Beyond the Microscope: A Comprehensive Framework for Validating Molecular Assays Against Microscopy Gold Standards
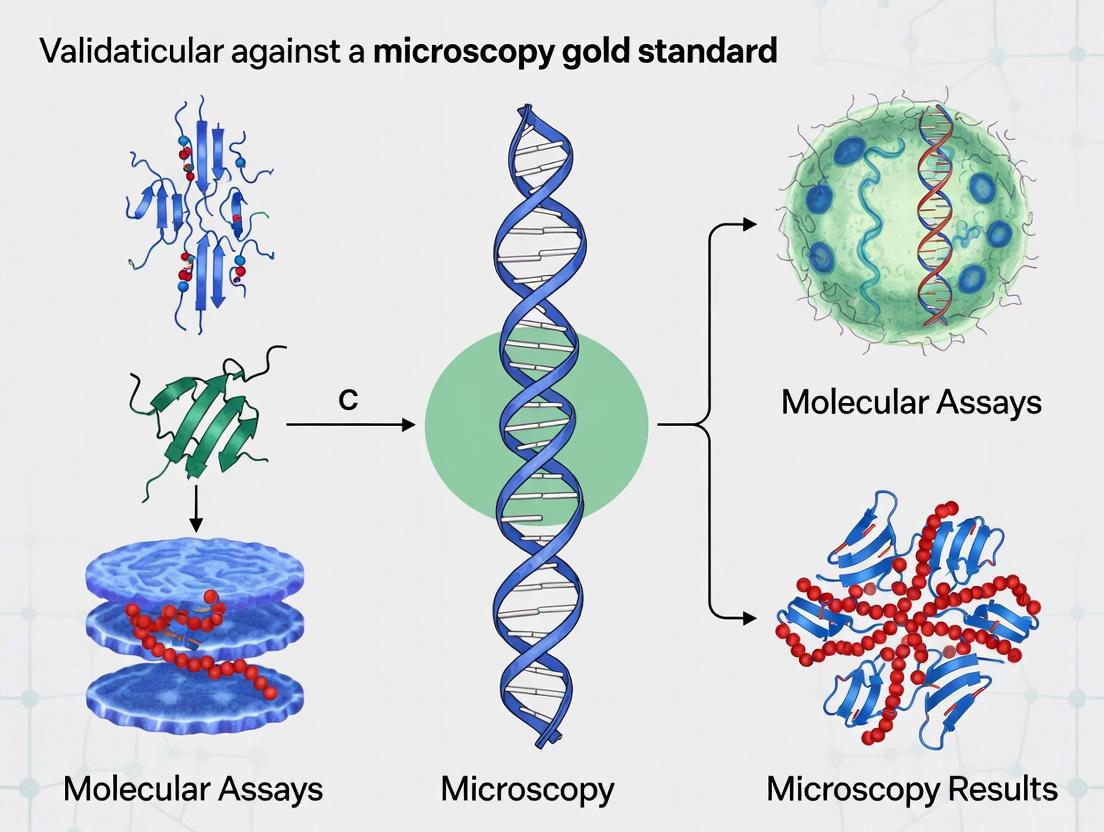
This article provides researchers, scientists, and drug development professionals with a structured guide for the analytical validation of molecular diagnostic tests against traditional microscopy.
Beyond the Microscope: A Comprehensive Framework for Validating Molecular Assays Against Microscopy Gold Standards
Abstract
This article provides researchers, scientists, and drug development professionals with a structured guide for the analytical validation of molecular diagnostic tests against traditional microscopy. It explores the foundational principles of validation, detailing specific methodological applications across diseases like malaria and leprosy. The content offers practical troubleshooting strategies for common assay challenges and establishes a rigorous framework for conducting comparative studies to demonstrate non-inferiority, equivalence, or superiority. By synthesizing current standards and real-world case studies, this resource aims to ensure that novel molecular methods meet the required diagnostic performance for clinical and research implementation.
The Why and What: Core Principles of Validation and the Established Gold Standard
Validation is the foundational process of establishing documented, scientific evidence that a diagnostic method reliably performs as intended for its specific purpose. In the context of medical diagnostics, this process ensures that assays and tests provide accurate, reproducible results that can be trusted to inform clinical decision-making. For diagnostic methods targeting infectious diseases like malaria and SARS-CoV-2, validation typically involves comparing new molecular assays against established reference methods, often referred to as "gold standards" [1]. For many infectious diseases, particularly in resource-limited settings, microscopy remains the benchmark against which newer technologies are measured [2]. However, the validation process must account for the limitations of even these established methods, as the choice of an inappropriate gold standard can significantly distort diagnostic outcomes [3].
This guide objectively compares the performance of various diagnostic platforms, focusing specifically on molecular assays validated against microscopy gold standards, to provide researchers and drug development professionals with evidence-based insights for selecting appropriate diagnostic tools.
Gold Standard Comparison: Microscopy Versus Molecular Methods
Performance Characteristics Across Diagnostic Platforms
Table 1: Comparative performance of diagnostic methods for infectious diseases
| Diagnostic Method | Target Pathogen | Sensitivity (%) | Specificity (%) | Agreement with Gold Standard | Limit of Detection |
|---|---|---|---|---|---|
| Microscopy (Gold Standard) | Plasmodium falciparum | 100 (Reference) | 100 (Reference) | N/A | 11-50 parasites/μL [2] |
| 18S qPCR | Plasmodium falciparum | 100 | 100 | Excellent (ICC: 0.97) [2] | 22 parasites/mL [2] |
| EasyNAT Malaria Assay | Plasmodium spp. | 100 | 97.5 | 96.3% congruency with LAMP [4] | Correlates with parasitemia [4] |
| Alethia Malaria LAMP Assay | Plasmodium spp. | 97.8 | 98.3 | 96.3% congruency with EasyNAT [4] | Not specified |
| Aptima SARS-CoV-2 Assay | SARS-CoV-2 | 100 | 100 | 97.6% with LDT-Fusion [5] | Not specified |
| LDT-Fusion SARS-CoV-2 Assay | SARS-CoV-2 | 100 | 100 | 97.6% with Aptima [5] | Not specified |
| R-GENE SARS-CoV-2 Assay | SARS-CoV-2 | 98.2 | 100 | 98.8% with Aptima & LDT-Fusion [5] | Not specified |
| IntelliPlex Lung Cancer Panel DNA | Lung cancer biomarkers | 97.73 | 100 | 98% with NGS [6] | 5% VAF [6] |
| IntelliPlex Lung Cancer Panel RNA | Lung cancer biomarkers | 100 | 100 | 100% with NGS [6] | Not specified |
Workflow Efficiency and Operational Characteristics
Table 2: Operational characteristics of diagnostic platforms
| Diagnostic Method/Platform | Hands-on Time (minutes) | Total Turnaround Time | Throughput | Automation Level |
|---|---|---|---|---|
| Microscopy | Significant (varies) | 30-60 minutes (expert dependent) | Low | Manual |
| Aptima SARS-CoV-2 (Panther) | 24 | Moderate | High | Fully automated, random-access [5] |
| LDT-Fusion SARS-CoV-2 | 25 | Moderate | High | Fully automated, random-access [5] |
| R-GENE SARS-CoV-2 | 71 | Long | Moderate | Manual processing [5] |
| NeuMoDx SARS-CoV-2 | Low (not specified) | Short | Highest | Fully automated [7] |
| DiaSorin Simplexa SARS-CoV-2 | Low (not specified) | Moderate | Moderate | Simplified workflow [7] |
| IntelliPlex Lung Cancer Panel | Not specified | Faster than NGS | High for targeted genes | Multiplexed detection [6] |
| 18S qPCR | Moderate (DNA extraction required) | Several hours | Moderate | Semi-automated [2] |
Experimental Protocols and Validation Methodologies
Protocol for Microscopy and Molecular Method Comparison
The following workflow represents a standardized approach for validating molecular diagnostic methods against microscopy gold standards:
Sample Collection and Preparation: For malaria studies, blood samples are collected in EDTA tubes, with thick and thin blood films prepared immediately. Thick films are used for parasite detection, while thin films allow for species identification [2]. For SARS-CoV-2 detection, nasopharyngeal swabs are collected in viral transport medium [5]. Nucleic acid extraction is performed using commercial kits such as the QIAamp DNA Blood Mini Kit for malaria [2] or system-specific protocols for automated platforms [5].
Microscopy Protocol: Experienced microscopists examine blood films following standardized WHO protocols. In malaria diagnostics, technicians count asexual parasites against 200 white blood cells (WBCs) in thick films. If the parasite count is less than 10 after examining 200 WBCs, counting continues up to 500 WBCs. Thin films are utilized when parasite density exceeds 250 parasites per 50 WBCs [2]. Parasitemia is calculated using the formula: (number of parasites counted / number of WBCs counted) × WBC count per μL [2].
Molecular Analysis Protocol: For 18S qPCR malaria detection, DNA is extracted from 200μL of packed RBCs. The Plasmodium-specific qPCR uses primers and probes targeting the 18S rRNA gene with a detection limit of approximately 22 parasites/mL. Samples are run in triplicate, with cycle threshold values greater than 50 considered non-detectable [2]. For SARS-CoV-2 detection, the Aptima assay uses transcription-mediated amplification (TMA) targeting two sequences on the ORF1ab gene, while the LDT-Fusion assay uses real-time RT-PCR targeting the RdRP gene [5].
Statistical Analysis: Concordance between methods is assessed using multiple statistical approaches. The intraclass correlation coefficient (ICC) measures consistency between quantitative measurements [2]. Passing-Bablok regression detects systematic and proportional biases [2]. Positive percent agreement (PPA) and negative percent agreement (NPA) are calculated against the consensus result, which is typically defined as agreement between at least two of three methods [5].
Validation Study Designs for Digital Microscopy
The transition from light microscopy to digital microscopy requires rigorous validation to ensure diagnostic accuracy is maintained. Several study designs have been employed:
Diagnostic Concordance Studies: These studies measure the agreement between diagnoses made using light microscopy versus digital whole-slide images. Multiple pathologists review cases using both modalities in randomized order, with washout periods between viewings to prevent recall bias [1].
Non-inferiority Designs: These studies test whether digital microscopy is not substantially worse than light microscopy by a predetermined margin. This approach is particularly relevant when implementing new technology where maintaining diagnostic accuracy is crucial [1].
Special Application Validations: Separate validation is recommended for different pathology applications, including routine histology with H&E staining, immunohistochemistry, and cytology specimens. Each application may require different scanning parameters and validation approaches [1].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key reagents and materials for diagnostic validation studies
| Reagent/Material | Application | Function in Experiment |
|---|---|---|
| Viral Transport Medium (VTM) | SARS-CoV-2 detection | Preserves viral integrity during transport and storage [5] |
| QIAamp DNA Blood Mini Kit | Malaria parasite DNA extraction | Extracts and purifies parasite DNA from whole blood [2] |
| EasyMAG Extraction System | Nucleic acid extraction | Automated extraction for SARS-CoV-2 RNA [5] |
| Primer/Probe Sets (18S rRNA) | Malaria qPCR | Amplifies and detects Plasmodium-specific DNA sequences [2] |
| πCODE MicroDiscs | IntelliPlex Lung Cancer Panel | Multiplexed detection of DNA/RNA targets through unique barcodes [6] |
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissue | Oncology biomarker detection | Preserves tissue architecture and biomolecules for analysis [6] |
| OncoSpan gDNA Reference Standard | Assay validation | Provides standardized control for limit of detection studies [6] |
| Positive and Negative Control Materials | Quality assurance | Verifies assay performance and identifies contamination [5] [2] |
Analysis of Validation Data and Interpretation
Statistical Approaches for Method Comparison
Validation studies employ multiple statistical methods to comprehensively evaluate agreement between methods. In malaria diagnostics, the high ICC value of 0.97 between microscopy and 18S qPCR indicates excellent consistency in measuring parasitemia levels [2]. The minimal mean difference of 0.04 log10 units/mL between methods demonstrated through paired t-tests provides evidence that 18S qPCR does not systematically over- or under-estimate parasitemia compared to microscopy [2].
Passing-Bablok regression is particularly valuable for detecting systematic biases that might not be apparent through simple correlation analysis. This method is robust to the distribution of measurements and can identify both constant and proportional differences between methods [2]. In the case of malaria diagnostics, the absence of significant systematic or proportional bias reinforces the suitability of 18S qPCR as a quantitative method comparable to microscopy [2].
Impact of Gold Standard Selection on Validation Outcomes
The choice of an appropriate gold standard significantly influences validation outcomes. A study comparing microscopy and radiography for dental caries diagnosis demonstrated that using an observer's scores from the radiographs being evaluated as validation, rather than the true gold standard (microscopy), produced misleading results. Accuracy measures were significantly higher when using an observer as the 'gold standard' compared to microscopy, and compressed, degraded images paradoxically appeared more accurate than originals when using observer validation [3]. This highlights the critical importance of selecting a biologically accurate reference method rather than relying on comparative human interpretation.
Throughput and Workflow Considerations
Beyond analytical performance, practical considerations significantly impact the utility of diagnostic methods in various settings. Automated, random-access systems like the Panther platform for SARS-CoV-2 testing offer substantially reduced hands-on time (24-25 minutes) compared to manual platforms (71 minutes for R-GENE) [5]. This efficiency becomes particularly crucial during high-prevalence periods when testing demand surges. Similarly, the NeuMoDx system demonstrates the shortest turnaround time among SARS-CoV-2 testing platforms, a critical factor for timely clinical decision-making [7].
The validation of diagnostic methods against established gold standards remains essential for ensuring reliable patient care. While microscopy maintains its position as a valuable reference method for numerous infectious diseases, molecular assays increasingly demonstrate equivalent or superior performance characteristics with enhanced throughput and efficiency. The validation process must employ appropriate statistical methods and study designs to provide meaningful comparisons, while considering the practical requirements of different healthcare settings. As diagnostic technologies continue to evolve, rigorous validation ensuring "fitness for purpose" will remain the cornerstone of reliable laboratory medicine.
The Role of Microscopy as a Historical and Clinical Gold Standard
For over 150 years, light microscopy has served as the foundational tool for pathological diagnosis, establishing itself as the historical and clinical gold standard against which all newer diagnostic technologies are measured [8]. The origin of microscopy was a gradual journey, with one of the earliest advancements being the invention of spectacles in 13th century Florence [8]. The development of the first compound microscope between 1590 and 1610, credited to Galileo Galilei in 1610 (who called it "occhialino") though Dutch spectacle makers Hans and Zacharias Janssen had reportedly used telescope lenses to enlarge small objects as early as 1590, marked the beginning of microscopic visualization of biological structures [8]. This revolutionary technology enabled Rudolf Virchow in the mid-19th century to integrate microscopy into autopsy studies, transforming pathology into a scientific field and cornerstone of modern medicine [8].
