Overcoming False Negatives in Dientamoeba fragilis PCR: A Research-Focused Guide to Enhanced Detection and Assay Validation
Molecular diagnostics, particularly PCR, have revolutionized the detection of Dientamoeba fragilis but are susceptible to false-negative results that can impede research and drug development.
Overcoming False Negatives in Dientamoeba fragilis PCR: A Research-Focused Guide to Enhanced Detection and Assay Validation
Abstract
Molecular diagnostics, particularly PCR, have revolutionized the detection of Dientamoeba fragilis but are susceptible to false-negative results that can impede research and drug development. This article provides a comprehensive analysis for scientists on the multifactorial causes of false negatives, from suboptimal DNA extraction due to the parasite's robust wall to assay selection and inhibitor management. We explore advanced methodological approaches, including melt curve analysis to differentiate true positives from cross-reactions and the validation of complementary techniques like culture. A comparative evaluation of commercial versus in-house PCR assays offers evidence-based guidance for protocol optimization, equipping researchers with the strategies needed to achieve maximal diagnostic sensitivity and ensure the reliability of their epidemiological and clinical studies.
Understanding the Roots of False Negatives in D. fragilis Molecular Detection
The accurate detection of Dientamoeba fragilis is fundamental to understanding its true epidemiology and clinical significance. For decades, diagnostic limitations have clouded our understanding of this intestinal protozoan, with false negatives creating a substantial barrier to determining its true prevalence and pathogenicity. The shift from traditional microscopic examination to molecular methods has revealed startling disparities in detection capabilities, fundamentally altering our perception of this parasite's distribution. This technical support document examines the sources and implications of false negative results in D. fragilis research and provides evidence-based solutions to enhance diagnostic accuracy for researchers and clinical laboratories.
Understanding the Diagnostic Landscape
The Sensitivity Gap Between Methodologies
Traditional microscopic examination has been the historical standard for D. fragilis detection but suffers from significant limitations that contribute to high rates of false negatives. Table 1 compares the performance characteristics of different diagnostic methods.
Table 1: Comparison of D. fragilis Detection Methods
| Method Type | Reported Sensitivity | Specificity | Key Limitations |
|---|---|---|---|
| Microscopy (trichrome stain) | 34.3% | 99% | Requires expert microscopist, fragile trophozoites degrade quickly [1] |
| Microscopy (Giemsa stain) | 52% | 100% | - [2] |
| Conventional PCR | 42.9%-76% | 100% | Variable performance between assays [1] [2] |
| Real-time PCR | 90%-100% | 100% | Platform-dependent variability [3] [1] [2] |
| Culture (MBD medium) | 40% | 100% | Time-consuming, not routine [1] |
Consequences of Underdetection
The systematic underdetection of D. fragilis has profound implications for epidemiological data and clinical understanding:
Prevalence Underestimation: Studies implementing PCR have detected prevalence rates between 0-62%, substantially higher than microscopy-based studies [4] [5]. One hospital study found 6.5% of tested patients were positive by PCR, with notable over-representation of younger patients [4].
Pathogenicity Debates: The high frequency of false negatives complicates assessment of clinical significance. Recent case-control studies found no significant difference in symptoms between infected and uninfected individuals, suggesting possible commensal status [4] [6].
Transmission Misunderstanding: Inaccurate prevalence data hinders understanding of transmission dynamics, including potential zoonotic pathways [7] [5].
Troubleshooting Guide: Addressing False Negatives
Pre-Analytical Variables
Issue: Sample Degradation During Transport and Storage
D. fragilis trophozoites are notoriously fragile and degrade rapidly after passage [8]. This degradation directly impacts DNA quality and quantity for PCR detection.
Solutions:
- Process fresh, unpreserved stool samples within 24 hours of collection [9] [2]
- If immediate processing is impossible, use appropriate preservatives (SAF fixative) to maintain DNA integrity [7]
- Establish standardized sample handling protocols across all collection sites
- Implement single-sample PCR approaches that demonstrate high sensitivity compared to traditional triple-sample microscopy [6] [2]
Issue: Inadequate Sample Representation
Protozoan distribution within stool can be heterogeneous, leading to sampling error.
Solutions:
- Thoroughly homogenize stool samples before DNA extraction [4]
- Use sufficient sample size (250-500 mg) to ensure representative sampling [4]
- Implement bead-beating homogenization (e.g., 7000 rpm for 70s) to improve DNA yield [4]
Analytical Limitations
Issue: Suboptimal DNA Extraction Efficiency
Incomplete cell lysis or DNA degradation during extraction reduces template availability.
Solutions:
- Use commercial stool DNA extraction kits with inhibitor removal technology [4] [7]
- Incorporate internal extraction controls to identify extraction failures [7]
- Include proteinase K digestion steps (10 min at 70°C) to improve lysis efficiency [4]
- Validate extraction efficiency using spike-in controls
Issue: PCR Inhibition
Stool samples contain numerous PCR inhibitors (bile salts, complex carbohydrates) that cause false negatives.
Solutions:
- Include internal positive controls in each reaction to detect inhibition [7]
- Implement 1:5 sample dilution and retesting for inhibited samples [7]
- Use inhibitor removal buffers during DNA extraction [4]
- Validate assay performance with extraction controls [7]
Issue: Assay Sensitivity Variability
Different PCR assays demonstrate substantial variation in detection capabilities, with some laboratory-developed tests showing up to three-fold lower sensitivity compared to commercial assays [8].
Solutions:
- Validate assay limit of detection using standardized controls
- Choose assays with high demonstrated sensitivity (0.90-0.97) and specificity (1.0) [3]
- Perform regular proficiency testing with blinded samples
- Consider melt curve analysis to confirm positive results [7]
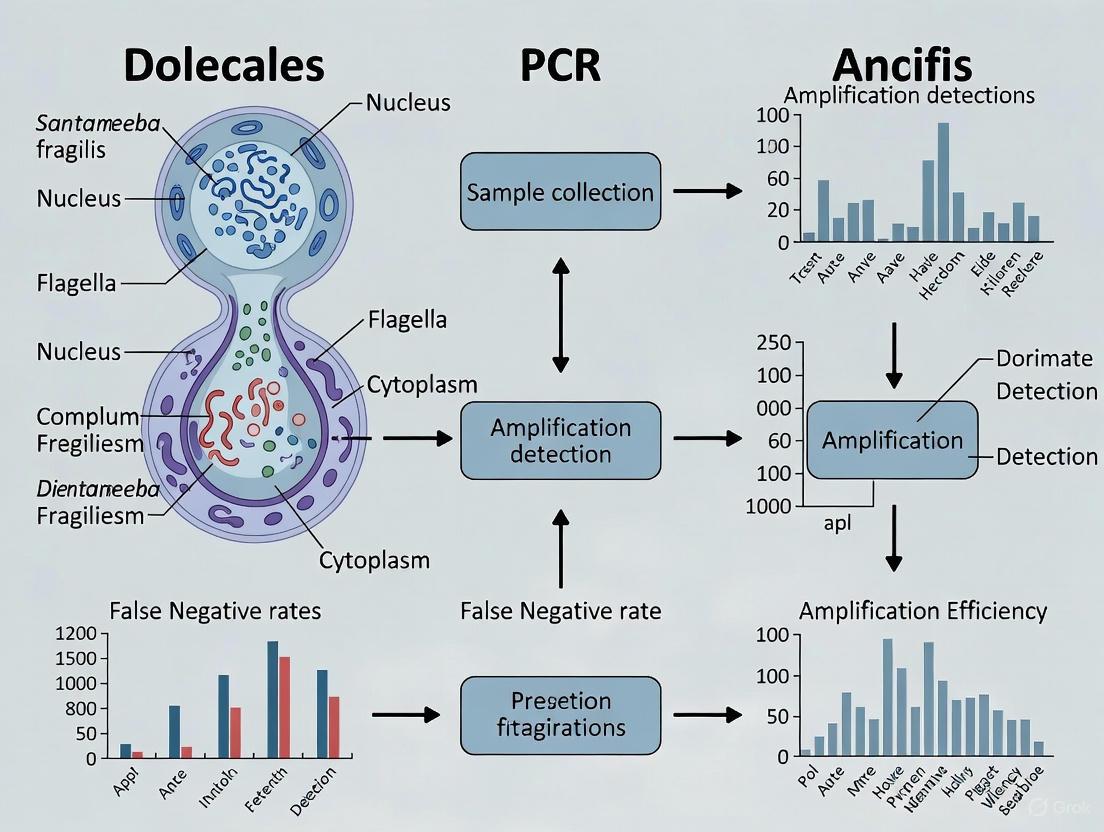
Diagram 1: PCR Workflow with Critical Control Points. Green ellipses represent mitigation strategies at each stage to reduce false negative risk.
Frequently Asked Questions
Q: What is the single most impactful improvement to reduce false negatives in D. fragilis detection?
A: Implementing real-time PCR methodology provides the most significant sensitivity improvement, with studies showing 100% sensitivity compared to 34.3-52% for microscopy [1] [2]. The combination of proper sample handling with optimized PCR reduces false negatives substantially.
Q: How does sample preservation affect detection sensitivity?
A: Sample preservation is critical. Fresh, unpreserved samples processed within 24 hours provide optimal DNA quality [9] [2]. When immediate processing is impossible, SAF fixative effectively preserves morphology and DNA integrity [7]. Improper preservation leads to trophozoite disintegration and DNA degradation.
Q: What controls should be included in every PCR run to ensure result reliability?
A: Implement a comprehensive control strategy:
- Internal extraction control to monitor extraction efficiency and inhibition [7]
- Positive amplification control to confirm PCR reagent functionality
- Negative control to detect contamination
- Quantitative standards for sensitivity monitoring
Q: Can high parasite load compensate for suboptimal detection methods?
A: While higher parasite loads increase detection probability, microscopy still misses a significant proportion of infections even at moderate loads. One study found real-time PCR detected 35 positive samples compared to only 12 by microscopy in the same population [1]. Method sensitivity is independent of parasite load.
Q: How can we validate a new PCR assay's performance for D. fragilis detection?
A: Use a panel of well-characterized positive samples (n=49-132) and negative controls (n=12-105) to determine diagnostic sensitivity (0.90-0.97) and specificity (1) [3]. Compare against a reference method and include cross-reactivity testing against phylogenetically related organisms [3] [7].
Research Reagent Solutions
Table 2: Essential Reagents for D. fragilis Detection
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| DNA Extraction Kits | High Pure PCR Template Preparation Kit (Roche), QIAamp Fast DNA Stool Mini Kit (Qiagen) | Efficient DNA isolation with inhibitor removal [4] [7] |
| PCR Master Mixes | Amplidiag Stool Parasites Real-Time PCR Kit (Hologic), EasyScreen Enteric Protozoan Detection Kit (Genetic Signatures) | Optimized for stool samples with internal controls [4] [7] [10] |
| Inhibition Control | qPCR Extraction Control Kit (Meridian Bioscience) | Identifies PCR inhibition leading to false negatives [7] |
| Sample Preservation | SAF fixative, phosphate-buffered saline | Maintains DNA integrity during transport [4] [7] |
| Homogenization | MagNA Lyser (Roche) with beads | Ensures representative sampling and efficient lysis [4] |
Advanced Verification Techniques
Discrepant Analysis and Resolution
When unexpected negative results occur, particularly in high-prevalence populations, implement a verification protocol:
Step 1: Inhibition Testing Retest with 1:5 dilution to overcome potential inhibition [7]. Compare cycle threshold (Ct) values between diluted and undiluted samples.
Step 2: Alternative Target Verification Use a second PCR target (e.g., different SSU rDNA region) to confirm negative results [7].
Step 3: Melt Curve Analysis Perform melt curve analysis (ramping from 40°C to 80°C) to distinguish specific amplification from non-specific products [7]. Expected melt temperature for D. fragilis is 63-64°C.
Step 4: Amplicon Sequencing Confirm positive results and investigate questionable amplifications through SSU rDNA sequencing [7].
Cross-Reactivity Assessment
False positives from cross-reactivity can inversely affect perceived test performance. One study identified Simplicimonas sp. as the cause of cross-reactivity in cattle specimens [7]. Implement comprehensive specificity testing against related organisms.
Diagram 2: Discrepant Result Verification Pathway. This workflow systematically addresses unexpected negative results to confirm true negatives versus false negatives.
The reduction of false negatives in D. fragilis detection requires a systematic approach addressing pre-analytical, analytical, and post-analytical variables. Implementation of real-time PCR with proper controls, optimized sample handling, and verification protocols provides the most reliable path toward accurate prevalence data. As diagnostic accuracy improves, the epidemiological understanding of this enigmatic parasite will continue to evolve, potentially resolving long-standing questions about its true clinical significance and transmission dynamics. Researchers must prioritize method validation and standardization to ensure comparable results across studies and populations, finally overcoming the critical challenge of false negatives that has hindered D. fragilis research for decades.
Dientamoeba fragilis is a single-celled protozoan parasite that inhabits the human gastrointestinal tract. Despite its discovery a century ago, it remains one of the most enigmatic and diagnostically challenging enteric pathogens [11]. The organism lacks a recognized cyst stage in its life cycle, and its trophozoites are notoriously fragile, degrading rapidly once excreted in stool [12]. These biological characteristics pose significant technical hurdles for molecular detection, leading to considerable rates of false negatives in conventional diagnostic workflows and potentially skewing epidemiological data and clinical understanding [1]. This technical support document examines the critical failure points in the PCR-based detection of D. fragilis, from initial sample handling to final amplification, and provides evidence-based troubleshooting guidance to overcome these challenges.
Critical Failure Points in theD. fragilisPCR Workflow
Sample Collection and Storage: The Pre-Analytical Bottleneck
The fragility of D. fragilis trophozoites represents the first major hurdle in the diagnostic pipeline. Improper handling at this initial stage can irrevocably compromise sample quality, leading to false-negative results downstream.
- Trophozoite Degradation: The D. fragilis trophozoite is highly labile and survives for a limited time—typically between 6 to 48 hours—after being passed in stool [13]. This makes prompt processing or appropriate preservation absolutely critical.
- Preservation is Key: While unpreserved samples stored at 4°C may yield detectable DNA for up to 8 weeks, the sensitivity is significantly higher from stained, preserved stool specimens [12] [14]. The use of specific preservatives designed for parasitological examination is strongly recommended to maintain DNA integrity [12].
- Multi-Sample Requirement: Due to potential intermittent shedding of the parasite, examination of a single stool specimen may be insufficient. Multiple samples—three or more—are often necessary to establish a reliable diagnosis [12].
DNA Extraction: The Efficiency Variable
The choice of DNA extraction methodology directly impacts the yield and purity of nucleic acids, thereby influencing the efficacy of subsequent PCR amplification.
- Extraction Kit Performance: A comparative study of two DNA extraction kits—the semi-automated EZ1 (Qiagen) and the manual QIAamp DNA Stool Mini Kit (Qiagen)—revealed notable differences in performance. While both kits performed equally well for the detection of D. fragilis and Cryptosporidium spp., the EZ1 system demonstrated significantly higher efficiency (as indicated by lower quantitative PCR cycle threshold values) for five other eukaryotic enteric pathogens [15].
- Inhibition Control: The complex composition of fecal samples means they often contain PCR inhibitors. Incorporating an internal control during the DNA extraction process is a critical step to detect inhibition and avoid false negatives [7].
Amplification and Detection: Navigating Sensitivity and Specificity
This phase harbors the most nuanced technical challenges, where the choice of assay and interpretation of results can make the difference between a true positive and a false result.
- Assay Sensitivity is Paramount: When compared to microscopy, xenic culture, and conventional PCR, real-time PCR (RT-PCR) has been unequivocally established as the most sensitive detection method. One study found RT-PCR detected 35 isolates, compared to 15 by conventional PCR and 12 by microscopy, demonstrating a sensitivity and specificity of 100% [1]. It must, therefore, be considered the gold standard for diagnosis.
- The Peril of Cross-Reactivity: A critical diagnostic dilemma arises when PCR assays developed for human diagnostics are applied to animal or environmental samples. Recent research has shown that the EasyScreen assay can cross-react with Simplicimonas sp. in cattle samples and Pentatrichomonas hominis [7]. This cross-reactivity can be identified by a distinct 9°C cooler melt curve than that expected for true *D. fragilis amplicons [7].
- Cycle Threshold Considerations: To reduce the risk of false-positive results from non-specific amplification, it is recommended to limit the number of PCR cycles to less than 40 [7].
Table 1: Comparison of Diagnostic Methods for D. fragilis Detection
| Method | Sensitivity | Specificity | Key Limitations |
|---|---|---|---|
| Microscopy (Permanent Stain) | 34.3% | 99% | Relies on operator skill; degraded trophozoites are undetectable [1] |
| Xenic Culture (MBD) | 40% | 100% | Time-consuming; requires viable organisms [1] |
| Conventional PCR | 42.9% | 100% | Less sensitive than RT-PCR [1] |
| Real-Time PCR (RT-PCR) | 100% | 100% | Risk of cross-reactivity with non-target organisms if not properly validated [7] [1] |
The following workflow diagram outlines the key steps in the D. fragilis diagnostic process and highlights the major points of potential failure.
Diagram 1: Diagnostic Workflow for D. fragilis with Key Failure Points. The diagram highlights the pre-analytical and analytical phases, marking the most common sources of false-negative and false-positive results.
The Scientist's Toolkit: Research Reagent Solutions
Selecting the appropriate reagents is fundamental to optimizing the detection of D. fragilis. The following table details key materials and their functions as cited in the literature.
Table 2: Essential Research Reagents for D. fragilis PCR Detection
| Reagent / Kit | Specific Function / Role | Experimental Notes |
|---|---|---|
| QIAamp DNA Stool Mini Kit (Qiagen) | DNA purification from fecal samples. | Used in laboratory-based qPCR protocols; effective for D. fragilis and Cryptosporidium detection [7] [15]. |
| EZ1 Advanced XL (Qiagen) | Semi-automated nucleic acid extraction. | Shown to be faster and as/more efficient than manual methods for multiple enteric pathogens [15]. |
| EasyScreen Enteric Protozoan Detection Kit (Genetic Signatures) | Multiplex RT-PCR detection. | Includes extraction and inhibition controls; known cross-reactivity with P. hominis; requires melt curve analysis for specificity [7]. |
| qPCR Extraction Control Kit (Meridian Bioscience) | Monitors DNA extraction efficiency and PCR inhibition. | Added during extraction to distinguish true negatives from technical failures [7]. |
| Hypochlorite (HClO) Solution | Surface sterilization of helminth eggs in transmission studies. | Used at 1% concentration to degrade external DNA, confirming internal location of D. fragilis DNA in E. vermicularis eggs [16]. |
Troubleshooting Guide & FAQ
This section provides direct, actionable answers to common technical questions and problems encountered in D. fragilis research.
Q1: My positive control is amplifying, but my patient samples are consistently negative. What could be wrong?
- A: This pattern suggests a pre-analytical or sample-specific issue. Focus on:
- Sample Freshness and Preservation: Confirm that samples are being preserved immediately after collection or are processed promptly (ideally within 24-48 hours). The trophozoites degrade quickly, and DNA integrity is lost [12] [13].
- Inhibition Check: Re-extract the negative patient samples and include an internal control (e.g., from a kit like Meridian's qPCR Extraction Control) in your PCR. If the internal control fails to amplify, it indicates the presence of PCR inhibitors in the sample. Diluting the DNA template 1:5 or 1:10 can often overcome this [7].
