Multicentre Study Validation of Parasitology Diagnostic Methods: From Traditional Microscopy to Molecular Assays and AI
This article synthesizes findings from recent multicentre studies to provide a comprehensive framework for the validation of parasitology diagnostic methods.
Multicentre Study Validation of Parasitology Diagnostic Methods: From Traditional Microscopy to Molecular Assays and AI
Abstract
This article synthesizes findings from recent multicentre studies to provide a comprehensive framework for the validation of parasitology diagnostic methods. Aimed at researchers, scientists, and drug development professionals, it explores the foundational principles of multicentre study design, details the application of both established and novel diagnostic techniques—including rapid tests, multiplex PCR, and automated image analysis—and addresses critical troubleshooting and quality assurance measures. Finally, it presents a comparative analysis of method performance, highlighting validation metrics and the evolving role of molecular and AI-driven diagnostics in achieving accurate, reliable, and standardized parasite detection in both endemic and non-endemic settings.
The Critical Role and Design of Multicentre Studies in Parasitology
The diagnosis of parasitic infections represents a formidable challenge in clinical laboratories worldwide. For decades, microscopic examination has remained the cornerstone of diagnosis, particularly for gastrointestinal parasites, despite being labor-intensive, time-consuming, and requiring a high level of expertise for accurate interpretation [1] [2]. The limitations of conventional methods are compounded by their inadequate sensitivity and specificity, especially for detecting low levels of infection or differentiating between morphologically similar species, such as pathogenic Entamoeba histolytica and non-pathogenic Entamoeba dispar [3] [4]. These diagnostic shortcomings have significant implications for patient management, public health surveillance, and the accurate assessment of disease burden.
In recent years, innovative diagnostic technologies have emerged, including sophisticated molecular methods such as real-time PCR and multiplexed nucleic acid amplification tests [5] [3]. While these promise enhanced sensitivity and specificity, their transition from development to routine clinical use requires robust validation. It is within this context that multicentre studies have become indispensable, providing the comprehensive evidence base needed to ensure diagnostic tests perform reliably across diverse populations, sample types, and laboratory environments. This guide explores the critical role of multicentre studies through the lens of parasitology diagnostics, comparing commercial assays and presenting experimental data that underscores why single-centre evaluations are insufficient for definitive diagnostic validation.
The Performance Landscape: Comparing Diagnostic Methods
The evolution from traditional to molecular methods represents a paradigm shift in parasitology diagnostics. The table below summarizes the core characteristics, advantages, and limitations of the primary diagnostic approaches.
Table 1: Comparison of Major Diagnostic Methods for Intestinal Protozoa
| Method Category | Examples | Key Advantages | Key Limitations |
|---|---|---|---|
| Traditional Microscopy | Direct smear, concentration techniques, staining (Giemsa, Trichrome) [3] [4] | Low cost; can detect a wide range of parasites [4] | Labor-intensive; requires expert personnel; low sensitivity; cannot differentiate some species [3] [4] |
| Immunological Assays | Immunochromatographic tests, ELISA [5] [4] | Rapid results; easier to perform than microscopy [4] | Variable performance; false positives/negatives occur; often requires confirmatory testing [6] [3] |
| Molecular Methods (PCR) | Singleplex & multiplex real-time PCR (e.g., Allplex, AusDiagnostics) [3] [4] | High sensitivity & specificity; species differentiation; automation-friendly [5] [3] | Requires specialized equipment; challenging DNA extraction; higher cost per test [4] |
The Crucial Data: Multicentre Performance of Molecular Assays
Multicentre studies provide the most realistic assessment of a diagnostic assay's real-world performance. The following table consolidates quantitative findings from recent Italian multicentre studies that evaluated two commercial PCR assays against traditional methods.
Table 2: Performance Metrics of Commercial PCR Assays from Multicentre Studies
| Parasite | Commercial Assay | Sensitivity (%) | Specificity (%) | Study Details |
|---|---|---|---|---|
| Entamoeba histolytica | Allplex GI-Parasite [3] | 100 | 100 | 368 samples, 12 labs |
| Giardia duodenalis | Allplex GI-Parasite [3] | 100 | 99.2 | 368 samples, 12 labs |
| Cryptosporidium spp. | Allplex GI-Parasite [3] | 100 | 99.7 | 368 samples, 12 labs |
| Dientamoeba fragilis | Allplex GI-Parasite [3] | 97.2 | 100 | 368 samples, 12 labs |
| Giardia duodenalis | AusDiagnostics [4] | High (specific value not given) | High (specific value not given) | 355 samples, 18 labs |
| Cryptosporidium spp. | AusDiagnostics [4] | High but limited by DNA extraction | High | 355 samples, 18 labs |
The data from these independent, multi-laboratory evaluations provide a strong foundation for laboratories to make informed procurement and implementation decisions. The near-perfect sensitivity and specificity of the Allplex assay for key pathogens demonstrate the maturity achievable by well-validated molecular tests [3]. Furthermore, the AusDiagnostics study highlights a critical function of multicentre trials: identifying non-assay related technical challenges, such as suboptimal DNA extraction protocols that can impede the detection of tough-walled parasites like Cryptosporidium and Dientamoeba fragilis [4].
Inside the Multicentre Study: Experimental Protocols and workflows
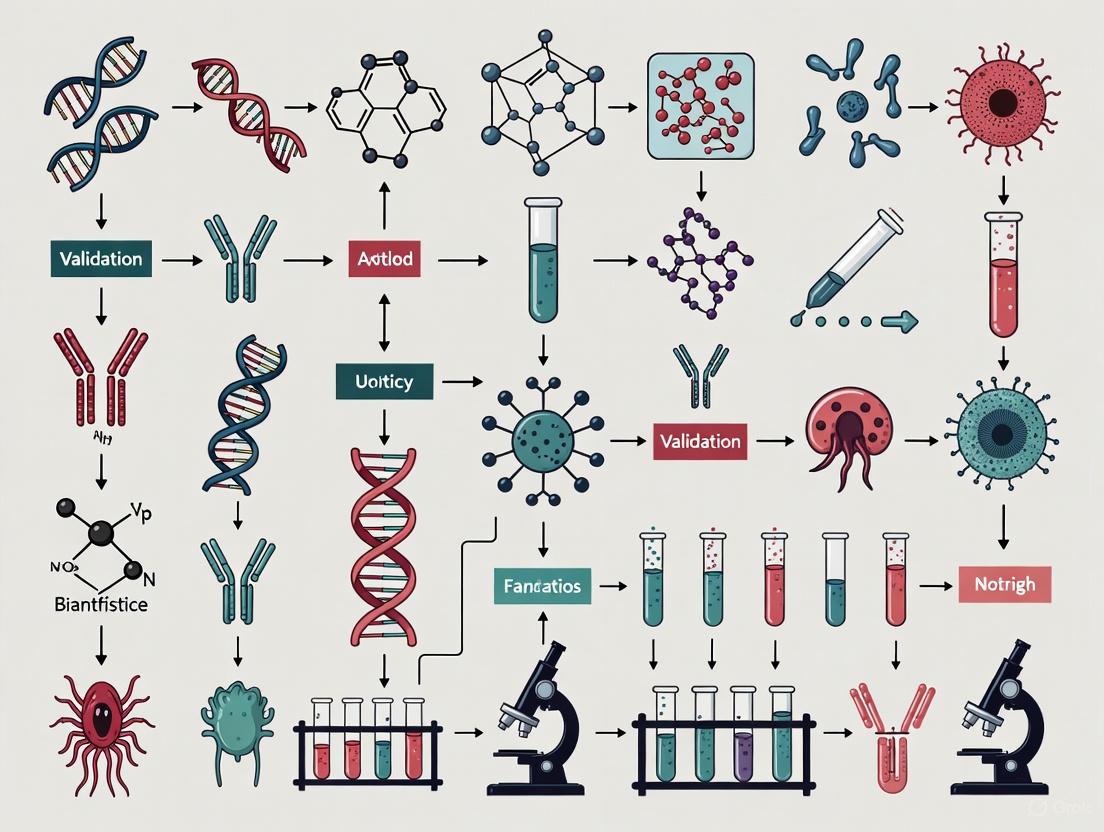
Understanding the design and execution of a multicentre study is key to appreciating its validating power. The following workflow illustrates the general structure of such a study, as seen in the evaluated research.
Diagram 1: Multicentre Validation Workflow
Detailed Experimental Protocol
The multicentre study evaluating the Allplex GI-Parasite Assay serves as a model for rigorous diagnostic validation. The methodology can be broken down into several critical phases [3] [7]:
Study Design and Sample Collection: Twelve laboratories across Italy participated, collecting 368 stool samples from patients suspected of enteric parasitic infection during routine diagnostics. This prospective collection ensures the sample population reflects the real-world clinical scenario in which the test will be used.
Reference Method Testing: Each sample was first examined using a battery of conventional techniques as a reference standard. This included:
- Macroscopic and microscopic examination after concentration.
- Staining with Giemsa or Trichrome stain.
- Antigen research for Giardia duodenalis, Entamoeba histolytica/dispar, and Cryptosporidium spp.
- Amoebae culture. This multi-faceted reference approach mitigates the limitations of any single traditional method.
Index Method Testing (Molecular Assay): Samples were stored frozen and later shipped to a central laboratory for batched testing with the index method, the Allplex GI-Parasite Assay, to ensure consistency.
- DNA Extraction: Approximately 50-100 mg of stool was lysed, and nucleic acids were extracted using the Microlab Nimbus IVD system, an automated platform for standardized processing [3].
- PCR Amplification and Detection: DNA extracts were amplified using the one-step real-time PCR multiplex kit on a CFX96 Real-Time PCR instrument. Results were interpreted automatically using Seegene Viewer software, with a Ct value of <45 defined as positive.
Data Analysis and Discrepancy Resolution: Sensitivity and specificity were calculated against the composite reference method. In cases of discrepant results between PCR and traditional methods, samples were retested by both methods to confirm the final classification, a process that strengthens the validity of the final performance metrics.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The successful execution of a multicentre study, and the subsequent deployment of any validated diagnostic assay, relies on a suite of essential reagents and instruments.
Table 3: Key Research Reagent Solutions for Molecular Parasitology Diagnostics
| Tool / Reagent | Specific Example | Function in the Workflow |
|---|---|---|
| Automated Nucleic Acid Extractor | Microlab Nimbus IVD System [3] | Standardizes and automates the critical DNA extraction step, reducing human error and variability between labs. |
| Extraction Kit | Lysis Buffers (e.g., ASL Buffer from Qiagen) [3] | Breaks down the tough (oo)cyst walls of parasites and stabilizes nucleic acids for extraction. |
| Multiplex Real-Time PCR Assay | Allplex GI-Parasite Assay [3] | Simultaneously detects and differentiates multiple parasite targets in a single reaction, saving time and sample. |
| Real-Time PCR Instrument | CFX96 Real-Time PCR (Bio-Rad) [3] | Amplifies target DNA and monitors fluorescence in real-time, providing quantitative and qualitative results. |
| Result Analysis Software | Seegene Viewer Software [3] | Automates the interpretation of complex multiplex PCR data, standardizing call rates across operators. |
The Evolution of Diagnostic Validation
The transition from single-center to multicentre validation represents a necessary evolution in the pathway from a novel diagnostic concept to a clinically trusted tool. The following diagram maps this progression and its impact on diagnostic reliability.
Diagram 2: Diagnostic Validation Pathway
This pathway underscores that multicentre studies are not merely a final checkmark but an integral phase that stress-tests an assay against the very variables that can lead to failure in clinical practice. These variables include differences in operator skill, the diversity of sample types and storage conditions across collection sites, and the use of various instrument models [1] [4]. The 2025 study by BioMed Central highlights this perfectly, revealing how DNA extraction efficiency from fixed versus fresh stool samples can significantly impact the sensitivity of detecting parasites like D. fragilis [4]—a finding only possible through a multicentre design with varied sample handling practices.
The evidence is clear: multicentre studies are not merely beneficial but essential for diagnostic validation in parasitology. They provide the rigorous, generalized evidence that moves a diagnostic assay from a promising prototype to a trusted clinical tool. As the field continues to advance with more complex molecular panels, biosensors, and AI-driven diagnostics [5], the principles of multicentre validation will become even more critical. They are the definitive mechanism for ensuring that new technologies truly meet the needs of diverse patient populations and healthcare systems, ultimately fulfilling the promise of improved patient care and public health outcomes.
Core Components of a Robust Multicentre Study Protocol
Multicentre studies are fundamental for the validation of diagnostic methods in parasitology, providing the statistical power and generalizability required for clinical implementation. This guide details the core components of a robust multicentre study protocol, objectively comparing the performance of various diagnostic platforms—including serological assays, conventional microscopy, and molecular techniques—based on recent experimental data. Framed within the broader context of method validation, this analysis provides parasitology researchers, scientists, and drug development professionals with a structured framework for designing, executing, and interpreting multicentre evaluations.
The validation of diagnostic methods for parasitic diseases, such as Chagas disease and intestinal protozoal infections, presents significant challenges due to variations in pathogen prevalence, operator expertise, and regional infrastructure. Multicentre studies address these challenges by evaluating diagnostic performance across multiple laboratories and patient populations, ensuring results are reproducible, reliable, and applicable in diverse clinical settings [8]. Such studies are crucial for transitioning promising diagnostic tools from research laboratories into widespread clinical use, ultimately improving the detection and management of neglected tropical diseases.
For parasitology, where "the diagnostic process... is complex, requiring clinical evaluation, epidemiological data, and laboratory testing" [8], multicentre validation provides the evidence base needed to establish standardized diagnostic guidelines. These studies are particularly important given that parasitic infections are often underdiagnosed; for Chagas disease, for instance, "only 7% of T. cruzi-infected individuals are diagnosed, and fewer than 1% receive etiological treatment" [8].
Core Methodological Components of a Multicentre Study
A robust multicentre study protocol in parasitology must incorporate several key components to ensure scientific validity and operational feasibility across participating sites.
Ethical Compliance and Sample Management
The foundational element of any clinical study is ethical governance. All participating institutions must obtain approval from their respective Institutional Review Boards (IRBs) or Ethics Committees, often requiring harmonization of protocols across sites [8] [3]. Patient data should be anonymized to maintain confidentiality, and the requirement for informed consent must be clearly addressed, with waivers obtained where appropriate for retrospective studies.
Sample collection and management require meticulous planning. The sample size must be calculated a priori using statistical software to achieve sufficient power, typically accounting for expected sensitivity and specificity with a defined confidence level and absolute error [8]. For multicentre studies on intestinal protozoa, samples are often collected during routine diagnostic procedures across participating laboratories, then stored frozen at -20°C or -80°C until batch analysis to preserve analyte integrity [3] [4]. The number of samples should meet minimum statistical requirements; for example, one Chagas disease study utilized 170 samples (111 positive and 59 negative) to ensure adequate power [8].
Laboratory Network and Standardization
Selecting participating laboratories that represent different geographical regions enhances the generalizability of findings. Studies often include laboratories from northern, central, and southern regions of a country to capture potential regional variations [3] [4]. To minimize inter-laboratory variability, all sites should adhere to Good Laboratory Practices and utilize the same batch of diagnostic kits distributed from a central location [8].
Standardized testing protocols are critical. For molecular studies, this includes using identical nucleic acid extraction systems, such as the MagNA Pure 96 System [4] or the Microlab Nimbus IVD system [3], and the same PCR platforms and cycling conditions across all participating sites. For serological studies, the same commercial kits from identical batches should be used at all testing sites [8].
Reference Standards and Statistical Analysis
Defining an appropriate reference standard is essential for evaluating new diagnostic methods. For parasitology studies, this typically involves comparison against conventional techniques considered the gold standard, such as "microscopic examination of stool samples" for intestinal protozoa [3] or a combination of serological techniques for Chagas disease [8].
Statistical analysis should include calculations of sensitivity, specificity, positive predictive value, and negative predictive value. Inter-rater reliability between different methods and laboratories is often assessed using kappa statistics, with values interpreted as follows: 0.01-0.20 (slight agreement), 0.21-0.40 (fair agreement), 0.41-0.60 (moderate agreement), 0.61-0.80 (substantial agreement), and 0.81-1.00 (perfect agreement) [3]. For molecular method validation, analysis of crossing threshold (Ct) values and establishment of clear positivity criteria (e.g., Ct <45) are essential components [3].
Table 1: Core Components of a Multicentre Study Protocol in Parasitology
| Component | Description | Implementation Example |
|---|---|---|
| Ethical Framework | IRB approvals from all participating sites | Multi-site approval with waived consent for anonymized samples [8] |
| Sample Size Calculation | Statistical determination of minimum samples needed | OpenEpi software with 2% absolute error, 95% CI [8] |
| Laboratory Network | Geographically diverse sites following standardized protocols | 12 Italian laboratories representing different regions [3] |
| Reference Standard | Established method against which new tests are compared | Microscopy, antigen tests, and culture for intestinal protozoa [3] |
| Blinded Testing | Concealment of sample status from evaluators | Use of blind-coded samples in validation studies [9] |
| Data Management | Centralized collection and statistical analysis | Descriptive statistics, sensitivity/specificity calculations, kappa values [3] |
Comparative Performance of Diagnostic Platforms
Recent multicentre studies have generated robust comparative data on various diagnostic platforms for parasitic diseases. The performance of these methods varies significantly, informing evidence-based selection for different clinical and resource settings.
Serological Assays for Chagas Disease
A comprehensive evaluation of 17 serological assays for detecting anti-T. cruzi antibodies revealed substantial variation in performance across platforms. Enzyme immunoassays (EIA) demonstrated high sensitivity, with some achieving 100% sensitivity, while chemiluminescent microparticle immunoassay (CMIA) also exhibited 100% sensitivity, highlighting its potential as a robust screening tool [8].
In contrast, indirect haemagglutination assays (IHA) and indirect immunofluorescence assays (IIF) demonstrated reduced specificity, with cross-reactivity with other parasitic diseases posing challenges to specificity, particularly in assays employing crude antigens [8]. The combination of different assay types improved overall sensitivity, often surpassing 99%, although specificity remained variable [8].
Table 2: Performance of Serological Assays for Chagas Disease Detection [8]
| Assay Type | Examples | Sensitivity | Specificity | Notes |
|---|---|---|---|---|
| Enzyme Immunoassay (EIA) | Biolisa Chagas Recombinante, Chagatest ELISA recombinante | Up to 100% | Variable | High sensitivity, performance varies by antigen |
| Chemiluminescent Microparticle Immunoassay (CMIA) | Architect Chagas | 100% | High | Robust screening tool |
| Indirect Haemagglutination (IHA) | Chagatest HAI screening, Chagas-HAI | Reduced | Reduced | Specificity challenges |
| Indirect Immunofluorescence (IIF) | Chagas IFA IgG+IgM, Imuno-Con Chagas | Reduced | Reduced | Cross-reactivity issues |
| Rapid Diagnostic Tests (RDT) | OnSite Chagas Ab Combo, SD Bioline Chagas AB | Variable | Variable | Convenient but variable performance |
Molecular Methods vs. Conventional Techniques for Intestinal Protozoa
Molecular diagnostic technologies, particularly real-time PCR (RT-PCR), are gaining traction in non-endemic areas characterized by low parasitic prevalence owing to their enhanced sensitivity and specificity [4]. Multicentre comparisons between conventional microscopy and molecular methods have demonstrated the superior performance of PCR-based approaches for detecting major intestinal protozoa.
For Giardia duodenalis, both commercial and in-house PCR methods demonstrate "high sensitivity and specificity, similar to those of conventional microscopy" [4]. For Cryptosporidium spp. and Dientamoeba fragilis detection, molecular methods showed "high specificity but limited sensitivity, likely due to inadequate DNA extraction from the parasite" [4]. Molecular assays seem to be particularly critical for the accurate diagnosis of Entamoeba histolytica, as they enable differentiation from non-pathogenic species like E. dispar, which is impossible with conventional microscopy [3] [4].
One multicentre study evaluating the Allplex GI-Parasite Assay reported excellent performance compared to traditional techniques, with sensitivity and specificity as follows: 100% and 100% for Entamoeba histolytica, 100% and 99.2% for Giardia duodenalis, 97.2% and 100% for Dientamoeba fragilis, and 100% and 99.7% for Cryptosporidium spp., respectively [3].
Table 3: Multicentre Comparison of Diagnostic Methods for Intestinal Protozoa
| Parasite | Reference Method | Molecular Method | Sensitivity | Specificity | Study |
|---|---|---|---|---|---|
| Entamoeba histolytica | Microscopy, antigen, culture | Allplex GI-Parasite Assay | 100% | 100% | [3] |
| Giardia duodenalis | Microscopy, antigen, culture | Allplex GI-Parasite Assay | 100% | 99.2% | [3] |
| Dientamoeba fragilis | Microscopy, stained smears | Allplex GI-Parasite Assay | 97.2% | 100% | [3] |
| Cryptosporidium spp. | Microscopy, antigen | Allplex GI-Parasite Assay | 100% | 99.7% | [3] |
| Cyclospora cayetanensis | BAM Chapter 19b qPCR | Modified Mit1C qPCR | 100% (200 oocysts), 69.2% (5 oocysts) | 98.9% | [9] |
Experimental Protocols for Key Methodologies
Detailed methodologies are essential for reproducing multicentre study findings and implementing diagnostic protocols in clinical practice.
Serological Testing Protocol
For serological assays, testing should be performed according to manufacturer instructions using kits from the same batch to minimize variability [8]. The protocol generally involves:
- Serum sample collection and proper storage at -20°C until testing
- Simultaneous testing of all samples with the same batch of reagents
- Including appropriate positive and negative controls in each run
- Interpretation of results according to established cut-off values
- Parallel testing with two different serological tests using distinct methodologies and antigens as per diagnostic standards [8]
In cases of discordant results between initial tests, retesting is advised, with a third test used to confirm the diagnosis if inconsistencies persist [8].
Molecular Detection Protocol
Molecular detection of parasitic DNA in stool samples follows a standardized workflow:
- Sample Preparation: 50-100 mg of stool specimens is collected and suspended in 1 mL of stool lysis buffer (e.g., ASL buffer; Qiagen). After pulse vortexing for 1 min and incubation at room temperature for 10 min, the tubes are centrifuged at full speed (14,000 rpm) for 2 min [3].
- Nucleic Acid Extraction: The supernatant is used for nucleic acid extraction using automated systems such as the MagNA Pure 96 System [4] or Microlab Nimbus IVD system [3].
- PCR Amplification: DNA extracts are amplified with one-step real-time PCR multiplex using systems such as CFX96 Real-time PCR (Bio-Rad) with manufacturer-recommended cycling conditions. Fluorescence is detected at specific temperatures (e.g., 60°C and 72°C), with a positive test result defined as a sharp exponential fluorescence curve that intersects the crossing threshold (Ct) at a value of less than 45 for individual targets [3].
- Result Interpretation: Results are interpreted using appropriate software (e.g., Seegene Viewer software), with positive and negative controls included in each run [3].
Diagram 1: Multicentre Study Workflow for Parasitology Diagnostics
Research Reagent Solutions for Parasitology Diagnostics
Successful multicentre studies require carefully selected research reagents and platforms that ensure reproducibility across participating laboratories. The following toolkit details essential materials used in featured parasitology diagnostic studies.
Table 4: Essential Research Reagents for Parasitology Diagnostic Studies
| Reagent Category | Specific Examples | Function/Application | Study Context |
|---|---|---|---|
| Serological Assays | Biolisa Chagas Recombinante, T. cruzi Ab - ELISA, Architect Chagas | Detection of anti-parasite antibodies | Chagas disease serology [8] |
| Molecular Assays | Allplex GI-Parasite Assay, AusDiagnostics GI Panel | Multiplex detection of parasitic DNA/RNA | Intestinal protozoa detection [3] [4] |
| Nucleic Acid Extraction Kits | MagNA Pure 96 DNA and Viral NA Small Volume Kit, Microlab Nimbus IVD system | Automated nucleic acid purification from clinical samples | DNA extraction from stool samples [3] [4] |
| Stool Processing Buffers | S.T.A.R Buffer (Stool Transport and Recovery Buffer), ASL buffer (Qiagen) | Sample preservation and preparation for DNA extraction | Stool sample processing for PCR [4] |
| PCR Master Mixes | TaqMan Fast Universal PCR Master Mix | Amplification of target DNA sequences | Real-time PCR detection [4] |
| Staining Reagents | Giemsa stain, Trichrome stain | Microscopic visualization of parasites | Conventional microscopy [3] |
| Antigen Detection Tests | Giardia duodenalis, Entamoeba histolytica/dispar, Cryptosporidium spp. antigen tests | Immunological detection of parasite antigens | Reference method comparison [3] |
Diagram 2: Diagnostic Method Classification for Parasitology
Robust multicentre study protocols are indispensable for advancing diagnostic methods in parasitology. The core components—ethical compliance, standardized laboratory protocols, appropriate sample sizing, and statistical rigor—provide the foundation for generating reliable, generalizable evidence on diagnostic performance. Recent multicentre comparisons demonstrate that while molecular methods offer superior sensitivity and specificity for many parasitic infections, particularly for differentiating pathogenic species, optimized serological assays and conventional microscopy remain important in specific diagnostic algorithms.
The future of parasitology diagnostics will likely involve integrated approaches that combine the strengths of different platforms, with multicentre studies continuing to play a critical role in validating these approaches across diverse clinical settings and populations. As molecular technologies become more accessible and standardized, their incorporation into routine diagnostic pathways, guided by robust multicentre validation data, promises to improve the detection and management of parasitic diseases globally.
In the field of parasitology, the transition from traditional microscopic techniques to modern molecular and artificial intelligence (AI)-based diagnostic methods represents a significant evolution. This shift is central to a broader thesis on the multicentre validation of parasitology diagnostic methods, which aims to establish standardized, sensitive, and specific testing protocols across diverse laboratory settings. Traditional microscopy, while widely used, faces challenges related to sensitivity, specificity, and operator dependency [3] [10]. Molecular techniques, particularly multiplex real-time PCR, offer enhanced sensitivity and specificity, allowing for the differentiation of morphologically similar species, such as the pathogenic Entamoeba histolytica from non-pathogenic species [3] [4]. Concurrently, AI-based tools are emerging as transformative technologies, demonstrating superior detection capabilities for intestinal parasites and malaria compared to conventional methods [11] [12] [13]. The consistent performance of these advanced diagnostics across different sites, however, is contingent upon rigorous site selection and comprehensive standardization of pre-analytical, analytical, and post-analytical procedures. This guide objectively compares the performance of various diagnostic alternatives and details the experimental protocols and reagent solutions essential for ensuring consistency in multicentre studies.
Performance Comparison of Diagnostic Methods
The evaluation of diagnostic methods across multiple research centres reveals significant differences in their ability to detect parasitic infections. The tables below summarize key performance metrics for methods targeting intestinal protozoa, soil-transmitted helminths (STHs), and malaria parasites, providing a data-driven basis for comparison.
