Microscopy vs. Molecular Methods for Protozoan Diagnosis: A Critical Comparison for Modern Laboratories
This article provides a comprehensive analysis for researchers, scientists, and drug development professionals on the evolving landscape of protozoan parasite diagnostics.
Microscopy vs. Molecular Methods for Protozoan Diagnosis: A Critical Comparison for Modern Laboratories
Abstract
This article provides a comprehensive analysis for researchers, scientists, and drug development professionals on the evolving landscape of protozoan parasite diagnostics. It explores the foundational principles of traditional microscopy and the technological advancements of molecular techniques. The content delves into methodological applications, troubleshooting common challenges, and presents validation data from recent comparative studies. By synthesizing evidence on sensitivity, specificity, and practical implementation, this review serves as a strategic guide for selecting diagnostic approaches, optimizing laboratory workflows, and informing the development of next-generation diagnostic tools and therapeutics.
The Diagnostic Paradigm Shift: From Microscopy to Molecular Assays
The Enduring Role and Inherent Limitations of Conventional Microscopy
Despite the advent of advanced molecular techniques, conventional microscopy remains a cornerstone for diagnosing pathogenic intestinal protozoa, which are significant causes of diarrheal diseases affecting approximately 3.5 billion individuals globally each year [1]. In many clinical and resource-limited settings, microscopic examination of stool specimens persists as the reference standard, providing a low-cost diagnostic method capable of detecting a broad range of parasites [2]. However, this technique faces significant challenges related to sensitivity, specificity, and operational requirements, which continue to fuel the comparison with emerging molecular diagnostics [1] [3].
This application note details the standardized protocols for conventional microscopic examination, analyzes its performance characteristics against molecular methods, and provides a technical resource for researchers and laboratory professionals working in parasitology diagnostics and drug development.
Established Protocols for Microscopic Diagnosis
Specimen Collection and Preparation
Optimal recovery and identification of protozoa depend critically on proper specimen handling. Key considerations include:
- Collection Interval: Collect multiple specimens, optimally every other day [2].
- Specimen Number: Analysis of three specimens increases detection yield by 11.3% for Giardia, 22.7% for E. histolytica, and 31.1% for D. fragilis compared to single samples [2].
- Preservation: Fresh specimens should be examined immediately or preserved appropriately. Fixed specimens (e.g., in Para-Pak media or formalin) enable concentration techniques and better morphological preservation [1].
Stool Concentration and Staining Workflow
The formalin-ethyl acetate (FEA) concentration method enhances parasite detection and represents the standard workflow for fixed specimens [1].
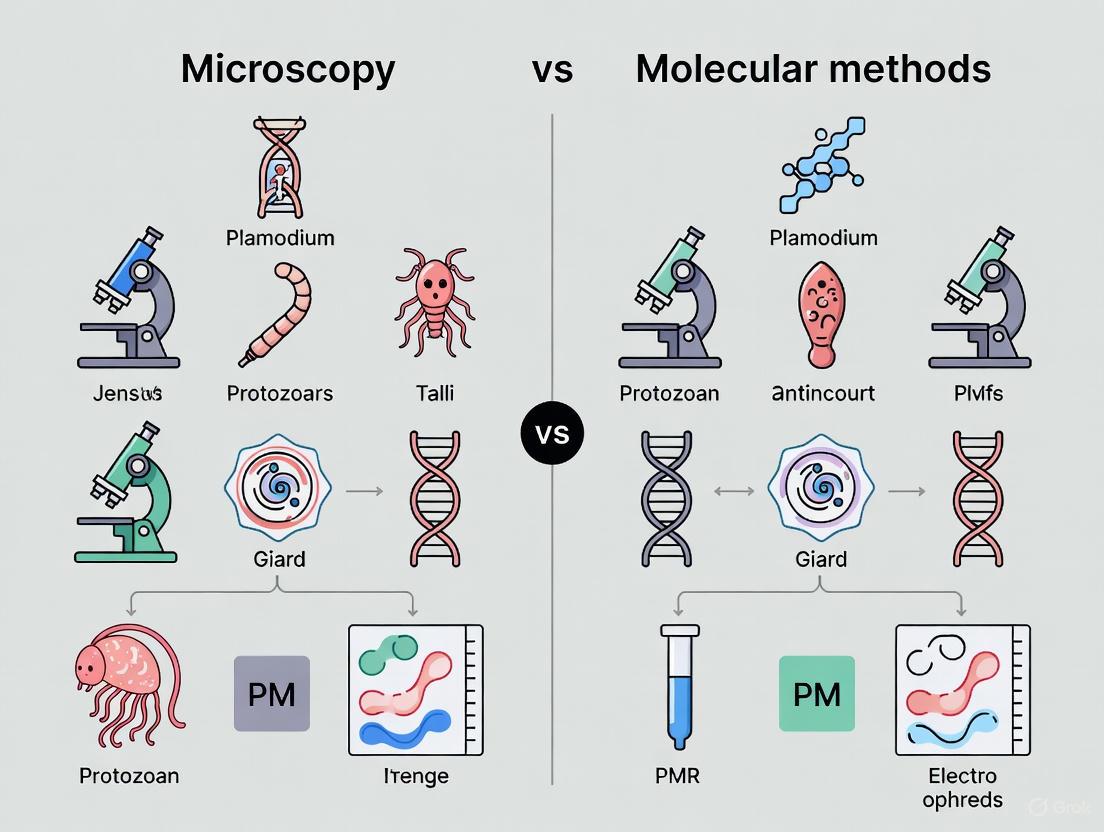
Figure 1: Standardized workflow for microscopic detection of intestinal protozoa, integrating both fresh and preserved sample pathways [1].
Microscopic Examination Procedure
- Fresh Specimens: Examine directly with Giemsa staining for immediate morphological assessment [1].
- Fixed Specimens: Process using the FEA concentration technique to concentrate parasitic elements [1].
- Microscopy: Systematically scan smears under both low-power (10×) and high-power (40×) objectives, with oil immersion (100×) for definitive identification.
- Quality Assurance: Review positive specimens with multiple trained technologists to maintain staff competency and identification accuracy [2].
Performance Analysis: Microscopy vs. Molecular Methods
Comparative Diagnostic Performance
Recent multicenter studies directly comparing microscopy with molecular techniques reveal distinct performance patterns across protozoan species.
Table 1: Comparative performance of microscopy versus molecular methods for protozoan detection [1] [4]
| Parasite | Microscopy Sensitivity Limitations | Molecular Method Advantages | Agreement (κ statistic) |
|---|---|---|---|
| Giardia duodenalis | Moderate; cyst excretion can be intermittent | High sensitivity and specificity; complete agreement between commercial & in-house PCR | Almost perfect (κ = 0.88) [4] |
| Cryptosporidium spp. | Low; requires special stains for oocyst visualization | Enhanced detection of low-intensity infections | Substantial (κ = 0.74) [4] |
| Entamoeba histolytica | Cannot differentiate from non-pathogenic E. dispar | Specific identification of pathogenic species | Critical for accurate diagnosis [1] |
| Dientamoeba fragilis | Low sensitivity (31.1% increase with 3 samples) [2] | Detects 16 additional infections missed by microscopy [4] | Limited sensitivity due to DNA extraction issues [1] |
Operational Limitations in Clinical Practice
Conventional microscopy faces significant implementation challenges that affect diagnostic reliability and efficiency.
Table 2: Key limitations of conventional microscopy in diagnostic parasitology [2]
| Limitation Category | Specific Challenges | Impact on Diagnostic Service |
|---|---|---|
| Technical Expertise | Requires experienced microbiologists; declining skilled workforce | Misidentification of species; inability to differentiate pathogens from non-pathogens |
| Sensitivity Issues | Single specimen detects only 58-72% of protozoa; irregular parasite shedding | False negatives; requirement for multiple specimens increases cost and turnaround |
| Operational Burden | Labor-intensive; time-consuming processing and analysis | Long turnaround times; testing often deferred until other tasks completed |
| Proficiency Maintenance | Low specimen positivity rates in non-endemic areas | Reduced technologist competency; challenges in training new staff |
| Differentiation Capacity | Cannot morphologically distinguish E. histolytica from E. dispar | Clinical misinterpretation; potential unnecessary treatment |
Essential Research Reagent Solutions
The following reagents and materials constitute the fundamental toolkit for conventional protozoan diagnosis.
Table 3: Essential research reagents for microscopic detection of intestinal protozoa
| Reagent/Material | Application | Technical Function |
|---|---|---|
| Para-Pak Preservation Media | Stool specimen transport and storage | Preserves parasite morphology for delayed examination [1] |
| Formalin-Ethyl Acetate (FEA) | Stool concentration | Separates parasitic elements from fecal debris for enhanced detection [1] |
| Giemsa Stain | Fresh specimen staining | Highlights nuclear and cytoplasmic details of trophozoites and cysts [1] |
| Saline Solution | Wet mount preparation | Provides medium for immediate examination of motile trophozoites [2] |
| Iodine Solution | Wet mount staining | Enhances internal structures of cysts for morphological identification [2] |
Integration with Modern Diagnostic Approaches
While microscopy remains fundamental, its limitations have driven development of supplemental and replacement technologies:
- Immunoassays: Immunochromatographic and ELISA tests offer rapid screening for specific pathogens like Giardia and Cryptosporidium but may yield false positives/negatives [1] [2].
- Molecular Diagnostics: PCR-based methods provide superior sensitivity and specificity, particularly for low-prevalence settings, but require DNA extraction optimization and cannot detect organisms not targeted by the assay [1] [5].
- Algorithmic Testing: Some laboratories implement front-line antigen testing followed by microscopy for negatives, though this requires clinical context often unavailable to laboratories [2].
The relationship between diagnostic methodologies can be visualized as a complementary system where each approach addresses specific limitations.
Figure 2: Evolution of diagnostic technologies for intestinal protozoa, showing complementary strengths at each developmental stage [3] [5].
Conventional microscopy maintains an enduring role in protozoan diagnosis due to its low cost, broad spectrum detection capability, and accessibility in resource-limited settings. However, its inherent limitations—including operator dependency, variable sensitivity, and inability to differentiate morphologically similar species—necessitate supplemental approaches for comprehensive diagnostic accuracy. Modern laboratories increasingly implement integrated diagnostic algorithms that leverage the strengths of both conventional and molecular methods, particularly for pathogenic species like Entamoeba histolytica and Dientamoeba fragilis where microscopic differentiation proves problematic. For researchers and drug development professionals, understanding these limitations is crucial for designing effective diagnostic strategies and interpreting clinical trial data across different geographical and resource settings.
The Global Burden of Protozoan Infections Driving Diagnostic Innovation
Pathogenic intestinal protozoa represent a significant global health challenge, with an estimated 3.5 billion people affected annually and approximately 1.7 billion episodes of diarrheal disorders each year [6] [7]. These infections contribute substantially to global diarrheal morbidity and mortality, particularly in resource-limited settings [8]. The most clinically significant enteric protozoa include Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, which collectively account for an estimated 500 million annual diarrheal cases worldwide [8]. These pathogens disproportionately affect children under five in low- and middle-income countries (LMICs), where they are responsible for 10-15% of diarrheal deaths and are increasingly recognized as contributors to long-term growth faltering and cognitive impairment [8].
The epidemiological control of protozoan diseases remains unsatisfactory due to difficulties in vector and reservoir control, while progress in vaccine development has been slow and arduous [9]. Currently, chemotherapy remains an essential component of both clinical management and disease control programs in endemic areas, though existing drugs face limitations including high cost, poor compliance, drug resistance, low efficacy, and poor safety [9]. Accurate diagnosis is therefore critical for both effective treatment and understanding the true burden of these diseases, yet diagnostic challenges persist, with microscopy-based surveillance potentially missing 30-50% of cases detectable by molecular methods [8].
Global Burden and Distribution
Quantitative Assessment of Protozoan Infections
Recent meta-analyses reveal that protozoan pathogens are found in approximately 7.5% of diarrheal cases globally, with the highest prevalence rates observed in the Americas and Africa [8]. The distribution and impact of these pathogens vary significantly by species, geographic region, and population characteristics.
Table 1: Global Prevalence and Health Impact of Major Intestinal Protozoa
| Parasite | Global Prevalence in Diarrheal Cases | Annual Symptomatic Infections | Key Health Impacts |
|---|---|---|---|
| Giardia duodenalis | 2-7% (developed countries), 30-40% (developing countries) [8] | ~280 million [8] [7] | Watery diarrhea, bloating, malabsorption, chronic malnutrition [8] |
| Cryptosporidium spp. | 1-4% worldwide; up to 10% in children in low-income regions [8] | ~200 million (estimated) [8] | Severe watery diarrhea; life-threatening in immunocompromised patients [8] |
| Entamoeba histolytica | ~1-2% true infections (10% carry Entamoeba species) [8] | Not specified | Amoebiasis - bloody diarrhea, dysentery, liver abscess [8] |
| Blastocystis spp. | 10-60% worldwide [8] | Not specified | Sometimes causes diarrhea and abdominal pain; often asymptomatic [8] |
Regional Distribution and Risk Populations
The burden of protozoan infections displays striking geographical disparities. The highest age-standardized prevalence rates for diseases like Chagas disease are found in southern Latin America (2485.9 per 100,000) and Andean Latin America (2313.8 per 100,000) [10]. While prevalence rates in endemic countries have decreased over time due to socioeconomic development and public health measures, non-endemic regions have experienced notable increases in prevalence due to migration from endemic countries [10].
Vulnerable populations include young children, pregnant people, travelers, and immunocompromised individuals, who are most likely to fall ill and endure chronic complications [11]. Nutritional status significantly influences both infection susceptibility and clinical outcomes, with malnourished children facing significantly higher mortality risks from infections like cryptosporidiosis [8].
Diagnostic Challenges and Methodological Comparisons
Limitations of Conventional Microscopy
Microscopic examination of concentrated fecal specimens remains the reference diagnostic method in clinical laboratories for protozoan intestinal infections, primarily due to its low cost and utility in resource-limited settings [6] [7]. However, this method presents substantial limitations:
- Requires qualified microscopists and is time-consuming [7]
- Exhibits limited sensitivity and specificity compared to molecular methods [6]
- Cannot differentiate closely related species (e.g., pathogenic E. histolytica from non-pathogenic E. dispar) [7]
- May miss 30-50% of cases detectable by molecular methods [8]
Immunofluorescence microscopy shows greater sensitivity and specificity than traditional microscopy but is expensive and still requires expert personnel [7]. Similarly, immunochromatography and enzyme-linked immunosorbent assay (ELISA) are regarded as suitable techniques for rapid screening but frequently yield elevated rates of false positive and false negative results [7].
Advancements in Molecular Diagnostics
Molecular diagnostic technologies, particularly real-time PCR (RT-PCR), are gaining traction in non-endemic areas characterized by low parasitic prevalence owing to their enhanced sensitivity and specificity [6] [7]. Recent multicenter studies comparing commercial and in-house molecular tests have demonstrated their potential while highlighting specific technical challenges.
Table 2: Performance Comparison of Diagnostic Methods for Intestinal Protozoa
| Parasite | Microscopy Limitations | Molecular Method Advantages | Technical Challenges in PCR Detection |
|---|---|---|---|
| Giardia duodenalis | Moderate sensitivity and specificity [6] | Complete agreement between commercial and in-house PCR methods; high sensitivity and specificity [6] [7] | Minimal challenges; reliable detection [6] |
| Cryptosporidium spp. | Cannot differentiate species; variable sensitivity [7] | High specificity; essential for accurate species identification [6] [7] | Limited sensitivity due to inadequate DNA extraction from oocysts [6] [7] |
| Entamoeba histolytica | Cannot differentiate from non-pathogenic E. dispar [7] | Critical for accurate diagnosis and differentiation from non-pathogenic species [6] [7] | Less challenging; effective detection with proper methods [6] |
| Dientamoeba fragilis | Detection challenging; often missed [6] | Enables detection of this neglected pathogen [6] [7] | Inconsistent results; limited sensitivity [6] [7] |
Experimental Protocols for Diagnostic Evaluation
Multicenter Study Design for Method Comparison
A recent multicenter study involving 18 Italian laboratories provides a robust protocol for comparing diagnostic methods for intestinal protozoa [7]. The study analyzed 355 stool samples (230 freshly collected and 125 stored in preservation media) examining infections with Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis [6] [7].
Sample Processing Protocol:
- Sample Collection: Collect fresh stool samples or preserve in Para-Pak media [7]
- Microscopic Examination: Process all samples using conventional microscopy following WHO and CDC guidelines [7]
- Staining Procedures: Stain fresh samples with Giemsa; process fixed samples using the FEA (formalin-ethyl acetate) concentration technique [7]
- Storage: Freeze samples promptly at -20°C until molecular analysis [7]
DNA Extraction and Molecular Analysis
DNA Extraction Protocol:
- Sample Preparation: Mix 350 µl of S.T.A.R (Stool Transport and Recovery Buffer) with approximately 1 µl of each fecal sample using a sterile loop [7]
- Incubation: Incubate for 5 minutes at room temperature [7]
- Centrifugation: Centrifuge at 2000 rpm for 2 minutes [7]
- Supernatant Collection: Carefully collect 250 µl of supernatant and transfer to a fresh tube [7]
- Internal Control: Combine with 50 µl of internal extraction control [7]
- Automated Extraction: Extract DNA using MagNA Pure 96 DNA and Viral NA Small Volume Kit on MagNA Pure 96 System [7]
In-house RT-PCR Amplification:
- Reaction Mixture: 5 µl MagNA extraction suspension, 12.5 µl 2× TaqMan Fast Universal PCR Master Mix, 2.5 µl primers and probe mix, sterile water to final volume of 25 µl [7]
- PCR Cycling Conditions:
- 1 cycle: 95°C for 10 minutes
- 45 cycles: 95°C for 15 seconds followed by 60°C for 1 minute [7]
- Detection System: ABI 7900HT Fast Real-Time PCR System [7]
Diagnostic Workflows and Methodological Integration
The following diagnostic workflow illustrates the integrated approach to protozoan diagnosis, combining traditional and molecular methods:
Research Reagent Solutions for Protozoan Diagnosis
The implementation of robust diagnostic protocols requires specific research reagents and laboratory materials. The following table details essential solutions for protozoan detection studies:
Table 3: Essential Research Reagents for Protozoan Diagnostic Studies
| Reagent/Material | Manufacturer/Source | Function in Protocol |
|---|---|---|
| Para-Pak Preservation Media | N/A | Preserves stool samples for transport and storage; maintains parasite integrity [7] |
| S.T.A.R Buffer (Stool Transport and Recovery Buffer) | Roche Applied Sciences | Facilitates stool sample processing for DNA extraction; stabilizes nucleic acids [7] |
| MagNA Pure 96 DNA and Viral NA Small Volume Kit | Roche Applied Sciences | Automated nucleic acid extraction using magnetic separation technology [7] |
| TaqMan Fast Universal PCR Master Mix | Thermo Fisher Scientific | Provides enzymes, dNTPs, and optimized buffer for efficient RT-PCR amplification [7] |
| Giemsa Stain | Various suppliers | Stains fresh stool samples for microscopic identification of parasites [7] |
| Formalin-Ethyl Acetate (FEA) | Various suppliers | Concentration technique for fixed stool samples prior to microscopic examination [7] |
| AusDiagnostics RT-PCR Test | AusDiagnostics Company (R-Biopharm Group) | Commercial molecular test for detection of major intestinal protozoa [6] [7] |
Discussion and Future Perspectives
Molecular methods show significant promise for the diagnosis of intestinal protozoan infections, particularly in non-endemic regions with low prevalence where high sensitivity is crucial [6] [7]. The molecular assays evaluated in recent studies perform well for G. duodenalis and Cryptosporidium spp. in fixed fecal specimens, though detection of D. fragilis remains inconsistent [6]. Overall, PCR results from preserved stool samples demonstrate better performance than those from fresh samples, likely due to superior DNA preservation in fixed specimens [6].
