Breaking Detection Limits: Advanced Strategies for Diagnosing Low-Intensity Parasite Infections
Accurate detection of low-intensity parasite infections is a critical frontier in the control and elimination of parasitic diseases.
Breaking Detection Limits: Advanced Strategies for Diagnosing Low-Intensity Parasite Infections
Abstract
Accurate detection of low-intensity parasite infections is a critical frontier in the control and elimination of parasitic diseases. This article synthesizes the latest advancements in diagnostic technologies, from refined concentration techniques to molecular and AI-powered methods, which are revolutionizing sensitivity for submicroscopic and low egg burden infections. Tailored for researchers, scientists, and drug development professionals, we explore the foundational challenges of light infections, evaluate novel methodological applications, provide frameworks for test optimization, and present comparative validation data. The content underscores how these innovations are essential for accurate surveillance, effective treatment, and ultimately, the interruption of disease transmission in elimination settings.
The Hidden Reservoir: Understanding the Challenge of Low-Intensity Parasite Infections
The Critical Impact of Subpatent Infections on Disease Transmission and Elimination Goals
FAQs: Understanding Subpatent Infections
What is a subpatent malaria infection? A subpatent infection is a Plasmodium falciparum malaria infection that is detectable by molecular methods (like PCR) but not detectable by standard field diagnostics such as microscopy or Rapid Diagnostic Tests (RDTs) [1] [2]. These infections are characterized by low parasite densities that fall below the detection threshold of conventional diagnostics.
How do subpatent infections challenge malaria elimination? Subpatent infections contribute significantly to the infectious reservoir. Individuals with subpatent asexual parasite densities are approximately one-third as infectious to mosquitoes as those with patent infections [1] [2]. Because they escape detection by standard diagnostics, they often remain untreated and can sustain silent transmission, even in areas where control efforts are intensifying [3].
In what settings are subpatent infections most prevalent? While subpatent infections occur in all transmission settings, they constitute a higher proportion of all infections in low transmission settings [1]. This is because the average parasite density in infected individuals is lower in these areas compared to higher transmission settings [1] [2].
Can a person with a subpatent infection develop symptoms later? Yes, longitudinal cohort studies indicate that subpatent infections are predictive of future periods of patent infection [1] [2]. Parasite densities fluctuate over time, and a low-density infection can evolve into a higher-density, symptomatic infection.
Troubleshooting Guides
Issue: High Proportion of PCR-Positive Samples are RDT-Negative in a Low Transmission Area
Problem: Your surveillance data shows a significant number of samples are positive by PCR but negative by RDT, suggesting a large subpatent reservoir.
Solution:
- Confirm with a sensitive, quantitative PCR (qPCR) method: Use qPCR to quantify the parasite densities in your samples [1]. This will help confirm that the infections are truly low-density.
- Re-assess your diagnostic strategy: In low-transmission settings aiming for elimination, consider switching to more sensitive diagnostics for surveillance, even if they are not yet deployable for routine case management [1].
- Investigate the infectious potential: If studying transmission, conduct mosquito feeding assays (e.g., membrane feeding) to determine the infectivity of these subpatent infections, as they can still transmit to mosquitoes [1] [2].
Issue: Inconsistent Microscopy Results Despite Positive PCR
Problem: Expert microscopists report negative slides, but your PCR results consistently come back positive for P. falciparum.
Solution:
- Understand the limitations of microscopy: The probability of detecting an infection by microscopy is highly variable. At a qPCR-detected density of 100 parasites/µL, the probability of microscopy detection across studies ranged from 3.8% to 69.7% [1]. Discrepancies are common.
- Quantify the density: Use qPCR to determine the actual parasite density. Many subpatent infections have densities >100 parasites/µL, a range often considered detectable by microscopy, yet they are still missed [1].
- Check for staining quality and reader experience: Ensure that your microscopy protocols are optimized and that readers are regularly trained and validated.
Key Data on Subpatent Infections
Table 1: Parasite Density and Detectability in Different Transmission Settings
| Transmission Setting (PCR Prevalence) | Median Parasite Density (parasites/µL) | Proportion of Infections that are Subpatent | Approx. % of Infections with Density >100 parasites/µL |
|---|---|---|---|
| Low Transmission | Below 5 | Highest Proportion | 1% - 40% (mean ~42%) |
| High Transmission | Up to 100 | Lower Proportion | Up to 97% (mean ~42%) |
Data synthesized from analysis of 22 locations, with molecular prevalence ranging from 0.4% to 90.6% [1].
Table 2: Comparison of Patent vs. Subpatent Infection Characteristics
| Characteristic | Patent Infection | Subpatent Infection |
|---|---|---|
| Detection by RDT/Microscopy | Yes | No |
| Detection by PCR | Yes | Yes |
| Relative Infectiousness to Mosquitoes | Baseline (1x) | ~1/3 as infectious [1] [2] |
| Typical Symptom Status | More likely symptomatic | More likely asymptomatic [2] |
| Contribution to Reservoir | Well-characterized | Significant, but often missed and untreated [4] |
Experimental Protocols
Protocol: Detecting and Quantifying Subpatent Infections via qPCR
Purpose: To accurately identify and quantify low-density Plasmodium falciparum infections in human blood samples.
Materials:
- Research Reagent Solutions:
- DNA Extraction Kit: Chelex-saponin-based method or commercial kit for extracting DNA from dried blood spots [4].
- Quantitative PCR (qPCR) Master Mix: Contains polymerase, dNTPs, and buffer.
- Primers/Probes: Specific for the P. falciparum 18S ribosomal subunit gene [4].
- Standard Curve DNA: Serial dilutions of a known quantity of P. falciparum DNA for absolute quantification.
Methodology:
- Sample Collection: Collect finger-prick blood onto filter paper (Whatman 3MM). Dry thoroughly and store with desiccant at -80°C until processing [4].
- DNA Extraction:
- Punch out 2-3 sections of the blood spot filter paper.
- Elute DNA using a Chelex-saponin protocol or a commercial kit optimized for blood spots [4].
- Centrifuge and collect the supernatant containing the DNA.
- qPCR Setup:
- Prepare reactions in duplicate/quadruplicate to ensure accuracy.
- Include a standard curve with known parasite densities (e.g., from 0.1 to 10,000 parasites/µL), negative controls (nuclease-free water), and positive controls.
- Amplification: Run the qPCR using cycling conditions optimized for your instrument and primer/probe set.
- Data Analysis:
- Use the standard curve to interpolate the parasite density (parasites/µL of blood) for each sample.
- Define the limit of detection (LOD) for your assay based on the lowest standard that amplifies consistently.
Protocol: Assessing Infectiousness of Subpatent Infections via Membrane Feeding Assay
Purpose: To determine the potential of subpatent infections to transmit to mosquito vectors.
Materials:
- Research Reagent Solutions:
- Mosquito Rearing: Laboratory-reared, pathogen-free Anopheles mosquitoes (e.g., 3-5 days old).
- Membrane Feeding Apparatus: Water-jacketed glass feeders with parafilm membranes.
- Human Serum: To supplement the blood meal.
Methodology:
- Participant Screening: Identify asymptomatic individuals who are PCR-positive but RDT-negative (subpatent) and those who are RDT-positive (patent) for comparison [1] [2].
- Blood Collection: Draw a small volume of venous blood (e.g., 5-10 mL) into heparinized or serum-coated tubes.
- Feeding Assay:
- Prepare the blood meal by mixing the participant's blood with human serum.
- Load the blood into the membrane feeder, warmed to 37°C.
- Allow mosquitoes to feed for 15-20 minutes in the dark.
- Mosquito Maintenance: After feeding, engorged females are separated and maintained with sugar solution for 7-14 days.
- Dissection and Analysis:
- Dissect mosquito midguts to count oocysts to determine the prevalence and intensity of infection.
- Alternatively, analyze salivary glands for sporozoites after a longer incubation period.
- Data Analysis:
- Calculate the proportion of infected mosquitoes (oocyst prevalence) and the mean oocyst intensity for each group (subpatent vs. patent).
- The relative infectiousness can be expressed as the ratio of these measures between the subpatent and patent groups [1].
Diagnostic and Research Workflows
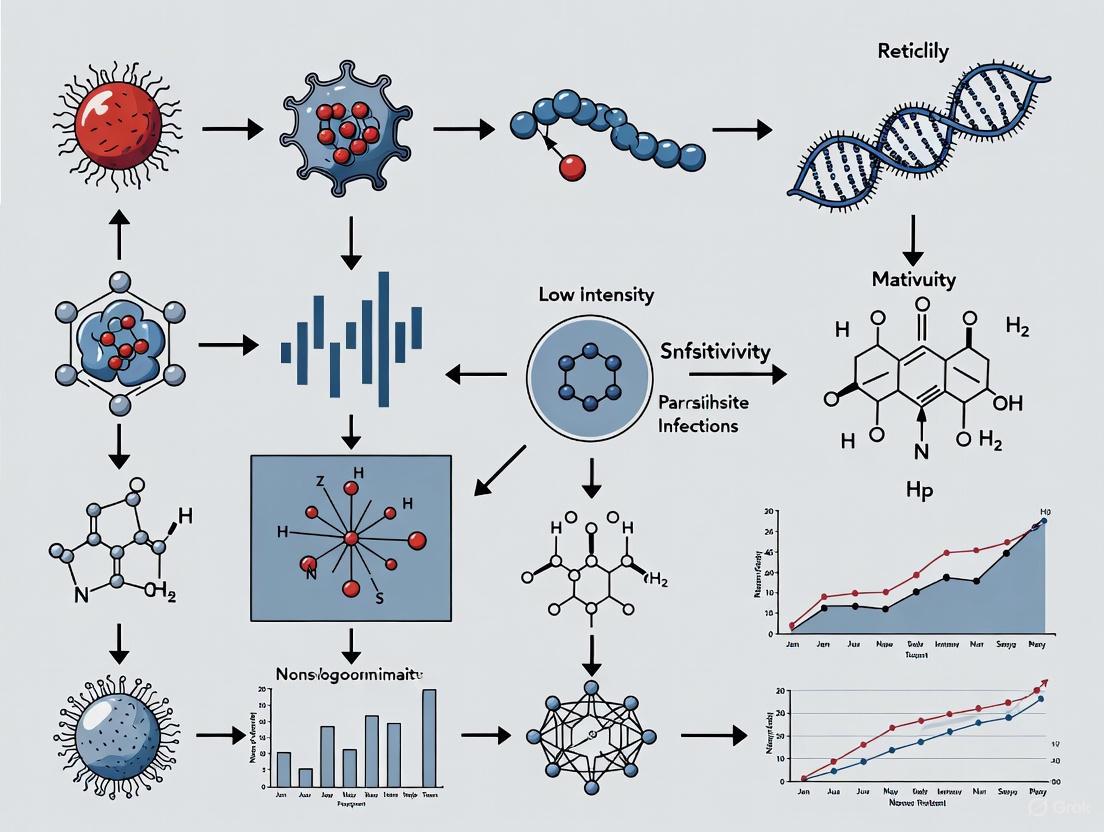
Diagram Title: Diagnostic Pathway for Subpatent Infection Identification
Diagram Title: Parasite Density Dynamics Across Transmission Settings
For researchers and drug development professionals working towards malaria elimination, a central challenge is the "diagnostic gap"—the inability of conventional diagnostic methods to detect low-density and asymptomatic malaria infections. These submicroscopic reservoirs sustain transmission and jeopardize control efforts [5] [6]. This guide details the performance limits of microscopy and Rapid Diagnostic Tests (RDTs), provides protocols for enhanced detection, and offers solutions to bridge this gap in your research.
FAQ: Understanding the Diagnostic Gap
1. What is the "diagnostic gap" in malaria research? The diagnostic gap refers to the significant number of malaria infections that remain undetected by conventional microscopy and RDTs due to low parasite density. These are often asymptomatic infections that act as hidden reservoirs for ongoing transmission, posing a major challenge for elimination campaigns [5] [6] [7].
2. How does decreasing malaria prevalence affect microscopy sensitivity? Counterintuitively, as malaria prevalence decreases, the detection threshold of microscopy appears to rise, leading to more missed infections. A recent longitudinal study in Brazil found that most infections in an urban setting were asymptomatic and undetected by microscopy, despite molecular methods confirming persistent parasite densities [5].
3. What are the typical detection limits for conventional methods? The following table summarizes the approximate limits of detection (LoD) for common diagnostic methods:
Table 1: Limits of Detection for Malaria Diagnostic Methods
| Diagnostic Method | Approximate Limit of Detection (parasites/µL) | Key Limitations |
|---|---|---|
| Light Microscopy | 50 - 500 [8] [7] [9] | Low sensitivity for low-density infections; requires expertise |
| Rapid Diagnostic Tests (RDTs) | ~100 [8] | pfhrp2/3 gene deletions, persistent antigens, lower sensitivity for non-falciparum species [8] [10] |
| PCR | 5 - 10 [8] | Complex, costly, not field-deployable |
| Quantitative PCR (qPCR) | 0.5 - 5 [7] | Complex, costly, not field-deployable |
4. What is the quantitative impact of false-negative results? The scale of the diagnostic gap is substantial. Studies from different endemic regions illustrate this:
Table 2: Documented False-Negative Rates in Field Studies
| Location | Method | False-Negative Rate vs. Reference | Reference Standard |
|---|---|---|---|
| Equatorial Guinea [8] | Microscopy | 19.4% | SnM-PCR |
| Equatorial Guinea [8] | RDT | 13.3% | SnM-PCR |
| Ghana (Children <6 yrs) [9] | Single Microscopy | 11.9% | Serial Microscopy (cumulative yield at 12h) |
5. How do asymptomatic infections contribute to the diagnostic gap? Asymptomatic infections are characterized by very low and fluctuating parasitemia, often falling below the detection threshold of conventional methods. Mathematical models indicate that asymptomatic cases can contribute approximately 30% to the basic reproduction number (R₀), highlighting their substantial role in sustaining transmission [6].
Troubleshooting Guides & Enhanced Protocols
Guide 1: Improving Microscopy Sensitivity for Low-Parasite Density Specimens
The standard single-thick smear examination is insufficient for detecting low-level parasitemia. The following workflow can significantly enhance detection sensitivity.
Experimental Protocol: Repeated Microscopy for Enhanced Detection
- Background: This protocol is adapted from a study showing that serial sampling improved malaria detection in children by 11.9% compared to a single test [9].
- Procedure:
- Baseline Smear: Collect a finger-prick blood sample and prepare a standard thick blood smear. Stain with 10% Giemsa for 10 minutes [9].
- Microscopy: Examine the smear under oil immersion (1000x magnification). A slide is only declared negative after reviewing a minimum of 100 microscopic fields without detecting any parasites [5] [8].
- Serial Sampling: For research subjects with a high clinical or epidemiological index of suspicion (e.g., fever in an endemic area) but a negative baseline smear, collect repeat samples at 6 hours and 12 hours post-baseline.
- Quality Control: Have all slides read by a second, experienced microscopist. In case of discrepancy, a third reader serves as a tie-breaker [10].
- Key Data: In the referenced study, the parasitaemia in initially negative patients was drastically lower (ranges: 1,708–7,110 parasites/µL at follow-up) compared to baseline positives (9,815–83,452 parasites/µL), explaining the initial missed diagnoses [9].
Guide 2: Validating RDT Results and Investigating False Negatives
RDTs are prone to false negatives due to low parasite density, pfhrp2/3 gene deletions, or issues with test performance.
Experimental Protocol: Molecular Confirmation of RDT Results
- Background: This protocol uses PCR or qPCR as a reference standard to identify false-negative RDTs resulting from low parasitemia or genetic deletions [8] [10] [7].
- Procedure:
- Sample Collection: For every subject, perform the RDT according to the manufacturer's instructions. Simultaneously, collect blood spotted onto filter paper (e.g., Whatman 903) for molecular analysis [8] [7].
- DNA Extraction: Use a standardized method such as the Saponin/Chelex protocol to extract genomic DNA from the dried blood spots [7].
- Molecular Diagnosis:
- Screening: Use a genus-specific PCR (e.g., targeting the
cytbgene) for high sensitivity [5]. - Species Identification & Quantification: Use species-specific quantitative TaqMan assays (e.g., targeting the
cox1gene for P. vivax or P. falciparum) to confirm the species and estimate parasite density [5].
- Screening: Use a genus-specific PCR (e.g., targeting the
- Investigate Gene Deletions: For P. falciparum isolates that are RDT-negative but PCR-positive, perform further assays (e.g., PCR amplification of the
pfhrp2andpfhrp3genes) to confirm deletions [10].
- Key Consideration: qPCR is the most sensitive method, capable of detecting parasitemia below 5 parasites/µL, making it essential for characterizing the submicroscopic reservoir [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating the Diagnostic Gap
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Whatman 903 Filter Paper | Stable, room-temperature storage of blood samples for DNA analysis; ideal for field collection and transport. | Used for collecting and transporting >11,000 asymptomatic samples in Kenya [7]. |
| Giemsa Stain (10%) | Standard staining of thick and thin blood films for microscopic visualization of parasites. | Used for staining slides in multiple studies; consistent protocol is critical [5] [8] [9]. |
| HRP2-based RDTs | Detects P. falciparum-specific Histidine-Rich Protein 2. Critical for studying pfhrp2 deletion mutants. |
The bivalent SD Bioline Malaria Ag P.f/P.v RDT was used in a 2025 Indian study [10]. |
| pLDH-based RDTs | Detects Plasmodium Lactate Dehydrogenase; used for detecting non-falciparum species and active infection. | The NADAL Malaria 4 species test (detects HRP2 and pLDH) was used in Equatorial Guinea [8]. |
| TaqMan Probe Master Mix | For quantitative PCR (qPCR) assays enabling highly sensitive and specific parasite detection and quantification. | Used with species-specific assays targeting mitochondrial genome sequences [5]. |
| Saponin/Chelex Reagents | DNA extraction from dried blood spots; effective and economical for processing large sample volumes. | Used to extract DNA from over 11,000 field samples in Western Kenya [7]. |
What is the central paradox discussed in this technical guide? This guide addresses a critical challenge in parasitic disease control: as mass drug administration (MDA) programs successfully reduce overall infection prevalence and intensity in a community, the proportion of remaining infections that are of low intensity increases. These low-intensity infections are harder to detect with standard diagnostics, creating a surveillance gap that can threaten the sustainability of control gains and the achievement of elimination goals [11] [12].
What key epidemiological shift occurs during successful control programs? The epidemiological transition in soil-transmitted helminth (STH) control is characterized by a shift from a high prevalence of moderate- and high-intensity infections to a situation where the majority of remaining cases are low-intensity infections. This shift is a direct result of the reduced worm burden in the population following repeated MDA. While this represents a public health success, it demands a corresponding shift in diagnostic and surveillance strategies, as the sensitivity of many common copro-microscopic tests declines significantly in low-transmission settings [11].
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Our control program has successfully reduced community worm burdens. Why are our lab staff now reporting more "negative" results in monitoring surveys, even though we suspect transmission continues?
- Problem: This is a classic symptom of the epidemiological shift. Standard diagnostics like the Kato-Katz method experience a significant drop in sensitivity in low-intensity settings.
- Root Cause: The Kato-Katz technique examines a small fixed amount of stool (typically 41.7 mg). In a low-intensity infection, the number of eggs per gram of stool is very low, increasing the probability that the small sample examined contains no eggs, resulting in a false negative [11].
- Solution: Transition to more sensitive diagnostic methods for post-control surveillance.
- FLOTAC and Mini-FLOTAC techniques process a larger stool sample (up to 1 gram and 0.5 grams, respectively), which dramatically increases the chance of detecting low egg counts [11].
- Formol-Ether Concentration (FEC) methods also concentrate parasites from a larger sample, improving sensitivity over direct smear or single Kato-Katz thick smear [11] [13].
- Molecular methods (PCR) offer high sensitivity and species-specific identification, though they may be more costly and require specialized equipment [14].
FAQ 2: How significant is the drop in sensitivity for the Kato-Katz method in low-intensity settings, and how does this impact our monitoring data?
- Problem: Without quantifying the sensitivity loss, programs may misinterpret falling prevalence figures as indicating elimination is near, when in fact infections are merely harder to detect.
- Data-Driven Solution: A Bayesian latent class meta-analysis provides the following estimates for test sensitivity. This data should inform your choice of diagnostic tool as your program progresses [11].
Table 1: Sensitivity of Diagnostic Tests for Soil-Transmitted Helminths (STH) by Infection Intensity
| Diagnostic Method | Overall Sensitivity (%) | Sensitivity in High-Intensity Settings (%) | Sensitivity in Low-Intensity Settings (%) |
|---|---|---|---|
| FLOTAC | 92.7 | High | Highest |
| Kato-Katz (double slide) | 74.0 - 95.0* | 74 - 95 | 53 - 80 |
| Mini-FLOTAC | Comparable to Kato-Katz | Comparable to Kato-Katz | Comparable to Kato-Katz |
| Direct Microscopy | 42.8 | Low | Lowest |
*Range depends on the specific STH species, with sensitivity lowest for hookworm and A. lumbricoides in low-intensity settings [11].
FAQ 3: Which programmatic parameters are most critical to manage for achieving interruption of transmission in the endgame phase?
- Problem: In the later stages of control, resources must be targeted efficiently. A sensitivity analysis of an STH transmission model identified the most influential parameters for interrupting transmission.
- Solution: Focus interventions and resources on optimizing the following key parameters, ranked by their influence on model outcomes [12]:
- The combined effect of improved water, sanitation, and hygiene (WASH), represented by parameter (φ).
- The number of treatment rounds (τ) and the drug efficacy (h).
- The proportion of the adult population treated (ga), highlighting the importance of community-wide treatment over child-targeted programs as elimination nears.
- The mortality rate of mature worms in the human host (μ) – a parameter influenced by drug efficacy.