Table 1: Performance Comparison of Methods for Detecting Intestinal Protozoa
| Diagnostic Method | Target Parasite | Sensitivity (%) | Specificity (%) | Notes / Reference Standard |
|---|---|---|---|---|
| Multiplex PCR (Allplex Assay) [3] | Entamoeba histolytica | 100.0 | 100.0 | Microscopy, antigen testing, culture |
| Giardia duodenalis | 100.0 | 99.2 | Microscopy, antigen testing, culture | |
| Dientamoeba fragilis | 97.2 | 100.0 | Microscopy, antigen testing, culture | |
| Cryptosporidium spp. | 100.0 | 99.7 | Microscopy, antigen testing, culture | |
| Commercial vs. In-House PCR [4] | Giardia duodenalis | High (Complete agreement) | High (Complete agreement) | Conventional microscopy |
| Cryptosporidium spp. | Limited | High | Conventional microscopy | |
| Dientamoeba fragilis | Limited | High | Conventional microscopy | |
| Traditional Microscopy [10] | General Pathogenic Parasites (1 sample) | 61.2 (Cumulative) | - | Analysis of 3 sequential samples |
| General Pathogenic Parasites (3 samples) | 100.0 (Cumulative) | - | Analysis of 3 sequential samples |
Table 2: Performance Comparison of Methods for STHs and Malaria Parasites
| Diagnostic Method | Target Parasite | Sensitivity (%) | Specificity (%) | Notes / Reference Standard |
|---|---|---|---|---|
| Manual Microscopy (Kato-Katz) [12] | Ascaris lumbricoides | 50.0 | >97 | Composite reference (physical + digital smears) |
| Trichuris trichiura | 31.2 | >97 | Composite reference (physical + digital smears) | |
| Hookworms | 77.8 | >97 | Composite reference (physical + digital smears) | |
| Expert-Verified AI (Kato-Katz) [12] | Ascaris lumbricoides | 100.0 | >97 | Composite reference (physical + digital smears) |
| Trichuris trichiura | 93.8 | >97 | Composite reference (physical + digital smears) | |
| Hookworms | 92.2 | >97 | Composite reference (physical + digital smears) | |
| qPCR [14] | Trichuris trichiura | Higher than Kato-Katz | - | Complement to Kato-Katz, especially post-treatment |
| Microscopy (Malaria) [15] | Plasmodium (Peripheral blood) | 73.8 | 100.0 | Multiplex qPCR as reference |
| RDTs (Malaria) [15] | Plasmodium (Peripheral blood) | 67.6 | 96.5 | Multiplex qPCR as reference |
| Multiplex qPCR (Malaria) [15] | Plasmodium (Peripheral blood) | 100.0 | 94.8 | Microscopy as reference |
Detailed Experimental Protocols
To ensure the reproducibility of results across different laboratories, a clear understanding of the experimental protocols used in the cited studies is essential. The following section details the methodologies for molecular, AI-based, and traditional diagnostic techniques.
Molecular Detection Protocol (Multiplex Real-Time PCR)
The protocol for the Allplex GI-Parasite Assay, as used in a multicentre study across 12 Italian laboratories, is summarized below [3].
- Sample Preparation: Approximately 50 to 100 mg of stool specimen was suspended in 1 mL of stool lysis buffer (ASL buffer; Qiagen). The suspension was pulse-vortexed for 1 minute and incubated at room temperature for 10 minutes. After centrifugation at 14,000 rpm for 2 minutes, the supernatant was used for nucleic acid extraction.
- Nucleic Acid Extraction: Extraction was performed using the Microlab Nimbus IVD system (Hamilton), which automated the nucleic acid processing and PCR setup.
- PCR Amplification and Detection: DNA extracts were amplified using a one-step real-time PCR multiplex on a CFX96 Real-time PCR system (Bio-Rad) with the Allplex GI-Parasite Assay (Seegene Inc.). Fluorescence was detected at two temperatures (60°C and 72°C). A positive result was defined as a sharp exponential fluorescence curve crossing the threshold (Ct) at a value below 45 for individual targets. Results were interpreted using Seegene Viewer software.
AI-Based Diagnostic Protocol for STHs
A study in Kenya compared AI-supported diagnosis with manual microscopy for STHs in Kato-Katz thick smears [12].
- Sample Collection and Slide Preparation: Stool samples were collected from school children. Kato-Katz thick smears were prepared according to standard WHO-recommended procedures.
- Slide Digitization: The prepared Kato-Katz smears were digitized using portable whole-slide scanners in a primary healthcare setting, creating whole-slide images for analysis.
- AI Analysis: The digital smears were analyzed by a deep learning-based AI model. The system employed convolutional neural networks, including an additional algorithm specifically trained to detect partially disintegrated hookworm eggs to improve sensitivity.
- Diagnostic Verification:
- Autonomous AI: The AI provided a diagnosis without human intervention.
- Expert-Verified AI: Experts reviewed the AI-detected eggs in the digital smears to provide a final verified diagnosis.
- Reference Standard: A composite reference standard was used, where a sample was considered positive if eggs were verified by an expert during manual microscopy or if two expert microscopists independently verified AI-detected eggs in the digital smears.
Protocol for Determining Optimal Stool Samples via Microscopy
A retrospective cross-sectional study in Thailand defined a protocol to determine the diagnostic yield of multiple stool examinations [10].
- Sample Collection: Patients submitted three stool specimens within a 7-day period.
- Microscopy Technique: Stool samples were analyzed using a combination of Kato's thick smear and direct smear techniques.
- Data Analysis: The diagnostic yield was calculated as the proportion of patients with parasitic infections diagnosed from one, two, or all three specimens. The sequence of positive results (e.g., first positive in the first, second, or third specimen) was analyzed using proportional ordinal logistic regression to identify factors associated with detection in later samples.
Workflow and Relationship Diagrams
The following diagrams illustrate the logical workflows for the multicentre validation of diagnostic methods and the comparative operational pathways between traditional and novel diagnostic approaches.
Multicentre Validation Workflow
Diagnostic Pathways Comparison
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation and standardization of parasitological diagnostics, particularly in multicentre trials, rely on a core set of reliable reagents and instruments. The following table details essential solutions used in the featured experiments.
Table 3: Essential Research Reagents and Materials for Parasitology Diagnostics
| Item Name | Function / Role | Example from Search Context |
|---|---|---|
| Stool Lysis & Transport Buffers | Facilitates sample homogenization, stabilization of nucleic acids, and disruption of hardy parasite (oo)cyst walls for efficient DNA release. | ASL Buffer (Qiagen) [3]; S.T.A.R. Buffer (Roche) [4] |
| Automated Nucleic Acid Extraction Systems | Standardizes the DNA/RNA purification process, minimizing inter-operator and inter-site variability, which is critical for PCR reproducibility. | Microlab Nimbus IVD System (Hamilton) [3]; MagNA Pure 96 System (Roche) [4] |
| Multiplex Real-Time PCR Kits | Allows simultaneous detection of multiple parasite targets in a single reaction, conserving sample volume and reducing reagent costs and time. | Allplex GI-Parasite Assay (Seegene Inc.) [3]; AusDiagnostics Parasite PCR Kit [4] |
| PCR Enzyme Master Mixes | Provides the necessary enzymes, dNTPs, and optimized buffers for efficient and specific amplification of target DNA during PCR. | TaqMan Fast Universal PCR Master Mix (Thermo Fisher) [4] |
| Deep Learning AI Models & Software | Automates the detection and identification of parasites in digital images, increasing throughput, consistency, and sensitivity. | DINOv2 models [13]; YOLOv8-m [13]; Custom CNNs for STHs [12] |
| Portable Slide Scanners | Digitizes microscope slides in field or primary care settings, enabling remote diagnosis and AI-based analysis where high-end microscopes are unavailable. | Portable whole-slide scanners [12] |
| Fecal Concentration Kits | Enriches parasite eggs, cysts, and oocysts in stool samples, improving the sensitivity of both microscopic and molecular downstream assays. | Formalin-Ethyl Acetate Concentration Technique (FECT) reagents [10] [13] |
Ethical Considerations and Patient Population Definition
Multicentre studies have emerged as the gold standard for validating parasitology diagnostic methods, providing the statistical power, epidemiological diversity, and generalizability required for robust evidence generation [16]. Unlike single-centre investigations, these collaborative research networks enable rapid recruitment across diverse geographical settings, encompassing the varied manifestations of parasitic diseases across different populations and environmental contexts [16]. The Severe Malaria in African Children (SMAC) network exemplifies this approach, having been established specifically because "single centers cannot enroll enough patients to detect reductions of 20–30% in mortality rates" for falciparum malaria, which kills more than one million children annually [16].
The validation of diagnostic methods for parasitic diseases presents unique ethical challenges and requires meticulous patient population definition. These considerations are not merely regulatory hurdles but fundamental scientific requirements that directly impact the validity, applicability, and ethical integrity of research findings. This guide examines the ethical frameworks and population definition strategies employed in contemporary multicentre studies validating parasitology diagnostics, providing researchers with evidence-based approaches for designing methodologically sound and ethically compliant studies.
Ethical Frameworks in Multicentre Diagnostic Studies
Core Ethical Principles and Implementation
Multicentre diagnostic studies operate within well-established ethical frameworks that prioritize participant welfare while ensuring scientific validity. The convergence of ethical principles across recent studies reveals a consistent pattern of requirements and implementations:
Table 1: Ethical Principles in Multicentre Parasitology Studies
| Ethical Principle | Implementation in Diagnostic Studies | Representative Examples |
|---|---|---|
| Informed Consent | Local language explanation with written or witnessed verbal consent; parental consent with child assent where appropriate | SMAC network: "Consent was sought from accompanying parent or guardian" with content "conveyed first in the appropriate local language" [16] |
| Ethical Review | Multiple approvals from local IRBs, coordinating center IRB, and funding agency review boards | ALIVE trial: "Ethical approvals were obtained from the respective national and institutional ethics committee in each participating country" [14] |
| Confidentiality | De-identification with coding systems; secure data transfer protocols | SMAC network: "All personal identifiers were removed, and only codes were used" [16] |
| Beneficence | Treatment provided to infected participants; post-trial benefit sharing | Malaria in pregnancy study: "Pregnant women who were infected with Plasmodium parasites were treated according to the national treatment guidelines" [15] |
| Justice | Inclusion of vulnerable populations with appropriate safeguards; equitable selection of participants | SMAC network: Focus on children as vulnerable population with enhanced protections [16] |
The SMAC network implementation exemplifies comprehensive ethical oversight, with their consent process requiring approval from "the local Institutional Review Board (IRB), by the Michigan State University IRB, and by the protocol review group at the National Institute of Allergy and Infectious Diseases" [16]. This multi-layered review ensures both international ethical standards and local contextual appropriateness are maintained.
Special Considerations for Vulnerable Populations
Research involving vulnerable populations requires additional ethical safeguards. Paediatric populations feature prominently in parasitic disease research, necessitating appropriate assent procedures alongside parental consent. The SMAC network, which enrolled children with severe malaria, implemented a consent process where "the parent/guardian could indicate their consent by signing the consent form, or by verbally agreeing in the presence of a witness" [16], accommodating varying literacy levels while maintaining ethical rigor.
Pregnant women represent another vulnerable population requiring special ethical considerations. The study of malaria diagnostics in pregnancy in Northwest Ethiopia explicitly stated that "written informed consent was obtained from pregnant women after briefing clearly about the purpose and benefits of the study" and emphasized that "they were also informed that they have the full right to withdraw from the study at any time" [15]. This attention to autonomous decision-making demonstrates the application of enhanced informed consent processes for vulnerable groups.
Diagram 1: Comprehensive ethical framework for multicentre parasitology studies illustrating the interconnection between core principles, vulnerable population safeguards, and implementation mechanisms.
Defining Patient Populations in Diagnostic Studies
Recruitment Strategies and Inclusion Criteria
Patient population definition in parasitology diagnostic studies requires careful consideration of epidemiological factors, clinical presentation, and practical constraints. The SMAC network implemented a standardized surveillance mechanism to capture "clinical, laboratory, and outcome data on all parasitemic children admitted to hospital" across five sites in Africa [16]. Their inclusion criteria specified that "all children who were suspected of having a malaria illness and who were sick enough to be admitted to hospital were screened, with a peripheral blood film, for the presence of P. falciparum parasitemia" with those under 180 months invited to participate [16].
The multicentre study validating Charcot's Triad and Tokyo Guidelines for acute ascending cholangitis adopted a retrospective approach, analyzing data from 1,643 patients across multiple centres between January 2016 and December 2021 [17]. This study specifically focused on the challenging diagnostic scenario of acute ascending cholangitis "secondary to liver cystic echinococcosis rupture in the biliary tree" [17], demonstrating how patient populations can be defined by specific pathological mechanisms rather than just clinical syndromes.
Geographical and Epidemiological Diversity
Incorporating geographical diversity ensures that diagnostic methods are validated across different epidemiological settings. The SMAC network intentionally included sites across Africa (Gambia, Malawi, Ghana, Kenya, Gabon) because "patients do reflect severe malaria in each setting, they represent the group most likely to participate in future clinical trials, and they encompass much of the epidemiological diversity of malaria across the continent" [16].
Similarly, the ALIVE clinical trial for trichuris trichiura treatment efficacy conducted multisite recruitment "in schools across Kwale County (Kenya), Bahir Dar Zuria (Ethiopia), and Manhiça District (Mozambique)" [14]. This geographical distribution across East and Southern Africa increases the generalizability of the diagnostic findings across different strains and transmission patterns.
Comparative Performance of Diagnostic Methods
Molecular vs. Conventional Methods
Recent multicentre studies have generated robust comparative data on parasitology diagnostic methods, particularly comparing molecular techniques with conventional microscopy:
Table 2: Comparative Performance of Diagnostic Methods in Multicentre Studies
| Study & Population | Comparison | Sensitivity | Specificity | Key Findings |
|---|---|---|---|---|
| Intestinal Protozoa Multicentre (Italy) [3] | Multiplex PCR vs. Microscopy | 100% (E. histolytica)100% (G. duodenalis)97.2% (D. fragilis) | 100% (E. histolytica)99.2% (G. duodenalis)100% (D. fragilis) | Multiplex PCR showed "excellent performance in the detection of the most common enteric protozoa" across 12 laboratories |
| Malaria in Pregnancy (Ethiopia) [15] | qPCR vs. Microscopy (peripheral) | 73.8% (Microscopy)100% (qPCR) | 100% (Microscopy)94.8% (qPCR) | "Multiplex qPCR had a better performance for Plasmodium infection diagnosis in pregnancy compared to microscopy and RDT" |
| Soil-Transmitted Helminths (Timor-Leste/Cambodia) [18] | Multiplex PCR vs. Microscopy | 2.9x higher for hookworms1.2x higher for Ascaris1.6x higher for Giardia | Comparable or superior to microscopy | "Multiplex PCR, in addition to superior sensitivity, enabled more accurate determination of infection intensity" |
| STH AI Microscopy (Kenya) [12] | Expert-verified AI vs. Manual Microscopy | 100% (A. lumbricoides)93.8% (T. trichiura)92.2% (Hookworms) | >97% for all STH | "Expert-verified AI had higher sensitivity than the other methods while maintaining high specificity for the detection of STH" |
The superior sensitivity of molecular methods is particularly evident in low-intensity infections. In the ALIVE trial for trichuris trichiura, researchers noted that "concordance between stool egg counts and Ct-value decreased post-treatment, likely due to reduced KK sensitivity in low-intensity infections" [14]. This has significant implications for patient population definition in treatment efficacy studies, where post-treatment monitoring requires highly sensitive detection methods.
Impact on Patient Management and Public Health
The diagnostic performance characteristics directly influence patient management decisions and public health interventions. The study of acute ascending cholangitis secondary to liver cystic echinococcosis found that "TG18, especially in its definite form, can effectively rule out AAC, whereas CT, despite its low sensitivity, remains useful due to its high specificity" [17]. This complementary diagnostic approach guides clinicians in selecting appropriate tests based on the clinical scenario.
For soil-transmitted helminths, the improved sensitivity of molecular methods has revealed significant underdetection by conventional microscopy. One study found that "higher parasite prevalence was detected by multiplex PCR (hookworms 2.9 times higher, Ascaris 1.2, Giardia 1.6, along with superior polyparasitism detection with this effect magnified as the number of parasites present increased" [18]. This improved detection has direct implications for defining truly infected populations in epidemiological studies and treatment programs.
Experimental Protocols in Multicentre Studies
Standardized Laboratory Procedures
Successful multicentre validation requires meticulous standardization of laboratory procedures across participating sites. The SMAC network implemented rigorous quality control measures where "before data collection began, at least one laboratory technician from each site attended a workshop and was trained in operating and maintaining the two instruments that were new and common to all five sites" [16]. This ensured consistent application of diagnostic methods across diverse settings.
The multicentre validation of the Allplex GI-Parasite Assay across 12 Italian laboratories utilized standardized DNA extraction protocols: "Nucleic acids were extracted, using the Microlab Nimbus IVD system which automatically performed the nucleic acid processing and PCR setup" [3]. Automation reduces inter-site variability and improves reproducibility of results.
Data Management and Quality Assurance
Robust data management systems are essential for maintaining data integrity in multicentre studies. The SMAC network implemented a system where "data were collected on a standardized case report form" and "two different people performed data entry" with "an automated verification program [that] generated an error file, and queries were created for data outside of the pre-defined allowable ranges" [16]. This systematic approach to data management minimized errors and ensured high-quality data collection.
The multicentre PCR validation for Cyclospora cayetanensis detection implemented a blind-coded sample approach where "each laboratory analyzed twenty-four blind-coded Romaine lettuce DNA test samples" [9]. This design reduced assessment bias and provided robust comparative data across multiple laboratories.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Multicentre Parasitology Diagnostics
| Reagent/Kit | Application | Performance Characteristics | Representative Use |
|---|---|---|---|
| Allplex GI-Parasite Assay (Seegene) | Multiplex detection of 6 protozoa | 100% sensitivity for Cryptosporidium; 97.2% for D. fragilis [3] | Multicentre validation across 12 Italian labs [3] |
| QIAamp DNA Mini Kit (Qiagen) | DNA extraction from stool | Enhanced protocol with PVPP for inhibitor removal [14] | ALIVE trial for STH diagnosis [14] |
| Powersoil DNA Isolation Kit (Mo Bio) | Environmental sample DNA extraction | Modified protocol for STH egg isolation [18] | Soil-transmitted helminth study in Timor-Leste/Cambodia [18] |
| Hamilton STARlet Automated System | High-throughput nucleic acid extraction | Reduced pre-analytical and analytical TAT by 7 hours [19] | Validation of enteric protozoa PCR in public health lab [19] |
| Sodium Nitrate Flotation | Microscopic STH detection | Traditional method compared to PCR in multicentre studies [18] | Reference method in diagnostic comparison studies [18] [20] |
| Kato-Katz Reagents | Microscopic STH egg quantification | WHO-recommended for intensity assessment [12] | Reference standard in AI microscopy validation [12] |
Diagram 2: Methodological framework for patient population definition and diagnostic validation in multicentre parasitology studies showing the relationship between definition criteria, diagnostic methods, and study outcomes.
The validation of parasitology diagnostic methods through multicentre studies requires meticulous attention to ethical frameworks and precise patient population definition. Current evidence demonstrates that molecular methods, particularly multiplex PCR platforms, offer superior sensitivity compared to conventional microscopy, especially for low-intensity infections and polyparasitism [3] [18]. However, the choice of diagnostic method must be aligned with the research objectives, population characteristics, and intended application of the results.
Ethical implementation requires genuine commitment to multi-layered review processes, culturally appropriate consent procedures, and special protections for vulnerable populations [16] [15]. The geographical diversity of study sites enhances the generalizability of findings but introduces methodological challenges that must be addressed through standardized protocols and rigorous quality control [16].
Future directions in parasitology diagnostics validation will likely involve increased automation, artificial intelligence-assisted methods [12], and the development of standardized panels for simultaneous detection of multiple pathogens. Regardless of technological advances, the fundamental principles of ethical research conduct and precise patient population definition will remain cornerstone requirements for generating valid, applicable evidence to guide clinical practice and public health interventions.
The Global Burden of Parasitic Diseases as a Driver for Improved Diagnostics
Parasitic diseases constitute a major global public health challenge, disproportionately affecting developing nations and imposing significant health and economic burdens. Vector-borne parasitic diseases (VBPDs) alone account for more than 17% of all infectious diseases worldwide [21] [22]. The disability-adjusted life years (DALYs) attributed to these diseases are immense, with malaria alone responsible for approximately 46 million DALYs in 2019 [22]. This staggering disease burden, coupled with the limitations of conventional diagnostic methods, has become a powerful driver for innovation in parasitology diagnostics. The need for precise, rapid, and accessible diagnostic tools is critical for disease management, surveillance, and achieving elimination targets, particularly for neglected tropical diseases (NTDs) [21] [23].
The global health community recognizes that progress against parasitic infections is hampered by diagnostic challenges. Traditional techniques, particularly microscopy, remain the mainstay in many settings but are beset by limitations including low sensitivity, requirement for high expertise, and prolonged turnaround times [3] [23]. This has accelerated a shift towards molecular and serological methods, whose performance must be rigorously validated across diverse epidemiological settings. Multicenter studies provide the highest level of evidence for this validation, demonstrating how a test performs across different populations, parasite strains, and laboratory conditions. This article analyzes the current landscape of parasitology diagnostics through the lens of multicentre study data, providing a comparative analysis of diagnostic performance and the experimental protocols that underpin these advancements.
The Global Burden of Parasitic Diseases
The epidemiology of parasitic diseases highlights the urgent need for improved diagnostics. A comprehensive analysis of the global burden of VBPDs from 1990 to 2021 reveals persistent and stark disparities. Malaria continues to dominate, comprising 42% of VBPD cases and a staggering 96.5% of VBPD deaths, with the burden overwhelmingly concentrated in sub-Saharan Africa [21]. Schistosomiasis ranks as the second most prevalent VBPD, accounting for 36.5% of cases [21]. While diseases like African trypanosomiasis, Chagas disease, lymphatic filariasis, and onchocerciasis have seen significant declines, the incidence of leishmaniasis is rising, with an estimated annual percentage change (EAPC) of 0.713 [21]. These diseases thrive in conditions of poverty, and low socio-demographic index (SDI) regions bear the highest burden, a phenomenon exacerbated by environmental factors, limited healthcare access, and resource distribution challenges [21] [22]. The morbidity extends beyond mortality, causing chronic disability, malnutrition, anemia, and stunted cognitive development in children, perpetuating a cycle of poverty and disease [23] [22].
Table 1: Key Epidemiological Metrics for Major Vector-Borne Parasitic Diseases (1990-2021)
| Disease | Percentage of Total VBPD Cases | Percentage of VBPD Deaths | Recent Trend | High-Burden Regions |
|---|---|---|---|---|
| Malaria | 42% | 96.5% | Slight upward incidence trend [21] | Sub-Saharan Africa [21] |
| Schistosomiasis | 36.5% | Not Dominant | Persistent high prevalence [21] | Asia, Africa, Latin America [21] |
| Leishmaniasis | Not Specified | Not Dominant | Rising prevalence (EAPC = 0.713) [21] | India, Nepal, Brazil, Ethiopia [24] |
| Chagas Disease | Not Specified | Not Dominant | Significant decline [21] | Latin America [21] |
| Lymphatic Filariasis | Not Specified | Not Dominant | Nearing elimination by 2029 forecast [21] | Sub-Saharan Africa, Asia [21] |
Multicenter Validation of Diagnostic Performance
Multicenter studies are the gold standard for evaluating diagnostic tests in real-world conditions. The tables below synthesize performance data from recent studies across various parasitic diseases and diagnostic platforms, highlighting their sensitivity, specificity, and operational characteristics.
Performance of Molecular Assays for Enteric Protozoa
Molecular multiplex PCR panels are revolutionizing the diagnosis of enteric protozoa, offering high throughput and objective results. The following data from multicenter evaluations demonstrate their performance compared to traditional microscopy.
Table 2: Multicenter Performance of Molecular Assays for Enteric Protozoa Detection
| Parasite | Assay Name | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Study Details |
|---|---|---|---|---|---|---|
| Giardia duodenalis | Allplex GI-Parasite | 100 | 99.2 | 68.8 | 100 | 368 samples, 12 Italian labs [3] |
| Automated High-Throughput PCR | 100 | 98.9 | 68.8 | 100 | 461 specimens [19] | |
| Cryptosporidium spp. | Allplex GI-Parasite | 100 | 99.7 | - | - | 368 samples, 12 Italian labs [3] |
| Automated High-Throughput PCR | 100 | 100 | 100 | 100 | 461 specimens [19] | |
| Entamoeba histolytica | Allplex GI-Parasite | 100 | 100 | - | - | 368 samples, 12 Italian labs [3] |
| Automated High-Throughput PCR (Fresh Specimens) | 33.3 | 100 | 100 | 99.6 | 461 specimens [19] | |
| Dientamoeba fragilis | Allplex GI-Parasite | 97.2 | 100 | - | - | 368 samples, 12 Italian labs [3] |
| Automated High-Throughput PCR | 100 | 99.3 | 88.5 | 100 | 461 specimens [19] | |
| Blastocystis hominis | Automated High-Throughput PCR | 93 | 98.3 | 85.1 | 99.3 | 461 specimens [19] |
Performance of Diagnostic Tests for Visceral Leishmaniasis
The diagnosis of visceral leishmaniasis (VL) employs a variety of methods. A large multicenter study across six countries evaluated a dipstick test, while a study in Ethiopia compared five different diagnostic methods.
Table 3: Performance of Diagnostic Tests for Visceral Leishmaniasis
| Test Type | Target/Principle | Sensitivity (%) | Specificity (%) | Geographic Region/Study |
|---|---|---|---|---|
| LAg Dipstick | Leishmania donovani membrane antigens | 97.1 | 93.44 | Multicenter (India, Nepal, Brazil, etc.) [24] |
| Direct Agglutination Test (DAT) | Antibody-mediated agglutination | 96.5 | 97.96 | Ethiopia (qPCR as reference) [25] |
| mini-dbPCR-NALFIA | Direct-on-blood PCR with lateral flow | 95.8 | 98.92 | Ethiopia (qPCR as reference) [25] |
| LAMP Assay | Loop-mediated isothermal amplification | 94.33 | 97.38 | Ethiopia (qPCR as reference) [25] |
| rk39 RDT | Recombinant K39 antigen | 88.11 | 83.33 | Ethiopia (qPCR as reference) [25] |
| Microscopy | Direct parasitological observation | 76.58 | 100 | Ethiopia (qPCR as reference) [25] |
Experimental Protocols and Workflows
A critical understanding of diagnostic test performance requires insight into the experimental methodologies used for their validation.
Molecular Workflow for Enteric Parasite Detection
The transition from sample to result in molecular diagnostics involves a standardized sequence of steps to ensure accuracy and reproducibility.
Diagram 1: Molecular Diagnostic Workflow
The molecular diagnostic process begins with Stool Sample Collection, where fresh, unpreserved specimens are often used [19]. A critical pre-analytical step is Mechanical Pretreatment, or bead beating, which is essential for breaking down the resilient walls of parasitic cysts, oocysts, and spores to release nucleic acids. One optimized protocol uses the TissueLyser II at 30 Hz for 60 seconds with small, commercial beads (e.g., ZR BashingBeads or MP Lysing Matrix E) to achieve optimal disruption without excessive DNA fragmentation [26]. Subsequently, Automated Nucleic Acid Extraction is performed on platforms like the Hamilton STARlet or Microlab Nimbus IVD, which use bead-based kits (e.g., STARMag from Seegene) to purify nucleic acid from the lysate, ensuring consistency and high throughput [3] [19]. The extracted DNA is then used for Multiplex Real-Time PCR Setup, where reagents like the Allplex GI-Parasite Assay are employed. These master mixes contain primers, probes, and enzymes for the simultaneous detection of multiple targets [3] [19]. The plate undergoes Amplification & Fluorescence Detection on a real-time PCR instrument (e.g., Bio-Rad CFX96) for 45 cycles. Finally, Result Interpretation is based on cycle threshold (Ct) values, with a result typically considered positive if the Ct is ≤43 as per manufacturer guidelines, followed by automated or software-assisted Report Generation [19].