- Multi-Sample Testing: D. fragilis shedding can be intermittent. Request and test two to three additional stool samples collected on non-consecutive days to increase detection sensitivity [12].
Q2: I am getting positive PCR signals from non-human host samples (e.g., cattle, dogs). How can I verify this is truly D. fragilis?
- A: A positive signal in a new host species requires rigorous confirmation to rule out cross-reactivity.
- Perform Melt Curve Analysis: This is the first and most rapid verification step. If using the EasyScreen assay, the true D. fragilis melt curve peaks at 63-64°C. A positive signal from cattle, for example, showed a melt curve 9°C cooler, which was later identified as Simplicimonas sp. [7].
- Confirm with DNA Sequencing: The gold standard for confirmation is to sequence the PCR amplicon. This definitively identifies the organism and differentiates D. fragilis from other trichomonads [7].
- Use a Second PCR Target: Employ a conventional PCR that targets a different gene, such as the small-subunit ribosomal RNA (SSU rDNA), followed by sequencing to validate your initial finding [7] [17].
Q3: What is the best way to definitively confirm a positive D. fragilis RT-PCR result?
- A: A multi-method approach is recommended for high-confidence results, especially in a research or novel clinical context.
- Melt Curve Analysis: Ensure the melt temperature (Tm) matches the expected value for your specific assay and probe chemistry [7].
- Sequencing: Sanger sequencing of the RT-PCR amplicon provides definitive proof of the organism's identity and can even be used for genotyping [7] [17].
- Microscopy: If a fresh or appropriately preserved sample is available, microscopic examination (e.g., using a permanent stain like modified iron-haematoxylin) can provide morphological confirmation, though its sensitivity is lower [12] [1].
The following decision tree visualizes the recommended process for verifying a positive result, particularly when working with samples from new animal hosts or when cross-reactivity is suspected.
Diagram 2: Specificity Verification Pathway for Positive qPCR Results. This workflow is essential to confirm the identity of the amplified product and prevent misidentification due to cross-reactivity, especially in studies investigating new host species.
The accurate detection of Dientamoeba fragilis hinges on a meticulous and informed approach to the entire molecular diagnostic pipeline. Failure to address the key technical hurdles—from the rapid degradation of trophozoites and suboptimal DNA extraction to the pitfalls of assay cross-reactivity—will inevitably lead to false negatives and an underestimation of the parasite's true prevalence and clinical impact. By implementing the troubleshooting strategies outlined herein, including the use of appropriate preservatives, validated extraction kits, highly sensitive RT-PCR assays, and mandatory specificity checks like melt curve analysis and sequencing, researchers and diagnosticians can significantly enhance the reliability of their results. Overcoming these technical failures is not merely a procedural necessity but a fundamental step toward unraveling the remaining mysteries of this elusive enteric protozoan.
FAQ: How do the biological characteristics ofDientamoeba fragiliscontribute to false negatives in diagnostic testing?
The biology of D. fragilis presents two major challenges that directly lead to false negative results: its rapid degradation and its intermittent shedding pattern.
- Rapid Trophozoite Degradation: The fragilis in its name refers to the fragile nature of the trophozoite, which is the stage typically found in stool [18]. Once outside the human body, the trophozoites degenerate rapidly, making them undetectable by microscopy if stool samples are not promptly examined or correctly fixed [18] [19] [8]. This fragility also compromises DNA integrity for PCR if samples are not preserved appropriately.
- Intermittent Shedding: The release of D. fragilis trophozoites into the stool is not constant. Instead, it occurs in a phasic or intermittent manner [6]. Relying on a single stool sample for diagnosis is therefore highly likely to miss the infection, as the parasite may not be present in that particular sample.
Recommendation: To counter these issues, it is strongly recommended to collect multiple stool samples (at least three) on separate days to maximize the chance of detection [6]. Furthermore, ensuring proper and rapid fixation of samples, or immediate freezing for molecular methods, is crucial to preserve parasite integrity [19].
FAQ: What is the relationship between parasite load and clinical significance, and how does it impact detection?
Emerging evidence indicates that parasite load is a critical factor, not just for detection sensitivity but also for determining the clinical relevance of a D. fragilis infection.
A 2025 prospective case-control study provided quantitative evidence linking high parasite loads to gastrointestinal symptoms. The study found that the proportion of individuals with a low parasite load (less than 1 trophozoite per field at 40x magnification) was significantly higher in asymptomatic individuals than in symptomatic cases (47.7% vs. 3.1%) [20]. This suggests that low-level detections may represent asymptomatic colonization, while high parasite loads are strongly associated with pathogenicity [20].
Impact on Detection:
- Microscopy: Low parasite loads fall near or below the effective detection limit of light microscopy, making them easy to miss, especially if the microscopist is not highly experienced [20] [21].
- Molecular Methods: While real-time PCR (qPCR) is more sensitive, the cycle threshold (Ct) value can serve as a useful quantitative indicator of parasite load. High Ct values (indicating low DNA quantity) should be interpreted with caution, as they may represent low-level colonization of uncertain clinical significance or even potential cross-reactivity [20] [22].
Recommendation: Any diagnostic approach for D. fragilis should be complemented by quantitative information (e.g., trophozoites per field for microscopy, Ct values for qPCR) to aid in interpreting the clinical significance of the finding and guiding treatment decisions [20].
FAQ: What are the major methodological challenges with PCR-based detection ofD. fragilis?
While PCR is a powerful tool, its application for D. fragilis detection is not without pitfalls, which can lead to both false positive and false negative results.
- Assay Sensitivity and Standardization: Different PCR assays have varying levels of sensitivity. A 2019 study comparing a commercially available assay (EasyScreen) with a widely used laboratory-developed test (LDT) found significant discrepancies [22]. The LDT generated multiple potential false-positive results on several PCR platforms, highlighting that not all assays are equally robust [22]. Furthermore, a lack of standardized assays across laboratories makes it difficult to compare prevalence studies [22] [6].
- Cross-Reactivity: Primers in some PCR assays may cross-react with non-target organisms. This is a particular concern when testing non-human specimens, but it can also affect human samples [7]. For instance, one study determined that a positive signal with the LDT in cattle feces was due to cross-reaction with Simplicimonas sp., not D. fragilis [7]. The EasyScreen assay has also been shown to cross-react with Pentatrichomonas hominis [7].
Troubleshooting Recommendations:
- Melt Curve Analysis: Always include and analyze the melt curve following qPCR. A discrepant melt temperature can be a key indicator of cross-reactivity with a non-target organism [7].
- Confirmatory Sequencing: For samples with atypical results (e.g., high Ct values, unusual melt curves) or from novel animal hosts, confirm the identity of the amplicon using DNA sequencing [7].
- Cycle Limit: To reduce the risk of false positives from non-specific amplification at late cycles, it is recommended to limit the number of PCR cycles to less than 40 [7].
Comparison of Diagnostic Methods forDientamoeba fragilis
| Method | Principle | Key Advantages | Key Limitations / Sources of Error |
|---|---|---|---|
| Light Microscopy | Visual identification of trophozoites on stained slides. | Low cost; allows for parasite load estimation [20]. | Low sensitivity [21]; requires high expertise [18] [8]; trophozoites degrade rapidly [19]; intermittent shedding requires multiple samples [6]. |
| Real-Time PCR (qPCR) | Amplification and detection of species-specific DNA sequences. | High sensitivity and specificity [23] [9]; provides quantitative data (Ct value) [20]; can test for multiple pathogens simultaneously [22]. | Risk of cross-reactivity [22] [7]; lack of standardized assays [22]; potential for false positives with high cycle counts [7]. |
Experimental Protocol: Determining Diagnostic Sensitivity and Specificity
This protocol outlines a standard method for validating a PCR assay for D. fragilis against a defined set of clinical samples, as demonstrated in several studies [19] [21] [9].
Objective: To determine the sensitivity, specificity, and negative predictive value of a novel PCR assay for the detection of Dientamoeba fragilis in human stool samples.
Materials and Reagents:
- Stool Samples: A panel of characterized samples, including microscopy-positive for D. fragilis, microscopy-negative, and samples containing other common protozoa (e.g., Giardia lamblia, Blastocystis hominis).
- DNA Extraction Kit: A kit validated for stool samples, such as the QIAamp Fast DNA Stool Mini Kit (Qiagen) [7] or the DNA Stool Mini Kit (Bioline) [21].
- PCR Reagents: Master mix (e.g., MyTaq Red Mix [21]), primers and probes specific for the D. fragilis SSU rRNA gene [23] [19], nuclease-free water.
- Equipment: Thermal cycler for conventional PCR or real-time PCR instrument.
Methodology:
- Sample Collection and DNA Extraction:
- PCR Amplification:
- For a 25 µL reaction, combine: 12.5 µL of 2X master mix, 10 pmoles of each primer, 1 µL of template DNA, and nuclease-free water to volume [21].
- Cycling conditions for conventional PCR [21]:
- Initial Denaturation: 95°C for 5 min.
- 35 Cycles of: Denaturation (95°C, 30 sec), Annealing (55°C, 1.5 min), Extension (72°C, 1.5 min).
- Final Extension: 72°C for 5 min.
- For qPCR, use established primer/probe sets and conditions, typically involving 45-50 cycles of amplification [23] [22].
- Analysis:
- Calculation of Assay Performance:
- Calculate Sensitivity as: (True Positives / (True Positives + False Negatives)) * 100.
- Calculate Specificity as: (True Negatives / (True Negatives + False Positives)) * 100.
Experimental Protocol: Assessing the Impact of Parasite Load on Detection Sensitivity
This protocol describes a quantitative approach to correlate parasite load with diagnostic outcomes, a key factor identified in recent research [20].
Objective: To compare the detection rates of microscopy and PCR across different levels of D. fragilis parasite load.
Materials and Reagents:
- Clinical Samples: Stool samples from a cohort of symptomatic and asymptomatic individuals.
- Microscopy Supplies: Microscope, slides, cover slips, trichrome or other permanent stain [21].
- Molecular Biology Supplies: DNA extraction kit, qPCR reagents and equipment, primers/probes for D. fragilis.
- Calprotectin Test (Optional): Fecal calprotectin (f-CP) test kit as an inflammatory marker [20].
Methodology:
- Sample Processing:
- Process each stool sample in parallel for microscopy and qPCR.
- Parasite Load Quantification by Microscopy:
- Examine trichrome-stained smears under oil immersion (1000x magnification).
- Quantify the parasite load as the number of trophozoites per field at a lower magnification (e.g., 400x), and categorize loads as high (>1 trophozoite/field) or low (<1 trophozoite/field) [20].
- Parasite Load Quantification by qPCR:
- Extract DNA and run qPCR for D. fragilis.
- Record the Cycle Threshold (Ct) value for each sample as a quantitative measure of parasite DNA concentration [20].
- Data Analysis:
- Correlate microscopy-based parasite load counts with qPCR Ct values.
- Compare the distribution of parasite loads (both microscopic counts and Ct values) between symptomatic and asymptomatic groups using statistical tests (e.g., Chi-square, t-test) [20].
Diagram: Experimental workflow for correlating parasite load with clinical symptoms using parallel microscopy and qPCR analysis.
Research Reagent Solutions
The following table details key materials and their functions for establishing a reliable D. fragilis research or diagnostic pipeline.
| Research Reagent | Function / Application |
|---|---|
| Trichrome Stain | Permanent stain for microscopic visualization of D. fragilis trophozoites and their characteristic fragmented nuclei; vital for morphological confirmation [21]. |
| SAF Fixative (Sodium Acetate-Acetic Acid-Formalin) | Preserves parasite morphology in stool samples for subsequent microscopic examination and staining [19]. |
| DNA Extraction Kit (e.g., QIAamp Fast DNA Stool Mini Kit) | Isolates high-quality PCR-ready DNA from complex and inhibitory fecal material [7]. |
| SSU rRNA Gene Primers/Probes | Targets the small subunit ribosomal RNA gene for highly specific PCR and qPCR detection of D. fragilis [23] [19] [21]. |
| Commercial Multiplex PCR Kit (e.g., EasyScreen) | Enables simultaneous detection of D. fragilis and other common gastrointestinal protozoa in a single, standardized reaction [22]. |
| Fecal Calprotectin (f-CP) Test | Measures intestinal inflammation as a non-invasive biomarker to support the assessment of clinical pathogenicity [20]. |
Core Concepts: Understanding PCR Inhibition in Stool Samples
What is PCR inhibition and why is it a particular problem for stool samples? PCR inhibition occurs when substances within a sample prevent or reduce the efficiency of the polymerase chain reaction. Stool is a complex biological matrix containing a wide variety of inorganic and organic compounds known to interfere with PCR amplification. These inhibitors can lead to reduced sensitivity or even false-negative results, which is especially problematic in diagnostic and research settings for pathogens like Dientamoeba fragilis [24] [25]. When inhibitors are present, you might observe amplification in your positive control but failure in your sample reactions, or see a complete failure to amplify even when you know the target DNA is present.
What are the common inhibitors found in stool samples? The following table summarizes major classes of PCR inhibitors frequently encountered in stool matrices and their proposed mechanisms of action [26] [25]:
| Inhibitor Category | Specific Examples | Proposed Mechanism of Interference |
|---|---|---|
| Organic Compounds | Bilirubin, bile salts, complex polysaccharides, lipids, hemoglobin, collagen [27] [25] | Bind to DNA polymerase or mimic nucleic acid structures, interfering with enzyme activity and primer binding [25]. |
| Inorganic Ions | Calcium, other metal ions [25] | Compete with magnesium ions (Mg++), which are essential co-factors for DNA polymerase [25]. |
| Complex Agents | Humic and fulvic acids, melanin, urea [25] | Interact with the template DNA and/or the polymerase enzyme, preventing the enzymatic reaction [25]. |
| Laboratory Reagents | Phenol, EDTA, heparin, SDS (detergents) [25] | Denature enzymes (phenol, SDS) or chelate essential Mg++ ions (EDTA) [25]. |
Troubleshooting Guide: From Symptom to Solution
What should I do if I get no PCR product from my stool sample? A lack of amplification, especially when your positive controls are working, strongly suggests the presence of PCR inhibitors. Follow this systematic approach:
- Run Critical Controls: Always include a positive control (with known target DNA) and a negative, no-template control. If the positive control fails, the issue is with your reaction mix or reagents. If only the sample fails, inhibition is likely [25].
- Dilute the Template: A simple and effective first step is to dilute your DNA template (e.g., 1:10 or 1:100). This can dilute the inhibitor to a level where it no longer affects the reaction. If dilution restores amplification, it confirms inhibition [25].
- Purify the DNA Further: If dilution does not work, re-purify your DNA sample using a silica-column-based cleanup kit or by ethanol precipitation to remove lingering impurities [28] [25].
- Use Inhibitor-Resistant Enzymes: Consider switching to a DNA polymerase specifically designed to be tolerant of common inhibitors found in complex samples like stool [25].
- Modify the Reaction Chemistry: The addition of Bovine Serum Albumin (BSA) at 200-400 ng/µL can bind to and neutralize certain inhibitors, such as phenolic compounds [26]. You can also try increasing the magnesium chloride (MgCl₂) concentration in 0.2-1 mM increments to counteract chelators [28].
How can I prevent false negatives in my Dientamoeba fragilis PCR assays? Preventing false negatives requires a multi-pronged strategy focusing on sample integrity and assay robustness.
- Incorporate an Internal Control: Use an Internal Control (IC), such as amplification of a mammalian housekeeping gene (e.g., GAPDH) or a spiked exogenous DNA sequence. The failure of the IC to amplify while your positive control works is a clear indicator of inhibition in the sample, alerting you to a potential false negative [26] [23].
- Optimize Sample Storage and Processing: Store stool samples at low temperatures and avoid excessive freeze-thaw cycles, which can degrade nucleic acids and release inhibitors [26]. Use effective and consistent homogenization and DNA extraction protocols validated for stool samples.
- Avoid Introduced Inhibitors: Be aware that powdered gloves or certain types of swabs (e.g., wooden cotton swabs) can introduce inhibitors. Use nuclease-free, sterile consumables [26].
Experimental Protocols & Workflows
Detailed Protocol: Spiking Experiment to Assess Inhibition This method helps you determine if your sample processing workflow introduces inhibition.
- Prepare Stool Sample: Process your stool sample as usual, including homogenization and DNA extraction.
- Spike with Control DNA: Divide the purified DNA sample into two aliquots. To one aliquot, add a known quantity of a non-target control DNA (e.g., a plasmid vector with a unique sequence not found in your samples) [26].
- Run Parallel PCRs: Perform two separate PCR reactions:
- Reaction A: Your standard D. fragilis PCR with the unspiked sample DNA.
- Reaction B: A PCR targeting the spiked control DNA sequence, using the spiked sample DNA.
- Interpret Results:
- If Reaction A is negative but Reaction B is positive, the sample contains D. fragilis DNA below the detection limit OR the D. fragilis assay is less robust than your control assay.
- If both reactions are negative, this is strong evidence of PCR inhibition in the sample, as even the spiked control failed to amplify [26].
Alternative Workflow: Immuno-PCR for Direct Detection To circumvent DNA extraction losses entirely, consider Immuno real-time PCR (iPCR). This method combines the specificity of antibody-based capture with the sensitivity of qPCR, eliminating the nucleic acid extraction step where significant DNA losses can occur [27]. In a study on human adenoviruses in stool, iPCR demonstrated a superior recovery rate (21-54%) compared to direct qPCR (0.3-9.5%), enabling detection of lower virus concentrations [27].
The workflow below illustrates the key steps in this method:
The Scientist's Toolkit: Essential Reagent Solutions
The following reagents are critical for overcoming inhibition and ensuring reliable detection of Dientamoeba fragilis.
| Reagent / Material | Function in the Context of Stool PCR |
|---|---|
| Inhibitor-Resistant DNA Polymerase | Polymerase enzymes engineered or formulated to maintain activity in the presence of common stool inhibitors like bilirubin and complex polysaccharides [25]. |
| Bovine Serum Albumin (BSA) | Acts as a "molecular sponge," binding to and neutralizing specific classes of PCR inhibitors (e.g., phenolics) [26]. |
| Internal Control DNA | A non-target DNA sequence spiked into the PCR reaction to distinguish true target absence from PCR failure due to inhibition [26] [23]. |
| Silica-Column DNA Purification Kits | Efficiently bind DNA while washing away many impurities and inhibitors; preferred over simple precipitation methods for dirty samples like stool [28]. |
| PCR Tubes with Aerosol Filters | Prevent cross-contamination between samples, which is a critical concern when working with high-copy amplification products [25]. |
| Specific Antibodies (for iPCR) | For immuno-PCR workflows; used to capture and detect intact pathogen particles directly from sample lysates, bypassing DNA extraction [27]. |
FAQs on PCR Inhibition in Stool
My positive control works, but my stool sample is negative. Is this definitely a true negative? No. This is a classic signature of potential PCR inhibition. The working positive control indicates your reagents and thermal cycler are functional, so the failure to amplify from the sample is likely due to inhibitors. You must perform additional tests, like template dilution or spiking with an internal control, to confirm the result is a true negative [26] [25].
