Commercial vs. In-House PCR for Protozoa Detection: A 2025 Guide for Diagnostics and Research
This article provides a comprehensive analysis for researchers and diagnostics professionals evaluating commercial and in-house PCR assays for protozoan detection.
Commercial vs. In-House PCR for Protozoa Detection: A 2025 Guide for Diagnostics and Research
Abstract
This article provides a comprehensive analysis for researchers and diagnostics professionals evaluating commercial and in-house PCR assays for protozoan detection. Covering foundational principles, methodological applications, and troubleshooting, it synthesizes recent multicentre study data to compare performance, cost, and standardization. The analysis highlights critical factors for assay selection, including sensitivity for Giardia duodenalis and Cryptosporidium spp., challenges in DNA extraction, and the impact of sample preservation. Future directions in digital PCR and standardized protocols are discussed to guide implementation in clinical and research settings targeting intestinal protozoa and other parasitic infections.
The Protozoa Diagnostic Landscape: Why PCR is Replacing Traditional Methods
The Global Burden of Pathogenic Intestinal Protozoa
Pathogenic intestinal protozoa represent a significant and persistent global health challenge, particularly in resource-limited settings. These parasites, including Giardia duodenalis, Entamoeba histolytica, and Cryptosporidium spp., are among the leading etiological agents of diarrheal diseases worldwide [1]. Recent systematic reviews estimate that intestinal protozoan parasites affect approximately 3.5 billion people globally, causing approximately 1.7 billion episodes of diarrheal disorders annually [1] [2]. Among these pathogens, Cryptosporidium alone causes an estimated 200,000 deaths annually, with the highest burden in sub-Saharan Africa and South Asia [3]. The global prevalence of protozoan pathogens in diarrheal cases is estimated at 7.5%, with the highest rates observed in the Americas and Africa [3].
The diagnosis of these infections poses formidable challenges for clinicians and researchers alike. Microscopic examination of stool samples remains the reference method in many clinical laboratories, particularly in endemic areas with high parasitic prevalence but limited resources [1]. However, this method suffers from significant limitations in sensitivity and specificity and requires highly qualified personnel [1] [4]. Molecular diagnostic technologies, particularly real-time PCR (RT-PCR), are increasingly gaining traction in non-endemic areas characterized by low parasitic prevalence due to their enhanced sensitivity and specificity [1] [4]. This review comprehensively compares commercial and in-house PCR methodologies for protozoa detection, providing researchers with experimental data and protocols to inform their diagnostic strategies.
Comparative Performance of Molecular Diagnostic Platforms
The evolution of diagnostic techniques for intestinal protozoa has progressed from traditional microscopy to advanced molecular methods. Microscopy, while cost-effective and widely available, has limited sensitivity and specificity and cannot differentiate between morphologically identical species, such as pathogenic E. histolytica and non-pathogenic E. dispar [1]. Immunodiagnostic methods like enzyme-linked immunosorbent assay (ELISA) and immunochromatography offer rapid screening capabilities but may yield elevated rates of false positives and negatives [1]. Molecular approaches, particularly RT-PCR, provide superior sensitivity and specificity, with the additional advantage of differentiating between species based on genetic markers [1] [4].
Recent multicenter studies have directly compared the performance of commercial and in-house PCR assays against traditional microscopy and each other. These comparisons are essential for laboratories seeking to implement molecular diagnostics, as they provide critical data on test reliability, cost-effectiveness, and technical requirements [1] [4] [5].
Performance Metrics for Major Pathogenic Protozoa
A 2025 multicenter study involving 18 Italian laboratories provided comprehensive performance data for both commercial and in-house RT-PCR assays compared to conventional microscopy [1] [6] [4]. The study analyzed 355 stool samples (230 freshly collected and 125 preserved in media) for infections with Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis [4].
Table 1: Performance comparison of molecular detection methods for intestinal protozoa
| Parasite | Method | Sensitivity (%) | Specificity (%) | Sample Type Considerations |
|---|---|---|---|---|
| G. duodenalis | AusDiagnostics Kit | 91.0 | 98.9 | Performs well on both fresh and preserved samples |
| In-house RT-PCR | 93.3 | 97.0 | Consistent performance across sample types | |
| Cryptosporidium spp. | AusDiagnostics Kit | 78.9 | 99.1 | Sensitivity limitations due to DNA extraction issues |
| In-house RT-PCR | 78.9 | 100 | Same sensitivity limitations as commercial kit | |
| D. fragilis | AusDiagnostics Kit | 68.4 | 91.9 | Inconsistent detection across platforms |
| In-house RT-PCR | 68.4 | 88.9 | Similar consistency issues as commercial kit | |
| E. histolytica | Molecular Methods | Critical for accurate diagnosis | High specificity reported | Microscopy cannot differentiate from non-pathogenic species |
The data reveal several important patterns. First, both commercial and in-house methods demonstrated excellent performance for Giardia duodenalis detection, with high sensitivity and specificity [6]. Second, preserved stool samples generally yielded better PCR results than fresh samples, likely due to better DNA preservation [4]. Third, both platforms showed limited sensitivity for Cryptosporidium spp. and D. fragilis, attributed to inadequate DNA extraction from these particular parasites [4]. Finally, molecular assays proved critical for accurate diagnosis of E. histolytica, which cannot be differentiated from non-pathogenic species using conventional microscopy [1].
A separate 2020 study compared one in-house and three commercial qPCR kits for 15 parasites and microsporidia, analyzing 500 DNA samples from patients with high likelihood of parasitic infections [5]. The results showed varying inter-assay agreement across different parasites, ranging from "almost perfect" (κ = 0.81-1.00) for Dientamoeba fragilis and Cryptosporidium spp. to "substantial" (κ = 0.61-0.80) for Giardia duodenalis and "slight" (κ = 0-0.20) for Cyclospora spp. and Strongyloides stercoralis [5]. This variability highlights the importance of platform selection based on the target parasites of interest.
Impact of Technical Factors on Detection Performance
The efficacy of molecular methods depends critically on the specific protocols employed at each stage of the diagnostic process. A comprehensive study evaluating 30 distinct protocol combinations for Cryptosporidium parvum detection demonstrated that different combinations of pre-treatment, extraction, and amplification methods yielded significantly varying results [7]. The optimal approach for detecting C. parvum DNA combined mechanical pre-treatment, the Nuclisens Easymag extraction method, and the FTD Stool Parasite DNA amplification method, which achieved 100% detection efficiency [7].
Table 2: Key technical factors influencing molecular detection performance
| Process Stage | Considerations | Impact on Results |
|---|---|---|
| Sample Collection & Storage | Fresh vs. preserved samples; preservation media | Preserved samples generally yield better DNA quality and more consistent PCR results [4] |
| DNA Extraction | Manual vs. automated methods; kit selection | Critical step affecting sensitivity; inadequate extraction particularly impacts Cryptosporidium and D. fragilis detection [7] [4] |
| Amplification Target | Single-copy vs. multi-copy genes; nuclear vs. mitochondrial DNA | Multi-copy targets (e.g., kinetoplast DNA) increase sensitivity; combining targets minimizes false negatives [8] |
| Inhibition Control | Internal extraction controls; inhibition monitoring | Essential for distinguishing true negatives from false negatives due to PCR inhibitors in stool samples [1] |
The complex wall structure of protozoan parasites presents particular challenges for DNA extraction. The robust oocyst walls of Cryptosporidium species require specialized disruption methods to release amplifiable DNA [1] [7]. This technical hurdle likely contributes to the lower sensitivity observed for Cryptosporidium detection across both commercial and in-house platforms [4].
Experimental Protocols for Molecular Detection
Standardized Workflow for Molecular Detection
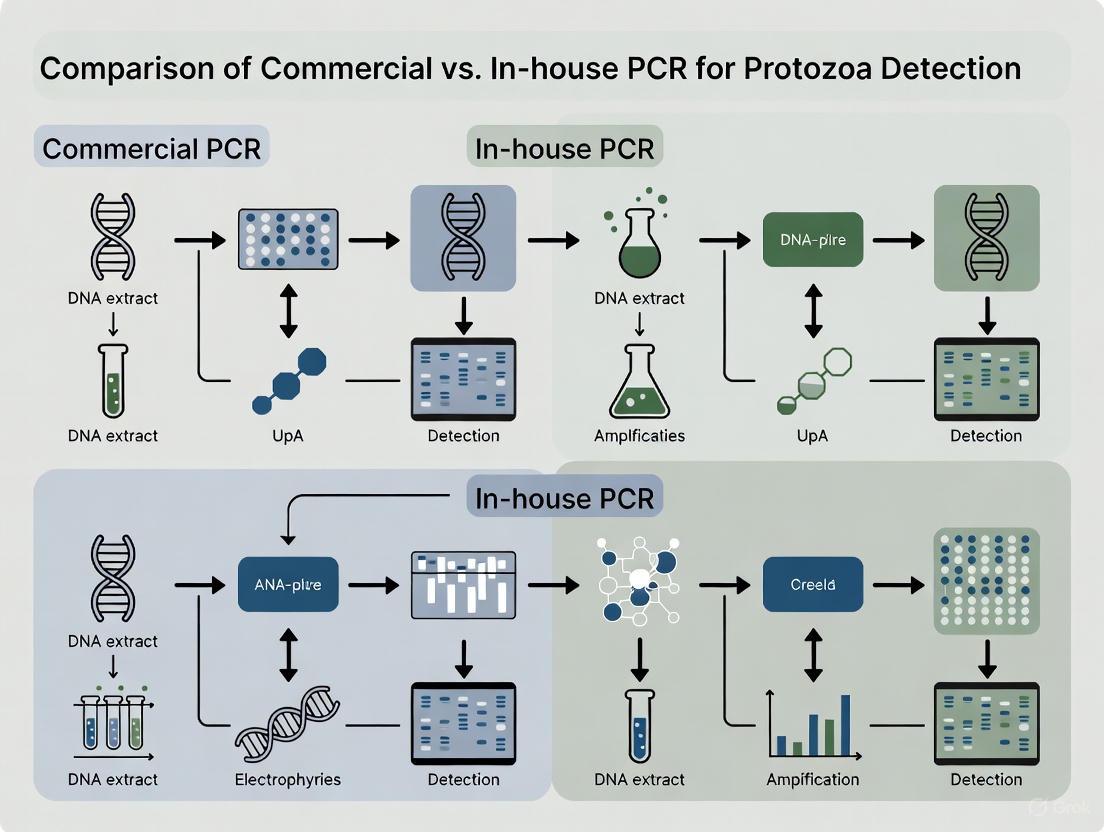
The molecular detection of intestinal protozoa follows a standardized workflow encompassing sample preparation, nucleic acid extraction, and amplification/detection. The following diagram illustrates the critical decision points in this process:
Sample Preparation and DNA Extraction
The sample preparation and DNA extraction phase is arguably the most critical determinant of success in protozoan detection. In the multicenter Italian study, approximately 1μl of each fecal sample was mixed with 350μl of S.T.A.R (Stool Transport and Recovery Buffer; Roche Applied Sciences, Basel, Switzerland) using a sterile loop and incubated for 5 minutes at room temperature [1]. After centrifugation at 2000 rpm for 2 minutes, 250μl of supernatant was carefully collected and combined with 50μl of internal extraction control [1]. DNA extraction was then performed using the MagNA Pure 96 DNA and Viral NA Small Volume Kit on the MagNA Pure 96 System (Roche Applied Sciences), representing a fully automated nucleic acid preparation based on magnetic separation of nucleic acid-bead complexes [1].
For the in-house PCR protocol, each reaction mixture included 5μl of MagNA extraction suspension, 12.5μl of 2× TaqMan Fast Universal PCR Master Mix (Thermo Fisher Scientific, Waltham, MA, USA), 2.5μl of primers and probe mix, and sterile water to a final volume of 25μl [1]. A multiplex tandem PCR assay was then performed using appropriate cycling conditions [1].
Emerging Detection Technologies
Beyond conventional PCR, emerging technologies show promise for protozoan detection. Microfluidic Impedance Cytometry (MIC) has been used to characterize the AC electrical (impedance) properties of single parasites, demonstrating rapid discrimination based on viability and species [9]. This technology achieved over 90% certainty in identifying live and inactive C. parvum oocysts and over 92% certainty in discriminating between Cryptosporidium parvum, Cryptosporidium muris, and Giardia lamblia [9]. MIC offers a label-free approach that requires minimal sample processing and can measure up to 1000 particles per second, significantly reducing identification time and labor demands compared to existing methods [9].
The Scientist's Toolkit: Essential Research Reagents
Successful detection and analysis of pathogenic intestinal protozoa requires carefully selected reagents and platforms. The following table details key research solutions and their applications in protozoan research:
Table 3: Essential research reagents and platforms for protozoan detection
| Reagent/Platform | Manufacturer/Distributor | Application & Function |
|---|---|---|
| MagNA Pure 96 System | Roche Applied Sciences | Automated nucleic acid extraction using magnetic bead technology [1] |
| S.T.A.R Buffer | Roche Applied Sciences | Stool Transport and Recovery Buffer for sample stabilization [1] |
| TaqMan Fast Universal PCR Master Mix | Thermo Fisher Scientific | Ready-to-use reaction mix for fast real-time PCR amplification [1] |
| AusDiagnostics PCR Kit | AusDiagnostics Company (R-Biopharm Group) | Commercial multiplex PCR test for intestinal protozoa detection [1] [4] |
| Para-Pak Preservation Media | Meridian Bioscience | Stool preservative for maintaining parasite DNA integrity during transport and storage [4] |
| FTD Stool Parasite DNA Amplification | Fast-Track Diagnostics | PCR-based detection method showing high efficiency for C. parvum [7] |
| Nuclisens Easymag | bioMérieux | Nucleic acid extraction system optimal for Cryptosporidium detection [7] |
The global burden of pathogenic intestinal protozoa remains significant, with billions of people affected worldwide. Molecular diagnostic methods, particularly RT-PCR, have revolutionized detection capabilities for these pathogens, offering superior sensitivity and specificity compared to traditional microscopy. Both commercial and in-house PCR platforms demonstrate excellent performance for detecting Giardia duodenalis, with sensitivity exceeding 90% for both platforms [6]. However, detection challenges persist for Cryptosporidium spp. and D. fragilis, primarily due to difficulties in DNA extraction from these organisms [4].
The choice between commercial and in-house molecular methods involves careful consideration of several factors. Commercial kits offer standardization and convenience, while in-house methods provide flexibility and potential cost savings for high-volume laboratories. Regardless of the platform selected, sample processing methods—particularly DNA extraction—critically impact detection sensitivity and must be optimized for the target pathogens [7]. Future directions in protozoan diagnostics include the refinement of automated platforms, the development of point-of-care molecular tests, and the implementation of new technologies like microfluidic impedance cytometry for rapid analysis [9]. As these technologies evolve, they promise to enhance our understanding of the global epidemiology of intestinal protozoa and improve control strategies for these significant pathogens.
For over a century, conventional light microscopy has served as the cornerstone of pathological diagnosis and parasitological identification. Despite its longstanding role as a reference method in many clinical laboratories, this technique faces significant challenges in modern diagnostic and research contexts, particularly when compared with emerging molecular technologies. Within the framework of comparing commercial versus in-house PCR for protozoa research, understanding these limitations becomes paramount for researchers aiming to optimize diagnostic accuracy, efficiency, and cost-effectiveness. This guide provides a comprehensive, evidence-based comparison between conventional microscopy and molecular methods, focusing on their performance characteristics and practical applications in protozoa research.
Analytical Limitations: Sensitivity and Specificity
The diagnostic performance of conventional microscopy is fundamentally constrained by limitations in sensitivity and specificity, which become particularly evident when compared to molecular techniques like PCR.
Table 1: Comparative Diagnostic Performance of Microscopy vs. PCR
| Parasite/Context | Microscopy Sensitivity | PCR Sensitivity | Microscopy Specificity | PCR Specificity | Study Reference |
|---|---|---|---|---|---|
| Soil-transmitted helminths (overall) | 22.4% | Reference | 94.3% | Reference | [10] |
| Ascaris lumbricoides | 33.3% | Reference | 97.3% | Reference | [10] |
| Necator americanus | 17.5% | Reference | 99.2% | Reference | [10] |
| Intestinal protozoa (multiplex PCR) | 28.75%* | 27.9%* | Limited differentiation | 100% concordance with sequencing | [11] |
| Entamoeba histolytica | Cannot differentiate from non-pathogenic species | Species-specific identification | Limited | High | [12] [13] |
*Percentage positive in patient samples; microscopy and PCR showed moderate to almost perfect agreement depending on parasite species [11].
Microscopy's limited sensitivity is especially problematic in low-prevalence settings or cases with low parasite burden, where the technique may fail to detect infections altogether. A study on soil-transmitted helminths demonstrated concerningly low sensitivity of just 22.4% for microscopy compared to PCR [10]. This deficiency stems from several factors: the intermittent shedding of parasites in stools, non-uniform distribution of parasites in samples, and low infection intensities that fall below microscopy's detection threshold [10] [13].
Regarding specificity, conventional microscopy struggles significantly with species differentiation, particularly for morphologically similar organisms. Crucially, microscopy cannot differentiate pathogenic Entamoeba histolytica from non-pathogenic Entamoeba dispar and Entamoeba moshkovskii, a distinction critical for appropriate treatment decisions [12] [11] [13]. This limitation necessitates additional testing or leads to potential misdiagnosis and unnecessary treatments.
Expertise Dependency and Operational Challenges
The reliability of conventional microscopy is exceptionally dependent on operator expertise, introducing substantial variability in diagnostic outcomes across different settings and practitioners.
Table 2: Operational Challenges of Conventional Microscopy
| Challenge Category | Specific Limitations | Impact on Diagnostics/Research |
|---|---|---|
| Expertise Dependency | Requires skilled microscopists for accurate identification [12] [10] | High inter-observer variability; limited to specialized personnel |
| Workflow Efficiency | Time-consuming manual process [13]; requires examination of multiple samples [10] [11] | Increased turnaround time; resource intensive |
| Identification Limitations | Subjective interpretation [14]; inability to differentiate morphologically similar species [12] [13] | Misidentification risk; compromised specificity |
| Data Management | No permanent digital record [15]; difficult retrospective reviews | Limited quality assurance; challenging for research comparisons |
The expertise requirement presents a significant barrier in many settings, as accurately differentiating parasites from artifacts and distinguishing between similar species demands substantial training and experience [12] [10]. This subjectivity introduces inter-observer variability that compromises the consistency and reliability of microscopic diagnosis [14] [13].
Operationally, conventional microscopy remains labor-intensive and time-consuming. The standard protocol requiring examination of three stool samples collected on alternate days creates logistical challenges for both patients and laboratories [10] [13]. This multi-sample requirement increases workload, extends turnaround times, and adds to overall diagnostic costs despite the apparent low per-test cost of microscopy itself.
Comparative Workflow Analysis: Microscopy vs. Molecular Methods
Comparative Methodologies: Experimental Protocols
Understanding the experimental protocols for both conventional microscopy and PCR methods is essential for evaluating their comparative advantages and limitations in research settings.
Conventional Microscopy Protocol
The standard microscopic examination typically follows this protocol:
- Sample Collection: Multiple stool samples (typically three) collected on alternate days to account for intermittent parasite shedding [13].
- Specimen Preparation: Fresh stool samples are stained with Giemsa, while fixed samples are processed using formalin-ethyl acetate (FEA) concentration techniques [12].
- Microscopic Examination: Prepared slides are examined under light microscopy at various magnifications (typically 10x, 40x) [15].
- Identification: Based on morphological characteristics of trophozoites, cysts, oocysts, or helminth eggs [12] [13].
This process remains labor-intensive, requiring approximately 15-30 minutes of expert technician time per sample, with sensitivity highly dependent on parasite load and examiner expertise [12] [10].
PCR-Based Detection Protocol
Molecular methods offer a standardized alternative with the following general protocol:
- DNA Extraction:
- PCR Amplification:
- Detection: Real-time PCR systems (e.g., ABI 7900HT, CFX 96) monitor amplification fluorescence [12] [13].
Multiplex PCR formats enable simultaneous detection of multiple pathogens (e.g., Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica) in a single reaction, significantly improving workflow efficiency [11].
The Researcher's Toolkit: Essential Reagent Solutions
Implementing either conventional or molecular diagnostic approaches requires specific reagents and equipment with distinct functional considerations.
Table 3: Essential Research Reagents and Materials
| Reagent/Equipment | Function/Purpose | Application Context |
|---|---|---|
| Formalin-Ethyl Acetate (FEA) | Stool sample preservation and concentration | Conventional microscopy [12] |
| Giemsa Stain | Visual enhancement of parasitic structures | Microscopic identification [12] |
| S.T.A.R. Buffer | Stool transport, recovery, and DNA stabilization | Molecular diagnostics/DNA extraction [12] |
| Polyvinylpolypyrrolidone (PvPP) | PCR inhibitor removal | DNA purification for PCR [13] |
| DNA Isolation Kits | Nucleic acid extraction and purification | PCR-based detection [12] [13] |
| TaqMan Master Mix | PCR reaction components | Real-time PCR amplification [12] |
| Specific Primers/Probes | Target DNA sequence recognition | Pathogen-specific detection [12] [13] |
| Internal Extraction Controls | Process efficiency monitoring | Quality control in molecular assays [12] [13] |
Transition to Digital and Molecular Solutions
The limitations of conventional microscopy have accelerated the adoption of digital pathology and molecular methods, which address many of these constraints while introducing new capabilities.
Digital pathology systems convert physical glass slides into high-resolution whole slide images (WSIs) that can be viewed, shared, and analyzed electronically [14] [15]. This digital transformation enables:
- Remote consultations and collaborations across geographical boundaries [15]
- Integration with AI-based tools for automated image analysis, reducing subjectivity [14]
- Improved workflow efficiency with reported turnaround time reductions of 3.72 days in one implementation study [16]
- Permanent digital archives for retrospective reviews and quality assurance [15]
Molecular methods, particularly PCR-based approaches, offer paradigm-shifting advantages for protozoa research:
- Single-sample requirement compared to multiple samples for microscopy [13]
- Superior sensitivity and specificity, especially in low-prevalence settings [10]
- Species-specific differentiation of morphologically identical organisms [12] [13]
- Standardization potential across laboratories and settings [12] [11]
The transition to these advanced methodologies represents a fundamental shift from subjective, expertise-dependent morphological assessment toward objective, standardized molecular detection that offers greater consistency, accuracy, and efficiency for research applications.
Conventional microscopy faces substantial limitations in sensitivity, specificity, and expertise dependency that constrain its effectiveness in modern protozoa research and diagnostics. While it remains a valuable tool for initial screening and in resource-limited settings, the evidence clearly demonstrates the superiority of molecular methods for accurate pathogen detection, species differentiation, and research standardization. The integration of digital pathology platforms and PCR-based detection represents the future of parasitological diagnosis, offering researchers enhanced capabilities for precise, efficient, and reproducible protozoa identification. As the field continues to evolve, the complementary use of these technologies—leveraging their respective strengths—will likely provide the most comprehensive approach for advancing protozoa research and improving diagnostic outcomes.
The diagnosis of parasitic infections has undergone a remarkable transformation, shifting from traditional reliance on microscopy and serological assays toward sophisticated molecular technologies. This evolution reflects an ongoing pursuit of greater diagnostic accuracy, specificity, and efficiency in both clinical and research settings. Enzyme-Linked Immunosorbent Assay (ELISA) long served as a cornerstone serological technique, providing a pragmatic bridge from microscopic methods to more standardized testing. However, the emergence of real-time Polymerase Chain Reaction (PCR) technologies has redefined diagnostic possibilities, offering unprecedented sensitivity and specificity for pathogen detection. Within molecular diagnostics itself, a significant debate continues regarding the relative merits of commercial PCR kits versus in-house laboratory-developed tests, each presenting distinct advantages in standardization, customization, cost, and performance. This guide objectively compares these diagnostic approaches, providing researchers and scientists with experimental data and protocols to inform their methodological selections for protozoan pathogen detection.
Methodological Comparison: ELISA vs. Real-Time PCR
Fundamental Principles and Workflows
ELISA operates on the principle of antigen-antibody recognition. In the context of parasitic diagnosis, plates are typically coated with parasite-specific antigens which bind to antibodies present in patient samples. This binding is then detected through enzyme-linked secondary antibodies that produce a measurable colorimetric signal [17]. The technique indirectly indicates infection by detecting the host's immune response, which can persist after successful treatment, potentially leading to false positives in treated individuals [17] [18].
In contrast, real-time PCR directly detects the genetic material of the parasite itself. This process involves the extraction of nucleic acids from clinical samples, followed by amplification of parasite-specific DNA sequences using target-specific primers and probes. The reaction enables both detection and quantification by monitoring fluorescence at each amplification cycle [17] [19]. This direct pathogen detection allows for differentiation between active and past infections, a significant advantage over serological methods.
Experimental Data and Performance Comparison
Recent studies provide robust quantitative comparisons between these methodologies. A 2024 study on human fascioliasis demonstrated that both ELISA and real-time PCR identified 44 out of 70 samples (62.86%) as positive for Fasciola hepatica, showing a high agreement of 94.4% (Cohen’s kappa ≥ 0.7) [17]. The study noted no cross-reactivity with other parasitic diseases in either test, confirming high specificity.
However, broader analyses reveal more nuanced performance differences. Research on intestinal protozoa found that molecular methods significantly outperform traditional techniques in sensitivity. One study reported that real-time PCR was positive in 72 of 98 samples (73.5%), whereas microscopic examination was positive in only 37 (37.7%) samples [19]. This enhanced sensitivity is particularly crucial for asymptomatic cases, where real-time PCR detected parasites in 57.4% (31/54) of samples compared to just 18.5% (10/54) by microscopy [19].
Table 1: Comparative Performance of Diagnostic Methods for Various Parasites
| Parasite | Diagnostic Method | Sensitivity | Specificity | Key Findings | Reference |
|---|---|---|---|---|---|
| Fasciola hepatica | ELISA vs. Real-Time PCR | 62.86% (both) | High (no cross-reactivity) | 94.4% agreement between tests | [17] |
| Gastrointestinal Parasites (Multiple) | Real-Time PCR vs. Microscopy | 73.5% vs. 37.7% | Not specified | Significant superiority in asymptomatic cases (57.4% vs. 18.5%) | [19] |
| Giardia duodenalis | Commercial vs. In-house PCR | Complete agreement | Complete agreement | High sensitivity and specificity for both methods | [1] [4] |
| Entamoeba histolytica | Molecular Assays | Critical for diagnosis | Critical for diagnosis | Essential for differentiation from non-pathogenic species | [1] [20] |
| Chronic Chagas Disease | ELISA | 97.7% | 96.3% | Remains primary diagnostic method | [18] |
| Chronic Chagas Disease | PCR | 50-90% | ~100% | Not recommended for primary diagnosis in chronic phase | [18] |
The critical advantage of molecular methods for specific differentiations is exemplified in amebiasis diagnosis. Microscopy cannot distinguish pathogenic Entamoeba histolytica from non-pathogenic Entamoeba dispar, whereas real-time PCR provides definitive identification, directly impacting clinical management [1] [20].