The integration of molecular diagnostics into parasitology laboratories represents a significant advancement, yet requires further standardization of sample collection, storage, and DNA extraction procedures to ensure consistent results [6]. While PCR techniques offer reliable and cost-effective parasite identification, some authors recommend molecular techniques as a complementary method rather than a replacement for conventional microscopy, as microscopic examination can reveal additional parasitic intestinal infections not targeted by specific PCR assays [7].
Future directions in protozoan diagnosis include the exploration of innovative drug repurposing strategies [12], enhanced food safety protocols to address foodborne transmission [11], and the application of artificial intelligence to improve diagnostic accuracy [12]. As the field continues to evolve, the combination of traditional and molecular methods will likely provide the most comprehensive approach to managing the global burden of protozoan infections.
Comparative Diagnostic Performance of Detection Methods
Table 1: Comparison of diagnostic sensitivity across detection methods for key protozoan pathogens.
| Pathogen | Microscopy | Immunoassay | PCR-Based Methods | Key Diagnostic Challenges |
|---|---|---|---|---|
| Giardia duodenalis | Variable sensitivity [1] | Suitable for rapid screening [1] | High sensitivity and specificity [1] [6] | Differentiation of viable vs. non-viable cysts [13] |
| Cryptosporidium spp. | 6%-23.2% [14] [15] | 15% [14] | 18%-26.8% [14] [15] | Requires high oocyst concentration (>50,000/mL) for microscopy [14] |
| Entamoeba histolytica | 3.17% [16] | Coproantigen ELISA: 4.6% [16] | Nested PCR: 4.75% [16]; Real-time PCR sensitivity: 75-100% [17] | Microscopy cannot differentiate from non-pathogenic E. dispar [17] [16] |
| Blastocystis hominis | Lower sensitivity than culture/molecular methods [18] | Not prominently reported | HRM analysis enables subtyping [18] | Pathogenicity debated; requires subtyping for clinical relevance [18] |
Detailed Experimental Protocols
Conventional Microscopy and Staining
2.1.1 Direct Wet Mount Microscopy
- Principle: Direct visualization of motile trophozoites, cysts, oocysts, or other parasitic forms in fresh stool.
- Procedure:
- Sample Preparation: Emulsify a small portion of fresh, unpreserved stool (approximately 1-2 mg) in a drop of 0.9% saline on a clean glass slide. Prepare a second smear in a drop of Lugol's iodine solution [16].
- Examination: Apply a coverslip and examine systematically under a light microscope using 10x and 40x objectives [14] [16].
- Identification: Look for characteristic structures: Giardia trophozoites/cysts, Cryptosporidium oocysts, Entamoeba cysts/trophozoites, or Blastocystis vacuolar forms [18] [16].
2.1.2 Concentration Techniques (Formalin-Ether Acetate - FEA)
- Principle: Increase detection sensitivity by concentrating parasitic elements.
- Procedure:
2.1.3 Special Stains
- Modified Kinyoun's Acid-Fast Stain (for Cryptosporidium):
- Procedure: Prepare a stool smear, fix it on a hot plate at 55°C, and stain with Kinyoun's carbol fuchsin for 1 minute. Decolorize with 1% HCl for 2 minutes, then counterstain with methylene blue. Examine under oil immersion (100x objective); Cryptosporidium oocysts stain bright red [14].
Immunological and Antigen-Detection Methods
2.2.1 Coproantigen Enzyme-Linked Immunosorbent Assay (ELISA)
- Principle: Detect pathogen-specific antigens in stool samples using antibody-coated wells.
- Procedure (for E. histolytica):
- Coating: Use a microtiter plate pre-coated with specific antibodies [16].
- Incubation: Add 100 µL of diluted stool specimen to the well and incubate for 1 hour at 37°C. Wash the plate [16].
- Conjugate: Add 100 µL of horseradish peroxidase-conjugated antibody and incubate for another hour at 37°C. Wash again [16].
- Detection: Add 100 µL of TMB substrate, incubate for 15 minutes at room temperature, and stop the reaction with a stop solution. Measure the absorbance at 450 nm. A sample is positive if the optical density exceeds the predetermined cutoff [16].
2.2.2 Immunochromatography (ICT)
- Principle: Rapid lateral flow test for detecting parasitic antigens.
- Procedure (for Cryptosporidium):
Molecular Detection and Characterization
2.3.1 DNA Extraction from Stool Samples
- Protocol (Silica Column-Based):
- Lysis: Transfer 200 mg of stool to a bead tube. Add lysis buffer and Proteinase K, then incubate at 60°C for 20 minutes [18].
- Binding: Centrifuge the sample and load the supernatant onto a silica column [18].
- Washing and Elution: Wash the column with wash buffers to remove impurities. Elute the purified DNA in 50-200 µL of elution buffer or deionized water [18]. Store extracted DNA at -20°C.
2.3.2 Real-Time PCR (RT-PCR) for Entamoeba histolytica
- Principle: Amplify and detect species-specific DNA sequences in real-time using fluorescent probes.
- Reaction Setup:
- Cycling Conditions: Follow standard real-time PCR cycles (denaturation, annealing, extension) on a suitable thermocycler with fluorescence detection [1]. Results are interpreted based on Cycle Threshold (Ct) values.
2.3.3 High-Resolution Melting (HRM) Analysis for Blastocystis Subtyping
- Principle: Distinguish Blastocystis subtypes based on the unique melting temperature of PCR amplicons from the SSU rRNA gene.
- Procedure:
- PCR Amplification: Perform real-time PCR with EvaGreen dye and specific primers targeting the SSU rRNA gene [18].
- Melting Curve Analysis: After amplification, gradually increase the temperature while continuously monitoring fluorescence. The dye is released from the DNA as it denatures, causing a drop in fluorescence [18].
- Subtype Identification: Different subtypes (ST1-ST7, etc.) are identified by their characteristic melting curve profiles and temperatures [18].
Diagnostic Workflow and Method Selection
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential reagents and materials for protozoan pathogen research and diagnosis.
| Category | Specific Item / Kit | Primary Function | Application Example |
|---|---|---|---|
| Cell Culture | Diamond's TYI-S-33 Medium | In vitro culturing of trophozoites | Giardia lamblia trophozoite culture [13] |
| Staining Reagents | Modified Kinyoun's Carbol Fuchsin | Acid-fast staining of oocysts | Cryptosporidium detection [14] |
| Immunoassays | Crypto/Giardia Rapid ICT Assay (Biotech, Spain) | Rapid immunochromatographic antigen detection | Cryptosporidium and Giardia screening [14] |
| Nucleic Acid Extraction | FavorPrep Stool DNA Isolation Mini Kit; MagNA Pure 96 System | Isolation of PCR-quality DNA from complex stool matrices | DNA extraction for PCR [1] [18] |
| PCR Reagents | HOT FIREPol EvaGreen HRM Mix; TaqMan Fast Universal PCR Master Mix | Fluorescent detection in real-time PCR and HRM | Blastocystis subtyping by HRM [18]; Multiplex RT-PCR [1] |
| Antibodies | Anti-Giardia Cyst Antibody (e.g., sc-57744) | Immunofluorescence labeling and confirmation | Cyst wall visualization in Giardia [13] |
The diagnosis of intestinal protozoan infections represents a significant challenge in clinical and research settings. For decades, microscopy has served as the conventional diagnostic method, yet it is hampered by limitations in sensitivity, specificity, and its inability to differentiate morphologically identical species [19] [1] [20]. Molecular detection methods, particularly Polymerase Chain Reaction (PCR) and Real-Time PCR (RT-PCR), have emerged as powerful tools that overcome these limitations, providing superior accuracy, species-level differentiation, and higher throughput for protozoan detection [19] [21] [20]. This document outlines the fundamental principles of these molecular techniques and provides detailed application protocols within the context of protozoan diagnosis, supporting research that compares traditional and molecular diagnostic approaches.
Fundamental Principles of PCR and RT-PCR
Polymerase Chain Reaction (PCR)
The Polymerase Chain Reaction (PCR) is a laboratory technique for amplifying a specific DNA sequence exponentially [22]. Introduced by Kary Mullis in 1985, it utilizes a thermostable DNA polymerase (typically Taq polymerase) to synthesize DNA strands complementary to a target sequence. The process involves three core steps repeated for 30-40 cycles in a thermal cycler:
- Denaturation: The double-stranded DNA template is heated to 90–95°C, breaking hydrogen bonds to separate it into two single strands.
- Annealing: The temperature is lowered to 55–72°C, allowing short, sequence-specific primers to bind (anneal) to their complementary sequences on either side of the target DNA.
- Extension: The temperature is raised to 72°C, the optimal temperature for Taq polymerase to add nucleotides to the 3' end of each primer, synthesizing new DNA strands [22].
This process can amplify a target sequence by a factor of 10^6 to 10^9, producing enough DNA for analysis by methods such as agarose gel electrophoresis [22].
Real-Time PCR (RT-PCR)
Real-Time PCR (also known as quantitative PCR or qPCR) builds upon conventional PCR by enabling the monitoring of amplification as it occurs in real time [22]. This is achieved through fluorescent reporters, which can be either:
- DNA-binding dyes: Non-specific dyes that fluoresce when intercalated with double-stranded DNA.
- Sequence-specific probes: Fluorescently labelled probes (e.g., TaqMan) that provide higher specificity by only binding to the exact target sequence [22].
The key output is the Cycle threshold (Ct), the number of cycles required for the fluorescent signal to cross a predefined threshold. The Ct value is inversely proportional to the starting quantity of the target nucleic acid, allowing for both detection and quantification [22]. RT-PCR eliminates the need for post-amplification processing, reduces the risk of contamination, and provides quantitative data, making it highly suitable for diagnostic applications [19] [22].
Performance Comparison: Microscopy vs. Molecular Methods
Molecular methods offer significant advantages in diagnostic sensitivity and specificity for detecting key intestinal protozoa, as shown by recent comparative studies.
Table 1: Comparative Performance of Microscopy vs. Multiplex RT-PCR for Protozoan Detection
| Protozoan | Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Key Advantage of RT-PCR |
|---|---|---|---|---|---|
| Blastocystis hominis | 93.0 [21] | 98.3 [21] | 85.1 [21] | 99.3 [21] | Higher throughput, objective readout [21] |
| Cryptosporidium spp. | 100 [21] | 100 [21] | 100 [21] | 100 [21] | Superior sensitivity, species differentiation [1] [20] |
| Cyclospora cayetanensis | 100 [21] | 100 [21] | 100 [21] | 100 [21] | Eliminates need for expert microscopy [21] |
| Dientamoeba fragilis | 100 [21] | 99.3 [21] | 88.5 [21] | 100 [21] | Detects parasite without cyst stage easily missed by microscopy [1] |
| Entamoeba histolytica | 33.3 - 75* [21] | 100 [21] | 100 [21] | 99.6 [21] | Differentiates pathogenic E. histolytica from non-pathogenic E. dispar [19] [20] |
| Giardia duodenalis | 100 [21] | 98.9 [21] | 68.8 [21] | 100 [21] | High sensitivity and specificity; automatable [1] [21] |
Sensitivity for *E. histolytica increased from 33.3% with fresh specimens to 75% when frozen specimens were included [21].
Table 2: Diagnostic Performance of Different PCR Primer Sets for Trypanosoma lewisi
| Primer Set | Sensitivity (%) | Specificity (%) | Diagnostic Reliability |
|---|---|---|---|
| LEW1S/LEW1R | 100 [23] | 97.22 [23] | Highest accuracy; consistent, distinct amplicons [23] |
| CATLew F/CATLew R | 96.43 [23] | 97.22 [23] | High performance [23] |
| TC121/TC122 | 67.86 [23] | 97.22 [23] | Moderate sensitivity [23] |
Experimental Protocols for Molecular Detection of Intestinal Protozoa
Protocol: Duplex RT-PCR for Entamoeba and Cryptosporidium
This protocol, adapted from recent research, enables simultaneous detection of multiple protozoa in a 10 µL reaction volume [19].
1. Sample Collection and DNA Extraction
- Sample Collection: Collect stool samples and store unpreserved at -20°C or in preservation media (e.g., Cary-Blair media) for molecular analysis [21]. Preserved samples often yield better DNA quality [1].
- DNA Extraction: Use automated, high-throughput systems (e.g., Hamilton STARlet with STARMag kit) or manual kits (e.g., QIAamp Fast DNA Stool Mini Kit) [21] [24]. Include an internal extraction control to monitor inhibition and extraction efficiency [24]. Elute DNA in a final volume of 100 µL [21].
2. Primer and Probe Design
- Target Genes: Conserved genomic regions, such as the small subunit ribosomal RNA (SSU rRNA) gene, are ideal targets [19].
- Design Criteria:
- Primer/Probe Sequences:
Table 3: Primer and Probe Sequences for Protozoan Detection
Organism Forward Primer (5'→3') Reverse Primer (5'→3') Probe Sequence (5'→3') Entamoeba histolytica / dispar AGG ATT GGA TGA AAT TCA GAT GTA CA [19] TAA GTT TCA GCC TTG TGA CCA TAC [19] TGA CGG AGT TAA TTG CAA TTA T [19] Cryptosporidium spp. ACA TGG ATA ACC GTG GTA ATT CT [19] CAA TAC CCT ACC GTC TAA AGC TG [19] ACT CGA CTT TAT GGA AGG GTT GTA T [19] Chilomastix mesnili TGC CTT GTC TTT TTG TTA CCA TAA AGA [19] GTC TGA ACT GTT ATT CCA TAC TGC AA [19] GCA GGT CGT GCC CTT GTG G [19]
3. RT-PCR Reaction Setup
- Reaction Mix (10 µL total volume):
- Thermal Cycling Conditions (on Bio-Rad CFX96 or similar):
- Initial Denaturation: 95°C for 10-20 min.
- 45 Cycles of:
- Denaturation: 95°C for 10 sec.
- Annealing/Extension: 60°C for 1 min (with fluorescence acquisition) [21].
4. Data Analysis
- A sample is considered positive if the cycle threshold (Ct) value is ≤43 [21].
- For melt curve analysis, ramp temperature from 40°C to 80°C in 1°C increments. A consistent melt temperature (e.g., 63-64°C for D. fragilis) confirms specific amplification, while shifts (e.g., 9°C lower) suggest cross-reactivity with non-target organisms [24].
Workflow: Molecular Detection of Intestinal Protozoa
The following diagram illustrates the complete workflow for the molecular detection of intestinal protozoa, from sample collection to final analysis.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Reagents and Materials for Molecular Detection of Protozoa
| Item | Function / Application | Example Products / Specifications |
|---|---|---|
| DNA Extraction Kits | Isolation of high-quality DNA from complex stool matrices; critical for assay sensitivity. | QIAamp Fast DNA Stool Mini Kit [24], STARMag Universal Cartridge [21] |
| PCR Master Mix | Provides buffer, dNTPs, and thermostable DNA polymerase for amplification. | TaqMan Fast Universal PCR Master Mix [1] |
| Primers & Probes | Sequence-specific binding for target amplification and detection. | HPLC-purified, designed against SSU rRNA [19] |
| Commercial Multiplex Kits | Validated, standardized panels for simultaneous detection of multiple pathogens. | Seegene Allplex GI-Parasite Assay [21], EasyScreen Enteric Protozoan Detection Kit [24] |
| Internal Controls | Monitor PCR inhibition and DNA extraction efficiency; essential for quality control. | qPCR Extraction Control Kits [24] |
| Automated Platforms | High-throughput, reproducible nucleic acid extraction and PCR setup. | Hamilton STARlet [21], MagNA Pure 96 System [1] |
| Real-Time PCR Cyclers | Instrument for amplification and fluorescent signal detection. | Bio-Rad CFX96 [19] [21] |
Critical Considerations for Molecular Detection
Primer Design and Specificity
Robust primer design is foundational for successful molecular detection. For protozoa, this involves:
- Accessing Genomic Data: Retrieve target sequences (e.g., SSU rRNA) from databases like NCBI [19].
- Identifying Conserved Regions: Align sequences to find highly conserved regions for broad detection and variable regions for species-specific differentiation [19].
- Specificity Checks: Use BLASTN to ensure minimal similarity to non-target organisms, especially close relatives [19] [25]. For example, primers must distinguish pathogenic E. histolytica from non-pathogenic E. dispar [19] [20].
- Validation: Test primers against a panel of positive and negative controls. Melt curve analysis and DNA sequencing of amplicons are crucial for verifying specificity and identifying cross-reactivity, as seen with Simplicimonas sp. in cattle samples misidentified as D. fragilis [24].
Optimization and Troubleshooting
- Annealing Temperature Optimization: Test a gradient (e.g., 55–65°C) to find the temperature yielding the lowest Ct and highest fluorescence with no non-specific amplification [25].
- Inhibition Management: Stool samples contain PCR inhibitors (e.g., bil salts, complex polysaccharides). Dilution of extracted DNA (e.g., 1:5) or use of inhibitor-resistant polymerases can mitigate this [22] [24].
- Cycle Threshold (Ct) Limit: Setting a maximum Ct (e.g., ≤43) helps prevent reporting false positives from late, non-specific amplification [21] [24]. Reducing the total number of cycles (e.g., to less than 40) is also recommended for the same reason [24].
Comparison of Molecular and Microscopy Methods
The following diagram summarizes the key procedural differences and outputs between conventional microscopy and molecular RT-PCR for protozoan diagnosis.
Implementing Modern Diagnostic Protocols: Commercial Kits, In-House Assays, and Workflow Integration
Commercial Multiplex PCR Panels vs. Laboratory-Developed In-House Tests
The diagnosis of pathogenic intestinal protozoa, significant global causes of diarrheal diseases affecting approximately 3.5 billion people annually, has long relied on traditional microscopy [7]. While microscopy remains a low-cost reference method, it is constrained by limitations in sensitivity, specificity, and the need for experienced personnel, particularly for differentiating morphologically similar species [7] [26]. Molecular diagnostics, especially real-time PCR (RT-PCR) technologies, have emerged as powerful alternatives, offering enhanced sensitivity and specificity [7] [26]. Clinical laboratories implementing these molecular methods face a critical choice: adopt commercially developed, CE-IVD/FDA-marked multiplex PCR panels or utilize laboratory-developed tests (LDTs), often referred to as "in-house" assays. This application note delves into this comparison, framing the discussion within a broader thesis on microscopy versus molecular methods for protozoan diagnosis. It provides a structured analysis of performance data, detailed experimental protocols, and essential considerations for researchers and drug development professionals navigating this evolving diagnostic landscape.
