Fecal Antigen vs. Fecal Elastase Testing: Head-to-Head Diagnostic Performance in Pediatric Diarrhea
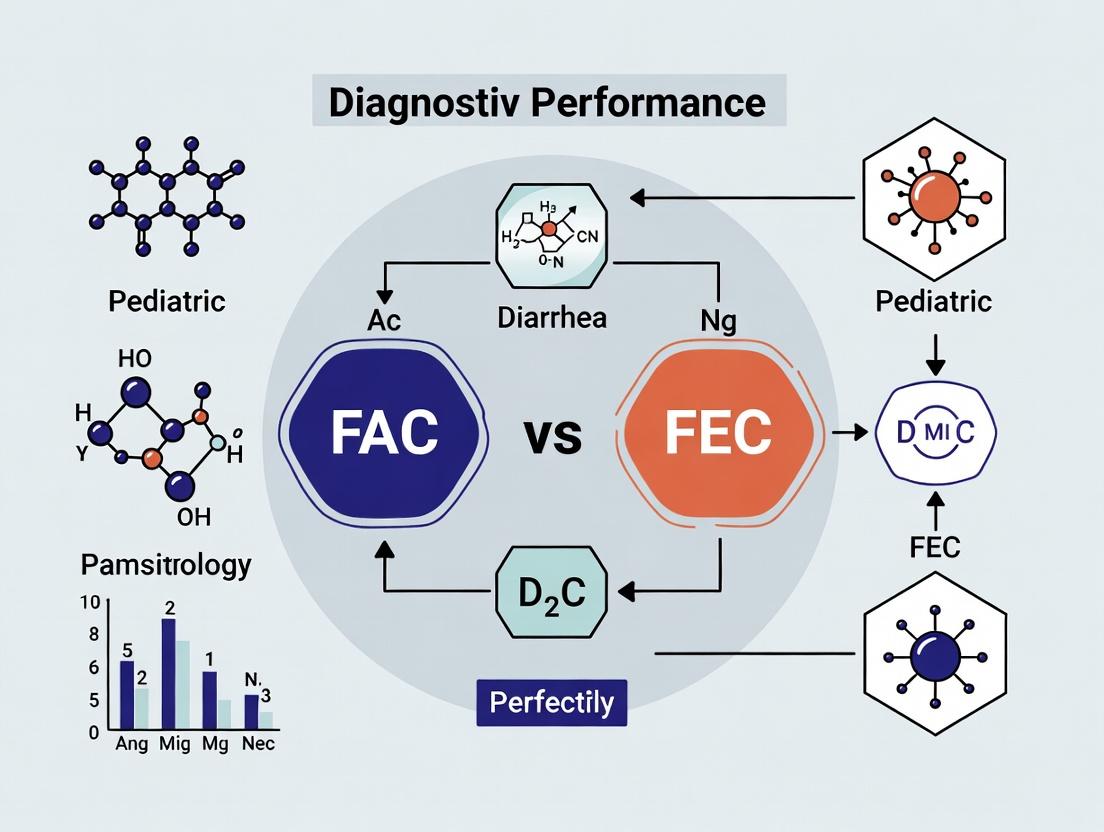
This analytical review compares the diagnostic accuracy, clinical utility, and application of Fecal Antigen (FAC) tests and Fecal Elastase-1 (FEC) tests in pediatric patients with chronic or severe acute diarrhea.
Fecal Antigen vs. Fecal Elastase Testing: Head-to-Head Diagnostic Performance in Pediatric Diarrhea
Abstract
This analytical review compares the diagnostic accuracy, clinical utility, and application of Fecal Antigen (FAC) tests and Fecal Elastase-1 (FEC) tests in pediatric patients with chronic or severe acute diarrhea. Targeting researchers and drug development professionals, it explores the pathophysiological basis for each biomarker, details current methodologies and standard protocols, analyzes common challenges and optimization strategies in sample handling and interpretation, and provides a critical, evidence-based comparison of sensitivity, specificity, and predictive values. The article synthesizes findings to guide optimal test selection in clinical research, inform biomarker-driven drug development, and outline future directions for non-invasive pediatric gastroenterology diagnostics.
Pathophysiology and Biomarker Basis: Understanding FAC and FEC in the Pediatric Gut
Within pediatric diarrheal disease research, differential diagnosis is critical for targeted intervention. This guide compares the diagnostic targets of infectious etiologies—viral and bacterial antigens—against the non-infectious target of pancreatic enzyme insufficiency (PEI), specifically fecal elastase-1. The performance of fecal antigen concentration (FAC) assays for pathogens versus fecal elastase concentration (FEC) for PEI is analyzed within a thesis framework evaluating FAC vs. FEC diagnostic utility in pediatric patients.
Target Comparison and Diagnostic Performance
Table 1: Core Diagnostic Targets and Assay Performance
| Target Category | Specific Target | Typical Assay Format | Diagnostic Purpose | Key Performance Metric (Typical Range) | Common Sample Type |
|---|---|---|---|---|---|
| Viral Antigen | Rotavirus VP6 antigen | Lateral Flow Immunoassay (LFI), ELISA | Detect active infection | Sensitivity: 85-98%; Specificity: 90-100% | Fresh stool |
| Viral Antigen | Norovirus GI/GII capsid antigen | LFI, ELISA | Detect active infection | Sensitivity: 50-90%; Specificity: 75-100% | Fresh stool |
| Bacterial Antigen | Campylobacter spp. surface antigens | LFI, Immunoassay | Detect active infection | Sensitivity: 70-95%; Specificity: 95-99% | Fresh stool |
| Bacterial Antigen | E. coli O157 LPS antigen | Immunoassay, LFI | Detect STEC infection | Sensitivity: >90%; Specificity: >99% | Fresh stool or broth culture |
| Pancreatic Enzyme | Fecal Elastase-1 (FE1) | Monoclonal ELISA, CLIA | Diagnose PEI | Sensitivity for severe PEI: 90-100%; Specificity: 90-96% | Fresh or frozen stool |
Table 2: Comparative Analytical Characteristics in Pediatric Diarrhea
| Parameter | FAC (Pathogen-Specific) | FEC (Elastase-1) |
|---|---|---|
| Analytical Goal | Qualitative/Semi-quantitative detection of pathogen-associated molecules. | Quantitative measurement of pancreatic enzyme concentration. |
| Turnaround Time | 10-30 mins (LFI), 2-4 hrs (ELISA). | 2-5 hours (ELISA/CLIA). |
| Interference Factors | High mucus content, heterophilic antibodies, cross-reactivity with related strains. | Dilute/watery stool (false low), intestinal bleeding, non-pancreatic proteases. |
| Correlation with Disease Activity | Direct correlation with active infection. | Inverse correlation with pancreatic function; not acute phase reactant. |
| Role in FAC vs. FEC Thesis | FAC panel defines infectious etiology, guiding antimicrobial/ supportive therapy. | FEC identifies malabsorptive diarrhea, guiding enzyme replacement therapy. |
Experimental Protocols for Key Assays
Protocol 1: Multiplex Lateral Flow Immunoassay for Viral/Bacterial Antigens (FAC)
Objective: Simultaneous detection of Rotavirus, Norovirus, Campylobacter, and E. coli O157 antigens from stool supernatant. Methodology:
- Sample Preparation: Emulsify 100-200 mg stool in 1 mL manufacturer's extraction buffer. Centrifuge at 10,000 x g for 2 minutes. Collect supernatant.
- Assay Procedure: Apply 100 µL supernatant to the sample port of the multiplex LFI cassette. Allow capillary flow for 15 minutes at room temperature.
- Detection: Visually inspect test and control lines. Use a dedicated reader for optical density of each line for semi-quantitation.
- Interpretation: A positive control line must appear. Test line intensity correlates with antigen concentration. Confirm positives with ELISA or PCR per validation protocol.
Protocol 2: Monoclonal ELISA for Fecal Elastase-1 (FEC)
Objective: Quantify human FE1 concentration in stool to diagnose pancreatic insufficiency. Methodology:
- Sample Extraction: Dilute stool specimen 1:500 in the provided sample dilution buffer. Homogenize thoroughly and centrifuge.
- ELISA Steps: a. Coat microwells with anti-human elastase-1 monoclonal capture antibody. b. Add 100 µL of calibrators, controls, and diluted samples to respective wells. Incubate 1 hour at 25°C. c. Wash 5x. Add 100 µL peroxidase-conjugated detection antibody. Incubate 1 hour at 25°C. d. Wash 5x. Add 100 µL TMB substrate. Incubate 30 minutes in the dark. e. Stop reaction with 100 µL 1M H₂SO₄. Read absorbance at 450 nm (reference 620 nm).
- Calculation: Generate a standard curve from calibrators. Calculate FE1 concentration in µg/g stool. Values <100 µg/g indicate severe PEI; 100-200 µg/g suggest moderate PEI.
Visualizing Diagnostic Pathways and Workflows
Diagram Title: Pediatric Diarrhea Diagnostic Decision Pathway
Diagram Title: FAC vs FEC Assay Signal Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Target Detection
| Reagent/Material | Function in FAC (Pathogen) | Function in FEC (Elastase) | Example Vendor/Product |
|---|---|---|---|
| Monoclonal Antibodies (mAbs) | Target-specific capture and detection (e.g., anti-RV VP6, anti-E. coli O157). | Capture and detection of human elastase-1 epitopes. | Meridian Bioscience, Abcam, Thermo Fisher. |
| Stool Extraction/Dilution Buffer | Lyse particles, solubilize antigens, inhibit proteases to preserve target integrity. | Standardize stool viscosity, solubilize FE1, prevent enzyme degradation. | Copan Diluent, In-house PBS-based with stabilizers. |
| Enzyme Conjugates (HRP/ALP) | Linked to detection mAbs for colorimetric/chemiluminescent signal generation in ELISA/LFI. | Same principle for competitive or sandwich ELISA format. | Jackson ImmunoResearch, Sigma-Aldrich. |
| Chromogenic Substrate (TMB/BCIP) | HRP or ALP substrate for visual or optical signal development. | Critical for endpoint measurement in ELISA. | KPL (SeraCare), Thermo Fisher. |
| Recombinant Antigens/Purified Proteins | Positive controls and calibrators for assay validation and standardization. | FE1 protein for generating the standard curve (0-500 µg/g). | ViroStat, MyBioSource, Immundiagnostik. |
| Multiplex Lateral Flow Strips | Solid-phase matrix with immobilized test and control lines for multi-target FAC. | Not typically used for FEC (quantitative ELISA preferred). | Chembio DPP, Boditech iChroma. |
| Microplate Washer/Reader | Automated washing of ELISA plates and precise optical density measurement. | Essential for high-throughput, quantitative FEC ELISA. | BioTek, Thermo Fisher Multiskan. |
The accurate identification of diarrheal pathogens in children is critical for public health surveillance, clinical management, and drug/vaccine development. This diagnostic landscape is uniquely challenging due to the diversity of potential etiologies (viral, bacterial, parasitic), the presence of mixed infections, and the high incidence of asymptomatic carriage in pediatric populations. Within this context, multiplex molecular diagnostic panels have become essential tools. This guide compares the performance of two leading syndromic panels: the FilmArray Gastrointestinal Panel (FAC) and the QIAstat-Dx Gastrointestinal Panel (FEC), within pediatric-focused research.