- The strength of density-dependent constraints on worm egg production (γ).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Sensitive Detection of Low-Intensity Parasite Infections
| Item | Function/Application | Technical Notes |
|---|---|---|
| FLOTAC Apparatus | Uses a flotation solution to separate and concentrate helminth eggs from a larger (1g) stool sample, significantly increasing sensitivity. | Ideal for low-intensity settings; requires a centrifuge. The Mini-FLOTAC is a field-adapted variant [11]. |
| Formol-Ether | A concentration method for preserving and concentrating parasites (both helminths and protozoa) from stool samples. | Effective for a broad range of parasites. Formalin preserves specimens, and ether dissolves fats and debris [11] [13]. |
| Kato-Katz Template & Cellophane | Prepares a standardized thick smear for quantitative estimation of STH egg counts. | The global standard for mapping but has known sensitivity limitations in low-transmission settings [11]. |
| Species-Specific Primers/Probes | For PCR-based detection of parasite DNA. Provides high sensitivity and specificity. | Crucial for species confirmation in complex multi-species infections and for detecting low-level infections missed by microscopy [14]. |
| Point-of-Care (POC) Immunoassays | Rapid tests detecting parasite-specific antigens or antibodies in blood or other fluids. | Useful for field surveillance; however, may not distinguish between past and current infection. Development is ongoing for many NTDs [14]. |
Experimental Protocols for Enhanced Detection
Protocol 1: FLOTAC Technique for Sensitive Detection of STH Eggs
Principle: This method uses a flotation solution (e.g., sodium nitrate, specific gravity 1.20-1.35) to isolate and concentrate helminth eggs from a relatively large stool sample, which is then examined microscopically in a specially designed chamber [11].
Workflow:
- Homogenize: Thoroughly homogenize 1g of fresh stool in a Falcon tube filled with 10ml of flotation solution.
- Filter: Pass the suspension through a fine mesh strainer to remove large debris.
- Load: Transfer the filtered suspension into the two chambers of the FLOTAC apparatus.
- Centrifuge: Centrifuge the apparatus according to manufacturer's specifications (typically without brakes).
- Read: After centrifugation, the helminth eggs float to the top and are positioned in the readable zone of the chamber. Rotate the dial of the apparatus to translate the chamber and examine the entire sample under a microscope.
Protocol 2: Formol-Ether Concentration Method
Principle: This method uses formalin to fix and preserve parasites and ether to dissolve fats and remove debris, concentrating the parasites for easier microscopic identification [13].
Workflow:
- Emulsify: Emulsify 1-2g of stool in 10ml of 10% formalin in a centrifuge tube and let stand for 30 minutes.
- Strain: Strain the suspension through a wire mesh or gauze into a second centrifuge tube.
- Centrifuge: Centrifuge the filtered suspension at 500 x g for 2 minutes. Decant the supernatant.
- Resuspend: Resuspend the sediment in 10ml of 10% formalin, add 3ml of ether, and shake vigorously.
- Recentrifuge: Centrifuge again at 500 x g for 2 minutes. This creates four layers: an ether plug, a debris plug, formalin, and the sediment.
- Examine: Free the debris plug by ringing the tube with an applicator stick and decant the top three layers. Examine the final sediment under a microscope.
Diagnostic & Epidemiological Workflow Visualization
Data Analysis & Modeling Support
How can mathematical modeling help us plan for this epidemiological shift?
- Application: Models incorporating global sensitivity analysis (GSA), like the extended Fourier Amplitude Sensitivity Test (eFAST), can identify which programmatic parameters (e.g., WASH coverage, treatment frequency) have the greatest influence on achieving transmission interruption. This allows programs to optimize resource allocation for the endgame [12].
- Troubleshooting Model Outputs:
- Problem: Model predictions are unstable or counter-intuitive.
- Solution: Perform a GSA to understand how uncertainty in input parameters affects your key outcomes (e.g., time to elimination). This will pinpoint which parameters require more precise estimation and which interventions will be most impactful [12].
- Problem: Calibrating agent-based or complex compartmental models with field data is difficult.
- Solution: Use statistical approaches like Gaussian process emulation. This creates a surrogate statistical model of your complex simulation, making parameter estimation and sensitivity analysis computationally feasible [15].
Clinical and Public Health Consequences of Undetected Light Infections
Undetected light or asymptomatic parasitic infections represent a significant and underappreciated challenge to both clinical management and public health control efforts. These infections, often characterized by low parasite burden and the absence of overt clinical symptoms, can lead to severe long-term morbidity, facilitate ongoing transmission, and complicate disease elimination programs. This technical support guide synthesizes current research and methodologies aimed at improving the detection of these elusive infections, providing the scientific community with advanced tools and troubleshooting advice to enhance diagnostic sensitivity and research efficacy.
The Diagnostic Evolution: From Microscopy to Advanced Technologies
The journey in parasitology diagnostics began with the microscopic era in the 17th century, which allowed for the initial visualization of parasites. [16] For centuries, conventional techniques such as microscopy, serological tests (e.g., ELISA), and histopathology formed the diagnostic cornerstone. However, these methods are constrained by significant limitations, including time consumption, requirement for a high level of technical expertise, and most critically, limited sensitivity and specificity, particularly in cases of low-intensity infections. [17] [16]
Table 1: Comparison of Diagnostic Methods for Parasitic Infections
| Parameter | Traditional Microscopy | Serological Tests (e.g., ELISA) | Molecular PCR | Advanced Nanobiosensors |
|---|---|---|---|---|
| Sensitivity | Low to Moderate | Moderate to High | Very High | Extremely High (e.g., femtomolar) |
| Specificity | Moderate (morphological overlap) | High (can have cross-reactivity) | Very High | Extremely High (target-specific) |
| Time-to-Result | Minutes to Hours | Hours (e.g., 4-6 h) | Hours to Days | Minutes to Hours |
| Cost | Very Low | Low to Moderate | High | High (nanomaterial synthesis) |
| Key Limitation | Depends on parasite load & technician skill | Cannot always distinguish past/current infection | Requires special equipment & fresh specimens | Limitations in mass production & standardization |
The following diagram illustrates the evolution and workflow of diagnostic approaches for parasitic infections:
Advanced Molecular and Nanotechnology Diagnostics
Molecular Techniques
Molecular methods have revolutionized parasite detection by offering enhanced sensitivity and specificity. Key technologies include:
- Polymerase Chain Reaction (PCR) and Multiplex PCR: Allows for the amplification of minute amounts of parasite DNA, enabling the detection of low parasite loads. Multiplex assays can simultaneously detect multiple pathogens from a single sample. [17] [16]
- Next-Generation Sequencing (NGS): Provides deep insights into parasite biology, drug resistance mechanisms, and transmission patterns by sequencing entire genomes. [17]
- Loop-Mediated Isothermal Amplification (LAMP): A rapid, field-adjustable technique that amplifies DNA at a constant temperature, making it suitable for resource-limited settings. [17]
Nanobiosensors
Nanobiosensors integrate nanotechnology with biological recognition elements to create powerful diagnostic tools. [18] They function by detecting specific parasitic antigens or genetic material.
Table 2: Nanobiosensor Applications for Key Parasites
| Parasite | Disease | Nanomaterial Used | Target Biomarker |
|---|---|---|---|
| Plasmodium | Malaria | Gold Nanoparticles (AuNPs) | PfHRP2 antigen |
| Leishmania | Leishmaniasis | Quantum Dots (QDs) | kDNA |
| Echinococcus | Cystic Echinococcosis | Carbon Nanotubes (CNTs) | Anti-EgAgB antibodies |
| Schistosoma | Schistosomiasis | Graphene Oxide (GO) | Soluble Egg Antigen (SEA) |
| Taenia | Taeniasis | Metallic Nanoparticles | Parasite-specific antigens |
The basic working principle of a nanobiosensor is visualized below:
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Advanced Parasite Detection Research
| Research Reagent / Material | Primary Function in Experimentation |
|---|---|
| Gold Nanoparticles (AuNPs) | Signal amplification in optical biosensors; used for lateral flow assays (e.g., detecting PfHRP2 in malaria). |
| Quantum Dots (QDs) | Highly fluorescent nanoparticles for labeling and detecting specific DNA sequences (e.g., Leishmania kDNA). |
| Carbon Nanotubes (CNTs) | Platform for electrochemical biosensors; functionalized with antibodies for high-sensitivity antigen detection. |
| CRISPR-Cas Proteins (e.g., Cas12, Cas13) | Programmable enzymes for specific nucleic acid detection; provide high specificity and can be used in field-deployable formats. |
| Polymerase Chain Reaction (PCR) Reagents | Enzymes (polymerases), primers, and probes for amplifying parasite DNA/RNA to detectable levels. |
| Specific Monoclonal Antibodies | Biorecognition elements for capturing and detecting parasite-specific antigens in immunoassays (ELISA, LFIA). |
| Microfluidic Chip Components | Create lab-on-a-chip devices for automating sample processing and analysis at the point-of-care. |
Artificial Intelligence in Diagnosis and Outbreak Prediction
Artificial Intelligence (AI) and Machine Learning (ML) are transforming parasitic disease control.
- AI-Based Diagnostics: Convolutional Neural Networks (CNNs) can be trained on vast datasets of microscopic images (blood smears, stool samples) to identify and classify parasitic stages (eggs, larvae, trophozoites) with high accuracy and speed, reducing reliance on human expertise. [16] [19]
- Predictive Modeling: AI algorithms analyze vast amounts of epidemiological data, environmental factors (temperature, rainfall), and population demographics to forecast disease outbreaks. For example, models have been developed to predict malaria and dengue fever outbreaks with high accuracy, enabling proactive public health interventions. [20] [19]
Troubleshooting Guides & FAQs
FAQ 1: Our molecular assays (PCR) for low-intensity helminth infections consistently yield false negatives despite using published protocols. What are the key areas to investigate?
- Potential Cause: Inhibitors in the sample matrix (e.g., complex carbohydrates in stool, heme in blood) co-purified with nucleic acids.
- Solution:
- Sample Purification: Incorporate a more rigorous DNA cleanup step using inhibitor removal kits or gel purification.
- Sample Dilution: Dilute the extracted DNA template to reduce the concentration of inhibitors in the reaction.
- Internal Control: Always use a process control (e.g., a spiked synthetic DNA) to distinguish between true target negativity and PCR inhibition.
- Inhibition Test: Perform a spike-and-recovery experiment by adding a known amount of target DNA to the sample extract to check for suppression of amplification.
FAQ 2: We are developing a rapid lateral flow test targeting a specific protozoan antigen, but the test line is faint and inconsistent. How can we improve sensitivity?
- Potential Cause: Low affinity of capture antibodies or suboptimal conjugation of detection antibodies to nanoparticles.
- Solution:
- Antibody Screening: Screen different monoclonal/polyclonal antibody pairs to identify a high-affinity, matched pair for capture and detection.
- Conjugation Optimization: Systematically optimize the pH, buffer composition, and blocking agents used during the conjugation of antibodies to gold nanoparticles or other labels.
- Membrane Selection: Test different nitrocellulose membranes with varying pore sizes and flow rates to find the one that provides the optimal balance between sensitivity and flow time.
- Signal Amplification: Investigate the use of enzymatic or fluorescent nanomaterial labels (e.g., Quantum Dots) instead of traditional gold nanoparticles for enhanced signal intensity. [18]
FAQ 3: Our AI model for automated detection of parasite eggs in stool microscopy images performs well on training data but poorly on new field samples. What could be the issue?
- Potential Cause: Overfitting to the training dataset and lack of generalization, often due to insufficient variability in the training images (e.g., same staining method, same microscope).
- Solution:
- Data Augmentation: Expand your training dataset by artificially creating variations (rotation, scaling, changes in brightness, contrast, and blur) to simulate field conditions.
- Diverse Data Collection: Curate a training set from multiple sources, using different microscopes, staining techniques, and operators.
- Transfer Learning: Utilize a pre-trained CNN model (e.g., on ImageNet) and fine-tune it on your specific parasitic dataset, which can improve generalization.
- Continuous Validation: Implement a pipeline for continuously validating the model with new, manually annotated field samples and retraining it periodically. [16] [19]
FAQ 4: What is the public health significance of detecting an asymptomatic, low-intensity infection in an individual?
- Answer: Detecting these infections is critical for several reasons:
- Preventing Long-Term Morbidity: Asymptomatic infections can cause insidious damage, leading to organ impairment (e.g., liver cirrhosis from chronic hepatitis, cardiomyopathy from Chagas disease), nutritional deficiencies, and cognitive deficits in children. [21] [22]
- Interrupting Transmission: Asymptomatic individuals act as silent reservoirs, unknowingly contributing to the transmission cycle. This is a major obstacle for disease elimination campaigns for infections like malaria, typhoid, and soil-transmitted helminths. [21] [22]
- Informing Accurate Burden Estimates: Undetected cases lead to a significant underestimation of true disease prevalence, which in turn affects resource allocation and the planning of public health interventions. [21]
Next-Generation Diagnostic Tools: From Lab-Bench to Field Applications
FAQs and Troubleshooting for the One-Step Formalin-Ether Concentration Technique (FECT)
What is the primary advantage of the One-Step FECT over conventional copromicroscopy?
The One-Step FECT offers superior sensitivity, particularly for detecting low-intensity infections. A 2024 comparative study found that ParaEgg, a formalin-ether concentration tool, detected 24% of positive human helminth cases, outperforming several conventional methods like the Formalin-Ether Concentration Technique (FET) which detected only 18% of cases, and the Harada Mori Technique (HM) which detected only 9% [23]. Its design improves copromicroscopic detection efficiency, making it more reliable for identifying parasites when their numbers in a sample are low [23].
My microscopy results show low egg recovery rates. What could be wrong?
Low egg recovery is often related to the sample preparation or sedimentation steps. To troubleshoot [24] [25] [26]:
- Problem Definition: Are you observing low counts for a single parasite type or across all types? [26]
- Theory of Probable Cause: The most common causes are insufficient washing of the sediment, incomplete sedimentation time, or overly vigorous handling which disturbs the final sediment layer during decanting [23].
- Plan of Action & Verification:
- Ensure Adequate Sedimentation Time: Allow the sample to settle for the full recommended duration without disturbance.
- Refine Decanting Technique: When decanting the supernatant, ensure the tube is stable and poured gently to avoid dislodging the sediment.
- Incorporate a Wash Step: Gently add a small amount of formalin or saline to the sediment, re-suspend, and repeat the sedimentation and decanting process to remove more debris.
- Verify with Seeded Samples: Test your procedure using a sample seeded with a known quantity of Ascaris or Trichuris eggs. The study showed ParaEgg can achieve recovery rates of 81.5% for Trichuris eggs and 89.0% for Ascaris eggs; use this as a benchmark [23].
How does the One-Step FECT compare to the Kato-Katz method?
The One-Step FECT is highly competitive with the Kato-Katz smear, which is often considered a gold standard in field epidemiology. The same 2024 study demonstrated that while Kato-Katz had a slightly higher sensitivity (93.7%), the One-Step FECT (ParaEgg) showed strong performance with a sensitivity of 85.7% and a specificity of 95.5% [23]. The choice between them may depend on your specific needs: Kato-Katz is excellent for quantifying egg burdens, while One-Step FECT is a robust concentration technique effective for detecting mixed infections and in low-intensity settings [23].
I am getting inconsistent results between operators. How can I improve standardization?
Inconsistency typically stems from deviations in the hands-on protocol. To address this [24] [25]:
- Gather Details: Identify at which specific step the results diverge most (e.g., during filtration, decanting, or slide preparation) [26].
- Reproduce the Problem: Have multiple technicians process aliquots of the same sample and document their exact steps [26].
- Develop a Hypothesis: The root cause is likely a non-standardized technique in a manual step.
- Implement a Fix:
- Create a Detailed SOP: Develop a standard operating procedure with precise timings and actions.
- Use Measured Reagents: Provide pre-measured formalin and ether solutions to ensure consistent volumes.
- Implement Training: Use the workflow diagram below for visual guidance and conduct hands-on training sessions to harmonize techniques across the team.
Experimental Protocol: One-Step FECT Workflow
The following diagram illustrates the core steps of the One-Step FECT procedure, which is designed to concentrate parasite eggs and cysts from stool samples for easier microscopic identification.
Detailed Methodology:
- Sample Preparation: Emulsify approximately 1-2 grams of fresh stool in 10-12 mL of 10% formalin in a disposable container. For preserved samples, use the submitted formalin-fixed material directly [27] [23].
- Filtration: Pour the emulsified mixture through a wire or plastic sieve (500-600 µm mesh) into a conical centrifuge tube to remove large debris.
- Solvent Addition: Add 3-4 mL of diethyl ether (or ethyl acetate) to the filtered suspension in the conical tube. Securely cap the tube.
- Mixing: Vigorously shake the tube by hand or vortex mix for 15 seconds. Remove the cap carefully to release pressure.
- Centrifugation: Centrifuge at 500 x g for 2-3 minutes. This will result in four distinct layers: ether, debris plug, formalin, and sediment.
- Ring Loosening: Use an applicator stick to carefully loosen the debris plug between the formalin and ether layers. This is a critical step for high recovery.
- Decanting: Quickly decant the top three layers (ether, plug, and formalin) while retaining the sediment pellet at the bottom.
- Microscopy: Use a pipette to transfer a small amount of the remaining sediment to a glass slide, add a drop of iodine, and apply a coverslip. Systematically examine the entire coverslip area under the microscope (10x and 40x objectives) for parasite eggs, cysts, and larvae [27] [23].
Troubleshooting Common Experimental Issues
When problems occur, a systematic approach is key. The following flowchart outlines a logical troubleshooting pathway for the One-Step FECT.
Performance Data: Comparison of Diagnostic Methods
The table below summarizes quantitative data from a 2024 study comparing the diagnostic performance of ParaEgg (a one-step FECT tool) against traditional methods in human samples [23].
Table 1: Comparative Diagnostic Performance of Copromicroscopic Methods in Human Samples
| Diagnostic Method | Positive Detection Rate (%) | Sensitivity (%) | Specificity (%) | Positive Predictive Value (PPV) (%) | Negative Predictive Value (NPV) (%) |
|---|---|---|---|---|---|
| One-Step FECT (ParaEgg) | 24.0 | 85.7 | 95.5 | 97.1 | 80.1 |
| Kato-Katz Smear (KK) | 26.0 | 93.7 | 95.5 | Not Reported | Not Reported |
| Formalin-Ether Technique (FET) | 18.0 | Not Reported | Not Reported | Not Reported | Not Reported |
| Sodium Nitrate Flotation (SNF) | 19.0 | Not Reported | Not Reported | Not Reported | Not Reported |
| Harada Mori Technique (HM) | 9.0 | Not Reported | Not Reported | Not Reported | Not Reported |
Research Reagent Solutions and Essential Materials
Table 2: Key Reagents and Materials for the One-Step FECT Protocol
| Item | Function in the Protocol |
|---|---|
| 10% Formalin Solution | Preserves parasite morphology and fixes the stool sample. |
| Diethyl Ether (or Ethyl Acetate) | Solvent that cleanses the sample by dissolving fats, trapping debris in a plug, and freeing parasite elements for sedimentation. |
| Conical Centrifuge Tubes | Tubes used for the concentration steps, allowing for the formation of distinct layers and easy decanting. |
| Filtration Sieve (500-600 µm mesh) | Removes large particulate matter and fibrous debris from the stool suspension. |
| Iodine Stain (e.g., Lugol's) | Stains glycogen and nuclei of protozoan cysts, enhancing their visibility under the microscope. |
| Microscope Slides and Coverslips | For preparing the final sediment for microscopic examination. |
Technical Support Center
qPCR Troubleshooting Guide
Q: My qPCR assay for low-parasitemia samples shows high Ct values and inconsistent replicates. What could be wrong?
- A: This is often due to inhibitors co-purified with the parasite nucleic acids or inefficient extraction. Use an inhibitor removal column during DNA extraction and include a sample processing control (SPC) to detect inhibition. Ensure template DNA is homogenously suspended.
Q: How can I improve the limit of detection (LOD) for my parasite qPCR assay?
- A: Implement a digital PCR (dPCR) workflow for absolute quantification, which is less affected by amplification efficiency and can detect single molecules. Alternatively, use a probe-based qPCR assay (e.g., TaqMan) instead of SYBR Green for higher specificity in complex samples.
LAMP Troubleshooting Guide
Q: I am getting false-positive LAMP amplification in my no-template controls (NTCs). How do I resolve this?
- A: Aerosol contamination is a common issue. Physically separate pre- and post-amplification areas, use uracil-DNA glycosylase (UDG) treatment with dUTP in the master mix, and employ dedicated equipment. Ensure all reagents are aliquoted to prevent cross-contamination.
Q: The colorimetric LAMP readout for my field samples is ambiguous. How can I make it more robust?
- A: Supplement the reaction with a quantitative dye like SYBR Green or use a portable fluorometer for objective measurement. For visual readout, include a clear positive and negative control on the same run to aid in color comparison.
CRISPR-Based Assay Troubleshooting Guide
Q: My lateral flow readout for a CRISPR assay shows a faint test line. Is this a positive result?
- A: A faint line is positive, but it indicates low target abundance. To enhance sensitivity, optimize the recombinase polymerase amplification (RPA) step to yield more amplicon and ensure the Cas-gRNA complex is fresh and active. Use a high-sensitivity lateral flow strip.
Q: The CRISPR assay lacks sensitivity compared to my qPCR benchmark. What can I optimize?
- A: Focus on the pre-amplification step. Titrate the RPA primers and increase the amplification time. Also, test different guide RNA (gRNA) sequences targeting various regions of the same amplicon to find the most efficient one.
FAQs
Q: Which technology is best for detecting ultra-low intensity parasite infections in a field setting?
- A: For field deployment, LAMP and CRISPR-based lateral flow assays are superior due to their isothermal nature and visual readouts. CRISPR assays generally offer higher specificity, while LAMP can be slightly faster.
Q: What is the most critical factor for achieving high sensitivity across all these platforms?
- A: Sample preparation is paramount. Efficient lysis of the parasite (e.g., using specialized lysis buffers with proteinase K) and high-yield nucleic acid extraction are critical to ensure the target molecule is present and accessible for amplification.