The advancement of pathology required complementary breakthroughs beyond microscopy itself. The introduction of the microtone in the 1830s enabled precise tissue sectioning, while paraffin embedding (introduced by Edward Klebs in 1869) and formalin fixation (by Ferdinand Blum in 1893) standardized tissue processing [8]. Most significantly, Franz Böhm's hematoxylin staining in 1865, combined with eosin staining, created hematoxylin and eosin (H&E) staining that remains a diagnostic gold standard today for its exceptional clarity, cost-efficiency, and wide applicability [8]. For over a century, this combination of microscopy and H&E staining has enabled pathologists to assess cellular-level alterations, providing critical insights for diagnosis and prognosis across countless disease states.
However, the limitations of traditional microscopy—including its susceptibility to human error, inter-observer variability, low throughput, and challenges with remote collaboration—have prompted the development of sophisticated molecular alternatives [8]. This guide objectively examines how modern molecular assays are validated against the microscopic gold standard, exploring their complementary roles in contemporary diagnostic practice and research.
Clinical Applications: Traditional Microscopy Versus Molecular Assays
Vaginitis Diagnostics
The diagnostic challenge of vaginitis perfectly illustrates the ongoing transition from microscopy to molecular methods in clinical practice. Historically, vaginitis has been diagnosed using microscopy for vulvovaginal candidiasis (CV) and Trichomonas vaginalis (TV), and Amsel's criteria or Nugent scoring (which involves Gram staining) for bacterial vaginosis (BV) [9]. The ability for rapid diagnosis by provider-performed wet-mount microscopy highlights the importance of treating these infections timely due to sequelae, loss to follow-up, and stigma [9]. However, these traditional methods lack sensitivity and specificity, as some vaginal infections mimic each other, and asymptomatic infections can lead to negative health outcomes [9].
Molecular nucleic acid amplification tests (NAATs) represent a significant advancement. A recent clinical evaluation of the Hologic Panther Aptima BV and CV/TV assays demonstrates their performance compared to conventional methods [9].
Table 1: Performance Comparison of Vaginitis Diagnostic Methods
| Diagnostic Method | Condition | Sensitivity (%) | Specificity (%) | Turnaround Time | Key Limitations |
|---|---|---|---|---|---|
| Wet Mount Microscopy | Trichomonas vaginalis | Low (method-dependent) | High | Minutes | Requires living organisms; low sensitivity |
| Nugent Scoring (Gram Stain) | Bacterial Vaginosis | 97.5 | 96.3 | Hours | Subjective; intermediate results challenging |
| Amsel's Criteria | Bacterial Vaginosis | Variable | Variable | Minutes | Lacks standardized interpretation |
| Hologic Panther Aptima BV Assay | Bacterial Vaginosis | 97.5 | 96.3 | Hours | Higher cost; limited clinical significance data |
| Hologic Panther Aptima CV/TV Assay | Vulvovaginal Candidiasis | 100 | 83.5 (vs. Gram stain) | Hours | Cannot differentiate Candida species |
| Hologic Panther Aptima CV/TV Assay | Trichomonas vaginalis | 100 | 100 | Hours | Higher cost than microscopy |
The table reveals a crucial diagnostic tradeoff: while molecular assays demonstrate superior sensitivity—particularly important for TV where microscopy sensitivity is low due to the need to visualize living organisms—they come with higher costs and questions about clinical significance for conditions like BV and CV where mere presence/absence of organisms doesn't necessarily indicate clinical disease [9].
Renal Transplant Rejection Diagnostics
In renal transplant pathology, a fascinating discrepancy analysis comparing the Molecular Microscope Diagnostic System (MMDx) with histology reveals critical insights about gold standard validation. Histology disagreed with MMDx in 37% of biopsies, including 315 clear discrepancies with therapeutic implications [10]. The patterns of disagreement were revealing: histology diagnoses of T cell-mediated rejection (TCMR) contained 14% MMDx antibody-mediated rejection (ABMR) and 20% MMDx no rejection [10].
Importantly, MMDx typically provided unambiguous diagnoses in cases with ambiguous histology (e.g., borderline and transplant glomerulopathy), and histology lesions associated with frequent discrepancies (tubulitis, arteritis, polyomavirus nephropathy) weren't associated with increased MMDx uncertainty [10]. This suggests molecular assessment can clarify biopsies with histologic ambiguity, though microscopy remains the foundational reference point.
Experimental Validation: Methodologies for Comparative Studies
Large-Scale Molecular-Histological Correlation
A groundbreaking 2025 study investigated correlations between nuclear features of healthy tissue cells and RNA expression patterns, providing an exemplary model for validating molecular findings against histological standards [11]. Based on 4,306 samples of 13 organs from the Genotype-Tissue Expression (GTEx) project, researchers constructed a deep learning-based automatic analysis framework to investigate geno-micro-correlations across tissues [11].
Experimental Protocol:
- Sample Preparation: H&E-stained whole slide images from GTEx database paired with RNA-Seq data [11]
- Parenchyma Extraction: Employed organ-specific methods including clustering-based approaches for breast tissue, RGB mean value thresholding for esophagus/colon/adrenal gland/pituitary/heart, and fine-tuned "Se-ResNext101" model for kidney glomeruli segmentation [11]
- Nucleus Segmentation: Implemented Efficient Deep Equilibrium Model for precise segmentation of nuclei across 13 organs [11]
- Feature Computation: Quantitative evaluation of nuclear morphological features [11]
- Molecular Correlation: Identification of gene sets specific to nuclear features and pathway analysis for biological significance [11]
This methodology demonstrates how modern validation studies leverage large-scale datasets and computational imaging to establish robust correlations between traditional histological phenotypes and molecular profiles.
Rapid Molecular Assay Development for Antimicrobial Resistance
The PathCrisp assay for detecting New Delhi metallo-beta-lactamase (NDM)-resistant infections exemplifies how novel molecular diagnostics are benchmarked against established methods [12].
Experimental Protocol:
- Assay Design: Combined loop-mediated isothermal amplification and CRISPR-based detection maintained at single temperature [12]
- Specificity Validation: Designed sgRNA and LAMP primers against conserved NDM regions using 122 isolate genomic sequences [12]
- Sensitivity Testing: Determined limit of detection using serial dilutions [12]
- Method Comparison: Tested 49 carbapenem-resistant enterobacteriaceae clinical isolates comparing PathCrisp with PCR-Sanger sequencing [12]
- Simplification: Implemented crude DNA extraction via heating rather than kit-based purification [12]
The PathCrisp assay demonstrated 100% concordance with PCR-Sanger sequencing while detecting as few as 700 NDM gene copies and providing results in approximately 2 hours [12]. This represents a significant advancement over conventional antibacterial susceptibility tests requiring 2-5 days [12].
The Evolving Diagnostic Toolkit: Integration Pathways
Digital Pathology and Computational Advances
The advent of digital pathology has created a bridge between traditional microscopy and modern computational analysis. By converting physical slides into high-resolution whole-slide images, digital pathology enables both remote expert consultation and implementation of artificial intelligence algorithms [8]. Several FDA-cleared AI systems now demonstrate this integration: Paige Prostate Detect showed 7.3% reduction in false negatives, while MSIntuit CRC triages colorectal cancer slides for microsatellite instability, prioritizing cases for confirmatory analyses [8].
Emerging technologies like Computational High-throughput Autofluorescence Microscopy by Pattern Illumination (CHAMP) promise to further transform histological imaging by enabling label-free, slide-free imaging of unprocessed tissues at 10 mm²/10 seconds with 1.1-µm resolution [13]. When combined with unsupervised learning (Deep-CHAMP), this approach can virtually stain tissue images within 15 seconds, potentially revolutionizing intraoperative assessment [13].
The Complementary Roles of Human and Digital Analysis
Rather than replacing human expertise, digital quantification complements pathological assessment. Each approach offers distinct advantages [14]:
Table 2: Pathologist Expertise vs. Software Quantification
| Aspect | Pathologist Scoring | Image Analysis Software |
|---|---|---|
| Strengths | Contextual interpretation, flexible adaptation to complexity, clinical relevance | Objective reproducible measurements, fine-grained quantification, high-throughput scalability |
| Limitations | Inter-observer variability, low data resolution, labor-intensive | Parameter sensitivity, difficulty handling artifacts, lack of biological context |
| Ideal Applications | Complex diagnoses, unusual findings, clinically validated scoring systems | Large-scale studies, subtle trend detection, quantitative biomarker analysis |
The integration of both approaches creates a powerful synergy—pathologists ensure biological relevance while software provides precise metrics, enabling improved accuracy through cross-validation [14].
Essential Research Reagent Solutions
The experimental protocols discussed utilize specific reagents and tools that constitute essential components of the modern pathology research toolkit:
Table 3: Essential Research Reagents and Tools
| Reagent/Tool | Function | Example Use Cases |
|---|---|---|
| H&E Staining | Provides foundational cellular contrast for histological assessment | Standard tissue examination across all organ systems [8] |
| Multi-Purpose LAMP Master Mix | Enables isothermal nucleic acid amplification without thermal cycler | PathCrisp assay for NDM detection [12] |
| CRISPR/Cas12a with sgRNA | Provides specific molecular detection through collateral trans-cleavage | NDM gene detection in PathCrisp assay [12] |
| DNeasy Blood & Tissue Kit | Extracts high-quality genomic DNA from diverse specimens | Preparation of samples for WGS in validation studies [12] |
| Efficient Deep Equilibrium Model | Segments nuclei in histology images with high accuracy | Nuclear feature extraction in GTEx study [11] |
| Cycle-Consistent GAN | Transforms label-free images into virtually stained counterparts | Deep-CHAMP for virtual H&E staining [13] |
Visualizing Diagnostic Workflows
Traditional Histopathology Workflow
Modern Molecular Validation Approach
Microscopy maintains its foundational role as the histological gold standard due to its extensive clinical validation, rich contextual information, and deep integration into medical practice and education. However, molecular assays are increasingly demonstrating complementary and, in specific applications, superior capabilities—particularly in sensitivity, objectivity, and throughput. The future of pathology lies not in replacement but in strategic integration, where microscopy provides the contextual framework and molecular methods contribute precise, quantitative data. This synergistic approach, enhanced by digital pathology and artificial intelligence, promises to advance both diagnostic accuracy and our fundamental understanding of disease mechanisms, ultimately benefiting researchers, clinicians, and patients through more precise and personalized healthcare interventions.
In the validation of molecular assays, demonstrating that a method is "fit-for-purpose" requires rigorous assessment of key performance parameters. When validating a new molecular method against an established gold standard like microscopy, understanding and quantifying specificity, sensitivity, precision, and accuracy is fundamental for researchers and drug development professionals. These parameters provide the statistical evidence that a new assay reliably detects the target analyte, delivers reproducible results, and agrees with established reference methods, ensuring confidence in data-driven decisions.
Defining the Key Validation Parameters
The following parameters form the foundation of assay validation, each providing distinct and complementary information about method performance.
| Parameter | Definition | What It Measures | Common Formulae |
|---|---|---|---|
| Specificity [15] [16] [17] | Ability to correctly identify the absence of a condition or analyte; measures true negatives. | How well the assay detects only the target analyte without interference from other components. | Specificity = True Negatives / (True Negatives + False Positives) |
| Sensitivity [15] [16] [17] | Ability to correctly identify the presence of a condition or analyte; measures true positives. | The lowest amount of analyte an assay can detect and/or reliably quantify. | Sensitivity = True Positives / (True Positives + False Negatives) |
| Precision [15] [18] [19] | The closeness of agreement between a series of measurements from multiple sampling of the same sample. | The random variation and reproducibility of the assay results under defined conditions. | Reported as % Relative Standard Deviation (%RSD) |
| Accuracy [15] [18] [16] | The closeness of agreement between a test result and an accepted reference or true value. | How close the measured value is to the true value, often expressed as percent recovery. | % Recovery = (Measured Value / True Value) x 100 |
Experimental Protocols for Parameter Assessment
Validating a new molecular assay against a gold standard requires a structured experimental approach. The protocols below outline key methodologies for generating the data needed to calculate these essential performance parameters.
Protocol for Specificity and Sensitivity Assessment
This experiment is designed to challenge the assay's ability to correctly identify true positives and true negatives, often using samples with known status determined by the gold standard method (e.g., microscopy).
- Sample Preparation: Obtain a panel of well-characterized samples. This should include samples confirmed positive for the target via the gold standard and samples confirmed negative. To test for cross-reactivity, include samples with potentially interfering substances that are structurally similar or commonly found in the sample matrix.
- Experimental Procedure: Process all samples through the new molecular assay using a blinded protocol so the operator is unaware of the known status. The results from the new assay (positive/negative) are then compared to the results from the gold standard test.
- Data Analysis: Construct a 2x2 contingency table to compare the outcomes. Calculate Sensitivity and Specificity using the formulae provided in the table above [17]. For a validation against microscopy, a high sensitivity is critical to ensure the molecular assay does not miss true positives identified by the gold standard.
Protocol for Precision Evaluation
Precision is evaluated at multiple levels to assess repeatability and intermediate precision, which is crucial for establishing the assay's reliability in a real-world laboratory setting [18].
- Sample Preparation: Prepare a homogeneous sample at a concentration within the quantitative range of the assay. Aliquots of this single sample are used for all precision testing.
- Experimental Procedure:
- Repeatability (Intra-assay): One analyst tests the multiple aliquots of the sample in a single run, using the same instrument and reagents [18]. The guidelines recommend a minimum of nine determinations across at least three concentration levels [15] [18].
- Intermediate Precision: A second analyst repeats the experiment on a different day, using a different instrument and preparing new reagents and standards [18]. This assesses the impact of normal, within-laboratory variations.
- Data Analysis: For each set of results (from Analyst 1 and Analyst 2), calculate the mean, standard deviation, and %RSD. The results from the two analysts can be subjected to statistical testing (e.g., Student's t-test) to determine if there is a significant difference in the mean values [18].
Protocol for Accuracy Determination
Accuracy is established by testing samples with known concentrations of the analyte and comparing the measured value to the expected value [15] [18].
- Sample Preparation: Prepare samples (in the appropriate matrix) spiked with known concentrations of the analyte. A minimum of nine determinations over three concentration levels (e.g., low, mid, and high) covering the specified range of the assay is recommended [15] [18].
