/A | Provide auditable data for excursions; should have alert triggers for breaches [77]. |
Frequently Asked Questions (FAQs)
Q1: What are the most critical checks to perform upon sample receipt? The most critical verification checks are often referred to as the "three verifications": sample identity (matching patient/subject identifiers on the sample tube and accompanying paperwork), sample integrity (checking for leaks, breaks, or visible signs of degradation like hemolysis), and documentation completeness (ensuring the requisition form is complete and all necessary sample information is provided) [63].
Q2: What are common reasons for rejecting a sample at receipt? Common reasons for sample rejection include [63]:
- Inadequate Sample Volume: Insufficient quantity for the requested tests.
- Hemolysis: Visible hemolysis in serum or plasma samples, which can interfere with many assays.
- Incorrect Sample Type: Use of an inappropriate collection tube (e.g., EDTA plasma instead of serum).
- Missing or Mismatched Information: Discrepancies between the sample label and the requisition form, or missing essential patient data.
- Improper Transport Conditions: Evidence of the sample being exposed to incorrect temperatures or excessive delay during transport.
Q3: How can we improve traceability during the sample receipt process? Implementing a Laboratory Information Management System (LIMS) is the most effective strategy. Upon receipt, each sample should be scanned (using barcodes or RFID tags) into the LIMS, which automatically logs its arrival, assigns a unique internal tracking ID, and links it to all associated metadata. This creates a secure, auditable chain of custody from receipt to disposal [14] [78].
Q4: What specific documentation is required for samples used in research? For research samples, documentation must comply with ethical and regulatory standards. This includes proof of Institutional Review Board (IRB) approval for the study and documented informed consent from all participants. The IRB ensures that appropriate steps are taken to protect the rights and welfare of the human subjects involved in the research [79] [80].
Troubleshooting Guides
Common Pre-Analytical Errors and Solutions
| Problem | Possible Cause | Corrective & Preventive Actions |
|---|---|---|
| Sample Hemolysis [63] | - Vigorous shaking of tubes- Using a needle that is too small- Difficult venipuncture | - Gently invert tubes 5-10 times; do not shake.- Use appropriate needle size (e.g., 21-22 gauge).- Ensure alcohol at puncture site has dried completely. |
| Insufficient Sample Volume [63] | - Inaccurate blood draw- Partial tube draw | - Train phlebotomists on proper fill volumes.- Verify tube fill levels upon collection and receipt. |
| Incorrect Sample Type [63] | - Wrong tube used for test ordered- Cross-contamination from tube additives | - Maintain updated collection guides per test.- Adhere to the standard order of draw: Blood cultures → Sodium citrate → Serum gel → Heparin → EDTA [63]. |
| Missing/Mismatched ID [63] | - Tubes labeled before collection- Transcription errors | - Label tubes after collection, in the presence of the patient.- Use at least two patient identifiers (e.g., name, DOB). |
| Degraded Samples [44] [63] | - Delayed transport- Incorrect storage temperature | - Establish and monitor strict transport timelines.- Use validated temperature-monitored shipping containers. |
Sample Acceptance and Rejection Workflow
The following diagram illustrates the logical decision process for verifying samples upon receipt in the laboratory.
Experimental Protocols for Sample Verification
Detailed Protocol: Initial Sample Triage and Registration
Objective: To establish a standardized, auditable procedure for the initial receipt, verification, and logging of incoming samples in a research or clinical laboratory setting, ensuring data integrity and sample traceability.
Materials:
- Personal Protective Equipment (PPE)
- Dedicated sample receipt area
- Cooler or insulated container for transported samples
- Barcode scanner
- Computer with access to LIMS
- Permanent ink pen
- Biohazard bags and sharps container
Methodology:
- Safety Precautions: Treat all samples as potentially infectious. Wear appropriate PPE (lab coat, gloves, safety glasses).
- Unpacking: Retrieve samples from the transport container. Immediately note the condition of the shipping container and any temperature monitors. Record the time and date of receipt.
- Initial Inspection: Visually inspect each sample for container integrity (cracks, leaks), correct fill volume, and presence of clots (if applicable).
- Documentation Review: Cross-reference the sample tubes with the accompanying requisition form or sample manifest. Confirm that at least two patient/subject identifiers (e.g., name, date of birth, subject ID) match exactly.
- LIMS Logging:
- Scan the barcode on each sample tube into the LIMS. If no barcode exists, assign one and label the tube.
- The LIMS will automatically check for duplicates and link the sample to existing subject data.
- Manually enter or verify critical metadata in the LIMS: sample type (e.g., whole blood, serum, plasma), collection date and time, and tests requested.
- Disposition:
- Acceptable Samples: Place them in a designated holding area at the appropriate storage temperature (e.g., 4°C, -20°C) pending processing/analysis.
- Unacceptable Samples: Do not process. Log the reason for rejection in the LIMS and physically quarantine the sample. Follow the notification protocol to inform the submitter.
Quality Control: Perform periodic audits of the receipt process to ensure compliance with the protocol and accuracy of data entry into the LIMS [44].
Sample Management and Storage Workflow
After acceptance, samples often enter a defined workflow for processing and storage. The following diagram outlines a standard pathway for managing samples destined for biobanking or long-term storage.
The Scientist's Toolkit: Research Reagent & Material Solutions
The following table details key materials and technologies essential for modern, standardized sample management, from receipt to storage.
| Item | Function & Importance in Standardization |
|---|---|
| Laboratory Information Management System (LIMS) | A software-based system that tracks samples and associated data throughout their lifecycle. It is the core tool for standardizing data entry, ensuring traceability, and managing storage inventory [14] [78]. |
| Barcoded Tubes & Labels | Pre-printed, unique identifiers that minimize transcription errors. When scanned, they automatically link the physical sample to its digital record in the LIMS, forming the foundation of sample identity verification [14]. |
| Automated Sample Storage Systems | Robotic systems that provide high-density, temperature-controlled storage (e.g., -80°C, liquid nitrogen). They standardize storage conditions, minimize freeze-thaw cycles by robotic retrieval, and integrate with LIMS for precise location tracking [14] [78]. |
| Temperature Monitoring Devices | Data loggers and continuous monitoring systems that provide validated records of storage and transport conditions. This documentation is critical for proving sample integrity and compliance with pre-analytical standards [44] [63]. |
| Standardized Collection Kits | Pre-assembled kits containing the correct tubes, needles, and stabilizers for specific sample types and tests. They reduce pre-analytical variability by ensuring consistent collection materials and protocols across different collection sites [63]. |
Within the critical field of sample management, the aliquotting process—dividing a primary sample into multiple smaller, identical portions—represents a key risk point where errors can compromise entire studies. For precious samples and high-throughput laboratories, these risks are magnified, making standardized, efficient workflows not just beneficial but essential. Proper aliquotting protects the integrity of the original sample by minimizing repeated freeze-thaw cycles, enables parallel testing for multiple analytes, and facilitates safe distribution to collaborating laboratories [81] [15]. This guide, framed within the broader context of standardizing sample collection and storage research, provides detailed troubleshooting and procedural protocols to safeguard sample integrity from collection to analysis.
Core Principles and Preparation for Aliquotting
Essential Pre-Aliquotting Considerations
Before beginning the aliquotting process, several key factors must be addressed to ensure success:
- Sample Stability: The stability of the analyte in its matrix under the planned processing conditions (e.g., temperature, time) must be known and respected [15].
- Labeling and Identification: Every aliquot must be labeled with a unique identifier that links it to the primary sample and the original donor or source. Handwritten labels should be avoided in favor of printed labels, barcodes, or QR codes to prevent errors [81] [82] [15]. Information should include a unique sample ID, matrix type, date and time of aliquotting, and operator initials.
- Aseptic Technique: Contamination during aliquotting must be prevented by using sterile equipment, wearing appropriate personal protective equipment (PPE), and working in a clean environment [81].
- Container Selection: Choose aliquot containers that are chemically compatible with the sample, leak-proof, and suitable for long-term storage at the required temperatures [81] [83].
The Scientist's Toolkit: Essential Materials for Aliquotting
The following table details key reagents and materials required for efficient and reliable sample aliquotting.
