High-Throughput Parasite Screening: Advanced Methodologies for Drug Discovery and Diagnostic Innovation
This article provides a comprehensive overview of modern high-throughput screening (HTS) methodologies transforming parasite research and drug development.
High-Throughput Parasite Screening: Advanced Methodologies for Drug Discovery and Diagnostic Innovation
Abstract
This article provides a comprehensive overview of modern high-throughput screening (HTS) methodologies transforming parasite research and drug development. It explores foundational principles of HTS automation and miniaturization, details specific applications across major human parasites including Plasmodium, Trichomonas, and helminths, and offers practical troubleshooting guidance for assay optimization. Through comparative analysis of molecular, phenotypic, and image-based approaches, we validate screening platforms that enable rapid antimalarial resistance profiling, natural product discovery, and anthelmintic testing. This resource equips researchers and drug development professionals with the knowledge to implement robust, scalable screening strategies that accelerate therapeutic innovation and improve diagnostic capabilities in parasitology.
The Foundations of High-Throughput Parasite Screening: Principles, Technologies, and Market Landscape
Defining High-Throughput Screening (HTS) and Ultra-HTS in Parasitology
Core Definitions and Quantitative Benchmarks
What is the fundamental difference between HTS and uHTS in a parasitology screening context?
High-Throughput Screening (HTS) is an automated method for scientific discovery, crucially used in drug discovery, that allows a researcher to rapidly conduct millions of chemical, genetic, or pharmacological tests [1]. Using robotics, data processing software, liquid handling devices, and sensitive detectors, HTS facilitates the identification of active compounds, antibodies, or genes that modulate a particular biomolecular pathway [1]. In parasitology, this technique is applied to identify compounds active against parasitic targets [2] [3].
Ultra-High-Throughput Screening (uHTS) is an evolution of HTS, representing an automated methodology for conducting hundreds of thousands of biological or chemical screening tests per day [4]. The distinction is somewhat arbitrary but is generally defined by a throughput in excess of 100,000 compounds per day [1] [4]. uHTS has become accessible to smaller research companies and academic groups as instrumentation costs have decreased [4].
Table 1: Key Quantitative Benchmarks for HTS and uHTS
| Parameter | Traditional HTS | uHTS |
|---|---|---|
| Throughput (compounds per day) | Tens of thousands to 100,000 [1] [4] | In excess of 100,000; systems exist for over 1,000,000 [1] [4] |
| Common Microplate Formats | 96, 384, 1536-well plates [1] | 1536, 3456, 6144-well plates; chip-based and droplet microfluidics [1] [4] |
| Assay Volume | Microliters (μL) to nanoliters (nL) in microplates [1] | Nanoliters (nL); picoliter (pL) volumes in droplet-based microfluidics [1] |
| Primary Screening Goal | Identify "hits" - compounds with a desired size of effects [1] | Rapidly process immense compound libraries to identify initial hits [5] |
Detailed Experimental Protocol: A Multiplexed Glycolysis Screen inTrypanosoma brucei
The following protocol is adapted from a recent (2024) open-access study that developed a high-throughput flow cytometry screening assay to identify glycolytic probes in bloodstream form Trypanosoma brucei, a kinetoplastid parasite [6].
1. Assay Principle: This method uses live parasites transfected with biosensors to simultaneously measure multiple glycolysis-relevant metabolites. It multiplexes biosensors for glucose (a FRET biosensor), ATP (a FRET biosensor), and glycosomal pH (a GFP-based biosensor), alongside a viability dye (thiazole red), in a single flow cytometry run [6].
2. Key Materials and Reagents:
- Cell Line: Bloodstream form Trypanosoma brucei parasites.
- Biosensors: Transfected cell lines expressing the FRET-based glucose and ATP sensors, and the GFP-based pH sensor.
- Compound Library: For example, the Life Chemicals Compound Library or other relevant chemical collections.
- Assay Plates: 384-well or 1536-well microplates.
- Instrumentation: A flow cytometer capable of high-throughput sampling from microplates.
3. Step-by-Step Workflow:
- Cell Preparation: Pool the sensor cell lines. The pH sensor has a different fluorescent profile from the FRET sensors, allowing simultaneous measurement of pH with either glucose or ATP [6].
- Plate Loading: Dispense the pooled sensor cell lines into the assay plates, which have been pre-loaded with the compound library. The library is analyzed twice: once with the pooled pH and glucose sensor cell lines, and once with the pooled pH and ATP sensor cell lines [6].
- Incubation: Incubate the plates to allow compound-parasite interaction.
- High-Throughput Flow Cytometry: Analyze the plates using the flow cytometer. The cytometer measures the fluorescence signals from all biosensors and the viability dye for each well simultaneously [6].
- Data Analysis: Process the data to determine the impact of each compound on the measured parameters (glucose, ATP, pH, and viability). Calculate Z'-factor values to confirm assay quality. Hit rates from the pilot screen of 14,976 compounds were between 0.2% and 0.4% [6].
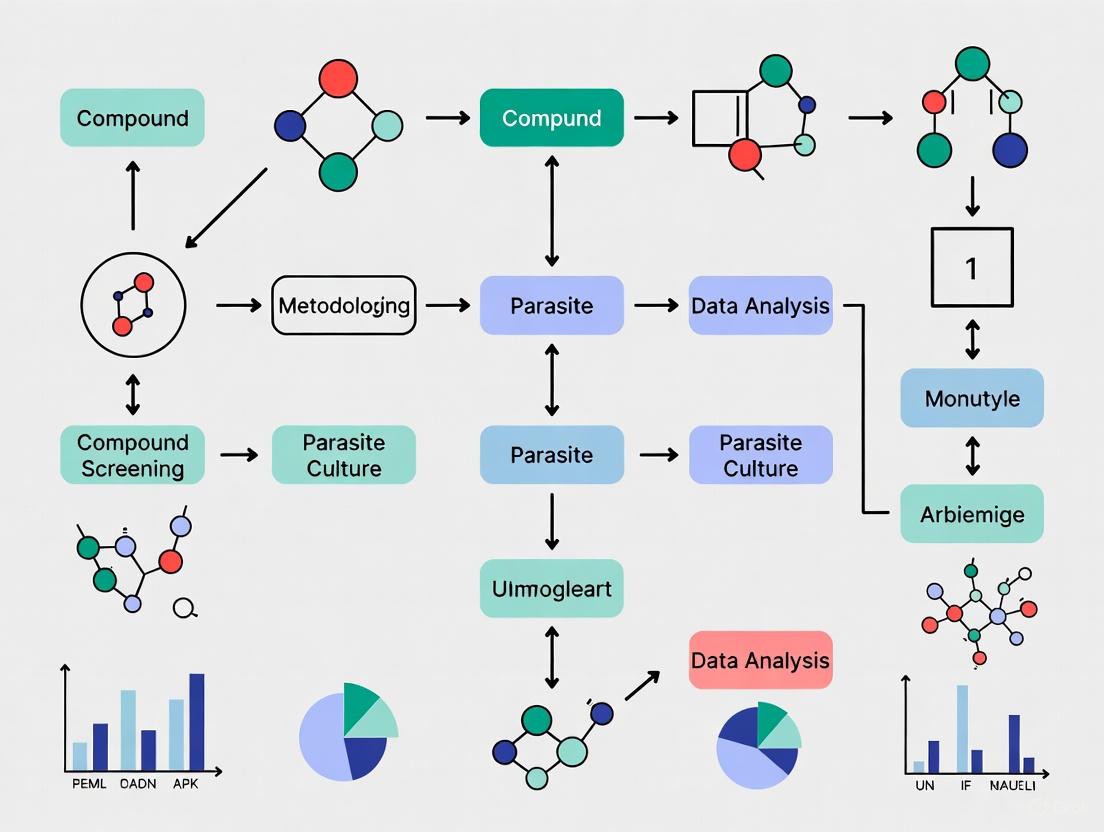
Diagram 1: Workflow for a multiplexed glycolysis screen.
Troubleshooting Guides and FAQs
FAQ 1: Our HTS campaign in Plasmodium is generating an unacceptably high number of false positives. What are the primary quality control measures we can implement? A high false-positive rate often indicates underlying assay quality issues. Implement these QC steps:
- Effective Plate Design: Incorporate both positive controls (a known inhibitor) and negative controls (DMSO-only) randomly across the plate to identify and correct for systematic errors, such as edge effects [1].
- Calculate a QC Metric: Use the Z'-factor to evaluate the assay's quality and its suitability for HTS. An assay with a Z'-factor >= 0.5 is considered excellent for screening [6]. The Z'-factor assesses the separation between the positive and negative control signals, factoring in their variations [1].
- Use Robust Hit Selection Methods: For primary screens without replicates, avoid simple metrics like percent inhibition that don't capture data variability. Instead, use robust statistical methods like the z-score or SSMD which are less sensitive to outliers [1].
FAQ 2: We have identified "hits" from our primary uHTS against Leishmania. What is the critical next step to confirm biological relevance? Primary hits must be advanced to secondary screening [5]. This involves:
- Hit Confirmation: Re-test the selected hits in a dose-response manner to confirm activity and eliminate false positives resulting from assay interference.
- Determine Specificity: Test confirmed hits for cytotoxicity against mammalian cell lines to assess selectivity for the parasite.
- Understand Mechanism: Begin to investigate the compound's mechanism of action and specificity, which may involve additional, more complex phenotypic assays [2] [5].
FAQ 3: Our assay uses a 384-well format, but we are considering moving to 1536-wells to increase throughput. What are the key technical challenges? Miniaturization to 1536-well plates and beyond introduces specific challenges:
- Liquid Handling: Requires highly accurate and precise nanoliter-volume liquid handlers to avoid volumetric errors that can cripple assay performance.
- Evaporation: Smaller volumes are more susceptible to evaporation, particularly in edge wells, which can create significant well-to-well variation. Using sealed plates or controlled humidity environments is critical.
- Assay Signal Strength: With less biological material and fewer cells per well, the signal intensity decreases. This requires highly sensitive detection systems, such as confocal imaging or advanced luminescence readers, to maintain a robust signal-to-noise ratio [4] [7].
Diagram 2: Troubleshooting a high false-positive rate.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagents and Materials for HTS in Parasitology
| Item | Function in HTS/uHTS | Example in Parasitology |
|---|---|---|
| Microtiter Plates | The key labware for HTS; disposable plastic plates with a grid of wells to hold assays and compounds. | Used in various formats (96 to 1536 wells) to host parasite cultures, recombinant parasitic enzymes, or cell-free systems for screening [1]. |
| Compound Libraries | Diverse collections of small molecules, natural product extracts, or oligonucleotides used to find initial "hits." | Unbiased compound collections screened against whole parasites (phenotypic) or specific parasitic targets (target-based) [2] [3]. |
| Biosensors | Genetically encoded or chemical tools that report on a specific metabolic or ionic state in live cells. | FRET-based biosensors for glucose or ATP, and GFP-based biosensors for organellar pH in T. brucei [6]. |
| Fluorescence & Luminescence Detection Kits | Enable highly sensitive, automation-compatible detection of biological activity. | Fluorescence polarization (FP), FRET, and luminescence assays are common. Thiazole red used as a viability dye in flow cytometry [7] [6] [8]. |
| Automated Liquid Handlers | Robotics for accurate and precise transfer of nanoliter to microliter volumes for assay plate preparation. | Critical for creating assay plates from stock compound plates and for adding reagents/parasites during uHTS campaigns [1] [4]. |
| Antibacterial agent 176 | Antibacterial agent 176, MF:C21H23ClN4O2, MW:398.9 g/mol | Chemical Reagent |
| Hsd17B13-IN-80 | Hsd17B13-IN-80, MF:C25H18Cl2F3N3O3, MW:536.3 g/mol | Chemical Reagent |
Within high-throughput screening (HTS) for parasite research, automation and miniaturization are critical for efficiently testing thousands of compounds. This technical support center addresses common operational challenges in these workflows, providing targeted troubleshooting guides and FAQs to help researchers maintain data integrity and experimental efficiency in critical research, such as the search for new anthelmintics [9].
Frequently Asked Questions (FAQs)
1. My automated liquid handler is dripping from the tips, contaminating the deck. What could be wrong? Dripping tips are often caused by a mismatch between the vapor pressure of your sample and the water used for system adjustment, or by the viscous nature of certain reagents [10] [11]. Solutions include sufficiently pre-wetting tips, adding an air gap after aspiration, or adjusting the aspirate and dispense speeds to account for the liquid's characteristics [11].
2. Our high-throughput screening of a 30,000-compound library is showing an unexpected rate of false negatives. What could be the source of this error? In the context of parasite screening, false negatives can be severely detrimental as active compounds may be overlooked [10]. A potential cause is the under-delivery of critical reagents by the liquid handler, which leads to lower-than-intended reagent concentrations in assay wells [10]. It is crucial to regularly verify the accuracy and precision of volume transfers through calibration and quantitative verification checks [10].
3. When performing serial dilutions for dose-response assays, the observed EC50 values are inconsistent. Where should I look? A common source of error in serial dilution protocols is insufficient mixing [10]. If the reagents in the wells are not homogenized before transfer, the concentration of critical reagents will differ from the theoretical concentration, leading to flawed results [10]. Ensure your method includes adequate mixing steps, such as multiple aspirate/dispense cycles, and validate that volumes are consistent across all dilution steps [10].
4. The robot arm is not moving to its taught positions correctly. What are the first things to check? First, check the teach pendant for any fault or alarm codes [12] [13]. Confirm that all safety mechanisms, such as gate sensors, have not been triggered [13]. A simple system restart can sometimes clear errors. If problems persist, check for mechanical issues like worn cables or calibrate the robot's motion and axis systems [14].
Troubleshooting Guides
Guide 1: Troubleshooting Liquid Handling Inaccuracies
Liquid handling errors can compromise screening data. Follow this logical pathway to diagnose common issues.
Common Liquid Handling Errors and Solutions The table below summarizes specific errors, their possible sources, and proven solutions [11].
| Observed Error | Possible Source of Error | Possible Solutions |
|---|---|---|
| Dripping tip or hanging drop | Difference in vapor pressure of sample vs. adjustment water [11] | Sufficiently pre-wet tips; Add an air gap after aspiration [11] |
| Droplets or trailing liquid during delivery | Viscosity and other liquid characteristics [11] | Adjust aspirate/dispense speed; Add air gaps/blow outs [11] |
| First/last dispense volume difference in sequential dispensing | Inherent to sequential dispense method [10] [11] | Dispense first/last quantity into reservoir/waste [11] |
| Serial dilution volumes varying from expected concentration | Insufficient mixing in the wells [10] | Measure and improve liquid mixing efficiency [11] |
| Incomplete aspiration or dispensing | Loose tip fit or worn equipment [15] | Press tip firmly for a 'click'; use correct pipette size; schedule calibration [15] |
Guide 2: General Robotic System Failure
When an industrial robot or automated system stops working, a systematic approach is key to minimizing downtime [13].
Experimental Protocols and Validation
Protocol: Validating Liquid Handler Performance for Critical Reagents
Purpose: To ensure automated liquid handlers dispense accurate and precise volumes of critical reagents, thereby protecting the integrity of HTS data and controlling costs associated with rare compounds [10].
Background: Inaccurate liquid handling can have severe economic consequences. For example, a 20% over-dispensing of a reagent costing $0.10 per well can lead to hundreds of thousands of dollars in additional annual costs in a large screening laboratory. More critically, under-dispensing can cause false negatives, potentially causing a promising therapeutic compound to be overlooked [10].
Methodology:
- Selection of Verification Method: Use a standardized, quantitative platform (e.g., gravimetric, photometric, or fluorometric) suitable for the volumes being tested [10].
- Assay Setup: Program the liquid handler to dispense the target volume(s) into a suitable microplate. Include a comparison of different tip types (vendor-approved vs. generic) if this is a variable [10].
- Execution: Run the verification protocol multiple times (e.g.,
n=50cycles) to observe repeatability and identify surface-level errors [12]. - Data Analysis: Calculate the accuracy (% deviation from target volume) and precision (% coefficient of variation) for each dispensing channel.
- Acceptance Criteria: Define and apply action limits based on the requirements of your specific assay. Systems failing these limits should be calibrated, serviced, or have their methods re-optimized [10].
Data Presentation: Economic Impact of Volume Transfer Error The following table models the potential financial impact of liquid handling inaccuracies in a large-scale screening environment, based on data from [10].
| Screening Parameter | Baseline Scenario | With 20% Over-Dispensing | Impact |
|---|---|---|---|
| Wells per screen | 1.5 million | 1.5 million | - |
| Screenings per year | 25 | 25 | - |
| Cost per well | $0.10 | $0.12 | +$0.02 |
| Annual reagent cost | $3.75 million | $4.5 million | +$750,000 |
Protocol: Automated Parasite Detection with the Orienter Model FA280
Purpose: To provide a high-throughput, automated alternative to the manual formalin-ethyl acetate concentration technique (FECT) for detecting parasite ova in stool samples [16].
Workflow Overview:
Key Considerations:
- Throughput: The FA280 processes batches of 40 samples in approximately 30 minutes [16].
- Agreement with FECT: The FA280 with user audit showed perfect agreement (κ = 1.00) with FECT for species identification of protozoa and strong agreement for helminths (κ = 0.857) in one study [16].
- Limitations: The FA280 may have lower sensitivity than FECT, potentially due to the smaller stool sample size (0.5 g vs. 2 g). Cost per test may also be higher [16].
The Scientist's Toolkit: Essential Research Reagents and Materials
| Item | Function/Application | Key Consideration |
|---|---|---|
| Vendor-Approved Pipette Tips | Accurate aspiration and dispensing of liquids [10]. | Cheap bulk tips may have variable properties (wettability, flash) causing delivery errors [10]. |
| Air Displacement Liquid Handler | Versatile pipetting for aqueous reagents [11]. | Prone to errors from pressure changes or leaks; ensure tight seals [11]. |
| Positive Displacement Liquid Handler | Pipetting viscous, foaming, or volatile liquids [11]. | Requires checking for bubbles, kinks, and leaks in tubing; liquid temperature affects flow rate [11]. |
| FRET-based Biosensors | Multiplexed measurement of metabolites (e.g., glucose, ATP) in live parasites during HTS [6]. | Enables simultaneous analysis of multiple pathways; Z'-factor should be acceptable for HTS [6]. |
| Formalin-Ethyl Acetate | Sedimentation and concentration of parasites in stool for FECT, the traditional gold standard [16]. | Uses a larger sample size (2 g), potentially increasing sensitivity compared to some automated methods [16]. |
| Microplates (96-well) | Standard platform for HTS assays [10]. | Proper deck layout definition in software is critical to avoid errors [10]. |
| Ret-IN-26 | Ret-IN-26, MF:C23H27N5O2, MW:405.5 g/mol | Chemical Reagent |
| (Trp4)-Kemptide | (Trp4)-Kemptide, MF:C40H66N14O9, MW:887.0 g/mol | Chemical Reagent |
This technical support center addresses the key technological considerations for implementing and troubleshooting microplate-based assays within high-throughput screening (HTS) for parasite research. The transition from standard 96-well formats to higher-density plates (384-well, 1536-well, and beyond) is a cornerstone of modern drug discovery, enabling the rapid testing of thousands of compounds against pathogenic parasites such as Plasmodium and Trypanosoma [17] [18]. The following guides and FAQs are designed to help researchers navigate the practical challenges of assay miniaturization and automation, directly supporting methodologies in high-throughput parasite screening.
Frequently Asked Questions (FAQs)
1. What are the primary factors to consider when choosing between a 96-well and a 384-well plate for a phenotypic screen of Plasmodium falciparum?
The choice involves a trade-off between throughput, sample volume, and experimental complexity [19].
- 96-well plates are suitable for smaller compound libraries or when larger sample volumes (typically 100-300 µL) are required for complex assay setups [20] [19]. They are also more amenable to manual pipetting.
- 384-well plates offer a four-fold increase in throughput and significantly reduce reagent and compound consumption, with well volumes typically ranging from 30-100 µL [20] [19]. This makes them ideal for large-scale HTS campaigns. However, they usually require automated liquid handling systems for efficient and accurate pipetting [20].
2. How does microplate color affect my assay readout in fluorescence-based parasite viability screens?
The microplate color is critical for optimizing signal-to-background ratios and minimizing well-to-well crosstalk [20].
- Black Microplates are recommended for standard fluorescence intensity assays (e.g., using fluorescent dyes like Hoechst 33342 [18]). The black color quenches signal, reducing background and crosstalk, which is vital when detecting strong signals [20].
- White Microplates are best for luminescence assays and time-resolved fluorescence (TRF) protocols, which typically have lower signal yields. The white color reflects the signal, maximizing the detected output [20].
- Clear Microplates are reserved for absorbance measurements, where light must pass through the sample [20].
3. My HTS data is showing a high rate of false positives. What are the common causes and solutions?
False positives are a well-known challenge in HTS and can arise from several factors [21]:
- Assay Interference: Compounds may chemically react with assay components, exhibit autofluorescence, or form colloidal aggregates that non-specifically inhibit enzymes [21].
- Solution: Implement counter-screens and use cheminformatic filters (e.g., pan-assay interference compound substructure filters) to triage HTS output [21]. The use of robust statistical methods for hit selection, such as setting a threshold at three standard deviations from the mean of control wells, is also recommended [17].
4. What are the key steps in validating a cell-based HTS assay for parasite drug discovery?
A robust HTS assay must be validated for performance and reproducibility [21].
- Robustness and Reproducibility: The assay should be optimized for miniaturization and automation, and tested for consistency across multiple experimental runs [21].
- Pharmacological Relevance: The assay should accurately reflect the biological pathway or phenotype being targeted [21].
- Statistical Validation: Use metrics like the Z′-factor to quantify the assay's suitability for HTS. A Z′-factor value of >0.5 is generally considered excellent for screening [6]. This involves measuring the signal-to-noise ratio by comparing positive and negative controls.
Troubleshooting Guides
Problem: Low Signal or Poor Signal-to-Noise Ratio in Absorbance Readouts
Potential Causes and Solutions:
- Incorrect Microplate Material: Standard polystyrene plates do not transmit UV light (<320 nm). For nucleic acid quantification (A260) or assays requiring UV light, use plates made from cyclic olefin copolymer (COC) or quartz [20].
- Absorbance Value Too High: For reliable quantitative measurements, absorbance values should ideally be between 0.1 and 1.0. Samples with absorbance greater than 3.0 are outside the reliable detection range and should be diluted [22].
- Suboptimal Sample Volume: As a general rule, the lowest recommended volume in a well is one-third of its maximum fill volume. For a standard 96-well plate (max 300 µL), do not go below 100 µL [20].
Problem: Inconsistent Results in a 384-Well Automated Screening Run
Potential Causes and Solutions:
- Pipetting Errors: Automated liquid handlers require regular calibration. Check for clogged tips or inconsistent dispensing.
- Edge Effects: Evaporation in outer wells can cause inhomogeneity. Use a plate sealer and ensure consistent temperature regulation across the plate during incubation [23].
- Cell Settling or Clumping: For cell-based parasite assays (e.g., with T. brucei), ensure cells are homogeneously suspended before dispensing. Using U-bottom or C-bottom plates can facilitate mixing and prevent uneven cell distribution [20].
