Cross-Reactivity in Immunoassays: Advanced Strategies for Detection, Troubleshooting, and Validation in Research and Drug Development
This article provides a comprehensive guide for researchers and drug development professionals confronting the pervasive challenge of cross-reactivity in immunoassays.
Cross-Reactivity in Immunoassays: Advanced Strategies for Detection, Troubleshooting, and Validation in Research and Drug Development
Abstract
This article provides a comprehensive guide for researchers and drug development professionals confronting the pervasive challenge of cross-reactivity in immunoassays. It explores the fundamental causes and impacts of cross-reactivity, from structural similarity to reagent choice. The content delivers practical methodological approaches for detection and application, advanced techniques for troubleshooting and optimization, and robust frameworks for assay validation and comparative analysis against gold-standard methods. By synthesizing foundational knowledge with cutting-edge strategies, this resource empowers scientists to improve assay reliability, data accuracy, and decision-making in preclinical and clinical studies.
Understanding Immunoassay Cross-Reactivity: From Fundamental Causes to Clinical Consequences
FAQs: Understanding and Troubleshooting Cross-Reactivity
What is cross-reactivity in the context of an immunoassay?
Cross-reactivity is the ability of an antibody to bind to molecules other than its intended target antigen. These molecules, called cross-reactants, often have a high structural similarity or homology to the target analyte [1]. This is not merely nonspecific binding; it is a specific reaction with a known, structurally similar substance that can be proven experimentally [2] [1].
Why is cross-reactivity more than just a nuisance in drug development?
In drug development, cross-reactivity is a critical safety and efficacy parameter. For therapeutic antibodies, a standard required test prior to Phase I clinical studies is the Tissue Cross-Reactivity (TCR) assay [2]. This immunohistochemistry-based method screens for off-target binding of the therapeutic candidate to human tissues, helping to identify potential toxicities early in the development process [3]. Undetected cross-reactivity can lead to drug failure or adverse patient effects.
I am developing a multiplex assay. What types of cross-reactivity should I test for?
In a multiplexed array format, where multiple assays run simultaneously on a single sample, you must test for several specific types of cross-reactivity to ensure each result is a true positive [4]. The table below summarizes the key types.
Table: Types of Cross-Reactivity in Multiplex Immunoassays
| Type of Cross-Reactivity | Description | Impact on Assay |
|---|---|---|
| Antigen-Capture Antibody [4] | A capture antibody binds the wrong antigen. | The two cross-reactive systems cannot be multiplexed under the tested conditions. |
| Detection-Capture Antibody [4] | A detection antibody binds directly to a capture antibody spot. | Often resolvable through reagent or diluent optimization. |
| Antigen-Detection Antibody [4] | A captured antigen is detected by the detection antibody from a different assay. | Not necessarily problematic; can sometimes be used as an additional detection method. |
| Capture Antibody-Conjugate [4] | The label (e.g., streptavidin-HRP) binds directly to a capture antibody. | Unacceptable; must be resolved for the assay to be valid. |
| Antigen-Conjugate [4] | The label binds directly to a captured antigen. | Unacceptable; must be resolved for the assay to be valid. |
My immunoassay is producing false positives. How can I determine if cross-reactivity is the cause?
A core experimental method to test for sample-based interference, including cross-reactivity, is the spike and recovery experiment [5]. This validation assesses whether components in a sample matrix interfere with accurate analyte detection.
Protocol: Spike and Recovery Experiment
- Sample Preparation: Prepare three sets of samples in duplicate or triplicate:
- Neat Matrix: The sample matrix (e.g., serum, plasma) with no additions.
- Spiked Buffer (Control): A known concentration of the pure analyte spiked into an ideal assay buffer.
- Spiked Matrix (Test): The same known concentration of analyte spiked into the actual sample matrix.
- Analysis: Run all samples according to your assay protocol.
- Calculation and Interpretation: Calculate the percentage recovery for the spiked matrix compared to the spiked buffer control [5].
Table: Interpreting Spike and Recovery Results
| % Recovery | Interpretation |
|---|---|
| 80–120% | Acceptable; minimal interference. |
| < 80% | Signal suppression; indicates matrix interference. |
| > 120% | Signal enhancement; suggests interference or cross-reactivity. |
A recovery value outside the acceptable range indicates that something in the sample matrix is interfering, prompting further investigation into the root cause [5].
How can I reduce or prevent cross-reactivity in my assays?
Several strategic and practical steps can minimize cross-reactivity:
- Use High-Affinity, Specific Antibodies: Antibodies with high affinity are less likely to have problematic cross-reactivity [1]. Monoclonal antibodies often provide higher specificity than polyclonal antibodies because they recognize a single epitope [6].
- Employ Blocking Agents: Use normal serum, Bovine Serum Albumin (BSA), casein, or commercial heterophilic antibody blockers to saturate potential interfering sites and prevent nonspecific binding [5].
- Optimize Assay Conditions: Cross-reactivity is not an immutable property of the antibodies alone. It can be influenced by the assay format, the concentrations of immunoreactants, and the reaction time. Shifting to assays that use lower reagent concentrations can sometimes increase specificity and lower cross-reactivity [7].
- Dilute the Sample: Dilution can reduce the concentration of interfering substances. Ensure the assay is validated for diluted samples [5] [6].
- Utilize Matched Antibody Pairs: Using validated matched monoclonal or polyclonal antibody pairs can significantly improve specificity [5].
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Reagents for Cross-Reactivity Assessment and Mitigation
| Reagent / Material | Function in Cross-Reactivity Studies |
|---|---|
| Monoclonal Antibodies [6] | Provide high specificity by recognizing a single epitope; ideal as capture antibodies to establish assay specificity. |
| Blocking Agents (BSA, Casein) [5] | Reduce nonspecific binding by saturating potential interfering sites on the solid support or sample proteins. |
| Heterophilic Antibody Blockers [5] | Specifically reduce interference from human anti-animal antibodies (HAAA), a common source of false positives. |
| Positive Control Sera/Plasma [5] | Contain known interferents (e.g., HAMA, Rheumatoid Factor) used as controls to validate mitigation strategies. |
| Matrix Effects Controls [5] | Purified substances (e.g., bilirubin, hemoglobin, cholesterol) used to spike samples and characterize their interfering effects. |
| High-Throughput Protein Arrays [3] | Platforms that screen antibody binding against hundreds or thousands of protein targets simultaneously to comprehensively profile cross-reactivity. |
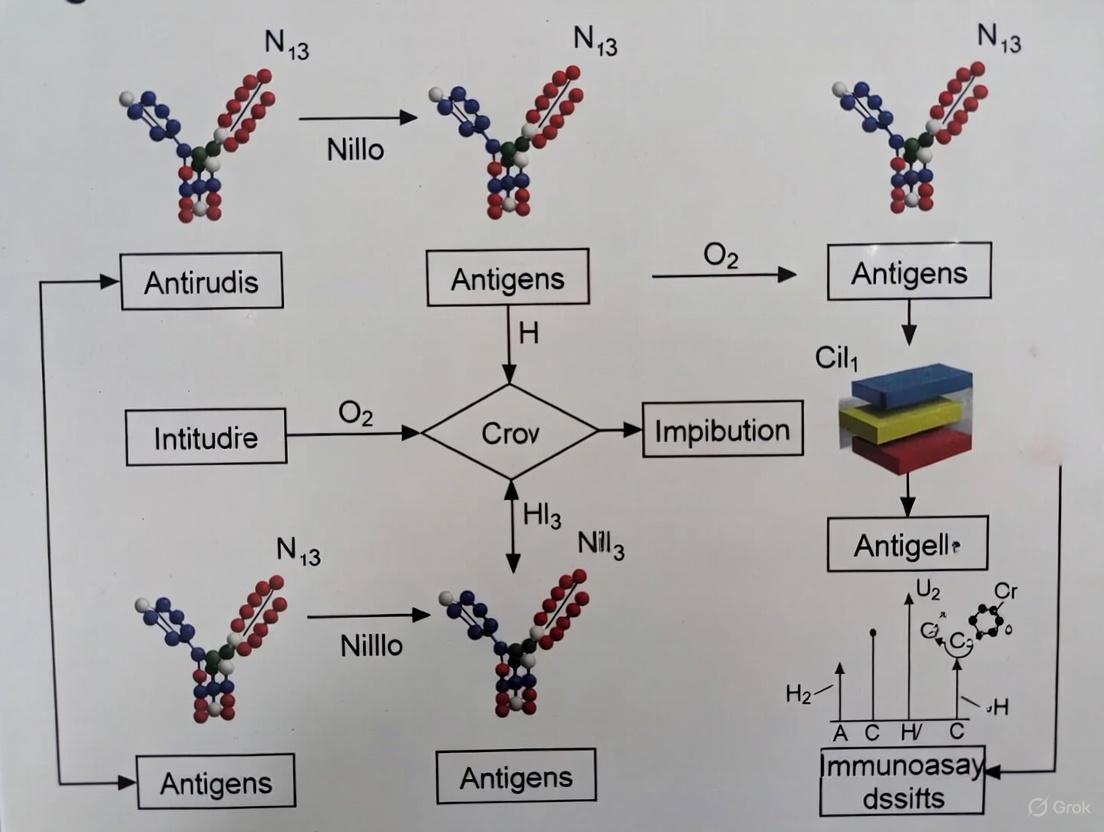
Experimental Guide: A Workflow for Systematic Cross-Reactivity Assessment
For a rigorous assessment, follow a structured workflow. The diagram below outlines the key stages, from initial testing to implementation of solutions.
A critical step is quantifying the level of cross-reactivity, especially in competitive immunoassays. The most accepted method is to compare the dose-response curves of the target analyte and the cross-reactant.
Protocol: Calculating Percent Cross-Reactivity
- Generate Dose-Response Curves: For both the target analyte and the potential cross-reactant, run a dilution series to create standard curves. The assay should be performed under equilibrium conditions for accurate comparison [7] [8].
- Determine IC50 Values: Calculate the concentration of each substance that causes a 50% decrease in the maximum assay signal (e.g., 50% binding of the labeled analyte) [2] [8].
- Calculate % Cross-Reactivity: Use the following formula [8]: > % Cross-Reactivity = (IC50 of Target Analyte / IC50 of Cross-Reactant) × 100%
A lower percentage indicates higher specificity of the assay for the target analyte over the interfering substance. This quantitative measure is essential for validating an assay's reliability [8].
Frequently Asked Questions
What is the fundamental mechanism behind antibody cross-reactivity? Cross-reactivity occurs when an antibody's antigen-binding site (paratope) recognizes and binds to two or more different antigens that share similar structural regions or epitopes. This similarity can exist in the three-dimensional shape and physicochemical properties of the epitopes, even if their amino acid sequences aren't identical. The antibody's Fab region has a specific amino acid sequence that dictates its affinity, and if another antigen presents a sufficiently similar structural region, binding can occur [9].
Why do some assays show cross-reactivity while others don't, even with the same antibodies? Cross-reactivity is not an intrinsic property of antibodies alone but is significantly influenced by assay conditions. Immunoassays implemented with sensitive detection systems that use low concentrations of antibodies and competing antigens typically demonstrate lower cross-reactivity and higher specificity. Conversely, assays requiring high concentrations of reagents tend to be less specific and show higher cross-reactivity. The format (competitive vs. sandwich), reagent concentrations, and reaction times all contribute to the observed cross-reactivity profile [7].
How can I computationally predict if my antibody will cross-react? You can perform a quick assessment using NCBI-BLAST for pair-wise sequence alignment between your immunogen sequence and the potential cross-reactive protein [9].
- >75% homology: Almost guaranteed cross-reactivity
- >60% homology: Strong likelihood of cross-reactivity, requires experimental verification Polyclonal antibodies generally have a higher propensity for cross-reactivity as they recognize multiple epitopes, whereas monoclonal antibodies, recognizing a single epitope, offer higher specificity [6] [9].
What are the key structural factors that make two epitopes cross-reactive? Two primary structural scenarios can lead to cross-reactivity [10]:
- Sequence Similarity: Epitopes with similar amino acid composition can produce similar interaction surfaces.
- Structural Mimicry: Sequences with no obvious similarity can exhibit nearly identical topographical and electrostatic charge distribution patterns, creating similar TCR interaction surfaces.
What are the practical consequences of cross-reactivity in research and diagnostics?
- Positive Implications: Enables broader pathogen protection; useful for developing cross-protective vaccines [11].
- Negative Implications: Causes false positives/negatives in immunoassays; may trigger autoimmune reactions when self and non-self epitopes are similar [12] [11].
Troubleshooting Guides
Problem: Unexpected Cross-Reactivity in Immunoassay
Unexpected cross-reactivity can lead to inaccurate data interpretation, particularly when detecting a specific analyte in the presence of structurally similar compounds.
Step-by-Step Investigation:
- Verify Assay Conditions: Transition your assay to conditions that use lower concentrations of antibodies and labeled antigens. This increases specificity by favoring only the highest-affinity interactions [7].
- Identify Potential Cross-Reactants: Compile a list of structurally similar compounds that might be present in your sample. Use database searches (e.g., PubChem) to find analogs and metabolites.
- Check Homology: Perform NCBI-BLAST alignment of your antibody's immunogen sequence against the proteome of your sample source to identify proteins with high sequence homology (>60%) [9].
- Test for Interference:
- Serial Dilution: A non-linear dilution curve suggests the presence of interference [13].
- Spike-and-Recovery: Add a known quantity of the target analyte and a suspected cross-reactant to the sample matrix. Poor recovery indicates interference [6].
- Use a Different Assay Format: If using a competitive format, try a sandwich format (if applicable), as it typically uses two antibodies and is less prone to certain cross-reactivities [13].
- Switch Antibody Type: If using a polyclonal antibody, consider switching to a monoclonal antibody for higher specificity to a single epitope [6] [9].
Problem: Determining Cross-Reactivity During Antibody Validation
Accurately characterizing an antibody's cross-reactivity profile is essential for ensuring experimental specificity.
Experimental Protocol:
- Objective: To quantify the ability of an antibody to distinguish between its target antigen and potential cross-reactants.
- Principle: A competitive immunoassay format is used to determine the concentration of cross-reactant required to displace the binding of a labeled reference analyte, compared to the unlabeled target itself.
| Step | Action | Key Parameter |
|---|---|---|
| 1. Preparation | Coat plates with the target antigen. | Use a consistent coating concentration. |
| 2. Competition | Pre-incubate a fixed antibody concentration with a serial dilution of either the target or cross-reactant. Then transfer to antigen-coated plates. | Use a wide concentration range (e.g., 0.1-1000 nM). |
| 3. Detection | Add detection antibody (species-specific) and substrate. Measure signal. | Signal is inversely proportional to competitor concentration. |
| 4. Analysis | Plot log(concentration) vs. response to generate inhibition curves. Calculate IC50 for target and cross-reactant. | IC50 is the concentration causing 50% signal inhibition. |
| 5. Calculation | Calculate cross-reactivity (CR):CR (%) = [IC50(target) / IC50(cross-reactant)] × 100% | A lower CR % indicates higher specificity [7]. |
Problem: Cross-Reactivity in Multiplexed Immunostaining
In experiments like immunohistochemistry or immunofluorescence, cross-reactivity can occur between secondary antibodies and off-target species immunoglobulins, leading to false-positive signals.
Solutions:
- Use Cross-Adsorbed Secondary Antibodies: These antibodies undergo an additional purification step to remove members that bind to off-target immunoglobulins, drastically reducing species cross-reactivity [9].
- Employ Directly Conjugated Primary Antibodies: By conjugating your primary antibody with a fluorophore or enzyme, you eliminate the need for secondary antibodies, thereby removing the source of this type of cross-reactivity [9].
- Select Antibodies from Different Hosts: Ensure that primary antibodies raised in different species are used when multiplexing. Then, use highly specific secondary antibodies that are raised against the immunoglobulin of one species and cross-adsorbed against others [9].
- Utilize Monoclonal Antibodies of Different Subtypes: When using multiple mouse monoclonal antibodies, select antibodies of different IgG subtypes (e.g., IgG1, IgG2a, IgG2b, IgG3). You can then use subtype-specific Nano-Secondary antibodies that show no cross-reactivity with other subclasses [9].
Data Presentation
Quantitative Guidance for Predicting Cross-Reactivity
The following table summarizes key quantitative thresholds and their implications for cross-reactivity based on sequence and structural analysis.
| Parameter | Threshold/Value | Implication for Cross-Reactivity | Source/Context |
|---|---|---|---|
| Sequence Homology | >75% | Almost guaranteed cross-reactivity [9] | NCBI-BLAST alignment of immunogen sequence. |
| >60% | Strong likelihood; requires experimental verification [9] | NCBI-BLAST alignment of immunogen sequence. | |
| Assay Concentration | Low [Ab], [Ag*] | Lower cross-reactivity; higher specificity [7] | Competitive immunoassay format. |
| High [Ab], [Ag*] | Higher cross-reactivity; lower specificity [7] | Competitive immunoassay format. | |
| Performance Metric (Influenza) | AUC ~0.9 | Stable, high performance in predicting antigenic similarity [14] | CE-BLAST tool validation on HI data. |
Research Reagent Solutions
This table details essential materials and computational tools used to study, predict, and mitigate cross-reactivity.
| Reagent/Tool | Function/Description | Utility in Cross-Reactivity Context |
|---|---|---|
| Monoclonal Antibody (mAb) | Homologous IgG population recognizing a single epitope [9]. | Increases assay specificity; reduces cross-reactivity risk. |
| Polyclonal Antibody (pAb) | Heterogeneous mixture recognizing multiple epitopes [6]. | Higher sensitivity; may show desired cross-reactivity across species. |
| Cross-Adsorbed Secondary Antibody | Secondary antibody purified to remove off-target species reactivity [9]. | Critical for multiplex staining to prevent false positives. |
| NCBI-BLAST | Tool for pair-wise sequence alignment [9]. | Quickly predicts potential cross-reactivity based on sequence homology. |
| CE-BLAST | Computational tool for calculating antigenic similarity based on 3D conformational epitopes [14]. | Predicts cross-reactivity for newly emerging pathogens independent of binding-assay data. |
| DockTope/CrossTope | In silico tools for modeling pMHC-I structures and comparing them to immunogenic targets [10]. | Identifies T-cell cross-reactivity by analyzing structural/physicochemical similarities. |
Experimental Protocols
Detailed Protocol: Calculating Cross-Reactivity in a Competitive ELISA
This protocol provides a standardized method to quantify the cross-reactivity of an antibody against structurally similar compounds.
1. Materials
- Target antigen and potential cross-reactants
- Validated primary antibody
- Coating buffer (e.g., carbonate-bicarbonate buffer, pH 9.6)
- Blocking buffer (e.g., PBS with 1-5% BSA)
- Washing buffer (e.g., PBS with 0.05% Tween 20)
- Detection antibody (enzyme-conjugated, specific for the primary antibody host species)
- Enzyme substrate
- Stop solution
2. Procedure 1. Coating: Dilute the target antigen in coating buffer to a predetermined optimal concentration. Add to the wells of a microtiter plate and incubate overnight at 4°C. 2. Blocking: Wash the plate 3 times with washing buffer. Add blocking buffer to each well and incubate for 1-2 hours at room temperature to block non-specific binding sites. 3. Competition: Prepare a fixed, constant concentration of primary antibody (determined from prior titration). In separate tubes, pre-incubate this antibody with a series of dilutions (e.g., from 0.1 nM to 1000 nM) of either: - The target antigen (standard curve) - Each potential cross-reactant - A negative control (buffer only) Incubate for a set time (e.g., 1-2 hours) at room temperature. 4. Binding: Transfer the pre-incubated mixtures to the washed, antigen-coated plate. Incubate to allow the free antibody to bind to the coated antigen. 5. Detection: Wash the plate. Add the enzyme-conjugated detection antibody and incubate. Wash again. Add the substrate solution and incubate for a defined period. 6. Stop and Read: Add stop solution and immediately measure the absorbance.
3. Data Analysis
1. Plot the mean absorbance (or % of maximum signal) for each concentration against the logarithm of the competitor concentration.
2. Fit a four-parameter logistic (4PL) curve to the data for the target and each cross-reactant.
3. From the curve, determine the IC50 value for each compound.
4. Calculate the percentage cross-reactivity for each cross-reactant using the formula:
Cross-Reactivity (%) = (IC50 of Target / IC50 of Cross-Reactant) × 100% [7].
Workflow: An Integrated Structural Approach to Troubleshoot T-Cell Cross-Reactivity
This workflow diagram outlines a computational and experimental pipeline for investigating T-cell epitope cross-reactivity, which is crucial for vaccine design and understanding immune responses.
Visualization of Concepts
Epitope Recognition and Cross-Reactivity Scenarios
This diagram illustrates the fundamental concepts of epitope recognition by antibodies and the two main scenarios that lead to cross-reactivity: shared linear sequence motifs and conformational similarity.
FAQ: Understanding Immunoassay Interference
What are the main types of interference in immunoassays? Interferences in immunoassays can be broadly categorized into two groups: those that alter the measurable concentration of the analyte in the sample and those that alter antibody binding [12]. The first group includes factors like hormone-binding proteins, autoanalyte antibodies, and pre-analytical errors. The second group includes heterophile antibodies, human anti-animal antibodies (HAAAs), rheumatoid factors, and the high-dose hook effect [12] [15].
How does cross-reactivity differ from other interferences? Cross-reactivity is a specific and often predictable type of interference where substances structurally similar to the target analyte compete for the antibody-binding site [8]. This is distinct from non-specific interferences like heterophile antibodies, which can bind to reagent antibodies regardless of the analyte's structure [12]. Cross-reactivity is a particular issue in competitive immunoassays and with drug metabolites [16] [15].
Why is cross-reactivity a significant problem in Therapeutic Drug Monitoring (TDM)? In TDM, metabolite cross-reactivity can lead to significant overestimation or underestimation of drug levels, potentially resulting in incorrect dosage adjustments. For example [16]:
- Digoxin immunoassays are affected by endogenous digoxin-like immunoreactive substances and various drugs and herbal supplements.
- Carbamazepine is metabolized to an epoxide, and the cross-reactivity of this metabolite in immunoassays can range from 0% to 94%.
- Immunosuppressants like cyclosporin A are subject to significant metabolite interference, leading to results up to 174% higher than reference methods [12].