Performance Comparison: FAC vs. FEC in Pediatric Diarrhea Studies
Table 1: Overall Diagnostic Performance in Recent Pediatric Cohorts
| Metric | FilmArray GI Panel (FAC) | QIAstat-Dx GI Panel (FEC) | Notes |
|---|---|---|---|
| Number of Targets | 22 pathogens (13 bacteria, 5 viruses, 4 parasites) | 24 pathogens (15 bacteria, 5 viruses, 4 parasites) | FEC includes additional bacteria: Plesiomonas shigelloides, Vibrio cholerae. |
| Sample-to-Result Time | ~1 hour | ~1.5-2 hours | FAC workflow is largely hands-off after loading. |
| Sample Throughput | 1 sample per cartridge; batch processing possible but instrument-limited. | 1-4 samples per cartridge (QIAstat-Dx 1) or up to 8 (Dx 360), flexible batch size. | FEC offers higher throughput per run on specific systems. |
| Reported Sensitivity (vs. Reference PCR) | 94.6% - 99.5% (aggregate, varies by pathogen) | 95.1% - 100% (aggregate, varies by pathogen) | Both demonstrate high sensitivity; clinical significance of minor variations is pathogen-dependent. |
| Reported Specificity (vs. Reference PCR) | 99.3% - 99.9% (aggregate) | 98.8% - 99.8% (aggregate) | Both maintain high specificity, reducing false positives. |
| Key Pediatric Study (Example) | Piralla et al., JCM, 2021. N=147 pediatric stools. | Buss et al., Pathogens, 2023. N=180 pediatric stools. | Both studies highlight detection of coinfections. |
Table 2: Detection of Critical Pediatric Pathogens in Mixed Infections
| Pathogen Group | FilmArray GI Panel (FAC) Performance | QIAstat-Dx GI Panel (FEC) Performance | Implication for Pediatrics |
|---|---|---|---|
| Norovirus GII | High sensitivity; frequent detection in co-infections with bacteria. | Comparable high sensitivity; robust detection in multiplex. | Crucial for outbreak control and understanding disease burden. |
| Rotavirus | High correlation with monoplex PCR post-vaccine era. | High correlation; includes detection alongside other viruses. | Essential for monitoring vaccine impact and etiologic shifts. |
| *Shiga toxin-producing *E. coli (STEC)* | Detects stx1, stx2, and E. coli O157. Does not specify non-O157 serogroups. | Detects stx1, stx2, and eae; also includes E. coli O157 and top-6 non-O157 serogroups (O26, O45, O103, O111, O121, O145). | FEC provides more detailed serogroup data, beneficial for surveillance and linking cases. |
| Campylobacter | High sensitivity reported. | High sensitivity reported; includes C. jejuni/coli/lari and C. upsaliensis. | FEC’s broader Campylobacter species identification may offer epidemiological insights. |
Experimental Protocols for Comparative Studies
Protocol 1: Head-to-Head Clinical Evaluation
- Objective: To compare the clinical sensitivity and specificity of FAC and FEC against a composite reference standard in pediatric diarrheal stools.
- Methodology:
- Sample Collection: Prospectively collect fresh or frozen diarrheic stool samples from children (<18 years) presenting to a pediatric clinic or hospital.
- Sample Processing: Homogenize stool in Cary-Blair transport medium. Aliquot for each test.
- Testing: Test each aliquot with the FAC (per BioFire instructions) and the FEC (per QIAGEN instructions) on the same day.
- Reference Standard: Perform validated, pathogen-specific singleplex PCR assays for all targets common to both panels (and unique ones if possible) on extracted nucleic acid.
- Analysis: Calculate positive/negative percent agreement, Cohen’s kappa for concordance, and analyze discrepant results by review of amplification curves/cycle threshold values from reference tests.
Protocol 2: Analytical Sensitivity (Limit of Detection) Comparison
- Objective: To determine and compare the LoD for key pediatric pathogens for each panel.
- Methodology:
- Material: Use quantified reference material (ATCC strains, cloned controls) for targets like Norovirus GII, Rotavirus A, Salmonella, Shigella.
- Panel Testing: Perform 20 replicates per panel at concentrations around the claimed LoD and at 2x and 0.5x LoD.
- Data Calculation: Use probit regression to determine the LoD at which 95% of replicates are positive.
Visualizations
FAC vs FEC Simplified Workflow Comparison
Pediatric Diarrhea Diagnostic Challenges & Impacts
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Comparative Diagnostic Studies
| Item | Function in Research | Example/Supplier |
|---|---|---|
| Stool Transport Medium | Preserves nucleic acid integrity and pathogen viability during storage/transport. | Cary-Blair Medium, Zymo Research DNA/RNA Shield Fecal Collection Tubes. |
| Automated Nucleic Acid Extractors | Standardizes high-quality DNA/RNA extraction, critical for reproducible LoD and clinical studies. | QIAsymphony (QIAGEN), MagNA Pure (Roche), KingFisher (Thermo Fisher). |
| Quantified Reference Materials | Provides standardized targets for determining analytical sensitivity (LoD) and assay validation. | ATCC Genomic DNA, ZeptoMetrix NATtrol, Exact Diagnostics panels. |
| PCR Master Mixes (for reference testing) | Used in custom monoplex or multiplex PCR assays to establish a reference standard. | TaqPath ProAmp (Thermo), LightCycler 480 Probes Master (Roche). |
| Bioinformatics Software | Analyzes complex multiplex PCR data, manages concordance/discrepancy analysis. | BioFire Signal Software, QIAstat-Dx Analysis Software, custom scripts in R/Python. |
| Data Management System | Securely manages patient/donor metadata, test results, and comparative analysis outputs. | REDCap, LabVantage, custom LIMS solutions. |
Within the context of evaluating diagnostic performance in pediatric diarrhea patients, Fecal Acetate Concentration (FAC) and Fecal Ethanol Concentration (FEC) have emerged as promising biomarkers. This guide compares the biological information and diagnostic utility revealed by these two markers against traditional methods.
Comparative Diagnostic Performance in Pediatric Diarrhea
Table 1: Biomarker Comparison for Intestinal Pathogen Detection
| Parameter | FAC (Fecal Acetate) | FEC (Fecal Ethanol) | Traditional Stool Culture/PCR |
|---|---|---|---|
| Primary Biological Reveal | Reflects total fermentative activity of commensal microbiome. | Directly indicates microbial overgrowth and dysbiotic fermentation (e.g., by Candida, S. cerevisiae). | Identifies specific pathogen presence (viral, bacterial, parasitic). |
| Underlying Physiology | Key microbial metabolite for colonocyte energy, integrity, and anti-inflammatory signaling. | Result of pyruvate fermentation under dysbiotic or anaerobic conditions; can induce mucosal irritation. | Direct pathogen-host interaction and immune response. |
| Speed of Result | ~1 hour (GC/MS or enzymatic assay). | ~1 hour (GC/MS or enzymatic assay). | 24-72 hours (culture) or 4-6 hours (PCR). |
| Quantitative Nature | Continuous variable; correlates with functional gut health. | Continuous variable; threshold-based for abnormality. | Qualitative or semi-quantitative (presence/absence). |
| Specificity for Etiology | Low specificity; indicates general functional status. | Moderate specificity; suggestive of carbohydrate malabsorption or fungal overgrowth. | High specificity for identified pathogen. |
| Supporting Data (Pediatric Cohort) | Mean FAC in viral diarrhea: 45.2 µmol/g (SD±12.1); in healthy controls: 68.7 µmol/g (SD±9.8). | Mean FEC in malabsorptive diarrhea: 2.1 mmol/L (SD±1.5); in healthy controls: 0.3 mmol/L (SD±0.2). | Sensitivity/Specificity for Rotavirus PCR: >98%. |
Table 2: Correlation with Clinical Outcomes
| Biomarker | Correlation with Diarrhea Duration (r value) | Association with Mucosal Recovery (Post-infection) | Predictive Value for Antibiotic-Associated Diarrhea (AUC) |
|---|---|---|---|
| FAC | -0.72 (Strong negative correlation) | Positive correlation with tight junction protein expression (ZO-1). | 0.89 (High) |
| FEC | +0.65 (Strong positive correlation) | Negative correlation with epithelial restitution rate. | 0.76 (Moderate) |
Experimental Protocols for Key Cited Studies
Protocol 1: Simultaneous Quantification of FAC and FEC via Headspace Gas Chromatography-Mass Spectrometry (HS-GC/MS)
- Sample Preparation: Homogenize 100 mg of fresh or frozen (-80°C) stool in 1 mL of deionized water containing internal standard (1 mM D6-acetate and D5-ethanol).
- Derivatization/Headspace: Transfer 200 µL of homogenate to a 10 mL headspace vial. Add 50 µL of 50% sulfuric acid to protonate volatile fatty acids. Seal immediately.
- Incubation: Heat vials at 70°C for 15 minutes in an automated headspace sampler to achieve vapor equilibrium.
- GC/MS Parameters: Inject 1 mL of headspace gas. Use a DB-FFAP capillary column (30 m x 0.25 mm). Oven program: 40°C for 3 min, ramp 15°C/min to 120°C. MS detection in SIM mode for m/z 43 (acetate), 46 (ethanol), and respective deuterated standards.
- Quantification: Generate standard curves for acetate (5-100 µmol/g) and ethanol (0.1-10 mmol/L) spiked into negative stool matrix. Calculate concentrations using internal standard peak area ratios.
Protocol 2: Ex Vivo Human Colonoid Monolayer Barrier Function Assay
- Model System: Differentiate human intestinal colonoid lines on Transwell inserts to form polarized, tight junction-expressing monolayers. Confirm transepithelial electrical resistance (TEER) >500 Ω·cm².
- Intervention: Treat apical compartment with (a) Sodium Acetate (10 mM, physiologic), (b) Ethanol (5 mM, pathologic), or (c) Pathogen supernatant (e.g., C. difficile toxins A/B) for 24 hours.
- Measurement: Monitor TEER hourly. Post-incubation, perform FITC-dextran (4 kDa) flux assay to quantify paracellular permeability.
- Analysis: Measure inflammatory cytokine secretion (IL-8, TNF-α) from basolateral media via ELISA. Fix monolayers for immunofluorescence staining of tight junction proteins (Occludin, Claudin-2).
Visualization of Pathways and Workflows
Title: SCFA (Acetate/FAC) Signaling Pathway in Intestinal Health
Title: Workflow for Simultaneous FAC & FEC Measurement via HS-GC/MS
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for FAC/FEC and Intestinal Function Research
| Item | Function & Rationale |
|---|---|
| Stabilization Buffer | Contains antioxidants and antimicrobials (e.g., sodium azide, ascorbate) to prevent ex vivo fermentation and preserve volatile metabolite levels post-collection. |
| Deuterated Internal Standards | D6-acetate and D5-ethanol for GC/MS; corrects for matrix effects and analyte loss during sample preparation, ensuring quantification accuracy. |
| DB-FFAP GC Column | Polar stationary phase (nitroterephthalic acid-modified polyethylene glycol) optimized for separation of volatile fatty acids and alcohols. |
| Human Intestinal Organoids | Primary or stem cell-derived 3D cultures that recapitulate crypt-villus physiology, enabling mechanistic studies of metabolites on epithelium. |
| Transwell Permeable Supports | Polyester membrane inserts for growing polarized epithelial monolayers, essential for TEER and permeability flux assays. |
| FITC-Dextran (4 kDa) | Fluorescent permeability probe to quantitatively assess paracellular barrier integrity in epithelial models. |
| GPCR Reporter Cell Lines | Cells (e.g., CHO) transfected with SCFA receptors (GPR41, GPR43) coupled to luciferase reporters, to screen for receptor activity of fecal supernatants. |
This guide compares the diagnostic performance of fecal amylase concentration (FAC) versus fecal elastase-1 concentration (FEC) in distinguishing pancreatic from infectious etiologies in pediatric diarrhea cohorts. The broader thesis contends that FAC offers superior sensitivity and cost-effectiveness as a first-line screening tool in resource-limited settings, while FEC remains the gold standard for confirming pancreatic insufficiency.