Table 1: Essential Research Reagent Solutions and Materials for Sample Aliquotting
| Item | Function & Importance |
|---|---|
| Sterile Pipette Tips | For accurate liquid transfer; using fresh tips for each sample is critical to prevent cross-contamination [81] [84]. |
| Appropriate Aliquot Tubes/Plates | Receptacles for the aliquoted samples; must be sterile and compatible with sample matrix and storage temperature (e.g., cryogenic vials for -80°C) [81]. |
| Personal Protective Equipment (PPE) | Protects the operator from biohazards and protects the sample from human contamination [81]. |
| Cooling Platform or Chilled Block | Maintains samples at a stable, cold temperature during the aliquotting process to preserve analyte stability. |
| Liquid Waste Container | For safe disposal of used pipette tips and other consumables that contact biological material [84]. |
| Laboratory Information Management System (LIMS) | A digital system for tracking sample identity, location, and chain of custody throughout the process [82] [15] [65]. |
Detailed Experimental Protocol for Manual Aliquotting
This protocol outlines a standardized method for manual aliquotting of liquid samples, such as serum or plasma, from a primary collection tube.
The following diagram visualizes the logical workflow and decision points for the sample aliquotting process.
Step-by-Step Methodology
Preparation:
- Workspace: Disinfect the work surface with 70% ethanol or a suitable disinfectant [81].
- Equipment: Gather all necessary materials (see Table 1). Ensure pipettes are calibrated and functioning correctly. Pre-chill a cooling block or rack to the required temperature (e.g., 4°C).
- Aliquot Tubes: Label all destination aliquot tubes before starting the transfer. Using printed barcode labels is highly recommended [82] [15].
Sample Access:
- Retrieve the primary sample from storage, handling it according to its classification (e.g., biohazard).
- If the sample is frozen, thaw it gently under controlled conditions, ideally on wet ice or in a refrigerator, to maintain stability [20]. Avoid repeated freeze-thaw cycles.
Sample Mixing:
- Once thawed (if applicable) and before pipetting, gently mix the primary sample by inverting the tube 5-10 times. Do not vortex unless the analyte is known to be unaffected by shear stress, as vortexing may denature proteins or disrupt cells.
Aliquot Transfer:
- Place the primary sample and the pre-labeled, chilled aliquot tubes in the chilled rack.
- Using an appropriate volume pipette and a sterile tip, carefully aspirate the target volume from the primary sample. Avoid introducing air bubbles.
- Dispense the liquid into the first aliquot tube. Change the pipette tip before proceeding to the next aliquot to prevent cross-contamination [84].
- Repeat until the required number of aliquots have been created, or the primary sample volume is exhausted (ensuring the minimum required volume for primary storage is maintained).
Post-Aliquotting:
High-Throughput Automation: Using a 96-Channel Workstation
For laboratories processing large volumes of samples, manual aliquotting becomes a bottleneck. Automated workstations dramatically increase efficiency and consistency.
The process for using a 96-channel manual workstation for aliquotting is summarized in the diagram below.
- Calibration and Setup: Calibrate the workstation using calibration fluid according to the manufacturer's manual. Set the desired dispensing volume via the control panel.
- Loading Samples and Tips: Place the primary samples into a suitable source container, like a trough, ensuring even distribution. Carefully attach a fresh set of 96 pipette tips to the pipette head.
- Aspiration and Dispensing: Lower the pipette head into the source trough and activate the aspirate function. Move the head over a 96-well destination plate and activate the dispense function to aliquot the samples.
- Post-Process Handling: Eject the used tips into a waste container. If processing more samples, use a fresh set of tips to prevent cross-contamination.
- Data Management: The 96-well plate must be scanned or its location recorded in the LIMS to link the new aliquots to their source.
Troubleshooting Guide: Common Aliquotting Issues and Solutions
This section addresses specific problems users may encounter during their experiments.
Table 2: Troubleshooting Common Sample Aliquotting Problems
| Problem | Possible Cause | Solution |
|---|---|---|
| Inconsistent Aliquot Volumes | Pipette calibration error; clogged or damaged pipette tip; air bubbles in the tip. | Recalibrate pipette or workstation [84]; check tips for blockages and replace; pre-wet tips and aspirate/dispense slowly to minimize bubbles. |
| Sample Clotting or Precipitation | Incompatible container; improper mixing; sample instability at processing temperature. | Ensure sample is mixed gently but thoroughly before aliquoting; keep samples chilled if necessary; check sample stability specifications. |
| Cross-Contamination Between Aliquots | Reusing pipette tips; aerosol generation; drips from the pipette tip. | Always use a fresh, sterile pipette tip for each sample and each aliquot [81] [84]; avoid splashing; use filter tips for potentially hazardous samples. |
| Leaking or Faulty Tubes | Poor quality tubes; incompatible caps; over-tightening. | Use certified leak-proof tubes; ensure cap O-rings are intact; do not over-tighten caps. |
| Low Sample Recovery (Hold-up Volume) | Significant liquid retained in filter pores or dead volume of container. | Use filter membranes with low hold-up volume (e.g., hydrophilic PVDF or PTFE) [85]; be aware of dead volume when working with very small sample volumes. |
| Analyte Adsorption to Tubes/Filter | Nonspecific binding of analyte (common for proteins/peptides). | Use low-binding plasticware (e.g., polypropylene); for filtration, use PVDF or PES membranes instead of nylon or glass fiber [85]. |
Frequently Asked Questions (FAQs)
Q1: How can I minimize the loss of my precious sample during aliquotting? A1: Use low-retention pipette tips and tubes to reduce surface adsorption. Ensure your equipment is properly calibrated for accurate volume transfer. For very small volumes, account for the "hold-up volume" of your containers and filters. Performing a filter binding investigation during method development is recommended to assess analyte loss [85].
Q2: What is the best way to label my aliquots to prevent errors? A2: Handwritten labels should be avoided. Use printed labels, barcodes, or QR codes, which are less prone to human error and can be read by automated systems [81] [82]. Ensure the label and ink are resistant to the storage conditions (e.g., freezer-safe, alcohol-resistant).
Q3: How many times can I freeze-thaw my sample? A3: The stability of an analyte to freeze-thaw cycles is specific to the sample type and analyte. This should be determined during method validation. As a general rule, repeated freezing and thawing should be minimized, as it can degrade many analytes, including IgM antibodies [20]. Creating single-use aliquots is the best practice.
Q4: Our lab is moving to high-throughput. What are the key considerations for implementing automated aliquotting? A4: Key factors include: 1) Container standardization – a limited range of tube sizes and properly applied labels improves automation reliability [86]; 2) Process volume capacity – know your peak and average specimen volumes to select the right system [86]; and 3) Integration with your LIMS to ensure seamless data tracking and traceability [86] [65].
Q5: Why is maintaining a chain of custody important, and how is it done? A5: The chain of custody documents the complete life cycle of a sample, proving it was handled appropriately and under stable conditions, which is critical for data integrity and regulatory compliance [15]. It is maintained by meticulously recording every sample movement, location change, and storage condition in a system like a LIMS, which provides an audit trail [15] [65].
Ensuring Excellence: Techniques for Quality Assurance and Comparative Analysis
Establishing a Data Quality Assessment Index System
A Data Quality Framework is a technique for measuring and managing data quality within an organization, providing a complete set of principles, processes, and tools to monitor, enhance, and assure data quality across the data lifecycle [87]. For biomedical research focusing on sample collection and storage, implementing such a framework is essential to ensure that data generated from biological specimens is accurate, complete, and reliable, thereby supporting valid scientific conclusions and regulatory compliance [76] [88].
In the context of sample collection and storage research, a robust data quality assessment index system ensures that pre-analytical variables—such as collection tube type, processing delays, and storage conditions—are properly controlled and documented, minimizing variations that could compromise biomarker measurements and research outcomes [76] [44].