What are some common sources of pre-analytical errors? Pre-analytical errors arise from issues in sample collection, storage, or processing [17]. These include:
- Haemolysis: The breakdown of red blood cells can release interferents.
- Incorrect Anticoagulants: The use of EDTA, citrate, or fluoride can chelate ions necessary for assay chemistry or inhibit enzyme labels [12] [17].
- Sample Contamination: Components from blood collection tubes (e.g., stoppers, separator gels) can leach into specimens or adsorb analytes [17].
- Delay in Processing or Incorrect Storage: This can lead to analyte degradation or generation of interfering substances [17].
Troubleshooting Guide: Identifying and Addressing Interference
The following table summarizes key interference sources, their effects, and potential solutions.
| Interference Source | Effect on Assay | Troubleshooting & Solutions |
|---|---|---|
| Metabolite Cross-reactivity [16] [15] | Falsely elevated or decreased reported drug concentration. | Use a more specific method (e.g., LC-MS/MS); verify results with a different immunoassay platform; be aware of metabolite profiles in specific patient populations. |
| Heterophile Antibodies & HAAAs [12] [15] | Primarily false-positive results in sandwich immunoassays; can also cause false negatives. | Use blocking reagents in the assay; re-analyze with a heterophile antibody blocking tube; dilute the sample to check for non-linearity; use an alternative assay format. |
| Endogenous Binding Proteins (e.g., cortisol-binding globulin) [12] | Alters the measurable free (active) concentration of the analyte. | Use assays that include steps to denature or block binding proteins; measure free analyte if clinically relevant. |
| Pre-analytical Variations [12] [17] | Variable and unpredictable effects on analyte stability and detection. | Follow standardized collection and storage protocols; ensure correct fill volumes; centrifuge samples to remove particulates and lipids [18]. |
| Concomitant Medications (structurally similar) [19] | False-positive results in drug screens (e.g., amphetamine, methadone assays). | Confirm all presumptive positive screening results with a specific method like GC-MS or LC-MS/MS. |
| Lipemia, Icterus, Hemolysis [12] | Can interfere with nephelometry/turbidimetry or physically quench signals. | Clarify samples by high-speed centrifugation prior to analysis [18]. |
Experimental Protocols for Investigating Interference
Protocol 1: Assessing Cross-Reactivity Using a Spiked Specimen
This methodology is commonly used to validate assay specificity and is detailed in commercial assay package inserts [8].
- Preparation of Spiked Samples: Obtain a drug-free biological matrix (e.g., pooled human serum or plasma). Prepare a concentrated stock solution of the potential cross-reactant. Spike the matrix with a known concentration of the cross-reactant. A common approach is to add 100 µg/dL of the cross-reactant to the specimen [8].
- Measurement: Assay both the unspiked (baseline) and spiked specimens using the immunoassay under investigation.
- Calculation of Cross-Reactivity: Calculate the percentage cross-reactivity using the formula: Cross-reactivity (%) = (Measured concentration in spiked sample – Baseline concentration) / Concentration of cross-reactant added × 100% [8]. Interpretation: A high percentage indicates significant cross-reactivity, which may lead to clinically relevant false positives.
Protocol 2: A Data-Driven Approach for Discovering Novel Cross-Reactivities
This systematic protocol, based on analysis of Electronic Health Record (EHR) data, can be used to discover previously unknown interferents [19].
- Data Assembly: Extract a large dataset of immunoassay results linked to documented medication exposures for the corresponding patients. The dataset should include both negative and presumptive positive results that were later confirmed as false positives by a reference method.
- Statistical Analysis: For each assay-ingredient pair, use logistic regression to quantify the association between previous exposure to a drug and a false-positive screen result. The outcome is expressed as an odds ratio, where a high odds ratio suggests the ingredient is a potential cross-reactant [19].
- Experimental Validation: Select compounds with the strongest statistical associations. Spike the candidate cross-reactant into drug-free urine or serum and test the spiked samples on the immunoassay to confirm the interference [19].
Visualizing Interference Mechanisms and Workflows
Interference Mechanisms in Immunoassays
Workflow for Systematic Interference Investigation
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for troubleshooting cross-reactivity.
| Research Reagent / Material | Function in Troubleshooting |
|---|---|
| Heterophile Blocking Reagents | Contains inert animal antibody fragments that bind to heterophile antibodies and HAAAs, preventing them from interfering with the assay antibodies [12]. |
| Stripped / Matrix-Matched Serum | Analyte-free biological matrix used as a baseline control and for preparing spiked samples in cross-reactivity and recovery experiments [8]. |
| Monoclonal vs. Polyclonal Antibodies | Monoclonal antibodies offer high specificity for a single epitope, while polyclonal antibodies may be more sensitive but can show broader cross-reactivity; choice depends on the desired selectivity [7]. |
| LC-MS/MS System | A reference method that separates molecules by mass, providing high specificity to confirm immunoassay results and definitively identify cross-reacting substances [16] [19]. |
| Solid-Phase Extraction (SPE) Cartridges | Used to clean up complex samples (e.g., urine, serum) by removing salts, lipids, and other potential interferents prior to analysis, reducing matrix effects. |
This technical support center provides a targeted resource for researchers troubleshooting cross-reactivity in immunoassays. The following guides and FAQs are framed within the context of a broader thesis on mitigating these issues in pharmaceutical and clinical research.
Frequently Asked Questions (FAQs)
What is cross-reactivity and why is it a problem?
Cross-reactivity occurs when an antibody in an immunoassay binds not only to its target analyte but also to structurally similar compounds it was not designed to detect [20]. Think of it like a lock (antibody) that can be opened by several similar, but not identical, keys (analytes) [20]. This is problematic because it can lead to false-positive results or inflated quantitative readings, compromising data integrity and leading to incorrect conclusions in both clinical diagnostics and drug development [19] [21]. For example, in urine drug screening, cross-reactivity from medications can suggest illicit drug use where there is none, potentially damaging the patient-provider relationship [19] [20].
Does a positive screening result always mean the target is present?
No. A presumptively positive result on an immunoassay screen should be interpreted with caution, as it may be caused by a cross-reactive substance [19] [20]. For example, the over-the-counter decongestant pseudoephedrine can cause a positive amphetamine screen [20]. It is a standard best practice to confirm presumptive positive results with a more specific technique, such as LC-MS/MS or GC-MS [19] [20].
Is cross-reactivity an inherent property of the antibodies alone?
Not exclusively. Recent research demonstrates that cross-reactivity is not a fixed parameter determined solely by the antibodies used [7]. The same antibody can exhibit different cross-reactivity profiles depending on the assay format (e.g., ELISA vs. FPIA), the concentration of reagents, and whether the assay is run under kinetic or equilibrium conditions [7]. Shifting to assay conditions that require lower concentrations of reagents and markers can reduce cross-reactivity, making the assay more specific [7].
Can the host species of a sample influence cross-reactivity?
Yes. Studies on serological assays have shown that absolute and relative antibody titers can vary systematically across different host species, even when infected with the identical pathogen strain [22] [23]. This means that the same infecting serovar can produce different cross-reactivity profiles in different host species, and the highest antibody titer is not always a reliable indicator of the infecting agent [23].
Quantitative Data on Common Cross-Reactants
The following table summarizes documented and potential cross-reactivities that can lead to false-positive or inflated results. Data is compiled from systematic analyses of electronic health records and subsequent experimental validation [19].
Table 1: Documented and Potential Cross-Reactivities in Urine Drug Screening Immunoassays
| Target Assay | Cross-Reactive Compound | Impact / Outcome | Evidence Level |
|---|---|---|---|
| Amphetamines | Pseudoephedrine | False Positive | Known Cross-Reactivity [20] |
| Amphetamines | Other Unspecified Medications | False Positive | Newly Discovered [19] |
| Buprenorphine | Unspecified Medications | False Positive | Newly Discovered [19] |
| Cannabinoids (THC) | Unspecified Medications | False Positive | Newly Discovered [19] |
| Methadone | Unspecified Medications | False Positive | Newly Discovered [19] |
| Opiates | Poppy Seeds | False Positive | Known Interference [20] |
Troubleshooting Guide: Mitigating Cross-Reactivity
Problem: Suspected cross-reactivity is causing inconsistent or unexpected positive results.
Step 1: Review Medication and Exposure History
- Action: Compile a complete list of the donor's or subject's prescriptions, over-the-counter medications, and supplements [20].
- Rationale: Many cross-reactivities are caused by legitimate medications with structures similar to the target illicit drug [19] [20].
Step 2: Implement Confirmatory Testing
- Action: Send the sample for confirmatory testing using a highly specific method like GC-MS or LC-MS/MS [19] [20].
- Rationale: These techniques can distinguish between the target analyte and structurally similar cross-reactants, providing a definitive result [20].
Step 3: Optimize Your Immunoassay Protocol
- Action: Consider adjusting your assay conditions to enhance specificity.
- Vary Reagent Concentrations: Using lower concentrations of antibodies and competing antigens can reduce cross-reactivity [7].
- Explore Heterologous Formats: Using a different antigen derivative in the assay than the one used for immunization can narrow the spectrum of antibody selectivity [7].
- Utilize Antibody Fragments: Using F(ab) antibody fragments instead of full IgG can help avoid interference from endogenous factors like rheumatoid factor and complement [21].
- Rationale: Cross-reactivity is modulated by assay conditions, not just antibody affinity, offering a path to improve specificity without developing new reagents [7].
Step 4: Use Blocking Agents
- Action: For specific interferents, add blocking agents to the sample or diluent.
- Rheumatoid Factor (RF): Add heat-aggregated IgG or use 2-mercaptoethanol to degrade RF [21].
- Complement: Use EDTA to chelate calcium and magnesium, preventing complement activation [21].
- Heterophilic Antibodies: Add an excess of animal IgG (e.g., mouse IgG) to the sample to block these antibodies [21].
- Rationale: These agents bind to or inactivate common interfering substances before they can interfere with the assay antibodies [21].
Experimental Protocol: Systematic Discovery of Cross-Reactive Substances
This methodology, adapted from a large-scale study using Electronic Health Record (EHR) data, provides a framework for proactively identifying unknown cross-reactants [19].
Objective: To systematically identify and validate previously unknown cross-reactive substances for a given immunoassay.
Materials:
- EHR dataset linked to historical immunoassay results (e.g., 698,651 results) [19].
- Data on previous medication exposures for tested individuals [19].
- Drug-free urine for spiking experiments [19].
- Suspect cross-reactive compounds and metabolites [19].
- Target immunoassay platform and confirmatory LC-MS/MS or GC-MS equipment [19].
Procedure:
Data Linkage and Analysis:
- Link each historical immunoassay result to all documented drug exposures for that individual in the 1-30 days prior to testing [19].
- Use statistical models (e.g., Firth's logistic regression) to quantify the association between exposure to a specific ingredient and the odds of a false-positive screen. An odds ratio (OR) greater than 1 suggests potential cross-reactivity [19].
- Prioritize compounds with the strongest statistical associations for experimental testing [19].
Experimental Validation:
- Spike drug-free urine with the suspected cross-reactive compound (or its metabolites) at physiologically relevant concentrations [19].
- Run the spiked sample on the target immunoassay.
- A presumptive positive result on the immunoassay, followed by a negative confirmation on the specific LC-MS/MS for the target drug, validates the substance as a cross-reactant [19].
The workflow below visualizes this systematic approach:
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Resources for Investigating Cross-Reactivity
| Tool / Reagent | Function / Application | Key Consideration |
|---|---|---|
| F(ab) Antibody Fragments | Replaces full IgG to avoid interference from RF, complement, and heterophilic antibodies [21]. | Increases specificity but may require custom preparation. |
| Animal IgG (e.g., Mouse IgG) | Added to sample as a blocking agent to neutralize heterophilic antibodies [21]. | Concentration is critical; insufficient amount will be ineffective [21]. |
| EDTA | Chelating agent used as an anticoagulant to inhibit complement interference [21]. | A simple and effective step for specific interferents. |
| Heterologous Assay Format | Uses a different antigen derivative in the assay than was used for immunization [7]. | Can narrow selectivity but requires additional chemical synthesis [7]. |
| Computational Tools (e.g., ARDitox) | AI-driven platform to predict off-target and cross-reactive epitopes for T-cell receptors, supporting safer immunotherapy design [24]. | Useful for early-stage risk assessment in cell therapy development. |
| Normalization Algorithms (for Luminex) | Computational methods (e.g., orthogonal regression, GAM) to correct for background fluorescence and machine drift, reducing false signals [25]. | Enhances assay reproducibility and minimizes technical noise. |
Frequently Asked Questions
1. What are the most common causes of interference in steroid hormone immunoassays? Interference in steroid hormone immunoassays primarily arises from:
- Cross-reactivity: Structurally similar compounds, such as endogenous steroid precursors, metabolites, or synthetic drugs (e.g., prednisolone), are mistakenly recognized by the assay antibodies [26] [27].
- Endogenous Antibodies: Human anti-animal antibodies (HAAA) or heterophile antibodies can bind to assay reagents, causing false elevation or suppression of results [26] [12] [28].
- Biotin: High circulating concentrations of biotin from supplement intake can interfere with assays that use biotin-streptavidin technology [26] [28].
- The High-Dose Hook Effect: In sandwich immunoassays, extremely high analyte concentrations can saturate both capture and detection antibodies, leading to a falsely low reported result [26] [28].
- Sample Matrix Effects: Abnormal levels of lipids, bilirubin, or haemoglobin can interfere with some assay detection systems [12] [28].
2. How can I recognize potential interference in my immunoassay results? Interference should be suspected when:
- The laboratory result is clinically inconsistent with the patient's presentation or previous history [26] [28].
- Results from different immunoassay platforms for the same sample are discordant [29] [30].
- There is an implausible hormone profile or a lack of correlation between related biomarkers [26].
- A result changes dramatically upon sample dilution in a non-linear fashion, which may indicate the hook effect [28].
3. What practical steps can I take to investigate suspected interference? If you suspect interference, the following investigative steps are recommended:
- Consult the Package Insert: Review the cross-reactivity data provided by the assay manufacturer for known interfering substances [27].
- Perform Serial Dilutions: A lack of linearity upon dilution can confirm the presence of an interferent [28] [6].
- Use a Blocking Reagent: Pre-incubating the sample with commercial blocking agents can neutralize heterophile antibody or HAAA interference [12].
- Re-assay with an Alternative Method: The most definitive approach is to re-measure the analyte using a different immunoassay platform or a reference method like liquid chromatography-tandem mass spectrometry (LC-MS/MS), which is less susceptible to such interferences [29] [27] [30].
4. When should I consider using mass spectrometry instead of immunoassay? Mass spectrometry (e.g., LC-MS/MS) is the preferred method in scenarios requiring high specificity and sensitivity, such as:
- Measuring steroids in pediatric endocrinology, where hormone concentrations are very low [29] [30].
- Diagnosing and monitoring complex endocrine disorders like congenital adrenal hyperplasia (CAH), where multiple structurally similar steroids need to be quantified accurately [30].
- Verifying unexpected or clinically implausible results obtained from an immunoassay [29] [27].
- Quantifying vitamin D metabolites, as LC-MS/MS minimizes cross-reactivity issues common in immunoassays [30].
Troubleshooting Guide: A Step-by-Step Experimental Protocol for Investigating Cross-Reactivity
This protocol outlines a systematic approach to confirm and characterize cross-reactivity in a steroid hormone immunoassay, based on established guidelines [27].
Objective: To determine if a specific compound (the "cross-reactant") interferes with the accurate measurement of the target steroid hormone.
Materials:
- The immunoassay platform and reagents under investigation.
- Pooled normal human serum or plasma (as an analyte-free matrix).
- Purified target analyte (the steroid of interest).
- Purified cross-reactive compound.
- Appropriate solvents for dissolving standards (ensure they do not interfere with the assay).
Experimental Workflow:
The following diagram illustrates the logical workflow for the experimental protocol.
Methodology:
- Preparation of Spiked Samples:
- Target Analyte Calibration Curve: Prepare a series of calibration standards by spiking the analyte-free matrix with known concentrations of the purified target analyte. This establishes the standard dose-response curve.
- Cross-reactant Samples: Prepare a separate series of samples by spiking the analyte-free matrix with a range of concentrations of the purified cross-reactive compound.
Immunoassay Execution:
- Run all spiked samples (both the target analyte and cross-reactant series) in the same immunoassay run to minimize inter-assay variability.
- Ensure each sample is analyzed in duplicate or triplicate for precision.
Data Analysis and Calculation:
- For the cross-reactant sample that produces an assay signal closest to the 50% inhibition point (IC₅₀) on the target analyte's calibration curve, calculate the percent cross-reactivity using the formula below [7] [27]:
% Cross-Reactivity = (IC₅₀ of Target Analyte / IC₅₀ of Cross-Reactant) × 100%
- IC₅₀ of Target Analyte: The concentration of the target analyte that reduces the assay signal by 50%.
- IC₅₀ of Cross-Reactant: The concentration of the cross-reactant that reduces the assay signal by 50%.
Interpretation:
- Strong Cross-Reactivity: ≥ 5% - High likelihood of clinical significance.
- Weak Cross-Reactivity: 0.5% - 4.9% - Clinical significance depends on the concentration of the interferent in patient samples.
- Very Weak/Negligible: < 0.5% - Unlikely to be clinically significant [27].
Data Presentation: Clinically Significant Cross-Reactivity Examples
The tables below summarize experimental data for compounds with known clinically significant cross-reactivity in common steroid hormone immunoassays [27].
Table 1: Cross-Reactivity in a Cortisol Immunoassay
| Compound | % Cross-Reactivity | Context for Clinical Significance | Reported Plasma Concentration (ng/mL) | Estimated False Cortisol (ng/mL) |
|---|---|---|---|---|
| Prednisolone | 69% | Glucocorticoid therapy | 100 - 1,500 [27] | 69 - 1,035 |
| 6-Methylprednisolone | 41% | Glucocorticoid therapy | 10 - 300 [27] | 4 - 123 |
| 21-Deoxycortisol | 11% | 21-Hydroxylase Deficiency | 2 - 60 [27] | 0.2 - 6.6 |
| 11-Deoxycortisol | 2.2% | 11β-Hydroxylase Deficiency / Metyrapone test | 50 - 500 [27] | 1.1 - 11 |
Table 2: Cross-Reactivity in a Testosterone Immunoassay
| Compound | % Cross-Reactivity | Context for Clinical Significance |
|---|---|---|
| Methyltestosterone | 35% | Anabolic steroid use |
| Danazol | 13% | Treatment of endometriosis |
| Norethindrone | 2.1% | Progestin therapy (may impact female testosterone measurements) |
| DHEA Sulfate | 0.6% | Endogenous androgenic precursor (may be significant at high concentrations) |
The Scientist's Toolkit: Research Reagent Solutions
This table details key materials and methodologies essential for developing and troubleshooting steroid hormone assays.
| Item | Function & Application | Key Considerations |
|---|---|---|
| Monoclonal Antibodies | Provide high specificity by recognizing a single epitope; ideal for capture antibody in sandwich assays to minimize cross-reactivity [6]. | Lower sensitivity compared to polyclonals as only one antibody binds per antigen [6]. |
| Polyclonal Antibodies | Recognize multiple epitopes; often used as detection antibodies to increase assay sensitivity [6]. | More prone to cross-reactivity due to a broader range of epitope recognition [6]. |
| Blocking Reagents | Neutralize interfering substances like heterophile antibodies and HAAA in patient samples prior to assay [12]. | A critical step for investigating and mitigating antibody-mediated interference. |
| LC-MS/MS | A highly specific reference method that separates and detects steroids based on mass, virtually eliminating antibody-based cross-reactivity [29] [30]. | Overcomes fundamental limitations of immunoassays; recommended for low-concentration steroids and complex diagnoses [30]. |
| Automated Platform (e.g., Gyrolab) | Uses microfluidics and flow-through technology to minimize reagent/sample contact time, reducing matrix interference and reagent consumption [6]. | Useful for precious samples and for improving assay robustness during development. |
Methodological Approaches for Detecting and Leveraging Cross-Reactivity
What is Cross-Reactivity? In immunoassays, cross-reactivity occurs when an antibody binds to an analyte that is structurally similar to, but different from, its target antigen. This binding can lead to false-positive results or an overestimation of the target analyte's concentration, compromising the accuracy and reliability of your data [12] [6]. In drug testing, for example, the over-the-counter decongestant pseudoephedrine can cause a positive amphetamine screen due to its similar molecular structure [20]. Understanding and quantifying cross-reactivity is therefore not merely an academic exercise but a critical component of assay validation.
The IC50 Method Explained The IC50 method is the most widely accepted approach for quantifying cross-reactivity in competitive immunoassay formats. Cross-reactivity is calculated by comparing the concentration of the target analyte required to produce a 50% reduction in the assay signal to the concentration of a cross-reactant needed to produce the same effect [7] [19]. The standard formula for calculating percent cross-reactivity (%CR) is: %CR = [IC50 (Target Analyte) / IC50 (Cross-Reactant)] × 100% [7] An IC50 value represents the inhibitory concentration of a compound that reduces a given biological or biochemical process by half [31]. In the context of a competitive immunoassay, this "process" is the binding of a marker (like a labeled antigen) to the antibody, which is inhibited by the presence of the free analyte.
Step-by-Step Calculation Protocol
Experimental Workflow for IC50 Determination
The following diagram outlines the complete experimental workflow for determining IC50 values and calculating percent cross-reactivity.
Detailed Experimental Methodology
Materials and Reagents:
- Target analyte and cross-reactant compounds of known purity
- Specific antibody (monoclonal or polyclonal)
- Labeled antigen (e.g., enzyme-conjugated, fluorescent)
- Assay buffers and substrate (if applicable)
- Microplates and laboratory equipment for liquid handling and signal detection
Procedure:
- Prepare Serial Dilutions: Create a series of dilutions for both the target analyte and the cross-reactant. A wide concentration range (e.g., spanning several orders of magnitude) is crucial for an accurate curve fit.
- Run Competitive Immunoassay: For each concentration, incubate the sample (containing the target or cross-reactant) with a fixed concentration of antibody and labeled antigen. Perform this in replicate (e.g., n=3) to ensure statistical robustness.
- Measure Signal: After incubation and washing (if required), measure the assay signal (e.g., absorbance, fluorescence, luminescence) for each well.
- Data Analysis:
- Calculate the average signal for each concentration.