Can I visually inspect my DNA sample to see if it's inhibited? No. PCR inhibitors are often present at molecular levels that do not change the physical appearance of the DNA solution (e.g., its color or viscosity). A sample that looks "clean" can still be heavily inhibited. Conversely, a slightly discolored sample might amplify perfectly well. Always rely on empirical controls rather than visual inspection [25].
How does the quality of the stool DNA extraction method impact inhibition? Significantly. The choice and execution of the DNA extraction protocol is one of the most critical factors. Low-quality methods may inefficiently remove inhibitors, leading to persistent problems. Automated, column-based extraction systems generally provide more consistent and pure DNA yields from complex matrices like stool compared to manual organic extraction methods, which can leave behind inhibitory residues [27] [25].
Advanced Protocols and Assay Selection for Maximizing D. fragilis Detection
Comparative Analysis of Commercial Multiplex PCR Kits (e.g., EasyScreen, AllPlex, AusDiagnostics)
In the specific context of Dientamoeba fragilis research, false negatives in multiplex PCR are a significant concern, potentially leading to an underestimation of prevalence and masking true clinical significance. A 2024 retrospective cohort study highlighted this challenge, finding that Dientamoeba fragilis was detected in 22.3% of over 27,000 patient samples but was not associated with gastrointestinal symptoms, raising questions about its pathogenicity and the accuracy of its detection [29]. This technical support center provides targeted troubleshooting guides and FAQs to help researchers overcome the technical hurdles that can compromise assay sensitivity and specificity, ensuring reliable results in the study of protists like Dientamoeba fragilis and Blastocystis.
Troubleshooting Guides
Guide 1: Addressing False Negatives
False negatives occur when a target sequence is present in a sample but is not amplified to a detectable level. In Dientamoeba fragilis research, this can directly impact the validity of clinical correlations.
- Problem: No amplification or low yield of the target signal.
- Potential Causes & Solutions:
- Target Secondary Structure: Folded RNA or DNA can block primer binding.
- Primer Dimers and Non-Specific Amplification: These spurious products consume reaction reagents, leaving fewer resources for the desired target amplification.
- Primer-Amplicon Interactions: A primer for one target may bind to and extend from an amplicon from a different target, generating shortened, non-detectable products.
- Solution: This is a more subtle issue. Utilize advanced primer design software that can check for cross-hybridization between all primers and all potential amplicons in the multiplex panel [30].
- Suboptimal Reaction Components: Multiplex reactions are more demanding than singleplex.
Guide 2: Resolving Uneven Amplification
This occurs when some targets in the panel amplify efficiently while others do not, skewing the results.
- Problem: Preferential amplification of certain targets over others.
- Potential Causes & Solutions:
- Unbalanced Primer Concentrations: Primers for highly abundant or efficiently amplifying targets can deplete shared reagents.
- Varying Primer Annealing Efficiencies: Primers with significantly different melting temperatures (Tm) will not anneal optimally at a single temperature.
- Solution: Design all primer pairs to have a very similar Tm (ideally within 1-2°C). A Tm of 55–60°C is often a good starting point [33].
- PCR Selection: inherent properties of the target, such as high GC content or complex secondary structure, can make it inherently less amplifiable.
- Solution: Besides additives like betaine, consider using specialized polymerase blends formulated for amplifying difficult templates [31].
Frequently Asked Questions (FAQs)
Q1: How can I validate that my multiplex PCR is working correctly after optimization? A1: Validation is a critical step. For each target, run both singleplex and multiplex reactions on the same plate using a standardized template. Calculate the difference in quantification cycle (ΔCq = Cqmultiplex – Cqsingleplex). A ΔCq of less than 1 indicates no significant loss in efficiency in the multiplex environment [33].
Q2: Our lab is considering a commercial kit. What performance metrics should we compare? A2: When evaluating commercial kits like EasyScreen, AllPlex, and AusDiagnostics, key metrics from comparative studies include [34] [35]:
- Sensitivity: The ability to correctly identify true positives.
- Specificity: The ability to correctly identify true negatives.
- Accuracy: The overall agreement with a reference method. Always request or review the manufacturer's validation data for the specific pathogens you are studying.
Q3: Why does our internal control amplify well, but the Dientamoeba fragilis target is inconsistent? A3: This points to an issue specific to the D. fragilis assay. The most likely causes are: 1) Sequence variation in the D. fragilis strain in your samples that affects primer/probe binding, necessitating a reassessment of your primer target region. 2) Inhibitors in the stool samples that may affect the D. fragilis assay more than the internal control due to its longer amplicon size or other factors. Implementing an appropriate DNA extraction method with inhibition removal steps is crucial [32].
Q4: What is the most critical factor for a successful one-step multiplex RT-qPCR? A4: For one-step RT-qPCR, which combines reverse transcription and PCR, the most critical factor is careful primer and probe design. All primers must have a similar Tm, amplicons should be short (70-150 bp), and probe Tm should be 8–10°C higher than the primers. Selecting fluorophores with minimal spectral overlap is also essential to prevent signal crosstalk [33].
Comparative Performance Data of Commercial Kits
The following tables summarize performance data from published comparative studies to aid in kit selection.
Table 1: Analytical Performance of Multiplex PCR Kits in Published Studies
| Kit Name | Target Area | Sensitivity (%) | Specificity (%) | Overall Accuracy (%) | Key Findings | Reference |
|---|---|---|---|---|---|---|
| Allplex STI Essential | Sexually Transmitted Infections | 98.1 | 94.1 | 96.7 | Demonstrated high sensitivity for multiple targets, though sensitivity for Trichomonas vaginalis was lower. | [35] |
| EUROArray STI | Sexually Transmitted Infections | 97.1 | 84.3 | 92.9 | Good sensitivity but lower specificity compared to the Allplex assay in the same study. | [35] |
| EasyScreen ESBL/CPO | Carbapenemase Genes | N/P | N/P | N/P | Allows rapid detection of clinically relevant carbapenemases; noted as a powerful diagnostic tool. | [34] |
| Allplex Entero-DR | Carbapenemase Genes | N/P | N/P | N/P | One of four compared platforms effective at detecting key carbapenemase genes like KPC. | [34] |
| AusDiagnostics MT CRE EU | Carbapenemase Genes | N/P | N/P | N/P | Included in a comparative study of molecular methods for CRE screening from rectal swabs. | [34] |
N/P: Specific performance metrics not provided in the abstract/full text of the searched results.
Table 2: Cost and Practicality Considerations
| Factor | Consideration | Impact on Workflow |
|---|---|---|
| Turnaround Time | Molecular tests dramatically reduce turnaround time compared to culture. | Allows for faster implementation of infection control precautions, potentially becoming cost-competitive despite higher reagent costs [34]. |
| Throughput | Platforms vary in the number of samples they can process per run. | Affects batch size and staffing requirements. Some systems can process up to 60 samples when paired with automated extractors [34]. |
| Automation | Compatibility with automated nucleic acid extraction and liquid handling workstations. | Reduces hands-on time and the risk of manual error, improving reproducibility [34] [35]. |
Experimental Workflow & Visualization
The following diagram illustrates a generalized workflow for developing, optimizing, and validating a multiplex PCR assay, incorporating critical steps to prevent false negatives.
Multiplex PCR Assay Development Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for Multiplex PCR Optimization
| Reagent / Material | Function in Multiplex PCR | Considerations for Use |
|---|---|---|
| Hot-Start DNA Polymerase | Reduces non-specific amplification and primer-dimer formation by remaining inactive until the first high-temperature denaturation step. | Critical for achieving high specificity in complex multiplex reactions. Use a formulation specifically tested for multiplexing [31]. |
| dNTP Mix | The building blocks (dATP, dCTP, dGTP, dTTP) for DNA synthesis. | Multiplex reactions require more dNTPs than singleplex. Ensure the mix is of high quality and at a concentration that supports simultaneous amplification of multiple targets [33]. |
| MgCl₂ Solution | A cofactor essential for DNA polymerase activity. Its concentration directly influences primer annealing and reaction specificity. | Optimize concentration carefully (e.g., 1.5 - 4.0 mM). Increased primer, probe, and dNTP concentrations in multiplex can chelate Mg²⁺, making it less available [36] [32]. |
| PCR Additives (e.g., Betaine, DMSO) | Betaine equalizes the melting temperatures of AT- and GC-rich sequences. DMSO helps denature DNA secondary structures. | Use to improve the amplification of targets with high GC content or complex secondary structure, a common cause of false negatives [31]. |
| Multiplex PCR Master Mix | A pre-mixed solution containing buffer, salts, polymerase, and dNTPs optimized for multiplexing. | Saves time and reduces pipetting error. Select a master mix with demonstrated performance for the level of multiplexing in your assay [33]. |
| Internal Control Template | A non-target nucleic acid sequence spiked into the reaction to monitor for PCR inhibition and reaction failure. | Essential for distinguishing true negatives from false negatives caused by reaction inhibition [32]. |
Core Principles for Maximizing DNA Yield and Quality
Why is the DNA extraction step from stool so critical for accurate D. fragilis PCR detection?
The accurate molecular detection of Dientamoeba fragilis is profoundly dependent on the initial DNA extraction step. Stool is a complex, inhibitor-rich sample where target parasite DNA is often present in low abundance and can be easily degraded. An inefficient extraction directly increases the risk of false-negative results by failing to recover sufficient intact D. fragilis DNA or by co-purifying substances that inhibit the subsequent PCR reaction.
What are the primary sources of false negatives related to DNA extraction?
False negatives in D. fragilis research primarily stem from three sources related to DNA extraction:
- PCR Inhibition: Substances such as heme, complex polysaccharides, bilirubin, and bile salts in stool can co-purify with DNA and inhibit polymerase activity in downstream PCR.
- Inefficient Lysis of the Parasite: The methods optimized for breaking open human or bacterial cells may not be sufficient to lyse the robust cell wall of protozoan parasites, leaving target DNA unrecovered.
- DNA Degradation: If stool samples are not preserved promptly or stored correctly, nucleases and microbial activity can fragment the target DNA, making it undetectable by PCR.
Detailed Experimental Protocols
Protocol 1: Optimized Workflow for Stool DNA Extraction
The following protocol, adapted from published methodologies, is designed to maximize the recovery of high-quality, PCR-ready DNA from stool specimens for sensitive detection of pathogens like D. fragilis [37] [38].
Workflow Overview:
Materials & Reagents:
- FastDNA Kit (or equivalent silica-membrane based kit) [38]
- Phosphate Buffered Saline (PBS), 0.01M, pH 7.2
- EDTA solution, 0.5M, pH 8.0
- PVP (Polyvinylpyrrolidone)
- FastPrep FP120 Disrupter or similar bead-beating instrument
Step-by-Step Procedure:
Sample Preservation & Preparation:
- Preserve stool samples immediately upon collection. 0.5 M EDTA (pH 8.0) has been demonstrated as an effective preservative for host and parasite DNA stabilization [37]. Alternatively, store samples at -80°C without preservative or preserve in 5% potassium dichromate or absolute ethanol [38].
- Centrifuge 300-500 µl of stool specimen at 14,000 × g for 5 minutes at 4°C. Discard the supernatant.
- Wash the pellet by resuspending it in 1 ml of PBS-EDTA buffer. Centrifuge again at 14,000 × g for 5 minutes. Repeat this wash step two more times to remove soluble PCR inhibitors [38].
- After the final wash, resuspend the pellet in PBS-EDTA to a final volume of approximately 300 µl.
Mechanical Lysis:
- Transfer the 300 µl of washed sample to a tube containing a lysing matrix (e.g., Lysing Matrix E).
- Add 400 µl of CLS-VF (Cell Lysis Solution), 200 µl of PPS (Protein Precipitation Solution), and PVP to a final concentration of 0.1% to 1%. PVP helps absorb polyphenolic compounds that can inhibit PCR [38].
- Securely close the tube and process it in a mechanical disrupter (e.g., FastPrep FP120) at a speed of 5.0-5.5 for 10-30 seconds. This bead-beating step is critical for efficient lysis of tough parasite cysts and trophozoites.
Purification and Binding:
- Centrifuge the lysate at 14,000 × g for 5 minutes to pellet debris.
- Transfer 600 µl of the supernatant to a new tube.
- Add 600 µl of Binding Matrix suspension (silica) and mix gently by inverting for 5 minutes to allow DNA binding.
Washing:
- Centrifuge the tube at 14,000 × g for 1 minute and carefully discard the supernatant.
- Resuspend the silica pellet in 500 µl of SEWS-M (Salt/Ethanol Wash Solution) by pipetting.
- Centrifuge again and discard the supernatant. Repeat the wash if the protocol requires it. Ensure all residual ethanol is removed by a final brief spin and pipetting.
Elution:
- Resuspend the clean silica pellet in 50-100 µl of DES (DNA Elution Solution) or TE buffer.
- Incubate at room temperature for 2-5 minutes to allow DNA to dissociate from the matrix.
- Centrifuge at 14,000 × g for 2 minutes and transfer the supernatant (containing purified DNA) to a clean, labeled tube.
- Store the DNA at -20°C until PCR analysis.
Protocol 2: Validating Extraction Success with PCR Assays
After extraction, validating the quality of the DNA is essential before proceeding with D. fragilis-specific PCR.
Materials & Reagents:
- Real-time PCR Master Mix
- Primers and Probes: Use validated assays. The Genetic Signatures EasyScreen assay is noted for its high specificity, while some laboratory-developed assays may show cross-reactivity [22] [7].
- Internal Positive Control (IPC) DNA to detect PCR inhibition.
Procedure:
- Inhibition Check: Perform a real-time PCR run spiked with a known quantity of IPC. A significant delay or failure in the IPC's amplification curve indicates the presence of inhibitors in the sample. Diluting the DNA template (1:5 or 1:10) is often an effective remedy [7].
- D. fragilis Detection: Use a robust real-time PCR assay. To minimize false positives from cross-reactivity, it is recommended to set the cycle threshold (CT) limit to 37 cycles and perform melt curve analysis where applicable. The expected melt temperature (Tm) for D. fragilis with the EasyScreen assay is 63-64°C; deviations may indicate non-specific amplification [7].
Troubleshooting Common DNA Extraction Problems
The table below outlines common issues, their potential causes, and evidence-based solutions.
Table 1: Troubleshooting Guide for Stool DNA Extraction
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low DNA Yield | Inefficient cell lysis | Incorporate a rigorous mechanical disruption step (bead beating) [37] [38]. |
| Incomplete inhibition removal | Ensure thorough washing steps with provided wash buffers; incorporate multiple wash cycles if needed [39]. | |
| PCR Inhibition | Co-purification of inhibitors (bile salts, complex carbs) | Add a pre-wash step with PBS-EDTA; use inhibitor removal chemistries like PVP; dilute DNA template 1:5 for PCR [39] [38] [7]. |
| Inconsistent Results | Sample heterogeneity | Ensure stool samples are thoroughly homogenized before aliquoting for DNA extraction [40]. |
| Degraded DNA | Preserve samples immediately in 0.5 M EDTA or freeze at -80°C; avoid repeated freeze-thaw cycles [37] [38]. | |
| False Positive/Negative PCR | Assay cross-reactivity | Use a validated commercial assay (e.g., EasyScreen); implement melt curve analysis and set a conservative CT cutoff (e.g., <37) [22] [7]. |
| Low assay sensitivity for degraded DNA | For suboptimal samples, target shorter amplicons (<200 bp) in your PCR assay to improve detection of fragmented DNA [37] [39]. |
Research Reagent Solutions
Selecting the right reagents is fundamental to a successful extraction workflow. The following table summarizes key solutions for optimizing DNA extraction from stool.
Table 2: Essential Reagents for Stool DNA Extraction
| Reagent / Kit | Primary Function | Key Consideration for D. fragilis Research |
|---|---|---|
| EDTA (0.5 M, pH 8.0) | Chelating agent that preserves DNA integrity by inhibiting nucleases [37]. | A simple and effective preservative shown to stabilize host DNA in stool; likely benefits parasite DNA similarly. |
| Silica-Membrane Kits (e.g., QIAamp Fast DNA Stool Mini Kit, InviSorb Spin Forensic Kit) | Selective binding and purification of DNA, removing proteins and inhibitors [39] [7]. | Kits optimized for pathogen detection from stool are preferable. The InviSorb kit is noted for handling degraded/low-yield samples [39]. |
| PVP (Polyvinylpyrrolidone) | Binds to polyphenols and other plant-based PCR inhibitors common in stool and food samples [38]. | Crucial for removing polysaccharide inhibitors that can cause false negatives in PCR. |
| Binding Matrix / Chaotropic Salts | Drives DNA to bind to silica membranes or magnetic beads in the presence of high salt concentrations. | Essential for efficient DNA capture from complex lysates. |
| Inhibitor Removal Buffers (e.g., InhibitEX) | Specific chemistry to adsorb and remove PCR inhibitors during the lysis step. | Integrated into many commercial kits (e.g., QIAamp kit) to improve downstream PCR success [7]. |
Leveraging Melt Curve Analysis to Discriminate D. fragilis from Non-Target Organisms
Accurate detection of Dientamoeba fragilis, a gastrointestinal protozoan, is crucial for diagnosing associated infections. Real-time PCR (qPCR) is a highly sensitive molecular tool for this purpose. However, a significant challenge in its application is the potential for cross-reactivity with non-target organisms, leading to false-positive results and inaccurate prevalence data. This technical guide focuses on leveraging melt curve analysis as a critical, post-amplification step to differentiate true D. fragilis signals from cross-reactions, thereby enhancing the reliability of your diagnostic and research outcomes.
Troubleshooting Guides
Scenario 1: Abnormal Melt Curve Peaks in Animal Specimen Screening
Problem: During a study to identify new animal hosts for D. fragilis, qPCR results from cattle specimens are positive, but the melt curves show a peak with a melting temperature (Tm) approximately 9°C cooler than the expected Tm for D. fragilis from human specimens [41].
Investigation & Solution: This discrepancy is a strong indicator of cross-reactivity. Follow this step-by-step verification protocol:
- Confirm Cross-Reactivity: The abnormal Tm suggests amplification of a non-target organism. In a documented case, this profile was traced to cross-reaction with Simplicimonas sp. [41].
- Sequencing Verification: To definitively identify the amplified product:
- Purify the qPCR product.
- Perform conventional PCR targeting the small-subunit (SSU) rDNA.
- Submit the PCR product for Sanger sequencing.
- Analyze the sequence using a database like BLAST to identify the true organism [41].
- Alternative Confirmatory Method: Next-Generation Sequencing (NGS) amplicon sequencing of the qPCR product can also be used to confirm the presence of D. fragilis or identify the cross-reactive organism [41].
Preventive Recommendation: When applying human-specific qPCR assays to new animal hosts, do not rely on a positive qPCR signal alone. Always confirm the result with melt curve analysis and, if the Tm is atypical, follow up with DNA sequencing [41].
Scenario 2: Multiple Peaks or Broad Peaks in Human Stool Samples
Problem: Melt curve analysis of human stool samples reveals multiple peaks or a single broad peak, suggesting potential non-specific amplification or primer-dimer formation [42].
Investigation & Solution:
- Analyze Peak Tm:
- Optimize Reaction Conditions:
- For primer-dimers (Tm < 80°C): Redesign your primers or lower the primer concentration in the reaction mix [42].
- For non-specific amplification (Tm > 80°C): Increase the annealing temperature during the PCR cycling program. A temperature gradient can help identify the optimal annealing temperature. Also, ensure that the DNA extraction method effectively removes inhibitors and consider protocols to reduce genomic DNA contamination [42].