Core Components of the Assessment Index System
Fundamental Data Quality Dimensions
The data quality assessment index system for sample collection and storage research should be built upon the following core dimensions, which serve as key metrics for understanding whether data quality processes are effective [87] [89] [90]:
Table 1: Core Data Quality Dimensions for Sample Collection and Storage Research
| Dimension | Description | Research-Specific Importance |
|---|---|---|
| Accuracy | Measure of how well data represents reality [87] | Ensures biomarker measurements reflect true biological values rather than artifacts of handling [76] |
| Completeness | Extent to which expected data is present [87] [89] | Verifies all required sample metadata and processing steps are recorded [44] |
| Timeliness | Data's availability within required timeframe [89] [90] | Critical for time-sensitive processing steps where delays affect sample integrity [76] |
| Consistency | Uniformity of data across different sources or systems [87] [89] | Ensures standardized procedures across multiple collection sites or studies [88] |
| Validity | Conformance to required formats, ranges, or business rules [89] [90] | Confirms data adheres to predefined formats (e.g., sample IDs, measurement units) [91] |
| Uniqueness | Absence of duplicate records [89] [90] | Prevents redundant sample entries while maintaining chain of custody [44] |
specialized Metrics for Biomedical Research
In addition to the standard dimensions, specialized metrics relevant to sample-based research include:
- Pre-analytical Stability: Measures how sample handling variations affect biomarker integrity [76]
- Sample-to-Data Traceability: Tracks the complete lineage from biological specimen to analytical result [44]
- Protocol Adherence Rate: Quantifies compliance with standardized collection and storage procedures [76] [88]
Implementation Methodology
Framework Implementation Workflow
The following diagram illustrates the systematic workflow for implementing the data quality assessment index system in sample collection and storage research:
Assessment Phase Protocol
The initial assessment phase requires these specific methodological steps:
- Source Identification: Document all data sources including laboratory instruments, electronic lab notebooks, and sample tracking systems [87] [90]
- Metadata Specification: Define required sample attributes including donor information, collection timestamp, processing details, and storage conditions [44]
- Data Quality Profiling: Execute automated data profile checks to analyze null values, value distributions, patterns, and outliers in existing sample data [87] [90]
- Baseline Establishment: Compare current data against predefined quality requirements to establish baseline quality scores [90]
Essential Research Tools and Solutions
Data Quality Management Tools
Table 2: Data Quality Tools for Biomedical Research
| Tool Name | Type | Key Features | Research Applications |
|---|---|---|---|
| Great Expectations | Open-source Python library [89] [92] | 300+ pre-built validation checks, data documentation [92] | Defining expectations for sample data formats and value ranges [89] |
| Soda Core | Open-source CLI tool [89] [92] | YAML-based checks, multi-source compatibility [92] | Automated validation of sample metadata across systems [92] |
| Monte Carlo | Commercial data observability platform [89] [92] | ML-powered anomaly detection, automated root cause analysis [92] | Monitoring sample data pipelines for unexpected changes [92] |
| dbt Core | Open-source transformation tool [89] | Built-in data testing, modular SQL-based transformations [89] | Implementing quality checks during sample data transformation [89] |
Research Reagent Solutions for Quality Assurance
Table 3: Essential Research Materials for Sample Data Quality
| Material/Reagent | Function in Quality Assurance | Quality Impact |
|---|---|---|
| Standardized Collection Tubes | Consistent sample acquisition with appropriate preservatives [76] | Primary collection tube type impacts all biomarker measurements by >10% [76] |
| Temperature Monitoring Devices | Track storage conditions throughout sample lifecycle [44] | Prevents analyte degradation; plasma Aβ42/Aβ40 decline >10% with improper storage [76] |
| Sample Tracking Systems | Unique identification and chain of custody maintenance [44] | Ensures data completeness and traceability from collection to analysis [88] |
| Quality Control Materials | Reference standards for assay validation [76] | Enables accuracy verification through comparison with known values [93] |
| Data Management Software | Electronic documentation of sample processing [44] | Standardizes data capture, improves consistency and validity [88] |
Troubleshooting Guides and FAQs
Common Data Quality Issues and Solutions
Q: Our biomarker measurements show unexpected variations between batches. How can we determine if this is due to sample handling rather than analytical issues?
A: Implement systematic pre-analytical controls based on the evidence-based handling protocol from the Global Biomarker Standardization Consortium [76]:
- Standardize collection tubes across all sites
- Control centrifugation delays (process within 30 minutes at room temperature or 2°C-8°C)
- Document and minimize storage delays before freezing
- Use the same freeze-thaw cycles across samples
- Monitor and record temperature excursions during storage
Q: We're experiencing inconsistent sample metadata across different research sites. What approach can improve data consistency?
A: Implement these standardized procedures [90] [88]:
- Develop a standardized data collection form with defined fields and formats
- Establish data quality rules for critical data elements (e.g., "sample_id must follow pattern: SITE-YYYYMMDD-XXX")
- Use automated validation checks in your electronic data capture system
- Conduct regular audits of data entry practices across sites
- Provide comprehensive training on data standards and their importance
Q: How can we efficiently track data lineage to identify the root cause of sample data issues?
A: Implement data lineage tracking through these methods [90] [92]:
- Use tools like Monte Carlo or Collibra that automatically map data flows [92]
- Establish unique identifiers that persist throughout the sample lifecycle [44]
- Document all transformation steps in sample processing protocols
- Implement automated monitoring that alerts when data patterns deviate from expectations [89]
Q: What specific metrics should we monitor to ensure ongoing data quality in our sample repository?
A: Track these critical metrics with defined thresholds [87] [90]:
- Sample data completeness rate (target: >98% for required fields)
- Processing delay compliance (target: >95% within protocol-specified timeframes)
- Temperature excursion rate (target: <2% of samples)
- Data entry error rate (target: <0.5% of records)
- Sample-to-data reconciliation success (target: 100% traceability)
Q: Our team spends excessive time cleaning and validating sample data before analysis. How can we automate these processes?
A: Implement these automation strategies [87] [89]:
- Integrate data quality checks directly into data pipelines using tools like Great Expectations or dbt [89]
- Set up automated alerts for data quality threshold violations [92]
- Use automated data profiling to continuously monitor data health [90]
- Implement automated data cleansing rules for common issues (standardizing date formats, unit conversions) [87]
Advanced Technical Support
Q: We're implementing CDISC standards for regulatory submissions. How does this impact our data quality assessment system?
A: CDISC implementation requires these specific enhancements to your data quality framework [88]:
- Align data quality rules with CDISC model validation rules
- Implement additional checks for SDTM and ADaM mapping compliance
- Extend metadata management to include CDISC-defined terminology
- Enhance traceability requirements to support regulatory audit trails
- Increase emphasis on data consistency across domains and studies
Q: How do we validate that our data quality framework is effectively supporting research reproducibility?
A: Use these validation approaches [88] [93]:
- Conduct periodic blinded data re-abstraction to verify accuracy
- Perform statistical process control analysis on key quality metrics
- Implement sample tracking verification through periodic audits
- Measure intra- and inter-rater reliability for subjective data elements
- Assess data quality before and after framework implementation to quantify improvement
This technical support center provides troubleshooting guides and FAQs to help researchers and scientists maintain sample integrity from collection to analysis, supporting the standardization of sample collection and storage research.
Troubleshooting Guides
Encountering unexpected results? This section addresses common sample integrity challenges and provides corrective methodologies.
Guide 1: Addressing Compromised Blood Sample Quality
Presenting Issue: Blood samples show abnormal test results, such as erroneously high potassium or low calcium levels, inconsistent with the donor's clinical presentation.
Investigation & Diagnosis:
- Action: Check the sample for signs of hemolysis (pink or red serum), and review the sample collection tube type and handling history.
- Diagnosis: The issue is likely a pre-analytical error. Common causes include [94] [95]:
- Sample Contamination: Using the wrong collection tube (e.g., EDTA contamination from a purple-top tube chelates calcium and falsely elevates potassium) [95].
- Improper Handling: Hemolysis from vigorous shaking or improper storage; cell metabolism from delayed processing alters glucose and electrolyte levels [94] [95].
- IV Contamination: Drawing blood from an arm with a running intravenous line dilutes the sample [95].
Corrective Methodology:
- Re-collect the sample using the correct tube type and protocol.
- Adhere to CLSI guidelines (e.g., GP41) for venipuncture, including the order of draw [96].
- Process promptly: Centrifuge and separate serum or plasma within a defined time frame (e.g., within 4 hours for glucose stability) [95].
- Implement automated sample quality assessment to detect hemolysis, lipemia, and icterus (ILH) before analysis [94] [96].
Guide 2: Managing Sample Degradation During Transport
Presenting Issue: Analyte instability or degradation during shipment, leading to unreliable data.
Investigation & Diagnosis:
- Action: Review shipment records and temperature monitor data logs.
- Diagnosis: Inadequate temperature control or excessive transit time. Temperature excursions can degrade sensitive analytes, while mechanical stress can cause hemolysis [96].
Corrective Methodology:
- Validate Shipment Conditions: Define and validate shipment conditions (e.g., on dry ice, wet ice, or ambient) for analyte stability [15].
- Use Qualified Packaging: Use validated shipping containers with sufficient coolant.