- Normalize the data, expressing the signal as a percentage of the maximum signal (typically from the zero-concentration control).
- Plot the normalized signal (%) against the logarithm of the concentration.
- Fit the data to a 4-parameter logistic (4PL) curve. The equation is: Y = Bottom + (Top - Bottom) / (1 + (X/IC50)^HillSlope) where Y is the response, X is the concentration, "Top" and "Bottom" are the plateaus, and the HillSlope describes the steepness of the curve.
- From the fitted curve, determine the IC50 value for both the target and the cross-reactant.
- Calculate % Cross-Reactivity: Apply the standard formula using the obtained IC50 values.
Example Calculation
Assume you have determined the following IC50 values for your target analyte and a potential cross-reactant:
- IC50 (Target Analyte): 5.0 nM
- IC50 (Cross-Reactant): 250.0 nM
The percent cross-reactivity is calculated as: %CR = (5.0 nM / 250.0 nM) × 100% = 2.0%
This result indicates that the cross-reactant is two orders of magnitude less potent than the target analyte in displacing the labeled antigen from the antibody.
Key Research Reagent Solutions
The reliability of your cross-reactivity data is fundamentally dependent on the quality and appropriateness of your research reagents. The table below details key materials and their functions.
Table 1: Essential Reagents for Cross-Reactivity Studies
| Reagent | Function & Importance | Selection Consideration |
|---|---|---|
| Antibody | The primary binding agent; its affinity and specificity define the assay's potential for cross-reactivity [6]. | Monoclonal antibodies offer higher specificity to a single epitope. Polyclonal antibodies can provide higher sensitivity but may increase cross-reactivity risk [6]. |
| Labeled Antigen | Competes with the free analyte for antibody binding sites; generates the detectable signal [7]. | The choice of label (enzyme, fluorescent, etc.) dictates the detection method. Using a "heterologous" label (different from the immunogen) can sometimes improve specificity [7]. |
| Target Analyte & Cross-Reactants | The molecules being tested; their purity and structural integrity are critical for accurate results. | Source compounds from reputable suppliers. Include known metabolites and structurally similar compounds likely to be present in sample matrices. |
| Assay Buffer | Provides the chemical environment (pH, ionic strength) for the antigen-antibody reaction. | Buffer composition can influence antibody affinity and specificity. Optimize to minimize non-specific binding [12]. |
Frequently Asked Questions (FAQs)
Q1: Why did I get a different cross-reactivity value when I changed my assay format (e.g., from ELISA to FPIA)? Cross-reactivity is not an absolute, fixed parameter of an antibody. It is highly dependent on assay conditions. A key factor is the concentration of immunoreagents used. Assays with sensitive detection that use low concentrations of antibodies and labeled antigens are typically more specific and show lower cross-reactivity. Formats requiring higher reagent concentrations can appear less specific [7]. Even within the same format, changing the ratio of reagents or the incubation time (shifting from kinetic to equilibrium conditions) can alter the measured cross-reactivity [7].
Q2: My assay shows high cross-reactivity with an unexpected compound. What should I do? First, verify the result by repeating the experiment. If confirmed, systematically investigate the cause:
- Check Structural Similarity: Analyze the molecular structures of your target and the unexpected cross-reactant. Even seemingly unrelated compounds can share a common sub-structure or epitope that the antibody recognizes [32].
- Review Reagent Specificity: The primary antibody may be promiscuous. A study found that 95% of monoclonal antibodies tested bound to non-target proteins, highlighting the pervasiveness of this issue [6]. Consider screening for a more specific antibody.
- Assay Conditions: Investigate if factors like pH, ionic strength, or matrix components are contributing to the interference [12].
Q3: Is there a way to make my existing immunoassay more specific without developing new antibodies? Yes, you can modulate selectivity by optimizing assay conditions. As demonstrated in research on sulfonamide and fluoroquinolone detection, shifting to lower concentrations of reagents can reduce cross-reactivities by up to five-fold, making the assay more specific [7]. Other strategies include using a heterologous assay format (where the labeled antigen is structurally different from the one used for immunization) or adding blocking agents to the matrix to reduce non-specific interference [7] [6].
Q4: How do I interpret a cross-reactivity value of 0.5%? A cross-reactivity of 0.5% means that the cross-reactant is 200 times less potent than the target analyte in your assay. Specifically, it would require 200 times more of the cross-reactant to produce the same 50% signal inhibition as the target analyte. This level of cross-reactivity is generally considered low, but its acceptability depends on the expected concentration of the cross-reactant in your real samples and the clinical or analytical decision limits of your assay.
Q5: Why is it important to use the IC50 point for calculation instead of another point on the curve? The IC50 point lies on the linear, steepest part of the sigmoidal dose-response curve. This region is most sensitive to changes in concentration and is generally the most precise and reproducible for comparative measurements. Using points at the extremes of the curve (e.g., IC20 or IC80), where the slope is shallow, can lead to greater variability and less reliable cross-reactivity estimates [7] [19].
Key Differences at a Glance
The choice between monoclonal and polyclonal antibodies is fundamental to experimental design, directly impacting specificity, sensitivity, and the potential for cross-reactivity. The table below summarizes their core characteristics:
| Feature | Monoclonal Antibodies (mAbs) | Polyclonal Antibodies (pAbs) |
|---|---|---|
| Origin & Composition | Derived from a single B-cell clone; homogeneous population [33] [34] | Derived from multiple B-cell clones; heterogeneous mixture of antibodies [33] [35] |
| Specificity | Bind to a single, specific epitope; high specificity [33] [36] | Recognize multiple epitopes on the same antigen; broader specificity [33] [35] |
| Cross-Reactivity Potential | Lower inherent risk due to single epitope recognition [35] [6] | Higher inherent risk as different epitopes on similar antigens may be recognized [35] [37] |
| Sensitivity | Can be more sensitive for protein level quantification; lower background noise [35] [36] | High sensitivity for detecting low-quantity proteins; quicker antigen capture [35] |
| Production | Time-consuming (∼6+ months), complex, and costly hybridoma technology [33] [36] | Relatively quick (∼3-4 months), simple, and cost-effective [33] [35] |
| Batch-to-Batch Variability | Low; high reproducibility and unlimited supply from hybridomas [33] [34] | High; requires careful validation for reproducible results [35] [36] |
Frequently Asked Questions & Troubleshooting Guides
How do I proactively check if an antibody will cross-react?
A: Cross-reactivity occurs when an antibody binds to non-target antigens that share structural similarities with the intended target [37]. Proactive checks are crucial for assay validation.
Step 1: Immunogen Sequence Analysis The most straightforward initial check is to perform a pair-wise sequence alignment using the NCBI BLAST tool. This assesses the percentage homology between the antibody's immunogen sequence and related proteins or the protein from your model organism [37].
- Action: Locate the immunogen sequence for your antibody (usually found in the product datasheet) and paste it into the NCBI BLAST "query sequence" box.
- Interpretation: Homology above 75% almost guarantees cross-reactivity. A homology over 60% indicates a strong likelihood and requires experimental verification [37].
Step 2: Antibody Type Consideration
- Polyclonal Antibodies: Have a higher inherent risk of cross-reactivity because they recognize multiple epitopes. If cross-reactivity is a persistent issue, consider switching to a monoclonal antibody [35] [37].
- Monoclonal Antibodies: Offer higher specificity but are not infallible. A single paratope can sometimes bind to unrelated epitopes (mimotopes) that share complementary shape and charge [38].
Step 3: Experimental Validation Always validate antibody specificity within your specific assay system. Key methods include:
- Using a knockout cell line or tissue to confirm the absence of signal.
- Pre-adsorption controls, where the antibody is incubated with an excess of the purified target antigen before application, should abolish the signal.
- Western Blotting to ensure the antibody detects a single band at the expected molecular weight.
My immunoassay shows high background noise. Could antibody choice be the cause?
A: Yes, antibody choice is a primary factor. The solution depends on the nature of the noise.
Scenario: High Background from Non-Specific Binding
- Problem: Polyclonal antibodies, due to their heterogeneity, can contain subpopulations that bind non-specifically to components in the sample matrix [35].
- Solution:
- Use Monoclonal Antibodies: Their uniform structure and single-epitope specificity make them superior for minimizing background noise [35] [36].
- Affinity-Purify Polyclonals: If you must use a polyclonal, ensure it is affinity-purified against the specific antigen to remove non-specific antibodies [35].
- Optimize Blocking and Dilution: Increase the concentration of blocking agents (e.g., BSA, non-fat milk) and titrate the antibody to find the optimal signal-to-noise ratio [39].
Scenario: Cross-Reactivity with Related Proteins
- Problem: The antibody is detecting homologous proteins or protein isoforms present in the sample [12] [6].
- Solution:
- Switch Antibody Type: A monoclonal antibody with high specificity for a unique epitope is the most direct solution [6].
- Use a "Heterologous" Assay Format: In competitive immunoassays, using a modified antigen (heterologous) that differs from the one used for immunization can narrow the spectrum of selectivity by ensuring only a subset of high-affinity antibodies are involved in the detection [7].
- Try a Different Assay Format: Shifting to an assay format that uses lower reagent concentrations (e.g., miniaturized, flow-through systems) can favor high-affinity, specific interactions and reduce low-affinity cross-reactivity [7] [6].
I need to detect a low-abundance target. Which antibody offers the best sensitivity?
A: For maximum sensitivity, polyclonal antibodies are often the preferred first choice.
- Reason: Because a polyclonal antibody mixture targets multiple epitopes on the same antigen, more antibody molecules can bind to a single target protein. This multi-valent binding amplifies the detection signal, making it highly effective for capturing low-quantity proteins [35].
- Best Applications: This makes polyclonal antibodies excellent as capture antibodies in sandwich ELISA, for immunoprecipitation (IP), and for detecting native proteins where epitopes may be partially masked [35] [36].
- Trade-off: The enhanced sensitivity comes with a potentially higher risk of cross-reactivity, which must be managed through careful validation and controls [35].
How can I minimize cross-reactivity in multiplex immunoassays?
A: Multiplex assays require careful planning to prevent secondary antibodies from cross-reacting with primary antibodies from different species.
Strategy 1: Use Cross-Adsorbed Secondary Antibodies
- Action: Always select secondary antibodies that have been cross-adsorbed or highly cross-adsorbed against the immunoglobulins of other species present in your experiment.
- Function: These antibodies undergo an additional purification step to remove contaminants that could bind to off-target immunoglobulins, drastically reducing species cross-reactivity [37].
Strategy 2: Use Monoclonal Antibodies of Different Subtypes
- Action: When multiplexing with mouse primary antibodies, use monoclonals of different IgG subtypes (e.g., IgG1, IgG2a, IgG2b).
- Function: You can then use subtype-specific secondary antibodies (e.g., anti-mouse IgG1, anti-mouse IgG2b) that will only bind to their designated primary antibody, eliminating cross-talk [37].
Strategy 3: Use Directly Conjugated Primaries
- Action: Label your primary antibodies directly with fluorophores or enzymes.
- Function: This eliminates the need for secondary antibodies altogether, thereby completely avoiding secondary antibody-mediated cross-reactivity [37].
The Scientist's Toolkit: Key Reagent Solutions
The following table details essential reagents and strategies for troubleshooting antibody-related issues.
| Reagent / Strategy | Function in Troubleshooting Cross-Reactivity & Improving Specificity |
|---|---|
| Monoclonal Antibodies (mAbs) | Provides high specificity to a single epitope; ideal for reducing background noise and minimizing cross-reactivity with structurally similar antigens [35] [6] [36]. |
| Affinity-Purified Polyclonal Antibodies | Reduces non-specific binding in polyclonal preparations by isolating only the antibodies that bind specifically to the target antigen [35]. |
| Cross-Adsorbed Secondary Antibodies | Critical for multiplexing; removes antibodies that react with immunoglobulins from other species, preventing off-target signal in complex experiments [37]. |
| Recombinant Antibodies | Defined amino acid sequence ensures no batch-to-batch variability and superior reproducibility. Their genetic nature allows for humanization and engineering for enhanced specificity [35] [36]. |
| "Heterologous" Immunoassay | A competitive assay format that uses a modified antigen to narrow antibody selectivity. This is a powerful method to increase specificity without developing new antibodies [7]. |
| Blocking Buffers (e.g., ChonBlock) | Specialized buffers designed to prevent non-specific binding interactions, thereby reducing background signal and false positives in assays like ELISA [39]. |
Experimental Protocol: Modifying Assay Conditions to Reduce Cross-Reactivity
This protocol is based on research demonstrating that cross-reactivity is not an immutable property of an antibody but can be modulated by the assay format and conditions [7].
Objective: To lower the cross-reactivity of an existing immunoassay by optimizing reagent concentrations and reaction times.
Principle: Immunoassays implemented with sensitive detection and low concentrations of reagents are characterized by lower cross-reactivities and higher specificity. Favoring kinetic over equilibrium conditions can further reduce low-affinity, cross-reactive binding [7].
Materials:
- Your current antibody and cross-reactive antigen.
- Components for your immunoassay (e.g., buffers, plates, detection system).
- Microplate reader or other appropriate detector.
Method:
- Titrate Reagent Concentrations: Set up your standard competitive immunoassay but with a significant (e.g., 5-10 fold) reduction in the concentration of both the antibody and the competing antigen (e.g., enzyme-conjugated hapten).
- Compare Cross-Reactivity: Run standard curves for both your target analyte and the main cross-reactant under the new (low-concentration) and old (standard-concentration) conditions.
- Calculate Cross-Reactivity (CR): For both conditions, calculate the CR using the formula:
CR (%) = [IC₅₀ (Target Analyte) / IC₅₀ (Cross-Reactant)] × 100%where IC₅₀ is the concentration causing 50% inhibition of the maximum signal [7]. - Shorten Incubation Times (Kinetic Mode): To shift the assay from equilibrium to kinetic mode, substantially reduce the incubation times for the antigen-antibody reaction. This favors the formation of high-affinity specific complexes over slower, low-affinity cross-reactive binding.
- Repeat Comparison: Measure the IC₅₀ values for the target and cross-reactant under these shortened incubation times and re-calculate the CR.
Expected Outcome: The low-concentration and kinetic-mode assays should show a lower cross-reactivity percentage (i.e., better differentiation between the target and cross-reactant) compared to the standard assay format, resulting in a more specific immunoassay [7].
Decision Workflow for Antibody Selection
The following diagram visualizes the key questions to guide your initial choice between monoclonal and polyclonal antibodies.
Immunoassays are powerful tools for quantifying molecules of biological interest, leveraging the specific binding between an antibody and its target analyte. The choice of assay format is a critical decision that directly impacts key performance parameters, including sensitivity, specificity, and perhaps most importantly for many applications, cross-reactivity. Cross-reactivity occurs when an antibody binds to structurally similar molecules other than the intended target, potentially leading to false positives or overestimation of analyte concentration [6]. This technical guide explores the fundamental differences between the two primary immunoassay formats—competitive and sandwich—within the context of troubleshooting cross-reactivity, providing researchers with clear protocols and decision-making frameworks.
FAQ: Core Concepts and Selection
What is the fundamental difference between a competitive and a sandwich immunoassay?
The fundamental difference lies in the assay design and the type of analyte each is best suited to detect.
- Sandwich Immunoassays are non-competitive and require that the analyte has multiple, distinct epitopes (antigenic sites). Two antibodies—a capture antibody and a detection antibody—bind to different parts of the same analyte molecule, effectively "sandwiching" it. The measured signal is directly proportional to the amount of analyte present. This format is almost exclusively used for large molecules, such as proteins [40].
- Competitive Immunoassays are used for small molecules (haptens) that typically possess only a single epitope. The labeled analyte (or analog) and the unlabeled analyte from the sample compete for a limited number of antibody-binding sites. The measured signal is inversely proportional to the amount of analyte in the sample [40].
When should I choose a competitive format over a sandwich format, and vice versa?
Your choice is primarily dictated by the size of your analyte.
- Choose a Sandwich Immunoassay if: Your target analyte is a large protein (typically >5 kDa) with at least two distinct antibody-binding sites. This format generally offers higher specificity, greater sensitivity, and a broader dynamic range [40].
- Choose a Competitive Immunoassay if: Your target analyte is a small molecule (hapten), such as a hormone, drug, or toxin, which is too small to be bound by two antibodies simultaneously. This is the standard format for quantifying small-molecule drugs, like sulfonamides and fluoroquinolones [7] [40].
How does the assay format influence cross-reactivity?
Cross-reactivity is an antibody-dependent phenomenon, but the assay format and its conditions can significantly modulate its impact.
- In Sandwich Immunoassays: The requirement for two distinct antibodies to bind simultaneously to the same molecule inherently increases specificity and can reduce cross-reactivity. A cross-reacting molecule must have epitopes for both the capture and detection antibodies to generate a signal [40].
- In Competitive Immunoassays: Cross-reactivity is a more common challenge. A molecule with a similar structure to the target analyte may bind to the antibody's single binding site. The degree of cross-reactivity can be influenced by assay conditions. Research shows that using lower concentrations of antibodies and competing antigens can make a competitive assay more specific by reducing cross-reactivities by up to five-fold [7].
Can I change the cross-reactivity of an assay without developing new antibodies?
Yes, cross-reactivity is not an immutable property of the antibody itself. For competitive immunoassays, you can modulate selectivity by adjusting experimental conditions [7]:
- Reagent Concentration: Shifting to lower concentrations of antibodies and labeled antigens can decrease cross-reactivity, making the assay more specific.
- Incubation Time: Varying the reaction time can shift the assay from a kinetic to an equilibrium mode, which can alter the measured cross-reactivity profile.
- Heterologous Assay Formats: Using a labeled antigen analog that is structurally different from the one used for immunization can narrow the spectrum of selectivity by making the assay dependent on only a subset of the antibodies produced [7].
Troubleshooting Guide: Cross-Reactivity
Problem: Suspected cross-reactivity causing false positive results.
Potential Cause 1: The sample contains a structurally similar compound (e.g., a metabolite, a related protein, or a common drug) that is cross-reacting with the antibody.
- Solution:
- Confirm with an Orthogonal Method: Always follow up a positive immunoassay screen with a confirmatory test using a more specific technique, such as LC-MS/MS or GC-MS [20].
- Test for Known Cross-reactants: Spike the sample with suspected cross-reactants (e.g., pseudoephedrine in an amphetamine assay) and observe the signal change [20].
- Perform Dilutional Linearity: If the sample is serially diluted and the measured analyte concentration does not dilute proportionally, it may indicate interference from a cross-reactant with a different affinity [6].
Potential Cause 2: The assay format or conditions are amplifying the inherent cross-reactivity of the antibody.
- Solution:
- Optimize Reagent Concentrations: For competitive assays, titrate down the concentrations of the antibody and labeled antigen. Assays with sensitive detection and low reagent concentrations are often more specific [7].
- Shorten Incubation Time: Reducing the contact time between reagents and the sample can favor high-affinity, specific interactions over lower-affinity, cross-reactive binding [6].
- Explore a Heterologous Format: If possible, test a different labeled antigen (heterologous assay) to potentially improve specificity [7].
Problem: High background noise reducing assay specificity.
Potential Cause: Non-specific binding of antibodies or other proteins to the solid phase or to matrix components.
- Solution:
- Optimize Blocking: Ensure that all non-specific binding sites on the solid phase (e.g., the microplate) are effectively blocked. Test different blocking buffers (e.g., 1% BSA, 10% host serum, or commercial protein-free blockers) [41].
- Increase Stringency of Washes: Add a mild detergent (e.g., 0.05% Tween-20) to the wash buffer and increase the number or volume of wash steps [41].
- Use a Monoclonal Antibody: For the capture antibody in a sandwich assay, a monoclonal antibody can provide higher specificity and lower background than a polyclonal mixture [6].
Experimental Protocols & Data Analysis
Protocol 1: Establishing a Competitive ELISA
This protocol is adapted for the detection of a small molecule analyte, such as an antibiotic or drug [7] [41].
1. Reagent Preparation:
- Coating: Dilute an antigen conjugate (e.g., a drug-protein conjugate) in a carbonate-bicarbonate coating buffer (50 mM, pH 9.6).
- Blocking: Prepare a blocking buffer (e.g., 1% BSA in PBS or Tris-buffered saline).
- Antibody & Analyte: Prepare dilutions of the primary antibody and the standard analyte in an appropriate matrix diluent.
2. Plate Coating & Blocking:
- Add the antigen conjugate to a high-binding microplate (e.g., 100 µL/well).
- Incubate overnight at 4°C or for 1-2 hours at 37°C.
- Wash the plate 3 times with a wash buffer (e.g., PBS with 0.05% Tween-20).
- Add blocking buffer (200-300 µL/well) and incubate for 1-2 hours at room temperature.
- Wash the plate 3 times.
3. Competitive Reaction:
- Add a fixed concentration of the primary antibody to all wells.
- Simultaneously add the standard (calibrator) or sample to the wells. The antibody, labeled antigen (on the plate), and unlabeled analyte (from the sample) will compete during incubation.
- Incubate for a defined period (e.g., 1 hour at 37°C).
- Wash the plate 3-5 times to remove unbound antibody.
4. Detection:
- Add an enzyme-conjugated secondary antibody (if using an unconjugated primary) or a streptavidin-enzyme conjugate (if using a biotinylated primary). Incubate and wash.
- Add the enzyme substrate (e.g., TMB for HRP) and incubate in the dark for a set time.
- Stop the reaction with an acid (e.g., 2M H₂SO₄ for TMB).
5. Data Analysis:
- Read the absorbance (450 nm for TMB).
- Plot the mean absorbance (or B/B₀, where B is the bound signal and B₀ is the maximum binding signal) against the log of the analyte concentration.
- Fit a 4- or 5-parameter logistic (4PL/5PL) curve to the data.
- Calculate the IC₅₀ (the concentration of analyte that inhibits 50% of the maximum signal). Cross-reactivity (CR) for a similar compound is calculated as: CR (%) = [IC₅₀ (Target Analyte) / IC₅₀ (Cross-reactant)] × 100% [7].
Protocol 2: Key Experiment to Modulate Cross-Reactivity
This experiment demonstrates how reagent concentration in a competitive immunoassay can be used to tune specificity [7].
Objective: To determine the effect of antibody and labeled antigen concentration on the observed cross-reactivity profile.
Methodology:
- Set up two versions of the same competitive immunoassay (e.g., for sulfonamides):
- Format A (High Stringency): Use a low, pre-optimized concentration of antibody and labeled antigen.