- Experimental Procedure: Analyze each of the spiked samples using the new molecular assay.
- Data Analysis: For each spiked sample, calculate the percent recovery: (Measured Concentration / Known Concentration) x 100. The overall accuracy of the method is demonstrated by the mean percent recovery across all tested concentrations and the confidence intervals (e.g., ±1 standard deviation) [18].
Visualizing Diagnostic Test Outcomes
The relationship between a new assay's results and the true disease status, as determined by a gold standard, is best understood through a contingency table. This framework allows for the calculation of all key validation parameters, highlighting the critical balance between sensitivity and specificity [17].
Diagram: Diagnostic Test Outcomes vs. Gold Standard. This 2x2 table illustrates how true positives, false positives, false negatives, and true negatives are defined in relation to a gold standard test, forming the basis for calculating sensitivity, specificity, and predictive values [17].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following reagents and instruments are critical for executing the validation protocols for molecular assays, such as PCR-based methods, against a gold standard like microscopy.
| Item | Function in Validation |
|---|---|
| Well-Characterized Sample Panel | Serves as the primary material for specificity/sensitivity testing. Includes samples with known status (positive/negative) confirmed by the gold standard and samples with potential interferents [15] [17]. |
| Certified Reference Materials (CRMs) | Provides the known, true quantity of the analyte for spiking experiments to establish accuracy and the standard curve for linearity. Essential for generating data on percent recovery [18]. |
| Homogeneous Sample Material | A single, well-mixed sample is used for precision testing (repeatability and intermediate precision) to ensure that any variation measured is from the assay itself and not from the sample [18]. |
| Appropriate Instrumentation | The analytical platform (e.g., qPCR machine, sequencer) must be properly qualified to ensure its performance does not adversely affect the validation data. This is a prerequisite for reliable method validation [18]. |
The rigorous validation of a molecular assay against a gold standard like microscopy is a cornerstone of reliable scientific research and drug development. By systematically quantifying specificity, sensitivity, precision, and accuracy, researchers can provide compelling, data-driven evidence of their assay's reliability. This process not only ensures the integrity of experimental data but also builds the foundational trust required for adopting new technologies in clinical and regulatory decision-making. As methodological advancements continue, these core validation parameters will remain the universal language for demonstrating assay quality and fitness-for-purpose.
The validation of new diagnostic tools against established gold standards is a critical cornerstone in the advancement of medical science. For centuries, manual microscopy has served as this foundational standard in pathology and microbiology, providing the benchmark against which newer technologies are measured [1] [20]. The transition to innovative molecular assays and digital platforms necessitates rigorous validation across multiple contexts to ensure diagnostic accuracy, reliability, and patient safety are maintained. This comparative guide examines the distinct frameworks of vendor-driven, academic, and clinical laboratory validation studies, with a specific focus on their application in validating molecular assays against microscopy gold standards. Each pathway addresses different objectives, regulatory requirements, and performance metrics, yet all converge on the common goal of establishing diagnostic confidence for researchers, scientists, and drug development professionals navigating this evolving landscape.
Defining the Three Validation Contexts
Validation studies are conducted in three primary contexts, each with distinct objectives, methodologies, and regulatory considerations. Understanding these frameworks is essential for interpreting validation data and applying it appropriately in research and clinical settings.
Vendor-Driven Studies are conducted by manufacturers to obtain regulatory clearance for their devices. These studies are comprehensive, targeting specific regulatory milestones such as FDA 510(k) clearance, and are designed to demonstrate that a new system performs as reliably as the established gold standard for its intended use [1]. The recent FDA clearance of Roche's Digital Pathology Dx system exemplifies this context, where massive clinical performance studies were conducted to prove non-inferiority to manual microscopy [20].
Academic Studies aim to explore the general feasibility, applicability, and limitations of new technologies through peer-reviewed research [1]. These investigations often examine broader research questions beyond immediate regulatory needs, such as novel applications or methodological innovations. For instance, academic research into leprosy diagnostics has evaluated new recombinant protein antigens and fusion versions like LID-1, exploring their potential for point-of-care testing beyond what current vendor offerings provide [21].
Clinical Laboratory Studies are performed by individual laboratories to validate a technology within their specific operational environment [1]. These studies ensure the combination of technology, personnel, and workflows in a particular laboratory setting produces reliable results for patient care. According to current standards, clinical validation of digital microscopy for primary diagnostic work is required for each laboratory initiating a transition from light microscopy to digital systems [1].
Table 1: Comparative Overview of Validation Contexts
| Validation Aspect | Vendor-Driven Studies | Academic Studies | Clinical Laboratory Studies |
|---|---|---|---|
| Primary Objective | Regulatory clearance and market approval [1] | General feasibility and novel applications [1] | Implementation in specific laboratory environment [1] |
| Typical Scale | Large, multi-site (e.g., 2,047 cases in Roche study) [20] | Variable, often limited by research scope | Tailored to laboratory's specific caseload and needs |
| Regulatory Focus | FDA, IVDR, and other regulatory body requirements [22] | Peer review and publication standards | Accreditation standards (e.g., ISO 15189) [22] |
| Outcome Measures | Precision, accuracy, non-inferiority [20] [23] | Novel biomarkers, mechanisms, methodologies [21] | Concordance with existing in-house methods |
| Key Stakeholders | Regulatory agencies, manufacturers [1] | Scientific community, journals [1] | Laboratory directors, accrediting bodies [24] |
Experimental Protocols and Methodologies
Validation studies employ meticulously designed protocols to generate statistically meaningful evidence of performance equivalence or superiority. The methodologies vary significantly across the three contexts but share common elements of rigorous comparison against reference standards.
Vendor-Driven Validation Protocols
Vendor-driven studies follow structured frameworks negotiated with regulatory bodies. The Roche Digital Pathology Dx validation exemplifies this approach, employing two complementary study designs [20]:
Precision/Inter-laboratory Reproducibility Study:
- Objective: Test repeatability and reproducibility across multiple sites
- Design: 23 histopathologic features across 3 sites, with slides scanned on 3 non-consecutive days
- Case Set: 69 glass slide "cases" (3 slides × 23 features) plus 12 "wildcard" cases
- Output Measurement: Percent agreement for feature identification between systems, days, and readers with predetermined acceptance criteria (lower bound of 95% CI ≥85%) [20]
Method Comparison/Accuracy Study:
- Objective: Compare diagnostic accuracy between digital and microscopy reads
- Design: 2,047 clinical cases evaluated by pathologists using both digital reads and manual microscopy
- Reference Standard: Original sign-out diagnosis
- Statistical Analysis: Non-inferiority testing with predetermined margin (-4% lower bound), difference in accuracy calculated as digital reads minus manual microscopy reads [20]
The Roche system successfully met all predetermined endpoints, with precision between systems/sites at 89.3%, between days at 90.3%, and between readers at 90.1%. The difference in accuracy between digital reads and manual microscopy was -0.61% (lower bound of 95% CI: -1.59%), demonstrating non-inferiority [20].
Academic Validation Methodologies
Academic studies often explore more innovative approaches while still maintaining methodological rigor. Research on leprosy diagnostics illustrates this context, focusing on validating molecular assays against microscopic examination of skin biopsies and slit-skin smears [21].
Molecular Detection of Mycobacterium leprae:
- Reference Standard: Microscopic identification of acid-fast bacilli in intradermal smears or histopathology sections [21]
- Index Test: Quantitative polymerase chain reaction targeting M. leprae-specific genes (e.g., RLEP gene) [21]
- Sample Considerations: Validation across leprosy spectrum (paucibacillary vs. multibacillary) with appropriate clinical correlation
- Performance Metrics: Sensitivity, specificity, limit of detection compared to microscopic bacillary index [21]
Academic validation of the PathCrisp assay for detecting NDM-resistant infections demonstrates another approach, combining loop-mediated isothermal amplification with CRISPR-based detection while maintaining a single temperature [12]. This methodology demonstrated 100% concordance with PCR-Sanger sequencing and sensitivity to detect as few as 700 copies of the NDM gene from clinical isolates [12].
Clinical Laboratory Verification Protocols
Clinical laboratories implement focused verification protocols tailored to their specific operational needs and patient populations. These studies typically follow established guidelines while adapting to local constraints [24].
Essential Verification Studies for FDA-Approved Tests:
- Precision: Within-run and day-to-day measurement using quality control materials
- Accuracy: Method comparison with 40 patient samples spanning analytical measurement range
- Reportable Range: Verification using samples across the analytical measurement range
- Reference Range Verification: Confirmation of manufacturer's reference intervals [24]
For non-FDA-approved tests or laboratory-developed tests, additional validation is required, including analytical sensitivity (limit of detection) and analytical specificity (interference studies) [24]. Performance goals are predefined based on allowable total error, with acceptability criteria established for each study before commencement [24].
Diagram 1: Clinical Laboratory Test Validation Workflow. This diagram outlines the decision process for validating both FDA-approved tests and laboratory-developed tests (LDTs), highlighting the additional requirements for LDTs [24].
Comparative Performance Data Analysis
Quantitative performance data forms the evidentiary foundation for diagnostic validation across all three contexts. Systematic comparison of this data reveals both consistencies and variations in validation approaches and outcomes.
Table 2: Validation Performance Metrics Across Diagnostic Technologies
| Technology Platform | Validation Context | Key Performance Metrics | Reference Standard | Outcome |
|---|---|---|---|---|
| Roche Digital Pathology Dx [20] | Vendor-Driven | Precision: 89.3%-90.3%Accuracy: -0.61% differenceReading time: 2.33 min (digital) vs 2.34 min (microscopy) | Manual microscopy | Non-inferiority demonstrated (lower bound 95% CI > -4%) |
| qPCR for M. leprae [21] | Academic | Sensitivity: High in multibacillary casesSpecificity: M. leprae-specificLimitation: Lower sensitivity in paucibacillary cases | Microscopic bacilloscopy of skin smears | Auxiliary diagnostic for confirmation, not replacement |
| PGL-I Serology POCT [21] | Academic | Sensitivity: High in multibacillary patientsSpecificity: VariableUtility: Equipment-free, rapid results | Clinical diagnosis with microscopic correlation | Recommended adjunct test, not stand-alone diagnosis |
| PathCrisp (LAMP+CRISPR) [12] | Academic | Sensitivity: 700 copy detectionConcordance: 100% with PCR-SangerTime: ~2 hours | PCR with Sanger sequencing | High sensitivity and specificity demonstrated |
| Digital Microscopy [1] | Clinical Laboratory | Diagnostic concordance: >95% typicallyVariation: Laboratory-dependent | Light microscopy | Implementation-specific performance |
The tabulated data reveals several important patterns. Vendor-driven studies typically employ large sample sizes and rigorous statistical margins to demonstrate non-inferiority, as seen in the Roche digital pathology system which utilized 2,047 cases to prove diagnostic equivalence to manual microscopy [20]. Academic studies often focus on more specific performance characteristics, such as the differential sensitivity of molecular leprosy tests between multibacillary and paucibacillary cases, acknowledging limitations while advancing the technology [21]. Clinical laboratory validations prioritize practical implementation metrics that ensure reliability in local practice settings.
Essential Research Reagent Solutions
Validation studies across all contexts rely on specialized reagents and materials to ensure accurate, reproducible results. These research tools form the foundation of reliable assay performance and comparability.
Table 3: Essential Research Reagents for Diagnostic Validation Studies
| Reagent/Material | Function in Validation | Application Examples |
|---|---|---|
| Phenolic Glycolipid-I (PGL-I) Antigens [21] | Semi-synthetic antigen for serological detection of M. leprae antibodies | Leprosy point-of-care tests, ELISA-based serology |
| LID-1/NDO-LID Fusion Antigens [21] | Recombinant protein antigens for improved serodiagnosis | Enhanced sensitivity leprosy serology, particularly in multibacillary cases |
| RLEP Gene Primers/Probes [21] | M. leprae-specific DNA target for molecular amplification | qPCR detection of M. leprae in clinical specimens |
| CRISPR/Cas12a with sgRNA [12] | Sequence-specific nucleic acid detection with collateral cleavage activity | PathCrisp assay for NDM gene detection |
| Bst Polymerase for LAMP [12] | Strand-displacing DNA polymerase for isothermal amplification | Loop-mediated isothermal amplification without thermal cycler |
| Whole Slide Imaging Systems [20] | Digital conversion of glass slides for virtual microscopy | Digital pathology primary diagnosis validation |
| International Color Consortium Profiles [20] | Standardized color management for digital pathology | Consistent color representation across digital pathology platforms |
Regulatory and Methodological Considerations
Validation approaches must adapt to evolving regulatory landscapes and methodological innovations. Understanding these frameworks is essential for designing compliant and effective validation studies.
Regulatory Evolution: The recent implementation of the European Commission's In Vitro Diagnostic Regulation and updates to ISO 15189 standards have increased requirements for validation and verification procedures [22]. These changes affect all validation contexts but place particular burdens on clinical laboratories to demonstrate rigorous method evaluation.
Allowable Total Error Framework: Performance goals for validation studies are increasingly defined through Allowable Total Error, which combines precision and accuracy metrics against clinically relevant thresholds [24]. This framework necessitates careful selection of acceptance criteria based on biological variation, clinical outcome studies, or state-of-the-art performance for each analyte.
Technology-Specific Challenges: Different technologies present unique validation challenges. For digital pathology, these include color representation fidelity, scan resolution adequacy, and focus layer requirements for cytology specimens [1]. For molecular assays, challenges include extraction efficiency, amplification inhibitors, and target sequence conservation [12].
The increasing integration of artificial intelligence and computational pathology into diagnostic systems introduces additional validation complexity, requiring demonstration of both analytical and clinical validity for algorithm-based interpretations [25].
Validation of diagnostic technologies against microscopy gold standards proceeds through three complementary yet distinct pathways, each serving essential roles in the technology adoption lifecycle. Vendor-driven studies provide the regulatory foundation for market approval through massive, rigorous demonstrations of non-inferiority. Academic investigations explore novel applications, mechanisms, and methodological innovations that push the boundaries of diagnostic capabilities. Clinical laboratory validations translate these advances into daily practice through localized verification of performance in specific operational environments.
The convergence of evidence from these three contexts builds the comprehensive understanding necessary for diagnostic implementation. As technological innovation accelerates, particularly in digital pathology and molecular diagnostics, this tripartite validation framework ensures that progress is matched by preserved diagnostic accuracy and patient safety. Researchers, scientists, and drug development professionals must navigate all three contexts to effectively advance and implement new diagnostic technologies in both research and clinical practice.