Problem: High Well-to-Well Crosstalk in Fluorescence Assay
Potential Causes and Solutions:
- Incorrect Plate Color: As outlined in the FAQs, using a black microplate is essential for fluorescence assays to absorb stray light and prevent signal leakage between adjacent wells [20].
- Well Shape: Square wells with shared walls are more susceptible to crosstalk than round wells. If crosstalk is a significant issue, consider switching to a microplate with round wells [20].
- Signal Saturation: If very bright samples are adjacent to dim ones, optical crosstalk can occur even in black plates. Consider re-arranging samples or diluting highly fluorescent ones.
Experimental Protocol for an Image-Based Antimalarial HTS
This protocol is adapted from a published HTS for Plasmodium falciparum inhibitors [18].
1. Objective: To identify novel antimalarial compounds from a chemical library using an image-based phenotypic screen.
2. Materials and Reagents:
- Parasites: Synchronized Plasmodium falciparum culture (e.g., strain 3D7).
- Compound Library: Pre-dispensed in 384-well glass-bottom microplates.
- Staining Solution: 1 µg/mL wheat agglutinin–Alexa Fluor 488 conjugate (stains RBCs) and 0.625 µg/mL Hoechst 33342 (stains nucleic acid) in 4% paraformaldehyde [18].
- Equipment: Automated plate washer, liquid handler, high-content imaging system (e.g., Operetta CLS).
3. Procedure:
- Step 1: Compound Transfer. Using an automated liquid handler, transfer compounds from the library to the assay plate. The final test concentration is typically 10 µM.
- Step 2: Parasite Inoculation. Dispense synchronized P. falciparum schizont-stage cultures at 1% parasitemia and 2% hematocrit into the compound-treated assay plates.
- Step 3: Incubation. Incubate the plates for 72 hours at 37°C in a mixed-gas chamber (1% O₂, 5% CO₂, balanced N₂).
- Step 4: Staining and Fixation. After incubation, dilute the plates to 0.02% hematocrit and stain with the staining solution for 20 minutes at room temperature.
- Step 5: Image Acquisition. Acquire nine microscopy image fields from each well using a 40x water immersion lens.
- Step 6: Image Analysis. Transfer images to analysis software (e.g., Columbus). An algorithm is used to identify and classify parasites based on the fluorescent stains, quantifying parasite growth inhibition for each well.
4. Data Analysis:
- Hit Selection: Compounds that cause a reduction in parasite count exceeding a pre-defined threshold (e.g., three standard deviations from the mean of the DMSO control wells) are classified as "hits" [17].
- Dose-Response: Confirm "hits" by retesting in a dose-dependent manner (e.g., from 10 µM to 20 nM) to determine the half-maximal inhibitory concentration (IC₅₀) [18].
Quantitative Data for Microplate Selection
Table 1: Comparison of Common Microplate Formats for HTS [20]
| Well Format | Total Wells | Typical Working Volume | Key Applications in Parasite HTS |
|---|---|---|---|
| 96-Well | 96 | 100 - 300 µL | Smaller-scale phenotypic screens, assay development. |
| 384-Well | 384 | 30 - 100 µL | Standard for large compound library screening against Plasmodium or Trypanosoma [18]. |
| 1536-Well | 1536 | 5 - 25 µL | Ultra-high-throughput screening (uHTS) for miniaturized assays; requires specialized automation [21]. |
| 3456-Well | 3456 | 1 - 5 µL | Specialized uHTS; not commonly used due to extreme handling requirements [20]. |
Table 2: Microplate Material and Color Selection Guide [20]
| Property | Options | Recommended Use |
|---|---|---|
| Material | Polystyrene | Standard absorbance assays and microscopy (transmits visible light). |
| Cyclic Olefin Copolymer (COC) | UV light applications (e.g., DNA/RNA quantification). | |
| Polypropylene | PCR or sample storage (stable across a wide temperature range). | |
| Color | Clear | Absorbance assays (e.g., ELISA). |
| Black | Fluorescence intensity assays (reduces crosstalk). | |
| White | Luminescence and time-resolved fluorescence (TRF) assays. |
Workflow and Pathway Visualizations
HTS Workflow for Parasite Screening
Microplate Format Selection Logic
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for High-Throughput Parasite Screening
| Reagent / Kit | Function | Example Use Case |
|---|---|---|
| EZ DNA Methylation-Lightning Kit | Bisulfite conversion of DNA for methylation analysis [24]. | Epigenetic studies in parasite development or drug resistance. |
| NEBNext Ultra II End repair/dA-tailing Module | Prepares DNA ends for adapter ligation [25]. | Next-generation sequencing library preparation for parasite genomics. |
| NEB Blunt/TA Ligase Master Mix | Ligates barcodes and adapters to DNA fragments [25]. | Multiplexing samples for high-throughput sequencing. |
| Qubit dsDNA HS Assay Kit | Highly specific quantification of double-stranded DNA [25]. | Accurate DNA measurement pre- and post-library prep. |
| Wheat agglutinin–Alexa Fluor 488 | Fluorescently labels red blood cell membranes [18]. | Image-based HTS to distinguish host cells from background. |
| Hoechst 33342 | Cell-permeant nucleic acid stain [18]. | Image-based HTS to identify and quantify intracellular parasites. |
| AMPure XP Beads | Solid-phase reversible immobilization (SPRI) for DNA size selection and clean-up [25]. | Purifying and size-selecting sequencing libraries. |
| Mao-IN-4 | Mao-IN-4, MF:C18H11Cl2N3OS, MW:388.3 g/mol | Chemical Reagent |
| Aurein 2.4 | Aurein 2.4, MF:C77H133N19O19, MW:1629.0 g/mol | Chemical Reagent |
Technical Support Center: High-Throughput Parasite Screening
Troubleshooting Guides
Issue 1: High False-Positive Rates in Primary Screening
- Problem: Initial HTS hits prove to be inactive in confirmatory assays.
- Solution:
- Confirm with Secondary Assays: Validate primary hits using an orthogonal assay with a different readout (e.g., follow a fluorescence-based assay with a microscopy-based viability check) [26] [27].
- Counter-Screens: Implement detergent-based or other counter-screens to identify and eliminate compounds that cause assay interference or non-specific binding [28].
- Check Compound Integrity: Confirm the identity and purity of the hit compounds to rule out degradation or mislabeling [27].
Issue 2: Poor Assay Performance (Low Z'-factor)
- Problem: The positive and negative controls in your assay plate are not well separated, leading to unreliable data.
- Solution:
- Optimize Reagents: Re-titrate key assay reagents, such as parasite density, substrate concentration, and incubation time, to improve the dynamic range [29] [27].
- Review Protocol: Check for inconsistencies in liquid handling, mixing, or incubation times that could increase variability. Automation can help standardize these steps [28].
- Aim for Z' > 0.5: A Z'-factor above 0.5 is generally considered acceptable for a robust HTS assay [6] [28].
Issue 3: Inconsistent Parasite Viability Measurements
- Problem: Cell viability readings are inconsistent across replicate wells.
- Solution:
- Standardize Culture: Ensure parasites are harvested during logarithmic growth phase and are maintained in a consistent, healthy state before the assay [6].
- Multiplexed Viability Readout: Incorporate a viability marker like thiazole red directly into a multiplexed flow cytometry assay to simultaneously measure metabolic activity and cell health [6].
- Use Validated Assays: Employ established cell viability or cytotoxicity assays, such as ATP-based luminescence assays, which are known for their sensitivity and wide dynamic range [27].
Frequently Asked Questions (FAQs)
Q1: What is the recommended number of compounds to screen for a novel parasite target? Screening campaigns can range from focused libraries of 10,000 compounds to larger libraries exceeding 30,000 compounds. The size depends on the project goals and resources [26] [9]. For example, one study successfully identified hits by screening 10,000 drug-like molecules against Leishmania donovani, while another screened over 30,000 compounds for anthelmintic activity [26] [9].
Q2: How many technical and biological replicates are sufficient for an HTS campaign? For primary screening, duplicates or even single-point measurements are often used due to the high volume. However, all initial "hit" compounds must be confirmed in dose-response curves (IC50 determinations) with at least triplicate replicates and multiple biological repeats to ensure reproducibility and accurate potency measurement [26] [9].
Q3: What are the key parameters to prioritize hits before moving to medicinal chemistry? Beyond potency (IC50), key parameters include:
- Selectivity Index (SI): The ratio of cytotoxicity in mammalian cells to anti-parasitic activity. An SI > 10 is often considered favorable [26].
- Drug-Likeness: Predicted ADME (Absorption, Distribution, Metabolism, Excretion) properties should indicate a high probability of oral bioavailability and a low risk of adverse effects [26].
- Morphological Assessment: Confirmation of anti-parasitic activity through visual techniques like scanning electron microscopy, which can reveal compound-induced physical damage to the parasites [26].
Q4: Our laboratory is new to HTS. What are the essential components for setting up a screening pipeline? A basic HTS pipeline requires:
- Compound Library: A curated collection of small molecules.
- Assay Reagents: Optimized biological components (e.g., stable parasite lines, substrates, buffers).
- Automation: Liquid handling robots for dispensing into microtiter plates (96, 384, or 1536-well format) [28].
- Detection Instrumentation: Plate readers or flow cytometers capable of measuring fluorescence, luminescence, or absorbance [27] [6].
- Data Analysis Software: Tools for data normalization, hit identification, and statistical analysis [28].
Experimental Protocols & Data
Table 1: Representative Quantitative Data from Recent HTS Campaigns Against Parasites
| Parasite | Library Size | Primary Hits (>80% Inhibition) | Confirmed Hits (IC50 < 10 µM) | Key Assay Type | Reference |
|---|---|---|---|---|---|
| Leishmania donovani | 10,000 | 99 | 4 | Cell viability / Phenotypic | [26] |
| Gastrointestinal Nematodes | 30,238 | 55 (Broad-spectrum) | 1 novel scaffold (F0317-0202) | Motility / Phenotypic | [9] |
| Trypanosoma brucei | 14,976 | 28 (Repeatable activity) | 1 (Low µM EC50) | Multiplexed Flow Cytometry | [6] |
Detailed Protocol: Multiplexed Flow Cytometry Screening for Glycolytic Probes in Trypanosoma brucei [6]
- Preparation of Biosensor Cell Lines: Transfect T. brucei bloodstream form parasites with biosensors for glucose (FRET-based), ATP (FRET-based), and glycosomal pH (GFP-based).
- Cell Pooling and Plating: Pool the sensor cell lines and dispense them into assay plates containing the compound library using automated liquid handling.
- Compound Incubation: Incubate the plates to allow compounds to take effect.
- Flow Cytometry Analysis: Analyze the plates using a high-throughput flow cytometer. The system simultaneously measures:
- FRET signals for glucose or ATP levels.
- GFP fluorescence for organelle pH.
- Thiazole red fluorescence for cell viability.
- Data Processing: Calculate Z'-factors for each biosensor readout to validate assay quality. Identify hits that cause significant changes in the measured metabolites compared to controls.
- Hit Confirmation: Re-test primary hits in dose-response experiments to determine EC50 values for the relevant sensors.
Detailed Protocol: High-Throughput Phenotypic Screening for Anti-Leishmanial Compounds [26]
- Parasite Culture: Maintain Leishmania donovani promastigotes or amastigotes in appropriate culture media.
- Assay Setup: Use automation to dispense parasites into 384-well plates. Add compounds from the library (e.g., 10,000 compounds from ChemDiv) at a single concentration (e.g., 50 µM).
- Incubation: Incubate plates for a predetermined period (e.g., 72 hours) to allow compound action.
- Viability Measurement: Add a cell viability indicator (e.g., alamarBlue or resazurin) and measure fluorescence or absorbance.
- Hit Identification: Calculate percent inhibition relative to untreated (100% viability) and compound-only (0% viability) controls. Select compounds showing >80% inhibition as primary hits.
- Dose-Response Confirmation: Re-test primary hits in a dilution series to determine the half-maximal inhibitory concentration (IC50).
- Secondary Assays:
- Cytotoxicity: Assess hits against mammalian cell lines (e.g., THP-1, J774) to calculate the Selectivity Index.
- Morphology: Use scanning electron microscopy (SEM) to examine compound-induced morphological alterations in the parasites.
Signaling Pathways and Workflows
HTS Drug Discovery Cascade
Multiplexed Biosensor Screening
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for High-Throughput Parasite Screening
| Item | Function & Application | Example / Specification |
|---|---|---|
| Compound Libraries | Collections of small molecules for screening against parasitic targets. | In-house ChemDiv library [26]; Life Chemicals Compound Library [6]; Target-focused (kinase, GPCR) libraries [9]. |
| Cell Viability Assays | Measure parasite metabolic activity or membrane integrity to assess compound lethality. | Fluorescence (e.g., alamarBlue) or luminescence (ATP-based) readouts [26] [27]. |
| Biosensor Cell Lines | Genetically engineered parasites expressing fluorescent reporters to monitor specific metabolic pathways in live cells. | FRET-based glucose/ATP sensors; GFP-based pH sensors [6]. |
| Automation Platforms | Robotics for precise, high-speed dispensing of liquids into microtiter plates. | Tecan or Hamilton liquid handlers; 384-well or 1536-well plate formats [28]. |
| Detection Instruments | Devices to measure assay signals from microtiter plates or cell suspensions. | Multimode plate readers (absorbance, fluorescence); High-throughput flow cytometers [6] [28]. |
| Antigen Detection Kits | Immunoassays (EIA, DFA, rapid tests) for specific, morphology-independent parasite diagnosis. | Commercial kits for Cryptosporidium, Giardia, and Entamoeba histolytica [30]. |
| iRGD-CPT | iRGD-CPT, MF:C75H100N18O27S3, MW:1781.9 g/mol | Chemical Reagent |
| Mbl-IN-2 | Mbl-IN-2, MF:C9H12F3NO3S, MW:271.26 g/mol | Chemical Reagent |
Addressing Parasitic Disease Burden Through Scalable Screening Solutions
Frequently Asked Questions (FAQs)
Q1: What are the main limitations of traditional diagnostic methods I might use in my research, and why are they unsuitable for high-throughput screening?
Traditional methods like microscopy, serology, and histopathology, while foundational, have several limitations for scalable screening. They are often time-consuming, require a high level of technical expertise, and are impractical in resource-limited settings. Their sensitivity and specificity can be variable, making them less reliable for large-scale or surveillance studies where high throughput and accuracy are critical [31].
Q2: Which advanced molecular techniques are most suitable for developing a high-throughput screening pipeline?
Several advanced techniques have shown great promise for scalable screening:
- Polymerase Chain Reaction (PCR) and Digital PCR: These methods offer enhanced sensitivity and specificity for detecting parasite DNA, even in cases of low parasitemia [31].
- Next-Generation Sequencing (NGS): NGS allows for the untargeted discovery of pathogens, detailed genomic characterization, and the ability to track drug resistance markers, making it powerful for comprehensive screening [31].
- Loop-mediated Isothermal Amplification (LAMP): This technique is particularly valuable for field applications or resource-limited settings as it does not require sophisticated thermocycling equipment and provides rapid results [31].
- CRISPR-Cas Systems: Emerging CRISPR-based diagnostics offer high specificity, portability, and potential for rapid, point-of-care detection of parasitic DNA or RNA [31].
Q3: How can "signature-based" diagnostics improve the accuracy of parasitic disease detection?
Signature-based diagnostics move beyond reliance on a single biomarker. Instead, they utilize a unique combination of multiple biomarkers—a diagnostic "fingerprint"—for a specific disease state. This approach can significantly improve both diagnostic accuracy and specificity. For example, a signature might combine specific parasite antigens with host-derived antibodies or cytokines to create a more robust and reliable diagnostic panel than any single marker could provide [32].
Q4: What are the key considerations for integrating Point-of-Care (POC) tests into a large-scale screening strategy?
When planning for POC integration, focus on tests that are:
- Rapid and Simple: They should deliver results quickly and require minimal training to administer.
- Equipment-Independent: Ideal POC tests for scalable screening do not rely on complex lab equipment.
- Stable: They must remain effective in various environmental conditions, especially when deployed in the field. The goal of POC testing is to enable rapid and accurate detection at or near the patient care site, which is vital for screening in remote or endemic areas without centralized laboratories [31].
Troubleshooting Guides
Issue 1: Low Sensitivity in Molecular Detection
Problem: Your PCR or other molecular assay is failing to detect known positive samples, indicating low sensitivity.
| Possible Cause | Solution |
|---|---|
| Inadequate DNA/RNA extraction | Optimize the extraction protocol for the specific sample type (e.g., blood, stool). Include a sample preparation step that efficiently breaks down tough parasite structures. |
| Inhibitors present in the sample | dilute the nucleic acid template or use purification kits designed to remove common inhibitors like heme or humic acids. Incorporate an internal control to detect the presence of inhibitors. |
| Suboptimal primer/probe design | Re-design primers and probes to target multi-copy genes or conserved regions specific to your parasite of interest. Validate them against a panel of well-characterized positive and negative controls. |
Issue 2: Inconsistent Results in Rapid Diagnostic Tests (RDTs)
Problem: Lateral flow immunoassays (RDTs) are producing variable results, including false negatives or faint test lines.
| Possible Cause | Solution |
|---|---|
| Improper storage or expired tests | Strictly adhere to manufacturer storage recommendations (often 2-30°C). Never use tests beyond their expiration date. |
| Deviation from protocol | Ensure precise sample and buffer volumes. Use a timer to adhere strictly to the recommended reading time, as reading too early or too late can cause errors. |
| Prozone effect (high analyte concentration) | If antigen levels are very high, it can paradoxically cause a false negative. Dilute the sample and re-run the test to check for a positive result. |
| Low parasite burden | Be aware that RDTs may fail during the early or chronic phases of infection when antigen/antibody levels are low. Confirm with a more sensitive molecular method [31]. |
Issue 3: High Background Noise in Serological Assays (e.g., ELISA)
Problem: Your ELISA plate shows high background signal, reducing the signal-to-noise ratio and making results difficult to interpret.
| Possible Cause | Solution |
|---|---|
| Insufficient washing | Increase the number of wash cycles after each incubation step and ensure the wash buffer is fresh and correctly prepared. |
| Non-specific antibody binding | Include a protein blocking step (e.g., with BSA or non-fat dry milk) prior to adding the primary antibody. Titrate antibodies to find the optimal concentration that maximizes specific signal and minimizes background. |
| Contaminated reagents | Prepare fresh reagents and ensure all buffers are free of microbial contamination. |
Experimental Protocols for Key Methodologies
Protocol 1: Multiplex PCR for Parallel Pathogen Detection
Objective: To simultaneously detect and differentiate multiple parasitic pathogens in a single reaction, increasing screening throughput.
Materials:
- Template DNA from patient samples
- Multiplex PCR Master Mix (containing buffer, dNTPs, hot-start polymerase)
- Primer mix (multiple primer pairs specific to different parasite targets, designed to have similar annealing temperatures)
- Thermocycler
- Gel electrophoresis equipment or capillary electrophoresis system for analysis
Methodology:
- Primer Design: Design primers to generate amplicons of distinct sizes for each target (e.g., 100bp, 200bp, 300bp) to allow for clear differentiation by gel electrophoresis. Ensure all primers have minimal self-complementarity and similar melting temperatures.
- Reaction Setup: Prepare the PCR reaction on ice. A typical 25µL reaction may contain: 12.5µL Master Mix, 2.5µL primer mix, 5µL template DNA, and nuclease-free water up to 25µL.
- Thermocycling: Use a standardized cycling protocol:
- Initial Denaturation: 95°C for 5 minutes
- 35-40 Cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing: 60°C for 30 seconds (optimize temperature based on primers)
- Extension: 72°C for 1 minute
- Final Extension: 72°C for 7 minutes
- Analysis: Separate the PCR products by gel electrophoresis. The presence of specific bands, corresponding to the expected sizes, indicates detection of that particular parasite.
Protocol 2: Biomarker Signature Validation using a Microfluidic Immunoassay
Objective: To validate a panel of putative biomarkers (a signature) for a specific parasitic disease using a highly parallelized microfluidic chip.
Materials:
- Microfluidic chip with multiple parallel chambers, each pre-functionalized with a capture antibody for a different biomarker [32].
- Fluorescently-labeled detection antibodies.
- Patient serum or plasma samples.
- 1X PBS buffer and blocking buffer (e.g., 1% BSA in PBS).
- Fluorescence scanner or microscope for detection.
Methodology:
- Chip Preparation: Prime the microfluidic channels with PBS. Load the blocking buffer to cover all potential protein-binding sites and incubate.
- Sample Incubation: Introduce the patient sample into the chip. Biomarkers of interest will bind specifically to their corresponding capture antibodies in the different chambers.
- Washing: Flush the chip with PBS buffer to remove unbound proteins and sample matrix.
- Detection: Introduce a mixture of fluorescent detection antibodies. Each detection antibody will bind to its specific captured biomarker.
- Final Wash and Reading: Perform a final wash to remove unbound detection antibodies. Scan the chip to measure the fluorescence intensity in each chamber.
- Data Analysis: The fluorescence pattern across the chambers constitutes the biomarker signature. Use statistical or machine learning models to determine if this signature accurately classifies the sample as infected or not, and potentially by which parasite [32].
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Parasite Screening |
|---|---|
| Monoclonal Antibodies | Highly specific reagents used in immunoassays (ELISA, RDTs, microfluidics) to capture and detect parasite-specific antigens with high consistency [32]. |
| Primers/Probes for qPCR | Oligonucleotides designed to target unique genomic sequences of parasites, enabling highly sensitive and quantitative detection of parasite DNA/RNA in patient samples [31]. |
| CRISPR-Cas Enzymes (e.g., Cas12a, Cas13) | Used in novel diagnostic platforms for their ability to specifically cleave parasite nucleic acids, often coupled with a reporter molecule for highly sensitive and specific point-of-care detection [31]. |
| Functionalized Magnetic Nanoparticles | Nanoparticles coated with antibodies or other capture molecules are used to isolate and concentrate specific parasites or their biomarkers from complex sample matrices like blood or stool, improving downstream assay sensitivity [31]. |
| Reference Genomic DNA | Purified DNA from well-characterized parasite strains serves as essential positive controls for validating molecular assays like PCR and NGS, ensuring accuracy and reliability [33]. |
| Synthetic Biomarker Panels | Defined mixtures of synthetic antigens or nucleic acids representing a diagnostic "signature." These are used to develop, optimize, and calibrate multi-analyte screening tests [32]. |
| Eupenicisirenin C | Eupenicisirenin C, MF:C13H18O4, MW:238.28 g/mol |
| Sydowimide A | Sydowimide A, MF:C15H16N2O4, MW:288.30 g/mol |
Advanced HTS Applications: From Molecular Detection to Phenotypic Drug Screening
The accurate detection of low-density malaria parasitemias is a critical challenge in elimination settings. Conventional molecular methods typically evaluate finger-prick capillary blood samples (∼5 μl), limiting detection to parasite densities above approximately 200 parasites/mL [34]. To address this sensitivity barrier, researchers have developed a highly sensitive "high-volume" quantitative PCR (qPCR) method based on Plasmodium sp. 18S RNA, adapted for blood sample volumes of ≥250 μl [34]. This technical support center provides comprehensive guidance for implementing this methodology within high-throughput parasite screening programs, addressing common experimental challenges and providing validated solutions for the research community.