Figure 1: Comparative Workflows of ELISA and Real-Time PCR. The diagram illustrates the fundamental procedural differences between the two methods, highlighting ELISA's indirect detection of immune response versus real-time PCR's direct detection of pathogen DNA.
Commercial vs. In-House Real-Time PCR Assays
Performance and Agreement Across Platforms
The choice between commercial and in-house PCR tests represents a significant consideration for diagnostic laboratories and research institutions. A comprehensive 2020 test comparison evaluated one in-house real-time PCR platform and three commercial kits for 15 parasites and microsporidia, analyzing 250-500 nucleic acid extracts from stool samples [5]. The study employed Latent Class Analysis (LCA) to estimate performance without a perfect gold standard, revealing variable inter-assay agreement across different parasite targets.
Table 2: Inter-Assay Agreement Between Commercial and In-House PCR Tests for Selected Parasites
| Parasite | Inter-Assay Agreement (Kappa Value) | Agreement Level | Positive Results per 250 Samples (Range Across Assays) |
|---|---|---|---|
| Dientamoeba fragilis | 0.81 - 1 | Almost Perfect | 26 - 28 |
| Cryptosporidium spp. | 0.81 - 1 | Almost Perfect | 27 - 36 |
| Ascaris lumbricoides | 0.81 - 1 | Almost Perfect | 79 - 96 |
| Giardia duodenalis | 0.61 - 0.8 | Substantial | 184 - 205 |
| Blastocystis spp. | 0.61 - 0.8 | Substantial | 174 - 183 |
| Entamoeba histolytica | 0.41 - 0.6 | Moderate | 7 - 16 |
| Strongyloides stercoralis | 0 - 0.2 | Slight | 6 - 38 |
| Cyclospora spp. | 0 - 0.2 | Slight | 6 - 13 |
The data indicates that agreement was highest for Dientamoeba fragilis, Cryptosporidium spp., and Ascaris lumbricoides (almost perfect), and substantial for Giardia duodenalis and Blastocystis spp [5]. However, agreement was only moderate for Entamoeba histolytica and slight for Strongyloides stercoralis and Cyclospora spp., highlighting the diagnostic challenges posed by these parasites [5].
A 2025 multicentre study in Italy involving 18 laboratories further reinforced these findings, showing complete agreement between commercial (AusDiagnostics) and in-house PCR methods for detecting Giardia duodenalis [1] [4]. Both methods demonstrated high sensitivity and specificity comparable to microscopy. For Cryptosporidium spp. and D. fragilis, both platforms showed high specificity but variable sensitivity, potentially due to differences in DNA extraction efficiency from resistant oocysts and cysts [1].
Practical Considerations for Implementation
Beyond raw performance metrics, several practical factors influence the choice between commercial and in-house platforms:
- Standardization and Compliance: Commercial kits offer superior standardization, with the European Union Regulation (EU) 2017/746 increasingly requiring certified tests unless additional benefit of in-house testing can be demonstrated [5].
- Customization and Flexibility: In-house assays provide greater flexibility to adapt to specific research needs, local pathogen variants, or to include novel targets not available in commercial panels [5] [20].
- Cost Structure: Commercial kits involve higher per-test reagent costs but lower development and validation overhead. In-house tests require significant upfront investment in development and validation but may be more cost-effective for high-volume specialized testing [5].
- Sample Preparation: The efficiency of DNA extraction varies significantly between protocols and directly impacts sensitivity. The Italian multicentre study identified DNA extraction as a critical factor affecting sensitivity, particularly for parasites with robust wall structures like Cryptosporidium [1].
Detailed Experimental Protocols
Protocol for ELISA-Based Detection
The following protocol for detecting anti-Fasciola antibodies using excretory-secretory antigens (ESAg) exemplifies a standardized serological approach [17]:
- Antigen Preparation: Coat ELISA microplates with 1 µg/mL of F. hepatica ESAgs in 0.05 M carbonate-bicarbonate buffer (pH 9.6), 100 µL/well. Incubate overnight at 37°C.
- Washing and Blocking: Wash plates five times with PBST (PBS with 0.05% Tween 20). Block excess binding sites with 3% skimmed milk in PBST and incubate for 2 hours at 37°C.
- Sample Incubation: Add 100 µL of diluted patient serum (1:500 in PBST) to wells. Incubate at 37°C for 30 minutes, then wash plates.
- Conjugate Incubation: Add 100 µL of diluted anti-human IgG horseradish-peroxidase conjugate (1:12,000 in PBST) to each well. Incubate for 30 minutes at 37°C, then wash.
- Detection: Add 100 µL/well of OPD substrate solution (o-phenylenediamine dihydrochloride with 0.025% H₂O₂ in 0.1 M citrate buffer, pH 5.0). Incubate for 30 minutes at room temperature in the dark.
- Signal Measurement: Stop the reaction with 50 µL of 1 M sulfuric acid. Measure the optical density at 492 nm using a microplate reader. The cut-off is typically set as the mean OD of negative controls plus two standard deviations.
Protocol for Real-Time PCR Detection
A representative protocol for real-time PCR detection of Fasciola hepatica targets the ribosomal ITS1 sequence [17]:
- DNA Extraction: Extract DNA from serum or stool samples using a commercial genomic DNA kit. Incorporate modifications as needed for specific sample types, such as mechanical disruption with glass beads for stool samples [19].
- Reaction Setup: Prepare a reaction mix containing:
- 5 µL of extracted DNA
- 12.5 µL of 2× TaqMan Fast Universal PCR Master Mix
- 2.5 µL of primer-probe mix (targeting ITS1 or other specific sequences)
- Nuclease-free water to a final volume of 25 µL
- Amplification Parameters: Run the real-time PCR using cycling conditions optimized for the specific instrument and primers. A typical program includes:
- Initial denaturation: 95°C for 2-10 minutes
- 40-45 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 1 minute (with fluorescence acquisition)
- Inhibition Control: Include an internal control (exogenous synthetic oligonucleotide or amplification of a universal bacterial sequence) to detect potential PCR inhibition in each sample [19].
- Data Analysis: Determine positive results based on cycle threshold (Ct) values crossing a predetermined fluorescence threshold. Samples with Ct values >35 may show reduced reproducibility and require careful interpretation [20].
Figure 2: Decision Framework for Commercial vs. In-House PCR Platforms. This diagram outlines the key advantages and disadvantages of each approach to guide researchers in selecting the most appropriate platform for their specific needs.
Essential Research Reagent Solutions
Successful implementation of parasitic diagnostics requires careful selection of core reagents and materials. The following table details key solutions used in the featured experiments.
Table 3: Key Research Reagent Solutions for Parasite Diagnosis
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Excretory-Secretory Antigens (ESAg) | Coating antigen for ELISA; captures specific antibodies from patient samples. | Prepared from adult F. hepatica worms cultured in RPMI 1640 medium [17]. |
| Microplates | Solid phase for ELISA reactions. | ELISA microplates (e.g., Nunc, Roskilde, Denmark) [17]. |
| Enzyme-Conjugated Antibodies | Detection antibodies that generate measurable signal in ELISA. | Anti-human IgG horseradish-peroxidase conjugate [17]. |
| DNA Extraction Kits | Isolation of high-quality nucleic acids from diverse clinical samples. | Commercial kits (e.g., QIamp DNA Stool Mini Kit, DNG-PLUS); mechanical disruption with glass beads improves yield [17] [19]. |
| PCR Master Mix | Provides optimal environment for DNA amplification; includes enzymes, dNTPs, buffer. | 2× TaqMan Fast Universal PCR Master Mix [1] [20]. |
| Specific Primers & Probes | Target parasite-specific DNA sequences for amplification and detection. | Hydrolysis probes (TaqMan) targeting ribosomal ITS1 (Fasciola), SSU rRNA (Entamoeba, Strongyloides), or other specific genes [17] [19] [20]. |
| Internal Controls | Monitor extraction efficiency and detect PCR inhibition. | Exogenous synthetic oligonucleotides or amplification of universal bacterial sequences [19]. |
The evolution from ELISA to real-time PCR represents a paradigm shift in parasitic disease diagnosis, moving from indirect serological assessment to direct, sensitive pathogen detection. While ELISA remains a valuable tool for seroprevalence studies and in resource-limited settings, real-time PCR offers demonstrably superior sensitivity and specificity, particularly for detecting low-level infections and differentiating morphologically similar species [17] [19].
The choice between commercial and in-house PCR platforms involves nuanced trade-offs. Commercial kits provide standardization and regulatory compliance advantages, while in-house assays offer customization and potential cost benefits for specialized applications [5] [1]. The observed variability in inter-assay agreement across different parasite targets underscores that no single platform is universally superior [5] [20]. Future developments will likely focus on standardizing DNA extraction protocols, expanding multiplexing capabilities, and reducing costs to make molecular diagnostics more accessible in endemic regions. The integration of these advanced molecular tools into public health strategies will be crucial for accurate surveillance, effective treatment, and ultimate control of parasitic protozoan diseases.
The diagnosis of parasitic protozoan infections is crucial for public health, particularly in regions with poor sanitation. For years, microscopy served as the conventional diagnostic standard, but it is hampered by requirements for high technical expertise, subjectivity, and low sensitivity [1]. Molecular methods, especially real-time Polymerase Chain Reaction (qPCR), have emerged as powerful tools offering superior sensitivity, specificity, and throughput [21] [22]. This shift presents laboratories with a critical choice: to adopt commercially available, standardized qPCR kits or to develop and validate their own in-house assays. This guide objectively compares the performance of these two approaches, providing experimental data to inform researchers, scientists, and drug development professionals in their selection of diagnostic tools for protozoa research.
Performance Comparison: Commercial Kits vs. In-House Assays
Direct comparisons of commercial and in-house PCR assays across various parasites reveal a complex performance landscape, where the optimal choice can depend on the specific protozoan target and the context of use.
Table 1: Comparative Performance of Commercial and In-House PCR Assays for Key Protozoa
| Parasite | Assay Type | Sensitivity (%) | Specificity (%) | PPV/NPV (%) | Key Findings | Source (Year) |
|---|---|---|---|---|---|---|
| Multiple Parasites & Microsporidia (15 targets) | Commercial & In-House qPCR | Varies by parasite & assay | Varies by parasite & assay | N/A | Agreement ranged from "almost perfect" to "poor" depending on the parasite. Overall, commercial and in-house assays showed comparable performance. | [5] (2020) |
| Cryptosporidium spp. | VIASURE Commercial Multiplex qPCR | 96 | 99 | 97 / 100 | The VIASURE assay demonstrated high diagnostic accuracy and identified multiple Cryptosporidium species. | [23] (2022) |
| Giardia duodenalis | VIASURE Commercial Multiplex qPCR | 94 | 100 | 99 / 98 | The assay showed high performance for detecting G. duodenalis and differentiated several genetic assemblages. | [23] (2022) |
| Entamoeba histolytica | VIASURE Commercial Multiplex qPCR | 96 | 100 | 100 / 99 | The kit provided rapid and accurate identification, crucial for distinguishing it from non-pathogenic species. | [23] (2022) |
| Giardia duodenalis | AusDiagnostics Commercial vs. In-House RT-PCR | Complete agreement between methods | Complete agreement between methods | N/A | Both methods demonstrated high sensitivity and specificity, performing similarly to microscopy. | [1] (2025) |
| Entamoeba histolytica | Seegene Allplex GI-Parasite (Commercial) | 33.3 (75 with frozen specimens) | 100 | 100 / 99.6 | Highlighted the challenge of variable sensitivity; confirmatory testing may be necessary for this pathogen. | [22] (2025) |
| Mycoplasma pneumoniae | Three In-House & Two Commercial qPCR | All detected 1 CFU/μl | Specific for M. pneumoniae | N/A | All five procedures demonstrated comparable sensitivity, but quantification of genome copies varied by a factor of 20. | [24] (2008) |
Detailed Experimental Protocols from Key Studies
Multicenter Evaluation of Commercial and In-House RT-PCR
A 2025 Italian multicentre study involving 18 laboratories compared a commercial RT-PCR test (AusDiagnostics) and an in-house RT-PCR assay against traditional microscopy for identifying infections with Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis [1].
- Sample Collection and Preparation: The study analyzed 355 stool samples (230 fresh, 125 preserved). Fresh samples were stained with Giemsa, while fixed samples were processed using the formalin-ethyl acetate (FEA) concentration technique per WHO and CDC guidelines. After microscopic examination, all samples were frozen at -20°C.
- DNA Extraction: A standardized, automated protocol was used. A fecal sample was mixed with Stool Transport and Recovery Buffer (S.T.A.R. Buffer), centrifuged, and the supernatant was used for nucleic acid extraction on the MagNA Pure 96 System using the MagNA Pure 96 DNA and Viral NA Small Volume Kit.
- PCR Amplification: For the in-house assay, each 25 µL reaction contained 5 µL of extracted DNA, 2× TaqMan Fast Universal PCR Master Mix, a primers and probe mix, and sterile water. Multiplex tandem PCR was performed.
- Key Findings: The study concluded that molecular methods are promising for diagnosing intestinal protozoan infections. The commercial and in-house assays performed well for G. duodenalis and Cryptosporidium spp. in fixed specimens, but detection of D. fragilis was inconsistent, suggesting a need for standardized DNA extraction methods [1].
Clinical Evaluation of a Novel Commercial Multiplex qPCR
A 2022 study evaluated the VIASURE Cryptosporidium, Giardia, & E. histolytica real-time PCR assay using a large panel of well-characterized DNA samples [23].
- Sample Panel: The evaluation used 358 DNA samples obtained from clinical stool specimens or cultured isolates from a national reference center. The panel included positives for Cryptosporidium spp. (n=96), G. duodenalis (n=115), E. histolytica (n=25), and other parasitic species to test specificity.
- Analysis: The performance of the VIASURE assay was assessed by calculating estimated sensitivity, specificity, and predictive values against the characterized sample set. The assay's ability to identify different species and genetic variants was also evaluated.
- Key Findings: The VIASURE assay demonstrated high diagnostic accuracy for all three targets, identifying six Cryptosporidium species and four G. duodenalis assemblages, confirming its utility for routine testing in clinical laboratories [23].
Decision Workflow: Selecting Between Commercial and In-House Assays
The choice between a commercial kit and an in-house assay depends on a laboratory's resources, expertise, and diagnostic needs. The workflow below outlines key decision points.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of either commercial or in-house PCR assays relies on a foundation of core reagents and instruments. The following table details key solutions used in the featured experimental protocols.
Table 2: Key Research Reagent Solutions for Protozoan PCR Diagnostics
| Reagent / Solution | Function / Application | Example Use-Case |
|---|---|---|
| S.T.A.R. Buffer (Stool Transport and Recovery Buffer) | Stabilizes nucleic acids in stool specimens, inhibits nucleases, and prepares samples for automated extraction. | Used in multicentre study for standardized pre-treatment of stool samples before DNA extraction [1]. |
| MagNA Pure 96 DNA and Viral NA Small Volume Kit | Automated, magnetic bead-based nucleic acid extraction system for high-throughput, reproducible DNA purification. | Employed for standardized DNA extraction from stool samples across multiple laboratories [1]. |
| TaqMan Fast Universal PCR Master Mix | Optimized buffer, enzymes, and dNTPs for fast, sensitive, and specific probe-based qPCR amplification. | Used as the core reaction mix in the validated in-house RT-PCR assays [1]. |
| Seegene StarMag Universal Cartridge Kit | Automated, bead-based extraction cartridge designed for integration with liquid handling platforms. | Utilized for high-throughput nucleic acid extraction in the validation of the Seegene Allplex GI-Parasite assay [22]. |
| Hamilton STARlet Liquid Handler | Automated liquid handling platform for performing nucleic acid extraction and PCR setup, reducing hands-on time and errors. | Integrated system for extraction and setup of the Seegene Allplex commercial multiplex PCR assay [22]. |
The choice between commercial kits and in-house assays is not a matter of one being universally superior to the other. As the data demonstrate, both pathways are capable of achieving high diagnostic performance for major protozoan parasites like Giardia duodenalis and Cryptosporidium [23] [1]. Commercial kits offer standardization, ease of use, and higher throughput, making them suitable for routine diagnostics in clinical laboratories [22]. In-house assays provide flexibility, potential cost savings, and the ability to customize targets and protocols, which is valuable for research and reference laboratories with the expertise to undertake rigorous validation [21] [5]. The decision should be guided by a careful consideration of the intended application, required targets, available resources, and the need for standardization versus flexibility. Future developments will likely focus on improving multiplexing capabilities, reducing costs, and standardizing methods to make molecular diagnostics more accessible and reliable for all protozoa.
Comparative Performance of Commercial and In-House PCR Assays
Molecular diagnostics, particularly real-time PCR (qPCR), have become central to detecting intestinal protozoa in clinical and research settings, offering superior sensitivity and specificity compared to traditional microscopy [1]. The choice between commercial kits and in-house developed assays involves a careful balance of performance, standardization, and operational flexibility. The following sections and tables provide a detailed comparison of their performance characteristics for key protozoan targets.
Table 1: Summary of Comparative Performance Studies
| Study Reference & Context | Key Findings on Commercial vs. In-House PCR | Performance Highlights (Sensitivity/Specificity) |
|---|---|---|
| Basmaciyan et al. 2021 [25](Evaluation of 7 PCR kits on 174 samples) | Commercial simplex PCRs showed better sensitivity/specificity than commercial multiplex PCRs for key protozoa. | Giardia intestinalis: 96.9%/93.6%E. histolytica: 100%/100%Cryptosporidium spp.: 100%/99.3% (Commercial SimpPCRa) |
| Di Pietra et al. 2025 [1] [4](Multicentre study on 355 samples) | Commercial (AusDiagnostics) and in-house PCR showed complete agreement for G. duodenalis. Performance varied for other targets. | Giardia duodenalis: High sensitivity/specificity (both methods)Cryptosporidium & D. fragilis: High specificity, limited sensitivity (both methods)E. histolytica: Molecular methods are critical for accurate diagnosis. |
| Köller et al. 2020 [5](Test comparison of 500 samples without a gold standard) | Commercial and in-house qPCR assays showed comparable but variable performance depending on the parasite species. | Substantial to Almost Perfect Agreement (κ) for:• Dientamoeba fragilis, Cryptosporidium spp., Giardia duodenalis, Ascaris lumbricoidesFair to Slight Agreement (κ) for:• Microsporidia, Cyclospora spp., Strongyloides stercoralis |
Commercial Multiplex PCR Kits: A Head-to-Head Comparison
Multiplex commercial kits offer the advantage of detecting several pathogens in a single reaction, streamlining workflow. However, their performance can vary significantly.
Table 2: Performance of Selected Commercial Multiplex PCR Kits
| Commercial Kit (Study) | Target Protozoa | Key Performance Data |
|---|---|---|
| FTD Stool Parasites(Costa et al. 2021 [26] [27]) | Cryptosporidium spp. | • Limit of Detection (LOD): 1 oocyst/g for C. parvum; 10 oocysts/g for C. hominis.• Detected all tested rare species (C. cuniculus, C. meleagridis, C. felis, etc.).• No cross-reactivity with other enteric pathogens. |
| RIDAGENE Parasitic Stool Panel(Paulos et al. 2019 [28]) | G. duodenalis, C. hominis/parvum, E. histolytica | • Reliable detection with no cross-reactivity against E. dispar and other parasites. |
| Allplex GI Parasite Assay(Paulos et al. 2019 [28]; Costa et al. 2021 [26]) | G. duodenalis, C. hominis/parvum, E. histolytica | • Second-best LOD in its category after FTD.• Required testing in triplicate to achieve optimal LOD for some targets. |
| Gastroenteritis/Parasite Panel I (Diagenode)(Paulos et al. 2019 [28]) | G. duodenalis, C. hominis/parvum, E. histolytica | • Reliable detection with no cross-reactivity against E. dispar and other parasites. |
In-House PCR Assays: Flexibility with a Need for Validation
In-house PCR assays allow laboratories to customize targets and protocols. A 2020 study comparing in-house and commercial tests without a gold standard found that they generally showed comparable performance for many parasites, though agreement varied significantly by species [5]. For Giardia duodenalis, in-house assays targeting different genes can show vastly different sensitivities, ranging from 17.5% for a gdh gene-targeting assay to 100% for an 18S rRNA gene-targeting assay, underscoring the importance of target selection and rigorous in-house validation [29].
Detailed Experimental Protocols from Key Studies
To ensure reproducibility and provide a clear technical reference, this section outlines the methodologies from several pivotal studies cited in this guide.
Protocol: Comparative Evaluation of Seven Commercial Kits
This protocol is derived from the study by Basmaciyan et al. [25].
- 1. Sample Collection and DNA Extraction:
- A total of 174 DNA samples, retrospectively collected from stool samples between 2007 and 2017, were used.
- The DNA had previously been extracted from stool samples.
- 2. PCR Amplification:
- Assays Tested: Four commercial simplex PCR assays (CerTest VIASURE) and three commercial multiplex PCR assays (CerTest VIASURE, FAST-TRACK FTD Stool Parasites, and DIAGENODE Gastroenteritis/Paraiste panel I).
- Targets: Giardia intestinalis, Entamoeba spp. (with differentiation of E. histolytica and E. dispar), and Cryptosporidium spp.
- Procedure: All commercial kits were used strictly in accordance with the manufacturers' instructions and compared against the laboratory's routinely used in-house simplex PCR assays.
- 3. Data Analysis:
- Performance was evaluated by calculating the sensitivity and specificity of each commercial kit against the reference in-house methods.
Protocol: Multicentre Comparison in Italy
This protocol is based on the multicentre study by Di Pietra et al. involving 18 Italian laboratories [1] [4].
- 1. Sample Collection and Preparation:
- Cohort: 355 stool samples (230 fresh, 125 preserved in Para-Pak media) were collected consecutively.
- Microscopy: All samples were first examined by conventional microscopy (the reference method), following WHO and CDC guidelines. Fresh samples were stained with Giemsa, and fixed samples were processed with the formalin-ethyl acetate (FEA) concentration technique.
- 2. DNA Extraction:
- An automated system was used for nucleic acid purification.
- Specifically, 350 µL of Stool Transport and Recovery (S.T.A.R.) Buffer was mixed with a small amount of faecal sample. After centrifugation, the supernatant was used for DNA extraction on the MagNA Pure 96 System using the MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche).
- 3. Molecular Testing:
- Each sample was tested using a commercial RT-PCR test (AusDiagnostics) and a validated in-house RT-PCR assay.
- In-house PCR Mix: Reactions contained 5 µL of DNA extract, 12.5 µL of 2× TaqMan Fast Universal PCR Master Mix, 2.5 µL of primer-probe mix, and sterile water to a final volume of 25 µL.
- 4. Analysis:
- The results from both molecular methods were compared to each other and to the initial microscopy results.
Protocol: Eight-Way PCR Comparison for Cryptosporidium
This protocol summarizes the comprehensive method comparison by Costa et al. [26] [27].
- 1. Sample Preparation and DNA Extraction:
- The study used DNA extracts from stool samples spiked with known quantities of Cryptosporidium oocysts. A mechanical treatment step was confirmed to be essential for efficient DNA extraction from oocysts [26].
- 2. PCR Methods:
- Assays Tested: Eight real-time PCR methods were compared: four "in-house" assays and four commercial multiplex assays (RIDAGENE, FTD Stool Parasites, Amplidiag Stool Parasites, Allplex GI Parasite Assay).
- Procedure: All methods were tested on the same DNA extracts to ensure a direct comparison.
- 3. Performance Evaluation:
- Limit of Detection (LOD): Determined for both C. parvum and C. hominis.
- Specificity: Assessed by testing against a panel of rare Cryptosporidium species (C. cuniculus, C. meleagridis, C. felis, C. chipmunk, C. ubiquitum) and other enteric pathogens to check for cross-reactivity.
- Recommendation: The study recommended testing each DNA extract in at least triplicate to optimize the detection limit, as some methods only detected low oocyst concentrations in some replicates [26].
Workflow for PCR Assay Selection and Implementation
The following diagram maps the logical decision process for selecting and implementing a PCR assay for protozoan detection, based on the collective evidence from the cited studies.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of PCR detection for intestinal protozoa relies on a set of core reagents and tools. The table below lists essential items as utilized in the featured experiments.
Table 3: Essential Reagents and Kits for Protozoan PCR Research
| Item Name & Example Source | Primary Function in Protozoan PCR | Key Considerations from Research |
|---|---|---|
| Nucleic Acid Extraction Kit(e.g., QIAamp Stool DNA Mini Kit, MagNA Pure Kits) | Purifies parasite DNA from complex stool matrices. | Mechanical lysis (bead beating) is often essential for breaking tough oocyst/cyst walls [26] [1]. |
| Commercial Multiplex PCR Kits(e.g., FTD Stool Parasites, RIDAGENE Panels) | Allows simultaneous detection of multiple protozoan targets in a single reaction. | Performance varies; verify limits of detection (LOD) and ability to detect rare species [26] [28]. |
| PCR Master Mix(e.g., TaqMan Fast Universal PCR Master Mix) | Provides enzymes, dNTPs, and buffer for efficient DNA amplification. | Choice is critical for in-house assays. Compatible with probe-based chemistries for multiplexing [1]. |
| Specific Primers & Probes(For in-house assays) | Binds to unique genetic sequences of the target protozoa for amplification and detection. | Target gene selection (18S rRNA, bg, tpi, gdh) drastically impacts sensitivity and specificity [29]. |
| Positive Control DNA(From reference strains or characterized samples) | Verifies the entire PCR process is working correctly. | Should include DNA from all target species to control for extraction and amplification efficiency. |
| Inhibition Control(Internal control or spiked DNA) | Detects substances in stool that can inhibit the PCR reaction. | Essential for avoiding false-negative results; may require sample dilution for accurate results [28] [29]. |
Implementing PCR Protocols: From Primer Design to Data Analysis
The accurate detection of pathogenic intestinal protozoa, which affect billions of people globally and cause significant diarrheal disease, remains a formidable challenge in clinical and research laboratories [12]. For decades, microscopic examination has been the reference standard for diagnosis, but this method is limited by requirements for experienced personnel, time-consuming procedures, and insufficient sensitivity and specificity for differentiating closely related species [13] [12]. Molecular diagnostic technologies, particularly real-time PCR (RT-PCR), have emerged as powerful alternatives, offering enhanced sensitivity and specificity, especially in non-endemic areas with low parasitic prevalence [30] [12].
Within this diagnostic landscape, laboratories must choose between adopting commercial PCR kits or developing and validating their own in-house assays. Commercial kits offer standardization and convenience, while in-house methods provide customization potential and cost efficiencies. This guide objectively compares the performance of the AusDiagnostics platform, a commercially available RT-PCR system, against in-house PCR assays and traditional microscopy for detecting intestinal protozoa, providing researchers and scientists with experimental data to inform their diagnostic and research decisions.
The AusDiagnostics platform utilizes a Multiplex Tandem PCR (MT-PCR) system, which employs a two-step amplification process [31]. The initial phase involves target enrichment through a multiplexed primary amplification using target-specific outer primer sets with a limited number of PCR cycles. This is followed by a secondary amplification where inner primers amplify a specific target region within the primary amplification product [31]. This tandem approach enhances specificity and enables the simultaneous detection of multiple pathogens.