In the validation of molecular assays for diagnostic use, the process is typically benchmarked against an established gold standard, often traditional light microscopy (LM) in pathology [1]. This framework, however, operates on the critical assumption that the gold standard itself is perfect—an assumption that is frequently flawed [26]. Diagnostic concordance between a new method and the reference standard can be significantly influenced by multiple sources of bias, chief among them being the complexity of the cases examined and the diagnostic experience of the pathologists involved [27] [1]. A precise understanding of these biases is not merely academic; it is fundamental to designing robust validation studies for molecular assays, accurately interpreting their performance data, and ensuring their safe implementation in clinical and research settings. This guide objectively compares the performance of diagnostic methods by examining the experimental data on how case complexity and expertise shape diagnostic concordance, providing a crucial framework for researchers and drug development professionals validating new technologies against microscopic standards.
Experimental Protocols for Assessing Diagnostic Concordance
To objectively compare diagnostic performance and understand sources of bias, researchers employ specific experimental designs. The following protocols are central to generating the data discussed in this guide.
Intra-observer Concordance Studies
This design is a cornerstone of digital pathology validation and is equally applicable to molecular assay verification [27] [1]. In this protocol, the same set of cases is evaluated first by the new method (e.g., a molecular assay or digital pathology) and then by the traditional gold standard (LM), with both assessments performed by the same pathologist. A washout period is incorporated between reviews to mitigate memory bias [1]. The primary outcome measure is the diagnostic concordance rate between the two modalities for the same observer [27]. This design directly tests the technological agreement between methods while controlling for inter-observer variability.
Expert Review versus Original Diagnosis
This protocol measures the impact of pathologist experience directly. A set of cases with an original diagnosis from a general pathologist is re-evaluated by a specialist pathologist (e.g., a sarcoma expert) [28]. The specialist typically has access to the same or additional material (including molecular data) to render a final diagnosis. The modification rate between the original and expert diagnoses is the key metric, which can be further categorized into changes that affect patient management (major discrepancies) and those that do not (minor discrepancies) [28]. This design quantifies the variability introduced by diagnostic expertise.
Bayesian Latent Class Models (LCMs)
When no perfect gold standard exists, Bayesian LCMs provide a statistical framework to estimate the true accuracy of diagnostic tests [26]. These models do not assume any test is perfect but instead estimate true disease prevalence and the sensitivity and specificity of each test simultaneously based on the observed patterns of agreement and disagreement across multiple tests applied to the same population [26]. This is particularly useful for validating new molecular assays in fields where the reference standard is known to be imperfect.
Quantitative Data: Factors Influencing Diagnostic Concordance
The following tables synthesize experimental data from published studies, summarizing the impact of key variables on diagnostic outcomes.
Table 1: Impact of Case Complexity and Diagnostic Expertise on Concordance and Modification Rates
| Factor | Study Context | Key Metric | Result | Experimental Protocol |
|---|---|---|---|---|
| Overall DP vs. LM Concordance | Meta-analysis of 24 studies (10,410 samples) [27] | Overall Clinical Concordance | 98.3% (95% CI 97.4 to 98.9) | Intra-observer concordance studies |
| Major Discordances (DP vs. LM) | Meta-analysis of 25 studies [27] | Proportion of Major Discordances | 546 major discordances reported | Analysis of discordant cases across multiple studies |
| Expert Review in Sarcoma | Prospective study of 119 sarcoma cases [28] | Diagnosis Modification Rate | 31.1% (37/119 cases) | Expert vs. original diagnosis review |
| Impact on Management (Sarcoma) | Prospective study of 119 sarcoma cases [28] | Management Modification Rate | 14.2% (17/119 cases) | Expert vs. original diagnosis review |
Table 2: Analysis of Major Diagnostic Discordances in Digital Pathology [27]
| Category of Major Discordance | Proportion of All Major Discordances | Specific Examples or Challenges |
|---|---|---|
| Nuclear Atypia, Grading of Dysplasia & Malignancy | 57% | Assessment of nuclear features, grading of cancerous and pre-cancerous lesions. |
| Challenging Diagnoses | 26% | Inherently difficult cases with overlapping histological features. |
| Identification of Small Objects | 16% | Finding small or sparse microscopic objects (e.g., microorganisms, mitotic figures). |
The Scientist's Toolkit: Key Research Reagent Solutions
The following reagents and materials are essential for conducting rigorous validation studies in diagnostic pathology.
Table 3: Essential Research Reagents and Materials for Validation Studies
| Item | Function in Validation | Specific Example / Note |
|---|---|---|
| FFPE Tissue Blocks | The primary source material for generating histology slides and nucleic acid extraction. | Ensure a range of case complexities and diagnoses. |
| H&E Stains | The foundational stain for histological diagnosis, used for initial morphological assessment. | Central to most validation study protocols [27]. |
| RNA/DNA Extraction Kits | To isolate genetic material for molecular testing via NGS or PCR. | Quality of extraction critical for NGS success [28]. |
| Targeted NGS Panels | For detecting gene fusions, mutations, and other genetic alterations. | e.g., 86-gene fusion panel for sarcoma diagnosis [28]. |
| FISH Assays | To validate specific genetic rearrangements or amplifications. | e.g., MDM2 amplification for liposarcoma diagnosis [28]. |
| Immunohistochemistry Kits | For protein-level detection of biomarkers to aid in diagnosis and classification. | Often used in the initial workup by expert pathologists. |
Visualizing Workflows and Bias Relationships
Diagnostic Validation and Bias Analysis Workflow
The following diagram illustrates the general workflow for a diagnostic validation study and the key points where bias can be introduced and analyzed.
Interplay of Factors Affecting Diagnostic Concordance
This diagram maps the logical relationships between the core factors of case complexity, pathologist experience, and the resulting diagnostic concordance, also showing how these elements feed into assay validation.
The validation of molecular assays against the traditional gold standard of light microscopy is a complex process fraught with potential bias. Experimental data consistently shows that diagnostic concordance is not uniform but is significantly influenced by case complexity—with nuclear atypia and dysplasia being major sources of discordance—and by the expertise of the diagnosing pathologist. A prospective study on sarcomas, for instance, found that expert review modified the original diagnosis in nearly a third of cases, directly altering patient management in over 14% of them [28]. Therefore, a robust validation framework must proactively account for these variables. This involves stratifying cases by complexity, incorporating expert review, and utilizing statistical models like Bayesian LCMs that do not presume the infallibility of the gold standard. For researchers and drug developers, this rigorous, bias-aware approach is fundamental to generating reliable performance data and ensuring that new diagnostic technologies are validated against the most accurate diagnostic truth possible.
From Theory to Bench: Implementing Molecular Assays for Pathogen Detection
The validation of molecular assays against traditional gold standards, such as microscopy, is a cornerstone of diagnostic research. This process ensures that new, rapid methods provide reliable and actionable results. Nucleic acid tests (NATs) have revolutionized diagnostic science by offering superior speed and sensitivity for detecting pathogens and genetic markers. Among these, quantitative polymerase chain reaction (qPCR) has long been the benchmark technique. However, the emergence of isothermal amplification methods, particularly loop-mediated isothermal amplification (LAMP) and its advanced derivatives like PathCrisp, presents compelling alternatives. These isothermal techniques challenge the conventional paradigm by offering simplicity and portability without relying on sophisticated thermal cycling equipment. This guide objectively compares the performance of qPCR, LAMP, and PathCrisp, providing experimental data and protocols to help researchers select the appropriate method for their validation studies against microscopy and other standards.
qPCR (Quantitative Polymerase Chain Reaction)
qPCR is a thermal-cycling-dependent method that amplifies and simultaneously quantifies a specific DNA target. It relies on repeated cycles of denaturation (at high temperatures, ~95°C), annealing (at primer-specific temperatures, ~50-65°C), and extension (~72°C) to exponentially amplify nucleic acids. Fluorescent probes or DNA-binding dyes allow real-time monitoring of the amplification process, enabling quantification of the initial target concentration based on the cycle threshold (Ct) value, the point at which fluorescence crosses a predefined threshold [29] [30]. Its requirement for precise temperature control and sophisticated instrumentation has been a key driver in the development of alternative methods.
LAMP (Loop-Mediated Isothermal Amplification)
LAMP is an isothermal nucleic acid amplification technique that operates at a constant temperature, typically between 60-65°C. It utilizes a strand-displacing DNA polymerase (e.g., Bst polymerase) and four to six specially designed primers that recognize six to eight distinct regions on the target genome. The amplification process involves the formation of stem-loop DNA structures, leading to very efficient amplification without the need for thermal denaturation. Results can be visualized through turbidity (from magnesium pyrophosphate precipitate), fluorescent intercalating dyes, or colorimetric changes [31] [32] [30]. This simplicity makes it suitable for point-of-care settings.
PathCrisp
PathCrisp represents a next-generation diagnostic tool that combines the amplification power of LAMP with the specific detection capabilities of the CRISPR-Cas12a system. In this method, LAMP first amplifies the target nucleic acid isothermally. The amplified products are then recognized by a CRISPR-Cas12a complex programmed with a specific guide RNA (crRNA). Upon binding to its target, the Cas12a enzyme is activated and exhibits collateral activity, cleaving nearby single-stranded DNA (ssDNA) reporters. This cleavage generates a fluorescent or colorimetric signal, providing a highly specific readout [12] [33]. This two-step verification process enhances specificity and reduces false positives.
Performance Comparison: Experimental Data
The following tables summarize key performance metrics from published studies comparing these NATs across various applications, from pathogen detection to antimicrobial resistance screening.
Table 1: Comparative Analytical Sensitivity of NATs from Clinical Studies
| Assay | Target | Pathogen/Application | Limit of Detection (LoD) | Source/Study |
|---|---|---|---|---|
| RT-qPCR | SARS-CoV-2 RNA | COVID-19 | 30-50 copies [34] | Bruce et al., 2020 |
| RT-qPCR (CDC) | SARS-CoV-2 RNA | COVID-19 | Most accurate among tested [29] | PMC10170900, 2023 |
| RT-LAMP | SARS-CoV-2 RNA | COVID-19 | 400-500 copies [34]; 71% sensitivity vs RT-qPCR on direct swabs [35] | Garafutdinov et al., 2020 |
| LAMP | Alternaria solani DNA | Plant Fungal Pathogen | 10-fold more sensitive than conventional PCR [31] | Frontiers in Microbiology, 2018 |
| Nested PCR | Alternaria solani DNA | Plant Fungal Pathogen | 100-fold more sensitive than LAMP [31] | Frontiers in Microbiology, 2018 |
| PathCrisp | NDM Gene | Antimicrobial Resistance | 700 copies; 100% concordance with PCR-Sanger sequencing [12] [36] | Scientific Reports, 2025 |
Table 2: Operational Characteristics and Practical Performance
| Parameter | qPCR/RT-qPCR | LAMP/RT-LAMP | PathCrisp |
|---|---|---|---|
| Amplification Temperature | Multiple (Thermocycling: ~95°, ~60°, ~72°C) | Constant (Isothermal: ~60-65°C) | Constant (Isothermal: LAMP at ~60°C, CRISPR at ~37°C) |
| Assay Time | 1.5 - 2 hours [34] [30] | ~45 - 70 minutes [31] [32] [35] | ~2 hours total [12] |
| Instrument Requirement | Complex (Thermal Cycler, Fluorometer) | Simple (Water Bath/Block Heater) | Simple (Water Bath/Block Heater) |
| Sensitivity | High (Gold Standard) | Moderate to High (Platform-dependent) | High |
| Specificity | High | High (from multiple primers) | Very High (Dual-check: LAMP + CRISPR) |
| Ease of Use | Requires trained personnel | Simpler; suitable for point-of-care | Requires careful setup but simple readout |
| Sample Preparation | Often requires purified RNA/DNA | Tolerant to crude samples; can use simple heating [12] [31] | Can use crude extraction from culture [12] |
| Key Advantage | Gold standard, quantitative | Rapid, simple, equipment-free | High specificity, low false positives |
Detailed Experimental Protocols
To ensure the reproducibility of results in a research setting, detailed protocols for key experiments are provided below.
Protocol: RT-qPCR for SARS-CoV-2 Detection (CDC Protocol)
This protocol is adapted from the study that found the CDC (USA) RT-qPCR protocol to be the most accurate for COVID-19 diagnosis [29].
- Sample Collection and RNA Extraction: Collect oro-nasopharyngeal swabs. Extract RNA using a commercial kit like QIAmp Viral RNA Kit (QIAGEN). Store extracted RNA at -80°C if not used immediately.
- Reaction Setup: Prepare a 20 μL reaction mixture containing:
- GoTaq Probe qPCR Master Mix with dUTP (10 μL)
- GoScript RT Mix for one-step RT-qPCR (0.4 μL)
- Sense and antisense primers (500 nM each) targeting the N1 and N2 genes of SARS-CoV-2
- Probes (125 nM)
- Nuclease-free water and 5 μL of template RNA
- Amplification Conditions: Run the reaction on a real-time PCR instrument with the following program:
- 45°C for 15 min (Reverse transcription)
- 95°C for 2 min (Initial denaturation)
- 40 cycles of: 95°C for 15 s (Denaturation) and 60°C for 1 min (Annealing/Extension)
- Result Interpretation: A sample is considered positive if amplification of both N1 and N2 gene fragments is detected at a cycle threshold (Ct) ≤ 37.
Protocol: LAMP Assay for Fungal Pathogen Detection
This protocol for detecting Alternaria solani, the causative agent of early blight in potatoes, demonstrates LAMP's application in plant pathology [31].
- DNA Extraction: Harvest mycelia from cultured isolates. Air-dry, then grind. Extract genomic DNA using a commercial kit (e.g., Bioteke kit) and quantify it with a spectrophotometer.
- Primer Design: Design LAMP primers (F3, B3, FIP, BIP) targeting a specific gene, such as the histidine kinase gene (HK1), using software like Primer Explorer V4.
- LAMP Reaction: Prepare a 25 μL reaction mixture containing:
- 2× reaction buffer (12.5 μL)
- Bst DNA polymerase (e.g., 0.4 μL of Bst1.0 enzyme)
- Outer primers (F3, B3; 0.2 μM each)
- Inner primers (FIP, BIP; 1.6 μM each)
- Target DNA template (1-2 μL)
- Incubation and Detection: Incubate the reaction at a constant temperature of 63°C for 60 minutes. Stop the reaction by heating at 80°C for 5 minutes. Detect amplification via:
- Visual Inspection: Add an intercalating dye like SYBR Green I; a color change under UV light indicates a positive result.