Experimental Protocols & Workflows
Core High-Volume qPCR Methodology
Blood Sample Collection and DNA Extraction
- Sample Collection: Collect whole blood samples (1 ml) in EDTA tubes [34]
- Processing: Centrifuge at 2,500 rpm for 10 min to remove all plasma together with 70-100 μl of the buffy coat per 1 ml of whole blood [34]
- Storage: Freeze the packed red blood cells (RBCs) at -30°C until DNA extraction [34]
- DNA Extraction: Use QIAamp blood minikit for sample volumes ≤200 μl or QIAamp blood midi kit for volumes between 200-2,000 μl packed RBCs [34]
- DNA Concentration: Completely dry purified DNA in a centrifugal vacuum concentrator and resuspend in a small volume of PCR-grade water to create a concentrate (1 μl template corresponds to 100 μl of whole blood) [34]
Quantitative Real-Time PCR Setup
- Template Volume: Use 2-μl aliquot of concentrated DNA per qPCR reaction [34]
- Chemistry: QuantiTect multiplex PCR NoROX with 1× QuantiTect buffer, 0.4 μM each primer, and 0.2 μM hydrolysis probe [34]
- Thermocycling Conditions:
- Initial denaturation: 95°C for 15 minutes
- Amplification: 50 cycles of 94°C for 15s (denaturation) and 60°C for 60s (annealing/extension) [34]
- Internal Control: Multiplex human beta-actin gene assay to monitor reaction efficiency [34]
Workflow Visualization
Performance Characteristics & Validation Data
Analytical Performance Metrics
Table 1: Validation Parameters of High-Volume qPCR for Malaria Detection
| Validation Parameter | Performance Result | Reference Method Comparison |
|---|---|---|
| PCR Efficiency | 90-105% | Similar to conventional qPCR |
| Analytical Detection Limit (LOD) | 22 parasites/mL (95% CI: 21.79-74.9) | 50x more sensitive than conventional PCR from filter paper [34] |
| Diagnostic Specificity | 99.75% | Comparable to established molecular methods [34] |
| Sample Throughput | ~700 samples/week | Higher than manual extraction methods [34] |
| Blood Volume Processed | ≥250 μL | 50x larger than standard 5μL filter paper spots [34] |
| Dynamic Range | 20 - 250,000 parasites/mL | Broader than microscopy and RDTs [34] |
Comparative Method Performance
Table 2: Comparison of Malaria Diagnostic Methods for Low-Density Infections
| Method | Effective Blood Volume | Limit of Detection | Throughput | Suitable for Asymptomatic Screening |
|---|---|---|---|---|
| High-Volume qPCR | ≥250 μL | 22 parasites/mL | High (700 samples/week) | Yes [34] |
| Conventional PCR | 2-5 μL | ~1,000 parasites/mL | Moderate | Limited [34] |
| Droplet Digital PCR | Varies | <1 parasite/μL | Moderate | Yes [35] |
| Light Microscopy | 0.025-0.0625 μL | 50-100 parasites/μL | Low | No [35] |
| Rapid Diagnostic Tests | Varies | ~100-200 parasites/μL | High | Limited [36] [37] |
Technical Support & Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of high-volume qPCR over conventional molecular methods for malaria detection?
High-volume qPCR increases the effective blood volume processed by 50-100 times compared to conventional methods that use only 2-5μL of blood [34]. This substantially improves the limit of detection to 22 parasites/mL, enabling identification of low-density infections that would be missed by standard PCR, microscopy, or rapid diagnostic tests [34]. These submicroscopic infections are increasingly recognized as important reservoirs for ongoing malaria transmission.
Q2: How should we handle inconsistent results between technical replicates in low-density samples?
For samples with densities <2 copies/μL, some replicates may return negative results due to stochastic effects [35]. We recommend:
- Running triplicate reactions for all samples
- Considering a sample positive if ≥2/3 replicates are positive
- Using a standardized DNA concentration method to minimize variation
- Implementing droplet digital PCR (ddPCR) for absolute quantification if replicate inconsistency persists, as ddPCR shows higher reproducibility for low-template samples [35]
Q3: What quality control measures are essential for reliable high-volume qPCR results?
Implement a comprehensive QC system including:
- Standard curves using FACS-sorted ring-stage parasites (range: 20-10,000 parasites) [34]
- Internal control (human beta-actin) multiplexed in each reaction [34]
- Extraction controls with known parasite densities in uninfected whole blood
- Regular monitoring of PCR efficiency (maintain 90-105%)
- Prospective CT cutoff set at 40 cycles to maximize sensitivity while maintaining specificity [34]
Q4: How does high-volume qPCR compare to emerging diagnostic technologies like droplet digital PCR?
While high-volume qPCR provides excellent sensitivity and throughput for population screening, ddPCR offers advantages in absolute quantification without standard curves and better reproducibility at very low parasite densities [35]. However, high-volume qPCR remains more practical for large-scale studies, processing ~700 samples weekly with automated systems [34]. The choice depends on study objectives: high-volume qPCR for high-throughput screening and ddPCR for precise quantification in mechanistic studies.
Q5: What are the common sources of false positives and how can they be minimized?
False positives in high-volume qPCR primarily occur due to contamination during sample processing. Root cause analysis identified these key areas [34]:
- Cross-contamination during DNA extraction: Use separated pre- and post-PCR areas
- Carryover during sample concentration: Implement unidirectional workflow
- Amplicon contamination: Use uracil-N-glycosylase systems and thorough cleaning Maintain diagnostic specificity >99.7% through rigorous contamination control protocols and include no-template controls in every run [34].
Research Reagent Solutions
Essential Materials for High-Volume qPCR Implementation
Table 3: Key Research Reagents and Their Applications in High-Volume qPCR
| Reagent/Equipment | Specification | Function in Workflow |
|---|---|---|
| DNA Extraction Kits | QIAamp blood minikit (≤200μL) or midi kit (200-2,000μL) [34] | Parasite DNA purification from packed RBCs |
| qPCR Master Mix | QuantiTect multiplex PCR NoROX [34] | Amplification with optimized buffer system |
| Primers/Probes | Plasmodium 18S rRNA-targeting with hydrolysis probes [34] | Species-specific detection and quantification |
| Internal Control Assay | Human beta-actin primers/probe [34] | Monitoring extraction and amplification efficiency |
| Reference Standards | FACS-sorted P. falciparum 3D7 ring stages [34] | Standard curve generation for absolute quantification |
| Automated Extraction System | QIAsymphony with DSP DNA midi kit [34] | High-throughput, reproducible DNA purification |
Advanced Applications in Parasite Screening
Integration with High-Throughput Surveillance Strategies
High-volume qPCR represents a cornerstone technology for modern malaria surveillance programs aiming for elimination. Its exceptional sensitivity (50-fold greater than conventional PCR) enables detection of the "submicroscopic reservoir" - asymptomatic individuals with low parasite densities who contribute significantly to transmission [34]. When processing 700 samples weekly, this method facilitates large-scale screening of populations in pre-elimination settings, providing crucial data for targeted intervention strategies [34].
The methodology is particularly valuable for:
- Molecular Monitoring of Interventions: Tracking real-time changes in parasite prevalence following control measures
- Asymptomatic Carrier Detection: Identifying reservoirs in low-transmission settings [38]
- Drug Efficacy Studies: Detecting emerging resistance through precise parasite density measurements
- Vaccine Trials: Providing sensitive endpoints for protective efficacy assessment
For comprehensive malaria surveillance programs, high-volume qPCR can be integrated with complementary approaches including bead-based antigen detection for high-throughput screening [37] and droplet digital PCR for absolute quantification in research applications [35]. This multi-platform approach provides program managers with the granular data needed to make informed decisions about intervention strategies in the pursuit of malaria elimination.
Image-Based High-Content Screening for Natural Product Discovery Against Trichomonas vaginalis
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: Why is a resazurin-based assay insufficient for our anti-T. vaginalis screening, and what is a superior alternative?
Answer: Resazurin assays lack sensitivity for detecting partial inhibition at standard inoculum sizes. A population of approximately 10,000 trichomonads per well in a 96-well plate is the threshold for a consistent signal, meaning a compound achieving 75% parasite kill could be misclassified as inactive. An image-based, high-content assay is a validated superior alternative. This method fixes parasites with glutaraldehyde and uses a dual cell-staining system with acridine orange (cell-permeable, stains all cells) and propidium iodide (cell-impermeant, stains only dead cells) for precise live/dead determination. This assay is robust (Z-factor of 0.92), can detect as few as one trichomonad per image field, and is compatible with colored or UV-active natural products, as images can be manually inspected to rule out interference [39].
FAQ 2: How do we address rapid parasite movement that causes blurring in live-cell imaging?
Answer: The rapid movement of flagellated trichomonads, which causes blurring even with fast exposure times, is resolved by fixing the cells with glutaraldehyde prior to imaging. This process halts all motion, enabling clear and quantifiable imaging of individual parasites for subsequent live/dead analysis using fluorescent DNA stains [39].
FAQ 3: Our natural product extracts are colored or fluorescent. Will this interfere with the assay readout?
Answer: Unlike colorimetric or fluorescence-intensity-based assays, the image-based high-content assay is highly resilient to such interference. While colored compounds can quench signals in other assay formats, the direct visualization and counting of individual cells in this platform allow for manual inspection of stored image files to identify and discount any potential false positives or negatives caused by interfering properties of the test substances [39].
FAQ 4: What is an appropriate vehicle for compound testing, and at what concentration?
Answer: Dimethyl sulfoxide (DMSO) is an acceptable vehicle for compound testing. A concentration of 1% by volume has been demonstrated to have no detrimental impact on the viability of T. vaginalis cells and is therefore suitable for use in this assay [39].
Experimental Protocols
Protocol 1: Image-Based High-Content Screening Assay forT. vaginalisViability
This protocol is adapted from the method developed to test a library of fungal natural product extracts and pure compounds [39].
1. Principle The assay fixes trichomonads to eliminate motility-based blurring and uses a dual fluorescent DNA stain to differentiate live from dead cells based on membrane integrity. Acridine orange penetrates all cells, while propidium iodide only penetrates cells with compromised membranes.
2. Materials
- Parasite Strain: T. vaginalis (e.g., ATCC strain)
- Culture Medium: Trypticase-yeast extract-maltose (TYM) or Diamond's medium, pH ~6.2 [40]
- Fixative: Glutaraldehyde solution
- Stains: Acridine Orange (AO) and Propidium Iodide (PI)
- Equipment: High-content imaging system (e.g., Operetta, PerkinElmer), 96-well or 384-well microtiter plates, anaerobic chamber or sealed environment for incubation [39]
3. Step-by-Step Procedure Step 1: Parasite Inoculation
- Harvest mid-logarithmic phase T. vaginalis cells by low-speed centrifugation.
- Resuspend parasites in fresh culture medium and adjust concentration.
- Dispense 40,000 trichomonads in a volume of 100-200 µL into each well of a 96-well microtiter plate. Include negative (medium only) and positive (untreated parasites) controls [39].
Step 2: Compound Addition
- Add test compounds, extracts, or controls (e.g., 25 µM metronidazole as a positive control) to respective wells. The final concentration of DMSO should not exceed 1% [39].
- Seal plates to maintain anaerobic conditions and incubate at 37°C for 24-48 hours.
Step 3: Fixation and Staining
- Carefully add glutaraldehyde to each well to a final concentration sufficient to fix cells (e.g., 0.5-1.0%). Incubate for a fixed time at room temperature.
- Remove fixative and wash cells with buffer if necessary.
- Add a solution containing both Acridine Orange and Propidium iodide to stain the fixed cells.
- Incubate in the dark for a predetermined time [39].
Step 4: Imaging and Analysis
- Image each well using a high-content imager, capturing at least two image fields per well.
- Use appropriate excitation/emission filters for AO (e.g., 502/526 nm, green) and PI (e.g., 536/617 nm, red).
- Employ analysis software to count total cells (AO-positive) and dead cells (PI-positive). The number of live cells is calculated as the difference [39].
Protocol 2: Validation with a Phenol Red pH-Based Growth Assay
This protocol provides a simpler, cost-effective complementary method for growth assessment [40].
1. Principle Trichomonad growth in culture medium produces acidic metabolites that lower the pH. The color change of the phenol red indicator from red (pH ~7.4) to yellow (pH ~6.0) can be used as a quantitative and qualitative indicator of growth.
2. Materials
- Phenol red-containing culture medium
- 96-well or 384-well microtiter plates
- Plate reader (to measure absorbance at ~560 nm)
3. Procedure
- Inoculate parasites into phenol red-containing medium in microtiter plates as in Protocol 1, Step 1.
- After incubation, measure the absorbance of the medium. A decrease in absorbance correlates with a drop in pH and increased parasite growth.
- This assay has demonstrated consistent dynamic ranges with Z′-factor values of 0.741 (384-well) and 0.870 (96-well), confirming its robustness for screening [40].
Table 1: Performance Metrics of Screening Assays for T. vaginalis
| Assay Type | Key Metric | Value | Significance/Interpretation |
|---|---|---|---|
| Image-Based High-Content [39] | Z-factor | 0.92 | Excellent robustness for high-throughput screening. |
| Detection Limit | 1 cell/field | Highly sensitive, can detect very low parasite numbers. | |
| Phenol Red (pH-Based) [40] | Z'-factor (384-well) | 0.741 | Robust for medium-throughput screening. |
| Z'-factor (96-well) | 0.870 | Robust for high-throughput screening. | |
| Resazurin-Based [39] | Detection Threshold | ~10,000 cells/well | Low sensitivity; may miss partial inhibition. |
Table 2: Exemplar Hit Compound from a Natural Product Screen
| Compound Name | Class | ECâ‚…â‚€ vs. T. vaginalis | Selectivity Index (SI) vs. 3T3 cells | Selectivity Index (SI) vs. Ect1 cells |
|---|---|---|---|---|
| Pyrrolocin A [39] | Decalin-linked tetramic acid | 60 nM | 100 | 167 |
| 2-Bromoascididemin [39] | Not Specified | Not Specified | 14 | Not Specified |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Image-Based HTS
| Reagent/Material | Function in the Assay | Key Details & Considerations |
|---|---|---|
| Acridine Orange | Cell-permeant nucleic acid stain. Labels all cells (live and dead). | Used in combination with PI for live/dead determination in fixed cells [39]. |
| Propidium Iodide (PI) | Cell-impermeant nucleic acid stain. Labels only dead/damaged cells. | Used in combination with AO. PI-positive cells are counted as dead [39]. |
| Glutaraldehyde | Fixative. Cross-links proteins, immobilizing parasites for clear imaging. | Eliminates motility-induced blurring. Concentration and exposure time must be optimized [39]. |
| Dimethyl Sulfoxide (DMSO) | Universal solvent for hydrophobic compounds and natural product extracts. | Final concentration in assay should be ≤1% to avoid cytotoxicity to parasites [39]. |
| Metronidazole | Nitroimidazole drug; standard positive control for inhibition. | Used as a reference compound (e.g., 25 µM) to validate assay performance [39]. |
| Phenol Red | pH indicator in culture medium. | Allows for chromogenic, growth-based screening in 96-/384-well formats [40]. |
| Hsd17B13-IN-32 | Hsd17B13-IN-32, MF:C23H15Cl2N5O3, MW:480.3 g/mol | Chemical Reagent |
| Parp7-IN-17 | Parp7-IN-17, MF:C20H20F3N7O2, MW:447.4 g/mol | Chemical Reagent |
Experimental Workflow Visualization
High-Throughput Screening Workflow
Real-Time Motility Monitoring for Anthelmintic Drug Screening and Resistance Diagnosis
Frequently Asked Questions (FAQs) & Troubleshooting Guide
Q1: Our motility readings for a known anthelmintic drug show high variability between assay plates. What could be causing this inconsistency?
A: Inconsistent results can stem from several sources related to parasite preparation and assay conditions.
- Parasite Health: Ensure parasites are harvested from synchronized cultures and are in the same developmental stage. Using a mix of stages can lead to differential drug responses [41] [42].
- Culture Conditions: Maintain strict temperature control. For example, Strongyloides ratti L3 are assayed at 21°C, while adult hookworms require 37°C [41] [42]. Evaporation can be minimized by filling inter-well spaces with PBS [41].
- Drug Preparation: Use a consistent DMSO concentration across all wells and dilutions. High concentrations can be toxic and confound results [43].
- Instrument Calibration: Perform regular background readings and calibrations as specified by the instrument manufacturer (e.g., the xCELLigence system or WMicrotracker) before initiating experiments [41] [43].
Q2: We are not detecting a significant motility phenotype for a compound that is known to be effective in vivo. Is our assay failing?
A: Not necessarily. Many effective anthelmintics require host immune components for full efficacy and may only produce subtle or "cryptic" phenotypes in vitro [44] [45].
- Phenotype Expansion: Move beyond simple motility reduction. Investigate other endpoints like oscillation frequency, movement speed, or changes in movement patterns (e.g., from sinusoidal to hyperactive/paralytic) [46]. High-content imaging combined with machine learning can analyze these complex phenotypes [44] [45].
- Assay Modification: Consider co-culturing parasites with host immune cells (e.g., neutrophils or peripheral blood mononuclear cells) to make the environment more "in vivo like." Drugs like ivermectin and diethylcarbamazine show enhanced activity in the presence of immune cells [44].
- Life Stage Consideration: Test the compound on different life stages (L3 larvae, adults) as sensitivity can vary significantly [41] [42].
Q3: How can we distinguish between a true resistance profile and a false positive caused by poor worm health in our resistance diagnosis assay?
A: Robust internal controls are essential.
- Control Strains: Always include known drug-susceptible and drug-resistant parasite isolates in parallel. The assay should clearly differentiate their motility responses, as demonstrated with Haemonchus contortus strains [41] [43].
- Viability Control: Include a vehicle control (e.g., DMSO) to confirm baseline parasite motility and health throughout the assay duration.
- Reference Drug: Use a reference anthelmintic with a well-defined mechanism of action. A significant shift in the ICâ‚…â‚€ value of the reference drug in your test isolate, compared to a susceptible one, indicates resistance [43].
Q4: Our high-throughput screen of a large compound library identified hits that paralyze worms, but we are concerned these may not translate to in vivo efficacy. How can we prioritize hits?
A: This is a common challenge. Prioritization should be based on a multi-parameter approach.
- Phenotypic Profiling: Use high-content imaging to determine if the paralysis is accompanied by other damaging effects, such as tegument disruption, which is a stronger indicator of irreparable damage [45].
- Chemical Properties: Filter hits based on novelty, pharmacokinetic properties (Cmax, T1/2), and cytotoxicity in mammalian cells [18].
- Secondary Assays: Subject hits to more physiologically relevant secondary assays, such as larval migration or development assays, to confirm efficacy [44].
Experimental Protocols for Key Applications
Protocol 1: Motility-Based Drug Screening on Larval Nematodes
This protocol is adapted for use with the WMicrotracker (WMA) system and third-stage larvae (L3) [43].
1. Reagent Preparation:
- Compound Plates: Prepare a dilution series of test compounds in DMSO in 96- or 384-well plates. The final DMSO concentration in the assay should not exceed 1% [43].
- Assay Buffer: Use an appropriate buffer, such as 0.5x PBS or culture medium, depending on the parasite species [41].
2. Parasite Preparation:
- Source: Harvest H. contortus L3 larvae from fecal cultures using standard migration techniques [41] [42].
- Concentration: Adjust the larval suspension to a density of approximately 3,000 L3 per 200 µL of assay buffer [41].
3. Assay Execution:
- Dispensing: Transfer 180 µL of the larval suspension to each well of the assay plate.
- Baseline Reading: Place the plate in the WMicrotracker and record baseline motility for 1-2 hours.
- Drug Addition: Add 20 µL of the 10x concentrated drug solution (or DMSO control) to the respective wells.
- Data Acquisition: Monitor and record motility continuously for 24-72 hours. The instrument automatically quantifies movement as a Cell Index or arbitrary motility units [43].
4. Data Analysis:
- Normalize motility data to the pre-drug baseline.
- Generate dose-response curves and calculate half-maximal inhibitory concentration (ICâ‚…â‚€) values using non-linear regression analysis.
Protocol 2: Phenotypic Resistance Diagnosis in Field Isolates
This protocol allows for the detection of macrocyclic lactone (ML) resistance in nematodes like H. contortus [43].
1. Isolate Collection:
- Collect eggs from sheep feces from both a farm with suspected resistance (based on FECRT) and a farm with known drug efficacy [43].
- Harvest L3 larvae from these eggs through standard laboratory culture.
2. Motility Assay:
- Follow the drug screening protocol (Protocol 1) using a dilution series of ML drugs (e.g., ivermectin, moxidectin, eprinomectin).
- Test the susceptible and suspected resistant isolates on the same plate to ensure direct comparability.
3. Analysis and Interpretation:
- Calculate the ICâ‚…â‚€ for each drug-isolate combination.
- Determine the Resistance Factor (RF) using the formula:
RF = ICâ‚…â‚€ (field isolate) / ICâ‚…â‚€ (susceptible isolate). - An RF significantly greater than 1 indicates a resistant phenotype. The WMA has successfully discriminated isolates with a 2.12-fold reduction in ivermectin sensitivity [43].
