Preserving Parasite Integrity: Advanced Strategies to Prevent Specimen Deterioration in Biomedical Research
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on preventing specimen deterioration in parasitology.
Preserving Parasite Integrity: Advanced Strategies to Prevent Specimen Deterioration in Biomedical Research
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on preventing specimen deterioration in parasitology. It synthesizes current evidence on preservation mediums, collection methodologies, and storage protocols to maintain specimen integrity for both morphological and molecular analyses. The scope covers foundational principles of parasite degradation, practical application of preservation techniques, troubleshooting for common pre-analytical errors, and a comparative validation of traditional versus modern diagnostic platforms. By addressing critical pre-analytical variables, this resource aims to enhance diagnostic reliability, ensure reproducible research outcomes, and support the development of robust parasitological assays in clinical and pharmaceutical settings.
The Science of Specimen Degradation: Understanding Parasite Vulnerability and Preservation Fundamentals
In parasitology, the integrity of collected specimens is a foundational requirement for accurate diagnosis and reproducible research. Rapid degradation of samples post-collection directly compromises diagnostic sensitivity by altering morphological features, breaking down antigenic targets, and causing nucleic acid fragmentation. This degradation manifests as false-negative results, reduced accuracy in parasite identification, and ultimately, an inability to replicate experimental findings across different laboratories. The challenges are particularly acute in field conditions and resource-limited settings where controlled storage is often unavailable. Understanding and mitigating these degradation pathways is therefore not merely a technical concern, but a prerequisite for generating reliable data in parasitology education, research, and drug development [1] [2].
Understanding the Degradation Challenge
Primary Mechanisms of Specimen Degradation
Parasitology specimens are vulnerable to several environmental and intrinsic factors that drive their degradation. The table below summarizes the key mechanisms and their specific impacts on diagnostic targets.
Table 1: Key Mechanisms of Specimen Degradation and Their Impacts
| Degradation Mechanism | Primary Effects on Specimen | Impact on Diagnostic Targets |
|---|---|---|
| Enzymatic Activity | Autolysis (self-digestion) of tissues and cells; breakdown of proteins and nucleic acids [2]. | Degradation of antigen epitopes for immunological tests; fragmentation of DNA/RNA for molecular assays [3]. |
| Oxidation | Damage to proteins, lipids, and nucleic acids via reactive oxygen species [4]. | Alteration of protein antigens, reducing antibody binding affinity in immunoassays [4]. |
| Microbial Putrefaction | Overgrowth of saprophytic bacteria and fungi consuming the specimen [2]. | Destruction of parasite structures; consumption of parasite DNA/RNA; obscuring of morphological details [2]. |
| Desiccation | Loss of moisture, leading to structural collapse and crystallization of biomolecules [2]. | Shriveling of helminth eggs and larval stages, making them unrecognizable under microscopy [2]. |
| Photolysis | Breakdown of molecules due to exposure to light, particularly UV radiation [4]. | Loss of fluorescence in labeled assays; bleaching of pigments in parasites like Plasmodium [4]. |
Consequences for Diagnostic Sensitivity
The practical consequence of these degradation processes is a marked decline in diagnostic sensitivity. For example, the viability of first-, second-, and third-stage larvae of nematodes from the Ancylostomatidae and Strongyloididae families is rapidly lost if fecal samples are frozen or dried immediately after collection, as these larvae require specific conditions for concentration techniques like the Baermann apparatus to work effectively. This can directly lead to false-negative results [2]. Similarly, morphological identification of adult worms is hampered if they are preserved incorrectly; placing worms directly in ethanol or cold buffer causes muscle contraction, distorting key taxonomic structures and leading to misidentification [2]. For molecular methods, which are increasingly central to parasitology, DNA degradation begins immediately after a sample is produced and accelerates at higher temperatures, directly reducing the sensitivity of PCR and other amplification techniques [2].
Troubleshooting Guides & FAQs
This section addresses common, specific challenges faced by researchers in managing specimen degradation.
FAQ 1: What is the single most critical step to ensure the reproducibility of parasitological results from field-collected samples?
Answer: The most critical step is the immediate stabilization and appropriate preservation of the sample based on the intended downstream analysis. There is no universal preservative, and the choice must be tailored to the diagnostic or research method planned. For instance, sample storage at room temperature is suitable for analysis within 24 hours, but DNA degradation begins immediately. For molecular studies, freezing at -20°C is the preferred method, though some larval forms may lose viability. The key to reproducibility is meticulously documenting the time of collection, the preservation method, and the time to final storage, and ensuring these protocols are uniform across all sample collections in a study [2].
FAQ 2: Our laboratory frequently obtains conflicting results when using molecular versus microscopic methods on the same batch of samples. Could degradation be a factor, and how can we troubleshoot this?
Answer: Yes, differential degradation is a likely factor. Microscopy relies on intact morphological structures, while molecular methods require high-quality nucleic acids. These components degrade at different rates.
Troubleshooting Guide:
- Problem: Positive microscopy but negative PCR.
- Possible Cause: Inhibitors in the sample or poor DNA extraction efficiency.
- Solution: Include an internal control in the PCR reaction to detect inhibitors. Re-optimize the DNA extraction protocol, including mechanical lysis for tough cysts or oocysts.
- Problem: Negative microscopy but positive PCR.
- Possible Cause: The parasites are degraded and no longer morphologically identifiable, but their DNA is still intact and detectable.
- Solution: This highlights the higher sensitivity of PCR for degraded samples. Standardize the time between collection and analysis to minimize this discrepancy and establish a clear criterion for a positive result.
- General Action: Always record the time lapse between sample collection and processing for both analyses. Using a multiplex PCR approach that can detect several parasites simultaneously can also help clarify ambiguous results [1] [2].
FAQ 3: For long-term biobanking of parasitic specimens, what preservation method best balances the needs for morphological, molecular, and immunological studies?
Answer: A single method is often insufficient for multi-modal research. The best practice involves tripartite preservation:
- For Morphology: Fixation in 10% neutral buffered formalin is the gold standard for preserving morphological detail for histology.
- For Molecular Biology: Preservation in 95%-100% ethanol or freezing at -80°C is optimal for maintaining DNA integrity. RNA requires immediate stabilization in RNAlater or flash-freezing in liquid nitrogen.
- For Immunology: Freezing at -80°C is generally best for preserving protein antigens for western blot or ELISA. Note that formalin fixation can cross-link and mask epitopes, making it unsuitable for many immunological assays [2].
Table 2: Optimal Sample Preservation Methods by Downstream Application
| Application | Recommended Method | Key Considerations |
|---|---|---|
| Microscopy (Ova/Parasite) | 10% Formalin, SAF, PVA (for fresh samples) [1] | Room temperature storage is acceptable; avoids freezing artifacts. |
| Molecular (PCR, NGS) | 95-100% Ethanol, Freezing (-20°C or -80°C) [2] | Freezing is superior for long-term DNA/RNA integrity. |
| Culture | Analysis within 1-2 hours; no preservative [1] | Refrigeration (4°C) can briefly maintain viability. |
| Immunoassays | Freezing (-80°C), Specific commercial buffers | Avoid formalin; can denature protein targets. |
| Morphology (Adult Worms) | Warm PBS/Saline (to relax), then 70% Ethanol [2] | Prevents contraction and distortion of taxonomic structures. |
Standardized Experimental Protocols to Mitigate Degradation
Protocol: Collection and Preservation of Fecal Samples for Multi-Method Analysis
Principle: To standardize the collection of fecal specimens to maximize their utility for concurrent microscopic, molecular, and cultural diagnostics, while minimizing pre-analytical degradation.
Materials:
- Clean, leak-proof, wide-mouth containers
- Disposable gloves and applicator sticks
- Labels and waterproof pens
- Cooler with ice packs or liquid nitrogen for flash freezing
- Preservatives: 10% formalin, 95% ethanol, RNAlater
- Pre-portioned containers for sub-sampling
Procedure:
- Collection: Using an applicator stick, collect multiple portions of the fecal specimen, focusing on areas with mucus or visible abnormalities. Place them into the primary container.
- Immediate Sub-sampling (Within 1-2 hours of collection):
- For Microscopy: Aliquot 1-2 g of feces into a container with 10 mL of 10% formalin. Mix thoroughly.
- For Molecular Biology: Aliquot 1-2 g of feces into a container with 5-10 mL of 95% ethanol. Ensure the sample is fully submerged. Alternatively, flash-freeze a 0.5 g aliquot in a cryovial.
- For Culture/Baermann: Process the fresh sample immediately. If a delay is unavoidable, refrigerate (4°C) for no more than 24 hours. Do not freeze or preserve.
- Documentation: Record the time of collection, time of preservation, and any preservatives used.
- Storage and Transport: Store formalin-fixed samples at room temperature. Store ethanol-preserved and frozen samples at -20°C (short-term) or -80°C (long-term). Transport on ice or with cold packs [2].
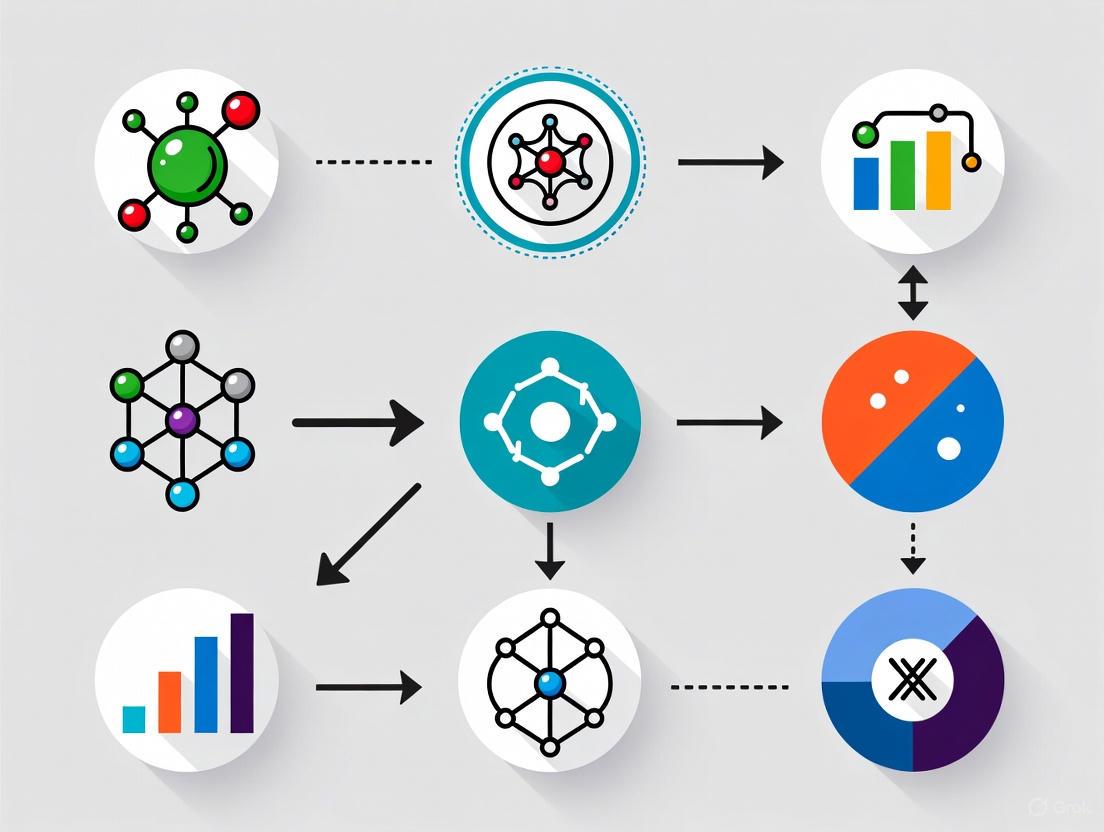
Workflow: Integrity Management of Parasitology Specimens
The following diagram illustrates the critical decision points and pathways for handling parasitology specimens to ensure integrity from collection to analysis.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for preventing specimen degradation in parasitology research.
Table 3: Essential Reagents for Specimen Integrity in Parasitology Research
| Reagent/Material | Function | Specific Use-Case |
|---|---|---|
| 95-100% Ethanol | Nucleic acid preservation and fixation [2]. | Ideal for long-term storage of feces, tissue, or arthropod vectors for DNA-based PCR and sequencing. |
| RNAlater Stabilization Solution | Stabilizes and protects cellular RNA [2]. | Preserving gene expression profiles in parasite-infected tissues; critical for transcriptomic studies. |
| 10% Neutral Buffered Formalin | Tissue fixation and morphological preservation [2]. | Gold standard for histopathological examination of tissue sections containing parasites. |
| Phosphate-Buffered Saline (PBS) | Isotonic buffer for temporary specimen maintenance [2]. | Washing parasites collected from cultures; relaxing adult helminths before preservation to prevent contraction. |
| Polyvinyl Alcohol (PVA) | Preservative and adhesive for fecal specimens [1]. | Fixing protozoan trophozoites and cysts in stool for permanent staining (e.g., Trichrome stain). |
| Sodium Acetate-Acetic Acid-Formalin (SAF) | All-purpose fixative for fecal specimens [1]. | Suitable for concentration procedures and permanent staining; allows for later molecular testing. |
| Hydrogen Peroxide (3%) | Oxidative stressor in forced degradation studies [4]. | Modeling oxidative degradation of drug compounds or diagnostic antigens in stability studies. |
Parasite Biology and Vulnerabilities
Understanding the fundamental biology and life cycles of parasites is the first step in identifying their critical vulnerabilities for both therapeutic intervention and specimen preservation.
Hookworm Biology and Life Cycle
Hookworms are nematode parasites with a direct life cycle involving several distinct developmental stages. The primary species infecting humans are Ancylostoma duodenale and Necator americanus [5] [6]. The table below summarizes the key stages and their characteristics:
Table 1: Hookworm Life Cycle Stages and Vulnerabilities
| Stage | Duration | Key Characteristics | Potential Vulnerabilities |
|---|---|---|---|
| Egg | 24-48 hours to hatch [7] | Passed in feces, thin-shelled oval shape [8] | Environmental conditions (desiccation, temperature extremes) [7] |
| Rhabditiform Larva (L1) | 1-2 days after hatching [5] | Feeds on feces, non-infective [5] | Limited survival outside host, requires specific conditions |
| Filariform Larva (L3) | 3-4 weeks in soil [5] | Developmentally arrested, infective stage [6] | Desiccation, direct sunlight, salt water [5] |
| Adult Worm | 1-5 years [5] | Inhabits small intestine, blood-feeding [7] | Blood-feeding mechanism, attachment to intestinal mucosa |
The life cycle begins when eggs are passed in human feces and deposited into soil [5]. Under appropriate warm, moist, shaded conditions, eggs hatch into first-stage rhabditiform larvae (L1) within 1-2 days [7] [5]. These larvae feed on feces and undergo two molts over 5-10 days to become infective filariform larvae (L3) [5]. These L3 larvae are developmentally arrested and can survive in damp soil for several weeks awaiting a host [5].
Infection occurs when L3 larvae penetrate human skin, most commonly through the feet [5] [6]. Upon penetration, larvae receive host-specific signals that cause them to resume development and secrete bioactive polypeptides [6]. The larvae migrate through the bloodstream to the lungs, break into alveoli, ascend the bronchial tree to the pharynx, and are swallowed [5] [8]. During pulmonary migration, they may cause Löffler syndrome with cough, wheezing, and eosinophilia [8].
Once in the small intestine, larvae undergo two further molts, developing a buccal capsule and attaining adult form [5]. Adult worms attach to the mucosal layer of the small intestine using teeth (A. duodenale) or cutting plates (N. americanus) [5] [6]. They release hydrolytic enzymes and anticoagulants that facilitate blood feeding and cause continuous blood loss from the host [5]. Adult worms become sexually mature in 3-5 weeks, after which females begin producing thousands of eggs daily that are passed in feces to continue the cycle [5].
Dientamoeba fragilis Biology and Challenges
Dientamoeba fragilis is a trichomonad parasite with a poorly understood life cycle and transmission mechanism [9] [10]. Unlike most intestinal protozoa, it appears to exist only in the trophozoite stage, with no confirmed cyst stage [10] [11]. This creates significant research challenges as the parasite is sensitive to aerobic environments and quickly degrades when placed in saline, tap water, or distilled water [11].
The parasite inhabits the mucosal crypts of the large intestine, from the cecum to the rectum, typically located close to the mucosal epithelium [11]. It is not considered invasive and does not cause cellular damage, but may invoke an eosinophilic inflammatory response that leads to superficial colonic mucosal irritation and symptoms [11].
Transmission mechanisms remain incompletely understood, with conflicting evidence. Proposed routes include direct fecal-oral spread, possible co-infection with pinworm (Enterobius vermicularis) eggs, and potential zoonotic transmission from pigs, which have been identified as natural hosts [10] [11]. The absence of a confirmed cyst stage and rapid degradation outside the host present significant challenges for both research and diagnostic purposes [11].
Specimen Preservation and Experimental Methodologies
Proper preservation of parasite specimens is critical for accurate research and diagnostic outcomes. Different parasites require specific handling protocols to maintain morphological integrity.
Hookworm Preservation Protocols
Stool Specimen Processing for Egg Identification:
- Collect fresh stool specimens in clean, dry containers
- Process within 24-48 hours for optimal egg viability [8]
- Use concentration techniques (e.g., formalin-ethyl acetate) for light infections
- Prepare permanently stained smears for morphological examination
- Maintain specimens at 4°C if immediate processing isn't possible
Adult Worm Preservation:
- Collect worms during endoscopic procedures or post-treatment
- For morphological studies, fix in 10% formalin or 70% ethanol
- For molecular studies, freeze at -80°C or preserve in RNA-later
- For teaching collections, consider plastination using S10 technique [12]
Plastination Protocol for Macroparasites (S10 Technique):
- Fixation: Specimens are fixed in 10% formalin
- Dehydration: Sequential dehydration in cold acetone baths (-25°C)
- Impregnation: Forced impregnation with silicone polymer under vacuum
- Curing: Gas curing with dichlorodimethylsilane [12]
This technique produces dry, odorless specimens free of carcinogenic preservatives, though some species may experience collapse requiring protocol modifications [12].
D. fragilis Preservation Challenges and Solutions
D. fragilis presents unique preservation challenges due to its lack of a cyst stage and sensitivity to environmental conditions [11]. The following workflow outlines the critical preservation pathway:
Critical Preservation Protocol:
- Immediate Processing: Preserve stool specimens immediately after passage using appropriate fixatives [11]
- Multiple Specimens: Collect a minimum of three fecal specimens every other day due to intermittent shedding [10]
- Fixative Selection: Use polyvinyl alcohol (PVA) or sodium acetate-acetic acid-formalin (SAF) fixatives
- Staining Requirements: Always prepare permanently stained smears (trichrome or iron-hematoxylin) for examination under oil immersion (1000×) [10]
- Molecular Preservation: For PCR studies, preserve samples in specific nucleic acid preservatives or freeze at -80°C
Culture Techniques: Though not routine in clinical laboratories, D. fragilis can be cultured from clinical specimens, providing another preservation method for research purposes [10].
Research Reagent Solutions
The following table outlines essential research reagents and their applications in parasitology research, particularly for hookworms and D. fragilis:
Table 2: Essential Research Reagents for Parasitology Studies
| Reagent/Category | Specific Examples | Research Application | Preservation Considerations |
|---|---|---|---|
| Fixatives | 10% Formalin, PVA, SAF, 70% ethanol [12] | Morphological preservation | Formalin preferred for histology; ethanol for molecular work |
| Staining Reagents | Trichrome stain, Iron-hematoxylin, Kato-Katz reagents [10] [13] | Microscopic identification | Trichrome essential for D. fragilis; Kato-Katz for egg quantification |
| Molecular Biology Kits | DNA/RNA extraction kits, PCR master mixes, RT-PCR reagents | Species identification, genotyping | RNase-free environment for RNA work; specific preservatives for nucleic acids |
| Culture Media | Locke-egg-serum medium, other trichomonad media [10] | Parasite propagation and maintenance | Strict temperature control; regular subculturing |
| Anthelmintic Agents | Albendazole, Mebendazole, Pyrantel pamoate [8] [13] | Drug efficacy studies | Proper storage conditions; solubility considerations for in vitro studies |
| Protease Inhibitors | EDTA, protease inhibitor cocktails | Enzyme function studies | Temperature-sensitive; aliquot to avoid repeated freeze-thaw cycles |
| Silicone Polymers | Biodur S10/S15 [12] | Plastination for teaching collections | Specific curing protocols; vacuum impregnation requirements |
Troubleshooting Common Research Scenarios
Hookworm-Specific Issues
Problem: Rapid degradation of hookworm eggs in stool samples Solution: Process stool samples within 24 hours of collection. If delayed, refrigerate at 4°C but avoid freezing. Use concentration techniques for low egg burdens [8].
Problem: Inconsistent egg counts in quantitative studies Solution: Utilize standardized egg counting methods like Kato-Katz technique. Account for day-to-day variation in egg output by multiple sampling. Be aware that egg production varies by species (A. duodenale: 10,000-30,000 eggs/female/day; N. americanus: 5,000-10,000 eggs/female/day) [5].
Problem: Poor recovery of adult worms for molecular studies Solution: Collect worms post-treatment with anthelmintics. Preserve immediately in 70% ethanol or RNA-later for genetic studies. For morphological studies, fix in hot (60°C) 70% ethanol or 10% formalin.
D. fragilis-Specific Issues
Problem: False-negative results in stool examination Solution: Collect multiple stool specimens (minimum of three) every other day due to intermittent shedding [10]. Use permanent stains and examine under oil immersion (1000×). Consider PCR-based detection for improved sensitivity.
Problem: Rapid degradation of trophozoites after passage Solution: Preserve specimens immediately in appropriate fixatives. Avoid saline, tap water, or distilled water which cause rapid disintegration [11]. Process fresh specimens within a few hours of collection.
Problem: Inability to maintain long-term cultures Solution: Use specialized trichomonad media with regular subculturing. Consider co-culture systems or addition of antimicrobial agents to prevent bacterial overgrowth.