- Turbidity: Directly observe the white precipitate of magnesium pyrophosphate.
- Gel Electrophoresis: Analyze the product for a characteristic ladder-like pattern.
Protocol: PathCrisp Assay for NDM Resistance Gene Detection
This protocol outlines the two-step method for detecting the New Delhi metallo-beta-lactamase (NDM) gene, a critical marker of carbapenem resistance [12].
- Step 1: LAMP Amplification
- Sample Preparation: Use crude bacterial lysate obtained by heating a colony, or purified DNA.
- LAMP Reaction: Set up a reaction with a LAMP master mix (e.g., Multi-Purpose LAMP Master Mix), Bst polymerase, and six specific LAMP primers designed to the conserved region of the NDM gene.
- Incubation: Incubate at 60°C for 1 hour.
- Step 2: CRISPR-Cas12a Detection
- Detection Mix Preparation: Pre-incubate 26 nM of Cas12a enzyme with 26 nM of target-specific sgRNA in an appropriate buffer (e.g., 1× NEBuffer 2.1) at room temperature for 10 minutes to form the RNP complex. Add a fluorescent ssDNA reporter (e.g., 200 nM of ssDNA-FQ with FAM and quencher).
- Trans-Cleavage Reaction: Add 10 μL of the LAMP amplification product to the detection mix. Incubate at 37°C for 10-20 minutes.
- Signal Readout: Measure fluorescence in real-time using a fluorimeter (excitation/emission: 480/520 nm). A positive result is indicated by a significant increase in fluorescence relative to the no-template control.
Workflow and Signaling Pathways
The diagrams below illustrate the core workflows and detection mechanisms for each nucleic acid test.
qPCR Workflow
qPCR involves cyclic temperature changes for amplification with real-time fluorescence monitoring.
LAMP Mechanism
LAMP uses multiple primers for isothermal amplification, generating products that yield visual signals.
PathCrisp Detection Principle
PathCrisp couples LAMP amplification with CRISPR-Cas12a activation, triggering a fluorescent reporter.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of these NATs relies on specific reagents and materials. The following table details essential components for setting up these assays.
Table 3: Essential Reagents and Materials for NATs
| Reagent/Material | Function/Purpose | Example Product/Note |
|---|---|---|
| Bst DNA Polymerase | Strand-displacing enzyme for LAMP amplification; enables isothermal reactions. | Available from suppliers like New England Biolabs (NEB). Critical for LAMP and PathCrisp [12] [31]. |
| Taq DNA Polymerase | Thermostable enzyme for PCR/qPCR; synthesizes new DNA strands during thermal cycling. | Often part of a master mix (e.g., GoTaq Probe qPCR Master Mix [29]). |
| Reverse Transcriptase | Converts RNA into complementary DNA (cDNA) for RT-qPCR and RT-LAMP. | M-MLV Reverse Transcriptase [34] or enzymes in one-step kits. |
| LAMP Primers | Set of 4-6 primers that bind to multiple regions of the target for specific isothermal amplification. | Designed with software like Primer Explorer V4 [31]. |
| CRISPR-Cas12a Enzyme & sgRNA | Cas12a nuclease and specific guide RNA for target recognition and collateral cleavage in PathCrisp. | Alt-R L.b. Cas12a (Cpf1) Ultra (IDT) [12]. The sgRNA is designed to a conserved target region. |
| Fluorescent Probe/Reporter | For real-time signal detection. In qPCR, a target-specific probe; in PathCrisp, a nonspecific ssDNA reporter. | TaqMan probes (qPCR) [29]; ssDNA-FQ with FAM/Quencher (PathCrisp) [12] [33]. |
| Intercalating Dye | Binds double-stranded DNA for detection in LAMP and some qPCR applications. | SYBR Green I [34]. Can be used for visual or fluorometric readouts. |
| Nucleic Acid Extraction Kit | Purifies DNA/RNA from complex samples (swabs, tissue, culture). | QIAmp Viral RNA Kit [29], Magnetic bead-based kits [33]. |
| dNTPs | Nucleotides (dATP, dCTP, dGTP, dTTP) that are the building blocks for DNA synthesis. | Essential for all amplification reactions [12] [34]. |
| Isothermal Buffer | Provides optimal pH, salt, and Mg²⁺ conditions for Bst polymerase activity. | Often included with the enzyme (e.g., NEBuffer, SD polymerase buffer [12] [34]). |
The choice between qPCR, LAMP, and advanced systems like PathCrisp depends heavily on the research context and the parameters of the validation study against a gold standard. qPCR remains the undisputed reference for quantitative accuracy and sensitivity in a controlled laboratory environment. LAMP offers a robust, rapid, and equipment-minimal alternative, ideal for field-use or point-of-care testing where speed and simplicity are paramount, even with a potential slight trade-off in sensitivity for some sample types. PathCrisp and other CRISPR-integrated assays represent a significant leap forward in specificity, effectively minimizing false positives through a dual-check mechanism, which is crucial for detecting specific resistance markers or low-abundance pathogens.
For researchers validating these assays against microscopy, the decision matrix is clear: use qPCR for establishing a quantitative baseline and maximum sensitivity; employ LAMP for rapid screening and settings where resources are limited; and adopt PathCrisp-like technology when unambiguous, high-specificity detection of a genetic marker is the primary goal. As these technologies continue to evolve, their integration into diagnostic pipelines will further bridge the gap between central laboratories and field-based diagnostics, enhancing our ability to respond to infectious disease threats and antimicrobial resistance.
The accurate quantification of Plasmodium falciparum is a cornerstone of modern malaria research, directly impacting the assessment of vaccine efficacy, drug treatments, and our understanding of parasite biology in controlled human malaria infection (CHMI) studies [37]. For decades, microscopy has served as the gold standard for parasite detection and quantification, but this method faces challenges related to sensitivity and operator expertise [38]. The emergence of quantitative polymerase chain reaction (qPCR) methodologies has introduced a powerful alternative capable of detecting sub-microscopic parasite densities, but requires rigorous validation to ensure reliability [37] [38].
This case study examines the comprehensive validation of a qPCR assay for P. falciparum quantification, positioning its performance against traditional microscopy and rapid diagnostic tests (RDTs). The validation framework encompasses specificity, sensitivity, accuracy, precision, and linearity assessments, providing researchers with a standardized approach for implementing molecular quantification in malaria studies [37]. As drug development professionals increasingly rely on precise parasite metrics for efficacy determinations, validated qPCR methods offer the reproducibility and sensitivity required for robust clinical trial outcomes.
Experimental Design and Methodologies
Parasite Culture and Standard Preparation
The validation process began with the cultivation of P. falciparum 3D7 parasites in human red blood cell suspensions using RPMI 1640 medium supplemented with L-glutamine, HEPES, gentamicin, glucose, and hypoxanthine [37]. Cultures were maintained at 37°C under 5% CO2 and synchronized at the ring stage using 5% sorbitol treatment to ensure stage-specific homogeneity [37]. The quantification of infected red blood cells was performed using flow cytometry, where 5μL of harvested P. falciparum-infected RBCs were stained with 1:1000 SYBR green for 30 minutes, washed twice with phosphate-buffered saline, and analyzed using a BD FACS Canto with an acquisition of 1,000,000 events per sample [37].
For the standardized parasite dilution series, donor whole blood from O-positive healthy donors was screened for the absence of P. falciparum using rapid diagnostic tests and confirmed by Taqman 18S rRNA qPCR [37]. These donor blood samples were subsequently spiked with in vitro cultured and counted asexual stage frozen P. falciparum parasites. A two-fold serial dilution of spiked whole blood was created, generating a parasite count range of 0.25 to 2,500 parasites/μL, which served as reference material for the validation experiments [37].
DNA Extraction and qPCR Protocol
DNA extraction was performed from whole blood spiked with P. falciparum using the QIAsymphony machine for automated DNA extraction and purification according to the manufacturer's instructions [37]. To determine the impact of blood volume on assay sensitivity, extractions were performed using four different sample volumes: 200μL, 400μL, 500μL, and 1000μL, with each extraction including known positive and negative control samples [37]. DNA was eluted in 50μL (for 200μL extraction volume) or 100μL of elution buffer (for larger extraction volumes).
The qPCR amplification targeted the multicopy (four to eight per parasite) 18S ribosomal RNA genes of P. falciparum (NCBI nucleotide database accession number: M19173) using primers and probes previously described by Hermsen et al. (2001) with modifications from the Oxford qPCR method [37]. The reaction mixture contained final concentrations of 1× universal PCR Master Mix, 10pmol/μL of each primer, and 10μmol of Non-Florescent Quencher with Minor Groove Binder moiety (NFQ-MGB) probe in a 50μL reaction [37]. The thermal profile consisted of 10 minutes at 95°C followed by 45 cycles of 15 seconds at 95°C and 1 minute at 60°C [37].
Table 1: Primer and Probe Sequences for P. falciparum 18S rRNA Gene Detection
| Component | Sequence (5' to 3') | Final Concentration |
|---|---|---|
| Forward Primer | GTAATTGGAATGATAGGAATTTACAAGGT | 10pmol/μL |
| Reverse Primer | TCAACTACGAACGTTTTAACTGCAAC | 10pmol/μL |
| Probe | FAM- AACAATTGGAGGGCAAG-NFQ-MGB | 10μmol |
All qPCR runs included known cultured parasite standards comprising seven serial dilutions of extracted DNA run in triplicates, unknown samples in triplicate, negative controls (uninfected red blood cells) in triplicate, and three replicates of Non-Template Control (water) [37]. Standard curves were generated by plotting the mean cycle CT values versus the logarithmic parasite concentration, with parasite concentration based on relative quantification using flow cytometry data [37].
Performance Comparison: qPCR vs. Conventional Diagnostic Methods
Sensitivity and Detection Limits
The validation of the qPCR assay demonstrated exceptional sensitivity compared to conventional diagnostic methods. The lower limit of detection (LLoD) was established at 0.3 parasites/μL, with a lower limit of quantification (LLoQ) of 2.6 parasites/μL [37]. This represents a significant improvement over microscopy, which typically has a detection limit of 4-20 parasites/μL depending on the number of fields evaluated and the expertise of the microscopist [37]. Rapid diagnostic tests show even greater limitations, with sensitivities declining substantially at parasite densities below 100 parasites/μL [39].
In a 2025 study comparing diagnostic methods among pregnant women in northwest Ethiopia, microscopy exhibited a sensitivity of 73.8% in peripheral blood and 62.2% in placental blood when using multiplex qPCR as a reference standard [40]. Similarly, RDTs showed sensitivities of 67.6% in peripheral blood and 62.2% in placental blood [40]. These findings highlight the particular challenge of detecting low-density infections in pregnant women, where placental sequestration further reduces peripheral parasitemia.
Specificity and Accuracy
The validated qPCR assay achieved 100% specificity across five independent experiments, demonstrating no cross-reactivity with non-target organisms [37]. This high specificity matches that of well-performed microscopy, which maintained 100% specificity in peripheral and placental blood samples in comparative studies [40]. RDTs showed slightly lower specificity, ranging from 96.5% in peripheral blood to 98.8% in placental blood [40].
In terms of accuracy, the qPCR method demonstrated excellent extraction efficiency of >90% and close agreement with microscopy in quantitative measurements [37]. A 2019 validation study comparing microscopy versus qPCR for quantifying P. falciparum parasitemia found no significant difference in log10 parasitemia values between the two methods (mean difference 0.04, 95% CI -0.01-0.10, p=0.088) [38]. The intraclass correlation coefficient between microscopy and 18S qPCR was 0.97, indicating excellent consistency between the methods across a wide range of parasitemia values [38].
Table 2: Comparative Performance of Malaria Diagnostic Methods
| Parameter | Microscopy | RDT | qPCR |
|---|---|---|---|
| Detection Limit | 4-20 parasites/μL [37] | ~100 parasites/μL [39] | 0.3 parasites/μL [37] |
| Sensitivity (Peripheral Blood) | 73.8% [40] | 67.6% [40] | 100% (reference) [40] |
| Specificity (Peripheral Blood) | 100% [40] | 96.5% [40] | 100% [37] |
| Quantification Capability | Yes | No | Yes |
| Species Differentiation | Yes | Limited | Yes |
| Time to Result | 30-60 minutes | 15-20 minutes | 2-4 hours |
Linearity, Precision, and Robustness
The validation study demonstrated excellent linearity with R² values ≥0.98 across the quantification range, with amplification efficiency between 89-100% and a slope of -3.8 to -3.1 [37]. Both inter-assay repeatability and intra-assay reproducibility showed high precision, with coefficients of variation (CV) values of <10% across replicate measurements [37].
The robustness of the assay was evaluated by testing different blood volumes for DNA extraction. The study revealed that using large blood volumes (1000μL) for extraction had an adverse effect on precision, highlighting the importance of standardized protocols in DNA extraction [37]. This finding has practical implications for study design, suggesting that optimal performance is achieved with blood volumes of 200-500μL rather than larger volumes that might intuitively be expected to increase sensitivity.
In a 2025 community-based study in Tanzania, the sensitivity of both RDTs and microscopy was low at very low parasitemia (<100 parasites/μL) but increased significantly with increasing parasitemia, reaching ≥99.6% at >10,000 parasites/μL [39]. This pattern underscores the limitations of conventional methods in detecting low-density infections that are increasingly recognized as important for malaria transmission and control.
qPCR Validation Workflow
The following diagram illustrates the comprehensive workflow for validating a qPCR assay for Plasmodium falciparum quantification:
Diagnostic Pathway Comparison
The following diagram compares the diagnostic pathways for malaria detection using different methodologies:
Essential Research Reagent Solutions
Table 3: Key Research Reagents for P. falciparum qPCR Validation
| Reagent/Equipment | Specification | Research Function |
|---|---|---|
| Primer/Probe Set | 18S rRNA gene targets (M19173) [37] | Specific detection of P. falciparum DNA |
| DNA Extraction System | QIAsymphony platform [37] | Automated nucleic acid purification |
| qPCR Master Mix | Universal PCR Master Mix [37] | Amplification reaction components |
| Parasite Culture Media | RPMI 1640 with supplements [37] | In vitro maintenance of P. falciparum |
| Flow Cytometry Reagent | SYBR Green stain [37] | Parasite quantification for standards |
| Reference Parasite Strain | P. falciparum 3D7 [37] | Controlled and standardized parasite material |
| Nucleic Acid Elution Buffer | Manufacturer-specific formulation [37] | DNA stabilization after extraction |
| Quality Control Materials | Positive and negative controls [37] | Assay performance verification |
Implications for Research and Clinical Applications
The validation of qPCR for P. falciparum quantification has significant implications for malaria research and clinical applications. In controlled human malaria infection studies, where precise monitoring of infection dynamics is crucial for assessing vaccine and drug efficacy, the enhanced sensitivity of qPCR enables earlier detection of patency and more accurate measurement of intervention effects [37]. The ability to detect parasites at densities as low as 0.3 parasites/μL represents a substantial improvement over microscopy, potentially reducing the time to treatment in challenge studies and providing more refined endpoints for efficacy evaluations [37].