- Confirm Product Purity: Run the qPCR product on a high-percentage agarose gel (e.g., 3%) to visualize the amplicons. A single, clean band of the expected size confirms a specific product, while multiple bands or a smear indicates issues [42].
Preventive Recommendation: Use in silico tools like uMelt prediction software during the assay design phase to forecast the melt profile of your intended amplicon and identify primers that may produce complex melt curves due to sequence composition [43].
Scenario 3: Discrepant Results Between Different qPCR Assays
Problem: Screening the same set of human stool samples with two different qPCR assays (e.g., the EasyScreen assay and a laboratory-developed assay) yields a significant number of discrepant results, with one assay detecting many more positives [22].
Investigation & Solution:
- Investigate False Positives: Discrepant samples that are positive only with the laboratory-developed assay may be false positives due to non-specific amplification. This is often characterized by very high cycle threshold (CT) values, which may be beyond the assay's reliable limit of detection [22].
- Adjust Cycle Thresholds: To reduce the risk of false positives from late-cycle amplification, it is recommended to set the cycle threshold to less than 40 cycles [41].
- Definitive Verification: Confirm the status of discrepant samples using an alternative method, such as:
Preventive Recommendation: Validate any laboratory-developed qPCR assay against a gold-standard method like sequencing across a range of sample types before implementing it for routine diagnostics or research [22].
Frequently Asked Questions (FAQs)
Q1: Why is melt curve analysis essential for D. fragilis detection? Melt curve analysis is a powerful, post-amplification step that assesses the specificity of your qPCR assay. Since D. fragilis primers can cross-react with other organisms (e.g., Simplicimonas sp. in cattle or other trichomonads), the melt curve provides a biophysical signature of the amplicon. A Tm shift or an abnormal curve shape is often the first indicator of a false positive, prompting further investigation and preventing erroneous conclusions [41] [22].
Q2: A single peak is supposed to indicate a single product. Why did sequencing show a non-target organism? A single peak generally indicates a homogeneous population of amplicons. However, it does not confirm that the amplicon is from your intended target. If the primers amplify a single, but non-target, DNA sequence from a different organism, the result will be a single, sharp peak. This underscores that a single melt peak confirms amplification specificity, but not necessarily target identity, which must be verified against known controls or through sequencing [41] [43].
Q3: Can high-resolution melt (HRM) analysis differentiate between D. fragilis genotypes? Yes, HRM is a more advanced form of melt curve analysis that is sensitive enough to detect minor sequence variations. Studies have shown that HRM can differentiate D. fragilis profiles, with some research identifying up to four different HRM profiles. These genotypic variations may even be correlated with different clinical manifestations, such as chronic versus acute diarrhea [45]. HRM is therefore a valuable tool for both identification and finer-scale genotyping.
Q4: My melt curve shows a slight slope or dip at the start. Does this affect my results? Minor fluctuations at the beginning of the melt curve, such as a slight slope or a dip, are often technical artifacts and typically do not impact the interpretation of the main melt peak or the results. The initial slope can be due to temperature-induced changes in solution pH or dye behavior before DNA denaturation begins. A dip can occur if some DNA strands re-anneal during the initial fluorescence collection phase. Focus your analysis on the primary melting transition [42].
Experimental Protocols for Validation
Protocol 1: SSU rDNA Sequencing to Confirm D. fragilis
This protocol is used to verify the identity of a qPCR amplicon when melt curve analysis suggests potential cross-reactivity [41] [44].
- DNA Extraction: Use a standardized kit (e.g., Qiagen EZ1 DNA tissue kit) for consistent results. Include a mock (no-feces) control.
- Conventional PCR:
- Primers: Use primers targeting the SSU rDNA gene, such as DF1 (5'-CTCATATCTACTTGGAAACCA A TT-3') and DF4 (5'-TTATAGTTTCTCTTATTAGCCCC-3'), which produce a ~662 bp amplicon [44].
- Reaction Mix: 50 μL volume containing PCR buffer, MgCl2 (e.g., 6 μL of 25 mM), dNTPs, primers, Taq polymerase, and template DNA. The addition of BSA or α-casein can help relieve PCR inhibition from fecal substances [44].
- Cycling Conditions: 40 cycles of denaturation (94°C, 1 min), annealing (52°C, 1 min), and extension (72°C, 1 min) [44].
- Gel Electrophoresis: Analyze the PCR product on a 1% agarose gel to confirm the amplicon is the expected size.
- Purification and Sequencing: Purify the PCR product and perform Sanger sequencing using the same primers.
- Analysis: Compare the obtained sequence to databases (e.g., NCBI BLAST) for definitive identification.
Protocol 2: Assessing Cross-Reactivity with HRM and Dynamic Time Warping (DTW)
This advanced protocol uses HRM and computational analysis for highly sensitive discrimination [46].
- PCR Amplification: Perform qPCR with a saturating DNA dye on a instrument capable of HRM data acquisition.
- HRM Data Acquisition: After amplification, heat the samples to 95°C, cool to 40°C to allow heteroduplex formation, and then heat slowly from 65°C to 95°C while collecting high-density fluorescence data.
- Data Analysis with DTW:
- Normalize and temperature-shift the raw melt curves.
- Use Dynamic Time Warping (DTW), a distance metric for time-series data, to compare the curve from your test sample to a database of reference curves from known D. fragilis genotypes and common non-target organisms.
- A large DTW distance indicates a dissimilar melt curve, suggesting a different organism or genotype [46].
Data Presentation
Table 1: Interpretation of Common Melt Curve Anomalies in D. fragilis PCR
| Observed Anomaly | Potential Cause | Recommended Action | Confirmatory Method |
|---|---|---|---|
| Single peak with Tm ~9°C lower than expected | Cross-reaction with non-target organism (e.g., Simplicimonas sp.) | Sequence the qPCR product | SSU rDNA sequencing [41] |
| Double peaks; minor peak Tm < 80°C | Primer-dimer formation | Redesign primers or lower primer concentration | Agarose gel electrophoresis [42] |
| Double peaks; minor peak Tm > 80°C | Non-specific amplification | Increase annealing temperature; check DNA quality | Agarose gel electrophoresis [42] |
| Discrepant positives between assays (high CT) | False positives from non-specific amplification | Set cycle threshold to < 40 cycles | NGS amplicon sequencing [41] [22] |
Table 2: Key Research Reagent Solutions for D. fragilis Melt Curve Analysis
| Reagent / Tool | Function | Application Note |
|---|---|---|
| EasyScreen Assay | Commercial qPCR kit for detecting D. fragilis and other enteric parasites. | Shown to have high specificity; considered a reference method in some regions [22]. |
| Laboratory-developed qPCR Assay | In-house PCR protocol, often based on the 5.8S rRNA gene. | Prone to cross-reactivity; requires rigorous validation and melt curve analysis [41] [22]. |
| SensiFAST HRM Mix | Pre-mixed solution containing DNA polymerase, dNTPs, and HRM-compatible dye. | Ideal for High-Resolution Melt analysis for genotyping and distinguishing sequence variants [46]. |
| uMelt Prediction Software | Free online tool to predict theoretical melt curves for a given DNA sequence. | Use during assay design to check if the chosen amplicon will produce a single, clean melt peak [43]. |
Workflow Visualization
The Role of Traditional Culture (e.g., Robinson's Medium) as a Sensitive Supplemental Tool
FAQs: Traditional Culture in a Modern Diagnostic Context
Why consider traditional culture when molecular methods like PCR are available? Despite the superior speed and sensitivity of PCR, traditional culture remains a valuable supplemental tool, particularly in research settings or in laboratories where PCR is not available. Culture is more sensitive than microscopic examination of stained smears and can supply live parasites for further studies, such as molecular typing or drug trials [47]. It serves as an effective independent method to investigate suspected PCR false negatives.
In what scenarios is culture most effectively used to investigate PCR false negatives? Culture is most effectively deployed when a clinical suspicion of D. fragilis infection exists despite a negative PCR result. This can occur due to PCR inhibition, low-level or intermittent shedding of parasites, or the presence of genetic variants that may not be detected by specific primers. Culturing provides a means to validate the PCR assay's performance.
What are the primary limitations of using culture for D. fragilis? The main limitations are the time required to obtain a result (at least 48-96 hours), the need for specialized expertise to prepare media and identify trophozoites, and the inability to perform culture on fixed stool samples [47]. Furthermore, culture is a labour-intensive process, making it less suitable for high-throughput diagnostic laboratories compared to PCR [1].
Which culture medium is recommended for optimal recovery of D. fragilis? Among the various media, Robinson's medium (RM) has been shown to be particularly effective. Studies comparing Robinson's, Dobell's (DM), and Talis's (TM) media found that Robinson's medium was not only the most sensitive but also supported the highest number of trophozoites, which is crucial for subsequent analyses [47].
Troubleshooting Guide: PCR and Culture
Troubleshooting PCR False Negatives
A false negative in PCR can obscure a true D. fragilis infection. The table below outlines common causes and solutions.
Table 1: Troubleshooting PCR False Negatives for D. fragilis Detection
| Problem Category | Specific Cause | Recommended Solution |
|---|---|---|
| Template Quality | PCR inhibitors in stool sample (e.g., polysaccharides, bile salts) [25]. | Dilute the template DNA 10- to 100-fold; use a DNA clean-up kit; or employ a polymerase resistant to inhibitors [48] [25]. |
| Degraded DNA template [48]. | Re-extract DNA from a fresh or appropriately preserved stool sample. | |
| Reaction Conditions | Suboptimal annealing temperature [48]. | Lower the annealing temperature in increments of 2°C for poor yield; increase for nonspecific bands. |
| Insufficient number of cycles [48]. | Increase cycle number by 3-5, up to 40 cycles. | |
| Inadequate primer or Mg²⁺ concentration [48]. | Optimize primer (0.05–1 µM) and Mg²⁺ (0.2–1 mM) concentrations. | |
| Primer/Target | Primer binding site polymorphism [49]. | Redesign primers or use a multiplex assay targeting different genetic regions [3]. |
| Low parasite load in sample. | Use culture to concentrate parasites from a larger stool volume before DNA extraction. |
Troubleshooting Traditional Culture
While culture is a powerful tool, its success depends on several factors.
Table 2: Troubleshooting Traditional Culture for D. fragilis
| Problem | Possible Cause | Solution |
|---|---|---|
| No Growth | Incorrect incubation temperature. | Incubate at the optimum temperature of 37°C for Robinson's medium and 41°C for Dobell's medium [47]. |
| Inappropriate atmosphere. | Provide a microaerophilic atmosphere for optimal growth [50]. | |
| Old or improperly prepared medium. | Prepare fresh media in small batches and ensure aseptic technique. | |
| Rapid degeneration of trophozoites in stool. | Inoculate culture medium with fresh, unpreserved stool immediately after collection [2]. | |
| Low Yield | Suboptimal culture medium. | Switch to or supplement with Robinson's medium, which supports higher trophozoite counts [47]. |
| Insensitive microscopic examination. | Examine culture sediments at 48, 72, and 96 hours post-inoculation. Use permanent stains (e.g., trichrome) for confirmation [47]. |
The following workflow integrates culture as a supplemental method to address PCR ambiguity.
Experimental Protocol: Supplemental Culture with Robinson's Medium
This protocol provides a detailed method for using Robinson's medium to cultivate D. fragilis from stool samples [47].
Materials and Reagents
Table 3: Key Research Reagent Solutions for D. fragilis Culture
| Reagent/Material | Function in the Protocol |
|---|---|
| Robinson's Medium | A diphasic (solid and liquid phase) xenic culture medium that supports the growth of intestinal protozoa [47]. |
| Rice Starch | A carbohydrate source included in the medium to support parasite nutrition [47]. |
| Fresh Stool Sample | The source of trophozoites. Must be unpreserved for successful culture [2]. |
| Microscope with 400x Magnification | Essential for examining culture sediments for motile trophozoites. |
| Trichrome Stain | A permanent stain used to confirm the morphology of D. fragilis trophozoites in culture sediment [47]. |
Step-by-Step Procedure
- Sample Inoculation: Inoculate approximately 0.5-1 g of fresh, unpreserved stool specimen into a tube of Robinson's medium.
- Incubation: Incubate the inoculated culture tube at 37°C for 96 hours [47].
- Microscopic Examination:
- After 48 hours of incubation, aseptically remove a drop of sediment from the culture tube.
- Place it on a microscope slide, add a coverslip, and examine under 400x magnification for motile trophozoites.
- Trophozoites may appear rounded with leaf-like, hyaline pseudopodia and may contain rice starch granules [47].
- Repeat Examination: If no trophozoites are seen at 48 hours, repeat the examination at 72 and 96 hours.
- Subculture: For samples with no growth at 96 hours, perform a subculture to a fresh medium tube and repeat the examination process to confirm a true negative [47].
- Confirmation: Prepare a trichrome-stained smear of the culture sediment to confirm the identity of the trophozoites based on nuclear characteristics [47].
Data Interpretation
- Culture Positive: Observation of motile trophozoites with characteristic morphology, confirmed by trichrome stain. This indicates a true infection and suggests a false negative in the initial PCR.
- Culture Negative: No trophozoites observed after 96 hours of incubation and a subsequent subculture. This supports the initial PCR negative result, provided the culture was performed correctly.
Comparative Data: Justifying the Supplemental Approach
The quantitative data below highlights the performance gap between different diagnostic methods and the relative efficacy of culture media.
Table 4: Comparative Sensitivity of Diagnostic Methods for D. fragilis [1]
| Diagnostic Method | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Real-Time PCR (RT-PCR) | 100 | 100 |
| Conventional PCR | 42.9 | 100 |
| Robinson's Medium Culture | 40.0 | 100 |
| Microscopy (Trichrome Stain) | 34.3 | 99 |
Table 5: Comparison of Culture Media Efficacy for D. fragilis Isolation [47]
| Culture Medium | Detection Rate from Microscopy-Negative Samples | Relative Trophozoite Yield |
|---|---|---|
| Robinson's Medium (RM) | 10.6% (11/104) | High (+++) |
| Talis's Medium (TM) | 3.8% (4/104) | Moderate (++) |
| Dobell's Medium (DM) | 2.9% (3/104) | Low (+) |
The following diagram outlines the decision-making process for a researcher investigating a discordant result between PCR and culture.
Strategic Troubleshooting and Workflow Refinement for Reliable PCR Outcomes
For researchers focused on the gastrointestinal protozoan Dientamoeba fragilis, achieving optimal Cycle Threshold (Ct) values in PCR assays is a critical yet challenging endeavor. This delicate balance directly impacts the sensitivity and specificity of detection, influencing the accuracy of prevalence studies, clinical diagnostics, and drug efficacy testing. Framed within the context of a broader thesis on addressing false negatives in D. fragilis PCR research, this guide provides targeted troubleshooting and FAQs to help scientists navigate the complexities of assay optimization and validation.
FAQs and Troubleshooting Guides
FAQ 1: What is the typical Ct value range for a true positiveD. fragilissample?
The expected Ct value range can vary based on the specific assay and sample type. In studies validating real-time PCR assays, positive control samples for D. fragilis have shown a median Ct value of approximately 32.2, with a observed range from 21.4 to 41.3 [51]. However, samples with Ct values approaching the upper limit of this range (e.g., >38) may represent low parasitic loads and require careful interpretation to distinguish from potential false positives or background noise.
FAQ 2: How can I determine if my high-Ct value sample is a true positive or a false positive?
High-Ct results necessitate confirmation through secondary methods. A primary step is to analyze the melt curve if using a probe-based system.
- Melt Curve Analysis: For the EasyScreen assay, the expected melt curve temperature for D. fragilis is 63–64°C [7]. A deviation of even 9°C can indicate cross-reactivity with a non-target organism, as was observed with Simplicimonas sp. in cattle specimens [7].
- Sequencing: Sanger sequencing or Next-Generation Sequencing (NGS) of the PCR amplicon provides definitive confirmation [7].
- Alternative PCR Targets: Using a different PCR assay that targets another gene region can help verify the result.
FAQ 3: What are the common causes of false negatives inD. fragilisPCR?
False negatives can significantly impact research on this parasite. Key causes include:
- PCR Inhibition: Co-purified inhibitors from stool samples can reduce amplification efficiency.
- Suboptimal DNA Extraction: The method may not efficiently lyse the parasite's cell wall or may recover insufficient DNA.
- Low Parasite Load: The number of organisms in the sample may be below the assay's Limit of Detection (LOD).
- Primer/Probe Mismatch: Genetic variation in the target region of local D. fragilis strains can prevent primer binding.
FAQ 4: How can I improve the sensitivity of myD. fragilisPCR assay?
To enhance sensitivity and reduce false negatives:
- Incorporate an Internal Control: Always use an internal control to detect PCR inhibition [7].
- Optimize DNA Extraction: Use kits designed for pathogen detection from stool and include a heating step (e.g., 10 minutes in InhibitEX buffer) to improve lysis [7].
- Lower the LOD: Validate your assay's LOD using a standardized DNA panel. One multiplex qPCR demonstrated a high diagnostic sensitivity of 0.90–0.97 for D. fragilis [51].
- Limit Cycle Number: To reduce the risk of false positives from non-specific amplification in later cycles, it is recommended to keep the number of PCR cycles below 40 [7].
Experimental Protocols for Validation
Protocol 1: Cross-Reactivity Testing for Specificity Assurance
Purpose: To ensure the D. fragilis assay does not amplify non-target organisms.
Methodology:
- Test Panel Assembly: Compile a DNA panel from other intestinal or phylogenetically related parasites. This should include organisms from the phyla Amoebozoa (e.g., Entamoeba), Apicomplexa, and Metamonada [51].
- qPCR Run: Process the cross-reactivity panel alongside positive and negative controls using your standard D. fragilis qPCR protocol.
- Melt Curve Analysis: Perform a post-amplification melt curve analysis (ramping from 40°C to 80°C in 1°C steps) [7].
- Data Interpretation: Any amplification from the non-target DNA must be investigated. Confirm the melt curve temperature matches the expected value for D. fragilis.
Protocol 2: Limit of Detection (LOD) and Sensitivity Determination
Purpose: To define the lowest concentration of D. fragilis that can be reliably detected by the assay.
Methodology:
- Standard Preparation: Create a standard curve using a quantified D. fragilis DNA sample. Serial dilutions should span several logs (e.g., from 10^6 to 10^1 copies/μL).
- Replicate Testing: Run each dilution in multiple replicates (e.g., 8-12 times) in a single qPCR experiment to determine the detection rate at each concentration [51].
- LOD Calculation: The LOD is the lowest concentration at which ≥95% of the replicates test positive.
- Sensitivity Calculation: Compare the qPCR results against a composite reference standard (e.g., microscopy, culture, or a validated commercial PCR) using a well-characterized sample set. Sensitivity is calculated as (True Positives / (True Positives + False Negatives)) [51].