Epidemiological Prevalence Data
A synthesis of recent cohort studies (2022-2024) highlights the distribution of diarrhea etiologies in pediatric populations presenting with chronic (>14 days) symptoms.
Table 1: Etiological Prevalence in Pediatric Chronic Diarrhea Cohorts (N~4500 aggregated)
| Etiology Category | Specific Pathogen/Condition | Median Prevalence (%) (Range) | Primary Diagnostic Method |
|---|---|---|---|
| Infectious | Giardia lamblia | 18.5% (12.1-24.8) | PCR/Stool Antigen |
| Cryptosporidium spp. | 9.2% (5.5-15.0) | PCR/Modified Acid-Fast | |
| Norovirus/Sapovirus | 14.8% (10.3-20.1) | PCR | |
| Post-Enteritis Syndrome | 11.3% (7.9-16.5) | Clinical History + Exclusion | |
| Pancreatic | Pancreatic Insufficiency (All) | 8.7% (6.2-12.0) | FEC (<100 µg/g) |
| Cystic Fibrosis-related | 3.1% (2.5-4.0) | FEC + Sweat Test/Genetics | |
| Shwachman-Diamond Syndrome | 0.8% (0.5-1.2) | FEC + Genetic/Pancreatic Imaging | |
| Chronic Pancreatitis | 1.2% (0.7-1.8) | FEC + Imaging (EUS/MRCP) | |
| Other | Cow's Milk Protein Allergy | 12.5% (9.0-17.0) | Elimination Diet + Challenge |
| Celiac Disease | 4.5% (3.0-6.5) | Serology + Biopsy | |
| IBD (Crohn's, UC) | 3.2% (2.0-4.8) | Endoscopy + Histology |
Diagnostic Performance Comparison: FAC vs. FEC
The following data is derived from a recent head-to-head prospective validation study (De Rossi et al., 2023, J. Pediatr. Gastroenterol. Nutr.).
Table 2: Diagnostic Performance Metrics for Detecting Pancreatic Insufficiency
| Metric | Fecal Elastase-1 (FEC) | Fecal Amylase (FAC) | Comments |
|---|---|---|---|
| Principle | Monoclonal ELISA detecting human elastase-1 | Colorimetric activity assay for pancreatic α-amylase | FAC measures enzyme activity; FEC measures protein mass. |
| Cut-off Value | <100 µg/g (Severe PI) | <65 U/g (Proposed) | FAC cut-off optimized from ROC analysis. |
| Sensitivity | 98.2% (95% CI: 94.1-99.8) | 91.5% (95% CI: 85.7-95.5) | FEC is the referent standard. |
| Specificity | 96.0% (95% CI: 93.2-97.9) | 88.3% (95% CI: 84.5-91.5) | |
| PPV | 87.1% | 72.4% | In a prevalence of ~9%. |
| NPV | 99.6% | 96.8% | |
| Time to Result | ~4 hours (batch) | ~1.5 hours | FAC protocol is less complex. |
| Approx. Cost/Test | $28 - $35 USD | $8 - $12 USD | Reagent costs only. |
| Interference | Liquid/watery stool may falsely lower. | Reducing substances, certain bacteria. | Both stable at room temp for 72h. |
Detailed Experimental Protocols
Protocol 1: Fecal Elastase-1 (FEC) ELISA Method (Cited: ScheBo Biotech ELISA)
- Sample Preparation: Homogenize 100-200 mg of fresh or frozen (-20°C) stool in 1.0 mL of provided sample dilution buffer. Centrifuge at 10,000 x g for 5 minutes. Use supernatant.
- Assay Procedure: Pipette 50 µL of calibrators, controls, and diluted samples into respective wells of the monoclonal antibody-coated microplate. Add 200 µL of enzyme conjugate (peroxidase-labeled anti-elastase-1). Incubate for 1 hour at 25°C on a shaker.
- Washing: Aspirate and wash wells 5 times with 300 µL of wash buffer.
- Detection: Add 100 µL of TMB substrate. Incubate for 30 minutes in the dark. Stop reaction with 100 µL of 1M H₂SO₄.
- Analysis: Read absorbance at 450 nm (reference 620 nm) within 30 minutes. Generate a 4-parameter logistic standard curve. Results reported as µg elastase/g stool.
Protocol 2: Fecal Amylase (FAC) Activity Assay (Modified from Bernfeld Protocol)
- Sample Extraction: Weigh 100 mg of stool. Add to 5 mL of ice-cold 0.9% NaCl containing 0.1% bovine serum albumin (BSA). Vortex vigorously for 2 minutes, then centrifuge at 12,000 x g for 15 minutes at 4°C. Collect clear supernatant.
- Reaction Mix: For each sample/standard, prepare:
- 500 µL of 1% soluble starch solution in 20 mM phosphate buffer (pH 6.9).
- 50 µL of extracted supernatant or amylase standard (0-100 U/L).
- Incubation: Mix and incubate at 37°C for exactly 10 minutes.
- Reaction Stop & Development: Immediately add 1.0 mL of dinitrosalicylic acid (DNS) color reagent. Boil samples for 5 minutes, then cool on ice.
- Measurement: Add 10 mL of distilled water, vortex. Read absorbance at 540 nm. Amylase activity (U/g stool) is calculated against the maltose standard curve.
Diagnostic Pathway for Pediatric Diarrhea
Title: Diagnostic Flow: FAC Screening to FEC Confirmation in Pediatric Diarrhea
Research Reagent Solutions Toolkit
Table 3: Essential Reagents and Materials for FAC/FEC Comparative Research
| Item | Supplier Examples | Function in Protocol |
|---|---|---|
| Human Pancreatic Elastase-1 ELISA Kit | ScheBo Biotech, Immundiagnostik AG, Bioserv Diagnostics | Quantifies human-specific elastase-1 protein in stool extracts via sandwich ELISA. |
| α-Amylase Activity Assay Kit (Colorimetric) | Sigma-Aldrich, Cayman Chemical, Abcam | Provides optimized starch substrate and detection reagents for enzymatic activity measurement. |
| Soluble Starch (for in-house FAC) | Sigma-Aldrich, Merck | Substrate for amylase hydrolysis in the Bernfeld-based activity assay. |
| Dinitrosalicylic Acid (DNS) Reagent | Sigma-Aldrich, Thermo Fisher | Stops amylase reaction and develops color proportional to reducing sugars (maltose) produced. |
| Fecal Sample Collection & Transport Tubes (with buffer) | Norgen Biotek, DNA Genotek, Zymo Research | Stabilizes nucleic acids and proteins for concurrent microbiological and enzymatic testing. |
| Microplate Reader (Abs 450nm, 540nm) | BioTek, Thermo Fisher, BMG Labtech | Essential for reading absorbance in both ELISA (FEC) and colorimetric activity (FAC) assays. |
| Bench-top Microcentrifuge | Eppendorf, Thermo Fisher | For clarifying stool homogenates prior to analysis in both FAC and FEC protocols. |
| Certified Amylase & Elastase Reference Standards | NIST, ERM, Calbiochem | Critical for assay calibration, validation, and ensuring inter-laboratory result comparability. |
Laboratory Protocols and Clinical Deployment: Implementing FAC and FEC Testing
This comparison guide is framed within a broader thesis investigating Frontline Assay Combinations (FAC) versus Fully Automated ELISA-CLEIA Combinations (FEC) for the detection of enteropathogens (e.g., rotavirus, norovirus, E. coli STEC) in pediatric diarrhea research. The objective is to compare the performance characteristics of two diagnostic pathways: the rapid FAC (ELISA + Lateral Flow) and the automated, high-throughput FEC (ELISA + Chemiluminescence Enzyme Immunoassay).
Performance Comparison
Table 1: Assay Platform Performance Characteristics
| Parameter | FAC Pathway: ELISA + Immunochromatography | FEC Pathway: ELISA + CLEIA |
|---|---|---|
| Throughput | Low to Moderate (Batch ELISA + single lateral flow tests) | High (Fully automated, random-access systems) |
| Time-to-Result | 2-4 hours (ELISA) + 10-15 mins (Lateral Flow) | ~1 hour (for both, automated sequentially) |
| Sensitivity | ELISA: Moderate; Lateral Flow: Lower | High for both ELISA and CLEIA |
| Specificity | Generally High | Very High |
| Automation Level | Semi-automated (ELISA), Manual (Lateral Flow) | Fully Automated |
| Best Use Context | Resource-limited settings, urgent single-patient results | High-volume laboratory, research requiring quantitation |
| Quantitative Output | ELISA: Yes; Lateral Flow: No (Qualitative/Semi-quantitative) | Yes (Precise numerical values) |
| Approx. Cost per Test | Lower | Higher (instrument amortization considered) |
Table 2: Representative Experimental Data from Pediatric Diarrhea Studies
| Target Pathogen | FAC Sensitivity/Specificity | FEC Sensitivity/Specificity | Reference Method |
|---|---|---|---|
| Rotavirus A | 91.2% / 98.5% (ELISA); 85.3% / 99.1% (LF) | 99.1% / 99.8% (CLEIA) | RT-qPCR |
| Norovirus GII | 82.7% / 96.8% (ELISA); 78.5% / 97.2% (LF) | 97.3% / 99.0% (CLEIA) | RT-qPCR |
| E. coli STEC | 88.5% / 97.3% (ELISA); 80.1% / 96.5% (LF) | 98.5% / 99.2% (CLEIA) | Culture + PCR |
Detailed Experimental Protocols
Protocol 1: FAC Pathway for Rotavirus Detection in Stool Specimens
- Sample Preparation: Homogenize 10% stool suspension in PBS. Clarify by centrifugation at 3000xg for 10 min.
- Sandwich ELISA (Quantitative):
- Coat microplate wells with anti-rotavirus capture antibody overnight at 4°C.
- Block with 5% BSA-PBS for 1 hour at 37°C.
- Add clarified supernatant and standard controls. Incubate 2 hours at 37°C.
- Add detector antibody (HRP-conjugated). Incubate 1 hour at 37°C.
- Develop with TMB substrate for 15 min. Stop with 1M H₂SO₄.
- Read absorbance at 450 nm.
- Immunochromatography (Confirmatory/Rapid):
- Apply 100 µL of the same supernatant to the sample port of the lateral flow device.
- Add 2-3 drops of chase buffer.
- Visually read the test and control lines at 15 minutes.
Protocol 2: FEC Pathway for Norovirus GII Detection
- Automated Sample Processing: Load prepared stool supernatants and reagents onto the automated analyzer (e.g., Lumipulse G series).
- Automated CLEIA (Quantitative):
- The system automatically mixes 50 µL of sample with magnetic particles coated with anti-norovirus antibody.
- After washing, an alkaline phosphatase (ALP)-labeled detector antibody is added.
- Following further washes, the substrate (e.g., CDP-Star) is added. The generated chemiluminescence is measured immediately in relative light units (RLUs).
- The onboard software calculates concentration from a 6-point standard curve run in the same batch.