- Include Temperature Loggers: Place temperature data loggers in shipments for continuous monitoring and documentation [15].
- Ship Aliquots Separately: For critical samples, split into Set 1 and Set 2 aliquots and ship in separate packages to preserve one set in case of shipping failure [15].
Guide 3: Resolving Sample Identification or Chain of Custody Gaps
Presenting Issue: Unlabeled or mislabeled samples, or inability to track sample location and storage history.
Investigation & Diagnosis:
- Action: Audit sample labels and trace the sample's journey using laboratory logs or the Laboratory Information Management System (LIMS).
- Diagnosis: Lack of standardized labeling or an integrated tracking system. Handwritten labels are a primary source of error [65].
Corrective Methodology:
- Eliminate Handwriting: Use pre-printed, machine-readable (e.g., barcode) labels for unambiguous identification [97].
- Standardize Label Information: Include Protocol Number, Subject Number, Matrix, and a Unique Identifier [15].
- Implement a LIMS: Use a LIMS to maintain a full chain of custody, recording every movement, storage location, and temperature exposure [15].
Frequently Asked Questions (FAQs)
Q1: What are the most critical steps to control immediately after sample collection? A1: The most critical steps are [15] [96]:
- Proper Labeling: Label samples with a unique identifier in the patient's presence using at least two identifiers.
- Correct Tube & Additive: Use the prescribed collection tube and ensure correct fill volume to maintain blood-to-additive ratio.
- Rapid Stabilization: Place samples at the required temperature (e.g., refrigerate or freeze) immediately after processing.
Q2: Our laboratory has multiple -80°C freezers from different manufacturers. How can we standardize storage documentation? A2: Instead of using specific temperatures (e.g., -70°C vs. -80°C) in documentation, adopt standardized terminology with defined temperature ranges [15]. This ensures consistency across different equipment and sites.
Table: Recommended Standardized Storage Terminology
| Term | Defined Temperature Range |
|---|---|
| Ultra-freezer | -60°C to -90°C |
| Freezer | -15°C to -30°C |
| Refrigerator | +2°C to +8°C |
| Room Temperature | +15°C to +25°C |
Q3: How can we reduce human error in repetitive sample handling tasks? A3: Automate repetitive tasks like scanning, weighing, sorting, and labeling. Automated systems minimize manual handling errors, improve traceability, and free up researcher time [97].
Q4: What should we do if a storage unit has a temperature excursion? A4: Follow a predefined SOP. The plan should include [15]:
- Immediate Notification: Alert designated personnel.
- Assessment: Evaluate the impact on sample stability based on the duration and magnitude of the excursion.
- Documentation: Record the event and any corrective actions taken.
- Sample Integrity Check: Test quality control samples stored in the same unit to determine if sample integrity was compromised.
Experimental Workflow for Integrity Validation
The following workflow outlines the key stages and critical control points for ensuring sample integrity.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Materials and Systems for Sample Integrity
| Item | Function & Purpose |
|---|---|
| Laboratory Information Management System (LIMS) | Software for end-to-end sample tracking, managing chain of custody, and recording storage conditions [15]. |
| Standardized Barcoded Labels | Pre-printed labels for unambiguous sample identification, reducing errors from handwritten labels [97]. |
| Validated Collection Tubes | Tubes with specified additives (e.g., EDTA, Heparin) and vacuum pressure to ensure correct fill volume and blood-to-additive ratio [96]. |
| Temperature Monitoring System | Data loggers and continuous monitoring systems for storage units and shipments to document conditions [15]. |
| Automated Storage System | Robotic systems (e.g., -80°C automates) for secure, trackable storage and retrieval, minimizing freeze-thaw cycles [97]. |
| Quality Control (QC) Materials | Commercial quality control samples used to verify analytical instrument performance and, by extension, the integrity of the testing process [96]. |
Within the framework of a broader thesis on standardizing sample collection and storage research, this technical support center addresses the pivotal challenge of selecting and maintaining optimal storage conditions for biological materials. The integrity of research data and the success of drug development pipelines are fundamentally linked to the precise control of storage parameters. Inconsistent or suboptimal storage can lead to sample degradation, compromised analytical results, and irreproducible data, thereby undermining research validity. This guide provides researchers, scientists, and drug development professionals with standardized troubleshooting guides, FAQs, and detailed protocols to navigate the complexities of sample storage, ensuring the longevity and reliability of valuable biological specimens.
Storage Condition Specifications and Applications
The following table summarizes the standard temperature ranges and primary applications for common storage conditions in a research setting.
Table 1: Comparative Analysis of Storage Conditions
| Storage Condition | Typical Temperature Range | Primary Applications & Rationale |
|---|---|---|
| Room Temperature | 15°C to 27°C [98] | Storing FFPE (formalin-fixed paraffin-embedded) tissues in climate-controlled rooms [98]. DNA from these tissues often yields partial readings, and RNA is highly volatile and typically cannot be extracted from non-frozen tissues [98]. |
| Refrigerated | 2°C to 10°C [98] | Short-term storage of frequently used reagents like enzymes and antibodies to prevent deterioration from repeated freeze-thaw cycles [98]. |
| Standard Freezer | -25°C to -10°C [98] | Short-term storage of temperature-reactive samples and reagents. DNA and RNA can be obtained from tissues suspended in preservative solutions at -20°C [98]. |
| Low-Temperature Freezer | -25°C to -40°C [98] | Provides a colder environment than standard freezers for more sensitive materials requiring sub-zero stability. |
| Ultra-Low Freezer (ULT) | -45°C to -86°C [98] | Long-term storage of sensitive molecular-based samples (e.g., DNA, RNA, proteins, cells, tissues) and mRNA vaccines [99] [98]. Slows molecular degradation; -80°C can preserve DNA and protein for years, though RNA may show degradation after ~5 years [99]. |
| Cryogenic Storage | -150°C to -190°C [98] [100] | Gold standard for long-term storage, halting all biological processes. Ideal for specimens not in preservative solutions, such as certain cell therapies [99] [100]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Sample Storage
| Item | Function & Application |
|---|---|
| Cryoprotective Agents (CPAs) | Mitigate cryoconcentration effects and sustain protein stability during freezing and thawing cycles (e.g., glycerol, glycol) [100]. |
| RNA Stabilizing Solutions | Preserve RNA integrity in samples that cannot be immediately frozen, such as RNAlater [99]. |
| Standardized Collection Tubes | Vacuum containers with color-coded caps indicate specific additives (e.g., anticoagulants, gels) for blood sample preservation [101]. |
| Single-Use Bags & Vials | Provide sterile, flexible containers for freezing biologics; compatible with controlled plate freezing systems [100]. |
| Barcodes and RFID Tags | Enable quick sample identification and tracking, reducing manual errors and improving traceability [102] [103]. |
Experimental Protocols for Sample Handling
Protocol: Procurement and Snap-Freezing of Tissue Biospecimens
Objective: To preserve tissue for genomic, transcriptomic, and proteomic analyses by minimizing ischemia time and achieving rapid stabilization.
Materials: Surgical tools, wet ice, cryovials, isopentane (pre-cooled in liquid nitrogen), liquid nitrogen, -80°C freezer or liquid nitrogen storage system [99].
Methodology:
- Minimize Warm Ischemia: Define warm ischemia as the time tissue is at ambient temperature after resection. A practical goal for most tissues is snap-freezing within 20 minutes of resection to mitigate artifactually altered gene expression and protein phosphorylation profiles [99].
- Utilize Cold Ischemia: If immediate freezing is not possible, place the tissue specimen on wet ice or in a 4°C refrigerator. This "cold ischemia" time should still be minimized and documented [99].
- Snap-Freezing: Submerge the tissue sample in isopentane pre-cooled by liquid nitrogen, or directly into liquid nitrogen. This rapid freezing prevents the formation of large ice crystals that can damage cellular structures [99].
- Long-Term Storage: Transfer the snap-frozen sample to a cryovial for permanent storage at -80°C or in liquid nitrogen (-150°C to -196°C) [99] [98].
Protocol: Establishing a Controlled Freezing Process for Biologics
Objective: To freeze biological drug substances (e.g., monoclonal antibodies, protein solutions) in a controlled manner to preserve stability and efficacy.
Materials: Biologic substance, cryovessels or single-use bags, controlled-rate freezer or controlled plate freezing system [100].