Advanced Experimental Workflows
For researchers investigating parasite biology and drug development, the following integrated workflow provides a framework for comprehensive study:
Target Identification Strategies
Hookworm Molecular Targets:
- Blood-feeding Mechanism: Metalloproteases and anticoagulant peptides that facilitate blood digestion [6]
- Larval Activation Proteins: Asparaginyl-tRNA synthetase and other secreted proteins released during host invasion [6]
- Neuronal Signaling Pathways: cGMP-dependent pathways involved in larval development resumption [6]
- Immune Evasion Molecules: Protease inhibitors and T-cell apoptosis inducers that enable chronic infection [13]
D. fragilis Research Targets:
- Metabolic Pathways: Unique enzymes identified through transcriptome sequencing [14]
- Kinome Analysis: Protein kinases potential drug targets [14]
- Degradome Characterization: Peptidases with potential pathogenicity roles [14]
- Virulence Factors: Mechanisms of pathogenicity despite non-invasive nature [14]
Drug Efficacy Testing Protocols
In vitro Hookworm Larval Assay:
- Collect fresh fecal samples containing hookworm eggs
- Incubate at 27°C for 7-10 days to allow development to L3 larvae
- Prepare drug dilutions in appropriate solvents
- Expose L3 larvae to various drug concentrations for 24-48 hours
- Assess larval motility and viability using standardized scoring systems
- Calculate LC50 values for compound comparison
Antigen Detection Assays for D. fragilis:
- Develop specific monoclonal antibodies against surface antigens
- Establish ELISA-based detection systems for culture supernatants
- Validate with clinical specimens of known status
- Correlate antigen levels with clinical symptoms and parasite burden
FAQs: Addressing Critical Research Challenges
Q: What is the most vulnerable stage in the hookworm life cycle for intervention? A: The L3 larval stage during skin penetration and migration is particularly vulnerable. At this stage, larvae are transitioning from free-living to parasitic forms and secreting various proteins essential for host invasion. These secreted proteins represent potential targets for vaccines or drugs [6].
Q: Why is D. fragilis so difficult to maintain in research settings? A: The primary challenges include: (1) absence of a confirmed cyst stage, limiting long-term survival; (2) sensitivity to aerobic environments; (3) rapid degradation in water-based solutions; and (4) lack of optimized axenic culture systems. Immediate preservation in appropriate fixatives and specialized culture media are essential [11].
Q: What preservation method is most suitable for teaching collections? A: Plastination using the S10 technique offers significant advantages: specimens are dry, odorless, maintain morphological features, and eliminate exposure to carcinogenic formaldehyde. However, protocol modifications may be needed for certain species prone to collapse [12].
Q: How can molecular techniques overcome limitations in parasite detection? A: PCR-based methods offer: (1) increased sensitivity for low-level infections; (2) species-specific identification; (3) ability to use fixed specimens; and (4) quantification of parasite burden. For D. fragilis, real-time PCR has shown superior sensitivity compared to microscopic examination [10].
Q: What are the key considerations when testing anthelmintic efficacy? A: Critical factors include: (1) parasite species and developmental stage; (2) drug solubility and stability; (3) appropriate outcome measures (egg reduction vs. worm burden); (4) accounting for natural variation in egg output; and (5) considering potential drug resistance mechanisms [8] [13].
Within parasitology education and research, the paramount goal is to prevent the deterioration of valuable and often irreplaceable biological specimens. The integrity of these specimens is foundational for accurate morphological diagnosis, training future parasitologists, and advancing research. Central to achieving this goal are preservatives, with formalin and ethanol being the most widely used. Understanding their mechanisms of action on cellular and molecular levels is not merely academic; it is crucial for selecting the right preservative for the intended application, whether for long-term morphological preservation, molecular analysis, or museum display. This technical support center delves into the science behind these common preservatives, providing troubleshooting guidance and protocols to empower researchers in making informed decisions for their specific experimental needs.
Core Mechanisms of Action
Formalin: The Cross-Linking Fixative
Formalin, an aqueous solution of formaldehyde, acts primarily through covalent cross-linking of biomolecules [15]. Its action can be broken down into a multi-step process:
- Initial Reaction: Formaldehyde rapidly reacts with primary amino groups (e.g., in lysine residues), sulfhydryl groups, and amide groups in proteins to form hydroxymethyl derivatives [16].
- Cross-linking: These hydroxymethyl groups then undergo slower condensation reactions with other nearby nitrogen atoms (e.g., from arginine, tryptophan, or tyrosine) or other reactive groups, forming stable methylene bridges (-CH2-) [16] [17]. This creates a three-dimensional network of cross-linked proteins.
Cellular and Molecular Consequences:
- Protein Immobilization: The cross-linking network stabilizes and hardens the tissue architecture, rendering proteins insoluble and inactivating enzymes that cause autolysis and decay [15] [17].
- Morphological Preservation: This cross-linking is exceptionally effective at preserving the fine structural details of cells and tissues, which is why it is the gold standard for histopathology [16].
- Nucleic Acid Impact: While it also reacts with and cross-links nucleic acids, this process fragments RNA and makes both DNA and RNA difficult to extract in a high-quality, intact form [18].
- Antigen Masking: Extensive cross-linking can sterically hinder antibody binding to specific epitopes, reducing immunorecognition in techniques like immunohistochemistry [16].
Diagram 1: Formalin's protein cross-linking mechanism.
Ethanol: The Dehydrating Agent
Ethanol (and other alcohols like methanol) functions primarily through dehydration and precipitation [17].
- Dehydration: Ethanol, being miscible with water, rapidly replaces water in the cells and tissues.
- Protein Precipitation: This dehydration disrupts the hydrogen-bonding network that maintains the tertiary and quaternary structures of proteins. This causes protein denaturation and precipitation, effectively halting enzymatic activity [17].
Cellular and Molecular Consequences:
- Bacterial Inhibition: By dehydrating and denaturing proteins, ethanol kills bacteria and fungi, preventing microbial decomposition [15] [19].
- Macromolecule Precipitation: It precipitates proteins and nucleic acids, which can help preserve them in a relatively stable state. Unlike formalin, it does not fragment RNA, allowing for the recovery of high-quality RNA for molecular studies [18].
- Structural Alteration: The precipitating action can cause tissue shrinkage and hardening. It is less effective than formalin at preserving fine cytological detail over the very long term and can leach color from specimens [19].
Diagram 2: Ethanol's protein dehydration and precipitation mechanism.
Comparative Data and Protocols
Quantitative Comparison of Preservative Effects
The choice between formalin and ethanol has measurable consequences for downstream analyses. The table below summarizes key comparative data.
Table 1: Quantitative Comparison of Formalin vs. Ethanol Effects
| Parameter | Formalin (10% NBF) | 70% Ethanol | Experimental Context |
|---|---|---|---|
| RNA Yield | Negligible quantity recovered [18] | ~70% of yield from fresh-frozen tissue [18] | Laser capture microdissected brain tissue [18] |
| RNA Integrity | Composed of low-MW fragments; RT-PCR often fails [18] | Integrity comparable to fresh frozen; RT-PCR successful [18] | Laser capture microdissected brain tissue [18] |
| Immunorecognition | Progressive loss with fixation >18h; complete loss for some antigens by 108h [16] | Maintained after transfer from 12h NBF fixation [16] | DU145 & SKOV3 cell lines, antibodies to PCNA, Ki67, cytokeratins [16] |
| Preservation Stability | Effective for several years; may discolor specimens [19] | Effective for several years; leaches color from specimens [19] | Long-term museum conservation [19] |
| Ideal Use Case | Morphological preservation for histology; long-term storage of structural detail [15] [16] | RNA/DNA preservation; post-fixation storage for IHC; disinfecting surfaces [16] [18] | Varies by experimental goal |
Key Experimental Protocols
Protocol 1: Optimized Fixation for Immunohistochemistry
This protocol, derived from cell line studies, demonstrates how to preserve immunorecognition by transferring specimens from formalin to ethanol [16].
Methodology:
- Fixation: Fix cells or thin (≤3mm) tissue samples in 10% Neutral Buffered Formalin (NBF) for 12 hours at room temperature.
- Transfer: Do not leave specimens in NBF indefinitely. After 12 hours, transfer them to 70% ethanol for storage until processing.
- Storage in Ethanol: Specimens can be stored in 70% ethanol for extended periods (tested up to 168 hours, or 7 days) without the significant loss of immunorecognition that occurs with prolonged formalin fixation [16].
- Processing: After storage in ethanol, process the tissues through standard dehydration and paraffin embedding.
Troubleshooting Note: Prolonged fixation in NBF beyond 18-36 hours leads to increased cross-linking and masking of epitopes for antibodies like PCNA and Ki67, resulting in decreased or complete loss of immunostaining [16].
Protocol 2: Preservation for RNA Analysis
This protocol highlights the superiority of ethanol for gene expression studies [18].
Methodology:
- Immersion Fixation: Immerse tissue samples (e.g., brain tissue) in 70% ethanol.
- Fixation Duration: Fixation can be performed at 4°C for up to 2 weeks without degrading RNA yield or quality [18].
- Processing: Process the ethanol-fixed tissues to paraffin embedding using standard protocols.
- RNA Extraction: Extract RNA using standard methods like TRIzol. The resulting RNA will be of high integrity, suitable for RT-PCR and cDNA microarray analysis, even after laser capture microdissection [18].
Troubleshooting Note: RNA extracted from formalin-fixed tissues is highly fragmented and often yields negligible amounts, making it unreliable for downstream molecular applications like RT-PCR [18].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Specimen Preservation
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| 10% Neutral Buffered Formalin (NBF) | Cross-linking fixative for superior morphological preservation. | Prevents acid formalin hematin pigment artifact; the buffer maintains neutral pH [15] [16]. |
| 70% Ethanol | Dehydrating fixative and storage medium. | Optimal concentration for penetration and protein precipitation; used for RNA preservation and storing formalin-fixed samples [16] [18]. |
| Polyvinyl Alcohol (PVA) | Preservative for fecal specimens in parasitology. | Contains a plastic resin that adheres stool to slides; allows permanent staining but contains mercury [20]. |
| Sodium Acetate-Acetic Acid-Formalin (SAF) | All-purpose fecal preservative. | Used for concentration and stained smears; mercury-free but has poor adhesive properties [20]. |
| Methanol | Alcohol-based fixative and permeabilizing agent. | Often used as a stabilizer in formalin; pre-fixes blood smears for shipment; denatures proteins [15] [17]. |
| Triton X-100 | Non-ionic detergent for permeabilization. | Disrupts lipid bilayers to allow antibody access to intracellular antigens after fixation [17]. |
| Saponin | Cholesterol-binding detergent for permeabilization. | Selectively permeabilizes plasma membranes without disrupting organelles, useful for intracellular staining [17]. |
Troubleshooting Guides and FAQs
FAQ 1: Why did my immunostaining fail even though I used a validated antibody on formalin-fixed tissue?
Answer: The most likely cause is over-fixation. While 10% NBF is excellent for morphology, fixation for longer than 18-36 hours can lead to excessive cross-linking, which masks the epitope your antibody recognizes [16].
- Solution: Limit fixation time in NBF to 6-12 hours for thin tissues. For unavoidable delays, transfer the tissue from formalin to 70% ethanol after 12 hours. This "holds" the tissue in a state that preserves immunorecognition much better than prolonged formalin storage [16].
FAQ 2: We need to perform both histological examination and RNA sequencing from the same rare parasite specimen. What is the best preservation strategy?
Answer: This is a common dilemma as the fixatives are mutually exclusive for a single sample. Formalin destroys RNA integrity, while ethanol provides inferior morphology [18].
- Solution: If possible, divide the specimen. Place one part in 10% NBF for optimal histology and another part in 70% ethanol for optimal RNA extraction [18]. If the specimen cannot be divided, 70% ethanol is the compromise, as it provides adequate histology for many diagnostic purposes and preserves high-quality RNA [18].
FAQ 3: In parasitology, what is the best preservative for stool specimens if I want to do both a concentration test and a permanent stain?
Answer: No single preservative is perfect, but Sodium Acetate-Formalin (SAF) and Polyvinyl Alcohol (PVA) are the top choices.
- SAF is mercury-free and can be used for both concentration and stained smears, though staining quality with trichrome may be inferior to PVA [20].
- PVA is the traditional choice for excellent permanent stained smears but contains mercury and is less ideal for concentrating some helminth eggs [20]. Your choice may depend on local regulations regarding mercury disposal and the specific parasites you are targeting.
FAQ 4: My tissue specimen preserved in ethanol has become shrunken and brittle. Is this normal?
Answer: Yes, some degree of shrinkage and hardening is a normal consequence of ethanol's dehydrating and precipitating action [19] [17]. This is a trade-off for its superior nucleic acid preservation. For display purposes where texture and color are critical, museums are experimenting with alternative fluids like fluorinated hydrocarbons, but these are not yet common in research laboratories [19].
Core Concepts: The Cold Chain and Molecular Integrity
What is the cold chain in the context of parasitology research?
The cold chain is an uninterrupted series of temperature-controlled storage and distribution activities designed to preserve the quality and integrity of biological materials, such as parasitic specimens. In parasitology education research, this ensures that samples like stool specimens remain viable for microscopic analysis, maintaining the morphological details of ova, cysts, larvae, and trophozoites for accurate identification and study [21] [22].
Why are time and temperature so critical for preserving parasitic specimens?
Temperature control is fundamental because exposure to unsuitable temperatures accelerates molecular degradation. Key molecular interactions affected include:
- Protein and Enzymatic Activity: Higher temperatures increase protease activity, leading to the breakdown of parasitic proteins and loss of morphological integrity [23].
- Water and Ice Transitions: During freezing, ice crystal formation can physically damage cellular structures. Rapid freezing or temperature fluctuations can cause ice crystals to expand and puncture cell membranes, destroying trophozoites and delicate cysts [23].
- Solute Exclusion: As water freezes, solutes are concentrated in the remaining liquid, creating a hypertonic environment that can denature proteins and disrupt cellular structures [23].
Time is a multiplier of these effects. The longer a specimen is exposed to a non-ideal temperature, the greater the cumulative damage, ultimately leading to loss of sample viability and unreliable research data [24].
Troubleshooting Guides
FAQ: How can I prevent my wet mount preparations from drying out during microscopy sessions?
Problem: Conventional saline or iodine wet mounts dry out quickly, especially in tropical climates, making detailed observation and demonstration difficult [22].
Solution: Use a methylene blue-glycerol wet mount preparation.
Detailed Protocol:
- Reagent Preparation: Prepare a methylene blue-glycerol solution by mixing methylene blue dye with glycerol. A 25% glycerol concentration is effective for prolonging slide life [22].
- Slide Preparation: Place a drop of the methylene blue-glycerol solution on a clean microscope slide. Add a small, thick smear of fresh, unpreserved faecal specimen and mix gently. Place a coverslip over the mixture [22].
- Examination: Examine the entire preparation under low-power (10x) and high-power (40x) objectives [22].
Why it Works: Glycerol is hygroscopic, absorbing water molecules from the environment and preventing the mount from drying out. This provides a semipermanent preparation that can last for hours, compared to minutes for conventional mounts [22]. Methylene blue stains internal structures of parasites, providing excellent contrast and making them easier to identify against background debris [22].
FAQ: Our lab has experienced a temperature excursion in our ultra-low freezer. How do I assess the impact on stored specimens?
Problem: A freezer alarm indicates that stored samples, including purified nucleic acids from parasites, were exposed to elevated temperatures.
Solution: Execute a systematic impact assessment and triage plan.
Action Plan:
- Immediate Containment: Do not open the freezer door until the temperature has stabilized. If possible, transfer samples to a backup unit while assessing the primary unit [24].
- Data Review: Download and review data from the continuous temperature monitoring system. Determine the exact duration and magnitude of the temperature deviation [25] [24].
- Sample Triage:
- Check Stability Data: Refer to stability studies for the specific specimen types. The table below summarizes general risks, but lab-specific data is crucial.
- Prioritize High-Risk Samples: Identify samples most susceptible to degradation, such as RNA, proteins, or live cultures [23] [26].
- Perform Quality Control: Select a representative subset of samples for integrity testing (e.g., RNA Integrity Number (RIN) analysis, protein assays, or viability staining) before using them in critical experiments [23].
Table: General Risk Assessment for Specimens After Temperature Excursion
| Specimen Type | Typical Storage Temp. | Potential Impact of Transient Warming | Recommended Action |
|---|---|---|---|
| RNA / Viral RNA | -80°C or liquid nitrogen | High risk of degradation by RNases; loss of integrity for PCR [23] | Perform QC (e.g., Bioanalyzer); prioritize for re-extraction if QC fails. |
| DNA | -20°C to -80°C | Lower risk; potential for slow degradation over time [26] | Generally stable; check by gel electrophoresis or PCR if concerned. |
| Proteins | -80°C | Risk of aggregation, loss of activity, or protease degradation [23] | Test functionality with an activity assay or Western blot. |
| Fixed Parasite Ova/Cysts | 2-8°C (refrigerated) | Lower risk from short excursions; morphology may be preserved [22] | Inspect under microscope for morphological changes. |
| Live Parasites/Cultures | Specific culture conditions | High risk of death or reduced viability [26] | Assess viability and subculture immediately. |
FAQ: What are the most common failure points in the cold chain during sample transport, and how can we mitigate them?
Problem: Samples arrive at the testing lab with evidence of temperature abuse, compromising their usability.
Solution: Implement proactive risk management at identified failure points.
Mitigation Strategies:
- Failure Point: Loading/Unloading (Dispatch/Receipt)
- Failure Point: Last-Mile Delivery
- Failure Point: Temperature Abuse in Transit
Cold Chain Failure Points & Solutions
Experimental Protocols & Best Practices
Detailed Protocol: Preserving Parasitic Morphology with Methylene Blue-Glycerol Mounts
This protocol is adapted from a published study evaluating techniques for intestinal parasite identification [22].
Principle: A combination of methylene blue dye and glycerol provides superior staining contrast for morphological details and prevents the rapid drying of wet mounts, facilitating accurate identification of parasites.
Materials Required:
- Fresh, unpreserved faecal specimen
- Microscope slides and coverslips
- Methylene blue dye
- Glycerol
- Physiological saline
- Lugol's iodine (for comparison)
- Compound microscope
Methodology:
- Prepare Staining Solution: Mix methylene blue dye with glycerol to create a 25% v/v glycerol solution.
- Create Smears:
- Prepare a saline wet mount and an iodine wet mount for initial comparison.
- For the test mount, place a drop of the methylene blue-glycerol solution on a slide. Add a larger volume of faeces to create a thick smear and apply a coverslip.
- Microscopic Examination:
- Systematically examine all mounts first under low-power (10x) and then high-power (40x) objectives.
- Document the clarity of morphological features, staining of internal structures, and contrast against artefacts.
- Assess Drying Time: Monitor the slides at ambient temperature (e.g., 25 ± 2°C) and record the time taken for the edges of the mount to show signs of drying.
Expected Results: The methylene blue-glycerol mount should provide clearer visualization of internal structures compared to saline and iodine mounts. Helminthic ova and cysts will be stained deep blue, offering excellent contrast. The preparation should remain intact for several hours, significantly longer than conventional mounts which may dry in under 10 minutes [22].
Best Practice: Temperature Mapping Storage Equipment
Objective: To identify temperature variations (hot/cold spots) within a storage unit (refrigerator, freezer, ultra-low freezer) to ensure all stored specimens are maintained within the required temperature range.
Methodology:
- Sensor Placement: Place calibrated temperature data loggers at critical locations defined in guidelines like those from WHO or ISPE. This includes the top, middle, and bottom shelves, near the door, vents, and in the center of the unit [25] [28].
- Study Duration: Run the study for a sufficient period (typically 24-72 hours) to capture normal operational cycles, including door openings and defrost cycles [28].
- Data Analysis: Download the data and create a map of the unit. Identify any locations where temperatures fall outside the validated range.
- Action: Based on the results, define the usable storage volume within the unit. Place the most temperature-sensitive specimens in the most stable zones. Repeat the mapping periodically (e.g., annually) or after any significant equipment maintenance [25] [28].
The Scientist's Toolkit: Essential Reagent Solutions
Table: Key Materials for Parasite Specimen Integrity
| Item | Function / Application | Key Consideration |
|---|---|---|
| Phase Change Materials (PCMs) | Maintain specific temp profiles (2-8°C, -20°C) during sample transport in passive shipping containers [27] [29]. | Must be pre-conditioned at the correct temperature before use to ensure performance [27]. |
| Cryogenic Vials | Long-term storage of samples at ultra-low temperatures (-80°C) or in liquid nitrogen vapor phase [26]. | Use screw-cap containers to prevent leakage and evaporation during long-term storage [26]. |
| Methylene Blue-Glycerol Solution | Creation of semi-permanent wet mounts for microscopy; provides contrast and prevents drying [22]. | A 25% glycerol concentration offers a good balance between preservation time and preventing morphological distortion [22]. |
| Vacuum-Insulated Packaging (VIP) | Provides superior thermal insulation for shipping high-value, temperature-sensitive specimens [27]. | Reduces thermal transfer from external conditions, extending the safe transit duration [27]. |
| IoT Data Loggers / Sensors | Continuous, real-time monitoring of temperature (and optionally humidity, shock) during storage and transport [27] [24]. | Enable proactive intervention via alerts; data is critical for regulatory compliance and investigating excursions [27] [25]. |
| Cryoprotectants | Chemicals (e.g., DMSO, Glycerol) added to cell suspensions or live parasites to protect against ice crystal damage during freezing [23]. | Must be optimized for specific cell types; often require controlled-rate freezing for maximum viability [23]. |
Parasite Specimen Handling Workflow
Optimized Preservation Protocols: A Practical Guide for Field and Laboratory Workflows
Frequently Asked Questions (FAQs)
Q1: What is the core trade-off between using formalin and ethanol for preserving parasitology specimens? Formalin is generally superior for long-term morphological studies as it preserves tissue structure by forming protein cross-links, making it ideal for microscopic identification. However, these cross-links fragment DNA, rendering samples unsuitable for most molecular studies. Ethanol, while it may cause some tissue dehydration and shrinkage, preserves DNA integrity effectively, enabling downstream genetic analyses like PCR and DNA barcoding [30] [31].
Q2: Can ethanol-preserved samples still be used for reliable morphological identification? Yes, under the right conditions. One study found that while formalin-preserved samples yielded a greater diversity of parasitic morphotypes, parasites in ethanol-preserved samples were still morphologically identifiable even after more than a year of storage [30] [31]. The key is that identification remains possible, though the quality of preservation for certain larval forms may be higher in formalin.
Q3: My primary goal is DNA analysis. Is formalin ever an option? For standard genetic analyses, formalin is not recommended. Research shows that RNA yield from formalin-fixed tissues is negligible and the RNA that is recovered is highly fragmented [32]. In contrast, RNA from ethanol-fixed tissues shows integrity comparable to that from fresh frozen specimens, making it suitable for techniques like RT-PCR and cDNA microarrays [32].
Q4: What concentration of ethanol is optimal for preserving specimens for molecular studies? High concentrations (e.g., 95% or 96% ethanol) are recommended for initial field preservation to denature proteins that might degrade DNA [30] [31] [33]. For very long-term storage, 70% ethanol is often used and has been shown to maintain DNA effectively while minimizing tissue brittleness [34] [33].
Q5: Are there any safety considerations when choosing a preservative? Yes. Formalin contains formaldehyde, which is toxic and a known carcinogen. It requires careful handling to prevent inhalation or skin contact. Ethanol is less toxic but is flammable and requires appropriate storage and shipping precautions [30] [31].