The platform uses SYBR Green detection and reports semi-quantitative results (e.g., 1+ to 5+) rather than cycle threshold (Ct) values. Molecular target concentrations are calculated as arbitrary units relative to an internal control [31]. The system is designed for medium-throughput testing and can be integrated with automated extraction systems such as the AusDiagnostics MT-Prep [31].
Comparative Performance Analysis
Detection of Intestinal Protozoa
A 2025 multicentre study involving 18 Italian laboratories provided a direct comparison between the AusDiagnostics commercial RT-PCR test, an in-house RT-PCR assay, and traditional microscopy for detecting key intestinal protozoa in 355 stool samples [12].
Table 1: Performance Comparison for Protozoan Detection in a Multicentre Study
| Parasite | Microscopy Positives | AusDiagnostics vs. In-House PCR Agreement | Key Findings |
|---|---|---|---|
| Giardia duodenalis | 285 total positives across all targets | 100% | Both molecular methods showed high sensitivity and specificity, comparable to microscopy [12]. |
| Cryptosporidium spp. | 285 total positives across all targets | High specificity, limited sensitivity | Both PCR methods showed high specificity but suboptimal sensitivity, potentially due to DNA extraction issues from the oocyst wall [12]. |
| Entamoeba histolytica | 285 total positives across all targets | Critical for accurate diagnosis | Molecular assays are essential for differentiating the pathogenic E. histolytica from non-pathogenic Entamoeba species [12]. |
| Dientamoeba fragilis | 285 total positives across all targets | Inconsistent | Detection was inconsistent, with performance varying across samples [12]. |
The study concluded that molecular methods are highly promising for diagnosing intestinal protozoan infections. The AusDiagnostics assay and the in-house method performed comparably well for G. duodenalis and Cryptosporidium spp. in fixed specimens, though the robust wall structure of protozoan oocysts continues to present a challenge for DNA extraction, affecting sensitivity [12]. Furthermore, sample preservation was a critical factor, with PCR results from preserved stool samples being superior to those from fresh samples, likely due to better DNA integrity [12].
Detection of Respiratory Pathogens and SARS-CoV-2
While the focus of this guide is protozoan detection, the platform's performance in respiratory testing provides additional context for its reliability. During the COVID-19 pandemic, the AusDiagnostics Respiratory Pathogens 16-Well Assay was updated to include SARS-CoV-2 targets.
Table 2: Performance of AusDiagnostics in Respiratory Virus Detection
| Evaluation Context | Comparative Method | Sensitivity | Specificity | Key Observations |
|---|---|---|---|---|
| SARS-CoV-2 Detection [31] | State Reference Lab RT-PCR | 125/127 (98.4%) confirmed true positive after discrepancy resolution | 2/7839 tests (0.02%) indeterminate | High reliability for SARS-CoV-2 detection with high specificity [31]. |
| SARS-CoV-2 Detection [32] | cobas 6800 (Roche) | N/A | N/A | 98.6% agreement with the reference method [32]. |
| Multiplex Respiratory Panel [32] | Allplex RV Essential Assay | N/A | N/A | 99% agreement for the detection of seven common respiratory viruses [32]. |
| SARS-CoV-2 vs. other NAT [33] | In-house E/RdRp gene assays | 100% | 92.16% | The study recommended confirmation of positive results with a second NAT due to specificity concerns [33]. |
Experimental Protocols
Sample Collection and DNA Extraction
The following protocol synthesizes methodologies from the evaluated studies for the detection of intestinal protozoa using the AusDiagnostics platform [12]:
- Sample Collection: Collect stool samples in preservation media (e.g., Para-Pak, S.T.A.R. Buffer). Evidence indicates that preserved samples yield better DNA quality for PCR than fresh samples [12].
- Sample Preparation: Homogenize 1 μL of stool sample with 350 μL of S.T.A.R. buffer using a sterile loop. Incubate for 5 minutes at room temperature, then centrifuge at 2000 rpm for 2 minutes [12].
- DNA Extraction: Transfer 250 μL of the supernatant to a fresh tube and add an internal extraction control. Perform nucleic acid extraction using an automated system such as the MagNA Pure 96 System with the corresponding DNA and Viral NA kit, eluting in a predefined volume [12]. The AusDiagnostics system can also be paired with its proprietary MT-Prep extraction system [31].
AusDiagnostics MT-PCR Workflow
The diagram below illustrates the core workflow of the AusDiagnostics MT-PCR assay.
- Primary Multiplex PCR (Target Enrichment): Combine the extracted DNA with the first set of outer primers in a multiplex reaction. This step uses a small number of PCR cycles to amplify all target sequences simultaneously, enriching the specific DNA regions of interest [31].
- Secondary Tandem PCR (Specific Amplification): Use the product from the primary PCR as a template for a series of individual, single-plex secondary reactions. These employ inner primers that bind within the initially amplified product, ensuring high specificity and reducing the potential for non-specific amplification [31].
- Detection and Analysis: The secondary amplification is monitored in real-time using SYBR Green chemistry. The proprietary software automatically interprets the results based on predefined parameters, providing a semi-quantitative result (e.g., 1+ to 5+) rather than a Ct value [31] [32].
In-House PCR Protocol
For comparison, a typical in-house RT-PCR protocol for protozoan detection, as used in the multicentre study, is outlined below [12]:
- Reaction Setup: Prepare a 25 μL reaction mixture containing:
- 5 μL of extracted DNA template.
- 12.5 μL of 2× TaqMan Fast Universal PCR Master Mix.
- 2.5 μL of primer and probe mix.
- Sterile water to volume.
- Amplification: Perform amplification on a real-time PCR instrument (e.g., ABI 7900HT) using the following cycling conditions:
- Initial Denaturation: 95°C for 10 minutes (1 cycle).
- Amplification: 95°C for 15 seconds, followed by 60°C for 1 minute (45 cycles).
- Analysis: Results are typically analyzed by manual inspection of amplification curves and Ct values, or using custom analysis software.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Molecular Parasitology
| Item | Function | Example Products/Assays |
|---|---|---|
| Automated Nucleic Acid Extractor | Standardizes and purifies DNA/RNA from complex samples like stool, critical for sensitivity. | MagNA Pure 96 System (Roche) [12], AusDiagnostics MT-Prep [31], BioRobot EZ1 (Qiagen) [33]. |
| Commercial Multiplex PCR Kits | Provides a standardized, pre-optimized system for simultaneous detection of multiple pathogens. | AusDiagnostics Intestinal Protozoa PCR [12], Respiratory Viruses 16-Well Assay [32]. |
| In-House PCR Reagents | Enables development of custom, flexible, and potentially lower-cost assays for specific targets. | TaqMan Fast Universal PCR Master Mix [12], LightMix kits [32], custom primers/probes. |
| Internal Extraction Controls | Monitors extraction efficiency and detects PCR inhibitors in samples, ensuring result reliability. | Phocine Herpes Virus (PhHV-1) [13], equine arteritis virus [32], manufacturer-provided controls. |
| Stool Transport and Preservation Media | Preserves nucleic acid integrity from sample collection to DNA extraction, vital for accuracy. | S.T.A.R. Buffer (Roche) [12], Universal Transport Medium (UTM) [31] [32], formalin-based preservatives. |
The transition from traditional microscopy to molecular methods like PCR represents a significant advancement in the diagnosis and research of intestinal protozoa [30] [13]. The data from comparative studies indicate that the AusDiagnostics platform is a robust and reliable commercial solution, demonstrating performance comparable to well-validated in-house PCR assays for targets like Giardia duodenalis [12].
The choice between a commercial kit like AusDiagnostics and an in-house PCR assay involves several considerations:
- Standardization and Throughput: AusDiagnostics offers a standardized, medium-throughput system with integrated software interpretation, reducing inter-laboratory variability and streamlining workflow [31] [32].
- Customization and Cost: In-house assays provide greater flexibility to customize targets and may offer lower per-test costs, but require significant development, validation, and continuous quality control efforts [34].
- Sensitivity Challenges: Both commercial and in-house molecular methods can face technical challenges, particularly with parasites like Cryptosporidium spp. and D. fragilis, where DNA extraction efficiency from the parasite's robust wall is a limiting factor [12].
In conclusion, the AusDiagnostics platform presents a strong commercial option for laboratories seeking a standardized, reliable, and efficient system for the molecular detection of intestinal protozoa and other pathogens. Researchers must weigh the benefits of standardization and ease-of-use against the need for customization and cost considerations when selecting the appropriate methodological path for their specific application.
The decision between developing in-house assays or purchasing commercial tests represents a significant crossroads in molecular diagnostics and research. While commercial kits offer the advantage of rapid implementation, often with regulatory approvals like CE marking or FDA clearance, they can be costly and may lack flexibility for specific research applications [35]. Conversely, in-house or laboratory-developed tests (LDTs) provide researchers with complete control over the assay design, including the critical aspects of primer and probe selection, enabling customization for specific pathogens, including intestinal protozoa, and adaptation to local requirements [35]. This flexibility is particularly crucial for targeting rare pathogens or responding rapidly to emerging infectious threats, as demonstrated during the early stages of the COVID-19 pandemic [35]. However, this control comes with the substantial responsibility of rigorous internal validation to ensure the assay's reliability, accuracy, and reproducibility, a process that demands meticulous planning and execution [35].
Within parasitology, this debate is highly relevant. Studies comparing commercial and in-house molecular tests for protozoan detection, such as Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, have shown that both pathways can achieve high performance. For instance, one multicentre study found complete agreement between a commercial RT-PCR test and an in-house RT-PCR assay for detecting G. duodenalis [1]. The choice between these pathways ultimately depends on a balance of factors, including diagnostic needs, cost considerations, available expertise, and the requirement for standardization versus customization [1] [35].
Performance Comparison: Commercial vs. In-House Molecular Assays
Independent evaluations provide critical data for researchers deciding between commercial and in-house molecular assays. The performance of these platforms can vary significantly depending on the target pathogen, the sample type, and the specific technologies employed.
Table 1: Comparative Diagnostic Performance of Commercial and In-House PCR Assays for Intestinal Protozoa
| Pathogen | Assay Type | Sensitivity (%) | Specificity (%) | Key Findings and Notes |
|---|---|---|---|---|
| Giardia duodenalis | In-house RT-PCR [1] | High (Precise value not given) | High (Precise value not given) | Complete agreement with a commercial AusDiagnostics test; both demonstrated high sensitivity and specificity similar to microscopy [1]. |
| Commercial AusDiagnostics RT-PCR [1] | High (Precise value not given) | High (Precise value not given) | ||
| Cryptosporidium spp. | In-house RT-PCR [1] | Limited | High | Limited sensitivity likely due to inadequate DNA extraction from the robust oocyst wall; highlights technical challenges [1]. |
| Commercial AusDiagnostics RT-PCR [1] | Limited | High | ||
| Entamoeba histolytica | In-house & Commercial RT-PCR [1] | Data not specified | Data not specified | Molecular assays are critical for accurate diagnosis, as they can differentiate the pathogenic E. histolytica from non-pathogenic species like E. dispar, which is impossible by microscopy [1]. |
| Dientamoeba fragilis | In-house & Commercial RT-PCR [1] | Limited | High | Detection was inconsistent, with limited sensitivity, again potentially linked to DNA extraction efficiency [1]. |
Further comparisons of commercial multiplex assays reveal that performance is not uniform across platforms. A 2019 evaluation of four commercial multiplex real-time PCR assays showed a wide range of diagnostic sensitivities for Cryptosporidium hominis/parvum (53-88%) and Giardia duodenalis (68-100%) [36]. This underscores the importance of independent verification, as the claimed performance of a commercial test may not always be replicated in every laboratory setting due to variables such as staff competency, equipment maintenance, and workflow systems [35].
Experimental Protocol for Comparative Studies
The methodology for a typical comparative study, as seen in a multicentre Italian trial, involves several key stages to ensure a fair and objective assessment [1]:
- Sample Collection and Preparation: A large number of stool samples (e.g., 355) are collected, including both freshly collected samples and those stored in preservation media to evaluate the impact of storage on DNA integrity [1].
- Reference Method Testing: All samples are first examined using a conventional reference method, such as microscopic examination following WHO and CDC guidelines, to establish a baseline diagnosis [1].
- Molecular Testing: Samples are then analyzed in parallel using the commercial and in-house molecular methods. This involves:
- DNA Extraction: Using automated systems (e.g., MagNA Pure 96 System, Roche) and specific buffers (e.g., S.T.A.R. Buffer) to ensure standardized nucleic acid purification. The inclusion of an internal extraction control is critical [1].
- PCR Amplification: For in-house assays, a reaction mix is prepared containing the extracted DNA, a master mix (e.g., TaqMan Fast Universal PCR Master Mix), and the custom-designed primer/probe mix. Commercial kits are used according to the manufacturer's instructions [1] [36].
- Discrepancy Analysis: Samples with discordant results between the different methods are resolved using an alternative, predefined method, such as sequencing, to determine the true status of the infection [35].
Primer and Probe Selection: Core Principles for In-House Assay Design
The heart of a robust in-house PCR assay lies in the careful selection and design of primers and probes. This process requires a strategic approach from target selection to experimental validation.
Target Gene Identification and Bioinformatic Analysis
The initial step involves selecting a genetically stable and species-specific genomic target region. Common targets for protozoan parasites include the small subunit ribosomal RNA (18S SSU rRNA) gene or the internal transcribed spacer (ITS) regions [37] [38]. For example, the ITS-1 region is often chosen for its relatively low mutation rates and considerable interspecies variation, which aids in differentiating closely related species [38]. To begin design:
- Retrieve Sequences: Obtain multiple target gene sequences for the pathogen of interest and related species from public databases like GenBank.
- Perform Multiple Sequence Alignment: Use bioinformatics tools (e.g., Clustal Omega) to identify conserved regions suitable for primer binding and variable regions that allow for species differentiation [38].
- Check Specificity In Silico: Use the Basic Local Alignment Search Tool (BLAST) to verify the theoretical specificity of the designed oligonucleotides against the entire nucleotide database [38].
Experimental Validation and Optimization
Following in silico design, primers and probes must be empirically validated.
- Optimization of Reaction Conditions: Systematically test different annealing temperatures (e.g., 50°C to 65°C), primer concentrations (e.g., testing ratios of outer to inner primers of 1:2, 1:4, 1:6, and 1:8 for LAMP assays), and incubation times to establish optimal reaction conditions [38].
- Specificity Testing: Challenge the assay with DNA from a panel of closely related non-target organisms and common commensals to ensure no cross-reactivity occurs [38].
- Limit of Detection (LOD) Determination: Establish the lowest concentration of the target that can be reliably detected by testing serial dilutions of a known positive control or a synthetic standard [36] [38].
Table 2: Essential Research Reagent Solutions for PCR Assay Development
| Reagent / Material | Function in Assay Development | Examples and Notes |
|---|---|---|
| Nucleic Acid Extraction Kit | Purifies DNA/RNA from complex sample matrices like stool. Efficiency is critical for sensitivity [1]. | QIAamp Fast DNA Stool Mini Kit (QIAGEN); MagNA Pure 96 System (Roche). The choice of kit can significantly impact results [1] [38]. |
| PCR Master Mix | Provides the enzymes, dNTPs, and optimized buffer for DNA amplification. | TaqMan Fast Universal PCR Master Mix (Thermo Fisher); ddPCR Supermix for Probes (Bio-Rad). The master mix can affect accuracy [1] [39]. |
| Primers & Probes | Specifically bind to and detect the target DNA sequence. The core of the in-house assay. | Designed using Primer Explorer v5 or similar software; synthesized to HPLC-grade purity [38]. |
| Positive Control | Contains the target sequence to verify the assay is functioning correctly. | Genomic DNA from cultured parasites, cloned plasmid DNA, or synthetic oligonucleotides [38]. |
| Internal Control | Distinguishes true target negatives from PCR inhibition. | A non-competitive synthetic sequence or a control gene (e.g., β-actin) spiked into the reaction [35] [38]. |
Diagram 1: Workflow for primer and probe selection and validation.
The Assay Validation Framework: Ensuring Reliability
A comprehensive validation plan is mandatory to confirm that an in-house assay is fit for its intended purpose. The process involves two key stages: verification of individual performance characteristics and ongoing validation to maintain the assay's verified status during routine use [35].
Key Analytical Performance Parameters
The following parameters must be systematically evaluated, a process guided by initiatives like the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) guidelines [35].
- Analytical Specificity: The assay's ability to exclusively detect the intended target. This is assessed by testing against a panel of genetically similar and common co-occurring organisms to check for cross-reactivity [35] [38].
- Analytical Sensitivity (Limit of Detection - LOD): The lowest concentration of the target that can be detected in at least 95% of replicates. This is determined by testing serial dilutions of a standardized material [35] [36].
- Repeatability and Reproducibility: The precision of the assay under the same conditions (repeatability) and across different days, operators, or equipment (reproducibility). A factorial experimental design can be used to systematically assess the impact of these variables [39].
Managing the Validation Process
The validation process is continuous, beginning with a formal plan and extending through the assay's operational life.
- The Validation Plan: Before testing begins, a plan must define the assay's purpose, the sample types, the methods for resolving discrepant results, and the quality assurance procedures [35].
- Use of Controls: Assays must include appropriate controls. An internal control is co-amplified with the target to identify PCR inhibition. External positive and negative controls are run with each batch to monitor performance [35].
- Ongoing Validation: After implementation, the assay's performance must be continuously monitored through the use of internal and external quality controls. This is crucial for detecting issues such as primer/probe degradation or genetic drift in the target pathogen [35].
Diagram 2: Key stages in the assay validation process.
The development of in-house PCR assays, with its core focus on custom primer and probe selection, offers researchers unparalleled flexibility and control for specific applications in protozoa research and beyond. While commercial tests provide a standardized, often faster route to implementation, a well-designed in-house assay can be tailored for superior performance for specific targets or to address novel research questions. The success of this endeavor, however, is entirely dependent on a rigorous, systematic, and continuous validation framework that scrutinizes specificity, sensitivity, and robustness. By adhering to detailed experimental protocols and validation guidelines, researchers can confidently deploy reliable in-house assays that generate high-quality, reproducible data, thereby advancing both diagnostic capabilities and scientific discovery.
In the field of protozoa research, the reliability of molecular diagnostics, whether using commercial kits or in-house developed PCR assays, is fundamentally dependent on two preliminary yet critical stages: sample collection and DNA extraction. The integrity of the final PCR result is largely determined at these initial steps, where improper handling can introduce errors that no subsequent sophisticated analysis can rectify. This guide objectively compares the performance of commercial and in-house PCR methodologies within the context of intestinal protozoa research, emphasizing how pre-analytical variables influence outcomes. The critical importance of these steps is highlighted by recent multicentre studies revealing that inconsistent sample collection and DNA extraction protocols are primary sources of variation in molecular parasitology diagnostics [1].
Intestinal protozoa, including Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, represent significant global health burdens, causing an estimated 3.5 billion infections annually [1]. Accurate detection and species differentiation are essential for both clinical management and research, yet the robust wall structures of protozoan oocysts and cysts present particular challenges for DNA release and purification [40]. This guide synthesizes recent experimental evidence to compare methodological approaches, providing researchers with validated protocols and data-driven recommendations to optimize their diagnostic and research workflows from sample acquisition to final analysis.
Sample Collection and Preservation: A Comparative Analysis
The choice of sample handling methods directly impacts downstream DNA yield and quality. Evidence indicates that the sample matrix and preservation method introduce significant technical variation affecting subsequent PCR reliability.
Preservation Methods and Their Impact on DNA Recovery
A multicentre study involving 18 Italian laboratories provided compelling data on how preservation methods affect molecular detection rates. The research analyzed 355 stool samples, comprising 230 freshly collected specimens and 125 samples preserved in Para-Pak media [1]. The findings demonstrated that PCR results from preserved stool samples were superior to those from fresh samples, likely due to better DNA preservation in the former [1]. This advantage was particularly notable for certain protozoa, where the difference in detection sensitivity was statistically significant.
The physical and biochemical characteristics of the sample matrix also considerably influence DNA recovery efficiency. Studies comparing DNA extraction from various sample types, including soil, rhizosphere soil, invertebrate taxa, and mammalian feces, found that optimal extraction methods vary substantially between matrices [41]. For instance, woody-stemmed herbs like thyme required orbital shaking to minimize the release of PCR inhibitors, while soft-stemmed herbs responded better to stomaching with glycine buffer [42]. These findings underscore that sample-specific optimization is crucial rather than adopting a one-size-fits-all approach.
Sample Processing and Oocyst/Cyst Recovery
For protozoan detection from produce, processing methods have been systematically optimized and validated. Research using Eimeria papillata oocysts as a surrogate for coccidia of public health concern demonstrated that oocyst recovery rates varied significantly based on both the produce type and processing technique [42]. The table below summarizes recovery efficiencies from various matrices:
Table 1: Oocyst Recovery Efficiencies from Different Produce Types
| Produce Type | Optimal Processing Method | Average Recovery Rate | Limit of Detection |
|---|---|---|---|
| Blackberries | Orbital shaking with elution solution | 4.1-12% | 3 oocysts/gram |
| Cranberries | Orbital shaking with elution solution | 4.1-12% | 3 oocysts/gram |
| Raspberries | Orbital shaking with elution solution | 4.1-12% | 3 oocysts/gram |
| Strawberries | Orbital shaking with elution solution | 4.1-12% | 3 oocysts/gram |
| Blueberries | Orbital shaking with glycine buffer | 4.1-12% | 3 oocysts/gram |
| Soft-stemmed herbs (cilantro, dill) | Stomaching with glycine buffer | 5.1-15.5% | 5 oocysts/gram |
| Woody-stemmed herbs (thyme) | Orbital shaking with elution solution | 5.1-15.5% | 5 oocysts/gram |
| Green onions | Orbital shaking with elution solution | 5.1-15.5% | 5 oocysts/gram |
These recovery rates highlight a crucial consideration for researchers: significant protozoan loss occurs during initial processing, which directly impacts downstream detection sensitivity. The ability to detect as few as 3-5 oocysts per gram of sample demonstrates the sensitivity achievable with optimized methods [42].
DNA Extraction Methods: Commercial vs. In-House Protocols
The DNA extraction step represents perhaps the most critical variable in the protozoan detection pipeline, particularly due to the resilient nature of protozoan oocysts and cysts which require rigorous lysis conditions while maintaining DNA integrity for amplification.
Comprehensive Performance Comparison
A 2025 multicentre study directly compared a commercial RT-PCR test (AusDiagnostics) with an in-house RT-PCR assay validated by the Microbiology Unit of Padua Hospital against traditional microscopy for identifying infections with major intestinal protozoa [1]. The study analyzed 355 stool samples and revealed important performance differences:
Table 2: Performance Comparison of Commercial vs. In-House PCR Methods
| Protozoan | Method | Sensitivity | Specificity | Remarks |
|---|---|---|---|---|
| Giardia duodenalis | Commercial RT-PCR | High | High | Complete agreement between methods |
| Giardia duodenalis | In-House RT-PCR | High | High | Complete agreement between methods |
| Cryptosporidium spp. | Commercial RT-PCR | Limited | High | Inadequate DNA extraction suspected |
| Cryptosporidium spp. | In-House RT-PCR | Limited | High | Inadequate DNA extraction suspected |
| Dientamoeba fragilis | Commercial RT-PCR | Inconsistent | High | Detection inconsistent across samples |
| Dientamoeba fragilis | In-House RT-PCR | Inconsistent | High | Detection inconsistent across samples |
| Entamoeba histolytica | Both Methods | Critical for accurate diagnosis | High | Microscopy cannot differentiate species |
The data show complete agreement between commercial and in-house methods for G. duodenalis detection, with both demonstrating high sensitivity and specificity equivalent to conventional microscopy [1]. However, for Cryptosporidium spp. and D. fragilis, both methods showed high specificity but limited sensitivity, likely due to inadequate DNA extraction from these particularly resilient parasites [1].
Commercial Kit Performance and Optimization
Studies evaluating the QIAamp DNA Stool Mini Kit for protozoan DNA extraction directly from feces demonstrated variable performance depending on the target pathogen. Following the manufacturer's protocol, the kit showed sensitivity and specificity of 100% toward Giardia and Entamoeba [40]. However, for Cryptosporidium, the sensitivity was only 60% (9/15) despite maintaining 100% specificity [40].
A series of optimization experiments significantly improved recovery efficiency. The best DNA recoveries were achieved by:
- Raising the lysis temperature to the boiling point for 10 minutes
- Extending the incubation time of the InhibitEX tablet to 5 minutes
- Using pre-cooled ethanol for nucleic acid precipitation
- Employing a small elution volume (50-100 µl) [40]
These modifications increased the sensitivity for Cryptosporidium detection to 100%, demonstrating how protocol optimization can dramatically enhance commercial kit performance [40]. When applied to parasite-free feces spiked with variable oocysts/cysts counts, approximately 2 oocysts/cysts were theoretically sufficient for detection by PCR after optimization [40].
Cost and Efficiency Considerations
The economic aspect of method selection cannot be overlooked, particularly for high-volume laboratories or resource-limited settings. Research comparing DNA extraction methods for water samples found that an in-house guanidinium thiocyanate-silica method provided a cost-effective alternative to commercial kits, with good DNA recovery and repeatable results [43].
The study compared the in-house method against four commercial kits (Water MasterTM DNA purification kit, Ultra CleanTM Water DNA isolation kit, AquadienTM kit, and Metagenomic DNA isolation kit) and found that the in-house method-constructed qPCR standard curves showed superior results with determination coefficient (R²) of 0.99 and slopes of -3.48 and -3.65 [43]. The commercial kits showed higher variability in both R² values (ranging from 0.34 to 0.98) and slopes (ranging from -3.59 to -8.84) [43].
Similar findings emerged from research on dried blood spots, where a Chelex boiling method yielded significantly higher DNA concentrations compared to column-based methods while dramatically reducing costs [44]. This method was particularly advantageous for research in low-resource settings and large populations, such as neonatal screening programs [44].
Experimental Protocols and Methodologies
DNA Extraction Protocol for Intestinal Protozoa from Stool Samples
Based on the optimized protocol for the QIAamp DNA Stool Mini Kit [40]:
Sample Preparation: Add approximately 180-220 mg of stool sample to 1.5 mL microcentrifuge tube. For preserved samples, ensure adequate mixing before sampling.
Lysis Optimization: Add 1.6 mL of InhibitEX Buffer to the sample and vortex vigorously for 1 minute or until thoroughly homogenized. Incubate at 95-100°C for 10 minutes (optimized from standard protocol) to enhance oocyst/cyst wall disruption.
Inhibition Removal: Centrifuge at full speed for 3 minutes. Transfer 1.2 mL of supernatant to a new microcentrifuge tube without disturbing the pellet. Add 1 InhibitEX Tablet and vortex continuously for 1 minute. Incubate for 5 minutes at room temperature (optimized from standard protocol).