For drug development professionals, validated qPCR methods offer robust tools for determining parasite clearance rates and detecting recrudescence after treatment [41]. The quantitative nature of PCR allows for precise measurement of parasite reduction ratios, a critical metric in antimalarial drug development [41]. Additionally, the capability to identify species-specific infections and mixed infections through molecular methods provides valuable insights into drug efficacy across different Plasmodium species [42].
In endemic settings, the high sensitivity of qPCR makes it particularly valuable for detecting low-density and subclinical infections that perpetuate transmission [39]. A 2025 study in Tanzania demonstrated that qPCR detected a significantly higher prevalence of Plasmodium infections (39.8%) compared to microscopy (32.1%) or RDTs (44.4%), highlighting the substantial proportion of infections that remain undetected by conventional methods [39]. These subpatent infections represent an important reservoir for continued transmission and may complicate malaria elimination efforts.
The comprehensive validation of qPCR for Plasmodium falciparum quantification establishes this molecular method as a robust, sensitive, and precise alternative to conventional microscopy in research settings. The demonstrated performance characteristics—including a detection limit of 0.3 parasites/μL, 100% specificity, high linearity (R² ≥0.98), and excellent precision (CV <10%)—position qPCR as an invaluable tool for malaria research, particularly in controlled human infection studies and drug development trials [37].
While microscopy remains the field-standard for clinical diagnosis in many settings, and RDTs provide rapid point-of-care testing, qPCR offers unparalleled sensitivity and quantification capabilities essential for advanced research applications [38] [39] [40]. The standardized protocols and validation frameworks described in this case study provide researchers with a roadmap for implementing reliable molecular quantification of P. falciparum, ultimately supporting the development of more effective malaria interventions through precise parasite monitoring and enhanced understanding of infection dynamics.
As malaria research continues to evolve, with increasing emphasis on low-density infections and transmission dynamics, validated qPCR methods will play an increasingly crucial role in generating accurate, reproducible data to guide elimination efforts. The integration of these molecular tools into standard research practice represents a significant advancement in our ability to quantify and understand Plasmodium falciparum infections with unprecedented precision.
The emergence and global spread of New Delhi Metallo-β-lactamase (NDM) genes represents a critical public health threat, rendering bacterial pathogens resistant to nearly all beta-lactam antibiotics, including carbapenems. Carbapenem-resistant Enterobacterales (CRE) and Acinetobacter baumannii are classified by the World Health Organization as critical-priority pathogens due to limited treatment options and significant associated mortality [43] [44]. The silent pandemic of antimicrobial resistance (AMR) was associated with 4.95 million deaths in 2019 alone, with carbapenem resistance mortality rates ranging from 26% to 70% globally [12]. Rapid and accurate detection of NDM-producing organisms is therefore essential for effective infection control, antimicrobial stewardship, and appropriate patient management. This case study provides a comprehensive comparison of current molecular diagnostics for NDM gene detection, evaluating their performance characteristics, technical requirements, and applicability in various clinical and research settings.
Comparative Performance of Molecular Detection Methods
Molecular diagnostics for NDM detection have evolved significantly, offering varying levels of sensitivity, speed, and technical complexity. The table below summarizes the performance characteristics of major molecular detection systems based on recent clinical evaluations.
Table 1: Performance Comparison of Molecular Methods for NDM Detection
| Method | Principle | Time to Result | Sensitivity | Specificity | Key Advantages | Major Limitations |
|---|---|---|---|---|---|---|
| Xpert Carba-R Assay [43] | Real-time PCR | ~50 minutes | 96.6% | 98.6% | Automated, simple workflow; direct from BC bottles | Higher cost per test; limited target range |
| NG-Test CARBA 5 [45] | Immunochromatographic | 15 minutes | >99% | >99% | Rapid; no instrument needed; cost-effective | Lower sensitivity for non-fermenters (84.62% for A. baumannii) [46] |
| Allplex Entero-DR Assay [46] | Multiplex real-time PCR | ~2 hours | 71.9% | N/R | Detects 5 carbapenemases + ESBL + vancomycin genes | Requires DNA extraction; specialized equipment |
| PathCrisp-NDM [12] | LAMP + CRISPR/Cas12a | ~2 hours | 100% (vs. PCR) | 100% (vs. PCR) | High sensitivity; constant temperature; crude extraction sufficient | Protocol optimization needed for POC use |
| REALQUALITY Carba-Screen [47] | Two-level qRT-PCR | 1h6min per step | 100% | 92.6% | Two-step workflow efficiently excludes negatives | Requires extraction and RT-PCR equipment |
Abbreviations: BC: blood culture; ESBL: extended-spectrum beta-lactamase; LAMP: loop-mediated isothermal amplification; N/R: not reported; POC: point-of-care; RT-PCR: real-time polymerase chain reaction.
Experimental Protocols for NDM Detection
Xpert Carba-R Assay Direct from Blood Cultures
The Xpert Carba-R assay (Cepheid) enables rapid NDM detection directly from positive blood culture bottles, significantly reducing turnaround time compared to traditional culture-based methods [43].
Sample Preparation:
- Aliquot 50 μL from positive blood culture bottle
- Mix with Sample Reagent Buffer
- Vortex at high speed for 10 seconds
- Transfer 1.7 mL to specimen chamber of Xpert cartridge
Detection Protocol:
- Load cartridge into GeneXpert platform
- Automated DNA extraction, amplification, and detection
- Results interpreted automatically by system in approximately 50 minutes
Target Detection: The assay detects blaNDM (all variants), blaKPC (all variants), blaVIM (all variants), blaIMP (blaIMP-1,3,6,10,25&30), and blaOXA-48-like (including blaOXA-48,162,163,181,204,232,244,245&247) [43].
PathCrisp-NDM Assay Protocol
The PathCrisp assay combines isothermal amplification with CRISPR-based detection for highly sensitive NDM detection [12].
DNA Preparation:
- Crude extraction: bacterial colonies suspended in nuclease-free water and heated at 98°C for 5 minutes
- Alternative: purified DNA using commercial kits
Isothermal Amplification:
- Multi-Purpose LAMP Master Mix (DNA) (Aurabiotech)
- Reaction composition: 5 μL of 2× reaction buffer, 0.4 μL Bst1.0 enzyme, 0.2 μM outer primers, 0.4 μM loop primers, 1.6 μM inner primers
- Incubation: 60°C for 1 hour
CRISPR-Based Detection:
- Detection mix: 26 nM sgRNA, 26 nM Cas12a, 200 nM ssDNA-FQ reporter in 1× NEBuffer 2
- Pre-incubate 10 minutes at room temperature for RNP complex formation
- Add amplified product to detection mix
- Incubate at 37°C with fluorescence reading (excitation 480 nm, emission 520 nm) every 2.5 minutes
REALQUALITY Carba-Screen Two-Level Screening
This protocol utilizes a two-level approach for efficient screening of rectal swabs [47].
Sample Processing:
- Aliquot 200 μL from liquid Amies medium of rectal swab
- Add 20 μL K proteinase and vortex
- Extract nucleic acids using semi-automated system (ANDiS 360)
- Elute DNA in 60 μL volume
Two-Level PCR Detection:
- Level 1 (Screening): 5 μL DNA + 20 μL Master Mix; detects class A, B, D carbapenemases and Acinetobacter OXA genes
- Level 2 (Confirmation): Positive samples undergo differential detection with:
- Mix Carba-B: blaNDM, blaVIM, blaIMP
- Mix Carba A + D: blaKPC, blaOXA48, mcr1,2,4
- Internal control: bacterial 16S RNA gene ensures sample adequacy
Technological Workflows and Method Selection
The molecular detection of NDM genes follows distinct technological pathways, each with specific advantages for different laboratory settings. The following diagram illustrates the key methodological approaches and their relationships:
Molecular Detection Method Pathways
The Scientist's Toolkit: Essential Research Reagents
Successful detection of NDM genes requires specific reagents and systems optimized for resistance gene detection. The following table catalogues essential research solutions documented in recent studies.
Table 2: Essential Research Reagents for NDM Gene Detection
| Reagent/System | Manufacturer | Function | Application Context |
|---|---|---|---|
| Xpert Carba-R Assay | Cepheid | Integrated cartridge for extraction, amplification, detection | Direct detection from blood cultures and bacterial colonies [43] |
| NG-Test CARBA 5 | NG Biotech | Immunochromatographic detection of 5 major carbapenemases | Rapid testing from bacterial colonies; 15-minute protocol [46] [45] |
| Allplex Entero-DR Assay | Seegene | Multiplex real-time PCR for carbapenemase + ESBL genes | Comprehensive resistance profiling from colonies and rectal swabs [46] |
| REALQUALITY Carba-Screen | AB ANALITICA | Two-level qRT-PCR screening | Direct detection from rectal swabs with internal control [47] |
| STARMag 96 × 4 Universal Cartridge Kit | Seegene | Automated nucleic acid extraction | DNA isolation for PCR-based carbapenemase detection [46] |
| PureLink Microbiome DNA Extraction Kit | Invitrogen | Manual DNA extraction | Whole-genome sequencing preparation [43] |
| Multi-Purpose LAMP Master Mix | Aurabiotech | Isothermal amplification | PathCrisp assay for NDM detection [12] |
| Alt-R L.b. Cas12a (Cpf1) Ultra | IDT | CRISPR enzyme for detection | PathCrisp trans-cleavage detection system [12] |
Analytical Sensitivity and Detection Limits
The analytical performance of NDM detection methods varies significantly between platforms, impacting their utility in different clinical scenarios.
PCR-Based Methods: The Allplex Entero-DR assay demonstrates a detection limit of 100 copies/reaction, providing high sensitivity for carbapenemase gene detection [46]. The Xpert Carba-R assay shows 96.6% sensitivity and 98.6% specificity for detecting NDM genes from cultured isolates and rectal swabs [43].
Immunochromatographic Methods: The NG-Test CARBA 5 detects NDM variants (NDM-1 through NDM-11 and NDM-19) with a detection limit of 150 pg/mL for the NDM protein [46]. This method demonstrated exceptional performance in a multicenter evaluation with sensitivity and specificity exceeding 99% for Enterobacterales [45].
Novel Technologies: The PathCrisp-NDM assay demonstrates the ability to detect as few as 700 copies of the NDM gene from clinical isolates, with 100% concordance with PCR-Sanger sequencing methods [12]. This sensitivity exceeds conventional PCR while operating at constant temperature.
Method Selection Guidance
Choosing the appropriate NDM detection method depends on multiple factors including laboratory infrastructure, required turnaround time, and patient population.
High-Throughput Clinical Laboratories: For facilities with advanced instrumentation, PCR-based systems like the Allplex Entero-DR or REALQUALITY Carba-Screen offer comprehensive resistance profiling with high sensitivity and specificity [46] [47]. These systems support infection control programs through efficient screening of surveillance specimens.
Rapid Response Settings: In critical care and oncology units where rapid results impact treatment decisions, the Xpert Carba-R assay provides results within 50 minutes directly from positive blood cultures [43]. This accelerated timeline enables earlier appropriate therapy for bloodstream infections.
Resource-Limited Environments: The NG-Test CARBA 5 immunochromatographic test offers a practical solution for laboratories without molecular infrastructure, providing results in 15 minutes at minimal cost [45]. The PathCrisp assay also shows promise for future point-of-care applications with its minimal equipment requirements [12].
Research and Surveillance Applications: For epidemiological studies and outbreak investigations, whole-genome sequencing remains the gold standard for comprehensive resistance gene detection, though it requires specialized bioinformatics expertise and remains cost-prohibitive for routine use [43] [48].
Leprosy, a chronic infectious disease caused by Mycobacterium leprae, continues to present significant diagnostic challenges that hinder eradication efforts. The current diagnostic paradigm relies heavily on clinical recognition of signs and symptoms, which requires specialized expertise increasingly scarce in many endemic regions [49]. While microscopy of slit-skin smears represents a historical "gold standard," this method suffers from low sensitivity (30-40%), particularly in paucibacillary (PB) forms of the disease that present with fewer bacilli [50]. The long incubation period of M. leprae further complicates early detection, allowing continued transmission within communities before diagnosis occurs [49].
In this context, serological assays and point-of-care tests (POCTs) detecting antibodies against M. leprae-specific antigens have emerged as promising tools to complement clinical diagnosis. These assays primarily target two categories of antigens: the phenolic glycolipid-I (PGL-I) and various protein antigens, notably the LID-1 fusion protein and its derivatives [51] [52]. The validation of these serological tools against traditional microscopy represents a critical advancement in leprosy diagnostics, offering potential for earlier detection, improved classification of clinical forms, and better identification of asymptomatic infections in household contacts.
Key Antigens and Their Serological Applications
Phenolic Glycolipid-I (PGL-I) and Synthetic Variants
PGL-I is a species-specific glycolipid located on the M. leprae cell wall that serves as a major immunological target in leprosy. The antigenicity of PGL-I is conferred by the terminal trisaccharide moiety, which is highly specific to M. leprae [53]. Detection of IgM antibodies against PGL-I correlates strongly with bacillary load, making it particularly useful for identifying multibacillary (MB) patients [49] [54]. The practical limitations of native PGL-I isolation have led to the development of synthetic analogs, including ND-O-BSA (natural disaccharide-octyl-bovine serum albumin), which mimics the immunodominant epitope of native PGL-I [50] [54].
Protein Antigens: LID-1 and NDO-LID
The LID-1 (leprosy IDRI diagnostic-1) antigen is a recombinant fusion protein combining the genes ml0405 and ml2331, which demonstrated improved sensitivity compared to the individual proteins alone [52]. Building on this concept, NDO-LID was created by conjugating LID-1 with a disaccharide mimetic of PGL-I, aiming to capture both antibody responses to protein antigens and the glycolipid PGL-I [51]. This chimeric antigen detects both IgM and IgG antibodies, potentially broadening its diagnostic utility across the leprosy spectrum [49].