Data Presentation
Table 1: Diagnostic Performance of Different Methods for Dientamoeba fragilis Detection
| Method | Sensitivity (%) | Specificity (%) | Notes |
|---|---|---|---|
| Real-time PCR (qPCR) | 93 - 100 [2] | 100 [2] | Considered the gold standard; allows for melt curve analysis. |
| Conventional PCR | 54 - 76 [52] [2] | 100 [52] | Lower sensitivity than qPCR; requires gel electrophoresis. |
| Microscopy (Trichrome Stain) | 0 - 93 [52] [2] | 98 - 99 [52] | Highly dependent on technician skill and sample freshness. |
| Microscopy (Iron Hematoxylin) | 46 - 67 [52] | 93 - 96 [52] | Requires significant expertise; time-consuming. |
| Wet Mount | ~13% detection rate [21] | N/A | Very low sensitivity; not recommended for diagnosis. |
Table 2: Key Reagent Solutions for D. fragilis PCR Research
| Reagent / Kit | Function | Example Use Case |
|---|---|---|
| QIAamp Fast DNA Stool Mini Kit (Qiagen) | DNA extraction from complex fecal material. | Used with a modified protocol (heating step) for optimal DNA yield [7]. |
| EasyScreen Enteric Protozoan Detection Kit (Genetic Signatures) | Multiplex PCR for simultaneous detection of enteric parasites. | Detects D. fragilis, Giardia, Cryptosporidium; includes internal controls [7]. |
| qPCR Extraction Control Kit (Meridian Bioscience) | Monitors DNA extraction efficiency and PCR inhibition. | Added during extraction to distinguish true negatives from failed extractions [7]. |
| D. fragilis-specific Primers & Probes | Amplifies target SSU rRNA gene sequence. | Target a ~662-bp fragment of the 18S SSU rRNA gene for conventional PCR [21]. |
| Multicolor Combinatorial Probe Coding (MCPC) | Fluorescent probe strategy for highly multiplexed PCR. | Allows detection of one-of-many targets in a single reaction by combining fluorophores [53]. |
Workflow Visualization
Diagram 1: D. fragilis PCR Diagnostic and Verification Workflow
Diagram 2: Cycle Threshold Optimization Logic
In the molecular diagnosis of Dientamoeba fragilis, effective DNA extraction is the foundational step that determines the accuracy of subsequent PCR analysis. The robust biological structure of parasite walls presents a significant challenge for efficient lysis, directly impacting the reliability of detection methods. False negatives in D. fragilis PCR research frequently originate from suboptimal DNA extraction protocols that fail to liberate sufficient genetic material from these hardy organisms [22] [21]. This technical guide addresses the critical lysis requirements for overcoming the structural barriers of D. fragilis, providing researchers with validated methodologies to enhance DNA yield and ensure diagnostic accuracy.
The challenge is substantiated by comparative studies showing significant discrepancies in detection rates between different methodological approaches. Research demonstrates that molecular techniques consistently identify more D. fragilis infections than traditional microscopy, with one study reporting PCR detection in 41% of samples compared to 13%-17% via microscopic examination [21]. These findings underscore the importance of optimized DNA extraction in unlocking the true prevalence of this parasite, whose pathogenic potential continues to be investigated [12] [5].
Molecular Diagnostics: Overcoming Structural Barriers
Understanding the Parasite's Structural Challenges
Dientamoeba fragilis presents unique structural characteristics that complicate DNA extraction. As a trichomonad parasite that inhabits the human gastrointestinal tract, it lacks a cyst stage in its life cycle under normal conditions, existing primarily as a trophozoite [12]. While this might suggest increased fragility, the organism demonstrates remarkable resilience to standard lysis protocols. Recent investigations have identified putative precyst forms that may possess enhanced structural integrity [5], further complicating DNA extraction efforts. The nuclear structure of D. fragilis, typically containing one or two nuclei with fragmented chromatin and no peripheral chromatin on the nuclear membrane [21], requires specialized lysis conditions to ensure complete DNA liberation.
Key Lysis Principles for Robust Parasite Walls
Effective lysis of D. fragilis depends on addressing its unique cellular composition through integrated mechanical, chemical, and enzymatic approaches:
- Cell Wall Disruption: The parasite's membrane integrity must be compromised through mechanical or chemical means to release intracellular components [22] [7].
- Inhibition Protection: Immediate inhibition of nucleases is crucial to prevent DNA degradation post-lysis [22].
- Cellular Debris Separation: Efficient removal of proteins, lipids, and other cellular components ensures pure DNA extraction suitable for PCR amplification [21] [7].
Technical Support Center
Troubleshooting Guide: Addressing Common DNA Extraction Challenges
Problem: Consistently low DNA yield from D. fragilis-positive stool samples
- Potential Cause: Incomplete lysis of robust parasite walls due to insufficient mechanical disruption or inadequate chemical lysis formulation.
- Solution: Implement a combined mechanical and chemical lysis approach. For mechanical disruption, use bead-beating with 0.1mm glass beads for 3 minutes at high frequency. Follow immediately with extended chemical lysis using G2 lysis buffer with proteinase K at 95°C for 15 minutes [22].
- Prevention: Validate extraction efficiency by spiking samples with a known quantity of cultured D. fragilis trophozoites and quantify DNA yield using fluorometric methods.
Problem: PCR inhibition despite adequate DNA concentration
- Potential Cause: Co-purification of PCR inhibitors from stool matrices, particularly polysaccharides and bile salts.
- Solution: Incorporate an inhibitor removal step using the InhibitEX buffer system [7]. Dilute extracted DNA 1:5 and retest if inhibition persists [7].
- Prevention: Include an internal control in the PCR reaction to detect inhibition early. Use DNA extraction kits specifically validated for stool samples.
Problem: Inconsistent results between sample replicates
- Potential Cause: Inhomogeneous distribution of parasites in stool samples, leading to variable DNA extraction.
- Solution: Ensure thorough homogenization of stool samples before aliquoting for DNA extraction. Use larger sample input (200mg instead of 100mg) to improve representation [21] [7].
- Prevention: Implement a standardized sample preparation protocol including suspension in buffer and vortexing for at least 2 minutes.
Problem: False negatives in samples confirmed positive by alternative methods
- Potential Cause: Degradation of DNA due to delayed processing or improper storage.
- Solution: Process samples within 24 hours of collection or preserve immediately in DNA stabilization buffer. Store at -20°C for short-term and -80°C for long-term preservation [21].
- Prevention: Establish a quality control system using known positive controls processed alongside clinical samples.
Frequently Asked Questions: Technical Guidance for Researchers
Q: What is the minimum number of D. fragilis organisms required for reliable PCR detection following DNA extraction? A: Studies indicate that real-time PCR assays can detect as few as 1-10 organisms per reaction when DNA extraction efficiency is optimized [22]. However, for consistent results in clinical samples, a minimum of 50-100 organisms per 100mg stool is recommended to account for potential extraction inefficiencies and PCR inhibitors.
Q: How does the choice of DNA extraction method impact detection sensitivity for D. fragilis? A: Extraction methodology significantly affects sensitivity. Automated systems like the GS1 DNA extraction machine used with the EasyScreen assay demonstrate higher sensitivity and reduced cross-reactivity compared to some laboratory-developed methods [22]. Kit-based methods utilizing specialized lysis buffers for difficult-to-lyse organisms consistently outperform traditional phenol-chloroform extraction for D. fragilis [21] [7].
Q: What quality control measures should be implemented to validate DNA extraction efficiency? A: A comprehensive quality control system should include:
- Process control: Exogenous DNA spike added to samples prior to extraction to monitor efficiency [7].
- Positive control: Known D. fragilis-positive stool sample extracted with each batch.
- Negative control: Extraction reagent blank to monitor contamination.
- Inhibition control: Internal control amplified alongside target to detect PCR inhibitors [22] [7].
Q: How can researchers troubleshoot cross-reactivity issues in PCR assays following DNA extraction? A: Cross-reactivity can be identified and addressed through:
- Melt curve analysis: D. fragilis exhibits a specific melt temperature (63-64°C in EasyScreen assay); deviations suggest cross-reactivity [7].
- DNA sequencing: Confirm positive results by sequencing PCR products [22] [7].
- Limit cycle threshold: Set CT value cutoffs (e.g., <38 cycles) to reduce false positives from non-specific amplification [22].
- Alternative primers: Validate results with a second PCR target to confirm specificity [7].
Comparative Analysis of Methodologies
DNA Extraction and PCR Detection Performance
Table 1: Comparison of Diagnostic Method Performance for Dientamoeba fragilis Detection
| Methodology | Sensitivity | Specificity | Remarks | Reference |
|---|---|---|---|---|
| Microscopy (Wet Mount) | 13-17% | 100% | Requires immediate examination; operator-dependent | [21] |
| Microscopy (Trichrome Stain) | 17% | 100% | Improved visibility of internal structures | [21] |
| Conventional PCR | 41% | 100% | Higher detection rate than microscopy | [21] |
| Real-time PCR (EasyScreen) | 100% | 100% | Gold standard; includes internal controls | [22] [2] |
| Laboratory-developed qPCR | Varies by platform | Potential cross-reactivity | Requires optimization and validation | [22] [7] |
DNA Extraction Efficiency Factors
Table 2: Critical Factors Influencing DNA Extraction Efficiency from Dientamoeba fragilis
| Factor | Impact on Efficiency | Optimal Condition | Validation Approach | |
|---|---|---|---|---|
| Sample Input Size | Directly correlates with DNA yield | 150-200mg stool | Quantitative spiking experiments | [21] [7] |
| Lysis Temperature | Critical for parasite wall disruption | 95°C for 10-15 minutes | Comparative yield assessment | [22] |
| Proteinase K Incubation | Digests structural proteins | 10μL per sample, 10min at 95°C | Pre- and post-extraction microscopy | [22] |
| Inhibition Removal | Reduces PCR false negatives | InhibitEX buffer system | Internal control amplification | [7] |
| Sample Preservation | Maintains DNA integrity | Immediate freezing at -20°C or use of preservatives | Time-course degradation study | [21] |
Research Reagent Solutions
Table 3: Essential Research Reagents for Effective DNA Extraction from Dientamoeba fragilis
| Reagent/Kit | Primary Function | Application Notes | Reference |
|---|---|---|---|
| G2 Lysis Buffer | Cellular disruption and DNA stabilization | Used in automated extraction systems; effective against robust parasite walls | [22] |
| Proteinase K | Proteolytic digestion of structural proteins | Critical for degrading tough parasite membranes; use at 95°C for 10min | [22] |
| InhibitEX Buffer | Removal of PCR inhibitors from stool | Particularly effective against polysaccharides and bilirubin | [7] |
| DNA Stool Mini Kit (Bioline) | Comprehensive DNA extraction | Optimized for difficult stool samples; includes inhibitor removal | [21] |
| QIAamp Fast DNA Stool Mini Kit (Qiagen) | Rapid DNA purification | Incorporates mechanical lysis options; suitable for high-throughput | [7] |
| EasyScreen Enteric Protozoan Detection Kit | Integrated extraction and detection | Includes internal controls for extraction efficiency | [22] [7] |
Experimental Workflow for DNA Extraction Validation
The following diagram illustrates the comprehensive workflow for validating DNA extraction efficiency from D. fragilis:
DNA Extraction Validation Workflow
Advanced Protocol: Validating Extraction Efficiency
Comprehensive Methodology for Extraction Efficiency Assessment
Sample Preparation and Spiking Protocol
- Negative Sample Selection: Identify D. fragilis-negative stool samples through preliminary screening using real-time PCR [22].
- Spike Preparation: Cultivate D. fragilis trophozoites and quantify using hemocytometer counting [5].
- Standardized Spiking: Introduce known quantities of trophozoites (10, 100, and 1000 organisms) into 200mg aliquots of negative stool matrix.
- Extraction Validation: Process spiked samples alongside unspiked controls using the standardized extraction protocol.
Efficiency Calculation Methodology
- Extract DNA from spiked samples and quantify using fluorometric methods specific for double-stranded DNA.
- Calculate extraction efficiency using the formula: Efficiency (%) = (Measured DNA / Expected DNA) × 100
- Establish expected DNA content based on genome size of D. fragilis (approximately 3.5 Mb) and quantity of spiked organisms [5].
Quality Threshold Establishment
- Set minimum efficiency thresholds: ≥70% for high-quality extractions, 50-70% for acceptable, and <50% requiring protocol optimization.
- Implement routine monitoring using 100-organism spikes as the quality control standard.
Cross-Platform Validation Approach
Multi-Method Verification
- Parallel Extraction: Process identical samples using both automated (GS1) and manual (QIAamp) extraction systems [22] [7].
- Comparative Sensitivity Assessment: Determine limit of detection for each method using serial dilutions of spiked samples.
- Inhibition Testing: Incorporate internal controls to identify method-specific inhibition issues [7].
Interlaboratory Validation
- Establish collaborative testing with partner laboratories using shared reference samples.
- Standardize reporting metrics including CT values, extraction efficiency, and inhibition rates to enable cross-comparison [22].
This comprehensive technical guide provides researchers with validated methodologies, troubleshooting solutions, and standardized protocols to overcome the critical challenge of DNA extraction efficiency in D. fragilis research. By implementing these evidence-based approaches, laboratories can significantly reduce false negatives and enhance the reliability of molecular detection for this clinically relevant parasite.
Implementing Rigorous Internal Controls to Monitor for PCR Inhibition
In the specific context of Dientamoeba fragilis PCR research, false negatives pose a significant threat to diagnostic accuracy and subsequent public health interventions. A primary, yet often overlooked, cause of these false negatives is polymerase chain reaction (PCR) inhibition. PCR inhibitors, which can co-extract with nucleic acids from clinical stool samples, impair the amplification process by interfering with the DNA polymerase, nucleic acids, or even the fluorescence detection itself [54]. This article provides a detailed technical guide for implementing robust internal controls to proactively detect and troubleshoot PCR inhibition in the laboratory.
FAQ: Understanding PCR Inhibition
What are PCR inhibitors and where do they come from in a clinical parasitology context?
PCR inhibitors are substances that interfere with the enzymatic amplification of DNA. In the context of Dientamoeba fragilis testing, the primary sample is stool, which contains a variety of potent inhibitors. These include complex polysaccharides, bilirubin, bile salts, and various organic acids [55]. Furthermore, reagents used in sample collection or DNA extraction can also introduce inhibitors [56].
How do PCR inhibitors actually work? What are the mechanisms?
Inhibitors operate through several distinct molecular mechanisms, which are crucial to understand for effective troubleshooting:
- Impairing DNA Polymerase Activity: Molecules like hemoglobin (from blood) and its derivative haematin bind to the DNA polymerase, blocking its active site and reducing its efficiency [54] [57].
- Interacting with Nucleic Acids: Immunoglobulin G (IgG) can bind to single-stranded genomic DNA, physically preventing primer annealing [57].
- Fluorescence Quenching: Substances like humic acid (common in soil and potentially on contaminated produce) and hemoglobin can quench the fluorescence of the dyes or probes used for amplicon detection in real-time PCR. This creates a false-negative signal, as amplification may occur but is not detected [54] [57].
- Co-factor Sequestration: Inhibitors like EDTA (an anticoagulant) chelate magnesium ions (Mg²⁺), which are essential co-factors for DNA polymerase activity [25].
Why is an Internal Control necessary, even when my PCR reagents work perfectly in clean samples?
The function of an internal control is to confirm that the entire process—from sample extraction to amplification—has worked for an individual sample. Without it, a negative result is uninterpretable; it could mean the target pathogen is absent, or that the reaction was inhibited [56]. A study of over 380,000 clinical samples found inhibition rates of up to 1% for some matrices, making it a non-trivial issue [56].
Troubleshooting Guide: Detection and Resolution of PCR Inhibition
Step 1: Implementing an Internal Control for Inhibition Monitoring
An effective internal control distinguishes true target absence from amplification failure.
| Control Type | Description | Advantage | Disadvantage |
|---|---|---|---|
| Pre-extraction Spiking | Adding a known quantity of a non-target organism or nucleic acid to the clinical sample before DNA extraction. | Controls for the efficiency of the entire extraction and amplification process. | Risk of cross-contamination; must be distinct from clinical targets. |
| Post-extraction Spiking | Adding a control template (e.g., a plasmid or synthetic DNA) to the purified DNA extract just before PCR setup. | Controls for the presence of inhibitors in the final extract and the amplification efficiency. | Does not control for inefficiencies during the DNA extraction step. |
The following workflow provides a standardized protocol for integrating these controls:
Step 2: Interpreting Internal Control Results and Identifying Inhibition
After running the PCR, use the following decision tree to interpret the internal control results and confirm the validity of your D. fragilis assay.
Step 3: Troubleshooting and Overcoming a Confirmed Inhibited Reaction
If the internal control indicates inhibition, several strategies can be employed to rescue the sample.
| Troubleshooting Strategy | Protocol / Application | Considerations for D. fragilis PCR |
|---|---|---|
| Dilution of DNA Extract | Perform a 1:10 or 1:100 dilution of the extracted DNA and re-amplify. | Simple and fast. However, it also dilutes the target D. fragilis DNA, potentially reducing sensitivity [25]. |
| Use of Inhibitor-Tolerant Polymerases | Replace the standard DNA polymerase with an inhibitor-tolerant enzyme blend. | A direct and powerful solution. Shown to increase tolerance to humic acid by 48-fold in dPCR [57]. |
| Additional Purification | Re-purify the DNA extract using a silica-column or magnetic bead-based clean-up kit. | Can effectively remove inhibitors, but always results in some loss of DNA, which is critical for low-abundance targets [54]. |
| Additives to the PCR Mix | Include additives like Bovine Serum Albumin (BSA) in the master mix. | BSA has been shown to improve inhibitor tolerance in Massively Parallel Sequencing (MPS) library preparation [57]. |
The following workflow visualizes a logical escalation path for applying these corrective actions:
The Scientist's Toolkit: Research Reagent Solutions
The selection of reagents is critical for robust PCR performance, especially with challenging samples. The table below summarizes key solutions for overcoming inhibition.
| Reagent / Kit | Function / Description | Evidence of Efficacy |
|---|---|---|
| Phire Hot Start II DNA Polymerase | An inhibitor-tolerant polymerase designed for amplification from difficult samples. | One of the top performers for direct detection in whole blood and soil samples [55]. |
| BSA (Bovine Serum Albumin) | A PCR additive that binds to inhibitors, preventing them from interfering with the polymerase. | Shown to mitigate the negative impact of humic acid and haematin in multiplex PCR for MPS [57]. |
| Inhibitor-Tolerant Buffer Blends | Specialized PCR buffers (e.g., STRboost, PCRboost) containing components that neutralize common inhibitors. | Use of an alternative DNA polymerase-buffer system dramatically increased inhibitor tolerance in digital PCR [57]. |
| Pre-extraction Internal Control | A non-target organism spiked into the sample prior to nucleic acid extraction. | Recommended to control for the entire analytical process, from extraction to amplification [56]. |
Advanced Considerations for D. fragilis Diagnostics
In the specific case of D. fragilis, vigilance against false positives is also required. A 2025 study highlighted that real-time PCR assays can cross-react with other organisms, such as Simplicimonas sp. in cattle specimens [7]. Melt curve analysis is a valuable technique to identify this; samples with D. fragilis typically have a specific melt temperature (e.g., 63–64°C for the EasyScreen assay), while cross-reacting organisms produce a distinct, cooler curve [7]. Furthermore, to reduce the risk of false positives from non-specific amplification, it is recommended to reduce the number of PCR cycles to less than 40 [7].
Implementing a rigorous system of internal controls is not optional but essential for reliable Dientamoeba fragilis PCR diagnostics. By understanding inhibition mechanisms, systematically monitoring for failure with spiked controls, and having a validated troubleshooting protocol, researchers and laboratory scientists can significantly reduce false-negative results. This ensures the accuracy of prevalence studies, clinical diagnoses, and treatment efficacy monitoring, ultimately strengthening the integrity of public health data and patient care.