Table 1: Instrument Comparison for Real-Time Motility Monitoring
| Instrument / Platform | Technology Principle | Key Applications | Throughput | Reported Parasite Models |
|---|---|---|---|---|
| xCELLigence (RTCA) | Measures electrical impedance changes caused by parasite movement on microelectrodes [41] [42] | Drug screening, ICâ‚…â‚€ determination, resistance diagnosis [41] [42] | High (96-well plate format) [41] | H. contortus L3, S. ratti L3, adult hookworms, adult S. mansoni [41] [42] |
| WMicrotracker (WMA) | Uses infrared light to detect interruptions in a beam grid caused by moving organisms [43] | Drug screening, resistance detection, high-throughput compound library screening [43] | High (96- and 384-well compatible) [43] | C. elegans, H. contortus L3 [43] |
| Lensless Holographic Imaging | Records time-varying holographic speckle patterns; analyzes motion via computational algorithms [47] | Sensitive detection of motile pathogens in bodily fluids (e.g., blood, CSF) for diagnosis [47] | Medium (screens ~3.2 mL in 20 min) [47] | Trypanosoma brucei, T. cruzi, T. vaginalis [47] |
Table 2: Exemplar Motility-Based Drug Response Data
| Parasite / Strain | Drug | Reported ICâ‚…â‚€ (nM) | Resistance Factor (RF) | Context & Notes |
|---|---|---|---|---|
| C. elegans (IVR10) | Ivermectin | Not specified | 2.12 | IVM-selected strain vs. wild-type N2B [43] |
| H. contortus (Susceptible) | Moxidectin | Most potent among MLs | - | Compared to IVM and EPR; highest efficacy observed [43] |
| H. contortus (Resistant) | Eprinomectin | Significant increase | Substantial RF | Isolate from a farm with EPR-treatment failure [43] |
Experimental Workflow Visualization
Workflow for Motility-Based Screening
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials
| Reagent / Material | Function / Application | Example Usage in Context |
|---|---|---|
| xCELLigence RTCA E-Plate | Specialized microtiter plate with integrated gold microelectrodes for label-free, real-time monitoring of parasite motility via electrical impedance [41] [42]. | Used for screening against larval and adult stages of helminths like H. contortus and S. mansoni [41] [42]. |
| WMicrotracker Assay Plates | Microplates designed for use with the WMicrotracker system, which uses infrared light beams to detect organism movement in a high-throughput format [43]. | Employed for high-throughput drug screening on C. elegans and H. contortus L3, and for assessing macrocyclic lactone resistance [43]. |
| Synchronized Parasite Cultures | Populations of parasites (eggs, larvae, adults) at the same developmental stage, crucial for obtaining consistent and reproducible drug response data [41] [43]. | Larvae are hatched and synchronized from eggs isolated from feces for assays; adult worms are harvested from infected hosts [41] [43]. |
| Reference Anthelmintic Drugs | Pharmacopeial-standard compounds (e.g., Ivermectin, Moxidectin, Praziquantel) used as positive controls to validate assay performance and for comparative resistance profiling [41] [43]. | Used to generate standard dose-response curves and to calculate Resistance Factors (RF) for field isolates [43]. |
| Drug-Resistant Parasite Strains | Genetically defined or field-derived parasite isolates with confirmed resistance to specific anthelmintic classes, serving as essential controls for resistance diagnosis assays [41] [43]. | Strains like H. contortus Wallangra (multi-resistant) and C. elegans IVR10 (IVM-selected) are used to optimize and validate resistance detection [41] [43]. |
| Myt1-IN-4 | Myt1-IN-4|Potent MYT1 Kinase Inhibitor|RUO | Myt1-IN-4 is a potent MYT1 kinase inhibitor for cancer research. It abrogates the G2/M cell cycle checkpoint. This product is For Research Use Only. Not for diagnostic or therapeutic use. |
| SOS1 Ligand intermediate-3 | SOS1 Ligand intermediate-3, MF:C24H27F3N4O2, MW:460.5 g/mol | Chemical Reagent |
Next-Generation Sequencing for High-Throughput Antimalarial Resistance Profiling
The emergence and spread of Plasmodium falciparum resistance to antimalarial drugs represents a critical challenge to global malaria elimination efforts. Next-generation sequencing (NGS) has revolutionized antimalarial resistance profiling by enabling high-throughput, cost-effective surveillance of parasite populations. This technical support center provides comprehensive troubleshooting guides and FAQs to assist researchers in implementing NGS-based resistance profiling methodologies within their laboratories, supporting the broader application of high-throughput parasite screening in malaria research and drug development.
Frequently Asked Questions (FAQs)
1. What are the key genetic markers for antimalarial drug resistance in P. falciparum?
Multiple genes harbor polymorphisms associated with resistance to various antimalarial drugs. The primary targets include:
- Pfcrt: Mutations associated with chloroquine resistance [48] [49]
- Pfmdr1: Involved in resistance to multiple drugs, including lumefantrine and mefloquine [48] [50]
- Pfdhfr: Mutations conferring resistance to pyrimethamine [48] [49]
- Pfdhps: Mutations associated with sulfadoxine resistance [48] [49]
- Pfk13: Mutations in the propeller domain linked to artemisinin delayed clearance [48] [50] [49]
2. What is the typical workflow for NGS-based resistance profiling?
The standard methodology involves a multi-step process [50] [49]:
- DNA Extraction: Isolate parasite DNA from patient blood samples.
- Multiplex PCR: Amplify target genes of interest simultaneously.
- Library Preparation: Incorporate custom dual indices for sample multiplexing.
- Next-Generation Sequencing: Process pooled libraries on platforms such as Illumina MiSeq or Ion Torrent.
- Bioinformatic Analysis: Map sequences, call variants, and determine haplotypes.
3. Our study encountered low sequencing coverage in several amplicons. What could be the cause?
Inconsistent coverage can result from several factors:
- PCR Amplification Bias: Primer mismatches due to genetic diversity can reduce amplification efficiency [50].
- DNA Quality/Quantity: Degraded or low-concentration template DNA yields poor results [49].
- Multiplexing Imbalance: Unequal pooling of libraries before sequencing can lead to variable depth across samples [50].
- Solution: Redesign primers for problematic regions, quantify DNA accurately using fluorometry, and optimize library normalization procedures.
4. How can we distinguish true low-frequency mutations from sequencing errors?
Accurate detection of minor variants requires:
- High Sequencing Depth: Aim for a minimum of 1,000-2,000 reads per position for reliable base calling [50].
- Bioinformatic Filtering: Implement quality score thresholds (e.g., Q≥30) and statistical significance testing (e.g., p-value < 0.05) for base calls [50].
- Replication: Confirm low-frequency mutations by repeating PCR and sequencing for the specific sample [49].
5. What controls should be included in each sequencing run?
Essential controls ensure data reliability:
- Negative Controls: DNA-free water controls to detect contamination during PCR and library prep [50].
- Positive Controls: Reference DNA samples with known haplotypes to verify assay performance [49].
- Positive Controls: Reference DNA samples with known haplotypes to verify assay performance [49].
Troubleshooting Guides
Problem 1: Poor Sample Representation After Multiplexing
Symptoms: Significant loss of specific samples after sequencing; inadequate read counts for particular index combinations.
Potential Causes and Solutions:
| Cause | Solution |
|---|---|
| Incomplete PCR amplification | Verify primer specificity and optimize PCR conditions. Use high-fidelity polymerases [49]. |
| Library quantification errors | Re-quantify libraries using fluorometric methods (e.g., Qubit) instead of spectrophotometry for accurate pooling [50]. |
| Index hopping or misassignment | Employ unique dual indexing strategies to minimize cross-talk between samples [50]. |
Problem 2: Inconsistent Base Calling Across SNP Positions
Symptoms: Low confidence in genotype calls at specific resistance-associated positions; high rates of "mixed" base calls.
Potential Causes and Solutions:
| Cause | Solution |
|---|---|
| Low sequence quality | Trim low-quality bases from read ends. Increase sequencing depth for problematic regions [50]. |
| Genuine mixed infections | In high-transmission areas, multiple clone infections are common. Establish a minimum threshold (e.g., 75% allele frequency) for calling dominant haplotypes [50] [49]. |
| Parasite genetic diversity | Validate primer binding sites in the target population to ensure they are not located in highly variable regions [49]. |
Problem 3: Failure to Detect Artemisinin Resistance Markers
Symptoms: Absence of validated PfK13 mutations despite clinical suspicion of resistance.
Potential Causes and Solutions:
| Cause | Solution |
|---|---|
| Limited PfK13 diversity | Sequence the entire PfK13 gene, not just common SNPs, to identify novel or region-specific mutations [48] [49]. |
| Emerging/unknown mechanisms | Acknowledge that artemisinin resistance may involve PfK13-independent pathways; consider investigating other genomic regions [49]. |
| Low parasite density | Enrich parasite DNA or use whole genome amplification prior to PCR for low-parasitemia samples [49]. |
Experimental Protocols & Data Presentation
Key NGS-Based Resistance Profiling Protocol
This protocol for targeted amplicon sequencing of P. falciparum drug resistance genes is adapted from established methodologies [50] [49].
Step 1: DNA Extraction and Qualification
- Extract genomic DNA from 100-200 μL of whole blood or filter paper spots using commercial kits (e.g., QIAamp DNA Blood Mini Kit).
- Quantify DNA using a fluorometer. While a nanodrop can be used for a quick check, fluorometry is more accurate for low-concentration samples.
- Assess DNA quality via gel electrophoresis or bioanalyzer to ensure high molecular weight and lack of degradation.
Step 2: Multiplex PCR Amplification
- Design primers to amplify fragments covering key resistance loci in pfcrt, pfmdr1, pfdhfr, pfdhps, and the entire pfk13 gene.
- Perform multiplex PCRs using 10-50 ng of genomic DNA in a 25 μL reaction volume.
- Use thermocycling conditions appropriate for your primer set and polymerase. Typically, this includes an initial denaturation (95°C for 3-5 min), followed by 30-40 cycles of denaturation (95°C for 30 s), annealing (55-60°C for 30 s), and extension (72°C for 1 min/kb), with a final extension (72°C for 5-10 min).
- Include negative controls (no-template) and positive controls (known genotype) in each run.
Step 3: Library Preparation and Indexing
- Clean up PCR products using bead-based purification (e.g., AMPure XP beads).
- Attach unique dual indices to each sample in a second, limited-cycle PCR reaction. This allows for high-level multiplexing.
- Purify the final indexed libraries and quantify them.
Step 4: Library Pooling and Sequencing
- Pool libraries in equimolar amounts based on quantification.
- Sequence the pooled library on an Illumina MiSeq or Ion Torrent platform, aiming for a minimum coverage of 1,000x per amplicon.
Step 5: Bioinformatic Analysis
- Demultiplex samples based on their unique dual indices.
- Trim adapters and low-quality bases.
- Map reads to a reference genome (e.g., 3D7).
- Call variants and determine haplotypes for each resistance gene.
Quantitative Profiling Data
Table 1: Representative Antimalarial Drug Resistance Profiles from Geographic Surveillance Studies
| Study Location | Sample Size | Primary Drug | Key Gene | Resistance Mutation Prevalence | Reference |
|---|---|---|---|---|---|
| Rourkela, India | 158 isolates | Chloroquine | pfcrt | High proportion of wild-type haplotype observed [49] | |
| Chennai & Nadiad, India | 158 isolates | Chloroquine | pfcrt | Mutant haplotypes were fixed [49] | |
| Guinea-Bissau | 457 infections | Artemisinin | pfk13 | Validated resistance-conferring SNPs absent [50] | |
| Multiple sites, India | 158 isolates | Sulfadoxine | pfdhps | Wild-type haplotype predominant [48] [49] |
Table 2: Performance Metrics of a High-Throughput NGS Resistance Profiling Method
| Metric | Result | Technical Notes |
|---|---|---|
| Average Read Depth | 2,043 reads per position [50] | Enables confident detection of minor variants. |
| Sample Throughput | 457 samples per run [50] | Custom dual indexing facilitates high-level multiplexing. |
| Base Calling Success Rate | 89.8-100% of samples [50] | Bases called with p-value < 0.05. |
| Cost per Sample | ~$10 USD [50] | Makes large-scale surveillance affordable. |
| Amplicon Representation | 98.1-100% [50] | Presence of sequences for a specific amplicon across samples. |
Workflow Visualization
NGS Workflow for Antimalarial Resistance Profiling
Troubleshooting Low Coverage
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for NGS-Based Resistance Profiling
| Reagent/Material | Function | Example Product/Note |
|---|---|---|
| DNA Extraction Kit | Isolate high-quality parasite genomic DNA from clinical samples. | QIAamp DNA Blood Mini/Midi Kit [49] |
| Target-Specific Primers | Amplify regions of interest in resistance-associated genes. | Designed to cover full length of pfk13, key codons in pfcrt, pfmdr1, etc. [50] [49] |
| High-Fidelity Polymerase | Perform accurate PCR amplification with minimal errors. | Essential for generating high-quality pre-sequencing amplicons. |
| Dual Indexed Adapters | Uniquely tag individual samples for multiplexing. | Custom indexes allow for pooling hundreds of samples in one run [50] |
| Size Selection Beads | Clean up PCR products and select optimal fragment sizes. | AMPure XP beads are commonly used for library purification. |
| Sequencing Platform | Generate millions of parallel sequences. | Illumina MiSeq, Ion Torrent [50] [49] |
| Tyrosinase-IN-19 | Tyrosinase-IN-19, MF:C20H20N2O5S, MW:400.4 g/mol | Chemical Reagent |
Comparative Stool Concentration Methods for Intestinal Protozoa and Helminth Detection
Intestinal parasitic infections, caused by protozoa and helminths, remain a significant global health burden, affecting billions of people worldwide. Accurate diagnosis is crucial for effective treatment, control, and eradication programs. Despite advances in molecular technology, microscopic examination of stool specimens remains the cornerstone of parasitic diagnosis in many clinical and research settings, particularly in resource-limited areas. This technical guide provides a comprehensive comparison of stool concentration techniques, framing them within modern high-throughput screening methodologies to support researchers and scientists in selecting and optimizing diagnostic approaches.
Technical Comparison of Major Concentration Methods
The following table summarizes the performance characteristics of different stool concentration techniques as reported in recent comparative studies:
Table 1: Performance comparison of stool concentration methods for parasite detection
| Method | Reported Detection Rate | Key Advantages | Key Limitations | Best Applications |
|---|---|---|---|---|
| Formalin-Ethyl Acetate Concentration (FAC) | 75% [51] | Higher recovery rate, safety, feasibility in rural settings [51] | Requires centrifugation | Routine parasitological diagnosis |
| Formalin-Ether Concentration (FEC) | 62% [51] | Widely standardized, good recovery | Ether flammability concern [51] | General parasite screening |
| ParaFlo Commercial Kits | 69-75% concordance with in-house [52] | Ready-to-use, standardized reagents, improved traceability [52] | Significant morphological changes to protozoa cysts [52] | Labs seeking standardization |
| Direct Wet Mount | 41% [51] | Rapid, low cost, minimal equipment | Low sensitivity due to small sample volume [16] | Initial rapid assessment |
| MIFC (Merthiolate-Iodine-Formaldehyde) | Superior diagnostic yield in older studies [53] | Comprehensive for both protozoa and helminths | Requires multiple reagents | Comprehensive parasite surveys |
Table 2: Organism-specific detection performance across methods
| Parasite | FAC Performance | FEC Performance | ParaFlo Performance | Molecular Methods |
|---|---|---|---|---|
| Giardia duodenalis | 16% detection rate [51] | 18% detection rate [51] | Lower than in-house methods [52] | High sensitivity and specificity [54] |
| Entamoeba histolytica | 24% detection rate [51] | 26% detection rate [51] | Variable detection [52] | Essential for species differentiation [54] |
| Blastocystis hominis | 15% detection rate [51] | 15% detection rate [51] | Poor detection [52] | Not consistently targeted |
| Soil-transmitted helminths | Good recovery [51] | Good recovery [51] | Comparable to in-house [52] | High sensitivity (10.1% vs 9.6% sedimentation) [55] |
| Cryptosporidium spp. | Not specified | Not specified | Detected [52] | Affected by DNA extraction efficiency [54] |
Experimental Protocols for Key Methods
Formalin-Ethyl Acetate Concentration (FAC) Technique
Principle: Utilizes formalin to fix parasites and ethyl acetate to dissolve fats and remove debris.
Procedure:
- Emulsify approximately 1g of stool in 7mL of 10% formol saline
- Fix for 10 minutes, then strain through three folds of gauze
- Mix filtrate with 3mL of ethyl acetate
- Centrifuge at 1500 rpm for 5 minutes
- Discard supernatant and examine sediment microscopically [51]
Quality Control: Check for proper layer formation after centrifugation. The protocol should yield four distinct layers: ethyl acetate, debris, formalin, and sediment.
Formalin-Ether Concentration Technique
Principle: Similar to FAC but uses diethyl ether as the organic solvent.
Procedure:
- Mix 1g stool with 7mL of 10% formol water in a conical centrifuge tube
- Filter suspension through a sieve into a 15mL conical tube
- Add 4mL diethyl ether to formalin solution
- Centrifuge at 300 rpm for 1 minute
- Discard supernatant, prepare smear from sediment [51]
Safety Note: Ether is highly flammable; perform in well-ventilated areas away from ignition sources.
Commercial ParaFlo Concentration Protocol
Procedure for ParaFlo DC:
- Suspend 4g stool in device pre-filled with 25mL merthiolate-formalin
- Add 200µL iodinated Lugol solution, homogenize gently
- Let stand for 3 minutes
- Transfer 5mL to conical tube, add 2.5mL ether
- Agitate and centrifuge at 200× g for 5 minutes
- Discard supernatant, resuspend pellet in 0.9% NaCl for examination [52]
High-Throughput and Automated Approaches
Automated Digital Feces Analysis
The Orienter Model FA280 represents technological advancement in parasite detection:
Workflow:
- Automatic sample loading with track-type carrier
- Pneumatic mixing system for homogenization
- High-resolution imaging of sample characteristics
- Automated microscopy with multifield tomography
- AI-based image analysis with optional user audit [16]
Performance: Shows perfect agreement with FECT for species identification when combined with user audit (κ = 1.00), though sensitivity remains lower than conventional FECT due to smaller sample size (0.5g vs 2g) [16].
Phenotypic Screening Platforms
For drug discovery applications, high-throughput systems like INVAPP/Paragon enable automated screening:
Capabilities:
- Quantifies nematode motility and growth
- Throughput of approximately 100 96-well plates per hour
- Uses movement scoring algorithm based on pixel variance [56]
Applications: Validated for screening compound libraries against model and parasitic nematodes, identifying novel anthelmintic chemotypes including benzoxaborole and isoxazole compounds [56].
Research Reagent Solutions
Table 3: Essential reagents and materials for stool concentration methods
| Reagent/Material | Function | Application Notes |
|---|---|---|
| 10% Formalin Solution | Parasite fixation and preservation | Maintains morphology but may affect DNA quality [54] |
| Ethyl Acetate | Organic solvent for debris extraction | Less flammable than ether [51] |
| Diethyl Ether | Organic solvent for lipid removal | Higher flammability risk [51] |
| Lugol's Iodine Solution | Staining agent for enhanced visualization | Differentiates internal structures of protozoa [52] |
| Merthiolate-Formalin (MIF) | Fixative and preservative | Used in diphasic concentration methods [52] |
| S.T.A.R. Buffer | Stool transport and DNA preservation | Optimized for molecular applications [54] |
| Para-Pak Preservation Media | Comprehensive stool preservation | Maintains parasites for both microscopy and molecular testing [54] |
Troubleshooting Guide: Frequently Asked Questions
Q: Our laboratory is experiencing low protozoa detection rates with concentration methods. What could be the issue?
A: Several factors can affect protozoa detection:
- Morphological changes: Some commercial methods like ParaFlo cause significant morphological alterations to protozoa cysts, hindering identification [52]
- Fixation time: Inadequate fixation can lead to degradation of delicate trophozoites
- Centrifugation speed: Excessive speed may distort protozoa; follow established protocols (typically 500-1500× g)
- Solution pH: Suboptimal pH can affect parasite morphology
Q: Which concentration method provides the highest sensitivity for routine diagnosis?
A: Recent comparative studies indicate that the Formalin-Ethyl Acetate Concentration (FAC) technique demonstrates superior detection rates (75%) compared to Formalin-Ether Concentration (FEC at 62%) and direct wet mount (41%) [51]. FAC provides an optimal balance of sensitivity, safety, and feasibility for rural or resource-limited settings.
Q: How do commercial concentration kits compare to traditional in-house methods?
A: Commercial kits like ParaFlo offer advantages in standardization and ease of use but may have limitations:
- Concordance with in-house methods ranges from 69-75% [52]
- Perform comparably for helminth detection but may underperform for protozoa compared to some in-house methods [52]
- Reduce technical variability but at higher cost per test
Q: When should molecular methods complement conventional concentration techniques?
A: Molecular methods are particularly valuable when:
- Differentiating pathogenic and non-pathogenic species (e.g., E. histolytica vs E. dispar) [54]
- Confirming low-level infections missed by microscopy
- Processing large sample volumes in high-throughput research
- Real-time PCR detected 10.1% of STH infections compared to 9.6% by sedimentation concentration in one study [55]
Q: What is the role of automated systems in high-throughput parasite screening?
A: Automated systems like the FA280 analyzer offer:
- Significant time savings (40 samples in ~30 minutes) [16]
- Reduced operator exposure to infectious material
- Digital archiving of samples for re-evaluation
- However, they currently have higher per-test costs and may have lower sensitivity than conventional FECT due to smaller sample volumes [16]
Method Selection Workflow
The following diagram illustrates a systematic approach to selecting appropriate detection methods based on research objectives:
The optimal stool concentration method for intestinal protozoa and helminth detection depends on the specific research context, available resources, and detection priorities. While FAC demonstrates superior sensitivity for conventional microscopy, automated systems offer advantages for high-throughput applications. Molecular methods provide crucial species differentiation capabilities but require specialized infrastructure. Researchers should consider implementing a tiered approach, combining methods to leverage their complementary strengths for comprehensive parasite detection in the context of high-throughput screening methodologies.
Optimizing HTS Assays: Troubleshooting Technical Challenges for Robust Performance
Understanding and Calculating Key Assay Quality Metrics
What are Z' Factor and Coefficient of Variation (CV), and why are they critical for High-Throughput Screening (HTS)?
In high-throughput screening, particularly in parasite drug discovery, the Z' factor and Coefficient of Variation (CV) are fundamental statistical parameters used to validate the quality and robustness of an assay before it is used to screen large compound libraries.
- Z' Factor: This is a dimensionless metric that quantifies the separation band between the positive and negative control signals, taking into account both the dynamic range of the assay and the data variation [57]. It is calculated using only control data (no test samples) and is defined during assay development and validation [57].
- Coefficient of Variation (CV): This metric represents the ratio of the standard deviation to the mean, expressed as a percentage. It is a measure of the precision or variability within your control groups [58]. A lower CV indicates greater consistency and less scatter in the data.
The following table summarizes their roles:
Table 1: Key Assay Quality Metrics
| Metric | Definition | Data Used | Purpose | Ideal Value | ||
|---|---|---|---|---|---|---|
| Z' Factor | ( Z' = 1 - \frac{3(\sigmap + \sigman)}{ | \mup - \mun | } ) Where ( \sigma ) = standard deviation and ( \mu ) = mean of positive (p) and negative (n) controls [59] | Positive and negative controls only [57] | Assess the quality and separation band of the assay itself during validation [57] | > 0.5 (Excellent) [60] |
| CV | ( CV = \frac{\sigma}{\mu} \times 100\% ) Where ( \sigma ) = standard deviation and ( \mu ) = mean | Replicate measurements of a single control | Measure the precision and variability within a control group [58] | < 10% (Excellent) [58] |
How do I calculate the Z' factor for my assay?
The Z' factor is calculated using the following equation, derived from the means and standard deviations of your positive and negative controls [59] [57]:
Formula: [ Z' = 1 - \frac{3(\sigmap + \sigman)}{|\mup - \mun|} ]
Where:
- ( \sigma_p ) = standard deviation of the positive control
- ( \sigma_n ) = standard deviation of the negative control
- ( \mu_p ) = mean of the positive control
- ( \mu_n ) = mean of the negative control
Interpretation of Z' Factor Values [60]:
- 1.0: An ideal assay (theoretically approached with a huge dynamic range and tiny standard deviations).
- 0.5 to 1.0: An excellent assay suitable for HTS.
- 0 to 0.5: A marginal or "yes/no" type assay. It may still be useful, but requires careful interpretation.
- < 0: The signals from the positive and negative controls overlap, making the assay unsuitable for screening.
Experimental Protocol for Assay Validation
A rigorous, multi-day assay validation is crucial to ensure your assay is robust and reproducible before committing to a full high-throughput screen [58].
Procedure:
- Assay Design: Perform the assay validation over three different days to account for inter-day variability.
- Plate Layout: On each day, run three assay plates. Each plate should contain a minimum of 16 replicates each of "high" (positive control), "low" (negative control), and "medium" (e.g., ECâ‚…â‚€ concentration of a control compound) signal controls.