Methodology:
- Container & Formulation: Select appropriate containers (vials, bags) considering volume and thermodynamic properties. Incorporate cryoprotective agents (CPAs) like sucrose into the formulation to protect proteins [100].
- Determine Optimal Cooling Rate: Conduct stability studies to characterize the product. Note that the optimal cooling rate is not universal and must be individualized for each biologic. The key is to control the time for phase transition (liquid to frozen) to minimize risks like cryoconcentration and pH shifts [100].
- Execute Controlled Freezing: Avoid slow, uncontrolled freezing. Instead, use a controlled-rate freezer or a controlled plate freezing system. These methods provide precise regulation of freezing rates and temperature gradients, ensuring homogeneous processing and minimizing ice crystal formation [100].
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: My RNA samples stored at -80°C for several years show signs of degradation. Is this normal? Yes, this is a documented phenomenon. While DNA and protein can be preserved for years at -80°C, RNA can show degradation at the 5-year mark, even at -70°C or -80°C [99]. For very long-term RNA storage, consider using RNA stabilizing solutions or storage at colder temperatures (e.g., -150°C) [99].
Q2: How many freeze-thaw cycles can my protein aliquots withstand? Tolerance for freeze-thaw events is tissue and sample type dependent [99]. As a best practice, minimize the number of freeze-thaw cycles. For frequently used reagents like enzymes and antibodies, prepare small aliquots for short-term refrigerated storage (2°C to 10°C) to avoid repeated thawing of the main stock [98].
Q3: I have sensitive patient data linked to my samples. How can I manage this responsibly? Granting agencies and publishers understand the need to protect sensitive data. Deposit requirements are not synonymous with Open Access. You can:
- De-identify and anonymize your data before deposition.
- Work with your funder, journal, or institutional review board to find a solution that protects patient privacy while meeting sharing requirements [104].
Q4: Is storage at -80°C sufficient, or should I invest in -150°C storage? It remains unresolved whether -150°C storage provides significant advantages for all sample types relative to -80°C [99]. However, -80°C is generally adequate for DNA and proteins for several years. Storage at -150°C (cryogenic storage) is considered the gold standard for long-term preservation, especially for sensitive samples like certain cell therapies, as it halts all biological activity [99] [98].
Troubleshooting Guide
Problem: Sample Degradation After Thawing
- Potential Cause 1: Excessive warm ischemia time during initial collection [99].
- Potential Cause 2: Uncontrolled or slow freezing process, leading to ice crystal formation and cryoconcentration [100].
- Solution: Transition from uncontrolled freezing to controlled-rate freezing methods, such as plate freezing or controlled cryogenic freezing, to ensure optimal cooling rates [100].
- Potential Cause 3: Multiple freeze-thaw cycles.
Problem: Inability to Locate Samples or Access Data
- Potential Cause: Inefficient sample tracking and documentation.
Problem: Freezer Failure or Temperature Excursion
- Potential Cause: Equipment malfunction or power loss.
Workflow Diagram: Sample Storage Pathway
The following diagram outlines the logical workflow for selecting the appropriate storage condition based on sample type and intended use, incorporating key decision points and quality assurance checks.
Sample Storage Decision Workflow
Fundamental Concepts: Chain of Custody vs. Audit Trails
In regulated laboratory environments, such as those involved in sample collection and storage research, understanding the distinct roles of Chain of Custody (CoC) and Audit Trails is fundamental to data integrity.
Chain of Custody is the chronological, documented trail that tracks the custody, control, and transfer of physical samples and data from their point of origin to their final destination [47]. Its core function is to ensure that a sample is never out of the direct supervision of an accountable party, thereby preventing unauthorized access, tampering, or contamination [47].
An Audit Trail is a detailed, time-stamped record within a Laboratory Information Management System (LIMS) that tracks every action, change, or event related to data handling and analysis [47]. It provides a transparent history of data modifications, which is invaluable for identifying discrepancies and ensuring accountability.
The table below summarizes their key differences:
| Feature | Chain of Custody (CoC) | Audit Trail |
|---|---|---|
| Primary Focus | The physical journey and custody of a sample [47] | The digital history and changes to data [47] |
| What It Tracks | Sample collection, transfers, storage, and analysis by personnel [50] | Every data modification, user login, and system action with a timestamp [47] |
| Main Purpose | Preserve sample integrity and prevent tampering [47] | Ensure data integrity and traceability of all electronic records [50] |
| Key Application | Forensic evidence, clinical trial samples, environmental samples [47] | Data quality assurance, regulatory compliance (e.g., FDA 21 CFR Part 11), process improvement [47] |
Troubleshooting Common Chain of Custody & Documentation Issues
A breakdown in the Chain of Custody can compromise the entire research project or forensic case. The following guides address common problems.
Guide: A Sample's Chain of Custody Documentation is Incomplete
Problem: Gaps are identified in the documentation log for a sample, with missing information about who handled it or where it was stored at a specific time.
Investigation & Resolution:
- Identify the Gap: Precisely determine the time period or process step where the documentation is missing. Check all related physical logs, electronic records in the LIMS, and storage area access logs [50].
- List Possible Causes:
- Human Error: Personnel forgot to log a sample transfer or storage step [105].
- Procedural Error: The sample was handled by an unauthorized individual who did not know the logging procedure.
- System Error: A temporary failure in the electronic tracking system (e.g., LIMS) failed to record the action [50].
- Collect Data: Interview all personnel involved in the sample's handling during the relevant period. Review automated system logs and audit trails for any anomalies or error messages related to the sample ID [50] [47]. Check if the sample's physical location can be corroborated by other means (e.g., security camera footage, independent experiment records).
- Eliminate Causes & Experiment: Based on the collected data, rule out possibilities. If human error is suspected, review and reinforce training on Standard Operating Procedures (SOPs). If a system error is possible, work with IT to diagnose the fault using the system's own audit trails [47].
- Identify the Root Cause & Corrective Action: The final cause might be, for example, a technician deviating from procedure during a night shift. The corrective action includes formally documenting the incident, re-training staff, and potentially implementing automated alerts in the LIMS for missed log entries [50].
Guide: A Regulatory Audit Has Found an Unexplained Discrepancy in the Audit Trail
Problem: An auditor has flagged an entry in the electronic audit trail where critical data was modified without a corresponding documented reason.
Investigation & Resolution:
- Identify the Discrepancy: Pinpoint the exact record, the nature of the change, the user ID associated with the change, and the timestamp [47].
- List Possible Causes:
- Legitimate Error Correction: A technician corrected a data entry error but failed to provide a mandatory reason in the system [105].
- Unauthorized Access: A user account was compromised or used inappropriately to alter data [50].
- Software Malfunction: A bug in the data management system caused an unintended change.
- Collect Data: Use the audit trail's capabilities to investigate the full history of that specific data point. Cross-reference the event with the individual's laboratory notebook, instrument printouts, and the sample's chain of custody records [50] [47]. The system's role-based access control logs can confirm if the user was authorized to make such a change [50].
- Eliminate Causes & Experiment: If the user was authorized and the change aligns with raw data in a notebook, the cause is likely a failure to document the reason. If the change is inconsistent with all other records, investigate potential unauthorized access.
- Identify the Root Cause & Corrective Action: The cause might be a lack of training on proper data amendment procedures. The corrective action is to provide immediate remedial training and to reconfigure the LIMS to make the "reason for change" field mandatory [50].
Investigation Path for Audit Trail Discrepancy
Frequently Asked Questions (FAQs)
Q1: What are the ALCOA+ principles, and how do they relate to chain of custody? ALCOA+ is a framework defining data integrity requirements. It stands for Attributable (who performed the action), Legible, Contemporaneous (recorded at the time of the action), Original, and Accurate, with the "+" encompassing Complete, Consistent, Enduring, and Available [50]. These principles are the foundation of a defensible chain of custody and audit trail, ensuring every sample handling step and data point is traceable and trustworthy [50].
Q2: Our lab is small. Do we need an electronic LIMS, or are paper records sufficient? While paper records can be sufficient if meticulously managed, they are highly prone to human error, loss, and damage [106]. An electronic LIMS is strongly recommended because it automatically generates timestamps, enforces role-based access, and creates immutable audit trails, significantly reducing the risk of custody breaks and simplifying regulatory compliance [50] [47].
Q3: What should we do if we identify a break in the chain of custody? Immediately document the incident and all known facts. Initiate an investigation to determine the cause and scope of the breach. The integrity of the affected sample may be compromised. Depending on the severity and the requirements of your regulatory body, the sample may need to be quarantined and excluded from research data, and in severe cases, decommissioned and replaced [106].