Troubleshooting Guides
Problem: Poor DNA Yield or Quality from Specimens
Potential Causes and Solutions:
- Cause: Use of formalin as a preservative.
- Solution: For future studies, preserve a portion of the sample in 95% ethanol. For existing formalin-fixed samples, be aware that DNA will be fragmented and may only be suitable for specialized assays designed for damaged DNA [32].
- Cause: Ethanol concentration was too low or sample was not adequately submerged.
- Cause: Prolonged storage at room temperature in suboptimal preservative.
- Solution: One study found that holding samples in 95% ethanol for up to six months at room temperature did not adversely affect DNA barcoding success. For maximum longevity, store samples in 70-95% ethanol in a cool, dark place [33].
Problem: Degraded Morphology Making Microscopic Identification Difficult
Potential Causes and Solutions:
- Cause: Preservation in ethanol, which can dehydrate and shrink tissues.
- Cause: Inadequate fixation time or volume of preservative.
Problem: Need to Perform Both Morphological and Molecular Analyses on a Single Sample
Solution: Ideally, partition the sample upon collection.
- Step 1: Divide the fresh sample into two halves.
- Step 2: Preserve one half in 10% formalin for morphological work.
- Step 3: Preserve the other half in 96% ethanol for molecular work. This is the methodology successfully employed in a comparative study of capuchin monkey parasites, allowing for direct comparison from the same host and time point [30] [31].
Data Presentation: Quantitative Comparisons
Table 1: Comparative Performance of Formalin vs. Ethanol for Parasite Preservation
| Preservation Metric | 10% Formalin | 96% Ethanol | Key Findings |
|---|---|---|---|
| Morphotype Diversity | Higher [31] | Lower [31] | Formalin revealed a greater number of distinct parasite types. |
| Parasites per Fecal Gram (PFG) | No significant difference [30] [31] | No significant difference [30] [31] | Both media were equally effective for quantifying parasite load. |
| Larval Preservation (e.g., Filariopsis) | Superior [31] | Good, but inferior [31] | Formalin better maintained larval cuticle and internal structures. |
| Egg Preservation (e.g., Strongyle-type) | Good [31] | Good, no significant difference [31] | Both media were equally effective for preserving eggs. |
| DNA Integrity | Poor (fragmented) [30] [32] | High (stable) [30] [33] | Ethanol is essential for PCR, sequencing, and other molecular methods. |
Table 2: Reagent Solutions for Parasite Preservation and Analysis
| Research Reagent | Function & Application | Key Considerations |
|---|---|---|
| 10% Buffered Formalin | Primary fixative for morphological microscopy; preserves helminth eggs, larvae, and protozoan cysts [20] [31]. | Toxic; requires careful handling and ventilation. Neutral buffered formalin helps prevent formalin pigment formation [34]. |
| 95% Ethanol | Primary preservative for molecular studies; denatures nucleases to protect DNA/RNA [31] [33]. | Flammable; may make tissues brittle. A 2:1 or 3:1 preservative-to-sample ratio is a minimum requirement [31]. |
| Polyvinyl Alcohol (PVA) | A resin added to fixatives (often Schaudinn's) as an adhesive for stool material to slides for permanent staining [20]. | Often contains mercury; disposal can be problematic. Allows for specimen shipment at room temperature [20]. |
| Sodium Acetate-Formalin (SAF) | A mercury-free, all-purpose fixative suitable for both concentration techniques and permanent stained smears [20] [35]. | Has poor adhesive properties; may require albumin-coated slides for optimal smear preparation [20]. |
| 70% Ethanol | Long-term storage solution for both gross specimens and DNA; minimizes tissue brittleness compared to higher concentrations [34] [35]. | Effective for preserving worm specimens for later identification [36]. |
Experimental Protocols
Detailed Methodology: Comparative Preservation Study
The following protocol is adapted from a published study comparing preservation media in primate fecal samples [30] [31].
1. Sample Collection and Partitioning:
- Collection: Collect fresh fecal samples immediately after defecation.
- Partitioning: Using a sterile tool, halve the sample. Approximately 2 grams of one half is placed in a 15 ml tube containing 10 ml of 10% buffered formalin. The other 2-gram half is placed in a separate 15 ml tube containing 6 ml of 96% ethanol [31].
- Storage: Gently agitate tubes to ensure the sample is fully permeated by the preservative. Samples can be stored at ambient temperature for several months prior to analysis [30] [31].
2. Coprological Processing (Modified Wisconsin Sedimentation):
- Separation: Pour the contents of each tube through a strainer to separate solid fecal matter from the liquid preservative. Weigh the solid portion to determine the fecal weight.
- Homogenization and Straining: Homogenize the solids with distilled water and strain the solution through a double-layered cheesecloth.
- Sedimentation: Centrifuge the strained solution at 1500 RPM for 10 minutes. Discard the supernatant.
- Microscopy: Re-homogenize the pellet with 5-10 ml of distilled water and distribute it into a 6-well microscopy plate for screening [30] [31].
3. Parasite Identification and Degradation Grading:
- Microscopy: Screen samples using a standard microscope. Identify parasites based on established morphological characteristics (e.g., size, shape, shell thickness for eggs; internal and external structures for larvae) [31].
- Grading Scale: Use a customized 3-point scale to grade preservation:
- Score 3 (Well-preserved): Intact cuticle (larvae) or shell (eggs); clear internal and external structures; easy to identify.
- Score 2 (Moderately preserved): Minor degradation of cuticle/shell or internal structures; identification is still possible.
- Score 1 (Poorly preserved): Severe degradation; difficult or impossible to identify [31].
Experimental Workflow and Decision Pathway
The following diagram illustrates the logical decision process for selecting a preservation method based on research objectives.
Preservation Method Decision Workflow
This workflow provides a logical guide for selecting the appropriate preservation medium based on your primary research objectives, ensuring sample integrity for your intended analyses.
In parasitology education research, the integrity of experimental data is fundamentally linked to the quality of specimen collection and preservation. Specimen deterioration poses a significant threat to diagnostic accuracy and research validity, potentially compromising morphological identification, molecular analysis, and ultimately, scientific conclusions. Standardized procedures for collecting adequate sample volumes and maintaining proper fixative-to-sample ratios are not merely procedural formalities but are critical determinants of research success. This technical support center provides targeted guidance and troubleshooting resources to help researchers, scientists, and drug development professionals prevent pre-analytical errors that can lead to specimen degradation.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
General Specimen Collection
What is the most critical factor to consider when choosing a fixative? The choice of fixative depends on your downstream applications. No single solution is optimal for all techniques [37]. For projects requiring both concentration techniques and permanent stained smears, SAF (Sodium Acetate Formalin) is a good mercury-free option, though it has poor adhesive properties requiring albumin-coated slides for smear preparation [37]. If permanent stained smears are the priority, especially for protozoan trophozoites and cysts, PVA (Polyvinyl Alcohol) is highly recommended, but it may not concentrate some helminth eggs as effectively as formalin-based fixatives [37].
Our laboratory is receiving specimens with distorted parasite morphology. What could be the cause? This is often a result of improper fixation or delayed processing [38].
- Cause 1: The fixative-to-sample ratio is incorrect. An inadequate volume of fixative will not properly preserve the specimen.
- Solution: Ensure a 3:1 or 5:1 ratio of preservative to fecal material is used [37] [35]. For liquid specimens, a 3:1 ratio is specifically recommended for PVA [37].
- Cause 2: Specimens are not being mixed thoroughly with the fixative, leading to incomplete fixation.
- Solution: After placing the specimen in the fixative, mix well by stirring with an applicator stick to create a homogeneous solution. Allow it to stand for 30 minutes at room temperature for adequate fixation [37].
Specific Specimen Types
Why is the timing of collection so important for certain specimens like blood and urine? Parasites can exhibit periodic shedding or circadian rhythms, meaning their presence in certain specimens fluctuates throughout the day. Collecting at the optimal time maximizes the probability of detection [35].
Table 1: Optimal Collection Times for Various Specimen Types
| Specimen Type | Target Parasite(s) | Optimal Collection Time / Notes |
|---|---|---|
| Blood | Plasmodium spp. (malaria) | Between paroxysms (chills/fever) [35] |
| Blood | Wuchereria bancrofti | Approximately midnight [35] |
| Blood | Loa loa | Approximately noon [35] |
| Urine | Schistosoma haematobium | Midday collection (peak egg excretion between 12-3 p.m.); collect terminal portion of urine [38] [35] |
| Perianal Sample | Enterobius vermicularis (pinworm) | 10-11 p.m. or upon waking, before a bowel movement [35] |
We need to ship parasitology specimens to a reference laboratory. What are the key considerations? Only preserved fecal specimens should be shipped to prevent specimen deterioration and reduce infection risk [37].
- Preservation: Use appropriate vials with adequate fixative (e.g., PVA or SAF) [37].
- Packaging: Follow universal regulations for shipping clinical specimens. Place the primary container into a sealed secondary container (e.g., metal sleeve or sealable bag), and then into a sturdy shipping container [37].
- Documentation: Ensure all specimens are accurately labeled and accompanied by required documentation.
Experimental Protocols for Validation
Protocol 1: Validating Fixative Performance for Fecal Specimens
This protocol is adapted from studies investigating the enhancement of the Kato-Katz method using formalin-fixed stool [39].
Objective: To compare the quality of parasite morphology and slide background clarity between formalin-fixed and unfixed stool specimens.
Materials:
- Fresh stool specimen (naturally infected or artificially seeded with parasite eggs like Echinostoma or Opisthorchis viverrini)
- 10% formalin solution
- Phosphate Buffered Saline (PBS) or Normal Saline Solution (NSS) at various pH levels
- Glycerol with 3% malachite green
- Standard Kato-Katz kit materials (cellophane strips, template, sieve)
- Light microscope
Methodology:
- Sample Preparation: Divide the stool specimen into multiple aliquots.
- Fixation Groups:
- Group A (Unfixed): Process fresh stool immediately.
- Group B (Formalin-fixed): Fix stool with 10% formalin at a 1:1 ratio for varying durations (e.g., 1, 3, 6, 12, 24 hours, and 7 days) [39].
- Group C (Formalin-fixed + Glycerol): After formalin fixation, incubate samples with glycerol for 1 hour to enhance clearing [39].
- Processing: Process all groups using the standard Kato-Katz technique [39].
- Analysis:
- Examine slides under a light microscope (40x magnification).
- Score parasite egg morphology as "normal" or "irregular."
- Score slide background clarity on a scale (e.g., +1 to +3, where +3 represents the clearest background with minimal fecal debris) [39].
- Perform statistical analysis (e.g., paired sample t-test) to compare the performance between groups. A p-value of < 0.05 is considered statistically significant [39].
Visual Workflow of the Validation Protocol:
Protocol 2: Assessing DNA Preservation in Different Fixatives
For research involving molecular parasitology, preserving DNA integrity is paramount.
Objective: To evaluate the efficacy of different preservatives in maintaining DNA integrity for long-term storage and molecular analysis.
Materials:
- Parasite samples (e.g., nematodes, protozoan cysts)
- Preservative solutions:
- DNA extraction kit
- Equipment for gel electrophoresis or bioanalyzer
Methodology:
- Preserve identical parasite samples in the different fixative solutions for a predetermined period (e.g., 6 months, 1 year).
- Extract DNA from all samples using a standardized protocol.
- Analyze the quality and quantity of the extracted DNA. Key metrics include:
- DNA Yield.
- Fragment Size (e.g., ability to amplify large DNA fragments >15 kb, which is well-preserved in DESS [40]).
- PCR Amplification Success for specific parasite genes.
Table 2: Key Research Reagent Solutions for Parasitology Specimen Preservation
| Reagent Solution | Primary Function | Key Advantages | Key Limitations |
|---|---|---|---|
| SAF (Sodium Acetate Formalin) | All-purpose fixative for concentration and stained smears [37]. | Mercury-free; good for helminth eggs and protozoan cysts; long shelf life [37]. | Poor adhesive property; protozoan morphology with trichrome stain not as clear as with PVA [37]. |
| PVA (Polyvinyl Alcohol) | Fixative with adhesive for permanent stained smears [37]. | Excellent for protozoan trophozoites and cysts; allows specimen shipment [37]. | Contains mercury compounds; some helminth eggs not concentrated well [37]. |
| 10% Formalin | Fixative for helminth eggs and larvae; used in concentration techniques [37] [39]. | Good routine preservative; long shelf life; suitable for Kato-Katz enhancement [37] [39]. | Permanent stained smears cannot be prepared [37]. |
| DESS (DMSO/EDTA/NaCl) | DNA and morphological preservation at room temperature [40]. | Maintains high molecular weight DNA; effective for morphology in many species [40]. | Not effective for organisms with calcium carbonate structures [40]. |
| Schaudinn's Fluid | Fixative for preparing smears from fresh specimens [37]. | Designed for slide fixation; easily prepared [37]. | Not for concentration techniques; contains mercury compounds [37]. |
Logical Framework for Preservative Selection
The following diagram outlines a decision-making pathway for selecting the appropriate preservative based on research objectives, from primary analysis to long-term storage considerations.
In the field of parasitology, the integrity of specimens is paramount for accurate diagnosis, education, and research. The decline in traditional morphological expertise, coupled with the increasing scarcity of parasite specimens in developed regions due to improved sanitation, underscores the need for robust specimen preservation and analysis methods [41]. Without proper techniques, specimens deteriorate, leading to a loss of valuable educational resources and potential diagnostic inaccuracies. The Merthiolate-Iodine-Formalin (MIF) method is a time-tested parasitological technique that combines fixation and staining to preserve and facilitate the identification of a wide range of parasitic structures in fecal samples [42] [43]. This article establishes a technical support center for implementing MIF within multi-method systems, focusing on protocols, troubleshooting, and its role in preventing specimen deterioration.
The Scientist's Toolkit: Essential Reagents and Materials
The successful application of the MIF technique relies on a specific set of reagents. The table below details the key components and their functions.
Table 1: Key Research Reagent Solutions for the MIF Technique
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Thimerosal (Merthiolate) | Acts as a preservative and bactericidal agent [44]. | Part of the stock MIF solution [45]. |
| Formalin | Fixes and preserves parasitic structures (cysts, eggs, larvae) [43]. | A component of the stock solution; ensures long-term structural integrity [43]. |
| Lugol's Iodine Solution | Stains parasitic structures (e.g., cysts), aiding in microscopic visualization [43]. | Added immediately before use; provides both fixation and staining [43]. |
| Glycerin | Helps prevent distortion of parasitic structures [44]. | A component of the stock MIF solution [45]. |
| Standard MIF Kit | A commercial collection system containing the necessary preservatives. | Typically a two-vial system for comprehensive specimen preservation [43]. |
Experimental Protocols and Workflows
MIF Staining Procedure: A Step-by-Step Guide
The following workflow outlines the standard procedure for preparing a fecal sample using the MIF method.
Detailed Methodology [45]:
- Sample Preparation: Thoroughly resuspend 3–5 grams of fecal material in 20 ml of phosphate-buffered saline (PBS).
- Filtration: Filter the homogenate through a sieve mesh with a 250 µm diameter to remove large debris.
- Concentration: Transfer the filtered suspension to a 10 ml tube and centrifuge at 1,500 rpm for 10 minutes. Carefully discard the supernatant after centrifugation.
- MIF Solution and Staining: The MIF solution is typically prepared as two stock solutions that are combined just before use [44]:
- MIF A: Contains distilled water, thimerosal (1:1000), formaldehyde, and glycerin.
- MIF B: Contains distilled water and potassium iodide (to form Lugol's iodine). The sediment is then mixed with the freshly prepared MIF solution.
- Microscopy: A smear is prepared from the mixture and examined under a microscope. The iodine component stains cysts, eggs, and larvae, aiding in their identification.
MIF in a Multi-Method Diagnostic Framework
For comprehensive parasite recovery, MIF should be part of a larger diagnostic strategy. The diagram below illustrates its role alongside other techniques.
Performance Data and Comparison
To inform method selection, the quantitative performance of MIF against other common techniques is critical.
Table 2: Comparative Performance of MIF Against Other Diagnostic Methods
| Method | Primary Application | Relative Sensitivity for Helminths | Key Advantages | Inherent Limitations |
|---|---|---|---|---|
| MIF | Broad qualitative survey of helminths and protozoa | Competitive with Kato-Katz for helminths like Trichuris trichiura [46]. | Simplicity; cost-effectiveness; stains and fixes simultaneously; good for field surveys [46] [43]. | Iodine can interfere with other stains and may distort some protozoa; not ideal for permanent stained smears [43]. |
| Kato-Katz | Quantitative detection of soil-transmitted helminths | Higher sensitivity for Trichuris trichiura and low parasite loads [46]. | Allows egg quantification (eggs per gram); gold standard for epidemiologic surveys [46]. | Not suitable for protozoa; may miss high parasite loads [46]. |
| Direct Immunofluorescence (DFA) | Detection of specific protozoa like Giardia and Cryptosporidium | Not applicable for helminths. | High sensitivity and specificity for target protozoa; considered a gold standard for these pathogens [45]. | Requires a fluorescence microscope; higher cost; limited to specific pathogens. |
| Formalin-ethyl Acetate Sedimentation | General concentration of parasites | Good recovery of helminth eggs and larvae, and protozoan cysts [42] [43]. | An all-purpose concentration method; excellent morphology preservation; suitable for immunoassays [43]. | Inadequate for trophozoite preservation [43]. |
Technical Support Center
Troubleshooting Guide
Table 3: Troubleshooting Common MIF Procedure Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor staining of cysts/nuclei | Degraded or outdated Lugol's iodine solution. | Prepare fresh Lugol's solution immediately before use [43]. |
| Distorted protozoan morphology | Over-exposure to iodine or improper fixation. | Ensure the ratio of fecal sample to MIF is correct (1:3 to 1:5) and do not let smears sit too long before reading [43]. |
| Difficulty identifying Cryptosporidium | Method is not specific for this parasite; oocysts are very small. | Use modified acid-fast staining or, preferably, DFA or PCR for specific detection [45] [43]. |
| Low diagnostic sensitivity | Low parasitic load in a single sample. | Examine multiple specimens collected at 2-3 day intervals [43]. |
| Inconsistent results | Inadequate mixing of stool with preservative. | Ensure the specimen is thoroughly mixed with the MIF solution to guarantee uniform fixation and staining [43]. |
Frequently Asked Questions (FAQs)
Q1: How does MIF compare to PVA for preserving protozoan cysts for morphological study? A1: While MIF is excellent for field surveys and combined fixation/staining, low-viscosity Polyvinyl Alcohol (PVA) is generally superior for creating permanent stained smears (e.g., with Trichrome stain) for detailed cytological study of protozoan trophozoites and cysts [43]. However, PVA has disadvantages, such as containing mercuric chloride and being unsuitable for concentration procedures [43].
Q2: Can MIF-preserved samples be used for molecular testing like PCR? A2: This is generally not recommended. Iodine can interfere with PCR. For molecular studies, other preservatives like Sodium Acetate-Acetic Acid-Formalin (SAF) or specific one-vial, non-mercuric fixatives are more suitable [43].
Q3: What is the "refugia" concept and how does it relate to diagnostic methods? A3: While primarily discussed in veterinary parasitology and anthelmintic resistance management, "refugia" refers to the portion of a parasite population not exposed to a drug, thereby maintaining genetic diversity and susceptible genes [47]. From a diagnostic perspective, using highly sensitive methods like MIF helps accurately monitor parasite prevalence and intensity, which is crucial for making informed decisions about targeted treatment strategies that can preserve refugia and slow resistance development.
Q4: Why is MIF particularly valuable in a resource-limited or educational setting? A4: MIF is simple, inexpensive, and has a long shelf life [46] [43]. Its ability to both fix and stain in a single step reduces the need for multiple reagents and complex procedures. For educational purposes, this allows for the creation of stable, long-term reference material, which is crucial as physical specimens become increasingly scarce in regions with improved sanitation [41].
Q5: What are the key advantages of MIF over the Kato-Katz technique? A5: The primary advantage is its broader scope. While Kato-Katz excels at quantifying key soil-transmitted helminths, MIF is also effective at detecting other helminths like Strongyloides stercoralis and, importantly, intestinal protozoa, for which the Kato-Katz technique is not suitable [46].
Troubleshooting Guides
DNA Degradation in Long-Term Storage
Problem: DNA samples show signs of degradation during long-term storage, leading to poor PCR amplification results.
Solutions:
- For silica gel-desiccated filters: For storage beyond one month, transfer samples to -20°C. While silica gel prevents degradation well for up to one month at a range of temperatures (18°C, 4°C, or -20°C), only storage at -20°C prevents a noticeable decrease in detectability at 5 and 12 months [48].
- For ethanol-preserved samples: Ensure initial preservation is done with 95% ethanol, which provides better penetration and nuclease deactivation compared to lower concentrations [49]. Samples can remain stable for at least 60 days at 4°C [49].
- Confirm drying efficiency: When using silica beads, ensure they are actively drying by checking color indicators. Inadequate drying capacity leads to residual moisture and DNA degradation [50].
Insufficient DNA Yield After Preservation
Problem: Low DNA concentration or purity after extraction from preserved samples.
Solutions:
- Check preservation ratios: For 95% ethanol preservation, maintain a minimum 2:1 volumetric ratio of ethanol to sample. While a 5:1 ratio is often recommended, studies show successful DNA barcoding can be achieved with a 2:1 ratio [33].
- Add mechanical disruption: For difficult samples like soil-transmitted helminth eggs in stool, incorporate a bead-beating step during DNA extraction to break down rigid egg shells, which substantially improves DNA recovery [51].
- Optimize precipitation: When concentrating DNA by precipitation, use 0.6-0.7 volumes of room-temperature isopropanol for large sample volumes or low DNA concentrations. Ensure thorough mixing and adequate centrifugation [52].
Preservation Method Selection for Field Conditions
Problem: Choosing between 95% ethanol and silica bead desiccation for specific field conditions.
Solutions:
- Assess temperature conditions: At elevated temperatures (e.g., 32°C), silica bead desiccation outperforms ethanol preservation by preventing progressive decreases in eDNA sample quality [48]. A two-step process using 90% ethanol overnight followed by silica-based desiccation has proven effective for hookworm DNA preservation in stool at 32°C [49].
- Consider transport regulations: Ethanol is flammable and classified as hazardous, complicating transportation. Silica gels pose fewer safety concerns [33].
- Evaluate sample type: For phyllosphere samples, silica gel packs effectively preserve microbial community DNA for metabarcoding analyses at ambient temperatures [53]. For fecal specimens, 95% ethanol often provides the most pragmatic choice considering toxicity, cost, and effectiveness [49].
Frequently Asked Questions (FAQs)
Q1: Which preservation method offers better DNA stability for long-term storage: 95% ethanol or silica beads?
A: The optimal method depends on storage temperature and duration:
- For storage up to one month: Both methods perform well across a range of temperatures (18°C to -20°C) [48].