Quantitative Data Comparison
Table 1: Comparison of Molecular Assay Performance for Low-Intensity Parasite Detection
| Assay Parameter | qPCR/dPCR | LAMP | CRISPR-Based |
|---|---|---|---|
| Theoretical LOD (parasites/µL) | 0.1 - 1 (qPCR); <0.1 (dPCR) | 1 - 10 | 0.1 - 1 |
| Assay Time | 60 - 120 min | 30 - 60 min | 60 - 90 min |
| Equipment Needs | Thermocycler (qPCR); dPCR machine | Heat block/water bath | Heat block (for RPA) |
| Readout Method | Fluorescent (real-time) | Turbidity, Fluorescent, Colorimetric | Fluorescent, Lateral Flow |
| Throughput | High | Medium | Low to Medium |
| Multiplexing Capability | High | Moderate | Low (improving) |
Experimental Protocols
Protocol 1: High-Sensitivity qPCR for Plasmodium falciparum
- DNA Extraction: Use a magnetic bead-based nucleic acid extraction kit with an inhibitor removal step. Elute in 50 µL of elution buffer.
- Primer/Probe Design: Target the 18S rRNA gene. Use a hydrolysis probe (e.g., FAM-labeled).
- qPCR Reaction: Prepare a 20 µL reaction containing 1X TaqMan Master Mix, 900 nM primers, 250 nM probe, and 5 µL of template DNA.
- Cycling Conditions: 95°C for 10 min; 45 cycles of 95°C for 15 sec and 60°C for 1 min (data acquisition).
- Analysis: A sample is positive if it produces an amplification curve that crosses the threshold line within 40 cycles.
Protocol 2: Colorimetric LAMP for Trypanosoma cruzi
- DNA Extraction: As per Protocol 1.
- Primer Design: Design 6 primers (F3, B3, FIP, BIP, LF, LB) targeting a repetitive genomic sequence.
- LAMP Reaction: Prepare a 25 µL reaction containing 1X Isothermal Amplification Buffer, 1.4 mM dNTPs, 6 mM MgSO₄, primer mix (1.6 µM FIP/BIP, 0.2 µM F3/B3, 0.8 µM LF/LB), 8 U Bst 2.0 WarmStart DNA Polymerase, and 5 µL template. Add 1 µL of phenol red (0.1% w/v) as pH indicator.
- Amplification: Incubate at 65°C for 45-60 minutes.
- Analysis: A color change from pink to yellow indicates a positive reaction.
Protocol 3: CRISPR-Cas12a Lateral Flow Assay for Schistosoma mansoni
- DNA Extraction & Pre-amplification: Extract DNA. Perform a 50 µL RPA reaction at 39°C for 20 minutes using specific primers.
- CRISPR Detection: Prepare a 20 µL Cas12a detection mix containing 1X Nuclease Buffer, 50 nM LbCas12a, 60 nM gRNA, and 200 nM ssDNA reporter (FAM-TTATT-BHQ1). Add 5 µL of the RPA product.
- Incubation: Incubate at 37°C for 15 minutes.
- Lateral Flow Readout: Dip a lateral flow strip (anti-FAM at test line) into the reaction tube. Results are visible within 5 minutes. Both control and test lines indicate a positive.
Workflow Diagrams
qPCR Workflow
LAMP Workflow
CRISPR Assay Workflow
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions
| Reagent/Material | Function |
|---|---|
| Inhibitor Removal Columns | Removes PCR/LAMP inhibitors (e.g., heme, humic acids) from complex biological samples, critical for sensitive detection. |
| Bst 2.0 / 3.0 DNA Polymerase | High-displacement isothermal polymerase for LAMP; provides robust amplification at constant temperature. |
| Recombinase Polymerase Amplification (RPA) Kit | Isothermal pre-amplification method used prior to CRISPR detection to amplify target DNA rapidly at low temperatures. |
| LbCas12a Nuclease | CRISPR-associated nuclease; upon binding to target DNA, exhibits collateral cleavage activity, enabling signal amplification. |
| Fluorescent/Lateral Flow Reporters | ssDNA oligonucleotides (e.g., FAM-BHQ1) for fluorescence quencher-based detection or FAM-biotin for lateral flow readout. |
| gRNA Synthesis Kit | For in vitro transcription of guide RNAs that direct Cas enzymes to the specific DNA target sequence. |
Technical Support Center: Frequently Asked Questions (FAQs)
FAQ 1: What are the primary causes of false-negative results in LAMP assays for submicroscopic malaria, and how can they be mitigated?
False negatives in submicroscopic malaria LAMP assays typically stem from suboptimal nucleic acid extraction or reaction inhibition. To address this:
- Inefficient DNA Extraction: Submicroscopic infections possess low parasite biomass. Use of a simple Chelex-100/boiling method with optimized concentrations (e.g., 2.5% whole blood in 10% Chelex-100 resin solution) has been clinically evaluated and provides a cost-effective, efficient DNA extraction suitable for field settings, yielding results comparable to commercial kits [28].
- Reaction Inhibition: Crude sample preparations can inhibit the Bst polymerase. Incorporating an Internal Control (IC) in a multiplex LAMP reaction is crucial. This control validates each test, ensuring that a negative result is due to the absence of target DNA and not reaction failure [28].
FAQ 2: How can I optimize my LAMP reaction conditions to maximize sensitivity for low-density infections?
Optimization is a systematic process. Key parameters to fine-tune based on recent studies are summarized in the table below [29] [30]:
Table 1: Optimization Parameters for LAMP Assay Sensitivity
| Parameter | Typical Range | Recommended Starting Point | Impact on Assay |
|---|---|---|---|
| Temperature | 63°C - 67°C | 65°C | Affects enzyme activity and primer stringency. |
| Time | 30 - 60 minutes | 45 minutes | Longer incubation can increase yield for very low targets. |
| Mg²⁺ | 6 - 12 mM | 8 mM | Essential for polymerase activity; concentration impacts yield and specificity. |
| Bst Polymerase | 6 - 12 U/reaction | 8 U/reaction | Drives amplification; insufficient enzyme reduces sensitivity. |
| Primer Concentration | F3/B3: 0.1-0.4 µM; FIP/BIP: 1.6-3.2 µM | F3/B3: 0.2 µM; FIP/BIP: 1.6 µM | Inner primers (FIP/BIP) are critical; high concentrations can cause primer-dimer formation. |
FAQ 3: My LAMP assay shows non-specific amplification (false positives). What are the likely causes and solutions?
Non-specific amplification is often related to primer design and handling.
- Primer Specificity: Ensure primers are designed against conserved, unique genomic targets using specialized software (e.g., Primer Explorer V5) and validated in silico against databases. Wet-lab validation against a panel of non-target pathogens is essential to confirm exclusivity [31] [29] [30].
- Aerosol Contamination: LAMP produces large amounts of amplicon, making cross-contamination a significant risk. Physically separate pre- and post-amplification workspaces, use aerosol-resistant pipette tips, and employ closed-tube detection methods like colorimetric dyes or microchip detection to prevent amplicon release [32] [28].
FAQ 4: What are the best methods for visualizing LAMP results in a point-of-care setting?
Several equipment-free or simple-equipment methods are available, moving beyond gel electrophoresis.
- Colorimetric Detection: Use pH-sensitive dyes (e.g., phenol red) or metal indicators (e.g., Hydroxynaphthol Blue). A positive reaction causes a visible color change, easily seen with the naked eye [32] [29].
- Turbidity/Micro-precipitate Detection: Monitor turbidity from magnesium pyrophosphate precipitate. The novel LAMP-MicroScanner (LAMP-MS) assay uses a portable microscope to visually detect these precipitates as granules in a microchip, providing a clear positive/negative readout [28].
- Lateral Flow Dipsticks (LFD): Use biotin- and FITC-labeled primers. Amplified products are detected on a dipstick via gold nanoparticle-conjugated anti-FITC antibodies, yielding a simple red test line [32].
Troubleshooting Guide: Common Experimental Issues and Solutions
Table 2: LAMP Assay Troubleshooting Guide
| Problem | Potential Causes | Suggested Solutions |
|---|---|---|
| No Amplification | 1. Inactive enzyme or reagents2. Inhibitors in sample3. Incorrect reaction temperature4. Low template quality/quantity | 1. Run a positive control with a known template. Check reagent aliquots.2. Re-purify DNA or dilute template. Include an Internal Control (IC).3. Calibrate heating block/water bath.4. Optimize and validate DNA extraction protocol [28]. |
| High Background or Non-Specific Bands | 1. Primer-dimer formation2. Excessive primer concentration3. Contaminated reagents | 1. Re-design primers, focusing on 5' end stability (ΔG > -4) [31].2. Titrate primer concentrations, especially inner primers (FIP/BIP) [29].3. Prepare fresh reaction mixes in a clean, UV-irradiated hood. |
| Low Sensitivity/High Limit of Detection | 1. Suboptimal Mg²⁺ or dNTP concentration2. Short reaction time3. Inefficient primers | 1. Systematically optimize Mg²⁺ and dNTP concentrations (e.g., 1.2-1.6 mM dNTPs) [29].2. Increase amplification time to 60 minutes.3. Re-design primers to target multi-copy genes (e.g., rRNA genes) [29]. |
| Inconsistent Replicates | 1. Poor sample mixing2. Inconsistent temperature across the heat block3. Pipetting errors | 1. Centrifuge all tubes briefly before reaction. Mix reagents thoroughly.2. Use a heat block with high thermal uniformity or a water bath.3. Use calibrated pipettes and master mixes to minimize volumetric error. |
Experimental Workflow and Signaling Pathways
The following diagram illustrates the core workflow and molecular mechanism of the LAMP assay for detecting malaria parasites.
Diagram 1: LAMP Assay Workflow for Malaria Detection.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for LAMP-based Malaria Detection
| Item | Function / Role | Examples & Notes |
|---|---|---|
| Bst DNA Polymerase | Engineered DNA polymerase with strand-displacement activity, essential for isothermal amplification. | Bst 2.0 or 3.0 (Warm Start versions recommended); typically 6-12 units per reaction [29]. |
| LAMP Primers | A set of 4-6 primers that recognize 6-8 distinct regions on the target DNA, ensuring high specificity. | Designed against conserved malaria targets (e.g., 18S rRNA, cox1). Must be highly purified [31] [5]. |
| Isothermal Buffer | Provides optimal pH, salt, and co-factor conditions for Bst polymerase activity. | Includes MgSO₄ (often optimized to 6-12 mM), (NH₄)₂SO₄, Tris-HCl, and Tween 20 [29]. |
| dNTPs | Building blocks (deoxynucleotide triphosphates) for synthesizing new DNA strands. | Typically used at 1.0-1.6 mM final concentration in the reaction mix [29]. |
| Detection Reagents | Chemicals that enable visualization of amplification products. | Colorimetric: Phenol red, Hydroxynaphthol Blue (HNB). Fluorescent: SYBR Green, Thiazole Green. Turbidity: Visualized directly or via micro-precipitate in LAMP-MS [32] [29] [28]. |
| Sample Prep Kit | For extracting and purifying parasite DNA from whole blood. | Commercial kits (e.g., QIAamp DNA Blood Mini Kit) or simple, field-friendly methods like Chelex-100/boiling [28]. |
Frequently Asked Questions (FAQs)
Q1: How does AI improve the detection of low-intensity helminth infections compared to manual microscopy?
Manual microscopy, the current gold standard, has low and variable sensitivity, particularly for light-intensity infections [33]. This low sensitivity is due to the inherent limitations of human vision for scanning large areas and the sporadic distribution of eggs in stool samples. AI overcomes this by using deep learning models to automatically and tirelessly analyze entire digitized microscope slides. Studies have validated that AI maintains high sensitivity even in low-intensity infections where manual microscopy fails. For example, in a field study in Kenya, expert-verified AI achieved a sensitivity of 92.2%-100% for various soil-transmitted helminths (STHs), drastically outperforming manual microscopy, which had a sensitivity as low as 31.2% for T. trichiura [34].
Q2: What types of AI models are most effective for helminth egg classification, and how do I choose?
Two main types of deep learning models are employed, each with strengths:
- Classification Models: These models, such as ConvNeXt Tiny, EfficientNet, and ResNet-50, are excellent for assigning a single label to an image (e.g., "Ascaris egg"). They are highly accurate for pre-segmented or single-egg images [35] [36].
- Object Detection Models: Models like the YOLO (You Only Look Once) family are designed to both locate and classify multiple objects within a single, larger image. This is crucial for analyzing real-world microscope fields of view that may contain multiple eggs, debris, and artifacts [36] [37].
The choice depends on your experimental setup. Use object detection for full-slide or large-field analysis and classification models for focused, single-object verification.
Q3: My AI model has high false positives for disintegrated hookworm eggs. How can this be resolved?
This is a recognized challenge. Hookworm eggs are fragile and can partially disintegrate, changing their visual appearance and confusing standard AI models. The solution is to incorporate a dedicated algorithm trained specifically to recognize disintegrated hookworm eggs. One study successfully addressed this by adding a second deep learning algorithm to their workflow that was optimized for these degraded forms. This intervention significantly increased the sensitivity for hookworm detection from around 61-66% to over 92% without compromising specificity in the expert-verified system [34].
Q4: What is the role of image pre-processing in an AI-based diagnostic pipeline?
Image pre-processing is a critical first step to enhance image quality and improve model performance. Key techniques include:
- Denoising: Using algorithms like Block-Matching and 3D Filtering (BM3D) to remove noise (e.g., Gaussian, Speckle) from the digital image [38].
- Contrast Enhancement: Applying methods like Contrast-Limited Adaptive Histogram Equalization (CLAHE) to improve the distinction between parasite eggs and the background [38].
- Segmentation: Using models like U-Net to precisely separate the regions of interest (eggs) from the background, which can then be fed into a classifier [38].
Q5: Can AI models distinguish between different helminth species in mixed infections?
Yes, advanced object detection and classification models are capable of this. Research has demonstrated that models like YOLOv4 can be trained to recognize and classify eggs from multiple species in a single image. For instance, one study achieved high accuracy in identifying up to three different helminth egg types in mixed smears, with accuracy rates for different groups ranging from 75.00% to 98.10% [37]. This capability is vital for accurate diagnosis in endemic areas where polyparasitism is common.
Troubleshooting Guides
| Potential Cause | Solution | Reference |
|---|---|---|
| Insufficient or low-quality training data | Expand your dataset with images from multiple sources, ensuring they are expertly annotated. Apply data augmentation techniques (rotation, scaling, color jitter) to increase variability. | [37] |
| Inappropriate model selection | Benchmark different model architectures (e.g., YOLO for detection, ConvNeXt for classification) on your validation set to select the best-performing one for your specific task. | [35] [36] |
| Suboptimal image quality | Implement a pre-processing pipeline including denoising (e.g., BM3D) and contrast enhancement (e.g., CLAHE) to standardize and improve input images. | [38] |
Issue 2: Model Fails on Specific Parasite Species
| Potential Cause | Solution | Reference |
|---|---|---|
| Class imbalance in training data | Use data sampling strategies (oversampling of rare classes, undersampling of frequent classes) or loss functions (focal loss) that penalize misclassification of minority classes more heavily. | [35] |
| Morphological complexity of certain eggs | For challenging cases like disintegrated hookworm eggs, develop and integrate a dedicated, specialized algorithm trained explicitly on these variants. | [34] |
Issue 3: Low Sensitivity in Light-Intensity Infections
| Potential Cause | Solution | Reference |
|---|---|---|
| Eggs are rare and easily missed by detection algorithms | Use a two-step verification process. First, run an autonomous AI. Second, have an expert human microscopist review all AI-proposed findings (expert-verified AI). This combines AI's speed with human expertise. | [34] |
| Inadequate scanning resolution | Ensure your whole-slide scanner is set to a sufficiently high magnification (e.g., 40x objective) to resolve the fine morphological details of low-contrast eggs. | [34] |
Table 1: Comparative Diagnostic Accuracy of AI vs. Manual Microscopy for Soil-Transmitted Helminths (STHs) in a Field Setting [34]
| Diagnostic Method | A. lumbricoides Sensitivity | T. trichiura Sensitivity | Hookworm Sensitivity | Specificity (All STHs) |
|---|---|---|---|---|
| Manual Microscopy | 50.0% | 31.2% | 77.8% | >97% |
| Autonomous AI | 50.0% | 84.4% | 87.4% | >97% |
| Expert-Verified AI | 100.0% | 93.8% | 92.2% | >97% |
Table 2: Performance of Deep Learning Models for Helminth Egg Classification on Microscope Images [35] [36]
| Deep Learning Model | Task | Accuracy | F1-Score / Key Metric |
|---|---|---|---|
| ConvNeXt Tiny | Classification (Ascaris, Taenia) | N/A | 98.6% (F1-Score) |
| DINOv2-Large | Classification (Multi-species) | 98.93% | 81.13% (F1-Score) |
| YOLOv8-m | Object Detection (Multi-species) | 97.59% | 53.33% (F1-Score) |
| YOLOv4 | Object Detection (Multi-species) | >93% (Mixed Groups) | High mAP (Mean Average Precision) |
Experimental Protocol: Implementing an AI-Based Detection Workflow
This protocol outlines the key steps for deploying a deep learning system to classify helminth eggs from Kato-Katz thick smears, optimized for sensitivity in low-intensity infections.
1. Sample Preparation and Digitization: * Prepare Kato-Katz thick smears from stool samples according to standard WHO protocols [33]. * Use a portable whole-slide scanner to digitize the entire smear at high resolution (e.g., using a 40x objective). This creates a whole-slide image (WSI) for analysis [34].
2. Image Pre-processing: * Denoising: Apply the BM3D algorithm to clean the image of noise that can interfere with analysis [38]. * Contrast Enhancement: Use the CLAHE technique to improve the contrast between the helminth eggs and the background, making features more distinct for the AI model [38]. * Segmentation (Optional but Recommended): Employ a segmentation model like U-Net to identify and isolate potential regions of interest (ROIs). The U-Net model can achieve high pixel-level accuracy (e.g., >96%) in delineating eggs [38].
3. Model Selection and Inference: * For Full-Slide Analysis: Choose an object detection model like YOLOv8-m or YOLOv4. These models will scan the entire whole-slide image and output bounding boxes and class labels for each detected egg [36] [37]. * For ROI Analysis: If using a segmentation model first, feed the extracted ROIs into a high-accuracy classification model like ConvNeXt Tiny or DINOv2-Large for final species confirmation [35] [36].
4. Results Verification and Quality Control: * For the highest sensitivity, especially in a research context, implement an expert-verified AI workflow. In this setup, a human expert reviews all eggs detected by the autonomous AI, confirming species identification and dismissing false positives [34]. * This hybrid approach has been proven to achieve the highest sensitivity while maintaining specificity.
Research Reagent and Material Solutions
Table 3: Essential Research Reagents and Materials for AI-Based Helminth Diagnosis
| Item | Function in the Experimental Pipeline | Key Consideration for Sensitivity |
|---|---|---|
| Kato-Katz Template | Standardizes the amount of stool sampled for the smear, ensuring consistent egg counts per gram (EPG) calculations. | Critical for quantitative assessment of infection intensity, the key parameter in light-infection research. |
| Whole-Slide Scanner | Digitizes the microscope slide, creating a high-resolution whole-slide image (WSI) for AI analysis. | Portability allows for field deployment. High resolution (40x) is essential for identifying low-contrast eggs in light infections. |
| Denoising Algorithm (BM3D) | A computational pre-processing step that removes noise from the digital image. | Improves signal-to-noise ratio, allowing the AI model to focus on relevant egg features and reducing false positives. |
| Contrast Enhancement Algorithm (CLAHE) | A computational pre-processing step that improves image contrast. | Makes subtle morphological features of eggs more pronounced, aiding in the detection of scarce or faint eggs. |
| Deep Learning Models (YOLO, ConvNeXt, DINOv2) | The core AI engines for detecting and classifying helminth eggs. | Model selection is crucial. Object detection (YOLO) scans large areas, while classification models (ConvNeXt) can provide higher accuracy for identified objects. |
Advanced Serological and Multiplex Platforms for Multi-Parasite Surveillance
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: What are the main advantages of using Multiplex Bead Assays over traditional single-pathogen serological tests?
Multiplex Bead Assays (MBAs) simultaneously measure antibodies to multiple antigens from the same or different pathogens in a single sample. This enables integrated serological surveillance, providing economies of scale by maximizing information from a single specimen. Key advantages include the ability to understand co-endemicity, identify populations vulnerable to multiple pathogens, and design integrated control strategies more efficiently than with siloed, single-pathogen tests [39] [40].
FAQ 2: My multiplex assay is producing false negatives. What are the potential causes?
False negatives, a major problem in multiplex panel design, can be caused by several factors [41]:
- Target Secondary Structure: Folded RNA or DNA targets can inhibit primer binding, reducing sensitivity. An energetic cost is required to break this secondary structure before a primer can bind.
- Non-Specific Amplification: Formation of primer-dimers or other false amplicons depletes primers and nucleotides (dNTPs), causing the main reaction to fail.
- Cross-Hybridization: Primers designed for one target may accidentally bind to a different, non-target amplicon (e.g., an Influenza A primer binding to a Zika virus target), preventing proper amplification of the intended target.
- Sequence Variation: Natural genetic variation in the target pathogen population can lead to mismatches with primers or probes, resulting in failed detection [41].
FAQ 3: What are the common challenges in standardizing multiplex serological assays across different laboratories?
A primary challenge is the lack of universally available reference standards and controls. While some pathogen-specific reference reagents exist, they are not calibrated for a broad range of pathogens simultaneously. Furthermore, there are no fully standardized approaches for cleaning raw data or establishing seropositivity thresholds, which can vary by antigen, available controls, and the population being studied [40].
FAQ 4: How can I improve the sensitivity of detection for low-intensity parasite infections?
For low-intensity infections, highly sensitive molecular techniques like multiplex quantitative PCR (qPCR) are recommended. Studies have shown that multiplex qPCR has superior sensitivity compared to traditional microscopy, especially in samples with low parasite burdens and in cases of polyparasitism (mixed infections). This makes it a more appropriate technique for epidemiologic studies and intervention trials in low-transmission settings [42].