- Interleaved Sample Distribution: To identify positional effects (e.g., edge effects, drift), distribute the "high," "medium," and "low" controls in different column-wise orders across the three plates [58]:
- Plate 1: "high-medium-low"
- Plate 2: "low-high-medium"
- Plate 3: "medium-low-high"
- Data Analysis: For each of the nine plates, calculate the Z' factor and the CV for all control groups.
Acceptance Criteria [58]:
- CV: The CV for the "high," "medium," and "low" raw signals should be < 20% in all plates.
- Z' Factor: The Z' factor should be > 0.4 in all plates. While >0.5 is an excellent target, a Z' > 0.4 can be acceptable for many screens, especially more variable cell-based assays [59] [58].
Troubleshooting Guides and FAQs
My Z' factor is below 0.5. What should I do?
A low Z' factor can result from a small dynamic range between controls or high variability. The requirement for Z' > 0.5, while ideal, should not be an absolute barrier for essential assays, such as phenotypic screens for parasites which are inherently more variable [59] [57]. A more nuanced approach is recommended.
- Investigate the Cause:
- Small Dynamic Range (( |\mup - \mun| )): Optimize the concentration of your controls. For example, in a binding assay, using an excessively high concentration of activator may prevent finding competitive antagonists [59].
- High Variability (( \sigmap + \sigman )): Review your technical procedures. Common sources include inconsistent cell seeding, reagent dispensing, temperature fluctuations, or inadequate mixing.
- Potential Solutions:
- Re-optimize the concentration of key reagents (e.g., substrate, co-factors, cell density).
- Ensure all liquid handling equipment is properly calibrated and maintained.
- Use fresh reagent preparations and consistent cell passage numbers.
- If the Z' factor remains low but is justified by the biological importance of the target, you can proceed by carefully setting an appropriate activity threshold to manage the trade-off between finding true hits and accepting false positives [59].
The CV of my controls is consistently above 10%. How can I improve precision?
A high CV indicates poor precision within your replicates.
- Check for Contamination: Contamination of kit reagents, especially with concentrated sources of the analyte (e.g., cell culture media, sera), can cause high background and poor duplicate precision [61]. Clean all work surfaces and equipment, use aerosol barrier pipette tips, and do not talk or breathe over uncovered microplates.
- Review the Washing Procedure: In plate-based assays (e.g., ELISA), incomplete or overly aggressive washing can result in high and variable background [61]. Follow the recommended washing technique precisely, and do not allow wash solution to soak in wells for extended periods.
- Verify Reagent Stability and Pipetting: Ensure all reagents are stable and at the correct temperature before use. Check that pipettes are accurately calibrated for the volumes being dispensed.
- Inspect for Edge Effects: Evaporation in edge wells can cause higher variability. Use a plate sealer or perform assays in a humidified incubator.
My assay suffers from high background (non-specific binding). What are the common fixes?
- Identify the Source: High background is often due to contamination or non-specific binding of detection antibodies [61].
- Troubleshooting Steps:
- Confirm Reagent Purity: Ensure your detection antibodies are specific and at the optimal dilution.
- Use a Blocking Agent: Incorporate a suitable blocking protein (e.g., BSA) to minimize non-specific binding.
- Optimize Wash Stringency: Add a mild detergent (e.g., Tween-20) to your wash buffer to reduce non-specific binding, but ensure it does not interfere with specific binding.
- Avoid Contamination: As above, strictly separate areas where concentrated analytes are handled from where the sensitive assay is performed [61].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Robust HTS Assays
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Cell Lines (e.g., Plasmodium falciparum) [18] | Provides the biological system for phenotypic or target-based screening. | Maintain consistent culture conditions, passage number, and synchronization protocols (e.g., sorbitol) to ensure reproducibility [18]. |
| Validated Positive/Negative Controls | Defines the dynamic range and allows for Z' calculation. | Select controls that are biologically relevant and provide a strong, consistent signal. Avoid unrealistically strong controls [59]. |
| Assay-Specific Diluents [61] | Dilutes samples to within the analytical range of the assay. | Use the diluent recommended by the kit manufacturer or a validated buffer to avoid matrix effects and adsorptive losses of analyte. |
| Stable Detection Reagents (e.g., Fluorescent dyes, HTRF reagents) [57] [18] | Generates the measurable signal for the assay readout. | Protect from light, ensure stability, and use consistent lot numbers. For fluorescence, use readers with high sensitivity and low noise [57]. |
| Microplate Readers [57] | Measures the assay endpoint signal. | Choose a reader with high sensitivity, low noise, and consistent performance across wells. For HTS, integration with automation is key. |
In high-throughput parasite screening, the integrity of experimental data is paramount. Automated liquid handling systems are indispensable in these workflows, enabling the rapid testing of vast compound libraries, as demonstrated in screens against pathogens like Plasmodium falciparum and Entamoeba histolytica [62] [63]. However, artifacts such as bubble formation and dispensing variability introduce significant inaccuracies, leading to false positives or negatives that can compromise drug discovery efforts. This guide provides targeted troubleshooting strategies to overcome these specific challenges, ensuring the reliability and reproducibility of your screening data.
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: Why do bubbles form in my liquid handler, and how can I prevent them? Bubbles often form due to the specific pipetting technology and liquid characteristics. For air displacement liquid handlers (common in fixed- and changeable-tip systems), bubbles can result from leaks in air lines or an incorrect fit between the liquid and the pipetting technology [11]. For positive displacement systems, bubbles can be introduced if the tubing is not flushed sufficiently before use [11].
- Solutions:
- Pre-wet Tips: Sufficiently pre-wetting tips before aspiration can minimize bubble formation by conditioning the interior surface [11].
- Adjust Aspirate/Dispense Speed: Slowing down the pipetting speed can reduce turbulence and bubble introduction, especially with viscous liquids [11].
- Check for Leaks: Regularly maintain system pumps and fluid lines to ensure a tight seal and prevent air leaks [11] [64].
- Flush Lines: For positive displacement systems, ensure lines are flushed adequately to remove any trapped air [11].
Q2: My dispensed volumes are inconsistent. What are the primary sources of this variability? Dispensing variability stems from multiple factors, including the liquid handler type, liquid properties, and instrument maintenance.
- Mechanical Issues: A leaky piston or cylinder in air displacement systems can lead to incorrect aspirated volumes [11]. Worn seals can also cause under-dispensing [64].
- Liquid Properties: Liquids with viscosity or vapor pressure significantly different from water can behave unpredictably, leading to hanging droplets, trailing liquid, or diluted samples [11].
- Tip and Tip Seals: Using a new lot of tips or tips that do not form a proper seal with the channel can cause random under-dispensing [64].
- Environmental Factors: Laboratory temperature and humidity can affect pipetting results, though typically to a lesser degree than mechanical issues [64].
Q3: How can I verify that my liquid handler is dispensing volumes accurately? Implementing a routine volume verification protocol is crucial for quality control. The methods can be broadly divided into reference and real-time techniques [64].
- Reference Methods: These provide a static check of performance.
- Gravimetric: Weighing dispensed water on a precision balance. This method is highly accurate but destructive and time-consuming [64].
- Photometric: Using dyes (e.g., Tartrazine measured at 472nm) in a plate reader to assess precision. This is a cheap and easy solution but does not measure accuracy well [64].
- Capillary Measurement: Optical image analysis of liquid-filled capillaries (e.g., VeriPlate) [64].
- Real-Time, In-Line Solutions: These measure your actual samples during the process.
- Acoustic Measurement: Uses sound waves to measure volume in the destination plate [64].
- Drop Detection: Some non-contact dispensers, like the I.DOT Liquid Handler, have in-built technology to verify that a drop was successfully dispensed [65].
- Optical Interferometry: A newer technology (e.g., VolumeSense) that provides high-resolution, non-contact volume measurement in-line with your method [64].
The table below summarizes the best practices for addressing specific liquid handling errors.
Table 1: Troubleshooting Common Liquid Handling Errors
| Observed Error | Possible Source of Error | Recommended Solutions |
|---|---|---|
| Dripping tip or drop hanging from tip | Difference in vapor pressure of sample vs. water [11] | Sufficiently prewet tips; Add an air gap after aspirate [11]. |
| Droplets or trailing liquid during delivery | Liquid viscosity different from water [11] | Adjust aspirate/dispense speed; Add air gaps and blow-outs [11]. |
| Incorrect aspirated volume | Leaky piston/cylinder [11] | Regular maintenance of system pumps and fluid lines [11] [64]. |
| Diluted sample with each transfer | System liquid is in contact with the sample [11] | Adjust the leading air gap [11]. |
| First/last dispense volume difference | Inherent to sequential dispense method [11] | Dispense the first and/or last quantity into a waste reservoir [11]. |
Experimental Protocols for Verification
Protocol 1: Gravimetric Volume Verification
This is a foundational method for verifying the accuracy and precision of your liquid handler's volume delivery [64].
- Materials: Precision balance (e.g., Mettler Toledo XL20), low-evaporation microtubes (e.g., Matrix), high-purity deionized (DI) water.
- Procedure:
- Place the balance in a stable location, away from vibrations and drafts. Allow it to warm up sufficiently for accuracy.
- Tare the weight of an empty microtube.
- Program your liquid handler to dispense the target volume (e.g., 10 µL) of DI water directly into the tube.
- Weigh the tube again and record the mass.
- Repeat this process for multiple channels and tips (e.g., n=16 or 32) to gather statistically significant data.
- Data Analysis:
- Convert the mass of the dispensed water to volume (1 µL DI water = 1 mg at standard conditions).
- Calculate the average volume (accuracy) and the coefficient of variation or standard deviation (precision).
- Compare results to your predefined acceptance criteria (e.g., ±5% accuracy, <5% CV). Investigate any out-of-specification results.
Protocol 2: Photometric Verification with Tartrazine
This method is excellent for quickly assessing precision across a full microplate [64].
- Materials: Tartrazine dye solution, UV-transparent microplate, microplate reader.
- Procedure:
- Prepare a homogeneous solution of Tartrazine.
- Use the liquid handler to dispense the dye into the wells of a microplate.
- Read the absorbance of the plate at 472 nm.
- Data Analysis:
- High variability in the absorbance readings across the plate indicates poor dispensing precision.
- This method does not easily provide absolute volume accuracy unless calibrated with standards.
The Scientist's Toolkit: Key Research Reagent Solutions
The following reagents and tools are essential for developing robust high-throughput screening assays and for troubleshooting liquid handling systems.
Table 2: Essential Reagents and Tools for HTS and Liquid Handling QC
| Item | Function in Parasite Screening & Troubleshooting |
|---|---|
| Cell-Based Assay Kits | Provide physiologically relevant data for target identification and primary screening in parasite research [66]. |
| Volume Verification Kits (e.g., Artel MVS, VeriPlate) | Tools designed to quantitatively measure the accuracy and precision of automated liquid handlers [64]. |
| Tartrazine Dye | A low-cost, photometric reagent used for assessing dispensing precision across a microplate [64]. |
| High-Purity Deionized Water | The standard fluid for gravimetric verification of liquid handling performance [64]. |
| Jump-stARter Library (Janssen) | An example of a curated, structurally diverse compound library used in high-throughput phenotypic screens against parasites like E. histolytica [63]. |
| Medicines for Malaria Box | A collection of compounds with known antimalarial activity, used for validating new screening assays [62]. |
Workflow and Relationship Diagrams
Liquid Handling Troubleshooting Logic
The following diagram outlines a systematic approach to diagnosing and resolving common liquid handling artifacts.
Diagram 1: A logical workflow for troubleshooting liquid handling artifacts.
High-Throughput Screening Workflow
This diagram places liquid handling within the broader context of a high-throughput parasite screening campaign, highlighting where artifacts can be introduced.
Diagram 2: A simplified HTS workflow where liquid handling is a critical source of artifacts.
Optimizing Source Plates and Dispensing Cassettes for Consistent Performance
Technical Support Center
Troubleshooting Guides and FAQs
This guide provides solutions for common issues encountered with source plates and dispensing cassettes in high-throughput screening (HTS) environments, particularly for sensitive applications like parasite drug discovery.
Frequently Asked Questions
Q1: My dispensing cassette is clogging frequently. What could be the cause and how can I prevent it?
Clogging typically results from residual proteins, cells, or salts crystallizing inside the tubing. For parasite screening assays involving culture media or biological samples, implement this cleaning protocol:
- Immediate Post-Use Cleaning: After dispensing, immediately flush the cassette with deionized water [67].
- Detergent Wash: Use a mild detergent to remove biological residues. Ensure the detergent is compatible with your cassette material (e.g., injection-molded silicone) [67].
- Final Rinse and Disinfection: Rinse thoroughly with deionized water to remove all detergent, then rinse with a disinfectant. Autoclaving the cassette is recommended to ensure sterility for the next use [67].
- Regular Inspection: Weekly, inspect aspiration probes and cassettes for "visible damage, blockage, or crystal formation" [68].
Q2: How can I minimize variability in parasite motility data when using a reagent dispenser?
Inconsistent dispensing can skew results in real-time parasite motility assays [42]. Optimize these factors:
- Dispensing Speed: Use the instrument's slowest speed setting to reduce shear forces that could affect fragile parasites or cells [67].
- Dispense Height: Lower the dispensing module's height above the plate to prevent splashing and ensure liquid lands consistently in the well center [67].
- Cassette Bore Size: If working with sensitive parasite larvae or other fragile biologicals, start with a large bore dispensing cassette which has a wider orifice and generates lower shear forces [67].
Q3: What is the recommended schedule for maintaining and validating my automated dispensing system?
A formalized maintenance schedule is non-negotiable for data integrity in longitudinal studies [68].
Table: Recommended Maintenance Schedule for Dispensing Systems
| Component | Maintenance Frequency | Action |
|---|---|---|
| Manifold & Tubing | Daily | Flush with deionized water [68]. |
| Aspiration Probes & Cassettes | Weekly | Inspect for damage or blockage. Soak in mild acid if needed [68]. |
| Pump/Valve System | Monthly | Check for air bubbles and leaks. Recalibrate dispensing volume [68]. |
| Inline Filter | Quarterly | Replace or clean to prevent particulates from entering the system [68]. |
| Full Gravimetric Calibration | Every 3-12 months | Perform a gravimetric test (weighing dispensed liquid) to verify accuracy [69]. |
Q4: How do I choose the right dispensing cassette for my high-throughput parasite assay?
Selection depends on throughput, reagent type, and the sensitivity of your biological material.
Table: Dispensing Cassette Selection Guide
| Cassette Type | Best For | Throughput | Key Advantage |
|---|---|---|---|
| Large Bore Cassette | Fragile cells, parasite larvae, viscous media | Standard | Gentle dispensing; lower shear force [67]. |
| Small Bore Cassette | Standard reagents, buffers, non-adherent cells | High | Can be used with fragile cells at optimized settings [67]. |
| Low-Dead-Volume Source Plates | Precious/expensive compounds, miniaturized assays | Ultra-High | Minimizes reagent waste, reduces costs [70]. |
Detailed Experimental Protocols
Protocol 1: Gravimetric Calibration for Dispensing Accuracy
Regular calibration is essential for data reproducibility. This protocol verifies the volume accuracy of your dispenser [69].
Materials:
- Dispenser with cassette
- Analytical balance (accurate to 0.1 mg)
- Distilled or deionized water (ISO 3696, grade 3)
- Thermometer (accuracy ±0.2 °C)
- Receiving vessel (e.g., narrow-mouth flask)
Method:
- Equilibration: Allow the dispenser and water to adjust to room temperature in the testing room for at least 1 hour [69].
- Temperature Measurement: Record the water temperature [69].
- System Priming: Prime the dispensing system with water to remove air bubbles [69].
- Gravimetric Testing:
- Set the dispenser to the nominal volume (e.g., 100 µL).
- Dispense water into a tared receiving vessel. Wipe the tip against the vessel wall.
- Weigh the vessel and record the mass.
- Repeat this process ten times for the nominal volume, 50% of the nominal volume, and 10% of the nominal volume [69].
- Data Analysis:
- Calculate the mean dispensed mass.
- Convert mass to volume using the Z-factor, which accounts for water density and air buoyancy. The formula is:
Mean Volume (µL) = Mean Mass (mg) * Z[69]. - Calculate accuracy (A%) and coefficient of variation (CV%) to compare against manufacturer specifications or internal quality limits [69].
Protocol 2: Bottom-Washing for Gentle Removal of Reagents from Adherent Cell or Parasite Cultures
In cell-based assays or when working with adherent parasite stages, standard washing can detach cells. This gentle technique minimizes shear stress [68].
Materials:
- Automated microplate washer with programmable settings
- Pre-warmed, physiological wash buffer (e.g., PBS with Ca²âº/Mg²âº)
Method:
- Buffer Formulation: Use an isotonic buffer, such as PBS, possibly supplemented with calcium and magnesium ions for cell-based assays. For immunoassays like ELISA, a surfactant like TWEEN 20 (typically 0.05-0.1%) can be added to reduce non-specific binding [68].
- Washer Programming:
- Dispense Rate: Set to "Low to Medium" to minimize fluid shear across the cell monolayer [68].
- Dispense Position: Program the dispenser to aim the buffer stream toward the side wall or the very center of the well, allowing liquid to pool gently rather than directly hitting the cells [68].
- Aspiration: Use angled aspiration probes positioned to remove liquid from the meniscus at the well's edge. This prevents a rapid rush of fluid across the central monolayer that can cause detachment [68].
- Execution: Run the wash cycle with a reduced number of cycles (e.g., 2-3 times) sufficient to remove background, but not so many as to stress the cells [68].
Essential Research Reagent Solutions
This table details key materials and their functions for ensuring consistent performance in high-throughput screening workflows.
Table: Essential Materials for HTS Workflows
| Item | Function/Application | Key Consideration |
|---|---|---|
| Dispensing Cassettes (e.g., EasySnap) | Reagent and cell dispensing for assays like MTT or motility tracking [67] [42]. | Reusable; made from molded silicone for consistent volume without recalibration [67]. |
| Low-Dead-Volume Source Plates | Precise nanoliter-scale dispensing for drug discovery and genomics [70]. | SBS-standard format; minimizes waste of valuable compounds/reagents [70]. |
| Wash Buffer (PBS/TBS + TWEEN 20) | Microplate washing in ELISA and cell-based assays to remove unbound material [68]. | TWEEN 20 concentration (e.g., 0.01-0.1%) is assay-specific; reduces non-specific binding [68]. |
| Cell Cryopreservation Microplates | High-throughput cryopreservation of cell lines or parasites for screening campaigns [71]. | Specialized "microplate-in-a-box" designs enable controlled cooling rates for optimal viability [71]. |
| Real-Time Cell Monitoring Plates (E-plate) | Label-free, real-time monitoring of parasite motility for anthelmintic drug screening [42]. | Enables automated, high-throughput quantification of drug effects (IC50) on parasite movement [42]. |
Workflow and Troubleshooting Diagrams
Dispensing Troubleshooting Logic
Cassette Cleaning and Calibration Workflow
Managing Transfection Variability in RNAi Screening Platforms
Troubleshooting Guides
Table 1: Common Transfection Problems and Solutions in RNAi Screening
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low Transfection Efficiency | Suboptimal cell health or confluency, incorrect reagent:RNAi complex ratio, poor reagent choice for cell type [72]. | Ensure cells are 70-90% confluent and >90% viable pre-transfection [72]. Perform a dose-response curve with different reagent:RNAi molecule ratios [73]. |
| High Cytotoxicity | Transfection reagent toxicity, excessive reagent:RNAi complex amounts, presence of antibiotics during transfection [73] [72]. | Test less cytotoxic reagents (e.g., FuGENE HD, certain in-house lipids [73]). Perform transfection in antibiotic-free medium [72]. |
| High Inter-well Variability | Inconsistent cell seeding, uneven complex formation or distribution, technical pipetting errors. | Implement automated liquid handling for cell seeding and reagent dispensing. Ensure transfection complexes are mixed thoroughly and added consistently [74]. |
| Inconsistent Knockdown Results | Off-target effects (OTEs) of RNAi reagents, low stability of RNAi molecules, inefficient delivery [75] [76]. | Use pooled or esiRNA libraries to minimize OTEs [75] [76]. Validate hits with multiple, distinct RNAi triggers targeting the same gene [76]. |
| Poor Correlation Between Screening and Validation | High false-positive rate from primary screen, context-specific gene essentiality, reagent-specific artifacts [76]. | Employ robust statistical hit-calling methods (e.g., Z-score > 2-3). Use orthogonal assays (e.g., CRISPR) for secondary validation. |
Table 2: Optimizing Cell Health and Culture Conditions
| Parameter | Optimal Condition | Impact on Transfection |
|---|---|---|
| Cell Passage Number | Use low-passage cells (<30 passages after thawing) [72]. | Excessive passaging reduces transfection efficiency and transgene expression [72]. |
| Cell Confluency | 70-90% for adherent cells; 5x10^5 to 2x10^6 cells/mL for suspension [72]. | Too high: contact inhibition; Too low: poor growth; both reduce nucleic acid uptake [72]. |
| Serum in Medium | Complex formation in serum-free medium; serum can be added/replaced post-transfection [72]. | Serum proteins can interfere with cationic lipid-RNAi complex formation [72]. |
| Antibiotics | Avoid during cationic lipid-mediated transfection [72]. | Increased antibiotic uptake leads to cytotoxicity and lower efficiency [72]. |
Frequently Asked Questions (FAQs)
Q1: Our RNAi screens consistently yield hundreds of hits, but most fail validation. How can we improve the signal-to-noise ratio? A1: This is a common challenge, often described as "too much hay and very few needles" [76]. To address it:
- Improve Hit Stringency: Use stricter statistical cut-offs (e.g., Z-score > 3) and require a phenotype to be consistent across multiple, distinct RNAi reagents targeting the same gene [76].
- Mitigate Off-Target Effects (OTEs): OTEs are a major source of false positives [76]. Where possible, use endoribonuclease-prepared siRNA (esiRNA) pools, which contain a heterogeneous mixture of siRNAs, to dilute out OTEs while maintaining on-target efficacy [75].
- Robust Validation: Plan for immediate orthogonal validation using a different technology (e.g., CRISPRi or cDNA rescue) to confirm phenotype specificity [76].
Q2: We are working with primary macrophages, which are difficult to transfect. What is the most effective delivery method? A2: For hard-to-transfect primary cells like macrophages, transient transfection of synthetic siRNAs is highly inefficient and requires prohibitively high doses [75]. Lentiviral delivery of shRNA is the preferred method. Lentiviral vectors can transduce non-dividing cells and provide stable, long-term knockdown, which is essential for studying long-term phenotypes in primary cells [75].
Q3: How does cellular heterogeneity impact our RNAi screening results, and how can we account for it? A3: Cellular heterogeneity is a significant, often overlooked, source of variability. Even in a clonal population, differences in cell cycle stage and other intrinsic factors can cause dramatic differences in transfection efficiency and gene expression. A recent study on AAV production found that less than 5% of cells were responsible for the majority of the output due to heterogeneity in plasmid uptake and expression [77].
- Account for this by: Using single-cell RNA sequencing (scRNA-seq) to deconvolute your cell population and understand how subpopulations respond to knockdown [77]. Ensuring your assay readout is robust enough to detect phenotypic changes despite underlying heterogeneity.