Diagnostic Method Performance forDientamoeba fragilis
The following table summarizes the performance characteristics of various diagnostic methods for D. fragilis detection, based on a comparative study of 650 clinical stool samples.
Table 1: Performance Comparison of Diagnostic Methods for Dientamoeba fragilis [58] [1]
| Diagnostic Method | Sensitivity (%) | Specificity (%) | Number of Positives Detected (n=650) |
|---|---|---|---|
| Real-time PCR (RT-PCR) | 100 | 100 | 35 |
| Conventional PCR | 42.9 | 100 | 15 |
| Culture (Modified Boeck & Drbohlav's Medium) | 40.0 | 100 | 14 |
| Culture (TYGM-9 Medium) | 28.6 | 100 | 10 |
| Microscopy (Permanent Stain) | 34.3 | 99 | 12 |
Experimental Protocols
Protocol 1: Real-Time PCR Detection from Stool Samples
This protocol is adapted from a study establishing RT-PCR as the gold standard for detection [58] [1].
1. DNA Extraction:
- Sample Preparation: Suspend approximately 200 mg of fresh or thawed unpreserved stool in 1 ml of a lysis buffer containing guanidine thiocyanate, EDTA, Triton X-100, and Tris-HCl [44].
- Purification: Use a commercial DNA extraction kit (e.g., Qiagen EZ1 DNA Tissue Kit or High Pure PCR Template Preparation Kit). Include a mock DNA isolation (no feces) as a negative control for each extraction batch [44].
2. Real-Time PCR Amplification:
- Primer Design: Primers should target the small-subunit (SSU) rRNA gene, which shows remarkably little genetic variation in D. fragilis [44].
- Reaction Mixture (50 µl):
- 20 µl of extracted DNA solution
- 100 ng of each primer
- 500 µM dNTP mix
- 5 µl of 10x PCR buffer
- 6 µl of 25 mM MgCl₂
- 5 µl of Bovine Serum Albumin (5 mg/ml)
- 5 µl of α-casein (20 mg/ml) - Critical for relieving PCR inhibition by fecal substances [44]
- 0.2 µl (5 IU/µl) of Taq polymerase
- Thermocycling Conditions: 40 cycles of denaturation at 94°C for 1 min, annealing at 52°C for 1 min, and extension at 72°C for 1 min [44].
Protocol 2: Xenic Culture forD. fragilis
This protocol details the maintenance of D. fragilis in a biphasic culture system, which is essential for obtaining viable organisms for sequencing and other studies [59].
1. Culture Medium Preparation (Biphasic System):
- Solid Phase: Prepare Loeffler's serum slopes in McCartney bottles. Insipissate at a 30-45° angle, then autoclave using a dry sterile cycle (e.g., 89°C for 15-20 min). Store solidified slopes at 4°C [59].
- Liquid Phase: Overlay the serum slope with 3 mL of Phosphate-Buffered Saline (PBS) supplemented with 0.1 g of refined rice starch granules [59].
2. Inoculation and Incubation:
- Inoculate approximately 10 mg of fresh stool sample directly into the culture vial [59].
- Incubate the culture at 37°C under microaerophilic conditions (e.g., 0.2% O₂, 9.9% CO₂, 5% H₂, and 84.9% N₂) in an anaerobic jar system [59].
3. Monitoring and Sub-culturing:
- After 48 hours of incubation, examine the culture for trophozoites using phase-contrast microscopy at 400x magnification. Identify D. fragilis by its characteristic morphology [59].
- Passage cultures into fresh media every 48-72 hours to maintain growth [59].
Protocol 3: Bacterial Reduction in Culture for Improved Sequencing
The presence of bacterial DNA in xenic cultures poses a major challenge for genome sequencing. This protocol outlines a systematic antibiotic approach to reduce bacterial complexity [59].
1. Antibiotic Treatment Regimen:
- Elimination of Gram-positive Bacteria: Add vancomycin to the culture. This treatment eliminates Gram-positive bacteria without affecting trophozoite growth [59].
- Targeted Elimination of Gram-negative Bacteria: Add meropenem to eliminate anaerobic Gram-negative bacteria. Note: This treatment can lead to protozoan death after ~5 days, suggesting a dependence on some Gram-negative bacteria. To prevent this, the culture can be seeded with a meropenem-resistant strain of Klebsiella pneumoniae (e.g., KPC-2) before meropenem treatment to serve as a food source [59].
2. DNA Extraction and Metagenomic Sequencing:
- Extract DNA from the antibiotic-treated culture using standard methods.
- Apply a metagenomic approach to genome assembly. The reduction in bacterial complexity allows for the identification of D. fragilis sequences, such as the 28S large ribosomal DNA subunit gene, from the complex sequencing data [59].
Frequently Asked Questions (FAQs)
Q1: Our PCR results for D. fragilis are negative, but clinical symptoms and microscopy are suggestive of infection. What could be the cause? A1: Several factors can lead to false-negative PCR results:
- PCR Inhibition: Fecal samples contain substances that can inhibit the PCR reaction. The addition of relief agents like BSA and α-casein to the PCR mixture is critical to overcome this [44].
- Low Parasite Load: Day-to-day shedding of trophozoites is highly variable. Testing multiple stool samples collected over consecutive days increases detection sensitivity [44].
- Sub-optimal DNA Extraction: Ensure the extraction method is optimized for tough-to-lyse protozoan trophozoites and can handle inhibitory substances in stool.
Q2: Why is it necessary to include culture in the diagnostic algorithm when PCR is more sensitive? A2: While RT-PCR is the most sensitive detection method, culture is vital for the confirmatory part of the algorithm [58] [1].
- Viability Check: Culture confirms the presence of living, viable parasites.
- Isolate Generation: Culture provides biomass for downstream applications like genotyping, antibiotic sensitivity testing, and genome sequencing, which are difficult or impossible to perform directly on stool samples [59] [44].
Q3: We are unable to obtain clean D. fragilis genome sequences from our cultured isolates due to high bacterial contamination. How can we resolve this? A3: This is a common challenge because D. fragilis grazes on bacteria and bacterial DNA co-purifies with protozoan DNA [59].
- Systematic Antibiotic Treatment: Implement a protocol to reduce bacterial complexity in the xenic culture. Treat cultures with vancomycin to remove Gram-positive bacteria. Carefully use meropenem to target Gram-negative bacteria, being aware of the potential need for a resistant bacterial food source [59].
- Metagenomic Bioinformatics: Use metagenomic sequencing and sophisticated bioinformatics tools to sort and assemble the D. fragilis sequences from the mixed pool of sequence data after wet-lab bacterial reduction [59].
Q4: What is the current consensus on the pathogenicity of D. fragilis? A4: The pathogenicity of D. fragilis is historically debated. Recent research presents conflicting conclusions:
- Evidence for Commensalism: A 2024 case-control study found no significant difference in clinical or laboratory signs between patients carrying D. fragilis and a matched control group, regardless of the parasite load. This study suggested D. fragilis could be considered a commensal [60].
- Evidence for Pathogenicity: Other studies and a 2018 clinical guideline cite evidence linking infection to symptoms like abdominal pain and diarrhea, with reports of clinical improvement after eradication therapy [5]. The detection of the parasite in a symptomatic patient in the absence of other causes is often considered grounds for treatment [5].
Research Reagent Solutions
Table 2: Essential Reagents and Their Functions in D. fragilis Research
| Reagent / Kit | Function / Application | Key Notes |
|---|---|---|
| PCR Relief Agents (BSA, α-casein) | Mitigates PCR inhibition from fecal compounds. | Crucial for sensitivity in direct stool PCR [44]. |
| Loeffler's Serum Slope Medium | Solid phase for biphasic xenic culture. | Supports the growth of trophozoites [59]. |
| Rice Starch Granules | Nutrient supplement for culture medium. | Serves as a food source for the parasite [59]. |
| Specific Antibiotics (e.g., Vancomycin) | Selective elimination of Gram-positive bacteria from culture. | Reduces microbial complexity without harming trophozoites [59]. |
| DNA Extraction Kit (e.g., Qiagen EZ1) | Nucleic acid purification from stool or culture. | Automated platforms can improve consistency [59] [44]. |
| Primers Targeting SSU rRNA Gene | Amplification of D. fragilis DNA by PCR. | Target a conserved and species-specific genetic region [44]. |
Troubleshooting Guides
Problem: Failure to Detect D. fragilis by PCR in Clinically Suspected Cases
- Potential Cause 1: PCR Inhibition.
- Solution: Include an internal control in the PCR reaction to detect inhibition. Re-extract the DNA and ensure the PCR mixture contains relief agents like BSA and α-casein [44].
- Potential Cause 2: Low Parasitic Load or Intermittent Shedding.
- Solution: Collect multiple stool samples (e.g., on 3 consecutive days) and test each individually to increase the probability of detection [44].
- Potential Cause 3: Primers/Target Failure.
- Solution: Verify the primer specificity and the integrity of the PCR reagents. Ensure the primers are targeting a validated, conserved region such as the SSU rRNA gene [44].
Problem: Culture Contamination or Overgrowth by Bacteria
- Potential Cause: Normal flora outcompeting the parasite.
- Solution: This is inherent to xenic culture. Incorporate antibiotic treatments into the culture protocol. Vancomycin can be used to control Gram-positive bacteria. For Gram-negative bacteria, use meropenem with caution, considering the potential need to supplement with a resistant bacterial strain to sustain D. fragilis growth [59].
Problem: Poor Quality D. fragilis Genome Sequence Data due to Bacterial DNA
- Potential Cause: Bacterial DNA outcompeting parasite DNA in sequencing reactions.
- Solution: Prioritize bacterial reduction in culture using the systematic antibiotic treatment described in Protocol 3. Following wet-lab reduction, employ metagenomic assembly strategies to bin and identify D. fragilis sequence contigs from the complex dataset [59].
Diagnostic and Research Workflows
Diagram 1: Multi-Method Confirmatory Diagnosis Algorithm. This workflow integrates PCR, culture, and sequencing to confirm D. fragilis infection and generate viable isolates for further research.
Diagram 2: Bacterial Reduction Workflow for Sequencing. This chart outlines the critical steps and decision points in using antibiotics to reduce bacterial contamination in xenic cultures to enable viable genome sequencing.
Benchmarking Performance: PCR Versus Traditional and Alternative Diagnostic Modalities
The detection of Dientamoeba fragilis, a gastrointestinal protozoan, is highly dependent on the diagnostic method employed. The following table summarizes the performance metrics of various techniques as established by comparative studies, demonstrating the clear superiority of molecular methods over traditional microscopy.
Table 1: Performance Metrics of D. fragilis Diagnostic Methods
| Diagnostic Method | Reported Sensitivity | Reported Specificity | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Real-time PCR (RT-PCR) | 89% - 100% [58] [61] [21] | 100% [58] [61] | Superior sensitivity; quantitative potential (parasite load); high throughput [58] [20] | Risk of primer cross-reactivity; requires specialized equipment [22] [7] |
| Conventional PCR | 42.9% - 76% [58] [2] | 100% [58] | Highly specific; allows for genotyping [21] | Lower sensitivity than RT-PCR; gel electrophoresis required [2] |
| Microscopy (Trichrome Stain) | 34.3% - 52% [58] [2] | 99% - 100% [58] [2] | Low cost; can detect other parasites simultaneously [21] | Low sensitivity; requires expert microscopist; subjective [62] [21] |
| Microscopy (Wet Mount) | ~34% [58] | Information Missing | Rapid; low cost | Very low sensitivity; trophozoites degrade rapidly [62] [21] |
| Xenic Culture (MBD) | 40% [58] | 100% [58] | Can amplify parasite number | Time-consuming; not routine in most labs [58] |
The accurate detection of Dientamoeba fragilis is a critical step in research aimed at understanding its epidemiology and pathogenic potential. For decades, microscopic examination of stained stool specimens was the primary diagnostic tool. However, the fragile nature of the trophozoite, its rapid degeneration after passage, and the irregular shedding pattern of the parasite lead to significant false-negative rates [63] [61]. The advent of polymerase chain reaction (PCR)-based methods has dramatically improved detection capabilities but introduced new challenges, including assay validation and interpretation of positive results in asymptomatic individuals [60] [22]. This guide provides a technical framework for researchers to troubleshoot these diagnostic hurdles, with a focus on minimizing false negatives in PCR-based studies.
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
FAQ 1: Why is microscopy considered an inadequate gold standard for D. fragilis detection in research settings?
Microscopy is plagued by inherently low sensitivity. The "fragile" trophozoites degrade quickly outside the body, requiring immediate fixation and expert analysis using permanent stains (e.g., trichrome). Even under optimal conditions, studies consistently show microscopy detects only about 34-52% of infections confirmed by PCR [58] [2] [21]. This high false-negative rate can severely skew prevalence data and confound associations in clinical studies.
FAQ 2: My RT-PCR assay is detecting D. fragilis in asymptomatic subjects. Are these results false positives?
Not necessarily. The high sensitivity of RT-PCR allows for the detection of low-level infections and asymptomatic carriage [60]. Recent evidence suggests that parasite load is a key differentiator. A 2025 case-control study found that high parasite loads were strongly associated with symptomatic disease, while low loads (e.g., <1 trophozoite per field) were more common in asymptomatic individuals [20]. Therefore, quantifying the parasite load (e.g., via cycle threshold (Ct) values) is crucial for interpreting positive results, rather than dismissing them as false positives.
FAQ 3: How can I ensure my PCR assay is specific for D. fragilis and not cross-reacting with other organisms?
Cross-reactivity is a valid concern. A 2025 study identified that a commonly used laboratory-developed RT-PCR assay cross-reacted with Simplicimonas sp. in cattle samples and produced false positives in human samples [7]. To ensure specificity:
- Perform Melt Curve Analysis: A discrepant melt curve temperature was a key indicator of cross-reactivity in the aforementioned study [7].
- Use Sequence-Confirmed Controls: Validate your assay with DNA from well-characterized D. fragilis strains and other related protozoa.
- Consider Commercial Kits: FDA-cleared multiplex assays (e.g., Genetic Signatures EasyScreen) are validated for specificity against a panel of common gastrointestinal pathogens [22] [62].
Troubleshooting Common Experimental Issues
Problem: Inconsistent detection of D. fragilis in longitudinal samples from the same subject.
Solution: This is likely due to the known intermittent shedding of trophozoites [61].
- Protocol Adjustment: Do not rely on a single stool sample. The recommended protocol is to collect at least three stool samples on alternate days [63] [21]. This significantly increases the probability of detection.
- Sample Preservation: Immediately preserve stool samples in appropriate fixatives (e.g., SAF, ethanol) suitable for DNA extraction to prevent trophozoite degradation [61] [21].
Problem: Low amplification signal or PCR inhibition in stool samples.
Solution: Stool is a complex matrix known to contain PCR inhibitors.
- Protocol Adjustment: Incorporate an Internal Amplification Control (IAC) into your RT-PCR reaction. The failure of the IAC to amplify indicates inhibition, alerting you to problematic samples [22] [61].
- Technical Remedy: If inhibition is detected, dilute the DNA template (e.g., 1:5 or 1:10) and re-run the PCR. Alternatively, use a DNA extraction kit specifically designed to remove inhibitors from fecal samples [7].
Experimental Protocols
Detailed Protocol: Real-Time PCR for D. fragilis Detection
This protocol is adapted from the laboratory-based assay widely used in clinical research [22] [61].
1. Sample Collection and DNA Extraction:
- Collection: Collect fresh stool sample and immediately preserve a portion in 100% ethanol (≈1 g/mL) for DNA isolation [61].
- Extraction: Use a commercial stool DNA extraction kit (e.g., QIAamp Fast DNA Stool Mini Kit). Include an extraction control DNA (e.g., from a qPCR Extraction Control Kit) to monitor extraction efficiency [7].
- Modification: Include a heating step (10 min at 95°C) of the stool suspension in InhibitEX buffer to improve lysis [7].
- Storage: Store eluted DNA at -20°C until use.
2. Real-Time PCR Setup:
- Primers/Probes: Target the 5.8S ribosomal RNA gene as described by Verweij et al. (2007) [61].
- Reaction Mix: Prepare a multiplex reaction containing:
- 1x TaqMan Universal PCR Master Mix
- Forward and Reverse Primers (e.g., 900 nM each)
- D. fragilis-specific TaqMan Probe (e.g., 200 nM)
- Internal Control (e.g., Phocid Herpesvirus, PhHV) primers and probe
- 5 µL of template DNA
- Nuclease-free water to a total volume of 25 µL
- Cycling Conditions (on a compatible real-time cycler):
- Enzyme Activation: 95°C for 10 min
- Amplification (45 cycles): 95°C for 15 sec (denaturation) → 60°C for 1 min (annealing/extension)
- Post-Run Analysis:
- Perform melt curve analysis by ramping from 40°C to 80°C in 1°C increments to check for specific amplification [7].
The following workflow diagram summarizes the key steps and quality control checkpoints in this protocol.
Detailed Protocol: Microscopic Examination (Trichrome Stain)
For comparative studies, microscopy remains a useful tool, particularly for observing parasite morphology [21].
1. Sample Preparation:
- Fixation: Prepare a thin smear of fresh stool on a microscope slide and immediately fix in Schaudinn's fluid.
- Staining: Follow the standard Wheatley's trichrome staining procedure [21]:
- De-stain in 70% ethanol with iodine.
- Place in 70% ethanol.
- Stain in trichrome stain for 8-10 minutes.
- Rinse in acid-alcohol for 1-3 seconds.
- Dehydrate through 95% ethanol, 100% ethanol, and xylene.
- Mount with a synthetic resin.
2. Microscopic Examination:
- Systematically examine the stained smear under oil immersion (100x objective).
- Identify Trophozoites: Look for pleomorphic organisms, 5-15 μm in diameter, with one or two nuclei. The nuclear chromatin is often fragmented, and the cytoplasm may be vacuolated [63] [21].
- Analysis: Examine a minimum of 300 microscopic fields to maximize sensitivity.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents for D. fragilis Detection Research
| Item | Function/Application | Example Products / Notes |
|---|---|---|
| Stool DNA Extraction Kit | Isolate PCR-quality DNA from complex fecal matrix. | QIAamp Fast DNA Stool Mini Kit (Qiagen) [7] |
| Real-Time PCR Master Mix | Enzymes and buffers for probe-based qPCR. | TaqMan Universal PCR Master Mix [61] |
| D. fragilis Primers/Probes | Specific detection of target gene sequences. | Lab-developed (5.8S rRNA target) [61] or commercial kits (e.g., Genetic Signatures EasyScreen) [22] |
| Internal Control (IC) | Monitors for PCR inhibition; essential for validating negative results. | Phocid Herpesvirus (PhHV) DNA [61] or commercial IC kits |
| Trichrome Stain | Permanent stain for morphological identification of trophozoites. | Wheatley's trichrome stain [21] |
| Sample Preservative | Prevents degradation of trophozoites for both microscopy and PCR. | SAF Preservative, 100% Ethanol [61] [21] |
In molecular research, the reproducibility of Polymerase Chain Reaction (PCR) assays across different laboratories is a fundamental requirement for generating reliable, comparable data. Multicenter studies provide the most realistic assessment of how PCR assays perform under real-world conditions, revealing inconsistencies that may not be apparent in single-center validations. These studies are particularly crucial in clinical diagnostics and drug development, where assay reliability directly impacts patient outcomes and research validity.