Q4: How can we improve our current chain of custody procedures?
- Automate: Use barcodes or RFID tags with a LIMS to automate sample tracking [50].
- Train: Implement regular, scenario-based training for all staff [50].
- Audit: Conduct periodic internal audits of your CoC and audit trails to find gaps before an external audit does [50].
- Simplify: Review and streamline procedures to minimize unnecessary handoffs, as each transfer is a potential point of failure.
The following table details key items and solutions crucial for maintaining chain of custody in research.
| Item/Solution | Function in Maintaining Chain of Custody |
|---|---|
| Laboratory Information Management System (LIMS) | The digital "nervous system" that automates the logging of sample transfers, storage, and analysis, creating an immutable and auditable record [50]. |
| Electronic Laboratory Notebook (ELN) | Provides a secure, time-stamped environment for recording experimental data and observations, linking them directly to specific samples [50]. |
| Tamper-Evident Seals & Bags | Provide physical evidence of unauthorized access to sample containers, crucial for forensic and clinical samples [106]. |
| Unique Sample Identifiers (Barcodes/QR Codes) | Link a physical sample directly to its digital record in the LIMS, allowing for quick, error-free reconciliation and tracking [50]. |
| Role-Based Access Control (RBAC) | A security feature in LIMS that ensures only authorized personnel can access, handle, or log data for specific samples, enforcing accountability [50]. |
| Normative Control Biofluid Bank | A centralized repository of well-characterized control samples that allows for inter-study comparison and validation of isolation and analysis methods [31]. |
Ideal Chain of Custody Workflow
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center provides troubleshooting guidance and best practices for researchers and scientists implementing Continuous Quality Improvement (CQI) in sample collection and storage workflows. These resources address common operational challenges to ensure data integrity, regulatory compliance, and process optimization.
Frequently Asked Questions (FAQs)
Q1: Our laboratory is experiencing an increase in sample misidentification errors. What CQI methodologies can help address this?
A: Sample misidentification is a critical defect that can be systematically reduced using CQI methodologies. The Plan-Do-Study-Act (PDSA) cycle is highly effective for this type of incremental process improvement [107] [108] [109]. You can structure a PDSA cycle as follows:
- Plan: Define the problem and benchmark your current error rate. Set a goal for reduction (e.g., 50% decrease in 3 months). Plan an intervention, such as replacing all handwritten labels with pre-printed barcodes [7] [110].
- Do: Implement the barcoding system on a small scale, for example, in one specific sample collection unit or for one type of sample.
- Study: Measure the error rate after the intervention. Compare it to your baseline data. Analyze if the barcoding system worked as expected and identify any unforeseen challenges.
- Act: If successful, standardize the barcoding system across all collection points. If not, analyze the reasons and begin a new PDSA cycle with a modified plan [107] [109].
Furthermore, the Six Sigma DMAIC (Define, Measure, Analyze, Improve, Control) framework is a powerful, data-driven approach to reducing such errors [107] [109]. Its phases directly target process defects:
- Define the project goals and customer requirements.
- Measure the current performance by collecting data on the misidentification rate.
- Analyze the data to identify the root causes of the errors.
- Improve the process by implementing and validating the solution (e.g., barcoding).
- Control the future process performance to maintain the gains [109].
Q2: We have noted inconsistencies in our sample storage temperatures. What are the best practices for monitoring and maintaining storage conditions?
A: Maintaining proper storage conditions is fundamental to sample integrity [83] [110]. Best practices include:
- Dedicated Equipment: Use dedicated refrigerators and freezers for sample storage, not household-grade units [83].
- Continuous Monitoring: Implement a continuous temperature monitoring system with digital loggers that provide real-time data and alerts for out-of-range conditions [7] [110].
- Redundancy Plans: Install backup power systems (e.g., UPS or generators) to protect against power outages. Have a documented plan for sample relocation in case of extended equipment failure [7].
- Regular Audits: Conduct regular inventory checks and audits of storage conditions. Implement a first-in, first-out (FIFO) system to prevent sample degradation over time [7] [110].
- Validation: Validate the performance of your storage units to ensure they maintain uniform temperature throughout the chamber.
Q3: How can we foster a culture of Continuous Quality Improvement among our research staff?
A: Building a CQI culture requires both structural and social elements [107] [108] [109]:
- Leadership Endorsement: Secure visible commitment and support from senior leadership. This includes allocating resources for CQI training and projects [109].
- Employee Engagement and Empowerment: Actively involve staff at all levels in the improvement process. Empower them to identify problems and suggest solutions. A culture of trust is essential, moving away from a "blame and punish" mindset to a focus on systemic issues [108] [109].
- Interprofessional Teams: Form CQI teams that include members from different roles (e.g., collectors, processors, analysts) to gain diverse perspectives [107].
- Training and Support: Invest in staff training on CQI principles (like Lean and Six Sigma) and the specific tools they will use [109].
- Celebrate Success: Share the results of successful CQI projects, highlighting how they improved workflows, reduced errors, or enhanced patient safety. This reinforces the value of the CQI process [107].
Core CQI Concepts and Impact
Continuous Quality Improvement (CQI) is a progressive, incremental improvement of processes, safety, and patient care [107]. It is rooted in the belief that there is always room for improvement, even in well-established practices [109]. The core principle is to repeatedly ask, "How are we doing?" and "Can we do it better?" [107].
Common CQI Goals in Research and Healthcare [107]:
- Reducing defects (e.g., sample mislabels, processing errors)
- Cost reduction
- Decreased wait times (e.g., in reporting results)
- Higher patient/staff satisfaction
- Increased patient and staff safety
Quantitative Impact of CQI Initiatives
The following table summarizes the demonstrated impacts of CQI across various healthcare and research settings, showcasing its effectiveness.
| Setting/Application | Measured Outcome | Impact of CQI Initiative | Source |
|---|---|---|---|
| HIV Patient Care (Alabama) | Missed appointment rate | Statistically significant decrease | [107] |
| Surgical Procedures | Process or outcome improvement | Improvement or benefit in over 88% of studies reviewed | [107] |
| Radiology Departments | Cost, wait time, patient volume, safety | Improvements in one or more areas across all 23 studies reviewed | [107] |
Essential Methodologies and Tools
CQI utilizes several structured methodologies. The choice depends on the organization's goals, resource feasibility, and the specific problem being addressed [107].
Comparison of Major CQI Methodologies
| Methodology | Core Focus | Key Process/Principles | Primary Application Context |
|---|---|---|---|
| Plan-Do-Study-Act (PDSA) [107] [108] [109] | Rapid, iterative testing of changes on a small scale. | A four-step cycle for learning and improvement: Plan a change, Do (implement it), Study (analyze the results), Act (adopt, adapt, or abandon). | Broadly applicable for most incremental process improvements. |
| Six Sigma [107] [109] | Reducing variation and eliminating defects in processes. | Uses the DMAIC (Define, Measure, Analyze, Improve, Control) framework. Aims for near-perfect processes (≤3.4 defects per million opportunities). | Problem-focused, aimed at solving specific, high-cost, or high-error processes. |
| Lean [107] [109] | Eliminating waste to improve flow and efficiency. | Identifies and removes 7 types of waste (e.g., transport, waiting, over-processing). Employs Kaizen (continuous incremental improvement). | Improving overall operational efficiency and throughput. |
| Baldrige Excellence Framework [107] [109] | Comprehensive organizational management and system performance. | A holistic framework with seven categories: Leadership, Strategy, Customers, Measurement, Workforce, Operations, and Results. | Enterprise-wide cultural transformation and system-level improvement. |
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and their functions in a standardized sample management system.
| Item/Reagent | Primary Function in Sample Management |
|---|---|
| Barcoded Labels | Provides a unique, machine-readable identifier for each sample to prevent misidentification and enable tracking [7] [110]. |
| Leak-Proof Storage Containers | Maintains sample integrity by preventing leakage, contamination, and evaporation during storage [83] [110]. |
| Temperature Monitoring Loggers | Continuously monitors and records storage temperature to ensure samples are maintained within specified viability ranges [7] [110]. |
| Chain of Custody (CoC) Forms | Documents every individual who handles a sample, ensuring accountability and traceability from collection to disposal [7]. |
| Laboratory Information Management System (LIMS) | A software platform that centralizes sample data, automates tracking, manages storage locations, and ensures regulatory compliance [7] [110]. |
CQI Implementation Workflow
The following diagram illustrates the logical workflow for implementing a Continuous Quality Improvement initiative, integrating core principles from major methodologies like PDSA and DMAIC.