Q4: What are the key differences between siRNA and shRNA in a screening context? A4: The choice depends on your biological question and experimental timeline.
- siRNA (synthetic): Ideal for transient, rapid knockdown in arrayed screens. Effects are "diluted out" with cell division, making it suitable for acute phenotypes. However, it can be costly for large-scale screens in primary cells [75].
- shRNA (vector-based): Provides stable, long-term knockdown. It is excellent for pooled screens and studies of chronic processes. It allows for selection of transduced cells, ensuring a homogeneous population for analysis. Lentiviral shRNA is the best option for primary and non-dividing cells [75].
Experimental Protocols for Key Experiments
Protocol 1: Systematic Titration of Transfection Reagents for a New Cell Line
This protocol is crucial for optimizing any RNAi screen, especially in the context of parasite research where unique host cell lines may be used.
1. Objective: To identify the optimal transfection reagent and RNAi molecule (siRNA/shRNA) ratio that maximizes knockdown efficiency while minimizing cytotoxicity for a specific cell line.
2. Materials:
- The cell line of interest (e.g., a host cell for parasite infection).
- A positive control siRNA (e.g., targeting a constitutively expressed gene like GAPDH).
- A non-targeting negative control siRNA.
- 2-3 candidate transfection reagents (e.g., Lipofectamine 2000, a low-cytotoxicity reagent, and a cost-effective in-house alternative like linear PEI or DOTMA:DOPE [73]).
- 96-well tissue culture plates.
- Equipment for viability (e.g., luminescence-based assay) and efficiency readouts (e.g., qRT-PCR, fluorescence microscope).
3. Methodology:
- Day 1: Cell Seeding. Seed cells in 96-well plates to achieve 70-90% confluency at the time of transfection (24 hours later). Include replicates for each condition [72].
- Day 2: Transfection.
- Prepare a matrix of transfection conditions. For each reagent, test multiple dilution factors (e.g., 1:1, 1:2, 1:4) against multiple siRNA concentrations (e.g., 10 nM, 25 nM, 50 nM).
- Form complexes according to the manufacturer's instructions, typically in a serum-free medium.
- Add complexes to the cells.
- Day 3/4: Analysis.
- Efficiency: 24-48 hours post-transfection, harvest cells for qRT-PCR to measure mRNA levels of the GAPDH target.
- Viability: Perform a luminescence-based viability assay in parallel. Calculate the percentage of viable cells relative to non-transfected controls.
- Calculation: Determine the condition that yields the highest knockdown with >80% cell viability.
Protocol 2: A Mini-Screen to Identify Modulators of Parasite Infection
This protocol outlines a focused RNAi screen to identify host factors involved in parasite entry or proliferation.
1. Objective: To perform a targeted RNAi screen using a library targeting 500 genes in a host cell line to identify factors that, upon knockdown, alter parasite infection rates.
2. Materials:
- Host cell line.
- A focused siRNA library (e.g., targeting kinases, membrane transporters).
- Optimized transfection reagent from Protocol 1.
- A reporter parasite (e.g., expressing GFP).
- Automated fluorescence microscope or high-content imaging system.
- Automation-compatible 384-well plates.
3. Methodology:
- Day 1: Reverse Transfection. Seed cells directly into plates pre-spotted with siRNA-transfection reagent complexes. This saves time and improves consistency for large-scale screens.
- Day 2/3: Infection. Infect cells with the reporter parasite at a pre-determined Multiplicity of Infection (MOI).
- Day 4: Fixation and Staining. Fix cells and stain with a nuclear dye (e.g., Hoechst) to count total cell numbers.
- Day 4: Imaging and Analysis. Image each well using an automated microscope. Quantify the percentage of GFP-positive (infected) cells per well using image analysis software.
- Hit Identification: Normalize infection rates to negative control wells. Apply a robust statistical method, such as Z-score normalization, to identify siRNAs that significantly increase or decrease infection. A Z-score >2 or <-2 is often used as an initial cutoff [78].
Research Reagent Solutions
Table 3: Key Reagents for RNAi Screening
| Reagent / Material | Function in RNAi Screening |
|---|---|
| Lipofectamine 2000 | A widely used commercial cationic lipid reagent known for high efficiency with DNA and RNA, but can be cytotoxic at high concentrations [73]. |
| FuGENE HD | A commercial reagent valued for its high transfection efficiency and notably reduced cytotoxicity profile [73]. |
| Linear PEI (25-40 kDa) | A cost-effective polyamine-based in-house alternative; 25 kDa version offers lower cytotoxicity, while 40 kDa offers higher binding capacity [73]. |
| Cationic Lipids (DOTAP/DOTMA) | Often mixed with helper lipid DOPE at various molar ratios (e.g., 0.5:1, 1:1, 2:1) to form stable, customizable in-house lipoplexes with high mRNA transfection efficiency [73]. |
| Lentiviral shRNA Vectors | Essential for stable gene knockdown in hard-to-transfect cells (e.g., primary macrophages); enables transduction of non-dividing cells [75]. |
| esiRNA Pools | Complex pools of siRNAs generated by enzymatic digestion of long dsRNA; reduce off-target effects (OTEs) by diluting out individual OTEs [75]. |
| Holographic Imaging Cell Counter | For accurate assessment of cell density and viability prior to transfection, a critical parameter for success (e.g., Norma XS) [77]. |
| High-Throughput Flow Cytometer | For analyzing transfection efficiency (e.g., via GFP reporter) and other cell-based assays in multi-well plates (e.g., Guava easyCyte) [77]. |
Workflow Visualization
RNAi Screen Optimization
Hit Validation Workflow
Root Cause Analysis of False Positives in Ultrasensitive Molecular Detection
Frequently Asked Questions (FAQs)
FAQ 1: What are the most common root causes of false positives in CRISPR-based molecular detection? False positives in CRISPR diagnostics primarily arise from off-target collateral cleavage activity, pre-amplification contamination, or non-specific signal generation. The trans-cleavage activity of Cas proteins (like Cas12 and Cas13), once activated by a target sequence, non-specifically degrades reporter molecules, which can sometimes be triggered by non-target molecules with partial homology, leading to false signals. Furthermore, in methods relying on pre-amplification steps (like RPA or LAMP), amplicon contamination between samples is a significant risk [79].
FAQ 2: How can environmental factors impact assay specificity in high-throughput settings? Environmental conditions like high humidity can critically degrade the performance of enzymatic components in molecular assays. Field studies have shown that Cas14-based assays can experience a 63% performance drop under high-humidity conditions, which may destabilize reagents and increase background noise or non-specific reactions. Robust assay design must include environmental stability testing to ensure results are reliable outside controlled lab environments [79].
FAQ 3: What strategies can improve specificity in amplification-free detection methods? Amplification-free methods enhance specificity by eliminating the risk of amplicon contamination. Key strategies include:
- Enzyme Engineering: Mutating Cas proteins to enhance their trans-cleavage activity and specificity [80].
- Signal Amplification: Employing engineered DNA amplifiers (e.g., dual stem-loop DNA amplifiers) that only produce a signal upon specific target recognition, thereby enhancing the signal-to-noise ratio without pre-amplifying the target [80].
- Sample Enrichment: Using microfluidic or droplet platforms to concentrate the target analyte from the sample matrix [80].
FAQ 4: Why might an assay's limit of detection (LOD) vary between different geographical sites? The observed Limit of Detection (LOD) for the same assay can vary significantly due to regional differences in pathogen strains, environmental conditions, and sample matrix effects. For example, a study on malaria RDTs found that the LOD for HRP2 antigen varied from 3.9 ng/mL in Tambacounda to 204.3 ng/mL in Diourbel, highlighting how local factors can influence diagnostic performance [37].
Troubleshooting Guide: Common Issues and Solutions
Table 1: Troubleshooting False Positives in Ultrasensitive Detection
| Problem Category | Specific Symptom | Potential Root Cause | Recommended Solution |
|---|---|---|---|
| Assay Design | High background fluorescence in no-template controls. | Non-optimal guide RNA (gRNA) design with off-target potential. | Redesign gRNA to avoid homology with non-target sequences; use computational tools for specificity check [79]. |
| False positives with closely related non-target species. | Insufficient target sequence specificity; conserved region targeting. | Select unique, variable genomic regions for probe design; perform in-silico specificity validation [79]. | |
| Reaction Components | Inconsistent results between reagent batches. | Variability in enzyme activity (e.g., Cas protein, polymerase). | Quality control check of enzymes; use commercial, standardized reagents where possible. |
| Signal in negative samples after pre-amplification. | Amplicon contamination from previous runs or lab environment. | Implement strict physical separation of pre- and post-amplification areas; use dUTP/UNG carryover prevention systems [79]. | |
| Sample & Environment | Reduced specificity with direct clinical samples (e.g., serum). | Inhibitors in complex sample matrices interfering with the reaction. | Dilute samples; incorporate sample purification steps; add blocker molecules (e.g., BSA) to the reaction mix [79] [80]. |
| Performance drop in field or point-of-care settings. | Degradation of sensitive reagents due to non-ideal storage (temperature, humidity). | Use lyophilized (freeze-dried) reagent formats; validate assay stability under intended use conditions [79]. |
Table 2: Advanced Techniques for False Positive Mitigation
| Technique | Principle | Application Example |
|---|---|---|
| Enzyme Engineering | Mutating Cas proteins to improve their specificity and reduce non-specific collateral cleavage. | Engineered high-fidelity Cas12/Cas13 variants with reduced off-target activity [80]. |
| Cascading Amplification | Using a multi-step, enzymatic signal amplification system that requires multiple specific recognition events. | The TCC method uses a dual stem-loop DNA amplifier that requires sequential activation by two CasΦ complexes, drastically reducing non-specific signals [80]. |
| Digital Counting & Detection | Partitioning the reaction into thousands of micro-compartments to count individual target molecules, distinguishing them from background noise. | The AVAC platform digitally counts individual plasmonic nanoparticles bound to targets, providing ultra-sensitive and specific quantification [81]. |
| Machine Learning-Assisted Analysis | Using computational models to classify complex signal patterns and distinguish specific signals from non-specific background. | Using PCA-LDA models to classify SERS spectra from bioprobes, achieving 97.33% accuracy in distinguishing cancer cell subtypes [82]. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Ultrasensitive Detection
| Item | Function in the Experiment | Key Consideration |
|---|---|---|
| Programmable Nucleases(e.g., Cas9, Cas12, Cas13, CasΦ) | Core enzyme for target recognition and signal generation via cis- or trans-cleavage. | Select based on target (DNA/RNA). CasΦ is compact and suitable for POC; Cas12a has strong trans-cleavage for DNA [79] [80]. |
| Guide RNA (gRNA/crRNA) | A short RNA sequence that directs the Cas protein to the specific target nucleic acid. | Design is critical for specificity. Avoid off-target sites; chemical modifications can enhance stability and performance [79]. |
| Fluorescent Reporter Probes | Single-stranded DNA or RNA probes with a fluorophore and quencher; cleavage generates a fluorescent signal. | Optimize length and sequence to be efficiently cleaved by the activated Cas protein with low background noise [79] [80]. |
| Signal Amplifiers(e.g., TCC Amplifier) | Engineered nucleic acid structures that amplify the detection signal only upon specific target recognition. | Enables amplification-free detection, reducing contamination risk and simplifying workflows [80]. |
| Lyophilized Reagent Formulations | Freeze-dried, stable versions of all reaction components. | Essential for point-of-care use; improves shelf life and robustness against environmental variations [79]. |
Experimental Protocol for Specificity Validation
This protocol outlines a key experiment for validating the specificity of a CRISPR-based detection assay and identifying conditions that may lead to false positives.
Title: Protocol for Assessing Off-Target Collateral Cleavage Activity.
Objective: To determine if the Cas protein's collateral activity is triggered by non-target sequences or environmental interferents.
Materials:
- Recombinant Cas protein (e.g., Cas12a, Cas13a)
- Target-specific crRNA
- Non-target crRNA (with no homology to the target or any sequence in the sample)
- Fluorescent reporter probe (ssDNA for Cas12, ssRNA for Cas13)
- Positive control: Synthetic target DNA/RNA template
- Test samples: Genomic DNA from closely related non-target organisms, human genomic DNA, or sample matrix (e.g., serum)
- Real-time PCR instrument or fluorometer
- Thermostatic water bath or heat block
Procedure:
- Reaction Setup: Prepare multiple reaction mixtures on ice containing the Cas protein, fluorescent reporter, and reaction buffer.
- Test Groups:
- Group 1 (Positive Control): Add target-specific crRNA and the synthetic target template.
- Group 2 (Specificity Control): Add target-specific crRNA and the non-target genomic DNA or sample matrix.
- Group 3 (Negative Control 1): Add target-specific crRNA but no template.
- Group 4 (Negative Control 2): Add non-target crRNA and the synthetic target template.
- Group 5 (Background Control): No crRNA and no template.
- Incubation and Data Collection:
- Transfer the reactions to a pre-heated instrument at 37°C.
- Measure fluorescence every 2 minutes for 60-90 minutes.
- Data Analysis:
- Plot fluorescence over time for all groups.
- A significant increase in fluorescence in Group 2 compared to the negative controls (Groups 3, 4, 5) indicates off-target collateral cleavage and a potential for false positives.
- Analyze the reaction kinetics (time to positive) and endpoint fluorescence to quantify the degree of non-specificity.
Diagnostic Workflows and Logical Pathways
The following diagram illustrates the logical workflow for analyzing a suspected false positive result, helping to systematically identify the root cause.
Validation and Comparison: Assessing Sensitivity, Specificity, and Clinical Utility
In high-throughput parasite screening and drug development research, selecting a diagnostic method with appropriate analytical sensitivity is crucial for detecting true infections, monitoring treatment efficacy, and making timely decisions. Analytical sensitivity refers to the lowest quantity of a target pathogen that an assay can reliably detect. This guide compares three common techniques—microscopy, conventional PCR, and real-time quantitative PCR (qPCR)—to help you select the optimal method for your specific research context.
Direct Sensitivity Comparison: Quantitative Data
The following table summarizes key performance metrics from comparative studies, illustrating the clear hierarchy in detection capability among these techniques.
Table 1: Comparative Analytical Sensitivity of Diagnostic Methods from Various Studies
| Study Organism / Context | Microscopy | Conventional PCR | Real-time PCR (qPCR) | Key Findings & Notes |
|---|---|---|---|---|
| Babesia bigemina (Bovines) [83] | 5/95 (5.26%) | 21/95 (22.10%) | 49/95 (51.58%) | qPCR detected parasites in samples with copy numbers as low as 10/µL, a range where other methods failed. |
| Mycoplasma gallisepticum (Poultry) [84] | Not Applicable | 48/146 (32.87%) | 58/146 (39.72%) | Compared to conventional PCR as a gold standard, qPCR showed 100% sensitivity and 89.8% specificity. |
| Streptococcus agalactiae (Pregnant Women) [85] | Not Applicable | 17.7% positivity | 29.2% positivity | Both PCR methods showed higher detection rates than culture (3.8%), with qPCR being the most sensitive. |
| AI-Parasite Detection (Stool Samples) [86] | Standard Sensitivity | Not Applicable | Not Applicable | A deep-learning AI system identified 169 additional parasites missed by manual microscopy review, demonstrating improved sensitivity. |
Experimental Protocols for Sensitivity Comparison
To ensure your method comparison is robust, here are detailed protocols for assessing the analytical sensitivity of each technique.
Protocol: Limit of Detection (LoD) Assessment for qPCR
This protocol is adapted from the development of a highly specific Perkinsus marinus qPCR assay [87].
- Standard Curve Generation: Create a standard positive control plasmid containing the target gene sequence. Perform 10-fold serial dilutions in duplicate, covering a range from a high copy number (e.g., 10^6 copies/µL) down to a theoretical single copy (10^0 copies/µL) [83] [87].
- qPCR Run: Amplify the serial dilutions using your optimized qPCR conditions.
- Data Analysis: Plot the mean Cycle Threshold (Ct) value for each dilution against the logarithm of its known concentration. The resulting standard curve allows you to determine the PCR efficiency [87].
- LoD Determination: The LoD is the lowest copy number per reaction volume that can be reliably detected. For example, in the Babesia study, samples with a Ct value of 36.92, corresponding to 10 copies/µL, were considered positive [83]. The idream-qPCR device achieved an LoD of 0.85 copies/µL for SARS-CoV-2 genes [88].
Protocol: Conventional PCR and Gel Electrophoresis
This method is common in studies comparing pathogen detection rates [84] [85].
- PCR Reaction Setup:
- Reaction Volume: 20-50 µL [85] [87].
- Components: Include 0.4-0.5 µM of each primer, 0.25 mM dNTP mix, 1x reaction buffer, 0.5-1.0 U of DNA polymerase, and template DNA [89] [87].
- Thermal Cycling: Conditions are target-specific. A general scheme includes an initial denaturation (e.g., 95°C for 4 min), followed by 30-40 cycles of denaturation (e.g., 94°C for 1 min), primer annealing (temperature varies for 1 min), and extension (e.g., 65-72°C for 1-3 min), with a final elongation step [87].
- Post-Amplification Analysis:
- Prepare a 1.5-2% agarose gel in an appropriate buffer.
- Mix PCR products with a loading dye and load into the gel wells, including a DNA molecular weight marker.
- Run the gel at a constant voltage until bands are adequately separated.
- Stain the gel with ethidium bromide or a safer alternative and visualize under UV light [87].
- Result Determination: A positive result is confirmed by the visual presence of an amplified band of the expected size [89].
Protocol: Microscopy for Parasite Detection
While sensitivity is lower, microscopy remains a valuable tool for morphological confirmation [83] [86].
- Sample Preparation:
- Examination:
- Systematically examine the smear or wet mount under oil immersion at high magnification (e.g., 1000x).
- Identify parasites based on morphological characteristics (e.g., size, shape, internal structures).
- Result Determination: The sample is considered positive if one or more parasitic structures (e.g., cysts, eggs, trophozoites) are definitively identified.
The workflow below illustrates the typical steps and outcomes for each method in a comparative diagnostic study.
Frequently Asked Questions (FAQs)
Q1: Is qPCR inherently more sensitive than conventional PCR?
A: Not necessarily. While many modern studies show qPCR has superior sensitivity, this is not an inherent property of the technology but a consequence of assay design. Factors that influence sensitivity include:
- Amplicon Size: qPCR typically uses shorter amplicons (e.g., 75-150 bp), which are amplified more efficiently than the longer targets (e.g., 800-1200 bp) often used in conventional PCR [90].
- Primer/Probe Design: The specificity and binding efficiency of primers and probes are critical [91] [87].
- Reaction Optimization: The sensitivity of any PCR assay, whether conventional or qPCR, is highly dependent on meticulous optimization of conditions like Mg²⺠concentration, annealing temperature, and DNA polymerase used [91] [90]. A well-designed, optimized conventional PCR (especially nested PCR) can be as sensitive as or even more sensitive than a poorly optimized qPCR assay [91].
Q2: Why does my qPCR assay have high Ct values and variable results?
A: High and variable Ct values often point to issues with sample quality, reaction inhibitors, or suboptimal reagent performance.
- Inhibitors: Substances from the sample (e.g., heme, humic acids) or the DNA extraction process can inhibit the PCR reaction. Re-purify your DNA or dilute the template to dilute out inhibitors.
- Sample Degradation: Poor sample collection or storage can lead to degraded nucleic acids, reducing the available target. Ensure standardized and rapid processing of specimens, as delays can significantly impact accuracy [89].
- Low Template Concentration: The target pathogen may be present at a very low level. Concentrate your sample or increase the template input volume if possible, bearing in mind that this can also increase inhibitors [91].
- Reagent Inefficiency: Check the efficiency of your primers and probe using a standard curve. PCR efficiency should be between 90-110% [87].
Q3: For high-throughput screening, should I completely replace microscopy with molecular methods?
A: Not entirely. While molecular methods like qPCR offer superior sensitivity and are better suited for high-throughput automation, microscopy still plays a vital role.
- Gold Standard for Morphology: Microscopy allows for the identification of parasite species based on morphology and can detect mixed infections that might be missed by a species-specific PCR [86].
- Viability Assessment: In some cases, microscopy can provide clues about the viability of the parasite. A synergistic approach is often best. Use qPCR for primary, high-throughput screening due to its speed and sensitivity, and reserve microscopy for confirmation, species identification, and training purposes. The integration of AI with microscopy is also emerging as a way to enhance the sensitivity and throughput of traditional microscopic examination [86].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and their critical functions in molecular assays for parasite detection.
Table 2: Key Reagents for Molecular Detection of Parasites
| Reagent / Material | Function | Example from Literature |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolates DNA/RNA from complex samples, removing inhibitors that can affect downstream PCR. | DNeasy Blood & Tissue Kit (Qiagen) [87], QIAamp DSP DNA Mini Kit [89] |
| Primers & Probes | Binds specifically to the target DNA sequence for amplification. Specificity is paramount. | TaqMan probe for P. marinus [87], broad-range 16S rRNA primers [89] |
| PCR Master Mix | Contains DNA polymerase, dNTPs, and optimized buffers for efficient amplification. | 2× PowerUp SYBR Green Master Mix [87], in-house prepared mixes [89] |
| Positive Control Plasmid | Contains a known quantity of the target sequence for standard curve generation and LoD determination. | Plasmid with cloned hypothetical protein gene from P. marinus [87] |
| Agarose | Matrix for gel electrophoresis to separate and visualize conventional PCR amplicons by size. | Used for analyzing PCR products in conventional methods [83] [87] |
Understanding Diagnostic Specificity in Screening
What is Diagnostic Specificity?
Diagnostic specificity is a crucial metric that measures a test's ability to correctly identify individuals who do not have a disease or condition. In mathematical terms, it is defined as the proportion of true negatives out of all subjects who do not have the disease [92] [93]. A test with high specificity reliably excludes individuals who do not have the condition, resulting in a high number of true negatives and low number of false positives [93].
Formula: Specificity = True Negatives / (True Negatives + False Positives) [92]
The Critical Role of Specificity in Low-Prevalence Settings
In low-prevalence settings, where most individuals in the population are healthy, even a test with high specificity can yield a substantial number of false positives. This occurs because although the percentage of false positives is low, the large number of healthy individuals means that a small false positive rate affects many people [92]. High specificity is particularly important when individuals identified as having a condition may be subjected to more testing, expense, stigma, or anxiety [93].
Key Concepts and Their Interrelationships
Specificity Versus Sensitivity Trade-Off
Sensitivity and specificity are inversely related: as sensitivity increases, specificity tends to decrease, and vice versa [92] [93]. This relationship necessitates careful consideration of the testing context and consequences of errors:
- Highly sensitive tests are optimal for ruling out disease (few false negatives)
- Highly specific tests are optimal for ruling in disease (few false positives) [92]
The balance between these metrics must be strategically determined based on the clinical or research context.
Predictive Values and Prevalence Dependence
Unlike sensitivity and specificity, which are intrinsic test characteristics, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) are highly dependent on disease prevalence [92]:
Formulas:
- PPV = True Positives / (True Positives + False Positives)
- NPV = True Negatives / (True Negatives + False Negatives)
When a disease is highly prevalent, the test is better at 'ruling in' the disease and worse at 'ruling it out' [92]. This relationship is particularly important in low-prevalence settings, where PPV tends to be lower despite good specificity.