Serological Testing Workflow for Visceral Leishmaniasis
Serological tests, such as rapid diagnostic tests (RDTs), provide a point-of-care solution for diseases like visceral leishmaniasis. The workflow is designed for simplicity and speed.
Diagram 2: Serological Test Workflow
The serological testing workflow for VL begins with Blood/Serum Sample Collection [24]. A small volume of serum or whole blood is applied directly to the Sample Application well of the test device, such as an rK39 RDT or an LAg-based dipstick [25] [24]. This is followed by the Addition of Buffer to facilitate capillary flow across the nitrocellulose strip. The test then undergoes a brief Incubation period, typically 10 to 20 minutes at room temperature, during which the sample migrates. If specific anti-Leishmania antibodies (e.g., against rK39 or LAg) are present, they bind to conjugated labels and then to immobilized capture reagents, forming a Visual Readout of Bands. A Positive result is confirmed by the appearance of both a control band (indicating proper test function) and a test band. A Negative result shows the control band only [24]. The entire process requires no specialized equipment and can be performed in basic clinical settings.
The Scientist's Toolkit: Key Research Reagents & Platforms
Advancements in parasitology diagnostics are enabled by a core set of reagents, instruments, and technologies. The following table details essential components featured in the cited multicenter studies.
Table 4: Essential Research Reagents and Platforms for Parasitology Diagnostics
| Category/Item | Specific Example(s) | Function & Application |
|---|---|---|
| Automated Nucleic Acid Extractors | Hamilton STARlet, Microlab Nimbus IVD | Perform high-throughput, automated purification of DNA from complex stool samples, reducing manual labor and variation [3] [19]. |
| Commercial Multiplex PCR Kits | Allplex GI-Parasite Assay (Seegene), BD MAX Enteric Parasite Panel | Provide pre-optimized master mixes and primers/probes for simultaneous detection of multiple enteric protozoa in a single reaction [3] [27]. |
| Mechanical Disruption Beads | ZR BashingBeads (ZymoResearch), MP Lysing Matrix E (MP Biomedicals) | Used with homogenizers (e.g., TissueLyser II) to rupture resilient parasitic (oo)cysts and spores during sample pretreatment, critically enhancing DNA yield [26]. |
| Real-Time PCR Instruments | Bio-Rad CFX96 | Platforms for running real-time PCR assays, enabling fluorescence detection and Ct value determination for qualitative and quantitative analysis [3] [19]. |
| Reference Standard Antigens | rK39 recombinant antigen, Native Leishmania membrane antigens (LAg) | Used as capture antigens in serological tests (RDTs, dipsticks) for detection of pathogen-specific antibodies in diseases like visceral leishmaniasis [25] [24]. |
| Isothermal Amplification Kits | LAMP Assay Kits | Enable nucleic acid amplification at a constant temperature, facilitating molecular testing in field settings without complex thermal cyclers [25]. |
Emerging Technologies and Future Directions
The field of parasitology diagnostics continues to evolve rapidly, driven by the persistent burden of disease and the limitations of current technologies. Several emerging approaches hold significant promise for the future.
- CRISPR-Cas Based Diagnostics: CRISPR-Cas technology is being leveraged for its precision and programmability in detecting parasitic DNA and RNA. These systems offer the potential for ultra-sensitive, portable, and cost-effective diagnostics that can be deployed at the point of care, potentially surpassing the complexity and equipment needs of traditional PCR [23].
- Nanotechnology and Biosensors: The application of nanotechnology in diagnostics is leading to the development of advanced nano-biosensors. Nanoparticles, due to their unique physical and chemical properties, can be used to create highly sensitive detection platforms, including magnetic isolation devices and lateral flow assays with enhanced performance characteristics [23].
- Artificial Intelligence (AI) in Imaging: AI and machine learning are beginning to transform the analysis of microscopic images for parasite identification. These systems can assist in automating the detection and classification of parasites in blood, stool, or tissue samples, reducing reliance on highly trained microscopists and increasing throughput and standardization [23].
- Multi-omics Integration: The integration of data from genomics, proteomics, and metabolomics ("multi-omics") provides a comprehensive understanding of parasite biology and host-parasite interactions. This holistic approach is identifying novel biomarkers for more accurate diagnostics and contributing to the understanding of drug resistance mechanisms [23].
The significant and ongoing global burden of parasitic diseases remains a powerful catalyst for innovation in diagnostic science. Multicenter validation studies provide the critical evidence that molecular assays and advanced serological tests offer superior sensitivity, specificity, and operational efficiency compared to traditional methods. As demonstrated by the comprehensive data, tests like the Allplex GI-Parasite panel and the LAg dipstick for VL deliver robust, reliable performance across diverse geographical settings. The future of parasitology diagnostics lies in the continued refinement of these technologies—making them more accessible, affordable, and adaptable through CRISPR, nanotechnology, and AI. The ultimate goal is to translate these technological advancements into effective field-deployable tools that can strengthen disease surveillance, guide targeted treatment, and accelerate progress towards the control and elimination of these pervasive diseases, thereby improving global health equity.
A Toolkit for Modern Parasite Detection: From Rapid Tests to Molecular Panels
In the field of clinical parasitology, microscopic examination of specimens remains a fundamental diagnostic approach, yet it faces significant challenges including labour-intensiveness, operator dependency, and variable sensitivity [28] [12]. While molecular techniques have advanced considerably, microscopy maintains critical importance in resource-limited settings and for specific diagnostic applications. This guide objectively compares the performance of enhanced traditional techniques—incorporating automation and artificial intelligence (AI)—against conventional microscopy and molecular alternatives, framed within the context of multicentre study validation for parasitology diagnostics.
The evolution of microscopy extends beyond mere visual enhancement through optics; it now integrates sophisticated digital imaging, machine learning algorithms, and automated sample processing systems. These technological integrations aim to address the well-documented limitations of conventional methods while maintaining the practical advantages of morphological diagnosis. Through multicentre validation, researchers have generated robust performance data enabling evidence-based selection of diagnostic approaches for various clinical and research scenarios.
Performance Comparison of Diagnostic Methods
Comprehensive Performance Metrics Across Parasitic Infections
Table 1: Diagnostic performance of microscopy, automated, and molecular methods for various parasitic infections
| Infection Type | Diagnostic Method | Sensitivity (%) | Specificity (%) | Reference Standard | Study Details |
|---|---|---|---|---|---|
| Soil-transmitted helminths [12] | Manual Microscopy (Kato-Katz) | 31.2-77.8* | >97 | Composite (physical + digital smear) | 704 smears, primary healthcare setting |
| Autonomous AI | 84.4-87.4* | >97 | Composite (physical + digital smear) | Portable whole-slide scanners | |
| Expert-verified AI | 92.2-100* | >97 | Composite (physical + digital smear) | Deep learning-based system | |
| Malaria [28] | miLab (Automated Mode) | 91.1 | 66.7 | Nested PCR | 190 patients, symptomatic |
| miLab (Corrected Mode) | 91.1 | 96.2 | Nested PCR | Operator intervention | |
| Expert Microscopy | 84.8-94.6 | 99.4-100 | Nested PCR | Comparator | |
| Intestinal Protozoa [4] | Conventional Microscopy | Variable [4] | Variable [4] | Consensus | 355 stool samples, 18 centres |
| Commercial RT-PCR | High for G. duodenalis [4] | High for G. duodenalis [4] | Consensus | AusDiagnostics platform | |
| In-house RT-PCR | High for G. duodenalis [4] | High for G. duodenalis [4] | Consensus | Validated assay | |
| Cryptosporidium [29] | Coproantigen ELISA | 98.86 | 94.32 | Microscopy/PCR | Multicenter evaluation |
| Conventional Microscopy | Lower than ELISA [29] | Lower than ELISA [29] | PCR | Requires experience |
*Varies by parasite species (A. lumbricoides, T. trichiura, hookworms)
Operational Characteristics Comparison
Table 2: Operational characteristics and technical requirements of diagnostic methods
| Method Category | Sample Throughput | Technical Skill Requirement | Equipment Cost | Infrastructure Demands | Automation Potential |
|---|---|---|---|---|---|
| Traditional Microscopy | Low | High (Expert dependent) | Low | Basic laboratory | Low |
| Automated Digital Microscopy [28] [12] | Medium-High | Medium (Operator verification) | High | Electricity, computing resources | High (Sample-to-result) |
| AI-Based Analysis [30] [12] | High | Low-Medium (After setup) | High | Advanced computing, storage | Full (With optional verification) |
| Molecular Methods [31] [4] | Medium-High | High | High | Molecular biology facility | Medium (Extraction to amplification) |
| Immunoassays [29] | High | Low-Medium | Medium | Basic laboratory with ELISA capability | High |
Experimental Protocols and Methodologies
Protocol for Automated Microscopy Validation in Malaria Diagnosis
The clinical validation of miLab for malaria diagnosis followed a standardized protocol in a prospective, case-control diagnostic accuracy study [28]:
Sample Collection and Processing:
- Capillary blood collection (120 μL via finger prick) from symptomatic patients ≥5 years old
- Division of sample for: reference microscopy (thin and thick smears), dried blood spots (DNA extraction), and miLab testing (5 μL)
- Immediate processing of all samples to maintain integrity
miLab Testing Procedure:
- Direct loading of 5μL fresh capillary blood onto single-use cartridge
- Automated processing: thin smear preparation, fixation, staining via proprietary stamping technology
- High-resolution digital imaging (500× lenses, CMOS sensor) with 400-field scanning
- Embedded AI analysis for parasite detection and quantification on server-free CPU
- Result display: images of parasitized/non-parasitized RBCs, parasite counts/μL
- Two reading modes: fully automated and operator-corrected for suspected results
Reference Standards and Statistical Analysis:
- Reference standard: nested PCR for definitive species identification
- Comparator: expert light microscopy following WHO standards
- Calculation of sensitivity, specificity with 95% confidence intervals
- Concordance measurement using kappa statistics and Bland-Altman analysis for parasite count agreement
Protocol for AI-Assisted Soil-Transmitted Helminth Diagnosis
A rigorous methodology was employed to validate AI-supported digital microscopy for soil-transmitted helminth diagnosis [12]:
Sample Preparation and Digitization:
- Stool sample collection from school children in endemic areas (Kwale County, Kenya)
- Kato-Katz thick smear preparation following WHO standards
- Whole-slide digitization using portable scanners in primary healthcare setting
- Image acquisition with quality control for focus and coverage
AI Analysis and Verification:
- Deep learning algorithm application with two components: original detection algorithm and additional algorithm for disintegrated hookworm eggs
- Autonomous AI analysis without human intervention
- Expert-verified AI analysis: independent review by two expert microscopists of AI-detected eggs
- Development of composite reference standard combining manual microscopy and verified digital findings
Diagnostic Accuracy Assessment:
- Comparison of three methods: manual microscopy, autonomous AI, expert-verified AI
- Calculation of sensitivity and specificity against composite reference
- Statistical analysis of differences using confidence intervals and p-values
- Subgroup analysis by infection intensity (light, moderate, heavy)
Molecular Method Validation Protocol
Multicenter comparison of molecular versus microscopic methods followed standardized protocols [4]:
Sample Collection and Processing:
- Prospective collection of 355 stool samples across 18 Italian laboratories
- Division into fresh samples (n=230) and preserved samples (n=125)
- Conventional microscopy following WHO/CDC guidelines with Giemsa staining for fresh samples and formalin-ethyl acetate concentration for preserved samples
DNA Extraction and Amplification:
- Automated nucleic acid extraction using MagNA Pure 96 System with Stool Transport and Recovery Buffer
- Parallel testing with commercial RT-PCR (AusDiagnostics) and validated in-house RT-PCR assays
- Multiplex tandem PCR amplification targeting G. duodenalis, Cryptosporidium spp., E. histolytica, and D. fragilis
- Internal extraction controls to monitor inhibition and extraction efficiency
Data Analysis:
- Calculation of agreement between methods using percent concordance
- Determination of sensitivity and specificity with microscopy as reference standard
- Subanalysis by sample type (fresh vs. preserved) and parasite species
Visual Workflows and Diagnostic Pathways
Automated Microscopy Diagnostic Workflow
Diagram 1: Automated microscopy diagnostic workflow illustrating the integrated process from sample collection to diagnostic reporting, highlighting decision points for expert verification.
Diagnostic Method Selection Pathway
Diagram 2: Diagnostic method selection pathway guiding appropriate technology selection based on operational constraints and diagnostic requirements.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for enhanced microscopy techniques
| Reagent/Material | Application | Function | Example in Protocols |
|---|---|---|---|
| miLab Cartridge [28] | Automated blood smear analysis | Integrated sample preparation and staining | Malaria diagnosis in symptomatic patients |
| Portable Whole-Slide Scanners [12] | Field-based digital pathology | Slide digitization for remote analysis | Soil-transmitted helminth diagnosis in primary care |
| Deep Learning Algorithms [30] [12] | Image analysis automation | Pattern recognition and parasite classification | Ascaris, Trichuris, hookworm detection |
| Stool Transport and Recovery Buffer [4] | Molecular parasitology | Nucleic acid preservation from stool samples | PCR-based protozoa detection |
| CoproELISA Cryptosporidium Kit [29] | Immunoassay detection | Cryptosporidium antigen detection in stool | High-throughput screening |
| MagNA Pure 96 System [4] | Nucleic acid extraction | Automated DNA purification from clinical samples | Multicenter molecular study |
| Real-Time PCR Master Mix [4] | Molecular amplification | Fluorescence-based target detection | Protozoan DNA amplification |
| Para-Pak Preservation Media [4] | Sample preservation | Maintains parasite morphology and nucleic acids | Multicenter sample consistency |
Discussion and Future Perspectives
The integration of automation and artificial intelligence with traditional microscopy techniques represents a paradigm shift in parasitology diagnostics. The experimental data demonstrate that while each method has distinct advantages and limitations, the enhanced microscopy approaches consistently outperform conventional microscopy in sensitivity while maintaining high specificity, particularly when incorporating expert verification systems [28] [12].
The operational characteristics of these enhanced methods reveal important considerations for implementation. Automated digital microscopy systems significantly reduce operator time and expertise requirements while improving standardization, though they require substantial initial investment and infrastructure support [28]. AI-supported analysis demonstrates particular value in high-throughput settings and for detecting low-intensity infections that frequently evade conventional microscopy [12]. Molecular methods, while offering superior sensitivity for specific applications, remain limited by cost, technical requirements, and inability to provide the morphological information that microscopy affords [4].
Future developments in parasitology diagnostics will likely focus on hybrid approaches that leverage the strengths of multiple technologies. The successful implementation of real-time analysis systems in X-ray microscopy [32] suggests similar approaches could benefit optical microscopy in parasitology. Additionally, the standardization of sample processing protocols and DNA extraction methods will be crucial for improving the consistency of molecular methods across different laboratory settings [4]. As these technologies evolve, multicentre validation studies will remain essential for establishing evidence-based guidelines for diagnostic method selection in both clinical and research contexts.
Immunochromatographic rapid diagnostic tests (RDTs) have revolutionized the point-of-care (POC) diagnosis of infectious diseases, particularly in resource-limited settings where access to sophisticated laboratory infrastructure remains constrained [33] [34]. These lateral flow assays provide critical diagnostic capabilities for parasitic diseases such as malaria and filariasis, enabling rapid case detection, treatment initiation, and surveillance activities essential for elimination programs [35] [36]. The Global Programme to Eliminate Lymphatic Filariasis (GPELF) and malaria control programs worldwide rely heavily on these tests for mapping transmission zones, monitoring mass drug administration (MDA) impact, and conducting transmission assessment surveys (TAS) [35] [37].
Within parasitology diagnostic methods research, multicentre studies play a pivotal role in validating RDT performance across diverse epidemiological settings and patient populations. Such studies provide essential evidence on real-world operational characteristics beyond manufacturer claims, including usability, stability under field conditions, and comparative accuracy against reference standards [38] [35] [37]. This guide objectively compares the performance of immunochromatographic tests for malaria and filariasis against alternative diagnostic methods, supported by experimental data from recent field evaluations and laboratory studies.
Performance Comparison of Diagnostic Methods
Malaria Rapid Diagnostic Tests
Table 1: Performance characteristics of malaria RDTs compared to reference standards
| RDT Product | Target Antigens | Reference Standard | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Study Details |
|---|---|---|---|---|---|---|---|
| RightSign RDT | HRP-2, Pv-pLDH | Microscopy | 100 | 98 | 98.2 | 100 | 105 subjects, Indonesia [38] |
| ScreenPlus RDT | HRP-2, Pan LDH | Microscopy | 100 | 98 | 98.2 | 100 | 105 subjects, Indonesia [38] |
| RightSign RDT | HRP-2, Pv-pLDH | Real-time PCR | 75 | 100 | 100 | NR | 105 subjects, Indonesia [38] |
| ScreenPlus RDT | HRP-2, Pan LDH | Real-time PCR | 75 | 100 | 100 | NR | 105 subjects, Indonesia [38] |
| Combined RDTs (HRP-2/pLDH) | HRP-2, pLDH | Microscopy | 93.6 | 99.4 | 84.6 | 99.8 | 1,414 children, UK [39] |
| Combined RDTs (HRP-2/pLDH) | HRP-2, pLDH | PCR (P. falciparum only) | 100 | 98.8 | 69.2 | 100 | 1,414 children, UK [39] |
NR = Not Reported; PPV = Positive Predictive Value; NPV = Negative Predictive Value
Filariasis Rapid Diagnostic Tests
Table 2: Performance characteristics of filariasis RDTs in field studies
| RDT Product | Target | Comparison Method | Concordance (%) | Kappa Statistic | Ag-Positivity (%) | Field Usability | Study Details |
|---|---|---|---|---|---|---|---|
| Filariasis Test Strip (FTS) | W. bancrofti Ag | Microfilariae slides | 100 (Mf-positive cases) | NR | 29.0 | Susceptible to user error | 344 participants, Samoa [37] |
| Q Filariasis Antigen Test (QFAT) | W. bancrofti Ag | Microfilariae slides | 100 (Mf-positive cases) | NR | 30.2 | Preferred for usability | 344 participants, Samoa [37] |
| FTS vs QFAT | W. bancrofti Ag | Paired testing | 93.6 | 0.85 | NR | QFAT required smaller blood volume | 344 participants, Samoa [37] |
| ICT vs FTS | W. bancrofti Ag | Paired testing | 93.8 sensitivity | NR | Variable | FTS more stable in field | 179 individuals, American Samoa [35] |
NR = Not Reported; Ag = Antigen; Mf = Microfilariae
Experimental Protocols and Methodologies
Standardized Testing Protocols for Multicentre Studies
Blood Sample Collection and Processing for Malaria RDT Evaluation In a 2020 Indonesian study evaluating RightSign and ScreenPlus RDTs, researchers collected whole blood samples in EDTA tubes from 105 participants [38]. Each sample underwent parallel testing using four methods: two RDTs (RightSign and ScreenPlus), microscopy of Giemsa-stained thick and thin blood smears, and real-time PCR using the abTESTMMalaria qPCR II kit [38]. The RDTs were performed according to manufacturer instructions, with interpretations made by two blind independent observers to minimize bias [38]. Microscopy examination followed WHO guidelines for species identification and parasitemia calculation, while real-time PCR utilized the Rotor-Gene Q system with species-specific primers and probes [38]. Statistical analysis included McNemar and Kruskal-Wallis tests to compare specificity, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) across methods [38].
Filariasis Test Strip Evaluation Protocol A 2024 Samoan study compared the STANDARD Q Filariasis Antigen Test (QFAT) with the Bioline Filariasis Test Strip (FTS) using 344 finger-prick blood samples collected in heparinized microvettes [37]. Samples were tested simultaneously with both RDTs under field laboratory conditions at 25-32°C [37]. To assess test stability, results were re-read at 1 hour and the next day [37]. Microfilariae status was determined through blood slides prepared from any sample positive by either antigen test [37]. Concordance between tests was calculated, and line intensity was evaluated as a potential predictor of microfilariae positivity [37]. The field team also documented usability preferences based on blood volume requirements, readability, and operational simplicity [37].
Reference Standard Methodologies
Microscopy for Malaria Diagnosis Microscopic examination remains the gold standard for malaria diagnosis in most validation studies [38] [36]. The protocol involves preparing Giemsa-stained thick and thin blood smears, with the thick smear used for parasite detection and the thin smear for species identification [38]. Stained slides are examined under 100× oil immersion objective, counting parasites against white blood cells to calculate parasite density [38]. Quality control requires examination by two independent microscopists, with a third resolving discrepancies [38]. While microscopy allows definitive species identification and parasitemia quantification, its limitations include detection threshold of approximately 50-100 parasites/μL, inter-observer variability, and time-intensive processing [38] [36].
Molecular Methods as Confirmatory Tools Real-time PCR provides higher sensitivity for detecting low-level infections and identifying mixed species infections [38] [3]. The abTESTMMalaria qPCR II kit identifies P. falciparum, P. vivax, P. ovale, P. malariae, and P. knowlesi using species-specific primers and hydrolysis probes with different fluorophores [38]. Similarly, multiplex PCR assays like the Allplex GI-Parasite Assay detect enteric protozoa with sensitivity of 97.2-100% and specificity of 99.2-100% compared to conventional methods [3] [19]. While molecular methods offer superior accuracy, they require specialized equipment, technical expertise, and higher costs, limiting their use as POC tests in resource-limited settings [38] [36].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for parasitology RDT evaluation
| Item | Specification | Research Application | Examples |
|---|---|---|---|
| Rapid Diagnostic Tests | Lateral flow immunochromatographic strips | Primary evaluation devices | RightSign, ScreenPlus (malaria); FTS, QFAT (filariasis) [38] [37] |
| Blood Collection Supplies | EDTA/heparin tubes, microtainers, lancets | Sample acquisition for testing | Heparinized microvettes (300μL for filariasis) [37] |
| Microscopy Materials | Glass slides, Giemsa stain, immersion oil | Reference standard preparation | Giemsa-stained thick/thin blood smears [38] |
| Nucleic Acid Extraction Kits | Commercial DNA/RNA isolation kits | Molecular reference testing | STARMag 96 × 4 Universal Cartridge [19] |
| PCR Master Mixes | Multiplex real-time PCR reagents | Molecular confirmation | Allplex GI-Parasite Assay [3] [19] |
| Thermal Cyclers | Real-time PCR instruments | Amplification and detection | Rotor-Gene Q, Bio-Rad CFX96 [38] [19] |
| Quality Control Materials | Positive/negative control samples | Assay validation | Manufacturer-provided controls [38] [37] |
Discussion and Future Perspectives
Immunochromatographic RDTs represent a cornerstone of parasitic disease management in resource-constrained settings, though their performance characteristics vary significantly between products and target pathogens [38] [35] [37]. The ASSURED criteria (Affordable, Sensitive, Specific, User-friendly, Rapid and robust, Equipment-free, and Deliverable) provide a valuable framework for evaluating POC tests destined for low-resource settings [36]. While current RDTs largely meet the rapid and equipment-free requirements, challenges remain in achieving optimal sensitivity for non-falciparum malaria species and maintaining test stability under extreme environmental conditions [39] [36].
Emerging technologies including microfluidics, nanotechnology, and lab-on-chip platforms promise to enhance future POC diagnostics for parasitic diseases [34] [36]. The integration of image processing and machine learning with mobile technology may revolutionize field-based microscopy, potentially creating hybrid systems that combine the advantages of RDTs with the diagnostic accuracy of microscopy [36]. Furthermore, the development of multiplexed platforms capable of detecting multiple parasitic infections from a single sample would represent a significant advancement for integrated neglected tropical disease programs [34].
For researchers conducting multicentre validations of parasitology diagnostics, standardized protocols, adequate sample sizes, and testing across diverse epidemiological settings remain essential for generating meaningful performance data [38] [35] [37]. Future studies should prioritize direct comparison of next-generation RDTs against both traditional microscopy and molecular reference standards to fully characterize their operational characteristics and limitations across the spectrum of clinical presentations and transmission settings.
Within the evolving landscape of parasitology diagnostics, molecular techniques have progressively supplanted conventional microscopic examination for detecting intestinal protozoa. Multiplex real-time PCR (mqPCR) assays, which allow for the simultaneous detection of multiple pathogens in a single reaction, are at the forefront of this diagnostic shift. This comparison guide objectively evaluates the two primary sources of these assays: commercial kits and in-house (or laboratory-developed) protocols. The context is framed by a growing body of multicentre research that seeks to validate these methods for clinical use, providing scientists and drug development professionals with evidence-based insights for their diagnostic choices. The transition to molecular methods is driven by the need for higher sensitivity, specificity, and throughput, especially during widespread outbreaks where rapid and accurate identification is paramount for public health [40].
Performance Comparison: Commercial vs. In-House mqPCR Assays
The choice between commercial and in-house mqPCR assays involves a careful consideration of performance metrics, including sensitivity, specificity, cost, and validation status. The following tables summarize key comparative data from multicentre studies and validation reports across various pathogens, providing a structured overview of their operational characteristics.
Table 1: Overall Assay Characteristics and Performance
| Feature | Commercial mqPCR Assays | In-House mqPCR Assays |
|---|---|---|
| Standardization | High; standardized reagents and protocols [41] | Variable; dependent on individual laboratory optimization [42] |
| Regulatory Status | Often CE-IVD marked or FDA-approved [43] | Laboratory Developed Tests (LDTs) [40] |
| Development Time | Minimal; ready-to-use | Lengthy; requires design, optimization, and validation [44] |
| Cost per Test | Higher [42] [40] | Significantly lower; affords considerable savings [42] |
| Flexibility | Low; fixed panel of targets | High; can be adapted to specific targets and emerging pathogens [40] |
| Multicentre Consistency | Generally high due to standardization [45] | Requires rigorous validation to ensure inter-laboratory reproducibility [45] |
Table 2: Analytical and Diagnostic Performance from Validation Studies
| Assay Type / Target Pathogen | Reported Sensitivity | Reported Specificity | Key Findings / Concordance | Source (Study Focus) |
|---|---|---|---|---|
| Commercial (AllPlex) for Intestinal Protozoa | N/A (Detection higher than microscopy) | N/A (Detection higher than microscopy) | 909 samples positive by PCR vs. 286 by microscopy; superior detection of Giardia, Cryptosporidium, E. histolytica, D. fragilis, and Blastocystis [41] | Intestinal Protozoa [41] |
| In-House (TaqMan) for Diarrheagenic E. coli | EPEC: 0.96, ETEC: 0.61-0.76, EAEC: 0.54-0.69 [42] | 0.94 - 1.0 [42] | Comparable to commercial test; discordant results associated with low pathogen quantities (late Ct values) [42] | Diarrheagenic E. coli [42] |
| Commercial (AllPlex) for STIs | 98.1% (Overall) [43] | 94.1% (Overall) [43] | High accuracy (96.7%); lowest sensitivity for Trichomonas vaginalis [43] | Sexually Transmitted Infections [43] |
| Commercial (EUROArray) for STIs | 97.1% (Overall) [43] | 84.3% (Overall) [43] | Good accuracy (92.9%); highlights variability between commercial kits [43] | Sexually Transmitted Infections [43] |
| In-House (FMCA-based) for Respiratory Pathogens | LOD: 4.94 - 14.03 copies/μL [40] | 98.81% agreement with reference RT-qPCR [40] | Cost-effective ($5/sample); detected 51.54% positives, including 6.07% co-infections [40] | Respiratory Pathogens [40] |
| In-House vs. Commercial for M. pneumoniae | All five assays could detect ~1 CFU/μL [44] | All assays specific for M. pneumoniae [44] | Significant differences in mean crossing points and calculated genome copies [44] | Mycoplasma pneumoniae [44] |
Experimental Protocols for Key Studies
Commercial Multiplex PCR for Intestinal Protozoa in a Clinical Setting
A large prospective study over three years compared a commercial multiplex qPCR (AllPlex Gastrointestinal Panel Assay, Seegene) with classical microscopy on 3,500 stool samples [41].