Sample Management Lifecycle
This diagram outlines the key stages and logical relationships in the end-to-end sample management lifecycle, highlighting critical control points for quality improvement.
Conclusion
The standardization of sample collection and storage is not a one-time task but a continuous commitment to quality that forms the bedrock of reliable and reproducible scientific research. By integrating the foundational principles, rigorous methodologies, proactive troubleshooting, and robust validation frameworks outlined in this guide, organizations can significantly enhance data integrity, ensure regulatory compliance, and foster successful collaboration. The future of biomedical research hinges on the ability to share and utilize high-quality biological samples effectively. Embracing these standardized practices, supported by emerging technologies like AI for data management and blockchain for traceability, will be pivotal in accelerating drug development and unlocking new frontiers in personalized medicine.
References
- 1. The 6 Data Quality Dimensions with Examples [https://www.collibra.com/blog/the-6-dimensions-of-data-quality]
- 2. Common Issues with Lab Samples Handling in Clinical Trials [https://solutionsop.co.uk/2020/04/27/common-issues-with-lab-samples-handling-in-clinical-trials/]
- 3. Introduction to Specimen Collection [https://www.labcorp.com/test-menu/resources/introduction-to-specimen-collection]
- 4. Overview of Data Quality: Examining the Dimensions, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9912223/]
- 5. 6 Dimensions for Assessing Usability Data in Analysis [https://www.nngroup.com/articles/usability-data-in-analysis/]
- 6. A Step-by-Step Guide to Specimen Collection [https://msoft360.cloud/guide/specimen-collection/]
- 7. Sample Collection & Processing Best Practices For Labs [https://qbench.com/blog/sample-collection-processing-best-practices-for-labs]
- 8. Data protection laws in the United States [https://www.dlapiperdataprotection.com/?c=US]
- 9. US State Privacy Legislation Tracker [https://iapp.org/resources/article/us-state-privacy-legislation-tracker/]
- 10. 2025 State Privacy Laws: What Businesses Need to Know ... [https://www.whitecase.com/insight-alert/2025-state-privacy-laws-what-businesses-need-know-compliance]
- 11. GxP in 2025: Ensuring Quality in Life Sciences [https://qpsag.com/gxps-future-quality-assurance/]
- 12. Transforming GxP Compliance in Life Sciences for 2025 [https://www.acldigital.com/blogs/gxp-compliance-2025-digital-transformation-life-sciences]
- 13. GxP Compliance: A Comprehensive Guide to 2025 [https://www.compliancequest.com/what-is-gxp-compliance-with-fda-regulations/]
- 14. Automated Sample Storage Systems Market Report, 2025- ... [https://www.gminsights.com/industry-analysis/automated-sample-storage-systems-market]
- 15. Sample Management: Recommendation for Best Practices ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4779093/]
- 16. Best practices and new trends in biological sample ... [https://www.clinigengroup.com/insight/insights/2025/best-practices-and-new-trends-in-biological-sample-management/]
- 17. Future Use Of Biological Specimens Collected Under ... [https://www.uab.edu/research/home/future-use-of-biological-specimens-collected-under-clinical-protocols]
- 18. Problems of Multi-Institutional Studies - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK235189/]
- 19. Quality matters: International standards for biobanking - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9357355/]
- 20. Collection, storage and shipment of specimens for laboratory ... [https://www.ncbi.nlm.nih.gov/books/NBK143256/]
- 21. ISO 20387:2018 - Biotechnology — Biobanking [https://www.iso.org/standard/67888.html]
- 22. ISO 20387:2018 – General Requirements for Biobanking [https://blog.ansi.org/anab/iso-20387-2018-general-requirements-biobanking/]
- 23. Overcoming 4 Challenges in Multicenter Clinical Trials [https://www.florencehc.com/overcoming-four-common-challenges-in-multicenter-research/]
- 24. Practical implementation issues and challenges for biobanks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3388905/]
- 25. Guides [https://www.biobanking.com/resources/guides/]
- 26. Guidelines for standardizing and increasing the transparency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5594115/]
- 27. Collection and Processing of Coagulation Specimens [https://www.laboratoryalliance.com/healthcare-providers/laboratory-services/specimen-collection-documents/collection-and-processing-of-coagulation-specimens/]
- 28. Hemostasis Preanalytical Guidelines to Introduce Blood ... [https://www.horiba.com/int/healthcare/academy/hemostasis-guide/preanalytical-guidelines/]
- 29. Best Practices for Collecting Data [https://blog.eskuad.com/best-practices-for-collecting-data]
- 30. Data collection: 8 best practices to avoid costly surprises [https://metergroup.com/expertise-library/data-collection-8-best-practices-to-avoid-costly-surprises/?srsltid=AfmBOoppG_k1Hndd8bFIowy78GxJDcmFfC-JIajqsaCViiiXfgpjNORm]
- 31. Standardization of sample collection, isolation and analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3760646/]
- 32. Aseptic Technique: What It Is & What To Know [https://my.clevelandclinic.org/health/treatments/aseptic-technique]
- 33. Chapter 4 Aseptic Technique - Nursing Skills - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK593203/]
- 34. Mastering Aseptic Technique: The Foundation of ... [https://www.labmanager.com/mastering-aseptic-technique-the-foundation-of-successful-cell-culture-34208]
- 35. Aseptic Laboratory Techniques and Safety in Cell Culture [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/aseptic-technique.html]
- 36. Aseptic Technique: Instruments [https://researchanimaltraining.com/articles/aseptic-technique-instruments/]
- 37. Laboratory Barcodes: A Complete Guide [https://computype.com/blog/laboratory-barcodes-guide/?srsltid=AfmBOoqM8rYEO4JHWj5dw5H7WOg2nxISE1YNILPGYdohCz-5wV4M1bQk]
- 38. The Ultimate Guide to QR Codes: Everything You Need ... [https://www.uniqode.com/blog/qr-code-basics/comprehensive-guide-to-qr-code]
- 39. QR Codes: Design Guidelines - Convincible Media [https://www.convincible.media/article/qr-codes]
- 40. Serialized QR Codes: Everything a brand should know [https://www.scantrust.com/serialized-qr-codes/]
- 41. 13 QR-Code Usability Guidelines [https://www.nngroup.com/articles/qr-code-guidelines/]
- 42. Monitoring of SARS-CoV-2 antibodies using dried blood ... [https://www.nature.com/articles/s41598-022-09699-4]
- 43. Correlation of dried blood spots and plasma for quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8631068/]
- 44. Review Biological sample storage in biomedical research [https://www.sciencedirect.com/science/article/abs/pii/S0009898125004176]
- 45. A state-of-the-science review and guide for measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9375076/]
- 46. How to Implement a Chain of Custody Program in Your Lab [https://qbench.com/blog/how-to-implement-a-chain-of-custody-program-in-your-lab]
- 47. The Importance of Maintaining Chain of Custody and Audit ... [https://www.labvantage.com/blog/the-importance-of-maintaining-chain-of-custody-and-audit-trails/]
- 48. 7 Signs Your Laboratory Needs a LIMS System [https://www.confience.io/blog/7-signs-your-laboratory-needs-a-lims-system]
- 49. Six Key Laboratory Issues Solved by LIMS Software [https://thirdwaveanalytics.com/blog/solving-laboratory-issues-with-lims/]
- 50. Evidence Chain of Custody Best Practices for Labs [https://www.labmanager.com/evidence-chain-of-custody-best-practices-building-trust-and-traceability-across-scientific-and-forensic-labs-34564]
- 51. Top Features to Look for in a Chain of Custody Testing Lab [https://keystonelab.com/uncategorized/chain-of-custody-testing-lab/]
- 52. 9 Considerations for a Successful LIMS Implementation [https://www.materials.zone/blog/successful-lims-implementation]
- 53. The Ultimate Guide to LIMS Implementation in 2026 [https://www.scispot.com/blog/the-ultimate-guide-to-lims-implementation]