- Format B (Low Stringency): Use a higher concentration of the same reagents.
- For both formats, run a standard curve for the primary target analyte and for at least one key cross-reactant.
- Generate the dose-response curves and calculate the IC₅₀ for each compound in both formats.
- Calculate the cross-reactivity (%) for the cross-reactant in both Format A and Format B.
Expected Outcome: The data will typically show that Format A (low reagent concentration) yields a lower cross-reactivity percentage than Format B, demonstrating enhanced specificity under these conditions [7].
Table 1: Example Data from a Cross-Reactivity Modulation Experiment
| Assay Format | Reagent Concentration | IC₅₀ (Target) (ng/mL) | IC₅₀ (Cross-reactant) (ng/mL) | Cross-reactivity (%) |
|---|---|---|---|---|
| Format A | Low | 1.0 | 25.0 | 4.0% |
| Format B | High | 5.0 | 25.0 | 20.0% |
Visual Workflows and Diagrams
Competitive vs. Sandwich Immunoassay Workflow
Troubleshooting Cross-Reactivity in Competitive Immunoassays
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Reagents for Immunoassay Development
| Item | Function & Description | Example Use Cases & Considerations |
|---|---|---|
| Solid Phase | Surface to which the capture molecule (antigen or antibody) is immobilized. | Microplates: Greiner, Costar, Nunc high-binding plates. Choice affects background and binding capacity [41]. |
| Coating Buffers | Provide optimal pH and ionic conditions for adsorbing proteins to the solid phase. | 50 mM Sodium Bicarbonate, pH 9.6 is common. PBS (pH 7.4) can also be used [41]. |
| Blocking Buffers | Proteins or other agents used to saturate remaining binding sites on the solid phase to reduce non-specific binding. | 1% BSA, 10% host serum, or commercial casein buffers. Critical for lowering background noise [41]. |
| Wash Buffers | Solutions with detergents used to remove unbound reagents and matrix components between assay steps. | PBS or Tris with 0.05% Tween-20 (PBST/TBST). Ensures specificity of the final signal [41]. |
| Detection Enzymes | Enzymes conjugated to antibodies or antigens that generate a measurable signal. | Horseradish Peroxidase (HRP) & Alkaline Phosphatase (AP). HRP with TMB substrate is a common colorimetric system [41]. |
| Antibody Pairs | Matched set of capture and detection antibodies that bind to different epitopes on the same analyte. | Critical for Sandwich ELISA. Must be validated for pairing to ensure they do not sterically hinder each other [41] [40]. |
Troubleshooting Guides & FAQs
FAQ 1: What is cross-reactivity in multiplexed sensor arrays, and why is it considered advantageous?
Traditionally, antibody cross-reactivity is viewed as a problem that reduces assay specificity. However, in pattern-recognition-based sensor arrays, cross-reactivity is an advantageous feature. These arrays use multiple, deliberately cross-reactive sensor elements. When exposed to an analyte, each element produces a weak, variable signal. The collective response from all elements generates a unique fingerprint or pattern for that specific analyte. This pattern can then be deconvoluted using computational tools to identify and quantify the target, even in complex mixtures. This approach moves beyond the traditional "lock-and-key" model to a powerful "cross-reactive array + pattern recognition" paradigm [42] [43].
FAQ 2: My multiplex assay shows high background signals. How can I troubleshoot cross-reactivity between reagents?
High background signals often stem from direct non-specific binding between assay reagents, a common challenge in multiplexed immunoassays [44]. To troubleshoot, you need to systematically identify the source of the cross-reactivity. The following table outlines the primary types and their characteristics [4]:
| Type of Cross-Reactivity | Description | Troubleshooting Action |
|---|---|---|
| Detection-Capture Antibody | A detection antibody binds directly to a capture antibody meant for a different target. | Optimize reagent concentrations and assay diluent; use different antibody pairs [4]. |
| Antigen-Capture Antibody | A capture antibody binds the wrong antigen. | The assays cannot be multiplexed under these conditions; screen for different capture antibodies or new assay conditions [4]. |
| Capture Antibody-Conjugate | The label (e.g., streptavidin-HRP) binds directly to a capture antibody. | Check for biotin contamination in antibody stocks; this is rare but must be resolved for assay validation [4]. |
A key experimental method for diagnosing these issues is a cross-reactivity grid test, where individual antigens and detection antibodies are run in various combinations on the array. Signals in wells with mismatched pairs indicate the specific type of cross-reactivity occurring [4]. Furthermore, using a platform that allows sequential addition of detection antibodies can help isolate and circumvent cross-reactivity problems [45].
FAQ 3: What machine learning models are best for analyzing data from cross-reactive sensor arrays?
The high-dimensional data from cross-reactive sensor arrays requires machine learning (ML) models with strong pattern recognition capabilities. The choice of model depends on your dataset size and the complexity of the classification task. The table below summarizes widely applied models [43]:
| Machine Learning Model | Typical Use Case in Sensor Arrays |
|---|---|
| Linear Discriminant Analysis (LDA) | A common, robust classifier for distinguishing between multiple bacterial species or analyte classes [43]. |
| Support Vector Machine (SVM) | Effective for high-dimensional data and finding complex separation boundaries between classes [43]. |
| k-Nearest Neighbors (k-NN) | A simple, effective algorithm for classification based on similarity in the feature space [43]. |
| Principal Component Analysis (PCA) | Primarily used for unsupervised exploration and visualization of data to identify natural clusters [43]. |
| Convolutional Neural Networks (CNN) | Can be applied to analyze complex fingerprint-like data, such as spectral patterns from SERS or FTIR [43]. |
FAQ 4: How can I improve the signal-to-noise ratio and sensitivity of my electrochemical immunosensor?
Employing nanomaterial-based signal amplification is a highly effective strategy. For instance:
- Graphene Oxide Composites: Fabricating a composite of Fe₃O₄ nanoparticles loaded onto graphene oxide (Fe₃O₄@GO) can serve as a paramagnetic carrier for antibodies. This allows for efficient capture and concentration of analytes onto an electrode surface, achieving ultra-sensitive detection. This approach has demonstrated detection of prostate cancer biomarkers PSA and PSMA at fg/mL levels, which is 1000-fold better than many commercial assays [46].
- Nanoparticle Labels: Using metal nanoparticle labels (nanotags) such as PbAu@γFe₂O₃, CuAu@γFe₂O₃, and ZnAu@γFe₂O₃ enables highly sensitive multiplexed detection. Each metal core produces a distinct voltammetric signal, allowing for the simultaneous measurement of multiple targets [46].
Key Experimental Protocols
Protocol: Cross-Reactivity Testing for a Multiplexed Immunoassay
This protocol is adapted from established methods for validating multiplex assays and is critical for troubleshooting reagent interactions [4].
1. Objective: To identify and quantify specific cross-reactivities between all capture antibodies, detection antibodies, and antigens within a planned multiplex panel.
2. Materials:
- Array Platform: A planar or bead-based array with spotted capture antibodies.
- Reagents: Individual purified antigens and individual detection antibodies for all targets in the panel.
- Buffers: Appropriate assay buffer (e.g., 1% BSA in PBS) and wash buffer (e.g., 0.1% BSA-PBS with 0.05% Tween 20) [45].
- Detection System: Required labels (e.g., streptavidin-HRP, fluorescent conjugates) and substrates.
3. Experimental Setup and Method:
- Layout: Design a grid experiment where each column receives a single antigen and each row receives a single detection antibody. Include negative control wells (buffer only) for both antigens and detection antibodies.
- Procedure:
- Run the assay under standard conditions.
- Add antigens and detection antibodies according to the grid layout in duplicate.
- Perform all incubation and wash steps as defined for your platform.
- Develop the signal and read the array.
4. Data Analysis:
- Calculate the concentration for every possible antigen-detection pair.
- Determine the percent cross-reactivity using the formula:
% Cross-Reactivity = (Calculated concentration of antigen with non-matched detection antibody) / (Calculated concentration of antigen with its intended detection antibody) × 100 [4]
- Interpretation: Generally, cross-reactivity greater than 1% is considered significant and may require reagent re-optimization or replacement [4].
Protocol: Building a Machine Learning-Supported Sensor Array for Bacterial Identification
This protocol outlines the general workflow for creating a cross-reactive sensor array that uses pattern recognition for multiplexed detection, such as identifying foodborne pathogens [43].
1. Objective: To differentiate between multiple bacterial species by creating a unique fingerprint based on interactions with a cross-reactive sensor array and classifying it with machine learning.
2. Sensor Array Design Mechanisms:
- Cell Envelop Interactions: Build sensor elements that interact with general features of the bacterial surface, such as:
- Hydrophobicity: Use sensors with varying hydrophobicities.
- Surface Charge: Employ cationic materials (e.g., gold nanoparticles, quantum dots) that interact differently with Gram-positive and Gram-negative cell walls [43].
- Metabolic Profiling: Detect volatile organic compounds (VOCs) or other metabolites produced by bacterial metabolism using an electronic nose (e-nose) approach [43].
3. Method:
- Sensor Fabrication: Select and immobilize your suite of cross-reactive sensing materials (e.g., nanoparticles, fluorescent probes) in a multi-well format or on a solid support.
- Sample Exposure: Incubate the array with purified bacterial cells or a suspension of the sample of interest.
- Signal Acquisition: Measure the signal from each sensor element (e.g., fluorescence, colorimetric change, electrochemical signal) to generate a multi-dimensional data vector (the "fingerprint") for each sample.
4. Machine Learning Workflow:
- Data Preprocessing: Normalize the data and perform feature extraction if needed.
- Model Training: Use a dataset with known bacterial identities to train a classifier (e.g., LDA, SVM).
- Validation: Validate the model's accuracy using a separate, blinded test set of samples.
The following diagram illustrates the core logical workflow and relationship between cross-reactivity and pattern recognition in such a system.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and their functions for developing and troubleshooting multiplexed assays based on pattern recognition [44] [46] [45].
| Item | Function in the Context of Cross-Reactive Arrays |
|---|---|
| Cross-Reactive Antibodies | Affinity reagents that bind multiple related analytes; used to generate diverse signal patterns for pattern recognition rather than single-target specificity [42]. |
| Alternative Capture Ligands (Aptamers) | Nucleic acid-based binders that can be engineered for specific or broad target recognition; offer an alternative to antibodies with potential for better stability and batch-to-batch consistency [44]. |
| Nanomaterial Composites (e.g., Fe3O4@GO) | Used in electrochemical sensors for signal amplification; enhances sensitivity by efficiently capturing analytes and facilitating electron transfer on the electrode surface [46]. |
| Magnetic Nanotags (MNTs) | Magnetic nanoparticle labels used in platforms like MagArray; allow for real-time, wash-free detection and are insensitive to optical interference from complex sample matrices like whole blood [45]. |
| Multiplexed Array Platform (Planar or Bead-Based) | The physical solid support (e.g., GMR sensor chip, fluorescent microspheres) on which capture ligands are immobilized to create the parallel assay system [44] [45]. |
| Machine Learning Software (e.g., Python/R with scikit-learn) | Essential for developing pattern recognition classifiers (LDA, SVM, CNN) to interpret the high-dimensional data from cross-reactive sensor arrays [43]. |
FAQs: Strategic Cross-Reactivity for NPS Detection
FAQ 1: How can a routine immunoassay help me detect NPS that are not included in its original design? Immunoassays can detect structurally similar NPS due to antibody cross-reactivity. Even if your targeted confirmation method (like mass spectrometry) does not initially include a specific NPS, a positive immunoassay screen alongside a negative confirmation can signal the presence of an unanticipated cross-reacting substance. By analyzing this discrepancy and investigating local drug seizure reports for emerging NPS, you can identify which compounds to add to your confirmation panel. One laboratory exploited this by adding NPS benzodiazepines like bromazolam to their MS panel, increasing the agreement between their screen and confirmation results from 0% to 95.8% [47].
FAQ 2: Is cross-reactivity a fixed property of an antibody reagent? No, cross-reactivity is not an intrinsic, fixed property. It can be modulated by the assay's design and running conditions [7]. The same antibody can exhibit different cross-reactivity profiles in different assay formats (e.g., ELISA vs. FPIA). Furthermore, parameters such as the concentration of antibodies and reagents, reaction times, and whether the assay is run under kinetic or equilibrium conditions can significantly impact selectivity. Shifting to lower reagent concentrations has been shown to decrease cross-reactivity, making an assay more specific [7].
FAQ 3: What is a systematic, data-driven approach to discovering unknown cross-reactivities? Traditional methods relying on sporadic case reports are inefficient. A modern approach involves analyzing large-scale Electronic Health Record (EHR) data [19]. This method statistically links documented patient medication exposures to unexpected immunoassay results (false positives). By calculating odds ratios, researchers can identify which drugs are strongly associated with false-positive screens on specific assays. These data-driven hypotheses can then be validated experimentally, leading to the discovery of previously unknown cross-reactivities [19].
FAQ 4: Why do different immunoassays for the same drug class show inconsistent cross-reactivity data? There is a lack of standardization in how manufacturers test and report cross-reactivity data in package inserts. Studies have found wide variability in the number of compounds tested, the units of concentration used, and the availability of this data online. This inconsistency is compounded by sparse testing for "off-target" drugs and designer drugs, making it challenging for laboratories to consistently interpret results [48].
Troubleshooting Guides
Guide 1: Troubleshooting Immunoassay and Mass Spectrometry Discrepancies
A significant discrepancy between a positive immunoassay screen and a negative mass spectrometry confirmation is a common issue that can reveal the presence of NPS.
| Observation | Possible Cause | Investigation & Resolution |
|---|---|---|
| Persistent positive immunoassay results with negative targeted MS confirmation | Presence of NPS not included in the targeted MS panel [47]. | Investigation: Review regional drug seizure reports and forensic data for emerging NPS. Analyze discrepancy rates to confirm they exceed typical false-positive levels.Resolution: Retrospectively re-test stored samples after expanding the MS confirmation panel to include identified NPS (e.g., bromazolam, flualprazolam) [47]. |
| Isolated false-positive result on a single sample | Cross-reactivity from a structurally similar legitimate medication (e.g., pseudoephedrine causing a positive amphetamine screen) [49]. | Investigation: Review the patient's medication list. Check manufacturer's package insert for known cross-reactivities.Resolution: Always confirm presumptively positive immunoassay results with a more specific technique like LC-MS/MS [19] [50]. |
| Unexpectedly high cross-reactivity in a newly developed assay | Suboptimal assay conditions, such as high concentrations of antibodies or detection reagents [7]. | Investigation: Perform a checkerboard titration of antibodies and reagents.Resolution: Shift to lower reagent concentrations and shorter incubation times to favor high-affinity specific binding over lower-affinity cross-reactions [7]. |
Guide 2: Addressing Common Immunoassay Interferences
Interference can lead to both false-positive and false-negative results, complicating data interpretation.
| Interference Type | Effect on Assay | Mitigation Strategies |
|---|---|---|
| Structural Analogues & Metabolites [12] | False positives due to antibody cross-reactivity. | Use monoclonal antibodies for higher specificity [6]. Confirm all positive results with LC-MS/MS [50]. |
| Matrix Effects [6] | Altered antibody binding due to sample components (lipids, proteins). | Dilute the sample (may reduce sensitivity). Use platforms that minimize contact time between sample matrix and reagents [6]. |
| Heterophile Antibodies [12] | False positives or negatives due to human antibodies interacting with assay antibodies. | Use blocking agents in the assay buffer. Re-test after treating samples with heterophile blocking tubes. |
Experimental Protocols for Cross-Reactivity Assessment
Protocol 1: Systematic Cross-Reactivity Discovery Using EHR Data
This protocol, adapted from a published study, uses real-world data to generate hypotheses about potential cross-reactants [19].
1. Data Extraction:
- Gather a large dataset of immunoassay results linked to confirmatory testing results.
- Extract all documented drug exposures (from medication lists, administrations, etc.) for each patient in the 1-30 days preceding the test.
2. Statistical Analysis:
- For each assay-ingredient pair, use Firth's logistic regression to model the relationship between drug exposure and a false-positive immunoassay result.
- Calculate an Odds Ratio (OR). An OR > 1 indicates that exposure to the ingredient increases the odds of a false-positive screen.
- Prioritize assay-ingredient pairs with the highest ORs and statistically significant confidence intervals for experimental validation.
3. Experimental Validation:
- Spike the suspected cross-reactive compound (or its metabolites) into drug-free urine or blood matrix at therapeutic concentrations.
- Run the spiked samples on the immunoassay in question.
- A positive result on the spiked sample confirms the hypothesized cross-reactivity.
Protocol 2: Modulating Cross-Reactivity via Assay Condition Optimization
This protocol outlines how to experimentally reduce unwanted cross-reactivity by optimizing reagent concentrations, based on principles described in research [7].
1. Prepare Reagents:
- Obtain the target analyte and the primary cross-reactant.
- Prepare a series of dilutions for both compounds in the appropriate matrix.
2. Titrate Assay Components:
- Set up a checkerboard titration. For a competitive ELISA, this would involve varying the concentration of the capture antibody and the competing antigen (enzyme-conjugated hapten) across the plate.
- For each condition, run standard curves for both the target analyte and the cross-reactant.
3. Calculate Cross-Reactivity:
- For each assay condition, determine the IC50 (the concentration that causes a 50% inhibition of the signal) for both the target and the cross-reactant.
- Calculate cross-reactivity (CR) as: CR (%) = (IC50 of target / IC50 of cross-reactant) × 100.
- Identify the assay conditions (antibody/antigen concentrations) that yield the lowest CR percentage, indicating highest specificity.
Data Presentation: Quantitative Cross-Reactivity Insights
Table 1: Impact of Expanding MS Confirmation Panels on NPS Detection
Data from a laboratory study on NPS benzodiazepines demonstrates the critical need for updated confirmation methods [47].
| Confirmation Panel | Immunoassay & MS Agreement | Key Action Taken |
|---|---|---|
| Limited to traditional benzodiazepines | 0% | Baseline - High discrepancy observed. |
| Expanded to include bromazolam, flualprazolam, flubromazolam, flubromazepam | 95.8% | Added 4 prevalent NPS benzodiazepines and their metabolites to the targeted MS panel. |
Table 2: Structural Analogues Causing False-Positive Amphetamine Immunoassays
A summary of common interferents, highlighting the challenge of structural similarity [49].
| Compound | Common Use | Potential for False-Positive Amphetamine Screen |
|---|---|---|
| Pseudoephedrine | Decongestant | High (75% false-positive rate reported with one specific assay) [49]. |
| Bupropion | Antidepressant/Smoking Cessation | High (primarily due to its metabolite, threohydrobupropion). |
| DMAA (1,3-dimethylamylamine) | Dietary Supplement | High. |
| Selegiline | Anti-Parkinson's drug | High (metabolized to l-methamphetamine and l-amphetamine). |
Workflow Visualization
Diagram: NPS Discovery via Discrepancy Analysis
Diagram: Modulating Cross-Reactivity in Assay Development
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents and Materials for Cross-Reactivity Research
| Item | Function in Research | Application Example |
|---|---|---|
| Monoclonal Antibodies (mAb) | Provide high specificity by recognizing a single epitope; ideal for establishing assay specificity as a capture antibody [6]. | Used in developing a highly selective assay for a specific NPS, minimizing detection of analogues. |
| Polyclonal Antibodies (pAb) | A mixture of antibodies that recognize multiple epitopes; can provide higher sensitivity but may increase cross-reactivity risk [6]. | Used as a detection reagent in a class-specific assay to broadly detect multiple NPS within a family. |
| LC-MS/MS System | The gold-standard confirmatory method; provides high specificity and sensitivity to definitively identify and quantify individual analytes [50]. | Used to validate immunoassay results and expand testing panels to include newly identified NPS [47]. |
| Spiked Drug-Free Matrix | A control sample created by adding a known concentration of a pure analyte to a biological matrix (e.g., urine, blood); essential for experimental validation of cross-reactivity [19]. | Used to test if a suspected medication causes a positive result on a specific immunoassay. |
| Heterologous Assay Formats | Using a different antigen derivative in the assay than was used for immunization; can narrow the spectrum of selectivity and reduce cross-reactivity [7]. | A strategy to make an assay more specific without the need to generate entirely new antibodies. |
Practical Troubleshooting and Optimization Techniques to Minimize Interference
In immunoassay research, effective sample pre-treatment is a critical frontline defense against cross-reactivity, a common obstacle that can compromise data integrity. The processes of sample dilution, analyte depletion, and the use of blocking agents are not merely preparatory steps but are fundamental to ensuring assay specificity and sensitivity. This guide provides targeted troubleshooting advice and detailed protocols to help you optimize these pre-treatment steps, minimizing non-specific interactions and improving the reliability of your experimental results.
► FAQs: Optimizing Pre-Treatment to Minimize Cross-Reactivity
1. How does sample dilution influence cross-reactivity and how can I optimize it?
Sample dilution is a primary strategy for reducing matrix effects and minimizing cross-reactivity caused by interfering substances. Over-dilution can lead to a loss of signal, while under-dilution can increase background noise and non-specific binding [51]. The optimal dilution factor must be determined empirically for each sample type.
- Experimental Protocol for Dilution Optimization:
- Prepare a series of sample dilutions (e.g., 1:2, 1:5, 1:10, 1:50, 1:100) using the appropriate assay buffer.
- Run the diluted samples in your immunoassay alongside a known standard curve.
- Plot the measured concentration (or signal) against the dilution factor. The optimal range is where the results fall within the linear portion of the standard curve and the signal is sufficiently above the background.
- Select the dilution factor that provides a strong, specific signal with minimal background. For samples with very high analyte concentrations, such as certain cytokines or hormones, a higher starting dilution may be necessary [51].
2. What is the role of blocking agents, and which one should I choose?
Blocking agents are proteins or other molecules used to coat unused binding sites on solid surfaces (like microplates or membranes) and in sample matrices. This prevents non-specific adsorption of your detection antibodies, thereby reducing background signal and cross-reactivity [52] [53].
- Common Blocking Agents and Their Applications:
- BSA (1%) or Casein (0.1-0.5%): Effective for many standard immunoassays. BSA is widely used, while casein (from milk) can offer superior blocking for some applications.
- Serum: Normal serum from the host species of the secondary antibody can be highly effective, as it contains a mix of proteins that saturate non-specific sites.