Performance Comparison: Commercial Kits vs. In-House Assays
The relative performance of commercial multiplex PCR panels and in-house tests varies significantly across different pathogens and study conditions. The tables below summarize key comparative data from recent studies.
Table 1: Comparative Sensitivity of Commercial Multiplex PCR Panels for Intestinal Protozoa
| Commercial PCR Panel | Giardia duodenalis | Cryptosporidium spp. | Entamoeba histolytica | Dientamoeba fragilis | Study |
|---|---|---|---|---|---|
| BD Max | 89% | 75% (C. parvum/hominis) | Consistent results | Not Specified | Autier et al. [27] |
| RIDAGENE | 41% | 100% (all species) | Consistent results | 71% | Autier et al. [27] |
| G-DiaPara | 64% | 100% (C. parvum/hominis) | Consistent results | Not Specified | Autier et al. [27] |
| AusDiagnostics | High (similar to microscopy) | High Specificity, Limited Sensitivity | Critical for accurate diagnosis | Inconsistent | [7] |
Table 2: Performance Comparison of In-House vs. Commercial PCR for Helminths
| Parameter | In-House RT-PCR | Biosynex Helminths AMPLIQUICK RT-PCR | Notes |
|---|---|---|---|
| S. mansoni Sensitivity | Not significantly different (p=1) | Not significantly different (p=1) | Performance comparable [28] |
| S. mansoni Specificity | Not significantly different (p=1) | Not significantly different (p=1) | Performance comparable [28] |
| S. stercoralis Sensitivity | Not significantly different (p=1) | Not significantly different (p=1) | Performance comparable [28] |
| S. stercoralis Specificity | Not significantly different (p=1) | Not significantly different (p=1) | Performance comparable [28] |
| Concordance for S. mansoni cases | Poor (AC1 = 0.38) | Poor (AC1 = 0.38) | Despite comparable metrics, discrepancies exist [28] |
| Concordance for S. stercoralis cases | Good (AC1 = 0.78) | Good (AC1 = 0.78) | [28] |
Experimental Protocols
Protocol: Multicenter Comparison of Commercial and In-House PCR for Intestinal Protozoa
This protocol is adapted from a multicenter study comparing a commercial RT-PCR test (AusDiagnostics) and an in-house RT-PCR assay against traditional microscopy for identifying infections with Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis [7].
1. Sample Collection and Storage
- Collect stool samples (e.g., 355 consecutive samples).
- Examine all samples using conventional microscopy (e.g., Giemsa staining for fresh samples; formalin-ethyl acetate (FEA) concentration technique for preserved samples) as a reference method.
- Preserve samples. Note: The study found that PCR results from preserved stool samples were better than those from fresh samples, likely due to superior DNA preservation [7].
- Store samples frozen at -20°C until molecular analysis.
2. DNA Extraction
- Use an automated nucleic acid extraction system (e.g., MagNA Pure 96 System with the MagNA Pure 96 DNA and Viral NA Small Volume Kit).
- Employ a stool transport and recovery buffer (e.g., S.T.A.R. Buffer).
- Include an internal extraction control.
- Critical Step: The study identified DNA extraction from the robust wall of protozoan oocysts as a critical challenge, directly impacting sensitivity [7].
3. In-House RT-PCR Amplification
- Reaction Mixture:
- 5 µL of extracted DNA.
- 12.5 µL of 2x TaqMan Fast Universal PCR Master Mix.
- 2.5 µL of custom primer and probe mix.
- Sterile water to a final volume of 25 µL.
- Cycling Conditions on a real-time PCR system (e.g., ABI 7900HT):
- 1 cycle: 95°C for 10 minutes (initial denaturation).
- 45 cycles: 95°C for 15 seconds (denaturation) and 60°C for 1 minute (annealing/extension).
4. Commercial RT-PCR Assay
- Perform the commercial test (e.g., AusDiagnostics kit) strictly according to the manufacturer's instructions on the same DNA extracts.
5. Data Analysis
- Compare the sensitivity, specificity, and positive/negative predictive values of the in-house and commercial PCR methods against the microscopy reference standard.
Protocol: Comparative Performance Evaluation of Commercial Multiplex PCR Assays
This protocol outlines the methodology for a head-to-head evaluation of multiple commercial multiplex PCR assays using a characterized DNA panel, as demonstrated in a study comparing four commercial kits [26].
1. Reference DNA Panel Preparation
- Establish a well-characterized DNA panel extracted from stool specimens of clinically confirmed patients.
- Include positive samples for target pathogens (e.g., Cryptosporidium hominis, C. parvum, Giardia duodenalis, Entamoeba histolytica) and negative controls.
- Include DNA from other organisms (e.g., E. dispar, Leishmania infantum) to assess cross-reactivity.
- Prepare multiple aliquots of each DNA sample to avoid freeze-thaw degradation.
2. Multiplex Real-Time PCR Testing
- Test all commercial kits (e.g., Diagenode Gastroenteritis/Parasite Panel I, R-Biopharm RIDAGENE Parasitic Stool Panel, Seegene Allplex Gastrointestinal Parasite Panel, FTD Stool Parasites) in parallel.
- Use a standardized input of DNA (e.g., 5 μL per reaction for most assays).
- Perform all reactions in a 25 μL final volume, following the manufacturer's instructions.
- Run assays on an appropriate real-time PCR cycler (e.g., Corbett Rotor-Gene 6000, CFX96, Mx3005P).
- Include negative, positive, and inhibition controls in each run.
3. Assessment of Mixed Infections and Limit of Detection
- Simulated Co-infections: Artificially generate mixes by combining equal amounts of positive DNA samples for different pathogens to mimic natural co-infections and assess assay specificity in a complex background [26].
- Relative Limit of Detection: Perform ten-fold serial dilutions of positive DNA samples to determine and compare the detection limits of each assay [26].
4. Analysis
- Calculate diagnostic sensitivity and specificity for each assay against the reference panel.
- Compare the results from simulated mixed infections and limit of detection experiments across the different kits.
Decision Workflow: Selecting a Diagnostic PCR Approach
The following diagram outlines the key decision points and considerations for researchers and laboratories when choosing between commercial and in-house PCR tests.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Molecular Diagnosis of Intestinal Parasites
| Reagent / Solution | Function / Application | Examples / Notes |
|---|---|---|
| Stool Transport & Recovery Buffer | Stabilizes nucleic acids in stool samples prior to DNA extraction, reducing PCR inhibitors. | S.T.A.R. Buffer (Roche) [7] [28] |
| Automated Nucleic Acid Extraction Systems | Standardizes and automates DNA purification, a critical step for sensitivity and reproducibility. | MagNA Pure 96 System (Roche) [7], KingFisher Flex (Thermo Fisher) [29], STARlet (Seegene) [29] |
| Internal Extraction Controls | Monitors efficiency of DNA extraction and identifies PCR inhibition. | Phocid alphaherpesvirus 1 (PhHV-1) [28] |
| Commercial Multiplex PCR Master Mixes | Pre-mixed solutions containing enzymes, dNTPs, and buffers optimized for multiplex real-time PCR. | TaqMan Fast Universal PCR Master Mix [7] |
| Commercial Protozoan PCR Panels | CE-IVD/FDA-marked kits for standardized, simultaneous detection of multiple enteric protozoa. | AusDiagnostics [7], RIDAGENE [27], BD MAX [26], Allplex (Seegene) [26] |
| Digital PCR Systems | Provides absolute quantification of target DNA without a standard curve; offers superior accuracy for viral load and co-infection studies. | QIAcuity (QIAGEN) [29] |
Regulatory and Implementation Considerations
The regulatory landscape for LDTs is dynamic and varies by region. In the United States, the FDA has historically exercised enforcement discretion, but this policy has been subject to recent legal challenges and rulemaking. As of late 2025, a federal court vacated a 2024 rule that would have regulated LDTs as medical devices, effectively restoring the status quo of FDA enforcement discretion for these tests [30] [31]. This is significant for hospital and health system labs, as stringent device regulations could have limited the availability of these tests [30]. In the European Union, the In Vitro Diagnostic Regulation (IVDR) imposes stringent requirements. Laboratories must justify the use of in-house assays over commercially available CE-IVD-marked kits and maintain detailed documentation of the entire test lifecycle [28]. From an implementation perspective, DNA extraction has been consistently identified as a critical step affecting sensitivity, particularly for parasites with robust cyst walls like Cryptosporidium and Dientamoeba fragilis [27] [7]. Furthermore, while molecular methods are highly sensitive for specific targets, microscopic examination retains value as it can reveal additional parasitic infections not covered by a targeted PCR panel [7].
Standardized Protocols for DNA Extraction from Stool Specimens
The diagnosis of intestinal protozoan parasites is undergoing a transformative shift from traditional microscopic examination to molecular techniques. Microscopy, while cost-effective and widely used, suffers from limitations in sensitivity and specificity and requires significant technical expertise [32] [7]. Molecular methods, particularly polymerase chain reaction (PCR) and related technologies, offer enhanced sensitivity and specificity, and have become increasingly central to diagnostic and research workflows [33] [32]. The reliability of these molecular assays is fundamentally dependent on the first and most critical step: the extraction of high-quality DNA from stool specimens [34] [35]. Stool samples present a unique challenge for molecular biology, as they contain inherent PCR inhibitors such as lipids, bil salts, and complex carbohydrates, while the robust cyst and oocyst walls of parasites like Giardia and Cryptosporidium are difficult to lyse [34] [36]. Failure to adequately address these challenges can lead to false-negative results, undermining the diagnostic process [34]. Therefore, the selection and optimization of a DNA extraction protocol is not merely a preliminary step but a decisive factor in the success of downstream applications. This Application Note details standardized protocols for DNA extraction, framed within the context of a thesis comparing microscopy and molecular methods for the diagnosis of protozoan parasites, to ensure reproducible, reliable, and high-quality results for researchers and scientists.
Comparative Analysis of DNA Extraction Methodologies
Performance Evaluation of Different Extraction Methods
The choice of DNA extraction method significantly impacts the quantity, quality, and ultimate amplifiability of DNA recovered from stool samples. A 2022 study directly compared four methods for extracting DNA from various intestinal parasites, including fragile protozoa like Blastocystis sp. and hardy helminths like Ascaris lumbricoides [34]. The methods evaluated were the conventional phenol-chloroform technique (P), a modified phenol-chloroform technique with a bead-beating step (PB), the QIAamp Fast DNA Stool Mini Kit (Q), and the QIAamp PowerFecal Pro DNA Kit (QB) [34]. While the phenol-chloroform-based methods (P and PB) yielded approximately four times higher DNA quantities, the QIAamp PowerFecal Pro DNA Kit (QB) demonstrated superior performance in the most critical parameter: PCR detection rate [34]. The QB method achieved a 61.2% PCR detection rate, far exceeding the 8.2% rate of the conventional phenol-chloroform method [34]. This underscores that DNA yield alone is a poor indicator of method efficacy; the efficient removal of inhibitors and successful lysis of parasitic forms are paramount.
Table 1: Comparative Performance of DNA Extraction Methods for Protozoan Parasites from Stool Samples
| Extraction Method | Reported DNA Yield | PCR Inhibition Resistance | Key Advantages | Key Limitations | Primary Application/Recommendation |
|---|---|---|---|---|---|
| Phenol-Chloroform (P) | High [34] [36] | Low [34] | High DNA yield; cost-effective [34] [36] | Time-consuming; hazardous organic solvents; poor inhibitor removal [34] | Research settings where cost is primary and inhibitors are less concern |
| Phenol-Chloroform with Bead-Beating (PB) | High [34] | Moderate [34] | Effective lysis of tough cyst/walls [34] | Time-consuming; requires specialized equipment (bead beater) [34] | Samples with hardy parasites (e.g., helminth eggs) |
| QIAamp Fast DNA Stool Mini Kit (Q) | Moderate [34] | Moderate-High [34] | Commercial standardization; good inhibitor removal [34] | May be less effective for certain tough-walled parasites [34] | Routine diagnostic PCR for common protozoa |
| QIAamp PowerFecal Pro DNA Kit (QB) | Moderate [34] | High [34] | Highest PCR detection rate; superior inhibitor removal; effective for wide parasite range [34] | Higher cost per sample than in-house methods [34] | Gold standard for sensitive detection of mixed parasitic infections |
| YTA Stool DNA Kit | Moderate [36] | Moderate [36] | Commercial; cost-effective alternative | 60% diagnostic sensitivity for G. duodenalis [36] | PCR-based detection when budget is a constraint |
Similar comparative studies focusing on specific parasites reinforce these findings. For instance, in the detection of Giardia duodenalis, the phenol-chloroform method showed a higher diagnostic sensitivity (70%) compared to two commercial kits (QIAamp and YTA, both at 60%) when targeting the SSU rRNA gene [36]. Furthermore, the method of extraction can influence the apparent composition of the sample. A 2020 study on Blastocystis sp. found that a manual DNA extraction method (QIAamp DNA Stool Minikit) identified significantly more positive specimens than an automated method (QIAsymphony), particularly in samples with a low parasite load [37].
Impact of Pre-Treatment and Sample Preservation
The DNA extraction process begins long before the application of lysis buffers. Sample preservation and pre-treatment are critical "front-end" factors that dictate the success of the entire molecular workflow.
Sample Preservation: The choice of transport medium directly affects DNA recovery. A 2024 study comparing ethanol and lysis buffer for preserving mammalian fecal samples found that lysis buffer was significantly superior [38]. Samples transported in lysis buffer yielded DNA concentrations and subsequent sequencing reads up to three times higher than those preserved in ethanol. The lysis buffer also provided more consistent DNA purity (A260/280 mean: 1.92, SD: 0.27) compared to ethanol (mean: 1.94, SD: 1.10) [38]. This highlights the importance of matching the preservation medium to the downstream molecular application.
Pre-Treatment (Bead-Beating): The inclusion of a mechanical lysis step, such as bead-beating, is one of the most significant modifications to improve DNA extraction efficiency from stool samples. The tough walls of protozoan cysts and oocysts can be resistant to chemical and enzymatic lysis alone [34] [36]. The bead-beating process uses rapid shaking of the sample with small, sterile glass or ceramic beads to physically disrupt these resilient structures. As evidenced in the 2022 study, adding a bead-beating step to the phenol-chloroform protocol (PB) substantially improved its performance over the standard protocol (P) [34]. For Giardia cyst disruption, protocols often employ multiple cycles of freeze-thawing in liquid nitrogen and a boiling water bath prior to DNA extraction to further facilitate wall breakdown [36].
Table 2: Essential Research Reagent Solutions for DNA Extraction from Stool
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Lysis Buffer (e.g., S.T.A.R. Buffer) | Sample preservation & transport; stabilizes DNA and inhibits nucleases [38] [7] | Superior to ethanol for DNA yield and quality in long-term storage [38] |
| Proteinase K | Enzymatic digestion of proteins; disrupts cellular structures [34] [36] | Critical for breaking down organic material and parasite stages; requires incubation at 55-65°C [34] |
| Silica Membrane Columns | Binding and purification of DNA; removal of PCR inhibitors [34] [37] | Core component of many commercial kits; allows washing and elution of pure DNA |
| Glass Beads (0.5mm) | Mechanical disruption (bead-beating) of tough cyst/oocyst walls [34] | Essential for hardy parasites; improves DNA recovery from a broad range of organisms [34] |
| Phenol:Chloroform:IAA | Organic extraction of DNA; separates DNA from proteins and other contaminants [34] [36] | Effective for high yield; involves hazardous chemicals and is time-consuming [34] |
| Inhibitor Removal Reagents (e.g., BSA) | Added to PCR to bind residual inhibitors and improve amplification [36] | Counteracts inhibitors that may persist even after efficient DNA extraction |
Recommended Standardized Protocols
Protocol 1: Phenol-Chloroform Extraction with Bead-Beating
This in-house protocol is effective for obtaining high DNA yields and lysing tough-walled parasites, though it requires more hands-on time and involves hazardous chemicals [34] [36].
Materials:
- Lysis Solution (20 mM Tris-HCl pH 7.6, 2.5 mM MgCl2, 50 mM KCl, 150 µg/mL proteinase K, 0.5% Tween-20)
- Phenol:Chloroform:Isoamyl Alcohol (25:24:1)
- Chloroform
- Ice-cold absolute ethanol and 70% ethanol
- 3M sodium acetate (pH 5.2)
- TE buffer (elution buffer)
- 0.5 mm sterile glass beads
- Microcentrifuge tubes
- Microcentrifuge
- Bead beater or vortex adapter for horizontal vortexing
Methodology:
- Sample Preparation: Transfer 200 mg of stool specimen into a 2 mL microcentrifuge tube. For specimens preserved in ethanol, wash the sample three times with sterile distilled water before use [34].
- Bead-Beating and Lysis: Add 250 mg of sterile 0.5 mm glass beads and 400 µL of lysis solution to the sample. Securely cap the tube and horizontally vortex at maximum speed for 10 minutes until the stool is homogenized [34].
- Incubation: Incubate the homogenized sample at 65°C for 3 hours, followed by a 10-minute incubation at 90°C to inactivate the proteinase K [34].
- Organic Extraction:
- Add 200 µL of phenol:chloroform:IAA to the lysate. Vortex thoroughly and centrifuge at 13,000 rpm at 4°C for 10 minutes [34].
- Carefully transfer the upper aqueous phase to a new microcentrifuge tube.
- Add 2 volumes of chloroform, mix thoroughly by inversion, and centrifuge again at 13,000 rpm at 4°C for 10 minutes. Transfer the upper aqueous phase to a new tube [34].
- DNA Precipitation:
- Add 2.5 volumes of ice-cold absolute ethanol and 0.1 volume of 3M sodium acetate (pH 5.2) to the aqueous phase. Mix and precipitate DNA at -20°C overnight [34].
- Pellet the DNA by centrifugation at 13,000 rpm at 4°C for 10 minutes.
- DNA Washing and Elution:
- Carefully decant the supernatant and wash the DNA pellet with 1 mL of 70% ethanol. Air-dry the pellet at room temperature.
- Resuspend the purified DNA pellet in 100 µL of TE buffer [34].
Protocol 2: QIAamp PowerFecal Pro DNA Kit (QB)
This commercial kit protocol is recommended for its high detection rate and effectiveness in removing PCR inhibitors, making it ideal for sensitive diagnostic applications [34].
Materials:
- QIAamp PowerFecal Pro DNA Kit (QIAGEN) containing InhibitEX tablets, proteinase K, buffers, and spin columns
- Microcentrifuge tubes
- Microcentrifuge
- Water bath or heating block set to 70°C
- Ethanol (96-100%)
Methodology:
- Sample Lysis:
- Aliquot 200 mg of stool sample into a tube. Add 1 mL of PowerFecal Pro Solution to the sample and vortex continuously for 5-15 minutes to homogenize. This step includes mechanical lysis [34].
- Inhibitor Removal:
- Centrifuge the lysate briefly to pellet coarse particles. Transfer up to 700 µL of the supernatant to a new tube containing an InhibitEX tablet. Vortex immediately and continuously for 1 minute to dissolve the tablet and bind inhibitors.
- Incubate the mixture at room temperature for 5 minutes.
- Centrifuge at full speed for 1 minute to pellet the inhibitor-bound matrix.
- DNA Binding:
- Transfer the supernatant to a new microcentrifuge tube. Add 15 µL of proteinase K.