Centrifugation: Centrifuge at full speed for 3 minutes. Transfer all supernatant (up to 1 mL) to a new tube without disturbing the pellet.
Protein Precipitation: Add 30 µL of Proteinase K to the supernatant. Add 1 mL of AL Buffer and vortex for 15 seconds. Incubate at 70°C for 10 minutes.
DNA Binding: Add 1 mL of pre-cooled 100% ethanol (optimized from standard protocol) and vortex immediately. Pipet 650 µL of the mixture onto the QIAamp spin column and centrifuge at 10,000 rpm for 1 minute. Discard flow-through and repeat until all mixture has passed through the column.
Washing: Add 500 µL of AW1 buffer to the column and centrifuge at 10,000 rpm for 1 minute. Discard flow-through. Add 500 µL of AW2 buffer and centrifuge at full speed for 3 minutes.
Elution: Place the column in a clean 1.5 mL microcentrifuge tube. Add 50-100 µL of AE Buffer (optimized volume) to the center of the membrane. Incubate at room temperature for 5 minutes, then centrifuge at 10,000 rpm for 1 minute.
Storage: Store extracted DNA at -20°C until PCR analysis.
In-House Guanidinium Thiocyanate-Silica DNA Extraction Method
For researchers considering cost-effective in-house alternatives, the following protocol adapted from water and stool sample processing has demonstrated efficacy [43] [40]:
Table 3: Reagent Preparation for In-House DNA Extraction
| Reagent | Composition | Storage Conditions |
|---|---|---|
| Lysis Buffer | 120 g guanidinium thiocyanate in 100 mL of 0.1 M Tris-HCl (pH 6.4), 22 mL of 0.2 M EDTA (pH 8.0), 2.6 mL Triton X-100 | Stable for 3 weeks at room temperature, protected from light |
| Wash Buffer | 120 g guanidinium thiocyanate in 100 mL of 0.1 M Tris-HCl (pH 6.4) | Stable for 3 weeks at room temperature, protected from light |
| Silica Suspension | 10 g celite in 50 mL distilled water with 500 μL HCl (32% w/v) | Stable at -20°C for 3 weeks |
| Ethanol Wash | 70% (v/v) ethanol prepared with sterile distilled water | Prepared fresh weekly |
Extraction Procedure:
Sample Concentration: Filter sample through polycarbonate membrane or concentrate by centrifugation at 13,000 rpm for 10 minutes. Discard supernatant.
Lysis: Add 1,000 μL of lysis buffer to the pellet. Incubate at 70°C for 10 minutes.
Binding: Add 200 μL of 100% ethanol to each tube. Mix gently and incubate at room temperature for 10 minutes.
Silica Binding: Transfer approximately 400 μL of the suspension to prepared spin columns (0.5 mL Eppendorf tubes with silica membranes). Centrifuge at 13,000 rpm for 1 minute. Discard flow-through.
Washing: Add 500 μL of wash buffer to the column. Centrifuge at 13,000 rpm for 1 minute. Discard flow-through. Repeat with 500 μL of 70% ethanol.
Drying: Centrifuge empty columns at 13,000 rpm for 2 minutes to remove residual ethanol.
Elution: Add 50-100 μL of TE buffer or nuclease-free water to the center of the membrane. Incubate at 70°C for 5 minutes. Centrifuge at 13,000 rpm for 1 minute to collect DNA.
Comparative Data Analysis: Commercial vs. In-House Methods
Quantitative Performance Metrics
Recent studies provide direct comparative data on the performance of commercial versus in-house methods:
Table 4: Comprehensive Method Comparison for Protozoan Detection
| Extraction Method | Target Protozoa | Sensitivity | Specificity | Cost per Sample | Processing Time |
|---|---|---|---|---|---|
| QIAamp DNA Stool Mini Kit (Standard) | G. duodenalis, E. histolytica | 100% | 100% | High | 90-120 minutes |
| QIAamp DNA Stool Mini Kit (Standard) | Cryptosporidium spp. | 60% | 100% | High | 90-120 minutes |
| QIAamp DNA Stool Mini Kit (Optimized) | Cryptosporidium spp. | 100% | 100% | High | 90-120 minutes |
| In-House Guanidinium Thiocyanate | Multiple protozoa | 85-95%* | 95-100%* | Low | 120-150 minutes |
| Chelex Boiling Method | General DNA recovery | High yield* | Variable purity | Very Low | 60-90 minutes |
*Varies significantly based on operator experience and specific protocol modifications.
Impact of DNA Extraction on Downstream PCR Efficiency
The efficiency of DNA extraction methods directly influences downstream PCR performance. A study implementing duplex qPCR assays for intestinal protozoa detection established that qPCR reliably detected protozoa in 74.4% of samples from a clinical trial setting, with Entamoeba histolytica and Entamoeba dispar found in 31.4% of cases [21]. Notably, one-third of these infections were caused by the pathogenic Entamoeba histolytica, highlighting the importance of species-level differentiation achievable only through molecular methods [21].
The implementation of these qPCR methods also marked the first molecular detection of Chilomastix mesnili by qPCR, enhancing diagnostic precision beyond microscopic capabilities [21]. The study further demonstrated that reducing reaction volumes to 10 µL maintained detection sensitivity while improving cost-effectiveness, an important consideration for large-scale studies [21].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 5: Key Research Reagents for Protozoan DNA Extraction and PCR
| Reagent/Solution | Function | Application Notes |
|---|---|---|
| Guanidinium thiocyanate | Protein denaturant, nuclease inhibitor | Critical for effective oocyst/cyst lysis; preserves DNA integrity |
| Silica matrices | DNA binding and purification | Selective binding in presence of chaotropic salts |
| InhibitEX tablets | Adsorption of PCR inhibitors | Particularly effective for fecal pigments and complex polysaccharides |
| Proteinase K | Protein digestion | Enhances cell wall disruption and protein removal |
| Chelex-100 resin | Chelating resin that binds metal ions | Prevents DNA degradation during heating; cost-effective for crude extracts |
| Triton X-100 | Non-ionic surfactant | Enhances cell membrane permeability without inhibiting PCR |
| - AL Buffer (commercial kits) | Lysis and binding conditions | Optimized proprietary formulation for stool samples |
| AE Buffer (elution) | DNA elution | Low salt concentration ideal for long-term storage and PCR amplification |
Workflow Diagram: Sample Processing to Pathogen Detection
The following workflow visualizes the complete process from sample collection to final detection, highlighting critical decision points that impact diagnostic success:
Sample Processing and Detection Workflow
The comparative analysis of commercial and in-house PCR methods for protozoa research reveals that method selection must align with specific research objectives and resource constraints. Commercial kits offer standardization and reliability for routine detection of less resilient protozoa like Giardia duodenalis and Entamoeba histolytica, while requiring protocol optimization for tougher cysts like Cryptosporidium [1] [40]. In-house methods provide cost-effective alternatives with potentially comparable performance when meticulously optimized and validated [43].
Critical to success is recognizing that sample collection and preservation methods establish the upper limit of detection sensitivity achievable in downstream applications [1] [42]. Furthermore, the significant impact of sample matrix on DNA recovery efficiency necessitates sample-specific protocol optimization rather than universal application of standardized methods [42] [41].
For researchers designing studies involving protozoan detection, the evidence supports a hybrid approach: validating commercial kits for primary detection while maintaining expertise in in-house methods for troubleshooting and specialized applications. This strategy balances efficiency with flexibility, ensuring reliable results across diverse sample types and research conditions. As molecular diagnostics continue evolving, attention to these foundational steps will remain essential for generating robust, reproducible data in protozoa research.
Multiplex Polymerase Chain Reaction (PCR) has revolutionized molecular diagnostics and research by enabling the simultaneous amplification of multiple nucleic acid targets in a single reaction. This technology dramatically increases throughput while conserving valuable samples and reagents, making it particularly valuable in settings requiring comprehensive pathogen detection or genetic analysis. A critical decision facing researchers and laboratory directors is whether to implement commercial multiplex PCR assays or develop custom in-house alternatives. This choice involves balancing multiple factors, including performance characteristics, regulatory compliance, cost considerations, and technical requirements [45].
The European In Vitro Diagnostic (IVD) Regulation (IVDR; Regulation (EU) 2017/746) has brought this decision into sharper focus, as it requires laboratories to justify the use of in-house assays when CE-IVD-marked commercial kits are available [46]. This comparative guide examines the performance characteristics of both approaches within the specific context of protozoa research, providing experimental data and methodological details to inform evidence-based laboratory decisions.
Performance Comparison: Commercial vs. In-House Assays
Detection of Intestinal Protozoa
A comprehensive Italian multicentre study comparing a commercial AusDiagnostics RT-PCR test with an in-house assay for detecting intestinal protozoa revealed important performance characteristics across different targets. The study analyzed 355 stool samples (230 fresh, 125 preserved) for Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis against conventional microscopy as a reference [1].
Table 1: Performance Comparison for Protozoan Detection
| Target Organism | Commercial vs. In-House Agreement | Performance Notes | Sample Considerations |
|---|---|---|---|
| Giardia duodenalis | Complete agreement | High sensitivity and specificity comparable to microscopy | Consistent performance across sample types |
| Cryptosporidium spp. | High specificity | Limited sensitivity, potentially due to DNA extraction issues | Better results with preserved stools |
| Entamoeba histolytica | Variable | Critical for accurate diagnosis vs. non-pathogenic species | Requires differentiation from E. dispar |
| Dientamoeba fragilis | High specificity | Inconsistent detection | DNA preservation methods crucial |
The study found that molecular methods showed particular promise for fixed fecal specimens, with PCR results from preserved stool samples generally outperforming those from fresh samples, likely due to better DNA preservation. However, the researchers noted that further standardization of sample collection, storage, and DNA extraction procedures is necessary for consistent results across all targets [1].
Detection of Helminths and Other Pathogens
Similar comparative studies have been conducted for other parasitic infections. Research comparing the commercial Biosynex Helminths AMPLIQUICK RT-PCR with an in-house multiplex RT-PCR for diagnosing Schistosoma mansoni and Strongyloides stercoralis found no statistically significant differences in sensitivity and specificity (p = 1). The study analyzed 45 S. mansoni cases with 52 controls and 29 S. stercoralis cases with 54 controls, reporting perfect concordance for controls (AC1 = 1) in both cohorts. However, concordance varied for positive cases, being poor for S. mansoni (AC1 = 0.38) but good for S. stercoralis (AC1 = 0.78) [46].
In respiratory virus detection, a comparison of four multiplex PCR assays (xTAG RVP, Fast-track RP, Easyplex, and an in-house RT-PCR) demonstrated remarkably similar performance, with 93-100% agreement across all comparisons. The study of 213 respiratory specimens found that detection rates ranged from 61.0% to 66.7% across the different assays, leading researchers to conclude that "other issues, such as through-put, technical requirements and cost, are likely to be as important for making a decision about which of these assays to use given their comparative performance" [45].
Table 2: Overall Performance Metrics Across Pathogen Types
| Pathogen Category | Sensitivity Range | Specificity Range | Key Factors Influencing Performance |
|---|---|---|---|
| Intestinal Protozoa | Variable by species | Generally high | DNA extraction efficiency, sample preservation |
| Helminths | No significant difference | No significant difference | Target genes, clinical specimen type |
| Respiratory Viruses | 93-100% agreement | 93-100% agreement | Sample collection method, transport media |
| HIV-1 Drug Resistance | 83.1-93.2% by fragment | High concordance | Viral load, fragment amplified |
For HIV-1 drug resistance testing, an in-house multiplex PCR assay demonstrated higher sensitivity for detecting the integrase (IN) fragment (93.2%) compared to the protease-reverse transcriptase (PR-RT) fragment (83.1%). The assay showed 100% concordance for IN drug resistance mutations compared to reference methods, but lower concordance for PR-RT (87.0%). The authors highlighted this approach as a cost-effective method for HIV-1 drug resistance testing since both PR-RT and IN fragments could be successfully amplified in a single reaction for most samples [47].
Experimental Protocols and Methodologies
DNA Extraction Protocols
Consistent nucleic acid extraction is critical for reliable multiplex PCR results. The protocols below represent standardized approaches used in comparative studies:
Protocol 1: Automated Extraction for Stool Samples
- Mix 350 μL of S.T.A.R. (Stool Transport and Recovery Buffer; Roche) with approximately 1 μL of fecal sample using a sterile loop
- Incubate for 5 minutes at room temperature
- Centrifuge at 2000 rpm for 2 minutes
- Collect 250 μL of supernatant and transfer to a fresh tube
- Add 50 μL of internal extraction control
- Extract DNA using MagNA Pure 96 DNA and Viral NA Small Volume Kit on MagNA Pure 96 System (Roche) [1]
Protocol 2: Manual Extraction with Pre-Extraction Processing
- Place sample in tubes containing beads (MagnaLyzer Green Beads) supplemented with 100 μL of S.T.A.R. buffer and 4 μL of internal control (Phocid alphaherpesvirus 1 - PhHV-1)
- Centrifuge in MagnaLyzer at 3000× g rpm for 30 seconds
- Brief centrifugation at 10,000× g rpm for 10 seconds in centrifuge with 20 cm radius rotor
- Incubate at 95°C for 10 minutes in thermal block
- Vortex for 10 seconds [46]
PCR Amplification Conditions
In-House Multiplex RT-PCR for Intestinal Protozoa
- Reaction mixture: 5 μL of MagNA extraction suspension, 2× TaqMan Fast Universal PCR Master Mix (12.5 μL), primers and probe mix (2.5 μL), and sterile water to final volume of 25 μL
- Multiplex tandem PCR performed using ABI platform [1]
In-House Multiplex PCR for HIV-1 Drug Resistance
- Simultaneous amplification of protease-reverse transcriptase (PR-RT) and integrase (IN) fragments in single reaction
- Evaluation using extracted total nucleic acids from clinical samples
- Sanger sequencing performed on amplicons
- HIV-1 drug-resistance mutations assessed using HIV Stanford drug resistance database [47]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Multiplex PCR
| Reagent/Equipment | Function | Examples/Alternatives |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA/RNA from clinical samples | MagNA Pure 96 (Roche), QIAamp (QIAGEN) |
| PCR Master Mixes | Provides enzymes, buffers, nucleotides for amplification | TaqMan Fast Universal PCR Master Mix |
| Primer/Probe Sets | Target-specific amplification and detection | Custom designs for in-house assays |
| Internal Controls | Monitoring extraction and amplification efficiency | Phocid alphaherpesvirus 1 (PhHV-1) |
| Transport/Preservation Media | Maintain sample integrity during storage/transport | S.T.A.R. Buffer (Roche), Cary-Blair medium |
| Real-time PCR Instruments | Amplification and detection of targets | CFX96 (Bio-Rad), Rotor-Gene 6000 (QIAGEN) |
Cost-Benefit Analysis and Operational Considerations
The decision between commercial and in-house multiplex PCR assays involves significant financial considerations alongside performance metrics. A detailed cost analysis for gastrointestinal pathogen testing revealed that the BioFire FilmArray Gastrointestinal Panel cost approximately €118.15 per test (€115.00 consumables + €3.15 labor), while the GI-EB Screening assay cost approximately €25.43 per test (€19.13 consumables including DNA extraction + €6.30 labor) [48]. This substantial difference highlights the economic appeal of in-house methods, particularly for high-volume testing.
Beyond direct costs, laboratories must consider several operational factors:
Throughput and Workflow Efficiency
- Commercial systems like BioFire FilmArray offer minimal hands-on time (approximately 10 minutes) but process one sample at a time
- In-house methods may require more technical time but enable higher batch processing
- Automated result calling in commercial systems reduces technical interpretation [45]
Regulatory Compliance
- Commercial CE-IVD marked kits simplify regulatory compliance under IVDR
- In-house assays require extensive validation and ongoing quality documentation
- Justification needed for using in-house assays when commercial alternatives exist [46]
Customization and Flexibility
- In-house assays can be tailored to specific research needs or regional pathogen prevalence
- Commercial tests offer standardized, reproducible performance across laboratories
- Ability to modify in-house assays as new targets emerge or pathogen genetics evolve [49]
The comparative data demonstrates that both commercial and in-house multiplex PCR assays can deliver excellent performance when properly validated and implemented. Commercial systems offer advantages in standardization, ease of use, and regulatory compliance, while in-house methods provide cost savings, customization flexibility, and higher throughput potential for batch processing.
For protozoa research specifically, the choice between approaches should consider:
- Target pathogens: Well-characterized targets may perform equally well with either method, while novel or regional variants may require custom designs
- Sample volume: High-volume testing favors in-house methods economically, while low-volume or sporadic testing may benefit from commercial kits
- Technical expertise: In-house development requires significant molecular biology expertise and validation capabilities
- Regulatory environment: IVDR compliance increasingly favors commercial assays unless specific justifications exist
The evolving landscape of molecular diagnostics continues to favor multiplex approaches, with the global multiplex PCR assays market projected to grow from $1.5 billion in 2025 to $3.3 billion by 2035, registering a compound annual growth rate of 8.1% [50]. This growth will likely yield further innovations in both commercial and in-house formats, providing researchers with increasingly sophisticated tools for protozoa detection and characterization.
This guide provides an objective comparison of commercial and in-house PCR assays for detecting pathogenic intestinal protozoa, focusing on analytical performance metrics. Based on a multicentre Italian study, both methodological approaches demonstrate viability but with distinct performance characteristics across different protozoan targets. The data reveals that while commercial and in-house methods show complete agreement for Giardia duodenalis, both exhibit limitations in sensitivity for detecting Cryptosporidium spp. and Dientamoeba fragilis, largely due to challenges in DNA extraction from resilient parasite structures. These findings underscore that molecular diagnostics offer significant advantages over traditional microscopy but require further standardization to achieve consistent performance across all protozoan targets [1].
Performance Data Comparison
The following tables summarize key quantitative performance data from a multicentre comparison study involving 18 Italian laboratories [1].
Table 1: Overall Sample Analysis and Method Agreement
| Parameter | Value |
|---|---|
| Total Stool Samples Analyzed | 355 [1] |
| Fresh Stool Samples | 230 [1] |
| Preserved Stool Samples (Para-Pak) | 125 [1] |
| Commercial RT-PCR Test | AusDiagnostics [1] |
| Comparison Method | In-house RT-PCR & Microscopy [1] |
| Agreement for G. duodenalis | Complete agreement between commercial and in-house PCR [1] |
Table 2: Performance Characteristics by Target Protozoan
| Protozoan Target | Sensitivity | Specificity | Key Findings and Notes |
|---|---|---|---|
| Giardia duodenalis | High [1] | High [1] | Complete agreement between both PCR methods; performance similar to microscopy [1]. |
| Cryptosporidium spp. | Limited [1] | High [1] | Limited sensitivity likely due to inadequate DNA extraction from the oocyst [1]. |
| Dientamoeba fragilis | Limited [1] | High [1] | Inconsistent detection; sensitivity issues potentially linked to DNA extraction [1]. |
| Entamoeba histolytica | Information Not Specified | Information Not Specified | Molecular assays are critical for accurate diagnosis versus non-pathogenic Entamoeba species [1]. |
Detailed Experimental Protocols
Multicentre Study Design and Sample Collection
The performance data cited in this guide originates from a comprehensive multicentre study [1].
- Participating Centers: 18 microbiological laboratories across Italy (12 in northern regions, 3 central, 3 southern) [1].
- Sample Collection: A total of 355 consecutive stool samples were collected over six months [1].
- Sample Preparation: Samples were divided into 230 fresh stools and 125 stools preserved in Para-Pak media [1].
- Reference Method: All samples underwent conventional microscopic examination per WHO and CDC guidelines. Fresh samples were stained with Giemsa, while fixed samples were processed using the formalin-ethyl acetate (FEA) concentration technique [1].
Nucleic Acid Extraction Protocol
The DNA extraction method was consistent across compared molecular tests [1]:
- Homogenization: Approximately 1 µL of fecal sample was mixed with 350 µL of Stool Transport and Recovery Buffer (S.T.A.R. Buffer, Roche) using a sterile loop and incubated for 5 minutes at room temperature [1].
- Clarification: The mixture was centrifuged at 2000 rpm for 2 minutes [1].
- Supernatant Collection: 250 µL of supernatant was transferred to a new tube and spiked with 50 µL of an internal extraction control [1].
- Automated Extraction: Nucleic acids were extracted using the MagNA Pure 96 DNA and Viral NA Small Volume Kit on the MagNA Pure 96 System (Roche), a fully automated instrument based on magnetic bead separation [1].
PCR Amplification and Detection
The study compared two primary molecular approaches [1]:
- Commercial PCR Assay: The AusDiagnostics commercial RT-PCR test was used according to the manufacturer's instructions [1].
- In-house PCR Assay: A previously validated in-house RT-PCR assay from the Microbiology Unit of Padua Hospital was employed. The reaction mixture consisted of:
- 5 µL of extracted nucleic acid
- 12.5 µL of 2× TaqMan Fast Universal PCR Master Mix
- 2.5 µL of primer and probe mix
- Sterile water to a final volume of 25 µL [1]
Workflow Visualization
The diagram below illustrates the key stages of the comparative study protocol.
Multicentre PCR Comparison Workflow
Research Reagent Solutions
Table 3: Essential Materials and Reagents for Protozoan PCR
| Item | Function/Description | Example Brand/Type |
|---|---|---|
| Stool Transport Buffer | Preserves nucleic acids and facilitates sample homogenization for downstream DNA extraction. | S.T.A.R. Buffer (Roche) [1] |
| Automated Nucleic Acid Extractor | Performs automated, high-throughput purification of DNA from complex stool matrices. | MagNA Pure 96 System (Roche) [1] |
| DNA Extraction Kit | Provides reagents for magnetic bead-based separation and purification of nucleic acids. | MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche) [1] |
| Commercial PCR Kit | Integrated reagent system optimized for specific protozoan targets; offers standardization. | AusDiagnostics RT-PCR Test [1] |
| Master Mix | Contains enzymes, dNTPs, and buffers essential for the PCR amplification reaction. | TaqMan Fast Universal PCR Master Mix [1] |
| Sample Preservation Media | Maintains parasite integrity and nucleic acid stability for later analysis. | Para-Pak Media [1] |
Solving Common PCR Challenges: Inhibition, Sensitivity, and Standardization
Overcoming PCR Inhibition from Fecal Samples
The shift from traditional microscopy to molecular diagnostics, particularly Polymerase Chain Reaction (PCR), represents a paradigm shift in the detection of pathogenic intestinal protozoa. Protozoan parasites such as Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica are significant causes of diarrheal diseases, affecting approximately 3.5 billion people globally each year [1]. While PCR offers superior sensitivity and specificity compared to conventional microscopy, its effectiveness is substantially compromised by PCR inhibitors present in complex sample matrices like human feces [51]. These inhibitory substances, including bile salts, complex carbohydrates, and proteins, can bind to template DNA, inhibit DNA polymerase activity, or chelate essential magnesium co-factors, leading to false-negative results and reduced analytical sensitivity [52]. Overcoming this challenge is crucial for accurate diagnosis, particularly in the context of comparing commercial versus in-house PCR assays for protozoa research. This guide provides a comprehensive comparison of strategies to mitigate PCR inhibition, enabling researchers to make informed decisions about their molecular diagnostic approaches.
Understanding PCR Inhibition in Fecal Samples
Fecal samples represent one of the most challenging matrices for molecular diagnostics due to their complex composition. Numerous substances have been identified as potential PCR inhibitors, including bile salts, complex polysaccharides, hemoglobin, heparin, urea, and various metabolic byproducts [51] [52]. The impact of these inhibitors can be profound, with studies showing that untreated fecal homogenate can completely inhibit PCR even after 1,000-fold dilution in water [51]. The diagnostic implications are significant, as inhibition can reduce test sensitivity; for example, in one study, relief of inhibition through dilution increased the sensitivity of a quantitative PCR test for Mycobacterium avium subspecies paratuberculosis from 55% to 80% compared to fecal culture [52].
Detection of Inhibition
Implementing internal amplification controls (IACs) is essential for distinguishing true negative results from false negatives due to PCR inhibition. Many commercial and in-house assays incorporate IACs, such as phocine herpesvirus (PhHV), which are added to each sample prior to DNA extraction [53]. The failure to amplify the IAC indicates the presence of inhibitors in the reaction. Furthermore, DNA extracts with higher DNA and protein content have been shown to have significantly higher odds (19.33 and 10.94 times, respectively) of showing inhibition, providing potential predictive parameters for identifying problematic samples [52].
Comparative Performance: Commercial vs. In-House PCR Methods
Methodological Approaches to Overcoming Inhibition
Both commercial and in-house PCR assays employ various strategies to mitigate the effects of PCR inhibitors. A recent multicentre study comparing a commercial RT-PCR test (AusDiagnostics) with an in-house RT-PCR assay demonstrated that both methods showed complete agreement for detecting G. duodenalis, with high sensitivity and specificity similar to conventional microscopy [1]. However, for other protozoa like Cryptosporidium spp. and Dientamoeba fragilis, both methods showed high specificity but limited sensitivity, likely due to inadequate DNA extraction from the parasite's robust wall structure [1].
Table 1: Performance Comparison of Commercial vs. In-House PCR Methods for Protozoan Detection
| Parasite | Commercial PCR Performance | In-House PCR Performance | Key Challenges |
|---|---|---|---|
| Giardia duodenalis | Complete agreement with in-house PCR; high sensitivity and specificity [1] | Complete agreement with commercial PCR; high sensitivity and specificity [1] | Less challenging for DNA extraction |
| Cryptosporidium spp. | High specificity but limited sensitivity [1] | High specificity but limited sensitivity [1] | Inadequate DNA extraction from oocysts |
| Entamoeba histolytica | Critical for accurate diagnosis; enables differentiation from non-pathogenic species [1] | Essential for species-level differentiation [1] [53] | Microscopy cannot differentiate pathogenic from non-pathogenic species |
| Dientamoeba fragilis | Inconsistent detection [1] | Inconsistent detection [1] | DNA extraction challenges |
| Multiple protozoa | High specificity but variable sensitivity by target DNA [54] | Detected parasites in more samples than commercial kits in one study [53] | Co-contamination issues in environmental samples |
Sample Preservation and Processing
The method of sample preservation significantly impacts PCR efficiency. Studies have demonstrated that PCR results from preserved stool samples were generally better than those from fresh samples, likely due to better DNA preservation in the former [1]. For environmental samples like water, processing methods must be optimized based on the sample type; for instance, stomaching with a glycine buffer was optimal for oocyst recovery in leafy herbs with soft stems, while aromatic woody-stemmed herbs required orbital shaking to minimize the release of PCR inhibitors [42].
Technical Solutions and Experimental Protocols
DNA Extraction and Purification Methods
Effective DNA extraction is a critical first step in overcoming PCR inhibition. Several methods have been developed specifically for this purpose:
Aqueous Two-Phase System (ATPS): This method utilizes a system composed of 8% (w/w) polyethylene glycol 4000 and 11% (w/w) dextran 40 to remove PCR-inhibitory substances. The majority of PCR-inhibitory substances, including bile salts, distribute in the polyethylene glycol-rich top phase, while target bacteria are detected in the dextran-rich bottom phase [51]. This system has been shown to decrease the detection level by three to five orders of magnitude compared to untreated samples [51].