- Experimental Protocol for Blocking: Incubate your coated plate or membrane with the blocking buffer for 1-2 hours at room temperature or overnight at 4°C. After blocking, wash the surface thoroughly with a wash buffer (e.g., PBS with 0.05% Tween-20) before adding your sample or antibodies [52].
3. When should I consider using depletion methods, and what are the options?
Depletion is used when a sample contains high-abundance, non-target proteins that cause significant cross-reactivity or mask the signal of a low-abundance target. This is common in complex matrices like serum or plasma.
- Common Depletion Methods:
- Immunodepletion: Uses antibodies immobilized on beads or columns to specifically remove the most abundant interfering proteins (e.g., albumin, IgG).
- Protein A/G/L Columns: Effectively deplete immunoglobulins from samples.
- Protocol Consideration: While powerful, depletion can sometimes co-remove your target of interest if it binds to the depleted proteins. A pilot experiment should be conducted to confirm that your target's recovery is acceptable after the depletion process.
4. How do I troubleshoot high background caused by the sample itself?
High background often stems from inadequate blocking, insufficient washing, or non-optimal sample dilution [51] [54].
- Troubleshooting Steps:
- Increase Blocking Time/Concentration: Ensure your blocking step is sufficient. Try a higher concentration of blocking agent or a longer incubation time [52].
- Optimize Wash Stringency: Increase the number of wash cycles or the concentration of detergent (e.g., Tween-20) in your wash buffer to remove loosely bound proteins [51] [54].
- Re-optimize Sample Dilution: Re-visit your dilution scheme. A higher dilution factor may be needed to dilute out interfering substances [51].
- Include Controls: Always run appropriate negative controls (e.g., sample without primary antibody, isotype control) to distinguish specific signal from background [53].
► Troubleshooting Guide: Common Pre-Treatment Issues
The table below outlines common problems, their potential causes, and solutions related to sample pre-treatment.
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High background signal | Inadequate blocking; Insufficient washing; Sample dilution too low [51] [54]. | Increase blocking agent concentration or time; Increase wash cycles/stringency; Test higher sample dilutions [51] [52] [54]. |
| Weak or no signal | Sample dilution too high; Analyte loss during depletion; Antibody degraded [51] [54]. | Test lower dilution factors; Validate analyte recovery post-depletion; Use fresh, properly stored antibodies [51] [54]. |
| High variability between replicates | Inconsistent sample mixing; Inconsistent pipetting during dilution; Plate washing inconsistency [51]. | Vortex or mix samples thoroughly before use; Calibrate pipettes and use reverse pipetting; Ensure uniform and complete washing [51]. |
| Inaccurate sample quantification | Matrix effects not accounted for; Cross-reactivity with similar epitopes [55]. | Use a matrix-matched standard curve; Employ affinity-purified or monoclonal antibodies to improve specificity [56] [55]. |
► Experimental Protocols for Pre-Treatment Optimization
Protocol 1: Systematic Optimization of Blocking Conditions
This protocol helps identify the most effective blocking agent for your specific assay.
- Coat your plate with the capture antibody as per your standard protocol.
- Prepare different blocking buffers (e.g., 1% BSA in PBS, 0.5% Casein in PBS, 5% normal serum from the secondary antibody host species).
- Block different wells with each blocking buffer. Include a well with no blocking agent as a negative control.
- Incubate for 1 hour at room temperature.
- Wash the plate thoroughly.
- Add your sample and detection antibodies, and develop the assay.
- Analyze the results. The optimal blocking buffer delivers the highest specific signal with the lowest background.
Protocol 2: Checkboard Titration for Antibody and Sample Dilution
This protocol simultaneously determines the optimal concentration of your capture/detection antibodies and the sample dilution factor.
- Coat the plate with a range of capture antibody concentrations (e.g., 0.5, 1, 2, 5 µg/mL) in a checkerboard pattern.
- Block the plate uniformly.
- Add a range of sample dilutions (e.g., neat, 1:5, 1:25, 1:125) orthogonal to the antibody concentrations.
- Proceed with your standard detection steps, using a range of detection antibody concentrations if necessary.
- Identify the combination of capture antibody, detection antibody, and sample dilution that provides the best signal-to-noise ratio.
► Visualizing the Pre-Treatment Workflow
The following diagram illustrates a logical workflow for troubleshooting cross-reactivity through sample pre-treatment.
Sample Pre-Treatment Troubleshooting Workflow
► The Scientist's Toolkit: Key Reagent Solutions
The table below lists essential reagents used in sample pre-treatment to mitigate cross-reactivity.
| Research Reagent | Function in Pre-Treatment |
|---|---|
| BSA (Bovine Serum Albumin) | A common blocking agent used to coat non-specific binding sites on assay surfaces and in diluents [52]. |
| Tween-20 | A non-ionic detergent added to wash buffers to help remove non-specifically bound proteins and reduce background [52]. |
| Normal Serum | Serum from the host species of secondary antibodies, used as a blocking agent to minimize cross-reactivity with sample components [53]. |
| Casein | A milk-derived protein effective as a blocking agent, often used as an alternative to BSA [52]. |
| Immunodepletion Columns | Solid-phase columns with immobilized antibodies for removing specific high-abundance interfering proteins from samples. |
| Affinity-Purified Antibodies | Antibodies purified to bind a single epitope, significantly reducing the potential for off-target binding and cross-reactivity [56]. |
Frequently Asked Questions
1. What is the fundamental principle behind using reduced contact time to minimize cross-reactivity? Molecular interactions causing interference in immunoassays are a function of affinity, concentration, and exposure time. Reducing contact time favors the most specific, high-affinity interactions (like the primary antibody-antigen binding) because these form more rapidly. In contrast, many non-specific, low-affinity interactions require longer periods to occur. By minimizing the time reagents are in contact, you selectively promote the desired high-affinity binding while suppressing slower, cross-reactive binding events [6].
2. In which assay formats can this strategy be most effectively implemented? This strategy is particularly effective in flow-through immunoassay platforms. In these systems, the contact time between reagents, the sample, and its matrix is inherently minimized by design, allowing for precise control over incubation periods. It is more challenging to implement in traditional plate-based assays like ELISA, where long, static incubations are common, though careful protocol adjustments can still yield benefits [6].
3. Can adjusting contact time change the apparent cross-reactivity of my assay? Yes. Cross-reactivity is not an immutable property of the antibodies alone but is an integral parameter sensitive to assay conditions. Changing parameters like reagent concentrations and interaction times (shifting from equilibrium toward kinetic modes) can directly modulate the observed cross-reactivity. Using sensitive detection methods that allow for lower reagent concentrations and shorter times can make an assay more specific [7].
4. What are the potential trade-offs of reducing contact time? The primary trade-off is a potential reduction in assay sensitivity. Sufficient time is required for the capture of low-abundance analytes. If the contact time is too short, even the high-affinity target binding may not reach a level that produces a robust, detectable signal. Therefore, optimization is crucial to find the balance that minimizes interference while maintaining adequate sensitivity for your application [6].
5. How can I systematically optimize the contact time in my assay? Perform a time-course experiment. Run the assay identically but vary the incubation time of the sample with the capture antibody. Then, plot the signal-to-noise ratio against time. The optimal contact time is typically at the point where the signal-to-noise ratio is highest before non-specific binding begins to increase significantly [57].
Troubleshooting Guide
| Problem | Potential Cause | Solution |
|---|---|---|
| High background signal | Non-specific, low-affinity binding has reached equilibrium. | Step 1: Gradually shorten the primary incubation time in a series of experiments. Step 2: Increase the stringency of wash steps immediately following the shortened incubation [6] [57]. |
| Low target signal | Contact time is too short for sufficient high-affinity complexes to form. | Step 1: Increase the concentration of the detection antibody to accelerate binding. Step 2: If signal remains low, incrementally extend the contact time until an acceptable signal is achieved without a proportional increase in background [57]. |
| Poor assay precision | Inconsistent manual pipetting or timing during short incubations. | Step 1: Implement automated liquid handling systems for reagent addition. Step 2: Use a flow-through system where contact times are controlled and consistent by design [6]. |
| Inconsistent cross-reactivity reduction | Assay conditions are not fully optimized or controlled. | Step 1: Use a Design of Experiments (DOE) approach to simultaneously optimize contact time, temperature, and ionic strength. Step 2: Validate the optimized protocol by testing against known cross-reactants and ensure consistent results [6] [7]. |
Experimental Data and Protocols
Table 1: Impact of Assay Format and Reagent Concentration on Cross-Reactivity Data adapted from a study on immunoassays for sulfonamides and fluoroquinolones, demonstrating that cross-reactivity (CR) is not a fixed parameter [7].
| Assay Format | Reagent Concentration | Interaction Mode | Observed Cross-Reactivity |
|---|---|---|---|
| Fluorescence Polarization Immunoassay (FPIA) | High | Near-equilibrium | High CR (e.g., 5-fold higher) |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Low | Kinetic | Low CR (More specific) |
| Theoretical Model (Competitive Immunoassay) | Low | Kinetic | Lower CR, increased specificity |
| Theoretical Model (Competitive Immunoassay) | High | Equilibrium | Higher CR, broader detection |
Protocol 1: Optimizing Contact Time via a Time-Course Experiment
Objective: To determine the incubation time that maximizes the signal-to-noise ratio for a target analyte in the presence of a cross-reactant.
Materials:
- Target antigen and known cross-reactant
- Capture and detection antibodies
- Assay buffers and wash solutions
- Appropriate detection instrumentation (e.g., plate reader)
Method:
- Prepare Samples: Create a series of identical sample mixtures containing a fixed, low concentration of your target analyte and a known concentration of a cross-reactant.
- Vary Incubation Time: Add the capture antibody to each sample mixture, but initiate a stop timer at different intervals (e.g., 1, 5, 10, 30, 60 minutes).
- Stop Reaction: At each time point, immediately remove unbound components with a stringent wash step.
- Complete Assay: Continue with the remainder of your standard assay protocol (e.g., add detection antibody, substrate).
- Measure and Calculate: Record the signals for both the target and the cross-reactant at each time point. Calculate the signal-to-noise ratio or directly compare the signals to determine the time point where target signal is robust while cross-reactant signal is minimized [6] [57].
Protocol 2: Evaluating Optimization Success with Spike and Recovery
Objective: To confirm that reducing contact time has not adversely affected the accurate detection of the target analyte.
Materials:
- Neat (blank) sample matrix
- Assay buffer
- High-purity target analyte
Method:
- Prepare Samples:
- Neat Matrix: Sample matrix with no spike.
- Spiked Buffer (Control): Known concentration of analyte spiked into assay buffer.
- Spiked Matrix (Test): Same concentration of analyte spiked into the sample matrix.
- Run Assay: Analyze all samples in duplicate or triplicate using your optimized (shorter contact time) protocol.
- Calculate Recovery:
% Recovery = (Measured Concentration in Spiked Matrix / Measured Concentration in Spiked Buffer) × 100%
- Interpret Results:
- 80–120% Recovery: Acceptable, indicates minimal interference.
- <80% Recovery: Suggests signal suppression or that the contact time is too short.
- >120% Recovery: Suggests signal enhancement, often due to interference or cross-reactivity, indicating further optimization is needed [5].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Optimizing High-Affinity Binding Assays
| Item | Function in Optimization |
|---|---|
| Monoclonal Antibodies (mAb) | As primary capture antibodies, they provide high specificity by recognizing a single epitope, which is foundational for reducing cross-reactivity [6]. |
| High-Affinity Ligands | Using antibodies or antigens with high inherent affinity for the target allows for shorter binding times while maintaining a strong signal [57]. |
| Blocking Agents (e.g., BSA, Casein) | Reduce non-specific binding by saturating potential interfering sites on surfaces, which is especially important when shorter wash times are used [6] [5]. |
| Automated Liquid Handling Systems | Ensure precision and reproducibility during rapid pipetting and short incubation steps, minimizing human-driven variability [6]. |
| Reference Standards & Controls | Critical for monitoring assay performance and ensuring consistency during and after method optimization [57]. |
Conceptual and Workflow Diagrams
High-Affinity Binding Optimization Workflow
This flowchart outlines the iterative process for optimizing contact time to favor high-affinity binding and reduce cross-reactivity.
Binding Interaction Dynamics
This diagram contrasts the outcomes of long versus short contact times. A long incubation allows both high-affinity target binding and low-affinity cross-reactive binding to occur, leading to high background. A short, optimized contact time primarily permits the rapid high-affinity binding, effectively suppressing most cross-reactivity [6].
Troubleshooting Guides
FAQ: Addressing Common Reagent Concentration Challenges
1. How does reducing reagent concentration improve assay specificity? Reducing the concentration of detection antibodies minimizes non-specific binding, a major source of false-positive signals. Excess antibodies can bind to non-target sites, but optimal concentrations favor specific, high-affinity interactions between the antibody and its target antigen. Using excessively high detection antibody concentrations is a well-documented cause of increased non-specific binding and background signal [58] [59].
2. What is the risk of reducing reagent concentrations too much? The primary risk is reduced assay sensitivity. If reagent concentrations are too low, the signal from true positive target binding may become too weak to detect accurately, particularly for low-abundance analytes. The goal is to find the concentration that provides the optimal balance between sensitivity and specificity [58].
3. How can I systematically determine the optimal reagent concentration? The most effective method is to perform a checkerboard titration, where you test a range of capture and detection reagent concentrations against each other. This identifies the combination that yields the strongest specific signal with the lowest background noise. The Single-Molecule Colocalization Assay (SiMCA) provides a methodology to directly quantify non-specific binding at different concentrations [59].
4. Besides concentration, what other factors can I adjust to improve specificity?
- Stringent Washes: Increase wash stringency to remove weakly bound antibodies.
- Blocking Agents: Use effective blockers to saturate non-specific binding sites on the assay substrate.
- Incubation Time: Reduce contact times to favor specific, high-affinity binding events.
- Antibody Quality: Use high-quality, affinity-purified antibodies with high specificity for your target [6] [58] [5].
Experimental Protocol: Optimizing Detection Antibody Concentration
This protocol is adapted from a single-molecule colocalization study that quantified non-specific binding [59].
Objective: To determine the detection antibody concentration that maximizes the signal-to-noise ratio.
Materials:
- Coated assay plates or coverslips with captured target antigen
- Detection antibody (labeled with fluorophore or enzyme)
- Assay buffer and wash solutions
- Standard laboratory equipment for your detection method (e.g., plate reader, microscope)
Method:
- Prepare a dilution series of your detection antibody in assay buffer. A suggested starting range is 10 nM to 500 nM.
- Apply the different detection antibody concentrations to your assay plates/coverslips. Include a negative control (no target antigen).
- Incubate according to your standard assay conditions, followed by stringent washing.
- Develop the signal according to your detection method and measure the output (e.g., fluorescence, absorbance).
- Data Analysis:
- Calculate the specific signal (mean signal of samples with antigen).
- Calculate the background signal (mean signal of negative controls).
- Calculate the Signal-to-Noise Ratio (SNR) for each concentration: SNR = Specific Signal / Background Signal.
- Plot the specific signal and SNR against the detection antibody concentration.
Interpretation: The optimal concentration is typically at the point where the specific signal begins to plateau while the SNR is at its maximum. A high concentration that gives a strong specific signal but a low SNR indicates high background and poor specificity.
Table 1: Impact of Detection Antibody Concentration on Assay Performance
The following data, derived from a single-molecule colocalization assay (SiMCA), quantitatively shows how reducing detection antibody concentration drastically lowers non-specific background without significantly affecting true positive signals [59].
| Detection Antibody Concentration | Non-Specific dAb Counts (Molecules per FOV) | Colocalized (True Positive) Counts (Molecules per FOV) | Key Performance Insight |
|---|---|---|---|
| 50 nM | 0.4 ± 0.6 | 0 ± 0.0 (No antigen) | Minimal non-specific binding observed. |
| 500 nM | 92 ± 23 | 2 ± 1.3 (No antigen) | High non-specific binding dominates signal. |
Table 2: Effect of Signal Normalization on Assay Reproducibility
To account for surface heterogeneity, normalizing the detected signal to the amount of capture reagent can significantly improve reproducibility. The following data demonstrates this effect [59].
| TNF-α Concentration | CV of Absolute dAb Counts | CV of Normalized Colocalized Counts | Improvement in Reproducibility |
|---|---|---|---|
| 100 pM | High CV | 4.8-fold lower CV | Normalization dramatically reduces variance. |
| 300 pM | -- | -- | Effect less pronounced as true signal increases. |
Workflow and Strategy Visualization
Diagram: Reagent Optimization Workflow
This diagram outlines the key decision points and steps for optimizing reagent concentrations to enhance immunoassay specificity.
Diagram: Specificity vs. Sensitivity Balance
This diagram illustrates the conceptual relationship between reagent concentration and key assay performance metrics, highlighting the critical balance between specificity and sensitivity.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Optimizing Immunoassay Specificity
| Reagent Type | Function in Specificity Enhancement | Example Products / Components |
|---|---|---|
| Blocking Buffers | Saturate non-specific binding sites on the solid phase to reduce background. | BSA, Casein, Normal Serum, Commercial blockers (e.g., StabilGuard, StabilCoat) [58]. |
| Assay Diluents | Provide an optimal matrix for reagents and samples while blocking matrix interferences (e.g., from HAMA or Rheumatoid Factor). | Protein-containing (e.g., MatrixGuard) or protein-free (e.g., Surmodics Assay Diluent) formulations [58]. |
| High-Quality Antibodies | Ensure high affinity and specificity for the target analyte, minimizing cross-reactivity. | Affinity-purified monoclonal or polyclonal antibodies from reputable suppliers [58]. |
| Stringent Wash Buffers | Remove weakly and non-specifically bound reagents during assay steps. | PBS or Tris buffers with detergents (e.g., 0.05% Tween-20) [41]. |
FAQ: Understanding Matrix Effects and Platform Solutions
What are matrix effects and why are they a problem? Matrix effects refer to interference caused by extraneous components in a sample (such as proteins, lipids, salts, or other biomolecules) that disrupt the specific binding between an analyte and its detection antibody [5] [60]. This interference can lead to inaccurate results, including false positives/negatives, reduced assay sensitivity, and increased variability, which compromises the reliability of data in diagnostics and drug development [6] [60].
How do flow-through systems minimize matrix effects? Flow-through systems, such as those employing microfluidics, minimize matrix effects by significantly reducing the contact time between the sample matrix and the assay reagents [6]. This short exposure time favors the specific, high-affinity interactions between the antibody and antigen, while minimizing the opportunity for weaker, non-specific binding from interfering matrix components to occur [6].
What are the benefits of miniaturization in immunoassays? Miniaturizing immunoassays to the nanoliter scale offers two key benefits related to matrix effects:
- Reduced Reagent Consumption: It drastically cuts the consumption of precious samples and expensive reagents [6].
- Enhanced Specificity: Performing assays at lower concentrations of immunoreactants can decrease cross-reactivity, making the assay more specific for the primary analyte over structurally similar compounds [7].
What sample pre-treatment methods can be used with these platforms? Sample pre-treatment remains a highly effective strategy. Common methods include:
- Sample Dilution: Reduces the concentration of interfering substances [6] [60].
- Acid Dissociation: Using a panel of acids followed by neutralization can disrupt interfering complexes, such as soluble dimeric targets in anti-drug antibody (ADA) assays [61].
- Buffer Exchange: Removes interfering components by transferring the analyte into an assay-compatible buffer [60].
Experimental Protocols for Mitigating Interference
Protocol 1: Acid Dissociation for Target Interference in Bridging ADA Assays
This protocol is designed to overcome false positive signals caused by soluble dimeric targets [61].
Materials:
- Panel of acids (e.g., Hydrochloric Acid - HCl)
- Neutralization buffer
- Master Mix (biotin- and SULFO-TAG-labeled drug)
- Assay plates and reader
Procedure:
- Acid Treatment: Mix the sample matrix (e.g., plasma or serum) with a pre-optimized type and concentration of acid.
- Incubation: Incubate the acidified sample to allow for dissociation of the target complexes.
- Neutralization: Add a neutralization buffer to restore the sample to a pH compatible with the immunoassay. This step is critical to prevent denaturation of other assay components.
- Assay Execution: Proceed with the standard steps of your bridging immunoassay using the treated sample [61].
Troubleshooting Tip: If sensitivity loss is observed, optimize the type of acid, its concentration, and the duration of the acid treatment step [61].
Protocol 2: Sample Dilution and Buffer Exchange
A standard method to reduce the concentration of interferents [60].
Materials:
- Assay-compatible buffer (e.g., phosphate-buffered saline)
- Pre-calibrated buffer exchange columns
- Dilution tubes
Procedure:
- Dilution: Dilute the sample with an appropriate buffer. This simple step lowers the concentration of all sample components, which can diminish the impact of interferents.
- Buffer Exchange (Alternative): For more robust removal of interferents, use a buffer exchange column according to the manufacturer's instructions. This process physically separates the analyte from smaller or larger interfering substances in the sample matrix [60].
- Validation: Always perform a spike-and-recovery experiment to ensure that the dilution or buffer exchange does not adversely affect the accurate detection of the analyte [5].