- Add 650 µL of Buffer FPP and mix by vortexing.
- Incubate at 70°C for 10-15 minutes.
- Column Purification:
- Briefly centrifuge the tube to remove drops from the lid.
- Add 650 µL of the lysate to an MBT Spin Column and centrifuge at full speed for 1 minute. Discard the flow-through and repeat with the remaining lysate.
- Washing and Elution:
- Add 500 µL of Buffer EA to the column. Centrifuge at full speed for 1 minute and discard the flow-through.
- Add 500 µL of Buffer EB to the column. Centrifuge at full speed for 1 minute and discard the flow-through.
- Place the column in a new collection tube and centrifuge at full speed for 1 minute to dry the membrane.
- Transfer the column to a clean elution tube. Apply 50-100 µL of Buffer ET to the center of the membrane, incubate at room temperature for 1-5 minutes, and centrifuge at full speed for 1 minute to elute the DNA [34].
Workflow Integration and Quality Control
The DNA extraction process is an integral component of a larger diagnostic and research workflow. As visualized below, it bridges the gap between sample collection and the final molecular analysis, and its quality directly influences all subsequent results.
Diagram 1: Integrated diagnostic workflow for intestinal protozoa, highlighting the parallel and complementary roles of microscopy and molecular methods.
To ensure the reliability of the extracted DNA, stringent quality control measures must be implemented:
- Spectrophotometry: Use a NanoDrop or similar instrument to assess DNA concentration (A260) and purity. Optimal A260/280 ratios are ~1.8, indicating minimal protein contamination. The A260/230 ratio should be >2.0, indicating removal of organic salts and other contaminants [34] [36].
- Inhibition Testing: A key quality control step is to test for the presence of residual PCR inhibitors. This can be done by spiking a known quantity of control plasmid DNA or a separate control amplicon into the extracted DNA and performing PCR. A delay or failure in the amplification of the spike indicates the presence of inhibitors [34]. Alternatively, some commercial multiplex PCR kits include an internal control within the reaction to monitor for inhibition [33] [37].
- Amplification of a Housekeeping Gene: Performing PCR for a conserved host or bacterial gene (e.g., 16S rRNA) can confirm the successful extraction of amplifiable DNA.
The transition from microscopy to molecular methods for protozoan parasite diagnosis represents a significant advancement in clinical and research parasitology. The efficacy of these powerful molecular tools, however, is fundamentally contingent upon the DNA extraction protocol employed. This Application Note has detailed that while mechanical pre-treatment like bead-beating is crucial for disrupting resilient parasitic forms, the use of specialized commercial kits (e.g., QIAamp PowerFecal Pro) generally provides the best combination of high DNA quality, effective inhibitor removal, and a superior PCR detection rate compared to traditional organic extraction methods [34]. Researchers must be aware that the entire process—from sample preservation and pre-treatment through extraction and amplification—forms an interconnected system where each step must be optimized for the specific sample type and parasitic targets of interest [35]. By adopting these standardized protocols and rigorous quality control measures, scientists can ensure the generation of robust, reliable, and reproducible molecular data, thereby strengthening both diagnostic accuracy and research outcomes in the field of intestinal parasitology.
The diagnosis of intestinal protozoan infections, such as Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, is a critical component of public health and clinical microbiology. The ongoing comparison between traditional microscopy and advanced molecular methods for protozoan diagnosis research hinges on a fundamental, pre-analytical factor: the initial choice between fresh or preserved stool specimens. Proper collection and preservation are paramount, as they directly impact the sensitivity and reliability of all subsequent diagnostic procedures [2]. This application note provides a detailed framework for optimizing stool sample collection, presenting structured data, validated protocols, and practical tools to guide researchers and scientists in making evidence-based decisions that enhance diagnostic accuracy.
Comparative Analysis: Diagnostic Performance in Context
The selection of sample type directly influences the detection capabilities of both microscopy and molecular techniques. The table below summarizes key performance characteristics.
Table 1: Impact of Sample Type on Diagnostic Method Performance
| Diagnostic Method | Recommended Sample Type | Key Advantages | Key Limitations |
|---|---|---|---|
| Microscopy (O&P Exam) | Fresh (for motility); Preserved (10% Formalin & PVA) [39] [40] | Low cost; Allows broad detection of parasites & helminths [2] | Low sensitivity (20-90%); Requires skilled technologist; Cannot differentiate pathogenic species [1] [2] |
| Molecular Methods (PCR/qPCR) | Preserved (SAF, 95% Ethanol) [1] [41] | High sensitivity & specificity; Species-specific differentiation; Automation-friendly [1] [42] | Higher cost; Limited target spectrum; May miss helminths [42] [2] |
Molecular assays have demonstrated superior sensitivity for detecting key protozoa. A large prospective study over three years found that multiplex qPCR detected Giardia intestinalis, Cryptosporidium spp., and Entamoeba histolytica in 1.28%, 0.85%, and 0.25% of samples, respectively, whereas microscopy detected the same organisms in only 0.7%, 0.23%, and 0.68% of samples [42]. Furthermore, a 2025 multicentre study confirmed that PCR results from preserved stool samples were often better than those from fresh samples, likely due to better DNA preservation [1].
Specimen Collection and Preservation Protocols
Universal Collection Guidelines
- Container: Collect stool in a dry, clean, leak-proof container. Care must be taken to avoid contamination with urine, water, or soil [39].
- Timing: Multiple specimens collected every 2-3 days are recommended to account for irregular shedding of parasites. A single stool specimen detects only 58-72% of protozoan infections [2].
- Interfering Substances: Specimens should be collected before the administration of, or after clearance from, substances like barium, bismuth, antacids, mineral oil, antimicrobial agents, and certain antidiarrheal preparations [39].
Processing Workflow: Fresh vs. Preserved Stool
The following workflow outlines the critical decision points and procedures for handling stool samples based on their initial state.
Step-by-Step Experimental Protocols
Protocol 1: Processing Fresh Stools for Microscopy
This protocol is optimal for observing motile trophozoites, which is not possible with preserved specimens [40].
Direct Wet Mount Preparation:
- Place a drop of 0.9% saline on a clean microscope slide.
- Emulsify a very small amount of fresh stool (about 2 mg) in the saline using an applicator stick.
- Add a coverslip. The mount should be thin enough to read newsprint through it.
- Examine systematically under microscope (10x and 40x objectives) for motile trophozoites, cysts, and helminth eggs.
Concentration for Enhanced Detection (Formalin-Ethyl Acetate Sedimentation): [40]
- Step 1: Strain approximately 3-5 ml of emulsified stool through wetted gauze into a 15 ml conical centrifuge tube. Add saline or 10% formalin to bring the volume to 15 ml.
- Step 2: Centrifuge at 500 × g for 10 minutes. Decant the supernatant.
- Step 3: Resuspend the sediment in 10 ml of 10% formalin and mix thoroughly.
- Step 4: Add 4 ml of ethyl acetate, stopper the tube, and shake vigorously for 30 seconds. Centrifuge again at 500 × g for 10 minutes.
- Step 5: Free the debris plug from the tube side and decant the top layers. Examine the resuspended sediment under a microscope.
Protocol 2: Preserving Stools for Molecular Diagnosis
For PCR-based methods, preservation with Sodium Acetate-Acetic Acid-Formalin (SAF) or 95% Ethanol is recommended for optimal DNA recovery [43] [41].
Preservation with SAF: [43]
- Add 1 volume of stool to 3 volumes of SAF preservative in a labeled, leak-proof container.
- Mix thoroughly until the specimen is homogenous. The fixed sample is stable for several months at room temperature.
- DNA Extraction Note: For DNA extraction from SAF-preserved stool, use a mechanical disruption step (e.g., bead beating) to break down robust protozoan walls, which is critical for efficient DNA recovery [1].
Preservation with 95% Ethanol: [41]
- Add 1 volume of stool to 2-3 volumes of 95% ethanol.
- Mix immediately and thoroughly to ensure the ethanol penetrates the entire sample, inactivating nucleases.
- This method provides a pragmatic and effective field-based option for stabilizing DNA, even at simulated tropical ambient temperatures (32°C) for up to 60 days.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Stool Sample Preservation and Processing
| Reagent/Fixative | Primary Function | Key Applications | Considerations |
|---|---|---|---|
| 10% Formalin | All-purpose fixative; preserves morphology of cysts, eggs, and larvae [39] | Concentration procedures; immunoassays; UV fluorescence | Not suitable for permanent stained smears with trichrome; can interfere with PCR after extended fixation [39] |
| Polyvinyl-Alcohol (PVA) | Preserves protozoan trophozoites and cysts; provides adhesive for slides [39] | Preparation of permanent stained smears (e.g., trichrome) | Contains mercuric chloride (disposal concerns); not suitable for concentration or immunoassays [39] [40] |
| SAF (Sodium Acetate-Acetic Acid-Formalin) | Fixative suitable for concentration and permanent staining [39] | Microscopy and molecular diagnostics; compatible with concentration and acid-fast stains | Requires an additive (e.g., albumin) for specimen adhesion to slides [39] |
| 95% Ethanol | Dehydrates and inactivates nucleases, preserving target DNA [41] | Optimal for PCR-based molecular studies | Pragmatic choice for field settings; balances DNA preservation with cost and toxicity [41] |
| RNAlater | Stabilizes nucleic acids by precipitating proteins and inactiating RNases [41] | Preservation of RNA and DNA for molecular studies | Provides some protective effect at elevated temperatures, but may be less effective than other methods for parasite DNA [41] |
| FTA Cards | Chemically treated cards for nucleic acid lysis and immobilization [41] | Room-temperature storage and shipping of samples for PCR | Effective for minimizing DNA degradation at 32°C; suitable for specific sample types [41] |
The optimization of stool sample collection is a critical first step that dictates the success of downstream diagnostic applications. While fresh specimens remain valuable for the immediate observation of motile forms under microscopy, preserved specimens offer unparalleled practicality, stability, and compatibility with both traditional and modern molecular techniques. The evidence strongly indicates that for the specific detection of pathogenic intestinal protozoa within a research framework comparing diagnostic methodologies, the use of appropriately preserved stool specimens—particularly with fixatives like SAF or 95% ethanol for molecular studies—provides the most reliable and robust foundation.
For many years, microscopy has been the cornerstone of diagnosing intestinal protozoan infections, requiring the examination of multiple stool samples collected on alternate days to overcome its limited sensitivity [44]. This approach is labor-intensive, time-consuming, and demands highly skilled personnel [7] [44]. The emergence of molecular diagnostic methods, particularly real-time PCR (RT-PCR), offers a paradigm shift by providing enhanced sensitivity and specificity, enabling accurate identification and differentiation of pathogenic protozoa, such as Entamoeba histolytica, from non-pathogenic species [6] [7].
This application note details the implementation of a single-sample molecular diagnostic workflow. Evidence demonstrates that a protocol utilizing one fecal sample for both a coproparasitological exam and RT-PCR achieves high sensitivity, reducing costs and saving time for patients and laboratories alike [44]. We provide a detailed protocol and resources to facilitate the integration of this efficient approach into routine laboratory practice.
Performance Comparison: Microscopy vs. Molecular Methods
Table 1: Comparative Performance of Diagnostic Methods for Key Intestinal Protozoa
| Pathogen | Microscopy Sensitivity & Specificity Limitations | Molecular Method (RT-PCR/RPA) Performance | Notes on Molecular Diagnosis |
|---|---|---|---|
| Giardia duodenalis | Poor sensitivity; requires skilled microscopist [45] [44] | High sensitivity and specificity; complete agreement between commercial and in-house PCR [6] [7] | Performs well on both fresh and preserved stool samples [7] |
| Cryptosporidium spp. | Low sensitivity (47.2-68.8% for some commercial EIAs); requires acid-fast staining [45] | High specificity; RPA showed 100% correlation with PCR in a clinical study [45] | Sensitivity can be limited by inadequate DNA extraction from oocysts [6] [7] |
| Entamoeba histolytica | Cannot differentiate from non-pathogenic E. dispar and E. moshkovskii [7] [44] | Critical for accurate diagnosis; enables specific identification of pathogenic species [6] [7] | Resolves a major limitation of microscopy [44] |
| Dientamoeba fragilis | Requires permanent staining for visualization; sensitivity variable [7] | High specificity; detection can be inconsistent, potentially due to DNA extraction issues [6] [7] | Molecular methods are more sensitive than microscopy for this pathogen [44] |
Table 2: Impact of Single-Sample Molecular Workflow on Laboratory Efficiency
| Parameter | Traditional Microscopy (3 Samples) | Single-Sample Molecular Approach | Reference |
|---|---|---|---|
| Number of Samples | 3 collected on alternate days | 1 | [44] |
| Workflow Complexity | High (multiple processing steps per sample) | Simplified (single processing workflow) | [44] |
| Personnel Skill Demand | High (requires expert microscopist) | Standardized (reduced reliance on specialized morphology skills) | [7] [44] |
| Differentiation of Entamoeba species | Not possible without additional tests | Direct and specific identification | [7] [44] |
| Reported Sensitivity | Lower (dependent on parasite load and examiner skill) | High sensitivity maintained despite sample reduction | [44] |
Experimental Protocols
Sample Collection and DNA Extraction
This protocol is adapted from a multicentre study comparing molecular methods for detecting intestinal protozoa [7].
Reagents and Equipment:
- Stool sample (fresh or preserved in Para-Pak media)
- S.T.A.R. Buffer (Stool Transport and Recovery Buffer; Roche Applied Sciences)
- Internal Extraction Control
- MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche Applied Sciences)
- MagNA Pure 96 System (Roche Applied Sciences)
- Sterile loops
- Microcentrifuge tubes
- Centrifuge
Procedure:
- Sample Preparation: Using a sterile loop, mix approximately 1 µl of fecal sample with 350 µl of S.T.A.R. Buffer.
- Incubation: Incubate the mixture for 5 minutes at room temperature.
- Clarification: Centrifuge the sample at 2000 rpm for 2 minutes.
- Supernatant Collection: Carefully transfer 250 µl of the supernatant to a fresh tube. Add 50 µl of the internal extraction control to the supernatant.
- Automated Extraction: Load the prepared sample into the MagNA Pure 96 System and execute the DNA extraction protocol using the MagNA Pure 96 DNA and Viral NA Small Volume Kit, following the manufacturer's instructions. The DNA is eluted in a final volume of 100 µl.
In-House Real-Time PCR (RT-PCR) Amplification
This protocol describes a multiplex RT-PCR for the simultaneous detection of Giardia duodenalis, Dientamoeba fragilis, and Blastocystis sp. [44]. A second multiplex can be performed for Entamoeba histolytica/E. dispar and Cryptosporidium sp. [44].
Reagents and Equipment:
- Extracted DNA template
- 2× TaqMan Fast Universal PCR Master Mix (Thermo Fisher Scientific)
- Primers and probes specific for target protozoa (see Table 3 for sequences and concentrations)
- Sterile, nuclease-free water
- ABI 7900HT Fast Real-Time PCR System (Applied Biosystems, Thermo Fisher Scientific) or equivalent real-time cycler
Procedure:
- Reaction Mix Preparation: For each reaction, combine the following components in a PCR tube or plate:
- 5 µl of extracted DNA
- 12.5 µl of 2× TaqMan Fast Universal PCR Master Mix
- 2.5 µl of primer and probe mix (for multiplex, see Table 3 for final concentrations)
- Sterile water to a final volume of 25 µl
- Thermal Cycling: Place the plate in the real-time PCR instrument and run the following program:
- Initial Denaturation: 1 cycle of 95°C for 10 minutes.
- Amplification: 45 cycles of:
- 95°C for 15 seconds (denaturation)
- 60°C for 1 minute (annealing/extension)
- Data Analysis: Analyze the amplification curves and determine cycle threshold (Ct) values. Include positive and negative controls in each run to ensure assay validity.
Table 3: Primer and Probe Sequences for Multiplex RT-PCR [44]
| Target | Primer/Probe | Sequence (5' to 3') | Final Concentration in Reaction |
|---|---|---|---|
| Giardia duodenalis | Forward Primer | AAC GGC GCA GGC GGA AAA | 300 nM each |
| Reverse Primer | GTT CGA GTT CGA TTC CGG AGT T | ||
| Probe | (CY5.5) CCC GCG GCG GTC CCT GCT AG (BHQ3) | 200 nM | |
| Dientamoeba fragilis | Forward Primer | CGG CCG AAG CGC TAT T | 100 nM each |
| Reverse Primer | CCT TCC TCA AAG TGT TTT ACG AA | ||
| Probe | (VIC) CGG AAT TCT TGG CCT TC (MGB) | 100 nM | |
| Blastocystis sp. | Forward Primer | GGA GGT AGT GAC AAT AAAT C | 300 nM each |
| Reverse Primer | TGC TAT TCA CCA AAT TAA GC | ||
| Probe | (FAM) CAT CTA GTT CAA TTA AGC ACA (MGB) | 100 nM |
Workflow Integration Diagram
The following diagram contrasts the traditional multi-sample microscopy workflow with the streamlined single-sample molecular approach, highlighting the significant reduction in steps and simplification.
Single-Sample Molecular vs. Traditional Microscopy Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagent Solutions for Molecular Diagnosis of Protozoa
| Item | Function/Application | Example Product/Note |
|---|---|---|
| Nucleic Acid Extraction Kit | Automated purification of DNA from complex stool samples; includes lysis buffers and magnetic beads. | MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche) [7] |
| Universal PCR Master Mix | Provides enzymes, dNTPs, and optimized buffer for efficient real-time PCR amplification. | TaqMan Fast Universal PCR Master Mix (Thermo Fisher Scientific) [7] |
| Specific Primers & Probes | Target unique genomic sequences of protozoa for specific identification in multiplex assays. | See Table 3 for sequences and labels [44] |
| Internal Extraction Control | Monitors efficiency of DNA extraction and detects presence of PCR inhibitors in the sample. | Phocine Herpes Virus (PhHV-1) or other non-human targets [44] |
| Stool Transport Buffer | Preserves nucleic acids in stool samples during transport and storage, stabilizing DNA for testing. | S.T.A.R. Buffer (Roche) or Para-Pak preservation media [7] |
| Automated Extraction System | Platform for hands-free, standardized nucleic acid purification, ensuring reproducibility. | MagNA Pure 96 System (Roche) [7] |
| Real-Time PCR Cycler | Instrument for DNA amplification and fluorescent signal detection for real-time quantification. | ABI 7900HT Fast Real-Time PCR System (Applied Biosystems) [7] |
Overcoming Diagnostic Hurdles: Sensitivity Gaps, Differentiation Challenges, and Technical Pitfalls
Intestinal protozoan infections represent a significant global health burden, and their accurate diagnosis remains a formidable challenge in clinical microbiology [1]. While microscopic examination of stool samples has long been the reference standard, its limitations are particularly pronounced for specific parasites such as Dientamoeba fragilis and Cryptosporidium spp [1] [32]. Molecular diagnostic technologies, particularly real-time PCR (RT-PCR), are gaining traction in non-endemic areas characterized by low parasitic prevalence owing to their enhanced sensitivity and specificity [1]. This application note delves into the variable sensitivity of diagnostic methods for these protozoa, presenting quantitative comparative data and detailed protocols to guide researchers and scientists in optimizing detection strategies.