- Sample Collection and Processing: All stool samples were analyzed in a routine clinical setting. For microscopy, each sample was examined using two different concentration methods. Acid-fast staining was additionally performed when Cryptosporidium detection was specifically requested.
- Nucleic Acid Extraction and mqPCR: DNA was extracted from stool samples according to standard laboratory procedures. The extracted DNA was then subjected to the commercial AllPlex PCR assay, following the manufacturer's instructions precisely. This panel detects Giardia intestinalis, Cryptosporidium spp., Entamoeba histolytica, Dientamoeba fragilis, and Blastocystis spp., among other targets.
- Data Analysis: Results from PCR and microscopy were directly compared. A sample was considered a true positive for a protozoan if it was detected by either method, acknowledging the higher sensitivity of PCR as the de facto standard [41].
In-House mqPCR Assay for DiarrheagenicE. coli
A comparative study evaluated one commercial and two in-house TaqMan mqPCR assays for detecting enteropathogenic (EPEC), enterotoxigenic (ETEC), and enteroaggregative (EAEC) E. coli [42].
- Sample Panel: The study utilized residual nucleic acid extractions from stool samples from two cohorts: returnees from tropical deployments and migrants from high-endemicity settings.
- PCR Amplification: Each sample was tested with all three PCR assays (one commercial and two in-house) in parallel. The in-house assays were based on previously published TaqMan probe-based protocols targeting specific virulence genes of each E. coli pathotype.
- Statistical Analysis: Since no perfect gold standard was available, the researchers used a latent class model (a statistical approach for method comparison in the absence of a gold standard) to estimate the sensitivity and specificity of each assay. Cycle threshold (Ct) values were compared descriptively, with late Ct values (indicating low target concentration) being closely examined in cases of discordant results [42].
In-House Fluorescence Melting Curve Analysis (FMCA) for Respiratory Pathogens
This protocol highlights the flexibility and cost-saving potential of in-house assays, which is directly applicable to parasitology diagnostics [40].
- Primer and Probe Design: Specific primers and probes for six respiratory pathogens were designed to bind conserved genomic regions. A key feature was the use of tetrahydrofuran (THF) residues in the probes to minimize the impact of base mismatches, enhancing robustness across genetic variants.
- Nucleic Acid Extraction: Automated extraction was performed on nasopharyngeal swab samples. To improve efficiency, samples were centrifuged and washed to remove debris and potential PCR inhibitors.
- Reverse Transcription-Asymmetric PCR and Melting Curve Analysis: The reaction used unequal primer ratios to produce single-stranded DNA, facilitating better probe hybridization. After amplification, a melting curve analysis was performed, where the temperature was gradually increased from 40°C to 80°C. Each pathogen was identified by its specific melting temperature (Tm) peak.
- Analytical Validation: The assay underwent rigorous validation, including determination of the limit of detection (LOD) through probit analysis, precision testing (intra- and inter-assay variability), and specificity testing against a panel of non-target pathogens.
Workflow and Logical Diagrams
The following diagram illustrates the key decision-making pathways and procedural steps involved in selecting and implementing multiplex PCR assays for diagnostic purposes, based on the reviewed studies.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and execution of both commercial and in-house mqPCR assays rely on a core set of reagents and instruments. The following table details these essential components and their functions.
Table 3: Key Research Reagent Solutions for mqPCR Assays
| Item | Function / Application | Specific Examples from Literature |
|---|---|---|
| Nucleic Acid Extraction Kit | Purification of DNA/RNA from clinical samples, a critical step for PCR accuracy. | QIAamp DNA Mini Kit (for M. pneumoniae and E. coli DNA) [42] [44]; Automated systems (e.g., Miracle-AutoXT) for high-throughput processing [46]. |
| PCR Master Mix | Provides enzymes, dNTPs, and buffers necessary for the PCR amplification. | LightCycler FastStart DNA Master HybProbe [44]; 2× Thunderbird probe qPCR mix [46]; One Step U* Mix for reverse transcription-PCR [40]. |
| Primers & Probes | Target-specific oligonucleotides for amplification and detection. Designed to bind conserved genomic regions. | TaqMan probes for E. coli pathotypes [42]; FMCA probes with THF residues for robust variant detection [40]. |
| Positive Control Templates | Validates assay performance and serves as a quantification standard. | Plasmid DNA containing cloned target sequences [46] [40]; Genomic DNA from reference strains (e.g., ATCC cultures) [46] [44]. |
| Real-Time PCR Instrument | Platform for amplification and fluorescent signal detection in real-time. | LightCycler systems [44]; Bio-Rad CFX-96 [46]; Hongshi SLAN-96S/P systems [47] [40]. |
| Commercial Multiplex Panels | Integrated, standardized tests for syndrome-specific pathogen detection. | AllPlex Gastrointestinal Panel Assay (Seegene) [41]; Respiratory Pathogens Multiplex Nucleic Acid Diagnostic Kit [47] [48]. |
The evidence from multicentre studies indicates that both commercial and in-house mqPCR assays are highly effective for the detection of intestinal protozoa and other pathogens, each with distinct advantages. Commercial kits offer a turnkey solution characterized by standardization, ease of use, and reliability, making them ideal for routine clinical laboratories where consistency and regulatory compliance are paramount [41] [43]. Conversely, in-house protocols provide a cost-effective and highly flexible alternative, which is particularly valuable in resource-limited settings, for surveillance of specific pathogen panels, or for rapid adaptation to novel and emerging pathogens [42] [40]. The decision between the two should be guided by the specific context of the diagnostic or research setting, including considerations of budget, required throughput, technical expertise, and the need for panel customization. Ultimately, the convergence of data from both approaches underscores the overarching superiority of molecular diagnostics over traditional microscopy for sensitive and specific detection of intestinal protozoa, while also highlighting that a complementary approach involving microscopy remains necessary to detect pathogens not included in molecular panels, such as helminths and Cystoisospora belli [41].
Automated DNA Extraction and PCR Setup in High-Throughput Laboratories
The shift toward high-throughput molecular diagnostics represents a paradigm change in clinical and research parasitology, directly addressing the critical need for scalable, sensitive, and standardized tools for parasite detection [49] [50]. Traditional microscopic examination, while foundational, is hampered by limitations in sensitivity and reproducibility and is ill-suited for processing the large sample volumes required in modern surveillance programs or drug efficacy studies [50]. Automated DNA extraction systems and advanced PCR technologies have emerged as cornerstone solutions, enabling laboratories to achieve unprecedented levels of efficiency, throughput, and analytical precision. This guide provides a objective comparison of these technologies, framed within the context of multicentre study validation, to aid researchers and drug development professionals in selecting and implementing optimal workflows for parasitology research.
Comparative Analysis of Automated DNA Extraction Systems
Automated DNA extraction systems are engineered to streamline the nucleic acid isolation process, minimizing manual labor, reducing potential for contamination, and enhancing reproducibility—attributes that are indispensable in a high-throughput setting [49].
The global market for automated DNA extraction is characterized by robust growth and technological innovation.
- Market Trajectory: The market is projected to reach an estimated $1,850 million by 2025, growing at a compound annual growth rate (CAGR) of 15.8% through 2033 [49].
- Primary Drivers: This growth is propelled by increasing demand for high-throughput sample processing in research and clinical settings, the rising prevalence of genetic diseases, and a growing emphasis on personalized medicine and pharmacogenomics [49].
- Concentration and Innovation: The market exhibits a moderate to high concentration, with established players like Thermo Fisher Scientific and Qiagen holding a significant combined market share. Innovation is concentrated on improving throughput, sample volume flexibility, and the yield and purity of extracted DNA, with a strong focus on integrating with downstream applications like PCR and next-generation sequencing [49].
System Type Comparison: Semi-Automatic vs. Full-Automatic
The core distinction in automation lies in the degree of human intervention required.
- Semi-Automatic Extraction Systems: These systems automate specific steps but require manual intervention for tasks like sample loading or reagent addition. They offer a balance of automation and flexibility, making them suitable for laboratories with moderate throughput needs or those working with a wide variety of sample types [49].
- Full-Automatic Extraction Systems: These are fully integrated platforms that automate the entire workflow from sample lysis to DNA elution, requiring minimal operator input. Designed for high-throughput, walk-away operation, they ensure maximum efficiency, reproducibility, and reduced risk of cross-contamination, making them ideal for large-scale research and clinical diagnostics [49].
Performance Validation in Parasitology: A Multicentre Perspective
The choice of DNA extraction method profoundly impacts the sensitivity of subsequent PCR detection, particularly for complex sample matrices like stool, which contain PCR inhibitors and parasites with resistant structures (e.g., helminth eggs or microsporidia spores) [51] [26]. Multicentre studies and comparative evaluations are critical for validating performance.
Table 1: Comparative Performance of DNA Extraction Methods for Stool Parasitology
| Extraction Method / Kit | Key Methodology | Performance Findings (Based on Cited Studies) | Ideal for Parasite Types |
|---|---|---|---|
| Phenol-Chloroform (P) [51] | Conventional manual technique using organic solvents. | Provided high DNA yields but resulted in the lowest PCR detection rate (8.2%); largely ineffective for most parasites in the study. | Limited utility for diverse intestinal parasites. |
| Phenol-Chloroform with Bead-Beating (PB) [51] | Manual method with a mechanical pretreatment step using glass beads. | Higher DNA yield than kit methods; improved detection over P alone, but was outperformed by specialized kits [51]. | Helminths with resistant structures. |
| QIAamp Fast DNA Stool Mini Kit (Q) [51] | Commercial silica-membrane based kit. | Lower DNA yield than phenol-chloroform methods; showed better PCR detection than P but was not the most effective [51]. | Routine protozoan detection. |
| QIAamp PowerFecal Pro DNA Kit (QB) [51] | Commercial kit incorporating a bead-beating step in its lysis buffer. | Demonstrated the highest PCR detection rate (61.2%); effectively extracted DNA from all tested parasite groups, including robust helminths [51]. | Broad-spectrum detection, including helminths (e.g., Ascaris lumbricoides, Strongyloides stercoralis) and protozoa [51]. |
| Nuclisens easyMAG [26] | Automated magnetic bead-based system. | In a multicentre study, it showed high detection frequency and low Ct values for low concentrations of Enterocytozoon bieneusi spores [26]. | Microsporidia and other parasites with resistant spores. |
| Quick DNA Fecal/Soil Microbe Microprep Kit [26] | Manual kit utilizing a bead-beating protocol. | Alongside easyMAG, delivered top-tier performance in detecting low spore concentrations in a multicentre comparison [26]. | Microsporidia and soil-transmitted helminths. |
A pivotal study highlights that the QIAamp PowerFecal Pro DNA Kit (QB), which incorporates mechanical beating, achieved a PCR detection rate of 61.2%, far surpassing the 8.2% rate of the conventional phenol-chloroform method [51]. Remarkably, the QB kit successfully detected all tested parasite groups, from fragile Blastocystis sp. to the robust eggs of Ascaris lumbricoides [51].
For the challenging detection of microsporidian spores (Enterocytozoon bieneusi), a multicentre study found that systems combining a robust mechanical pretreatment (bead-beating) with efficient nucleic acid purification, such as the Nuclisens easyMAG and the Quick DNA Fecal/Soil Microbe Microprep Kit, provided the highest detection rates and lowest quantification cycle (Cq) values, especially at low spore concentrations [26].
Workflow: Optimal DNA Extraction from Complex Samples
The following workflow synthesizes the optimal methodology for extracting DNA from stool samples containing diverse parasites, as validated by multicentre studies.
Diagram 1: Workflow for optimal DNA extraction from stool samples for parasitology diagnostics.
Experimental Protocol: DNA Extraction with Mechanical Pretreatment [51] [26]
- Sample Preparation: Aliquot 180-200 mg of stool into a 2 mL tube containing lysing matrix beads (e.g., 0.5 mm glass beads or commercial beads like ZR BashingBeads).
- Lysis and Bead-Beating: Add appropriate lysis buffer. Securely fasten tubes in a bead-beater homogenizer (e.g., TissueLyser II) and process at 30 Hz for 60 seconds [26].
- Incubation: Following bead-beating, incubate the sample at elevated temperature (e.g., 65°C to 95°C) to facilitate complete chemical and enzymatic lysis.
- Nucleic Acid Purification: Transfer the supernatant to an automated extraction system or proceed with a manual kit protocol. Purification is typically achieved via binding to silica membranes or magnetic beads, followed by washes to remove inhibitors.
- Elution: Elute the purified DNA in a low-EDTA Tris buffer or nuclease-free water. The eluate is now ready for PCR analysis.
Comparative Analysis of PCR Systems for Diagnostic Parasitology
Following high-quality DNA extraction, selecting the appropriate PCR technology is critical for accurate detection and quantification.
- Real-Time PCR (qPCR): The workhorse of molecular diagnostics, qPCR allows for the monitoring of amplification in real-time, providing relative quantification of the target nucleic acid. It is widely used for its speed, robustness, and multiplexing capabilities [52] [50].
- Digital PCR (dPCR): A third-generation technology, dPCR provides absolute quantification without the need for a standard curve. By partitioning a sample into thousands of individual reactions, it offers unparalleled sensitivity and resistance to PCR inhibitors, making it ideal for detecting low-abundance targets and for use in complex sample backgrounds [53].
System Comparison and Performance Data
Table 2: Comparative Analysis of Advanced PCR Systems for Parasitology
| PCR System | Technology | Key Features & Specifications | Throughput | Parasitology Application Evidence |
|---|---|---|---|---|
| Applied Biosystems QuantStudio 3 [52] | qPCR | OptiFlex system for precise temperature control, intuitive touchscreen, cloud connectivity, multiplexing (up to 4 dyes). | 96-well or 384-well | Ideal for routine gene expression, pathogen detection, and genotyping; a reliable workhorse for high-throughput screening [52]. |
| Bio-Rad CFX Opus96 [52] | qPCR | Advanced thermal cycling, gradient functionality, BR.io cloud integration, multiplexing (up to 5 targets), factory-calibrated optics. | 96-well | Suited for high-performance, mid-to-high throughput research and clinical labs requiring advanced data analysis for applications like parasite quantification and species identification [52]. |
| Bio-Rad QX200 AutoDG Droplet Digital PCR [52] [53] | ddPCR | Partitions samples into ~20,000 droplets for absolute quantification; automated droplet generation (AutoDG); high sensitivity. | Medium to High | Superior for absolute quantification; detects rare targets and minor resistance alleles; minimizes impact of inhibitors in complex samples (e.g., stool) [52] [53]. |
| BD MAX Enteric Parasite Panel [27] | Fully Automated qPCR | Integrated extraction and amplification; detects Giardia, Cryptosporidium, E. histolytica; minimal hands-on time. | High | Demonstrated 100% specificity and 87.8% sensitivity in clinical validation; excellent for high-volume clinical diagnostics of common protozoa [27]. |
The performance of a fully automated, integrated system like the BD MAX Enteric Parasite Panel has been validated in clinical settings, showing 100% specificity and a sensitivity of 87.8% for detecting major protozoan parasites, demonstrating the practical efficacy of automation in diagnostic parasitology [27].
Digital PCR (dPCR), particularly droplet digital PCR (ddPCR), offers significant advantages for parasitology. Its ability to perform absolute quantification is invaluable for tracking parasite load in intervention studies. Furthermore, its resilience to PCR inhibitors common in stool and environmental samples makes it a powerful tool for detecting low-level infections that might be missed by qPCR [53].
Workflow: Molecular Detection of Parasites in Clinical Samples
The complete diagnostic pathway, from sample receipt to result, integrates the technologies discussed above.
Diagram 2: High-level workflow for molecular detection of parasites, showcasing qPCR and dPCR pathways.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are fundamental to executing the validated protocols discussed in this guide.
Table 3: Essential Research Reagents and Materials for Parasitology Molecular Diagnostics
| Item | Function | Application Note |
|---|---|---|
| Lysing Matrix Beads (e.g., 0.5mm glass beads, ZR BashingBeads) | Mechanical disruption of tough parasite walls (eggs, cysts, spores) during DNA extraction. | Critical for efficient lysis of helminths and microsporidia; optimal performance depends on material, size, and beating protocol [51] [26]. |
| Inhibitor Removal Buffers | Binding and removal of PCR inhibitors (e.g., bilirubin, bile salts, complex carbohydrates) common in stool samples. | A key component of specialized stool DNA extraction kits; essential for achieving robust and reproducible PCR results from complex matrices [51]. |
| Species-Specific Primers & TaqMan Probes | Selective amplification and detection of target parasite DNA in qPCR/dPCR assays. | Designed against unique genetic markers (e.g., ITS, SSU rRNA); hydrolysis probes (TaqMan) provide high specificity and enable multiplexing [53] [50]. |
| Digital PCR Supermixes | Optimized reagent mixtures for efficient amplification in partitioned samples (droplets or wells). | Formulated to generate stable droplets and support robust amplification in dPCR systems, enabling absolute quantification of parasite DNA [53]. |
| External Run Controls (Positive, Negative, Inhibition) | Monitoring PCR performance, detecting contamination, and verifying the absence of inhibition in each run. | Mandatory for ensuring assay validity and reliability in both clinical diagnostics and research settings [27] [50]. |
The integration of automated DNA extraction systems employing mechanical pretreatment and advanced PCR technologies like dPCR represents the current gold standard for high-throughput parasitology diagnostics. Evidence from multicentre studies consistently demonstrates that methods incorporating bead-beating (e.g., QIAamp PowerFecal Pro Kit, Nuclisens easyMAG with pretreatment) significantly enhance detection sensitivity for a broad spectrum of parasites, particularly those with resistant structures. For detection, dPCR offers superior sensitivity and inhibitor tolerance for the most challenging applications, including cryptic infections and resistance monitoring, while automated qPCR panels provide exceptional efficiency for routine, high-volume clinical screening. The continued validation and adoption of these integrated, automated workflows are paramount for advancing parasitology research, enhancing disease surveillance, and accelerating drug development efforts.
The field of medical parasitology is undergoing a profound transformation through the integration of artificial intelligence (AI) and automated image analysis. Traditional diagnostic methods for detecting ova and cysts in stool samples primarily rely on manual microscopy, which is time-consuming, labor-intensive, and subject to inter-observer variability. AI technologies, particularly deep learning and computer vision algorithms, are now enabling rapid, accurate, and high-throughput detection of parasitic elements, revolutionizing both clinical diagnostics and research applications. These emerging frontiers in automated detection are particularly valuable for large-scale screening programs, drug efficacy studies, and multicenter research validation where consistency and reproducibility are paramount.
The adoption of AI in parasitology diagnostics addresses several critical challenges. In resource-limited settings with high parasitic disease burdens, expert microscopists are often scarce, leading to diagnostic delays and potential misidentification. AI systems can function as force multipliers, augmenting the capabilities of available technicians and providing expert-level second opinions. For research scientists and drug development professionals, these technologies offer standardized, quantifiable endpoints for clinical trials and epidemiological studies, enabling more robust comparisons across different study sites and populations. The integration of federated learning approaches, as demonstrated in other medical imaging domains, further allows for collaborative model improvement while maintaining data privacy across multiple institutions—a particularly valuable feature for multicenter validation studies.
Comparative Performance of AI Diagnostic Platforms
Quantitative Comparison of AI Diagnostic Performance
Table 1: Performance metrics of various AI-assisted diagnostic platforms in detecting parasitic elements
| Platform/Model | Accuracy (%) | Sensitivity (%) | Specificity (%) | AUC | Remarks |
|---|---|---|---|---|---|
| Multi-model AI Framework (Malaria) [54] [55] | 96.47 | 96.03 | 96.90 | - | Combined DL models with majority voting |
| YOLOv3 (Malaria) [56] | 94.41 | - | - | - | False negative: 1.68%; False positive: 3.91% |
| miLab MAL (Malaria) [57] | - | 100 | 100 | - | Superior to standard microscopy (81.8% sensitivity) |
| FedEmbryo (IVF) [58] | - | - | - | 0.80 | Internal test set; 0.76 in external validation |
| AI Ultrasound (HP Diagnosis) [59] | 92.4 | 94.2 | 88.4 | 0.835 | Superior to traditional ultrasound (AUC=0.696) |
Table 2: Comparative analysis of AI model architectures for medical image analysis
| Model Architecture | Technical Approach | Advantages | Limitations |
|---|---|---|---|
| Multi-model Fusion [54] [55] | Ensemble of 3 DL models with majority voting | 96.47% accuracy, reduced misclassification | Computational complexity |
| YOLOv3 [56] | Single-stage detector for real-time recognition | 94.41% accuracy, rapid processing | Lower performance vs. newer YOLO versions |
| Federated Task-Adaptive Learning [58] | Combines multi-task learning with federated learning | Data privacy preservation, handles non-IID data | Requires synchronous training across centers |
| AI-assisted Ultrasound [59] | CNN-based image analysis model | AUC 0.835, 94.2% sensitivity when combined | Dependent on image acquisition quality |
Experimental Protocols and Methodologies
Detailed Methodologies for AI Model Development and Validation
Multi-Model AI Framework Development
The high-performance multi-model AI framework achieving 96.47% accuracy in malaria detection employed a sophisticated methodology integrating multiple deep learning architectures [54] [55]. Researchers utilized an extensive dataset of 27,558 blood smear images, implementing a strategic fusion approach where three distinct deep learning models performed feature extraction independently. The framework incorporated a majority voting mechanism for final classification decisions, effectively reducing misclassification risk. This ensemble approach demonstrated statistically significant improvement over any single model, with reported sensitivity of 96.03%, specificity of 96.90%, and precision of 96.88%. The implementation emphasized computational efficiency to ensure potential deployment in resource-constrained settings, requiring no specialized equipment for operation.
YOLOv3-Based Detection Protocol
The YOLOv3 implementation for Plasmodium falciparum recognition followed a meticulously optimized protocol [56]. Researchers collected thin blood smears from patients with confirmed malaria infections, followed by comprehensive image preprocessing using sliding window cropping and resizing to 416×416 pixels. The model training employed an 8:1:1 dataset split (training:validation:test) with a batch size of 16 adapted to GPU memory constraints. Learning rate was managed via cosine decay strategy for stable convergence, with training continuing for up to 300 epochs and early stopping implemented if no improvement was observed after 50 epochs. This approach achieved 94.41% overall recognition accuracy with a false negative rate of 1.68% and false positive rate of 3.91%. The protocol specifically addressed challenging differentiation between malaria parasites and similarly shaped components like platelets through meticulous labeling.
Federated Learning Implementation for Multi-Center Studies
The FedEmbryo system demonstrates a highly relevant approach for multi-center validation studies while addressing data privacy concerns [58]. This federated task-adaptive learning (FTAL) framework incorporates a Hierarchical Dynamic Weight Adaptation (HDWA) mechanism that dynamically balances task attention and aggregation weights based on continuous learning feedback (loss ratios). Each participating center maintains a unified client architecture with shared layers and task-specific layers, enabling simultaneous processing of single tasks (e.g., specific parasite detection) and multiple tasks (e.g., comprehensive morphological assessment). The system dynamically adjusts weights for different tasks during local training and assigns appropriate aggregation weights during center model combination, effectively addressing the non-IID data distribution challenges common in multi-center parasitology studies. This approach has demonstrated performance improvements of up to 26.47% over local models in validation studies.
Validation Protocols for Multi-Center Studies
Robust validation of AI models for ova and cyst detection across multiple research centers requires standardized protocols that account for inter-site variability while maintaining methodological consistency [58]. The FedEmbryo implementation established a comprehensive framework in which each participating center maintained complete data privacy, with only model updates (not raw data) shared during the federated learning process. External validation cohorts were utilized to assess model generalizability, with performance metrics separately reported for internal and external test sets. This approach demonstrated the system's robustness, with the federated model achieving an AUC of 0.80 on internal tests and 0.76 on external validation sets—significantly outperforming single-center models. For parasitology applications, similar validation frameworks would include standardized staining protocols, consistent imaging parameters, and harmonized annotation guidelines across participating centers.
Visualization of Workflows and Architectures
Diagram 1: Multi-model AI workflow for parasite detection
Diagram 2: Federated learning architecture for multi-center studies
Essential Research Reagent Solutions
Table 3: Essential research reagents and materials for AI-based parasitology diagnostics
| Reagent/Material | Function | Application Example |
|---|---|---|
| Standardized Staining Reagents | Enhance contrast for parasitic structures | Differentiation of ova/cysts from background |
| Digital Whole Slide Imaging Systems | High-resolution digitization of samples | Creating training datasets for AI models |
| Annotated Reference Datasets | Ground truth for model training/validation | Multi-center study standardization |
| Data Augmentation Algorithms | Increase dataset diversity/robustness | Improving model generalization |
| Model Explainability Tools (e.g., SHAP, IG) | Interpret AI decisions | Clinical validation and trust building |
| Federated Learning Frameworks | Privacy-preserving multi-center collaboration | FedEmbryo-like implementations [58] |
The integration of AI and automated image analysis for ova and cyst detection represents a paradigm shift in parasitology diagnostics with profound implications for multi-center research validation. As demonstrated by performance metrics across various medical imaging domains, AI systems can achieve diagnostic accuracy exceeding 96% while maintaining high sensitivity and specificity. The implementation of federated learning frameworks addresses critical concerns regarding data privacy in multi-center studies while enabling collaborative model improvement. For researchers and drug development professionals, these technologies offer standardized, quantifiable endpoints essential for robust clinical trials and epidemiological studies. Future developments will likely focus on expanding model capabilities to encompass a broader spectrum of parasitic organisms, further improving generalization across diverse populations, and streamlining deployment in resource-constrained settings where the burden of parasitic diseases is highest.
Overcoming Diagnostic Hurdles: Quality Assurance and Technical Optimization
Establishing a Comprehensive Quality Assurance (QA) Program
In parasitology research, a Comprehensive Quality Assurance (QA) Program is fundamental for ensuring the reliability, reproducibility, and accuracy of diagnostic data, particularly in multicentre studies where standardization across different laboratories is a significant challenge. The core objective of such a QA program is to implement a structured system of processes and controls that minimizes variability and error, thereby strengthening the validity of scientific findings. This is especially critical when comparing the performance of different diagnostic methods, where consistent protocols and stringent quality controls are prerequisites for a fair and meaningful comparison. Framing this within the context of multicentre validation—a gold-standard approach for assessing diagnostic methods under real-world conditions—this guide will objectively compare common parasitological techniques, supported by experimental data, and detail the essential components of an effective QA framework.