Data Presentation: Quantitative Comparisons
Table 1: Impact of Reagent Concentration on Assay Cross-Reactivity [7]
| Immunoassay Format | Reagent Concentration | Cross-Reactivity (CR) Example | Key Factor |
|---|---|---|---|
| Standard Format | High concentrations of antibodies and antigens | Higher CR (e.g., 100% baseline) | Equilibrium conditions favor binding of lower-affinity analogs. |
| Miniaturized/Sensitive Format | Low concentrations of antibodies and markers | Up to 5-fold lower CR (e.g., 20% of baseline) | Kinetic mode favors highest-affinity binding partners. |
Table 2: Performance Comparison of Immunoassay Platforms with LC-MS/MS [62]
| Analytical Platform | Correlation with LC-MS/MS (Spearman's r) | Sample Preparation | Key Characteristic |
|---|---|---|---|
| LC-MS/MS (Reference) | 1.000 | Requires sophisticated preparation | Gold standard for specificity. |
| Mindray CL-1200i | 0.998 | Direct (no extraction) | Excellent correlation, simplified workflow. |
| Snibe MAGLUMI X8 | 0.967 | Direct (no extraction) | Good correlation, high throughput. |
| Roche e801 | 0.951 | Direct (no extraction) | Good correlation, competitive electrochemiluminescence. |
| Autobio A6200 | 0.950 | Direct (no extraction) | Good correlation, wide linear range. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Overcoming Immunoassay Challenges
| Reagent / Material | Function in Mitigating Interference |
|---|---|
| Human Anti-Animal Antibody (HAAA) Blockers | Blocks interfering human antibodies (e.g., HAMA) that bind to assay immunoglobulins, reducing false signals [5]. |
| BSA or Casein Blockers | Used as blocking agents to saturate nonspecific binding sites on surfaces and proteins, minimizing background noise [5]. |
| Acid Panel (e.g., HCl) | Used in sample pre-treatment to dissociate drug-target complexes or multimeric interferents that cause false positives [61]. |
| Matched Monoclonal Antibody Pairs | Improve assay specificity and reduce cross-reactivity by targeting a single, well-defined epitope on the analyte [5]. |
| PEG-based Conjugation Reagents (e.g., Biotin-PEG4-NHS) | Used for labeling drugs or antigens with minimal aggregation, ensuring high-quality reagents for sensitive detection in bridging assays [61]. |
| Diatomaceous Earth | Used in sample pre-treatment and clean-up procedures to adsorb interfering substances from complex matrices like food samples [63]. |
Workflow Comparison: Traditional vs. Flow-Through Systems
Addressing Prozone Effect and Bidirectional Interference in Sandwich Assays
This technical support center resource addresses the critical challenges of the prozone effect (high-dose hook effect) and bidirectional interference encountered during the development and execution of sandwich immunoassays. This guide is framed within the broader context of a thesis on troubleshooting cross-reactivity in immunoassay research, providing actionable protocols for researchers, scientists, and drug development professionals.
Fundamental Concepts: Mechanisms and Manifestations
What is the prozone effect and how does it occur in a sandwich assay?
The prozone effect, also known as the high-dose hook effect, is an analytical interference that can cause falsely low or negative results in one-step sandwich immunoassays when the analyte concentration is exceptionally high [13] [64]. In a typical sandwich assay, the analyte forms a "bridge" between a capture antibody and a detection antibody, generating a signal proportional to the analyte concentration. The prozone effect occurs when the analyte is present in such excess that it saturates both the capture and detection antibody binding sites independently. This prevents the formation of the necessary antibody-analyte-antibody "sandwich" complex, leading to a dramatic and misleading drop in the detected signal [64] [65].
Bidirectional interference refers to substances or conditions in a sample that can cause either a false increase (positive interference) or a false decrease (negative interference) in the reported analyte concentration [13]. Unlike the prozone effect, which is a specific type of negative interference, bidirectional interference encompasses a wider range of factors. The table below summarizes the most common sources of this interference.
| Interference Source | Type | Mechanism of Action | Typical Impact on Result |
|---|---|---|---|
| Heterophilic Antibodies [13] [66] | Endogenous | Bind nonspecifically to assay antibodies (often at Fc region) | Positive or Negative |
| Human Anti-Animal Antibodies (HAAA) [13] [66] | Endogenous | Bind specifically to animal-derived assay antibodies (e.g., HAMA) | Positive or Negative |
| Cross-Reacting Substances [13] [66] | Endogenous/Exogenous | Compounds with similar epitopes compete for antibody binding sites | Positive or Negative |
| Autoantibodies [13] | Endogenous | Found in individuals with autoimmune disorders; bind self-analytes | Positive or Negative |
| Therapeutic Antibodies [13] | Exogenous | Administered drugs (e.g., Digibind) interfere until excreted | Positive or Negative |
| Elevated Serum Components [13] | Endogenous | Hemoglobin (hemolysis), bilirubin (icterus), lipids (lipemia) | Mostly Negative |
Troubleshooting Guides and FAQs
How can I detect a suspected prozone effect in my assay?
The prozone effect should be suspected when there is a clear discrepancy between the immunoassay result and the patient's clinical presentation or other laboratory findings [64]. For example, a patient with severe symptoms or a known condition suggesting very high analyte levels (e.g., nephrotic syndrome for urine albumin) who presents with a normal or only slightly elevated result is a prime candidate for this interference [65]. Many modern automated analyzers are programmed to flag abnormal assay kinetics that may suggest antigen excess [64]. The definitive test is to perform a serial dilution of the sample. If the measured concentration, when adjusted for the dilution factor, increases significantly upon dilution, the prozone effect is confirmed [13] [66] [65].
What is the established experimental protocol to resolve the prozone effect?
The primary solution for the prozone effect is sample dilution [13] [64] [65].
Protocol: Serial Dilution for Prozone Resolution
- Materials: The patient sample, appropriate assay diluent (commercial or recommended by the kit manufacturer) [66], and calibrated pipettes.
- Procedure: Prepare a series of sample dilutions (e.g., 1:2, 1:10, 1:20, 1:50, 1:100) [66]. The choice of dilution factors should be guided by the suspected level of interference and the dynamic range of your assay.
- Analysis: Re-analyze each diluted sample.
- Interpretation: The corrected result is taken from a dilution where the measured concentration falls within the assay's linear range and the dilution-adjusted results plateau. For instance, if a 1:100 dilution gives a result of 500 units, the corrected concentration is 50,000 units. A result that was falsely low in the neat sample will show a several-fold increase after correction [66].
Our research involves detecting multiple structurally similar compounds. How can we manage cross-reactivity?
Cross-reactivity is a major challenge in immunoassay research, occurring when an antibody binds to non-target analytes that share structural similarities with the target [6] [7]. Managing it requires a strategic approach:
- Antibody Selection: In general, monoclonal antibodies (mAbs) offer higher specificity as they recognize a single epitope, making them ideal for distinguishing between closely related compounds. Polyclonal antibodies (pAbs) can provide higher sensitivity but may be more cross-reactive [6].
- Reagent Concentration Optimization: Research demonstrates that cross-reactivity is not an immutable property of the antibodies themselves. Using lower concentrations of antibodies and labeled antigens in competitive assays can lead to lower cross-reactivities (higher specificity). Shifting assay formats (e.g., from FPIA to ELISA) can inherently alter selectivity due to differing reagent concentration requirements [7].
- Use of Blocking Agents: Commercial antibody blocking agents (e.g., heterophile blocking tubes) can be added to the sample to absorb interfering antibodies before analysis [66].
What are the common causes of high background and weak signals in sandwich ELISAs?
High background and weak signals are frequent technical challenges that can obscure true results.
| Problem | Potential Causes | Troubleshooting Solutions |
|---|---|---|
| High Background | Non-specific binding [67] [68], insufficient washing [69] [67], cross-reactivity [68], substrate contamination [69] | Optimize blocking buffer (e.g., BSA, casein) and concentration [69] [70]. Increase wash number/duration [69]. Use fresh, clean plastics to avoid HRP contamination [69]. |
| Weak Signal | Low antibody concentration [69], poor antigen-antibody binding [67], degraded standard [69], incompatible antibody pairs [69] | Titrate and increase primary/secondary antibody concentration [69]. Verify standard integrity and preparation [69]. For sandwich assays, ensure capture/detection antibodies recognize distinct epitopes [69]. |
What experimental workflow should I follow when investigating interference?
The following diagram outlines a systematic workflow for troubleshooting suspected interference in immunoassay results, integrating checks for both the prozone effect and other bidirectional interferents.
Data Presentation: Quantitative Interference Analysis
The following table synthesizes quantitative data from a retrospective study, illustrating the prevalence and impact of analytical interferences across various common immunoassay parameters [66]. This data underscores the very real-world frequency of these issues in a clinical laboratory setting.
Table: Retrospective Analysis of Immunoassay Interferences Over Six Months (n=42 samples investigated) [66]
| Assay Parameter | Samples with Interference | Positive Interference | Negative Interference | Primary Resolution Method |
|---|---|---|---|---|
| Beta HCG | 6 | 2 | 4 | Serial Dilution / Alternate Platform / Antibody Blocking |
| Estradiol | 3 | 2 | 1 | Antibody Blocking |
| CA-125 | 3 | 2 | 1 | Antibody Blocking / Serial Dilution |
| Alfa Feto Protein (AFP) | 2 | 2 | 0 | Antibody Blocking |
| Prolactin | 1 | 1 | 0 | Antibody Blocking |
| Troponin I | 2 | 2 | 0 | Antibody Blocking |
| Hepatitis B Surface Antigen | 1 | 0 | 1 | Not Specified |
| Total | 19 | 11 | 8 |
The Scientist's Toolkit: Key Research Reagent Solutions
Successfully troubleshooting immunoassays requires a set of key reagents designed to mitigate interference and improve assay robustness. The following table details essential tools for the researcher's toolkit.
| Research Reagent | Function & Utility in Troubleshooting |
|---|---|
| Heterophile Blocking Reagents | Commercially available mixtures (e.g., containing anti-human IgG Fc fragments) that bind to heterophilic antibodies and HAMA in the sample, preventing them from interfering with assay antibodies [66]. |
| Assay/Sample Diluents | Protein-based (e.g., MatrixGuard) or protein-free solutions used to dilute samples. This can reduce matrix interference and, critically, resolve the prozone effect [66] [67] [68]. |
| Protein Stabilizers & Blockers | Formulations (e.g., StabilZoat, StabilGuard) used during plate coating and blocking to minimize non-specific binding by occupying unused sites on the solid phase, thereby reducing high background [67] [68]. |
| Alternative Platform Reagents | Access to reagents for a different immunoassay platform (e.g., CLIA vs. ELISA) or methodology. Interference is often method-dependent, and an alternate platform may provide an accurate result [66]. |
| Serial Dilution Buffers | Pre-validated, matrix-matched diluents (often provided with kits) that ensure sample integrity is maintained during the dilution process, which is crucial for obtaining valid corrected results [66]. |
Validation, Comparative Analysis, and Confirmation of Assay Specificity
Frequently Asked Questions: Core Validation Concepts
Q1: What is the practical purpose of testing for parallelism in an immunoassay? Parallelism confirms that the natural analyte present in your sample (e.g., in serum or plasma) is recognized by the assay antibodies in the same way as the recombinant or purified standard used to generate the calibration curve [71]. A lack of parallelism indicates that the sample matrix is interfering with the assay, meaning the concentration you calculate for your sample may be inaccurate [72].
Q2: A spike-and-recovery experiment yielded a recovery of 65%. Is my assay invalid? Not necessarily, but it requires investigation. While an average recovery of 80–120% is generally considered acceptable for many applications [71], a value of 65% indicates significant signal suppression, likely due to matrix interference [5]. You should analyze the recovery profile scientifically; for a highly sensitive assay, a lower recovery might be justifiable. The next step is to troubleshoot by trying different sample dilutions or adding blocking agents to mitigate the interference [72].
Q3: How can I improve the precision of my assay across multiple runs? Poor inter-assay precision (variation between runs on different days) is often due to inconsistencies in manual procedures [73]. To improve precision:
- Establish strict protocols: Standardize pipetting, incubation timing, and washing techniques.
- Use calibrated controls: Run tri-level quality controls with established ranges in every assay to monitor day-to-day variability [73].
- Control reagents: Ensure all reagents are at room temperature before use and use the same reagent lots throughout a longitudinal study where possible [73].
Troubleshooting Guides for Common Validation Challenges
Issue 1: Failure to Demonstrate Parallelism
Problem: The dose-response curve of the serially diluted sample is not parallel to the standard curve.
| Potential Cause | Investigation & Solution |
|---|---|
| Matrix Interference | Components in the sample matrix (e.g., lipids, proteins, bilirubin) are disrupting the antibody-antigen interaction [5] [6]. |
| Action: Increase the minimum sample dilution to reduce the concentration of interferents. Test different dilution buffers or include a blocking agent like BSA or casein in the diluent [5] [41]. | |
| Wrong Calibrator | The recombinant protein standard does not adequately mimic the native form of the analyte in the biological sample [72]. |
| Action: If possible, source a different standard. For quasi-quantitative assays like immunogenicity testing, consider switching to a titer-based approach instead of using a calibration curve [72]. |
Issue 2: Unacceptable Spike-and-Recovery Results
Problem: The percentage recovery of a known amount of analyte spiked into the sample matrix is outside the acceptable range (typically 80-120%) [71].
| Observed Result | Interpretation & Solution |
|---|---|
| Recovery < 80% | This indicates signal suppression. Something in the sample is preventing the antibody from binding to the analyte [5]. |
| Action: Dilute the sample to reduce interference, ensuring the assay is validated for diluted samples [5]. Use a blocking agent like heterophilic antibody blockers or normal serum to saturate nonspecific binding sites [5] [41]. | |
| Recovery > 120% | This indicates signal enhancement. This can be caused by cross-reactivity with similar molecules or other interferents [5]. |
| Action: Investigate potential cross-reactants. Use matched antibody pairs to improve specificity [5]. For drug interference, ask patients to pause supplements if clinically safe (e.g., biotin) [5]. |
Issue 3: Poor Precision (High % CV)
Problem: The coefficient of variation (% CV) for replicate samples is high, both within a single plate (intra-assay) and between different runs (inter-assay).
| Scope of the Problem | Investigation & Solution |
|---|---|
| High Intra-Assay CV | The imprecision is within a single run. |
| Action: Check for pipetting errors, uneven washing, or temperature gradients across the plate. Ensure reagents are thoroughly mixed and the plate reader is functioning correctly. | |
| High Inter-Assay CV | The imprecision is between runs performed on different days, by different operators, or with different reagent lots [73]. |
| Action: Implement rigorous quality control procedures using tri-level controls to monitor operator and day-to-day variability [73]. Establish and adhere to standardized, detailed protocols for all steps. Use automation where possible to minimize user inconsistency [73]. |
Experimental Protocols & Data Interpretation
Protocol 1: Spike-and-Recovery Experiment
This experiment assesses whether the sample matrix affects the accurate detection of the analyte [5] [71].
1. Sample Preparation:
- Neat Matrix: The sample matrix (e.g., pooled normal serum) with no spike.
- Spiked Buffer (Control): A known concentration of analyte spiked into the ideal assay buffer.
- Spiked Matrix (Test): The same known concentration of analyte spiked into the sample matrix.
- Ideally, test low, medium, and high analyte concentrations in duplicate or triplicate [5].
2. Running the Assay: Run all prepared samples according to your immunoassay protocol.
3. Calculation:
% Recovery = (Measured concentration in Spiked Matrix / Measured concentration in Spiked Buffer) x 100 [71]
Interpretation Table:
| % Recovery | Interpretation |
|---|---|
| 80–120% | Acceptable; minimal interference [5] [71]. |
| < 80% | Signal suppression; matrix interference is likely [5]. |
| > 120% | Signal enhancement; possible interference or cross-reactivity [5]. |
Protocol 2: Assessing Parallelism
This experiment verifies that the standard curve is an appropriate tool for quantifying the analyte in the biological sample [71] [72].
1. Sample Preparation: Make a series of dilutions of a positive sample that contains the endogenous analyte. The dilutions should span the anticipated working range of the assay.
2. Running the Assay: Run the serially diluted sample alongside the standard curve calibrators.
3. Data Analysis: Plot the measured concentration (or assay signal) for each dilution against the dilution factor or the expected concentration. The resulting curve should be parallel to the standard curve. A lack of parallelism suggests matrix interference or that the standard is not immunologically similar to the native analyte [72].
Protocol 3: Determining Precision
Precision is measured by testing multiple replicates of samples at various concentrations.
- Intra-Assay Precision: Test at least 3 samples with low, mid, and high analyte concentrations in 14 or more replicates on the same plate [71].
- Inter-Assay Precision: Test the same 3 samples in duplicate over multiple separate assay runs (e.g., 36 times over multiple days) [71].
Calculation:
% CV = (Standard Deviation / Mean) x 100
A % CV of <10% is typically considered acceptable for immunoassays [71].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Blocking Agents (BSA, Casein) | Reduce nonspecific binding by saturating potential interfering sites on the solid phase and sample components [5] [41]. |
| Heterophilic Blocking Reagents | Specifically reduce interference from human anti-animal antibodies (HAAA) like HAMA, which can cause false positives/negatives [5] [41]. |
| Matched Antibody Pairs | Pre-optimized capture and detection antibody pairs improve assay specificity and reduce the risk of cross-reactivity [5]. |
| Tri-Level QC Controls | Recombinant or pooled natural samples with established ranges are essential for monitoring operator, inter-assay, and lot-to-lot variability [73]. |
| Normal Sera | Serum from various species (human, mouse, goat, etc.) can be used as a component of blocking buffers or to assess matrix effects [5]. |
Workflow Visualization
Parallelism Assessment Workflow
Spike & Recovery Workflow
Urine drug screening (UDS) immunoassays are a primary method for assessing exposure to drugs of abuse. Although fast and relatively inexpensive, these tests frequently produce false-positive results due to cross-reactivity with structurally similar compounds or metabolites they were not designed to detect [19]. This limitation can lead to incorrect assumptions about drug exposure and damage the provider-patient relationship. For example, a 2020 study analyzing 698,651 UDS results found that exposure to certain medications significantly increased the odds of a false-positive screen, validating 12 out of 13 suspected assay-ingredient interferences affecting tests for amphetamines, buprenorphine, cannabinoids, and methadone [19]. This cross-reactivity problem extends beyond clinical toxicology into food allergen detection, where ELISA methods struggle to distinguish between similar allergenic proteins, such as those in pistachios and cashews [74]. In research and diagnostic settings, Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) serves as the gold standard comparator to confirm results and overcome these limitations, providing the specificity needed for accurate identification and quantification of target analytes.
FAQ: LC-MS/MS as a Confirmatory Method
1. Why is LC-MS/MS considered the gold standard for confirming immunoassay results? LC-MS/MS is regarded as the gold standard due to its high specificity and sensitivity. Unlike immunoassays, which rely on antibody-antigen binding and are prone to cross-reactivity, LC-MS/MS separates compounds by liquid chromatography (LC) and then identifies them based on their precise mass-to-charge ratio (MS/MS) [75]. This two-stage separation and detection process allows it to distinguish between structurally similar molecules, thereby definitively confirming the presence and identity of a target analyte [19] [74].
2. What are the key advantages of LC-MS/MS over immunoassays? The core advantages are its multiplexing capability and freedom from antibody cross-reactivity [74]. LC-MS/MS can simultaneously detect dozens of analytes in a single run from a small sample volume. It directly measures the analyte (or a proteolytic peptide in the case of protein allergens) rather than relying on an antibody, which makes it unaffected by the cross-reactivity that pliques ELISA and can lead to false positives [74] [19].
3. My immunoassay shows a positive result, but the LC-MS/MS confirmation is negative. What is the most likely explanation? The most probable explanation is a false-positive immunoassay caused by cross-reactivity [19]. The sample may contain a compound that is structurally similar enough to the target drug to bind the assay's antibody but is differentiated by the highly specific mass spectrometry process. It is standard practice to confirm any presumptive positive immunoassay result with a more specific technique like LC-MS/MS [19].
4. What software tools are available for processing LC-MS/MS data? MAVEN is an open-source software program specifically designed for interactive processing of LC-MS-based metabolomics data [76]. It enables rapid and reliable metabolite quantitation from multiple reaction monitoring (MRM) data or high-resolution full-scan mass spectrometry data. The software assists with peak alignment across samples, isotope-labeling quantification, and visualization of raw data [76].
Troubleshooting Common LC-MS/MS Workflow Issues
Peak Detection and Alignment
- Problem: Poor alignment of peaks for the same metabolite across multiple samples due to retention time drift.
- Solution:
Data Quality and Noise
- Problem: Excessive noise in the data obscures peaks of interest.
- Solution:
- Spectral filtering: Apply software algorithms to remove noise and facilitate peak detection [75].
- Optimize LC method: Use shorter HPLC columns with smaller particle sizes to improve separation and reduce noise [75].
- Pre-import filtering: When using MAVEN, utilize the "File Import" options to centroid data or eliminate low-intensity data points during the file loading process to reduce file size and noise [76].
Method Specificity and Discrimination
- Problem: Inability to distinguish between two highly similar allergens (e.g., pistachio vs. cashew).
- Solution:
- Develop a targeted LC-MS/MS (QqQ) method: As demonstrated for food allergen analysis, a targeted method can focus on unique peptide markers for each allergen [74].
- Validate for specificity: Ensure the method can unequivocally identify and differentiate the target analytes from all other components in the sample matrix [74].
Experimental Protocol: Validating an LC-MS/MS Method to Overcome Cross-Reactivity
This protocol outlines the development and validation of a discriminatory LC-MS/MS method, based on a 2025 study that differentiated pistachio and cashew allergens [74].
Sample Preparation
- Extract analytes from the relevant matrix (e.g., urine, food samples).
- For protein allergens, proteins are extracted, purified, and then digested with an enzyme like trypsin to generate characteristic peptides for analysis [74].
- For small molecules (e.g., drugs), a protein precipitation or solid-phase extraction is typically used.
LC-MS/MS Analysis
- Chromatography: Use a reversed-phase UHPLC column to separate digested peptides or small molecules based on hydrophobicity.
- Mass Spectrometry: Operate the triple quadrupole (QqQ) mass spectrometer in Multiple Reaction Monitoring (MRM) mode.
- Q1: Selects the precursor ion (specific parent mass).
- Collision Cell: Fragments the precursor ion.
- Q3: Monets for a specific, unique fragment ion.
- This two-stage mass selection provides high specificity [74].
Method Validation
Validate the following parameters to ensure method reliability [74]:
- Specificity: Confirm the method can distinguish the target analytes from any potential interferents.
- Screening Detection Limit (SDL): Determine the lowest concentration at which the analyte can be reliably detected.
- Precision: Assess the repeatability and reproducibility of the method.
- Ruggedness: Test the method's robustness to small, deliberate variations in operational parameters (e.g., temperature, flow rate).
Workflow Diagram
The following table summarizes the core performance characteristics that should be assessed when validating an LC-MS/MS method designed to address cross-reactivity, as exemplified by food allergen analysis [74].