Comparative Performance of Diagnostic Methods
The following table summarizes key comparative data from recent studies, highlighting the stark differences in detection capability between microscopic and molecular methods.
Table 1: Comparative detection rates of microscopy versus molecular methods for intestinal protozoa
| Parasite | Study Reference | Microscopy Detection Rate (No. of samples) | Molecular Method Detection Rate (No. of samples) | Notes |
|---|---|---|---|---|
| Dientamoeba fragilis | Fernández et al. (2023) [32] | 0% (0/274) | 5.5% (15/274) | D. fragilis was not visualized in any case by microscopy. |
| Cryptosporidium spp. | Iranian Pediatric Study (2024) [15] | 23.2% (32/138) | 26.8% (37/138) | PCR demonstrated superior sensitivity. |
| Giardia duodenalis | Cuban Study [46] | 12.8% (17/133) | 15.8% (21/133) | Concordance between methods was almost perfect (κ = 0.88). |
| Mixed Protozoa | Fernández et al. (2023) [32] | 9.5% (26/274) | 27.0% (74/274) | Molecular methods identified significantly more positives. |
Analysis of Methodological Performance
The data consistently demonstrates the higher sensitivity of molecular methods. For D. fragilis, microscopy shows a profound diagnostic weakness, failing to identify infections that are readily detected by PCR [32] [46]. This is largely because D. fragilis is a fragile trophozoite that rapidly disintegrates in stool samples, making morphological identification difficult [1] [46].
For Cryptosporidium spp., while microscopy using specific staining techniques (e.g., Ziehl-Neelsen) is more reliable, PCR still identifies a higher number of infections [15]. The sensitivity of molecular assays for Cryptosporidium can be influenced by the DNA extraction efficiency from the parasite's robust oocysts [1]. Furthermore, molecular methods provide the crucial advantage of species and subtype differentiation, which is essential for understanding transmission dynamics and pathogenesis [47] [15].
Table 2: Summary of advantages and limitations of diagnostic methods for D. fragilis and Cryptosporidium spp.
| Method | Key Advantages | Key Limitations |
|---|---|---|
| Microscopy | Low cost; can detect a wide range of parasites; useful in high-prevalence, low-resource settings [1]. | Low sensitivity and specificity; inability to differentiate related species (e.g., E. histolytica/dispar); requires experienced personnel [1] [44]. |
| Immunoassays (ELISA/ICT) | Rapid; suitable for screening [1] [48]. | Variable sensitivity and specificity; cannot differentiate species; reports of false positives/negatives [1] [48]. |
| Molecular Methods (PCR) | High sensitivity and specificity; species and subtype differentiation; essential for detecting D. fragilis [1] [47] [32]. | Higher cost; requires specialized equipment; DNA extraction efficiency can impact results [1]. |
Experimental Protocols for Molecular Detection
Standardized DNA Extraction Protocol
Efficient DNA extraction is critical, especially for Cryptosporidium oocysts, which have a robust wall structure [1].
Materials:
- Stool sample (fresh or preserved in Para-Pak media)
- S.T.A.R. Buffer (Stool Transport and Recovery Buffer; Roche)
- MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche)
- Internal extraction control (e.g., Phocine Herpes Virus type-1, PhHV-1)
- Sterile loops and microcentrifuge tubes
Procedure:
- Sample Preparation: Homogenize 1 µL of fecal sample with 350 µL of S.T.A.R. Buffer using a sterile loop. Incubate for 5 minutes at room temperature [1].
- Clarification: Centrifuge the mixture at 2000 rpm for 2 minutes [1].
- Supernatant Collection: Carefully transfer 250 µL of the supernatant to a fresh tube. Add 50 µL of the internal extraction control to monitor for inhibition and extraction efficiency [1] [44].
- Automated Extraction: Perform DNA extraction using the MagNA Pure 96 System according to the manufacturer's instructions (Roche). Elute the DNA in a final volume of 100 µL [1] [44].
- Storage: Store purified DNA at -20°C until PCR amplification [47].
Real-Time PCR Amplification Protocol
This protocol is adapted from multicentre evaluations for the detection of G. duodenalis, Cryptosporidium spp., E. histolytica, and D. fragilis [1] [44].
Reaction Setup:
- DNA Template: 5 µL of extracted DNA
- Master Mix: 12.5 µL of 2× TaqMan Fast Universal PCR Master Mix (Thermo Fisher Scientific)
- Primers and Probes: 2.5 µL of a custom primer-probe mix. The following concentrations are suggested for a multiplex targeting Cryptosporidium and D. fragilis [44]:
- Cryptosporidium spp.: 200 nM of each primer, 100 nM of probe (e.g., labeled with CY5.5-BHQ3)
- Dientamoeba fragilis: 100 nM of each primer, 100 nM of probe (e.g., labeled with VIC-MGB)
- Internal Control: Include primers (80 nM) and a probe (200 nM) for the internal control (e.g., PhHV-1) [44].
- Nuclease-free Water: To a final reaction volume of 25 µL.
Amplification Conditions:
- Initial Denaturation: 95°C for 3 minutes
- 40 Cycles of:
Data Analysis:
- A positive result is determined by a cycle threshold (Ct) value below a predetermined cut-off (e.g., 39.9) [44].
- The internal control should amplify correctly to rule out PCR inhibition.
- For species differentiation of Cryptosporidium, positive samples can be further analyzed by nested PCR and sequencing of the gp60 gene [47].
Optimized Diagnostic Workflow
The following diagram illustrates a recommended diagnostic algorithm that integrates molecular methods to address the sensitivity gaps for D. fragilis and Cryptosporidium spp., based on recent study conclusions [1] [44].
The Scientist's Toolkit: Research Reagent Solutions
The table below details key reagents and kits used in the featured experiments, providing a resource for protocol implementation.
Table 3: Essential research reagents and materials for molecular detection of intestinal protozoa
| Reagent / Kit | Manufacturer / Source | Function in Protocol |
|---|---|---|
| S.T.A.R. Buffer | Roche Applied Sciences | Stool transport and recovery; aids in sample homogenization and stabilization prior to DNA extraction [1]. |
| MagNA Pure 96 DNA and Viral NA Small Volume Kit | Roche Applied Sciences | Automated, high-throughput nucleic acid purification based on magnetic bead technology [1]. |
| TaqMan Fast Universal PCR Master Mix (2X) | Thermo Fisher Scientific | Ready-to-use reaction mix containing DNA polymerase, dNTPs, and optimized buffer for fast, sensitive real-time PCR [1]. |
| RIDAQUICK Cryptosporidium | R-Biopharm AG | Immunochromatographic rapid test for Cryptosporidium antigen detection; used for comparative studies [47] [48]. |
| FastDNA SPIN Kit for Feces | MP Biomedicals | Manual DNA extraction kit optimized for difficult stool samples, using mechanical lysis via homogenizer and glass beads [47]. |
| Seegene Allplex Parasite Assay | Seegene | Commercial multiplex PCR panel for detection of a broad range of intestinal parasites from a single sample [32]. |
The evidence firmly establishes that molecular methods are indispensable for the accurate diagnosis of Dientamoeba fragilis and Cryptosporidium spp., effectively addressing the variable sensitivity of traditional microscopy [32] [46]. While microscopy remains a valuable tool for broad parasitological surveys, the integration of PCR into diagnostic workflows significantly improves detection rates, enables species differentiation, and enhances patient care [1] [44]. For researchers and drug development professionals, the standardized protocols and reagents outlined here provide a foundation for reliable detection and characterization of these clinically important protozoa. Future efforts should focus on standardizing DNA extraction procedures and making molecular tests more accessible and cost-effective for wider adoption [1].
The Entamoeba histolytica species complex comprises morphologically identical protozoan parasites with vastly different clinical implications. Entamoeba histolytica represents a significant global health threat as the causative agent of amebiasis, while Entamoeba dispar and Entamoeba moshkovskii are generally considered non-pathogenic [49]. The World Health Organization estimates that amebiasis causes over 100,000 deaths annually, ranking as the second leading cause of parasite-related mortality worldwide [50] [51]. Accurate differentiation between these species is therefore critically important for appropriate treatment decisions, public health interventions, and avoidance of unnecessary chemotherapy [52] [50].
Traditional microscopic examination, while widely used in resource-limited settings, cannot reliably distinguish these species, leading to significant diagnostic challenges [51] [49]. This diagnostic limitation has profound implications for both patient care and epidemiological understanding, as approximately 90% of Entamoeba infections are asymptomatic, with E. dispar infections being significantly more prevalent than E. histolytica in many populations [52] [51]. This application note provides a comprehensive comparison of current diagnostic methodologies and detailed protocols for accurate species differentiation within the Entamoeba complex, contextualized within the broader framework of microscopy versus molecular methods for protozoan diagnosis.
Comparative Analysis of Diagnostic Methods
Performance Characteristics of Diagnostic Platforms
Table 1: Performance comparison of diagnostic methods for Entamoeba histolytica detection
| Method | Principle | Time to Result | Sensitivity | Specificity | Species Differentiation | Key Limitations |
|---|---|---|---|---|---|---|
| Microscopy | Morphological identification of cysts/trophozoites | 30-60 minutes | Low [51] | Low [51] | No [51] [49] | Cannot differentiate species; requires expertise |
| Trichrome Staining | Enhanced morphological detail | 60-120 minutes | 53.85% [50] | 100% [50] | Limited (based on erythrophagocytosis) | Insufficient for reliable differentiation |
| Antigen Detection (ELISA) | Detection of E. histolytica-specific adhesins (Gal/GalNAc lectin) | 2-4 hours | 80-94% [20] | High [20] | Yes (with specific tests) | Requires fresh/unpreserved samples [20] |
| Serology (IHA) | Detection of anti-amebic antibodies | 4-6 hours | 96.77% [50] | 78.57% [50] | Indirect evidence only | Cannot distinguish current from past infection [51] |
| PCR | Amplification of species-specific rRNA gene sequences | 6-8 hours | 87-100% [52] [53] | 96-100% [52] [53] | Yes | Requires specialized equipment and technical expertise |
Clinical Application and Limitations
Microscopic examination remains the most accessible diagnostic tool in resource-limited settings but demonstrates significant limitations for species-specific identification. While the observation of trophozoites with ingested erythrocytes (erythrophagocytosis) is classically associated with E. histolytica, this finding is rarely observed on stained smears and may occasionally occur with E. dispar, making it an unreliable differential criterion [49]. One study demonstrated that when 90 samples initially identified as E. histolytica/E. dispar by microscopy were subjected to antigen testing, 62.2-75.6% were negative for E. histolytica, highlighting the substantial false-positive rate associated with microscopic diagnosis [50].
Immunoassay platforms provide significant advantages in species differentiation. Antigen detection tests, particularly those targeting the E. histolytica-specific Gal/GalNAc lectin, offer rapid results with good sensitivity and specificity [20]. However, their performance can vary considerably between commercial platforms, and not all available tests differentiate E. histolytica from E. dispar [20]. Serological methods detect host antibodies against the parasite and are particularly valuable for diagnosing extraintestinal amebiasis, but they cannot distinguish between current and past infections [51].
Molecular methods, particularly PCR-based assays, represent the current gold standard for sensitive and specific differentiation of Entamoeba species. These methods typically target multi-copy genes such as the small-subunit (SSU) rRNA gene to maximize sensitivity [52]. A comparative study demonstrated that PCR identified 68 Entamoeba-positive specimens with clear species differentiation: 2 with E. histolytica and 66 with E. dispar, highlighting both the technique's discriminatory power and the relative prevalence of non-pathogenic infections in the study population [52].
Experimental Protocols
PCR-Based Differentiation of Entamoeba Species
Table 2: Essential research reagents for molecular differentiation of Entamoeba species
| Reagent Category | Specific Product | Application/Function |
|---|---|---|
| DNA Extraction | QIAamp DNA Mini Kit (Qiagen) | Nucleic acid purification from stool specimens [52] |
| PCR Master Mix | HotStar Taq DNA Polymerase (Qiagen) | High-fidelity DNA amplification [52] |
| Species-Specific Primers | EH1 (5'-GTACAAAATGGCCAATTCATTCAATG-3') | E. histolytica-specific forward primer [52] |
| ED1 (5'-TACAAAGTGGCCAATTTATGTAAGTA-3') | E. dispar-specific forward primer [52] | |
| EHD2 (5'-ACTACCAACTGATTGATAGATCAG-3') | Universal reverse primer for both species [52] | |
| Positive Controls | SSU rDNA plasmids (E. histolytica/E. dispar) | Reaction validation and specificity confirmation [52] |
| Internal Control | pBR322-derived amplification control | Inhibition detection in fecal DNA extracts [52] |
Sample Preparation and DNA Extraction
Sample Collection: Collect approximately 10 mg of fresh or frozen stool specimen. Avoid formalin-fixed samples as formalin concentrations higher than 1% can inhibit PCR amplification, particularly with fixation times exceeding 4 days [52].
DNA Extraction: Use the QIAamp DNA Mini Kit according to manufacturer specifications:
- Add stool sample to ATL buffer for initial lysis
- Incubate at 56°C for 1 hour with occasional vortexing
- Add AL buffer and ethanol sequentially
- Bind DNA to QIAamp membrane, wash with AW1 and AW2 buffers
- Elute DNA in AE buffer [52]
Quality Assessment: Include an internal amplification control (IC) prepared by amplifying a 190-bp fragment of pBR322 with specific primers (EHDICF and EHDICR) to detect potential PCR inhibitors in fecal DNA extracts [52].
PCR Amplification and Analysis
Reaction Setup: Prepare 50 μL reactions containing:
- 5 μL extracted DNA template
- 50 μM each deoxynucleoside triphosphate
- 2 mM MgCl₂
- 20 pmol each of species-specific primers (EH1 for E. histolytica or ED1 for E. dispar, with EHD2 as the common reverse primer)
- 1× HotStar Taq buffer
- 5 U HotStar Taq DNA polymerase [52]
Thermal Cycling Conditions:
- Initial activation: 15 min at 94°C
- 40 cycles of:
- Denaturation: 30 sec at 94°C
- Annealing: 60 sec at 51°C
- Extension: 40 sec at 72°C
- Final extension: 5 min at 72°C [52]
Amplicon Detection: Separate PCR products on a 3% agarose gel stained with ethidium bromide. E. histolytica and E. dispar produce a 135-bp amplicon visible under UV illumination [52].
Diagram 1: Molecular Workflow for Entamoeba Differentiation
Antigen Detection Protocol
TechLab E. histolytica II Test Procedure
Sample Preparation:
Assay Procedure:
- Add 100 μL of diluted sample to monoclonal antibody-coated wells
- Incubate for 60 minutes at room temperature
- Wash 5 times with wash buffer
- Add enzyme-conjugated detector antibody
- Incubate for 30 minutes at room temperature
- Wash 5 times to remove unbound conjugate
- Add substrate solution and incubate for 20 minutes
- Stop reaction and read absorbance at 450 nm [52] [50]
Interpretation:
- Samples exceeding the cutoff value are positive for E. histolytica
- Negative samples in patients with confirmed Entamoeba infection suggest E. dispar infection [52]
Discussion
Diagnostic Implications in Clinical Practice
The accurate differentiation of Entamoeba species has direct implications for patient management. Treatment is specifically indicated for E. histolytica infection, while E. dispar infection typically does not require chemotherapy [52] [50]. This distinction is particularly crucial in non-endemic areas where the prevalence of E. histolytica is low, and most infections detected by microscopy represent non-pathogenic species [52]. Studies have confirmed that E. dispar infection is significantly more common among travelers returning from endemic regions, further emphasizing the importance of species-specific diagnosis in guiding appropriate therapeutic interventions [52].
The limitations of microscopy extend beyond species differentiation to basic detection sensitivity. One multicenter study comparing various diagnostic methods found that molecular assays were critical for the accurate diagnosis of E. histolytica, with PCR techniques demonstrating superior performance for reliable parasite identification [1]. This enhanced detection capability has important epidemiological implications, as previous prevalence studies likely overestimated the true burden of E. histolytica infection due to diagnostic limitations [51].
Method Selection Framework
Diagram 2: Diagnostic Decision Pathway for Entamoeba Complex
The selection of appropriate diagnostic methods must consider clinical context, available resources, and performance requirements. In acute care settings with limited laboratory capabilities, antigen detection tests offer a reasonable balance between performance and technical demands [20]. For epidemiological studies or reference laboratory applications, PCR-based methods provide the highest sensitivity and specificity while enabling molecular characterization of isolates [52] [54].
Sample handling considerations significantly impact test performance. Molecular and antigen-based assays achieve optimal sensitivity with fresh or frozen unfixed stool samples, while formalin fixation can inhibit PCR amplification in a time-dependent manner [52]. When feasible, parallel testing using multiple methodologies provides the most comprehensive diagnostic approach, though this may be impractical in routine clinical practice.
The differentiation of pathogenic E. histolytica from non-pathogenic Entamoeba species requires species-specific diagnostic methods beyond conventional microscopy. While antigen detection tests provide a practical solution for many clinical laboratories, PCR-based methods represent the most sensitive and specific approach for definitive species identification. The integration of these advanced diagnostic tools into clinical practice and research protocols is essential for appropriate patient management, accurate epidemiological surveillance, and improved understanding of Entamoeba biology and pathogenesis. As molecular technologies continue to evolve and become more accessible, they offer promising avenues for enhanced diagnostic capabilities in both endemic and non-endemic settings.
The diagnosis of protozoan infections stands at a crossroads, balancing classic microscopic techniques against advanced molecular methods. For decades, microscopy has been the cornerstone of parasitological diagnosis, but its limitations in sensitivity and specificity are increasingly apparent [55]. The robust cyst wall of protozoan parasites represents a fundamental barrier to effective molecular diagnosis, protecting the organism in harsh environments but simultaneously impeding access to genetic material essential for PCR-based identification [56].
The critical importance of overcoming this physical barrier cannot be overstated. Inefficient lysis of these resilient structures directly translates to failed DNA extraction, resulting in false-negative diagnoses that compromise patient care and epidemiological accuracy [7]. This challenge is particularly acute for organisms like Cryptosporidium spp., Giardia duodenalis, and Entamoeba histolytica, whose cyst walls are exceptionally resistant to conventional disruption methods [56]. This application note details the technical hurdles posed by robust cyst walls and presents optimized, practical protocols to maximize DNA yield and quality for reliable molecular diagnosis.
The Diagnostic Shift: Microscopy vs. Molecular Methods
Traditional microscopy, while cost-effective and widely available, suffers from significant limitations. It is time-consuming, requires expert microscopists, and struggles to differentiate between morphologically identical species, such as pathogenic Entamoeba histolytica and non-pathogenic Entamoeba dispar [55] [44]. Most critically, its sensitivity is fundamentally constrained by intermittent parasite shedding and low parasite loads in samples [32].
Molecular methods, particularly real-time PCR (Rt-PCR), have demonstrated superior sensitivity and specificity. A 2023 study found molecular diagnosis detected parasites in 27% of samples compared to just 9.5% by microscopy [32]. The table below summarizes key comparative studies.