- For storage beyond one month at room temperature: Silica gel desiccation demonstrates superior performance by preventing progressive decreases in eDNA quality [48].
- For long-term storage (>1 year): Silica gel preservation at -20°C maximizes sample integrity [48].
- At consistent 4°C: Both methods show comparable effectiveness for at least 60 days [49].
Q2: What is the minimum ethanol-to-sample ratio needed for effective DNA preservation?
A: A 2:1 volumetric ratio of 95% ethanol to sample is sufficient for successful DNA preservation and downstream molecular applications, as demonstrated in DNA barcoding studies with benthic macroinvertebrates. While higher ratios (5:1) are often recommended, the 2:1 ratio provides effective preservation while reducing logistical constraints [33].
Q3: How can I regenerate silica gel beads for reuse in DNA preservation?
A: Silica gel beads can be regenerated by heating:
- Oven method: Heat at 200-250°F (93-121°C) for 1-2 hours [50].
- Microwave method: Heat on defrost setting for 1.5-5 minutes, but avoid overheating which can damage beads [50].
- Important precautions: Never microwave cobalt chloride-containing (blue) beads due to toxicity concerns. Use only clear or orange indicator beads in microwaves, and preferably use non-indicating beads for this application [50].
Q4: How does temperature fluctuation during field transport affect DNA preserved with different methods?
A: Silica gel desiccation provides more consistent DNA preservation quality under temperature fluctuations:
- Silica gel beads: Maintain DNA detection stability even at 23°C/32°C, preventing the progressive decrease in sample quality observed with ethanol at elevated temperatures [48] [49].
- 95% ethanol: While effective at 4°C, samples preserved in ethanol show decreased DNA detection efficiency when stored at 32°C compared to silica gel methods [48] [49].
Quantitative Data Comparison
Table 1: Comparison of DNA Preservation Efficacy Between 95% Ethanol and Silica Gel Beads
| Parameter | 95% Ethanol | Silica Gel Beads | Experimental Context |
|---|---|---|---|
| Short-term stability (≤1 month) | Stable at 4°C [49] | Stable at 18°C, 4°C, and -20°C [48] | Filter-immobilized eDNA [48] |
| Long-term stability (>1 month) | Progressive decrease in quality at 23°C [48] | Prevents decrease at 23°C; -20°C required for >1 month [48] | Filter-immobilized eDNA over 15 months [48] |
| High temperature performance | Decreased detection efficiency at 32°C [49] | Outperforms ethanol at 32°C [48] [49] | Hookworm DNA in stool [49] |
| Optimal storage temperature | 4°C [49] | -20°C for long-term [48] | Multiple sample types [48] [49] |
| Sample matrix compatibility | Effective for stool, benthic macroinvertebrates [49] [33] | Effective for filters, phyllosphere, stool [48] [49] [53] | Various environmental and clinical samples |
Table 2: Preservation Protocol Comparison for Different Sample Types
| Sample Type | Recommended Method | Alternative Methods | Key Considerations |
|---|---|---|---|
| Filter-immobilized eDNA | Silica gel desiccation, -20°C for long-term [48] | 95% ethanol (adequate for short-term) [48] | Silica gel superior at room temperature [48] |
| Human stool (STH detection) | 95% ethanol (most pragmatic) [49] | Two-step: 90% ethanol + silica desiccation [49] | Consider toxicity, cost, shipping [49] |
| Phyllosphere samples | Silica gel packs at ambient temperature [53] | RNAlater, LifeGuard [53] | Maintains microbial community structure [53] |
| Benthic macroinvertebrates | 95% ethanol at 2:1 ratio [33] | 70% ethanol (after initial preservation) [33] | Successful barcoding with minimal protocol modification [33] |
Experimental Protocols
Protocol 1: Silica Gel Bead Desiccation for Filter-Immobilized eDNA
Purpose: To preserve environmental DNA immobilized on filter membranes for molecular analysis [48].
Materials:
- Filter membranes with immobilized eDNA
- Silica gel beads (non-indicating or with color indicator)
- Airtight containers or desiccator
- Humidity indicator cards (optional)
Procedure:
- After sample collection, place filter membranes in a container with an excess of silica gel beads.
- Ensure complete surrounding of filters with silica gel beads (recommended ratio: ≥5:1 beads to filter mass).
- Seal containers tightly to prevent moisture ingress.
- Store samples at appropriate temperature:
- Regenerate silica beads as needed by heating at 200-250°F for 1-2 hours [50].
Validation: In targeted qPCR assays, silica gel-preserved filters showed stable detection of abundant eDNA targets over 15 months at -20°C and 4°C, outperforming ethanol preservation at 23°C [48].
Protocol 2: Two-Step Ethanol-Silica Desiccation for Challenging Samples
Purpose: To preserve difficult samples like hookworm DNA in stool under field conditions with high temperatures [49].
Materials:
- 95% ethanol
- Silica gel beads
- Airtight containers
- Sample tubes or containers
Procedure:
- Preserve samples in 90-95% ethanol overnight at room temperature.
- Remove samples from ethanol and transfer to containers with silica gel beads.
- Ensure complete desiccation of samples in the silica gel environment.
- Store at ambient temperature (effective even at 32°C for up to 60 days) [49].
Validation: This method minimized Cq value increases in qPCR detection of hookworm DNA at 32°C over 60 days, performing comparably to FTA cards and potassium dichromate [49].
Workflow Visualization
DNA Preservation Method Selection Guide
Research Reagent Solutions
Table 3: Essential Materials for DNA Preservation Protocols
| Reagent/Material | Function | Application Notes |
|---|---|---|
| 95% Ethanol | Denatures proteins and nucleases, prevents DNA degradation [49] [33] | Use minimum 2:1 ratio (ethanol:sample); higher concentrations improve nuclease deactivation [49] |
| Silica Gel Beads | Adsorbs moisture, creates dry environment to inhibit enzymatic degradation [48] | Use with color indicator to monitor saturation; can be regenerated by heating [50] |
| Sodium Acetate (3M, pH 5.2) | Provides counterions to neutralize DNA charge, facilitating precipitation [52] | Used in ethanol/isopropanol precipitation protocols [52] |
| Isopropanol (100%) | Precipitates DNA from large volumes at room temperature [52] | Use 0.6-0.7 volumes per sample volume; preferred for low DNA concentrations [52] |
| RNAlater | Commercial preservative that stabilizes cellular RNA and DNA [49] [53] | Effective for phyllosphere samples and stool preservation [49] [53] |
| Potassium Dichromate | Chemical preservative for stool samples [49] | Effective but toxic; requires careful handling [49] |
| FTA Cards | Commercial solid matrix for nucleic acid preservation [49] | Effective for hookworm DNA in stool at 32°C [49] |
Essential Concepts and Classification
What is UN3373, and when does it apply to my parasitology samples?
UN3373 refers to the regulatory classification for "Biological Substance, Category B." This applies to infectious substances that are not classified as Category A, meaning they are not capable of causing permanent disability, life-threatening, or fatal disease in otherwise healthy humans or animals [54] [55]. In the context of parasitology research, this typically includes diagnostic specimens where pathogens are suspected but do not pose a highest-level risk [56] [57]. Adhering to these guidelines is fundamental to preventing specimen deterioration and ensuring integrity during transit for education and research.
What is the critical difference between Category A and Category B infectious substances?
Correct classification is the first and most critical step in the shipping process. The table below outlines the key differences.
| Feature | Category A (UN2814/UN2900) | Category B (UN3373) |
|---|---|---|
| Definition | Substances capable of causing permanent disability, life-threatening or fatal disease [54] [55]. | Infectious substances that do not meet the criteria for Category A [54] [55]. |
| Risk Level | High consequence, life-threatening pathogens [58]. | Moderately hazardous and/or potentially pathogenic substances [58]. |
| Example Pathogens | Bacillus anthracis, Ebola virus, Mycobacterium tuberculosis cultures [57]. | Specimens suspected of containing parasites like Giardia, Plasmodium, or helminths [56]. |
| Primary Packaging | Packing Instruction 620 (IATA) [58] [57]. | Packing Instruction 650 (IATA) [58] [59]. |
My specimen is fixed and preserved. Is it still considered an infectious substance?
Yes, most preserved parasitology specimens remain regulated. Common preservatives like Polyvinyl Alcohol (PVA) and Sodium Acetate Formalin (SAF) are used specifically to maintain parasite morphology for later analysis [20]. The preservation process fixes the specimen but does not necessarily neutralize all pathogens. Therefore, preserved fecal specimens, parasite cysts, and oocysts must still be shipped as UN3373 if infectious substances are present [20].
Packaging and Documentation Protocols
What are the step-by-step packaging requirements for a UN3373 shipment?
Packing Instruction 650 (P650) mandates a triple-packaging system [59] [54]. The following workflow and details ensure compliance and protect your specimens from leakage, shock, and pressure changes.
Primary Receptacle
- Function: The immediate container holding the specimen (e.g., cryovial, specimen tube) [58] [55].
- Requirements: Must be leak-proof for liquids or sift-proof for solids [59]. It must contain no more than 1 liter (liquid) or 4 kilograms (solid) [54].
- Methodology: For liquid parasitology specimens in transport, the primary receptacle or secondary packaging must be capable of withstanding an internal pressure of 95 kPa (0.95 bar) without leakage [54].
Secondary Packaging
- Function: Protects the primary receptacle(s) [59].
- Requirements: Must be leak-proof [59]. If multiple fragile primary receptacles are used, they must be individually wrapped or separated to prevent contact [59] [55].
- Methodology: For liquids, place absorbent material between the primary and secondary packaging in sufficient quantity to absorb the entire contents of all primary receptacles [59] [55].
Outer Packaging
- Function: The shipping box that protects the contents during transit.
- Requirements: Must be rigid and of adequate strength for its capacity, mass, and intended use [59]. At least one surface must have minimum dimensions of 100 mm x 100 mm to accommodate the marking [59] [54]. The completed package must be capable of passing a 1.2-meter drop test without leakage [59].
What documentation and markings are required on the outer box?
Accurate marking is required for regulatory compliance and safety. A UN3373 shipment does not require a Shipper's Declaration for Dangerous Goods [57]. The required markings are summarized below.
| Marking/Label Element | Description | Specifications |
|---|---|---|
| UN3373 Diamond Mark | A diamond-shaped mark with "UN3373" [59]. | Minimum dimensions: 50 mm x 50 mm; line width ≥ 2 mm; text ≥ 6 mm high [59]. |
| Proper Shipping Name | The text "BIOLOGICAL SUBSTANCE, CATEGORY B" [59]. | Letters at least 6 mm high, marked adjacent to the diamond [59]. |
| Sender/Receiver Info | Name, address, and telephone number of both shipper and receiver [56]. | Clearly visible on the outer packaging. |
| Air Waybill | The air waybill for the shipment. | Must indicate the contents as per carrier requirements [57]. |
Troubleshooting Common Shipping Issues
How should I ship specimens that require refrigeration?
Using Dry Ice (Solid Carbon Dioxide):
- Dry ice is classified as a Class 9 dangerous good (UN1845) and requires additional markings [60] [57].
- Placement: Dry ice must be placed outside the secondary packaging [55].
- Ventilation: The outer packaging must permit the release of carbon dioxide gas to prevent a pressure build-up [57] [55].
- Marking: The outer package must be marked with "Dry Ice" or "Carbon dioxide, solid," the UN number UN1845, and the net quantity in kilograms [55]. A Class 9 miscellaneous hazard label is also required [57] [55].
- Integrity: The primary receptacle and secondary packaging must maintain integrity at the temperature of the dry ice as well as the temperatures and pressures that could result if refrigeration is lost [59] [55].
What is the most common cause of package failure, and how can I prevent it?
The most common failures are inadequate sealing of primary receptacles and insufficient absorbent material for liquid specimens. To prevent this:
- Methodology: Ensure all primary receptacle caps are properly tightened and consider using parafilm or laboratory tape to seal them [20].
- Verification: Use absorbent material with enough capacity to absorb the entire volume of liquid in all primary receptacles. The absorbent should be placed in the secondary packaging, surrounding the primary receptacles [59] [55].
My shipment was rejected by the carrier. What are the likely reasons?
Common reasons for rejection include:
- Incorrect or Missing Markings: The UN3373 diamond and proper shipping name must be clearly visible on the outer package [59].
- Exceeded Quantities: The outer packaging must not contain more than 4 liters or 4 kilograms of Category B substance [57] [54].
- Damaged or Non-Compliant Packaging: The outer box must be rigid and undamaged. Using certified, commercially available packaging systems can prevent this issue.
The Researcher's Toolkit: Essential Shipping Materials
The following table details key materials required for preparing a UN3373-compliant shipment of parasitology specimens.
| Item | Function | Specification / Example |
|---|---|---|
| Primary Receptacle | Holds the specimen directly. | Leak-proof cryovials, specimen tubes [58]. |
| Specimen Preservative | Prevents specimen deterioration and fixes morphology. | PVA, SAF, or formalin-based fixatives [20]. |
| Absorbent Material | Contains leaks from primary receptacles. | Sufficient to absorb entire liquid volume [59] [55]. |
| Secondary Container | Encapsulates primary receptacle(s) and absorbent. | Leak-proof plastic bag or sealed container [59]. |
| Rigid Outer Box | Protects contents during transit; withstands shocks. | Fiberboard box of adequate strength [59]. |
| Cushioning Material | Prevents contact and breakage; secures secondary packaging. | Bubble wrap, cellulose wadding, foam [59]. |
| UN3373 Mark & Label | Identifies package contents for handlers. | Diamond mark with "UN3373" and proper shipping name [59]. |
Training and Compliance FAQs
Is formal training required to ship Category B substances?
Yes. Individuals involved in preparing and shipping infectious substances as UN3373 are required by law to receive formal training on the applicable regulations [56] [60]. This training must be recurrent, typically every two years [58].
What is the single most important step to ensure my specimen arrives intact for research?
The cornerstone of successful specimen transport is rigorous adherence to the triple-packaging protocol. This system of primary, secondary, and outer packaging creates multiple independent barriers specifically designed to prevent leakage and protect morphological integrity, which is paramount for parasitology education and research [58] [59]. Always perform a final check to ensure all closures are secure and all required markings are present and correct before dispatching the shipment.
Solving Pre-Analytical Challenges: Expert Strategies for Compromised Specimens and Suboptimal Conditions
Frequently Asked Questions (FAQs)
What is the consequence of using an expired collection vial? Using an expired vial can lead to specimen deterioration and compromised diagnostic results. Preservatives in the vials may lose their efficacy over time, failing to maintain parasite morphology or nucleic acid integrity. This can result in false-negative results or the inability to identify parasites accurately during microscopic examination or molecular testing [61].
Why is insufficient specimen volume a problem? An insufficient sample may not contain enough preservative to properly fix the specimen, leading to degradation of parasitic elements. Furthermore, a small volume reduces the probability of detecting parasites, especially those shed intermittently or in low numbers, thereby lowering test sensitivity and increasing the likelihood of a false-negative result [35] [62].
How does improper mixing affect the sample? Failing to thoroughly mix the stool specimen with the preservative in the vial can lead to inadequate fixation. This can cause the degradation of fragile trophozoites and cysts, making them unrecognizable under the microscope. Improper mixing can also cause uneven distribution of the sample, leading to an unrepresentative aliquot being tested [35].
How long can a preserved stool specimen remain stable? Stability depends on the preservative used. When placed in an appropriate preservative, a stool specimen can typically remain stable for several days at room temperature. In contrast, an unpreserved sample must be processed quickly—within 30 minutes for liquid stools and within 24 hours if refrigerated for formed stools [61] [35].
What is the best practice to rule out a parasitic infection? Due to the intermittent shedding of many parasites, a single negative test is not sufficient. To confidently rule out parasitism, it is recommended to conduct examinations on three separate specimens collected over 7 to 10 days [35] [63].
Troubleshooting Guides
Issue 1: Expired or Compromised Collection Vials
The Problem: The use of expired vials or vials with a compromised preservative integrity.
Underlying Principle: Preservatives such as formalin, polyvinyl alcohol (PVA), and sodium acetate-acetic acid-formalin (SAF) have a finite shelf life. Over time, their chemical properties can change, reducing their ability to fix and preserve parasitic structures effectively [61] [64].
Prevention & Resolution:
- Adherence to Expiry Dates: Strictly use collection vials within their manufacturer-stated expiration date.
- Proper Storage: Store vials as directed, typically at room temperature and away from direct light, to maintain preservative efficacy.
- Quality Control: Implement a laboratory quality control program to periodically check the performance of preservative lots.
- Alternative Preservatives: Consider newer, non-mercurial, single-vial fixatives like Ecofix, which have been evaluated as acceptable alternatives to traditional formalin and LV-PVA [64].
Issue 2: Insufficient Specimen Volume
The Problem: The volume of stool submitted in the preservative vial is too low.
Underlying Principle: A minimum volume of feces is required to achieve the correct specimen-to-preservative ratio (e.g., 1 part feces to 3 parts fixative) [35]. Insufficient volume can lead to inadequate fixation and poor sample representation.
Impact of Insufficient Volume on Test Outcomes:
| Specimen Volume | Risk of Inadequate Fixation | Impact on Test Sensitivity | Potential Outcome |
|---|---|---|---|
| Insufficient | High | Significantly Lowered | False negative; degraded organisms |
| Below Minimum | Moderate | Lowered | Reduced detection of low-shedders |
| Meets Requirement | Low | Optimal | Reliable and accurate results |
Prevention & Resolution:
- Clear Instructions: Provide patients with explicit instructions and visual aids demonstrating the need to fill the vial to the indicated "fill line" [35].
- Verification at Receipt: Upon receipt in the lab, check that the vial contains enough fixed specimen. If volume is insufficient, request a repeat collection.
- Targeted Collection: Instruct patients to collect sample from areas of the stool that are slimy, bloody, or watery, as these parts are more likely to contain parasites [35].
Issue 3: Improper Mixing of Specimen
The Problem: The stool specimen is not thoroughly mixed with the preservative solution upon collection.
Underlying Principle: Immediate and thorough mixing is critical to ensure all parts of the specimen come into contact with the fixative. This halts degenerative processes and preserves the morphology of cysts, eggs, and fragile trophozoites [35].
Prevention & Resolution:
- Standardized Protocol: Follow a clear step-by-step procedure to ensure consistent and proper mixing.
- Patient Education: Provide simple, written instructions for patients to "mix well" after placing the stool into the preservative vial.
- Allow Fixation Time: After mixing, let the vial stand at room temperature for the recommended time (e.g., 30 minutes) to ensure adequate fixation before transportation or processing [35].
The following workflow outlines the critical steps for proper specimen collection to prevent common errors:
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for proper parasitology specimen collection and preservation, based on commercial systems and published evaluations [61] [64] [65].
| Item | Primary Function | Application Note |
|---|---|---|
| Formalin (10%) | Fixes and preserves helminth eggs and protozoan cysts for wet mount examination. | A traditional "gold standard" for wet preparations; concerns exist regarding toxicity [64]. |
| Low-Viscosity PVA (LV-PVA) | Preserves protozoan cysts and trophozoites for permanent stained smears; facilitates adhesion to slide. | Often contains mercuric chloride, making disposal difficult. Acceptable alternatives are available [64]. |
| SAF (Sodium Acetate-Acetic Acid-Formalin) | A single-vial, non-mercurial fixative for both concentration and permanent staining. | Serves as a safer alternative to formalin-PVA combinations [35] [64]. |
| EcoFix | A single-vial, non-mercurial, commercial preservative. | Evaluated as comparable to traditional LV-PVA for visualization of protozoa in stained smears [64]. |
| Zinc Sulfate (ZnSO4) Flotation Medium | A solution with high specific gravity used to concentrate parasites via flotation. | Considered the best option for centrifugal flotation to detect Giardia cysts [63]. |
| TRIzol Reagent | A mono-phasic solution for the simultaneous isolation of RNA, DNA, and proteins from cell and tissue samples. | An optimized protocol exists for co-extraction from large nematodes like Dirofilaria immitis for advanced research [66]. |
Detailed Experimental Protocol: Evaluation of Preservative Efficacy
This protocol is adapted from studies that compare the performance of commercial preservatives against traditional "gold standards" [64].
Objective: To compare the performance of a novel or commercial preservative against 10% formalin and LV-PVA for the detection and identification of helminths and protozoa in human fecal specimens.
Methodology:
- Sample Collection and Aliquoting: Obtain fresh, human fecal specimens and aliquot them within 12 hours of collection into multiple vials containing the different preservatives under evaluation (e.g., formalin, LV-PVA, SAF, EcoFix, etc.).
- Storage and Processing: Store all preserved samples for a defined period (e.g., 1 month) at room temperature before processing to simulate transport conditions.
- Microscopic Preparation and Staining: For each preserved sample, prepare:
- Direct and concentrated wet mounts for immediate examination.
- Permanent stained smears (e.g., using Wheatley's trichrome stain) according to the manufacturers' instructions.
- Blinded Examination: A trained microscopist, blinded to the preservative used, examines all prepared slides.
- Grading and Assessment: Each sample is graded based on the following criteria:
- Quality of Diagnostic Characteristics: clarity and preservation of helminth eggs, protozoan cysts, and trophozoites.
- Ease of Use: for both processing and staining.
- Overall Diagnostic Accuracy: rate of successful identification of positive specimens.
Expected Outcome: The study will identify which preservatives provide comparable or superior performance to traditional, more hazardous options, supporting the adoption of safer, one-vial systems in clinical and research laboratories.
Frequently Asked Questions (FAQs)
1. Why is a standardized scale for morphological degradation necessary in parasitology? A standardized scale is crucial because it ensures consistent assessment of specimen quality across different observers and laboratories. It provides an objective framework to document how preservation affects key morphological features, which is vital for accurate parasite identification, reliable research data, and valid comparison of studies over time and between different sites [67] [68].
2. What are the primary consequences of poor specimen morphology on research and diagnosis? Poor specimen morphology can lead to missed diagnoses, incorrect taxonomic identification, and a misunderstanding of parasitic community structures within a host. This ultimately negatively impacts patient care, public health surveillance, and the accuracy of epidemiological data [67].
3. How does the choice of preservative affect parasite morphology? The preservative fundamentally alters how parasites degrade. Formalin preserves internal structures and overall form but can cause bubbling or opacity over time. Ethanol dehydrates tissues, often leading to cuticle shrinkage, puckering, and increased brittleness. The optimal preservative can depend on the parasite taxon (e.g., larvae vs. eggs) and the intended downstream analyses [68].
4. Can I use the same specimen for both morphological and molecular analysis? Yes, but it requires careful planning. Formalin, the preferred medium for morphology, fragments DNA and inhibits PCR. For combined studies, it is recommended to divide the sample: preserve one part in a molecular-friendly fixative like 70-96% ethanol, and another in formalin for morphological analysis. Some commercial fixatives are now designed to preserve both morphology and DNA [67] [68].