Troubleshooting Guide for Common Experimental Issues
Issue 1: Low Sensitivity or False Negatives in Multiplex PCR
| Potential Cause | Troubleshooting Action | Principle |
|---|---|---|
| Target secondary structure [41] | Use predictive software to model DNA/RNA folding and select primer binding sites in accessible regions. | Reduces energetic cost for primer binding, increasing hybridization efficiency. |
| Primer-dimer formation [41] | Optimize primer design to avoid 3'-end complementarity between any primer pair. Adjust Mg²⁺ concentration and thermal cycling conditions. | Prevents depletion of primers and dNTPs by non-specific amplification. |
| Primer-amplicon interactions [41] | In silico check all primers for complementarity to all non-target amplicons in the panel. | Prevents cross-hybridization that can block amplification of the correct target. |
Issue 2: High Background or False Positives in Serological Assays
| Potential Cause | Troubleshooting Action | Principle |
|---|---|---|
| Non-specific antibody binding | Optimize serum sample dilution and include blocking agents (e.g., BSA, non-fat milk) in the assay buffer. | Reduces non-specific interactions between serum components and the assay solid phase. |
| Cross-reactive antigens | Use highly specific, validated recombinant antigens. Pre-adsorb serum samples if necessary. | Minimizes antibody detection against unrelated pathogens due to shared epitopes. |
| Inadequate washing | Ensure stringent and consistent washing steps between incubations. | Removes unbound antibodies and reagents that contribute to background signal. |
Issue 3: Poor Reproducibility Between assay Runs
| Potential Cause | Troubleshooting Action | Principle |
|---|---|---|
| Inconsistent bead coupling | Use quality-controlled, batch-tested coupled beads. Validate each new bead lot before use. | Ensures consistent antigen presentation and binding capacity across experiments. |
| Variable reagent quality | Use calibrated reference reagents and include standard curves and internal controls in every run. | Allows for normalization of data and controls for inter-assay variation [40]. |
| Instrument calibration | Adhere to a strict routine maintenance and calibration schedule for platforms like Luminex. | Guarantees consistent instrument performance and accurate fluorescence detection [40]. |
Detailed Experimental Protocols
Protocol 1: Multiplex Bead Assay (MBA) for Serological Surveillance
This protocol outlines the steps for performing a multiplex bead-based immunoassay to detect IgG antibodies against multiple parasite antigens, adapted from methodologies used in large-scale serosurveys [39].
1. Sample Collection and Preparation:
- Collect venous blood or dried blood spots (DBS). DBS are ideal for field studies in resource-limited settings [39].
- For DBS, elute punches in a suitable buffer (e.g., PBS with 0.1% Tween-20 and 1% BSA) to obtain protein solutions for testing [39].
2. Antigen-Coupled Bead Incubation:
- Combine different antigen-coupled magnetic beads into a master mix. Each bead region is conjugated to a specific parasite antigen (e.g., Plasmodium falciparum AMA1, MSP1₁₉) [39].
- Add the bead mix to a 96-well plate.
- Transfer the prepared serum or DBS eluate into the plate wells.
- Incocate the plate with shaking for a specified duration (e.g., 1-2 hours at room temperature) to allow antibodies in the sample to bind to their target antigens.
- Wash the plate multiple times using a magnetic plate washer to remove unbound antibodies and other sample components.
3. Detection Antibody Incubation:
- Add a biotinylated detection antibody (e.g., biotin-SP-conjugated AffiniPure F(ab')₂ Fragment Goat Anti-Human IgG) to the wells.
- Incubate with shaking to allow the detection antibody to bind to the captured human IgG.
- Perform a series of washes to remove excess, unbound detection antibody.
4. Signal Amplification and Reading:
- Add a streptavidin-conjugated fluorophore (e.g., Streptavidin-R-Phycoerythrin) to the wells.
- Incubate and wash. The streptavidin binds to the biotin on the detection antibody, providing a fluorescent signal proportional to the amount of antibody bound.
- Resuspend the beads in a reading buffer and analyze the plate on a Luminex instrument. The instrument identifies each bead by its internal color code and quantifies the median fluorescence intensity (MFI) for each antigen.
5. Data Analysis:
- Establish seropositivity thresholds using a validated method, which may involve comparing to negative control populations or using mixture models [39].
- Calculate seroprevalence as the proportion of positive individuals for each antigen.
Protocol 2: Multiplex qPCR for Detection of Intestinal Parasites
This protocol is for the simultaneous detection and quantification of multiple intestinal parasites from stool samples, demonstrating higher sensitivity than microscopy [42].
1. DNA Extraction:
- Preserve fecal samples in 5% w/v potassium dichromate or other suitable preservatives for transport [42].
- Centrifuge samples to remove preservative, wash the pellet with PBS, and proceed with DNA extraction using a commercial kit (e.g., Powersoil DNA Isolation Kit with minor protocol modifications for optimal recovery of parasite DNA) [42].
2. Multiplex qPCR Setup:
- Design and validate primer and probe sets for the target parasites (e.g., Ascaris lumbricoides, Necator americanus, Giardia duodenalis).
- Prepare two separate multiplex reactions to efficiently cover a broad pathogen panel without interference [42]:
- Panel 1: Soil-transmitted helminths (e.g., N. americanus, Ancylostoma spp., Ascaris spp., Trichuris trichiura).
- Panel 2: Protozoa and other helminths (e.g., Entamoeba histolytica, Cryptosporidium spp., G. duodenalis, Strongyloides stercoralis).
- Include a positive control (e.g., a plasmid spiked with a known target) and a negative control (no-template) in each run [42].
3. qPCR Amplification:
- Run the plates on a real-time PCR instrument using cycling conditions optimized for the specific chemistry and primers used.
- Monitor fluorescence in each channel corresponding to the different probes.
4. Quantification and Interpretation:
- Use standard curves for each target to convert cycle threshold (Ct) values into quantitative measures (e.g., parasite DNA load) [42].
- Determine positive/negative status based on pre-defined Ct cut-offs.
Workflow and Signaling Pathway Visualizations
Multiplex Serology Assay Workflow
MBA Detection Signaling Pathway
Research Reagent Solutions
Essential materials and reagents for implementing advanced multi-parasite surveillance platforms.
| Item | Function/Benefit |
|---|---|
| Dried Blood Spot (DBS) Cards | Enables simplified collection, transport, and storage of blood samples from remote field sites; stable for multiple pathogens [39]. |
| Antigen-Coupled Magnetic Beads | The core of the MBA; different bead regions are covalently coupled with specific parasite antigens to allow simultaneous antibody detection [39] [40]. |
| Biotinylated Anti-Human IgG | A polyclonal detection antibody that binds to human IgG captured on the beads; the biotin tag allows for subsequent signal amplification [39]. |
| Streptavidin-R-Phycoerythrin | The fluorescent reporter molecule; binds with high affinity to biotin, providing a strong, quantifiable signal for detection on a Luminex instrument [39]. |
| Luminex Instrumentation | The analysis platform; identifies beads by their internal color and quantifies the fluorescence intensity (MFI) for each antigen-antibody reaction [40]. |
| Validated Antigen Panel | A pre-selected and validated set of recombinant parasite antigens known to elicit strong and specific antibody responses in infected individuals [39] [40]. |
Navigating Practical Hurdles: Strategies for Optimizing Diagnostic Sensitivity and Specificity
Foundational Concepts & FAQs
FAQ 1: Why is optimizing for sensitivity particularly important in low-intensity parasite infection research? In low-intensity infections, parasite densities often fall below the detection threshold of conventional diagnostic methods like microscopy and rapid diagnostic tests (RDTs) [43]. These submicroscopic and asymptomatic infections are now recognized as significant reservoirs for ongoing disease transmission [44]. Optimizing case definitions and diagnostic sensitivity is therefore critical for accurate surveillance and effective elimination strategies, as missing these infections can undermine control efforts [43] [44].
FAQ 2: How do I balance high sensitivity with the risk of false positives? Optimizing for sensitivity often comes at the cost of reduced specificity, which can lead to false positives [45]. The balance is quantified by Positive Predictive Value (PPV) and Negative Predictive Value (NPV). In low-prevalence settings, even tests with excellent sensitivity can have low PPV, meaning a positive result has a high chance of being false [45]. The decision to prioritize sensitivity should be normative, considering the consequences of missing an infection versus the costs of investigating false alarms [45] [46].
FAQ 3: What is a "sensitivity-optimized case definition"? A sensitivity-optimized case definition does not rely solely on a single diagnostic test. Instead, it defines a case as an individual who tests positive OR displays specific, pre-identified clinical symptoms or other biomarkers associated with the infection [45]. This approach increases the overall probability of detecting a true positive.
FAQ 4: My molecular assay is showing inhibition. What could be wrong? Inhibition in molecular assays like LAMP or PCR can often be traced to the sample preparation process. For viscous or protein-rich samples like blood, ensure your nucleic acid extraction protocol includes a heat-activated enzymatic lysis step (e.g., with proteinase K) and sufficient wash steps to reduce carry-over of inhibitors [44]. Vortex mixing, rather than manual shaking, is also recommended for better homogenization during extraction [44].
Diagnostic Performance & Method Comparison
The table below summarizes the performance characteristics of various diagnostic methods for parasitic infections, highlighting the limitations of conventional tools and the advancements offered by new technologies.
Table 1: Comparison of Diagnostic Methods for Parasitic Infections
| Diagnostic Method | Approximate Limit of Detection | Key Advantages | Key Limitations |
|---|---|---|---|
| Light Microscopy | 50-100 parasites/μL [44] | Low cost, widely available. | Low sensitivity for submicroscopic infections; subjective, requires expertise [43] [44]. |
| Rapid Diagnostic Tests (RDTs) | 100-200 parasites/μL [44] | Fast, easy to use, low cost. | Limited sensitivity; PfHRP2/3 gene deletions affect reliability [44]. |
| PCR / qPCR | As low as 0.002 parasites/μL [44] | Very high sensitivity and specificity; gold standard. | Requires advanced lab infrastructure, skilled technicians, and is time-consuming [44]. |
| LAMP-based Assays | ~0.6 parasites/μL [44] | High sensitivity; isothermal amplification; simpler equipment than PCR. | Sample prep can still be complex; some platforms have limited throughput [44]. |
| Nanobiosensors [47] | Varies by target/design (detects low conc. biomarkers) | Rapid, high sensitivity, potential for point-of-care use. | Mostly in research phase; challenges with mass production and standardization [47]. |
Table 2: Performance of a Near-POC LAMP Assay vs. Traditional Methods in Field Studies
| Diagnostic Method | Sensitivity for All Infections | Sensitivity for Asymptomatic Infections | Sensitivity for Submicroscopic Cases |
|---|---|---|---|
| Near-POC LAMP Platform [44] | 95.2% (90.4–98.1) | 94.9% (130/137) | 95.3% (41/43) |
| Expert Microscopy [44] | 70.1% | Not specified | 0% |
| Rapid Diagnostic Test (RDT) [44] | 49.6% | Not specified | 4.7% |
Experimental Protocols & Workflows
Protocol 1: Workflow for a Near Point-of-Care LAMP Test using Capillary Blood
This protocol is adapted from a recently published study for detecting Plasmodium falciparum [44].
1. Sample Collection:
- Collect 100 μL of EDTA-anticoagulated capillary blood via finger prick.
2. Nucleic Acid Extraction (SmartLid-based method):
- Lysis: Add a heat-activated enzymatic (proteinase K) lysis step to the blood sample. Incubate at 65°C for 5 minutes to break down the protein-rich matrix.
- Binding: Add silica-coated superparamagnetic beads to bind nucleic acids.
- Washing: Use a disposable lid with a removable magnetic key to transfer the beads through multiple wash buffers. Vortex mixing is used for adequate agitation. An additional wash step is included to reduce contaminants.
- Elution: Elute the purified DNA in a final buffer. The entire extraction process for 12 samples takes under 15 minutes.
3. Isothermal Amplification (Colorimetric LAMP):
- Use lyophilized, colorimetric LAMP reagents rehydrated with the eluted DNA.
- Amplify both pan-Plasmodium and P. falciparum-specific targets in a single reaction well.
- Incubate in a low-cost, portable dry-bath heat block at a constant temperature (e.g., 65°C) for 25-40 minutes.
4. Result Interpretation:
- Read results visually by observing a distinct color change from pink (negative) to yellow (positive).
- The total sample-to-result time is under 45 minutes.
Protocol 2: Framework for Creating a Sensitivity-Optimized Case Definition
This methodological framework is based on modelling for preventive strategies [45].
1. Define Components:
- Diagnostic Component: Select a diagnostic test (e.g., RDT, LAMP) and note its standalone sensitivity (SeD) and specificity (SpD).
- Symptom/Syndrome Component: Identify a set of
nobservable clinical symptoms (e.g., from seroconversion syndrome) that are associated with the target infection.
2. Calculate Composite Metrics: The overall sensitivity and specificity of the new case definition are calculated as follows:
- Overall Sensitivity:
Se_Overall = 1 - (1 - Se_D) * (1 - Se_Symptoms)Se_Symptomsis the probability that an infected individual displays at leastkout of thensymptoms.
- Overall Specificity:
Sp_Overall = Sp_D * Sp_SymptomsSp_Symptomsis the probability that a non-infected individual displays fewer thankof thensymptoms.
3. Evaluate Predictive Performance:
- Calculate the Positive Predictive Value (PPV) and Negative Predictive Value (NPV) using the overall sensitivity and specificity, and an estimate of the population prevalence.
- PPV = (SeOverall × Prevalence) / [ (SeOverall × Prevalence) + (1 - Sp_Overall) × (1 - Prevalence) ]
- NPV = (SpOverall × (1 - Prevalence)) / [ (SpOverall × (1 - Prevalence)) + (1 - Se_Overall) × Prevalence) ]
4. Validate and Refine:
- Test the proposed case definition against a reference standard (e.g., qPCR) in the target population.
- Adjust the number of required symptoms (
k) or the specific symptoms included to find an acceptable balance between SeOverall and SpOverall for the intended public health or research purpose.
Visual Workflows & Pathways
Diagnostic Selection Logic
LAMP Assay Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Advanced Parasite Diagnostics
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Lyophilized Colorimetric LAMP Mix [44] | Isothermal amplification of parasite DNA/RNA. Contains pH-sensitive dyes for visual detection. | Enables cold-chain-free storage and instrument-free result readout. Ideal for field deployment. |
| Silica-coated Magnetic Beads [44] | Solid-phase nucleic acid extraction and purification from complex samples like whole blood. | Allows for rapid, centrifugation-free extraction protocols. Compatibility with automated magnetic handlers. |
| Proteinase K [44] | Enzymatic lysis of blood cells and degradation of nucleases in sample preparation. | A heat-activated step (65°C) significantly improves nucleic acid yield from blood. |
| Functionalized Nanomaterials (e.g., Gold Nanoparticles, Quantum Dots) [47] | Signal amplification in nanobiosensors. Used for optical or electrochemical detection of parasite antigens or genetic material. | High sensitivity and potential for multiplexing. Challenges include batch-to-batch consistency and biological matrix interference. |
| Genus- and Species-Specific Primers/Probes (e.g., for P. vivax cox1, P. falciparum mitochondrial genome) [43] [44] | Target-specific amplification and detection in molecular assays (PCR, qPCR, LAMP). | Critical for assay specificity. Must be designed against conserved and unique genomic regions. |
| Superparamagnetic Nanoparticles [47] | Used in magnetic nanobiosensors to isolate and concentrate target biomarkers from bulk sample. | Effective for analyzing complex specimens like blood, improving sensitivity by enriching low-abundance targets. |
Frequently Asked Questions (FAQs): Diagnostic Sensitivity
Q1: Why is diagnostic sensitivity a major challenge in low-resource settings, particularly for parasite infections?
In low-resource settings, health systems face a combination of financial pressures, human resource limitations, and underdeveloped infrastructure [48]. For parasite diagnostics, this is critical because as disease transmission decreases, infections often become lower in intensity and frequently asymptomatic. Microscopy, a common diagnostic tool, has been shown to become significantly less sensitive in these low-intensity settings, resulting in a high number of missed infections [5]. This occurs even though the underlying parasite density, as estimated by more sensitive molecular methods, may remain similar [5].
Q2: What does "low-resource setting" truly encompass beyond financial constraints?
The term "low-resource setting" (LRS) is multi-dimensional. A systematic scoping review identified nine major themes that characterize LRSs [48]:
- Financial pressure
- Suboptimal healthcare service delivery
- Underdeveloped infrastructure
- Paucity of knowledge
- Research challenges and considerations
- Restricted social resources
- Geographical and environmental factors
- Human resource limitations
- The influence of beliefs and practices This complexity means that LRSs are not homogenous and can even exist within high-income countries, requiring tailored strategies rather than one-size-fits-all solutions [48].
Q3: How can implementation science help overcome resource constraints in diagnostics?
Implementation science provides a framework to develop and execute strategies that generate or maximize limited resources. Instead of viewing resources only as a fixed context, it treats them as a primary research object. Key approaches include [49]:
- Creating Resources: Using tele-education to advance health workers' skills, task-shifting to alleviate strain on highly-skilled workers, and increasing laboratory capacity with new technologies.
- Changing Behavior: Implementing competency-based training, audits, and feedback to promote more efficient delivery of evidence-based practices.
- Fostering Creativity/Reverse Innovation: Resource constraints can drive innovation, such as developing new models of care or supply chain innovations that can later be transferred to resource-rich settings.
Q4: What are the relative sensitivities of common diagnostic tests for soil-transmitted helminths (STH)?
A Bayesian latent class meta-analysis evaluated the sensitivity of common copro-microscopic diagnostic methods. The table below summarizes the findings, showing that test performance is strongly influenced by the intensity of infection [11].
Table 1: Sensitivity of Diagnostic Tests for Soil-Transmitted Helminths
| Diagnostic Method | Overall Sensitivity | Sensitivity in High-Intensity Settings | Sensitivity in Low-Intensity Settings |
|---|---|---|---|
| FLOTAC | 92.7% | Highest | Highest |
| Kato-Katz (double slide) | 74–95%* | 74–95% (varies by species) | 53–80% (lowest for hookworm) |
| Mini-FLOTAC | Comparable to Kato-Katz | Comparable to Kato-Katz | Comparable to Kato-Katz |
| Direct Microscopy | 42.8% | Low | Low |
Kato-Katz sensitivity range is for the three STH species (Ascaris lumbricoides, *Trichuris trichiura, and hookworms) [11].
Experimental Protocols for Improved Sensitivity
Protocol: Molecular Diagnosis of Low-IntensityPlasmodiumInfections
This protocol is adapted from a study investigating urban malaria in Brazil and is designed for sensitivity in low-parasite-density scenarios [5].
1. Sample Collection:
- Collect finger-prick capillary blood from participants, regardless of symptoms.
- Prepare thick blood smears for microscopy. Stain with Giemsa and examine under 1000x magnification, reviewing a minimum of 200 fields.
- Spot blood onto filter paper or collect in an appropriate buffer for molecular analysis.
2. DNA Extraction:
- Perform DNA extraction from blood samples using a standardized kit or protocol suitable for the sample type (filter paper or liquid blood).
3. Genus-Specific PCR Screening:
- Initially screen all samples with a genus-specific PCR targeting a conserved sequence (e.g., the cytb gene of human-infecting Plasmodium).
- Use a detection threshold of 0.2 amplicon copies/µL, which is equivalent to as few as 4 parasites/mL.
4. Species-Specific qPCR Confirmation and Quantification:
- Test PCR-positive samples with separate, species-specific quantitative TaqMan assays.
- Targets:
- P. vivax: An 84-bp domain of the cox1 gene.
- P. falciparum: A 90-bp domain spanning the 3' end of the cox1 gene and the nearby intergenic region.
- These assays amplify DNA from peripheral blood parasites and from sequestered parasites, providing an estimate of the total parasite burden.
Protocol: Parasite Genotyping Using Microsatellite Markers
This protocol details the steps for genetic characterization to understand transmission dynamics [5].
1. Marker Selection:
- For Plasmodium vivax, type 6 microsatellite loci: MS2, MS5, MS6, MS7, MS9, and MS15.
- For Plasmodium falciparum, type 6 microsatellite loci: polyα, TAA81, TAA42, TA87, TA109, and TA60.
2. Genotyping and Haplotype Definition:
- Amplify loci using appropriate primers and conditions.
- Define haplotypes as unique combinations of alleles at each locus. When more than two alleles are detected in a single sample (indicative of multiple strains), consider only the most abundant allele for analysis.
3. Data Analysis:
- Genetic Diversity: Calculate the expected heterozygosity.
- Linkage Disequilibrium: Calculate the standardized index of association using software like LIAN 3.7 to measure multilocus linkage disequilibrium.
- Genetic Relatedness: Use the goeBURST algorithm (e.g., in PHYLOViZ software) to identify clusters of genetically related haplotypes, which can inform about parasite migration patterns.
Workflow Visualization
Low-Parasite-Density Diagnostic & Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Sensitive Parasite Detection and Analysis
| Reagent / Material | Function / Application | Key Considerations for LRS |
|---|---|---|
| Giemsa Stain | Staining thick and thin blood smears for microscopic identification and quantification of parasites. | Standard method, but sensitivity drops sharply with low parasite density and requires expert microscopists [5]. |
| DNA Extraction Kits | Isolating pathogen DNA from blood (fresh or on filter paper) for downstream molecular assays. | Select kits that are effective with dried blood spots and do not require constant refrigeration (cold chain independence). |
| Genus-Specific PCR Master Mix | Initial highly sensitive screening for the presence of any Plasmodium species DNA. | Enables detection of submicroscopic infections. Reagents should be stable with limited freezer availability [5]. |
| Species-Specific qPCR Assays | Confirming the parasite species and providing quantitative data on parasite load. | TaqMan probes offer high specificity. Consider cost; nested PCR is an alternative but increases contamination risk. |
| Microsatellite Panel Primers | Amplifying highly variable genetic regions for genotyping parasites and tracking transmission. | Essential for understanding transmission dynamics and distinguishing between relapse and new infection [5]. |
| Rapid Diagnostic Tests (RDTs) | Point-of-care immunochromatographic tests for detecting parasite antigens. | Useful in remote clinics, but sensitivity for low-density infections is a known limitation [5]. |
Accurate detection of low-intensity parasitic infections, such as soil-transmitted helminths (STH), represents a significant challenge in global health research. As mass drug administration programs reduce infection prevalence and intensity, diagnostic methods must evolve to maintain detection sensitivity. Traditional microscopy techniques like Kato-Katz thick smear demonstrate limited sensitivity in low-intensity settings, potentially missing true infections and compromising surveillance data [50]. Quantitative polymerase chain reaction (qPCR) has emerged as a vital tool with enhanced sensitivity, detecting up to 4-fold more hookworm infections compared to conventional methods [50]. However, this increased sensitivity introduces new challenges in standardization and harmonization across laboratories and studies.