Cationic Surfactant-Based Extraction: Catrimox-14, a cationic surfactant, has been successfully applied to eliminate PCR-inhibitory substances from animal fecal specimens. This method enabled the detection of canine parvovirus in fecal specimens from 13 different animal species, whereas pretreatment by gel-filtration or boiling failed to remove inhibitors from samples from mouse, goat, rat, and sheep [55].
Magnetic Separation Systems: Automated systems like the MagNA Pure 96 System (Roche Applied Sciences) using magnetic separation of nucleic acid-bead complexes have been employed in multicentre studies for consistent DNA extraction [1]. Prior to extraction, samples are often mixed with Stool Transport and Recovery Buffer (S.T.A.R. Buffer; Roche) to stabilize nucleic acids.
PCR Amplification Strategies
Once inhibitors have been addressed through extraction methods, several amplification strategies can further enhance detection:
Dilution of DNA Extracts: Simple dilution of DNA extracts (e.g., five-fold dilution) can relieve inhibition by reducing the concentration of inhibitors to sub-critical levels. This approach has been shown to increase test sensitivity significantly, from 55% to 80% in one study [52].
Polymerase Selection: Different polymerase enzymes exhibit varying susceptibility to PCR inhibitors. Selecting polymerases with higher resistance to inhibitors can improve amplification efficiency [52].
Multiplex PCR Optimization: For commercial multiplex PCR kits, optimization of reaction volumes and components can enhance performance. One study implemented duplex qPCR assays using a 10 µL reaction volume, reducing costs while maintaining detection efficiency [21].
The following workflow diagram illustrates a comprehensive approach to managing PCR inhibition in fecal samples:
Figure 1: Comprehensive Workflow for Managing PCR Inhibition in Fecal Samples
Commercial Kit Performance
Evaluation of commercial multiplex PCR kits reveals variable performance in handling inhibition. One study comparing three commercial multiplex real-time PCR (MT-PCR) kits found that in-house assays detected parasites in more samples from patients suspected of having parasitosis than did any of the kits [53]. However, another study reported that a commercial multiplex real-time PCR kit proved to be highly specific, enabling the detection of E. histolytica and a subset of Cryptosporidium spp., while finding 10 times more samples contaminated with G. lamblia than direct immunofluorescence assay (DFA) [54].
Table 2: Comparison of Inhibition Management in Commercial PCR Kits
| Commercial Kit | Inhibition Management Features | Performance Notes | Reference |
|---|---|---|---|
| AusDiagnostics Company | Used in multicentre comparison; automated DNA extraction | Complete agreement with in-house PCR for G. duodenalis; limited sensitivity for Cryptosporidium and D. fragilis | [1] |
| RIDAGENE Parasitic Stool Panel | Includes internal control DNA | Performance varies; may detect fewer positives than in-house methods | [53] |
| LightMix Modular Gastroenteritis Assays | Includes internal control DNA | Performance varies; may detect fewer positives than in-house methods | [53] |
| BD MAX Enteric Parasite Panel | Integrated DNA extraction on BD MAX system | Performance varies; may detect fewer positives than in-house methods | [53] |
| Unspecified MRT-PCR | Internal amplification control | Highly specific; 10x more sensitive than DFA for G. lamblia; substantial agreement with nPCR | [54] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Overcoming PCR Inhibition
| Reagent/Category | Specific Examples | Function/Application | Reference |
|---|---|---|---|
| DNA Extraction Systems | MagNA Pure 96 System (Roche), NucliSENS easyMAG (bioMérieux) | Automated nucleic acid purification with minimal inhibitor carryover | [1] [53] |
| Inhibition Removal Reagents | Catrimox-14, Polyethylene glycol 4000/Dextran 40 ATPS | Cationic surfactant or polymer system to separate inhibitors from target DNA | [51] [55] |
| Sample Transport Media | S.T.A.R. Buffer (Roche), Para-Pak preservation media | Stabilize nucleic acids and maintain sample integrity during storage/transport | [1] |
| Specialized PCR Master Mixes | TaqMan Fast Universal PCR Master Mix (2×), No AmpErase UNG | Optimized buffer formulations with enhanced resistance to inhibitors | [1] [53] |
| Internal Amplification Controls | Phocine Herpesvirus (PhHV), kit-specific internal controls | Distinguish true negatives from inhibition-related false negatives | [53] |
| Sample Wash Buffers | Glycine buffer, Elution solution (0.01% chemical not specified) | Remove inhibitors during sample processing, especially for complex matrices | [42] |
overcoming PCR inhibition in fecal samples requires a multifaceted approach that combines appropriate sample collection, effective DNA extraction methods, and optimized amplification strategies. Both commercial and in-house PCR methods face challenges with inhibitor management, but the choice between them depends on specific research needs. Commercial kits offer standardization and convenience, while in-house methods provide flexibility for optimization. The key to success lies in understanding the sources of inhibition, implementing appropriate controls, and selecting the most suitable combination of methods for the specific research context. As molecular diagnostics continue to evolve, further standardization of sample collection, storage, and DNA extraction procedures will be necessary for consistent results across different laboratory settings [1].
Optimizing DNA Extraction from Robust Protozoan Cysts and Oocysts
Molecular diagnostics for intestinal protozoa are increasingly vital in clinical and research settings, yet the robust walls of protozoan cysts and oocysts present significant challenges for DNA extraction. Efficient lysis of these structures is the critical first step determining the success of downstream molecular applications, from routine PCR to advanced metagenomic sequencing. This guide systematically compares commercial and in-house DNA extraction methods, evaluating their performance across different protozoan parasites to identify optimal protocols for research and diagnostic purposes.
The resistance of protozoan cysts and oocysts stems from their complex structural compositions. Giardia cysts possess a filamentous outer layer, Cryptosporidium oocysts have a robust bilayered wall, and microsporidian spores contain chitin-rich exteriors, all requiring specialized disruption techniques [1] [56]. Inefficient DNA extraction from these pathogens remains a primary limitation in molecular detection, often leading to false-negative results and underestimation of parasite prevalence [1] [57].
Performance Comparison of DNA Extraction Methods
Commercial Kits Versus In-House Methods
Recent multicenter evaluations demonstrate that both commercial and in-house methods can effectively extract DNA from intestinal protozoa, but their performance varies significantly by target organism and specific protocols.
Table 1: Comparative Performance of Molecular Methods for Protozoan Detection
| Parasite | Method Type | Sensitivity | Specificity | Key Findings | Reference |
|---|---|---|---|---|---|
| Giardia duodenalis | Commercial & In-house RT-PCR | High | High | Complete agreement between methods; performance similar to microscopy | [1] |
| Cryptosporidium spp. | Commercial & In-house RT-PCR | Limited | High | Reduced sensitivity due to inadequate DNA extraction from oocysts | [1] |
| Dientamoeba fragilis | Commercial & In-house RT-PCR | Inconsistent | High | Detection inconsistency across methods | [1] |
| Entamoeba histolytica | Commercial & In-house RT-PCR | Critical for diagnosis | High | Molecular methods essential for differentiation from non-pathogenic species | [1] |
| Multiple enteric protozoa | Five commercial kits | Variable | Variable | Performance depended on parasite species and infection burden | [57] |
A 2025 Italian multicenter study comparing commercial AusDiagnostics RT-PCR with an in-house method revealed complete concordance for Giardia duodenalis detection, with both demonstrating high sensitivity and specificity comparable to microscopy [1]. However, for Cryptosporidium spp. and Dientamoeba fragilis, both methods showed high specificity but limited sensitivity, which authors attributed to inadequate DNA extraction from the parasite structures [1].
Another evaluation of five commercial DNA extraction kits (QIAamp DNA Stool Mini, SpeedTools DNA Extraction, DNAExtract-VK, PowerFecal DNA Isolation, and Wizard Magnetic DNA Purification) found that all yielded amplifiable DNA, but performance varied significantly depending on the target parasite and infection intensity [57]. Methods combining chemical, enzymatic, and mechanical lysis at temperatures ≥56°C proved most efficient for releasing Cryptosporidium DNA [57].
Impact of Sample Preservation on DNA Yield
Sample preservation methods significantly impact DNA extraction efficiency. The 2025 multicenter study found superior PCR results from preserved stool samples compared to freshly processed specimens, likely due to better DNA preservation in fixed samples [1]. Similarly, research on neonatal gut microbiota profiling observed that DNA yields decreased most dramatically within the first 24 hours of storage post-collection [58].
Bead-beating-based kits (PowerSoil and ZymoBIOMICS) consistently outperformed the QIAamp Fast DNA Stool Mini kit, which produced negligible yields across all conditions [58]. Both bead-beating kits achieved highest DNA concentrations with fresh processing without preservatives, while yields declined sharply after just one day of storage [58].
Optimizing Mechanical Pretreatment Protocols
Bead-Beating Parameters
Mechanical disruption through bead-beating represents a crucial step for breaching resilient protozoan walls. A comprehensive 2024 study systematically evaluated parameters for optimizing Enterocytozoon bieneusi spore disruption, with findings applicable to other robust protozoan forms [56].
Table 2: Mechanical Pretreatment Optimization for Protozoan DNA Extraction
| Parameter | Optimal Conditions | Effect on DNA Yield | Key Findings |
|---|---|---|---|
| Grinding Speed | 30 Hz | Highest DNA yield | Lower speeds insufficient for complete disruption; higher speeds may cause excessive DNA shearing |
| Grinding Duration | 60 seconds | Optimal balance between disruption and DNA integrity | Longer durations (180 s) showed no significant improvement |
| Bead Types | ZR BashingBeads or MP Lysing Matrix E | Superior to glass beads alone | Small, heterogeneous beads (0.1-2.0 mm) most effective |
| Equipment | TissueLyser II (Qiagen) | Consistent performance | Standardized oscillation critical for reproducibility |
| Spore Concentration | All levels (50-50,000/mL) | Improved detection, especially at medium loads | Ct gain most pronounced at medium spore loads (5,000/mL) |
The study compared seven extraction methods incorporating various mechanical pretreatment approaches. Methods utilizing the TissueLyser II (Qiagen) at 30 Hz for 60 seconds with commercial beads (ZR BashingBeads or MP Lysing Matrix E) demonstrated superior performance, particularly for samples with low microsporidia loads [56]. The optimal protocol employed a "strong but short bead beating" approach, effectively disrupting the chitinous spore walls while minimizing DNA fragmentation.
Bead Composition and Size
Bead composition significantly influences disruption efficiency. The 2024 study found that commercial beads specifically formulated for microbial lysis (ZR BashingBeads or MP Lysing Matrix E) outperformed homogeneous glass beads across multiple spore concentrations [56]. These specialized beads typically contain a mixture of different sizes (0.1-2.0 mm) and materials (ceramic, silica, zirconium), creating more effective shear forces for breaking resistant parasite walls.
For Cryptosporidium oocysts, which possess particularly robust bilayered walls, methods combining chemical, enzymatic, and mechanical lysis procedures at temperatures of at least 56°C proved most efficient [57]. The integration of multiple disruption mechanisms appears essential for overcoming the structural diversity among different protozoan species.
DNA Extraction Workflow for Protozoan Cysts and Oocysts
The following workflow diagram summarizes the optimal DNA extraction process for robust protozoan cysts and oocysts, integrating the most effective methods identified in comparative studies:
Research Reagent Solutions Toolkit
Table 3: Essential Reagents for Optimal Protozoan DNA Extraction
| Reagent Category | Specific Products | Application & Function | Performance Notes |
|---|---|---|---|
| Bead-Beating Kits | DNeasy PowerSoil Pro, ZymoBIOMICS DNA Miniprep | Mechanical disruption of resistant walls | Consistently outperformed non-bead methods; higher DNA yields [58] |
| Commercial DNA Extraction Kits | QIAamp DNA Stool Mini, SpeedTools DNA Extraction, PowerFecal DNA Isolation | DNA purification and inhibitor removal | Performance varies by parasite; combination methods most effective [57] |
| Mechanical Disruption Beads | ZR BashingBeads, MP Lysing Matrix E | Heterogeneous beads for optimal lysis | Superior to homogeneous glass beads; various sizes (0.1-2.0mm) [56] |
| Lysis Buffers | Buffer C (200mM Tris, 25mM EDTA, Tween-20, Proteinase K) | Chemical and enzymatic degradation | Effective for museum specimens; applicable to resistant forms [59] |
| Automated Systems | Nuclisens easyMAG, MagNA Pure 96 | Standardized, high-throughput processing | Good performance for microsporidia; reduces cross-contamination [56] |
Discussion and Future Perspectives
The optimization of DNA extraction from robust protozoan cysts and oocysts remains a dynamic field, with bead-beating emerging as a critical enhancement to traditional chemical lysis methods. While commercial kits offer standardization and convenience, in-house methods allow customization for specific research needs and parasite targets. The optimal approach depends on the specific protozoan target, sample type, and available resources.
Future developments will likely focus on integrating multiple disruption mechanisms, adapting methods from related fields such as food safety testing where efficient parasite detection from complex matrices like lettuce has been achieved through innovative lysis techniques [60]. The OmniLyse device, for instance, has demonstrated rapid (3-minute) lysis of oocysts and cysts for metagenomic detection of foodborne parasites [60].
Standardization of extraction protocols across laboratories will enhance reproducibility and comparability of research findings. As molecular diagnostics continue to replace microscopic examination in clinical settings, refined DNA extraction methods will play an increasingly crucial role in accurate parasite detection and differentiation [1] [61]. The consistent finding that DNA extraction efficiency significantly impacts detection sensitivity underscores the need for continued optimization and validation of extraction methods specifically for protozoan parasites.
The accurate diagnosis of intestinal protozoan parasites is a cornerstone of public health, clinical management, and research in infectious diseases. The choice of how to handle stool specimens—whether to analyze them fresh or to use a fixed preservative—profoundly impacts the downstream diagnostic results, particularly with the growing use of molecular methods like PCR. This guide objectively compares the performance of fresh versus fixed stool samples within the context of a broader thesis comparing commercial and in-house PCR assays. The selection of sample preservation method is not merely a logistical step but a critical analytical variable that influences DNA yield, pathogen detectability, and the feasibility of integrating different diagnostic platforms in both well-resourced and remote settings.
Comparative Analysis: Fresh vs. Fixed Stool Samples
The decision between using fresh or fixed stool samples involves trade-offs between diagnostic speed, morphological integrity, molecular stability, and logistical practicality. The table below summarizes the core characteristics of each approach.
Table 1: Fundamental Characteristics of Fresh and Fixed Stool Samples
| Feature | Fresh Stool Samples | Fixed Stool Samples |
|---|---|---|
| Primary Definition | Unpreserved, analyzed immediately or refrigerated for a short period [62] | Stool mixed with a chemical preservative (e.g., formalin, SAF, ethanol, PVA) for storage [63] |
| Optimal Use Case | Observation of motile trophozoites; rapid antigen testing [62] [64] | Long-term storage and transport; biobanking; high-volume batch testing [63] [12] |
| Key Advantage for Microscopy | Allows observation of parasite motility [62] [65] | Excellent preservation of morphological detail for eggs and cysts [63] [66] |
| Key Advantage for Molecular Diagnostics | Potentially higher initial DNA quality (if processed immediately) [12] | Protects DNA/RNA from nucleases during storage and transport; enables retrospective studies [67] [12] |
| Main Disadvantage | Rapid degradation of parasites and DNA; stringent time constraints for processing [62] [64] | Some fixatives (e.g., formalin) can fragment DNA and inhibit PCR; toxicity of some agents [67] [63] [68] |
Impact on Diagnostic Sensitivity and Workflow
The method of sample preservation directly affects the sensitivity of diagnostic assays. A comparative study found that examining sodium acetate-acetic acid-formalin (SAF)-preserved specimens, which involved analyzing both concentrated sediment and a permanent stained smear, identified intestinal protozoa in 149 out of 247 patients. In stark contrast, the conventional examination of unpreserved specimens detected protozoa in only 89 of the same 247 patients [66]. This demonstrates a significant increase in the chance of recovering intestinal protozoa with a fixed-preservation system.
Furthermore, a 2025 multicentre study evaluating PCR methods noted that molecular results from preserved stool samples were superior to those from fresh samples. The authors concluded that this was likely due to better DNA preservation in the fixed samples, which stabilizes nucleic acids against degradation during storage and transport prior to DNA extraction [12].
Table 2: Impact of Preservation on Specific Diagnostic Outcomes
| Study Focus | Performance of Fresh Samples | Performance of Fixed Samples | Key Finding |
|---|---|---|---|
| Protozoa Detection (Microscopy) | Identified protozoa in 89/247 patients (36%) [66] | Identified protozoa in 149/247 patients (60%) [66] | Fixed samples (SAF) increased detection rate by ~67% |
| DNA Quality for PCR | Risk of degradation without immediate freezing; variable quality in fresh-frozen samples shipped internationally [69] [12] | Better DNA preservation during storage/transport; commercial PCR kits validated for fixed samples [67] [12] | Fixed samples provide more stable DNA for molecular assays in multi-site studies |
| Helminth Egg DNA Recovery | Fresh freezing is the "gold standard" but often impractical in the field [67] [69] | Low-cost DESS buffer showed better sensitivity and higher inferred egg abundance than fresh freezing in one field study [69] | Certain chemical preservatives can outperform fresh freezing in field conditions |
Experimental Protocols for Preservation Comparison
To generate reliable data when comparing commercial and in-house PCR assays, standardizing the evaluation of sample preservation is crucial. Below is a detailed methodological framework based on cited studies.
Protocol 1: Systematic Comparison of Multiple Preservatives for PCR
This protocol is adapted from a 2018 study designed to evaluate the effectiveness of various preservatives for hookworm DNA detection via quantitative real-time PCR (qPCR) [67].
- Sample Preparation: A naïve human stool sample from a single donor is spiked with a known quantity of parasite eggs (e.g., Necator americanus) to create a homogeneous, characterized material [67].
- Preservation and Storage Conditions:
- Tested Preservatives: The study should include 95% ethanol, RNA later, PAXgene, FTA cards, potassium dichromate, silica bead desiccation, and a "no preservative" control [67].
- Storage Temperatures and Duration: Aliquots of spiked stool for each preservative are stored at two temperatures: 4°C (refrigerated) and 32°C (simulating tropical ambient temperature). Samples are analyzed at multiple time points, for example, on days 1, 7, 30, and 60 [67].
- Control: A "gold standard" control is established by rapidly freezing aliquots at -20°C or -80°C [67].
- DNA Extraction and qPCR Analysis:
- At each time point, DNA is extracted from replicate samples using a standardized kit or method suitable for complex stools [67] [12].
- The extracted DNA is subjected to a targeted qPCR assay (e.g., for a hookworm-specific gene). The primary outcome measure is the quantification cycle (Cq) value. A smaller increase in Cq value over time indicates better preservation of the target DNA [67].
Protocol 2: Morphological vs. Molecular Preservation in Ethanol vs. Formalin
This protocol, inspired by a 2024 study on primate samples, is ideal for research requiring both microscopic and molecular data from the same specimen [68].
- Sample Collection and Partitioning: Fresh fecal samples are collected and immediately divided into two equal portions [68].
- Dual Preservation:
- Downstream Analysis:
- Morphological Assessment: Formalin-preserved samples are processed using a sedimentation concentration technique. Parasites are identified microscopically and rated for preservation quality using a standardized degradation grading scale (e.g., 1-3 based on cuticle integrity and clarity of internal structures for larvae, and shell intactness for eggs) [68].
- Molecular Assessment: DNA is extracted from the ethanol-preserved halves and subjected to in-house and commercial PCR assays for target protozoa. The success of PCR amplification, DNA yield, and Cq values are compared [68].
The following workflow diagram illustrates the key decision points and procedures for selecting and processing fresh versus fixed stool samples in a research setting, based on the described protocols.
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the appropriate preservatives and reagents is fundamental to designing robust experiments for comparing commercial and in-house PCR tests. The table below details key solutions used in the featured research.
Table 3: Essential Reagents for Stool Sample Preservation and Analysis
| Research Reagent | Primary Function | Key Considerations for Protozoa PCR Research |
|---|---|---|
| 95% Ethanol | A fixative and preservative that dehydrates tissues and inactivates nucleases [67] [68] | Considered a pragmatic, effective choice for DNA preservation in field settings; less toxic than alternatives; suitable for both STH and protozoa [67]. |
| SAF (Sodium Acetate-Acetic Acid-Formalin) | An all-purpose fixative for concentration procedures and permanent staining [63] | Compatible with immunoassays and some molecular techniques; studies show superior protozoa detection vs. fresh samples [63] [66]. |
| RNAlater | A commercial, aqueous solution that stabilizes and protects cellular RNA and DNA [67] | Effective at minimizing Cq value increases for DNA targets at elevated temperatures; can be more expensive than in-house options [67]. |
| Formalin (10%) | A cross-linking fixative that preserves morphological structure [62] [63] | The gold standard for morphological preservation but can fragment DNA and inhibit PCR, complicating molecular assays [63] [68]. |
| DESS Buffer | A salt-based buffer (DMSO, EDTA, NaCl) for tissue/DNA preservation [69] | A low-cost, non-toxic in-house solution; shown to effectively preserve STH DNA and gut microbiota for 16S sequencing [69]. |
| Para-Pak / Commercial Kits | Integrated collection systems often containing multiple vials with different preservatives [12] | Standardizes sample collection; specific media (e.g., Para-Pak) have been successfully used in multicentre PCR studies [12]. |
| S.T.A.R. Buffer | A stool transport and recovery buffer for DNA extraction [12] | Used to homogenize stool samples prior to automated nucleic acid extraction, improving DNA yield and consistency for PCR [12]. |
Implications for Commercial vs. In-House PCR Assays
The choice between fresh and fixed samples directly influences the validation and performance of commercial and in-house PCR assays.
- Assay Validation and Compatibility: Commercial PCR kits often undergo extensive validation using specific preservation media. For instance, the AusDiagnostics test showed reliable performance with samples preserved in Para-Pak media [12]. In-house assays offer the flexibility to be optimized for a wider range of preservatives, including low-cost in-house solutions like DESS buffer [69] or 95% ethanol [67], which can be crucial for large-scale field studies.
- Inhibitor Resistance and DNA Quality: Fixed samples, especially those in formalin, can introduce PCR inhibitors or contain fragmented DNA [67] [68]. A well-optimized in-house PCR protocol may include additional purification steps or inhibitor-resistant polymerases to overcome this. Commercial kits provide a standardized, often optimized extraction and amplification system but may be less adaptable to specific challenges posed by certain fixatives.
- Standardization vs. Flexibility in Multi-Centre Studies: For multi-centre research, the use of fixed samples in standardized commercial collection kits minimizes pre-analytical variability, ensuring that samples from different sites are comparable [12]. This is a significant advantage for commercial PCR platforms. In-house assays, while potentially more variable, allow researchers to tailor the entire workflow—from preservation to amplification—to the specific constraints and goals of their study, such as prioritizing low cost or maximizing sensitivity for a particular parasite [67] [69].
The decision between using fresh or fixed stool samples is a foundational one that resonates through all subsequent diagnostic and research steps. While fresh samples are indispensable for observing motile trophozoites, fixed samples provide a robust, practical, and often more sensitive alternative for most research applications, especially those involving molecular techniques. The experimental data clearly demonstrates that fixed preservation can significantly enhance the detection of intestinal protozoa compared to fresh samples.
For researchers comparing commercial and in-house PCR assays, the preservation method is a critical variable of the protocol. Commercial tests benefit from the standardization offered by approved fixation kits, whereas in-house methods provide the adaptability to leverage a wider array of preservatives, including cost-effective and non-toxic options, without compromising diagnostic sensitivity. Therefore, the optimal choice is not a matter of which method is universally superior, but which system—fresh or fixed, commercial or in-house—is most appropriately matched to the specific research objectives, logistical constraints, and target pathogens.
Addressing Variable Sensitivity Across Protozoan Targets
Molecular diagnostics, particularly real-time PCR (qPCR), have revolutionized the detection of intestinal protozoan parasites, offering significant advantages over traditional microscopy in specificity and throughput [1] [70]. However, a critical challenge persists: no single molecular assay demonstrates uniformly high sensitivity across all major protozoan targets. Performance varies considerably between organisms such as Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis [1] [4]. This variability presents a significant hurdle for researchers and clinicians who require reliable, comprehensive diagnostic tools. The core of the issue often lies in the intricate balance between assay chemistry, DNA extraction efficiency from robust parasite structures, and the genetic diversity of the target organisms [1] [70]. This guide objectively compares the performance of commercial and in-house PCR assays, providing the experimental data and protocols necessary to inform selection and optimization for specific research objectives.
Comparative Performance Data of Molecular Assays
Understanding the variable sensitivity profiles of different PCR methods is fundamental for selecting the appropriate tool for a specific research context. The data below, synthesized from recent comparative studies, highlights that while some protozoa are reliably detected, others remain challenging.
Table 1: Comparative Sensitivity of PCR Assays Across Protozoan Targets
| Protozoan Target | Commercial qPCR Performance | In-House qPCR Performance | Key Factors Influencing Sensitivity |
|---|---|---|---|
| Giardia duodenalis | High sensitivity and specificity; complete agreement with in-house methods [1] [4]. | High sensitivity and specificity; performs well comparable to microscopy [1] [4]. | Robust DNA extraction; less genetic variation impacting primer binding [1]. |
| Cryptosporidium spp. | High specificity, but can exhibit limited sensitivity [1] [4]. | High specificity, but can exhibit limited sensitivity [1]. | Inadequate DNA extraction from hardy oocysts is a major limiting factor [1]. |
| Entamoeba histolytica | Critical for accurate diagnosis; enables differentiation from non-pathogenic E. dispar [1] [21]. | Critical for accurate diagnosis; enables differentiation from non-pathogenic E. dispar [1]. | Primer/probe specificity is essential to distinguish from morphologically identical species [21] [70]. |
| Dientamoeba fragilis | High specificity, but detection can be inconsistent with limited sensitivity [1] [4]. | High specificity, but detection can be inconsistent with limited sensitivity [1]. | Inconsistent detection, potentially due to inadequate DNA extraction [1]. |
| Blastocystis spp. | Detected by specialized in-house and commercial panels [21]. | Reliably detected by implemented qPCR assays [21]. | Generally well-detected; prevalence can be high in certain regions [21]. |
| Chilomastix mesnili | Not widely included in commercial panels. | Can be detected with newly designed assays; first qPCR detection reported [21]. | Newly designed primers/probes based on conserved 18S rRNA regions [21]. |
Beyond the core targets, the sample type itself significantly influences the result. A multicentre study found that PCR results from preserved stool samples were generally better than those from fresh samples, likely due to superior DNA preservation in fixation media [1]. Furthermore, multiplexing assays to detect multiple pathogens simultaneously is a key advancement. One study implemented a duplex qPCR for Entamoeba dispar + E. histolytica and another for Cryptosporidium spp. + Chilomastix mesnili, alongside singleplex assays for other targets, using a reduced 10 µL reaction volume to enhance cost-effectiveness [21].