Quantitative Framework for Specificity Assessment
Key Diagnostic Performance Metrics
Table 1: Essential Diagnostic Test Performance Metrics
| Metric | Definition | Formula | Impact in Low-Prevalence Settings |
|---|---|---|---|
| Specificity | Ability to correctly identify healthy individuals | True Negatives / (True Negatives + False Positives) | Critical for minimizing false alarms |
| Positive Predictive Value (PPV) | Proportion of true positives among all positive results | True Positives / (True Positives + False Positives) | Decreases significantly in low-prevalence settings |
| Negative Predictive Value (NPV) | Proportion of true negatives among all negative results | True Negatives / (True Negatives + False Negatives) | Remains high in low-prevalence settings |
| Positive Likelihood Ratio (LR+) | How much the odds of disease increase with a positive test | Sensitivity / (1 - Specificity) | Not affected by disease prevalence [92] |
| Negative Likelihood Ratio (LR-) | How much the odds of disease decrease with a negative test | (1 - Sensitivity) / Specificity | Not affected by disease prevalence [92] |
Example Calculation Scenario
Table 2: Specificity Impact in Low vs. High Prevalence Scenarios
| Parameter | Low Prevalence Scenario (1%) | High Prevalence Scenario (20%) |
|---|---|---|
| Population Size | 10,000 | 10,000 |
| True Disease Cases | 100 | 2,000 |
| Healthy Individuals | 9,900 | 8,000 |
| Assumed Specificity | 95% | 95% |
| False Positives | 495 | 400 |
| True Positives (assuming 100% sensitivity) | 100 | 2,000 |
| Positive Predictive Value | 16.8% | 83.3% |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Our high-throughput screening assay has excellent sensitivity but poor specificity, generating too many false positives for follow-up. What optimization strategies should we prioritize?
A1: Focus on these specific optimization approaches:
- Increase stringency thresholds: Adjust your positive call threshold to favor specificity over sensitivity [92]
- Implement orthogonal verification: Use a secondary assay with different detection principles to confirm primary hits [18]
- Optimize reagent concentrations: Titrate detection reagents, antibodies, or probes to reduce non-specific binding
- Include additional controls: Incorporate more specific negative controls to identify and subtract background signal
- Analyze at multiple timepoints: Distinguish specific from non-specific signals based on kinetic profiles
Q2: How can we accurately assess specificity when a true gold standard test is unavailable for our parasitic disease model?
A2: Employ these practical alternatives to gold standard testing:
- Composite reference standard: Combine multiple imperfect tests to create a better reference [92]
- Latent class analysis: Use statistical models that don't require a perfect gold standard
- Clinical follow-up: Track progression in test-positive and test-negative individuals over time
- Expert panel review: Use consensus diagnosis from multiple experts as a provisional standard
Q3: What statistical approaches best handle verification bias in our specificity calculations when follow-up testing is incomplete?
A3: Implement these bias-correction methodologies:
- Multiple imputation: Model missing verification status based on available variables
- Inverse probability weighting: Weight verified cases by the inverse probability of being verified
- Selection models: Explicitly model the verification process simultaneously with test accuracy
Q4: How does disease prevalence affect the practical impact of specificity improvements in population screening?
A4: Consider this quantitative relationship: In low-prevalence settings (e.g., 1%), improving specificity from 95% to 99% reduces false positives by 80%, dramatically improving PPV. The same improvement in high-prevalence settings (e.g., 20%) reduces false positives but has less dramatic impact on PPV. Always calculate PPV specific to your population.
Q5: What experimental design considerations are most critical for accurate specificity estimation in early drug discovery?
A5: Focus on these design elements:
- Adequate negative controls: Include sufficient true negative samples to reliably estimate specificity [9]
- Blinded assessment: Ensure test interpreters are blinded to true disease status
- Population representativeness: Include samples that reflect the spectrum of conditions in the target population
- Sample size calculation: Ensure sufficient sample size for precise specificity estimates
Experimental Protocols for Specificity Optimization
Protocol 1: Specificity Validation in High-Throughput Parasite Screening
Purpose: To systematically evaluate and optimize diagnostic specificity in high-throughput parasite drug screening assays [18].
Materials & Reagents:
- Synchronized parasite cultures (include drug-sensitive and resistant strains) [18]
- Compound libraries (include known negatives and positives) [18] [9]
- Fluorescence detection system (e.g., nucleic acid stains, viability markers) [18]
- High-content imaging system (e.g., Operetta CLS with 40× water immersion lens) [18]
- Multi-well plates (384-well format recommended) [18]
Procedure:
- Prepare compound plates: Array compounds in dose-dependent manner (e.g., 10 µM to 20 nM in 1:2 serial dilutions) [18]
- Inoculate with parasites: Dispense synchronized parasite cultures (1% schizont-stage at 2% hematocrit) into compound-treated plates [18]
- Incubate: Maintain plates at 37°C in appropriate gas mixture (1% O₂, 5% CO₂ in N₂) for 72 hours [18]
- Stain and fix: Treat with staining solution containing wheat agglutinin-Alexa Fluor 488 conjugate (1 µg/mL) and Hoechst 33342 (0.625 µg/mL) in 4% paraformaldehyde [18]
- Image acquisition: Capture nine microscopy image fields per well using high-content imaging system [18]
- Image analysis: Transfer images to analysis software (e.g., Columbus v2.9) for automated parasite classification and quantification [18]
Specificity Optimization Steps:
- Threshold calibration: Use ROC curve analysis to determine optimal cutoff that maintains >90% specificity
- Cross-reactivity assessment: Test against related but non-target parasite species
- Interference testing: Evaluate potential compound interference with detection signals
Protocol 2: Orthogonal Confirmatory Assay for False Positive Reduction
Purpose: To validate primary screening hits using an orthogonal detection method to eliminate false positives.
Materials & Reagents:
- Primary hit compounds from initial screening
- Alternative detection technology (e.g., different fluorescence channel, luminescence, enzymatic assay)
- Secondary parasite strains (include resistant variants) [18]
- Viability assay reagents with different detection mechanisms
Procedure:
- Select primary hits: Identify compounds showing activity in primary screen
- Design confirmation plates: Rearray hits with appropriate concentration gradients
- Apply orthogonal detection: Implement detection method with different principle than primary screen
- Compare results: Assess concordance between primary and secondary assays
- Calculate confirmatory rates: Determine percentage of primary hits verified by orthogonal method
Research Reagent Solutions
Table 3: Essential Research Reagents for Specificity Optimization
| Reagent/Category | Specific Function | Application in Specificity Optimization |
|---|---|---|
| Strain Panels [18] | Provides biological diversity for cross-reactivity testing | Includes drug-sensitive (3D7, NF54) and resistant (K1, Dd2) P. falciparum strains |
| Fluorescent Probes [18] | Enables multi-parameter detection | Wheat agglutinin-Alexa Fluor 488 conjugate for membranes; Hoechst 33342 for DNA |
| High-Content Imaging Systems [18] | Allows morphological assessment beyond simple fluorescence | Operetta CLS system with 40× water immersion lens |
| Orthogonal Detection Reagents | Provides alternative detection mechanisms | ATP-based viability assays, enzymatic markers, luminescence probes |
| Compound Libraries [18] [9] | Includes known negatives for specificity assessment | FDA-approved compounds, diversity sets, target-focused libraries |
Workflow for Systematic Specificity Optimization
This technical support center provides resources for researchers engaged in high-throughput screening of gastrointestinal parasites. The following guides and FAQs address common challenges in diagnostic methodology, from classic microscopic techniques to advanced molecular and artificial intelligence (AI) applications, supporting robust experimental design and data interpretation in drug development research.
The table below summarizes the key characteristics of major diagnostic methodologies for parasite detection, providing a foundation for technique selection in screening programs.
Table 1: Comparison of Parasite Diagnostic Techniques
| Technique | Principle | Key Advantage | Primary Limitation | Best Use-Case Scenario |
|---|---|---|---|---|
| Direct Wet Mount [94] [95] | Direct microscopic exam of fresh stool in saline/iodine. | Low cost, rapid, detects motile trophozoites [94] [96]. | Low sensitivity [94] [96]. | Rapid initial assessment, detection of motile protozoan stages [95]. |
| Formol-Ether Sedimentation (FEC) [94] [97] | Formalin fixation and ether concentration to sediment parasites. | Low cost, essential for helminth ova detection [94] [96]. | Requires centrifugation; hookworm eggs can be damaged [94] [96]. | General qualitative stool exam; broad parasite detection [97]. |
| Kato-Katz [94] [95] | Stool sieved and cleared with glycerin for microscopic exam. | WHO gold standard for STH; quantifies egg counts [94] [95]. | Low sensitivity for low-intensity and Strongyloides infections [94] [96]. | Epidemiologic surveys of soil-transmitted helminths (STH) [95]. |
| Flotation Techniques [97] [98] | Uses high-specific-gravity solution to float parasites to surface. | Produces cleaner material with less debris than sedimentation [97]. | Can collapse eggs/cysts; not all parasites float [97]. | Detection of protozoan cysts and some helminth eggs [97]. |
| Molecular (PCR, LAMP) [94] [99] | Detection of parasite-specific DNA/RNA sequences. | High sensitivity and specificity; species differentiation [94] [99]. | Higher cost, requires specialized equipment and expertise [99]. | Species-specific identification, low-intensity infections, and research [94]. |
| AI-Powered Microscopy [86] | Deep-learning algorithm analyzes digital images of samples. | High-throughput; 98.6% agreement with manual review; detects missed organisms [86]. | Requires initial training on thousands of samples [86]. | High-volume labs; improving diagnostic consistency and throughput [86]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Our Kato-Katz results for hookworm are inconsistent. What could be the issue?
- Potential Cause: The thin hookworm eggshell is fragile and can be damaged during the sample stirring or sieving process, leading to false negatives [96]. Furthermore, glycerol clearance must be timed correctly; over-clearing can make eggs invisible [95].
- Solution: Ensure proper technique during sample preparation to minimize physical stress on the eggs. For critical drug efficacy studies, confirm results with a molecular method like PCR, which is not affected by egg morphology and offers higher sensitivity for hookworm species differentiation [94].
Q2: When should we choose sedimentation over flotation, and vice versa?
- Sedimentation (e.g., Formol-Ether): This is the recommended technique for general diagnostic laboratories [97]. It is easier to perform, less prone to technical errors, and recovers a wider variety of parasites because it does not rely on specific gravity. It is ideal for detecting most helminth eggs and larvae, and operculated eggs that do not float well [97] [98].
- Flotation: This technique is superior for producing a cleaner preparation with less fecal debris, which can make identification easier [97]. It is excellent for protozoan cysts (e.g., Giardia) and some helminth eggs. However, it may distort fragile structures, and not all parasite eggs will float [97].
Q3: We need maximum sensitivity for a low-intensity infection study. Which method is best?
- Answer: For the highest sensitivity, particularly in low-intensity infections or for detecting submicroscopic carriage, molecular techniques are superior [94] [99]. Methods like PCR and multiplex bead assays can detect parasite DNA or antigens at levels far below the threshold of microscopy [37].
- Implementation Tip: In a high-throughput research context, consider integrating AI-powered digital microscopy or high-throughput bead-based antigen detection systems. These platforms maintain high sensitivity while drastically increasing processing speed for large sample sizes [86] [37].
Q4: How can we manage the high cost and expertise required for molecular diagnostics in resource-limited settings?
- Strategy: For large-scale surveillance where molecular methods are prohibitive, a dual approach is effective. Use a highly sensitive technique like quantitative PCR (qPCR) to establish the "true" prevalence in a subset of samples, while using a cheaper, field-deployable method like Kato-Katz for broader monitoring [95]. Alternatively, explore loop-mediated isothermal amplification (LAMP), which offers high sensitivity with less complex equipment than PCR [95].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for Parasitological Diagnostics
| Item | Function | Application Notes |
|---|---|---|
| 10% Buffered Formalin | Preserves parasitic structures (eggs, larvae, cysts) for long-term storage and safety [97] [98]. | Standard fixative for concentration procedures; maintains morphology. |
| Ethyl Acetate | Solvent used as a lipid and debris extractor in sedimentation concentration [97]. | Less flammable and safer alternative to diethyl ether [97]. |
| Zinc Sulfate or Sheather's Sugar Solution | High-specific-gravity flotation media to buoy parasites [97]. | Concentration of protozoan cysts and some helminth eggs. |
| Cellophane Coverslips | Used in Kato-Katz for glycerol-based clearing of fecal debris [94] [95]. | Allows for visualization of helminth eggs; requires specific immersion time. |
| Specific Primers & Probes | Oligonucleotides for targeted amplification of parasite DNA/RNA [94] [99]. | Essential for PCR/qPCR; specificity determines which parasite is detected. |
| Fluorescent Dyes (e.g., Hoechst, Wheat Germ Agglutinin) | Stain nucleic acids and cell membranes for image-based high-throughput screening [18]. | Enables automated imaging and analysis of parasites in phenotypic drug screens. |
Experimental Workflow for High-Throughput Screening
The diagram below outlines a generalized workflow for a high-throughput drug screening project against parasites, integrating modern and classic techniques.
Evaluating Commercial vs. In-House Concentration Kits for Intestinal Parasites
Within high-throughput parasite screening methodologies, efficient sample preparation is a critical bottleneck that significantly impacts downstream analysis. The concentration of parasitic elements from stool specimens represents a fundamental pre-analytical step that directly influences the sensitivity and reliability of diagnostic results. For research and drug development professionals, the choice between commercial concentration kits and in-house (often "homemade") procedures involves careful consideration of performance, cost, workflow integration, and compatibility with automated screening platforms.
Evidence suggests that while commercial kits offer standardization and convenience, their performance may vary significantly. A comparative evaluation of four commercial kits against one homemade procedure found that for some parasites, the homemade method demonstrated superior effectiveness, particularly for preconcentration specimens that tested negative [100]. This technical support center provides detailed guidance to help researchers navigate these critical methodological decisions and troubleshoot common experimental challenges encountered in parasitological research.
Technical Comparison: Performance Data at a Glance
The following tables summarize key quantitative findings from comparative studies to inform your kit selection process.
Table 1: Comparative Detection Thresholds of Concentration Methods for Protozoa
| Parasite | EasyPara (Last Positive Dilution) | Para-Selles (Last Positive Dilution) | Significant Difference |
|---|---|---|---|
| Entamoeba histolytica/dispar | 1/100 (9 cysts) | 1/100 (7 cysts) | Yes (p<0.05) |
| Giardia intestinalis | 1/20 | 1/20 | No |
| Entamoeba coli | 1/100 (3 cysts) | 1/100 (2 cysts) | Yes (p<0.05) |
Table 2: Comparative Detection Thresholds of Concentration Methods for Helminths
| Parasite | EasyPara (Last Positive Dilution) | Para-Selles (Last Positive Dilution) | Significant Difference |
|---|---|---|---|
| Ascaris lumbricoides | 1/10 | 1/10 | No |
| Taenia solium | 1/10 | 1/10 | No |
| Strongyloides stercoralis | 1/100 | 1/100 | Yes (p<0.05) |
Table 3: Overall Method Comparison for High-Throughput Applications
| Parameter | Commercial Kits | In-House Procedures |
|---|---|---|
| Standardization | High (standardized components) | Variable (requires quality control) |
| Cost per Test | Generally higher | Generally lower |
| Technical Complexity | Often simplified with proprietary devices | Multiple steps requiring technical expertise |
| Flexibility | Limited to manufacturer's design | Highly customizable for specific research needs |
| Solvent Requirements | Some are solvent-free (e.g., EasyPara) | Often require organic solvents (e.g., ethyl acetate) |
| Recovery Efficiency | Variable between brands and parasite species | Can be optimized for specific parasites |
Experimental Protocols for Method Validation
Side-by-Side Comparison Protocol
For researchers validating concentration methods for high-throughput applications, the following protocol provides a standardized approach for comparative evaluation:
Sample Preparation: Create a polyparasitized artificial stool sample by pooling clinical specimens containing target parasites (protozoa and helminths). Include Giardia intestinalis cysts, Entamoeba histolytica/dispar cysts, Ascaris lumbricoides eggs, and Strongyloides stercoralis larvae to represent different morphological forms [101].
Dilution Series: Prepare serial dilutions (½, ¼, 1/10, 1/20, 1/100, 1/400) in 0.9% sodium chloride solution to simulate varying parasite densities [101].
Parallel Processing: Process each dilution with both commercial and in-house methods according to their standardized protocols. For commercial kits, strictly follow manufacturer instructions. For in-house methods, use established laboratory protocols.
Microscopic Analysis: Resuspend obtained pellets in 0.9% sodium chloride solution. Prepare slides and examine under microscope at 10X and 40X magnifications. Count all cysts, eggs, and larvae in the entire suspension.
Statistical Analysis: Apply appropriate statistical tests (e.g., paired Student's t-test on log-transformed values) to compare recovery rates between methods at each dilution level [101].
Integrated DAF-AI Workflow for High-Throughput Screening
The dissolved air flotation (DAF) technique coupled with artificial intelligence represents an emerging approach for high-throughput screening applications:
DAF-AI Workflow for Parasite Concentration and Detection
This integrated approach has demonstrated a 73% slide positivity rate with DAF processing using 7% CTAB surfactant, compared to 57% positivity with the modified TF-Test technique [102]. When coupled with automated diagnosis of intestinal parasites (DAPI) systems, this method achieved a sensitivity of 94% with substantial agreement (kappa = 0.80) compared to conventional methods [102].
Troubleshooting Guides & FAQs
Common Experimental Challenges and Solutions
Table 4: Troubleshooting Common Concentration Method Issues
| Problem | Potential Causes | Solutions |
|---|---|---|
| Low parasite recovery in commercial kits | Incompatible solvent systems | Verify kit suitability for target parasites; procedures with biphasic solvents generally show higher performance [100] |
| Inconsistent results between operators | Variable technique in manual steps | Implement standardized training; consider automated processing systems |
| Poor morphological preservation | Improper fixative or prolonged storage | Use complementary preservatives (10% formalin for helminths, PVA for protozoa) [103] |
| High debris in concentrated samples | Inadequate filtration or washing | Optimize filtration steps; consider gradient-based systems like EasyPara [101] |
| Inhibitors affecting downstream molecular analysis | Carry-over of organic solvents | Incorporate additional washing steps; validate DNA extraction protocols |
Frequently Asked Questions
Q: Which concentration method shows better performance for low parasite densities? A: Studies indicate that for preconcentration specimens that tested negative, a homemade procedure was most effective, though two of four commercial kits performed satisfactorily for routine applications [100]. The optimal choice depends on the specific parasite targets and their densities.
Q: How do solvent-free commercial kits compare to traditional sedimentation methods? A: Solvent-free kits like EasyPara demonstrate significantly better recovery for certain parasites including Entamoeba histolytica/dispar and Strongyloides stercoralis larvae, while showing comparable performance for others like Giardia intestinalis cysts and Ascaris lumbricoides eggs [101].
Q: What preservation method is optimal for combined microscopic and molecular applications? A: No single preservative is ideal for all applications. 10% formalin provides good morphological preservation for helminths and is suitable for concentration procedures, while PVA is superior for protozoan trophozoites and permanent stained smears [103]. For molecular work, specific preservatives like SAF or one-vial fixatives may be more appropriate.
Q: How can we improve consistency between operators in high-throughput settings? A: Implementing standardized protocols with detailed specifications for each step (vortexing time, centrifugation speed, sample volumes) improves consistency. Additionally, regular proficiency testing and transition to automated systems like DAF can reduce operator-dependent variability [102].
Q: What is the optimal approach for integrating concentration methods with automated screening platforms? A: The DAF protocol combined with AI-based image analysis (DAPI system) shows promise for high-throughput applications, achieving 94% sensitivity with substantial agreement (kappa = 0.80) compared to conventional methods [102]. This approach standardizes the pre-analytical phase and enables automated analysis.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 5: Key Research Reagent Solutions for Parasite Concentration
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| CTAB Surfactant | Enhances parasite recovery in flotation | 7% concentration shown optimal in DAF protocols [102] |
| Ethyl Acetate | Organic solvent for sedimentation | Replaces ether in modern safety-conscious protocols [101] |
| 10% Formalin | All-purpose fixative | Ideal for helminth eggs/larvae; compatible with concentration procedures and immunoassays [103] |
| LV-PVA | Preservation of protozoan morphology | Superior for trophozoites and permanent stained smears [103] |
| Porosity Gradient Filters | Debris removal and parasite retention | 200-400 μm filters in EasyPara improve recovery [101] |
| S.T.A.R. Buffer | Stool transport and recovery | Optimized for molecular applications and DNA preservation [104] |
| DAF System | Automated parasite flotation | Includes saturation chamber, compressor, and tube rack for standardized processing [102] |
Emerging Methodologies and Future Directions
The field of parasitological diagnostics is rapidly evolving with several emerging technologies showing promise for high-throughput screening applications. Artificial intelligence approaches, particularly deep-learning models like DINOv2-large and YOLOv8-m, have demonstrated remarkable accuracy in parasite identification, with DINOv2-large achieving 98.93% accuracy, 84.52% precision, and 78.00% sensitivity [105]. These systems can significantly reduce analysis time and operator dependency while maintaining high diagnostic performance.
Molecular techniques, particularly multiplex real-time PCR assays, continue to advance with commercial platforms like the Allplex GI-Parasite Assay showing excellent performance characteristics including 100% sensitivity and specificity for Entamoeba histolytica and 100% sensitivity and 99.2% specificity for Giardia duodenalis [106]. While molecular methods currently complement rather than replace conventional microscopy in most settings, they offer particular advantages for species differentiation and high-throughput applications where traditional morphological expertise may be limited.
For research and drug development professionals, the optimal approach often involves a hybrid strategy that leverages the standardized processing of commercial concentration kits with emerging detection technologies. This integration enables more efficient, reproducible, and scalable parasite screening while addressing the specific requirements of high-throughput research environments.
Correlating Parasite Intensity with Molecular Detection Thresholds (Ct Values)
Core Concepts: Parasite Load and Ct Value Relationship
Table 1: Correlation between Parasite Intensity and qPCR Ct Values in Selected Parasites
| Parasite Species | Sample Type | Diagnostic Method | Correlation with Ct Value | Key Findings | Citation |
|---|---|---|---|---|---|
| Plasmodium falciparum | Dried Blood Spots (DBS) | pfldh qPCR vs. Microscopy | Inverse Correlation | qPCR detected ~4.6x more infections (10.7%) than microscopy (2.3%); lower Ct values indicate higher parasite density. [107] | |
| Plasmodium spp. | Used Rapid Diagnostic Tests (RDTs) | Duplex qPCR vs. DBS qPCR | Strong Inverse Correlation (r=0.78, p<0.001) | Parasite density quantification from used RDTs is feasible and correlates well with standard DBS methods across a range of densities. [108] | |
| Trichuris trichiura | Ethanol-preserved Stool | qPCR vs. Kato-Katz (KK) | Complex Inverse Correlation | qPCR and KK show parallel efficacy patterns post-treatment; concordance decreases in low-intensity infections due to reduced KK sensitivity. [109] |
The Cycle Threshold (Ct) value is the number of amplification cycles required for a qPCR signal to cross a predefined threshold. It is inversely correlated with the amount of target DNA in the original sample: a low Ct value indicates a high quantity of parasite DNA (high parasite intensity), while a high Ct value indicates a low quantity (low parasite intensity). [107] [109] [108]
This relationship is foundational for high-throughput screening, allowing researchers to rapidly quantify parasite burden and assess drug efficacy. Molecular methods like qPCR are significantly more sensitive than traditional microscopy, especially for detecting low-intensity, submicroscopic infections crucial for accurate screening outcomes. [107]
Troubleshooting Guides & FAQs
No or Late Amplification (High Ct Values)
Q: My qPCR results show no amplification or unusually late Ct values. What could be the cause and how can I fix it?