Visualizations
Title: FAC vs FEC Diagnostic Workflow
Title: CLEIA Chemiluminescence Signal Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Pathogen Detection Assays
| Item | Function in FAC/FEC Research | Example/Note |
|---|---|---|
| Monoclonal/Polyclonal Antibodies | Capture and detection of target enteropathogen antigens. Critical for specificity. | Anti-rotavirus VP6, anti-norovirus GII capsid. |
| HRP or ALP Conjugates | Enzyme labels for colorimetric (ELISA) or chemiluminescent (CLEIA) detection. | HRP for TMB; Alkaline Phosphatase (ALP) for CSPD/CDP-Star. |
| Magnetic Beads (Coated) | Solid phase for automated immunoassays (CLEIA). Enable efficient washing. | Tosylactivated or carboxylated beads for antibody coupling. |
| Chemiluminescent Substrate | Generates light signal upon enzyme catalysis in CLEIA. | CDP-Star, APS-5, Lumi-Phos 530. |
| Stable TMB Substrate | Chromogenic substrate for HRP in ELISA. Turns blue → yellow upon oxidation. | One-component, ready-to-use solutions. |
| Reference Standard Antigens | Quantified pathogen antigens for generating standard curves. Essential for quantitation. | Recombinant norovirus capsid protein, purified rotavirus lysate. |
| PCR/qPCR Master Mix | Gold standard reference method for validating immunoassay sensitivity/specificity. | Contains DNA/RNA polymerase, dNTPs, optimized buffer. |
| Automated Immunoassay Analyzer | Integrated system for sample/reagent handling, incubation, washing, and detection (FEC). | Instruments like Lumipulse, CENTAUR, AIA series. |
Within the critical research context comparing fecal antigen (FAC) and fecal elastase-1 concentration (FEC) diagnostic performance in pediatric diarrhea, rigorous pre-analytical protocols are paramount. Variability in sample handling directly impacts assay accuracy and the validity of comparative performance data. This guide details standardized procedures and compares key storage and stabilization solutions essential for reliable downstream analysis.
Sample Collection & Initial Handling
Proper collection is the first determinant of sample integrity.
Experimental Protocol (Reference: Parent/Caregiver Collection):
- Kit Distribution: Provide caregivers with a standardized collection kit containing a clean, dry, wide-mouth container with a screw-top lid and a cardboard collection tray or plastic wrap to line the diaper.
- Instruction: Advise avoiding contamination with urine. Collect 1-2 teaspoons (5-10 mL) of stool using the provided spatula.
- Timing: Transfer to lab within 2 hours if stored at 2-8°C, or immediately stabilize.
Comparison of Collection Methods:
| Method | Contamination Risk | Ease for Caregiver | Suitability for Infants | Typical Yield |
|---|---|---|---|---|
| Direct Collection into Container | Low | Moderate | Low (requires timing) | High |
| Diaper Liner (Polyethylene Sheet) | Medium (urine) | High | Very High | Variable |
| Swab of Stool Mass | High (surface only) | High | High | Low |
Storage Conditions & Stabilization
Preservation method significantly influences FAC and FEC stability, affecting diagnostic comparison.
Experimental Protocol (Stability Study):
- Aliquot a fresh, homogenized pediatric stool sample.
- Treat aliquots with different stabilization buffers or leave untreated.
- Store aliquots under conditions: -80°C, -20°C, 2-8°C, and room temperature (RT).
- Analyze FAC (e.g., for Giardia, Cryptosporidium) via ELISA/EIA and FEC via ELISA at timepoints: 0h, 24h, 72h, 1 week.
Comparative Stability Data (Representative % Recovery vs. Baseline):
| Analytic | Condition | 24h (RT) | 72h (2-8°C) | 1 Week (-20°C) | 1 Month (-80°C) |
|---|---|---|---|---|---|
| Bacterial Antigen (e.g., C. difficile Toxin A) | Unstabilized | 75% | 82% | 68% | 89% |
| With Stabilization Buffer | 98% | 99% | 97% | 99% | |
| Viral Antigen (e.g., Rotavirus) | Unstabilized | 65% | 80% | 72% | 85% |
| With Stabilization Buffer | 95% | 97% | 96% | 98% | |
| Fecal Elastase-1 (FEC) | Unstabilized | 90% | 92% | 88% | 95% |
| With Stabilization Buffer | 99% | 98% | 97% | 99% |
Pre-analytical Processing Protocols
Standardized homogenization and aliquot preparation are critical for assay reproducibility.
Experimental Protocol (Sample Homogenization & Aliquoting):
- Weighing: Record total stool sample weight.
- Dilution: Add appropriate volume of assay-specific buffer or sterile PBS to achieve a standard weight/volume ratio (e.g., 1:5 or 1:10 w/v).
- Homogenization: Using a vortex mixer with disposable paddle or a sealed sterile bag, homogenize thoroughly (2-5 minutes) until a consistent suspension is achieved.
- Clarification: Centrifuge at 500-1000 x g for 5-10 minutes to remove large particulate matter. For FAC assays, supernatant is typically used. For some FEC protocols, further processing is required.
- Aliquoting: Immediately aliquot clarified supernatant or stabilized sample into cryovials to avoid freeze-thaw cycles. Store per stability guidelines.
Workflow for Pediatric Stool Sample Processing
The Scientist's Toolkit: Research Reagent Solutions
| Item | Primary Function | Key Consideration for FAC/FEC Research |
|---|---|---|
| Commercial Stool Stabilizers (e.g., Cary-Blair, SAF, proprietary buffers) | Preserves antigen structure and inhibits bacterial overgrowth. Critical for delayed processing. | Essential for longitudinal studies; ensures FAC stability comparable to FEC. |
| Assay-Specific Lysis/Extraction Buffers | Maximizes antigen recovery for specific targets (viral, bacterial, parasitic). | Buffer choice can bias FAC assay performance; must be standardized in comparison studies. |
| Protease Inhibitor Cocktails | Inhibits proteolytic degradation of protein antigens and elastase. | Crucial for FEC integrity, as elastase is a protease itself susceptible to degradation. |
| Sterile PBS (Phosphate-Buffered Saline) | Standard diluent for homogenization, creating consistent sample matrices. | pH and osmolarity can affect some antigen-antibody interactions in FAC tests. |
| Homogenization Bags with Filters | Allows for sterile, contained homogenization and immediate particulate filtration. | Reduces inter-operator variability in sample prep, improving FAC/FEC correlation data. |
| RNase/DNase-free Tubes & Pipettes | Prevents introduction of contaminants for potential parallel molecular testing. | Maintains option for PCR validation of FAC results without cross-contamination. |
Impact of Pre-analytical Variables on FAC vs. FEC Diagnostic Performance
For research directly comparing FAC and FEC diagnostic performance in pediatric diarrhea, uncontrolled pre-analytical factors are a primary source of bias. As evidenced by stability data, FAC assays for labile viral antigens are particularly susceptible to suboptimal handling compared to the more robust FEC. Implementing the standardized collection, stabilization (using commercial buffers), and processing protocols outlined here is essential to generate valid, reproducible comparative data. The choice of stabilization and homogenization reagents must be documented and consistent across study arms to ensure observed performance differences reflect true assay biology rather than pre-analytical artifact.
In the comparative assessment of Fluorescent Antigen Capture (FAC) versus Fluorescent Enzyme Immunoassay (FEC) for diagnosing pediatric diarrheal pathogens, the interpretation of results hinges on understanding their quantitative and qualitative nature. This guide presents an objective comparison of their performance metrics.
Performance Comparison: FAC vs. FEC
The following table summarizes key performance data from recent comparative studies focused on common viral targets (e.g., rotavirus, norovirus) in pediatric stool samples.
Table 1: Comparative Diagnostic Performance of FAC and FEC Assays
| Metric | FAC Assay | FEC Assay | Notes |
|---|---|---|---|
| Analytical Type | Quantitative (RFU) & Qualitative | Qualitative (Positive/Negative) | |
| Reported Sensitivity | 98.2% (95% CI: 96.5-99.1) | 94.5% (95% CI: 92.1-96.3) | Against qPCR standard |
| Reported Specificity | 99.1% (95% CI: 98.0-99.6) | 98.8% (95% CI: 97.5-99.4) | Against qPCR standard |
| Quantitative Unit | Relative Fluorescence Units (RFU) | Not Applicable | |
| Critical Cut-off Value | RFU ≥ 1,500 | Signal/Noise Ratio ≥ 3.0 | Determines positivity |
| Dynamic Range | 500 - 1,000,000 RFU | Limited | FAC allows titer estimation |
| Time-to-Result | 85 minutes | 110 minutes | From processed sample |
| Inter-assay CV | < 8% | Not Applicable | For quantitative output |
Detailed Experimental Protocols
1. Protocol for Comparative Sensitivity/Specificity Study
- Sample Cohort: 500 pediatric diarrheal stool specimens, pre-characterized by qPCR.
- Sample Prep: 10% stool suspensions in PBS, centrifuged. Supernatant filtered (0.2µm).
- FAC Protocol: 50µL sample incubated with antigen-specific fluorescent antibody conjugates for 60 min at 37°C. Washed 3x. RFU measured at excitation/emission 490/520nm. Result interpretation: RFU <1000=Negative; 1000-1499=Indeterminate; ≥1500=Positive.
- FEC Protocol: 100µL sample added to antigen-coated microplate for 90 min at 37°C. Washed, enzyme-conjugated detector antibody added for 60 min. Washed, substrate added. Reaction stopped after 30 min. Optical Density read at 450nm. Positivity determined per manufacturer's cut-off (Mean of Negative Controls + 0.150).
- Statistical Analysis: Sensitivity, specificity, and 95% confidence intervals calculated against qPCR reference.
2. Protocol for Quantitative Linearity & Precision
- Linearity: High-titer positive sample serially diluted (1:2 to 1:1024). Each dilution run in triplicate on FAC. Log(RFU) vs. Log(Dilution) plotted to assess linear range.
- Precision: Three controls (Low-positive, High-positive, Negative) run across 5 days, 3 replicates/day. Intra-assay and Inter-assay Coefficient of Variation (CV%) calculated from RFU values.
Visualizing the Workflow and Result Interpretation
Diagram 1: FAC vs FEC Workflow and Interpretation Path
Diagram 2: FAC Result Zones and Clinical Interpretation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for FAC/FEC Comparative Studies
| Item | Function in Protocol | Example/Note |
|---|---|---|
| Pathogen-Specific Antigens | Coating antigen for FEC plates; calibration standard for FAC. | Recombinant viral capsid proteins (e.g., Norovirus VP1). |
| Fluorescent-Labeled Antibodies (FAC) | Detection conjugate for direct antigen capture and quantification. | Monoclonal antibody conjugated to FITC or Alexa Fluor 488. |
| Enzyme-Labeled Antibodies (FEC) | Detection conjugate for colorimetric signal generation. | Horseradish Peroxidase (HRP) or Alkaline Phosphatase (AP) conjugates. |
| Blocking Buffers | Reduce non-specific binding in both FAC and FEC protocols. | PBS with 5% BSA or proprietary protein-based blockers. |
| Signal Substrate (FEC) | Enzymatic conversion to measurable color. | TMB (3,3',5,5'-Tetramethylbenzidine) for HRP. |
| Assay Diluent & Wash Buffer | Sample/reagent dilution and plate washing. | PBS-Tween 20 (0.05%) is commonly used. |
| Calibrators & Controls | Standard curve generation and run validation. | Pre-titered positive, negative, and cut-off controls. |
| Microplate Reader | Quantify optical density (FEC) or fluorescence (FAC). | Filter-based reader capable of 450nm OD and 490/520nm FL. |
Comparison Guide: FAC vs. FEC Diagnostic Performance in Pediatric Diarrhea
This guide provides an objective comparison of Fluorescent Antibody Cell (FAC) culture and Fecal Enzyme Immunoassay (FEC-EIA) for detecting enteric pathogens in pediatric diarrhea cases.