Comparative Analysis of Parasitological Diagnostic Methods
The choice of diagnostic method in parasitology involves trade-offs between sensitivity, specificity, speed, and cost. A multicentre approach is invaluable for validating these methods across different laboratory settings, operators, and sample populations, providing a robust assessment of their real-world performance.
Performance Comparison of Coproparasitological Techniques
A cross-sectional study comparing three common coproparasitological techniques—Ritchie’s method, direct wet mount, and the Paratest system—for diagnosing intestinal parasites in patients with malabsorption syndrome demonstrated significant differences in performance [60].
Table 1: Comparison of Coproparasitological Techniques for Protozoan Infections
| Diagnostic Method | Sensitivity for Protozoa in General | Specificity | Agreement with Consensus (Kappa Index) | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Ritchie’s Method | 100% | 100% | 0.81 (vs. Direct wet mount) | Superior for detecting commensal protozoa; high sensitivity [60]. | Requires use of formalin and ether [60]. |
| Direct Wet Mount | 78.1% | 100% | 0.84 (vs. Paratest) | Rapid, simple, and low-cost [60]. | Lower sensitivity for general protozoan infections [60]. |
| Paratest System | 78.1% | 100% | 0.81 (vs. Ritchie) | Commercial sedimentation system; easy to perform [60]. | Lower sensitivity, particularly for non-pathogenic commensals [60]. |
The study, which used a consensus result from all three methods as the "gold standard," found that Ritchie’s formalin-ether concentration technique was significantly superior to both the Paratest and direct wet mount for identifying infections with protozoa in general and commensals specifically [60]. The degree of agreement between methods was almost perfect for pathogenic protozoa, underscoring the importance of selecting a method fit for the specific diagnostic question [60].
Performance Comparison of Visual, Morphometric, and Molecular Identification
A double-blind, multicentre trial assessed the efficiency of visual, morphometric, and molecular techniques for identifying the notifiable fish pathogen Gyrodactylus salaris, simulating real-world outbreak conditions [61].
Table 2: Multicentre Comparison of G. salaris Identification Methods
| Identification Method | Probability of Correctly Identifying G. salaris | Key Findings from Multicentre Testing |
|---|---|---|
| Visual Identification by Expert | 81% | The most experienced salmonid gyrodactylid expert correctly identified 95.1% of specimens, but this level of skill is rare [61]. |
| Morphometric Statistical Classification | 58% | Demonstrated a need for wider training; highly dependent on specimen quality and measurement precision [61]. |
| Molecular (ITS-RFLP/COI sequencing) | 92% | Conducted in the most experienced lab, identified 100% of true G. salaris; highest accuracy and reliability [61]. |
The study also revealed practical bottlenecks, such as the time required for specimen preparation [62]. Based on these findings, a tiered QA protocol was recommended: during routine surveillance with low specimen numbers, all specimens should be analysed with molecular methods; during suspected outbreaks with high volume, initial visual screening to select "G. salaris-like" specimens should be followed by molecular confirmation [61].
Validation of Molecular Diagnostics in Low-Endemic Areas
Evaluating molecular diagnostics with clinical samples in low-endemic areas is challenging due to the lack of positive samples. A 2025 study used simulated stool samples spiked with known pathogens to validate the BD MAX Enteric Parasite Panel (EPP), a fully automated multiplex PCR test [27].
Table 3: Performance of BD MAX Enteric Parasite Panel with Simulated Samples
| Parasite | Limit of Detection (LoD) | Concordance at LoD | Overall Sensitivity | Overall Specificity |
|---|---|---|---|---|
| Giardia lamblia | 781 cysts/mL | 100% at ≥6,250 cysts/mL | 87.8% (for the entire panel) | 100% [27] |
| Cryptosporidium parvum | 6,250 oocysts/mL | 50-75% at LoD; 100% at 10x LoD | 70.6% (for C. parvum) | 100% [27] |
| Entamoeba histolytica | 125 DNA copies/mL | Information Missing | Information Missing | Information Missing |
The study concluded that the BD MAX EPP showed good performance for clinical use and that spiked samples are a useful QA strategy for evaluating protozoan PCR assays in low-incidence regions [27]. This approach provides a model for how to rigorously validate new technologies even when natural clinical samples are scarce.
Experimental Protocols for Method Validation
The following are detailed methodologies for key experiments cited in the comparison guides, which can serve as templates for robust QA protocol design.
Multicentre Protocol for Gyrodactylus Species Identification
This protocol was designed to test visual, morphometric, and molecular identification methods under double-blind conditions across multiple expert centres [61] [62].
- Specimen Collection and Preparation: Gyrodactylus specimens were collected from 28 UK sites from various salmonid hosts. Infected fish were screened, and parasites were removed using needles and forceps. A total of 389 specimens were processed, with each specimen assigned a unique identifier and distributed to participating laboratories [62].
- Visual Identification: Specimens were mounted on slides and examined by a panel of expert parasitologists. Identifications were based on the morphology of the haptoral attachment hooks [61] [62].
- Morphometric Analysis: For each specimen, ten key morphological features of the haptoral hooks were measured using digital image analysis. These measurements were processed using statistical classifiers (e.g., Linear Discriminant Analysis) to assign species identity [61] [62].
- Molecular Characterization: DNA was extracted from individual specimens. Two molecular techniques were employed:
- ITS-RFLP: The ITS rDNA region was amplified by PCR and digested with restriction enzymes to generate species-specific banding patterns [61].
- COI Sequencing: The cytochrome c oxidase I (COI) gene was amplified and sequenced. Sequences were compared to reference sequences in databases for species identification [61].
- Data Analysis and Consensus Identity: A "true" consensus identity for each specimen was established by combining the results from all three methods alongside host and location data. The performance of each method was assessed against this consensus [61].
Protocol for Comparing Coproparasitological Techniques
This protocol outlines the comparison of three stool diagnostic techniques in a clinical setting [60].
- Study Population and Sample Collection: The study included 82 adult patients with symptoms of intestinal malabsorption. From each patient, three consecutive stool samples were collected [60].
- Sample Processing and Analysis: Each stool sample was divided and processed in parallel by three techniques:
- Direct Wet Mount: A smear of fresh stool was examined microscopically in saline and/or iodine [60].
- Ritchie’s Formalin-Ether Concentration: Stool was fixed in formalin, concentrated by ether sedimentation, and the sediment examined microscopically [60].
- Paratest System: A commercial sedimentation concentration method was used according to the manufacturer's instructions, and the sediment was examined [60].
- Gold Standard and Statistical Analysis: A sample was considered a "true positive" if it was positive by any of the three methods. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and Kappa index (KI) for agreement were calculated for each technique against this composite standard [60].
Essential Diagrams for Diagnostic Workflows and QA
QA Protocol for Suspected Parasite Outbreak
This workflow visualizes the tiered QA protocol for identifying a notifiable pathogen, balancing speed and accuracy during a high-volume incident [61].
Establishing a QA Framework for Diagnostic Studies
This diagram outlines the key, interconnected stages of a comprehensive QA program for untargeted sciences like metabolomics, which is directly applicable to parasitology diagnostics [63].
The Scientist's Toolkit: Key Research Reagent Solutions
The following reagents and materials are critical for executing the experimental protocols described in this guide and ensuring QA in parasitology diagnostics.
Table 4: Essential Research Reagents for Parasitology Diagnostics
| Reagent/Material | Function in QA and Diagnostics | Example Application in Protocol |
|---|---|---|
| Formalin & Ether | Used in concentration techniques to fix specimens and separate debris from parasitic elements via sedimentation [60]. | Ritchie's method for concentrating cysts, oocysts, and helminth eggs from stool samples [60]. |
| Specific Primers & Probes | Oligonucleotides designed to bind to unique DNA sequences of target parasites, enabling specific amplification and detection in PCR assays [27]. | BD MAX Enteric Parasite Panel for detecting Giardia, Cryptosporidium, and Entamoeba histolytica [27]. |
| Restriction Enzymes | Enzymes that cut DNA at specific sequences, generating fragment length polymorphisms (RFLP) that can discriminate between species [61]. | ITS-RFLP protocol for differentiating between Gyrodactylus salaris and G. thymalli [61]. |
| Reference DNA Sequences | Curated genomic data from authoritative databases (e.g., GenBank) used as a benchmark for validating and comparing newly generated sequences [61]. | Confirming species identity by comparing sequenced COI gene fragments to reference data [61]. |
| Certified Reference Materials | Commercially available, standardized samples containing a known quantity of parasites (e.g., cysts, oocysts), essential for determining LoD and validating assays [27]. | Spiking stool samples to create simulated positive samples for validating the BD MAX EPP in a low-endemic setting [27]. |
Navigating DNA Extraction Challenges from Robust Parasite Cysts and Oocysts
The accurate detection and identification of protozoan parasites such as Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica represents a significant challenge in clinical and food safety laboratories worldwide. These challenges stem primarily from the robust physical structure of parasite cysts and oocysts, which have evolved to protect the genetic material within from environmental stressors. The thick, chitinous walls of these forms act as formidable barriers to efficient DNA extraction, ultimately impacting the sensitivity of downstream molecular applications [4] [3]. In the context of multicentre studies, where standardization is paramount for validating diagnostic methods, the inconsistency in DNA extraction efficiency across different platforms and protocols introduces substantial variability that can compromise the reliability of comparative data [4] [64].
The limitations of traditional diagnostic methods have intensified the need for improved molecular approaches. Microscopy, long considered the gold standard, suffers from limitations in sensitivity and specificity and requires considerable expertise, particularly for differentiating between morphologically similar species [4] [3]. Immunoassays, while useful, may also yield false positives or negatives [4]. Molecular diagnostics, especially PCR-based methods, offer a path to greater sensitivity and specificity. However, their effectiveness is entirely contingent on the release of amplifiable DNA from the resilient cyst and oocyst walls, making the initial extraction step the most critical bottleneck in the entire workflow [65] [66]. This article will objectively compare the performance of various DNA extraction methodologies and technologies, presenting experimental data from recent multicentre studies to guide researchers in selecting and optimizing protocols for robust parasitological diagnostics.
Comparative Analysis of DNA Extraction Method Performance
The performance of different DNA extraction methods varies significantly based on the parasite species, the complexity of the sample matrix (e.g., stool, food, water), and the specific technology employed. The following tables summarize key performance metrics from recent studies.
Table 1: Performance of Commercial Multiplex PCR Assays for Protozoan Detection in Stool Samples
| Assay Name | Target Parasites | Sensitivity (%) | Specificity (%) | Study Characteristics |
|---|---|---|---|---|
| Allplex GI-Parasite Assay [3] [19] | G. duodenalis | 100 | 99.2 | Multicentre, 368 samples, compared to microscopy & EIA |
| Cryptosporidium spp. | 100 | 99.7 | ||
| E. histolytica | 100 | 100 | ||
| D. fragilis | 97.2 | 100 | ||
| BD MAX Enteric Parasite Panel [27] | G. lamblia | 100* | 100 | Simulated samples, low endemic area |
| C. parvum | 70.6-100 | 100 | ||
| E. histolytica | 100* | 100 | ||
| Automated High-Throughput (Seegene) [19] | G. lamblia | 100 | 98.9 | 461 unpreserved specimens |
| Cryptosporidium spp. | 100 | 100 | ||
| D. fragilis | 100 | 99.3 | ||
| B. hominis | 93 | 98.3 | ||
| E. histolytica | 33.3-75* | 100 |
*At concentrations exceeding 6,250 cysts/mL. Sensitivity was concentration-dependent: 50-75% at 6,250 oocysts/mL and 89-100% at 62,500 oocysts/mL. *Sensitivity was 33.3% for fresh specimens and increased to 75% when frozen specimens were included.
Table 2: Comparison of DNA Extraction Methods for Specific Parasites
| Method/Kits | Parasite | Key Findings | Reference |
|---|---|---|---|
| Phenol-Chloroform Isoamyl alcohol | G. duodenalis | Highest DNA concentration; 70% diagnostic sensitivity. | [66] |
| QIAamp DNA Stool Mini Kit | G. duodenalis | Best DNA purity (A260/230); 60% diagnostic sensitivity. | [66] |
| YTA Stool DNA Isolation Mini Kit | G. duodenalis | 60% diagnostic sensitivity. | [66] |
| OmniLyse Lysis + Acetate Precipitation | C. parvum | Enabled detection of as few as 100 oocysts in 25g lettuce. | [65] [67] |
| Nuclisens easyMAG | E. bieneusi | One of the best performances for low spore concentrations. | [64] |
| Quick DNA Fecal/Soil Microbe Microprep | E. bieneusi | One of the best performances for low spore concentrations. | [64] |
Detailed Experimental Protocols and Methodologies
Metagenomic Detection from Leafy Greens
A 2025 study developed a sensitive metagenomic next-generation sequencing (mNGS) assay for detecting parasites on lettuce, with a critical focus on overcoming the DNA extraction barrier [65] [67].
- Sample Preparation: Romaine lettuce leaves (25 g) were experimentally spiked with varying numbers (as few as 100) of C. parvum oocysts, G. duodenalis cysts, or T. gondii oocysts. Parasites were washed from the lettuce surface using buffered peptone water with 0.1% Tween in a stomacher. The wash fluid was filtered and centrifuged to pellet the oocysts/cysts [65].
- Lysis and DNA Extraction: The pellet was resuspended and lysed using the OmniLyse device, which achieved efficient mechanical disruption of the robust walls within 3 minutes. DNA was then purified from the lysate using acetate precipitation [65] [67].
- Whole Genome Amplification: Given the low yield of DNA from small numbers of parasites, the extracted DNA was subjected to whole genome amplification to generate sufficient quantities (0.16–8.25 μg, median = 4.10 μg) for sequencing [65].
- Sequencing and Analysis: The amplified DNA was sequenced using both MinION (Oxford Nanopore) and Ion GeneStudio S5 platforms. The resulting sequence data was analyzed using the CosmosID bioinformatics platform for microbial identification [65] [67].
This protocol highlights the successful combination of a rapid mechanical lysis device with a chemical precipitation method to enable highly sensitive detection of parasites from a complex food matrix.
Multicenter Comparison of DNA Extraction for Microsporidia
A 2024 multicenter study specifically evaluated seven different DNA extraction methods for the detection of Enterocytozoon bieneusi spores in stool, focusing heavily on the mechanical pretreatment step [64].
- Sample Matrix: Stool samples spiked with defined concentrations of E. bieneusi spores (from 5 to 5,000 spores/mL).
- Compared Methods: The study compared seven methods from five different centers, varying the grinder (TissueLyser II, FastPrep-24, MagnaLyser, Vortex), bead type (glass, ceramic, silica, garnet), and DNA extraction kit/manual protocol [64].
- Optimal Parameters: The best analytical performance for detecting low spore concentrations was achieved with methods using strong, short bead-beating (e.g., 30-60 seconds at high speed) with small, heterogeneous beads (e.g., 0.1 and 0.5 mm ZR BashingBeads or a mix of ceramic and silica beads). The Nuclisens easyMAG lysis buffer and the Quick DNA Fecal/Soil Microbe Microprep kit yielded the highest detection frequencies and lowest Ct values [64].
- Key Finding: The study concluded that the mechanical pretreatment step was a decisive factor in extraction efficiency, with optimal performance requiring a protocol that aggressively disrupts the resilient spore wall.
This comparative design provides a robust framework for evaluating extraction components and identifies specific parameters that maximize recovery of nucleic acids from resistant parasite forms.
Diagram 1: Generalized Workflow for DNA Extraction from Parasite Cysts and Oocysts. The critical lysis and extraction steps requiring optimization for robust walls are highlighted.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful nucleic acid extraction from resilient parasite forms relies on a suite of specific reagents and instruments. The following table details key solutions identified in the reviewed studies.
Table 3: Key Research Reagent Solutions for DNA Extraction from Cysts and Oocysts
| Item Name | Category | Function & Application Notes | Evidence/Study |
|---|---|---|---|
| OmniLyse Device | Mechanical Lysis | Rapid (3-min) mechanical disruption of oocysts/cysts for metagenomic sequencing. | [65] [67] |
| ZR BashingBeads (0.1 & 0.5 mm) | Beads | Small, heterogeneous beads for efficient breakdown of microsporidia spore walls. | [64] |
| Nuclisens easyMAG Lysis Buffer | Lysis Buffer | Used in a protocol achieving top performance for low-concentration E. bieneusi spores. | [64] |
| Quick DNA Fecal/Soil Microbe Microprep Kit | DNA Extraction Kit | Effective for DNA extraction from microsporidia spores in stool samples. | [64] |
| QIAamp DNA Stool Mini Kit | DNA Extraction Kit | Provides high-purity DNA, though diagnostic sensitivity for Giardia may be lower than other methods. | [66] |
| Allplex GI-Parasite Assay | Multiplex PCR Assay | Automated high-throughput PCR panel showing high sensitivity/specificity for common enteric protozoa. | [3] [19] |
| BD MAX Enteric Parasite Panel | Automated PCR System | Fully automated assay for detecting G. duodenalis, C. parvum/hominis, and E. histolytica. | [27] |
Diagram 2: Multicenter Study Framework for Method Validation. This design uses standardized samples to objectively compare different extraction methods across multiple laboratories.
The data from recent multicentre studies consistently demonstrates that navigating the challenges of DNA extraction from robust parasite cysts and oocysts requires a deliberate and optimized approach. The choice of method presents a trade-off: while traditional chemical methods like PCI can yield high concentrations of DNA, automated commercial kits and integrated platforms offer superior purity, standardization, and throughput, which are critical for large-scale surveillance and clinical diagnostics [66] [19]. The decisive factor for success, particularly with the most resilient parasites like Cryptosporidium oocysts and microsporidial spores, is the incorporation of an effective mechanical pretreatment step, with bead-beating emerging as a highly effective strategy [65] [64].
The future of parasitology diagnostics is firmly rooted in molecular methods. The trend is moving toward fully automated, high-throughput multiplex systems that can simultaneously detect a broad panel of pathogens from minimal sample input [3] [19]. For widespread adoption, future research and development must focus on further standardizing the pre-analytical phase, particularly the sample preparation and lysis steps, to ensure consistency across different laboratories and settings. Furthermore, reducing the cost and complexity of advanced techniques like mNGS will open the door for its use not just in outbreak investigations but also in routine surveillance, ultimately strengthening our ability to control and prevent parasitic infections globally.
Optimizing Sample Collection, Storage, and Preservation Media
In the field of parasitology diagnostics, the reliability of molecular and morphological detection is fundamentally dependent on the methods used for sample collection, storage, and preservation. This is particularly critical in multicentre studies, where standardized protocols are essential for ensuring comparable and valid results across different research sites. The choice of preservation medium can significantly impact DNA recovery for molecular assays and morphological integrity for microscopic identification. This guide objectively compares the performance of various preservation media, drawing on experimental data from recent multicentre and comparative studies to inform researchers, scientists, and drug development professionals in the field of parasitology diagnostic research.
Comparative Analysis of Preservation Media Performance
The effectiveness of preservation media is evaluated based on their ability to maintain the integrity of parasitic elements—whether DNA for molecular diagnostics or morphology for microscopic examination—under varying storage conditions and durations. The table below summarizes key performance metrics for common preservation methods, derived from experimental data.
Table 1: Performance Comparison of Fecal Sample Preservation Media for Parasite Diagnostics
| Preservation Medium | Primary Use Case | DNA Integrity (PCR Performance) | Morphological Preservation | Optimal Storage Temperature | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| 95% Ethanol | Molecular diagnostics (STH, protozoa) | Effective; minimal Cq increase at 32°C over 60 days [68] | Good for eggs; dehydrates and brittles larvae [69] | 4°C to 32°C (with protection) [68] | Low cost, readily available, low toxicity [68] | Dehydrates tissues; suboptimal for larval morphology [69] |
| 10% Formalin | Microscopy, morphology | Poor; causes DNA fragmentation [69] | Excellent; considered a gold standard for morphology [69] | Ambient | Excellent tissue fixation, cost-effective [69] | Toxic; not suitable for downstream molecular work [69] |
| Silica Gel Beads | Molecular diagnostics (STH) | Effective for hookworm DNA at 32°C [68] | Not typically assessed for morphology | Ambient | Non-toxic, stable at room temperature [68] | Requires a two-step desiccation process for best results [68] |
| Potassium Dichromate | Molecular diagnostics (STH, Giardia) | Effective for hookworm DNA at 32°C [68] | Not typically assessed for morphology | Ambient | Proven efficacy for specific parasites [68] | Toxic and requires careful handling [68] |
| RNAlater | Molecular diagnostics | Some protective effect at 32°C [68] | Not typically assessed for morphology | -20°C (long-term) | Stabilizes nucleic acids [68] | Higher cost compared to ethanol [68] |
| FTA Cards | Molecular diagnostics (STH) | Effective for hookworm DNA at 32°C [68] | Not applicable | Ambient | Easy to transport and store [68] | Limited to small sample quantities [68] |
Experimental Protocols and Workflows
To ensure the validity of data in multicentre studies, it is crucial to adhere to standardized experimental protocols. The following workflows and methodologies are derived from published studies comparing preservation techniques.
Protocol for Evaluating DNA Preservation Efficacy
A study evaluating preservation techniques for soil-transmitted helminth (STH) diagnostics provides a robust methodology for assessing DNA integrity [68].
Methodology:
- Sample Preparation: A naive human stool sample from a single donor was used to create 628 aliquots of 50 mg each. Each aliquot was spiked with a suspension containing approximately 20 Necator americanus (hookworm) eggs.
- Preservation and Storage: The spiked samples were preserved using seven different commercial products (including 95% ethanol, potassium dichromate, silica beads, RNAlater, and FTA cards) and a no-preservative control. These were compared against a "gold standard" of immediate freezing at -20°C.
- Storage Conditions: For each preservative, samples were stored at two temperatures: 4°C (refrigerated) and 32°C (simulating tropical ambient temperature). Samples were analyzed at multiple time points: 1, 7, 30, and 60 days post-preservation.
- DNA Extraction and Analysis: DNA was extracted from all samples at the designated time points. The effectiveness of preservation was measured using quantitative real-time PCR (qPCR) to detect target hookworm DNA. The primary metric was the efficiency of DNA amplification, reflected by the Cq (quantification cycle) values.
Protocol for Comparing Morphological Preservation
A study on wild capuchin monkeys directly compared the morphological preservation of parasites in ethanol versus formalin [69].
Methodology:
- Sample Collection: Fresh fecal samples were collected and immediately divided into two halves.
- Preservation: One half was stored in 96% ethanol, and the other in 10% buffered formalin. All samples were stored at ambient temperature for 8-19 months before analysis.
- Microscopic Analysis: Samples were processed using a modified Wisconsin sedimentation technique. The resulting pellets were screened microscopically for parasite eggs and larvae.
- Preservation Scoring: A standardized three-point degradation grading scale was developed for both ethanol and formalin. Parasites were graded based on the integrity of their cuticle (larvae), shell (eggs), and the visibility of internal structures.
Workflow for a Multicentre Molecular Study
A multicentre study comparing commercial and in-house PCR tests for intestinal protozoa outlines a typical diagnostic validation workflow [4].
Diagram Title: Multicentre Molecular Diagnostic Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Successful parasitology research and diagnostics depend on a suite of essential reagents and materials. The table below details key solutions used in the featured experiments.
Table 2: Essential Research Reagents for Parasitology Sample Processing
| Reagent / Material | Function in Research | Example Use Case |
|---|---|---|
| 95% Ethanol | Preserves nucleic acids by dehydrating samples and deactivating nucleases. | Recommended as a pragmatic field preservative for stool samples intended for PCR-based detection of STHs [68]. |
| 10% Buffered Formalin | Cross-links proteins to preserve morphological structures of parasites. | Gold standard for preserving parasite eggs and larvae for microscopic identification [69]. |
| S.T.A.R. Buffer | Stabilizes nucleic acids in stool samples for transport and storage. | Used in DNA extraction protocols to homogenize stool samples before automated nucleic acid extraction [4]. |
| Silica Gel Beads | Desiccate samples by absorbing moisture, preserving DNA at ambient temperature. | Used in a two-step desiccation process to preserve hookworm DNA in stool without a cold chain [68]. |
| FTA Cards | Chemically treated cards for room-temperature collection and preservation of DNA. | Effective for preserving hookworm DNA from stool samples for molecular detection [68]. |
| Para-Pak Preservation Media | Commercial medium containing fixatives to preserve parasite morphology for microscopy. | Used in multicentre studies to store stool samples before concentration and microscopic examination [4]. |
| MagNA Pure Kits | Automated, magnetic bead-based system for high-throughput nucleic acid extraction. | Used to extract DNA from stool samples in a multicentre comparison of PCR assays [4]. |
| TaqMan Master Mix | Ready-to-use reaction mix for sensitive and specific qPCR amplification. | Used in both commercial and in-house RT-PCR assays to detect protozoan DNA [4]. |
Discussion and Data Interpretation
The experimental data reveals critical trade-offs that guide the selection of preservation media.
- Molecular vs. Morphological Diagnostics: The choice between media like ethanol and formalin is fundamentally dictated by the analytical endpoint [68] [69]. For multicentre studies aiming to use both methods, splitting the sample and preserving in both media is a recommended strategy [69].
- Impact of Storage Conditions: Temperature and time are critical factors. One study found that at 4°C, DNA amplification efficiency remained high for 60 days regardless of the preservative used. At 32°C, however, significant differences emerged, with FTA cards, potassium dichromate, and silica beads performing best [68]. Furthermore, one study noted that PCR results from preserved stool samples were better than those from fresh samples, likely due to improved DNA stability in the preservative medium [4].
- Considerations for Multicentre Studies: Beyond pure performance, factors like cost, toxicity, shipping requirements, and labor are paramount when standardizing protocols across multiple sites. 95% ethanol often represents a balanced choice, offering effective DNA preservation, low cost, and relative safety [68].
The optimization of sample collection, storage, and preservation media is a cornerstone of robust parasitology diagnostics, especially in a multicentre validation context. The experimental data demonstrates that no single preservative is universally superior; 95% ethanol excels for cost-effective molecular screening, formalin remains indispensable for morphological studies, and specialized media like silica gels offer non-toxic alternatives for DNA stabilization. The selection of an appropriate preservation strategy must be a deliberate decision, guided by the diagnostic targets, intended analytical methods, logistical constraints of the study sites, and the imperative for standardized protocols to ensure the validity and reproducibility of research outcomes across all centres.
Addressing Inhibitors in Stool Samples for Molecular Assays
Molecular assays have revolutionized the detection of gastrointestinal pathogens, offering greater sensitivity and specificity than traditional microscopic examination [70] [3]. However, the accurate detection of enteric protozoa and other stool-based pathogens using molecular methods such as PCR is significantly hampered by the presence of inhibitory substances in stool samples. These inhibitors, which include complex polysaccharides, bile salts, bilirubin, and hemoglobin, can lead to false-negative results by interfering with DNA extraction and amplification processes [71] [72]. The impact of these inhibitors is particularly relevant in multicentre studies validating parasitology diagnostic methods, where standardization across laboratories is essential for obtaining reliable and comparable results [70] [3]. This guide objectively compares the performance of various approaches and products designed to overcome these inhibitory challenges, presenting experimental data from recent studies to inform researchers, scientists, and drug development professionals.