Table 1: Essential Validation Parameters for a Discriminatory LC-MS/MS Method
| Parameter | Description | Target Performance |
|---|---|---|
| Specificity | Ability to distinguish target analyte from interferents. | No false positives/negatives from cross-reactants. |
| Screening Detection Limit (SDL) | Lowest concentration for reliable detection. | e.g., 1 mg/kg for food allergens [74]. |
| Precision | Closeness of repeated measurements under set conditions. | Good reproducibility (e.g., for pistachio detection) [74]. |
| Ruggedness | Robustness against deliberate method parameter changes. | All critical parameters must be strictly controlled [74]. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for LC-MS/MS Experiments
| Item | Function |
|---|---|
| Triple Quadrupole (QqQ) Mass Spectrometer | The core instrument for targeted, highly specific analysis via MRM [74]. |
| Reversed-Phase UHPLC Column | Separates components of the mixture by hydrophobicity before they enter the MS [74]. |
| Isotopically Labelled Internal Standards | Added to the sample to correct for losses during preparation and variations in ionization efficiency [74]. |
| Enzymes (e.g., Trypsin) | Digests proteins into specific peptides for bottom-up proteomic analysis of allergens [74]. |
| Data Processing Software (e.g., MAVEN) | Open-source tool for peak alignment, quantitation, and visualization of LC-MS data [76]. |
Troubleshooting Guide: Resolving Cross-Reactivity in Immunoassays
Cross-reactivity occurs when an antibody binds to non-target molecules that are structurally similar to the intended antigen, leading to false positives or an overestimation of the analyte concentration [6]. The table below outlines common symptoms, their root causes, and practical solutions.
Table: Troubleshooting Guide for Cross-Reactivity and Interference
| Problem Observed | Potential Root Cause | Recommended Solution |
|---|---|---|
| High background noise or false positives | Antibody cross-reactivity with similar compounds or non-specific binding to non-target structures [77] [78]. | - Use monoclonal antibodies for higher specificity [6] [79].- Pre-absorb or use cross-adsorbed antibodies [77].- Optimize antibody concentration to minimize non-specific binding [78]. |
| Inconsistent results between similar assays | Varying cross-reactivity intrinsic to different immunoassay formats and reagent concentrations, even with the same antibody pair [7] [80]. | - Standardize reagent concentrations and ratios across methods [7].- Transfer to a more specific format (e.g., from ELISA to a fluorescence-based method) [7]. |
| Interference from complex sample matrices | Matrix components (e.g., related proteins, binding factors, endogenous antibodies) interfering with the antigen-antibody interaction [6]. | - Dilute the sample to reduce interference, balancing this with sensitivity needs [6].- Use a platform with minimal contact time between reagents and the sample matrix to favor specific, high-affinity interactions [6]. |
| Weak specific signal alongside high background | Antibody concentration is too high, leading to both specific and non-specific binding [78] [79]. | Titrate the antibody to find the optimal working concentration that maximizes signal-to-noise ratio [79]. |
| Non-specific staining in cell-based assays | Fc receptor-mediated binding on certain cell types (e.g., immune cells) [81]. | - Use Fc-silenced antibodies [81].- Include an Fc receptor blocking step prior to antibody staining [81]. |
Frequently Asked Questions (FAQs) on Immunoassay Performance
Q1: What are the primary factors that contribute to antibody cross-reactivity? Cross-reactivity is primarily caused by the structural similarity between the target analyte and other molecules present in the sample [6]. An antibody's binding site may recognize and bind to shared epitopes or structures with similar conformations on different proteins or compounds. The use of polyclonal antibodies, which recognize multiple epitopes, can sometimes increase the risk of cross-reactivity compared to monoclonal antibodies [6] [79]. Furthermore, the cross-reactivity profile is not an immutable property of the antibody itself; it can be significantly influenced by the specific assay format, reagent concentrations, and incubation times used [7] [80].
Q2: How can I minimize background noise in my immunoassay? Several strategies can effectively reduce background noise:
- Optimized Blocking: Use serum from the same species as the secondary antibody or BSA for effective blocking of non-specific binding sites [77] [79].
- Thorough Washing: Implement stringent and consistent washing steps after each incubation to remove unbound antibodies and reagents [78].
- Antibody Titration: Avoid using excessively high antibody concentrations, which can exacerbate non-specific binding. Always determine the optimal dilution for your specific experimental conditions [78] [79].
- Advanced Detection Systems: Employ modern detection kits that offer higher sensitivity and cleaner signals, which can help distinguish specific signal from background [77].
Q3: Can I change an assay's cross-reactivity without developing new antibodies? Yes, it is possible. Research has demonstrated that cross-reactivity can be modulated by altering the assay conditions [7] [80]. Shifting to an immunoassay format that operates with lower concentrations of antibodies and labeled antigens can make the assay more specific and reduce cross-reactivity. Furthermore, even within the same format, adjusting the ratio of immunoreactants' concentrations can fine-tune the selectivity of the detection [7] [80].
Q4: What are the key differences between monoclonal and polyclonal antibodies in assay development?
- Monoclonal Antibodies (mAbs): These are derived from a single B-cell clone and recognize a single, specific epitope on an antigen. They generally provide higher specificity and lower cross-reactivity, making them ideal for distinguishing between highly similar molecules. However, they may have lower overall sensitivity [6] [79].
- Polyclonal Antibodies (pAbs): These are a mixture of antibodies produced by different B-cell clones, recognizing multiple epitopes on the same antigen. They typically offer higher sensitivity due to this multi-epitope recognition and are more tolerant of minor antigen changes (e.g., glycosylation). The trade-off is a potentially higher risk of cross-reactivity [6] [79].
Q5: How does sample matrix interference affect immunoassay results, and how can it be addressed? The sample matrix (e.g., serum, plasma, tissue homogenates) contains various components that can interfere with the antibody-antigen reaction, leading to inaccurate results [6]. This can manifest as either suppression or enhancement of the signal. To address this:
- Demonstrate Parallelism: Ensure the dilution curve of the sample is parallel to the standard curve prepared in the assay buffer.
- Determine Recovery: Spike a known amount of the analyte into the matrix and calculate the percentage recovered.
- Use Minimal Dilution: Dilute the sample to the minimum extent possible to reduce matrix effects while maintaining the analyte within the detectable range of the assay [6].
Experimental Protocols for Key Analyses
Protocol 1: Evaluating and Minimizing Cross-Reactivity
Objective: To assess the cross-reactivity profile of an antibody and implement strategies to enhance specificity.
Materials:
- Primary antibody (monoclonal or polyclonal)
- Target antigen and structurally similar analogs (cross-reactants)
- Appropriate immunoassay platform (e.g., ELISA, Gyrolab platform)
- Blocking buffers (e.g., BSA, animal serum)
- Washing buffers
- Detection reagents
Methodology:
- Cross-Reactivity Screening:
- Set up your standard competitive immunoassay calibration curve with the primary target analyte.
- In parallel, run the same assay using potential cross-reacting compounds over a wide concentration range.
- Calculate the cross-reactivity (CR) for each compound using the formula: CR (%) = [IC₅₀ (Target Analyte) / IC₅₀ (Cross-Reactant)] × 100% [7] [80].
- A high CR percentage indicates significant cross-reactivity.
- Optimization for Specificity:
- Reagent Concentration Titration: Lower the concentrations of the antibody and the labeled antigen. Assays with sensitive detection and low reagent concentrations often demonstrate higher specificity [7].
- "Heterologous" Assay Setup: Use a slightly different antigen derivative for the detection system than the one used for immunization. This can selectively engage a subset of antibodies with higher specificity [7].
- Assay Format Transfer: If possible, transition the assay to a more specific format (e.g., from ELISA to a fluorescence polarization immunoassay (FPIA)), which may inherently reduce cross-reactivity [7] [80].
Protocol 2: Balancing Signal Strength and Background Noise in Multiplex Immunohistochemistry (mIHC)
Objective: To achieve clear, specific staining for multiple markers on a single tissue section with minimal background.
Materials:
- Validated primary antibodies from different host species or with different labels
- Fc receptor blocking reagent (e.g., Fc block) or Fc-silenced antibodies [81]
- Multiplex IHC detection kit (e.g., fluorescent or chromogenic)
- Antigen retrieval solution (e.g., citrate buffer, pH 6.0 or Tris-EDTA, pH 9.0)
- Serum for blocking
Methodology:
- Tissue Preparation and Antigen Retrieval:
Blocking and Antibody Incubation:
- Block the tissue with an appropriate serum (from the same species as the secondary antibody) to occupy non-specific sites [79].
- For assays on immune cells, include an Fc receptor blocking step or use Fc-silenced antibodies to prevent non-specific antibody binding [81].
- Incubate with primary antibodies, ideally one at a time, or as a pre-validated cocktail. Use the lowest effective concentration determined by prior titration [77] [78].
Signal Detection and Visualization:
- Use a highly sensitive and specific detection system, such as a tyramide signal amplification (TSA) kit, to achieve strong signals without high background [77].
- Keep DAB or other chromogen incubation times consistent and monitor under a microscope to prevent over-development, which increases background [78] [79].
Key Signaling Pathways and Workflows
The following diagram illustrates the core concepts of competitive immunoassays and the primary sources of interference.
The Scientist's Toolkit: Essential Research Reagent Solutions
This table lists key reagents and technologies that are critical for developing robust and specific new-generation immunoassays.
Table: Essential Reagents for Advanced Immunoassay Development
| Reagent / Technology | Primary Function | Application Note |
|---|---|---|
| Monoclonal Antibodies (mAbs) | Recognize a single epitope, providing high specificity and reducing cross-reactivity [6]. | Ideal for capture antibodies in sandwich assays to establish a highly specific foundation for the test. |
| Fc-Silenced Antibodies | Genetically engineered antibodies with mutations in the Fc region to prevent binding to Fc receptors on cells [81]. | Crucial for flow cytometry and IHC on immune cells to eliminate non-specific, Fc-mediated background staining. |
| Gyrolab & Other Miniaturized Platforms | Automated, miniaturized flow-through immunoassay systems that use nanoliter volumes of samples and reagents [6]. | Reduces matrix interference through short contact times and enables high-precision data from precious samples (e.g., pediatric studies). |
| Heterologous Antigens | A derivative of the target antigen with a slightly different structure, used in the detection system of a competitive assay [7]. | A strategic method to narrow the selectivity of an immunoassay by engaging only a subset of highly specific antibodies from a polyclonal mixture. |
| Multiplex IHC Detection Kits | Enable simultaneous detection of multiple biomarkers on a single tissue section using fluorescent or chromogenic tags [77]. | Requires careful antibody validation and signal balancing. Advanced kits offer stronger signals and clearer marker localization. |
Cross-reactivity (CR) represents one of the most significant technical obstacles in developing robust and reliable multiplex bead-based antibody arrays. This interference occurs when antibodies bind to non-target proteins or analytes, potentially compromising assay specificity and accuracy. In multiplexed sandwich assays (MSAs), where capture and detection antibodies are applied as mixtures, the vulnerability to cross-reactivity increases quadratically with the number of targets, fundamentally limiting scalability [82] [83]. Unlike single-plex immunoassays, where cross-reactivity primarily arises from sample components, multiplex formats introduce reagent-driven cross-reactivity, where detection antibodies may inadvertently bind to non-matched capture antibodies immobilized on different beads [83]. This challenge is compounded by the fact that antibodies are inherently "imperfect building blocks" that often display unexpected binding to off-target proteins, even when validated for monoplex applications [83]. Understanding, evaluating, and mitigating these effects is crucial for researchers, scientists, and drug development professionals relying on multiplex protein quantification for biomarker discovery, validation, and translational research.
Troubleshooting Guide: Frequently Asked Questions
General Cross-Reactivity Issues
What are the primary symptoms of cross-reactivity in my multiplex assay data?
Unexpectedly elevated background signals, non-parallel displacement in standard curves, poor spike-and-recovery results, and inconsistent data between single-plex and multiplex formats indicate potential cross-reactivity issues. Specifically, when some analytes in a panel show unexpectedly high signals in samples where they should be low or undetectable, cross-reactive interference should be suspected [84] [83]. Additionally, measurements that contradict established biological expectations or previously validated data may signal cross-reactivity problems requiring investigation.
Why do antibodies that work well in single-plex assays show cross-reactivity in multiplex formats?
Antibodies validated for monoplex immunoassays may display cross-reactivity with other proteins in multiplex formats due to the fundamental difference in assay architecture. In single-plex sandwich immunoassays, the dual binding requirement (both capture and detection antibodies must bind the target) provides inherent protection against false positives from single cross-reacting species [83]. However, in multiplexed sandwich assays (MSAs), detection antibodies are applied as a mixture, creating opportunities for these detection antibodies to bind non-specifically to capture antibodies directed against different analytes [82] [83]. This reagent-driven cross-reactivity represents a distinct challenge not present in single-plex formats and necessitates application-specific antibody validation [44].
How does multiplexing level affect cross-reactivity vulnerability?
The vulnerability of multiplex sandwich assays to cross-reactivity increases quadratically with the number of targets, creating a fundamental scalability limitation [82]. This mathematical relationship arises because each additional analyte introduces new potential interaction pairs between non-matched capture and detection antibodies. Experimental evidence substantiates that scaling up conventional multiplex sandwich assays beyond approximately 30-50 targets becomes increasingly challenging due to this combinatorial complexity [82] [83]. This vulnerability metric explains why extensive optimization is required for even moderate-plex assays and why alternative approaches are needed for high-plex applications.
Experimental Design and Optimization
What strategies can I implement during assay development to minimize cross-reactivity?
- Comprehensive Antibody Screening: Employ rigorous validation protocols beyond Western blotting, using multiplexed immobilized proteins or peptides to concurrently analyze epitope recognition and binding affinity [44]. Suspension arrays on the Luminex platform can determine antibody specificity toward up to 100 antigens within hours [44].
- Optimized Assay Diluents: Utilize specifically formulated diluents containing proprietary blocking reagents that significantly reduce false signals by addressing non-specific binding, cross-reactivity, and antibody interference [84] [85]. These diluents are particularly important for mitigating interference from factors like human anti-mouse antibodies (HAMA) and rheumatoid factor (RF) in biological samples [84].
- Buffer Composition Optimization: Implement buffers designed to minimize nonspecific protein binding while maintaining antibody affinity and specificity. Specialized bead diluents contain "a cocktail of proprietary blocking reagents which significantly reduces false signal to ensure true biomarker measurement" [85].
- Concentration Optimization: Shift to lower concentrations of immunoreactants where possible, as this can decrease cross-reactivities by up to five-fold in some assay systems [7].
Can I combine analytes from different MILLIPLEX kits to create a custom panel?
Manufacturers generally discourage combining kits due to significant risks of antibody cross-reactivity, incompatible sample dilution factors, inappropriate serum matrix, buffers, or incubation periods that can collectively skew results [85]. Each kit is developed and verified to perform optimally with its included reagents according to specific protocol recommendations. For custom panel needs, specialized custom assay services should be consulted instead of manually combining kits [85].
How should I handle samples with complex matrices to reduce interference?
For serum and plasma samples, ensure at least a 1:1 ratio of sample to assay diluent to mitigate matrix effects [86]. For cell lysates or tissue homogenates, confirm appropriate dilution in assay buffer to reduce detergent concentration to ≤0.01% [86]. Always clarify samples by centrifugation (5-10 minutes recommended) to remove debris and lipids before analysis [86]. Additionally, qualify your standard curve by checking for plateaus, abnormal curve fits, and outliers that may indicate matrix interference [86].
Technical Validation and Quality Control
What quality control measures specifically address cross-reactivity?
Reputable manufacturers implement comprehensive testing protocols including cross-reactivity validation between assay components [85]. When evaluating commercial kits, review available cross-reactivity data provided in package inserts or technical specifications. Additionally, implement rigorous spike-and-recovery experiments using known cross-reactants specific to your panel [87]. For custom arrays, systematic combinatorial testing for cross-reactivity between each antibody and all other antibodies and analytes is essential, though this process is notoriously costly and labor-intensive [82].
How can I verify whether observed signals represent true detection or cross-reactivity?
Implement orthogonal validation using alternative platforms or methodologies for a subset of samples and analytes [83]. Additionally, performance verification with standard addition methods (spike-and-recovery) can help distinguish true detection from cross-reactive signals. The Proximity Extension Assay (PEA) technology provides an alternative approach that molecularly discriminates specific binding from cross-reactivity through DNA barcode pairing that only occurs when both antibodies bind their correct target [83] [88].
Quantitative Data on Cross-Reactivity
Table 1: Experimentally Determined Cross-Reactivity in Steroid Hormone Immunoassays
| Compound | Target Assay | Cross-Reactivity | Likelihood of Clinically Significant Interference |
|---|---|---|---|
| 6-Methylprednisolone | Cortisol | 249% | High |
| Prednisolone | Cortisol | 148% | High |
| 21-Deoxycortisol | Cortisol | 45.4% | High in 21-hydroxylase deficiency |
| 11-Deoxycortisol | Cortisol | 4.6% | High in 11β-hydroxylase deficiency |
| Canrenone | Cortisol | 1.8% | Possible during peak concentrations |
| 17-Hydroxyprogesterone | Cortisol | 1.6% | High in 21-hydroxylase deficiency |
| Methyltestosterone | Testosterone | 144% | High |
| Danazol | Testosterone | 29% | Moderate to High |
| Norethindrone | Testosterone | 9.4% | Possible in women receiving therapy |
Table 2: Multiplex Assay Performance Characteristics and Verification Criteria
| Performance Parameter | Verification Criteria | Importance for Cross-Reactivity Management |
|---|---|---|
| Assay Sensitivity | Limit of detection (LOD) and quantification (LOQ) | Determines minimum detectable analyte concentration |
| Cross-Reactivity | Systematic testing of structurally similar compounds | Identifies potential interferents |
| Precision | Intra- and inter-assay coefficient of variation (CV) | Assesses assay reproducibility |
| Dynamic Range | Upper and lower limits of quantification | Ensures accurate measurement across analyte concentrations |
| Specificity | Evaluation against related proteins and metabolites | Confirms target-specific recognition |
| Recovery | Spike-and-recovery in relevant matrices | Verifies accuracy in biological samples |
| Parallelism | Dilution linearity of native samples | Confirms appropriate matrix composition |
Experimental Protocols for Cross-Reactivity Evaluation
Systematic Cross-Reactivity Testing for Custom Multiplex Arrays
This protocol provides a comprehensive, step-by-step methodology for evaluating cross-reactivity in custom-made multiplex bead-based antibody microarrays, as required for ensuring assay reliability and accuracy [87].
Materials and Reagents
- Custom multiplex bead-based array with immobilized capture antibodies
- Detection antibody cocktail
- Analyte standards for all targets in the panel
- Potential cross-reactants (structurally similar compounds, related proteins, known interferents)
- Assay buffer (optimized for multiplexing)
- Wash buffer
- Detection reagents (e.g., streptavidin-phycoerythrin)
- Luminex instrument or appropriate detection system
Procedure
- Preparation of Cross-Reactivity Testing Solutions: Prepare individual solutions containing each potential cross-reactant at concentrations spanning the physiological and pathological range, using the same matrix as your samples (e.g., serum, plasma) [89].
- Single Analyte Spike-In Experiments: For each potential cross-reactant, run the complete multiplex assay protocol using samples containing only that compound (no target analytes present). This identifies detection antibodies that may bind directly to non-matched capture beads [83].
- Cross-Reactivity Calculation: Quantify percent cross-reactivity using the formula:
CR (%) = (Measured Apparent Target Concentration / Actual Cross-Reactant Concentration) × 100[89]. - Combinatorial Testing: Test mixtures of potential cross-reactants to identify synergistic interference effects not apparent in single compound testing.
- Dilutional Linearity Assessment: Perform serial dilutions of samples with known cross-reactants to determine if observed interference shows expected concentration dependence.
Interpretation and Optimization
- Compounds showing >5% cross-reactivity generally warrant further investigation and potential assay modification [89].
- For cross-reactants with known physiological concentrations, calculate whether the interference would be clinically or biologically relevant [89].
- If specific cross-reactivities are identified, consider modifying detection antibody concentrations, optimizing blocking reagents, or replacing problematic antibody pairs.
Antibody Colocalization Microarray as an Alternative Approach
For researchers facing intractable cross-reactivity issues with conventional multiplex sandwich assays, the Antibody Colocalization Microarray (ACM) protocol offers a fundamentally different approach that eliminates reagent-driven cross-reactivity by avoiding mixing of detection antibodies [82].
Workflow Overview
Figure 1: Antibody Colocalization Microarray Workflow. This approach physically separates the application of detection antibodies to prevent mixture-induced cross-reactivity [82].
Key Advantages
- Eliminates Reagent-Driven Cross-Reactivity: By applying each detection antibody precisely to its matched capture spot, this method prevents detection antibodies from interacting with non-matched capture antibodies [82].
- Maintains Sandwich Assay Sensitivity: The approach preserves the dual recognition benefits of traditional sandwich immunoassays while overcoming the fundamental scalability limitation of conventional MSAs [82].
- Enables Higher Multiplexing: The ACM technology has been successfully implemented with up to 50 targets, demonstrating improved scalability compared to conventional MSAs [82].
Implementation Considerations
- Requires access to a microarrayer capable of precise spotting operations
- Demands careful optimization of spotting buffers and humidity control during printing
- Necessitates validation against reference methods to ensure quantitative accuracy
Research Reagent Solutions for Cross-Reactivity Management
Table 3: Essential Reagents for Cross-Reactivity Troubleshooting in Multiplex Assays
| Reagent / Material | Function in Cross-Reactivity Management | Implementation Tips |
|---|---|---|
| Optimized Assay Diluent | Reduces non-specific binding and antibody interference | Use manufacturer-recommended diluents containing proprietary blocking reagents [84] |
| Bead Diluent | Significantly reduces false signal through blocking reagent cocktail | Ensure proper reconstitution and storage conditions [85] |
| Serum Matrix Solution | Provides appropriate matrix for standard dilution | Use when preparing standards for serum/plasma samples to simulate native protein environment [85] |
| Assay Buffer | Maintains optimal antibody binding specificity | Avoid substitution with non-validated buffers to prevent altered specificity [86] |
| Wash Buffer | Removes unbound proteins and detection antibodies | Follow recommended wash cycles precisely to minimize non-specific signal [86] |
| Magnetic Beads | Solid support for capture antibodies | Protect from light and organic solvents to prevent degradation [86] |
| Detection Antibody Cocktail | Binds captured analytes for detection | Verify specificity through cross-reactivity testing [85] |
| Quality Controls (High/Low) | Monitors assay performance and detects interference | Include in every run to identify developing cross-reactivity issues [85] |
Cross-reactivity remains a fundamental challenge in multiplex bead-based arrays that demands systematic evaluation and mitigation strategies. The quadratic increase in vulnerability with increasing multiplex level creates an inherent scalability limitation for conventional multiplexed sandwich assays [82]. Successful management requires comprehensive antibody validation, optimized assay conditions, and rigorous quality control measures. Emerging technologies like Antibody Colocalization Microarrays [82] and Proximity Extension Assays [83] [88] offer promising alternatives that address the fundamental mechanisms of reagent-driven cross-reactivity. As multiplexed protein profiling continues to advance in biomarker research and drug development, implementing robust cross-reactivity evaluation protocols will be essential for generating reliable, reproducible, and biologically meaningful data.