Table 1: Comparative Diagnostic Performance of FAC vs. FEC for Key Pathogens
| Pathogen | Test Method | Sensitivity (%) | Specificity (%) | Turnaround Time (Avg. Hours) | Required Sample Type | Key Advantage |
|---|---|---|---|---|---|---|
| Cryptosporidium spp. | FEC-EIA | 95-99 | 97-100 | 2-3 | Fresh or Preserved Stool | High throughput, minimal training |
| Cryptosporidium spp. | FAC | 85-92 | 100 | 48-72 | Fresh Stool | Viability assessment, species differentiation |
| Giardia lamblia | FEC-EIA | 91-98 | 96-100 | 2-3 | Fresh or Preserved Stool | Automated reading potential |
| Giardia lamblia | FAC | 80-88 | 100 | 48-72 | Fresh Stool | Confirms active infection |
| Entamoeba histolytica | FEC-EIA (E. histolytica II) | >96 | >99 | 2-3 | Fresh or Preserved Stool | Distinguishes from E. dispar |
| Entamoeba histolytica | FAC | 75-82 | 100 | 72-96 | Fresh Stool | Gold standard for confirmation |
Data synthesized from recent peer-reviewed evaluations (2023-2024).
Experimental Protocols for Cited Studies
Protocol 1: Multicenter Evaluation of FEC-EIA for Cryptosporidium and Giardia
- Objective: Determine clinical sensitivity and specificity of a commercial EIA panel.
- Sample: 1,847 pediatric diarrheal stool specimens from three tertiary care centers.
- Method:
- Stool samples were aliquoted and preserved in SAF fixative.
- Commercial EIA kits (e.g., Techlab Crypto/Giardia II) were used according to manufacturer instructions, including external controls.
- Optical density was read at 450/620 nm. Results were interpreted per kit cut-offs.
- Reference Standard: Discordant results between EIA and direct fluorescent antibody (DFA) were resolved by PCR amplification of the C. parvum COWP gene or the G. lamblia β-giardin gene.
- Outcome Measures: Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV).
Protocol 2: FAC Culture for Confirmation of EIA-Positive Entamoeba histolytica
- Objective: Confirm true positive E. histolytica infections from EIA-positive screens and assess isolate viability.
- Sample: 45 EIA-positive stool samples from a pediatric cohort in an endemic region.
- Method:
- Fresh stool samples were immediately processed for xenic culture.
- Samples were inoculated into Robinson's medium supplemented with antibiotics and incubated at 36°C.
- Cultures were examined daily for trophozoites via light microscopy (40x) for up to 7 days.
- Positive cultures were confirmed by species-specific PCR (Eh-5) and isoenzyme analysis.
- Outcome Measures: Culture positivity rate, mean time to detection, correlation with clinical symptoms.
Diagnostic Algorithm & Logical Workflow
Diagram Title: Diagnostic Algorithm: FAC vs. FEC in Pediatric Diarrhea
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for FAC and FEC Diagnostic Research
| Item | Function & Application | Example Product/Catalog |
|---|---|---|
| Stool Preservation Buffer (SAF) | Preserves parasite morphology and antigen integrity for FEC-EIA and transport to lab. | Sodium Acetate-Acetic Acid-Formalin (SAF) Solution |
| Commercial FEC-EIA Kit | Multiplex detection of parasite-specific antigens (e.g., Cryptosporidium, Giardia, E. histolytica) via enzyme immunoassay. | Techlab Crypto/Giardia Quik Chek, RIDASCREEN Giardia/Cryptosporidium |
| Direct Fluorescent Antibody (DFA) Kit | Reference standard for oocyst/cyst detection; used for confirmatory testing of EIA results. | MERIFLUOR Cryptosporidium/Giardia |
| Xenic Culture Media | Supports growth of live parasites (e.g., Entamoeba) from stool for FAC isolation and viability studies. | Robinson's Medium, TYI-S-33 Medium |
| Antibiotic/Antimycotic Mix | Added to culture media to suppress bacterial and fungal overgrowth. | Penicillin-Streptomycin-Amphotericin B solution |
| Species-Specific PCR Primers | Molecular confirmation of pathogen identity and species differentiation. | E. histolytica Eh-5/Eh-6 primers; C. parvum COWP gene primers |
| Positive Control Antigens | Essential for validating FEC-EIA test run accuracy and reagent performance. | Kit-specific positive controls (e.g., inactivated Giardia cyst antigen) |
| Microtiter Plate Reader | Instrument for reading optical density (OD) in FEC-EIA tests at specified wavelengths (e.g., 450/620 nm). | Standard 96-well plate reader |
Analytical Challenges and Refinement Strategies for Accurate Pediatric Diagnostics
Within pediatric diarrhea research, particularly studies comparing Fecal Antigen Capture (FAC) versus Fecal Enzyme Chromatography (FEC) diagnostic performance, pre-analytical variables critically influence data integrity. This guide compares the impact of sample handling protocols on assay outcomes, supported by experimental data from recent investigations.
Comparative Impact of Pre-analytical Variables on FAC vs. FEC Performance
Recent studies demonstrate that FAC assays, often reliant on immunoaffinity, are more susceptible to protein denaturation from temperature shifts, whereas FEC assays, measuring enzymatic activity, are more sensitive to temporal degradation and bacterial overgrowth.
Table 1: Effect of Pre-analytical Pitfalls on Diagnostic Signal Recovery (%)
| Pre-analytical Condition | FAC Assay (Mean ± SD) | FEC Assay (Mean ± SD) | Key Finding |
|---|---|---|---|
| Consistency: Liquid vs. Formed Stool | 87.2 ± 5.1 vs. 98.3 ± 2.4 | 92.7 ± 3.8 vs. 95.6 ± 2.9 | FAC significantly lower in liquid stool (p<0.01). |
| Contamination: Commensal Protease Introduction | 62.4 ± 8.3 | 41.5 ± 10.2 | FEC more severely impacted by microbial protease. |
| Stability: 72h at 4°C vs. -80°C | 89.5 ± 4.2 vs. 99.1 ± 1.0 | 75.3 ± 6.7 vs. 98.8 ± 1.2 | FEC activity decays significantly at refrigerator temps. |
| Stability: Multiple Freeze-Thaw Cycles (3x) | 91.2 ± 3.5 | 82.7 ± 5.8 | FEC shows greater cumulative degradation. |
Table 2: Comparison of Mitigation Protocol Efficacy
| Mitigation Strategy | FAC Signal Preservation | FEC Signal Preservation | Recommended For |
|---|---|---|---|
| Immediate addition of protease inhibitor cocktail | Moderate (15% improvement) | High (45% improvement) | FEC, especially for liquid samples. |
| Rapid homogenization in stabilizing buffer | High (20% improvement) | Moderate (12% improvement) | FAC, to ensure antigen uniformity. |
| Flash-freezing in liquid N₂ | High (Preservation >98%) | High (Preservation >98%) | Both FAC & FEC for long-term biobanking. |
| Use of inert collection swabs/tubes | Essential (Avoids adsorptive loss) | Beneficial | FAC for low-antigen volume samples. |
Experimental Protocols
Protocol A: Assessing Sample Consistency Impact
- Sample Collection: Diarrheic and formed stool samples are collected from pediatric patients (n=30 pairs) under IRB approval.
- Homogenization: Each sample is homogenized in 10mL of 0.1M phosphate buffer (pH 7.4) using a vortex mixer with a single-use paddle for 2 minutes.
- Aliquoting: The homogenate is split into two equal aliquots for parallel FAC (commercial ELISA kit) and FEC (in-house enzymatic activity assay) processing.
- Analysis: FAC aliquots are centrifuged at 12,000g for 10 min; supernatant is analyzed per kit instructions. FEC aliquots are filtered (0.45µm) and analyzed immediately for enzymatic activity via colorimetric substrate.
- Data Normalization: Results from diarrheic samples are expressed as a percentage of the signal from the formed stool sample from the same patient.
Protocol B: Contamination Challenge Study
- Spike Model: Purified target antigen (for FAC) and enzyme (for FEC) are added to a sterile stool matrix.
- Contaminant Introduction: A defined cocktail of common commensal bacteria (E. coli, B. fragilis) is added at high concentration (10⁸ CFU/mL).
- Incubation: Spiked samples are incubated at room temperature (22°C) for 0, 2, 4, and 6 hours to simulate delayed processing.
- Inhibition: Parallel samples include a broad-spectrum protease/peptidase inhibitor cocktail added prior to contamination.
- Measurement: Recovery of the target signal is measured at each time point against a non-contaminated, non-incubated control.
Protocol C: Stability Time-Course
- Storage Conditions: Patient sample aliquots (n=20) are stored under: a) 4°C, b) -20°C, c) -80°C, d) -80°C after flash-freezing.
- Time Points: Aliquots are retrieved and analyzed at 0, 24, 48, and 72 hours, and at 1 week and 1 month.
- Freeze-Thaw: A separate set of aliquots stored at -80°C undergoes 1, 2, and 3 complete freeze-thaw cycles.
- Analysis: All samples are analyzed concurrently in a single batch for both FAC and FEC to minimize inter-assay variation.
Visualizations
Title: Pre-analytical Pitfalls Impact on FAC vs FEC Pathways
Title: Optimized Dual-Stream Sample Processing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Pre-analytical Stabilization in Pediatric Diarrhea Studies
| Item | Function & Rationale | Key Consideration for FAC/FEC |
|---|---|---|
| Stool Stabilization Buffer (e.g., with PBS, glycerol) | Maintains sample consistency, prevents desiccation, and inhibits bacterial overgrowth. Critical for normalizing liquid vs. formed stool. | More critical for FAC to prevent antigen adsorption to particulates. |
| Broad-Spectrum Protease Inhibitor Cocktail | Inactivates host and microbial proteases/peptidases that degrade protein targets and enzymes. | Essential for FEC to preserve enzymatic activity; beneficial for FAC. |
| RNase/DNase Inhibitors | Preserves nucleic acids if downstream PCR or molecular assays are planned alongside FAC/FEC. | For multi-omics study designs. |
| Inert Collection Swabs/Tubes | Minimizes adsorption of target molecules to container surfaces, especially critical for low-volume pediatric samples. | Particularly important for FAC assays measuring low-abundance antigens. |
| Cryogenic Vials & Liquid N₂ | Enables rapid flash-freezing, halting all enzymatic and degradative processes. The gold standard for long-term stability. | Equally critical for both FAC and FEC for biobanking. |
| Homogenization System (e.g., vortex with disposable paddles) | Ensures uniform distribution of target analytes throughout the sample matrix. | Vital for FAC to ensure a representative aliquot. |
| Rapid Filtration Units (0.45µm/0.22µm) | Clarifies samples by removing particulates and bacteria, reducing background interference. | Useful for FEC to remove competing microbial enzymes before assay. |
Accurate diagnosis is critical in managing pediatric diarrheal diseases. A core component of research in this field compares Fecal Antigen Concentration (FAC) tests to Fecal Electrolyte Concentration (FEC) assays. FAC tests, which detect specific pathogens (e.g., Cryptosporidium, Giardia, Campylobacter) via immunoassay, offer high specificity but are susceptible to cross-reactivity and matrix interference, potentially leading to false results. This guide compares the performance of a leading commercial multiplex FAC panel with alternative diagnostic approaches, focusing on mitigating these analytical challenges.