Table 1: Comparative Performance of Microscopy vs. Molecular Methods for Protozoan Diagnosis
| Study Reference | Microscopy Sensitivity | Molecular Method Sensitivity | Key Findings |
|---|---|---|---|
| Sante Fernández et al., 2023 [32] | 9.5% (26/274 samples) | 27% (74/274 samples) | Molecular methods detected significantly more Blastocystis hominis, Dientamoeba fragilis, and Giardia lamblia infections. |
| Formenti et al., 2017 [55] [44] | Lower than combined methods | Higher than microscopy alone | A combination of one microscopic exam plus Rt-PCR on a single sample showed high sensitivity, replacing the need for three separate microscopic exams. |
| Multicentre Study, 2025 [7] | Variable; reference standard | High for G. duodenalis | Molecular assays are critical for accurate diagnosis of E. histolytica and perform well for G. duodenalis and Cryptosporidium in fixed specimens. |
The Central Challenge: The Robust Cyst Wall
The primary obstacle to effective molecular diagnosis of intestinal protozoa is the resilient cyst wall, a complex structure designed to protect the organism from chemical and physical stress in the external environment [56]. This wall acts as a formidable barrier to conventional DNA extraction protocols, leading to several critical technical challenges:
- Incomplete Lysis: Standard lysis buffers and conditions often fail to disrupt the cyst wall effectively, resulting in low DNA yield [56].
- PCR Inhibition: Fecal samples contain complex mixtures of bilirubin, bile salts, complex carbohydrates, and other substances that can co-extract with DNA and inhibit downstream enzymatic reactions like PCR [56].
- Variable Cyst Wall Composition: The structure and composition of cyst walls vary between protozoan species, meaning a one-size-fits-all extraction approach is often suboptimal [7].
These challenges are quantified by performance data. For instance, one study initially reported a sensitivity of only 60% (9/15 samples) for detecting Cryptosporidium when using a commercial DNA extraction kit with its standard protocol, directly attributable to inefficient oocyst wall breakdown [56].
Optimized DNA Extraction Protocol
Based on extensive evaluation and optimization experiments, the following protocol is recommended for efficient DNA extraction from protozoan cysts in stool specimens. The core of this protocol involves critical amendments to standard commercial kit procedures to maximize cyst wall disruption and DNA recovery.
Research Reagent Solutions
The following reagents are essential for successfully overcoming the cyst wall challenge.
Table 2: Essential Reagents for DNA Extraction from Protozoan Cysts
| Reagent / Kit | Function | Application Note |
|---|---|---|
| QIAamp DNA Stool Mini Kit (Qiagen) | DNA isolation from feces | Effective but requires protocol optimization for protozoan cysts [56]. |
| S.T.A.R. Buffer (Roche) | Stool transport and recovery | Aids in homogenization and stabilization of stool samples prior to DNA extraction [7]. |
| InhibitEX Tablets (included in Qiagen kit) | Adsorption of PCR inhibitors | Removes fecal impurities; extended incubation time improves efficacy [56]. |
| Polyvinylpolypyrrolidone (PvPP) | Binding of polyphenolic compounds | Reduces PCR inhibitors in stool samples; used in lysis buffer [55] [44]. |
| Proteinase K | Enzyme digestion | Degrades proteins and aids in cell lysis. |
| Lysis Buffer ASL (included in Qiagen kit) | Initial cell lysis | Must be used at an elevated temperature for effective cyst wall disruption [56]. |
Step-by-Step Workflow with Critical Modifications
Sample Preparation:
- Preservation: Collect approximately 200 mg of stool in a preservative compatible with molecular diagnostics, such as TotalFix, Unifix, or modified Zn- or Cu-based PVA. Avoid formalin and SAF as they degrade DNA and inhibit PCR [57].
- Homogenization: Mix the preserved stool sample with S.T.A.R. Buffer or a PBS solution containing 2% Polyvinylpolypyrrolidone (PvPP) to homogenize and begin inhibitor removal [55] [44].
Optimized DNA Extraction: The workflow below outlines the optimized steps for maximum DNA yield, with key amendments specifically targeting the robust cyst wall.
Figure 1: Optimized DNA extraction workflow for protozoan cysts, highlighting critical amendments to standard protocols.
Critical Amendments to Standard Protocols:
- Enhanced Lysis: The most crucial modification is the elevated lysis temperature. Instead of the standard incubation, samples should be heated to the boiling point (100°C) for 10 minutes to physically disrupt the tough cyst wall [56].
- Inhibitor Removal: Extend the incubation time with the InhibitEX tablet to 5 minutes to more effectively adsorb and remove PCR inhibitors common in feces [56].
- DNA Precipitation and Elution: For steps involving alcohol precipitation, using pre-cooled ethanol improves nucleic acid recovery. Finally, elute the purified DNA in a small volume (50-100 µl) to increase the final DNA concentration [56].
Downstream Molecular Analysis
- Real-Time PCR (Rt-PCR): Use multiplex Rt-PCR assays for highly sensitive and specific identification of common protozoa. A typical reaction mix includes:
- 5 µl of extracted DNA
- 12.5 µl of 2× TaqMan Fast Universal PCR Master Mix
- Custom primer/probe mix for targets like Giardia, Cryptosporidium, E. histolytica, and D. fragilis
- Sterile water to a final volume of 25 µl [7]
- Cycling Conditions: Amplify with an initial hold at 95°C for 10 minutes, followed by 45 cycles of 95°C for 15 seconds and 60°C for 1 minute [7].
Performance Data and Validation
The impact of the optimized protocol is substantial. For Cryptosporidium detection, amending the standard QIAamp Stool Mini Kit protocol raised the sensitivity from 60% to 100% in controlled tests [56]. Furthermore, seeding experiments demonstrated that the optimized method could theoretically detect as few as 2 oocysts/cysts in a sample, highlighting its extreme sensitivity [56].
Multicenter studies confirm that molecular methods, enabled by effective DNA extraction, are indispensable for specific pathogens. They are particularly critical for the accurate diagnosis of Entamoeba histolytica, which is morphologically identical to non-pathogenic species [7]. The overall sensitivity of a diagnostic approach using a single stool sample for both Rt-PCR and microscopy was found to be very high, offering a more practical and efficient routine compared to the traditional method of examining three separate samples by microscopy [55] [44].
Overcoming the robust cyst wall is the pivotal factor in unlocking the full potential of molecular diagnostics for protozoan parasites. The optimized DNA extraction protocol detailed herein, centering on enhanced mechanical lysis through boiling and improved inhibitor removal, directly addresses this challenge. By implementing these amendments, laboratories can achieve significantly higher DNA quality and yield, leading to more sensitive, specific, and reliable detection of intestinal protozoa. This advancement supports the ongoing paradigm shift in clinical parasitology from traditional microscopy to molecular methods, ultimately improving patient diagnostics and public health outcomes.
The diagnostic landscape for intestinal protozoan infections is undergoing a significant transformation, moving from traditional microscopic techniques toward sophisticated molecular methods. This shift presents new opportunities and challenges for researchers and clinicians, particularly in the interpretation of complex results such as co-infections and quantitative parameters like Cycle Threshold (Ct) values. Within the broader context of comparing microscopy versus molecular diagnostics for protozoan diseases, understanding these elements is crucial for accurate pathogen detection, clinical correlation, and drug development efforts. This application note provides a structured framework for navigating these complex diagnostic results, supported by experimental data and standardized protocols.
Molecular techniques, particularly real-time PCR (rt-PCR), offer enhanced sensitivity and specificity for detecting intestinal protozoa including Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica [20]. Unlike microscopy, which struggles to differentiate morphologically similar species, molecular assays can precisely identify pathogens and reveal complex co-infation profiles that were previously underestimated [1] [44]. The Cycle Threshold (Ct), representing the amplification cycle at which target DNA becomes detectable, provides a semi-quantitative measure of parasite load that correlates with traditional measures of microbial burden [58]. However, interpreting these values requires careful consideration of methodological and biological variables.
Comparative Performance of Diagnostic Methods
Detection Rates of Microscopy Versus Multiplex PCR
Extensive evaluations demonstrate the superior detection capabilities of molecular methods for most intestinal protozoa, though microscopy retains value for detecting pathogens not included in molecular panels and for providing morphological context.
Table 1: Comparative Detection Rates of Intestinal Protozoa by Microscopy and Multiplex PCR
| Parasite | Detection by Microscopy (%) | Detection by Multiplex PCR (%) | Study Characteristics |
|---|---|---|---|
| Giardia intestinalis | 0.7% (25/3495) | 1.28% (45/3495) | 3,495 stools, Seegene AllPlex GIP [33] |
| Cryptosporidium spp. | 0.23% (8/3495) | 0.85% (30/3495) | 3,495 stools, Seegene AllPlex GIP [33] |
| Entamoeba histolytica | 0.68% (24/3495)* | 0.25% (9/3495) | 3,495 stools, Seegene AllPlex GIP [33] |
| Dientamoeba fragilis | 0.63% (22/3495) | 8.86% (310/3495) | 3,495 stools, Seegene AllPlex GIP [33] |
| Blastocystis spp. | 6.55% (229/3495) | 19.25% (673/3495) | 3,495 stools, Seegene AllPlex GIP [33] |
Microscopy cannot differentiate *E. histolytica from non-pathogenic E. dispar and E. moshkovskii, reporting them as E. histolytica/dispar [33] [20].
Molecular methods significantly increase detection rates for parasites like Dientamoeba fragilis and Blastocystis spp., which are often missed by conventional microscopy due to their fragile nature or staining characteristics [33]. However, microscopy remains essential for detecting parasites not targeted by multiplex PCR panels, such as Cystoisospora belli and helminths, highlighting the complementary value of both techniques in comprehensive parasitological assessment [33].
Correlation Between Ct Values and Conventional Diagnostic Measures
Ct values from molecular assays provide a semi-quantitative estimate of parasite burden that correlates with established diagnostic measures, though these relationships vary across pathogen and host factors.
Table 2: Correlation of Ct Values with Smear Microscopy and Culture in Tuberculosis Assessment
| Correlation Measure | Correlation Coefficient | Study Details | Clinical Implications |
|---|---|---|---|
| Xpert Ct vs. Smear Grade | 0.55 (moderately strong) | 387 TB patients in Uganda [58] | Ct can replace smear for bacterial burden |
| Xpert Ct vs. MGIT-TTP | 0.37 (weak) | 187 TB patients in Uganda [58] | Ct cannot replace culture |
| Xpert Ct vs. LJ Culture | 0.34 (weak) | 387 TB patients in Uganda [58] | Ct cannot replace culture |
| Smear Positivity Cut-off | Ct ≤ 23.62 | ROC analysis [58] | Predicts infectiousness |
The relationship between Ct values and disease severity is complex and context-dependent. For instance, a study of COVID-19 found no clear correlation between Ct values and clinical severity, highlighting that viral load represents only one component of disease pathogenesis [59]. Similarly, in intestinal protozoa, factors such as host immune status, pathogen strain virulence, and co-morbidities significantly influence clinical outcomes independent of parasite load [20].
Experimental Protocols for Method Comparison
Standardized DNA Extraction and Multiplex PCR Protocol
Consistent nucleic acid extraction is fundamental for reliable Ct values and accurate detection of co-infections. The following protocol is adapted from contemporary studies comparing molecular and microscopic methods [1] [33].
Protocol: DNA Extraction and Multiplex PCR for Intestinal Protozoa
Sample Preparation:
- Sample Collection: Collect 200-500 mg of fresh stool or stool preserved in appropriate transport media (e.g., S.T.A.R. buffer, Para-Pak, FecalSwab). Preservation media often improves DNA yield [1] [44].
- Homogenization: Suspend sample in buffer containing an internal extraction control (e.g., Phocine Herpes Virus, PhHV-1) to monitor extraction efficiency and PCR inhibition [44].
- Pre-treatment: Freeze samples at -20°C overnight, then boil for 10 minutes at 100°C to disrupt hardy cyst walls [44].
DNA Extraction:
- Automated Extraction: Use automated systems (e.g., MagNA Pure 96 System, Hamilton MICROLAB STARlet) with commercial kits (e.g., MagNA Pure 96 DNA and Viral NA Small Volume Kit, Roche) following manufacturer's "DNA I Blood_Cells High performance II" protocol or equivalent [1] [33] [44].
- Elution: Elute DNA in a final volume of 50-100 µL of elution buffer [44].
Multiplex Real-Time PCR:
- Reaction Setup: Prepare 25 µL reactions containing:
- 12.5 µL of 2× TaqMan Fast Universal PCR Master Mix
- Primers and probes at optimized concentrations (e.g., 300 nM each Giardia primer, 200 nM probe)
- 5 µL of extracted DNA template
- Sterile water to volume
- Amplification Parameters: Perform on a calibrated real-time PCR instrument (e.g., CFX96, Bio-Rad; QuantStudio 5):
- 95°C for 3 minutes
- 40-45 cycles of: 15 seconds at 95°C, 30-60 seconds at 60°C
- Analysis: Set fluorescence threshold manually or using instrument software. Cq values ≤40 are typically considered positive. Include positive controls (with high and low Cq values) and negative controls in each run [33] [44].
Comprehensive Microscopy Examination Protocol
Protocol: Microscopic Identification of Intestinal Protozoa
Sample Processing:
- Fresh Sample Examination: For liquid or soft stools, examine a direct wet mount (approximately 22×22 mm coverslip) immediately for motile trophozoites [33].
- Concentration: For formed stools, use formalin-ethyl acetate (FEA) concentration or a modified Ritchie's technique to concentrate parasitic elements [44].
- Staining: Prepare permanent stained smears (e.g., trichrome, Giemsa) for detailed observation of internal structures [1] [20].
Microscopic Examination:
- Systematic Screening: Screen the entire coverslip area under 100× magnification, using 400× for identification. Examine at least 300 microscopic fields for concentrated specimens [33].
- Identification: Identify protozoa based on size, morphology, nuclear structure, and inclusion characteristics. Differentiate pathogenic from non-pathogenic species where possible [20].
- Special Stains: Perform modified acid-fast stain for Cryptosporidium spp., Cystoisospora, and Cyclospora when suspected [20].
Quality Control: All examinations should be performed by trained microscopists, with referral to a senior parasitologist for ambiguous specimens [33].
Visualizing Diagnostic Workflows and Result Interpretation
Integrating molecular and microscopic findings requires systematic approaches for both testing procedures and interpreting complex results like co-infections.
Integrated Diagnostic Workflow for Protozoan Detection
The following diagram illustrates a comprehensive diagnostic pathway that leverages the strengths of both molecular and microscopic methods.
Figure 1. Diagnostic workflow for protozoan infection testing. This integrated pathway allows for parallel processing of samples by molecular and microscopic methods, with final synthesis of all results for comprehensive reporting.
Interpretation Framework for Co-infections and Ct Values
The relationship between Ct values, co-infections, and clinical significance requires careful interpretation, as illustrated in the following decision pathway.
Figure 2. Interpretation framework for PCR results and co-infections. This pathway guides the systematic evaluation of molecular results, incorporating both quantitative (Ct value) and qualitative (co-infection profile) parameters before clinical correlation.
Research Reagent Solutions
Successful implementation of protozoan diagnostic methods requires specific research-grade reagents and controls.
Table 3: Essential Research Reagents for Molecular Detection of Intestinal Protozoa
| Reagent Category | Specific Product/Type | Function & Application | Considerations |
|---|---|---|---|
| DNA Extraction | S.T.A.R. Buffer (Roche) | Stool transport & DNA stabilization | Preserves nucleic acids during storage [44] |
| MagNA Pure 96 DNA Kit | Automated nucleic acid extraction | Standardized yields for PCR [1] | |
| PCR Master Mix | TaqMan Fast Universal PCR MM | Probe-based qPCR amplification | Enables multiplex target detection [1] |
| SsoFast Master Mix (Bio-Rad) | High-efficiency PCR amplification | Fast cycling parameters [44] | |
| Internal Control | Phocine Herpes Virus (PhHV-1) | Extraction & amplification control | Monitors inhibition [44] |
| Commercial Panels | AllPlex GIP (Seegene) | Multiplex detection of 6 protozoa | Includes internal control [33] |
| AusDiagnostics RT-PCR | Commercial protozoa detection | Good performance on fixed samples [1] |
Molecular diagnostics have revolutionized protozoan detection by revealing complex co-infation patterns and providing semi-quantitative data through Ct values. However, these advances require sophisticated interpretation frameworks that integrate molecular findings with clinical context and, when necessary, traditional morphological assessment. The protocols and interpretive guidelines presented here provide researchers and drug development professionals with standardized approaches for navigating these complex diagnostic scenarios. As molecular technologies continue to evolve, maintaining a nuanced understanding of both their capabilities and limitations remains essential for advancing our understanding of protozoan diseases and developing effective interventions.
Data-Driven Decisions: Validating Performance Through Multicenter Studies and Meta-Analyses
Within clinical and research parasitology, the accurate detection of protozoan pathogens is fundamental to diagnosis, outbreak control, and drug development. For decades, light microscopy has been the cornerstone technique, prized for its direct visualization of parasitic forms. However, the advent of molecular methods, particularly Polymerase Chain Reaction (PCR), has revolutionized the diagnostic landscape. This application note provides a structured comparison of the sensitivity and specificity of microscopy versus PCR for diagnosing key intestinal protozoan infections, delivering essential performance metrics and detailed protocols for researchers and scientists engaged in diagnostic development.
Performance Data Comparison
The following table summarizes key performance metrics for microscopy and PCR in the detection of major intestinal protozoa, as evidenced by comparative studies.
Table 1: Comparative Sensitivity and Specificity of Microscopy and PCR for Protozoan Detection
| Parasite | Microscopy Sensitivity (%) | PCR Sensitivity (%) | Microscopy Specificity (%) | PCR Specificity (%) | Study Context |
|---|---|---|---|---|---|
| Cryptosporidium spp. [60] | 83.7 | 100 | 98.9 | 100 | Comparative study on 511 stool specimens. |
| Giardia intestinalis [33] | 0.7 (Prevalence) | 1.28 (Prevalence) | Not Reported | Not Reported | Prospective study on 3,495 stool samples. |
| Entamoeba histolytica [33] | 0.68 (Prevalence) | 0.25 (Prevalence) | Not Reported | Not Reported | Prospective study on 3,495 stool samples. |
| Dientamoeba fragilis [33] | 0.63 (Prevalence) | 8.86 (Prevalence) | Not Reported | Not Reported | Prospective study on 3,495 stool samples. |
| Blastocystis spp. [33] | 6.55 (Prevalence) | 19.25 (Prevalence) | Not Reported | Not Reported | Prospective study on 3,495 stool samples. |
| General Intestinal Protozoa [44] | ~50 (Estimated from workflow) | >90 (Estimated from workflow) | Not Reported | Not Reported | Retrospective study evaluating a single-sample PCR vs. triple-sample microscopy. |
The data consistently demonstrates the superior sensitivity of PCR-based detection. The study on Cryptosporidium provides a clear head-to-head comparison, revealing that PCR identified all true positive cases (100% sensitivity), while microscopy missed a significant number, detecting only 83.7% of the positives confirmed by PCR [60]. Furthermore, the higher prevalence rates reported by PCR for parasites like Dientamoeba fragilis and Blastocystis spp. in a large prospective study underscore its enhanced detection capability, particularly for organisms that can be difficult to identify morphologically [33].