Implementing Confirmatory Testing Strategies for Critical Results
FAQs: Addressing Common Cross-Reactivity Challenges
FAQ 1: Why did our screening assay reactive rate increase after switching to a new, more automated platform? A recent large-scale retrospective study highlights that transitioning from manual Enzyme Immunoassays (EIA) to automated Chemiluminescent Microparticle Immunoassays (CMIA) can lead to significantly increased reactive rates for markers like HBsAg, HIV-1/2 antibodies, and HTLV-I/II antibodies [90]. This increase was not associated with a corresponding rise in confirmatory Nucleic Acid Test (NAT) reactive results, indicating a potential rise in false positives or non-viremic results due to the different technology [90]. This underscores the necessity of confirmatory testing before finalizing critical results.
FAQ 2: What are the primary sources of interference and cross-reactivity in immunoassays? Interference can be analyte-dependent or independent [12]. Key sources include:
- Endogenous Interferents: Heterophile antibodies, human anti-animal antibodies, autoantibodies, rheumatoid factors, and other binding proteins unique to an individual can alter antibody binding [12].
- Cross-reactivity: This occurs when an antibody binds to a structurally similar compound instead of the target analyte, leading to false positives [20]. This is a significant concern in drug testing [20] and with metabolites of target analytes [12].
- Matrix Effects: The complex composition of biological samples (e.g., serum, plasma) can cause non-specific interference, affecting assay robustness and specificity [6].
- Exogenous Interferents: These include certain medications, drug metabolites [12], and substances that alter the measurable analyte concentration, such as binding proteins [12].
FAQ 3: Our immunoassay shows acceptable specificity during validation. Why are we still seeing inconsistent results in patient samples? Even well-validated assays can be susceptible to interference from unique patient-specific factors. A survey indicated that matrix interference is the single most important challenge in ligand binding assays for large molecules [6]. Furthermore, cross-reactivity is not a fixed parameter intrinsic only to the antibodies; it can vary significantly with different assay formats, reagent concentrations, and incubation times [7]. A result that is inconsistent with the clinical picture should be investigated for potential interference.
FAQ 4: When is a confirmatory test absolutely required? Confirmatory testing is mandatory when a screening immunoassay result is reactive or positive, especially if it is critical or unexpected. Regulatory guidelines, such as those for federal workplace drug testing, explicitly require confirmation of all positive screening tests using a highly specific technique like LC-MS/MS [91]. In other contexts, such as deceased donor eligibility for tissue transplantation, a reactive screening result mandates deferral regardless of other test results, highlighting the high-stakes impact of false positives [90].
Troubleshooting Guides
Guide 1: Systematic Approach to a Suspected False Positive
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1. Verify Result | Repeat the analysis on the original sample using the same immunoassay. | Rules out random analytical error or pipetting mistake. Follow standard operating procedures precisely. |
| 2. Dilution Test | Perform a linearity (parallelism) study by serially diluting the patient sample with an appropriate matrix (e.g., assay buffer or negative serum). | In a true positive, the measured analyte concentration should decrease linearly with dilution. Non-linearity suggests interference from substances like heterophile antibodies [12]. |
| 3. Confirm with Orthogonal Method | Analyze the sample using a method with a different principle of detection, such as LC-MS/MS or a different immunoassay platform. | LC-MS/MS provides superior specificity by separating and identifying analytes based on mass, effectively ruling out immunological cross-reactivity [92]. This is the gold standard for confirmation. |
| 4. Use Blocking Reagents | Pre-treat the sample with commercial blocking reagents designed to neutralize heterophile antibodies. | These reagents contain a mixture of non-specific animal immunoglobulins that bind and "block" heterophile antibodies, preventing them from interfering with the assay antibodies [12]. A significant change in result post-blocking indicates this type of interference. |
This logical workflow moves from simple verification to definitive identification of interference, ensuring efficient use of laboratory resources.
Guide 2: Protocol for Evaluating Cross-Reactivity During Assay Development
Objective: To quantitatively determine the cross-reactivity of an immunoassay with structurally similar compounds.
Methodology:
- Preparation of Cross-Reactant Solutions: Prepare stock solutions of the target analyte and each potential cross-reactant (e.g., metabolites, related drugs). Ensure they are dissolved in a matrix similar to the sample matrix (e.g., negative serum) [7].
- Dose-Response Curves: Run the immunoassay using a series of concentrations for both the target analyte and each cross-reactant. Each concentration should be tested in duplicate or triplicate.
- Data Analysis: For each substance, calculate the concentration that causes a 50% inhibition of the signal (IC50) in a competitive format, or the midpoint of the calibration curve in immunometric assays [7].
- Cross-Reactivity Calculation: Calculate the percentage cross-reactivity (CR%) for each cross-reactant using the standard formula [7]:
- CR% = (IC50 of target analyte / IC50 of cross-reactant) × 100%
Interpretation:
- A high CR% (e.g., >50%) indicates significant cross-reactivity, meaning the assay may not distinguish well between the two compounds.
- A low CR% (e.g., <1%) indicates high specificity for the target analyte.
Key Technical Consideration: Cross-reactivity is not an absolute value. It can be modulated by changing assay conditions. Research shows that using lower concentrations of antibodies and labeled antigens in competitive immunoassays can significantly reduce cross-reactivity, making the assay more specific [7].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and strategies to mitigate cross-reactivity and interference.
| Item / Solution | Function & Explanation |
|---|---|
| High-Affinity Monoclonal Antibodies | Monoclonal antibodies recognize a single epitope, providing high specificity and reducing the chance of cross-reaction with structurally similar but distinct molecules [6]. |
| Heterophile Blocking Reagents | A mixture of animal immunoglobulins and inert proteins used to pre-treat samples. They neutralize heterophile antibodies and human anti-animal antibodies, preventing false signal generation [12]. |
| LC-MS/MS Systems | The gold-standard confirmatory technique. It separates compounds by liquid chromatography and identifies them by mass, providing definitive confirmation and distinguishing target analytes from cross-reactants [92]. |
| Platforms with Pre-treatment Steps | Technologies like Fujirebio's iTACT method incorporate a fully automated pre-treatment step using detergents/denaturants to break down antigen complexes and inactivate interferents, enhancing accuracy [93]. |
| Anti-Metatype Antibodies | A novel solution for detecting small molecules. These antibodies bind to the complex of an antibody and a small-molecule antigen, enabling a specific sandwich assay format that is traditionally difficult to achieve for small analytes [93]. |
| Miniaturized & Automated Platforms | Systems like the Gyrolab platform use microfluidics and nanoliter-scale volumes. The short, controlled contact times in flow-through systems favor specific high-affinity interactions while minimizing low-affinity matrix interference [6]. |
Conclusion
Cross-reactivity is an inherent property of immunoassays that can be systematically managed and, in some cases, strategically leveraged. A modern approach moves beyond viewing it as a mere technical flaw to understanding it as a tunable parameter influenced by reagent choice, assay format, and operating conditions. The key to success lies in a holistic strategy that combines rigorous reagent validation, intelligent assay design optimized for the specific analytical question, and robust confirmation with orthogonal methods like LC-MS/MS. Future directions will be shaped by advanced antibody engineering, the integration of AI and machine learning for predicting interference, and the development of sophisticated multiplexed systems that transform cross-reactivity from a liability into a source of rich, multi-analyte information. For researchers and drug developers, mastering these principles is essential for generating reliable, high-quality data that accelerates discovery and ensures patient safety.
References
- 1. cross-reactivity in immunoassays - CANDOR Bioscience [https://www.candor-bioscience.de/en/immunoassays/glossary/interference/cross-reactivity/]
- 2. Cross-reactivity - Wikipedia [https://en.wikipedia.org/wiki/Cross-reactivity]
- 3. Cross-Reactivity Assessment [https://www.creative-diagnostics.com/protein-array/cross-reactivity-assessment.html]
- 4. Cross reactivity testing at Quansys Biosciences [https://www.quansysbio.com/support/cross-reactivity-testing/]
- 5. An Introduction To Immunoassay Interference | Blog [https://www.biosynth.com/blog/immunoassay-interference]
- 6. Solutions to immunoassay interference, cross reactivity and ... [https://www.gyrosproteintechnologies.com/spinblog/immunoassay-interference-crossreactivity-challenges]
- 7. Changing Cross-Reactivity for Different Immunoassays ... [https://www.mdpi.com/2076-3417/11/14/6581]
- 8. Cross-Reactivity - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/immunology-and-microbiology/cross-reactivity]
- 9. How do I know if the antibody will cross-react? [https://www.ptglab.com/news/blog/how-do-i-know-if-the-antibody-will-cross-react/?srsltid=AfmBOooNaaLaQ3SVpTgqLxOLtAAXqQNZQitoaddJJVtgKnC2_cUPtLEq]
- 10. pMHC Structural Comparisons as a Pivotal Element to Detect and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6952977/]
- 11. Antigen structure and recognition | Immunobiology Class... | Fiveable [https://fiveable.me/immunobiology/unit-3/antigen-structure-recognition/study-guide/xDGHddEVT8ZoEvZB]
- 12. Interferences in Immunoassay - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC1904417/]
- 13. How to Detect and Solve Immunoassay Interference [https://myadlm.org/cln/articles/2015/october/how-to-detect-and-solve-immunoassay-interference]
- 14. CE-BLAST makes it possible to compute antigenic similarity for newly... [https://www.nature.com/articles/s41467-018-04171-2?error=cookies_not_supported]
- 15. in quantitative immunochemical... - Biochemia Medica Interferences [https://www.biochemia-medica.com/en/journal/19/1/10.11613/BM.2009.005/fullArticle]
- 16. Impact of including interferences crossreactivity on... metabolite [https://pubmed.ncbi.nlm.nih.gov/22846896/]
- 17. Immunoassay | Sources of Interference & their Effects [https://www.elgalabwater.com/blog/immunoassay]
- 18. Tips & Tricks | Immunoassay Protocols & Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/product-supporting/milliplex/tips-tricks-immunoassay-protocol-troubleshooting-advice?srsltid=AfmBOopSQwShR8ZYC1toVYsyXv3uoMrk7-DNbxdIavN4ZbYowolZ_gAi]
- 19. Discovering Cross-Reactivity in Urine Drug Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7055671/]
- 20. Immunoassay Cross-reactivity: The Important of Accurate ... [https://blog.averhealth.com/immunoassay-cross-reactivity-the-important-of-accurate-interpretation]
- 21. 临床免疫检验中的15大干扰因素,不知道怎么能行? [https://csmedlab.com/2022/06/02/%E4%B8%B4%E5%BA%8A%E5%85%8D%E7%96%AB%E6%A3%80%E9%AA%8C%E4%B8%AD%E7%9A%8415%E5%A4%A7%E5%B9%B2%E6%89%B0%E5%9B%A0%E7%B4%A0%EF%BC%8C%E4%B8%8D%E7%9F%A5%E9%81%93%E6%80%8E%E4%B9%88%E8%83%BD%E8%A1%8C%EF%BC%9F/]
- 22. Navigating cross-reactivity and host species effects in a ... [https://pubmed.ncbi.nlm.nih.gov/39365836/]
- 23. Navigating cross-reactivity and host species effects in a ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0012042]
- 24. Computational identification of cross-reactive TCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579651/]
- 25. Comprehensive normalization and binary classification ... [https://www.sciencedirect.com/science/article/abs/pii/S0022175925000262]
- 26. Hormone Immunoassay Interference: A 2021 Update - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8368230/]
- 27. Cross-reactivity of steroid hormone immunoassays [https://bmcclinpathol.biomedcentral.com/articles/10.1186/1472-6890-14-33]
- 28. Spurious Serum Hormone Immunoassay Results [https://touchendocrinology.com/general-endocrinology/journal-articles/spurious-serum-hormone-immunoassay-results-causes-recognition-management/]
- 29. Steroid Assays and Endocrinology: Best Practices for Basic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4020931/]
- 30. Leveraging mass spectrometry for pediatric endocrine ... [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/pediatric-endocrine-disorders-mass-spectrometry.html]
- 31. The Importance of IC50 Determination [https://visikol.com/blog/2022/06/07/the-importance-of-ic50-determination/]
- 32. The specificity of cross-reactivity: Promiscuous antibody ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2366915/]
- 33. Monoclonal vs. Polyclonal Antibodies [https://www.thermofisher.com/us/en/home/life-science/antibodies/primary-antibodies/monoclonal-vs-polyclonal-antibodies.html]
- 34. Demystified …: Monoclonal antibodies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1186915/]
- 35. Polyclonal vs. monoclonal antibodies [https://www.ptglab.com/news/blog/polyclonal-vs-monoclonal-antibodies/?srsltid=AfmBOorMOCiYj0KF8RGdQwaj9ZC6SGttgD0Cw8T55dal0aE7x6ta6r-u]
- 36. monoclonal vs polyclonal antibodies, how to choose [https://www.bosterbio.com/blog/post/monoclonal-vs-polyclonal-antibodies-how-to-choose?srsltid=AfmBOooy4lpF6DEKcEqf12ooR5gsLg4qRhGn9HCYZTb4Q5CbuPFiVjDr]
- 37. How do I know if the antibody will cross-react? [https://www.ptglab.com/news/blog/how-do-i-know-if-the-antibody-will-cross-react/?srsltid=AfmBOoqAKM6olvryo0nqBnCYz9PUBH0OPYrIg81c5STsLWz49gQmAl8V]
- 38. Specificity and Cross-Reactivity - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK2396/]
- 39. Troubleshooting common problems during ELISA ... [https://www.mybiosource.com/learn/troubleshooting-common-problems-during-elisa-experiments/]
- 40. Types Of Immunoassay - And When To Use Them [https://www.quanterix.com/immunoassay-technologies-past-present-and-future/]
- 41. Immunoassay Methods - Assay Guidance Manual - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK92434/]
- 42. Redefining antibody cross-reactivity as an advantage for ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779925001829]
- 43. Machine learning-supported sensor array for multiplexed ... [https://www.sciencedirect.com/science/article/abs/pii/S0924224424004631]
- 44. Antibody-Based Protein Multiplex Platforms - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2901849/]
- 45. Multiplex Immunoassay Protocol [https://www.creative-diagnostics.com/multiplex-immunoassay-protocol.htm]
- 46. Multiplexed Immunosensors and Immunoarrays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7202053/]
- 47. Can immunoassays help detect novel psychoactive ... [https://myadlm.org/science-and-research/scientific-shorts/2025/can-immunoassays-help-detect-novel-psychoactive-substances]
- 48. A Difficult Challenge for the Clinical Laboratory: Accessing ... [https://www.sciencedirect.com/science/article/pii/S2374289521003274]
- 49. The Scientific Advances in Psychoactives Versus Artifacts ... [https://www.mdpi.com/2813-1851/4/2/12]
- 50. Modern drug testing in clinical laboratories: a narrative review ... [https://jlpm.amegroups.org/article/view/10561/html]
- 51. ELISA 故障排除指南 [https://stressmarq.cn.com/%E4%BA%A7%E5%93%81%E6%94%AF%E6%8C%81/%E6%8A%80%E6%9C%AF%E6%94%AF%E6%8C%81/%E6%95%85%E9%9A%9C%E6%8E%92%E9%99%A4%E6%8C%87%E5%8D%97/elisa-%E6%95%85%E9%9A%9C%E6%8E%92%E9%99%A4%E6%8C%87%E5%8D%97/]
- 52. 侧向免疫层析开发方案(很实用) [https://virion-serion.net/2023/06/28/3ac2a9e8b5/]
- 53. 成功的免疫荧光法:抗体稀释度和孵育条件 - CST 博客 [https://blog.cellsignal.cn/successful-immunofluorescence-antibody-dilution-and-incubation]
- 54. ELISA故障排除- Berthold Technologies GmbH & Co.KG [https://www.berthold.cn/bioanalytic/applications/elisa/troubleshooting/]
- 55. 新冠病毒抗RBD 免疫球蛋白水平的预测价值 [https://www.ebiotrade.com/newsf/2025-4/20250410072226097.htm]
- 56. Duolink® PLA故障排除指南 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/protein-biology/protein-and-nucleic-acid-interactions/duolink-troubleshooting-guide?srsltid=AfmBOopwKwJvFGlBjB_1Z1X4tBPGsPc2z0bWXZvk0SQTJItm4Y2pIzn3]
- 57. Optimizing Ligand Binding Assay Conditions for Accurate ... [https://swordbio.com/blog/optimizing-ligand-binding-assay-conditions-for-accurate-and-reproducible-results/]
- 58. Improving Specificity in your Immunoassay [https://shop.surmodics.com/improving-specificity-in-your-immunoassay]
- 59. Improved immunoassay sensitivity and specificity using ... [https://www.nature.com/articles/s41467-022-32796-x]
- 60. What is Matrix Interference and How Does It Affect Testing? [https://www.arborassays.com/what-is-matrix-interference/?srsltid=AfmBOork2mcOzwSf9GNaQNnGA7C9bN1fAK0JYQTCAh6i23XJcEbtesMR]
- 61. Overcoming target interference in bridging anti-drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413034/]
- 62. Comparative evaluation of four new immunoassays and LC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205834/]
- 63. Investigation of the matrix effects on structural stability and ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625024999]
- 64. Antigen excess in modern immunoassays: To anticipate on ... [https://www.sciencedirect.com/science/article/abs/pii/S1568997214002390]
- 65. Diagnosis and Discussion - Case 864 | Department of Pathology [https://www.path.pitt.edu/diagnosis-and-discussion-case-864]
- 66. Retrospective Approach to Evaluate Interferences in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5655638/]
- 67. What are Some Potential Errors that can Occur in an ELISA? [https://shop.surmodics.com/elisa-test-results-troubleshooting]
- 68. What Causes High Background in ELISA Tests? [https://shop.surmodics.com/elisa-test-results-high-background-causes]
- 69. ELISA Troubleshooting Guide [https://www.bio-techne.com/resources/protocols-troubleshooting/elisa-troubleshooting]
- 70. ELISA Assay Challenges | MyBioSource Learning Center [https://www.mybiosource.com/learn/troubleshooting-elisa-assay-challenges]
- 71. ELISA Kit Validation and Quality Testing [https://www.thermofisher.com/us/en/home/life-science/antibodies/immunoassays/elisa-kits/elisa-kit-validation-quality-testing.html]
- 72. Recommendations for the design and optimization of ... [https://www.sciencedirect.com/science/article/abs/pii/S0022175904001978]
- 73. Immunoassay Selection and Optimization Advice [https://www.bio-techne.com/applications/immunoassays/immunoassay-expert-advice]
- 74. Allergens in Food: Analytical LC-MS/MS Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428185/]
- 75. How to Read LC-MS Chromatograms [https://www.news-medical.net/life-sciences/How-to-Read-LC-MS-Chromatograms.aspx]
- 76. LC-MS Data Processing with MAVEN: A Metabolomic Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055029/]
- 77. 常见的挑战多重免疫组织化学 [https://www.celnovte.com/zh-CN/solution/overcoming-challenges-in-multiplex-immunohistochemistry-experiments-common-challenges-in-multiplex-immunohistochemistry/]
- 78. IHC常见染色问题和解决方法 [https://www.biolabreagent.com/archive/1377.html?srsltid=AfmBOooRu8ExYQAk-Epbp6pZ-lWkrb6eRlhI-cLyvydcmlzD49W3pbGQ]
- 79. IHC实验常见问题及解决方案- 武汉菲恩生物科技有限公司 [https://www.fn-test.cn/faqs/common-problems-and-solutions-of-ihc-experiment/]
- 80. 免疫分析:相同的抗体不同的交叉反应率 [https://www.antiby.com/hynews-861.html]
- 81. 重磅新品| Fc沉默流抗:FcZero-rAb™新型骨架流式抗体正式 ... [https://www.ptgcn.com/news/blog/fczero-rab-launched-fc-receptor-blocking-free-flow-antibodies-with-innovative-scaffold-design/]
- 82. Antibody Colocalization Microarray: A Scalable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3322566/]
- 83. Cross-reactivity in antibody microarrays and multiplexed ... [https://www.sciencedirect.com/science/article/abs/pii/S1367593113002317]
- 84. Luminex HP Assays: Overcoming Multiplexing Challenges [https://www.rndsystems.com/blog/luminex-hp-assays-101-overcoming-multiplexing-challenges]
- 85. MILLIPLEX® Multiplex Assays FAQs [https://www.sigmaaldrich.com/US/en/technical-documents/product-supporting/milliplex/milliplex-multiplex-assays-faqs?srsltid=AfmBOoqspEb2A-T2JrWiXJhK768COe-gBMT9N4VasUv2sPQYjQKqQxGc]
- 86. ProcartaPlex Assays Support – Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/antibodies-immunoassays-support-center/luminex-assays-support/luminex-assays-support-troubleshooting.html]
- 87. Evaluating Cross-Reactivity in Custom-Made Multiplex ... [https://pubmed.ncbi.nlm.nih.gov/40601146/]
- 88. Multiplex Immunoassay for Biomarker Research [https://olink.com/blog/multiplex-immunoassay-for-biomarker-research]
- 89. Cross-reactivity of steroid hormone immunoassays [https://pmc.ncbi.nlm.nih.gov/articles/PMC4112981/]
- 90. Increased serologic reactivity with automated CMIA testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417225/]
- 91. Mandatory Guidelines for Federal Workplace Drug Testing ... [https://www.federalregister.gov/documents/2025/01/16/2025-00425/mandatory-guidelines-for-federal-workplace-drug-testing-programs-authorized-testing-panels]
- 92. Defensible Clinical Testing Results: Boost Your Patient Trust [https://keystonelab.com/uncategorized/defensible-clinical-testing-results/]
- 93. Next-generation immunoassays for diagnosis [https://www.nature.com/articles/d42473-024-00342-6]