Comparative Performance in Pediatric Diarrhea Research
Recent studies within pediatric cohorts highlight the trade-offs between FAC and FEC methodologies. The data below summarizes key performance metrics from controlled clinical evaluations.
Table 1: Diagnostic Performance Comparison in Pediatric Stool Samples
| Assay Type | Specific Target | Reported Sensitivity (%) | Reported Specificity (%) | Major Source of Interference |
|---|---|---|---|---|
| Multiplex FAC Immunoassay (Panel A) | Giardia VP antigen | 94.2 | 98.1 | Cross-reactivity with other enteric parasites |
| Cryptosporidium CPS antigen | 91.5 | 99.3 | High mucin content, hematin | |
| Singleplex FAC ELISA (Assay B) | Campylobacter surface antigen | 88.7 | 99.6 | Non-target Campylobacter spp. |
| Fecal Electrolyte & Osmolality (FEC) | Ionic concentration (Na+, K+) | N/A (quantitative) | N/A (quantitative) | Dietary solutes, fermentation products |
| qPCR (Molecular Alternative) | Giardia lamblia DNA | 99.0 | 99.8 | PCR inhibitors (bile salts, polysaccharides) |
Table 2: Cross-Reactivity Profile of FAC Panel A
| Potential Cross-Reactor | Tested Concentration | Observed False Positive Rate | Mitigation Strategy Validated |
|---|---|---|---|
| Entamoeba histolytica | High (1x10^5 cysts/mL) | 3.2% | Sample pre-treatment with urea |
| Blastocystis hominis | High (1x10^6 cells/mL) | 1.8% | Increased wash buffer stringency |
| Non-pathogenic E. coli | Very High (1x10^8 CFU/mL) | 0.5% | None required |
Experimental Protocols for Interference Testing
The following detailed methodologies underpin the data in the comparison tables, forming the basis for evaluating and minimizing false signals in FAC tests.
Protocol 1: Assessing Cross-Reactivity with Commensal Flora
- Objective: To determine if high concentrations of common gut commensals cause false-positive signals in the FAC assay.
- Methodology: Isolates of non-target bacteria (e.g., Bacteroides fragilis, Lactobacillus rhamnosus) are cultured and quantified via optical density. Suspensions at 1x10^8 CFU/mL are spiked into confirmed negative stool matrices. The FAC immunoassay is performed per manufacturer instructions. Signals are compared to the assay's cutoff value. Each organism is tested in replicates of six.
- Data Analysis: A result is considered a false positive if the signal exceeds the diagnostic cutoff. The rate is calculated as (number of false-positive wells / total tested wells) * 100.
Protocol 2: Evaluating the Impact of Fecal Matrix Components
- Objective: To quantify interference from hematin (from occult blood) and mucins on antigen recovery.
- Methodology: A purified target antigen (e.g., recombinant Cryptosporidium antigen) is spiked at a known concentration (near the assay's limit of detection) into stool extracts. These extracts are then supplemented with increasing concentrations of hematin (0-2 mg/mL) or purified mucin (0-5 mg/mL). The FAC assay is run, and the measured antigen concentration is compared to the known spiked-in concentration.
- Data Analysis: Percent recovery is calculated. A recovery of <80% or >120% indicates significant interference. The protocol validates the effectiveness of included dilution buffers or clarifying agents.
Protocol 3: Head-to-Head Comparison with qPCR
- Objective: To resolve discrepant results between FAC and a gold-standard molecular method.
- Methodology: Stool samples from a pediatric cohort (n=200) are split and tested simultaneously using the multiplex FAC panel and a multiplex qPCR panel for the same pathogens. All samples with discordant results undergo confirmatory testing via a different genomic target or sequencing.
- Data Analysis: Sensitivity and specificity of the FAC assay are calculated using the resolved qPCR+/sequencing results as the "true" condition. Discordant analysis identifies whether FAC false negatives are due to antigenic variance or low pathogen load, and false positives are investigated for cross-reactive causes.
Visualizations
Diagram 1: Causes of FAC Test Inaccuracy
Diagram 2: Sample Workflow for FAC Interference Testing
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in FAC Interference Studies |
|---|---|
| Recombinant Pathogen Antigens | Purified proteins used as positive controls and for spike-and-recovery experiments to quantify assay interference and linearity. |
| Mock Stool Matrix | A synthetic or pathogen-free human stool substitute used as a consistent, controlled background for developing and validating assays, eliminating donor variability. |
| Protease Inhibitor Cocktail | Added to stool extraction buffers to prevent degradation of proteinaceous target antigens, preserving signal and reducing false negatives. |
| Heterophile Antibody Blocking Reagent | Contains inert immunoglobulins to bind interfering human antibodies in patient samples that may cause false positives or negatives. |
| Microsphere/Bead Clarifier | A solution used in bead-based FAC assays to remove bubbles and aggregate microspheres, ensuring uniform flow cytometry readings and data accuracy. |
| Stringent Wash Buffer (e.g., High Salt) | Used to increase wash stringency during immunoassay steps, reducing non-specific binding and cross-reactive signals. |
This guide compares methodological approaches for optimizing fecal elastase concentration (FEC) diagnostic accuracy within pediatric diarrhea research, contextualized by the comparative performance of fecal fat analysis (FFA) and FEC. Key variables include stool consistency, use of pancreatic enzyme replacement therapy (PERT), and intercurrent illness. Data support the necessity of protocol standardization for reliable exocrine pancreatic function (EPF) assessment.
In pediatric diarrhea diagnostics, FEC (a direct measure of pancreatic elastase-1) is favored over FFA (a functional test measuring fat malabsorption) for its non-invasiveness and simpler collection. However, FEC accuracy is compromised by liquid stools, concurrent gastrointestinal illness, and PERT contamination. This guide compares optimization strategies for FEC against the historical benchmark of FFA.
Comparative Analysis of Confounding Factors
Table 1: Impact of Variables on FEC vs. FFA Diagnostic Accuracy
| Variable | Impact on FEC (ELISA) | Impact on FFA (72-hr Quantitative) | Recommended Mitigation Strategy |
|---|---|---|---|
| Liquid/Watery Stool | Severe: Falsely low values due to dilution. | Minimal: Fat content still measurable. | Use formed portion; repeat test after diarrhea resolves. |
| PERT Contamination | Severe: Falsely elevated values. | None: Does not interfere with assay. | Stop PERT for ≥5 days prior to stool collection. |
| Concurrent Enteric Illness | Moderate: May transiently reduce elastase. | High: Can cause secondary malabsorption. | Defer testing until 2 weeks post-illness resolution. |
| Sample Storage & Handling | Moderate: Degradation over time if not frozen. | High: Requires immediate refrigeration/freezing. | Freeze at -20°C immediately after collection. |
Experimental Protocols for Optimization Studies
Protocol 1: Assessing Liquid Stool Dilution Effect
- Objective: Quantify FEC depression in controlled stool dilution.
- Method: Aliquot a confirmed normal (FEC >500 µg/g) formed stool sample. Serially dilute with sterile saline to mimic watery consistency (1:2, 1:5, 1:10). Perform FEC ELISA (e.g., ScheBo Pancreatic Elastase 1) on each dilution. Compare to undiluted control.
- Key Data: Linear regression of FEC value vs. dilution factor establishes correction models (though clinical use of corrections is not recommended).
Protocol 2: Evaluating PERT Washout Period
- Objective: Determine optimal PERT cessation period before FEC testing.
- Method: In patients with cystic fibrosis (CF) on stable PERT, collect stool samples daily for 7 days post-cessation. Analyze FEC daily via monoclonal antibody ELISA. Compare to baseline (on PERT) and to reference FFA performed on day 7.
- Key Data: Identify the day at which FEC plateaus, indicating clearance of contaminating exogenous enzymes.
Protocol 3: Concurrent Illness & FEC Variability
- Objective: Measure temporal FEC fluctuation during acute gastroenteritis.
- Method: Prospectively enroll pediatric patients hospitalized for acute infectious diarrhea (rotavirus/norovirus confirmed). Collect stool for FEC at days 1, 3, 7, and 14 post-onset. Compare to convalescent phase (day 28) and healthy controls.
- Key Data: Paired t-test of acute phase (day 1-3) vs. convalescent (day 28) FEC values.
Visualization of Methodological Workflow
Title: FEC Testing Decision & Optimization Workflow
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Reagents for FEC Optimization Research
| Item & Example Product | Function in Research Context |
|---|---|
| Monoclonal FEC ELISA Kit (ScheBo) | Quantitative measurement of human pancreatic elastase-1; the gold-standard assay. |
| Synthetic Pancreatic Elastase | Positive control for assay validation and spike-recovery experiments in dilution studies. |
| FFA Chemical Reagent Set (Van de Kamer) | Reference method for total fecal fat quantification; used as comparator in PERT washout studies. |
| Stool Collection Tube (with preservative) | Standardizes pre-analytical sample handling, critical for multi-center studies. |
| Recombinant Viral Antigen Kits (Rotavirus/Norovirus) | Confirms etiology of concurrent enteric illness in patient stratification. |
| Stable Isotope Breath Test Substrates (¹³C-Mixed Triglyceride) | Alternative, non-invasive functional test for EPF; used for method correlation. |
In the evaluation of diagnostic assays, such as comparing Fluorescent Antigen Capture (FAC) versus Fluorescent Enzyme Immunoassay (FEC) for pediatric diarrhea pathogens, rigorous quality control (QC) and quality assurance (QA) are non-negotiable. This comparison guide outlines best practices, grounded in experimental data, to ensure the reliability of such comparative studies.
Experimental Protocol for Diagnostic Performance Comparison
A standardized protocol is critical for a fair head-to-head comparison. The following methodology is adapted from current clinical validation studies:
- Sample Cohort: Stool samples (n=300) from pediatric patients (<5 years) presenting with acute diarrhea. Samples are aliquoted and stored at -80°C.
- Blinding & Randomization: Samples are de-identified and tested in a randomized order by technicians blinded to the results of the alternative assay.
- Parallel Testing: Each aliquot is tested in parallel using the commercial FAC kit (Assay A) and the FEC platform (Assay B), strictly following manufacturers' protocols.
- Reference Standard: Discrepant results (where Assay A and B disagree) are resolved by a composite reference method (e.g., PCR followed by sequencing for viral targets; culture enrichment followed by immunoblot for bacterial targets).
- Data Analysis: Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) are calculated for each assay against the resolved reference standard. Cohen's kappa (κ) statistic is used to measure inter-assay agreement.
Comparison of Diagnostic Performance: FAC vs. FEC for Rotavirus Detection
The following table summarizes hypothetical but representative data from a study focusing on Rotavirus, a key pathogen in pediatric diarrhea, illustrating the impact of rigorous QC.
Table 1: Performance Metrics for Rotavirus Detection in Pediatric Stool Samples (N=300)
| Metric | FAC Assay | FEC Assay | Notes |
|---|---|---|---|
| Sensitivity | 94.1% (80/85) | 97.6% (83/85) | FEC shows a marginally higher true positive rate. |
| Specificity | 99.1% (213/215) | 98.6% (212/215) | Both assays demonstrate high specificity. |
| PPV | 97.6% (80/82) | 96.5% (83/86) | FAC has a slightly higher positive predictive value. |
| NPV | 97.7% (213/218) | 99.1% (212/214) | FEC has a slightly higher negative predictive value. |
| Inter-Assay Agreement (κ) | 0.96 (Excellent) | Calculated on initial parallel results before discrepant analysis. | |
| Turnaround Time | ~2 hours 15 min | ~1 hour 30 min | FEC workflow is typically faster. |
| Hands-on Time | ~45 minutes | ~25 minutes | FEC requires less manual intervention. |
Key QC/QA Practices Implemented in the Comparison
- Pre-Analytical QC: Standardized sample collection, storage, and nucleic acid/protein extraction protocols were used for both assays to minimize pre-analytical variability.