The Challenge of PCR Inhibition in Stool Samples
The complex composition of human stool presents a unique challenge for molecular diagnostics. PCR inhibitors in stool samples can act through various mechanisms, including interference with cell lysis, degradation of nucleic acids, or inhibition of DNA polymerase activity [72]. The extent of inhibition varies significantly between individuals and sample types, complicating the development of universal diagnostic protocols.
The effect of these inhibitors is quantifiable through efficiency values measured in inhibition plots. Ideal PCR efficiency should be 100%, with values between 90-110% generally considered acceptable. Studies have documented efficiency values ranging from 96.7% to as high as 114.0% in stool samples, with elevated values indicating the presence of PCR inhibitors that can lead to preferential amplification or false results [72]. The impact is particularly pronounced for pathogens with robust cell walls, such as Cryptosporidium oocysts and Giardia cysts, where inadequate lysis further reduces detection sensitivity [70].
Comparative Performance of Methodological Approaches
DNA Extraction Methods
The DNA extraction method plays a critical role in determining both the yield of amplifiable DNA and the effectiveness of inhibitor removal. Recent comparative studies have demonstrated significant performance differences between extraction techniques.
Table 1: Comparison of DNA Extraction Method Performance for Stool Samples
| Extraction Method | Technology | Inhibitor Removal Efficiency | Gram-positive Bacterial Lysis | DNA Yield | Best Application |
|---|---|---|---|---|---|
| PowerLyzer PowerSoil Kit | Mechanical lysis (bead beating) | High | Excellent | Moderate | Optimal for Gram-positive bacteria and integrity-critical applications [72] |
| QIAamp DNA Stool Mini Kit | Chemical/enzymatic lysis | Moderate | Limited | High | Suitable for high-yield applications where Gram-positive detection is less critical [72] |
| Magnetic Bead-based Methods | Magnetic separation with bacterial isolation | High | Good (varies by method) | High | Optimal for bloodstream infection detection in whole blood; principles applicable to stool [71] |
| Nuclisens Easymag | Magnetic silica technology | High | Good | Moderate | Effective for Cryptosporidium detection when combined with appropriate pretreatment [73] |
Mechanical disruption methods, particularly those incorporating bead beating, have demonstrated superior performance for lysing difficult-to-break pathogens like Cryptosporidium oocysts and Gram-positive bacteria [70] [72]. One study directly compared the PowerLyzer PowerSoil DNA Isolation Kit with the QIAamp DNA Stool Mini Kit, finding that while the QIAamp kit produced higher DNA yields, the PowerLyzer kit provided better DNA integrity and more effective lysis of Gram-positive bacteria [72].
Magnetic bead-based technologies have shown promising results for pathogen detection in complex samples. In a study comparing sepsis diagnostics, magnetic bead-based methods (K-SL DNA Extraction Kit and GraBon system) demonstrated significantly higher accuracy (77.5% and 76.5% respectively) compared to column-based methods (65.0%) for E. coli detection in whole blood samples [71]. While this study focused on blood samples, the principles of magnetic bead technology for improving purity and reducing inhibitors are applicable to stool-based diagnostics.
Sample Pretreatment and Storage Conditions
Sample collection and pretreatment methods significantly impact the effectiveness of inhibitor removal and subsequent molecular detection.
Table 2: Impact of Sample Handling on Molecular Detection Efficiency
| Processing Method | Effect on Inhibitors | DNA Quality Preservation | Impact on Sensitivity | Remarks |
|---|---|---|---|---|
| Stool Container Sampling | Lower PCR inhibitors | Better DNA integrity | Higher number of observed OTUs | Easier manipulation, better for DNA quality [72] |
| Swab-based Sampling | Higher PCR inhibitors | Lower DNA integrity | Reduced sensitivity for some targets | Less comfortable for participants, may affect compliance [72] |
| Sample Preservation | Varies by media | Dependent on fixative | Improved for fixed specimens | Fixed specimens may show better DNA preservation for some targets [70] |
| Mechanical Pretreatment | Significant reduction | Improved for tough cysts | Enhanced for Cryptosporidium | Essential for robust-walled parasites [73] |
A systematic evaluation of sampling kits found that stool containers provided significantly better results compared to swab-based methods across multiple parameters. Samples collected with stool containers showed lower PCR inhibition (significantly lower efficiency values) and better DNA integrity [72]. This combination of factors resulted in a higher number of observed operational taxonomic units (OTUs), indicating better preservation of microbial diversity.
The timing of sample processing and the use of preservation media also affect detection sensitivity. One multicentre study on intestinal protozoa found that PCR results from preserved stool samples were generally better than those from fresh samples, likely due to better DNA preservation in fixed specimens [70]. However, the effectiveness varied by pathogen, with some protozoa demonstrating better detection in fixed specimens while others showed inconsistent results.
Integrated Workflow Comparisons
The most effective approach to addressing inhibitors involves optimizing all stages of the molecular diagnostic process. A comprehensive study evaluating 30 different protocol combinations for Cryptosporidium parvum detection demonstrated that the effectiveness of molecular diagnosis depends on the integration of all stages - pretreatment, extraction, and amplification [73]. A PCR method may not be effective with an unsuitable extraction technique but can yield optimal results with an appropriate one.
The optimal combination identified for C. parvum detection included mechanical pretreatment, the Nuclisens Easymag extraction method, and the FTD Stool Parasite DNA amplification method [73]. This integrated approach achieved 100% detection efficiency, highlighting the importance of coordinated optimization across all workflow stages.
Experimental Protocols for Inhibitor Management
Standardized DNA Extraction Protocol for Inhibitor Removal
The following protocol, adapted from multicentre studies, provides a robust method for DNA extraction from stool samples while effectively addressing inhibitors:
Sample Pretreatment: Homogenize 180-220 mg of stool sample in stool lysis buffer (e.g., ASL buffer from Qiagen). Include a pulse vortexing step for 1 minute followed by incubation at room temperature for 10 minutes [3].
Mechanical Lysis: Transfer the supernatant to a tube containing lysing matrix (ceramic or glass beads) and process using a bead beater or similar mechanical disruption device. The PowerLyzer PowerSoil protocol recommends rigorous shaking for 10-15 minutes to ensure effective lysis of tough-walled pathogens [72].
Inhibitor Removal: For column-based methods, include multiple wash steps with inhibitor removal solutions. For magnetic bead-based methods, ensure adequate separation and washing steps. The MagNA Pure 96 System protocol includes a fully automated nucleic acid preparation based on magnetic separation of nucleic acid-bead complexes, which improves purity [70].
DNA Elution: Elute DNA in a low-ionic-strength buffer such as TE buffer or nuclease-free water. The elution volume should be optimized to balance concentration and purity - typically 50-100 μL for most applications [3] [19].
Inhibitor Detection and Quality Control Protocol
Implementing quality control measures to detect inhibition is crucial for validating results:
Inhibition Plots: Include internal controls in PCR reactions to monitor inhibition. Calculate efficiency values from standard curves, with values between 90-110% considered acceptable [72].
DNA Quality Assessment: Evaluate DNA purity using spectrophotometric ratios (A260/A280 ideally 1.8-2.0) and assess integrity through fragment analysis or gel electrophoresis [72].
Sample Dilution Test: If inhibition is suspected, test serial dilutions of extracted DNA. A decrease in Ct value with dilution indicates the presence of PCR inhibitors [70].
Visualizing Optimal Workflows
The following workflow diagram illustrates the optimized process for handling stool samples to minimize the impact of inhibitors in molecular assays:
This workflow emphasizes critical control points where inhibitor management strategies are most effective, from sample collection through final interpretation.
The Researcher's Toolkit: Essential Reagents and Solutions
Table 3: Essential Research Reagents for Addressing Stool Inhibitors
| Reagent/Solution | Primary Function | Performance Considerations | Example Products |
|---|---|---|---|
| Inhibitor Removal Buffers | Neutralize or remove PCR inhibitors | Varies by manufacturer; critical for complex samples | ASL Buffer (Qiagen), S.T.A.R Buffer (Roche) [70] [3] |
| Mechanical Lysis Matrices | Disrupt tough pathogen walls | Essential for Cryptosporidium, Gram-positive bacteria | Ceramic/silica beads in PowerLyzer kit [72] [73] |
| Magnetic Separation Beads | Selective nucleic acid binding | Higher purity, automation compatibility | STARMag beads (Seegene), K-SL beads (KingoBio) [71] [19] |
| Nucleic Acid Preservation Media | Stabilize DNA during storage | Impacts downstream detection sensitivity | Para-Pak media, Cary-Blair media [70] [19] |
| Internal Control Targets | Detect inhibition in amplification | Quality control essential for result validation | Included in commercial PCR kits [3] [19] |
Effectively addressing inhibitors in stool samples requires a comprehensive, integrated approach spanning sample collection, processing, and analysis. The experimental data presented demonstrates that mechanical disruption methods coupled with magnetic bead-based purification technologies generally provide superior performance for challenging samples, particularly those containing tough-walled pathogens or high levels of inhibitors. The implementation of rigorous quality control measures, including inhibition testing and DNA quality assessment, is essential for validating results, particularly in multicentre studies where standardization is critical. As molecular diagnostics continue to evolve, ongoing optimization of these approaches will further enhance the sensitivity and reliability of stool-based pathogen detection, ultimately improving patient care and public health outcomes.
Continuous Training and Competency Assessment for Laboratory Personnel
In the field of parasitology diagnostics, the reliability of any advanced technological platform is fundamentally dependent on the expertise and competency of the laboratory personnel operating them. Within the context of multicentre studies validating new diagnostic methods, standardized training and rigorous competency assessment become paramount to ensuring data integrity and cross-site comparability. Quality assurance (QA) in parasitology laboratories is not merely a technical requirement but a professional and ethical obligation, as accurate results directly impact patient care, influence public health policies, and contribute to global efforts against neglected tropical diseases [74]. The foundation of strengthening any diagnostic laboratory is a robust QA system, which enhances the confidence of both treating physicians and patients. This system hinges on continuous professional development, as detailed in the following sections.
Comparative Performance Data: Molecular vs. Conventional Methods
Multicentre studies provide critical data on how diagnostic performance is influenced by the choice of method and, by extension, the skill sets required to perform them. The table below summarizes key performance metrics from recent validation studies, highlighting the operational implications for laboratory staff.
Table 1: Comparative Diagnostic Performance of Parasitology Methods from Multicentre Studies
| Pathogen | Diagnostic Method | Sensitivity (%) | Specificity (%) | Sample Size (N) | Citation |
|---|---|---|---|---|---|
| Giardia duodenalis | Allplex GI-Parasite PCR | 100.0 | 99.2 | 368 | [3] |
| Conventional Microscopy/Antigen | Reference | Reference | |||
| Cryptosporidium spp. | Allplex GI-Parasite PCR | 100.0 | 99.7 | 368 | [3] |
| Conventional Microscopy/Antigen | Reference | Reference | |||
| Dientamoeba fragilis | Allplex GI-Parasite PCR | 97.2 | 100.0 | 368 | [3] |
| Conventional Microscopy/Staining | Reference | Reference | |||
| Entamoeba histolytica | Allplex GI-Parasite PCR | 100.0 | 100.0 | 368 | [3] |
| Conventional Microscopy/Culture | Reference | Reference | |||
| Blastocystis hominis | Automated Multiplex PCR | 93.0 | 98.3 | 461 | [19] |
| Microscopy | Reference | Reference | |||
| Cyclospora cayetanensis (in produce) | Modified Real-Time PCR (Mit1C) | 100.0 (200 oocysts) | 98.9 | 24/test lab | [9] |
| Reference Method (18S qPCR) | 100.0 (200 oocysts) | 100.0 |
The data consistently demonstrates that molecular techniques, such as multiplex real-time PCR, generally offer superior sensitivity and specificity for detecting common intestinal protozoa compared to conventional microscopy [3] [19]. However, this shift in technology necessitates a concurrent shift in staff training. Personnel must transition from being experts in morphological identification to being proficient in molecular biology techniques, including nucleic acid extraction, PCR setup, operation of automated platforms, and data interpretation using specialized software. Furthermore, the variable performance for certain pathogens, such as the initially low sensitivity (33.3%) for Entamoeba histolytica in one study [19], underscores the need for continuous assay-specific training and validation to ensure optimal performance.
Experimental Protocols for Multicentre Validation
The implementation of a multicentre study for validating parasitology diagnostics requires a meticulously controlled protocol to minimize inter-laboratory variability—a factor directly tied to personnel competency. The following workflow, derived from published studies, outlines a standardized operational procedure.
Diagram 1: Multicentre Validation Workflow.
Detailed Methodological Steps
Sample Collection and Initial Processing: Participating laboratories collect stool samples during routine diagnostics from patients suspected of enteric parasitic infections [3] [4]. These are examined using conventional techniques—such as macro- and microscopic examination after concentration, various staining methods, antigen detection, and culture—as per WHO and CDC guidelines [3]. This initial step relies heavily on the traditional microscopy competency of local staff.
Standardized Storage and Shipment: Samples are aliquoted and stored frozen at -20°C or -80°C to preserve nucleic acid integrity until they are shipped to a central coordinating laboratory for molecular analysis [3] [4]. Adherence to this protocol is crucial to prevent DNA degradation and ensure valid results.
Centralized Nucleic Acid Extraction and PCR Setup: To reduce variability, nucleic acid extraction and PCR setup are often performed at a central site using automated systems [3] [19]. For example, the Hamilton STARlet or Nimbus IVD system with bead-based extraction kits (e.g., STARMag) is used to process stool suspensions [3] [19]. This step requires personnel trained in operating and troubleshooting automated liquid handling platforms.
Multiplex Real-Time PCR Amplification: DNA extracts are amplified using commercial multiplex PCR assays, such as the Allplex GI-Parasite Assay, on platforms like the Bio-Rad CFX96 [3] [19]. The process involves a denaturing step followed by 45 cycles of amplification, with fluorescence detection at multiple wavelengths. Personnel must be competent in setting up and running these assays, including the use of appropriate positive and negative controls in each run.
Data Analysis and Discrepancy Resolution: Results are interpreted using manufacturer-provided software (e.g., Seegene Viewer) with a predetermined cycle threshold (Ct) value for positivity (e.g., ≤43) [3]. In case of discrepancies between PCR and conventional method results, samples are retested with both techniques to resolve the final status [3]. This analytical phase requires skills in data interpretation and problem-solving.
The Scientist's Toolkit: Essential Research Reagents & Platforms
The consistent execution of multicentre studies depends on access to and proper use of specific reagents and platforms. The following table details key materials and their functions within the experimental workflow.
Table 2: Key Research Reagent Solutions for Molecular Parasitology
| Item Name | Primary Function | Specific Example (from search results) |
|---|---|---|
| Automated Nucleic Acid Extraction System | Standardized DNA/RNA purification from complex samples like stool. | Hamilton STARlet with STARMag 96 × 4 Universal Cartridge kit [19] |
| Multiplex Real-Time PCR Assay | Simultaneous detection of multiple parasite targets in a single reaction. | Allplex GI-Parasite Assay (Seegene) [3] [19] |
| Stool Transport and Lysis Buffer | Stabilize nucleic acids and facilitate homogenization and lysis of hardy parasite cysts/oocysts. | ASL Buffer (Qiagen) [3]; S.T.A.R. Buffer (Roche) [4] |
| Thermal Cycler | Amplify target DNA sequences and detect results in real-time via fluorescence. | Bio-Rad CFX96 Real-time PCR System [3] [19] |
| Proficiency Testing Panels | For external quality assessment (EQA) to validate and compare laboratory performance. | Provided by professional bodies [74] |
Regulatory Framework and Standardized Competency Requirements
The recent updates to the Clinical Laboratory Improvement Amendments (CLIA) personnel requirements underscore the critical link between formalized education, continuous training, and diagnostic quality. Effective December 2024, these rules emphasize the need for specific scientific credentials and ongoing education for laboratory directors and staff [75].
Key updates with training implications include:
- Laboratory Directors: Non-physician directors of high-complexity labs must now hold a doctoral degree in a chemical, biological, or clinical laboratory science and have at least two years of experience directing or supervising high-complexity testing [75]. They must also complete at least 20 continuing education hours covering director responsibilities.
- Educational Qualifications: CMS has eliminated "physical science" degrees as automatic qualifications for many laboratory positions, now recognizing only degrees in biological or chemical sciences, or clinical/medical laboratory technology [75]. This necessitates a review of academic backgrounds for new hires.
- Nursing Personnel: Nurses with a BSN are no longer automatically qualified to perform high-complexity testing without additional training in laboratory science concepts like quality control and proficiency testing [75].
- Technical Consultants: A new pathway allows individuals with an associate degree and four years of experience to qualify as technical consultants for moderate-complexity testing, expanding the pool of professionals who can perform competency assessments [75].
These regulatory changes formalize the necessity of a structured approach to competency assessment and continuous professional development, ensuring that personnel are not only initially qualified but also maintain their expertise in line with evolving technologies and standards.
The transition to molecular diagnostics in parasitology, validated through rigorous multicentre studies, offers clear advantages in sensitivity and specificity. However, this evolution renders continuous training and competency assessment not merely beneficial but essential. The performance data, standardized protocols, and regulatory frameworks detailed in this guide collectively demonstrate that the accuracy and reliability of any diagnostic result are inextricably linked to the skill of the human operator. Therefore, embedding QA principles, investing in capacity building through regular refresher training, and integrating digital technologies for competency evaluation are fundamental to maintaining laboratory credibility and upholding the ethical obligation to patient care [74].
Benchmarking Performance: Sensitivity, Specificity, and Real-World Applicability
In the field of parasitology diagnostics, the definition of a gold standard method is fundamental to validating new technologies and ensuring diagnostic accuracy. Conventional techniques, particularly microscopic examination of stool samples, have long served as the reference standard for detecting intestinal protozoal infections [3] [4]. However, these methods present significant limitations, including high technical expertise requirements, prolonged turnaround times, and variable sensitivity and specificity [3] [19]. The emergence of polymerase chain reaction (PCR)-based molecular diagnostics has introduced a paradigm shift, offering enhanced sensitivity and specificity while reducing operator dependency [3] [76].
This transition has created a critical methodological challenge: how to validate new PCR assays when the established gold standard itself demonstrates imperfect performance. Discrepancies between conventional methods and PCR results necessitate sophisticated resolution strategies and statistical approaches to accurately assess diagnostic performance. Multicentre studies provide the robust evidence base needed to redefine diagnostic standards through systematic comparison and validation of molecular methods against traditional techniques across diverse laboratory settings [3] [4] [19].
Performance Comparison of Diagnostic Methods
Detection of Intestinal Protozoa
Table 1: Comparative performance of multiplex PCR versus conventional methods for intestinal protozoa detection
| Parasite | Reference Method | PCR Sensitivity (%) | PCR Specificity (%) | Study |
|---|---|---|---|---|
| Giardia duodenalis | Microscopy + Antigen Test | 100 | 99.2 | [3] |
| Giardia lamblia | Microscopy | 100 | 98.9 | [19] |
| Entamoeba histolytica | Microscopy + Antigen Test | 100 | 100 | [3] |
| Entamoeba histolytica | Microscopy + ELISA | 33.3-75 | 100 | [19] |
| Cryptosporidium spp. | Microscopy + Antigen Test | 100 | 99.7 | [3] |
| Cryptosporidium spp. | Microscopy | 100 | 100 | [19] |
| Dientamoeba fragilis | Microscopy | 97.2 | 100 | [3] |
| Dientamoeba fragilis | Microscopy | 100 | 99.3 | [19] |
| Blastocystis hominis | Microscopy | 93 | 98.3 | [19] |
| Cyclospora cayetanensis | Microscopy | 100 | 100 | [19] |
The data from multicentre studies demonstrate consistently superior performance of multiplex PCR assays compared to conventional methods across most intestinal protozoa [3] [19]. The exceptional sensitivity and specificity for Giardia duodenalis and Cryptosporidium spp. highlight the reliability of molecular methods for these pathogens. The variable performance for Entamoeba histolytica between studies underscores the impact of different reference standards and sample processing methods on perceived assay performance [19].
Notably, the Allplex GI-Parasite Assay achieved perfect (100%) sensitivity for three of the four major protozoa in a 368-sample multicentre evaluation, establishing a compelling case for molecular methods as potential new reference standards [3]. The consistently high specificity across all targets (≥99.2%) confirms the method's reliability in avoiding false positives, a critical consideration in low-prevalence settings.
Detection of Blood Parasites
Table 2: Performance comparison of malaria diagnostic methods in pregnant women
| Method | Sample Type | Sensitivity (%) | Specificity (%) | Reference Standard |
|---|---|---|---|---|
| Microscopy | Peripheral Blood | 73.8 | 100 | Multiplex qPCR [77] |
| Microscopy | Placental Blood | 62.2 | 100 | Multiplex qPCR [77] |
| RDT | Peripheral Blood | 67.6 | 96.5 | Multiplex qPCR [77] |
| RDT | Placental Blood | 62.2 | 98.8 | Multiplex qPCR [77] |
| Multiplex qPCR | Peripheral Blood | 100 | 94.8 | Microscopy [77] |
For blood parasites, particularly malaria, multiplex qPCR demonstrates significantly enhanced sensitivity compared to both microscopy and rapid diagnostic tests (RDTs), especially in challenging diagnostic scenarios such as placental malaria and low-parasitemia infections [77]. The 100% sensitivity of multiplex qPCR when compared to microscopy as a reference, coupled with its ability to detect submicroscopic infections, positions it as a superior tool for epidemiological surveillance and critical clinical situations.
The performance gap between methods is particularly pronounced in placental blood samples, where conventional methods detected only 62.2% of infections confirmed by multiplex qPCR [77]. This has profound implications for pregnancy outcomes, as undetected placental malaria can cause maternal anemia, intrauterine growth retardation, and stillbirth despite negative peripheral blood tests.
Experimental Protocols for Diagnostic Validation
Multicentre Study Design for PCR Validation
Multicentre validation studies for parasitology diagnostics employ standardized protocols to ensure consistency and reliability across participating laboratories. The following core methodologies represent current best practices derived from recent multicentre evaluations:
Sample Collection and Processing:
- Sample Size: Studies typically include hundreds of samples to ensure statistical power; for example, 368 samples across 12 laboratories in the Allplex assay evaluation [3] and 355 samples across 18 laboratories in the AusDiagnostics comparison [4].
- Storage Conditions: Samples are stored at -20°C or -80°C until batch testing to preserve nucleic acid integrity [3] [4].
- Preservation Methods: Both fresh and preserved stool samples are included to evaluate method performance across different sample types [4].
Reference Method Implementation:
- Microscopic Examination: Performed according to WHO and CDC guidelines, including concentration techniques and specialized staining (Giemsa, Trichrome) [3] [4].
- Antigen Detection: Supplementary immunoassays for specific pathogens like Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica [3] [19].
- Culture Methods: Used for specific pathogens like amoebae when applicable [3].
Molecular Testing Protocols:
- DNA Extraction: Automated systems such as MagNA Pure 96 (Roche) or Hamilton STARlet with bead-based extraction kits [4] [19].
- PCR Conditions: Multiplex real-time PCR with 45 amplification cycles, using manufacturer-recommended threshold values (typically Ct <45) [3] [19].
- Quality Control: Inclusion of internal extraction controls, positive controls, and negative controls in each run [4] [19].
Discrepancy Resolution Methodology
When discrepancies occur between PCR results and reference methods, multicentre studies employ rigorous resolution protocols:
Initial Retesting:
- All discordant samples undergo retesting with both the index PCR assay and the reference method [3].
- This controls for technical errors in initial testing procedures.
Additional Confirmatory Testing:
- Alternative Molecular Methods: Use of different PCR targets or in-house validated assays [4].
- Enhanced Reference Methods: Additional microscopic examination by expert microscopists [77].
- Supplementary Antigen Testing: ELISA or immunochromatographic tests when available [19].
Expert Panel Review:
- Resolution of persistent discrepancies through consensus review by subject matter experts [77].
- Consideration of clinical context and analytical performance characteristics.
Statistical Adjustment:
- Application of latent class analysis (LCA) when no perfect reference standard exists, as demonstrated in schistosomiasis diagnostic studies [78].
- Calculation of kappa statistics to measure agreement beyond chance [3] [77].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents and platforms for parasitology molecular diagnostics
| Reagent/Platform | Manufacturer | Function | Application Example |
|---|---|---|---|
| Allplex GI-Parasite Assay | Seegene Inc. | Multiplex PCR detection of 6 protozoa | Intestinal protozoa detection [3] [19] |
| AusDiagnostics Parasite PCR | AusDiagnostics | Multiplex tandem PCR detection | Intestinal protozoa comparison [4] |
| MagNA Pure 96 System | Roche Applied Sciences | Automated nucleic acid extraction | High-throughput DNA purification [4] |
| Hamilton STARlet | Hamilton Company | Automated liquid handling | DNA extraction and PCR setup [19] |
| Bio-Rad CFX96 | Bio-Rad | Real-time PCR detection | Amplification and fluorescence detection [3] [19] |
| STARMag Universal Cartridge | Seegene Inc. | Bead-based DNA extraction | Nucleic acid purification from stools [19] |
| S.T.A.R Buffer | Roche Applied Sciences | Stool transport and recovery | DNA stabilization in fecal samples [4] |
The validation of molecular diagnostics for parasitology requires specialized reagents and platforms designed to overcome the challenges of complex sample matrices like stool. Automated nucleic acid extraction systems are particularly crucial for standardizing DNA purification across multiple laboratory sites, reducing technical variability in multicentre studies [4] [19]. Bead-based extraction methods have demonstrated effectiveness in breaking down the robust walls of parasite cysts and oocysts, which traditionally hampered DNA extraction efficiency [19].
Multiplex PCR assays targeting the most clinically relevant parasites provide comprehensive detection while conserving sample material and reducing processing time [3] [76]. The integration of automated liquid handling platforms with standardized extraction and detection kits creates streamlined workflows that enhance reproducibility across different laboratory environments, a critical consideration for multicentre validation studies.
Implications for Diagnostic Standards
The accumulating evidence from multicentre studies suggests a paradigm shift in parasitology diagnostics is underway. Molecular methods, particularly multiplex PCR assays, are demonstrating performance characteristics that challenge the status of conventional microscopy as the unchallenged gold standard [3] [19] [76]. The superior sensitivity of PCR enables detection of low-level infections that would be missed by microscopy, while the exceptional specificity prevents misidentification of morphologically similar species [3].
The redefinition of gold standards must consider context of use. In clinical management, PCR's rapid turnaround time and objectivity offer advantages for timely treatment decisions [19]. For public health surveillance and eradication programs, the ability to detect submicroscopic infections makes PCR invaluable for identifying reservoirs of transmission [77]. In resource-limited settings, the cost-benefit analysis may still favor conventional methods, though the landscape is rapidly changing with the introduction of more affordable molecular platforms [78] [77].
The resolution of discrepancies between methods requires sophisticated approaches, including discrepancy analysis, expert review, and statistical methods like latent class analysis that acknowledge the imperfect nature of existing reference standards [78]. As molecular methods continue to evolve and validate across diverse populations and settings, they are poised to become the new benchmark for parasitology diagnostics, ultimately enhancing patient care and disease control efforts globally.