Troubleshooting Guides
Problem: Poor Preservation of Parasite Larvae
Issue: Larvae appear shrunken, brittle, or with obscured internal structures, making identification difficult.
Possible Causes & Solutions:
- Cause: Unsuitable Preservative.
- Solution: For long-term morphological studies, 10% buffered formalin is generally superior for preserving larval structures. If ethanol is used for molecular purposes, be aware of the expected shrinkage and cuticle artifacts and grade accordingly [68].
- Cause: Delayed or Inadequate Fixation.
- Cause: Long-term storage in ethanol.
- Solution: Recognize that ethanol causes progressive dehydration. For larvae, a formalin-based rubric will be more appropriate for high-quality morphological assessment. If stored in ethanol, a lower preservation score may be inevitable [68].
Problem: Degraded or Collapsed Helminth Eggs
Issue: Egg shells are dented, broken, or overly thickened, and internal embryos are not visible.
Possible Causes & Solutions:
- Cause: Physical pressure during processing.
- Solution: Use gentle methods during homogenization and straining. Avoid grinding the sample. Use wide-bore pipettes when handling samples containing eggs [38].
- Cause: Age of the sample or preservative evaporation.
- Solution: Ensure samples are stored in adequately filled, sealed containers. Monitor preservative levels during long-term storage. Top up with fresh preservative if needed. Strongyle-type eggs have been shown to be similarly preserved in both formalin and ethanol [68].
Problem: Inconsistent Morphological Grading Between Technicians
Issue: Different staff members assign different degradation scores to the same specimen.
Possible Causes & Solutions:
- Cause: Lack of a standardized, visual reference.
- Solution: Implement the use of a detailed, image-based grading rubric. Provide clear examples of each score for different parasite types (eggs, larvae, cysts) as a daily reference for all staff [68].
- Cause: Insufficient training in morphological parasitology.
Standardized Morphological Degradation Rubric
The following three-point scale is adapted from a 2024 study to standardize the assessment of parasite preservation. All parasites in a sample should be graded, and an average rating for the sample can be calculated [68].
Table 1: Morphological Degradation Scale for Parasite Larvae
| Grade | Description - Ethanol-Preserved | Description - Formalin-Preserved |
|---|---|---|
| 3 (Well-Preserved) | Fully intact cuticle; visible, clear internal structures; identifiable, unaltered external features [68]. | Fully intact cuticle; visible, clear internal structures; identifiable, unaltered external features [68]. |
| 2 (Moderately Degraded) | Degradation of cuticle (e.g., shrinking, puckering, thinning) OR internal structures; partially interferes with identification [68]. | Degradation of cuticle OR internal structures; may have some bubbles in body cavity; partially interferes with identification [68]. |
| 1 (Severely Degraded) | Heavily degraded; significant cuticle and internal structure changes; difficult or impossible to identify [68]. | Heavily degraded; internal structures completely obscured by bubbles or other artifacts; difficult or impossible to identify [68]. |
Table 2: Morphological Degradation Scale for Helminth Eggs
| Grade | Description for All Preservatives |
|---|---|
| 3 (Well-Preserved) | Clear, correct shape/size for taxon; visible embryo/larva; continuous, unobstructed, unbroken shell [68]. |
| 2 (Moderately Degraded) | Minor shell deformations (dents, breaks, increased opacity); may have impacted the developing parasite inside [68]. |
| 1 (Severely Degraded) | Badly preserved; severe shell collapse or rupture; embryo not discernible [68]. |
Experimental Protocol: Comparing Preservative Efficacy
This protocol provides a methodology for quantitatively assessing the impact of different preservatives on parasite morphology, as described in a 2024 study [68].
Objective: To evaluate the preservation quality of gastrointestinal parasites in fecal samples stored in 96% Ethanol versus 10% Buffered Formalin over time.
Materials:
- Fresh fecal sample
- Sterile 15 ml tubes
- 96% Ethanol
- 10% Buffered Formalin
- Distilled water
- Double-layered cheesecloth
- Centrifuge
- 6-well microscopy plate
- Microscope with camera
Methodology:
- Collection & Partitioning: Collect a fresh fecal sample and immediately partition it into two approximately equal halves (~2g each) [68].
- Preservation: Place one half into a tube containing 6 ml of 96% Ethanol. Place the other half into a tube containing 10 ml of 10% Buffered Formalin. Ensure samples are fully submerged and gently agitate to assist preservative permeation [68].
- Storage: Store all samples at ambient temperature for the desired study duration (e.g., 1 month, 1 year) [68].
- Processing: Process samples using a standardized sedimentation technique (e.g., modified Wisconsin technique): a. Separate solids from liquid and weigh the fecal matter. b. Homogenize with distilled water and strain through cheesecloth. c. Centrifuge the solution (10 min at 1500 rpm), discard supernatant. d. Re-homogenize the pellet with 5-10 ml distilled water. e. Transfer to a 6-well plate for microscopic screening [68].
- Analysis: Screen all samples microscopically. For each parasite found, identify it morphologically and assign a degradation score (1-3) using the standardized rubrics in Tables 1 and 2. Calculate the average preservation rating for each sample and compare between preservative groups [68].
Specimen Integrity Workflow
Research Reagent Solutions
Table 3: Essential Materials for Parasite Morphology Studies
| Reagent / Material | Function in Research |
|---|---|
| 10% Buffered Formalin | Primary fixative for optimal long-term morphological preservation; cross-links proteins to maintain tissue structure [68]. |
| 96% Ethanol (Ethanol) | A less toxic preservative suitable for molecular analysis; dehydrates tissues, which can alter morphology but preserves DNA [68]. |
| 70% Ethanol | Common concentration for long-term storage of samples intended for DNA extraction; prevents PCR inhibition from denatured alcohol [67]. |
| Commercial Non-Formalin Fixatives | Specialized fixatives designed to preserve both morphological detail and nucleic acid integrity for combined studies [67]. |
| Physiological Saline (0.9% NaCl) | A temporary storage medium that maintains osmotic balance, suitable for short-term holding before dividing samples for specific preservatives [67]. |
Mitigation Strategies for DNA Degradation in Suboptimal Storage Conditions
DNA degradation poses a significant challenge in parasitology research and education, particularly when specimens are stored under suboptimal conditions. Proper preservation is critical for maintaining both morphological integrity for traditional microscopy and DNA quality for genomic applications. This technical support center provides troubleshooting guidance and practical solutions to help researchers, scientists, and drug development professionals prevent DNA degradation in their parasitology work, ensuring reliable results for both educational and research purposes.
Frequently Asked Questions (FAQs)
What are the primary factors that accelerate DNA degradation in parasite specimens? DNA degradation is influenced by temperature, humidity, ultraviolet radiation, and enzymatic activity. Higher temperatures significantly accelerate degradation rates, making room temperature storage particularly problematic for DNA preservation. In parasitology, the choice of preservative solution is crucial, as some common fixatives like ethanol provide poor long-term DNA protection compared to specialized solutions like DESS [69] [70].
Which preservation method provides the best DNA quality for genomic applications? Research indicates that DESS (20% DMSO, 0.25 M EDTA, NaCl saturated solution) provides superior DNA preservation compared to ethanol, particularly for long-term storage. One study found that DNA stored in ethanol showed high levels of degradation within just 24 hours, while DESS-preserved samples maintained DNA integrity for up to three months, making them more suitable for next-generation sequencing applications [69].
Can I use the same preservation method for both morphological study and DNA analysis? Some preservatives support both applications, but with limitations. Polyvinyl Alcohol (PVA) allows preparation of permanent stained smears for morphological examination and can be used for concentration techniques, though it may not preserve all helminth eggs equally well. Sodium Acetate Formalin (SAF) permits both concentration techniques and stained smears without containing mercury compounds, though protozoan morphology with trichrome stain may not be as clear as with PVA [20].
How does specimen storage temperature affect DNA degradation rates? Storage temperature significantly impacts DNA degradation. One study demonstrated that arthropod specimens stored at room temperature for four weeks showed markedly higher DNA degradation compared to those immediately frozen at -20°C. This is particularly relevant for samples collected via passive sampling devices like Malaise traps, which may remain in the field for extended periods under suboptimal conditions [71].
Troubleshooting Guides
Problem: Poor DNA Yield from Archived Parasite Specimens
Possible Causes and Solutions:
- Cause: Inappropriate preservative used during initial specimen collection
- Solution: For new collections, use DESS solution instead of ethanol for better long-term DNA preservation [69]
- Cause: Extended storage at room temperature
- Solution: Implement cold storage (freezing) for long-term preservation whenever possible [71]
- Cause: Formalin-based preservation damaging DNA
- Solution: For specimens requiring morphological analysis, consider SAF (Sodium Acetate Formalin) which is less damaging than standard formalin for DNA analysis [20]
Problem: Inconsistent PCR Amplification from Parasite DNA
Possible Causes and Solutions:
- Cause: DNA fragmentation from degradation
- Solution: Use PCR primers that target shorter DNA fragments (under 350 bp) for more reliable amplification of degraded samples [71]
- Cause: PCR inhibitors carried over from preservation solutions
- Solution: Implement additional purification steps or use inhibitor-resistant polymerase enzymes
- Cause: Preferential amplification of less degraded DNA
- Solution: Use multiplex PCR systems specifically designed for degraded DNA, targeting smaller amplicons [72]
Problem: Maintaining Both Morphology and DNA Quality for Educational Specimens
Possible Causes and Solutions:
- Cause: Single preservative unable to serve both purposes optimally
- Solution: Create duplicate specimens preserved differently - PVA for morphological study and DESS for DNA analysis [69] [20]
- Cause: Digital alternatives not utilized
- Solution: Develop whole-slide imaging (WSI) collections of parasite specimens to preserve morphology indefinitely while allowing original specimens to be optimized for DNA preservation [41]
Experimental Protocols & Data
Comparative Analysis of Preservation Solutions
Table 1: DNA Preservation Performance of Different Solutions Over Time
| Preservation Solution | 24 Hours | 1 Week | 1 Month | 3 Months | Suitable for Genomic Sequencing |
|---|---|---|---|---|---|
| DESS | Minimal degradation | Minimal degradation | Moderate degradation | Moderate degradation | Yes |
| >99.5% Ethanol | High degradation | High degradation | High degradation | High degradation | No |
| DMSO-salt solution | Minimal degradation | Minimal degradation | Minimal degradation | Minimal degradation | Yes [73] |
| 10% Formalin | Moderate degradation | Moderate degradation | High degradation | High degradation | No [20] |
Table 2: Applications of Common Parasitology Preservatives
| Preservative | Primary Use | DNA Preservation | Morphology Preservation | Limitations |
|---|---|---|---|---|
| Schaudinn's | Stained smears | Poor | Excellent | Contains mercury; not for concentration |
| PVA | Stained smears & concentration | Moderate | Good | Contains mercury; some morphology distortion |
| SAF | Concentration & stained smears | Fair | Good | Poor adhesive properties |
| 10% Formalin | Concentration | Poor | Excellent | Cannot prepare stained smears |
| MIF | Field surveys | Poor | Fair | Unstable; difficult stained smears |
DNA Size Selection Protocol for Degradation Assessment
This protocol helps researchers evaluate the extent of DNA degradation in their specimens [71]:
- Extract DNA from parasite specimens using standard extraction kits
- Perform size selection using 0.75X concentration of Ampure Beads XP:
- Retain DNA bound to beads (high molecular weight fraction)
- Precipitate low molecular weight DNA from supernatant
- Amplify both fractions using the same primer pairs (e.g., mitochondrial COI for parasites)
- Compare results between high and low molecular weight fractions to assess degradation bias
DNA Degradation Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for DNA Preservation in Parasitology Research
| Reagent | Function | Application Notes |
|---|---|---|
| DESS (20% DMSO, 0.25 M EDTA, NaCl saturated) | DNA preservation | Superior for genomic applications; prevents degradation for up to 3 months [69] |
| DMSO-salt solution | Tissue preservation without freezing | Excellent DNA protection for up to 2 years; better than ethanol or lysis buffer [73] |
| Polyvinyl Alcohol (PVA) | Morphology preservation with DNA utility | Allows stained smears and molecular techniques; contains mercury compounds [20] |
| Sodium Acetate Formalin (SAF) | Mercury-free alternative | Suitable for concentration and stained smears; better with hematoxylin than trichrome [20] |
| Ampure Beads XP | DNA size selection | Enables separation of degraded vs. intact DNA for quality assessment [71] |
| Qiagen Puregene Kit | DNA extraction | Effective for parasite specimens; compatible with various preservatives [71] |
Advanced Techniques for Degraded DNA Analysis
When working with historically preserved specimens or suboptimally stored samples, these advanced approaches can recover valuable data:
Mitochondrial DNA Targeting: Due to its higher copy number per cell, mitochondrial DNA often survives when nuclear DNA is too degraded for analysis. This is particularly useful for identifying parasite species from degraded specimens [70] [72].
Short Amplicon Strategies: Design PCR primers to amplify shorter DNA fragments (200-350 bp) that are more likely to remain intact in degraded samples. This approach has proven successful in metabarcoding studies of arthropod communities with partially degraded DNA [71].
Whole Genome Amplification: For extremely limited or degraded samples, multiple displacement amplification using bacteriophage DNA polymerase can amplify the entire genome from small amounts of starting material, enabling subsequent analysis [72].
Digital Archiving Complement: Create whole-slide digital images of parasite specimens for morphological reference while optimizing original specimens for DNA preservation. This approach helps balance the needs of traditional parasitology education with modern molecular techniques [41].
FAQs on Handling High-Risk Infectious Specimens
Q1: What defines a specimen as 'high-risk'? A specimen is classified as 'high-risk' if it comes from a patient known or suspected to be infected with certain pathogens. These include Hepatitis B or C, HIV, HTLV-1, Creutzfeldt-Jakob disease (CJD), Viral Haemorrhagic Fevers (e.g., Ebola), and other hazardous pathogens such as TB, Typhoid, and Brucella. This classification also includes all febrile travelers returning from areas at high risk for Typhoid and Brucella [74].
Q2: What are the mandatory labeling and packaging requirements for high-risk specimens? Each high-risk specimen must be clearly labelled 'DANGER OF INFECTION' and sealed in its own separate plastic bag. The request card or tab at the top of the specimen bag must also state 'DANGER OF INFECTION'. The request card should not be sealed in the same pocket as the specimen to prevent contamination [74]. For suspected smallpox cases, high-risk specimens must be packaged and transported as a Category A infectious substance (UN 2814) [75].
Q3: What personal protective equipment (PPE) is required when handling high-risk specimens? The required PPE is extensive, especially for post-mortem procedures [75]:
- Protective Garments: Scrub suit, surgical cap, impervious gown with full sleeve coverage, shoe covers, and a double set of gloves with an interposed layer of cut-proof synthetic mesh gloves.
- Respiratory Protection: Fit-tested N95 or N100 respirators or Powered Air-Purifying Respirators (PAPR) with a HEPA filter are required for all personnel, including those with recent vaccinations.
- Eye and Face Protection: Goggles or a face shield are mandatory.
Q4: What are the critical engineering controls for an autopsy suite handling high-risk pathogens? Autopsy suites must have specific engineering designs to ensure safety [75]:
- Air Handling: The suite must have a minimum of 12 air exchanges per hour and must be at a negative pressure relative to adjacent areas.
- Air Exhaust: Air should be exhausted directly outdoors, away from air intake systems and human gathering spaces.
- Containment Devices: Biosafety cabinets should be available for handling smaller specimens, and oscillating saws with vacuum shrouds should be used to reduce aerosols.
Troubleshooting Guide for Inhibitor-Rich Samples
Inhibitor-rich samples, such as soils, stool, and sputum, contain substances that can suppress enzymatic reactions critical to molecular analyses like PCR and DNase digestion [76] [77]. The table below outlines common symptoms and their solutions.
Table 1: Troubleshooting Common Issues with Inhibitor-Rich Samples
| Observed Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Failed or inefficient DNase digestion during RNA extraction, leading to genomic DNA contamination [76]. | Enzyme inhibition due to co-purified contaminants (e.g., humic acids, polyphenolics). | Implement extensive purification of nucleic acids prior to all enzymatic procedures. Do not perform enzymatic treatments on crude extracts [76]. |
| Low sensitivity or false negatives in qPCR/RT-qPCR from crude samples (e.g., stool, sputum, blood) [77]. | PCR inhibitors in the sample are co-purified with nucleic acids or are present in the lysate. | Use an inhibitor-tolerant qPCR or RT-qPCR master mix designed for direct amplification from crude lysates, eliminating the need for extraction [77]. |
| Poor recovery of nucleic acids from complex environmental samples [76]. | Inefficient lysis or binding due to sample heterogeneity and inhibitors. | Optimize the lysis step by testing different bead types for bead-beating. Introduce additional purification steps and use precipitation methods that improve yield in the presence of inhibitors [76]. |
| Inconsistent digestion results between replicate samples [76]. | Variable carryover of inhibitors between samples, making "representative" testing unreliable. | Treat each sample individually and ensure rigorous, uniform purification for all replicates before DNase addition [76]. |
Experimental Protocols for Ensuring Sample Integrity
Protocol: Preserving Fecal Specimens for Parasitology
This protocol ensures the preservation of protozoan cysts and helminth eggs and larvae for morphological diagnosis [20] [78].
Methodology:
- Add Specimen to Preservative: Wear gloves. Add a portion of fecal material (a grape-sized formed specimen or about 5 ml of liquid) to a preservative vial.
- Achieve Correct Ratio: Use a 3:1 or 5:1 ratio of preservative to fecal material.
- Mix Thoroughly: Mix well with an applicator stick to create a homogeneous solution.
- Fixation Time: Allow the mixture to stand for 30 minutes at room temperature for adequate fixation.
Table 2: Common Preservatives for Fecal Parasitology
| Preservative | Primary Use | Key Advantages | Key Disadvantages |
|---|---|---|---|
| 10% Buffered Formalin [20] | Concentration techniques for protozoan cysts and helminth eggs/larvae. | Good all-purpose preservative; long shelf life; commercially available [20]. | Permanent stained smears cannot be prepared from formalin-preserved specimens [20]. |
| PVA (Polyvinyl Alcohol) [20] | Permanent stained smears and concentration techniques. | Excellent preservation for protozoa; allows long-term storage and shipment [20]. | Contains mercury compounds (disposal issues); some helminth eggs are not concentrated well [20]. |
| SAF (Sodium Acetate Formalin) [20] | Concentration techniques and stained smears. | Contains no mercury compounds; long shelf life [20]. | Has poor adhesive properties, often requiring albumin-coated slides for smears [20]. |
Protocol: Optimized DNA/RNA Co-extraction from Inhibitor-Rich Soils
This protocol, optimized from phenol-chloroform methods, is designed for metagenomic and metatranscriptomic analyses of challenging environmental samples [76].
Key Methodological Improvements:
- Enhanced Purification Prior to Enzymatic Treatment: The core principle is to introduce extensive purification procedures before any enzymatic step, particularly before DNase digestion. This removes enzymatic inhibitors that are ubiquitous in inhibitor-rich soils [76].
- Pre-DNase Purification: Crude nucleic acid extracts must be purified to remove contaminants like humic and fulvic acids. This step is critical to activate the DNase enzyme fully.
- Post-DNase Verification: After digestion, the success of genomic DNA removal must be verified using a sensitive technique like quantitative PCR. This verification should be performed on each sample replicate, as digestion efficiency may vary [76].
The following workflow diagram outlines the critical steps for handling inhibitor-rich samples, highlighting the points where troubleshooting interventions are most critical.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for High-Risk and Inhibitor-Rich Sample Analysis
| Item / Reagent | Function | Application Note |
|---|---|---|
| Inhibitor-Tolerant qPCR/RT-qPCR Mix [77] | Enables direct amplification from crude, unprocessed samples. | Eliminates need for nucleic acid extraction; ideal for sputum, stool, saliva, urine, and blood; provides robust results despite inhibitors [77]. |
| PVA (Polyvinyl Alcohol) Fixative [20] | Preserves morphology and allows stained smears of parasites. | Critical for parasitology; preserves protozoan trophozoites and cysts; enables preparation of permanent stained slides for diagnosis [20]. |
| 10% Buffered Formalin [20] [75] | All-purpose fixative for histology and parasitology concentration. | Used for preserving helminth eggs and larvae in stool; also used for fixing tissue specimens during autopsy for histopathology [75]. |
| Fit-Tested N95/PAPR Respirators [75] | Protects respiratory system from airborne pathogens. | Mandatory PPE for all personnel handling high-risk specimens in autopsy settings, even if recently vaccinated [75]. |
| Sharps Disposal Containers [79] | Safe disposal of contaminated sharps. | An engineering control to prevent percutaneous injuries; contaminated sharps must not be bent, recapped, or removed [79]. |
FAQs: Understanding Sample Rejection
What are the most common reasons for sample rejection in parasitology?
Samples are most commonly rejected for labeling errors, improper collection, and excessive transport delays [80]. Unlabeled or partially labeled specimens cannot be processed and are automatically rejected. Samples delayed in transport for over 24 hours are not suitable for analysis, as parasite morphology deteriorates, compromising identification accuracy [80]. Additionally, samples received with needles attached to syringes are immediately discarded due to safety hazards [80].
How should fecal specimens be collected to avoid rejection?
Proper fecal specimen collection requires approximately 10 grams of fresh feces collected in a clean container uncontaminated by urine, oil, water, or disinfectants [81]. Specimen containers must be free from antiseptics and disinfectants that could destroy parasites [81]. For formed samples, short-term refrigeration at +4°C is acceptable, but preservation is needed if examination delays exceed a few hours [81]. Any whole worms or segments passed should be placed in a separate container [81].
What are the essential labeling requirements for specimens?
Essential labeling requirements include [80]:
- Patient's full name or unique coded identifier
- NHS, CHI, Health and Care Number, or Hospital number
- Date of birth and/or hospital number
- Date and time of collection (essential for certain tests)
- Identification of person taking the sample (essential for blood tests)
Request forms must also include gender, patient location, requesting practitioner, required investigations, and clinical information including relevant medication [80].
What specialized handling do parasitology specimens require?
Parasitology specimens often require immediate processing or appropriate preservation to prevent morphological deterioration [38]. Examination should be performed by experienced staff trained in parasitology who regularly process these specimens [38]. For certain parasitic infections, specialized testing through serology or polymerase chain reaction performed at reference laboratories may be necessary [38].