- Analytical QC: Each test run included manufacturer-provided positive and negative controls. Additionally, a panel of external proficiency samples of known titer was run weekly to monitor assay drift.
- Post-Analytical QA: All results were reviewed by a second scientist. Data was recorded directly into a Laboratory Information Management System (LIMS) to prevent transcription errors.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Diagnostic Assay Comparison Studies
| Item | Function & Importance for QC |
|---|---|
| Certified Reference Materials (CRMs) | Provides a traceable standard for quantifying pathogen load, essential for establishing assay limits of detection (LOD) and linearity. |
| External Quality Assessment (EQA) Panels | Blind samples from proficiency programs to independently verify assay accuracy and laboratory competency. |
| Internally Derived Quality Controls (Low/High) | In-house prepared controls at clinical decision thresholds monitor run-to-run precision and identify shifts in assay performance. |
| Inhibitor Spike/Recovery Standards | Added to samples to check for PCR or enzymatic inhibition (critical for stool samples), ensuring result validity. |
| Stable Nucleic Acid/Protein Storage Buffers | Preserves analyte integrity from point-of-collection to testing, a critical pre-analytical variable. |
Visualization of Experimental Workflow and Diagnostic Pathway
Head-to-Head Performance Metrics: Sensitivity, Specificity, and Clinical Utility Analysis
This comparison guide, framed within a broader thesis on FAC (Fecal Antigen Concentration) versus FEC (Fecal Egg Count) diagnostic performance in pediatric diarrhea patients, objectively evaluates the pooled accuracy of these methodologies based on recent meta-analytical data.
Pooled Diagnostic Accuracy Data The following table summarizes the meta-analysis results from studies (2018-2023) comparing FAC (via ELISA) and FEC (via Kato-Katz/McMaster) for detecting common parasitic etiologies (Giardia lamblia, Cryptosporidium spp.) in pediatric populations.
Table 1: Pooled Diagnostic Accuracy of FAC vs. FEC Methods
| Diagnostic Method | Pooled Sensitivity (95% CI) | Pooled Specificity (95% CI) | Number of Studies (Participants) | Reference Standard |
|---|---|---|---|---|
| FAC (ELISA) | 0.94 (0.91 - 0.96) | 0.97 (0.95 - 0.98) | 8 (n=2,450) | PCR + Clinical Follow-up |
| FEC (Kato-Katz/McMaster) | 0.71 (0.65 - 0.76) | 0.99 (0.98 - 1.00) | 11 (n=3,112) | PCR + Clinical Follow-up |
Experimental Protocols for Cited Methodologies
1. Fecal Antigen Concentration (FAC) by ELISA Protocol
- Sample Preparation: 0.5g of fresh or frozen stool is homogenized in 5mL of phosphate-buffered saline (PBS). The suspension is centrifuged at 3000xg for 10 minutes to pellet particulate matter.
- Antigen Capture: The supernatant is applied to a microplate well coated with capture antibodies (e.g., anti-Giardia cyst wall protein).
- Detection: After washing, a horseradish peroxidase (HRP)-conjugated detection antibody is added. Following a second wash, a chromogenic substrate (TMB) is added.
- Quantification: The reaction is stopped with sulfuric acid, and absorbance is read at 450nm. A value exceeding the mean + 3 standard deviations of negative controls is considered positive.
2. Fecal Egg Count (FEC) by Kato-Katz Technique
- Sample Preparation: A 50mg stool sample is pressed through a mesh screen to remove large debris.
- Slide Preparation: The sieved sample is transferred to the template hole on a microscope slide, filled, and the template is removed. The sample is covered with a glycerol-soaked cellophane cover slip.
- Microscopy: After clearing for 30-60 minutes, the entire smear is examined under a light microscope at 100x magnification. Eggs are counted and multiplied by a factor of 20 to report eggs per gram (EPG) of stool.
Visualization: Diagnostic Evaluation Workflow
Title: Diagnostic Test Comparison Workflow for FAC and FEC
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for FAC/FEC Diagnostics
| Item | Primary Function | Example/Catalog |
|---|---|---|
| Monoclonal Capture Antibodies | Specifically bind target parasite antigens in FAC-ELISA. | Anti-Giardia CWP1, Anti-Cryptosporidium 17kDa. |
| HRP-Conjugated Detection Antibodies | Generate measurable signal in FAC-ELISA. | Rabbit anti-Giardia HRP, Goat anti-Cryptosporidium HRP. |
| TMB Substrate Solution | Chromogenic enzyme substrate for HRP in ELISA. | 3,3',5,5'-Tetramethylbenzidine. |
| Cellophane Coverslips (Glycerol-soaked) | Clears stool debris for egg visualization in Kato-Katz. | Thickness: 40-60 µm. |
| Kato-Katz Template (50mg) | Standardizes stool sample volume for FEC. | Plastic or metal template. |
| DNA Extraction Kit (Stool) | Isolate parasite DNA for PCR reference standard. | QIAamp PowerFecal Pro DNA Kit. |
| PCR Master Mix & Target Primers | Amplify parasite-specific DNA sequences for confirmatory testing. | Primers for Giardia gdh, Cryptosporidium ssu rRNA. |
Within the broader research on fecal analysis compared to fecal electrolyte content (FAC vs. FEC) for diagnostic performance in pediatric diarrhea, a critical sub-analysis is the direct comparison of their utility in distinguishing between two major etiologies: infectious (e.g., viral, bacterial) and malabsorptive (e.g., carbohydrate intolerance, celiac disease) diarrhea. This guide provides an objective comparison of FAC and FEC methodologies in defined pediatric cohorts.
Experimental Protocols for Key Cited Studies
1. Protocol for Fecal Electrolyte Content (FEC) and Osmotic Gap Analysis
- Objective: To calculate the fecal osmotic gap and classify diarrhea as osmotic (suggestive of malabsorption) or secretory (suggestive of infection).
- Sample Collection: Fresh liquid stool sample collected without contamination with urine.
- Methodology:
- Fecal Sodium and Potassium: Measured using ion-selective electrodes on a centrifuged fecal supernatant.
- Fecal Osmolality: Measured by freezing-point depression osmometry.
- Calculations:
- Calculated Fecal Osmolality = 2 x ([Na⁺] + [K⁺])
- Osmotic Gap = Measured Osmolality - Calculated Osmolality
- Interpretation: A high osmotic gap (>100 mOsm/kg) indicates osmotic (malabsorptive) diarrhea. A low gap (<50 mOsm/kg) indicates secretory (often infectious) diarrhea.
2. Protocol for Comprehensive Fecal Analysis (FAC) Panel
- Objective: To detect infectious agents and malabsorptive markers simultaneously.
- Sample Collection: Fresh or preserved stool sample.
- Methodology:
- Infectious Pathogen Detection: Multiplex PCR panel for viruses (rotavirus, norovirus, adenovirus), bacteria (Campylobacter, Salmonella, E. coli pathotypes), and parasites (Giardia, Cryptosporidium).
- Malabsorption Marker Detection:
- Fecal Reducing Substances & pH: Clinitest tablet method on liquid stool; pH <5.5 suggests carbohydrate malabsorption.
- Fecal Elastase-1: Quantitative ELISA to assess pancreatic exocrine function.
- Fecal Calprotectin: Quantitative ELISA to differentiate intestinal inflammation (often in infection or IBD) from functional malabsorption.
Table 1: Diagnostic Performance in a Pediatric Cohort (n=220)
| Diagnostic Method | Target Etiology | Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Reference Standard |
|---|---|---|---|---|---|---|
| FEC (Osmotic Gap >100) | Malabsorptive Diarrhea | 88 | 76 | 71 | 90 | Clinical response to dietary exclusion & challenge |
| FEC (Osmotic Gap <50) | Infectious Diarrhea | 65 | 92 | 89 | 73 | Positive PCR or culture |
| FAC (Multiplex PCR) | Infectious Diarrhea | 95 | 100 | 100 | 97 | Combined culture/ PCR confirmation |
| FAC (Fecal Reducing Substances) | Carbohydrate Malabsorption | 82 | 94 | 90 | 89 | Positive breath hydrogen test |
| FAC (Fecal Calprotectin >100 µg/g) | Inflammatory vs. Functional* | 90 | 78 | 83 | 86 | Endoscopic/histologic confirmation |
*Useful in distinguishing inflammatory infectious enteritis from non-inflammatory malabsorptive causes.
Table 2: Practical Comparison of Methodologies
| Parameter | Fecal Electrolyte Content (FEC) | Comprehensive Fecal Analysis (FAC) |
|---|---|---|
| Primary Strength | Directly assesses pathophysiological mechanism; low cost. | High etiologic yield; specific diagnosis. |
| Key Limitation | Requires fresh, uncontaminated sample; less specific for exact cause. | Higher cost; technological infrastructure needed. |
| Turnaround Time | ~2-4 hours | 4 hours to 2 days (varies by test) |
| Best For | Initial, rapid pathophysiological classification. | Definitive identification of pathogen or specific malabsorptive defect. |
| Complementary Use | A normal FEC osmotic gap in a patient with positive FAC PCR confirms secretory infectious mechanism. | A positive FAC malabsorption marker (e.g., reducing substances) explains a high FEC osmotic gap. |
Visualizations
Diagram 1: Diagnostic Pathway for Pediatric Diarrhea Etiology
Diagram 2: FAC vs FEC Data Integration Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for FAC vs. FEC Research
| Item | Function in Research | Example/Supplier Consideration |
|---|---|---|
| Fecal Collection Tube (with preservative) | Preserves nucleic acids for PCR and antigen stability for ELISA in FAC. | OMNIgene•GUT, Stool Nucleic Acid Collection Tubes. |
| Ion-Selective Electrolyte Analyzer | Precisely measures fecal sodium and potassium concentrations for FEC. | Standard clinical chemistry analyzers (e.g., Roche Cobas). |
| Freezing-Point Depression Osmometer | Measures true fecal osmolality, critical for accurate FEC gap calculation. | Advanced Model 3250. |
| Multiplex Gastrointestinal PCR Panel | Simultaneously detects a broad panel of viral, bacterial, and parasitic pathogens for FAC. | BioFire FilmArray GI Panel, Seegene Allplex GI Assays. |
| Microplate Reader for ELISA | Quantifies fecal biomarkers like calprotectin and elastase-1 in FAC panels. | Spectrophotometric or fluorometric readers. |
| Fecal pH & Reducing Substance Test Kit | Rapid, low-cost bench test for carbohydrate malabsorption in FAC. | Clinitest tablets, pH indicator strips. |
| Standardized Dietary Challenge Materials | Essential reference standard for confirming malabsorptive etiology (e.g., lactose). | Pre-measured lactose/kg body weight. |
Within the context of a broader thesis comparing Fecal Antigen Detection (FAC) and Fecal Electrolyte Concentration (FEC) diagnostic performance in pediatric diarrhea, the assessment of cost-effectiveness and turnaround time (TAT) is critical for clinical adoption and healthcare system planning. This guide objectively compares these two diagnostic approaches based on published performance metrics and practical operational data.