Experimental Protocols
To ensure reproducibility and provide a clear framework for methodology comparison, detailed protocols for both techniques are outlined below.
Protocol: Microscopic Examination with Acid-Fast Staining for Cryptosporidium
This protocol is adapted from the conventional Ziehl-Neelsen staining procedure used in comparative studies [60].
1. Sample Preparation:
- Create a thin smear of fecal suspension on a glass slide, similar to a blood film.
- Fix the smear in absolute alcohol for 10 minutes.
2. Staining Procedure:
- Flood the slide with carbol fuchsin stain and allow it to sit for 1 hour.
- Wash the slide gently with water to remove excess stain.
- Decolorize the slide using 3% acid-alcohol for 15 seconds to 1 minute. The duration should be adjusted based on the thickness of the smear.
- Wash the slide again with water.
- Apply 1% methylene blue counterstain for 4 minutes.
- Perform a final wash, air-dry the slide, and proceed to examination.
3. Examination & Interpretation:
- Examine the slide systematically under 20x and 40x objectives.
- Cryptosporidium oocysts appear as bright pink to red spherical structures against a blue or green background.
- A minimum of 5 minutes should be allocated for examining each slide. In cases of low parasite load, screening multiple slides (up to seven) may be necessary to achieve detection [60].
Protocol: PCR Detection of Cryptosporidium from Stool Specimens
This protocol details the DNA extraction and PCR amplification process used in the comparative study [60].
1. DNA Extraction:
- Dilute the stool specimen 1:4 in phosphate-buffered saline (PBS).
- Aliquot 20 µL of the diluted stool suspension into a tube containing 80 µL of 10% Polyvinylpolypyrrolidone (PVPP) to reduce PCR inhibition.
- Boil the mixture for 10 minutes, then centrifuge briefly.
- Transfer the supernatant to a fresh tube containing 200 µL of AL buffer (Qiagen) and 10 µL of glass milk (Bio-Rad).
- Vortex the mixture and incubate at 72°C for 5 minutes.
- Centrifuge the sample and discard the supernatant.
- Wash the pellet twice with 700 µL of AW wash buffer (Qiagen).
- Vacuum-dry the pellet and elute the DNA by adding 50 µL of AE elution buffer (Qiagen), incubating at 72°C for 10 minutes, and centrifuging. The final supernatant contains the purified DNA.
2. PCR Amplification:
- Use 2.5 µL of the extracted DNA in a PCR reaction with genus-specific primers.
- Run all samples in duplicate. One reaction should contain the test sample, and a second "spiked" reaction should contain the test DNA plus a known Cryptosporidium DNA control to rule out PCR inhibition.
- Include a molecular mass ladder and positive and negative controls in each batch run.
- The amplification conditions are as follows: initial denaturation, followed by 40 cycles of denaturation, primer annealing, and extension, as previously described [60].
4. Result Analysis:
- Analyze amplification products by gel electrophoresis.
- The presence of a band of the correct molecular size indicates a positive result. The size of the band can also differentiate between human and bovine genotypes of C. parvum [60].
Workflow Diagram
The following diagram illustrates the key procedural steps and decision points for the two diagnostic methods, highlighting their complexity and hands-on requirements.
Diagram 1: Comparative diagnostic workflows for microscopy and PCR.
The Scientist's Toolkit
The table below lists key reagents and their critical functions in the PCR protocol for protozoan detection.
Table 2: Essential Research Reagent Solutions for PCR-based Protozoan Detection
| Reagent/Kit | Function in the Protocol |
|---|---|
| Polyvinylpolypyrrolidone (PVPP) | Added to the fecal suspension to adsorb PCR inhibitors, thereby improving amplification efficiency [60]. |
| Lysis Buffer (e.g., AL Buffer) | Disrupts cell and oocyst membranes to release nucleic acids for extraction [60]. |
| Silica Matrix (e.g., Glass Milk) | Binds to the released DNA, allowing for its separation from other stool components through centrifugation [60]. |
| Wash Buffer (e.g., AW Buffer) | Washes away impurities and salts from the silica-bound DNA without eluting the DNA itself, resulting in a purer final extract [60]. |
| PCR Master Mix | Contains DNA polymerase, dNTPs, and optimized buffers necessary for the enzymatic amplification of the target DNA [60] [44]. |
| Species-Specific Primers & Probes | Short, custom DNA sequences that define the target region for amplification, providing the high specificity of the assay [60] [44]. |
| Internal Control (e.g., PhHV-1) | Exogenous DNA added to the sample to monitor for the presence of PCR inhibitors and validate the entire extraction and amplification process [44]. |
| Positive Control DNA | DNA from a known target parasite, used to confirm that the PCR assay is functioning correctly [60]. |
Application Note
This application note summarizes findings from an Italian multicenter study evaluating the performance of a commercial RT-PCR test versus an in-house molecular assay for detecting major intestinal protozoa. The study demonstrates that molecular methods, particularly for Giardia duodenalis and Entamoeba histolytica, provide reliable identification comparable to or surpassing conventional microscopy, which remains the diagnostic reference standard despite limitations in sensitivity and species differentiation [6] [7]. The data reveal complete concordance between commercial (AusDiagnostics) and in-house PCR methods for G. duodenalis detection, with both platforms exhibiting high sensitivity and specificity. These findings underscore molecular diagnostics' growing importance in clinical parasitology, while highlighting areas requiring standardization, particularly for DNA extraction from robust protozoal structures.
Intestinal protozoan infections represent a significant global health burden, causing approximately 1.7 billion episodes of diarrheal disease annually and affecting an estimated 3.5 billion people worldwide [7]. Accurate diagnosis remains challenging; microscopy is the traditional reference method but suffers from limitations including operator dependency, limited sensitivity, and inability to differentiate morphologically similar species, such as pathogenic Entamoeba histolytica from non-pathogenic Entamoeba dispar [6] [7].
Molecular diagnostic technologies, especially real-time PCR (RT-PCR), are gaining traction in non-endemic areas with low parasitic prevalence due to their enhanced sensitivity and specificity [6] [7]. This application note details a comparative analysis to bridge knowledge gaps regarding the operational performance of standardized commercial tests versus laboratory-developed in-house assays in a multicenter setting.
Key Comparative Data
The following tables summarize the quantitative findings and performance characteristics observed in the study.
Table 1: Overall Sample Analysis and Result Distribution
| Parameter | Description |
|---|---|
| Total Samples | 355 stool samples [7] |
| Sample Types | 230 fresh samples; 125 samples preserved in Para-Pak media [7] |
| Microscopy-Positive Samples | 285 samples [7] |
| Microscopy-Negative Samples | 70 samples [7] |
| Target Protozoa | Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, Dientamoeba fragilis [6] |
Table 2: Comparative Performance of Molecular Methods vs. Microscopy
| Parasite | Commercial vs. In-House PCR Agreement | Key Performance Observations | Notes on Sample Type |
|---|---|---|---|
| Giardia duodenalis | Complete agreement [6] [7] | High sensitivity and specificity, comparable to microscopy [6] [7] | Reliable detection in both fresh and preserved samples. |
| Cryptosporidium spp. | High specificity, limited sensitivity [6] [7] | Inadequate DNA extraction suspected cause for sensitivity issues [6] | Better PCR results from preserved samples [6]. |
| Entamoeba histolytica | Not explicitly stated | Critical for accurate diagnosis (differentiates from non-pathogenic species) [6] [7] | Molecular assay is a significant improvement over microscopy. |
| Dientamoeba fragilis | High specificity, limited and inconsistent detection [6] [7] | Inadequate DNA extraction suspected cause for sensitivity issues [6] | Detection was inconsistent across methods [6]. |
Discussion of Findings
The study provides compelling evidence that molecular techniques are viable for diagnosing key intestinal protozoa. The complete agreement between commercial and in-house PCR for G. duodenalis confirms robust assay performance for this parasite, making either method a suitable choice for laboratories [6] [7].
A critical finding was the superior performance of molecular assays for E. histolytica, a scenario where microscopy fundamentally fails to distinguish pathogenic from non-pathogenic species [7]. This highlights a primary advantage of molecular diagnostics in ensuring correct clinical management.
The lower sensitivity observed for Cryptosporidium spp. and D. fragilis was attributed to challenges in breaking down the robust wall structure of these organisms during DNA extraction [6] [7]. This indicates that the pre-analytical phase, rather than the PCR chemistry itself, is a key bottleneck. Furthermore, the better PCR results from preserved stool samples versus fresh samples underscore the importance of DNA preservation for reliable molecular detection [6].
This multicenter study confirms that molecular methods, both commercial and in-house, are highly reliable for detecting Giardia duodenalis and essential for the accurate identification of Entamoeba histolytica. While microscopy retains utility for broad screening, molecular assays offer a time-efficient, cost-effective, and specific alternative that reduces reliance on highly skilled microscopists [7].
For consistent implementation, the study concludes that further standardization of sample collection, storage, and DNA extraction procedures is necessary [6]. Laboratories must carefully weigh the benefits of commercial kits (standardization, convenience) against in-house assays (customizability, potential cost savings) based on their specific needs and resources.
Experimental Protocols
Detailed Methodologies
Study Design and Sample Collection
This was a multicentre study conducted across 18 Italian laboratories [7]. A total of 355 consecutive stool samples were collected over six months [7].
- Sample Preparation: Of the 355 samples, 230 were freshly collected and 125 were preserved in Para-Pak media [7].
- Microscopic Examination: All samples underwent conventional microscopy per WHO and CDC guidelines. Fresh samples were stained with Giemsa, while fixed samples were processed using the formalin-ethyl acetate (FEA) concentration technique [7].
- Sample Storage: Following examination, samples were frozen and stored at -20°C prior to molecular analysis [7].
Nucleic Acid Extraction
DNA was extracted from all 355 samples, with a uniform protocol applied for both subsequent PCR methods [7].
- Sample Preparation: 350 µL of Stool Transport and Recovery Buffer (S.T.A.R. Buffer, Roche) was mixed with ~1 µL of fecal sample. After incubation for 5 minutes at room temperature, the mixture was centrifuged at 2000 rpm for 2 minutes [7].
- Supernatant Collection: 250 µL of the supernatant was transferred to a new tube and combined with 50 µL of an internal extraction control [7].
- Automated Extraction: DNA extraction was performed using the MagNA Pure 96 DNA and Viral NA Small Volume Kit on the MagNA Pure 96 System (Roche), a fully automated platform based on magnetic bead separation [7].
Molecular Detection by In-House RT-PCR
The in-house tandem multiplex RT-PCR assay was designed to detect G. duodenalis, Cryptosporidium spp., E. histolytica, and D. fragilis [7].
- Reaction Setup: Each 25 µL reaction mixture contained:
- 5 µL of extracted DNA
- 12.5 µL of 2x TaqMan Fast Universal PCR Master Mix
- 2.5 µL of a custom primers and probe mix
- Nuclease-free water to volume [7].
- Amplification Protocol: Amplification was performed on an ABI 7900HT Fast Real-Time PCR System using the following cycling conditions:
- 1 cycle: 95°C for 10 minutes (initial denaturation/activation)
- 45 cycles: 95°C for 15 seconds (denaturation) and 60°C for 1 minute (annealing/extension) [7].
Molecular Detection by Commercial RT-PCR
The commercial method utilized the AusDiagnostics Company RT-PCR test kit, distributed by Nuclear Laser Medicine [7]. The specific protocols for cycling conditions and reaction setup for the commercial assay were performed according to the manufacturer's instructions, as referenced in the study.
Workflow and Pathway Visualizations
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Application | Specific Example/Note |
|---|---|---|
| Stool Transport & Recovery (S.T.A.R.) Buffer | Stabilizes nucleic acids in stool specimens for downstream molecular analysis. | Used from Roche Applied Sciences [7]. |
| Para-Pak Preservation Media | Preserves parasite morphology for microscopy and nucleic acids for molecular testing. | Used for 125 samples; associated with better DNA preservation [7]. |
| MagNA Pure 96 System & Kits | Automated, high-throughput nucleic acid extraction system based on magnetic bead technology. | Used with the "DNA and Viral NA Small Volume Kit" [7]. |
| TaqMan Fast Universal PCR Master Mix | Optimized buffer/enzyme mix for fast, sensitive, and specific real-time PCR assays. | Used for the in-house RT-PCR assay [7]. |
| Commercial RT-PCR Kit | Standardized, ready-to-use reagents for detecting specific protozoan targets. | AusDiagnostics test, distributed by Nuclear Laser Medicine [7]. |
| Internal Extraction Control | Monitors the efficiency of nucleic acid extraction and checks for PCR inhibition. | Added to the sample supernatant prior to automated extraction [7]. |
| Primers and Probes Mix | Target-specific oligonucleotides for the amplification and detection of parasite DNA. | Custom mix for in-house assay; proprietary in commercial kit [7]. |
For many years, conventional diagnostic methods such as microscopy and culture have been the cornerstone of detecting infectious diseases. However, their limitations in sensitivity, specificity, and turnaround time have led to significant underdiagnosis of many pathogens [44]. Molecular diagnostics, particularly nucleic acid amplification tests (NAATs), have dramatically improved the detection of pathogens that are difficult to culture, occur in low numbers, or are morphologically indistinguishable from non-pathogenic species [61] [62]. This application note details how these methods uncover missed infections, with a specific focus on protozoan diagnosis, providing structured data and actionable protocols for researchers and scientists.
Comparative Detection Rates: Molecular Methods vs. Conventional Techniques
Molecular methods consistently demonstrate superior sensitivity and specificity compared to traditional microscopy and culture, leading to significantly higher detection rates for a range of pathogens.
Table 1: Comparative Detection Rates for Gastrointestinal Protozoa
| Pathogen | Microscopy Detection Rate | Molecular Method Detection Rate | Notes | Source |
|---|---|---|---|---|
| Giardia duodenalis | Baseline (Reference Method) | 100% Agreement; Higher Sensitivity | Complete agreement between commercial & in-house PCR; microscopy misses cases. | [1] |
| Cryptosporidium spp. | Baseline (Reference Method) | High Specificity; Variable Sensitivity | Molecular assays critical; sensitivity impacted by DNA extraction efficiency. | [1] |
| Entamoeba histolytica | Cannot differentiate from non-pathogenic E. dispar | Specific Identification | Molecular methods are essential for accurate diagnosis and differentiation. | [1] [44] |
| Dientamoeba fragilis | Baseline (Reference Method) | High Specificity; Inconsistent Sensitivity | Detection inconsistency likely due to inadequate DNA extraction from the parasite. | [1] |
| General Protozoan Detection | 16.8% (Microscopy on one sample) | 76.7% (Real-time PCR on one sample) | Multiplex real-time PCR significantly increases diagnostic yield for targeted protozoa. | [44] |
Table 2: Impact on Detection in Systemic and Other Infections
| Infection / Context | Conventional Method & Limitation | Molecular Method & Impact | Source |
|---|---|---|---|
| Bloodstream Infections (Sepsis) | Culture: 1-3 days for positivity, low sensitivity post-antibiotics. | PCR: Detection in 2 hours, identifies pathogens in culture-negative cases. | [61] [63] |
| Campylobacter Enteritis | Culture Sensitivity: ~51.2% | Molecular Test Sensitivity: Significantly higher (Specifics not provided) | [64] |
| Pneumonia (Atypical Pathogens) | Culture/Viral PCR: Often negative for key pathogens. | Multiplex PCR: Uncovered Bordetella, Legionella, Mycoplasma in previously negative samples. | [64] |
| Polymicrobial UTI | Culture: Detected 22% of polymicrobial infections. | PCR: Detected 95% of polymicrobial infections. | [64] |
Detailed Experimental Protocols
Protocol 1: Multiplex Real-Time PCR for Intestinal Protozoa from Stool Samples
This protocol, adapted from Formenti et al. (2017) and a 2025 multicentre study, allows for the simultaneous detection of major intestinal protozoa from a single stool sample [1] [44].
Sample Collection and Storage:
DNA Extraction:
- Use approximately 200 mg of stool. Add to a solution of 1X PBS with 2% polyvinylpolypyrrolidone (PVPP) to inhibit PCR inhibitors.
- Include an internal extraction control (e.g., Phocine Herpes Virus, PhHV-1) to monitor for inhibition and successful DNA isolation [44].
- Perform mechanical lysis (e.g., bead beating) to ensure rupture of tough protozoan cysts.
- Extract nucleic acids using a automated system with a magnetic bead-based kit, such as the MagNA Pure 96 System and "DNA I Blood_Cells High performance II" kit (Roche). Elute DNA in a final volume of 100 µL [1] [44].
Real-Time PCR Amplification:
- Reaction Mix: Prepare a 25 µL volume containing:
- 5 µL of extracted DNA template.
- 12.5 µL of 2x TaqMan Fast Universal PCR Master Mix.
- Primers and probes for target pathogens (see Table 3 for examples).
- Primers and probe for the internal control (PhHV-1).
- Nuclease-free water to volume.
- Cycling Conditions:
- Initial Denaturation: 3 min at 95°C.
- 40 Cycles of:
- Denaturation: 15 sec at 95°C.
- Annealing/Extension: 30 sec at 60°C.
- Detection: Perform on a real-time PCR detection system (e.g., CFX 96, Bio-Rad). Include positive controls (with high and low Ct values) and negative controls in each run [44].
- Reaction Mix: Prepare a 25 µL volume containing:
Table 3: Research Reagent Solutions for Protozoan PCR
| Reagent | Function / Target | Example Specifications | Source/Reference |
|---|---|---|---|
| S.T.A.R. Buffer | Stool transport, recovery, and homogenization for DNA extraction. | Commercially available (Roche). | [44] |
| PVPP (Polyvinylpolypyrrolidone) | Binds polyphenols; reduces PCR inhibitors in stool samples. | Molecular biology grade. | [44] |
| MagNA Pure 96 DNA Kit | Automated, high-throughput nucleic acid purification. | "DNA I Blood_Cells High performance II" protocol (Roche). | [1] [44] |
| TaqMan Master Mix | Provides enzymes/dNTPs for probe-based real-time PCR. | 2x concentration, suitable for fast cycling. | [1] |
| PhHV-1 Control | Exogenous internal control for extraction & amplification. | Specific primers/probe for Phocine Herpes Virus. | [44] |
| Pathogen-Specific Primers/Probes | Targets for Giardia, Cryptosporidium, E. histolytica, etc. | Fluorophore-labeled (FAM, VIC, CY5.5) with appropriate quenchers. | [44] |
Protocol 2: Season-Specific Multiplex PCR for Respiratory Pathogens
This protocol, based on a 2025 pneumonia study, demonstrates how tailoring molecular panels to local epidemiology improves detection rates [65].
Panel Design:
- Analyze local surveillance data to define seasonal pathogen prevalence (e.g., Spring vs. Autumn-Winter).
- Design two distinct multiplex PCR panels targeting viruses and bacteria prevalent in each season.
Sample Processing:
- Collect respiratory samples (e.g., nasopharyngeal swabs, sputum) in universal transport media.
- Extract nucleic acids using an automated extraction system, eluting in a final volume of 50-100 µL.
PCR Amplification and Analysis:
- Use a commercial or custom-designed multiplex PCR platform.
- The seasonal panel slashed the median time to pathogen report from ~48 hours to ~12 hours, drastically accelerating diagnosis [65].