Emerging Antigens and Platforms
Recent research has explored additional antigens, including MMP-II (major membrane protein-II), which induces primarily IgG responses and may complement PGL-I-based assays [54]. Innovative approaches include the development of mimotopes – synthetic peptides that mimic the carbohydrate epitopes of PGL-I – created using phage display technology to overcome the limited availability of native antigen [53]. These advancements have been incorporated into various diagnostic platforms, from conventional ELISA to rapid lateral flow tests and sophisticated biosensors utilizing surface plasmon resonance (SPR) technology [53].
Performance Comparison of Major Serological Assays
The diagnostic performance of serological tests varies significantly depending on the antigen used, leprosy classification (MB vs. PB), and population setting. The tables below summarize key performance metrics from recent studies.
Table 1: Comparative sensitivity of serological assays across leprosy classifications
| Antigen | Target Antibody | MB Sensitivity | PB Sensitivity | References |
|---|---|---|---|---|
| PGL-I (RDT) | IgM | 81.0% | 32.0% | [49] |
| NDO-LID (RDT) | IgM/IgG | 73.6% | 34.0% | [49] |
| LID-1 (ELISA) | IgG | 89.0% | Not reported | [52] |
| NDO-LID (ELISA) | IgM/IgG | 95.0% | Not reported | [52] |
| NDO-BSA (ELISA) | IgM | 94.9% | 42.9% | [54] |
| MMP-II (ELISA) | IgG | 84.7% | 47.6% | [54] |
Table 2: Specificity and predictive values of serological assays
| Antigen | Specificity | Positive Predictive Value | Negative Predictive Value | References |
|---|---|---|---|---|
| PGL-I (RDT) | 75.9% | 43.4% | 94.6% | [49] |
| NDO-LID (RDT) | 81.7% | 47.9% | 93.1% | [49] |
| LID-1 (ELISA) | 96.0% | Not reported | Not reported | [52] |
| NDO-LID (ELISA) | 88.0% | Not reported | Not reported | [52] |
| PGL-I Mimotope (ELISA) | 100% | Not reported | Not reported | [53] |
The data reveal consistent patterns across multiple studies. First, all serological assays demonstrate markedly higher sensitivity for MB cases compared to PB cases, reflecting the stronger antibody responses in MB patients [49] [54]. Second, while specificity is generally high, the moderate positive predictive values (PPV) indicate limitations in confirmatory diagnosis, whereas the high negative predictive values (NPV) suggest these tests are more reliable for excluding leprosy [49]. Third, the combination of different antigen types (glycolipid and protein) appears to enhance diagnostic performance, as evidenced by the improved sensitivity of the chimeric NDO-LID antigen [51] [52].
Experimental Protocols for Assay Validation
Serum Collection and Patient Classification
Robust validation of leprosy serological assays requires careful study design and standardized methodologies. In typical protocols, serum samples are collected from newly diagnosed, untreated leprosy patients classified according to Ridley-Jopling and WHO operational classifications (PB/MB) [51] [52]. Control groups should include endemic controls (healthy individuals from the same area), household contacts, and when assessing specificity, patients with other diseases such as tuberculosis that may cause cross-reactivity [50] [54]. All participants should provide informed consent, with studies approved by relevant ethics committees [49] [51].
ELISA Protocol for Anti-PGL-I/NDO-BSA Antibody Detection
The ELISA protocol for detecting anti-PGL-I antibodies follows these key steps:
- Coating: High-affinity polystyrene plates are coated with 50-100 ng/well of NDO-BSA antigen in carbonate/bicarbonate buffer (pH 9.6) and incubated overnight at 4°C [51] [54].
- Blocking: Plates are blocked with PBS containing 1-5% bovine serum albumin (BSA) for 1-2 hours at 37°C to prevent non-specific binding [53] [51].
- Sample Incubation: Serum samples diluted 1:100 to 1:300 in blocking buffer are added in duplicate and incubated for 1-2 hours at 37°C [53] [54].
- Secondary Antibody: Anti-human IgM conjugated with horseradish peroxidase (diluted 1:10,000) is added and incubated for 1-1.5 hours at 37°C [51].
- Detection: The reaction is developed using OPD (o-phenylenediamine dihydrochloride) or TMB (3,3',5,5'-tetramethylbenzidine) substrate, stopped with H₂SO₄, and absorbance read at 490-492 nm [51] [54].
- Cut-off Determination: Optimal cut-off values are typically established using Receiver Operating Characteristic (ROC) curve analysis comparing confirmed leprosy patients and endemic controls [50] [54].
Rapid Diagnostic Test (RDT) Protocol
Lateral flow immunochromatographic tests (such as PGL-I and NDO-LID RDTs) provide point-of-care alternatives:
- Sample Application: A small volume of serum, plasma, or whole blood is applied to the sample pad [49].
- Migration: The sample migrates by capillary action across the strip containing conjugated detection antibodies.
- Antigen-Antibody Reaction: If target antibodies are present, they bind to antigen-conjugated particles and subsequently to capture antigens at the test line.
- Result Interpretation: Results are visually interpreted after 10-20 minutes by trained personnel, with discordant results resolved by a third reader [49].
Quality Control Measures
To ensure reproducibility, studies should incorporate multiple quality control measures, including: testing samples in duplicate or triplicate, using standardized antigen batches, including positive and negative controls on each plate, and having two independent readers interpret RDT results with a third arbiter for discrepancies [49] [51].
Relationship Between Serological Responses and Disease Spectrum
Antibody responses in leprosy follow a distinct pattern across the clinical spectrum, reflecting the underlying immunology of the disease. Patients at the lepromatous pole (LL/BL) typically show strong Th2-skewed immune responses with high antibody titers but poor cellular immunity, resulting in uncontrolled bacterial multiplication [52]. In contrast, patients at the tuberculoid pole (TT/BT) mount robust Th1-mediated cellular responses that control bacterial growth but produce lower antibody levels [52]. This immunological gradient explains why MB patients consistently show higher seropositivity rates across all antigen types compared to PB patients [49] [54].
The quantitative antibody levels against both glycolipid and protein antigens show strong positive correlation with bacillary load [52]. One study reported correlation coefficients of r=0.84 for LID-1 and r=0.82 for LID-NDO with bacterial burden, demonstrating that antibody titers can serve as a proxy for disease severity [52]. This relationship enhances the utility of serological assays not just for diagnosis but also for stratifying patients according to transmission potential, as MB patients with high antibody titers are considered the main source of community transmission [51].
Comparison with Microscopy and Molecular Methods
Advantages Over Traditional Microscopy
When validated against microscopy as a reference standard, serological assays demonstrate several advantages. While microscopy has high specificity but low sensitivity (30-40%), particularly in PB cases, serological tests offer objectively quantifiable results, higher throughput, and less operator dependency [50]. Rapid serological tests additionally provide results within 15-20 minutes without requiring specialized equipment, making them suitable for field use in resource-limited settings [49]. The high negative predictive value of tests like PGL-I and NDO-LID (exceeding 93% in some studies) makes them valuable for excluding leprosy in diagnostic algorithms [49].
Complementary Role with Molecular Methods
Molecular methods such as PCR targeting the M. leprae-specific RLEP element offer superior sensitivity for detecting pauci-bacillary infection, with one study reporting 86.07% positivity in field cases [51]. However, PCR requires specialized equipment and technical expertise, limiting its application in resource-poor settings. Serological assays and PCR therefore play complementary roles: antibody detection identifies individuals with robust humoral responses (typically MB), while PCR can confirm infection in seronegative PB cases and household contacts [51]. Combining multiple diagnostic approaches provides the most comprehensive assessment of transmission dynamics, as demonstrated in geospatial studies overlaying different biomarker data [55].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents for leprosy serological studies
| Reagent / Material | Specifications | Research Application |
|---|---|---|
| NDO-BSA Antigen | Natural disaccharide-octyl-BSA conjugate, synthetic PGL-I analog | Coating antigen for ELISA, measure anti-PGL-I IgM responses [54] |
| LID-1 Antigen | Recombinant fusion protein (ml0405 + ml2331) | Detection of anti-M. leprae IgG antibodies, broad spectrum detection [52] |
| NDO-LID Antigen | Chimeric antigen (LID-1 + NDO disaccharide) | Simultaneous detection of IgM and IgG antibodies, improved sensitivity [49] [51] |
| Anti-Human IgM-HRP | Horseradish peroxidase conjugate, typically 1:10,000 dilution | Secondary antibody for PGL-I/NDO-BSA ELISA [51] |
| Anti-Human IgG-HRP | Horseradish peroxidase conjugate, typically 1:20,000 dilution | Secondary antibody for LID-1 ELISA [51] |
| OPD Substrate | o-phenylenediamine dihydrochloride | Chromogenic substrate for ELISA development [51] |
| PGL-I Mimotope | Synthetic peptide mimicking PGL-I carbohydrate epitope | Alternative to native PGL-I, high specificity (100% in studies) [53] |
Serological assays for leprosy based on PGL-I and LID-1 antigens represent significant advancements in the field of neglected tropical disease diagnostics. While these tests demonstrate limited sensitivity for detecting paucibacillary cases, their high negative predictive value, correlation with bacterial load, and point-of-care applicability make them valuable tools for screening programs and contact surveillance [49] [52]. The integration of multiple antigens in chimeric proteins like NDO-LID shows promise for enhancing diagnostic sensitivity across the leprosy spectrum [51].
Future developments should focus on combining serological markers with other biomarkers to create multiplex tests that can simultaneously assess infection status, disease classification, and transmission risk. As leprosy elimination efforts intensify, these serological tools will play an increasingly important role in identifying hidden prevalence, monitoring intervention effectiveness, and ultimately interrupting transmission chains. The lessons from leprosy serology also provide valuable insights for developing diagnostic strategies for other neglected tropical diseases where similar challenges exist.
Liquid biopsy, the analysis of tumor-derived components in bodily fluids, has emerged as a transformative approach in oncology [56]. Among its various targets, Circulating Tumor Cells (CTCs)—cancer cells shed into the bloodstream from primary or metastatic tumors—provide a complete biological entity for analysis [57] [58]. Their study offers unique insights into cancer metastasis, tumor heterogeneity, and therapeutic resistance [59]. However, CTCs are exceptionally rare, with concentrations as low as 1 cell per billion blood cells in early-stage cancer, presenting significant detection challenges [58].
Within this field, quantitative microscopy serves as a foundational tool and reference standard for validating emerging molecular assays. While advanced technologies like mass cytometry and genomic sequencing offer high-plex capabilities, microscopy provides direct, visual confirmation of CTC morphology, enumeration, and basic protein expression [60]. This article objectively compares current CTC analysis technologies, highlighting how quantitative microscopy remains integral for validating sophisticated molecular assays in the researcher's toolkit.
Comparative Analysis of CTC Detection Platforms
The following table summarizes the key operational characteristics and performance metrics of major CTC analysis platforms, illustrating the complementary roles of imaging and molecular techniques.
Table 1: Comparison of Major CTC Analysis Platforms
| Technology | Primary Principle | Key Metrics | Key Limitations | Validation Role |
|---|---|---|---|---|
| CellSearch | Immunomagnetic enrichment (EpCAM), fluorescent microscopy for identification (CK+, DAPI+, CD45-) [57] [61] | - FDA-cleared for prognostic use in metastatic breast, prostate, and colorectal cancer [61]- High standardization and reproducibility [61] | - Relies on EpCAM expression; may miss CTCs undergoing Epithelial-to-Mesenchymal Transition (EMT) [58] [59]- Limited to enumeration and basic phenotyping [57] | Imaging Gold Standard: Provides the reference method for CTC enumeration against which new assays are often validated [61]. |
| Parsortix PC1 | Microfluidic size-based and deformability-based capture (cells >6.5µm) [61] [60] | - Captures CTCs independent of surface markers, including EMT phenotypes [61]- Preserves cell viability for downstream culture and analysis [61] | - Throughput can be a limitation [58]- Purity depends on efficient leukocyte separation [58] | Platform for Assay Development: IsCTCsis are compatible with multiple downstream analysis methods, including microscopy and mass cytometry, facilitating validation workflows [60]. |
| Mass Cytometry (CyTOF) | High-parameter proteomic analysis using metal-tagged antibodies and time-of-flight detection [62] [60] | - High-Plex Capability: Simultaneously measures 41+ protein markers [60]- Resolves CTC heterogeneity (epithelial, early/advanced EMT) and signaling states [62] [60] | - Requires prior CTC enrichment- Destructive to cells; no possibility for live-cell analysis [60] | Beyond Microscopy: Extends phenotyping far beyond the scope of fluorescent microscopy, but often relies on microscopy-validated enrichment systems. |
Experimental Protocols for CTC Characterization
This section details specific methodologies cited in recent literature, demonstrating the integration of microscopy with advanced molecular techniques.
Protocol: Mass Cytometry for Deep Phenotyping of Head and Neck SCC CTCs
This protocol, adapted from a 2023 study, exemplifies high-plex proteomic validation using a microscopy-compatible platform [60].
- Step 1: Blood Collection and Preservation: Collect venous blood directly into Transfix blood collection tubes to stabilize cell phenotype for up to 72 hours, accommodating logistical delays in multi-center trials [60].
- Step 2: CTC Enrichment: Process fixed blood within 48 hours using the Parsortix PC1 system with a pressure of 99 bar and a 6.5 µm cutoff cassette to capture cells based on size and deformability [60].
- Step 3: Sample Preparation for Staining: Combine Parsortix-enriched cells with:
- Barcoded autologous PBMCs: Serve as carrier cells to minimize loss during processing.
- Osmium-labelled activated control cells: Provide a positive control for phospho-protein staining [60].
- Step 4: Mass Cytometry Staining and Acquisition: Stain the cell mixture with a pre-optimized panel of 41 metal-tagged antibodies targeting immune lineage, EMT, stemness, proliferation, immune checkpoints, and phosphorylated signaling proteins. Acquire data on a fluidigm Helios mass cytometer, maintaining an event rate below 500 events/second [60].
- Step 5: CTC Identification and Analysis: In the analysis software, gate on the Parsortix-enriched population. Identify CTCs as events with:
- Low expression: CD45 and immune lineage markers (CD3, CD14, etc.)
- Intermediate to high expression: Pan-cytokeratin (epithelial marker) [60].
- Key Outcome: The study detected CTCs in 13 out of 14 patients (2-24 CTCs/mL) and used unsupervised clustering to stratify them into epithelial, early EMT, and advanced EMT subgroups with distinct signaling pathway activation [60].