Troubleshooting Guides
Guide: Addressing Common Sample Rejection Issues
| Rejection Cause | Prevention Strategy | Corrective Action |
|---|---|---|
| Incomplete Labeling [80] | Use pre-printed labels with essential patient identifiers; verify before dispatch. | Re-collect sample with complete identification. |
| Improper Transport Temperature [80] | Maintain required temperature (e.g., 4°C for cryoglobulins); use appropriate transport containers. | Discard sample; educate staff on specific test requirements. |
| Excessive Transport Delay [80] [38] | Arrange prompt transport; use preservatives for delays >4 hours [81]. | Process specimen if within acceptable timeframe; otherwise reject. |
| Hemolyzed Samples [82] | Use proper needle size; avoid forced transfer from syringes. | Re-collect if hemolysis affects test accuracy. |
| Insufficient Sample Volume [82] | Collect recommended blood volume (e.g., 2.0 mL minimum for biochemistry). | Re-collect with adequate volume for requested tests. |
| Wrong Collection Tube [82] | Consult tube selection guide; fill tubes with correct additive-to-blood ratio. | Re-collect using specified tube type for test. |
Guide: Parasitology-Specific Rejection Scenarios
| Rejection Scenario | Quality Concern | Resolution |
|---|---|---|
| Unpreserved Stool >24-48 Hours [81] | Trophozoite degradation; cyst distortion. | Reject sample; request fresh collection with preservative. |
| Urine for S. haematobium - Random Sample [38] | Low egg excretion rate; false negative. | Request terminal urine (last 10-20 mL) or 24-hour collection. |
| Multiple Patient Samples in One Bag [80] | Cross-contamination risk; biohazard if leakage. | Discard all samples; require separate packaging per patient. |
| Inadequate Clinical Information [38] | Improper test selection; interpretation difficulty. | Contact requester for travel history, symptoms, exposure risks. |
Table 1: Specimen Labeling and Handling Rejection Criteria
| Criterion | Essential Requirements | Rejection Trigger |
|---|---|---|
| Patient Identification [80] | Full name, NHS/CHI number, Date of Birth | Missing or mismatched identifiers |
| Sample Labeling [80] | Date/time of collection, sample type/source | Unlabeled or partially labeled specimens |
| Transport Conditions [80] | Appropriate temperature, timely delivery | >24-hour delay; improper temperature |
| Sample Integrity [80] | No leakage, proper container, no attached needles | Leaking containers, needles attached, wrong container type |
| Request Form Completion [80] | Complete clinical data, tests clearly marked | Missing clinical information, tests not specified |
Table 2: Technical Rejection Criteria by Sample Type
| Sample Type | Rejection Criteria | Quality Impact |
|---|---|---|
| Blood Samples [82] | Hemolysis, improper anticoagulant ratio, underfilled tubes | Altered cell morphology, inaccurate chemistry results |
| Stool for Parasitology [81] | Unpreserved delay >4 hours, urine contamination, insufficient quantity | Trophozoite disintegration, parasite degradation |
| Urine for Parasites [38] | Non-terminal stream, improper preservation | Missed S. haematobium infection (low egg count) |
| Tissue/Aspirates [38] | Delay in processing, improper fixation | Cellular autolysis, parasite morphology loss |
Research Reagent Solutions
Table 3: Essential Materials for Parasitology Specimen Processing
| Item | Function | Application Notes |
|---|---|---|
| Saline Solution [81] | Wet mount preparation for initial examination | Demonstrates worms' eggs, larvae, protozoan trophozoites, and cysts |
| Iodine Solution [81] | Stains glycogen and nuclei of cysts | Enables specific identification of cysts |
| Buffered Methylene Blue [81] | Stains amoebic trophozoites | Confirms presence of suspected amoebic trophozoites |
| Formalin (10%) [38] | Preserves parasite morphology in urine | Prevents hatching of S. haematobium eggs during storage |
| Sodium Citrate Tubes [82] | Anticoagulant for coagulation studies | Light blue tops; requires 3-4 gentle inversions after collection |
| EDTA Tubes [82] | Anticoagulant for hematology | Lavender tops; requires 8 gentle inversions after collection |
| Serum Separator Tubes [82] | Clot activator and gel for serum separation | For serum determinations in chemistry; requires 5 inversions |
Experimental Protocols for Quality Assurance
Protocol 1: Direct Saline and Iodine Wet Mount Preparation
Purpose: Initial microscopic examination of stools for worm eggs, larvae, protozoan trophozoites, and cysts [81].
Materials: Microscope slides, coverslips, saline solution, iodine solution, applicator sticks, fresh stool specimen.
Methodology:
- Label slide with patient identifier and date using a wax pencil [81].
- Place drop of saline on left half of slide and drop of iodine on right half [81].
- With applicator stick, pick small portion of specimen (match head size) and mix with saline drop [81].
- Using same applicator, pick another portion and mix with iodine drop [81].
- Apply coverslips to both preparations, avoiding air bubbles [81].
- Examine systematically under microscope, beginning with 10x objective [81].
Quality Notes: If amoebic trophozoites are suspected, use warm saline (37°C) [81]. Examine mounts immediately for optimal trophozoite motility and morphology.
Protocol 2: Specimen Concentration Procedure
Purpose: Separate parasites from fecal debris to increase detection sensitivity [81].
Principle: Concentration procedures increase the number of parasites in sediment while removing organic and inorganic debris, making parasites more visible [81].
Method Selection Guide:
- Sedimentation: Preferred for heavy eggs (Ascaris), operculated eggs (trematodes), and larvae (Strongyloides stercoralis) [81].
- Flotation: Recommended for non-operculated eggs (cestodes, hookworms, Trichostrongylus) and cysts [81].
Quality Assurance: A minimum of three serial stools must be examined before considering a patient free from parasitic infections [81].
Workflow Diagrams
Sample Quality Control Workflow
Parasitology Rejection Criteria
Validating Preservation Efficacy: Comparative Studies of Traditional and Emerging Diagnostic Platforms
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: Why did my molecular test return a positive result when my microscopy examination was negative? This is a common scenario due to the higher sensitivity of molecular methods. One study found that 20.57% (72 out of 350) of samples diagnosed as negative by microscopy for Plasmodium falciparum were positive by nested PCR [83]. For specific parasites like Cryptosporidium spp., microscopy may fail to detect the organism entirely, while PCR can identify positive cases [84]. This discrepancy is often due to the molecular method's ability to detect very low parasite loads that are below the detection threshold of conventional microscopy.
Q2: My fresh stool sample was negative for Giardia by microscopy, but I suspect the result is inaccurate. What are my options? You should consider testing with a molecular method. A comparative study demonstrated that the sensitivity of microscopy for detecting Giardia intestinalis was only 38% compared to PCR [84]. Furthermore, if the sample was not preserved correctly or there was a delay in examination, parasite morphology may have degraded. Submitting a preserved sample for PCR analysis is a highly reliable alternative, as PCR is less affected by delays and can provide definitive identification [85] [86].
Q3: What is the primary disadvantage of using molecular methods like PCR in resource-limited settings? While molecular methods offer superior sensitivity and specificity, their implementation in resource-limited settings is challenged by several factors [86]:
- They require expensive and sophisticated equipment.
- They depend on highly trained personnel.
- They need molecular-grade reagents, reliable electricity, and controlled storage conditions. Although newer, simpler isothermal techniques are being developed, infrastructure deficiencies often impede widespread NAAT adoption [86].
Q4: For which parasites is molecular differentiation particularly crucial? Molecular methods are essential for differentiating between morphologically identical species that have vastly different clinical implications. The most notable example is distinguishing the pathogenic Entamoeba histolytica from the non-pathogenic Entamoeba dispar [85] [87] [86]. Microscopy alone cannot tell them apart, which can lead to misdiagnosis and inappropriate treatment.
Troubleshooting Guides
Problem: Low Sensitivity in Molecular Detection of Dientamoeba fragilis from Preserved Stool.
- Potential Cause: Inadequate DNA extraction due to the robust wall structure of protozoan cysts and oocysts [85].
- Solution: Review and optimize the DNA extraction protocol. Ensure that the method includes mechanical disruption steps (e.g., bead beating) to effectively break down the parasite wall and release DNA. Comparing the performance of your extraction method with a commercial kit validated for parasitology may be beneficial [85].
Problem: Distorted Morphology of Helminth Eggs in Preserved Specimens.
- Potential Cause: Use of an inappropriate preservative. For instance, polyvinyl alcohol (PVA) is excellent for protozoa but is known to distort the morphology of some helminth eggs, such as Trichuris trichiura, and Giardia cysts [20].
- Solution: For comprehensive parasitological surveys aiming to detect both protozoa and helminths, 10% neutral buffered formalin is the recommended preservative as it is suitable for concentrating helminth eggs and larvae and preserving protozoan cysts [20]. Always match the preservative to your primary diagnostic goals.
Problem: High Rate of False-Negative Malaria Results by Microscopy.
- Potential Cause: Low parasite density and reliance on a single diagnostic method [83].
- Solution: Implement a diagnostic algorithm that uses rapid antigen tests for initial, quick screening and follows up smear-negative but clinically suspected cases with a more sensitive molecular method like nested PCR. This approach significantly reduces misdiagnosis [83].
Data Comparison: Method Performance
Table 1: Comparative Sensitivity of Diagnostic Methods for Key Parasites
| Parasite | Microscopy Sensitivity (vs. Reference) | Molecular Method (PCR) Sensitivity | Key Contextual Notes |
|---|---|---|---|
| Plasmodium falciparum | Not explicitly calculated [83] | 100% [83] | Study found 72/350 microscopy-negative samples were positive by nested PCR [83]. |
| Giardia intestinalis | 38% (vs. PCR) [84] | Used as reference [84] | Median CT values for PCR-only positive samples were higher (32.02), indicating lower parasite load [84]. |
| Cryptosporidium spp. | 0% (vs. PCR) [84] | Used as reference [84] | Detected in 16 samples by PCR, all with high CT values (>32) [84]. |
| Blastocystis sp. | 30% (vs. culture) [84] | Not Applicable | Culture was used as the comparative method in this study [84]. |
| Entamoeba histolytica | Limited, cannot differentiate from non-pathogenic E. dispar [85] | High, enables species-specific detection [85] [86] | Molecular assays are critical for accurate diagnosis [85]. |
Table 2: Advantages and Disadvantages of Common Specimen Preservatives
| Preservative | Primary Use | Advantages | Disadvantages |
|---|---|---|---|
| PVA (Polyvinyl Alcohol) | Permanent stained smears; preserves protozoan trophozoites and cysts [20] | Allows concentration and stained smears; long shelf life; good for shipping [20] | Contains mercury compounds; not ideal for helminth egg concentration (can distort morphology) [20] |
| 10% Formalin | Concentration techniques for helminth eggs/larvae and protozoan cysts [20] | Good all-purpose preservative; long shelf life; commercially available [20] | Cannot be used to prepare permanent stained smears [20] |
| SAF (Sodium Acetate Formalin) | Concentration and permanent stained smears [20] | Mercury-free; long shelf life [20] | Poor adhesive property for smears; protozoan morphology with trichrome stain not as sharp as with PVA [20] |
| Schaudinn's Fluid | Fixation for permanent stained smears from fresh samples [20] | Excellent for protozoan morphology on stained smears [20] | Not recommended for concentration; contains mercury compounds [20] |
Experimental Protocols
Protocol 1: DNA Extraction from Dried Blood Spots for Malaria PCR
This protocol is adapted from a study comparing microscopy and PCR for Plasmodium falciparum detection [83].
- Sample Preparation: Cut a 4mm² piece of filter paper with a dried blood spot.
- Incubation: Incubate the sample in 0.5% saponin in 1X PBS overnight at 4°C to lyse blood cells.
- Washing: Remove the brown saponin solution and replace it with 1X PBS. Incubate for 20 minutes.
- DNA Extraction: Remove the PBS and add 100µl of DNase-free water followed by 50µl of 20% Chelex resin.
- Heating: Place the tubes in a heating block. Vortex them every 2 minutes for a total of 5 cycles to lyse parasites and release DNA.
- Collection: Centrifuge the solution. Carefully transfer the supernatant, which contains the extracted DNA, to a new tube.
- Storage: Store DNA aliquots at -20°C until PCR analysis [83].
Protocol 2: Formol-Ethyl Acetate Concentration Technique (FECT) for Stool Specimens
This is a standard method for concentrating parasites in stool samples prior to microscopic examination [84].
- Emulsification: Emulsify 1-2 grams of fresh or preserved stool in 10 mL of 10% formalin.
- Filtration: Filter the suspension through gauze or a sieve into a conical tube to remove large debris.
- Solvent Addition: Add 3-4 mL of ethyl acetate to the filtrate. Stopper the tube and shake it vigorously for 30 seconds.
- Centrifugation: Centrifuge the tube at 500 x g for 2-3 minutes. This will create four layers: ethyl acetate (top), plug of debris, formalin, and sediment (bottom).
- Sediment Recovery: Loosen the debris plug by ringing it with an applicator stick. Decant the top three layers carefully.
- Examination: Use a swab or pipette to transfer a drop of the sediment onto a microscope slide for examination. Examine both unstained and iodine-stained preparations [84].
Workflow Visualization
The following diagram illustrates the decision-making workflow for selecting a diagnostic method based on research objectives and resources, as discussed in the cited literature.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Parasitology Diagnostics
| Item | Function & Application |
|---|---|
| Chelex Resin | A chelating resin used in rapid, small-scale DNA extraction protocols, particularly from blood spots, by binding metal ions that can degrade DNA [83]. |
| Polyvinyl Alcohol (PVA) | A plastic resin added to Schaudinn's fixative. It acts as an adhesive, allowing stool material to stick to glass slides for permanent staining, and is ideal for preserving protozoan trophozoites and cysts [20]. |
| Neutral Buffered Formalin (10%) | An all-purpose fixative and preservative ideal for helminth eggs and larvae and protozoan cysts. It is used primarily for concentration techniques [20]. |
| Ethyl Acetate | A solvent used in the Formol-Ethyl Acetate Concentration Technique (FECT) to extract fats and debris from fecal suspensions, resulting in a cleaner sediment for microscopic examination [84]. |
| Whatman Filter Paper | Used for collecting and storing dried blood spots (DBS) or fecal samples. DBS are a stable and convenient way to transport specimens for later DNA extraction and PCR analysis [83]. |
| MagNA Pure System | An automated platform for nucleic acid extraction. It standardizes and streamlines the DNA/RNA purification process, reducing hands-on time and variability in molecular workflows [85]. |
Systematic Comparison of Commercial and In-House PCR Assays for Fixed vs. Fresh Specimens
In parasitology education and research, the integrity of biological specimens is paramount. The choice between using formalin-fixed paraffin-embedded (FFPE) tissue versus fresh specimens, and the subsequent selection of appropriate PCR assays, significantly impacts diagnostic accuracy and experimental outcomes. This technical support center resource provides a systematic framework for comparing commercial and in-house PCR methodologies, with particular emphasis on preventing specimen deterioration through optimized protocols. The guidance herein is specifically contextualized within parasitology research, addressing unique challenges such as the preservation of parasite DNA and the inhibition caused by fixatives used in specimen preparation.
Performance Comparison Tables
Table 1: Comparison of commercial vs. in-house PCR assay performance across multiple pathogens
| Target Pathogen | Assay Type | Sensitivity | Specificity | Specimen Type | Key Limitations |
|---|---|---|---|---|---|
| Various Fungi | In-house ITS2 PCR | 53.8% | 100% | FFPE tissue | Degraded DNA, PCR inhibitors [88] |
| Various Fungi | In-house ITS1-2 PCR | 38% | 100% | FFPE tissue | Longer amplicon more affected by degradation [88] |
| Enteropathogenic Bacteria | FTD Commercial Kit | 75-100% (strong positive), 20-100% (weak positive) | 98.6-100% | Stool | Variable sensitivity for weakly positive samples [89] |
| Enteropathogenic Bacteria | ampliCube Commercial Kit | 87.3-100% (strong positive), 20-100% (weak positive) | 96-100% | Stool | Wide sensitivity range for weak positives [89] |
| Mycoplasma pneumoniae | In-house RepMp1 | ~100% | ~100% | Respiratory specimens | Multicopy target advantage [90] |
| Mycoplasma pneumoniae | artus Commercial Kit | ~100% | ~100% | Respiratory specimens | Comparable to in-house [90] |
| Pneumocystis jirovecii | In-house PCR | 65% | 85% | BAL | Requires cut-off value (Ct=34) [91] |
| Pneumocystis jirovecii | Bio-Evolution Commercial PCR | 72% | 82% | BAL | Requires cut-off value (2.8×10⁵ copies/mL) [91] |
Practical Implementation Considerations
Table 2: Operational characteristics and practical considerations for PCR assays
| Parameter | Commercial Kits | In-House Assays |
|---|---|---|
| Standardization | High (standardized protocols, reagents) | Variable (lab-dependent optimization) |
| Regulatory Compliance | CE-IVD marked [89] | Must meet Regulation (EU) 2017/746 [89] |
| Turnaround Time | Optimized workflows | May require additional confirmation steps |
| Customization Flexibility | Limited | High (primer/probe modification possible) |
| Inhibition Resistance | Varies by kit; some include inhibition controls [89] | Can be optimized for specific specimen types |
| Cost Structure | Higher reagent cost | Lower reagent but higher development/validation costs |
| Multi-target Capacity | Fixed multiplex panels | Customizable multiplexing |
Experimental Protocols
DNA Extraction from FFPE Tissue for Fungal Detection
Purpose: To obtain quality DNA from formalin-fixed paraffin-embedded tissue for panfungal PCR detection in parasitology research [88].
Specimen Requirements: Three 20μm tissue slices from FFPE block collected from sterile sites.
Reagents and Materials:
- Xylol
- Ethanol (100%)
- QIAamp Mini Kit (Qiagen)
- Proteinase K
- ATL buffer
- AE buffer
Procedure:
- Transfer tissue slices to a sterile 1.5 mL vial.
- Add 1 mL xylol and incubate for 5 minutes.
- Centrifuge at 14,000 rpm for 1 minute and discard xylol.
- Add 1 mL ethanol and incubate at room temperature for 1 minute.
- Centrifuge at 14,000 rpm for 1 minute and discard ethanol.
- Dry deparaffinized tissue in SpeedVac for 20 minutes.
- Extract DNA using QIAamp Mini Kit according to manufacturer's instructions with modification: add heating step of 95°C for 12 minutes after adding 200 μL AL buffer.
- Incubate samples overnight in proteinase K and ATL buffer at 56°C.
- Elute DNA with 100 μL AE buffer.
- Store extracted DNA at -20°C.
Quality Assessment:
- Evaluate DNA quality using multiplex PCR amplification of beta-globin gene fragments (262 bp, 408 bp, 860 bp) [88].
- Test for PCR inhibition by spiking with C. krusei DNA and monitoring amplification.
Verification Protocol for Commercial PCR Assays
Purpose: To validate commercial PCR assays against established in-house methods prior to implementation [89].
Specimen Requirements:
- 241 patient stool samples
- 100 external laboratory control scheme samples
Reagents and Materials:
- QIAamp DNA Stool Mini Kit (Qiagen)
- FTD Bacterial Gastroenteritis Kit (Siemens) or ampliCube Gastrointestinal Bacterial Panels 1&2 (Mikrogen)
- Rotor-Gene Q cycler (Qiagen)
Procedure:
- Extract nucleic acids from all specimens using QIAamp DNA Stool Mini Kit.
- Store extracted nucleic acids at -80°C until analysis.
- Test all specimens in parallel with in-house PCR and commercial assays.
- For in-house PCR: Use established protocols targeting Salmonella spp., Shigella spp./EIEC, Campylobacter jejuni, and Yersinia spp. with Phocid Herpes virus DNA internal control [89].
- For commercial assays: Follow manufacturer instructions precisely.
- Include appropriate controls: negative controls (external laboratory samples confirmed negative), strongly positive samples (Ct<34), weakly positive samples (Ct>34).
Performance Assessment:
- Calculate sensitivity and specificity with in-house PCR as gold standard.
- Perform latent class analysis for method comparison without gold standard.
- Assess intra- and inter-assay variation by calculating Ct value variability.
- Compute Cohen's kappa for agreement between methods.
Troubleshooting Guides & FAQs
Specimen-Related Issues
Q: Why is my PCR sensitivity lower with FFPE specimens compared to fresh specimens? A: Formalin fixation causes DNA degradation and crosslinking, significantly reducing PCR sensitivity. In FFPE tissues, shorter amplicon targets (e.g., ITS2 at 53.8% sensitivity) outperform longer targets (e.g., ITS1-2 at 38% sensitivity) [88]. To maximize sensitivity:
- Design primers to amplify shorter fragments (<200 bp)
- Implement an extended proteinase K digestion (overnight at 56°C)
- Add a heating step (95°C for 12 minutes) after lysis buffer addition
- Use DNA polymerases with high processivity tolerant to inhibitors [92]
Q: How can I prevent specimen deterioration in parasitology research? A: Proper preservation begins immediately after collection:
- For fresh specimens for molecular work: freeze immediately at -80°C or use nucleic acid preservation buffers
- For morphological preservation: use 4% buffered formalin for no more than 24-48 hours to minimize DNA damage [88]
- For stool specimens in parasitology: use appropriate transport systems like Para-Pak with formalin, PVA, or SAF based on intended testing [61]
- Limit storage time of FFPE blocks; significant time-dependent degradation occurs, affecting PCR success [88]
PCR Amplification Problems
Q: What should I do when no amplification products are obtained? A: Follow this systematic troubleshooting approach:
- First, verify all PCR components were included using a positive control [93]
- Increase cycle number (3-5 cycles at a time, up to 40 cycles) for low-abundance targets [93]
- Reduce stringency: lower annealing temperature in 2°C increments, increase extension time [93]
- Check for PCR inhibitors: dilute template 10-100 fold or repurify using silica membrane columns [93]
- For FFPE DNA: test different input volumes (0.5, 2, 5, and 10 μL) to overcome inhibitors [88]
Q: How can I reduce nonspecific amplification in my PCR assays? A: Nonspecific bands indicate suboptimal reaction conditions:
- Increase annealing temperature incrementally (2°C steps) or use touchdown PCR [93]
- Reduce template amount by 2-5 fold [93]
- Use hot-start DNA polymerases to prevent primer-dimer formation [92]
- Optimize Mg2+ concentration (typically 1-5 mM); excess Mg2+ promotes nonspecific amplification [92]
- Review primer design using BLAST to ensure specificity to target [93]
- Shorten annealing time (5-15 seconds) for high-fidelity polymerases [93]
Assay Selection & Validation
Q: When should I replace my in-house PCR assay with a commercial kit? A: Consider transition to commercial assays when:
- Implementing Regulation (EU) 2017/746 for in-vitro diagnostics [89]
- Commercial assays demonstrate comparable performance to in-house methods [89]
- Standardization across multiple laboratories is required
- Resources for extensive validation and quality control are limited
- However, retain in-house assays for emerging targets or unique requirements not addressed by commercial kits
Q: How do I establish cut-off values for quantitative PCR in diagnostic parasitology? A: Determining clinical relevant cut-offs requires:
- Correlation with clinical classification (e.g., definite vs. unlikely infection) [91]
- Analysis of receiver operating characteristics (ROC curves)
- Consideration of patient population (immunocompromised vs. immunocompetent)
- For Pneumocystis jirovecii: Ct value of 34 (in-house PCR) or 2.8×10⁵ copies/mL (commercial PCR) differentiated definite from unlikely PCP [91]
- Validation against gold standard (when available) and clinical outcomes
Workflow Diagrams
Diagram 1: Specimen processing and PCR assay selection workflow
Diagram 2: PCR assay verification and validation workflow
The Scientist's Toolkit
Table 3: Essential research reagent solutions for PCR-based parasitology diagnostics
| Reagent/Kit | Primary Function | Application Notes |
|---|---|---|
| QIAamp DNA Mini Kit (Qiagen) | Nucleic acid extraction | Effective for diverse specimens; used in FFPE, stool, and respiratory sample protocols [88] [89] |
| Para-Pak Stool Collection System (Meridian) | Specimen transport & preservation | Preserves pathogen integrity; available in 1,2,3-vial configurations for different testing needs [61] |
| Hot-Start DNA Polymerases | PCR amplification | Reduces nonspecific amplification; essential for complex specimens [92] |
| FTD Bacterial Gastroenteritis Kit (Siemens) | Multiplex pathogen detection | Detects Campylobacter, Salmonella, Shigella/EIEC, Yersinia; includes internal control [89] |
| artus M. pneumoniae LC PCR Kit (Qiagen) | Species-specific detection | Targets RepMp1 repetitive elements; shows sensitivity comparable to in-house assays [90] |
| EvaGreen DNA Binding Dye | Detection chemistry | Cost-effective for dPCR; binds double-stranded DNA; requires high specificity primers [94] |
| Hydrolysis Probes (TaqMan) | Sequence-specific detection | Fluorophore-quencher system; higher specificity than intercalating dyes [94] |
| Phocid Herpes Virus DNA | Internal control | Monitors PCR inhibition; essential for validating negative results [89] |
DAF Technical Support Center
Troubleshooting Guides
Problem: Low Parasite Recovery Efficiency
- Possible Cause 1: Incorrect coagulant or flocculant type or dosage.