Experimental Protocols and Methodologies
The data presented in the previous section are derived from rigorous experimental designs. Reproducing or critically evaluating these findings requires a detailed understanding of the underlying methodologies.
Multicenter Comparison Protocol (Commercial vs. In-House PCR)
A 2025 multicentre study involving 18 Italian laboratories provides a robust framework for comparing commercial and in-house assays [1] [4].
- Study Design: The study analyzed 355 stool samples (230 fresh, 125 preserved) using traditional microscopy as a reference. All samples were subsequently tested with a commercial RT-PCR test (AusDiagnostics) and a validated in-house RT-PCR assay.
- DNA Extraction: A standardized protocol was employed. Briefly, 350 µL of Stool Transport and Recovery Buffer (S.T.A.R. Buffer) was mixed with a small aliquot of fecal sample. After centrifugation, the supernatant was combined with an internal extraction control. DNA was then purified using the MagNA Pure 96 DNA and Viral NA Small Volume Kit on a MagNA Pure 96 System, a fully automated platform for nucleic acid preparation [1].
- In-House PCR Amplification: The in-house reaction mixture included 5 µL of extracted DNA, 2× TaqMan Fast Universal PCR Master Mix, a custom primers and probe mix, and sterile water to a final volume of 25 µL. A multiplex tandem PCR was performed [1].
- Commercial PCR: The commercial AusDiagnostics test was used according to the manufacturer's instructions, with the specific reaction composition proprietary [1].
This workflow, from sample collection to result analysis, can be visualized as follows:
Triplex qPCR Development and Workflow
To address the need for detecting multiple pathogens efficiently, a 2022 study developed a triplex qPCR for the simultaneous detection of E. histolytica, G. lamblia, and C. parvum [71].
- Primer and Probe Design: Specific primers and TaqMan probes were designed for the E. histolytica 16S-like SSU rRNA gene, the G. lamblia gdh gene, and the C. parvum 18S rRNA gene. Specificity was confirmed via in silico BLAST analysis.
- Assay Validation: The researchers constructed standard plasmids for each target. The limit of detection (LOD), specificity, and reproducibility were rigorously evaluated. The triplex qPCR demonstrated no cross-reactivity and could detect as few as 500 copies/µL of plasmid DNA, with high amplification efficiency (>95%) and excellent repeatability [71].
- Practical Application: The assay was successfully used to test 163 clinical fecal samples, identifying four positive for C. parvum [71].
The process for developing and validating such a multiplex assay is systematic:
The Scientist's Toolkit: Key Research Reagents & Materials
Successful implementation of PCR diagnostics for protozoa relies on a suite of specific reagents and instruments. The following table details key solutions used in the featured studies.
Table 2: Essential Research Reagents for Protozoan PCR Diagnostics
| Item Name | Function / Application | Example Use-Case |
|---|---|---|
| S.T.A.R. Buffer | Stool Transport and Recovery Buffer; stabilizes nucleic acids in fecal samples prior to DNA extraction. | Used in a multicentre study for sample preparation before automated extraction [1]. |
| MagNA Pure 96 System | Fully automated instrument for high-throughput nucleic acid purification. | Used for standardized DNA extraction in a multi-laboratory comparison study [1]. |
| TaqMan Fast Universal PCR Master Mix | Ready-to-use reaction mix for probe-based qPCR, enabling fast cycling conditions. | Used as the core reaction mix for the in-house RT-PCR assays [1]. |
| Specific Primers & TaqMan Probes | Oligonucleotides designed to bind and detect unique genetic sequences of target protozoa. | Designed for E. histolytica, G. duodenalis, and C. parvum in a triplex assay [71]. Also for C. mesnili [21]. |
| Standard Plasmids | Quantified plasmids containing the target gene sequence; essential for determining assay LOD, efficiency, and absolute quantification. | Constructed for each target in the triplex qPCR to generate standard curves and validate sensitivity [71]. |
| QIAamp DNA Stool Mini Kit | Manual column-based kit for the purification of genomic DNA from stool samples. | Used for DNA extraction from stool specimens for subsequent qPCR analysis [71]. |
The data and methodologies summarized in this guide underscore a central tenet in protozoan molecular diagnostics: sensitivity is highly target-dependent. Assays for Giardia duodenalis consistently demonstrate high performance, whereas detection of Cryptosporidium spp. and Dientamoeba fragilis is often hampered by challenges in DNA extraction. The choice between commercial and in-house PCR is not a matter of one being universally superior. Commercial kits offer standardization and ease of use, which is valuable in clinical diagnostic settings. In-house assays provide flexibility, allowing researchers to adapt to new genetic data, include novel targets like Chilomastix mesnili [21], and optimize reactions for specific research questions or to reduce costs, such as by implementing low-volume reactions [21]. Ultimately, the optimal approach depends on the research priorities—whether they lie in standardized throughput or adaptable, investigative power—and must be made with a clear understanding of the inherent variability in sensitivity across the intended protozoan targets.
The diagnosis of pathogenic intestinal protozoa, significant global causes of diarrheal diseases, relies heavily on effective laboratory techniques [12]. While traditional microscopy has been the reference method for decades, molecular diagnostic technologies, particularly real-time polymerase chain reaction (qPCR), are gaining traction due to enhanced sensitivity and specificity [12] [28]. This shift necessitates a critical evaluation of the two primary molecular approaches: commercial PCR kits and laboratory-developed in-house tests. This analysis objectively compares the cost-benefit profiles of these approaches, focusing on reagent costs, labor requirements, and infrastructure needs, to inform decision-making for researchers, scientists, and drug development professionals.
Performance Comparison: Commercial vs. In-House PCR
The choice between commercial and in-house PCR assays involves balancing performance, cost, and operational complexity. The tables below summarize key comparative data from recent studies.
Table 1: Diagnostic Performance Comparison for Key Protozoa
| Parasite | Assay Type | Sensitivity (%) | Specificity (%) | Notes | Study (Year) |
|---|---|---|---|---|---|
| Giardia duodenalis | Commercial (AusDiagnostics) | High (complete agreement with in-house) | High | Performance similar to microscopy [12]. | Di Pietra et al. (2025) [12] |
| In-house RT-PCR | High (complete agreement with commercial) | High | Performance similar to microscopy [12]. | Di Pietra et al. (2025) [12] | |
| Commercial (Allplex) | 100 | 99.2 | Superior performance in a multicentric study [72]. | Multi-centre (2025) [72] | |
| Cryptosporidium spp. | Commercial (AusDiagnostics) | Limited | High | Limited sensitivity likely from DNA extraction issues [12]. | Di Pietra et al. (2025) [12] |
| In-house RT-PCR | Limited | High | Limited sensitivity likely from DNA extraction issues [12]. | Di Pietra et al. (2025) [12] | |
| Commercial (Allplex) | 100 | 99.7 | Excellent performance reported [72]. | Multi-centre (2025) [72] | |
| Dientamoeba fragilis | Commercial (AusDiagnostics) | Limited | High | Inconsistent detection [12]. | Di Pietra et al. (2025) [12] |
| In-house RT-PCR | Limited | High | Inconsistent detection [12]. | Di Pietra et al. (2025) [12] | |
| Commercial (Allplex) | 97.2 | 100 | High performance in a multicentric study [72]. | Multi-centre (2025) [72] | |
| Entamoeba histolytica | Commercial (Allplex) | 33.3 (fresh), 75 (frozen) | 100 | Sensitivity highly dependent on sample preservation [22]. | Validation Study (2025) [22] |
| Commercial (Allplex) | 100 | 100 | Excellent performance reported in a different cohort [72]. | Multi-centre (2025) [72] |
Table 2: Relative Strengths and Weaknesses in Performance
| Feature | Commercial PCR Kits | In-House PCR Assays |
|---|---|---|
| Sensitivity | Variable by manufacturer and target; can be very high (e.g., 100% for Giardia with Allplex) [72] or lower (e.g., for E. histolytica) [22]. | Can outperform some commercial kits, as shown in a 2014 study where in-house tests detected more Giardia and Cryptosporidium cases [73]. |
| Specificity | Generally very high (often >99%) and consistently reported [22] [72]. | Generally high, but requires rigorous validation and optimization by the lab [12]. |
| Species Differentiation | Excellent for differentiating morphologically identical species like E. histolytica and E. dispar [74] [72]. | Capable of species differentiation, but assay design and validation rely entirely on the laboratory [74]. |
| Reproducibility | High, due to standardized, quality-controlled reagents and protocols [28]. | Can be lower, as it is dependent on in-lab consistency in reagent preparation and protocols [12]. |
| Detection of Co-infections | Designed for multiplexing, allowing simultaneous detection of multiple pathogens in a single reaction [22] [28]. | Multiplexing requires significant development and optimization effort, limiting the number of targets per reaction [74]. |
Detailed Experimental Protocols
Understanding the methodologies behind the performance data is crucial for a thorough cost-benefit analysis. The following protocols are derived from the cited studies.
Multicenter Comparison Protocol (Commercial vs. In-House)
A 2025 multicentre study involving 18 Italian laboratories directly compared a commercial RT-PCR test (AusDiagnostics) with an in-house RT-PCR assay against microscopy [12].
- Sample Collection and Preparation: 355 stool samples (230 fresh, 125 preserved in Para-Pak media) were collected. Fresh samples were stained with Giemsa, while fixed samples were processed using the formalin-ethyl acetate (FEA) concentration technique. All samples were stored frozen at -20°C before molecular analysis [12].
- DNA Extraction: A semi-automated protocol was used. Briefly, 350 µL of Stool Transport and Recovery Buffer (S.T.A.R., Roche) was mixed with a small amount of fecal sample. After centrifugation, the supernatant was combined with an internal extraction control. DNA was extracted using the MagNA Pure 96 DNA and Viral NA Small Volume Kit on the MagNA Pure 96 System (Roche) [12].
- In-House RT-PCR Amplification: The reaction mixture (25 µL total volume) included 5 µL of extracted DNA, 12.5 µL of 2× TaqMan Fast Universal PCR Master Mix, a custom primers and probe mix, and sterile water. Amplification was performed on an ABI 7900HT Fast Real-Time PCR System with the following cycling conditions: 95°C for 10 minutes, followed by 45 cycles of 95°C for 15 seconds and 60°C for 1 minute [12].
- Commercial PCR Amplification: The same DNA extracts were tested using the AusDiagnostics RT-PCR kit according to the manufacturer's instructions [12].
Validation Protocol for a Commercial Multiplex Assay
A 2025 study validated a fully automated high-throughput multiplex system, providing a protocol for a streamlined commercial approach [22].
- Sample Preparation: Unpreserved stool specimens were used. A swab full of stool was inoculated into a FecalSwab tube containing Cary-Blair media and vortexed [22].
- Automated DNA Extraction and PCR Setup: The sample tubes were loaded into a Hamilton STARlet automated liquid handling platform. Nucleic acid was extracted using the STARMag 96 × 4 Universal Cartridge kit (Seegene). The platform then automatically set up the PCR reactions using the Allplex GI-Parasite Assay [22].
- Real-Time PCR Amplification: The PCR reaction used 5 µL of extracted DNA in a 25 µL total volume. The run was performed on a Bio-Rad CFX96 thermal cycler with a denaturing step followed by 45 cycles of 95°C for 10 seconds, 60°C for 1 minute, and 72°C for 30 seconds. A cycle threshold (Ct) value of ≤43 was considered positive [22].
Low-Volume Duplex qPCR Protocol (In-House)
A 2025 study implemented a cost-effective in-house qPCR using low reagent volumes, demonstrating an approach to reduce per-test costs [74].
- Primer and Probe Design: Sequences for Blastocystis spp., Cryptosporidium spp., E. histolytica, E. dispar, and G. duodenalis were obtained from an established diagnostic center. For Chilomastix mesnili, primers and probes were designed by identifying conserved regions in the small ribosomal subunit using BLASTN, ensuring specificity [74].
- Assay Optimization: Primer and probe concentrations, as well as cycle conditions, were optimized using plasmid controls and positive stool samples. Sensitivity was determined using ten-fold plasmid dilution series [74].
- Duplex qPCR Setup: The study established two duplex reactions (E. dispar + E. histolytica and C. mesnili + Cryptosporidium spp.) and singleplex assays for G. duodenalis and Blastocystis spp.). Each qPCR was performed in a very low 10 µL reaction volume, reducing reagent consumption [74]. A human 16S mitochondrial rRNA target was used as an internal control [74].
Cost and Infrastructure Analysis
Beyond performance, the economic and operational implications of each approach are fundamental to the decision-making process.
Table 3: Analysis of Reagent, Labor, and Infrastructure Requirements
| Cost & Workflow Factor | Commercial PCR Kits | In-House PCR Assays |
|---|---|---|
| Reagent Costs | Higher per-test cost; includes licensing and quality control [28]. | Lower per-test reagent cost; involves sourcing individual components [73]. |
| Labor Requirements | Lower for setup and execution; protocols are standardized and often automated [22]. | Higher; requires extensive labor for development, optimization, validation, and reagent preparation [74]. |
| Initial Development & Validation | Minimal; performed by the manufacturer [28]. | Significant investment of time and resources required [74]. |
| Infrastructure & Equipment | Often compatible with automated high-throughput systems (e.g., Hamilton STARlet) [22]. | Can be run on standard real-time PCR instruments (e.g., ABI 7900HT, Bio-Rad CFX96) [12] [74]. |
| Throughput & Turnaround Time | Higher throughput; one study reported a 7-hour reduction in pre-analytical and analytical time using an automated platform [22]. | Lower throughput and longer turnaround time due to more manual processes [22]. |
| Assay Flexibility & Customization | Fixed panel of targets; limited ability to modify or add new targets [28]. | Highly flexible; targets, primers, and probes can be modified or added as research needs change [74]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and their functions used in the molecular detection of intestinal protozoa, as cited in the research.
Table 4: Key Reagents and Materials for Protozoan PCR
| Item | Function / Application | Examples from Research |
|---|---|---|
| Nucleic Acid Extraction Kit | Purifies DNA from complex stool samples, a critical step given the robust wall of protozoan (oo)cysts and PCR inhibitors in stool [12] [72]. | MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche) [12]; STARMag Universal Cartridge kit (Seegene) [22]. |
| Commercial Multiplex PCR Kit | Provides a standardized, ready-to-use master mix for the simultaneous detection of multiple protozoan targets. | Allplex GI-Parasite Assay (Seegene) [22] [72]; AusDiagnostics Parasite PCR test [12]. |
| PCR Master Mix | Contains DNA polymerase, dNTPs, buffers, and salts essential for the amplification reaction. | TaqMan Fast Universal PCR Master Mix (Thermo Fisher) [12]. |
| Primers & Probes | Sequence-specific oligonucleotides that define the target to be amplified and detected. | Custom designed probes for C. mesnili [74]; manufacturer-provided primer/probe mixes [22]. |
| Stool Transport Buffer | Preserves nucleic acids in stool samples during transport and storage, critical for accurate results. | S.T.A.R. Buffer (Roche) [12]; Cary-Blair media in FecalSwab tubes [22]. |
| Automated Liquid Handling System | Automates nucleic acid extraction and PCR setup, increasing throughput, reproducibility, and reducing hands-on time. | Hamilton STARlet platform [22]; Microlab Nimbus IVD system [72]. |
| Real-Time PCR Thermocycler | Instrument that performs the DNA amplification and fluorescent detection in real-time. | ABI 7900HT (Applied Biosystems) [12]; CFX96 (Bio-Rad) [22] [72]. |
Workflow and Decision-Making Diagrams
The following diagrams visualize the procedural and strategic aspects of implementing PCR for protozoa research.
Diagram 1: Molecular Detection Workflow. This chart outlines the key steps in processing stool samples for protozoan detection via PCR, highlighting points where method choice (manual/automated, commercial/in-house) impacts the process.
Diagram 2: PCR Strategy Decision Guide. A flowchart to guide researchers in choosing between commercial and in-house PCR based on their project's specific requirements and constraints.
The choice between commercial and in-house PCR for protozoa research is not a one-size-fits-all decision but a strategic trade-off. Commercial kits offer a clear advantage in operational efficiency, providing standardized, high-throughput solutions that save valuable time and labor, which is crucial in clinical diagnostics and large-scale surveillance studies [22] [72]. Conversely, in-house assays provide superior flexibility and lower per-test reagent costs, making them ideal for research environments focused on novel targets, specific customizations, or operating under significant reagent budget constraints [74] [73]. The decision ultimately hinges on the specific context: laboratories should prioritize commercial solutions for standardized, high-efficiency workflows and lean towards validated in-house methods when flexibility, specific research needs, or minimizing reagent costs are the primary drivers.
Performance Benchmarking: Multicenter Study Results and Analytical Validation
The accurate detection of Giardia duodenalis (also known as G. lamblia or G. intestinalis) is a critical concern in clinical diagnostics, public health surveillance, and epidemiological research. As one of the most prevalent diarrhoea-causing protozoa globally, it accounts for significant morbidity in both resource-limited and developed nations [28]. For decades, microscopy stood as the primary diagnostic method, but its limitations in sensitivity and operator-dependence have prompted a shift toward molecular techniques [75] [1].
This transition has created a fundamental question for laboratory professionals and researchers: what is the optimal molecular approach for Giardia detection? The choice often lies between commercially developed, standardized PCR kits and laboratory-developed in-house PCR assays. This guide provides a detailed, evidence-based comparison of these platforms, drawing on recent head-to-head evaluations to inform method selection for diagnostic and research applications.
Performance Data at a Glance
The following tables synthesize key performance metrics from comparative studies, offering a direct overview of how different detection methods for Giardia duodenalis measure against each other.
Table 1: Comparative Performance of Giardia duodenalis Screening PCR Assays Targeting Different Genes [75] [29]
| Target Gene | Estimated Sensitivity (%) | Estimated Specificity (%) | Notes |
|---|---|---|---|
| 18S rRNA | 100.0 | 100.0 | Demonstrates best overall diagnostic accuracy for screening. |
| Beta-giardin (bg) | 31.7 | 100.0 | High specificity but significantly lower sensitivity. |
| Glutamate dehydrogenase (gdh) | 17.5 | 92.3 | Lowest sensitivity among the compared assays. |
Table 2: Performance of Assemblage-Specific PCR Assays for Giardia duodenalis [75] [29]
| Target Gene | Assemblage | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| bg (without LNA*) | A | 100.0 | 100.0 |
| bg (with LNA) | A | 100.0 | 97.8 |
| tpi | A | 100.0 | 97.8 |
| bg (without LNA) | B | 100.0 | 100.0 |
| bg (with LNA) | B | 96.4 | 84.0 |
| tpi | B | 82.1 | 100.0 |
*LNA: Locked Nucleic Acid
Table 3: Commercial Multiplex PCR Assays for Diarrhoea-Causing Protozoa [28]
| Commercial Assay Name | Reported Sensitivity for G. duodenalis | Reported Specificity for G. duodenalis |
|---|---|---|
| Gastroenteritis/Parasite Panel I (Diagenode) | 92% | 100% |
| RIDAGENE Parasitic Stool Panel (R-Biopharm) | Information in study | Information in study |
| Allplex Gastrointestinal Parasite Panel 4 (Seegene) | Information in study | Information in study |
| FTD Stool Parasites (Fast Track Diagnostics) | Information in study | Information in study |
Table 4: Comparison of Microscopy and PCR for Giardia Detection [76]
| Method | Sensitivity (%) | Specificity (%) | Kappa Value |
|---|---|---|---|
| Microscopy | 64.4 | 86.6 | 0.51 |
| PCR (gdh gene) | 100.0 | 100.0 | 1.00 |
Detailed Experimental Protocols from Key Studies
To critically assess the data from comparative studies, understanding their underlying methodologies is essential. This section outlines the experimental designs of several pivotal head-to-head evaluations.
Comparative Evaluation of Real-Time Screening PCRs
A 2022 study conducted a rigorous head-to-head assessment of different real-time PCR assays without a conventional reference standard, instead employing Latent Class Analysis (LCA) for statistical evaluation [75] [29].
- Sample Materials: The study utilized 872 non-preselected residual nucleic acid extracts from stool samples of Ghanaian HIV patients, a population with a high pre-test probability for Giardia infection. For assemblage-specific PCRs, 53 samples positive by at least two screening PCRs were used [75] [29].
- Nucleic Acid Extraction: DNA was extracted from stool samples using the QIAamp Stool DNA Mini Kit (Qiagen, Hilden, Germany). Extracts were stored deep-frozen at -80°C prior to PCR assessment [75] [29].
- Screening PCR Assays: Three distinct in-house real-time PCR assays were compared, each targeting a different gene:
- Assemblage Discrimination Assays: Three duplex real-time PCRs were evaluated for discriminating the zoonotic assemblages A and B:
- Quality Control: Each run included plasmid-based positive controls and negative controls. An inhibition control PCR (Phocid herpes virus) was performed, and samples showing inhibition were excluded [75].
Multicenter Comparison of Commercial and In-House Platforms
A 2025 Italian multicentre study involving 18 laboratories compared a commercial RT-PCR test (AusDiagnostics) against an in-house RT-PCR assay validated by the Padua Hospital Microbiology Unit [1].
- Sample Collection: The study analyzed 355 stool samples, comprising 230 fresh samples and 125 samples preserved in Para-Pak media [1].
- Reference Method: All samples were first examined by conventional microscopy following WHO and CDC guidelines. Fresh samples were stained with Giemsa, while fixed samples were processed using the formalin-ethyl acetate (FEA) concentration technique [1].
- DNA Extraction: A standardized, automated protocol was used. Stool samples were mixed with Stool Transport and Recovery (S.T.A.R) Buffer, centrifuged, and the supernatant was used for DNA extraction on the MagNA Pure 96 System (Roche) with the MagNA Pure 96 DNA and Viral NA Small Volume Kit [1].
- PCR Amplification: The in-house RT-PCR was performed using a TaqMan Fast Universal PCR Master Mix (Thermo Fisher Scientific) on an ABI platform [1].
Broad Comparison of Commercial and In-House qPCRs
A 2020 study provided a extensive test comparison of one in-house real-time PCR (qPCR) platform and three commercial qPCR kits for 15 parasites and microsporidia, including Giardia duodenalis [5] [79].
- Study Design: The evaluation was designed as a test comparison without a gold standard, using LCA to estimate diagnostic sensitivity and specificity [5].
- Samples: The study used residual nucleic acid extracts from 500 stool samples from patients with a high likelihood of parasitic infection. Due to volume limitations, 250 samples were tested per assay [5].
- Results for G. duodenalis: The in-house platform and commercial kits showed substantial agreement (Kappa 0.61-0.8) for the detection of Giardia duodenalis. The number of positive detections per 250 samples ranged from 184 to 205 across the different platforms, highlighting the variation in assay performance [5].
Signaling Pathways and Workflows
The following diagram illustrates the general diagnostic workflow for detecting Giardia duodenalis via molecular methods, highlighting key decision points and processes derived from the cited studies.
The Scientist's Toolkit: Research Reagent Solutions
Successful detection of Giardia duodenalis relies on a suite of specific reagents and instruments. The table below details key solutions used in the featured experiments.
Table 5: Essential Research Reagents and Kits for Giardia PCR Detection
| Item | Specific Function / Role | Example Products / Assays (from search results) |
|---|---|---|
| DNA Extraction Kit | Purifies parasite DNA from complex stool matrices; critical for downstream PCR sensitivity. | QIAamp Stool DNA Mini Kit (Qiagen) [75] [76] [80], MagNA Pure 96 System (Roche) [1] |
| Commercial Multiplex PCR Kits | Provides standardized, multi-target detection of diarrhoea-causing protozoa in a single reaction. | AusDiagnostics test [1], G-DiaParaTrio (Diagenode) [78], RIDAGENE (R-Biopharm) [28], Allplex (Seegene) [28], FTD (Fast Track Diagnostics) [28] |
| In-House PCR Components | Core reagents for laboratory-developed tests; allow for customization of targets and conditions. | GoTaq HotStart Polymerase (Promega) [80], TaqMan Fast Universal PCR Master Mix (Thermo Fisher) [1], Tib MolBiol assays [79] |
| Positive Control Material | Validates PCR assay performance and helps monitor for inhibition; essential for quality assurance. | Plasmid controls with cloned target sequences [75] [80], DNA from axenic cultures (e.g., ATCC 50803, ATCC 50581) [80] |
| Reference Microscopy Reagents | Used as a comparator in validation studies, though with recognized limitations in sensitivity. | Formalin-ethyl acetate (FEA) for concentration [1], Iodine and Giemsa stains [76] [1] [80] |
The body of evidence demonstrates that molecular methods, particularly PCR, have superseded microscopy as the most sensitive method for detecting Giardia duodenalis in stool samples [75] [76]. The choice between commercial and in-house PCR platforms is nuanced. Commercial kits offer standardization and convenience, with performance similar to well-validated in-house assays for common targets like Giardia [1] [5] [28]. However, in-house assays provide unparalleled flexibility, allowing researchers to select the most sensitive targets, such as the 18S rRNA gene, and to develop specialized tests for genotyping assemblages A and B using the bg gene [75] [29]. The decision ultimately depends on the laboratory's priorities: standardization and workflow integration favor commercial kits, while analytical sensitivity, cost-control, and research flexibility favor in-house development.
Comparative Analysis for Cryptosporidium and Dientamoeba fragilis
Intestinal protozoan parasites represent a significant global health burden, with pathogenic species like Cryptosporidium and Dientamoeba fragilis causing millions of cases of diarrheal disease annually [81] [1]. Accurate detection of these pathogens is crucial for clinical management, epidemiological studies, and drug development. In contemporary parasitology, molecular diagnostic methods have increasingly supplemented or replaced traditional techniques like microscopy, which suffers from limitations in sensitivity and specificity [1]. This review provides a comparative analysis of detection methods for Cryptosporidium and Dientamoeba fragilis, with a specific focus on the performance characteristics of commercial versus in-house PCR assays. We synthesize recent experimental data to guide researchers and scientists in selecting appropriate diagnostic approaches for their specific applications.
Cryptosporidium
Cryptosporidium species, particularly C. parvum and C. hominis, are apicomplexan protozoan parasites responsible for significant gastrointestinal illness in humans and animals [81] [82]. They colonize the duodenum, jejunum, and ileum, causing symptoms ranging from mild, self-limiting diarrhea to severe, persistent gastroenteritis with nausea, abdominal pain, and low-grade fever [81]. In immunocompromised individuals, including HIV/AIDS patients and those undergoing immunosuppressive therapy, Cryptosporidium infection can lead to severe, chronic diarrhea, volume depletion, wasting, and potentially biliary and respiratory involvement [81] [1]. The impact is particularly devastating in resource-constrained regions, with an estimated annual death rate of >200,000 children below 2 years of age [81].
Dientamoeba fragilis
Dientamoeba fragilis is a flagellate protozoan, closely related to trichomonads, that inhabits the human gastrointestinal tract [83]. Once considered a commensal, it is now recognized as a cause of human illness, with clinical manifestations including abdominal pain, diarrhea, weight loss, anorexia, flatulence, nausea, vomiting, and anal pruritus [83] [1] [84]. Studies have found it to be one of the most frequently identified intestinal protozoa, with prevalence rates varying from 0% to over 82% depending on geographic location, population studied, and diagnostic methods used [83]. In some studies, D. fragilis was found to equal or exceed the incidence of giardiasis [83], and it was the most common pathogenic protozoan isolated in some patient populations [84].