Comparative Analysis of Diagnostic Test Performance Metrics
The accurate diagnosis of parasitic infections remains a cornerstone of effective public health interventions and clinical management, particularly in resource-limited settings where the burden of these diseases is highest. This guide provides an objective comparison of contemporary diagnostic methods, framing the analysis within the context of multicentre study validation for parasitology diagnostics. For researchers and drug development professionals, understanding the performance metrics, operational requirements, and appropriate use cases for each diagnostic modality is essential for selecting optimal tools for surveillance, clinical trials, and routine care. The following sections synthesize experimental data from recent studies to compare traditional, molecular, and emerging diagnostic technologies.
Performance Metrics Comparison of Diagnostic Methods
The table below summarizes key performance metrics for various parasitology diagnostic methods, based on recent multicentre studies and validation research.
Table 1: Comparative Performance Metrics of Parasitology Diagnostic Methods
| Diagnostic Method | Target Parasites/Context | Sensitivity | Specificity | Accuracy/Other Metrics | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Multiplex Real-Time PCR (Allplex GI-Parasite Assay) [3] | Giardia duodenalis | 100% | 99.2% | N/A | High throughput, species differentiation, automation-friendly | Requires specialized lab, higher cost, complex DNA extraction |
| Entamoeba histolytica | 100% | 100% | N/A | |||
| Dientamoeba fragilis | 97.2% | 100% | N/A | |||
| Cryptosporidium spp. | 100% | 99.7% | N/A | |||
| Deep Learning Model (DINOv2-large) [13] | Human Intestinal Parasites (Microscopy) | 78.00% | 99.57% | Accuracy: 98.93%, Precision: 84.52%, F1: 81.13%, AUROC: 0.97 | High-throughput analysis, objective, reduces expert workload | Requires large, annotated datasets and computational resources |
| Deep Learning Model (YOLOv8-m) [13] | Human Intestinal Parasites (Microscopy) | 46.78% | 99.13% | Accuracy: 97.59%, Precision: 62.02%, F1: 53.33%, AUROC: 0.76 | Object detection capabilities, suitable for mixed infections | Lower sensitivity compared to SSL models |
| Rapid Diagnostic Test (RDT) [79] | Plasmodium falciparum (School survey, Senegal) | Variable by region (LOD(_{95}): 3.9-204.3 ng/mL) | N/A | Positivity Rate: 7.2% (overall); Strong predictor: HRP2 concentration (aOR: 14.55 per log10 increase) | Point-of-care, rapid, low cost, user-friendly | Variable performance, limited sensitivity for low-density infections |
| Bead-Based Antigen Detection [79] | Plasmodium falciparum (HRP2 quantification) | Higher than RDT for low-density | N/A | Classified HRP2 positivity using Gaussian mixture model | High-throughput, quantifies antigen, useful for surveillance | Not a point-of-care test; requires laboratory processing |
Detailed Experimental Protocols and Methodologies
Protocol: Multicenter Evaluation of a Multiplex Real-Time PCR Assay
This protocol was used to evaluate the Allplex GI-Parasite Assay across 12 Italian laboratories [3].
- 1. Sample Collection and Reference Methods: A total of 368 stool samples were collected from patients suspected of enteric parasitic infection. These samples were first examined using a panel of conventional techniques considered the reference standard. This panel included:
- Macroscopic and microscopic examination after concentration.
- Staining with Giemsa or Trichrome stain.
- Antigen research for Giardia duodenalis, Entamoeba histolytica/dispar, and Cryptosporidium spp.
- Amoebae culture.
- 2. Sample Storage and Transport: Samples were frozen at -20°C or -80°C by the participating laboratories and later sent to a central laboratory (Papa Giovanni XXIII Hospital, Bergamo, Italy) for molecular testing.
- 3. Nucleic Acid Extraction: From each stool sample, 50-100 mg was suspended in 1 mL of stool lysis buffer (ASL buffer; Qiagen). The suspension was vortexed, incubated at room temperature for 10 minutes, and centrifuged. The supernatant was used for automated nucleic acid extraction using the Microlab Nimbus IVD system.
- 4. Real-Time PCR Setup and Amplification: The extracted DNA was amplified using the Allplex GI-Parasite Assay on a CFX96 Real-time PCR system (Bio-Rad). The assay is a one-step multiplex real-time PCR targeting G. duodenalis, D. fragilis, E. histolytica, B. hominis, C. cayetanensis, and Cryptosporidium spp. A positive result was defined by a fluorescence curve crossing the threshold (Ct) value of less than 45. Results were interpreted using Seegene Viewer software.
- 5. Discrepancy Analysis: In cases of discordant results between the PCR and the reference methods, the samples were retested using both PCR and the traditional methods to resolve the discrepancy.
Protocol: Validation of Deep-Learning Models for Stool Examination
This study compared the performance of deep learning models against human experts in identifying intestinal parasites from stool samples [13].
- 1. Ground Truth Establishment: Human experts performed the formalin-ethyl acetate centrifugation technique (FECT) and Merthiolate-iodine-formalin (MIF) technique on stool samples. The results from these methods served as the ground truth for parasite species identification.
- 2. Image Dataset Preparation: A modified direct smear was conducted on the samples to gather a large set of microscopic images. These images were split into a training dataset (80% of images) and a testing dataset (20% of images).
- 3. Model Training and Operation: Several state-of-the-art deep learning models were trained and operated using an in-house platform (CIRA CORE). The models included:
- Object Detection Models: YOLOv4-tiny, YOLOv7-tiny, YOLOv8-m.
- Classification Models: ResNet-50.
- Self-Supervised Learning (SSL) Models: DINOv2 (base, small, and large).
- 4. Performance Evaluation: The models' performance on the testing dataset was evaluated using:
- Metrics: Confusion matrices were used to calculate accuracy, precision, sensitivity, specificity, and F1 score, using one-versus-rest and micro-averaging approaches.
- Curves: Receiver operating characteristic (ROC) and precision-recall (PR) curves were plotted for visual comparison.
- Statistical Agreement: Cohen’s Kappa and Bland-Altman analyses were used to measure the level of agreement between the models and the human experts.
Protocol: Integrated RDT and Bead-Based Antigen Detection in School Surveys
This study evaluated RDT performance using high-throughput bead-based antigen detection during malaria surveys in Senegalese schools [79].
- 1. Study Design and Population: A cross-sectional study enrolled 3,748 school-aged children from three districts in Senegal (Diourbel, Tambacounda, and Kédougou) in November 2021.
- 2. Field Testing and Sample Collection: All participants were tested for malaria using HRP2-based Rapid Diagnostic Tests (RDTs). Simultaneously, dried blood spots (DBS) were collected from each participant.
- 3. Bead-Based HRP2 Quantification: The DBS samples were analyzed in the laboratory using a high-throughput, multiplex bead-based assay to precisely quantify the level of HRP2 antigen.
- 4. Data Analysis and Model Fitting: A Gaussian mixture model was applied to the HRP2 concentration data to classify samples as HRP2 positive or negative. Logistic regression was then used to assess the relationship between the quantitative HRP2 concentration and the binary outcome of the RDT. From this model, the limit of detection for RDTs (LOD95, the antigen concentration at which 95% of tests are positive) was calculated for each district.
Workflow and Signaling Pathways
The following diagram illustrates the generic workflow for a multicenter validation study of a new diagnostic method (e.g., PCR or AI) against conventional techniques.
Multicenter Diagnostic Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for Parasitology Diagnostics
| Item/Solution | Function/Application | Example Use Case/Note |
|---|---|---|
| Formalin-Ethyl Acetate (FECT) [13] | Stool concentration technique; preserves parasites and enhances detection by microscopy. | Used as a gold standard and routine diagnostic procedure; suitable for preserved samples. |
| Merthiolate-Iodine-Formalin (MIF) [13] | Fixation and staining solution for stool samples; combines preservation and staining. | Effective for field surveys due to easy preparation and long shelf life. |
| Stool Lysis Buffer (e.g., ASL Buffer) [3] | Lyses (oo)cysts and other parasitic forms; inactivates inhibitors and releases nucleic acids for molecular assays. | Critical first step in DNA extraction from stool for PCR; used in automated extraction systems. |
| Multiplex Real-Time PCR Assay (e.g., Allplex GI-Parasite) [3] | Simultaneously detects multiple protozoan DNA targets in a single reaction. | High-throughput screening for common enteric protozoa; requires specific thermal cycler and software. |
| Dried Blood Spot (DBS) Cards [79] | Collection and storage of blood samples for later antigen or molecular analysis; stable and easy to transport. | Used in field surveys for malaria antigen detection (e.g., HRP2). |
| Bead-Based Antigen Assay [79] | High-throughput, quantitative detection of specific parasitic antigens (e.g., HRP2) from numerous samples. | Used as an external validation tool for RDTs and for detecting low-density infections. |
| Deep Learning Model (e.g., DINOv2, YOLO) [13] | Automated identification and classification of parasites from microscopic images. | Requires a curated dataset of images for training and validation; operates on specialized platforms. |
Malaria, a life-threatening parasitic disease, continues to be a significant global health challenge, with its diagnosis in non-endemic areas like the United States complicated by limited clinician familiarity and technical expertise in laboratory identification. Timely and accurate diagnosis is particularly critical for Plasmodium falciparum malaria, which constitutes a medical emergency requiring immediate intervention. This case study examines the multicenter validation of the OptiMAL rapid diagnostic test within the U.S. healthcare infrastructure, evaluating its performance against conventional microscopy as the traditional gold standard. The research was framed within the broader context of improving diagnostic accuracy for parasitic diseases in clinical settings where technologists have limited experience with malaria parasite identification. The persistent challenges of malaria diagnosis in non-endemic regions, including delayed detection and misdiagnosis in emergency rooms, underscore the necessity for reliable, easy-to-use diagnostic tools that can be effectively deployed across diverse hospital systems [80].
Study Design and Methodology
Multicenter Study Framework
The validation of the OptiMAL test was conducted across six major U.S. metropolitan hospitals: UCLA Medical Center (Los Angeles, CA), Boston Medical Center (Boston, MA), Washington Hospital Center (Washington, D.C.), Kings County Hospital Center (Brooklyn, NY), Elmhurst Hospital Center (Elmhurst, NY), and Regions Hospital/HealthPartners (St. Paul, MN). This geographic diversity ensured that the evaluation encompassed varying patient demographics and hospital laboratory practices, providing a robust assessment of the test's real-world applicability [80].
Institutional Review Board (IRB) approval was obtained from the University of Florida and independently from each participating hospital. The study employed a comparative design where each patient sample was evaluated using both microscopy and the OptiMAL test, with readers blinded to the results of the alternative method. This approach minimized bias and allowed for direct comparison of the two diagnostic techniques [80].
Patient Recruitment and Selection
Patient recruitment targeted individuals presenting with symptoms consistent with malaria and a history of travel to countries where malaria is endemic. A total of 216 patients meeting these clinical criteria were enrolled across the six participating sites. Informed consent was obtained from each participant, except at two sites where the study qualified for IRB exemption as it was categorized as a laboratory comparative technique study that required no additional blood draws beyond standard care procedures [80].
Diagnostic Methods
Reference Standard: Microscopy
The reference method for malaria diagnosis consisted of microscopic examination of Giemsa-stained thin and thick blood smears prepared from EDTA-anticoagulated blood samples. This standardized methodology followed established protocols for parasitological confirmation. For quality assurance, samples identified as positive by hospital laboratories underwent secondary confirmation, either by a hospital pathologist or the respective State Department of Health, enhancing the diagnostic reliability of the reference standard [80].
Investigational Method: OptiMAL Test
The OptiMAL rapid test is an immunochromatographic assay that detects parasite lactate dehydrogenase (pLDH), an enzyme produced by metabolizing malaria parasites. The test differentiates between P. falciparum and non-P. falciparum species (P. vivax, P. ovale, and P. malariae) through specific antibody reactions. The testing process requires approximately 15 minutes and involves applying a drop of blood to a test strip, which wicks the sample through a nitrocellulose matrix containing immobilized antibodies [80].
Table 1: Key Characteristics of Diagnostic Methods in the Validation Study
| Method | Principle | Target | Time to Result | Species Differentiation |
|---|---|---|---|---|
| Microscopy | Visual parasite identification in stained blood films | Morphology of parasites | 30-60 minutes | Yes, based on parasite morphology |
| OptiMAL Test | Immunochromatographic detection | Parasite lactate dehydrogenase (pLDH) | 15 minutes | Yes (P. falciparum vs. non-P. falciparum) |
| PCR | DNA amplification | Species-specific DNA sequences | Several hours | Yes (definitive species identification) |
Resolution of Discrepant Results
To address discordant findings between microscopy and the OptiMAL test, the study employed polymerase chain reaction (PCR) analysis as a definitive arbiter. This molecular method, based on the protocol described by Snounou et al., provided superior specificity for parasite identification and was considered the reference truth in cases where the initial methods yielded conflicting results, thereby strengthening the analytical validity of the comparative evaluation [80].
Experimental Results and Performance Data
Diagnostic Accuracy
The multicenter evaluation demonstrated that the OptiMAL test exhibited exceptional performance characteristics compared to conventional microscopy. Of the 216 patient specimens tested, microscopy identified 43 (20%) as positive for malaria parasites (32 with P. falciparum, 11 with non-P. falciparum), while OptiMAL detected 42 (19%) positives (31 with P. falciparum, 11 with non-P. falciparum) [80].
Table 2: Performance Metrics of the OptiMAL Test Versus Microscopy
| Performance Measure | Value | Interpretation |
|---|---|---|
| Sensitivity | 98% | Ability to correctly identify true positive cases |
| Specificity | 100% | Ability to correctly identify true negative cases |
| Positive Predictive Value | 100% | Probability that positive results truly have malaria |
| Negative Predictive Value | 99% | Probability that negative results truly do not have malaria |
The high sensitivity (98%) indicates that the test rarely misses actual malaria infections, while the perfect specificity (100%) signifies that it does not produce false positive results in uninfected individuals. These metrics establish OptiMAL as a highly reliable diagnostic tool in clinical settings [80] [81].
Comparative Analysis with Alternative Diagnostic Methods
When contextualized within the broader landscape of malaria diagnostics, the OptiMAL test demonstrates distinct advantages over other available methods, particularly in non-endemic settings like U.S. hospitals where technologist expertise in malaria parasite identification may be limited.
Table 3: Comparative Performance of Malaria Diagnostic Methods Across Studies
| Diagnostic Method | Sensitivity | Specificity | Infrastructure Requirements | Technical Expertise | Time to Result |
|---|---|---|---|---|---|
| OptiMAL Test | 98% [80] | 100% [80] | Low | Moderate | 15 minutes |
| Standard RDT (Bioline SD) | 62.5% [82] | 92.73% [82] | Low | Moderate | 15-20 minutes |
| Presumptive Diagnosis | 70.83% [82] | 25.82% [82] | None | Low (clinical assessment) | Immediate |
| Deep Learning Models | 78-95% [13] [23] | 99+% [13] [23] | High (computational resources) | High | Variable |
The data reveals that the OptiMAL test outperforms both presumptive diagnosis and standard RDTs in overall accuracy. Presumptive diagnosis based on clinical symptoms alone demonstrates particularly poor specificity, leading to substantial overdiagnosis and unnecessary treatment. While emerging technologies like deep learning models show promising performance metrics, their implementation requires sophisticated computational infrastructure that may not be readily available in all clinical settings [82] [13].
Technological Workflow and Diagnostic Principles
OptiMAL Test Procedure
The OptiMAL test operates on the immunochromatographic principle of detecting parasite-specific lactate dehydrogenase. The procedural workflow involves several critical steps that ensure accurate results. First, a drop of patient blood is added to a well in a microtiter plate and mixed with a specific buffer solution. Next, the OptiMAL test strip is inserted into the well, allowing the blood-buffer mixture to migrate up the nitrocellulose strip via capillary action. After complete sample migration, the strip is transferred to a wash buffer well to clear background interference. Results are interpreted visually after 15 minutes based on the presence or absence of specific colored bands [80].
Analytical Principle of pLDH Detection
The fundamental mechanism of the OptiMAL test centers on detecting parasite-specific lactate dehydrogenase enzyme. This metabolic enzyme is produced by live, metabolically active malaria parasites, making it an excellent marker for active infection. The test employs monoclonal antibodies that specifically capture and detect pLDH but do not cross-react with human LDH isoenzymes. The differential detection of P. falciparum versus non-P. falciparum species is achieved through species-specific antibodies immobilized in discrete zones on the nitrocellulose strip. This specific antigen-antibody interaction forms the basis for the test's diagnostic and differentiation capabilities [80].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Materials for Malaria Diagnostic Validation
| Reagent/Material | Function | Application in Validation |
|---|---|---|
| OptiMAL Test Strips | Immunochromatographic detection of pLDH | Primary investigational device for rapid diagnosis |
| EDTA-Anticoagulated Blood | Prevents coagulation while preserving parasite morphology | Standardized sample collection for both microscopy and RDT |
| Giemsa Stain | Differential staining of parasitic components | Reference method preparation for microscopic examination |
| PCR Reagents | Amplification of parasite-specific DNA sequences | Resolution of discrepant results and definitive species identification |
| Wash Buffer Solution | Removal of unbound components and background clearance | OptiMAL test procedure optimization |
| Parasite Lactate Dehydrogenase | Native target antigen for antibody binding | Analytical sensitivity determination and quality control |
Discussion and Future Directions
Implications for Diagnostic Parasitology
The successful multicenter validation of the OptiMAL test represents a significant advancement in diagnostic parasitology, particularly for non-endemic regions where maintaining expert microscopy capabilities is challenging. The study demonstrated that the integration of rapid diagnostic tests into the U.S. healthcare infrastructure provides an important tool for the timely diagnosis of malaria, potentially addressing the critical issue of preventable malaria deaths often associated with delayed or missed diagnosis [80]. Participating physicians and laboratory directors independently reported that the OptiMAL test was accurate, easy to use, and well accepted by diagnostic laboratory personnel, suggesting that its implementation would face minimal operational barriers [80] [81].
The high specificity (100%) and positive predictive value (100%) are particularly valuable in minimizing false positive diagnoses, which is essential in low-prevalence settings like the U.S. where the prior probability of disease is relatively low. This performance characteristic ensures that patients without malaria are not subjected to unnecessary antimalarial treatments, thereby reducing medication side effects and healthcare costs [80].
Emerging Technologies in Parasitic Disease Diagnosis
While the OptiMAL test demonstrated excellent performance in this validation study, the field of parasitic disease diagnostics continues to evolve with several promising technologies emerging. Deep learning approaches applied to microscopy image analysis have shown remarkable performance, with models like DINOv2-large achieving 98.93% accuracy, 84.52% precision, and 78.00% sensitivity in stool parasite identification, suggesting potential applications in malaria diagnosis [13].
Nanotechnology-based biosensors are emerging as next-generation tools offering enhanced sensitivity through the unique physical, chemical, and biological properties of nanoparticles. These platforms provide versatile diagnostic capabilities while addressing limitations of traditional methods such as lengthy procedures and complex laboratory setups [23].
CRISPR-Cas systems have also entered the parasitology diagnostic landscape, leveraging the precision and programmability of CRISPR-associated proteins to identify parasite-specific nucleic acid sequences. These systems offer sensitive, portable, and cost-effective detection methods that could complement existing diagnostic approaches [23].
Integration into Diagnostic Algorithms
The validation data support the incorporation of the OptiMAL test into standardized diagnostic algorithms for suspected malaria cases in U.S. hospitals. Its rapid turnaround time (15 minutes) and species differentiation capability make it particularly valuable for initial screening, potentially followed by microscopic confirmation for positive cases to quantify parasitemia and provide quality assurance. This complementary approach leverages the strengths of both methods while mitigating their individual limitations [80].
For optimal experimental design in future diagnostic validations, the D-optimality criterion—which seeks to maximize the determinant of the information matrix—would be particularly valuable for multivariate parameter estimation in assessing diagnostic test performance across multiple sites and parasite species [83].
Intestinal parasitic infections, a significant global health burden affecting billions annually, have traditionally been diagnosed through microscopic examination of stool samples [3]. While this method has long been the reference standard, it presents considerable challenges including being labor-intensive, time-consuming, and highly dependent on operator expertise [3] [19]. Furthermore, microscopic techniques struggle with poor sensitivity and an inability to differentiate between pathogenic and non-pathogenic species, such as distinguishing the invasive Entamoeba histolytica from the non-pathogenic E. dispar [3].
Molecular diagnostic techniques, particularly multiplex real-time PCR assays, have emerged as promising alternatives that overcome many limitations of conventional microscopy [3]. This case study evaluates the implementation and performance of the Allplex GI-Parasite Assay (Seegene Inc., Seoul, Korea) within the context of a multicentric Italian study. The research was framed within a broader thesis on validating parasitology diagnostic methods through multicentre study approaches, providing critical insights into the transition from traditional to molecular diagnostic paradigms in medical parasitology.
The Allplex GI-Parasite Assay represents an advanced molecular diagnostic platform that detects and differentiates six major gastrointestinal protozoa in a single reaction: Blastocystis hominis (Bh), Cryptosporidium spp. (CR), Cyclospora cayetanensis (Cc), Dientamoeba fragilis (Df), Entamoeba histolytica (Eh), and Giardia lamblia (GL) [84]. The assay incorporates several innovative technological features that enhance its diagnostic utility.
A cornerstone of this technology is Seegene's proprietary MuDT (Multiple Detection Temperature) system, which enables reporting of multiple Ct values for different targets within a single fluorescence channel [84]. This innovative approach significantly expands the multiplexing capacity of conventional real-time PCR instruments. The assay also incorporates a UDG (Uracil-DNA glycosylase) system to prevent carry-over contamination, utilizes a whole process control to validate each step from extraction to amplification, and is compatible with automated platforms like Seegene's NIMBUS and STARlet systems, streamlining laboratory workflow and reducing hands-on time [84].
Multicenter Study Design and Methodology
Study Design and Sample Collection
The Italian multicentre study employed a retrospective design with participation from 12 clinical laboratories across northern (n=10), central (n=1), and southern (n=1) Italy, including sites in Bergamo, Bologna, Treviso, Pavia, Lecco, Napoli, Legnano, Modena, Verona, Ancona, Pinerolo, and Brunico [3]. This geographical distribution ensured a representative sample of parasitological cases across Italy.
Researchers collected a total of 368 stool samples during routine parasitological diagnostic procedures from patients suspected of enteric parasitic infection [3]. All samples underwent conventional examination according to WHO and CDC guidelines before molecular analysis, providing a robust reference standard for comparison.
Conventional Diagnostic Methods
The conventional diagnostic techniques used as reference methods included:
- Macro- and microscopic examination after concentration
- Giemsa or Trichrome stain for enhanced morphological differentiation
- Antigen detection tests for Giardia duodenalis, Entamoeba histolytica/dispar, and Cryptosporidium spp.
- Amoebae culture for enhanced detection of viable organisms [3]
These methods represent the comprehensive approach typically employed in specialized parasitology laboratories to maximize detection sensitivity through multiple complementary techniques.
Molecular Testing Protocol
The molecular testing followed a standardized protocol across all participating sites:
Sample Preparation: Between 50-100 mg of stool specimens was suspended in 1 mL of stool lysis buffer (ASL buffer; Qiagen, Valencia, CA, USA) [3]. The suspension was vortexed for 1 minute and incubated at room temperature for 10 minutes to ensure proper homogenization.
Nucleic Acid Extraction: The automated Microlab Nimbus IVD system (Hamilton, Reno, NV, USA) performed nucleic acid extraction, incorporating both sample processing and PCR setup in an automated workflow to minimize manual intervention and potential cross-contamination [3].
PCR Amplification and Detection: DNA extracts were amplified using one-step real-time PCR multiplex on the CFX96 Real-time PCR system (Bio-Rad, California, USA) with the Allplex GI-Parasite Assay [3]. The thermal cycling protocol included fluorescence detection at two different temperatures (60°C and 72°C) to accommodate the MuDT technology. A positive result was defined as a sharp exponential fluorescence curve crossing the threshold (Ct) at a value below 45 for individual targets [3].
Result Interpretation: The Seegene Viewer software (version 3.28.000) automatically interpreted results, providing objective analysis and facilitating laboratory information system (LIS) interoperation [84].
Statistical Analysis
The research team employed descriptive statistics to calculate sensitivity, specificity, and predictive values for each pathogen detected by the PCR assay [3]. Conventional methods served as the reference standard for determining true positive (TP), true negative (TN), false positive (FP), and false negative (FN) results. In cases of discrepant results between methods, samples were retested using both approaches to resolve discrepancies [3]. Additionally, inter-rater reliability between traditional methods and the PCR assay was assessed using Kappa statistics, with values interpreted as follows: 0.01-0.20 (slight agreement), 0.21-0.40 (fair agreement), 0.41-0.60 (moderate agreement), 0.61-0.80 (substantial agreement), and 0.81-1.00 (perfect agreement) [3].
Comparative Performance Analysis
Diagnostic Accuracy in the Italian Study
The multicentric Italian evaluation demonstrated exceptional performance characteristics for the Allplex GI-Parasite Assay across the most clinically relevant enteric protozoa [3]. The following table summarizes the comprehensive performance metrics compared to conventional diagnostic methods:
Table 1: Performance Metrics of Allplex GI-Parasite Assay in the Italian Multicenter Study
| Parasite | Sensitivity (%) | Specificity (%) | Agreement with Conventional Methods |
|---|---|---|---|
| Entamoeba histolytica | 100 | 100 | Perfect |
| Giardia duodenalis | 100 | 99.2 | Substantial to Perfect |
| Dientamoeba fragilis | 97.2 | 100 | Substantial to Perfect |
| Cryptosporidium spp. | 100 | 99.7 | Substantial to Perfect |
The assay achieved perfect sensitivity and specificity for Entamoeba histolytica at 100% each, overcoming a critical limitation of microscopy which cannot differentiate this pathogenic species from the non-pathogenic E. dispar [3]. Similarly, the assay demonstrated perfect sensitivity (100%) and near-perfect specificity (99.2%) for Giardia duodenalis, a major cause of parasitic gastroenteritis worldwide [3].
For Dientamoeba fragilis, the assay showed high sensitivity (97.2%) and perfect specificity (100%), particularly notable given the challenges in detecting this parasite by conventional methods due to its fragile trophozoite stage and morphological similarity to non-pathogenic protozoa [3]. Cryptosporidium spp. detection also showed perfect sensitivity (100%) and near-perfect specificity (99.7%), representing a significant improvement over conventional acid-fast staining methods which have variable sensitivity and require significant technical expertise [3].
International Comparative Performance
The Italian study findings are corroborated by international validation studies conducted in different laboratory settings. A Canadian study at Public Health Ontario Laboratories evaluated the assay using 461 unpreserved fecal specimens with microscopy as the reference standard, supplemented by stool ELISA for E. histolytica [19]. The following table compares their results with the Italian study:
Table 2: International Comparison of Allplex GI-Parasite Assay Performance
| Parasite | Italian Study Sensitivity (%) | Canadian Study Sensitivity (%) | Canadian Study Specificity (%) |
|---|---|---|---|
| Blastocystis hominis | Not reported | 93.0 | 98.3 |
| Cryptosporidium spp. | 100 | 100 | 100 |
| Cyclospora cayetanensis | Not reported | 100 | 100 |
| Dientamoeba fragilis | 97.2 | 100 | 99.3 |
| Entamoeba histolytica | 100 | 33.3 (75 with frozen specimens) | 100 |
| Giardia lamblia | 100 | 100 | 98.9 |
The Canadian validation showed more variable performance for Entamoeba histolytica, with sensitivity of only 33.3% for fresh specimens, though this improved to 75% when including frozen specimens [19]. This discrepancy highlights potential variations in sample preservation and processing protocols across different laboratory settings. The authors noted that despite this limitation, the widespread availability of confirmatory serology and stool antigen testing for E. histolytica mitigates concerns about the assay's performance for this particular pathogen [19].