- Solution: Perform jar tests to determine the optimal chemical program for your specific water matrix and target parasites. Common coagulants include ferric chloride or aluminum sulfate [95].
- Possible Cause 2: Inadequate micro-bubble formation.
- Possible Cause 3: Excessive hydraulic flow rate disrupting the flotation zone.
- Solution: Reduce the inflow to the recommended rate for the DAF unit. Laminar flow conditions are essential for effective separation; turbulent flow can break up floc-parasite aggregates [96].
Problem: Specimen Deterioration Post-Processing
- Possible Cause 1: Prolonged processing times before fixation.
- Solution: Minimize the time between sample collection and DAF processing. For unpreserved specimens, transport and process liquid stools within 30 minutes and formed stools within 24 hours (under refrigeration) [35].
- Possible Cause 2: Mechanical damage from overly aggressive mixing or pumping.
- Solution: Ensure flocculation mixing speeds are slow enough to form clusters without shearing delicate parasite stages. Use pumps that minimize shear forces [97].
Problem: Thick or Watery Sludge Consistency
- Possible Cause 1: Skimmer speed is too fast or slow.
- Solution: Adjust the skimmer speed and frequency to match the sludge accumulation rate. A slower skimmer speed typically yields a thicker sludge [97].
- Possible Cause 2: Chemical conditioning is suboptimal.
- Solution: Review polymer dosage and type used for sludge thickening. Conduct bench tests to identify the best polymer for dewatering [98].
Frequently Asked Questions (FAQs)
Q1: How does DAF improve parasite recovery compared to traditional sedimentation? DAF uses millions of microscopic air bubbles to attach to and lift suspended particles, including parasites and their eggs, to the water surface. This process is significantly faster and more efficient than relying on gravity alone in sedimentation, leading to higher recovery rates of low-density specimens that do not settle well [95]. The vertical flow design in modern DAF units allows for much higher hydraulic loading rates (up to 25-40 m/h) while maintaining laminar flow conditions ideal for separation [96].
Q2: What are the critical parameters to monitor for consistent DAF performance in a research setting? Key operational parameters include:
- Hydraulic Loading Rate: The flow rate of water per unit surface area of the DAF tank (e.g., m/h) [96].
- Recycle Ratio: The proportion of clarified effluent that is pressurized, saturated with air, and recycled back to the inlet [98].
- Saturation Pressure: The pressure at which air is dissolved into the recycle stream [95].
- Chemical Dosages: The precise amounts of coagulants and flocculants used [95].
Q3: Can DAF be used to concentrate parasites from all types of water samples? DAF is highly effective for water sources with low turbidity, high color, and those containing many algae, which are characteristics that can make sedimentation less effective [95]. It is particularly suited for recovering parasites that are difficult to settle due to their density or small size. The feasibility for highly viscous or oily samples should be evaluated on a case-by-case basis.
Q4: How does this method contribute to preventing specimen deterioration? The core thesis of this research is to maintain morphological integrity for education and diagnosis. DAF contributes by:
- Rapid Processing: Reducing the time parasites spend in a potentially degrading aqueous environment.
- Gentle Handling: When optimized, the flotation process is less abrasive than repeated centrifugation.
- Immediate Preservation: The concentrated sludge from the DAF skimmed froth can be directly transferred to appropriate fixatives, aligning with parasitology guidelines that require liquid specimens to be examined or fixed within 30 minutes of collection to preserve morphology [35] [41].
Experimental Protocols & Data
Detailed Methodology for DAF-Assisted Parasite Concentration
1. Sample Preparation and Chemical Conditioning
- Collect the water sample in a clean, wide-mouth container [35].
- Using a jar test apparatus, rapidly mix (~100-150 rpm) the sample while adding a predetermined dose of coagulant (e.g., 5-50 mg/L ferric chloride). Mix for 1 minute.
- Reduce the mixing speed to a slow stir (~20-30 rpm) and add a flocculant (e.g., 0.1-0.5 mg/L of a cationic polymer). Continue slow mixing for 15 minutes to allow for the formation of large, stable floc particles that can entrap parasites and eggs [95].
2. DAF Unit Operation
- Transfer the conditioned sample to the DAF unit's inlet tank.
- Set the hydraulic loading rate to a recommended research scale flow of 5-10 m/h [96].
- Ensure the recycle system is operational, typically with a recycle ratio of 10-20% and a saturation pressure of 5-6 bar [98].
- The clarified water will exit from the bottom of the tank, while the floated sludge layer containing the concentrated parasites will accumulate on the surface.
3. Sludge Collection and Specimen Preservation
- Activate the skimmer to remove the floating sludge layer.
- Immediately transfer the collected sludge to a vial containing an appropriate preservative, such as Sodium Acetate-Acetic Acid-Formalin (SAF), to prevent the deterioration of parasite morphology. Mix well and allow to stand at room temperature for at least 30 minutes for adequate fixation [35].
- The preserved concentrate can then be used for downstream microscopic analysis, molecular testing, or permanent slide preparation for educational databases [41].
Quantitative DAF Performance Data
The table below summarizes key performance metrics for DAF systems based on the literature.
Table 1: DAF System Performance and Operational Parameters [96] [97] [98]
| Parameter | First Generation DAF | Second Generation DAF | Third Generation DAF | NIHAO DAF-30 Model |
|---|---|---|---|---|
| Typical Flow Rate | 2 - 5 m/h | 5 - 10 m/h | 25 - 40 m/h (up to >60 m/h reported) | ~ |
| Tank Geometry | Shallow, narrow, long | Almost square, rather deep | Deep, square | 7.0m (L) x 2.1m (W) x 2.1m (H) |
| Flow Conditions | Laminar | Laminar | Turbulent possible | Laminar |
| Reported TSS Reduction | - | - | - | Up to 97% |
| Reported COD Removal | - | - | - | Up to 85% |
Research Reagent Solutions
The table below lists essential materials and their functions for DAF-based parasite concentration experiments.
Table 2: Essential Research Reagents and Materials for DAF Parasite Recovery [35] [95]
| Item | Function / Explanation |
|---|---|
| Coagulants (e.g., Ferric Chloride) | Neutralizes the electrical charges of suspended particles, allowing them to come together and form microflocs. |
| Flocculants (e.g., Polyacrylamide) | Forms bridges between microflocs, creating larger, stronger floc clusters that can more easily entrap parasites and be lifted by bubbles. |
| Sodium Acetate-Acetic Acid-Formalin (SAF) | A preservative for collected sludge; it fixes parasitic forms while maintaining morphological detail for microscopy and is suitable for various stains [35]. |
| Pressurized Air Supply | Source of gas for micro-bubble generation. Must be clean and oil-free to prevent interference with the flotation process. |
| Dissolved Air Flotation Unit | The core apparatus where pressure release, bubble formation, flotation, and separation occur. |
Workflow and Conceptual Diagrams
DAF Parasite Concentration and Preservation Workflow
Relationship Between DAF and Specimen Integrity
Technical Support Center
Troubleshooting Guides
Guide 1: Troubleshooting Low Parasite Recovery in Automated Dissolved Air Flotation (DAF) Systems
- Problem: Low recovery of parasite eggs, larvae, or cysts in the float supernatant, leading to reduced diagnostic sensitivity.
- Possible Causes & Solutions:
- Cause 1: Suboptimal Surfactant Type or Concentration.
- Solution: Validate the surfactant against your target parasites. The cationic surfactant Hexadecyltrimethylammonium bromide (CTAB) has been shown to yield high slide positivity. A concentration of 7% CTAB achieved a maximum slide positivity of 73% in validation studies [99].
- Cause 2: Inadequate Saturation or Depressurization.
- Solution: Ensure the air saturation chamber is pressurized to 5 bar with a saturation time of at least 15 minutes. Verify that the depressurization cannula is correctly inserted and that the saturated fraction (e.g., 10% of the tube volume) is injected effectively to generate microbubbles [99].
- Cause 3: Incorrect Sample Filtration.
- Solution: Use a sequential filtration system with mesh filters of 400 μm and 200 μm diameters to remove large fecal debris while allowing parasites to pass through. Agitate the filter set in vortex equipment for 10 seconds to ensure proper mechanical filtration [99].
- Cause 1: Suboptimal Surfactant Type or Concentration.
Guide 2: Addressing Poor Image Quality and Analysis in AI-Based Diagnostic Systems
- Problem: The automated image analysis system (e.g., DAPI) fails to accurately identify and classify parasitic structures in digital slides.
- Possible Causes & Solutions:
- Cause 1: Poor Smear Preparation on Microscopy Slide.
- Solution: Standardize the smear assembly. After DAF processing, homogenize the recovered sample with ethyl alcohol. Transfer a 20 μL aliquot to a slide and add 40 μL of 15% Lugol’s dye solution and 40 μL of saline to enhance contrast for the AI algorithm [99].
- Cause 2: Inadequate Training of the Convolutional Neural Network (CNN).
- Solution: Train the AI model on a large, diverse dataset of parasite images. Models like DeepMalaria, a Graph CNN, have shown high effectiveness when trained on extensive datasets, with over 85% of identified compounds showing parasite inhibition [100]. Ensure the training dataset includes images from both low-magnification (e.g., eggs, adults) and high-magnification (e.g., malarial parasites) observations [41].
- Cause 3: Suboptimal Preservation Affecting Morphology.
- Solution: Use appropriate preservatives like Formalin or Polyvinyl Alcohol (PVA) in collection kits to maintain morphological integrity from the point of collection. This ensures the parasites in the digital images match the features the AI was trained to recognize [61].
- Cause 1: Poor Smear Preparation on Microscopy Slide.
Guide 3: Mitigating Specimen Deterioration in Educational and Research Collections
- Problem: Physical slide specimens deteriorate over time due to repeated use, compromising their utility for education and AI training.
- Possible Causes & Solutions:
- Cause 1: Repeated Physical Handling of Glass Slides.
- Solution: Implement a Whole-Slide Imaging (WSI) system to create a digital parasite specimen database. Digital slides do not deteriorate and can be accessed simultaneously by multiple users without risk to the original specimen [41].
- Cause 2: Improper Storage Conditions of Physical Specimens.
- Solution: For physical collections, follow standardized storage protocols. For digital collections, store virtual slide data on a secure, shared server with regulated access. This preserves specimen integrity and ensures long-term availability for parasitology education and research [41].
- Cause 1: Repeated Physical Handling of Glass Slides.
Frequently Asked Questions (FAQs)
Q1: What is the diagnostic performance of an integrated system using DAF for sample processing and AI (DAPI) for analysis?
A1: When used together, these systems show high performance. Laboratory validation of a DAF protocol with 7% CTAB surfactant for fecal processing, followed by automated analysis with the DAPI system, demonstrated a sensitivity of 94% and a substantial kappa agreement of 0.80 [99].
Q2: How does AI contribute to drug discovery for parasitic diseases?
A2: AI streamlines and accelerates the drug discovery pipeline. It analyzes genomic, proteomic, and chemical data to identify novel drug targets, predict the efficacy and safety of drug candidates, and repurpose existing drugs. For example, the AI system "Eve" identified the antimicrobial fumagillin as a potential inhibitor of Plasmodium falciparum, which was later confirmed in a mouse model [100]. This can reduce development time from decades to months [100].
Q3: Our laboratory faces a shortage of skilled staff for microscopic analysis. Can AI help?
A3: Yes. AI-driven digital plate reading (DPR) and automated image analysis can significantly improve efficiency. These systems can interpret images immediately after capture, reducing the time to results. For instance, one AI implementation decreased the average time to report urine culture results by nearly 5 hours for negative specimens, mitigating the impact of staff shortages [101].
Q4: What are the best practices for stool specimen transport to ensure sample integrity for automated analysis?
A4: Proper transport is critical. Use collection systems with appropriate preservatives.
- For multiple diagnostic methods (O&P exams, antigen tests), use a two-vial or three-vial system with preservatives like Formalin, PVA, or SAF [61].
- Unpreserved samples should be processed within 2 hours of collection. Preserved samples are typically stable for several days at room temperature or refrigerated [61].
- Always follow the laboratory's specific instructions for storage and transport.
Quantitative Performance Data of Automated Diagnostic Systems
The following table summarizes key quantitative data from recent studies on AI and automated systems in parasitology.
Table 1: Performance Metrics of AI and Automated Systems in Parasitology
| System / Technology | Application / Target | Reported Performance / Outcome | Source |
|---|---|---|---|
| DAF + DAPI System | Diagnosis of intestinal parasites | 94% sensitivity, 0.80 kappa agreement | [99] |
| Convolutional Neural Network (CNN) | Prediction of disease outbreaks (chikungunya, malaria, dengue) | 88% accuracy in predicting outbreaks | [100] |
| DeepMalaria (Graph CNN) | Discovery of antiplasmodial compounds | >85% of identified compounds showed parasite inhibition | [100] |
| Digital Slide Database | Education & morphology training | Supports ~100 simultaneous users via shared server | [41] |
| AI for Gram Stain Analysis | Identification of microorganism morphology | 95% whole-slide classification accuracy | [101] |
Experimental Protocols
Protocol 1: Standardized Laboratory Protocol for Stool Processing via Dissolved Air Flotation (DAF)
This protocol is designed to optimize parasite recovery for subsequent automated diagnosis [99].
- Saturation Chamber Preparation: Fill the DAF device's chamber with 500 ml of treated water and add 2.5 ml of a cationic surfactant (e.g., 10% CTAB). Pressurize the chamber to 5 bar and allow a saturation time of 15 minutes.
- Sample Collection and Filtration: Collect a total of approximately 900 mg of fecal sample divided across three collection tubes on alternate days. Couple the tubes to a filter set with meshes of 400 μm and 200 μm. Agitate the set for 10 seconds in a vortex mixer.
- Flotation Tube Setup: Transfer 9 ml of the filtered sample to a 10 ml or 50 ml test tube. (Note: studies show no significant difference in parasite recovery between these tube volumes [99]).
- Microbubble Injection: Insert the depressurization cannula into the bottom of the tube. Inject a saturated water fraction equal to 10% of the tube's volume (e.g., 1 ml for a 10 ml tube).
- Flotation and Recovery: Allow the microbubbles to act for 3 minutes. After this, use a Pasteur pipette to carefully retrieve 0.5 ml of the floated sample from the supernatant.
- Smear Preparation for Analysis: Transfer the recovered sample to a microcentrifuge tube containing 0.5 ml of ethyl alcohol. Homogenize and place a 20 μL aliquot on a microscope slide. Add 40 μL of 15% Lugol's dye and 40 μL of saline solution before coverslipping for automated analysis.
Protocol 2: Creation of a Digital Parasite Specimen Database for Education and AI Training
This protocol outlines the steps for digitizing physical specimens to prevent deterioration and create a shareable resource [41].
- Specimen Selection: Curate existing slide specimens of parasitic eggs, adults, and arthropods. Ensure specimens are free of personal identifying information and are intended for educational or research use.
- Digital Scanning: Use a research-grade slide scanner (e.g., SLIDEVIEW VS200). For thicker specimens, employ the Z-stack function to accumulate layer-by-layer data and ensure all focal planes are captured.
- Image Quality Control: Review all digitally scanned images for focus and clarity. Rescan any slides with out-of-focus areas as needed.
- Database Construction and Annotation: Upload the final images to a dedicated server. Organize the digital slides into folders based on taxonomic classification. Attach explanatory notes for each specimen in multiple languages (e.g., English and Japanese) to facilitate international use.
- Access Management: Implement a secure login system (ID and password) to control access to the database, ensuring it is used for agreed-upon educational and research purposes.
Workflow Visualization
DAF Sample Processing Workflow
Digital Specimen Database Creation
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Automated Parasitology Diagnostics
| Item | Function / Application | Key Feature / Consideration |
|---|---|---|
| Cationic Surfactants (e.g., CTAB, CPC) | Modifies surface charge in DAF protocols to enhance parasite recovery in the float supernatant. | A 7% CTAB solution yielded 73% slide positivity in validation studies [99]. |
| Stool Transport Kits (Multi-vial) | Preserves specimen integrity during transport for multiple downstream tests (O&P, antigen, molecular). | Kits combining Formalin, PVA, or SAF allow for comprehensive analysis from a single sample [61]. |
| Lugol's Dye Solution (15%) | Stains parasitic structures in smear preparations for contrast enhancement in automated image analysis. | Critical for AI-based systems to accurately identify morphological features [99]. |
| Whole-Slide Imaging (WSI) Scanner | Digitizes physical glass slides for creating permanent, shareable digital specimen databases. | Prevents specimen deterioration and enables wide-access for education and AI training [41]. |
| CON-Trate Reagent | Used in concentration techniques for recovering protozoan cysts and helminth eggs from preserved specimens. | An efficient and cost-effective method for improving detection sensitivity [61]. |
Troubleshooting Guides
Guide 1: Addressing Poor Parasite Morphology in Stored Specimens
Problem: Parasite eggs or larvae appear degraded, making morphological identification difficult or impossible.
Question: Why are my preserved parasites degraded, and how can I improve specimen quality?
Investigation and Solution:
- Confirm Preservation Medium: Identify whether the specimen was stored in ethanol or formalin. A recent comparative study on capuchin monkey fecal samples found that while formalin is superior for preserving larval nematodes like Filariopsis barretoi, both 96% ethanol and 10% formalin are equally effective for preserving strongyle-type eggs [68].
- Check Storage Duration and Conditions: Specimens stored for extended periods (over 1 year) at ambient temperature may show degradation. Formalin is generally more resistant to long-term degradation for a wider range of morphotypes [68].
- Assess for Typical Degradation Signs:
- In Ethanol-Preserved Larvae: Look for cuticle shrinking, puckering, thinning, increased opacity, and deformation of internal structures [68].
- In Formalin-Preserved Larvae: Look for the presence of 'bubbles' within the body cavity that can obscure internal structures [68].
- In Eggs: Look for dents, breaks, or increased opacity of the shell, which may impact the developing parasite within [68].
- Corrective Action: For future collections, select the preservative based on the target parasite. For general purposes and to enable a wider range of downstream analyses, formalin is recommended. If molecular analysis is a future possibility, 96% ethanol is a suitable alternative, though larval morphology may not be optimal [68].
Guide 2: Choosing a Preservative for Combined Morphological and Molecular Work
Problem: A preservative is needed that allows for both morphological identification and genetic analysis from a single sample.
Question: Is there a universal preservative that supports both microscopy and PCR?
Investigation and Solution:
- Understand Preservative Limitations:
- Formalin (especially in LV-PVA): Excellent for morphology but causes DNA fragmentation, making it unsuitable for many molecular tests like Cyclospora or Cryptosporidium genotyping [102].
- Ethanol (70-96%): Effective for DNA preservation and is less toxic, but may dehydrate tissues, leading to brittle specimens and morphologically altered parasites [68].
- Review Your Test Requirements: For CDC surveillance programs like CryptoNet, specimens fixed in Zn-PVA, Cu-PVA, or other non-formalin fixatives are required. Formalin-containing fixatives like LV-PVA are explicitly not acceptable as they interfere with testing [102].
- Corrective Action: No single preservative is perfect for all techniques. The optimal strategy is to split the specimen.
Guide 3: Managing Specimen Submission and Shipping Errors
Problem: Specimens are rejected by a reference laboratory upon arrival.
Question: What are the common reasons for specimen rejection, and how do I ship them correctly?
Investigation and Solution:
- Pre-Submission Checklist:
- Labeling: Ensure primary containers have at least two unique patient identifiers [102].
- Form Completion: Submit a fully completed requisition form, specifying the test requested. Using block letters instead of cursive improves legibility [102].
- Container Integrity: Secure lids to prevent leakage [102].
- Fixative Volume: Maintain a ratio of 3:1 to 5:1 of preservative to fecal material [20].
- Expiration Dates: Do not use expired collection vials [102].
- Shipping Compliance:
- Preserved fecal specimens are classified as Category B Biological Substances (UN3373) [102].
- Ship in compliant packaging with appropriate markings and labels.
- For fixed samples, room temperature shipping is generally acceptable. For unfixed or raw stool, ship overnight with cold packs (2-8°C). Do not use dry ice unless specified [102].
Frequently Asked Questions (FAQs)
FAQ 1: What is the best all-around preservative for routine parasitology diagnosis in a clinical setting?
For general-purpose use in a clinical lab, 10% formalin is a strong candidate. It is an all-purpose fixative appropriate for helminth eggs, larvae, and protozoan cysts, and it is specifically required for concentration techniques [20]. It provides good long-term preservation and is commercially available. However, if your laboratory also performs permanent stained smears from the same specimen, SAF (Sodium Acetate-Acetic Acid-Formalin) or PVA (Polyvinyl Alcohol) are recommended, as formalin alone is not suitable for stained smears [20].
FAQ 2: How does ethanol compare to formalin for preserving different parasite stages?