The reproducibility of qPCR results depends critically on standardized practices across all experimental phases. Recent research highlights that even the choice of standard material can significantly impact quantification, with different commercial standards yielding variations in detected SARS-CoV-2 RNA levels in wastewater surveillance [51]. Such variability poses particular challenges for STH research in elimination settings, where accurately distinguishing positive from negative samples at very low infection intensities directly impacts treatment decisions and resource allocation [52]. This technical support center provides actionable guidance to address these challenges, with specific focus on applications in low-intensity parasite infection research.
Core Principles of qPCR Standardization
Understanding the MIQE Guidelines
The Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines provide an essential framework for ensuring reproducibility and credibility in qPCR experiments [53]. These guidelines establish standardized reporting requirements for all aspects of qPCR experiments, from sample preparation to data analysis. Compliance with MIQE guidelines enables independent verification of experimental results and facilitates meaningful comparisons across studies—a critical requirement for multi-center clinical trials and surveillance networks.
For parasite diagnostics, key MIQE considerations include comprehensive documentation of sample collection and storage conditions, nucleic acid extraction methods, primer and probe sequences (or commercial assay identifiers), and detailed validation data including limits of detection and quantification [53] [54]. When using predesigned assays such as TaqMan assays, providing the unique Assay ID typically satisfies sequence disclosure requirements, as these identifiers correspond to fixed, unchanging primer and probe sequences [53].
Selection and Harmonization of Standard Materials
The critical importance of standard material selection cannot be overstated, as different standards directly impact quantification results. A recent study comparing three common standards for SARS-CoV-2 detection found statistically significant differences in measured RNA levels depending on the standard used [51]. The CODEX standard yielded more stable results compared to IDT and EURM019 standards, with observed differences of approximately 0.3-0.5 Log10 GC/100 mL between standards [51]. These findings have direct relevance to parasite diagnostics, where accurate quantification in low-intensity settings is essential for monitoring intervention effectiveness.
Table 1: Impact of Standard Material Selection on Quantification Results
| Comparison | Difference in Quantification | Correlation Strength | Performance Characteristics |
|---|---|---|---|
| IDT vs. CODEX | IDT: 4.36 Log10 GC/100 mL vs. CODEX: 4.05 Log10 GC/100 mL | Spearman's rho median: 0.79 | CODEX standard yielded more stable results |
| IDT vs. EURM019 | IDT: 5.27 Log10 GC/100 mL vs. EURM019: 4.81 Log10 GC/100 mL | Spearman's rho median: 0.59 | Significant variability between standards |
To promote harmonization:
- Use the same lot of standards throughout a study when possible
- Follow manufacturer recommendations for storage and handling
- Prepare fresh dilution series for each experiment to prevent evaporation-related concentration changes [55]
- Include standard curves in every run to monitor reaction efficiency [51]
Experimental Design for Reproducibility
Robust experimental design incorporates multiple controls to identify potential contamination and efficiency issues:
- No Template Controls (NTC): Contain all reaction components except nucleic acid template to detect reagent contamination [56]
- No Amplification Controls (NAC): Omit reverse transcriptase in RT-qPCR to detect genomic DNA contamination [56]
- Positive Controls: Verify reaction efficiency and primer functionality
- Internal Controls: Monitor sample-specific inhibition and nucleic acid recovery [51]
For STH research specifically, the inclusion of an internal control throughout DNA extraction and amplification processes is essential to account for sample-specific inhibitors common in stool matrices [50] [57].
Troubleshooting Guide: Common qPCR Issues and Solutions
Amplification Curve Abnormalities
Understanding amplification curve morphology is essential for identifying potential issues early in the experimental process. A standard qPCR amplification curve should display three distinct phases: baseline, exponential growth, and plateau [58].
Table 2: Troubleshooting Abnormal Amplification Patterns
| Observation | Potential Causes | Corrective Actions |
|---|---|---|
| Exponential amplification in NTC | Contamination from laboratory exposure or reagents | Clean work area with 10% bleach; prepare fresh reagents; use separate pre- and post-PCR areas [58] [56] |
| Unusually shaped amplification; irreproducible data | Poor PCR efficiency; primer Tm mismatch >5°C; sample inhibitors; annealing temperature too low | Optimize primer concentrations and annealing temperature; redesign primers; test for inhibitors using dilution series [58] |
| Ct values much earlier than anticipated | Genomic DNA contamination (RNA work); multiple products; high primer-dimer; poor specificity | DNase-treat RNA samples before reverse transcription; redesign primers for specificity; optimize primer concentration [58] [56] |
| Jagged signal throughout amplification | Poor amplification; weak probe signal; mechanical error; buffer instability | Ensure sufficient probe concentration; mix solutions thoroughly; contact equipment technician [58] |
| Plateau much lower than expected | Limiting reagents; degraded dNTPs or master mix; inefficient reaction; incorrect probe concentration | Check master mix calculations; repeat with fresh stock solutions; compare endpoint fluorescence [58] |
Reaction Efficiency and Standard Curve Problems
Maintaining optimal reaction efficiency (90-110%) is fundamental to accurate quantification [56]. Efficiency deviations directly impact quantification accuracy, particularly critical in low-intensity infections where small differences substantially impact prevalence estimates.
Table 3: Standard Curve and Efficiency Troubleshooting
| Observation | Potential Causes | Corrective Actions |
|---|---|---|
| Slope of standard curve outside -3.6 to -3.1 (Efficiency outside 90-110%) | PCR inhibitors; inaccurate dilutions; standard curve exceeds linear range; pipetting error | Dilute template to reduce inhibitors; prepare fresh standard dilutions; eliminate extreme concentrations; improve pipetting technique [58] [56] |
| R² value < 0.98 | Pipetting error; standard curve not prepared fresh; data variability at concentration extremes | Prepare fresh standard curves; use calibrated pipettes; consider using carrier molecules in dilution buffer [55] [58] |
| High variation between technical replicates (Cq difference > 0.5 cycles) | Pipetting error; insufficient mixing; low expression causing stochastic amplification; high Cq values | Calibrate pipettes; mix all solutions thoroughly; optimize reaction conditions; increase template input [58] |
| Overlap of low concentration standards | Limited linear range; template contamination; primer-dimer formation | Remove contamination; optimize assay conditions; redesign primers to avoid dimers [58] |
Sample-Specific Issues in Parasite Research
The complex matrix of human stool presents unique challenges for STH detection by qPCR. Inhibitors such as complex carbohydrates, bilirubin, and bile salts can significantly reduce amplification efficiency [50] [57]. Including an internal control throughout extraction and amplification processes is essential to identify inhibition issues [50]. If inhibition is detected, sample dilution or additional purification steps may be necessary.
RNA degradation during storage or extraction represents another common challenge, particularly in field settings with limited refrigeration. Prior to reverse transcription, verify RNA concentration and quality using spectrophotometry (ideal 260/280 ratio of 1.9-2.0) or agarose gel electrophoresis [55] [56]. For DNA targets, ensure proper storage at -20°C to -80°C and minimize freeze-thaw cycles.
Frequently Asked Questions (FAQs)
Q1: How can we improve comparability of qPCR results across different laboratories working on STH detection? A: Implement harmonized protocols using standardized DNA extraction methods, common reference materials, and validated primer/probe sets [52] [57]. Participation in external quality assessment schemes allows laboratories to evaluate performance relative to peers. The establishment of STH biorepositories from different geographical locations would provide essential reference materials for validating new diagnostics and ensuring uniform performance [52].
Q2: What steps can minimize cross-contamination in high-throughput qPCR workflows? A: Implement strict spatial separation of pre- and post-PCR activities, use dedicated equipment and supplies for each area, regularly decontaminate surfaces with DNA degradation solutions, and include adequate negative controls throughout the process [56]. Automated liquid handling systems with closed designs can significantly reduce contamination risk while improving pipetting precision [59].
Q3: How can we determine whether presence/absence qPCR results in low-intensity settings represent true infections? A: In low-prevalence settings, 'presence/absence' should be carefully evaluated to confirm that presence equals infection [52]. This requires establishing clinically relevant threshold values and correlating qPCR results with complementary diagnostic methods when possible. Replicate testing and consideration of the biological and clinical context are essential for appropriate interpretation.
Q4: What normalization strategies are most appropriate for parasite burden quantification? A: For absolute quantification, include external standard curves with known copy numbers in each run [54]. For relative quantification in gene expression studies, use invariant endogenous controls with stable expression across samples [56]. The inclusion of an internal process control (e.g., mengovirus) added to samples before nucleic acid extraction can monitor extraction efficiency and inhibition [51].
Q5: How can we balance the need for high sensitivity with practical constraints in resource-limited settings? A: Implement pooling strategies where samples are combined before testing, significantly reducing costs while maintaining population-level surveillance capability [52]. Optimize DNA extraction protocols for cost-effectiveness without compromising sensitivity. Explore the development of point-of-care molecular platforms that maintain sensitivity while reducing infrastructure requirements.
Standardized Experimental Protocols
High-Throughput STH Detection Platform
The DeWorm3 project exemplifies a rigorously validated approach to high-throughput STH detection [57]. This multiplexed qPCR platform enables simultaneous detection of four STH species with accuracy measuring at or above 99.5% and 98.1% for each target species at the level of technical replicate and individual extraction, respectively [57].
Protocol Steps:
- Sample Collection and Storage: Collect stool samples without preservative and transport in cooled containers. Store at -20°C to -80°C until processing [50] [57].
- DNA Extraction: Use MP Bio Fast DNA Spin kit for Soil with bead-beating to break open helminth eggs. Include an internal control to validate extraction consistency [50] [57].
- qPCR Reaction Setup: Prepare 7μL reactions containing 2μL DNA, 3.5μL TaqPath ProAmp Master Mix, and 1.5μL species-specific primers, probes, and nuclease-free water [57].
- Amplification Conditions: Initial activation at 95°C for 10 minutes, followed by 40 cycles of denaturation (95°C for 15 seconds) and annealing/extension (60°C for 30-60 seconds) [57].
- Data Analysis: Calculate DNA copy number from standard curves using linear regression of positive standard controls included on each plate [50].
Validation Procedures for Diagnostic Assays
Comprehensive validation is essential before implementing qPCR assays in research or clinical settings. Key validation parameters include:
- Specificity: Ensure no cross-reactivity with genetically similar species or host DNA
- Sensitivity (Limit of Detection): Determine the minimum number of copies reliably detected in ≥95% of replicates
- Linearity and Dynamic Range: Establish the range of concentrations where quantification remains accurate
- Precision: Evaluate intra-assay and inter-assay variability using multiple replicates across different runs
- Accuracy: Compare results with established reference methods when available [54] [57]
For regulatory compliance in gene therapy applications, additional validation criteria may include stability studies, robustness testing, and reproducibility across operators and equipment [54].
Research Reagent Solutions
Table 4: Essential Reagents for Standardized qPCR in Parasite Diagnostics
| Reagent Category | Specific Examples | Function and Importance |
|---|---|---|
| Standard Materials | CODEX #SC2-RNAC-1100; IDT #10006625; EURM019 | Quantification reference; critical for comparability across studies [51] |
| Nucleic Acid Extraction Kits | MP Bio Fast DNA Spin kit for Soil; Chemagic Viral DNA/RNA kit | Efficient lysis of parasite eggs; inhibitor removal; consistent yield [51] [50] |
| Master Mixes | TaqPath ProAmp Master Mix; TaqMan Fast Virus 1-step Master Mix | Enzyme stability; buffer optimization; reduced inter-well variability [51] [57] |
| Internal Controls | Mengovirus (ATCC VR-1597); synthetic DNA/RNA sequences | Process monitoring; inhibition detection; extraction efficiency [51] |
| Primer/Probe Sets | Species-specific TaqMan assays; validated custom designs | Target detection; assay specificity; multiplexing capability [50] [57] |
Addressing Sample Processing, Preservation, and Workflow Efficiency
FAQs and Troubleshooting Guides
Sample Preservation and Processing
What is the most pragmatic preservative for stool samples intended for PCR-based detection of parasites in field conditions? For field conditions where a cold chain is unreliable, 95% ethanol provides a highly effective and pragmatic preservative for stool samples. It protects target DNA from degradation by nucleases, especially at elevated temperatures. At 32°C, simulating tropical ambient temperatures, 95% ethanol, along with preservatives like FTA cards and potassium dichromate, has been proven to minimize the increase in quantitative PCR (qPCR) cycle threshold (Cq) values, indicating successful DNA preservation over 60 days. When balancing DNA preservation with factors like cost, toxicity, and shipping requirements, 95% ethanol is often the most balanced choice [60].
Why might DNA yield be low when extracting from tissue samples? Low DNA yield from tissue samples can result from several factors [61]:
- Improper handling of cell pellets: Thawing frozen cell pellets too abruptly or resuspending them harshly can compromise cell integrity.
- Incomplete tissue digestion: Large tissue pieces prevent efficient lysis. Tissues should be cut into the smallest possible pieces or ground with liquid nitrogen.
- Nuclease activity: Tissues rich in nucleases (e.g., pancreas, liver, intestine) can degrade DNA if not stored properly at -80°C or kept on ice during processing.
- Column overloading: DNA-rich tissues like spleen or liver can clog the silica membrane of extraction columns if the recommended input amount is exceeded.
- Incorrect lysis protocol: Adding Cell Lysis Buffer concurrently with Proteinase K can create a viscous lysate that impedes proper enzyme mixing.
How can protein contamination be minimized during DNA extraction from fibrous tissues? Protein contamination often arises from incomplete digestion or the presence of indigestible fibers in tissues like muscle, heart, skin, and ear clips [61]. To minimize this:
- Ensure tissues are cut into very small pieces.
- Extend the lysis time by 30 minutes to 3 hours after the tissue appears dissolved.
- For fibrous tissues, centrifuge the lysate at maximum speed for 3 minutes to pellet the fibers before transferring the supernatant to the binding column.
- Do not exceed recommended input amounts (e.g., 12–15 mg for ear clips and brain tissue).
Diagnostic Sensitivity and Workflow
What diagnostic approach is recommended for detecting low-intensity parasite infections? For low-intensity infections, a multi-technique approach is advised as no single method is 100% effective [62]. This includes:
- Using concentration techniques: Methods like flotation or sedimentation increase sensitivity by removing fecal debris and concentrating parasitic structures [62].
- Combining diagnostic tests: Using two or more sensitive techniques together provides a more reliable "gold standard" result than relying on a single test [62].
- Adopting new technologies: Lab-on-a-chip (LoD) technologies, such as the SIMPAQ device, show high potential for detecting low-intensity infections by concentrating eggs through centrifugation and flotation, allowing for single-image quantification [63].
How can workflow efficiency be optimized in a diagnostic laboratory? Optimizing lab workflow involves a strategic combination of process improvement and technology [64] [65]:
- Centralize data management: Use a centralized system, like a Laboratory Information Management System (LIMS), as a single source of truth for sample details, protocols, and results. This reduces errors and speeds up decision-making [64].
- Automate routine tasks: Automate repetitive tasks like sample tracking, data logging, and test scheduling to free up researchers for high-priority work and reduce manual errors [64].
- Standardize procedures: Develop and follow clear Standard Operating Procedures (SOPs) to ensure consistency, quality, and compliance [65].
- Apply Lean principles: Identify and eliminate waste (e.g., defects, waiting, unnecessary motion) in your processes through value stream mapping [65].
Quantitative Data and Methodologies
Comparison of Preservation Method Efficacy
The table below summarizes the performance of different preservatives in maintaining amplifiable hookworm DNA in stool samples stored at 32°C for 60 days, as measured by qPCR Cq values [60].
Table 1: Efficacy of Stool Preservatives at 32°C for DNA-Based Diagnosis
| Preservation Method | Performance at 32°C (vs. no preservative) | Key Considerations |
|---|---|---|
| FTA Cards | Most advantageous for minimizing Cq increase | Low volume capacity, specialized for molecular analysis. |
| Potassium Dichromate | Most advantageous for minimizing Cq increase | Toxic reagent. |
| Silica Bead Desiccation | Most advantageous for minimizing Cq increase | Two-step process can be more labor-intensive. |
| RNAlater | Demonstrates a protective effect | |
| 95% Ethanol | Demonstrates a protective effect | Low cost, low toxicity, pragmatic for field use. |
| PAXgene | Demonstrates a protective effect | |
| No Preservative | Significant increase in Cq value | Not recommended for long-term storage without cold chain. |
Comparison of Serological Assay Performance
The table below compares the sensitivity and specificity of different ELISA formats and Hemagglutination Inhibition (HI) tests for detecting Swine Influenza A Virus (swIAV) antibodies, highlighting their suitability for screening or confirmatory testing [66].
Table 2: Performance of Serological Assays for swIAV Surveillance
| Assay Type | Sensitivity (%) | Specificity (%) | Recommended Use |
|---|---|---|---|
| HI Test (expanded panel) | 97.77 | N/A | Gold standard; provides subtype-level information. |
| Indirect ELISA (ELISA 1) | 95.69 | 60.00 | High sensitivity适合用于 herd-level screening. |
| Competitive ELISA (ELISA 2) | 81.36 | 83.33 | Higher specificity适合用于 confirmatory testing. |
| Blocking ELISA (ELISA 3) | 82.89 | 76.67 | Higher specificity适合用于 confirmatory testing. |
Detailed Protocol: Modified SIMPAQ Sample Preparation
The following protocol is modified to minimize egg loss and improve the capture efficiency of soil-transmitted helminth (STH) eggs in stool for the SIMPAQ LoD device [63].
Objective: To prepare a stool sample for high-efficiency separation and quantification of STH eggs using a lab-on-a-disk device. Materials: Fresh stool sample, saturated sodium chloride (NaCl) flotation solution, surfactant (e.g., Tween 20), 200 µm filter mesh, SIMPAQ disk, centrifuge compatible with the disk, digital camera. Procedure:
- Homogenization and Filtering: Homogenize 1 gram of fresh stool with 10 mL of saturated NaCl flotation solution containing a small amount of surfactant (e.g., 0.1% Tween 20) to reduce egg adhesion to surfaces.
- Coarse Filtration: Filter the mixture through a 200 µm mesh to remove large debris that could clog the disk.
- Disk Loading: Introduce the filtered suspension into the injection port of the SIMPAQ disk.
- Centrifugation: Place the disk in a centrifuge and spin at the optimized speed (pre-determined to maximize egg capture in the Field of View).
- Imaging: After centrifugation, capture a single digital image of the disk's imaging zone (Field of View) for egg quantification.
Key Modifications for Optimization:
- Surfactant Use: Adding a surfactant to the flotation solution significantly reduces the adhesion of eggs to the walls of pipettes, tubes, and the disk itself, minimizing egg loss [63].
- Debris Removal: The coarse filtration step is critical for preventing larger particles from obstructing the disk's channels and imaging zone, thereby improving egg capture efficiency [63].
- Disk Design: A shorter channel length in the disk (e.g., 27 mm vs. 37 mm) helps minimize the effects of Coriolis and Euler forces, which can deflect eggs away from the imaging zone [63].
Workflow and Process Diagrams
Optimized Sample Processing Workflow
The diagram below outlines a generalized, optimized workflow for processing stool samples for the molecular diagnosis of parasitic infections, integrating best practices for preservation and preparation.
Optimized Parasite Diagnostic Workflow
Preservation Method Selection Logic
This decision tree guides the selection of an appropriate preservation method based on the research objectives and field constraints.
Preservation Method Selection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Sensitive Parasitology Research
| Reagent / Material | Function / Application |
|---|---|
| 95% Ethanol | An effective and pragmatic preservative for stool samples in field settings, protecting DNA from degradation at ambient temperatures [60]. |
| Saturated Sodium Chloride (NaCl) | A flotation solution used in concentration techniques (e.g., SIMPAQ, FLOTAC) to isolate parasite eggs from fecal debris based on density [63]. |
| Surfactants (e.g., Tween 20) | Added to flotation solutions to reduce surface tension and minimize the adhesion of parasite eggs to laboratory ware, thereby reducing egg loss during processing [63]. |
| Formalin-Ethyl Acetate | Used in centrifugation-sedimentation concentration techniques for the recovery and identification of a wide range of intestinal parasites [62]. |
| Proteinase K | A broad-spectrum serine protease used in DNA extraction to digest proteins and inactivate nucleases, crucial for obtaining high-quality DNA from complex samples like tissue and stool [61] [67]. |
| Silica Gel Membrane Columns | The core of many modern DNA extraction kits; DNA binds to the silica membrane under high-salt conditions and is eluted under low-salt conditions, providing a rapid and efficient purification method [67]. |
| CTAB (Cetyltrimethylammonium Bromide) | A detergent used in the "gold standard" CTAB method for plant DNA extraction, effective in precipitating polysaccharides and polyphenols that commonly contaminate nucleic acid preparations [67]. |
| PVP (Polyvinylpyrrolidone) | Used in DNA extraction buffers, particularly for plant tissues, to bind and remove polyphenols that can oxidize and co-precipitate with DNA, inhibiting downstream applications [67]. |
Economic and Regulatory Challenges in Diagnostic Development and Deployment
Welcome to the Technical Support Center for Diagnostic Development. This resource provides troubleshooting guides and FAQs to help researchers, scientists, and drug development professionals navigate the economic and regulatory challenges in developing and deploying diagnostics, with a specific focus on improving sensitivity for low-intensity parasite infections.
Key Challenges in Diagnostic Development
Researchers in this field face a complex landscape of interconnected barriers. The table below summarizes the core economic and regulatory challenges identified in recent global assessments [68].