Table 1: Epidemiological and Clinical Features of Cryptosporidium and Dientamoeba fragilis
| Feature | Cryptosporidium | Dientamoeba fragilis |
|---|---|---|
| Classification | Apicomplexa (Diaphoretickes) | Trichomonadina (Excavata) |
| Primary Site of Infection | Duodenum, jejunum, ileum | Colon |
| Key Pathogenic Species | C. parvum, C. hominis | D. fragilis |
| Major Clinical Symptoms | Watery diarrhea, nausea, vomiting, abdominal pain, low-grade fever | Abdominal pain, diarrhea, flatulence, nausea, weight loss |
| At-Risk Populations | Children in developing countries, immunocompromised individuals | Children, travelers, institutionalized groups |
| Global Prevalence | Varies; major cause of persistent diarrhea | 0% to >82% depending on population and diagnostics |
Diagnostic Methodologies
Conventional Diagnostic Techniques
Traditional methods for detecting intestinal protozoa have relied primarily on microscopic examination of stained fecal specimens. The modified Ziehl-Neelsen (mZN) technique is commonly used for Cryptosporidium detection, while trichrome staining is often employed for D. fragilis [82] [83]. Microscopy, while cost-effective and widely available in resource-limited settings, has significant limitations. It is time-consuming, requires experienced personnel, and lacks sensitivity and specificity, particularly for differentiating between morphologically similar species [1] [85]. For D. fragilis, microscopy is further complicated by the fragile nature of the trophozoites, which degrade quickly after passage [83].
Immunoassay-based methods including enzyme-linked immunosorbent assay (ELISA) and rapid immunochromatographic tests (RDTs) have been developed to detect parasite-specific antigens. These assays offer advantages in speed and ease of use compared to microscopy. However, performance varies considerably between commercial products. One evaluation of the CerTest Crypto RDT reported an overall sensitivity of only 49.6% and specificity of 92.5% compared to a composite PCR reference standard [82]. Similarly, a study of Cryptosporidium diagnostics in cattle found immunochromatographic assays had high false-positive rates, suggesting caution in interpreting positive results without confirmation [85].
Molecular Detection Methods
Molecular techniques, particularly polymerase chain reaction (PCR) and real-time PCR (qPCR), have revolutionized detection of intestinal protozoa by offering superior sensitivity and specificity compared to traditional methods [1] [86]. These methods enable species-level differentiation that is impossible with microscopy alone, such as distinguishing pathogenic E. histolytica from non-pathogenic E. dispar [1]. However, molecular detection of intestinal protozoa presents unique technical challenges. The robust wall structure of cysts and oocysts complicates DNA extraction, and PCR inhibitors present in fecal material can reduce assay sensitivity [1] [7].
Table 2: Comparison of Diagnostic Methods for Cryptosporidium and Dientamoeba fragilis
| Method | Principle | Advantages | Limitations | Reported Sensitivity | Reported Specificity |
|---|---|---|---|---|---|
| Microscopy (mZN for Crypto, Trichrome for D. fragilis) | Visual identification of parasites in stained fecal smears | Low cost, widely available, can detect multiple parasites | Requires expertise, time-consuming, low sensitivity, cannot differentiate species | Variable; for Crypto: 47.22% [85] | Variable; for Crypto: 98.29% [85] |
| Immunochromatographic RDTs | Detection of parasite-specific antigens by lateral flow immunoassay | Rapid (10-15 min), easy to perform, minimal equipment | Variable performance, false positives | For Crypto: 49.6-74.07% [82] [85] | For Crypto: 89.97-92.5% [82] [85] |
| qPCR (Commercial and In-House) | Amplification and detection of parasite-specific DNA sequences | High sensitivity and specificity, species differentiation, quantitative potential | Requires specialized equipment, technical expertise, DNA extraction challenges | Generally high but variable between assays | Generally high but variable between assays |
Comparative Performance: Commercial vs. In-House PCR Assays
Multicenter Evaluation of PCR Assays
A comprehensive multicenter study comparing a commercial RT-PCR test (AusDiagnostics) with an in-house RT-PCR assay for detecting intestinal protozoa, including Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis, revealed important insights [1]. The study analyzed 355 stool samples from 18 Italian laboratories using both molecular methods alongside traditional microscopy as a reference.
For Giardia duodenalis detection, complete agreement was observed between the commercial and in-house PCR methods, with both demonstrating high sensitivity and specificity comparable to microscopy [1]. For Cryptosporidium spp. and D. fragilis detection, both molecular methods showed high specificity but limited sensitivity, which authors attributed to potential issues with DNA extraction from these particular parasites [1]. The study also found that PCR results from preserved stool samples were generally better than those from fresh samples, likely due to improved DNA preservation in fixed specimens [1].
Technical Considerations in PCR Detection
The effectiveness of molecular detection is highly dependent on the specific protocols employed at each stage of the process, including pretreatment, DNA extraction, and amplification [7]. One systematic evaluation of 30 distinct protocol combinations for detecting C. parvum demonstrated that different combinations yielded significantly varying results [7]. The optimal approach identified combined mechanical pretreatment, the Nuclisens Easymag extraction method, and the FTD Stool Parasite DNA amplification method, which achieved 100% detection [7]. Manual extraction methods also demonstrated excellent outcomes despite being more time-consuming [7].
For D. fragilis, a unique challenge involves potential cross-reactivity when applying human-designed qPCR assays to animal specimens [87]. One study found that PCR products from cattle initially identified as D. fragilis had a 9°C cooler melt curve than human-derived products, and subsequent DNA sequencing determined that Simplicimonas sp. was responsible for this cross-reactivity [87]. This highlights the importance of melt curve analysis and confirmatory sequencing when applying these assays to new host species.
Diagram 1: Workflow for Selecting and Validating PCR Assays for Protozoan Detection. This diagram outlines the decision process for implementing reliable PCR detection, highlighting key validation steps to address challenges like cross-reactivity.
Experimental Protocols and Research Reagents
DNA Extraction Protocols
Effective DNA extraction is critical for successful molecular detection of both Cryptosporidium and D. fragilis. Multiple protocols have been employed across studies:
Modified MO BIO-Qiagen Stool DNA Extraction: This protocol incorporates six main steps: sample treatment, cell lysis, inhibitors removal, DNA binding, a wash step, and DNA elution [82]. Genomic DNA is extracted from 250 mg of stool using the DNeasy PowerSoil Kit (QIAGEN), following manufacturer's instructions with nucleic acids eluted in 100 μL volume [82].
QIAamp Fast DNA Stool Mini Kit Protocol: Used with a laboratory-based qPCR assay for D. fragilis, this method extracts DNA from 200 mg fecal material with modifications including heating the stool suspension in InhibitEX buffer for 10 minutes and adding Internal Control DNA [87].
Fully Automated Extraction: Systems like the MagNA Pure 96 System (Roche Applied Sciences) enable fully automated nucleic acid preparation based on magnetic separation of nucleic acid-bead complexes, improving reproducibility and throughput [1].
PCR Amplification Conditions
Amplification protocols vary between commercial and in-house assays:
Commercial AusDiagnostics Assay: This multiplex PCR system includes an extraction control and an internal positive control to detect PCR inhibition [1].
In-House RT-PCR Amplification: A typical reaction mixture includes 5 μL of extracted DNA, 2× TaqMan Fast Universal PCR Master Mix (12.5 μL), primers and probe mix (2.5 μL), and sterile water to a final volume of 25 μL [1]. Multiplex tandem PCR assays are performed using standard thermocycler conditions.
Duplex qPCR Assays: Recent implementations include two duplex qPCR assays to detect Entamoeba dispar + Entamoeba histolytica and Cryptosporidium spp. + Chilomastix mesnili, along with singleplex assays for Giardia duodenalis and Blastocystis spp., using a 10 μL reaction volume [86].
Table 3: Research Reagent Solutions for Protozoan Detection
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| DNA Extraction Kits | DNeasy PowerSoil Kit (QIAGEN), QIAamp Fast DNA Stool Mini Kit (Qiagen) | Isolation of inhibitor-free DNA from difficult stool matrices | Manual methods show excellent results but are time-consuming; automated systems improve throughput [82] [7] [87] |
| Commercial PCR Kits | AusDiagnostics Enteric Protozoan PCR Kit, EasyScreen Enteric Protozoan Detection Kit | Standardized detection of multiple parasites in a single reaction | Include internal controls for extraction and amplification; performance varies between targets [1] [87] |
| Enzyme Master Mixes | HotStart Taq master mix kit (QIAGEN), TaqMan Fast Universal PCR Master Mix | Provide optimized reaction components for efficient amplification | Choice affects sensitivity, specificity, and resistance to PCR inhibitors in stool samples [82] [1] |
| Sample Pretreatment Reagents | S.T.A.R. Buffer (Stool Transport and Recovery Buffer), Mechanical lysis beads | Disruption of robust cyst/oocyst walls and stabilization of nucleic acids | Critical step that significantly impacts downstream detection sensitivity [1] [7] |
| Control Materials | qPCR Extraction Control Kits, Known positive control reagents | Monitoring extraction efficiency and PCR inhibition | Essential for validating assay performance and identifying false negatives [87] |
Discussion and Future Directions
The comparative analysis of detection methods for Cryptosporidium and Dientamoeba fragilis reveals a complex landscape where method selection must balance performance characteristics, practical constraints, and specific research objectives. Molecular methods, particularly qPCR, generally offer superior sensitivity and specificity compared to traditional microscopy and antigen-based assays, but their performance is highly dependent on the specific protocols employed throughout the entire diagnostic process [7].
For both pathogens, the commercial versus in-house PCR comparison does not yield a universally superior approach. Commercial kits provide standardization, quality control, and often include useful internal controls, making them suitable for clinical diagnostics where reproducibility is paramount [1]. In-house assays offer greater flexibility for customization and optimization for specific research needs, potentially at lower cost [1] [7]. The optimal choice depends on the specific application, available resources, and technical expertise.
For Cryptosporidium detection, recent research highlights the critical importance of considering all stages of the molecular process simultaneously, as a PCR method may perform poorly with an unsuitable extraction technique but yield optimal results with an appropriate one [7]. The FTD Stool Parasite technique has demonstrated excellent performance when combined with appropriate pretreatment and extraction methods [7].
For D. fragilis, the confirmation of a cyst stage has clarified transmission routes, supporting fecal-oral transmission [83]. However, molecular detection faces unique challenges, including potential cross-reactivity with related organisms when assays developed for human diagnostics are applied to animal specimens [87]. Melt curve analysis after qPCR provides a valuable technique to help differentiate true D. fragilis detection from cross-reactions [87]. Additionally, reducing PCR cycles to less than 40 may help minimize false positives from non-specific amplification [87].
Future directions in the field should focus on standardizing sample collection, storage, and DNA extraction procedures to enable more consistent results across studies [1]. Additionally, the development of multiplex assays capable of simultaneously detecting multiple protozoan pathogens with high sensitivity and specificity will be valuable for both clinical diagnostics and epidemiological studies. As molecular methods continue to evolve, their integration into diagnostic algorithms for intestinal protozoa will likely expand, potentially replacing traditional methods in settings where resources permit.
Diagram 2: Key Challenges in Molecular Detection of Intestinal Protozoa and Corresponding Solutions. This diagram outlines major technical obstacles in PCR-based detection of Cryptosporidium and D. fragilis, along with implemented strategies to address these limitations.
The Critical Role of PCR in Differentiating Entamoeba histolytica/dispar
For decades, the diagnosis of intestinal amoebiasis relied primarily on microscopic examination of stool samples, a method that presents a significant clinical challenge due to the morphological identical nature of pathogenic Entamoeba histolytica and non-pathogenic Entamoeba dispar and Entamoeba moshkovskii [88]. This diagnostic limitation has profound implications for patient management, as it can lead to unnecessary treatment of individuals infected with non-pathogenic species or failure to treat those with pathogenic E. histolytica infections [88]. The World Health Organization has specifically recommended that E. histolytica "should be specifically identified and if present should be treated" [89]. Traditional microscopy is not only unable to differentiate these species but also has limited sensitivity, ranging from only 10% to 60% even under optimal conditions [89]. Although culture followed by isoenzyme analysis enables differentiation, this method requires one to several weeks to obtain results and needs special laboratory facilities, making it impractical for routine diagnosis [90].
The development of polymerase chain reaction (PCR)-based methods has revolutionized the detection and differentiation of Entamoeba species. These molecular techniques provide a solution to the diagnostic dilemma by enabling specific identification directly from clinical samples [91] [88]. Both conventional and real-time PCR assays have demonstrated superior sensitivity and specificity compared to microscopy and antigen detection tests [19] [89]. Within PCR methodologies, a key consideration for laboratories is the choice between implementing commercially available kits or developing in-house protocols. This decision balances factors including standardization, cost, turnaround time, and performance characteristics, making a comparative understanding of these approaches essential for diagnostic and research applications in parasitology.
Methodological Approaches: Commercial vs. In-House PCR
Experimental Protocols for Entamoeba Detection
The fundamental principle underlying PCR detection of Entamoeba species involves amplifying species-specific DNA sequences, typically from the small-subunit ribosomal RNA (rRNA) gene, which contains sufficient genetic variation to distinguish between the morphologically identical species [88] [90]. DNA extraction represents a critical first step, with most protocols utilizing commercial stool DNA extraction kits such as the QIAamp DNA Stool Mini Kit (Qiagen) to obtain inhibitor-free DNA from fecal specimens [91] [89]. For real-time PCR protocols, the extracted DNA is amplified in the presence of species-specific primers and fluorescence-labeled probes, with detection performed using platforms such as the LightCycler system (Roche) or i-Cycler system (Bio-Rad) [91] [89].
Table 1: Key Protocol Steps for Entamoeba Species Detection by PCR
| Protocol Step | Commercial PCR Workflow | In-House PCR Workflow |
|---|---|---|
| DNA Extraction | Kit-based standardized protocols (e.g., QIAamp DNA Stool Mini Kit) | Kit-based or laboratory-developed methods |
| Primers/Probes | Provided with kit; standardized concentrations | Laboratory-designed and optimized; species-specific |
| Amplification | Pre-optimized thermal cycling conditions | Laboratory-optimized cycling conditions |
| Detection | Real-time fluorescence detection on compatible instruments | Real-time detection or gel electrophoresis |
| Analysis | Automated software with pre-set thresholds | Laboratory-determined analysis parameters |
Nested PCR protocols provide an alternative approach, involving two rounds of amplification for enhanced sensitivity. The primary PCR uses genus-specific primers (e.g., E-1 and E-2) that amplify a segment of the small-subunit rRNA gene from all Entamoeba species [88]. The secondary, nested PCR then uses species-specific primer sets to differentiate E. histolytica (primers EH-1 and EH-2 producing a 439 bp product), E. dispar (primers ED-1 and ED-2 producing a 174 bp product), and E. moshkovskii (primers Mos-1 and Mos-2 producing a 553 bp product) [88] [90]. This method has been adapted into a nested multiplex PCR format that allows simultaneous detection and differentiation of all three Entamoeba species in a single reaction tube, significantly improving workflow efficiency compared to performing separate reactions for each species [90].
Visualizing the PCR Detection Workflow
The following diagram illustrates the comparative workflow for Entamoeba detection using commercial versus in-house PCR methods:
Performance Comparison: Sensitivity, Specificity, and Practical Considerations
Quantitative Performance Metrics
Multiple studies have systematically evaluated the performance of PCR-based methods for Entamoeba detection. When compared to traditional diagnostic methods, real-time PCR demonstrates显著更高的敏感性. In a comprehensive study evaluating real-time PCR for detection of gastrointestinal parasites, PCR was positive in 73.5% (72/98) of samples compared to only 37.7% (37/98) by microscopic examination [19]. This enhanced sensitivity was particularly evident in asymptomatic patients, where PCR detected parasites in 57.4% (31/54) of cases compared to just 18.5% (10/54) by microscopy [19].
Table 2: Performance Comparison of PCR Methods for Entamoeba Detection
| Detection Method | Sensitivity | Specificity | Detection Limit | Time to Result |
|---|---|---|---|---|
| Microscopy | 10-60% [89] | Cannot differentiate species | Varies with parasite load | 1-2 hours |
| Culture + Isoenzyme | ~88% vs. PCR [91] | 100% [91] | Varies with viability | 1-3 weeks |
| Antigen Detection | 79% vs. real-time PCR [89] | 96% vs. real-time PCR [89] | Varies with antigen load | 2-3 hours |
| Nested PCR | 80-94% [88] [90] | 100% [90] | ~25 parasites [90] | 6-8 hours |
| Real-time PCR (in-house) | 86.2% [88], significantly higher than microscopy [91] | 100% [91] | 0.1 parasite/g feces [91] | 2-3 hours |
| Real-time PCR (commercial) | Varies by kit; generally high | Varies by kit; generally high | Varies by kit; generally comparable | 2-3 hours |
The exceptional sensitivity of real-time PCR is evidenced by its ability to detect as little as 0.1 parasite per gram of feces, a detection limit that surpasses both microscopy and culture methods [91]. This sensitivity is maintained even in mixed infections, with studies demonstrating that real-time PCR can detect E. histolytica even when present at very low proportions (0.01%) in background populations of non-pathogenic species [90]. The specificity of well-designed PCR assays is equally impressive, with both in-house and commercial formats demonstrating 100% specificity for their target Entamoeba species without cross-reactivity with other Entamoeba species even when present in exceeding amounts [91] [90].
Commercial vs. In-House PCR: Comparative Considerations
The choice between commercial and in-house PCR assays involves multiple considerations beyond basic performance metrics. Commercial kits typically offer standardized protocols with pre-optimized reagents, reducing the need for extensive validation and technical expertise [92]. This standardization facilitates consistency across different laboratories and may improve reproducibility. However, commercial kits can be more expensive per test and may offer less flexibility in protocol modification for specific research needs [93].
In-house PCR methods provide greater customization options, allowing researchers to adjust reaction conditions, modify primer sequences, or incorporate novel detection chemistries [93]. While initial development and validation require significant investment of time and expertise, in-house methods may be more cost-effective for high-volume testing [24]. Comparative studies of commercial versus in-house PCR assays for other pathogens have shown that while both approaches can provide excellent results, differences in quantitative standards and amplification efficiencies can lead to variations in absolute quantification values [93]. This highlights the importance of using common standards when comparing results between different laboratories and methodologies.
Essential Research Reagent Solutions
The implementation of effective PCR-based detection of Entamoeba species requires several key reagent solutions. The following table outlines essential materials and their functions based on protocols described in the research literature:
Table 3: Essential Research Reagents for Entamoeba PCR Detection
| Reagent Category | Specific Examples | Function in Protocol |
|---|---|---|
| DNA Extraction Kits | QIAamp DNA Stool Mini Kit (Qiagen), Mo Bio Power Soil DNA Isolation Kit | Efficient extraction of inhibitor-free DNA from complex stool samples |
| PCR Enzymes/Master Mixes | FastStart DNA Master Hybridization Probes (Roche), iTaq DNA Polymerase (Bio-Rad) | Enzymatic amplification of target DNA sequences with high fidelity |
| Specific Primers/Probes | E. histolytica: Eh-S26C, Eh/Ed-AS25; E. dispar: Ed-27C, Eh/Ed-AS25 [91] | Species-specific recognition and amplification of target sequences |
| Fluorescent Detection Systems | LC-Red 640, Fluorescein-labeled probes, Molecular Beacons [91] [89] | Real-time detection of amplified products without post-processing |
| Quantification Standards | Plasmid DNA, Genomic DNA from reference strains [93] | Calibration for quantitative PCR and comparison across experiments |
| Inhibition Detection | Exogenous synthetic oligonucleotides, internal control genes [19] | Identification of PCR inhibitors in sample extracts |
PCR technology has fundamentally transformed the diagnostic landscape for Entamoeba infections, providing the specificity and sensitivity necessary to distinguish pathogenic E. histolytica from non-pathogenic E. dispar and E. moshkovskii. Both commercial and in-house PCR approaches offer significant advantages over traditional microscopic examination, with real-time PCR formats providing additional benefits in workflow efficiency and reduced contamination risk. The choice between commercial and in-house methods involves balancing standardization against flexibility, with both approaches capable of delivering highly accurate results when properly validated. As molecular technologies continue to advance, PCR remains an indispensable tool in both clinical diagnosis and research applications for enteric protozoa, enabling appropriate treatment decisions and advancing our understanding of the epidemiology and pathogenesis of these medically significant organisms.
In the field of protozoa research, the choice between commercial and in-house real-time PCR (qPCR) platforms presents a significant challenge for laboratories. The reproducibility and standardization of these diagnostic tools are paramount, as they directly impact the reliability of surveillance data, clinical trials, and drug development research. Multi-laboratory assessments provide the essential framework for objectively comparing these platforms, revealing not only their performance characteristics but also the critical importance of standardized protocols and reagents. Without such rigorous validation, inter-laboratory variations can compromise the integrity of research findings and hinder the development of effective therapeutics.
This guide objectively compares the performance of commercial and in-house qPCR platforms for detecting protozoa and microsporidia in human stool samples, contextualized within a broader thesis on methodological standardization. The data and experimental protocols summarized herein provide researchers with the evidence base to select appropriate molecular tools and implement standardized approaches that ensure reproducible, reliable results across multiple research sites.
Performance Comparison: Commercial vs. In-House qPCR Platforms
Detection Rates and Inter-Assay Agreement
A comprehensive test comparison of in-house and commercial qPCR kits for detecting 15 parasites and microsporidia in human stool samples revealed significant variation in performance characteristics. The study, which analyzed 500 DNA samples without a gold standard reference, found that detection rates differed substantially depending on the assay used [79].
Table 1: Comparison of Pathogen Detection Rates Across Different qPCR Platforms (per 250 samples)
| Pathogen | Detection Range Across Assays | Inter-Assay Agreement (Kappa) | Agreement Strength |
|---|---|---|---|
| Giardia duodenalis | 184-205 | 0.61-0.8 | Substantial |
| Blastocystis spp. | 174-183 | 0.61-0.8 | Substantial |
| Trichuris trichiura | 118-120 | 0.61-0.8 | Substantial |
| Ascaris lumbricoides | 79-96 | 0.81-1 | Almost perfect |
| Necator americanus | 78-106 | 0.61-0.8 | Substantial |
| Hymenolepis nana | 40-42 | 0.81-1 | Almost perfect |
| Cryptosporidium spp. | 27-36 | 0.81-1 | Almost perfect |
| Dientamoeba fragilis | 26-28 | 0.81-1 | Almost perfect |
| Schistosoma spp. | 13-23 | 0.61-0.8 | Substantial |
| Entamoeba histolytica | 7-16 | 0.41-0.6 | Moderate |
| Strongyloides stercoralis | 6-38 | 0-0.2 | Slight |
| Cyclospora spp. | 6-13 | 0-0.2 | Slight |
| Microsporidia | 1-5 | 0.21-0.4 | Fair |
| Taenia spp. | 1-4 | <0 | Poor |
The data reveals that inter-assay agreement varies dramatically across pathogen targets, with some organisms showing consistent detection (almost perfect agreement for Ascaris lumbricoides, Hymenolepis nana, Cryptosporidium spp., and Dientamoeba fragilis) while others demonstrate concerning discrepancies (slight to poor agreement for Strongyloides stercoralis, Cyclospora spp., and Taenia spp.) [79]. These variations highlight the critical importance of platform selection for specific research objectives and the challenges in comparing data generated using different methodologies.
Comparative Sensitivity: qPCR Versus Traditional Microscopy
When evaluating the overall value of qPCR platforms, their performance relative to traditional microscopic examination provides crucial context. A study comparing real-time PCR assays to microscopic examination for detection of intestinal parasites demonstrated qPCR's significant sensitivity advantage [19].
Table 2: Detection Capabilities of qPCR vs. Microscopy
| Performance Metric | Real-time PCR | Microscopic Examination | Statistical Significance |
|---|---|---|---|
| Overall positive rate | 73.5% (72/98 samples) | 37.7% (37/98 samples) | P < 0.001 |
| Detection in asymptomatic patients | 57.4% (31/54) | 18.5% (10/54) | P < 0.05 |
| Co-infections detected | 25.5% | 3.06% | Not specified |
| Agreement between techniques | 100% for 7 species; 64.2%-98.9% for others | 100% for 7 species; 64.2%-98.9% for others | Varies by species |
The superior detection capability of qPCR platforms is particularly evident in asymptomatic cases and polyparasitism assessment, making them invaluable for sensitive surveillance and drug efficacy studies [19]. However, the perfect agreement between techniques for seven specific species suggests that for certain research contexts targeting these organisms, microscopy may remain adequate.
Experimental Protocols and Methodologies
Sample Collection and DNA Extraction
The reliability of any qPCR platform depends heavily on proper sample collection, handling, and nucleic acid extraction procedures. The following methodology has been employed in rigorous comparative studies [19]:
- Sample Collection: Stool samples should be collected in clean, sealed containers and processed immediately or within 30 minutes of collection. For delayed processing, samples must be transported on ice and examined within 1 hour.
- Fixation: After initial examination, samples should be fixed in absolute ethanol (96-100%) typically between 45 minutes and 1 hour after collection, then stored at 4°C before DNA extraction.
- DNA Extraction: Using a modified Qiagen stool procedure, aliquot 200 mg (200 μL for liquid stools) into tubes containing 200 mg of 2-mm glass beads and 1.5 mL of ASL buffer. Agitate vigorously at 3,200 rpm for 90 seconds, followed by heating at 95°C for 10 minutes. Complete extraction following manufacturer's protocols with an additional proteinase K incubation (55°C for 2 hours).
- Inhibition Assessment: Include an exogenous synthetic oligonucleotide internal control in the extraction process to detect potential PCR inhibition, amplifying this control post-extraction to validate results.
qPCR Amplification and Detection
For comparative studies, these experimental approaches ensure standardized evaluation:
- Assay Design: Utilize species-specific primers and TaqMan probes (hydrolysis probes) targeting conserved genomic regions. Design new primers using multiple sequence alignment tools (ClustalW2) and PRIMER 3 software, with specificity verified through BLAST analysis [19].
- Experimental Design Considerations: Implement efficient design strategies that use dilution-replicates instead of identical replicates. This approach allows simultaneous measurement of PCR efficiency and quantity, requiring fewer reactions while maintaining statistical power [94].
- Efficiency Calculation: Apply the standard curve method based on the relationship Cq = -log(d)/log(E) + log(T/Q(0))/log(E), where E represents PCR efficiency, d is dilution factor, T is threshold, and Q(0) is initial quantity [94].
- Data Analysis: Employ a collinear fit of standard curves across all samples to estimate a global PCR efficiency, increasing the accuracy of quantification when assuming E is constant across samples [94].