- 54. Understanding Key Warehouse Temperature Terms in ... [https://kanbanlogistics.com/blog/understanding-key-warehouse-temperature-terms-logistics]
- 55. Temperature Sensitive Shipping Glossary [https://a2cargo.com/en/temperature-controlled/temperature-sensitive-shipping-glossary/]
- 56. Best Practices for Temperature-Sensitive Items in 2025 [https://www.atomixlogistics.com/blog/temperature-sensitive-shipping]
- 57. Cold Chain Storage & Distribution: Best Practices 2025 - tempk [https://www.tempcontrolpack.com/knowledge/cold-chain-storage-distribution-best-practices-2025/]
- 58. Temperature-Controlled Warehouses: Effective Guide for ... [https://wareiq.com/resources/blogs/temperature-controlled-warehouses/]
- 59. The EasyLog Guide to Cold Chain Compliance in 2025 [https://lascarelectronics.com/cold-chain-compliance-in-2025/]
- 60. Temperature Standards for Cold Chain Logistics [https://www.linkedin.com/pulse/temperature-standards-cold-chain-logistics-michael-steedman-2e]
- 61. Temperature−Controlled Shipping: All You Need to Know [https://arkcryo.com/blog/everything-you-need-to-know-about-temperature-controlled-shipping.html]
- 62. Temperature Control Regulations (TCR) [https://www.iata.org/en/publications/manuals/temperature-control-regulations/]
- 63. Preparation for blood tests: what can go wrong before the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377977/]
- 64. Pre-analytical variables in coagulation testing: Why do they ... [https://myadlm.org/science-and-research/scientific-shorts/2023/pre-analytic-variables-in-coagulation-testing-why-do-they-matter]
- 65. Common Challenges in Sample Management | QIA [https://www.qi-a.com/learning-center/common-challenges-in-sample-management/]
- 66. Five common pre-analytical variables - Streck [https://www.streck.com/blog/five-common-pre-analytical-variables/]
- 67. Method Comparison and Investigation of Interference ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12444007/]
- 68. Freeze-Thaw Cycles and Why We Shouldn't Do It [https://bitesizebio.com/19700/freeze-thaw-cycles-and-why-we-shouldnt-do-it/]
- 69. The Impact of Sample Storage on Integrity in Clinical ... [https://www.needle.tube/resources-articles/the-impact-of-sample-storage-on-integrity-in-clinical-laboratories]
- 70. The Impact of Repeated Freeze-Thaw Cycles on ... [https://pubmed.ncbi.nlm.nih.gov/28930488/]
- 71. How to Reduce Sample Contamination [https://blog.omni-inc.com/blog/how-to-reduce-sample-contamination]
- 72. Best Practices in Bioinventory Storage | Safeguarding ... [https://genvault.com/best-practices-in-bioinventory-storage-safeguarding-scientific-research/]
- 73. Best Practices for Sample Preparation & Assay Development [https://lifesciences.danaher.com/us/en/products/microplate-readers/topics/best-practices-sample-preparation-assay-development.html]
- 74. Managing Temperature Excursions in Pharmaceutical Cold ... [https://www.eawlogistics.com/managing-temperature-excursions-in-pharmaceutical-cold-chain-logistics-a-comprehensive-guide/]
- 75. How to Manage Temperature Excursions in Pharma Cold ... [https://cdmoworld.com/how-to-manage-temperature-excursions-in-pharma-cold-chain-logistics/]
- 76. Evidence-based standardized sample handling protocol for ... [https://pubmed.ncbi.nlm.nih.gov/41025225/]
- 77. Proven Strategies to Protect Temperature Sensitive Products [https://www.tempcontrolpack.com/knowledge/cold-chain-risk-management-in-2025-proven-strategies-to-protect-temperaturesensitive-products/]
- 78. Automated Sample Storage Systems Market [https://www.futuremarketinsights.com/reports/automated-sample-storage-systems-market]
- 79. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 80. Frequently Asked Questions: Research Involving Human ... [https://www.nsf.gov/funding/faq/research-involving-human-subjects]
- 81. Efficient sample collection, labeling and storage | INTEGRA [https://www.integra-biosciences.com/united-states/en/blog/article/easy-guide-efficient-sample-collection-labeling-and-storage]
- 82. Common Problems In Clinical Sample Management And ... [https://genemod.net/blog/common-problems-in-clinical-sample-management-and-how-to-solve-them]
- 83. Proper Storage Conditions for Specimen Samples in ... [https://www.needle.tube/resources-18/Proper-Storage-Conditions-for-Specimen-Samples-in-Medical-Diagnostic-Labs:-Best-Practices-and-Guidelines]
- 84. How to use a 96 Channel Manual Workstation for sample ... [https://www.prcxi-liquidmoving.com/blog/how-to-use-a-96-channel-manual-workstation-for-sample-aliquoting-1365195.html]
- 85. Troubleshooting Sample Preparation [https://www.chromatographyonline.com/view/troubleshooting-sample-preparation-0]
- 86. Workflow Automation Can Address the Needs of Large and ... [https://www.clinicallab.com/workflow-automation-can-address-the-needs-of-large-and-small-labs-27493]
- 87. Data Quality Framework: Best Practices & Tools [2025] [https://lakefs.io/data-quality/data-quality-framework/]
- 88. 良好数据质量是生物统计学审评基础- [https://www.ccfdie.org/zryyxxw/scxx/zhxx/webinfo/2014/07/1485614806478983.htm]
- 89. 12 Best Data Quality Tools for 2025 [https://lakefs.io/data-quality/data-quality-tools/]
- 90. Data Quality Framework: A Step‑By‑Step Guide [2025] [https://www.ewsolutions.com/data-quality-framework/]
- 91. GB/T 45214-2025 - 国家标准全文公开 [https://openstd.samr.gov.cn/bzgk/std/newGbInfo?hcno=487F7030FA30F18F4B4401E463FF2EA0]
- 92. The 10 Best Data Quality Assessment Tools Of August 2025 [https://www.montecarlodata.com/blog-best-quality-assessment-tools/]
- 93. 如何衡量数据准确性- IDBS [https://www.idbs.com/zh/%E7%9F%A5%E8%AF%86%E5%BA%93/%E5%A6%82%E4%BD%95%E8%A1%A1%E9%87%8F%E6%95%B0%E6%8D%AE%E7%9A%84%E5%87%86%E7%A1%AE%E6%80%A7/]
- 94. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 95. THE PREANALYTICAL ERRORS: A CONTINUOUS… [https://ascls.org/the-preanalytical-errors/]
- 96. Sample Integrity from Collection to Results [https://www.labmanager.com/sample-integrity-from-collection-to-results-34600]
- 97. The Ultimate Guide to Effective Sample Management in ... [https://www.sptlabtech.com/blog/sample-management-ultimate-guide]
- 98. What to Freeze, What to Store at Room Temperature [https://k2sci.com/blogs/news/streamlining-the-cold-chain-storage-of-research-samples-what-to-freeze-what-to-store-at-room-temperature?srsltid=AfmBOorThp1_VT-zmS1ubUoN4yejnM1PxiYHeu5bObkds0JfADb8xJHT]
- 99. The procurement, storage, and quality assurance of frozen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3982909/]
- 100. Freezing and cold chain solutions for biologics [https://www.susupport.com/blogs/knowledge/freezing-cold-chain-solutions-biologics-best-practices]
- 101. What does each cap color say about your sample? [https://micronic.com/blog-posts/what-does-each-cap-color-say-about-your-sample/]
- 102. 10 Steps To Streamline Your Specimen Collection Today [https://www.diagnosticsupportservices.com/blog/10-secrets-to-streamlining-your-specimen-collection-process]
- 103. Our Guide to Optimizing Biobank Sample Management [https://www.scisure.com/blog/guide-optimising-biobank-sample-management]
- 104. Frequently Asked Questions - Research Data Management at ... [https://libguides.tru.ca/rdm/faq]
- 105. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOooI59nlpli-UkkSGTcdNrFYBWGuFMYocTrOWgRy32D8ZF2bMinX]
- 106. Chain-of-Custody Best Practices for Election Equipment & Other Critical Assets in Government [https://www.facilityos.com/blog/chain-of-custody-best-practices-for-election-equipment-other-critical-assets-in-government]
- 107. Continuous Quality Improvement - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK559239/]
- 108. A scoping review of continuous quality improvement in ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-024-10828-0]
- 109. Continuous Quality Improvement (CQI): Driving ... [https://www.6sigma.us/six-sigma-in-focus/continuous-quality-improvement-cqi/]
- 110. Ultimate Guide to Lab Sample Management: Best Practices [https://www.qi-a.com/learning-center/lab-sample-management-guide/]