Table 1: Key Economic and Regulatory Challenges in Diagnostic Development
| Challenge Category | Specific Barriers | Impact on Low-Intensity Infection Research |
|---|---|---|
| Economic Challenges | - Unpredictable demand and lack of financial incentives [68]- Suboptimal financing models and inadequate surge investment mechanisms [68]- Highly concentrated manufacturing with limited regional capacity [68] | - Difficult to secure sustained funding for rare or neglected diseases.- Limits scale-up of promising assays for field deployment. |
| Regulatory Challenges | - Fragmented and inconsistent regulatory systems [68]- Lack of harmonized processes and agile emergency pathways [68]- Complex and lengthy pathways for test verification and regulatory approval [69] | - Delays in getting new, sensitive tests to market and into field use.- Creates uncertainty for developers, discouraging investment. |
| Research & Development | - Underinvestment in R&D and delays in access to critical data [68]- Severe challenges in accessing and validating clinical samples [68] | - Directly impedes development of highly sensitive tests for low-parasite-load conditions.- Slows down assay validation and refinement. |
Experimental Protocols for Enhancing Diagnostic Sensitivity
Protocol: Loop-Mediated Isothermal Amplification (LAMP) for Low-Intensity Infections
LAMP is a powerful nucleic acid amplification technique that serves as a practical alternative to PCR in resource-limited settings. It is particularly valuable for detecting low-abundance pathogen DNA [70].
Detailed Methodology:
- Sample Preparation: Use a crude preparation method. Boil the patient sample (e.g., blood, stool) for 5-10 minutes to lyse cells and release pathogen DNA. A brief centrifugation step can be used to pellet debris.
- Reaction Setup: Prepare a master mix containing:
- Strand-displacing DNA polymerase (e.g., Bst polymerase)
- dNTPs
- Betaine (to assist DNA strand separation)
- Four to six primers specifically designed to recognize six to eight distinct regions of the target parasite DNA sequence.
- Magnesium sulfate (MgSO₄)
- Amplification: Incubate the reaction tube at a constant temperature of 60–65°C for 15–60 minutes. No thermal cycling is required.
- Detection: Results can be visualized by:
- Colorimetric change: Add a metal indicator like hydroxy naphthol blue (HNB) to the master mix beforehand. A color change from violet to sky blue indicates a positive reaction.
- Turbidity: Positive reactions produce a white precipitate of magnesium pyrophosphate, visible to the naked eye or measurable with a turbidimeter.
- Fluorescence: Use intercalating dyes under UV light.
Troubleshooting Guide:
- Problem: Low sensitivity in detecting low-parasite-load samples.
- Solution: Re-optimize primer concentrations and ratios. Increase the amplification time to 60 minutes. Ensure sample preparation efficiently removes PCR inhibitors.
- Problem: High background or false positives.
- Solution: Improve primer specificity using dedicated design software. Implement strict physical separation of pre- and post-amplification areas. Use uracil-DNA glycosylase (UDG) to carryover contamination.
Protocol: Multiplexed Lateral Flow Immunoassay (LFIA) for Co-Infections
Multiplexed LFIAs enable the simultaneous detection of multiple parasite-specific antigens or antibodies in a single test, which is crucial for diagnosing co-infections with similar clinical presentations [70].
Detailed Methodology:
- Antibody Conjugation: Conjugate different specific capture antibodies (e.g., for Plasmodium HRP-II, Leishmania antigens) to distinct labels (e.g., gold nanoparticles, quantum dots, latex beads of different colors).
- Test Strip Assembly: On a nitrocellulose membrane, immobilize the capture antibodies at discrete test lines (T1, T2, etc.). A control line with anti-species antibodies is also applied.
- Assay Procedure: Apply the patient sample (e.g., serum, whole blood) to the sample pad. Add a running buffer to mobilize the sample and conjugated antibodies.
- Result Interpretation: As the liquid flows, if the target analyte is present, it forms a complex with the conjugated antibody and is captured at the corresponding test line, producing a visible band. The control line must always appear for the test to be valid.
Troubleshooting Guide:
- Problem: Cross-reactivity between test lines leading to false positives.
- Solution: Optimize antibody pairs to ensure they are highly specific to their respective targets. Use a dual-zone test strip design to physically separate test lines further. Adjust reagent concentrations and blocking agents in the running buffer.
- Problem: Weak or faint test lines for low-abundance targets.
- Solution: Incorporate more sensitive labels such as fluorescent or lanthanide-doped nanoparticles. Use a smartphone-based reader for quantitative, objective measurement of the line intensity [70].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Sensitive Diagnostic Development
| Reagent / Material | Function | Application in Parasite Diagnostics |
|---|---|---|
| Strand-displacing DNA Polymerase (e.g., Bst polymerase) | Enzymatically amplifies DNA at a constant temperature, eliminating the need for a thermal cycler [70]. | Core enzyme for LAMP assays to detect parasite DNA in blood or tissue samples. |
| Gold Nanoparticles | Serve as a colorimetric label in immunoassays, producing a red line upon accumulation [70]. | Commonly used label for lateral flow tests detecting parasite antigens (e.g., malaria HRP-II). |
| Quantum Dots / Lanthanide-doped Nanoparticles | Fluorescent labels that offer higher sensitivity and enable multiplexing [70]. | Used in advanced LFIAs for quantifying low levels of multiple parasite biomarkers simultaneously. |
| Betaine | A chemical additive that reduces the melting temperature of DNA secondary structures [70]. | Used in LAMP master mixes to improve amplification efficiency and specificity, crucial for sensitive detection. |
| Crude Sample Preparation Reagents (e.g., Chelex resin) | Rapidly purifies nucleic acids by removing inhibitors and proteins without complex equipment. | Enables quick DNA extraction from blood or stool in field settings for downstream LAMP or PCR. |
| Monoclonal & Polyclonal Antibody Pairs | Highly specific binding proteins that form the core of antigen-detection assays. | Critical for developing sensitive and specific immunoassays (ELISA, LFIA) for parasite antigens. |
Diagnostic Development and Evaluation Workflow
The following diagram illustrates the critical pathway from concept to deployment for a new diagnostic test, highlighting key stages where economic and regulatory challenges arise.
Regulatory Navigation and Verification Framework
Navigating the regulatory landscape is a major hurdle. The diagram below outlines a proposed framework for engaging with regulatory bodies and independent verification centers, based on successful models like RADx [69].
Frequently Asked Questions (FAQs)
Q1: Our research team has developed a highly sensitive LAMP assay for a low-intensity parasite infection. What is the biggest economic challenge we will face in transitioning from a research prototype to a commercially available test?
A: The most significant economic challenge is the "valley of death" between initial innovation and sustainable commercialization. This is characterized by [68]:
- Unpredictable Demand: For neglected diseases, the commercial market may be perceived as small, deterring private investment.
- Lack of Surge Financing: There are often no ready mechanisms for the significant, rapid investment needed to scale up manufacturing.
- Fragmented Procurement: The absence of large, guaranteed purchase agreements (e.g., volume guarantees) makes it financially risky for a manufacturer to commit to production.
Q2: We are experiencing inconsistent results when validating our new diagnostic test with clinical samples. The sample access process is slow and the samples are poorly characterized. How can we troubleshoot this?
A: This is a common barrier [68]. To troubleshoot:
- Audit Your Sample Bank: Document the exact collection, storage, and handling conditions for each sample. Inconsistent results can stem from sample degradation.
- Establish a Detailed SOP: Create a strict standard operating procedure (SOP) for sample processing that all team members follow.
- Collaborate with Clinical Sites: Build stronger partnerships with clinical sites to ensure samples are collected with the necessary metadata (e.g., patient symptomology, co-infections, parasite load via a standard method).
- Utilize Biobanks: Where possible, source samples from established, high-quality biobanks that provide well-characterized reference materials.
Q3: What is test verification, and how can it help our small startup navigate the complex regulatory process for a new diagnostic?
A: Test verification is an independent, impartial evaluation of a diagnostic test's performance (e.g., analytical sensitivity, specificity, repeatability) conducted by a third-party laboratory [69]. This process, as pioneered by the NIH's RADx program, is immensely helpful for smaller developers because it:
- De-risks Development: Provides objective data that can attract further investment.
- Accelerates Regulatory Review: Regulatory agencies like the FDA can use this independent data with higher confidence, potentially speeding up the authorization process.
- Provides Expert Feedback: Verification hubs often work iteratively with developers to identify and fix performance issues before formal regulatory submission.
Q4: How can we design our diagnostic test to be more suitable for use in low-resource settings, which are often endemic for low-intensity parasite infections?
A: Design your test to meet the WHO REASSURED criteria [70]:
- Real-time connectivity
- Equipment-free
- Affordable
- Sensitive
- Specific
- User-friendly
- Rapid and robust
- Equipment-free
- Deliverable to end-users Focus on attributes like low cost, minimal or no reliance on external equipment, stability at high temperatures, and simple visual readouts. Integrating with mobile health (mHealth) platforms for result interpretation and data sharing can also enhance utility [70].
Data-Driven Decisions: Comparative Performance and Validation of Sensitive Diagnostics
Diagnostic Sensitivity Comparison Tables
The following tables summarize quantitative data from head-to-head studies comparing the sensitivity of novel molecular methods against conventional diagnostic techniques for various parasitic infections.
Protozoan Parasites
| Parasite | Conventional Method | Sensitivity (%) | Novel Method | Sensitivity (%) | Citation |
|---|---|---|---|---|---|
| Leishmania spp. (Cutaneous) | Microscopy | 76.7% | PCR (kDNA) | 93.6% | [71] |
| Leishmania spp. (Cutaneous) | Culture (NNN medium) | 50.7% | PCR (kDNA) | 93.6% | [71] |
| Plasmodium falciparum | Light Microscopy | 77.8% | mRDT (Blood) | 75.8% | [72] |
| Plasmodium falciparum | Light Microscopy | 77.8% | mRDT (Saliva) | 74.5% | [72] |
| Plasmodium falciparum | Light Microscopy | 77.8% | mRDT (Urine) | 70.7% | [72] |
Helminth Parasites
| Parasite | Conventional Method (3 Samples) | Sensitivity (%) | Hybrid Method (1 Sample: qPCR + FEA + Culture) | Sensitivity (%) | Citation |
|---|---|---|---|---|---|
| Strongyloides spp. | FEA Microscopy & Culture | Reference | qPCR + FEA + Culture | 100.0% | [73] |
| Trichuris trichiura | FEA Microscopy & Culture | Reference | qPCR + FEA + Culture | 90.9% | [73] |
| Hookworm species | FEA Microscopy & Culture | Reference | qPCR + FEA + Culture | 86.8% | [73] |
| Giardia duodenalis | FEA Microscopy & Culture | Reference | qPCR + FEA + Culture | 75.0% | [73] |
Experimental Protocols for Key Comparisons
This protocol describes the comparative methodology used to evaluate diagnostic sensitivity for Cutaneous Leishmaniasis.
- Sample Collection: Obtain tissue from the cleaned margin of skin lesions using a disposable lancet. Make a small incision, scrape along the cut edge, and smear the tissue on a glass microscope slide.
- Microscopy: Fix dried smears with 100% methanol. Stain with Giemsa and examine under a light microscope for the presence of amastigotes.
- Culture: Inoculate scraped tissue into the liquid phase of Novy-McNeal-Nicolle (NNN) medium. Incubate at 25°C and examine weekly for promastigote growth for up to one month.
- DNA Extraction for PCR:
- Scrape the dried smear from the slide with a sterile scalpel.
- Add scrapings to 200 µl of lysis buffer [50 mM Tris-HCl (pH 7.6), 1 mM EDTA, 1% Tween 20] containing proteinase K.
- Incubate at 56°C for 2 hours.
- Perform phenol:chloroform:isoamyl-alcohol extraction and precipitate DNA with cold absolute ethanol.
- Resuspend DNA in 50 µl of double-distilled water.
- PCR Amplification:
- Primers: Use forward LINR4 (5′-GGG GTT GGT GTA AAA TAG GG-3′) and reverse LIN17 (5′-TTT GAA CGG GAT TTC TG-3′) to amplify variable regions of the minicircle kinetoplast DNA (kDNA).
- Reaction Mix: 25-µl volume containing 250 µM dNTPs, 1.5 mM MgCl2, 1 U Taq polymerase, 1 µM of each primer, and DNA extract.
- Thermal Cycling: 5 min at 94°C; 30 cycles of 30 sec at 94°C, 30 sec at 52°C, 1 min at 72°C; final extension of 5 min at 72°C.
- Analysis: Electrophorese PCR products on a 1.5% agarose gel, stain with ethidium bromide, and visualize under UV light.
This protocol outlines a hybrid approach for detecting gastrointestinal parasites from a single stool sample.
- Sample Collection: Collect a single faecal sample and store appropriately.
- Traditional Methods (Performed on one sample):
- Formalin-Ethyl Acetate (FEA) Concentration: Concentrate the stool sample using the FEA method to separate and concentrate parasites.
- Light Microscopy: Examine the concentrated sediment under a microscope to identify helminth eggs, larvae, and protozoan cysts.
- Charcoal Culture: Culture the sample to allow larvae to hatch and multiply for detection.
- Molecular Method (Performed on the same sample):
- DNA Extraction: Extract DNA from a portion of the stool sample using a commercial kit or standard method.
- Multiplex qPCR: Use a multiplex TaqMan qPCR assay to simultaneously screen for five helminths and three protozoa. The assay uses specific primers and fluorescent probes for each target.
Workflow: Hybrid Diagnostic Approach for GI Parasites
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Our PCR for Leishmania detection shows weak or no amplification, despite positive microscopy. What could be wrong? [71] [74]
- Inhibition Check: Always include a control to check for PCR inhibitors co-extracted from the sample. Consider diluting the DNA template or using a purification kit designed to remove inhibitors.
- DNA Yield: For stained slides, the scraping method may yield low DNA. Ensure the slide is thoroughly scraped and consider using multiple slides for extraction.
- Primer Specificity: Verify that your primers (e.g., LINR4/LIN17) are specific for the Leishmania species in your region. Mismatches can lead to failed amplification.
- Thermal Cycler Calibration: Check the calibration of your thermal cycler to ensure it reaches the denaturing, annealing, and extension temperatures specified in the protocol.
Q2: When comparing novel vs. conventional methods, what are the essential experimental controls? [75] [74]
- Positive Control: Include a known positive sample for each parasite species you are detecting (e.g., reference strain DNA for PCR, a known infected stool for microscopy).
- Negative Control: Include a known negative sample to ensure your reagents and process are not contaminated.
- Process Control: For molecular tests, include a control to monitor the DNA extraction efficiency and the presence of PCR inhibitors (e.g., a human gene target or an exogenous DNA spike).
- Clinical Reference Standard: In diagnostic comparisons, define a reference standard. This is often a composite result from multiple tests (e.g., the result from three stools tested traditionally [73]) or a highly sensitive molecular test to judge the performance of the method under evaluation.
Q3: What are the key advantages of a hybrid diagnostic approach? [73]
The hybrid approach leverages the strengths of different methods. Molecular methods like qPCR offer high sensitivity for detecting low-intensity infections, particularly for protozoa and those helminths where egg shedding is intermittent. Traditional microscopy provides a direct view of the parasite and can detect a broad range of unexpected organisms. Using both on a single sample maximizes detection rates, can reduce the need for repeated patient sampling, and provides a more comprehensive parasitological assessment.
Q4: How can we improve the detection of low-density malaria infections in field surveys? [72] [76]
- High-Sensitivity Antigen Detection: Integrate high-throughput bead-based immunoassays (e.g., for HRP2) which have a much lower limit of detection than Rapid Diagnostic Tests (RDTs) and are suitable for processing large numbers of samples. [76]
- Molecular Tools: Use PCR or loop-mediated isothermal amplification (LAMP) as a reference standard to identify sub-microscopic infections that are missed by RDTs and microscopy. [17] [72]
- Non-Invasive Samples: Explore the use of saliva and urine with highly sensitive detection methods, though optimization is needed as sensitivity with current RDTs is lower than blood-based tests. [72]
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Application | Example / Note |
|---|---|---|
| Novy-Nicolle-McNeal (NNN) Medium | For culturing promastigotes of Leishmania species from clinical samples. | Contains rabbit blood; requires weekly examination for up to one month. [71] |
| LINR4 & LIN17 Primers | PCR primers that amplify the variable region of the minicircle kinetoplast DNA (kDNA) of Leishmania. | Allows for high-sensitivity detection and can be used for species identification based on amplicon size. [71] |
| Multiplex TaqMan qPCR Assay | Simultaneous detection and quantification of multiple gastrointestinal parasite targets in a single reaction. | Highly sensitive for parasites like Strongyloides spp. and Giardia duodenalis; requires specific primer-probe sets. [73] |
| PfHRP2/pLDH Rapid Test | Immunochromatographic test for detection of Plasmodium falciparum specific antigen (HRP2) and pan-Plasmodium antigen (pLDH). | Used for point-of-care diagnosis on blood, and researched for use on non-invasive samples like saliva and urine. [72] |
| High-Throughput Bead-Based HRP2 Assay | A multiplex immunoassay for sensitive quantification of HRP2 antigen from dried blood spots; used in large-scale surveillance. | More sensitive than RDTs, useful for detecting low-density infections and assessing transmission in communities. [76] |
| Nanomaterial | Target Parasite | Application |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Plasmodium | Detection of PfHRP2 antigen for malaria diagnosis. |
| Quantum Dots (QDs) | Leishmania | Labeled with DNA probes for sensitive detection of Leishmania kDNA. |
| Carbon Nanotubes (CNTs) | Echinococcus | Functionalized with anti-EgAgB antibodies to detect hydatid cyst fluid antigen. |
| Graphene Oxide (GO) | Schistosoma | Based on soluble egg antigen (SEA) binding for schistosomiasis diagnosis. |
Frequently Asked Questions
Q1: Our field team is reporting inconsistent results with HRP2-based Rapid Diagnostic Tests (RDTs) in a low-transmission area. What could be causing this?
Inconsistent RDT results, particularly in low-transmission settings, are frequently caused by infections with low parasite densities that fall below the test's detection threshold. The limit of detection (LOD) for RDTs can vary significantly between geographic locations. One study in Senegal found the LOD₉₅ (the antigen concentration detected 95% of the time) varied from 3.9 ng/mL to 204.3 ng/mL across different districts [76]. Furthermore, the deletion of the PfHRP2 and PfHRP3 genes in the parasite population compromises the effectiveness of HRP2-based RDTs [44]. For community screening where asymptomatic, low-density infections are common, consider supplementing RDTs with a more sensitive molecular method.
Q2: We need to process hundreds of samples from a field survey. What high-throughput, sensitive diagnostic method is suitable for a laboratory with limited molecular biology infrastructure?
A high-throughput, bead-based antigen detection method (a one-step multiplex assay) is well-suited for screening large sample sets from field surveys [76]. This immunoassay can detect multiple antigens simultaneously and integrates well with traditional RDT methods to assess community-wide infection rates. For a molecular method, a recently developed near point-of-care LAMP-based platform can process up to 12 samples in a 45-minute workflow, requires only a simple, portable heat block, and uses visual (colorimetric) readout, eliminating the need for complex instrumentation [44]. It has a high sensitivity of 95.2% and specificity of 96.8% when benchmarked against qPCR [44].
Q3: How effective are deep learning models compared to human experts in identifying intestinal parasites from microscope images?
Recent evaluations show that deep-learning-based approaches have strong agreement with human experts and can achieve high accuracy. One study reported that state-of-the-art models like DINOv2-large achieved an accuracy of 98.93%, a sensitivity of 78.00%, and a specificity of 99.57% in identifying parasites from stool sample images [36]. The study also found a strong level of agreement (Cohen’s Kappa >0.90) between the models and medical technologists [36]. These models perform particularly well with helminthic eggs and larvae due to their more distinct morphology [36].
Troubleshooting Guides
Issue: Poor Sensitivity of RDTs in Community Screening
Problem: RDTs are failing to detect a known number of positive cases, especially in asymptomatic individuals.
Investigation & Resolution:
| Investigation Step | Possible Cause | Recommended Action |
|---|---|---|
| Determine parasite density | Low-density submicroscopic infections | Validate RDT results against a highly sensitive molecular reference standard (e.g., qPCR or LAMP) [44]. |
| Quantify HRP2 antigen | Low antigen concentration below RDT detection | Use a bead-based HRP2 quantification assay to establish the actual antigen levels in samples and determine the specific LOD for your region [76]. |
| Collect sample for genetic analysis | PfHRP2/3 gene deletions | Perform PCR analysis on dried blood spots (DBS) to confirm the presence of wild-type PfHRP2/3 genes [44]. |
Issue: Low Throughput of Sensitive Molecular Tests in the Field
Problem: Gold-standard molecular methods like qPCR are too slow and complex for the required survey scale.
Investigation & Resolution:
| Investigation Step | Possible Cause | Recommended Action |
|---|---|---|
| Analyze workflow bottlenecks | Lengthy, complex nucleic acid extraction | Implement a magnetic bead-based nucleic acid extraction method (e.g., SmartLid technology) that processes 12 samples in under 15 minutes without a centrifuge [44]. |
| Evaluate amplification method | Reliance on sophisticated thermocyclers | Switch to an isothermal amplification method like LAMP, which uses a simple, portable heat block [44]. |
| Assess result interpretation | Need for fluorescent readers | Adopt a colorimetric LAMP format where a color change (pink to yellow) provides a visual result, eliminating the need for expensive instruments [44]. |
Diagnostic Tool Performance Data
The following tables summarize the quantitative performance of various diagnostic tools as reported in recent studies, crucial for selecting the right method for community-based screening.
Table 1: Performance of Novel Molecular and Antigen Detection Platforms
| Diagnostic Platform / Model | Sensitivity | Specificity | Limit of Detection (LOD) | Key Advantage |
|---|---|---|---|---|
| LAMP-based (Pan/Pf) | 95.2% | 96.8% | 0.6 parasites/μL | Near point-of-care; 45 min workflow; colorimetric readout [44]. |
| Bead-based HRP2 Assay | (N/A - Quantification) | (N/A - Quantification) | (Varies by region) | High-throughput; quantitative data; useful for validating RDTs [76]. |
| DINOv2-large (AI Model) | 78.00% | 99.57% | (N/A) | High accuracy & specificity for parasite egg identification [36]. |
| YOLOv8-m (AI Model) | 46.78% | 99.13% | (N/A) | Object detection model for identifying multiple parasites in an image [36]. |
Table 2: Comparative Performance of Diagnostics for Detecting Asymptomatic & Submicroscopic Malaria
| Diagnostic Method | Sensitivity (Asymptomatic) | Sensitivity (Submicroscopic*) | Notes / Context |
|---|---|---|---|
| LAMP-based (Pan/Pf) | 94.9% (130/137) | 95.3% (41/43) | Capillary blood; community survey in The Gambia & Burkina Faso [44]. |
| Expert Microscopy | 70.1% | 0% | Benchmark against LAMP/qPCR in the same study [44]. |
| HRP2-based RDT | 49.6% | 4.7% | Benchmark against LAMP/qPCR in the same study [44]. |
Submicroscopic defined as <16 parasites/μL in the cited study [44].