Workflow Visualization: Molecular vs. Conventional Diagnosis
The following diagram illustrates the streamlined, sensitive workflow of molecular diagnosis compared to the traditional, multi-step microscopic approach.
The data and protocols presented confirm that molecular methods are fundamentally unmasking a significant burden of previously missed infections. The transition from a multi-sample microscopic examination to a single-sample molecular test not only improves diagnostic yield but also enhances workflow efficiency, reducing time and costs for both laboratories and patients [44]. The ability of multiplex PCR to identify polymicrobial and co-infections provides a more comprehensive clinical picture, enabling precise treatment and better antibiotic stewardship [65] [64].
For protozoan diagnosis, molecular methods are indispensable for differentiating pathogenic from non-pathogenic species, such as Entamoeba histolytica from E. dispar, a critical distinction that microscopy cannot make [1] [44]. The continued standardization of sample collection, DNA extraction, and assay design will further solidify the role of molecular diagnostics as the new gold standard for sensitive and accurate pathogen detection in research and clinical practice.
The diagnosis of intestinal protozoan infections, caused by pathogens such as Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, represents a significant challenge for clinical laboratories worldwide [6] [7]. These infections affect approximately 3.5 billion people annually, causing substantial diarrheal disease burden [7]. For decades, microscopic examination of stool specimens has been the reference standard for detection, but this method requires significant expertise, is time-consuming, and has limitations in sensitivity and species differentiation [55] [66]. Molecular diagnostic technologies, particularly real-time PCR (RT-PCR), are increasingly gaining traction in non-endemic areas with low parasitic prevalence due to their enhanced sensitivity and specificity [6]. This application note provides a comprehensive cost-benefit and operational analysis comparing these diagnostic approaches within the context of a broader thesis on protozoan diagnosis research, focusing specifically on laboratory efficiency and patient throughput metrics relevant to researchers, scientists, and drug development professionals.
Comparative Performance Analysis of Diagnostic Methods
Sensitivity and Specificity Profiles
Table 1: Comparative Diagnostic Performance of Microscopy vs. Molecular Methods for Intestinal Protozoa Detection
| Parasite | Method | Sensitivity Range (%) | Specificity Range (%) | Key Limitations |
|---|---|---|---|---|
| Giardia duodenalis | Microscopy | 83.3 [66] | Not specified | Limited by parasite shedding intermittency & operator skill |
| RT-PCR (Commercial) | 89 [67] | High [6] | DNA extraction efficiency critical | |
| RT-PCR (In-house) | Complete agreement with commercial [6] | High [6] | Requires validation & standardization | |
| Cryptosporidium spp. | Microscopy (with staining) | Variable | Variable | Difficult to differentiate species |
| RT-PCR (Commercial) | 75-100 [67] | High [6] | Variable performance across species | |
| RT-PCR (In-house) | High specificity, limited sensitivity [6] | High [6] | Sensitivity depends on DNA extraction | |
| Entamoeba histolytica | Microscopy | Not quantifiable | Not quantifiable | Cannot differentiate from non-pathogenic E. dispar |
| RT-PCR | Critical for accurate diagnosis [6] | High [6] | Enables species-specific identification | |
| Dientamoeba fragilis | Microscopy | Low | Low | Easily missed without specific staining |
| RT-PCR | 71 [67] | High [6] | Detection inconsistent across platforms [6] | |
| Soil-transmitted helminths | Microscopy (Kato-Katz) | Variable by species intensity [66] | 99.7 [68] | Low sensitivity for low-intensity infections |
| Molecular | Higher sensitivity [66] | High [66] | Differentiates hookworm species [66] |
Operational Efficiency Metrics
Table 2: Operational Workflow Comparison Between Microscopy and Molecular Methods
| Parameter | Traditional Microscopy | Molecular Approach (RT-PCR) |
|---|---|---|
| Sample Requirement | Multiple samples (typically 3) on alternate days [55] | Single sample sufficient [55] |
| Hands-on Time | High (30-60 minutes/sample) [69] | Reduced after extraction automation [69] |
| Time-to-Results | 24-72 hours (multiple samples) [55] | <4 hours after DNA extraction [55] |
| Operator Skill Requirement | High (experienced microscopist essential) [6] [7] | Moderate (training on specific platforms) |
| Automation Potential | Low | High (full automation available) [67] |
| Multiplexing Capability | Limited (additional stains required) | High (multiple targets in single reaction) [55] |
| Throughput Capacity | 10-20 samples/technician/day | 48-96 samples/run (batch processing) [67] |
Experimental Protocols for Method Comparison
Traditional Microscopy Protocol for Intestinal Protozoa
Protocol Title: Standardized Microscopic Examination of Stool Samples for Intestinal Protozoa Detection
Principle: Morphological identification of protozoan trophozoites, cysts, oocysts, and helminth eggs through direct visualization and concentration techniques.
Materials and Reagents:
- Fresh stool samples (minimum 3 collected on alternate days)
- 10% formalin solution
- Ethyl acetate
- Saline solution (0.85% NaCl)
- Lugol's iodine solution
- Microscope slides and coverslips
- Centrifuge and conical tubes
- Formol-ether concentration equipment [55]
Procedure:
- Sample Collection: Collect three stool samples on alternate days to account for intermittent parasite shedding [55].
- Direct Wet Mount:
- Emulsify 1-2 mg of stool in saline solution
- Add coverslip and examine microscopically (10× and 40× objectives)
- Prepare duplicate with iodine stain for cyst visualization
- Formol-Ether Concentration (Ritchie's Method):
- Mix 1 g stool with 10% formalin, filter through sieve
- Add 4 mL diethyl ether, centrifuge at 300 rpm for 1 minute
- Discard supernatant, prepare smear from sediment [66]
- Microscopic Examination:
- Systematically scan entire coverslip area (approximately 22 × 22 mm)
- Identify protozoa based on size, morphology, internal structures
- Differentiate pathogenic vs. non-pathogenic species where possible
Quality Control: Include positive control samples with known parasites; cross-verify difficult specimens with experienced microscopist.
Limitations: Cannot differentiate E. histolytica from E. dispar; sensitivity depends on parasite load and examiner expertise [7].
Molecular Detection Protocol for Intestinal Protozoa
Protocol Title: Multiplex Real-Time PCR Detection of Major Intestinal Protozoa
Principle: Simultaneous detection and differentiation of Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis through targeted amplification of species-specific genetic markers.
Materials and Reagents:
- Stool samples (fresh or preserved in Para-Pak media)
- S.T.A.R. Buffer (Stool Transport and Recovery Buffer; Roche)
- MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche)
- MagNA Pure 96 System (Roche) or equivalent automated extractor
- Primers and probes for target pathogens [6] [55]
- TaqMan Fast Universal PCR Master Mix (Thermo Fisher)
- Real-time PCR instrument (ABI 7900HT or equivalent)
Procedure:
- Sample Preparation:
- Mix 350 μL S.T.A.R. Buffer with approximately 1 μL faecal sample
- Incubate 5 minutes at room temperature, centrifuge at 2000 rpm for 2 minutes
- Transfer 250 μL supernatant to fresh tube [7]
- DNA Extraction:
- Real-Time PCR Amplification:
- Prepare reaction mix: 5 μL DNA template, 12.5 μL 2× TaqMan Master Mix, 2.5 μL primers/probes mix, sterile water to 25 μL
- Cycling conditions: 95°C for 10 min; 45 cycles of 95°C for 15 sec and 60°C for 1 min [7]
- Result Interpretation:
- Analyze amplification curves using instrument software
- Determine positivity based on cycle threshold (Ct) values
- Report species identification based on probe channel
Quality Control: Include extraction controls, positive amplification controls, and negative controls in each run.
Advantages: Differentiates E. histolytica from non-pathogenic species; higher sensitivity for low-level infections [6].
Workflow Visualization
Diagram 1: Comparative diagnostic workflows for protozoan detection. The microscopy pathway (yellow) requires multiple sample collections and extensive expert involvement, while the molecular pathway (green) utilizes a single sample with automated processing steps, significantly reducing hands-on time and subjective interpretation.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for Protozoan Molecular Detection
| Reagent/Kit | Manufacturer | Function | Application Note |
|---|---|---|---|
| MagNA Pure 96 DNA and Viral NA Small Volume Kit | Roche Applied Sciences | Automated nucleic acid extraction | High-quality DNA extraction crucial for PCR sensitivity [7] |
| S.T.A.R. Buffer | Roche Applied Sciences | Stool transport and recovery | Preserves nucleic acids before DNA extraction [7] |
| AusDiagnostics RT-PCR test | AusDiagnostics (R-Biopharm) | Commercial multiplex PCR detection | Complete agreement with in-house methods for G. duodenalis [6] |
| TaqMan Fast Universal PCR Master Mix | Thermo Fisher Scientific | Real-time PCR amplification | Reliable performance in multiplex protozoan detection [7] |
| Para-Pak preservation media | Multiple suppliers | Stool sample preservation | Better DNA preservation for molecular assays [6] |
| Formol-ether concentration reagents | Multiple suppliers | Stool processing for microscopy | Reference method for comparative studies [66] |
| RIDAGENE Parasitic Stool Panel I | R-BioPharm | Multiplex PCR detection | 100% sensitivity for all Cryptosporidium species [67] |
| BD Max Enteric Parasite Panel | Becton Dickinson | Fully automated detection | 89% sensitivity for Giardia detection [67] |
Cost-Benefit Analysis and Operational Impact
The transition from microscopy to molecular methods for intestinal protozoa detection presents significant operational advantages despite higher reagent costs. Studies demonstrate that molecular screening provides higher sensitivity, reduced hands-on time, and faster time-to-results, leading to improved diagnostic efficiency [69]. The implementation of a molecular approach based on the analysis of a single fecal sample (combining coproparasitological examination and RT-PCR) demonstrated equivalent sensitivity to the traditional approach requiring three samples, with the advantage of reducing costs and saving time for both patients and the laboratory [55].
The most significant operational benefit comes from sample number reduction. Where microscopy requires three samples collected on alternate days to account for intermittent parasite shedding, molecular methods demonstrate sufficient sensitivity with a single sample [55]. This reduction directly improves patient throughput by eliminating return visits and streamlining sample processing while maintaining diagnostic accuracy.
Automation potential represents another key efficiency differentiator. Fully automated systems like the BD Max platform enable walk-away processing after sample loading, while microscopy demands constant expert technician involvement [67] [69]. This automation reallocates skilled personnel to more complex tasks and standardizes interpretation, reducing inter-operator variability inherent in microscopic examination [6].
Molecular methods for intestinal protozoa detection offer compelling advantages in laboratory efficiency and patient throughput compared to traditional microscopy. While microscopy remains a valuable tool in resource-limited settings and for detecting a broad spectrum of parasites, molecular technologies provide superior sensitivity, species differentiation, and operational efficiency in high-volume or specialized diagnostic settings. The implementation of PCR-based detection reduces sample collection burden, decreases hands-on technical time, and provides faster results without compromising diagnostic accuracy. Further standardization of sample collection, storage, and DNA extraction procedures will enhance the consistency of molecular methods, solidifying their role as primary diagnostic tools for intestinal protozoa in modern laboratory practice.
Conclusion
The comparative analysis unequivocally demonstrates that molecular methods, particularly RT-PCR, represent a superior diagnostic approach for protozoan infections in terms of sensitivity, specificity, and operational efficiency, especially in low-prevalence or non-endemic settings. However, microscopy retains its value in resource-limited environments and for detecting a broad range of parasites beyond the targets of molecular panels. The future of parasitology diagnostics lies in integrated and innovative approaches. This includes the standardization of sample processing, the adoption of cost-effective single-sample workflows, and the development of advanced technologies such as nanobiosensors, artificial intelligence for automated microscopy, and leveraging genomic data for drug discovery and repurposing. For researchers and drug development professionals, these advancements not only promise more accurate diagnosis but also open new avenues for identifying novel therapeutic targets and managing parasitic diseases on a global scale.
References
- 1. Comparative analysis of commercial and “In-House ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317615/]
- 2. Detection of Intestinal Protozoa in the Clinical Laboratory - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3957779/]
- 3. Parasitic diagnosis: A journey from basic microscopy to cutting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617590/]
- 4. of intestinal Diagnosis infections in patients in Cuba by... protozoan [https://pubmed.ncbi.nlm.nih.gov/33188802/]
- 5. Recent advancements in the diagnosis of parasitic diseases [https://www.sciencedirect.com/science/article/abs/pii/S0166685125000428]
- 6. Comparative analysis of commercial and "In-House ... [https://pubmed.ncbi.nlm.nih.gov/40751255/]
- 7. Comparative analysis of commercial and “In-House ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 8. Burden and Distribution of Protozoan Pathogens in Diarrhea ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494489/]
- 9. Drug Development to Protozoan Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3103878/]
- 10. Global, regional, and national burden of Chagas disease ... [https://www.healthdata.org/research-analysis/library/global-regional-and-national-burden-chagas-disease-1990-2023-systematic]
- 11. Experts tackle hidden risks of foodborne parasites in global ... [https://www.fao.org/food-safety/news/news-details/fr/c/1739613/]
- 12. Exploration of innovative drug repurposing strategies for ... [https://www.sciencedirect.com/science/article/pii/S2095177924001813]
- 13. Identifying Molecular Changes in Giardia lamblia Stages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427673/]
- 14. Comparison of four diagnostic techniques for Cryptosporidium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371275/]
- 15. Molecular characterization and phylogenetic analysis of ... [https://www.sciencedirect.com/science/article/pii/S2052297525000617]
- 16. A Comparative Analysis of Microscopy, Coproantigen ... [https://jlabphy.org/a-comparative-analysis-of-microscopy-coproantigen-serology-and-nested-multiplex-pcr-in-the-laboratory-diagnosis-of-entamoeba-histolytica-infection/]
- 17. Evaluation of Each Three Entamoeba histolytica [https://www.mdpi.com/2076-2607/13/9/1976]
- 18. Detection and subtyping of Blastocystis sp. in human and ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-10423-y]
- 19. Implementation of real-time PCR assays for diagnosing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11978536/]
- 20. Diagnostic Methods of Common Intestinal Protozoa [https://www.mdpi.com/2414-6366/7/10/253]
- 21. Validation of an Automated High-Throughput Multiplex ... [https://www.mdpi.com/2673-947X/5/1/8]
- 22. Polymerase Chain Reaction (PCR) - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK589663/]
- 23. Comparative evaluation of three polymerase chain reaction ... [https://www.veterinaryworld.org/Vol.18/August-2025/21.php]
- 24. Diagnostic dilemma: application of real-time PCR assays for ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06730-1]
- 25. An optimized protocol for stepwise optimization of real-time ... [https://www.nature.com/articles/s41438-021-00616-w]
- 26. Comparative performance evaluation of four commercial ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0215068]
- 27. Comparison of three commercial multiplex PCR assays for ... [https://pubmed.ncbi.nlm.nih.gov/30230444/]
- 28. Performance Comparison of In-House and Commercial ... [https://www.mdpi.com/2075-4418/15/22/2928]
- 29. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 30. FDA vacates final rule regulating lab-developed tests as ... [https://www.aha.org/news/headline/2025-09-18-fda-vacates-final-rule-regulating-lab-developed-tests-medical-devices]
- 31. FDA Reverses Final Rule on LDTs: A Win for Labs, a Shift ... [https://www.swlaw.com/publication/fda-reverses-final-rule-on-ldts-a-win-for-labs-a-shift-in-regulatory-strategy/]
- 32. Microscopy vs. molecular biology in the diagnosis of ... [https://pubmed.ncbi.nlm.nih.gov/36453171/]
- 33. Improvement of the diagnosis of intestinal protozoa using a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077082/]
- 34. Comparative Study of DNA Extraction Methods for the PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9689707/]
- 35. Performance of 30 protocol combinations for the detection ... [https://www.sciencedirect.com/science/article/pii/S1684118225000064]
- 36. Evaluation of Three Protocols of DNA Extraction for ... [https://brieflands.com/journals/jjm/articles/63096]
- 37. Comparison of DNA Extraction Methods and Real-Time ... [https://www.mdpi.com/2076-2607/8/11/1768]
- 38. Comparison of DNA quantity and quality from fecal ... [https://www.sciencedirect.com/science/article/pii/S2352771424000570]
- 39. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimencoll.html]
- 40. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimenproc.html]
- 41. A comparative analysis of preservation techniques for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5773002/]
- 42. a prospective study on 3500 stool samples over 3 years [https://pubmed.ncbi.nlm.nih.gov/40162804/]
- 43. Comparison of fresh versus sodium acetate acetic acid ... [https://link.springer.com/article/10.1007/BF01590942]
- 44. Molecular Biology Can Change the Classic Laboratory ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.02191/full]
- 45. Molecular diagnosis of protozoan parasites by Recombinase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6779323/]
- 46. Diagnosis of intestinal protozoan infections in patients ... [https://www.sciencedirect.com/science/article/pii/S0167701220308186]
- 47. Molecular characterization of Cryptosporidium spp. ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9009872/]
- 48. Sensitivity, specificity and comparison of three ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5790642/]
- 49. DPDx - Amebiasis [https://www.cdc.gov/dpdx/amebiasis/index.html]
- 50. Comparison of Various Methods in the Diagnosis of ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4970550/]
- 51. Conventional Microscopy Versus Molecular and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3573523/]
- 52. Detection and Differentiation of Entamoeba histolytica and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC149615/]
- 53. Comparison of PCR, isoenzyme analysis, and antigen ... [https://pubmed.ncbi.nlm.nih.gov/9466756/]
- 54. Differential diagnosis of human Entamoeba infections ... [https://www.sciencedirect.com/science/article/pii/S0325754123000494]
- 55. Molecular Biology Can Change the Classic Laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5681914/]
- 56. DNA Extraction from Protozoan Oocysts/Cysts in Feces for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4096637/]
- 57. Molecular diagnosis - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/moleculardx.html]
- 58. Comparison of GeneXpert cycle threshold values with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6519814/]
- 59. Comparison of Real-time RT-PCR cycle threshold (Ct) ... [https://www.sciencedirect.com/science/article/pii/S2667038023000133]
- 60. Comparison of PCR and Microscopy for Detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC104676/]
- 61. Molecular Methods for Diagnosis of Infective Endocarditis [https://pmc.ncbi.nlm.nih.gov/articles/PMC2928072/]
- 62. Molecular Approaches to Diagnosing and Managing ... [https://wwwnc.cdc.gov/eid/article/7/2/70-0312_article]
- 63. Culture-free detection of bacteria from blood for rapid ... [https://www.nature.com/articles/s41746-025-01948-w]
- 64. Is it time to substitute culture with molecular diagnostics for ... [https://www.thermofisher.com/blog/clinical-conversations/is-it-time-to-substitute-culture-with-molecular-diagnostics-for-infectious-diseases/]
- 65. Rapid, season-specific PCR testing versus traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318422/]
- 66. Advantages and Limitations of Microscopy and Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9979072/]
- 67. Comparison of three commercial multiplex PCR assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6144649/]
- 68. Diagnostic accuracy of screening and diagnostic tests used ... [https://www.nature.com/articles/s41598-025-94346-x]
- 69. Impact of transition from microscopy to molecular screening ... [https://www.sciencedirect.com/science/article/pii/S1198743X14653556]