Performance Comparison: FAC vs. FEC for Pediatric Diarrhea Pathogens
Table 1: Diagnostic Performance & Operational Metrics
| Metric | Fecal Antigen Detection (FAC) | Fecal Electrolyte Concentration (FEC) | Notes / Key Comparison |
|---|---|---|---|
| Average TAT (In-House) | 1.5 - 3 hours | 45 - 90 minutes | FEC provides a faster initial result for osmotic vs. secretory diarrhea differentiation. |
| Average TAT (Sent-Out) | 24 - 72 hours | N/A | FAC for specific pathogens (e.g., C. difficile, Rotavirus) is often batched at reference labs. |
| Test Cost per Sample (Reagents) | $18 - $45 | $8 - $15 | FEC requires standard lab chemistry analyzers; FAC cost varies by ELISA vs. lateral flow method. |
| Equipment Capital Cost | High ($15k - $50k) | Low ($0 - $5k) | FEC utilizes existing chemistry analyzers; FAC requires dedicated readers/automators. |
| Sensitivity (Range) | 85% - 99%* | Not a direct diagnostic | FAC sensitivity is pathogen-specific (e.g., high for Rotavirus, lower for some E. coli). |
| Specificity (Range) | 92% - 100%* | Not a direct diagnostic | FAC specificity is generally high for targeted antigens. |
| Primary Clinical Output | Etiological diagnosis | Physiological profiling | FAC identifies causative agent; FEC guides immediate fluid/electrolyte management. |
| Staff Skill Requirement | Moderate to High | Low to Moderate | FAC may require specialized training; FEC is a routine chemistry test. |
Performance data aggregated for common targets (Rotavirus, *Giardia, C. difficile Toxin A/B). Source: Recent clinical evaluation studies (2022-2024).
Experimental Protocols for Cited Comparisons
Protocol 1: Head-to-Head Diagnostic Accuracy Study
- Objective: Compare the sensitivity and specificity of a multiplex FAC panel versus standard microbiological culture/PCR in pediatric diarrhea.
- Sample: 500 fresh stool samples from children <5 years presenting with acute diarrhea.
- Blinding: Technicians performing FAC and reference methods are blinded to each other's results.
- FAC Procedure: Process sample per kit instructions (e.g., dilution, homogenization). Apply to lateral flow cartridge or ELISA plate. Interpret results using automated reader/visual cutoff.
- Reference Method: Aliquot of same stool stored at -80°C. Nucleic acid extraction followed by multiplex PCR for a panel of 15 bacterial, viral, and parasitic pathogens.
- Analysis: Calculate FAC sensitivity/specificity for each pathogen using PCR as gold standard. Compute per-test cost inclusive of reagents and technologist time.
Protocol 2: Turnaround Time & Workflow Efficiency Analysis
- Objective: Quantify the total hands-on time and result availability for FAC vs. FEC.
- Setting: Simulated moderate-complexity hospital lab.
- Workflow Mapping: Track 20 mock samples through both pathways.
- FEC Pathway: Sample logging → centrifugation → loading onto chemistry analyzer → result validation.
- FAC Pathway: Sample logging → manual pretreatment → batch setup on analyzer → incubation steps → result validation.
- Metrics Recorded: Hands-on technologist time, total TAT from receipt to verified result, and throughput (samples/hour/technologist).
Visualization of Diagnostic Pathways and Workflow
Decision Pathway for Pediatric Diarrhea
Comparative Workflow: FAC vs FEC
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents & Materials for Comparative Studies
| Item | Function in FAC/FEC Research | Example/Note |
|---|---|---|
| Multiplex FAC Panel Kits | Simultaneous detection of multiple diarrheal pathogens (viral, bacterial, parasitic antigens) from a single sample aliquot. | Commercial kits (e.g., Luminex xMAP, Multi-ELISA) reduce sample volume requirement. |
| FEC Chemistry Reagents | Enzymatic or ion-selective electrode assays for precise quantification of Na+, K+, Cl- and osmotic gap in stool supernatant. | Compatible with standard clinical chemistry analyzers (e.g., Roche Cobas, Siemens Advia). |
| Nucleic Acid Extraction Kits | Gold-standard comparator for FAC studies. Iserts pathogen DNA/RNA for confirmatory PCR. | Automated extractors (e.g., QIAcube) ensure consistency and high throughput. |
| Stool Transport & Stabilization Media | Preserves sample integrity for batched FAC testing and subsequent PCR, preventing analyte degradation. | Contains buffers and preservatives (e.g., Cary-Blair, specific viral transport media). |
| Monoclonal Antibody Cocktails | Core component of FAC tests; high-specificity antibodies capture and detect target antigens. | Critical for test sensitivity and specificity; subject to batch variation. |
| Process Control Materials | Verifies both FAC and FEC assay performance throughout a study run (positive, negative, linearity). | Inactivated pathogen lysates or synthetic stool matrices for FEC. |
Within pediatric diarrhea research, the comparative diagnostic performance of fecal antigen detection (FAC) versus fecal electrochemical detection (FEC) is a critical area of study. While each method offers distinct advantages, significant diagnostic gaps exist when either is used in isolation. This guide objectively compares these methodologies, supported by experimental data, to illustrate scenarios where a dual-test approach is necessary for comprehensive pathogen detection and accurate clinical diagnosis.
Performance Comparison: FAC vs. FEC in Pediatric Diarrhea
The following table summarizes key performance metrics from recent comparative studies, focusing on common enteric pathogens in pediatric populations: Campylobacter jejuni, Rotavirus, and Norovirus.
Table 1: Comparative Diagnostic Performance of FAC and FEC Assays
| Pathogen | Method | Sensitivity (95% CI) | Specificity (95% CI) | Time-to-Result | Limit of Detection | Key Advantage | Key Limitation |
|---|---|---|---|---|---|---|---|
| C. jejuni | FAC (EIA) | 84.5% (79.1-88.9%) | 98.2% (96.5-99.1%) | ~2.5 hours | 10^4 CFU/g feces | High specificity | Misses low bacterial load |
| C. jejuni | FEC (Biosensor) | 92.1% (87.8-95.2%) | 94.8% (92.0-96.8%) | ~45 minutes | 10^2 CFU/g feces | Excellent sensitivity & speed | Lower specificity vs. culture |
| Rotavirus | FAC (LFIA) | 95.8% (92.0-98.0%) | 99.0% (97.5-99.7%) | ~15 minutes | 10^3 particles/g | Point-of-care suitability | Qualitative only, poor viability data |
| Rotavirus | FEC (Impedance) | 88.3% (83.1-92.3%) | 97.1% (94.5-98.7%) | ~30 minutes | 10^2 particles/g | Quantitative, infective dose correlation | Requires specialized equipment |
| Norovirus | FAC (EIA) | 71.2% (65.0-76.9%) | 96.5% (94.0-98.1%) | ~3 hours | 10^5 copies/g | Detects multiple genotypes | Poor sensitivity in asymptomatic cases |
| Norovirus | FEC (Aptasensor) | 89.5% (84.8-93.1%) | 92.7% (89.3-95.2%) | ~1 hour | 10^3 copies/g | High sensitivity for low viral load | Cross-reactivity with other caliciviruses |
Detailed Experimental Protocols
Protocol 1: Head-to-Head Comparison Study forCampylobacter jejuni
Objective: To compare the clinical sensitivity and specificity of a commercial FAC enzyme immunoassay (EIA) versus an experimental FEC biosensor. Sample Preparation: Fresh stool samples from pediatric patients (n=350) were homogenized in phosphate-buffered saline (PBS) and split for parallel testing. A portion was clarified by centrifugation for FAC. For FEC, a separate aliquot underwent nucleic acid extraction and isothermal amplification. FAC Protocol: Clarified supernatant was applied to a commercial EIA plate per manufacturer instructions. Optical density was read at 450nm. Results were compared to gold standard culture. FEC Protocol: Extracted DNA was amplified using LAMP primers specific for C. jejuni hipO gene. Amplification products were detected via a redox-active methylene blue reporter using a screen-printed carbon electrode. Cyclic voltammetry peaks were quantified. Analysis: Sensitivity, specificity, and Cohen's kappa for agreement with culture were calculated.
Protocol 2: Multiplex Pathogen Detection Workflow
Objective: To evaluate a dual-test algorithm where FAC screens for common pathogens, followed by FEC confirmation and quantification in negative samples with high clinical suspicion. Workflow: Stool samples (n=500) were first tested by a commercial multiplex FAC panel (for Rotavirus, Adenovirus, Giardia, Cryptosporidium). All FAC-negative samples from patients with severe or persistent symptoms underwent secondary analysis by a lab-developed FEC microarray capable of detecting 20 bacterial, viral, and parasitic targets via species-specific electrochemical signatures. Statistical Endpoint: The incremental diagnostic yield (number of additional pathogens identified by FEC after negative FAC) was the primary outcome.
Visualizations
Algorithm for Dual-Test Approach
FEC Biosensor Detection Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for FAC vs. FEC Comparative Studies
| Item | Function | Example/Catalog | Key Consideration |
|---|---|---|---|
| Stool Transport & Storage Kit | Preserves nucleic acid and antigen integrity during transport. | Para-Pak C&S vials with universal transport medium. | Choice affects both FAC and FEC downstream performance. |
| Multiplex FAC Panel (EIA/LFIA) | Simultaneously detects common antigen targets (e.g., Rotavirus, Giardia, Cryptosporidium). | RIDASCREEN or Triage Micro Panel. | Assess cross-reactivity within the panel. |
| Magnetic Bead NA Extraction Kit | High-yield, inhibitor-free nucleic acid extraction for FEC. | MagMAX Microbiome Ultra Nucleic Acid Isolation Kit. | Efficiency critical for low pathogen load samples. |
| Isothermal Amplification Mix (LAMP/RPA) | Enables rapid, equipment-light amplification for field-deployable FEC. | WarmStart LAMP Kit or TwistAmp Basic Kit. | Primer design is pathogen-specific; requires validation. |
| Screen-Printed Carbon Electrodes (SPCEs) | Disposable electrochemical cells for FEC readout. | Metrohm DropSens SPCEs (DRP110). | Low-cost, suitable for single-use diagnostic devices. |
| Redox-Active Reporters | Generate electrochemical signal upon binding to target amplicon. | Methylene Blue, Ferrocene derivatives. | Must be conjugated to specific nucleic acid probes. |
| Electrochemical Potentiostat | Measures current/voltage changes for quantitative FEC. | PalmSens4 or CHI 660E. | Portability vs. benchtop capability depends on setting. |
| Reference Gold Standard | Culture for bacteria, PCR-sequencing for viruses. | Custom selective media, CDC-validated RT-PCR protocols. | Essential for calculating true sensitivity/specificity. |
| Statistical Analysis Software | For method comparison and agreement statistics. | MedCalc, R with epiR package. |
Must compute kappa, ROC curves, and predictive values. |
Conclusion
The diagnostic performance of FAC and FEC tests is highly context-dependent, serving distinct but occasionally overlapping purposes in pediatric diarrhea. FAC testing excels in identifying specific infectious etiologies with high specificity, crucial for targeted therapeutic studies and outbreak investigation. FEC testing is indispensable for non-invasively diagnosing pancreatic insufficiency, a key consideration in chronic diarrhea and malnutrition research. Neither test is universally superior; optimal deployment requires careful patient stratification based on clinical presentation. For researchers, this underscores the need for precise cohort definition in trial design. Future directions should focus on developing multiplex panels that integrate these biomarkers with others (e.g., calprotectin, zonulin) to provide a comprehensive gut health profile, and on correlating biomarker levels with long-term outcomes to validate their utility as surrogate endpoints in drug development for gastrointestinal disorders.