For researchers investigating protozoan parasites like Dientamoeba fragilis, understanding and mitigating sources of PCR inconsistency is essential. This technical support center provides troubleshooting guides and FAQs specifically designed to help scientists identify, understand, and resolve the most common issues affecting PCR assay consistency across multiple research sites.
Key Research Reagent Solutions
The table below outlines essential reagents and materials referenced in multicenter PCR studies, along with their specific functions in ensuring assay consistency:
Table 1: Key Research Reagents and Their Functions in PCR Assays
| Reagent/Material | Function in PCR Assays | Consistency Considerations |
|---|---|---|
| Idylla EGFR Mutation Test Cartridges | Fully automated RT-PCR testing for EGFR variants in NSCLC [64] | Standardized reagents reduce inter-laboratory variability |
| EasyScreen Enteric Protozoan Detection Kit | Multiplex PCR for detection of gastrointestinal protozoa including D. fragilis [65] | Includes internal controls for inhibition detection |
| SYBR Green I & Hydrolysis Probes (TaqMan) | Fluorescence-based detection of amplified DNA [66] | Dye chemistry affects specificity requirements and data interpretation |
| QIAamp Fast DNA Stool Mini Kit | DNA extraction from complex fecal samples [65] | Standardized extraction critical for sample-to-sample consistency |
| RNA/DNA Preservation Solutions (SAF fixative) | Preserves nucleic acid integrity in clinical samples [65] | Prevents degradation between sample collection and processing |
| PCR Enhancers (DMSO, Trehalose, Tween 20) | Additives to improve amplification efficiency [67] | Optimization required for specific template-primer combinations |
Troubleshooting Common PCR Consistency Issues
FAQ: Why do we observe different results when using the same PCR protocol across multiple centers?
Answer: Discrepancies in multicenter PCR results often stem from these key factors:
- Sample quality variations: Differences in sample collection, storage, and nucleic acid extraction methods significantly impact PCR efficiency [65]. For example, the time between sample collection and preservation affects D. fragilis detection due to rapid trophozoite degeneration [47].
- Instrument calibration differences: Thermal cycler temperature variations even as small as 0.5°C can dramatically affect amplification efficiency [66].
- Reagent lot variations: Different lots of enzymes, primers, and master mixes may have varying efficiencies [67].
- Operator technique: Manual pipetting errors and subjective interpretation of results contribute to inter-laboratory variability [68].
- Inhibition differences: Varying levels of PCR inhibitors in different sample batches affect results inconsistently [65] [21].
FAQ: How can we minimize false negatives in Dientamoeba fragilis detection?
Answer: False negatives in D. fragilis research can be addressed through these strategies:
- Implement melt curve analysis: After qPCR, perform melt curve analysis to differentiate true D. fragilis amplification from cross-reactions with non-target organisms [65]. One study found a 9°C difference in melt curves between true D. fragilis and cross-reacting Simplicimonas sp. [65].
- Use multiple detection targets: Target different genomic regions to confirm positive results and reduce primer-specific false negatives [9].
- Optimize cycle thresholds: Reduce the number of PCR cycles to less than 40 to decrease the risk of false positives from non-specific amplification, which can mask true positives [65].
- Include complementary methods: Combine PCR with microscopic examination or culture techniques for verification [47] [21]. One study found culture increased detection rates from 3.3% to 5.2% compared to microscopy alone [47].
- Validate with DNA sequencing: Confirm positive identifications with SSU rDNA sequencing, especially when testing new host species [65].
Experimental Protocols for PCR Verification
Protocol: Cross-Reactivity Assessment for Dientamoeba fragilis Assays
This protocol is adapted from recent multicenter research on D. fragilis detection [65]:
Sample Collection and Preservation:
- Collect fecal samples and split into two portions
- Add one portion to SAF fixative for morphological preservation
- Reserve the second portion without preservative for molecular analysis
DNA Extraction:
- Use QIAamp Fast DNA Stool Mini Kit following manufacturer's instructions
- Include an extraction control to monitor inhibition
- Elute DNA in buffer AE and store at -20°C
qPCR Setup:
- Perform two parallel qPCR assays: EasyScreen and laboratory-based protocol
- Include no-template controls and positive controls in each run
- Use the following cycling conditions:
- Initial denaturation: 95°C for 10 minutes
- 40 cycles of: 95°C for 15 seconds, 60°C for 1 minute
- Melt curve analysis: 40°C to 80°C in 1°C increments
Melt Curve Analysis:
- Compare melt curve temperatures between samples
- True D. fragilis produces a melt curve of 63-64°C with EasyScreen assay
- Significant deviations (e.g., 9°C cooler) indicate potential cross-reactivity
Sequencing Verification:
- Perform conventional PCR targeting SSU rDNA
- Sequence amplified products and compare to reference databases
- Use BLAST analysis for species confirmation
Protocol: Multicenter QC Assessment for PCR Assays
This protocol provides a framework for validating PCR consistency across multiple sites:
Standardized Material Distribution:
- Prepare aliquots of reference DNA/cDNA samples at central facility
- Distribute identical panels to all participating laboratories
- Include samples spanning expected detection range
Cross-Site Testing:
- Each site performs PCR using standardized protocol
- Sites document all deviations and local conditions
- Return raw data and amplification plots for centralized analysis
Data Analysis:
- Calculate PCR efficiency for each site using dilution series
- Determine linearity (R²) of standard curves
- Assess limit of detection and quantification across sites
- Compare Cq values for identical samples
Diagram 1: Multicenter PCR assessment workflow for identifying consistency issues across testing sites.
Quantitative Data Analysis from Multicenter Studies
Recent multicenter studies provide valuable quantitative insights into PCR performance variability:
Table 2: Performance Metrics from PCR Multicenter Studies
| Study & Assay | Sample Size | Overall Agreement | Positive Agreement | Negative Agreement | Turnaround Time |
|---|---|---|---|---|---|
| FACILITATE: Idylla EGFR vs. Local Methods [64] | 1,474 parallel tests | 97.7% (95% CI: 96.8–98.3) | 87.4% (95% CI: 81.8–91.4) | 99.2% (95% CI: 98.5–99.6) | ~1 day vs. ~22 days |
| D. fragilis Detection: PCR vs. Microscopy [21] | 100 stool samples | 59.5% agreement (kappa=0.21, fair) | PCR detected 41/100 vs. microscopy 17/100 | N/A | N/A |
| TB Detection: Indigen MTB/DR-TB RT-PCR [69] | 610 sputum specimens | 94.12% sensitivity, 98.32% specificity | 78.57% sensitivity in AFB-negative cases | 98.34% specificity in AFB-negative cases | N/A |
Advanced Technical Guide: Statistical Approaches for PCR Consistency
Statistical Methods for Multicenter PCR Data Analysis
Robust statistical analysis is essential for interpreting multicenter PCR data:
- Multiple Regression Models: Develop models to derive ΔΔCt from estimation of interaction between gene and treatment effects while accounting for center-specific variations [68].
- ANCOVA (Analysis of Covariance): Use ANCOVA models to derive ΔΔCt from analysis of effects of variables across different testing sites [68].
- Poisson Statistics for Digital PCR: Apply Poisson statistics to calculate initial target molecule numbers from positive/negative partitions in digital PCR platforms [67].
- "Dots in Boxes" Quality Scoring: Implement high-throughput data analysis method that captures PCR efficiency, dynamic range, target specificity, and precision as a single data point [66].
MIQE Guideline Implementation for Quality Assurance
The Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines establish critical performance metrics that should be reported to ensure robust assay performance and reproducibility [66]:
- PCR Efficiency: Measure using dilution series of known template concentrations; ideal efficiency is 90-110% [66]
- Dynamic Range: Establish upper and lower quantification limits; should be linear for 3-6 log10 concentrations [66]
- Limit of Detection: Determine the lowest concentration detectable with 95% confidence [66]
- Target Specificity: Confirm through product size, sequencing, or melt curve analysis [66]
- Assay Precision: Assess through multiple replicates; variation increases with decreasing copy number [66]
Diagram 2: Troubleshooting pathway for resolving false negative results in Dientamoeba fragilis PCR detection.
Multicenter studies reveal that PCR assay consistency depends on rigorous standardization, comprehensive quality control measures, and appropriate statistical analysis. The implementation of MIQE guidelines, cross-site validation protocols, and multiple verification methods significantly enhances the reliability of PCR-based detection, particularly for challenging targets like Dientamoeba fragilis. By adopting the troubleshooting guides and protocols outlined in this technical support center, researchers can identify and resolve common sources of variability, ultimately improving the reproducibility and clinical utility of their molecular assays.
The detection of the intestinal protozoan parasite Dientamoeba fragilis presents a significant challenge in clinical and research laboratories. This case study examines a common scenario where initial polymerase chain reaction (PCR) screening results for D. fragilis are discrepant with other diagnostic methods, creating a diagnostic dilemma. We explore how Small Subunit Ribosomal DNA (SSU rDNA) sequencing serves as a definitive confirmatory tool to resolve these discrepancies, with particular focus on addressing false negatives in PCR-based research. The SSU rDNA is a preferred genetic marker for phylogenetic analysis and pathogen identification due to the presence of highly conserved regions across a wide range of organisms alongside highly variable sequences specific to genus or species levels [70]. This property makes it exceptionally valuable for differentiating between closely related species and confirming pathogen identity.
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: Why do we need a confirmatory gold standard when our real-time PCR assays are highly sensitive?
Even highly sensitive real-time PCR (qPCR) assays can yield false positives due to cross-reactivity with non-target organisms. A 2025 study demonstrated that qPCR assays designed for human D. fragilis detection can cross-react with Simplicimonas sp. in cattle specimens, identified through a 9°C cooler melt curve discrepancy [65]. Furthermore, a 2019 comparative study found that a widely used laboratory-developed real-time assay produced multiple false-positive results on multiple PCR platforms when compared to a commercial assay (EasyScreen) and confirmatory sequencing [10]. SSU rDNA sequencing provides definitive identification by analyzing the genetic sequence itself, thereby confirming the presence of D. fragilis and not a cross-reacting organism.
FAQ 2: What is the specific sensitivity limitation of conventional PCR that leads to false negatives?
Conventional PCR is substantially less sensitive than real-time PCR for detecting D. fragilis. A 2010 comparative study found that while real-time PCR detected 35 isolates, conventional PCR detected only 15 out of the same 35 positive samples, yielding a sensitivity of just 42.9% [1]. A 2022 study corroborated this, showing conventional PCR identified 41 positives, while microscopy detected only 13-17 [21]. This high false-negative rate makes conventional PCR suboptimal as a standalone diagnostic method and necessitates a more sensitive confirmatory technique like SSU rDNA sequencing.
FAQ 3: Can't we rely on microscopic examination to confirm PCR results?
Microscopy lacks the sensitivity and specificity required for reliable confirmation. The same 2010 study showed microscopy had a sensitivity of only 34.3% compared to real-time PCR [1]. Microscopic identification relies on examiner expertise, and trophozoites degrade rapidly after sample collection [21]. While culture techniques like Robinson's medium can improve detection over microscopy (identifying 10.6% additional positives in one study), they are still less sensitive than molecular methods and require several days for results [47].
FAQ 4: What steps should we take when SSU rDNA sequencing reveals a false negative in our initial PCR?
When SSU rDNA sequencing identifies a false negative, a systematic troubleshooting approach is essential. First, review the nucleic acid extraction method, as inhibitors in stool samples can affect PCR efficiency. Next, verify the PCR protocol, particularly the number of amplification cycles; a 2025 study recommends reducing cycles to below 40 to minimize non-specific amplification while maintaining sensitivity [65]. Additionally, ensure you are using a high-fidelity DNA polymerase to minimize errors during amplification, as demonstrated in a 2017 study on ciliates which found that low-fidelity polymerases exaggerate sequence variation estimates [71].
Troubleshooting Guide for Discrepant Results
Table 1: Common Discrepancies and Recommended Actions
| Discrepancy Scenario | Potential Causes | Corrective Actions | Confirmatory Step |
|---|---|---|---|
| Positive qPCR but negative culture/microscopy | Higher sensitivity of qPCR; cross-reactivity with non-target organisms | Perform melt curve analysis; check for cross-reacting organisms | SSU rDNA sequencing with specific primers targeting 18S SSU rRNA gene [65] [10] |
| Positive conventional PCR but negative real-time PCR | Lower sensitivity of conventional PCR; primer mismatch | Optimize conventional PCR conditions; use nested PCR if necessary | Confirm with real-time PCR and SSU rDNA sequencing [1] |
| Positive microscopy but negative PCR | PCR inhibition; DNA degradation; low parasite load | Re-extract DNA with inhibition removal steps; concentrate sample | Repeat PCR with internal control; culture in Robinson's medium [47] |
| Discrepant results between different qPCR assays | Variations in primer/probe specificity; different detection limits | Compare assay parameters; use validated commercial assays | SSU rDNA sequencing as arbiter [10] |
Experimental Protocol: SSU rDNA Sequencing for Confirmatory Diagnosis
Objective: To confirm the identity of Dientamoeba fragilis in samples with discrepant PCR results using SSU rDNA sequencing.
Materials and Equipment:
- DNA extracted from stool samples
- Dientamoeba-specific primers (e.g., DF1: 5'-CTCATAATCTACTTGGAACCAATT-3', DF4: 5'-CCCCGATTATTCTCTTTGATATT-3') [21]
- High-fidelity DNA polymerase (e.g., Q5 Hot Start High-Fidelity) [71]
- Thermal cycler
- Agarose gel electrophoresis equipment
- PCR purification kit
- Sequencing facilities
Methodology:
- DNA Extraction: Extract genomic DNA from 150-200 mg of fecal sample using a commercial stool DNA kit (e.g., DNA Stool Mini Kit). Include extraction controls. [21] [65]
- SSU rDNA Amplification: Set up PCR reaction with:
- 1 μL template DNA
- 10 pmoles of each primer (DF1/DF4)
- 12.5 μL of 2X PCR master mix with high-fidelity polymerase
- Nuclease-free water to 25 μL
- Cycling Conditions:
- Initial denaturation: 95°C for 5 minutes
- 35 cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing: 55°C for 1.5 minutes
- Extension: 72°C for 1.5 minutes
- Final extension: 72°C for 5 minutes [21]
- Amplicon Verification: Run 5 μL PCR product on 1% agarose gel. Expected amplicon size: 662 bp.
- Sequencing: Purify PCR products and submit for bidirectional sequencing.
- Sequence Analysis: Compare obtained sequences with reference sequences in genomic databases (GenBank, EMBL) using BLASTN or FASTA algorithms. A similarity score ≥99% confirms D. fragilis identity. [72]
Workflow Visualization
Table 2: Comparison of Diagnostic Methods for D. fragilis Detection [1] [21]
| Diagnostic Method | Sensitivity (%) | Specificity (%) | Number of Positives Detected | Limitations |
|---|---|---|---|---|
| Real-time PCR (qPCR) | 100% | 100% | 35/35 (2010 study) | Potential cross-reactivity with non-target organisms [65] |
| Conventional PCR | 42.9% | 100% | 15/35 (2010 study); 41/100 (2022 study) | High false-negative rate; lower sensitivity [1] [21] |
| Microscopy (Wet Mount) | 34.3% | 99% | 12/35 (2010 study); 13/100 (2022 study) | Rapid trophozoite degeneration; requires expert microscopist [1] [21] |
| Microscopy (Trichrome Stain) | Not specified | Not specified | 17/100 (2022 study) | Improved over wet mount but still less sensitive than PCR [21] |
| Culture (Robinson's Medium) | 40% | 100% | 14/35 (2010 study); 11/104 (2019 study) | Time-consuming (48-96 hours); technically demanding [1] [47] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for D. fragilis Detection and Confirmation
| Reagent/Kit | Specific Function | Application Notes |
|---|---|---|
| High-Fidelity DNA Polymerase (e.g., Q5 Hot Start) | Amplifies target SSU rDNA with minimal errors | Critical for reducing experimental artifacts during PCR; significantly impacts sequence variation estimates [71] |
| Stool DNA Extraction Kit (e.g., QIAamp Fast DNA Stool Mini Kit) | Isolates microbial DNA from complex fecal material | Includes inhibitors removal steps; essential for efficient PCR amplification [65] |
| SSU rDNA Primers (DF1/DF4) | Specifically targets 662-bp region of 18S SSU rRNA gene | Positions 100-123 and 739-761 of SSU rDNA gene; enables specific D. fragilis detection [21] |
| Robinson's Culture Medium | Supports growth of D. fragilis trophozoites | Diphasic xenic medium; useful when PCR unavailable; supplies trophozoites for further studies [47] |
| EasyScreen Enteric Protozoan Detection Kit | Commercial multiplex PCR for protozoan detection | Includes D. fragilis detection; reduced cross-reactivity compared to lab-developed assays [10] |
| SSU rDNA Reference Sequences (e.g., GenBank FJ649228) | Gold standard for sequence comparison | Enables definitive identification through BLAST analysis; ≥99% similarity confirms D. fragilis [1] [72] |
Standard multiplex PCR panels for enteric pathogens represent a significant advancement over traditional microscopy, offering high throughput and improved sensitivity for detecting common protozoan parasites [73]. However, a critical gap exists in their coverage, as several parasites and pathogens remain undetected by these standardized assays. This gap is particularly consequential for the trichomonad parasite Dientamoeba fragilis, a recognized cause of gastrointestinal illness whose detection can be inconsistent across commercial panels [5] [65]. The limitations of these panels, combined with technical challenges in multiplex PCR design, can lead to false-negative results, misdirecting clinical management and obscuring the true prevalence of this pathogen. This technical guide addresses the specific experimental hurdles in D. fragilis PCR research and provides troubleshooting protocols to ensure reliable detection, accurate diagnosis, and robust research outcomes.
Parasites and Pathogens Outside Standard Panels
Standard multiplex PCR panels typically target a core set of six to eight protozoan parasites. The table below summarizes commonly targeted organisms and notable omissions that can lead to diagnostic gaps.
Table 1: Pathogen Coverage of Standard Multiplex PCR Panels
| Pathogen | Typically Included in Standard GI Panels? | Notes / Evidence of Diagnostic Gap |
|---|---|---|
| Giardia duodenalis | Yes [74] [73] | A standard target in validated panels. |
| Cryptosporidium spp. | Yes [74] [73] | A standard target in validated panels. |
| Entamoeba histolytica | Yes [74] [73] | Often requires differentiation from non-pathogenic E. dispar. |
| Dientamoeba fragilis | Yes (in some panels) [74] [73] | Detection can be variable; some assays show cross-reactivity or poor sensitivity [65]. |
| Blastocystis hominis | Yes (in some panels) [74] | Pathogenicity is debated, but included in several commercial assays. |
| Cyclospora cayetanensis | Yes (in some panels) [73] | A standard target in more comprehensive panels. |
| Enterobius vermicularis | No | Specifically identified as only detected by microscopy, not by a multiplex PCR panel [74]. |
| Apathogenic amoebae (e.g., Entamoeba coli) | No | Specifically identified as only detected by microscopy, not by a multiplex PCR panel [74]. |
| Simplicimonas sp. | No | Can cause cross-reactivity in some D. fragilis qPCR assays, leading to false positives if not properly identified [65]. |
| Pentatrichomonas hominis | No | Known to cross-react with the EasyScreen D. fragilis assay, necessitating melt curve analysis for discrimination [65]. |
Troubleshooting False Negatives inDientamoeba fragilisPCR
The challenge of false negatives is a central concern in D. fragilis research. The following FAQs address the most common issues and their solutions.