- Potential Cause: PCR inhibitors from complex biological samples (stool, blood).
- Solution:
- Dilute the Template: Diluting the sample DNA can dilute inhibitors to a non-inhibitory concentration. [110] [111]
- Add BSA: Adding Bovine Serum Albumin (BSA) at 0.4 – 4.4 mg/ml to the reaction can bind to and neutralize common inhibitors. [110]
- Optimize DNA Extraction: Use extraction kits validated for your sample type (e.g., stool kits designed to remove inhibitors) and ensure proper washing steps. [109] [112]
- Verify DNA Quality: Check DNA concentration and purity (A260/A280 ratio). Degraded DNA or low concentration will lead to high Ct values. [112] [111]
Non-Specific Amplification
Q: I am observing multiple peaks in my melt curve or non-specific amplification. How do I resolve this?
- Potential Cause: Poorly designed primers leading to primer-dimer formation or non-specific binding.
- Solution:
- Redesign Primers: Use software like Primer3 or NCBI Primer-BLAST to design primers with high specificity. [112]
- Use a Hot-Start Taq Polymerase: This prevents premature enzyme activity during reaction setup, reducing non-specific amplification. [112]
- Include a Melt Curve Analysis: This is essential for SYBR Green-based assays to identify non-specific products or primer-dimers, which typically melt at lower temperatures than the specific product. [112] [111]
Inconsistent Results Across Replicates
Q: My biological replicates show high variability in Ct values. What should I check?
- Potential Cause: Inconsistent sample quality, pipetting errors, or minimal starting material.
- Solution:
- Check RNA/DNA Quality: Prior to reverse transcription (for RNA targets), check concentration and quality with a spectrophotometer and/or gel electrophoresis. [111]
- Repeat Nucleic Acid Isolation: If quality is poor, repeat the extraction with a method more suited to your sample matrix. [111]
- Improve Pipetting Technique: Prepare samples in technical triplicates, ensure pipettes are calibrated, and create fresh serial dilutions for standard curves. [111]
Contamination and False Positives
Q: I am detecting amplification in my No-Template Control (NTC). What is the source and how do I decontaminate?
- Potential Cause: Contaminated reagents, aerosol contamination during pipetting, or primer-dimer formation.
- Solution:
- Use Separate Work Areas: Physically separate areas for sample preparation, PCR setup, and post-PCR analysis. [112]
- Decontaminate Workspace: Clean benches and pipettes with 10% bleach or 70% ethanol. [112] [111]
- Prepare Fresh Reagents: Make new primer dilutions and use new master mix components if contamination is suspected. [111]
- Strategic Plate Layout: Place NTC wells away from high-concentration sample wells to prevent splashing or aerosol cross-contamination. [111]
Experimental Protocols for Correlation Studies
Protocol 1: Validating Parasite Density via qPCR from Dried Blood Spots
This protocol is adapted from studies quantifying Plasmodium parasite density. [107] [108]
1. Sample Collection and DNA Extraction:
- Collection: Apply 50 μL of peripheral blood to Whatman FTA filter paper. Air-dry completely and store in a sealed bag with desiccant. [107]
- Extraction: Use a robotic or manual system with a dedicated kit (e.g., QIAsymphony SP/AS with the "Investigator" or "Blood" kit, or QIAamp DNA Mini Kit). Incubate the blood spot with buffer MTL with continuous mixing at 70°C for 1 hour before the automated extraction program. Elute DNA in 100 μL of elution buffer. [107] [108]
2. Real-time PCR Setup:
- Reaction Mix (25 μL total volume):
- 12.5 μL Universal PCR Master Mix
- Forward and Reverse Primers (e.g., pfldh): 250 nM each
- TaqMan Probe (e.g., pfldh): 300 nM
- 1-2 μL of extracted gDNA
- Molecular-grade water to volume [107]
- Cycling Conditions:
- Hold: 50°C for 2 min, 95°C for 10 min
- 40 Cycles: 95°C for 15 sec, 60°C for 1 min [107]
- Controls: Include a standard curve of known parasite genomic DNA (e.g., 10, 1, 0.1, 0.01 ng/μL) for quantification, a no-template control (NTC), and a negative human DNA control. [107] [108]
3. Data Analysis:
- Determine the Ct value for each sample.
- Use the standard curve to interpolate the parasite density (parasites/μL) from the Ct value. [108]
- Compare qPCR-derived densities with counts from microscopy (thick blood smears) for validation. [107]
Protocol 2: High-Throughput Image-Based Antimalarial Screening
This protocol supports the integration of phenotypic screening with molecular validation. [18]
1. In Vitro Culture and Compound Treatment:
- Culture synchronized Plasmodium falciparum asexual stages (e.g., strain 3D7) in human O+ RBCs at 2% hematocrit and 1% parasitemia (schizont stage). [18]
- Dispense cultures into 384-well plates pre-dispensed with compounds from a library. Test compounds at a single concentration (e.g., 10 μM) or in a dose-dependent manner. [18]
- Incubate plates for 72 hours at 37°C in a mixed-gas chamber (1% O₂, 5% CO₂, balanced N₂). [18]
2. Staining and Image Acquisition:
- After incubation, dilute the culture to 0.02% hematocrit in PhenolPlate 384-well microplates. [18]
- Stain with a solution containing:
- 1 µg/mL wheat agglutinin–Alexa Fluor 488 (stains RBCs)
- 0.625 µg/mL Hoechst 33342 (stains nucleic acids)
- 4% paraformaldehyde (fixes the culture)
- Incubate for 20 minutes at room temperature. [18]
- Acquire nine microscopy image fields per well using a high-content imaging system (e.g., Operetta CLS with a 40x water immersion lens). [18]
3. Image and Data Analysis:
- Transfer images to analysis software (e.g., Columbus).
- Use algorithms to classify and count infected vs. non-infected RBCs based on fluorescence.
- Calculate percentage inhibition of parasite growth for each compound well.
- Hits from this primary screen can be advanced for further molecular analysis, including qPCR to confirm parasite reduction and determine Ct values for residual parasite load. [18]
Workflow and Pathway Visualizations
High-Throughput Parasite Screening & Ct Correlation Workflow
Troubleshooting Guide for Abnormal Ct Values
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for qPCR-Based Parasite Detection and Quantification
| Reagent / Material | Function / Application | Example Use Case | Citation |
|---|---|---|---|
| Whatman FTA Cards | Collection and preservation of blood samples for DNA stabilization at room temperature. | Collection of peripheral blood for Plasmodium DNA analysis and long-term storage. [107] [108] | |
| QIAamp DNA Mini Kit / QIAsymphony | Silica-membrane based extraction of high-quality genomic DNA from complex samples (blood, stool). | Robust DNA extraction from dried blood spots or inhibitor-rich stool samples for sensitive qPCR. [107] [109] | |
| Bovine Serum Albumin (BSA) | Additive to qPCR reactions that binds to and neutralizes common PCR inhibitors. | Improving amplification efficiency from difficult samples like stool, leading to more reliable Ct values. [110] | |
| TaqMan Probes (FAM/VIC) | Sequence-specific fluorescent probes for highly specific detection in multiplex qPCR assays. | Duplex qPCR for simultaneous quantification of Plasmodium DNA and human DNA (internal control) from a single sample. [107] [108] | |
| Universal PCR Master Mix | Optimized buffer, enzymes, and dNTPs for efficient and robust qPCR amplification. | Standardized reaction setup for high-throughput screening of compound libraries against parasite cultures. [107] [18] |
Conclusion
High-throughput parasite screening methodologies represent a transformative advancement in parasitology, enabling unprecedented scalability in drug discovery and diagnostic precision. The integration of ultrasensitive molecular techniques like high-volume qPCR, sophisticated phenotypic platforms such as real-time motility monitoring, and automated high-content imaging has dramatically improved our capacity to detect low-density infections, identify novel therapeutic candidates, and track resistance emergence. Future directions will focus on further miniaturization, integration of artificial intelligence for data analysis, development of multiplexed point-of-care diagnostics, and the creation of more complex physiological models using stem cell technologies. These innovations will ultimately accelerate the development of urgently needed new anthelmintics and antiprotozoal agents while enhancing global capacity for monitoring and containing drug-resistant parasites, fundamentally advancing both biomedical research and clinical practice in parasitic disease management.
References
- 1. High-throughput screening [https://en.wikipedia.org/wiki/High-throughput_screening]
- 2. high throughput technologies applied to parasitology [https://pubmed.ncbi.nlm.nih.gov/16454900/]
- 3. high throughput technologies applied to parasitology [https://www.ovid.com/journals/paras/pdf/00006407-200410001-00008~screening-and-synthesis-high-throughput-technologies-applied]
- 4. Evolution of Ultra-High-Throughput Screening [https://www.labmanager.com/evolution-of-ultra-high-throughput-screening-17974]
- 5. Ultra High Throughput Screening (uHTS) Applications [https://lifesciences.danaher.com/us/en/application/high-throughput-screening-drug-discovery.html]
- 6. A multiplexed high throughput screening assay using flow ... [https://www.sciencedirect.com/science/article/pii/S2211320724000381]
- 7. High Throughput Screening - an overview [https://www.sciencedirect.com/topics/chemistry/high-throughput-screening]
- 8. Technological advances in high-throughput screening [https://pubmed.ncbi.nlm.nih.gov/15287820/]
- 9. High-Throughput Screening of More Than 30000 Compounds ... [https://pubmed.ncbi.nlm.nih.gov/39653369/]
- 10. Automated Liquid Handlers As Sources of Error [https://www.bioprocessintl.com/assays/automated-liquid-handlers-as-sources-of-error]
- 11. Your liquid handling robot is broken. Or is it? (Part 2) [https://www.aicompanies.com/education-training/knowledge-center/your-liquid-handling-robot-is-broken-or-is-it-part-2/]
- 12. How to Troubleshoot a Robot [https://www.nrtcautomation.com/blog/how-to-troubleshoot-a-robot]
- 13. Troubleshooting Common Robot Problems [https://www.acieta.com/blog/robot-troubleshooting/]
- 14. Troubleshooting Industrial Robots: Skills Technicians Need [https://www.uti.edu/blog/robotics-and-automation/troubleshooting-industrial-robots-skills]
- 15. 5 Common Liquid Handling Errors and How to Prevent Them [https://pipettetips.com/blogs/blog/5-common-liquid-handling-errors-and-how-to-prevent-them?srsltid=AfmBOooj4NNAcnC80LNSJuQj4opmXjh6lb2oaNSbZ4VEie5lcOdBOZU8]
- 16. High-throughput detection of parasites and ova in stool using ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-023-06108-1]
- 17. High-Throughput Screening Platforms in the Discovery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7926814/]
- 18. High-throughput screening and meta-analysis for lead ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590855/]
- 19. 384 Well Plate vs. 96 Well Plate Choosing the Right Plate [https://pipette.com/solutions/384-well-plate-vs-96-well-plate-choosing-the-right-plate?srsltid=AfmBOooBFeXdmiEnk3nqypMim944YwG11e_jEN0INmpP53RgfRgKTh3L]
- 20. The microplate: utility in practice [https://www.bmglabtech.com/en/the-microplate-utility-in-practice/]
- 21. High-Throughput Screening - Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/high-throughput-screening-principles-applications-and-advancements-405121]
- 22. Optical density and absorbance measurements [https://www.bmglabtech.com/en/blog/optical-density-for-absorbance-assays/]
- 23. SpectraMax ABS & ABS Plus Absorbance ELISA Readers [https://www.moleculardevices.com/products/microplate-readers/absorbance-readers/spectramax-abs-plate-readers]
- 24. Bisulfite Conversion for Illumina Methylation Arrays [https://www.zymoresearch.com/blogs/blog/bisulfite-conversion-for-illumina-methylation-arrays?srsltid=AfmBOoopVyLQS90fZZN_h0NUkagKx9x9bljovuZzz3rvmiVdkFh6wwuW]
- 25. Ligation sequencing gDNA - Native Barcoding Kit 24 V14 ... [https://nanoporetech.com/document/ligation-sequencing-gdna-native-barcoding-v14-sqk-nbd114-24]
- 26. High-throughput screening identifies novel chemical ... [https://pubmed.ncbi.nlm.nih.gov/40610818/]
- 27. Assay Guidance Manual - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK53196/]
- 28. High-Throughput Screening (HTS): A Simple Guide ... [https://www.chemcopilot.com/blog/hts-material-discovery]
- 29. Resources for Assay Development and High Throughput ... [https://drugdiscovery.msu.edu/facilities/addrc/resources-for-assay-development-and-high-throughput-screening.aspx]
- 30. Stool Specimens – Detection of Parasite Antigens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/antigendetection.html]
- 31. Recent advancements in the diagnosis of parasitic diseases [https://www.sciencedirect.com/science/article/abs/pii/S0166685125000428]
- 32. Scalable signature-based molecular diagnostics through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7785517/]
- 33. DPDx - Resources for Parasitic Diseases [https://www.cdc.gov/dpdx/reference.html]
- 34. High-Throughput Ultrasensitive Molecular Techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4313154/]
- 35. Sensitive and accurate quantification of human malaria ... [https://www.nature.com/articles/srep39183]
- 36. Malaria Diagnostic Tests [https://www.cdc.gov/malaria/hcp/diagnosis-testing/malaria-diagnostic-tests.html]
- 37. RDT performance through high-throughput bead-based ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1598280/full]
- 38. Global malaria diagnostic testing programme [https://www.who.int/teams/global-malaria-programme/case-management/diagnosis]
- 39. Design and Application of a High-Throughput ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10782576/]
- 40. TriTOX: A novel Trichomonas vaginalis assay platform for ... [https://www.sciencedirect.com/science/article/pii/S2211320721000014]
- 41. A Novel High Throughput Assay for Anthelmintic Drug Screening and Resistance Diagnosis by Real-Time Monitoring of Parasite Motility - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2982823/]
- 42. A Novel High Throughput Assay for Anthelmintic Drug Screening and Resistance Diagnosis by Real-Time Monitoring of Parasite Motility | PLOS Neglected Tropical Diseases [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0000885]
- 43. Evaluation of nematode susceptibility and resistance to ... [https://www.nature.com/articles/s41598-025-02866-3]
- 44. High-content approaches to anthelmintic drug screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC8364491/]
- 45. High-content approaches to anthelmintic drug screening [https://www.sciencedirect.com/science/article/abs/pii/S1471492221001136]
- 46. Mobile Diagnostics Based on Motion? A Close Look at Motility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4931419/]
- 47. Motility-based label-free detection of parasites in bodily ... [https://www.nature.com/articles/s41377-018-0110-1]
- 48. Antimalarial Drug Resistance Profiling of Plasmodium ... [https://pubmed.ncbi.nlm.nih.gov/37066213/]
- 49. Antimalarial drug resistance profiling of Plasmodium ... [https://www.frontiersin.org/journals/malaria/articles/10.3389/fmala.2024.1363969/full]
- 50. High throughput resistance profiling of Plasmodium ... [https://www.nature.com/articles/s41598-017-02724-x]
- 51. Evaluation of different concentration techniques for microscopic diagnosis of protozoa and helminths in stool samples of children - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922389/]
- 52. Evaluation of Commercial Concentration Methods for Microscopic Diagnosis of Protozoa and Helminths in Human Stool Samples in a Non-Endemic Area - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9230666/]
- 53. Comparison of different methods for the detection of intestinal protozoa and helminths in stool - PubMed [https://pubmed.ncbi.nlm.nih.gov/741504/]
- 54. Comparative analysis of commercial and “In-House†molecular tests for the detection of intestinal protozoa in stool samples | Parasites & Vectors | Full Text [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 55. Prevalence of intestinal parasites and comparison of detection techniques for soil-transmitted helminths among newly arrived expatriate labors in Jeddah, Saudi Arabia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823990/]
- 56. An automated high-throughput system for phenotypic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5734697/]
- 57. The Z prime value (Z´) [https://www.bmglabtech.com/en/blog/the-z-prime-value/]
- 58. Assay Validation in High Throughput Screening [https://www.intechopen.com/chapters/48130]
- 59. Z' Does Not Need to Be > 0.5 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7509605/]
- 60. Calculating a Z-factor to assess the quality of a screening ... [https://www.graphpad.com/support/faq/calculating-a-z-factor-to-assess-the-quality-of-a-screening-assay/]
- 61. Troubleshooting & FAQs [https://www.cygnustechnologies.com/resources/guidelines?srsltid=AfmBOoqm9TJjujyN19qqoKlNgh21jerlk60ge2_o9hXhswRweFPYt4uC]
- 62. Development and application of a high - throughput assay... screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC7645381/]
- 63. - High phenotypic throughput identifies a new... | PLOS One screen [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0280232]
- 64. Checking Dispensing Volume - liquid-handling [https://labautomation.io/t/checking-dispensing-volume/2933]
- 65. How Automation Overcomes Variability & Limitations in ... [https://dispendix.com/blog/how-automation-overcomes-variability-limitations-in-hts-troubleshooting]
- 66. High Throughput Screening Market [https://www.futuremarketinsights.com/reports/high-throughput-screening-market]
- 67. Expert Advice: Navigating reagent dispensing [https://www.drugdiscoverynews.com/expert-advice-navigating-reagent-dispensing-15798]
- 68. How to Optimize Microplate Washing for ELISA and Cell- ... [https://www.labx.com/resources/how-to-optimize-microplate-washing-for-elisa-and-cell-based-assays/5573]
- 69. Dispensette® Testing Instructions (SOP) [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/analytical-chemistry/wet-chemical-analysis/dispensette-testing-instructions-sop?srsltid=AfmBOorxrEEGEC3vn1d7vzUYTErZp4fNhKji4QghIOowJGYFM3IOQP60]
- 70. DISPENDIX Source Plates: The Key To Precise Dispensing [https://dispendix.com/blog/dispendix-source-plates-the-key-to-precise-dispensing]
- 71. Microplate-in-a-Box: thermophysical exploration of cold ... [https://www.sciencedirect.com/science/article/pii/S001122402500104X]
- 72. Factors Influencing Transfection Efficiency [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/transfection-basics/factors-influencing-transfection-efficiency.html]
- 73. A systematic comparison of in-house prepared transfection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603952/]
- 74. High Throughput Screening Market Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/high-throughput-screening-market]
- 75. RNAi screening: tips and techniques - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3036573/]
- 76. A Decade of RNAi Screening: Too much hay and very few ... [https://www.ddw-online.com/a-decade-of-rnai-screening-too-much-hay-and-very-few-needles-676-201308/]
- 77. Heterogeneity in an adeno-associated virus transfection ... [https://www.nature.com/articles/s41598-025-26261-0]
- 78. High Throughput Screening Assays for Drug Discovery [https://bellbrooklabs.com/high-throughput-screening-assays-drug-discovery/?srsltid=AfmBOorOCoJ0ADSYTRSlHK4m5Nyj1xP-D2W84JXiMSnIBDbJ27KsyRjo]
- 79. CRISPRâ€driven diagnostics: Molecular mechanisms, clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464570/]
- 80. Ultrasensitive detection of clinical pathogens through a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032082/]
- 81. Introducing AVAC as an ultra-sensitive platform with broad ... [https://www.nature.com/articles/s41598-025-88992-4]
- 82. Highly Sensitive Detection and Molecular Subtyping of ... [https://www.sciopen.com/article/10.26599/NBE.2025.9290113]
- 83. Comparative evaluation of real-time polymerase chain ... [https://pubmed.ncbi.nlm.nih.gov/39493490/]
- 84. Comparative study on conventional and real-time PCR ... [https://www.sciencedirect.com/science/article/pii/S2950194624000335]
- 85. Assessment of conventional PCR and real-time ... [https://www.sciencedirect.com/science/article/pii/S1413867017305135]
- 86. AI System Outperforms Human Detection of Parasites in ... [https://clpmag.com/disease-states/infectious-diseases/gastrointestinal-infections/ai-system-outperforms-human-detection-parasites-stool-samples/]
- 87. A highly sensitive and specific real-time quantitative ... [https://www.nature.com/articles/s41598-024-76822-y]
- 88. Infectious disease diagnostic device using rapid and ... [https://www.nature.com/articles/s41378-025-00972-w]
- 89. A Comparative Study of Broad-Range Real-Time PCR and ... [https://www.mdpi.com/2075-4418/15/8/966]
- 90. PCR vs qPCR Sensitivity [https://bitesizebio.com/2641/pcr-vs-qpcr-sensitivity/]
- 91. Quantitative Real-Time PCR Is Not More Sensitive than “ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2446855/]
- 92. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 93. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 94. Advantages and Limitations of Microscopy and Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9979072/]
- 95. Diagnostic Techniques of Soil-Transmitted Helminths [https://www.mdpi.com/2414-6366/5/2/93]
- 96. Advantages and limitations of microscopy and molecular... [https://sciendo.com/fr/article/10.2478/helm-2022-0034?tab=article]
- 97. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimenproc.html]
- 98. A historical review of the techniques of recovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7269538/]
- 99. Effective Laboratory Diagnosis of Parasitic Infections of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11475984/]
- 100. Evaluation of Comparative Procedures... Commercial Concentration [https://pubmed.ncbi.nlm.nih.gov/30590699/]
- 101. Diagnosis of Intestinal Parasitoses: Comparison of Two Commercial [https://www.longdom.org/open-access/diagnosis-of-intestinal-parasitoses-comparison-of-two-commercial-methods-for-faecal-concentration-using-a-polyparasitize-35303.html]
- 102. Laboratory validation of the automated diagnosis of intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11363502/]
- 103. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimencoll.html]
- 104. Performance Comparison of In-House and Commercial ... [https://www.mdpi.com/2075-4418/15/22/2928]
- 105. Performance validation of deep-learning-based approach in ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06878-w]
- 106. Evaluation of Allplex™ GI-Parasite Assay—A Multiplex Real ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390207/]
- 107. Comparison of real-time PCR and microscopy for malaria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2984567/]
- 108. Molecular quantification of Plasmodium parasite density ... [https://www.nature.com/articles/s41598-019-41438-0]
- 109. Assessing the diagnostic value of qPCR for Trichuris trichiura [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1679294/full]
- 110. General troubleshooting for low product or late Ct values [https://pcrbio.com/resources/faqs/lyo-ready-probe-1-step-kit/general-troubleshooting-for-low-product-or-late-ct-values-2/]
- 111. qPCR Troubleshooting Guide [https://azurebiosystems.com/qpcr-resources/troubleshooting/]
- 112. Common Pitfalls and How to Troubleshoot Your Results - qpcr [https://qpcr.odoo.com/blog/news-2/qpcr-in-parasitology-common-pitfalls-and-how-to-troubleshoot-your-results-3]