Detailed Experimental Protocols
Protocol 1: High-Throughput Bead-Based HRP2 Antigen Detection for RDT Validation
This protocol is adapted for validating RDT performance in large-scale surveys by quantifying HRP2 antigen levels [76].
Key Applications:
- Determining the actual limit of detection (LOD) of RDTs in a specific region.
- Identifying false-negative RDT results caused by low antigen concentration.
- Providing quantitative data for correlating antigen level with transmission intensity.
Materials:
- Dried Blood Spot (DBS) samples from participants.
- Bead-based HRP2 immunoassay kit (e.g., multiplex assay with fluorescent-coded beads).
- Plate reader capable of detecting fluorescence.
- Gaussian mixture model software (e.g., R or Python) for classifying HRP2 positivity from quantitative data.
Procedure:
- Sample Collection: Collect capillary blood from participants via finger prick. Perform RDT on site. Prepare DBS on filter paper for subsequent bead-based analysis.
- Elution: Punch discs from the DBS and elute the HRP2 antigen into a buffer solution.
- Multiplex Immunoassay: Incubate the eluted sample with the bead-based assay according to manufacturer specifications. This typically involves antigen-antibody binding, washing, and detection with a fluorescent reporter.
- Data Acquisition: Run the plate on a fluorescent reader to obtain quantitative HRP2 concentration values for each sample.
- Data Analysis:
- Use a Gaussian mixture model to determine a threshold for classifying samples as HRP2-positive or negative based on the concentration data.
- Perform logistic regression to analyze the relationship between HRP2 concentration and the RDT outcome (positive/negative).
- Calculate the LOD₉₅ for the RDTs used in the survey.
Protocol 2: Near Point-of-Care LAMP for Sensitive Community Screening
This protocol details the use of a streamlined LAMP workflow for the detection of submicroscopic Plasmodium infections in capillary blood [44].
Key Applications:
- Active case detection in elimination settings.
- Community-level test-and-treat strategies requiring high sensitivity.
- Surveillance of asymptomatic reservoirs of infection.
Materials:
- SmartLid Blood DNA/RNA Extraction Kit (or equivalent magnetic bead-based kit).
- Lyophilised colourimetric LAMP pellets (Pan/Pf specific).
- EDTA-capillary blood tubes.
- Portable dry-bath heat block.
- Disposable tube strips and a reusable magnetic key.
Procedure:
- Sample Preparation: Collect 100 μL of EDTA-anticoagulated capillary blood.
- Nucleic Acid Extraction (Duration: ~15 min):
- Add a proteinase K lysis step (5 min at 65°C) to the blood sample.
- Use the SmartLid technology with vortex mixing to transfer magnetic beads through lysis, wash, and elution buffers.
- Elute purified DNA in a final volume.
- Amplification & Detection (Duration: ~45 min total):
- Add the eluted DNA to the tube containing the lyophilised LAMP pellets.
- Place the tube in a dry-bath heat block at a constant temperature (e.g., 65°C) for 30-40 minutes.
- Visual Readout: Observe the color change. A positive result is indicated by a change from pink to yellow.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Diagnostic Validation
| Reagent / Material | Function in the Context of Validation |
|---|---|
| Dried Blood Spot (DBS) Cards | Stable, easy-to-transport medium for collecting and storing blood samples from remote field sites for subsequent batch analysis in a central lab [76]. |
| Magnetic Bead-based NA Extraction Kits | Enable rapid, high-throughput purification of nucleic acids from blood without the need for centrifugation, crucial for field-deployable molecular workflows [44]. |
| Lyophilised LAMP Reagents | Stable, cold-chain-independent pellets containing all necessary enzymes and buffers for isothermal amplification, ideal for resource-limited settings [44]. |
| Multiplex Bead-Based Assay Kits | Allow for simultaneous, quantitative detection of multiple antigens (e.g., HRP2, pLDH) from a single sample, providing rich data for assay validation and epidemiological research [76]. |
| Proteinase K | An essential enzyme for the efficient lysis of blood cells and degradation of proteins during DNA extraction, improving nucleic acid yield and purity from whole blood [44]. |
Workflow Visualization
The following diagram illustrates the streamlined workflow for the near point-of-care LAMP diagnostic method.
Near-POC LAMP Workflow
FAQs on Key Analytical Metrics
Q1: What is the critical difference between sensitivity and the Limit of Detection (LOD)?
Sensitivity and the Limit of Detection (LOD) are distinct but related concepts. Sensitivity is formally defined as the slope of the analytical calibration curve, indicating how much the measurement signal changes with a unit change in analyte concentration [77] [78]. In contrast, the Limit of Detection (LOD) is the lowest concentration of an analyte that can be reliably distinguished from a blank sample with a stated level of confidence [79] [77] [80]. It is a measure of the ultimate detection capability of an assay, not its quantitative responsiveness. A common point of confusion arises because the ELISA industry and some other fields often use the term "sensitivity" colloquially to refer to the detection limit [78].
Q2: How does diagnostic sensitivity differ from analytical sensitivity?
This is a crucial distinction in laboratory medicine:
- Diagnostic Sensitivity: This is a statistical measure of a test's clinical accuracy. It is defined as the proportion of individuals with a disease who are correctly identified as positive by the test. It is calculated as (True Positives) / (True Positives + False Negatives) [81] [82].
- Analytical Sensitivity: This is a performance characteristic of the assay itself, often synonymous with the LOD. It is the lowest concentration of an analyte that an assay can reliably detect, expressed as a concentration (e.g., ng/mL, copies/μL) [83] [84]. It is concerned with the smallest physical amount that can be seen, not the correct classification of patients.
Q3: Why is my assay showing high sensitivity but poor specificity, and how can I troubleshoot this?
Sensitivity and specificity are often inversely related; as one increases, the other tends to decrease [81]. High sensitivity with poor specificity means your assay is excellent at detecting the true positive cases but is also generating a large number of false positives.
Troubleshooting steps to improve specificity:
- Check for Cross-Reactivity: Review the analytical specificity (cross-reactivity) studies for your assay. A high level of cross-reactivity with related but non-target organisms or substances is a primary cause of false positives [83]. Ensure your primers, probes, or antibodies are highly specific for your target parasite.
- Optimize Reaction Stringency: For molecular methods like PCR, increase the annealing temperature or optimize the buffer conditions to enhance primer binding specificity. For immunoassays, adjust washing stringency and buffer composition.
- Re-evaluate the Cut-off Value: The threshold for defining a positive result might be set too low. Analyze your receiver operating characteristic (ROC) curve to determine if a different cut-off value would better balance sensitivity and specificity [85] [82].
- Review Sample Integrity: Assess if sample degradation or the presence of interfering substances in the sample matrix is contributing to non-specific signals [83].
Q4: What is the relationship between LOD and Limit of Quantification (LOQ)?
The LOD and LOQ define different capability levels for an assay [79] [78] [80].
- LOD: The lowest level that can be detected, but not necessarily quantified with precision. It answers the question, "Is the analyte there?"
- LOQ: The lowest level that can be measured with stated acceptable precision and accuracy. It answers the question, "How much of the analyte is there?"
The concentration scale is often divided into three regions: below the LOD ("not detected"), between the LOD and LOQ ("qualitatively detected"), and above the LOQ ("quantitatively measured") [78]. Statistically, the LOQ is typically set at a higher multiple of the blank signal noise than the LOD (e.g., LOD = meanblank + 3σblank; LOQ = meanblank + 10σblank) [78].
Table 1: Key Definitions for Analytical Performance Metrics
| Metric | Formal Definition | Key Interpretation |
|---|---|---|
| Sensitivity (Analytical) | Slope of the analytical calibration curve (S = dy/dx) [77]. |
Measure of the method's responsiveness to concentration change. |
| Limit of Detection (LOD) | The lowest concentration that can be reliably distinguished from a blank, with a stated confidence level [79] [80]. | The minimum detectable amount of analyte. |
| Limit of Quantification (LOQ) | The lowest concentration that can be measured with acceptable precision and accuracy [79] [80]. | The minimum quantifiable amount of analyte. |
| Sensitivity (Diagnostic) | Proportion of truly diseased individuals who test positive [81] [82]. | The test's ability to correctly identify true cases of disease. |
| Specificity (Diagnostic) | Proportion of truly healthy individuals who test negative [81] [82]. | The test's ability to correctly exclude non-cases. |
Table 2: Experimental Determination of LOD and LOQ
| Parameter | Typical Experimental Approach | Key Statistical Considerations |
|---|---|---|
| LOD (for qPCR) | Measure multiple replicates of a blank and low-concentration samples. Use logistic regression on binary (positive/negative) data across a dilution series to find the concentration at which 95% of replicates are detected [79]. | Standard deviation cannot be calculated for samples that return a negative result (e.g., no Cq value). Data is not normally distributed in linear space [79]. |
| LOD (for Chromatography) | Measure multiple replicates of a blank. The LOD can be estimated as LOD = Mean_blank + 3 * SD_blank or via a calibration curve at low concentrations [80]. |
Assumes a normal distribution of the blank signal and homoscedasticity (constant variance) at low levels, which may not always hold true [80]. |
| LOQ | Determined by measuring multiple low-concentration samples and identifying the lowest level that can be measured with a pre-defined relative standard deviation (RSD), e.g., 20% [79] [80]. | The LOQ is the concentration at which the signal is sufficiently robust and precise for quantitative purposes. |
Detailed Experimental Protocol: Determining LOD for a qPCR Assay
This protocol is adapted from established statistical methods for qPCR [79], which are highly relevant for detecting low-intensity parasite infections where target nucleic acid is scarce.
Objective: To determine the lowest concentration of a parasite DNA target that can be reliably detected by a qPCR assay 95% of the time.
Materials:
- Target Analyte: Purified parasite genomic DNA or synthetic oligo.
- qPCR Reagents: Master mix, primers, and probe for the specific target.
- Equipment: qPCR instrument, pipettes, microcentrifuge, tubes, plates.
Methodology:
- Sample Preparation: Prepare a 2-fold serial dilution of the target DNA, covering a range from a concentration expected to be consistently positive down to a concentration expected to be near or below the detection limit. An example range could be from 64 copies/μL to 0.5 copies/μL.
- Replicate Testing: Analyze each dilution level in a high number of replicates (e.g., n=64). The most diluted sample (lowest concentration) should be run in even more replicates (e.g., n=128) to obtain a robust statistical estimate at the limit [79].
- qPCR Run: Perform the qPCR run according to optimized cycling conditions.
- Data Preprocessing: Manually set a consistent threshold in the exponential phase of amplification across all plots. Record the Cq value for each well. Remove statistical outliers using an appropriate method like Grubb's test [79].
- Data Analysis using Logistic Regression:
- Convert the continuous Cq data into binary data. Assign a value of
1for a detected result (Cq < cut-off, e.g., 40) and0for an undetected result (Cq is undetermined or > cut-off) [79]. - For each concentration (converted to log2 scale), calculate the proportion of positive replicates (
z_i / n_i). - Use statistical software (e.g., GenEx, R) to fit a logistic regression model to the binary data. The model is:
f_i = 1 / (1 + e^(-(β_0 + β_1 * x_i))), wherex_iis log2(concentration) andf_iis the probability of detection [79]. - The LOD is defined as the concentration at which the probability of detection, as predicted by the fitted logistic regression curve, is 0.95. The software will calculate this value and its confidence interval.
- Convert the continuous Cq data into binary data. Assign a value of
Conceptual Workflow for Metric Application
The following diagram illustrates the logical relationship between key analytical concepts and the experimental process for defining an assay's detection capabilities.
Research Reagent Solutions for Sensitivity Optimization
Table 3: Essential Materials for High-Sensitivity Detection Experiments
| Reagent / Material | Function in the Experiment | Critical Considerations for Low-Intensity Infections |
|---|---|---|
| ACCURUN / AccuSeries Controls | Whole-organism positive controls and linearity panels to challenge the entire assay process from extraction to detection [83]. | Using whole parasites (bacteria/viruses) as controls, rather than pure nucleic acids, more accurately reflects the efficiency and LOD of the full diagnostic process [83]. |
| Nucleic Acid Isolation Kits | To extract and purify parasite DNA/RNA from clinical samples. | The extraction efficiency is a major component of the overall LOD. The control for the extraction process is required by CAP guidelines to detect errors in this critical step [83]. |
| Calibrated Genomic DNA | DNA standard calibrated against a recognized standard (e.g., NIST) for creating an accurate standard curve [79]. | Essential for achieving accurate absolute quantification of parasite load, which is critical for monitoring treatment efficacy in low-intensity infections [79]. |
| Target-Specific Primers/Probes | To amplify and detect a unique sequence of the target parasite. | Analytical specificity is paramount. The assay must be tested against a panel of related alleles or organisms to rule out cross-reactivity and prevent false positives [83]. |
| Inhibition-Resistant Master Mix | The chemical environment for the enzymatic amplification of the target. | Samples like blood can contain PCR inhibitors. A master mix designed to resist inhibitors helps prevent false negatives, thereby protecting the diagnostic sensitivity of the assay [79]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is a composite reference standard (CRS) and when should I use one? A composite reference standard (CRS) combines the results of multiple imperfect diagnostic tests to classify a subject as disease positive or negative. You should consider using one in low-prevalence settings or for diseases like parasitic infections where a single perfect reference test ("gold standard") does not exist. CRSs are particularly valuable when the current reference standard has low disease detection capability in your population of interest [86].
FAQ 2: What are the most common biases when implementing a CRS? The most common bias occurs when using an "OR" rule (classifying as positive if any component test is positive). While this increases sensitivity, it does so at the expense of specificity, unless every component test has perfect specificity. This trade-off can lead to significant bias in the accuracy estimates of your index test. The magnitude of bias depends on disease prevalence and the accuracy of the CRS components [87].
FAQ 3: How does disease prevalence affect my choice of diagnostic method? In low-prevalence settings, the limitations of traditional microscopy methods like Kato-Katz (KK) become pronounced. For example, one study found KK sensitivity was only 32% for Necator americanus (hookworm) in a field setting, whereas qPCR achieved 98% sensitivity. As prevalence decreases after treatment rounds, molecular methods like multi-parallel qPCR provide more reliable surveillance by maintaining high sensitivity for detecting light infections [88].
FAQ 4: What is the impact of conditional dependence between tests? Conditional dependence occurs when the errors of your index test and the tests in your CRS are correlated. This can lead to an overestimation of your index test's accuracy (sensitivity and specificity). When this dependence is suspected, statistical models like latent class analysis should be researched instead of relying on simple CRSs [87].
FAQ 5: Can I incorporate treatment response into a reference standard? Yes, this is an innovative approach for complex diseases. One validated framework for vasospasm diagnosis uses a multi-stage hierarchical system. Patients without a definitive diagnosis at primary (imaging) or secondary (clinical/imaging sequelae) levels proceed to a tertiary level where diagnosis is assigned based on their response to appropriate therapy [86].
Troubleshooting Guides
Issue 1: Low Sensitivity in Low-Prevalence Settings
Problem: Your current diagnostic method fails to detect enough true positive cases in a low-prevalence population after mass drug administration.
Solution: Implement a multi-parallel qPCR approach.
- Step 1: Switch from single-target to multi-parallel qPCR assays. This allows simultaneous detection of 8 or more parasites from a single stool sample [88].
- Step 2: Use cryopreserved stool samples (200 mg) stored at -15°C without fixatives and transport on dry ice to a central lab for analysis [88].
- Step 3: Validate your qPCR results against a CRS that includes a quantitative method (like KK) and a clinical outcome, such as worm expulsion post-treatment. The number of worms expelled has been shown to correlate with both KK and qPCR intensity measurements [88].
Issue 2: Bias from a Poorly Constructed CRS
Problem: Your composite reference standard is yielding biased estimates of your new test's accuracy.
Solution: Critically evaluate the structure and components of your CRS.
- Step 1: Avoid using a simple "any-positive" CRS rule unless you are certain all component tests have near-perfect specificity. Explore a "dual composite reference standards (dCRS)" approach that uses both "any-positive" and "all-positive" rules to bracket the true accuracy [89].
- Step 2: Assess potential conditional dependence between your new index test and the tests in your CRS. If they rely on similar biological principles, their errors might be correlated [87].
- Step 3: If bias is suspected, transition to statistical methods like latent class analysis (LCM). LCM can estimate test accuracy and disease prevalence without a perfect standard, though it requires multiple tests and careful model selection [89].
Issue 3: Integrating Clinical and Imaging Data for a Complex Disease
Problem: You need a reference standard for a complex disease (e.g., vasospasm) that encompasses both clinical symptoms and imaging findings, and is applicable to an entire population, not just a subgroup.
Solution: Develop a hierarchical, multi-level reference standard [86].
- Step 1 (Primary Level): Use the highest evidence standard (e.g., DSA for vasospasm) for patients who receive it. Define clear thresholds for disease severity (e.g., mild: <50% luminal narrowing; severe: >75% narrowing) [86].
- Step 2 (Secondary Level): For patients not tested with the primary standard, assess sequelae of the disease using both clinical criteria (e.g., permanent neurological deficits distinct from baseline) and imaging criteria (e.g., delayed infarction on CT/MRI) [86].
- Step 3 (Tertiary Level): For treated patients without sequelae, assign a diagnosis based on response-to-treatment. Patients showing improvement upon administration of appropriate therapy are classified as having the disease [86].
Data Presentation
Table 1: Comparison of Diagnostic Methods for Soil-Transmitted Helminths
This table summarizes quantitative data from a field study in Kenya comparing the sensitivity of multi-parallel qPCR and Kato-Katz (KK) for detecting parasitic infections [88].
| Parasite | qPCR Prevalence | KK Prevalence | qPCR Sensitivity | KK Sensitivity | Notes |
|---|---|---|---|---|---|
| Ascaris lumbricoides | 17% | Not Reported | 98% | 70% | Worm expulsion count correlated with both qPCR (r=0.60) and KK (r=0.63) intensity. |
| Necator americanus | 18% | Not Reported | 98% | 32% | qPCR allows species-level identification, which is impossible with KK. |
| Giardia lamblia | 41% | Not Detected | Not Reported | Not Applicable | KK cannot detect protozoan infections like Giardia. |
| Trichuris trichiura | <1% | Not Reported | Detected | Missed | qPCR detected infections that were missed by the KK method. |
Table 2: Pros and Cons of Common Diagnostic Methods in Low-Prevalence Settings
This table provides a high-level comparison of different diagnostic techniques [18] [90] [88].
| Method | Key Advantage | Key Limitation | Best Use Case |
|---|---|---|---|
| Microscopy (e.g., Kato-Katz) | Low cost; provides intensity data; field-deployable [90]. | Low sensitivity, especially for light infections and hookworm [88]. | Initial impact assessment in high-prevalence areas; resource-limited settings. |
| Multi-parallel qPCR | High sensitivity & specificity; detects multiple pathogens; quantifies infection [88]. | Higher cost; requires lab infrastructure and technical expertise [88]. | Surveillance in low-prevalence settings; monitoring MDA success; research on coinfections. |
| Nanobiosensors | Potential for rapid, sensitive point-of-care detection; high specificity [18]. | Early stage of development; challenges with mass production and standardization [18]. | Future point-of-care diagnostics; integration with lab-on-a-chip platforms. |
| Composite Reference Standard | More accurate than a single imperfect test; incorporates multiple data types [86]. | Can introduce bias if poorly constructed (e.g., low specificity components) [87]. | Complex diseases with no single gold standard; combining clinical and lab data. |
Experimental Protocols
Protocol 1: Implementing a Multi-parallel qPCR for STH Surveillance
Objective: To detect and quantify multiple gastrointestinal parasites from human stool samples with high sensitivity, particularly in low-intensity infection settings.
Materials:
- Precellys Soil grinding SK38 2 mL tubes (or similar)
- Liquid Nitrogen or -80°C freezer for storage
- Dry ice for shipment
- Multi-parallel qPCR assay kits for target parasites (e.g., A. lumbricoides, N. americanus, G. lamblia, E. histolytica)
- Real-time PCR system
Methodology [88]:
- Sample Collection: Collect fresh stool samples from participants. For longitudinal studies, aim for multiple samples per participant.
- Preservation: Weigh 200 mg of stool into a Precellys tube. Do not use fixatives. Store samples at -15°C immediately (within 8 hours of collection).
- Shipment: Transport samples to a central laboratory on dry ice. Store at -80°C upon arrival until processing.
- DNA Extraction: Perform DNA extraction using a robust kit suitable for complex stool samples.
- qPCR Setup: Run multi-parallel qPCR reactions according to manufacturer protocols. Include appropriate standard curves for quantification and negative controls.
- Data Analysis: Calculate infection intensity based on standard curves. Compare cycle threshold (Ct) values to predefined cut-offs for presence/absence.
Protocol 2: Validating a New Test Against a Hierarchical CRS
Objective: To assess the accuracy of a new diagnostic test for a complex disease by comparing it to a validated, multi-level composite reference standard.
Materials:
- Patient population with and without symptoms
- Equipment for primary standard test (e.g., DSA machine)
- Equipment for secondary standard tests (e.g., CT/MRI, clinical exam tools)
- Defined treatment protocol (e.g., Triple H therapy)
Methodology (Adapted from [86]):
- Apply Primary Standard: All patients who received the primary reference test (e.g., DSA) are classified based on its results. This is the highest level of evidence.
- Apply Secondary Standard: Patients not tested by the primary standard are evaluated using secondary criteria (e.g., clinical sequelae and imaging evidence of delayed infarction). A patient meeting either criterion is classified as positive.
- Apply Tertiary Standard: Patients not classified in steps 1 or 2, but who received treatment, are evaluated based on their response-to-treatment. Improvement with therapy leads to a positive classification; no improvement with an alternative etiology identified leads to a negative classification.