Evidence from a controlled study shows the performance varies by parasite stage [68]:
- Larvae: Formalin provides significantly better morphological preservation.
- Eggs (e.g., strongyle-type): Both 96% ethanol and 10% formalin provide equivalent preservation.
- Morphotype Diversity: More parasitic morphotypes are typically identified in formalin-preserved samples compared to ethanol-preserved ones.
FAQ 3: We are building a digital parasite database for education. What are the key advantages of this approach?
Creating a digital database using whole-slide imaging (WSI) technology offers several evidence-based benefits [41]:
- Prevention of Deterioration: Virtual slides do not deteriorate over time, unlike physical glass slides that degrade with repeated use.
- Wide Accessibility: Data can be accessed simultaneously by approximately 100 users via a web browser on various devices, facilitating remote learning and collaboration.
- Preservation of Scarce Specimens: It secures morphological data of parasites that are becoming increasingly rare in developed countries due to improved sanitation.
- Standardization: It helps maintain diagnostic expertise in parasite morphology, which is declining despite remaining the gold standard for many infections.
FAQ 4: Are there safety and environmental concerns related to common parasitology preservatives?
Yes, safety and environmental impact are critical considerations.
- Safety: Formalin is toxic and requires careful handling to prevent inhalation and skin contact. Ethanol is less toxic and easier to source [68].
- Environmental: The environmental risk of pharmaceuticals, including antiparasitic drugs, is a growing concern. Regulatory bodies like the European Medicines Agency (EMA) require Environmental Risk Assessments (ERAs) for new veterinary products to evaluate their impact on non-target organisms in soil and water [103]. The "One Health" concept emphasizes the need to consider these ecological risks early in the drug development process [103].
Experimental Protocols for Evidence-Based Preservation
Detailed Methodology: Comparative Preservation Study
The following protocol is adapted from a published study comparing ethanol and formalin for preserving gastrointestinal parasites from non-invasively collected fecal samples [68].
Objective: To evaluate the preservation quality of gastrointestinal parasites in fecal samples stored in 96% ethanol versus 10% formalin over an extended period.
Materials:
- Fresh fecal samples
- Sterile 15 ml tubes
- 96% Ethanol
- 10% Buffered Formalin
- Applicator sticks or "Spork" inserts
- Gloves
- Laboratory equipment for coproscopy: microscope, centrifuge, cheesecloth, distilled water, 6-well microscopy plate
Procedure:
- Sample Collection and Partitioning: Immediately after collection, partition each fresh fecal mass into two halves.
- Preservation: Place approximately 2g of one half into a tube containing 6 ml of 96% ethanol. Place the other 2g half into a tube containing 10 ml of 10% buffered formalin.
- Mixing: Gently agitate the tubes to ensure the solvent fully permeates the sample.
- Storage: Store all samples at ambient temperature for the desired study duration (e.g., 8-19 months).
- Processing: Process samples using a standardized sedimentation technique (e.g., modified Wisconsin sedimentation technique): a. Separate solids from the liquid preservative and record the fecal weight. b. Homogenize the sample with distilled water and strain through a double-layered cheesecloth. c. Centrifuge the solution (10 min at 1500 rpm), discard the supernatant, and homogenize the pellet with 5-10 ml of distilled water. d. Transfer the pellet to a 6-well microscopy plate for screening.
- Microscopy and Scoring: a. Screen all samples microscopically. b. Identify parasites morphologically and rate their preservation using a standardized 3-point grading scale for both ethanol and formalin separately.
- Data Analysis: a. Calculate morphotype diversity and parasites per fecal gram (PFG) for each sample. b. Compare the average preservation rating, morphotype diversity, and PFG between the two preservation mediums using statistical tests (e.g., Wilcoxon-Signed Rank tests for non-normal data).
Data Presentation
Table 1: Comparison of Common Parasitology Preservatives
| Preservative | Primary Use | Advantages | Disadvantages | Suitability for Molecular Testing |
|---|---|---|---|---|
| 10% Formalin | All-purpose fixative for helminth eggs/larvae and protozoan cysts [20]. | Good long-term preservation; suitable for concentration techniques [20]. | Not suitable for permanent stained smears; toxic; causes DNA fragmentation [102] [20]. | Poor - Interferes with PCR and genotyping [102]. |
| PVA (Polyvinyl Alcohol) | Permanent stained smears; combined use with other fixatives [20]. | Allows concentration and stained smears; good for protozoan stages; long shelf life [20]. | Contains mercury (disposal issues); some helminth eggs not concentrated well; morphology may be distorted [20]. | Variable - Depends on base fixative. Traditional mercury-based is poor. |
| SAF (Sodium Acetate Formalin) | Concentration techniques and stained smears [20]. | Mercury-free; long shelf life [20]. | Poor adhesive property (requires albumin-coated slides); protozoan morphology with trichrome not as clear as PVA [20]. | Better - Non-formalin versions are suitable. |
| 96% Ethanol | Molecular studies; alternative for morphology [68]. | Less toxic; good for DNA preservation; successfully used in coprological studies [68]. | Dehydrates tissues; can degrade larvae morphology; not ideal for all morphological IDs [68]. | Excellent - Preferred for DNA analysis [68]. |
| Non-Formalin Fixatives (e.g., Zn-PVA, Cu-PVA, Ecofix) | CDC surveillance and genotyping for parasites like Cryptosporidium and Cyclospora [102]. | Required for specific molecular assays; no formalin interference. | May not be ideal for all morphological techniques. | Excellent - Specifically designed for molecular testing [102]. |
| Grade | Description for Larvae | Description for Eggs |
|---|---|---|
| 3 (Well-Preserved) | Fully intact cuticle; visible internal structures; identifiable, morphologically unaltered external features. | Clear, appropriate shape/size; visible embryos/larvae; continuous, unbroken shell. |
| 2 (Moderately Preserved) | Degradation of cuticle (shrinking, puckering) OR internal structures, partially interfering with identification. | Minor shell deformations (dents, breaks, increased opacity); may impact the developing parasite. |
| 1 (Poorly Preserved) | Heavy degradation; difficult or impossible to identify due to significant changes in cuticle and internal/external structures. | Significant shell breakage or deformation; internal structures not visible (not observed in the cited study but included for completeness) [68]. |
Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function | Key Considerations |
|---|---|---|
| 10% Buffered Formalin | All-purpose fixative ideal for preserving helminth eggs and larvae for microscopic examination and concentration procedures [102] [20]. | Neutral buffering helps maintain organism morphology during long-term storage [20]. |
| Polyvinyl Alcohol (PVA) | A preservative used for preparing permanent stained smears; allows for detailed morphological study of protozoa [20]. | Often contains Schaudinn's fluid (mercuric chloride), which poses disposal challenges [20]. |
| 96% Ethanol | A preservative suitable for DNA analysis and morphological identification of some parasite stages, particularly eggs [68]. | Causes tissue dehydration, which can lead to suboptimal preservation of larvae and other delicate structures [68]. |
| Zn-PVA / Cu-PVA / Ecofix | Non-formalin fixatives designed for molecular parasitology tests, such as CDC surveillance programs for Cryptosporidium and Cyclospora [102]. | Essential when PCR-based genotyping is required, as formalin inhibits these tests [102]. |
| Schaudinn's Fixative | Used for immediate fixation of fresh stool specimens onto slides for permanent staining [20]. | Not recommended for concentration techniques; contains mercury compounds [20]. |
| SAF (Sodium Acetate Formalin) | A mercury-free fixative that can be used for both concentration techniques and preparation of permanent stained smears [20]. | Requires the use of albumin-coated slides for better adhesion of the specimen to the glass slide [20]. |
Conclusion
Effective prevention of specimen deterioration is a cornerstone of reliable parasitology research and diagnostics. The evidence confirms that no single preservation method universally excels; rather, the choice must align with specific analytical goals—formalin for superior morphological preservation and ethanol for molecular applications. The integration of optimized pre-analytical protocols with emerging technologies like AI and advanced flotation techniques presents a transformative opportunity to enhance diagnostic sensitivity. Future directions should focus on standardizing preservation protocols across laboratories, developing integrated multi-omics approaches that work with well-preserved specimens, and creating novel fixatives that simultaneously optimize morphological and molecular analysis. For the biomedical research community, mastering these preservation fundamentals is essential for advancing drug development, improving diagnostic accuracy, and ensuring the reproducibility of parasitological studies in both clinical and research settings.
References
- 1. State-of-the-Art Techniques for Diagnosis of Medical Parasites and Arthropods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8470585/]
- 2. Wildlife parasitology : sample collection and processing, diagnostic... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-024-06226-4]
- 3. Current Advances in the Development of Diagnostic Tests Based on... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7693570/]
- 4. Development of forced degradation and stability indicating studies of drugs—A review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5761119/]
- 5. Hookworm Disease: Background, Pathophysiology, Etiology [https://emedicine.medscape.com/article/218805-overview]
- 6. Human Hookworm Infection in the 21st Century - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2268732/]
- 7. : Stages, Diagram & Key Facts Explained Hookworm Life Cycle [https://www.vedantu.com/biology/hookworm-life-cycle]
- 8. Infection - Infectious Diseases - Merck Manual... Hookworm [https://www.merckmanuals.com/professional/infectious-diseases/nematodes-roundworms/hookworm-infection]
- 9. Current treatment options for Dientamoeba fragilis infections - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3862407/]
- 10. sciencedirect.com/topics/immunology-and-microbiology/ dientamoeba ... [https://www.sciencedirect.com/topics/immunology-and-microbiology/dientamoeba-fragilis]
- 11. Infection: Practice Essentials, Pathophysiology... Dientamoeba Fragilis [https://emedicine.medscape.com/article/997239-overview]
- 12. Folia Parasitologica: Preservation of macroparasite species via classic... [https://folia.paru.cas.cz/artkey/fol-201801-0019_preservation_of_macroparasite_species_via_classic_plastination_an_evaluation.php]
- 13. Hookworm - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK546648/]
- 14. The Transcriptome Sequence of Dientamoeba Offers New... fragilis [https://pubmed.ncbi.nlm.nih.gov/26188431/]
- 15. : Formalin , Uses & Preparation Explained Simply Structure [https://www.vedantu.com/chemistry/formalin]
- 16. of immunorecognition by transferring Preservation from 10... cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC3737737/]
- 17. Guide to Fixation and Permeabilization - FluoroFinder [https://fluorofinder.com/guide-to-fixation-and-permeabilization/]
- 18. (PDF) Comparison of Ethanol Versus Formalin Fixation on... [https://www.academia.edu/27562457/Comparison_of_Ethanol_Versus_Formalin_Fixation_on_Preservation_of_Histology_and_RNA_in_Laser_Capture_Microdissected_Brain_Tissues]
- 19. Seeking An Eternal Solution [https://cen.acs.org/articles/86/i44/Seeking-Eternal-Solution.html]
- 20. My Scientific Blog - Research and Articles: Preservation of specimens for Parasitology [https://upendrats.blogspot.com/2013/09/preservation-of-specimens-for.html]
- 21. Food quality and safety risk diagnosis in the food cold chain through failure mode and effect analysis - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0956713520304175]
- 22. Identification and Preservation of Intestinal Parasites Using Methylene... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4003778/]
- 23. Temperature Matters: The Role of Biobank... - Biobanking.com [https://www.biobanking.com/temperature-matters-the-role-of-biobank-management-systems-in-maintaining-sample-integrity-in-the-cold-chain/]
- 24. Cold Chain Logistics: Challenges, Solutions & Best Practices 2025 [https://www.hopstack.io/blog/cold-chain-logistics-challenges-solutions-best-practices]
- 25. Pharmaceutical Temperature Monitoring: GxP Compliance & Product Quality [https://www.processsensing.com/en-us/industries/pharmaceutical-temperature-monitoring.htm]
- 26. Essential Protocols for Proper Storage and Handling of Biological... [https://editverse.com/essential-protocols-for-proper-storage-and-handling-of-biological-specimens/]
- 27. Innovation: Ensuring Cold in Biologics and... Chain Integrity [https://www.biotouchglobal.com/resources/blog/cold-chain-innovation-ensuring-integrity-in-biologics-and-decentralized-trials/]
- 28. Pharmaceutical temperature mapping guidelines [https://eupry.com/temperature-mapping/guidelines-pharmaceutical/]
- 29. in Pharmaceutical and Biotech Logistics... Cold Chain Integrity [https://www.eawlogistics.com/cold-chain-integrity-in-pharmaceutical-and-biotech-logistics/]
- 30. Short Communications: Assessing morphological preservation of... [https://www.researchsquare.com/article/rs-3424524/v1]
- 31. Assessing morphological preservation of gastrointestinal parasites... [https://www.nature.com/articles/s41598-024-53915-2?error=cookies_not_supported&code=64742b0a-ee6e-4ad1-9625-2eed181787e0]
- 32. of Comparison Versus Ethanol Fixation on Formalin of... Preservation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8096012/]
- 33. Evaluating Ethanol -based Sample Preservation to... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0051273]
- 34. Tissue Preservation | StainsFile [https://www.stainsfile.com/theory/tissue-preparation/preservation/]
- 35. Parasitology Specimen Collection Guidelines » Laboratory Alliance of Central New York, LLC [https://www.laboratoryalliance.com/healthcare-providers/laboratory-services/specimen-collection-documents/parasitology-specimen-collection-guidelines/]
- 36. Submitting Parasitology Specimens to the Lab | Texas DSHS [https://www.dshs.texas.gov/submitting-parasitology-specimens-lab]
- 37. My Scientific Blog - Research and Articles: Preservation of specimens for Parasitology [https://upendrats.blogspot.com/2013/09/preservation-of-specimens-for.html?m=1]
- 38. Best Practice No 174: Best practice guidelines for the examination of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1770126/]
- 39. Formalin-fixed stool improves the performance of the Kato–Katz method - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10884569/]
- 40. DNA Specimen Preservation Using DESS and DNA Extraction in Museum Collections - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189647/]
- 41. Construction of a preliminary digital parasite specimen database for parasitology education and research | Scientific Reports [https://www.nature.com/articles/s41598-025-07673-4]
- 42. A historical review of the techniques of recovery of parasites for their detection in human stools - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7269538/]
- 43. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimencoll.html]
- 44. The Comparison of the Efficacy of Various Fixatives on Diverse... [https://scialert.net/fulltext/?doi=pjbs.2009.1212.1216]
- 45. Enhancing diagnostic accuracy: Direct immunofluorescence assay as... [https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-024-04297-0]
- 46. Comparison between merthiolate - iodine - formalin and Kato-Katz... [https://pubmed.ncbi.nlm.nih.gov/27790963/]
- 47. Integrated parasite management with special reference to gastro-intestinal nematodes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5339188/]
- 48. The effect of silica under different storage conditions on... desiccation [https://pubmed.ncbi.nlm.nih.gov/33743816/]
- 49. A comparative analysis of preservation techniques for the optimal molecular detection of hookworm DNA in a human fecal specimen | PLOS Neglected Tropical Diseases [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0006130]
- 50. Drying rechargeable desiccant beads - User Mods - Bambu Lab Community Forum [https://forum.bambulab.com/t/drying-rechargeable-desiccant-beads/120521]
- 51. Comparison of four DNA extraction and three preservation protocols for the molecular detection and quantification of soil-transmitted helminths in stool | PLOS Neglected Tropical Diseases [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0007778]
- 52. Isopropanol DNA Precipitation Protocol for Pure Yield | QIAGEN [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/dna/handling-dna/isopropanol-precipitation-of-dna]
- 53. as a suitable alternative to cold-storage of phyllosphere... Desiccation [https://pubmed.ncbi.nlm.nih.gov/39905028/]
- 54. and P650 Compliance | Intelsius UK UN 3373 [https://intelsius.com/un3373-compliance/]
- 55. Regulations [https://www.un3373.com/enveloppeninfo/regulations]
- 56. Shipping and Transportation of Biologicals - Environmental Health and Safety Office [https://www.unthsc.edu/safety/biosafety/shipping-transportation-biologicals/]
- 57. Guidance for Shipping Biological Materials at Cornell University | Environment, Health and Safety [https://ehs.cornell.edu/shipping-and-transportation/hazardous-materials-shipping/biological-materials/guidance-shipping]
- 58. Shipping Biological Materials | Environmental Health & Safety [https://www.ehs.ucsb.edu/programs-services/biological-safety/shipping-biological-materials]
- 59. Packaging and transport for patient samples – requirements UN 3373 [https://www.gov.uk/government/publications/packaging-and-transport-requirements-for-patient-samples-un3373/packaging-and-transport-requirements-for-patient-samples-un3373]
- 60. Biological Materials Shipping & Transport - FAA USA Safety and... [https://uwm.edu/safety-health/biosafety/shipping-transport/]
- 61. Para-Pak Stool Transport Systems | Meridian Bioscience [https://www.meridianbioscience.com/para-pak/]
- 62. common lab error , and effect of anticoagulant [https://labpedia.net/common-lab-errors-and-effect-of-various-anticoagulants-on-tests/]
- 63. in Veterinary Practice - Clinical Pathology and... Parasitology [https://www.msdvetmanual.com/clinical-pathology-and-procedures/parasitology/parasitology-in-veterinary-practice]
- 64. Evaluation of commercially available preservatives for laboratory... [https://pubmed.ncbi.nlm.nih.gov/10790128/]
- 65. Collection And Transportation | Thermo Fisher Scientific Parasitology [https://www.thermofisher.com/search/browse/featured/ru/ru/80013069]
- 66. Optimized protocol for DNA/RNA co-extraction from adults of Dirofilaria immitis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6861604/]
- 67. Where Have All the Diagnostic Morphological Parasitologists Gone? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9667774/]
- 68. Assessing morphological preservation of gastrointestinal parasites from fecal samples of wild capuchin monkeys (Cebus imitator) stored in ethanol versus formalin | Scientific Reports [https://www.nature.com/articles/s41598-024-53915-2]
- 69. in fish: Practical solutions and guidelines to improve... DNA degradation [https://pubmed.ncbi.nlm.nih.gov/32884647/]
- 70. An overview of DNA and its implications in forensic... degradation [https://ejfs.springeropen.com/articles/10.1186/s41935-024-00389-y]
- 71. The effect of DNA bias in passive sampling... | PLOS One degradation [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0189188]
- 72. Overcoming DNA in Forensic Science Degradation [https://www.news-medical.net/life-sciences/Overcoming-DNA-Degradation-in-Forensic-Science.aspx]
- 73. Noncryogenic preservation of mammalian tissues for DNA extraction... [https://pubmed.ncbi.nlm.nih.gov/11989787/]
- 74. - Microbiology - Oxford University Hospitals High risk samples [https://www.ouh.nhs.uk/microbiology/diagnostic-tests/high-risk-samples/]
- 75. Collection and Transport Guidelines for Suspect... | CDC Specimen [https://www.cdc.gov/smallpox/hcp/laboratories/specimen-collection-suspect-smallpox-cases.html]
- 76. Frontiers | Transparent DNA/RNA Co-extraction Workflow Protocol Suitable for Inhibitor-Rich Environmental Samples That Focuses on Complete DNA Removal for Transcriptomic Analyses [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2016.01588/full]
- 77. Inhibitor-Tolerant qPCR & RT-qPCR Mixes [https://collateral.meridianlifescience.com/view/33799571]
- 78. Best Practice No 174: Best practice guidelines for the examination of specimens for the diagnosis of parasitic infections in routine diagnostic laboratories [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770126/]
- 79. 1910.1030 - Bloodborne pathogens. | Occupational Safety and Health Administration [https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.1030]
- 80. Specimen acceptance/ rejection | Health Services criteria Laboratories [https://www.hslpathology.com/services/hsl-rapid-response-laboratories/specimens/specimen-acceptancerejection-criteria/]
- 81. Basic Identification Parasitology | PPTX | Infectious Diseases methods [https://www.slideshare.net/slideshow/parasitology-basic-identification-methods/86341845]
- 82. Laboratory Diagnosis and Test Protocols - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7158162/]
- 83. of Sensitivity Compared to Microscopy Diagnosis of... Molecular [https://pmc.ncbi.nlm.nih.gov/articles/PMC3497842/]
- 84. Comparison of Microscopy and PCR for Detection of Intestinal Parasites in Danish Patients Supports an Incentive for Molecular Screening Platforms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3264173/]
- 85. Comparative analysis of commercial and “In-House” molecular tests... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 86. Molecular Diagnostics in the Diagnosis of Parasitic Infection - ... [https://www.sciencedirect.com/science/article/abs/pii/S0580951715000070]
- 87. Medical Parasitology - Clinical Tree [https://clinicalpub.com/medical-parasitology/]
- 88. Performances of two different panfungal PCRs to detect mould DNA in... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-014-0692-z]
- 89. of two Comparison and one commercial - in real-time house ... PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC7753976/]
- 90. Comparison of Commercial and In-House Real-Time PCR Assays Used for Detection of Mycoplasma pneumoniae - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2643664/]
- 91. Comparison of 2 real-time PCR assays for diagnosis of Pneumocystis jirovecii pneumonia in human immunodeficiency virus (HIV) and non-HIV immunocompromised patients - PubMed [https://pubmed.ncbi.nlm.nih.gov/25801778/]
- 92. PCR Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-troubleshooting.html]
- 93. Troubleshooting your PCR [https://www.takarabio.com/learning-centers/pcr/faq/troubleshooting]
- 94. dPCR assay development | Digital PCR troubleshooting - Qiagen [https://www.qiagen.com/us/applications/digital-pcr/beginners/dpcr-guide/setup-and-troubleshooting]
- 95. - Wikipedia Dissolved air flotation [https://en.wikipedia.org/wiki/Dissolved_air_flotation]
- 96. Development of dissolved technology from the first... air flotation [https://pubmed.ncbi.nlm.nih.gov/11394261/]
- 97. - Dissolved ( Air ) Equipment For Wastewater Treatment Flotation DAF [https://www.nihaowater.com/product/daf-machine/]
- 98. ( Dissolved ) Systems | Ecologix Environmental... Air Flotation DAF [https://ecologixsystems.com/dissolved-air-flotation-system]
- 99. Laboratory validation of the automated of intestinal... diagnosis [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-024-06434-y]
- 100. Artificial intelligence in parasitic disease control: A paradigm shift in health care - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10911181/]
- 101. Experts Weigh in On the Evolving Age of Artificial Intelligence in... [https://www.copanusa.com/blogs/experts-weigh-in-on-the-evolving-age-of-artificial-intelligence-in-medical-diagnostics/]
- 102. Submitting Parasitology Specimens to the Lab | Texas DSHS [https://www.dshs.texas.gov/laboratory-services/programs-laboratories/microbiology-unit/medical-parasitology/submitting-parasitology-specimens-lab]
- 103. Assessing Environmental Risks during the Drug Development Process for Parasitic Vector-Borne Diseases: A Critical Reflection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11019539/]