A more recent 2024 Belgian study conducted in a travel clinic setting further confirmed the excellent performance for protozoan detection, reporting 100% sensitivity for Dientamoeba fragilis and 95% for Blastocystis hominis, significantly outperforming their conventional workflow which achieved only 47.4% and 77.5% sensitivity respectively [85].
Workflow Efficiency and Automation Benefits
Beyond analytical performance, the Allplex GI-Parasite Assay demonstrated significant advantages in operational efficiency. The Canadian study documented a reduction in pre-analytical and analytical testing turnaround time by approximately 7 hours per batch compared to conventional methods [19]. This acceleration stems from the automated workflow enabled by platforms like the Hamilton STARlet system, which integrates nucleic acid extraction and PCR setup into a single automated process [19].
The automated system processes samples in a high-throughput manner using the STARMag 96 × 4 Universal Cartridge kit for nucleic acid extraction, with the entire procedure—from stool suspension in Cary-Blair media to PCR preparation—requiring minimal manual intervention [19]. This automation not only reduces hands-on time but also enhances reproducibility and reduces the risk of cross-contamination or human error, critical factors in high-volume diagnostic laboratories [19].
Research Reagent Solutions and Essential Materials
The implementation of the Allplex GI-Parasite Assay requires specific reagents and platforms optimized for parasitology molecular diagnostics. The following table details the essential research reagents and their functions based on the protocols described in the multicenter studies:
Table 3: Essential Research Reagents for Allplex GI-Parasite Assay Implementation
| Reagent/Platform | Function | Specification/Application |
|---|---|---|
| Allplex GI-Parasite Assay | Multiplex PCR detection | Detects 6 protozoa simultaneously; includes master mix and primers/probes |
| STARMag 96 × 4 Universal Cartridge | Nucleic acid extraction | Magnetic bead-based DNA extraction optimized for stool samples |
| ASL Buffer (Qiagen) | Stool lysis and homogenization | Initial suspension and disruption of sturdy parasite cyst walls |
| Cary-Blair Media | Transport and preservation | Maintains nucleic acid integrity for unpreserved specimens |
| eNAT Medium | Sample transport and storage | Preserves nucleic acids at room temperature for transport |
| Microlab Nimbus IVD/Hamilton STARlet | Automated processing | Integrated system for nucleic acid extraction and PCR setup |
| Bio-Rad CFX96 Real-time PCR System | Amplification and detection | Platform for real-time PCR with multiple fluorescence detection channels |
The critical importance of proper DNA extraction is worth emphasizing, as the thick-walled cysts and oocysts of parasitic protozoa present particular challenges for nucleic acid liberation, while stool samples contain numerous PCR inhibitors that must be effectively removed during extraction [3]. The automated extraction systems specified in the protocol effectively address these challenges through bead-beating mechanical lysis combined with chemical disruption, ensuring efficient DNA recovery from resilient parasitic forms [19].
Discussion and Implications for Diagnostic Parasitology
Advantages and Limitations in Clinical Practice
The multicentric Italian study demonstrates that the Allplex GI-Parasite Assay provides a robust molecular platform for detecting common intestinal protozoa with performance characteristics equal or superior to conventional microscopy [3]. The assay's exceptional sensitivity for pathogens like Dientamoeba fragilis—which requires stained fixed fecal smears for morphological identification and is easily missed in routine examination—represents a particular advancement [3] [85].
The multiplex PCR platform also addresses several systematic challenges in diagnostic parasitology. It reduces dependency on scarce morphological expertise, standardizes result interpretation across laboratories, accommodates higher testing volumes, and provides objective, reproducible results independent of operator skill level [3] [19]. These advantages are particularly valuable in non-endemic areas where maintaining microscopic expertise is challenging due to low sample positivity rates [85].
However, the assay does present certain limitations. The 2024 Belgian study noted that the companion Allplex GI-Helminth assay showed suboptimal performance for detecting helminths (59.1% sensitivity compared to 100% for microscopy), limiting its utility for comprehensive parasitological diagnosis [85]. Additionally, the fixed-panel nature of commercial multiplex PCR assays means they cannot detect parasites not included in the panel, such as Cystoisospora belli or Schistosoma mansoni, which may be identified through morphological examination [85].
Methodological Considerations for Implementation
The comparative studies reveal several important methodological considerations for laboratories implementing molecular parasitology diagnostics:
Sample Preservation: The variable sensitivity for Entamoeba histolytica between fresh and frozen specimens observed in the Canadian study suggests that sample preservation methods significantly impact detection efficiency for some targets [19].
Inhibition Management: The high concentration of PCR inhibitors in stool samples necessitates robust nucleic acid extraction methods with effective inhibition removal, highlighting the importance of using validated extraction systems [3].
Result Interpretation: The Belgian study established a protocol of retesting samples with weak positive PCR results (Ct ≥ 38), acknowledging the potential for reduced reproducibility near the assay's limit of detection [85].
Complementary Testing: Even with high-performance molecular assays, complementary techniques like antigen detection or specific PCRs may be necessary to resolve discrepancies or detect pathogens outside the multiplex panel [85].
Workflow Integration and Economic Considerations
The integration of molecular assays into diagnostic parasitology workflows requires careful consideration of operational and economic factors. The significant reduction in hands-on time and the potential for batch testing with automated platforms like the STARlet system can offset the higher reagent costs of molecular methods in high-volume settings [19]. Furthermore, the increased detection rate for parasites like Dientamoeba fragilis and Blastocystis hominis may lead to more targeted treatment and improved patient outcomes, though the clinical significance of detecting some parasites at low levels requires careful interpretation [85].
The following diagram illustrates the automated workflow for the Allplex GI-Parasite Assay implementation:
Diagram 1: Automated Workflow for GI Parasite Detection
The Italian multicentre case study demonstrates that the Allplex GI-Parasite Assay provides a highly sensitive and specific molecular platform for detecting common intestinal protozoa, effectively addressing many limitations of conventional microscopic methods. The assay's excellent performance characteristics, combined with its automated workflow and reduced turnaround time, position it as a valuable tool for modernizing parasitology diagnostics, particularly in settings where expert microscopy is unavailable.
While the assay shows some limitations for helminth detection and requires complementary methods for parasites outside its panel, its implementation represents a significant step forward in the molecular reimagination of parasitology diagnostics. Future developments will likely focus on expanding target panels, further optimizing automation, and establishing standardized protocols for sample processing to ensure consistent performance across different laboratory environments.
For optimal implementation, laboratories should consider their specific patient population, the prevalence of various parasitic pathogens, and available confirmatory testing resources when integrating multiplex PCR assays into diagnostic workflows. When deployed strategically alongside conventional methods, the Allplex GI-Parasite Assay significantly enhances diagnostic capabilities for intestinal protozoal infections.
Assessing Cost-Effectiveness and Operational Feasibility for Endemic vs. Non-Endemic Regions
The accurate diagnosis of parasitic diseases is a cornerstone of effective clinical management and disease control. The choice of diagnostic method, however, is heavily influenced by a complex interplay of cost, operational feasibility, and the epidemiological context—factors that differ dramatically between endemic and non-endemic regions. In endemic, often resource-limited settings, the priority lies in deploying affordable, rugged, and easily deployable tests for large-scale case management. In contrast, non-endemic, high-resource regions face the challenge of identifying imported cases or infections among at-risk migrant populations through targeted screening programs, where test cost may be secondary to high sensitivity and specificity. This guide objectively compares the cost-effectiveness and operational performance of various parasitology diagnostic methods, framing the analysis within a multicentre study validation context to provide researchers and drug development professionals with a evidence-based framework for decision-making.
Comparative Cost-Effectiveness of Diagnostic Approaches
The economic value of a diagnostic strategy is not absolute but is critically dependent on the disease prevalence, the target population, and the local healthcare infrastructure. The following tables synthesize data from recent economic evaluations.
Table 1: Cost-Effectiveness of Malaria Diagnostic Methods in Endemic Sub-Saharan Africa
| Diagnostic Strategy | Malaria Prevalence in Febrile Outpatients | Incremental Cost-Effectiveness vs. Comparator | Key Assumptions & Context |
|---|---|---|---|
| Rapid Diagnostic Tests (RDTs) | Up to 62% (95% certainty) | Cost-effective vs. presumptive treatment [86]. | Compared to presumptive treatment; cost-effective if <$150/DALY averted. ACT cost: $1-2.4; RDT cost: $0.6-1 [86]. |
| Rapid Diagnostic Tests (RDTs) | All prevalence levels | >85% likely cost-effective vs. microscopy [86]. | Reflects superior real-life accuracy of RDTs over field-standard microscopy [86]. |
| RDTs vs. Microscopy | Low transmission setting | ICER: $25 per additional patient correctly treated [87]. | Provider perspective; ACT cost: $2.4/adult course; RDT: $0.81; Microscopy: $0.26/slide [87]. |
| RDTs vs. Microscopy | High transmission setting | ICER: $7 per additional patient correctly treated [87]. | Larger effectiveness difference due to higher prevalence improves RDT cost-effectiveness [87]. |
Table 2: Cost-Effectiveness of Screening Programs in Non-Endemic Regions
| Disease & Strategy | Population & Setting | Incremental Cost-Effectiveness Ratio (ICER) | Key Assumptions & Context |
|---|---|---|---|
| Congenital Chagas Disease Screening | Pregnant Latin American migrants in Italy | €15,193 per QALY gained (95% CI: €14,885–€15,552) [88] [89]. | Versus no screening; well below Italian cost-effectiveness threshold (€30,000–€50,000/QALY) [88] [89]. |
| Sentinel Schistosomiasis Screening | Co-testing with malaria RDTs in Uganda | Dependent on schistosomiasis prevalence and test accuracy/price [90]. | High prevalence: Mass Drug Administration (MDA) preferred. Average prevalence: testing preferred. Requires economies of scope or high-accuracy tests [90]. |
Experimental Protocols for Diagnostic Evaluation
Robust, multicentre study designs are essential for generating generalizable evidence on diagnostic performance and operational feasibility.
Protocol: Diagnostic Accuracy and Field Feasibility (Cryptosporidiosis)
This protocol, adapted from a study in Ethiopia, exemplifies a comprehensive field evaluation [91].
- 1. Study Design: Prospective diagnostic accuracy study in consecutive series of patients presenting at healthcare facilities.
- 2. Participant Recruitment:
- Cases: Children under 5 years with diarrhea or dysentery.
- Controls: Community controls without diarrhea, matched by geography, age, and enrolment week to establish quantitative cutoffs for symptomatic disease.
- 3. Index Tests:
- LED Fluorescence Microscopy with Auramine-Phenol Staining (LED-AP): Performed on stool samples according to standard protocols.
- Lateral-Flow Test Strip: A room-temperature stable immunochromatographic test performed on stool samples.
- 4. Reference Standard: A composite standard to definitively classify true positives and negatives, comprising:
- Quantitative Immunofluorescent Antibody Test (qIFAT)
- Enzyme-Linked Immunosorbent Assay (ELISA)
- Quantitative PCR (qPCR)
- 5. Operational Feasibility Metrics:
- Cost Calculation: Comprehensive calculation of cost per test, including reagents, equipment, and personnel time.
- Turnaround Time: Time from sample collection to result availability.
- Infrastructure Requirements: Assessment of need for electricity, refrigeration, and technical expertise.
- 6. Data Analysis:
- Calculation of sensitivity and specificity with 95% confidence intervals for each index test against the reference standard.
- Analysis of operational data to determine feasibility for integration into local health systems.
Protocol: Cost-Effectiveness of a Screening Program (Chagas Disease)
This protocol outlines a model-based evaluation for a non-endemic setting, as used in the Italian study [88] [89].
- 1. Model Structure: Development of a Bayesian decision tree model with a lifetime horizon to capture long-term outcomes.
- 2. Comparators:
- Screening Scenario: Serological testing of at-risk pregnant women and follow-up testing and treatment of infected newborns.
- No-Screening Scenario: Standard care without targeted testing.
- 3. Input Parameters:
- Epidemiological: Disease prevalence in the target population, probability of congenital transmission.
- Test Performance: Sensitivity and specificity of the diagnostic algorithms.
- Clinical: Probability of disease progression, treatment efficacy.
- Costs: All direct medical costs from the health system perspective (e.g., test kits, medications, clinical visits).
- Utilities: Health-related quality of life weights (for QALY calculation).
- 4. Analysis:
- Base-Case Analysis: Calculation of the Incremental Cost-Effectiveness Ratio (ICER).
- Sensitivity Analysis: Probabilistic sensitivity analysis to assess model robustness and the impact of parameter uncertainty. Value of Information analysis to prioritize future research.
Diagnostic Evaluation Workflow
The following diagram visualizes the core logical pathway for the multicentre validation of a new parasitology diagnostic test, integrating both accuracy and cost-effectiveness assessments.
Diagram: Multicentre Diagnostic Validation Pathway. This workflow outlines the phased evaluation of parasitology diagnostics, from initial analytical validation to assessment of cost-effectiveness and societal impact, as recommended by WHO/TDR frameworks [92]. TAT: Turnaround Time.
The Scientist's Toolkit: Key Research Reagent Solutions
The experiments and evaluations cited rely on a suite of critical reagents and technologies.
Table 3: Essential Research Reagents and Materials for Parasitology Diagnostic Evaluation
| Reagent / Material | Primary Function in Diagnostic Research | Example Application in Cited Studies |
|---|---|---|
| International Biological Reference Preparations | Serve as a gold standard for calibrating reagents and ensuring comparability of results across laboratories and studies [92]. | Used in pre-clinical evaluation to standardize antigens, antibodies, and DNA probes [92]. |
| Composite Reference Standard Panels | Panels of well-defined clinical samples (e.g., sera, stool) used to accurately assess the sensitivity and specificity of new index tests [92] [91]. | Provided to participating labs in multicentre studies to evaluate performance of commercial tests for toxoplasmosis and cryptosporidiosis [92] [91]. |
| Target-Specific Antigens & Antibodies | Core components of serological tests like ELISA, immunoblot, and Rapid Diagnostic Tests (RDTs) for detecting pathogen-specific antibodies or antigens [93]. | Used in the lateral-flow test strip for Cryptosporidium and in serological tests for Chagas disease (e.g., ELISA, IFA) [91] [88] [93]. |
| Primers & Probes for Molecular Assays | Designed to target parasite-specific DNA/RNA sequences, enabling highly sensitive and specific detection via PCR, qPCR, and other molecular platforms [91] [94] [93]. | Constituted the quantitative PCR (qPCR) component of the composite reference standard for cryptosporidiosis [91]. |
| Multiplex Diagnostic Platforms | Devices capable of simultaneously testing a single sample for multiple pathogens, increasing efficiency and enabling "sentinel screening" [90] [94]. | Evaluated for co-detection of malaria and schistosomiasis in a single assay in Uganda [90]. |
The evidence clearly demonstrates that the optimal parasitology diagnostic strategy is context-dependent. In endemic regions, RDTs and dual-use technologies like LED-AP microscopy are cost-effective and operationally feasible, providing a pragmatic solution for case management where laboratory infrastructure is limited [91] [87] [86]. Their value is maximized when test results are adhered to, ensuring appropriate treatment and generating cost savings from reduced drug consumption. Conversely, in non-endemic regions, targeted screening programs—even for diseases of low prevalence—can be highly cost-effective by preventing severe long-term sequelae and onward transmission, as demonstrated for congenital Chagas disease [88] [89].
For researchers validating diagnostic methods, a phased, multicentre approach following established frameworks is critical [92]. Future efforts should focus on developing and validating multiplexed, low-cost, high-accuracy tests that can be deployed at the point-of-care. Furthermore, generating robust local cost-effectiveness evidence and ensuring strong stakeholder engagement are essential for the successful implementation and scale-up of any new diagnostic strategy, ultimately contributing to the control and elimination of parasitic diseases globally.
Conclusion
Multicentre studies are indispensable for validating parasitology diagnostic methods, providing the rigorous evidence base needed to transition from traditional microscopy to advanced molecular and automated technologies. The consistent findings across recent studies underscore that while rapid immunochromatographic tests offer invaluable point-of-care solutions, multiplex PCR assays provide superior sensitivity and specificity for detecting low-level and mixed infections, particularly for intestinal protozoa. The integration of AI and automated sample processing, as demonstrated by the DAPI system and dissolved air flotation technique, promises to further revolutionize the field by enhancing throughput and reducing human error. Future efforts must focus on standardizing protocols, improving DNA extraction efficiencies, and making advanced diagnostics accessible and cost-effective for low-resource settings. Ultimately, these validated, precise diagnostic tools are the cornerstone of effective patient management, robust disease surveillance, and successful global control and elimination programs for parasitic diseases.
References
- 1. Effective Laboratory Diagnosis of Parasitic Infections of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11475984/]
- 2. Diagnosis of Parasitic Infections: What's Going On? [https://www.sciencedirect.com/science/article/pii/S2472555222071696]
- 3. Evaluation of Allplex™ GI-Parasite Assay—A Multiplex Real ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390207/]
- 4. Comparative analysis of commercial and “In-House ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 5. Multi-technology parasite detection: The intersection of ... [https://www.sciencedirect.com/science/article/abs/pii/S0001706X25001287]
- 6. Multicenter Evaluation of Clinical Diagnostic Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4844741/]
- 7. Evaluation of Allplex™ GI-Parasite Assay—A Multiplex ... [https://www.mdpi.com/2414-6366/10/8/234]
- 8. A multicentre comparative study of serological methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12165711/]
- 9. Multi-laboratory validation of a modified real-time PCR ... [https://www.sciencedirect.com/science/article/pii/S0740002025000073]
- 10. Factors associated with detecting pathogenic intestinal ... [https://link.springer.com/article/10.1007/s00436-025-08570-5]
- 11. AI tool detects intestinal parasites in stool samples more ... [https://www.news-medical.net/news/20251023/AI-tool-detects-intestinal-parasites-in-stool-samples-more-accurately-than-traditional-methods.aspx]
- 12. AI-supported versus manual microscopy of Kato-Katz ... [https://www.nature.com/articles/s41598-025-07309-7]
- 13. Performance validation of deep-learning-based approach in ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06878-w]
- 14. Assessing the diagnostic value of qPCR for Trichuris trichiura [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1679294/full]
- 15. Comparative performance of microscopy, rapid diagnostic ... [https://pubmed.ncbi.nlm.nih.gov/39833795/]
- 16. Standardized data collection for multi-center clinical studies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1459261/]
- 17. Validation of charcot's triad and Tokyo guidelines 2018 as ... [https://pubmed.ncbi.nlm.nih.gov/41023890/]
- 18. Application of a Multiplex Quantitative PCR to Assess ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4731196/]
- 19. Validation of an Automated High-Throughput Multiplex ... [https://www.mdpi.com/2673-947X/5/1/8]
- 20. A comparative study with conventional copromicroscopy [https://www.sciencedirect.com/science/article/pii/S240567312500042X]
- 21. Global Epidemiology of Vector-Borne Parasitic Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472468/]
- 22. Global impact of parasitic infections and the importance ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1546195/full]
- 23. Recent advancements in the diagnosis of parasitic diseases [https://www.sciencedirect.com/science/article/abs/pii/S0166685125000428]
- 24. A multicentric evaluation of dipstick test for serodiagnosis ... [https://www.nature.com/articles/s41598-019-46283-9]
- 25. Comparison of the Diagnostic Performances of Five ... [https://pubmed.ncbi.nlm.nih.gov/38248040/]
- 26. Multicenter comparative study of Enterocytozoon bieneusi ... [https://www.nature.com/articles/s41598-024-66154-2]
- 27. Performance validation of the BD MAX Enteric Parasite ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11895086/]
- 28. Diagnostic accuracy of an automated microscope solution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11212432/]
- 29. Multicenter Evaluation of an ELISA for the Detection ... [https://www.mdpi.com/2076-2607/9/2/209]
- 30. A clinical microscopy dataset to develop a deep learning ... [https://www.nature.com/articles/s41597-024-02975-0]
- 31. Comparison and clinical validation of qPCR assays targeting ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008750]
- 32. Scientists pioneer new X-ray microscopy method for data ... [https://www.anl.gov/article/scientists-pioneer-new-xray-microscopy-method-for-data-analysis-on-the-fly]
- 33. A review on point of care tests in parasitology [https://www.sciencedirect.com/science/article/pii/S0255085722000391]
- 34. A review on point of care tests in parasitology [https://pubmed.ncbi.nlm.nih.gov/35248402/]
- 35. Comparison of Immunochromatographic Test (ICT) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293346/]
- 36. Technologies for the point-of-care diagnosis of malaria [https://idpjournal.biomedcentral.com/articles/10.1186/s40249-025-01329-1]
- 37. Field laboratory comparison of STANDARD Q Filariasis ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0012386]
- 38. Performance comparison of two malaria rapid diagnostic test ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7447940/]
- 39. A Diagnostic Accuracy Study to Evaluate Standard Rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10231394/]
- 40. Development and clinical validation of a novel multiplex ... [https://www.nature.com/articles/s41598-025-16434-2]
- 41. a prospective study on 3500 stool samples over 3 years [https://pubmed.ncbi.nlm.nih.gov/40162804/]
- 42. Comparison of one commercial and two in-house TaqMan ... [https://pubmed.ncbi.nlm.nih.gov/28906580/]
- 43. Comparison of two commercial multiplex PCR assays for ... [https://jidc.org/index.php/journal/article/view/35298429]
- 44. Comparison of Commercial and In-House Real-Time PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2643664/]
- 45. Multicenter validation of a multiplex PCR assay for ... [https://pubmed.ncbi.nlm.nih.gov/16355837/]
- 46. Performance of three multiplex real-time PCR assays for ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2024.1421427/full]
- 47. Multicenter evaluation of fast multiplex PCR for detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528164/]
- 48. Multicenter evaluation of fast multiplex PCR for detection ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1643991/full]
- 49. Automated DNA Extraction Systems Analysis 2025 and ... [https://www.archivemarketresearch.com/reports/automated-dna-extraction-systems-320356]
- 50. Performance of Real-Time Polymerase Chain Reaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5508894/]
- 51. Comparative Study of DNA Extraction Methods for the PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9689707/]
- 52. Best PCR Systems of 2025: Top Picks for Research ... [https://www.labx.com/resources/best-pcr-systems-of-2025-top-picks-for-research-clinical-industry-labs/4817]
- 53. Digital PCR: modern solution to parasite diagnostics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10131454/]
- 54. 多模型AI诊断疟疾准确率达96.47% [https://www.stdaily.com/web/gjxw/2025-07/17/content_371511.html]
- 55. 国际研究团队利用AI诊断疟疾准确率达96.47% [https://ecas.cas.cn/xxkw/kbcd/201115_148053/ml/xxhcxyyyal/202508/t20250820_5079961.html]
- 56. 通过基于深度学习的YOLOv3平台,快速准确地识别恶性疟 ... [https://www.ebiotrade.com/newsf/2025-10/20251031000446016.htm]
- 57. Noul基于人工智能的疟疾诊断解决方案已在国际学术期刊上 ... [https://www.venturesquare.net/zh/998187]
- 58. FedEmbryo:基于联邦任务自适应学习的个性化IVF胚胎选择 ... [https://www.ebiotrade.com/newsf/2025-11/20251119004424314.htm]
- 59. AI辅助阴道彩超联合血清标志物诊断IVF-ET后宫内外复合妊娠的 ... [http://kyxuebao.kmmu.edu.cn/cn/article/doi/10.12259/j.issn.2095-610X.S20251014]
- 60. Comparison of parasitological techniques for the diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5555921/]
- 61. Multi-centre testing and validation of current protocols for ... [https://pubmed.ncbi.nlm.nih.gov/20595003/]
- 62. Multi-centre testing and validation of current protocols for ... [https://www.sciencedirect.com/science/article/abs/pii/S0020751910001840]
- 63. Establishing a framework for best practices for quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10861687/]
- 64. Multicenter comparative study of Enterocytozoon bieneusi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11224372/]
- 65. Metagenomic detection of protozoan parasites on leafy ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1566579/full]
- 66. Evaluation of Three Protocols of DNA Extraction for ... [https://brieflands.com/journals/jjm/articles/63096]
- 67. Metagenomic detection of protozoan parasites on leafy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949954/]
- 68. A comparative analysis of preservation techniques for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5773002/]
- 69. Assessing morphological preservation of gastrointestinal ... [https://www.nature.com/articles/s41598-024-53915-2]
- 70. Comparative analysis of commercial and “In-House ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317615/]
- 71. Comparison evaluation of bacterial DNA extraction ... [https://www.nature.com/articles/s41598-025-87225-y]
- 72. Stool sampling and DNA isolation kits affect DNA quality ... [https://www.nature.com/articles/s41598-019-49520-3]
- 73. Performance of 30 protocol combinations for the detection ... [https://www.sciencedirect.com/science/article/pii/S1684118225000064]
- 74. Ensuring quality assurance in parasitology laboratories [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617588/]
- 75. CMS Implements First Major Updates to Lab Personnel ... [https://www.mwe.com/insights/cms-implements-first-major-updates-to-lab-personnel-requirements-in-30-years/]
- 76. Multiplex Polymerase Chain Reaction Panels for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541719/]
- 77. Comparative performance of microscopy, rapid diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11748328/]
- 78. Comparative performance of Kato–Katz, POC-CCA and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12323140/]
- 79. Frontiers | RDT performance through high-throughput bead-based... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1598280/full]
- 80. Multicenter Study To Evaluate the OptiMAL Test for Rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC262482/]
- 81. Multicenter study to evaluate the OptiMAL test for rapid ... [https://www.healthpartners.com/knowledgeexchange/display/document-rn38508]
- 82. Comparative Performance Evaluation of Routine Malaria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5055952/]
- 83. Optimal experimental design [https://en.wikipedia.org/wiki/Optimal_experimental_design]
- 84. Allplex™ GI-Parasite Assay [https://www.seegene.com/assays/allplex_gi_parasite_assay]
- 85. Evaluation of the Allplex GI Parasite and Helminth PCR ... [https://www.mdpi.com/2075-4418/14/18/1998]
- 86. Cost-effectiveness of malaria diagnostic methods in sub-Saharan Africa in an era of combination therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2647374/]
- 87. The Cost-Effectiveness of Parasitologic Diagnosis for ... [https://www.ncbi.nlm.nih.gov/books/NBK1690/?report=reader]
- 88. Cost-effectiveness analysis of screening for congenital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12484535/]
- 89. Cost-effectiveness analysis of screening for congenital ... [https://www.nature.com/articles/s41467-025-63760-0]
- 90. Cost-effectiveness of sentinel screening of endemic diseases ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11309411/]
- 91. Performance and operational feasibility of two diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8064915/]
- 92. [Diagnostic kits in parasitology: which controls?] - PubMed [https://pubmed.ncbi.nlm.nih.gov/15305705/]
- 93. Diagnosis of Parasitic Diseases: Old and New Approaches [https://pmc.ncbi.nlm.nih.gov/articles/PMC2804041/]
- 94. Parasitic diagnosis: A journey from basic microscopy to cutting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617590/]