- Compare New Test: The result of the new index test is compared against the final classification from the hierarchical CRS to calculate sensitivity, specificity, and predictive values.
Visualizations
Diagram 1: Hierarchical CRS Workflow
This diagram illustrates the sequential, multi-level process of a hierarchical composite reference standard for diagnosing a complex condition like vasospasm [86].
Diagram 2: Diagnostic Method Comparison
This diagram compares the diagnostic breadth and typical application flow of traditional microscopy versus modern multi-parallel qPCR [88] [18].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Advanced Parasitological Research
This table details key reagents and materials used in the development and application of sensitive diagnostic methods for parasitic infections.
| Item | Function | Example Application |
|---|---|---|
| Precellys Soil Grinding Tubes | Homogenize and preserve stool samples for molecular analysis without the need for fixatives, preserving nucleic acid integrity [88]. | Sample preparation for multi-parallel qPCR [88]. |
| Multi-parallel qPCR Assays | Simultaneously detect and quantify DNA from multiple parasitic pathogens in a single reaction, greatly expanding diagnostic breadth [88]. | Sensitive surveillance of STH and protozoan infections in post-MDA settings [88]. |
| Functionalized Nanomaterials | Enhance signal detection in biosensors. Includes gold nanoparticles (AuNPs), quantum dots (QDs), and carbon nanotubes (CNTs) [18]. | Developing highly sensitive point-of-care nanobiosensors for parasite antigens or genetic material [18]. |
| Albendazole | A broad-spectrum anthelmintic drug used for mass drug administration (MDA) and as a positive control in therapeutic efficacy studies [88]. | Treatment and worm expulsion studies to validate diagnostic intensity measurements [88]. |
Cost-Effectiveness and Operational Feasibility for Large-Scale Implementation
Accurate diagnosis is the cornerstone of effective parasitic disease control and research. In low-intensity infection settings—a critical focus as control programs successfully reduce transmission—conventional diagnostic methods face significant sensitivity limitations. This creates an operational challenge for large-scale research and surveillance programs, where cost-effectiveness and feasibility are paramount. Microscopy, long considered the gold standard, shows markedly reduced sensitivity in low-transmission settings, with the widely used Kato-Katz method dropping to 53-80% sensitivity for certain soil-transmitted helminths in low-intensity environments [11]. This diagnostic gap necessitates strategic implementation of support infrastructures that can deliver technically sound, operationally feasible, and economically sustainable solutions to researchers working at the forefront of neglected tropical disease research.
Operational Framework for a Technical Support Center
A technical support center for diagnostic researchers must be structured to provide rapid, accurate, and accessible assistance. The following framework outlines the core operational components.
Foundational Best Practices for Research Support Operations
- Minimal Effort to Seek Help: Support contact options must be prominently displayed and easily accessible from multiple website locations, including headers, footers, and menus. Email addresses should link directly to new messages, and support hours should be clearly communicated for all contact channels [91].
- Prompt Issue Resolution: Response times must be minimized, with clear expectations set for resolution timelines. Automated responses should specify when a researcher can expect a detailed follow-up, and support tickets should be handled within defined, reasonable timeframes [91].
- Multi-channel Support: Researchers should be able to contact support through their preferred channel, including email, phone, web portal, and chat. This ensures accessibility for diverse research environments with varying connectivity and resource constraints [92].
Self-Service Knowledge Infrastructure
A comprehensive self-service portal significantly enhances operational feasibility by empowering researchers to resolve common issues independently, reducing support ticket volume by deflecting repetitive inquiries [93].
Table 1: Self-Service Knowledge Base Components
| Component | Function | Research Application |
|---|---|---|
| Troubleshooting Guides | Step-by-step protocols for common diagnostic issues | Addressing false negatives in low-parasite-density samples |
| FAQ Pages | Rapid answers to frequently encountered problems | Optimizing specimen preservation for molecular assays |
| Interactive Workflows | Guided pathways for complex diagnostic procedures | Bayesian latent class analysis for test validation [11] |
| Knowledge Base Software | Centralized repository for all support resources | Platforms like ProProfs or Zendesk for content management [94] |
Support Team Composition and Expertise
Specialized help desk groups should be established to address distinct research domains [92]. For parasitic diagnostics, this includes:
- Molecular Diagnostics Group: Expertise in PCR, LAMP, and other amplification techniques
- Microscopy Support Group: Proficiency in stool examination, blood smear preparation, and concentration methods
- Serology and Rapid Test Group: Knowledge of immunochromatographic assays and serological interpretation
- Data Analysis Group: Assistance with statistical analysis of diagnostic performance, including sensitivity/specificity calculations
Diagnostic Methods: Performance and Cost Considerations
Selecting appropriate diagnostic methods requires balancing technical performance with operational feasibility for large-scale implementation.
Comparative Diagnostic Performance
Table 2: Sensitivity of Diagnostic Methods for Soil-Transmitted Helminths [11]
| Diagnostic Method | Overall Sensitivity (%) | High Intensity Setting | Low Intensity Setting |
|---|---|---|---|
| FLOTAC | 92.7 | Highest performance | Highest performance |
| Kato-Katz (double slide) | 74.0-95.0* | Good performance | Reduced (53-80%) |
| Mini-FLOTAC | Comparable to Kato-Katz | Comparable to Kato-Katz | Comparable to Kato-Katz |
| Direct Microscopy | 42.8 | Low performance | Low performance |
| Formol-Ether Concentration | Intermediate | Intermediate | Intermediate |
*Range represents performance across Ascaris lumbricoides, Trichuris trichiura, and hookworms
Diagnostic Protocols for Low-Intensity Infections
Enhanced Stool Examination Protocol
For comprehensive detection of soil-transmitted helminths in low-intensity settings:
- Sample Collection: Collect three stool samples on separate days to improve detection sensitivity [95]
- Preservation: Place specimens in special containers with preservative fluid immediately after collection; if unavailable, refrigerate (do not freeze) until examination
- Processing: Utilize the FLOTAC method with specific gravity adjustments for different parasite species
- Examination: Systematic microscopic examination of multiple fields; consider duplicate slides
- Quantification: Count eggs and calculate eggs per gram (EPG) for infection intensity assessment
- Quality Control: Have a second trained technician review a subset of slides (minimum 10%)
This multi-sample approach addresses the day-to-day variation in parasite egg excretion that significantly impacts sensitivity in low-intensity infections [95].
Serological Testing Protocol for Protozoan Infections
For serological diagnosis of parasitic infections like Chagas disease and toxoplasmosis:
- Sample Collection: Collect blood sample in appropriate vacutainer tubes
- Serum Separation: Centrifuge and aliquot serum using standard protocols
- Initial Screening: Perform first serological test (ELISA or rapid diagnostic test)
- Confirmatory Testing: Conduct a second, different serological test for positive results
- Interpretation: Require positive results on at least two different tests for definitive diagnosis [96]
This algorithm is particularly important for chronic infections where parasite load is minimal and direct detection methods have limited utility.
Molecular Diagnostics Implementation
While molecular methods like PCR offer superior sensitivity, their cost and technical requirements present feasibility challenges for large-scale field implementation. A tiered approach is recommended:
- Initial Screening: Use cost-effective methods like Kato-Katz or mini-FLOTAC
- Confirmatory Testing: Apply multiplex PCR for discordant or suspicious cases
- Quality Assurance: Use molecular methods to validate traditional diagnostics in a subset of samples
This balanced approach maintains cost-effectiveness while improving overall diagnostic accuracy.
Visualizing the Diagnostic Support Workflow
The following workflow diagram illustrates the integrated support pathway for researchers diagnosing low-intensity parasitic infections:
Diagram 1: Diagnostic Support Workflow for Researchers
Research Reagent Solutions for Enhanced Sensitivity
Table 3: Essential Research Reagents for Low-Intensity Infection Diagnostics
| Reagent/Kit | Primary Function | Application in Sensitivity Improvement |
|---|---|---|
| FLOTAC Reagents | High-sensitivity flotation solutions for parasite concentration | Increases egg recovery rate from stool samples compared to conventional methods [11] |
| DNA Extraction Kits | Nucleic acid purification from diverse sample types | Enables molecular detection of low parasite loads undetectable by microscopy |
| Multiplex PCR Master Mixes | Simultaneous detection of multiple parasites in single reaction | Reduces sample volume requirements and processing time for comprehensive screening |
| Immunochromatographic Strips | Rapid antigen detection at point-of-care | Provides quick screening in field settings with reasonable sensitivity |
| Preservation Buffers | Stabilizes nucleic acids in clinical samples | Maintains target integrity during transport from remote collection sites |
| Bayesian Latent Class Analysis Software | Statistical analysis without perfect reference standard | More accurate estimation of true test performance in absence of gold standard [11] |
Cost-Benefit Analysis of Support Infrastructure
Implementing a technical support center requires careful consideration of both direct costs and long-term benefits for research programs.
Implementation Cost Drivers
- Staffing and Training: Technical experts require competitive compensation and ongoing training, representing approximately 60-70% of total operational costs [91]
- Diagnostic Equipment: FLOTAC apparatus, microscopes, and molecular biology equipment constitute major capital investments
- Reagent Costs: Consumables for high-sensitivity methods typically cost 2-3 times more than conventional diagnostics
- Knowledge Management Systems: Commercial FAQ and knowledge base software ranges from free basic plans to enterprise solutions exceeding $200/month [94]
Economic Benefits and Efficiencies
- Reduced Diagnostic Errors: Improved sensitivity decreases false negatives, enhancing research validity and preventing costly study repetitions
- Accelerated Research Timelines: Rapid troubleshooting minimizes project delays, accelerating publication and intervention development
- Standardized Methodologies: Consistent application of optimized protocols improves inter-study comparability and data pooling capabilities
- Training Efficiency: Centralized knowledge resources reduce repetitive training demands for new research staff
For large-scale research programs focused on low-intensity parasitic infections, a strategically implemented technical support infrastructure delivers significant operational advantages. The most cost-effective approach combines:
- Tiered Diagnostic Protocols: Matching method sensitivity to program phase, using cost-effective screening with targeted high-sensitivity confirmation
- Robust Self-Service Systems: Comprehensive knowledge bases that address common technical challenges before requiring direct support intervention
- Specialized Support Teams: Technical experts organized by diagnostic modality to provide precise, efficient troubleshooting
- Continuous Improvement Cycles: Regular analysis of support metrics and diagnostic outcomes to refine both support services and laboratory methods
This integrated approach maximizes diagnostic sensitivity within operational constraints, ultimately enhancing research quality and accelerating progress toward elimination targets for neglected parasitic diseases.
Conclusion
The fight against parasitic diseases is increasingly becoming a battle against low-intensity, hidden infections that evade conventional diagnostics. The synthesis of advancements presented here—from the refined one-step FECT to field-deployable molecular platforms like LAMP and AI-driven image analysis—demonstrates a clear path forward. These tools are not merely incremental improvements but represent a paradigm shift towards the level of sensitivity required for effective surveillance and elimination. Future efforts must focus on integrating these technologies into public health systems, making them affordable and accessible in endemic regions. For researchers and drug developers, this evolving diagnostic landscape underscores the need for companion diagnostics in clinical trials and the importance of accurately measuring drug efficacy against the entire parasite reservoir, including subpatent infections. Ultimately, closing the diagnostic sensitivity gap is the cornerstone for achieving and sustaining the elimination of parasitic diseases of poverty.
References
- 1. The temporal dynamics and infectiousness of subpatent Plasmodium falciparum infections in relation to parasite density | Nature Communications [https://www.nature.com/articles/s41467-019-09441-1]
- 2. The temporal dynamics and infectiousness of subpatent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6440965/]
- 3. Low-density Plasmodium falciparum infection: "Even a ... [https://pubmed.ncbi.nlm.nih.gov/39986449/]
- 4. High Levels of Asymptomatic and Subpatent Plasmodium falciparum Parasite Carriage at Health Facilities in an Area of Heterogeneous Malaria Transmission Intensity in the Kenyan Highlands - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4257630/]
- 5. Lower Microscopy Sensitivity with Decreasing Malaria ... [https://wwwnc.cdc.gov/eid/article/30/9/24-0378_article]
- 6. Impact of asymptomatic infections on malaria transmission ... [https://www.sciencedirect.com/science/article/pii/S2468042725000715]
- 7. Low Parasitemia in Submicroscopic Infections Significantly ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0121763]
- 8. Comparison of three diagnostic methods (microscopy, RDT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6142353/]
- 9. Repeated sampling improved the sensitivity of malaria ... [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-020-05359-w]
- 10. A cross-sectional survey of Plasmodium falciparum and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581485/]
- 11. Sensitivity of diagnostic tests for human soil-transmitted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4186778/]
- 12. Sensitivity Analysis of a Transmission Interruption Model ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.841883/full]
- 13. An Epidemiological Survey of Intestinal Parasitic Infection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10055958/]
- 14. Diagnosis of Parasitic Infections: What's Going On? [https://www.sciencedirect.com/science/article/pii/S2472555222071696]
- 15. Parameter estimation and sensitivity analysis in an agent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2789658/]
- 16. Parasitic diagnosis: A journey from basic microscopy to cutting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617590/]
- 17. Recent advancements in the diagnosis of parasitic diseases [https://www.sciencedirect.com/science/article/abs/pii/S0166685125000428]
- 18. Nanobiosensors for revolutionizing parasitic infections diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12168311/]
- 19. Artificial intelligence in parasitic disease control: A paradigm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10911181/]
- 20. Early detection of emerging infectious diseases [https://www.sciencedirect.com/science/article/pii/S0264410X23006308]
- 21. How Silent Infections Can Destroy Your Health Without ... [https://hsenations.com/silent-infections-can-destroy-your-health/]
- 22. Invisible epidemics: ethics and asymptomatic infection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7738616/]
- 23. A comparative study with conventional copromicroscopy [https://www.sciencedirect.com/science/article/pii/S240567312500042X]
- 24. 5 Steps to Troubleshooting That Will Fix Just About Anything [https://limblecmms.com/learn/maintenance-operations/troubleshooting/]
- 25. Use a Troubleshooting Methodology for More Efficient IT ... [https://www.comptia.org/en-us/blog/use-a-troubleshooting-methodology-for-more-efficient-it-support/]
- 26. 4 steps to troubleshooting (almost) any IT issue [https://www.spiceworks.com/it-articles/troubleshooting-steps/]
- 27. Effective Laboratory Diagnosis of Parasitic Infections of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11475984/]
- 28. Development of a rapid malaria LAMP-MS assay for ... [https://www.nature.com/articles/s41598-025-92935-4]
- 29. Optimization of loop-mediated isothermal amplification ... [https://www.nature.com/articles/s41598-024-72228-y]
- 30. Optimization of a loop-mediated isothermal amplification ... [https://www.sciencedirect.com/science/article/pii/S1056617124001119]
- 31. Validation and optimization of the loop-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10997836/]
- 32. Recent advances in loop-mediated isothermal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9325740/]
- 33. Estimating sensitivity of the Kato-Katz technique for the ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0005953]
- 34. AI-supported versus manual microscopy of Kato-Katz ... [https://www.nature.com/articles/s41598-025-07309-7]
- 35. Comparative Evaluation of Deep Learning Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943284/]
- 36. Performance validation of deep-learning-based approach ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06878-w]
- 37. Recognition of parasitic helminth eggs via a deep learning- ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1485001/full]
- 38. An artificial intelligence-based approach for human ... [https://www.sciencedirect.com/science/article/pii/S2772442525000516]
- 39. Multiplex bead assays enable integrated serological ... [https://www.nature.com/articles/s41467-025-62305-9]
- 40. Challenges and Approaches to Establishing Multi-Pathogen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11542533/]
- 41. The Four Most Common Problems in Multiplex pcr Design [https://www.dnasoftware.com/common-problems-in-multiplex-panel-design/]
- 42. Application of a Multiplex Quantitative PCR to Assess ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4731196/]
- 43. Lower Microscopy Sensitivity with Decreasing Malaria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11346994/]
- 44. Sensitive near point-of-care detection of asymptomatic and ... [https://www.nature.com/articles/s41467-025-64027-4]
- 45. Optimization of Case Definitions for Sensitivity as a ... [https://www.mdpi.com/2075-4418/11/11/2079]
- 46. Framework for Evaluating Public Health Surveillance ... [https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5305a1.htm]
- 47. Nanobiosensors for revolutionizing parasitic infections diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02685-2]
- 48. Unravelling 'low-resource settings': a systematic scoping ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8183220/]
- 49. The Role of Implementation Science in Advancing Resource ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7970459/]
- 50. The increased sensitivity of qPCR in comparison to Kato ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7315547/]
- 51. The effects of RT-qPCR standards on reproducibility and ... [https://www.nature.com/articles/s41598-024-77155-6]
- 52. How qPCR complements the WHO roadmap (2021–2030) ... [https://www.sciencedirect.com/science/article/abs/pii/S1471492221000854]
- 53. MIQE Guidelines | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/why-choose-taqman-assays/publish-real-time-pcr-results.html]
- 54. qPCR and qRT-PCR analysis: Regulatory points to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7786041/]
- 55. qPCR Troubleshooting Guide [https://azurebiosystems.com/qpcr-resources/troubleshooting/]
- 56. Ten Tips for Successful qPCR - Behind the Bench [https://www.thermofisher.com/blog/behindthebench/ten-tips-for-successful-qpcr/]
- 57. Development and validation of a high-throughput qPCR ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0012760]
- 58. Troubleshooting qPCR: Interpreting Amplification Curves [https://blog.biosearchtech.com/thebiosearchtechblog/bid/63622/qpcr-troubleshooting]
- 59. qPCR Troubleshooting: How to Ensure Successful ... [https://dispendix.com/blog/qpcr-troubleshooting]
- 60. A comparative analysis of preservation techniques for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5773002/]
- 61. Troubleshooting Guide for Genomic DNA Extraction & ... [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/troubleshooting-guide-for-t3010?srsltid=AfmBOoouJEVneFGJn48wfrabIbX3sJv0TcKn4BrOIzzzA2wW3DxZnGLd]
- 62. A historical review of the techniques of recovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7269538/]
- 63. A Modified Sample Preparation Protocol for High-Efficiency ... [https://www.mdpi.com/2072-666X/16/8/847]
- 64. Rethinking Lab Workflow Optimization [https://www.labkey.com/lab-workflow-optimization/]
- 65. Workflow optimization mastery: top strategies for tech- ... [https://blog.superhuman.com/workflow-optimization/]
- 66. Diagnostic performance of ELISA kits and expanded ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12557959/]
- 67. Advances in DNA Extraction: Methods, Improvement and ... [https://www.cd-genomics.com/blog/dna-extraction-methods-optimization-troubleshooting/]
- 68. New global assessment reveals persistent barriers in ... [https://ippsecretariat.org/news/2025-diagnostics-gap-assessment/]
- 69. The need for new test verification and regulatory support for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9007716/]
- 70. Emerging Trends in Point-of-Care Technology Development ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312415/]
- 71. Comparison of Three Methods for Diagnosis of Cutaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3279850/]
- 72. Comparison of conventional and non-invasive diagnostic tools ... [https://idpjournal.biomedcentral.com/articles/10.1186/s40249-021-00859-8]
- 73. A comparative study of traditional and molecular diagnostic ... [https://www.sciencedirect.com/science/article/pii/S0163445324002585]
- 74. PCR Troubleshooting and Optimization: The Essential Guide [https://www.caister.com/pcr-troubleshooting]
- 75. A guideline for reporting experimental protocols in life sciences [https://pmc.ncbi.nlm.nih.gov/articles/PMC5978404/]
- 76. RDT performance through high-throughput bead-based ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1598280/full]
- 77. Chapter 7 - Sensitivity and Limit of Detection [https://www.sciencedirect.com/science/chapter/bookseries/pii/S092234870870220X]
- 78. The difference between sensitivity and detection range in ... [https://www.bosterbio.com/blog/post/the-difference-between-sensitivity-and-the-minimum-level-of-assay-range-in-elisa-testing?srsltid=AfmBOoryNdeDiVEghAOCFxhmPkkEm1h3QIM6deywwrmpElnJzfst7V21]
- 79. Methods to determine limit of detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496743/]
- 80. Limit of Detection and Limit of Quantification Determination ... [https://www.intechopen.com/chapters/46058]
- 81. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 82. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 83. Molecular Diagnostics - Part 5: Analytical Sensitivity and ... [https://blog.seracare.com/molecular-serology-blog/verification-part5]
- 84. Analytical Sensitivity [https://www.apsnet.org/DAVN/Tools/Calculators/Pages/Analytical-Sensitivity.aspx]
- 85. Sensitivity and Specificity: A Complete Guide [https://www.datacamp.com/tutorial/sensitivity-specificity-complete-guide]
- 86. Developing a New Reference Standard… Is Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2919497/]
- 87. Bias due to composite reference standards in diagnostic ... [https://pubmed.ncbi.nlm.nih.gov/26555849/]
- 88. Multi-parallel qPCR provides increased sensitivity and ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-016-1314-y]
- 89. Diagnostic research in the absence of a gold standard [https://www.semanticscholar.org/paper/Diagnostic-research-in-the-absence-of-a-gold-Smeden/a7b5782ce4b27c0603353e1629c04b8c71a8897e]
- 90. Rapid diagnosis of parasitic diseases: current scenario and ... [https://www.sciencedirect.com/science/article/pii/S1198743X18303951]
- 91. 8 Tech Support Best Practices [https://www.eiresystems.com/8-tech-support-best-practices/]
- 92. Top 17 Help Desk Best Practices for 2025 [https://www.desk365.io/blog/help-desk-best-practices/]
- 93. 6 tips for building a thriving help center [https://www.zendesk.com/blog/6-tips-for-building-a-thriving-help-center/]
- 94. 16 Best FAQ Software & Tools in 2025 to Create FAQ [https://www.proprofskb.com/blog/best-faq-software/]
- 95. Diagnosis of Parasitic Diseases [https://www.cdc.gov/parasites/testing-diagnosis/index.html]
- 96. Neglected Parasitic Infections: What Family Physicians ... [https://www.aafp.org/pubs/afp/issues/2021/0900/p277.html]