FAQ 1: Our PCR results forD. fragilisare negative, but clinical symptoms and microscopy are suggestive of infection. What could be causing this?
False negatives in PCR can arise from several factors related to sample integrity, assay design, and laboratory technique.
Probable Cause A: Suboptimal Sample Collection and Storage
- Issue: D. fragilis trophozoites are notoriously fragile and degrade rapidly after defecation [21]. Using preserved stool is critical for reliable microscopy, and this degradation can also impact DNA yield for PCR.
- Solution: For PCR, collect fresh stool and freeze immediately at -20°C or lower until DNA extraction [21] [9]. While PCR is more robust than microscopy for slightly degraded samples, prompt stabilization is still considered best practice.
Probable Cause B: Sequence Variation in Primer Binding Sites
- Issue: Genetic variation in D. fragilis strains can lead to mismatches between the parasite's DNA and the primers/probes used in the assay. This prevents hybridization and amplification, resulting in a false negative [30].
- Solution: If using an in-house PCR assay, verify that your primer sequences are specific to conserved regions of the D. fragilis genome, such as the small subunit ribosomal RNA (SSU rRNA) gene [21] [9]. For commercial kits, consult the manufacturer for information on known genetic variants.
Probable Cause C: PCR Inhibition
- Issue: Stool samples contain complex mixtures of substances that can inhibit the DNA polymerase enzyme, preventing the PCR reaction from proceeding efficiently.
- Solution: Always include an internal control in your PCR reactions. This control will fail to amplify in inhibited samples, alerting you to the problem. Diluting the DNA template (e.g., 1:5 or 1:10) can often overcome inhibition [65].
FAQ 2: How can I validate the sensitivity and specificity of myD. fragilisPCR assay?
A rigorous validation is essential to ensure your results are trustworthy.
- Experimental Protocol: Assay Validation
- Sample Selection: Obtain a panel of well-characterized samples. This should include microscopy-positive samples for D. fragilis and other common parasites (e.g., Giardia, Blastocystis, Entamoeba) to test specificity [21].
- DNA Extraction: Use a commercial DNA extraction kit designed for stool samples, such as the QIAamp Fast DNA Stool Mini Kit, which includes steps to remove PCR inhibitors [65].
- PCR Amplification: Perform the PCR using your chosen assay. A conventional PCR targeting a 662-bp fragment of the SSU rRNA gene has been successfully used with high sensitivity (93.5%) and specificity (100%) [21] [9].
- Confirmation: Confirm the identity of PCR products by Sanger sequencing. This is the gold standard for verifying that the amplified DNA is indeed from D. fragilis and not a cross-reacting organism [65].
FAQ 3: We are developing a custom multiplex PCR. What are the key design challenges for includingD. fragilis?
Designing a robust multiplex PCR is complex, and failure to account for these factors is a major source of false negatives.
Challenge A: Primer Dimerization and Off-Target Amplification
- Issue: In a multiplex reaction with many primers, they can bind to each other (forming primer dimers) or to non-target sequences. This depletes reagents (dNTPs, primers, enzyme) and can outcompete the amplification of the true D. fragilis target [30].
- Solution: Use specialized software (e.g., PrimerPlex, DNA Software tools) to screen all primer pairs for cross-homology and dimerization potential [30] [75]. This analysis is not feasible manually for a large multiplex set.
Challenge B: Uneven Amplification Efficiency
- Issue: In a multiplex reaction, some targets (amplicons) amplify more efficiently than others. If the D. fragilis assay is less efficient, its signal may be weak or absent, especially in samples with low parasite load.
- Solution: Meticulously optimize primer concentrations and annealing temperatures. The goal is to "balance" the reaction so that all targets amplify with similar efficiency. This requires extensive empirical testing with control samples [30].
Diagram 1: False Negative Troubleshooting Path
Advanced Considerations for Research-Grade Detection
Addressing Cross-Reactivity and False Positives
While false negatives are a primary focus, false positives can also confound research. When applying human-derived qPCR assays to animal samples to investigate zoonotic transmission, significant cross-reactivity can occur.
- Evidence: One study found that a qPCR assay detecting D. fragilis in cattle was actually cross-reacting with a different parasite, Simplicimonas sp. This was identified because the melt curve temperature of the PCR product was 9°C cooler than that of true D. fragilis [65].
- Best Practice: Always perform and analyze melt curves post-qPCR when using assays on new sample types. Any deviation from the expected melt temperature should be investigated via DNA sequencing to confirm the organism's identity [65].
The Critical Role of Multiplex PCR Design
The fundamental technical hurdles of multiplex PCR directly contribute to diagnostic gaps and false negatives.
Table 2: Multiplex PCR Design Problems and Solutions
| Problem | Impact on Results | Solution |
|---|---|---|
| Target Secondary Structure [30] | Primer cannot bind to its target site, causing false negatives. | Use sophisticated prediction software (N-state model) to model DNA folding and select accessible primer binding sites. |
| Primer Dimer Formation [30] [75] | Depletes reagents, reduces overall yield, and can cause false negatives for low-abundance targets. | Software-aided primer design to check for self- and cross-complementarity between all primers in the pool. |
| Primer-Amplicon Interactions [30] | A primer from one assay binds to and extends off an amplicon from another, producing short, non-specific products and depleting primers. | A more subtle problem requiring advanced software to predict interactions across the entire panel. |
| Variable Primer Tm [75] | Primers with different melting temperatures will not hybridize efficiently at a single annealing temperature, leading to uneven or failed amplification. | Design all primers to have a similar Tm (e.g., 55-60°C, with <5°C variation within the pool). |
Diagram 2: Multiplex PCR Assay Development Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Dientamoeba fragilis PCR Research
| Reagent / Kit | Function | Example / Note |
|---|---|---|
| DNA Extraction Kit | Purifies microbial and host DNA from complex stool matrix while removing PCR inhibitors. | QIAamp Fast DNA Stool Mini Kit (Qiagen) [65]. |
| PCR Primers | Specifically targets and amplifies a unique D. fragilis gene sequence. | DF1/DF4 primers targeting the SSU rRNA gene [21]. |
| PCR Master Mix | Contains DNA polymerase, dNTPs, and buffer optimized for efficient amplification. | MyTaq Red Mix (Bioline) or similar [21]. Include an internal control. |
| Automated Platform | For high-throughput, consistent nucleic acid extraction and PCR setup. | Hamilton STARlet with Seegene STARMag kits [73]. |
| Positive Control DNA | Essential for validating each PCR run and confirming assay sensitivity. | DNA from a confirmed D. fragilis-positive sample or a cloned plasmid [21]. |
| Sequencing Service | Confirms the identity of PCR amplicons and investigates cross-reactivity. | Used to distinguish D. fragilis from Simplicimonas sp. [65]. |
Conclusion
Addressing false negatives in Dientamoeba fragilis PCR requires a multifaceted strategy that moves beyond reliance on a single diagnostic method. The integration of advanced techniques, such as meticulous melt curve analysis and rigorous assay validation, is paramount for distinguishing true infections from cross-reactivity, as evidenced by findings of Simplicimonas sp. in cattle. Furthermore, standardizing DNA extraction protocols and implementing a judicious PCR cycle threshold are critical technical adjustments that enhance reliability. For the research and drug development community, future directions must include the development of even more robust and standardized PCR assays, a deeper investigation into the genomic diversity of D. fragilis, and the establishment of a consensus multi-method diagnostic algorithm. Such advancements will not only improve diagnostic accuracy but also solidify the foundation of high-quality epidemiological and pathogenicity studies essential for public health.
References
- 1. Comparison of microscopy, two xenic culture techniques , conventional... [https://link.springer.com/article/10.1007/s10096-010-0876-4]
- 2. (PDF) Real Time PCR for Dientamoeba : a comparison... fragilis [https://www.academia.edu/144360554/Real_Time_PCR_for_Dientamoeba_fragilis_a_comparison_between_molecular_and_microscopical_approach]
- 3. Development, Optimisation and Validation of a Novel Multiplex... [https://pubmed.ncbi.nlm.nih.gov/36365028/]
- 4. No evidence of pathogenicity of Dientamoeba following... fragilis [https://pmc.ncbi.nlm.nih.gov/articles/PMC11271704/]
- 5. A clinical guideline on Dientamoeba fragilis infections | Parasitology | Cambridge Core [https://www.cambridge.org/core/journals/parasitology/article/clinical-guideline-on-dientamoeba-fragilis-infections/D369D9EB36DEBE7C941F0006E4AFAF0A]
- 6. Should Dientamoeba fragillis be looked for in pediatric digestive... [https://www.elsevier.es/es-revista-enfermedades-infecciosas-microbiologia-clinica-english-428-articulo-should-dientamoeba-fragillis-be-looked-S2529993X22001885]
- 7. Diagnostic dilemma: application of real-time PCR assays for the detection of Dientamoeba fragilis in medical and veterinary specimens | Parasites & Vectors | Full Text [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06730-1]
- 8. Dientamoeba fragilis - Certest Biotec - Raw Materials | Diagnostics | Pharma [https://www.certest.es/products/dientamoeba-fragilis-qpcr/]
- 9. Detection of Dientamoeba fragilis in fresh stool specimens using PCR - PubMed [https://pubmed.ncbi.nlm.nih.gov/15619516/]
- 10. Comparison and Recommendations for Use of Dientamoeba fragilis Real-Time PCR Assays - PubMed [https://pubmed.ncbi.nlm.nih.gov/30814263/]
- 11. : An emerging pathogen | Enfermedades... Dientamoeba fragilis [https://www.elsevier.es/es-revista-enfermedades-infecciosas-microbiologia-clinica-english-428-resumen-dientamoeba-fragilis-an-emerging-pathogen-S2529993X25000838]
- 12. : A harmless commensal or a mild pathogen? Dientamoeba fragilis [https://pmc.ncbi.nlm.nih.gov/articles/PMC2851273/]
- 13. Detection and Transmission of Dientamoeba fragilis from Environmental and Household Samples - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3269272/]
- 14. Real-time PCR for the detection of Dientamoeba fragilis in fecal samples - PubMed [https://pubmed.ncbi.nlm.nih.gov/17587544/]
- 15. Evaluation of two DNA extraction methods for the PCR-based detection of eukaryotic enteric pathogens in fecal samples - PubMed [https://pubmed.ncbi.nlm.nih.gov/29587846/]
- 16. DNA of Dientamoeba fragilis detected within surface-sterilized eggs of Enterobius vermicularis - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0014489412003207]
- 17. Direct amplification and genotyping of Dientamoeba fragilis from human stool specimens - PubMed [https://pubmed.ncbi.nlm.nih.gov/14766828/]
- 18. , the Neglected Trichomonad of the Human... Dientamoeba fragilis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4861990/]
- 19. Detection of Dientamoeba fragilis in fresh stool specimens using PCR - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0020751904001936]
- 20. Parasite load as a marker of pathogenicity in Dientamoeba fragilis infections - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11957650/]
- 21. Evaluation of microscopy and PCR for detection of Dientamoeba ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9832490/]
- 22. Comparison and Recommendations for Use of Dientamoeba fragilis Real-Time PCR Assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6498029/]
- 23. (PDF) Real-time PCR for the detection of Dientamoeba in... fragilis [https://www.academia.edu/17291816/Real_time_PCR_for_the_detection_of_Dientamoeba_fragilis_in_fecal_samples]
- 24. False-positive and false-negative COVID-19 cases: respiratory prevention and management strategies, vaccination, and further perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8074645/]
- 25. Troubleshooting your PCR [https://www.takarabio.com/learning-centers/pcr/faq/troubleshooting]
- 26. Preventing False Positive and False Negative PCR Results | Today's Clinical Lab [https://www.clinicallab.com/preventing-false-positive-and-false-negative-pcr-results-26261]
- 27. Detection of small amounts of human adenoviruses in stools ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7162227/]
- 28. neb.com/en/tools-and-resources/ troubleshooting - guides / pcr ... [https://www.neb.com/en/tools-and-resources/troubleshooting-guides/pcr-troubleshooting-guide]
- 29. The clinical significance of Dientamoeba and Blastocystis in... fragilis [https://pubmed.ncbi.nlm.nih.gov/37689266/]
- 30. The Four Most Common Problems in Multiplex ... | DNA Software pcr [https://www.dnasoftware.com/common-problems-in-multiplex-panel-design/]
- 31. Multiplex PCR: Optimization and Application in Diagnostic Virology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC88949/]
- 32. Sample Preparation Troubleshooting in Issues Multiplex PCR [https://www.linkedin.com/advice/0/how-do-you-troubleshoot-sample-preparation-issues]
- 33. Do More with Less: Five Steps to Great Results Using One-Step Multiplex RT-qPCR [https://www.bioradiations.com/do-more-with-less-five-steps-to-great-results-using-one-step-multiplex-rt-qpcr/]
- 34. of Four Comparison Screening Assays for the Detection... Commercial [https://pmc.ncbi.nlm.nih.gov/articles/PMC6956118/]
- 35. of two Comparison assays for the... commercial multiplex PCR [https://www.jidc.org/index.php/journal/article/view/35298429]
- 36. Multiplex PCR: critical parameters and step-by-step protocol - PubMed [https://pubmed.ncbi.nlm.nih.gov/9298224/]
- 37. A Pipeline for Faecal Host DNA Analysis by Absolute Quantification of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6447604/]
- 38. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/dnaextraction.html]
- 39. Optimizing Forensic DNA : Extraction for Trace and... Best Practices [https://blog.invitek.com/articles/lifescience/optimizing-forensic-dna-extraction-best-practices-for-trace-and-degraded-evidence]
- 40. Guide: Mastering 7 Essential Sample Types DNA Extraction [https://www.thermofisher.com/blog/life-in-the-lab/dna-extraction-guide-mastering-7-essential-sample-types/]
- 41. Diagnostic dilemma: application of real-time PCR assays for the... [https://pubmed.ncbi.nlm.nih.gov/40055708/]
- 42. Why Does Your Melt Look So Strange? Curve [https://www.yeasenbio.com/blogs/molecular-biology/why-does-your-melt-curve-look-so-strange]
- 43. Explaining multiple peaks in qPCR melt | IDT curve analysis [https://www.idtdna.com/page/support-and-education/decoded-plus/interpreting-melt-curves-an-indicator-not-a-diagnosis/]
- 44. Direct Amplification and Genotyping of Dientamoeba fragilis from Human Stool Specimens - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC344490/]
- 45. : An emerging pathogen | Enfermedades... Dientamoeba fragilis [https://www.elsevier.es/es-revista-enfermedades-infecciosas-microbiologia-clinica-28-articulo-dientamoeba-fragilis-an-emerging-pathogen-S0213005X24003069]
- 46. Dynamic time warping assessment of high-resolution melt curves provides a robust metric for fungal identification | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0173320]
- 47. The effectiveness of the Culture for Dientamoeba fragilis from the Stool [https://www.idcmjournal.org/choosing-culture-for-dientamoeba-fragilis-detection-in-stool-when-pcr-is-not-available-assessment-of-its-efficacy-and-comparison-of-three-culture-media]
- 48. PCR Troubleshooting Guide | GenScript [https://www.genscript.com/pcr-troubleshooting-guide.html]
- 49. Emerging from Obscurity: Biological, Clinical, and Diagnostic Aspects of Dientamoeba fragilis - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC452553/]
- 50. Newly defined conditions for the in vitro cultivation and cryopreservation of Dientamoeba fragilis: new techniques set to fast track molecular studies on this organism - PubMed [https://pubmed.ncbi.nlm.nih.gov/20609278/]
- 51. Development, Optimisation and Validation of a Novel Multiplex... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9693193/]
- 52. [ Dientamoeba infection in patients with gastrointestinal system... fragilis [https://pubmed.ncbi.nlm.nih.gov/29933734/]
- 53. Multicolor Combinatorial Probe Coding for Real-Time PCR - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3021529/]
- 54. in qPCR, dPCR and MPS—mechanisms and solutions... PCR inhibition [https://pmc.ncbi.nlm.nih.gov/articles/PMC7072044/]
- 55. Evaluation of Inhibitor -Resistant Real-Time PCR for... Methods [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0073845]
- 56. Inhibition Controls for Qualitative Real-Time PCR Assays: Are They Necessary for All Specimen Matrices? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4042775/]
- 57. mechanisms in forensic DNA analysis - Lund University PCR inhibition [https://portal.research.lu.se/en/publications/pcr-inhibition-mechanisms-in-forensic-dna-analysis/]
- 58. Comparison of microscopy, two xenic culture techniques, conventional... [https://pubmed.ncbi.nlm.nih.gov/20155433/]
- 59. Diversity profiling of xenic cultures of Dientamoeba fragilis following systematic antibiotic treatment and prospects for genome sequencing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10317699/]
- 60. No evidence of pathogenicity of Dientamoeba following... fragilis [https://pubmed.ncbi.nlm.nih.gov/39052010/]
- 61. Real-time PCR for the detection of Dientamoeba fragilis in fecal samples - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S089085080700045X]
- 62. Dientamoeba fragilis laboratory diagnosis – Genetic Signatures USA [https://geneticsignatures.com/us/our-products/gastrointestinal-infections/d-fragilis-laboratory-diagnosis/]
- 63. sciencedirect.com/topics/immunology-and-microbiology/ dientamoeba ... [https://www.sciencedirect.com/topics/immunology-and-microbiology/dientamoeba-fragilis]
- 64. FACILITATE: A real - world , multicenter , prospective study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9927408/]
- 65. Diagnostic dilemma: application of real-time PCR assays for the... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11889766/]
- 66. High-Throughput Data Analysis for qPCR | NEB | NEB [https://www.neb.com/en-us/tools-and-resources/feature-articles/development-of-a-high-throughput-data-analysis-method-for-quantitative-real-time-pcr]
- 67. Measuring Digital PCR Quality: Performance Parameters and Their Optimization | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0153317]
- 68. Statistical analysis of real-time PCR data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1395339/]
- 69. Frontiers | Evaluation of a real -time PCR performance to detect... assay [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1372647/full]
- 70. Small Subunit Ribosomal RNA - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/small-subunit-ribosomal-rna]
- 71. Disentangling sources of variation in SSU rDNA sequences from single cell analyses of ciliates: impact of copy number variation and experimental error - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5543213/]
- 72. Comparison of Conventional and Molecular Methods for Identification of Aerobic Catalase-Negative Gram-Positive Cocci in the Clinical Laboratory - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC404636/]
- 73. Validation of an Automated High-Throughput Multiplex Real-Time PCR Assay for Detection of Enteric Protozoa [https://www.mdpi.com/2673-947X/5/1/8]
- 74. Evaluation of the Roche LightMix Gastro parasites multiplex PCR assay detecting Giardia duodenalis, Entamoeba histolytica, cryptosporidia, Dientamoeba fragilis, and Blastocystis hominis - PubMed [https://pubmed.ncbi.nlm.nih.gov/29581055/]
- 75. Multiplex PCR: An overview of multiplex PCR assay, primer design for multiplexing, primer design software for multiplex PCR. [http://www.premierbiosoft.com/tech_notes/multiplex-pcr.html]