Multi-Laboratory Assessment Design
Robust validation of qPCR platforms requires carefully designed multi-laboratory studies:
- Study Phases: Implement sequential studies that progressively introduce additional sources of variability (e.g., sample preparation, instrumental analyses) to assess their impact on quantitative measurements [95].
- Standardized Protocols: Develop and distribute detailed standard operating procedures (SOPs) covering all aspects from sample preparation through data analysis to minimize inter-laboratory variation [95].
- Reference Materials: Utilize common reference materials and blinded samples across participating laboratories to enable direct comparison of results [79].
- Data Quality Control: Establish predefined quality control metrics and criteria for data inclusion, such as PCR efficiency ranges, correlation coefficients for standard curves, and limits of detection/quantification [79] [19].
Multi-laboratory qPCR validation workflow
Essential Research Reagent Solutions
The consistent performance of qPCR platforms depends heavily on the quality and standardization of research reagents. The following table details essential materials and their functions in protozoa detection studies [79] [19]:
Table 3: Essential Research Reagents for Protozoa qPCR Detection
| Reagent/Category | Function | Implementation Considerations |
|---|---|---|
| Species-Specific Primers/Probes | Target amplification and detection of specific protozoa | Must be designed against conserved genomic regions; require rigorous BLAST validation |
| DNA Polymerase | Enzymatic amplification of target sequences | Different polymerases may generate varying artifact profiles; affects reproducibility |
| Internal Control Oligonucleotides | Detection of PCR inhibition; quality control | Added during extraction process; co-amplified with sample DNA |
| DNA Extraction Kits | Nucleic acid purification from complex matrices | Critical for removing PCR inhibitors; significantly impacts sensitivity |
| Quantitative Standards | Standard curve generation for quantification | Serial dilutions of known templates; essential for determining PCR efficiency |
| Inhibition Assessment System | Detection of substances that may inhibit PCR | Uses synthetic sequence amplified alongside targets; validates negative results |
Standardization Strategies and Technical Considerations
Methodological Standardization Approaches
The observed variations in inter-assay agreement highlight the necessity for rigorous standardization, particularly in multi-center studies. Several strategies can enhance reproducibility:
- Implementation of Standard Operating Procedures (SOPs): Detailed SOPs for every stage from sample collection through data analysis are essential. These should specify acceptable sample types, storage conditions, extraction methodologies, and quality control checkpoints [19] [95].
- Reference Materials Utilization: Incorporate well-characterized reference materials and controls in each run to monitor assay performance and enable normalization across different laboratories and platforms [95].
- Cross-Platform Calibration: When using multiple platforms, implement cross-calibration protocols using shared reference samples to correct for systematic biases between systems [79].
- Data Reporting Standards: Adhere to established reporting guidelines such as the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) guidelines to ensure complete transparent reporting of methodological details [94].
Technical Factors Influencing Platform Performance
Several technical factors contribute to the observed performance differences between commercial and in-house platforms:
- Primer/Probe Design Specificity: Variations in target regions and oligonucleotide design significantly impact detection specificity and sensitivity, particularly for genetically diverse protozoa species [19].
- Amplification Efficiency Differences: The efficiency of the amplification reaction, influenced by polymerase fidelity and reaction chemistry, affects quantitative accuracy and detection limits [94].
- Inhibitor Tolerance: Stool samples contain numerous PCR inhibitors; platform differences in resistance to these substances can dramatically affect performance in clinical samples [19].
- Automation Level: Commercial kits typically offer higher standardization through pre-aliquoted reagents and simplified protocols, while in-house methods allow greater customization but require more rigorous validation [79].
Technical factors affecting qPCR platform performance
The multi-laboratory assessment of qPCR platforms for protozoa detection reveals a complex landscape where no single solution optimally addresses all research scenarios. Commercial platforms offer superior standardization and reproducibility between laboratories, making them preferable for multi-center studies, clinical trials, and surveillance programs where consistency across sites is paramount. In-house methods provide greater flexibility for targeting emerging pathogens or rare genetic variants and can be more readily adapted to specific research needs.
The substantial to almost perfect inter-assay agreement observed for most common protozoa indicates that with proper validation and standardization, multiple platforms can generate reliable data. However, the slight to poor agreement for certain species underscores the necessity of platform-specific validation and cautions against comparing data generated using different methodologies without proper cross-calibration. As molecular diagnostics continue to evolve, ongoing multi-laboratory assessments will remain essential for establishing performance benchmarks and guiding the selection of appropriate tools for specific research objectives in protozoology and drug development.
The detection and quantification of protozoan pathogens are critical for public health, ecological studies, and drug development. For years, traditional microscopy and quantitative PCR (qPCR) have been the cornerstone techniques in this field. However, the persistent challenges of detecting low-abundance pathogens, overcoming PCR inhibitors in complex samples, and achieving absolute quantification without standard curves have driven the adoption of more advanced technologies. Among these, Digital PCR (dPCR) has emerged as a powerful third-generation PCR technology that offers superior sensitivity, precision, and absolute quantification of nucleic acids [96].
This guide objectively compares the performance of dPCR platforms and assays against other molecular methods, specifically within the context of protozoa research. The focus on commercial versus in-house PCR assays is particularly relevant for researchers and scientists who must balance assay performance, standardization, cost, and flexibility in their experimental designs. Recent studies directly comparing these approaches for parasites like Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica provide valuable experimental data to inform these decisions [1] [4] [5].
Technology Comparison: dPCR, qPCR, and Traditional Methods
Performance Characteristics and Applications
Molecular diagnostic technologies, particularly real-time PCR (qPCR), have been gaining traction in non-endemic areas characterized by low parasitic prevalence due to their enhanced sensitivity and specificity compared to traditional microscopy [1]. However, dPCR, which is based on the partitioning of a PCR mixture into thousands of individual reactions, presents powerful advantages including high sensitivity, absolute quantification, high accuracy and reproducibility, as well as a rapid turnaround time [96].
The table below summarizes the core characteristics of these technologies based on recent comparative studies.
Table 1: Comparison of Diagnostic Technologies for Protozoan Pathogen Detection
| Technology | Key Principle | Quantification Method | Advantages | Key Limitations |
|---|---|---|---|---|
| Microscopy [1] | Visual identification of parasites in stained samples | Not quantitative (semi-quantitative estimates) | Low-cost; useful in high-prevalence, low-resource settings; can detect non-targeted parasites | Low sensitivity & specificity; investigator-dependent; cannot differentiate closely related species |
| qPCR / RT-qPCR [97] [98] | Amplification monitored in real-time via fluorescence | Relative quantification, requires a standard curve | High throughput; standardized commercial kits available; faster than conventional PCR | Affected by PCR inhibitors; quantification relies on accurate standards |
| Digital PCR (dPCR) [98] [96] | Limiting dilution & end-point fluorescence detection of partitioned reactions | Absolute quantification using Poisson statistics; no standard curve needed | Higher resilience to inhibitors; superior sensitivity for low-abundance targets; precise for copy number variation | Higher per-sample cost; limited throughput compared to qPCR; unable to sequence products directly [99] |
Experimental Data: Sensitivity and Detection Rates
Direct comparisons of diagnostic techniques consistently demonstrate the superior sensitivity of dPCR, especially in samples with low pathogen loads. A study on vector-borne pathogens in wild animals from Brazil provides compelling experimental data.
Table 2: Comparative Positivity Rates of Different PCR Techniques in Wild Animal Samples [99]
| Pathogen Group | nPCR Positivity Rate | qPCR Positivity Rate | dPCR Positivity Rate |
|---|---|---|---|
| Piroplasmids | Information Missing | Information Missing | 85.5% |
| Bartonella spp. | Information Missing | Information Missing | 33.6% |
| Borrelia spp. | Information Missing | Information Missing | 16.7% |
For all tested agents, dPCR proved to be the technique with the highest sensitivity, making it a useful tool for screening vector-borne agents in biological samples from wild animals with low parasitemia [99]. This enhanced sensitivity is crucial for environmental monitoring, wildlife disease surveillance, and detecting subclinical infections in humans.
Comparative Analysis of Commercial vs. In-House PCR Assays
Performance Agreement in Intestinal Protozoa Detection
The choice between commercial and in-house PCR assays is a critical one for laboratories. A multicentre study involving 18 Italian laboratories compared a commercial RT-PCR test (AusDiagnostics) and an in-house RT-PCR assay against traditional microscopy for identifying infections with key intestinal protozoa [1] [4].
Table 3: Comparison of Commercial and In-House PCR for Intestinal Protozoa (n=355 samples) [1] [4]
| Parasite | Agreement Between Commercial and In-House PCR | Noted Performance and Challenges |
|---|---|---|
| Giardia duodenalis | Complete agreement | Both methods demonstrated high sensitivity and specificity, similar to microscopy. |
| Cryptosporidium spp. | High specificity, but limited sensitivity for both | Limited sensitivity likely due to inadequate DNA extraction from the robust oocyst wall. |
| Dientamoeba fragilis | High specificity, but limited and inconsistent detection | Detection was inconsistent across methods. |
| Entamoeba histolytica | Molecular assays critical for accurate diagnosis | Microscopy cannot differentiate from non-pathogenic Entamoeba species. |
The study concluded that while molecular methods are promising, further standardization of sample collection, storage, and DNA extraction procedures is necessary for consistent results, particularly for some parasites [1] [4]. Another broad test comparison of 15 parasites and microsporidia in human stool samples found that the agreement between different commercial and in-house qPCR assays varied substantially by pathogen, ranging from "almost perfect" to "poor," highlighting the diagnostic challenges and the need for careful assay validation [5].
dPCR Platform-Specific Comparisons
Different dPCR platforms have been developed, primarily based on droplet (ddPCR) or chip-based partitioning. A 2025 study directly compared the QX200 droplet digital PCR from Bio-Rad and the QIAcuity One nanoplate-based digital PCR from QIAGEN for copy number comparisons in protists [100]. Both platforms demonstrated similar detection and quantification limits and yielded high precision across most analyses. The study also found that the choice of restriction enzyme (HaeIII vs. EcoRI) impacted precision, especially for the QX200 system [100]. This highlights that, beyond the platform itself, sample preparation is a critical factor for robust performance.
Experimental Protocols from Key Studies
Protocol 1: Comparative dPCR Platform Performance for Protist Gene Copy Number
This protocol is derived from a 2025 study comparing the precision of two dPCR applications for copy number comparisons in protists [100].
- Sample Preparation:
- Use synthetic oligonucleotides or DNA extracted from a known number of cells (e.g., the ciliate Paramecium tetraurelia).
- Test the impact of different restriction enzymes (e.g., HaeIII and EcoRI) on gene copy number quantification.
- Partitioning and Amplification:
- Use the QX200 ddPCR System (Bio-Rad) and the QIAcuity One System (QIAGEN) according to manufacturers' instructions.
- Partition the PCR mixture containing the sample DNA, primers, probes, and master mix. The QX200 system generates droplets, while the QIAcuity system uses nanoplates with integrated partitions.
- PCR Cycling:
- Perform endpoint PCR amplification using a standard thermal cycling protocol optimized for the specific primer-probe sets.
- Data Analysis:
- Read the partitions on the respective instruments (droplet reader for QX200, imaging for QIAcuity).
- Use the manufacturer's software to analyze the fraction of positive and negative partitions.
- Apply Poisson statistics to calculate the absolute concentration of the target gene (copies per microliter) in the original sample.
- Validation:
- Assess linearity by analyzing DNA from a series of increasing cell numbers.
- Compare the precision (reproducibility) and limits of detection/quantification between the two platforms.
Protocol 2: ddPCR for Enumeration ofCryptosporidiumOocysts
This protocol is based on a seminal study comparing ddPCR with qPCR for the enumeration of Cryptosporidium oocysts in faecal samples [98].
- DNA Sources:
- Extract DNA from a range of templates: recombinant plasmids, haemocytometer-counted purified oocysts, commercial oocyst standards, and faecal DNA from sheep, cattle, and humans.
- ddPCR Reaction:
- Set up a 20μL probe-based PCR reaction mixture using a ddPCR supermix.
- Generate droplets from the reaction mixture using a droplet generator (e.g., QX200 Droplet Generator, Bio-Rad).
- PCR Amplification:
- Transfer the emulsified samples to a 96-well plate and perform PCR amplification in a thermal cycler.
- Droplet Reading and Analysis:
- Place the plate in a droplet reader (e.g., QX200 Droplet Reader, Bio-Rad) which measures the fluorescence of each droplet.
- Use associated software to classify droplets as positive or negative and calculate the absolute concentration of the target DNA (copies/μL) based on Poisson statistics.
- qPCR Comparison:
- Run the same DNA samples in parallel using qPCR with a standard curve constructed from known concentrations of the target DNA.
- Comparison Metrics:
- Evaluate and compare both methods for linearity, precision, limit of detection, and cost.
Diagram 1: ddPCR Workflow for Absolute Quantification.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting dPCR experiments in protozoa research, based on methodologies described in the search results.
Table 4: Essential Reagents and Materials for dPCR in Protozoa Research
| Item | Function / Application | Examples / Notes |
|---|---|---|
| dPCR Master Mix | Provides optimized buffer, dNTPs, and polymerase for amplification in partitions. | Specific ddPCR supermix for droplet systems [98]; QIAcuity PCR Master Mix for nanoplate systems [100]. |
| Primers & Hydrolysis Probes | Target-specific amplification and detection. | Designed for specific protozoan genes (e.g., 18S rRNA, actin) [98]; kDNA minicircle for Leishmania [101]. |
| Restriction Enzymes | Digest genomic DNA to reduce viscosity and improve access to target genes, enhancing precision. | HaeIII, EcoRI [100]. |
| DNA Standards | Used for qPCR standard curves and for validating dPCR absolute quantification. | Recombinant plasmids, quantified synthetic oligonucleotides, genomic DNA from counted oocysts [98]. |
| Partitioning Consumables | Physical media for creating nanoscale reactions. | DG8 Cartridges and Droplet Generation Oil for ddPCR [98]; QIAcuity Nanoplate for partition-based dPCR [100] [99]. |
| DNA Extraction Kits | Isolate inhibitor-free DNA from complex samples (stool, water, tissue). | Kits with inhibitor removal steps are critical; method significantly impacts sensitivity [1] [97]. MagNA Pure 96 System [1]. |
| Inhibition Controls | Detect the presence of PCR inhibitors in the sample. | Internal extraction controls [1]; murine hepatitis virus (MHV) seeded as an RNA extraction control [97]. |
Market Trends and Future Directions
The global dPCR market is experiencing significant growth, driven by its advantages in sensitivity and quantification. The market is projected to grow from USD 857.2 million in 2025 to USD 3,678.8 million by 2032, exhibiting a CAGR of 23.1% [102]. A key trend is the gradual shift from droplet-based to chip-based dPCR systems, as chips reduce the risk of cross-contamination and offer a more automated, technically simple workflow [102]. This is evidenced by the popularity of systems like the QIAcuity [100] [96].
Future applications will likely expand in several key areas relevant to protozoa research:
- Environmental Monitoring: Detecting low levels of pathogenic protozoa in water systems with higher accuracy [100] [97].
- One Health and Wildlife Surveillance: Unraveling the occurrence of piroplasmids, Bartonella, and Borrelia in wild animal reservoirs with superior sensitivity [99].
- Clinical Diagnostics: Moving beyond a complementary role to become a primary diagnostic tool for challenging pathogens, especially as costs decrease and standardization improves [1] [96].
Diagram 2: dPCR Market and Technology Trends.
Conclusion
The choice between commercial and in-house PCR for protozoa detection is context-dependent, requiring careful consideration of performance needs, resources, and infrastructure. Recent multicenter studies confirm that both methods show excellent agreement for common targets like Giardia duodenalis, but commercial kits offer standardization while in-house assays provide flexibility. Key challenges remain in DNA extraction efficiency and sample preservation, particularly for Cryptosporidium and Dientamoeba fragilis. Future success hinges on standardizing sample processing, adopting digital PCR for absolute quantification, and developing multiplex assays that expand diagnostic panels. For researchers and drug developers, these advancements promise more accurate epidemiological data, enhanced clinical trial monitoring, and robust therapeutic efficacy assessments, ultimately advancing global protozoa disease control.
References
- 1. Comparative analysis of commercial and “In-House ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317615/]
- 2. Epidemiological Characteristics of Intestinal Protozoal ... [https://www.researchprotocols.org/2025/1/e66350]
- 3. Burden and Distribution of Protozoan Pathogens in Diarrhea ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494489/]
- 4. Comparative analysis of commercial and "In-House ... [https://pubmed.ncbi.nlm.nih.gov/40751255/]
- 5. Comparison of commercial and in-house real-time PCR ... [https://www.sciencedirect.com/science/article/abs/pii/S0001706X19317693]
- 6. Comparative analysis of commercial and “In-House ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9/tables/3]
- 7. Performance of 30 protocol combinations for the detection ... [https://www.sciencedirect.com/science/article/pii/S1684118225000064]
- 8. Performance Evaluation of a Commercial Real-Time PCR ... [https://www.mdpi.com/2076-2607/8/11/1692]
- 9. Analysis of Parasitic Protozoa at the Single-cell Level using ... [https://www.nature.com/articles/s41598-017-02715-y]
- 10. Performance of microscopy compared to conventional PCR ... [https://www.sciencedirect.com/science/article/abs/pii/S0255085723001433]
- 11. Multiplex PCR for gastrointestinal parasites in stool [https://www.sciencedirect.com/science/article/abs/pii/S0732889324003018]
- 12. Comparative analysis of commercial and “In-House ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 13. Molecular Biology Can Change the Classic Laboratory ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.02191/full]
- 14. Strength, weakness, opportunities and challenges (SWOC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12305316/]
- 15. Digital Pathology vs. Traditional Methods [https://www.grundium.com/blog/digital-pathology-vs-traditional-methods/]
- 16. Comparison of the efficiency of digital pathology with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12088733/]
- 17. Comparative evaluation of real-time PCR and ELISA for the ... [https://www.nature.com/articles/s41598-024-54602-y]
- 18. ELISA versus PCR for diagnosis of chronic Chagas disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC3004908/]
- 19. Performance of Real-Time Polymerase Chain Reaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5508894/]
- 20. Evaluation of Each Three Entamoeba histolytica [https://www.mdpi.com/2076-2607/13/9/1976]
- 21. Implementation of real-time PCR assays for diagnosing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11978536/]
- 22. Validation of an Automated High-Throughput Multiplex ... [https://www.mdpi.com/2673-947X/5/1/8]
- 23. Evaluation of a Novel Commercial Real-Time PCR Assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9241732/]
- 24. Comparison of Commercial and In-House Real-Time PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2643664/]
- 25. Commercial Simplex and Multiplex PCR Assays for the ... [https://pubmed.ncbi.nlm.nih.gov/34835453/]
- 26. Comparative Performance of Eight PCR Methods to Detect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8224656/]
- 27. Comparative Performance of Eight PCR Methods to Detect ... [https://pubmed.ncbi.nlm.nih.gov/34071125/]
- 28. Comparative performance evaluation of four commercial ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0215068]
- 29. Comparative Evaluation of Real-Time Screening PCR ... [https://www.mdpi.com/2076-2607/10/7/1310]
- 30. Transitioning from microscopy to PCR for protozoa in Norway [https://pmc.ncbi.nlm.nih.gov/articles/PMC12281236/]
- 31. Clinical evaluation of AusDiagnostics SARS-CoV-2 multiplex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7236671/]
- 32. Evaluation of Two Broadly Used Commercial Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9324506/]
- 33. An evaluation of the commercial AusDiagnostics versus in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7195305/]
- 34. Comparison of In-house PCR with Conventional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2615280/]
- 35. Validating Real-Time Polymerase Chain Reaction (PCR) Assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC7834634/]
- 36. evaluation of four Comparative multiplex... performance commercial [https://pmc.ncbi.nlm.nih.gov/articles/PMC6453453/]
- 37. Optimization of the real-time PCR platform method using ... [https://pubmed.ncbi.nlm.nih.gov/41038937/]
- 38. Development of loop mediated isothermal amplification ... [https://www.nature.com/articles/s41598-025-93995-2]
- 39. In-house validation of a droplet digital PCR system using ... [https://www.sciencedirect.com/science/article/pii/S0003267025005665]
- 40. DNA Extraction from Protozoan Oocysts/Cysts in Feces ... [https://www.parahostdis.org/m/journal/view.php?doi=10.3347/kjp.2014.52.3.263]
- 41. Comparison of DNA extraction methods on different ... [https://www.nature.com/articles/s41598-024-59086-4]
- 42. Optimization and validation of methods for isolation ... [https://www.sciencedirect.com/science/article/pii/S2405676615300299]
- 43. Comparison of DNA Extraction Methods for the Direct ... [https://www.mdpi.com/2073-4441/14/22/3736]
- 44. Comparison and Optimization of DNA Extraction Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11932244/]
- 45. Comparison of four multiplex PCR assays for the detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7119551/]
- 46. Performance Comparison of In-House and Commercial ... [https://www.mdpi.com/2075-4418/15/22/2928]
- 47. Performance of an in-house multiplex PCR assay for HIV-1 ... [https://www.sciencedirect.com/science/article/pii/S0166093424001587]
- 48. A comparison of two multiplex-PCR assays for the diagnosis ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-05885-3]
- 49. Multiplex PCR assay for the rapid detection of Klebsiella ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578128/]
- 50. Multiplex PCR Assays Market | Global Market Analysis ... [https://www.futuremarketinsights.com/reports/multiplex-pcr-assays-market]
- 51. Removal of PCR inhibitors from human faecal samples ... [https://www.sciencedirect.com/science/article/abs/pii/S0167701297009792]
- 52. Frontiers | PCR of a Quantitative Inhibition for Detection of... PCR [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.00115/full]
- 53. Selecting PCR for the Diagnosis of Intestinal Parasitosis: Choice of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5695021/]
- 54. Assessment of a commercially available multiplex real-time ... [https://www.sciencedirect.com/science/article/pii/S1944398624118632]
- 55. Rapid and efficient method to eliminate substances ... [https://pubmed.ncbi.nlm.nih.gov/8914252/]
- 56. Multicenter comparative study of Enterocytozoon bieneusi ... [https://www.nature.com/articles/s41598-024-66154-2]
- 57. Evaluation of five commercial methods for the extraction ... [https://www.sciencedirect.com/science/article/abs/pii/S0167701216301075]
- 58. Comparative evaluation of DNA extraction protocols for ... [https://www.sciencedirect.com/science/article/pii/S2950194625001669]
- 59. a comparison of DNA extraction and library building methods [https://www.nature.com/articles/s41598-025-88443-0]
- 60. Metagenomic detection of protozoan parasites on leafy ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1566579/full]
- 61. [PDF] Comparative analysis of commercial and “In-House” ... [https://www.semanticscholar.org/paper/Comparative-analysis-of-commercial-and-%E2%80%9CIn-House%E2%80%9D-Pietra-Gargiulo/a337fdce909109634c2da0842d79fcbd7dc1ca40]
- 62. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimenproc.html]
- 63. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimencoll.html]
- 64. Detection of Intestinal Protozoa in the Clinical Laboratory - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3957779/]
- 65. Advantages and Limitations of Microscopy and Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9979072/]
- 66. Comparison of fresh versus sodium acetate acetic acid ... [https://pubmed.ncbi.nlm.nih.gov/8681983/]
- 67. A comparative analysis of preservation techniques for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5773002/]
- 68. Assessing morphological preservation of gastrointestinal ... [https://www.nature.com/articles/s41598-024-53915-2]
- 69. Effective low-cost preservation of human stools in field ... [https://www.sciencedirect.com/science/article/pii/S0020751921001119]
- 70. The impact of genetic diversity in protozoa on molecular ... [https://www.sciencedirect.com/science/article/abs/pii/S1471492210002345]
- 71. Development and Preliminary Application of a Triplex Real ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.888529/full]
- 72. Evaluation of Allplex™ GI-Parasite Assay—A Multiplex ... [https://www.mdpi.com/2414-6366/10/8/234]
- 73. - In had greater sensitivity than house test kits for... PCR commercial [https://www.healio.com/news/gastroenterology/20140908/icaachartmeyer_10-3928_1081_597x_20140901_07_1354957]
- 74. Implementation of real-time PCR assays for diagnosing ... [https://link.springer.com/article/10.1007/s00436-025-08483-3]
- 75. Comparative Evaluation of Real-Time Screening PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9321168/]
- 76. Comparison of Microscopy and PCR for Detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8047253/]
- 77. Comparison of Giardia duodenalis point-of-care antigen ... [https://www.sciencedirect.com/science/article/pii/S030440172400027X]
- 78. Is real-time PCR-based diagnosis similar in performance to ... [https://www.sciencedirect.com/science/article/pii/S1198743X15009441]
- 79. Comparison of commercial and in-house real-time PCR ... [https://pubmed.ncbi.nlm.nih.gov/32371221/]
- 80. An Improved PCR-RFLP Assay for Detection and ... [https://www.parahostdis.org/m/journal/view.php?number=1978]
- 81. Comparative Pathobiology of the Intestinal Protozoan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6789772/]
- 82. Performance of a rapid diagnostic test for the detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7377516/]
- 83. Dientamoeba fragilis, One of the Neglected Intestinal Protozoa [https://pmc.ncbi.nlm.nih.gov/articles/PMC5005499/]
- 84. A comparison of Dientamoeba fragilis and Giardia lamblia ... [https://www.sciencedirect.com/science/article/pii/S1201971205002080]
- 85. Performance of diagnostic assays used to detect ... [https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-022-03435-w]
- 86. Implementation of real-time PCR assays for diagnosing ... [https://pubmed.ncbi.nlm.nih.gov/40198454/]
- 87. Diagnostic dilemma: application of real-time PCR assays for ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06730-1]
- 88. Real-time PCR assay in differentiating Entamoeba histolytica ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/1756-3305-6-250]
- 89. Real-Time-PCR Assay for Diagnosis of Entamoeba ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1153781/]
- 90. A novel nested multiplex polymerase chain reaction (PCR ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/1471-2180-7-47]
- 91. Real-Time PCR for Detection and Differentiation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC154634/]
- 92. Comparative assessment of three commercial kits and in ... [https://www.sciencedirect.com/science/article/pii/S2215016124003303]
- 93. Comparison of commercial and in-house Real-time PCR ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/1471-2180-7-22]
- 94. Efficient experimental design and analysis of real-time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3710343/]
- 95. Multi-site assessment of the precision and reproducibility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2855883/]
- 96. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 97. Comparison of RT-qPCR and RT-dPCR Platforms for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8848507/]
- 98. Comparison of next-generation droplet digital PCR ... [https://www.sciencedirect.com/science/article/abs/pii/S0020751914002264]
- 99. Using Digital PCR to Unravel the Occurrence of ... [https://www.mdpi.com/2076-0817/14/6/567]
- 100. Comparing the precision of two digital PCR applications for ... [https://pubmed.ncbi.nlm.nih.gov/40715338/]
- 101. Exploring real-time PCR techniques for diagnosing ... [https://pubmed.ncbi.nlm.nih.gov/40397177/]
- 102. Digital PCR Market Share, Growth Analysis | Forecast [2032] [https://www.fortunebusinessinsights.com/digital-pcr-market-102014]