Protocol: Assessing Homologous Recombination in Breast Cancer CTCs
A 2025 study used mass cytometry to functionally characterize CTCs, moving beyond enumeration to direct assessment of drug resistance mechanisms [62].
- Step 1: Sample Collection: Collect longitudinal blood samples from metastatic breast cancer patients (e.g., 52 samples from 13 patients) [62].
- Step 2: Parallel Analysis:
- Enumerate CTCs using the CellSearch system as a reference.
- Isolate CTCs mixed with Peripheral Blood Mononuclear Cells (PBMCs) for mass cytometry.
- Collect plasma for cell-free DNA (cfDNA) analysis [62].
- Step 3: Functional Phenotyping by Mass Cytometry: Stain the CTC/PBMC mixture with a panel containing antibodies against:
- DNA damage response proteins: γH2AX, 53BP1, RAD51.
- Other relevant markers (13 antibodies total) [62].
- Step 4: Data Correlation: Correlate CyTOF-based CTC identification with CellSearch counts and cfDNA tumor fraction. Monitor the dynamics of DNA damage and Homologous Recombination (HR) status during genotoxic therapy [62].
- Key Outcome: The assay successfully identified CTCs, detected DNA damage, and monitored HR proficiency dynamics in real-time, providing a method to identify emerging chemoresistance [62].
Visualizing Workflows and Biological Pathways
The following diagrams illustrate the core experimental workflow and a key biological process in CTC analysis.
Diagram 1: High-Plex CTC Proteomic Workflow. This workflow integrates sample preservation, enrichment, and mass cytometry to achieve deep single-cell proteomic characterization of CTCs [60].
Diagram 2: EMT in CTC Biology. EMT is a key molecular process that alters CTC phenotype, impacting detection by marker-dependent platforms like CellSearch and contributing to therapy resistance [58] [59].
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of the described protocols relies on a suite of specialized research reagents and platforms.
Table 2: Essential Research Reagent Solutions for CTC Analysis
| Category / Item | Specific Example | Critical Function in CTC Workflow |
|---|---|---|
| Blood Collection & Preservation | Transfix Blood Collection Tubes | Stabilizes cell surface epitopes and phosphorylation states for up to 72h, critical for multi-center trials [60]. |
| CTC Enrichment Systems | Parsortix PC1 Cassette (6.5µm) | Captures CTCs based on size/deformability, independent of EpCAM, preserving cell viability [61] [60]. |
| Immunomagnetic Enrichment | CellSearch CTC Test | FDA-cleared, immunomagnetic (EpCAM) system for standardized CTC enumeration; used as a prognostic benchmark [57] [61]. |
| High-Plex Antibody Panels | Mass Cytometry Panel (41-plex) | Metal-tagged antibodies allow simultaneous single-cell analysis of lineage, EMT, checkpoint, and phospho-protein markers [62] [60]. |
| Carrier Cells for Processing | Autologous PBMCs (Barcoded) | Added during staining to minimize non-specific cell loss of rare CTCs, improving assay robustness and recovery [60]. |
| Controls for Signaling Assays | Osmium-labelled Activated PBMCs | Serves as an internal positive control for phospho-specific antibody staining across multiple patient samples [60]. |
The field of CTC analysis is advancing from simple enumeration toward deep functional characterization at the single-cell level [62] [60]. In this evolving landscape, quantitative microscopy remains the foundational gold standard for initial validation of CTC enrichment efficiency and morphological confirmation. However, as demonstrated, its role is powerfully complemented by high-plex proteomic and genomic technologies that can unravel CTC heterogeneity, EMT status, and dynamic drug resistance mechanisms [62] [59] [60].
The future of CTC biomarker analysis lies in integrated workflows that leverage the strengths of each technology: the visual certainty of microscopy, the phenotypic breadth of mass cytometry, and the mutational insight of sequencing. For researchers and drug developers, this multi-platform approach, built on a foundation of rigorous validation, is key to unlocking the full potential of CTCs in precision oncology.
Solving the Puzzle: Overcoming Common Hurdles in Assay Development
The pre-analytical phase—encompassing specimen collection, handling, and processing—is a fundamental component of laboratory medicine that profoundly influences the reliability of diagnostic results [63]. Inaccuracies during this phase account for a substantial proportion of laboratory testing errors, potentially rendering samples useless for subsequent analysis [64] [65]. For molecular assays, particularly those validated against traditional methods like microscopy, controlling pre-analytical variables becomes paramount to ensure diagnostic accuracy and meaningful comparison between methodologies [1] [66]. This guide objectively compares how key pre-analytical factors—sample preparation approaches, nucleic acid extraction efficiency, and blood volume requirements—impact assay performance, providing researchers with evidence-based data to optimize their diagnostic workflows.
The validation of any molecular method against an established gold standard, such as microscopy, requires meticulous attention to pre-analytical conditions to ensure fair and accurate comparison [1] [66]. As molecular techniques like PCR and digital PCR (ddPCR) offer increasingly sensitive detection of pathogens and biomarkers, the influence of pre-analytical handling on the analyte of interest becomes more pronounced [67] [68]. This guide examines the experimental evidence surrounding these critical variables to support researchers in developing robust, standardized protocols that minimize pre-analytical bias and enhance diagnostic reproducibility across laboratory settings.
Sample Collection & Processing: Foundation for Quality Results
The initial steps of sample collection and processing establish the foundation for all subsequent analyses. Variations in these early stages can introduce significant artifacts that compromise data integrity and comparability between different analytical methods.
Blood Collection Tube Selection and Processing Timelines
The choice of blood collection tubes and adherence to processing timelines significantly impact sample quality, particularly for metabolomic and cell-free DNA (cfDNA) analyses. Experimental comparisons have demonstrated that different tube types maintain analyte stability under varying conditions.
Table 1: Comparison of Blood Collection Protocols for Plasma Preparation
| Collection Protocol | Mean LMW GE/mL Plasma | Low Molecular Weight (LMW) Fraction | Significant Differences | Key Applications |
|---|---|---|---|---|
| EDTA tubes (processed within 1 hour) | 1,925 [67] | 87% [67] | Reference standard | cfDNA analysis, metabolomics [67] [68] |
| Cell-free DNA BCT (processed within 24 hours) | 1,591 [67] | 88% [67] | No significant difference in yield or LMW fraction vs. EDTA [67] | Multi-center studies, delayed processing [67] |
| Cell-free DNA BCT (processed within 72 hours) | 1,514 [67] | 90% [67] | No significant difference in yield or LMW fraction vs. EDTA [67] | Biobanking, transport logistics [67] |
The experimental data from a study of 23 healthy volunteers revealed no statistically significant differences in cfDNA yield or fragment size between EDTA tubes processed within 1 hour and cell-free DNA blood collection tubes (BCTs) processed within 24 or 72 hours [67]. This demonstrates that specialized collection tubes can effectively maintain sample integrity for molecular analyses when immediate processing is not feasible, a common challenge in clinical practice and multi-center research studies.
Plasma versus Serum Matrix Considerations
The decision between plasma and serum as a matrix for analysis introduces specific pre-analytical artifacts that must be considered during experimental design. Methodological studies have quantified differences between these matrices:
- Serum Preparation: Requires room temperature exposure for 30-60 minutes to allow clotting, during which cellular metabolism continues and platelets release metabolites including lysophosphatidylcholines, serotonin, and various amino acids [69]. This process results in generally higher absolute analyte counts and elevated concentrations of many metabolites compared to plasma [69] [67].
- Plasma Preparation: Utilizes anticoagulants and immediate centrifugation to separate cellular components, better preserving the in vivo metabolic state but retaining platelets that can contribute to inter-sample variability, particularly with differential centrifugation protocols [69].
The experimental evidence indicates that serum tends to demonstrate higher sensitivity for detecting group differences in disease states, while plasma typically offers greater analytical reproducibility, as demonstrated by higher mean correlation coefficients (0.83 in plasma versus 0.80 in serum) in paired samples [69]. This trade-off between sensitivity and reproducibility should guide matrix selection based on specific research objectives.
Nucleic Acid Extraction Efficiency: Comparative Performance of Isolation Methods
Nucleic acid extraction represents a critical pre-analytical step that directly impacts downstream analytical sensitivity and reliability. Significant variability in extraction efficiency exists among different kits and methodologies.
Experimental Comparison of cfDNA Extraction Kits
A rigorous methodological comparison evaluated seven different cfDNA extraction kits (three spin column-based and four magnetic beads-based) using a pooled control plasma sample with 10 replicates per kit [67]. The study employed a multiplexed droplet digital PCR (ddPCR) assay targeting 9 single-copy genomic loci to precisely quantify both cfDNA yield and fragment size distribution.
Table 2: Extraction Kit Performance Comparison for cfDNA Isolation
| Extraction Method | Median LMW Yield (GE/mL plasma) | Median LMW Fraction | Yield Variability | Technology Type |
|---|---|---|---|---|
| Kit A | 1,936 [67] | 89% [67] | Low variability | Spin column |
| Kit B | 1,760 [67] | Not specified | Higher variability | Spin column |
| Kit E | 1,515 [67] | 90% [67] | Not specified | Magnetic beads |
| Inter-Kit Comparison | ANOVA p = 5.01 × 10⁻¹¹ [67] | ANOVA p = 1.16 × 10⁻¹¹ [67] | Wide variability across all kits | Both technologies |
The experiments revealed statistically significant differences in both cfDNA yield and fragment size distribution across the tested kits [67]. Kit A (spin column-based) demonstrated the highest median yield of LMW cfDNA, while Kit E (magnetic beads-based) showed comparable LMW fraction but significantly lower yield [67]. These findings highlight that extraction methodology selection can substantially influence the quantity and quality of recovered nucleic acids, potentially affecting downstream diagnostic sensitivity.
Impact of Extraction Efficiency on Diagnostic Sensitivity
The efficiency of nucleic acid extraction directly impacts the diagnostic sensitivity of molecular assays, particularly when validating against less sensitive gold standard methods like microscopy. In clinical validation studies for leishmaniasis diagnosis, qPCR assays targeting both 18S rDNA and HSP70 genes demonstrated significantly improved sensitivity compared to traditional microscopy examination of lesion imprints or biopsy specimens [66]. The implementation of optimized extraction protocols contributed to the qPCR assays achieving 98.5% sensitivity and 100% specificity when testing 88 clinical samples from patients with different clinical forms of American Tegumentary Leishmaniasis [66]. This enhanced detection capability underscores how proper pre-analytical handling, including efficient nucleic acid extraction, enables molecular methods to identify true positive cases that might be missed by conventional techniques with lower inherent sensitivity.
Blood Volume and Sample Quality: Minimum Requirements and Effects
Adequate blood volume collection is essential for obtaining reliable results, while insufficient volumes can compromise analytical quality and diagnostic accuracy.
Optimal Blood Volume Recommendations
Evidence-based guidelines specify minimum blood volumes required for different laboratory testing scenarios:
- Standard clinical chemistry testing (20 analytes): 3-4 mL of whole blood for heparinized plasma; 4-5 mL for serum [65]
- Hematology testing: 2-3 mL of EDTA blood [65]
- Coagulation studies: 2-3 mL of citrated blood [65]
- Immunoassays: 1 mL of whole blood sufficient for 3-4 immunoassays [65]
- Blood gas analysis: 50 μL arterial blood for capillary sampling; 1 mL heparinized blood for venous sampling [65]
These volume recommendations account for both the analytical volume required for testing and the dead volume of sample cups, replicates, and secondary tubes [65]. Calculating optimal sample volume safeguards patients from excessive blood collection while ensuring sufficient material for accurate analysis.
Consequences of Inadequate Sample Volume
Insufficient sample volume can introduce significant analytical errors that compromise diagnostic validity. A documented case report illustrates this phenomenon: an 85-year-old female patient showed dramatically discrepant hematology results (hemoglobin: 22.9 g/dL vs. previous 10.3 g/dL) from an overfilled blood collection tube [65]. The overfilled tube prevented proper mixing on a rocking mixer, yielding invalid results. Only after sufficient blood was aspirated to create adequate headspace did the mixing become effective and generate results consistent with previous measurements [65]. This case demonstrates how proper sample volume relative to container size is critical for adequate mixing and accurate analytical results.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Pre-Analytical Optimization
| Reagent/Material | Function | Application Examples | Experimental Considerations |
|---|---|---|---|
| Cell-free DNA BCTs | Stabilizes nucleated blood cells for up to 72 hours | Multi-center studies, delayed processing | No significant difference in cfDNA yield vs. EDTA with immediate processing [67] |
| EDTA Tubes | Standard anticoagulant for plasma preparation | cfDNA analysis, metabolomics | Requires processing within 1 hour for optimal results [67] |
| Droplet Digital PCR (ddPCR) | Absolute quantification of nucleic acid molecules | Extraction efficiency validation, fragment size analysis | Enables precise quantification of amplifiable DNA concentration and fragment size [67] |
| Spin-column Extraction Kits | Nucleic acid purification based on binding to silica membranes | DNA/RNA isolation from plasma, serum | Highest demonstrated yield for cfDNA extraction in comparative studies [67] |
| Magnetic Beads Extraction Kits | Nucleic acid purification using magnetic particle technology | High-throughput automation, DNA/RNA isolation | Lower yield but comparable LMW fraction to best spin-column kits [67] |
Integrated Workflow: From Sample Collection to Analysis
The relationship between pre-analytical variables and their impact on final analytical results follows a logical pathway that researchers must understand to properly design experiments and interpret data.
This workflow diagram illustrates how pre-analytical decisions directly impact sample quality metrics, which subsequently determine the reliability of analytical outcomes and concordance with gold standard methods.
The experimental data comprehensively demonstrate that pre-analytical variables exert substantial effects on sample quality and subsequent analytical performance. Key findings indicate that extraction kit selection can cause statistically significant variations in cfDNA yield (ANOVA p = 5.01 × 10⁻¹¹) and fragment size distribution (ANOVA p = 1.16 × 10⁻¹¹) [67]. Specialized blood collection tubes enable extended processing windows without compromising sample integrity [67]. Sample volume adequacy is critical for preventing analytical errors caused by inadequate mixing or insufficient material [65].
For researchers validating molecular assays against microscopy gold standards, controlling these pre-analytical factors is essential for meaningful methodological comparisons. Standardized protocols must be implemented across all sample processing stages to minimize technical variability and ensure that observed differences reflect true biological signals or genuine methodological performance characteristics rather than pre-analytical artifacts. By adhering to evidence-based practices for sample preparation, extraction efficiency optimization, and blood volume management, researchers can enhance the reliability and reproducibility of their molecular diagnostics validation studies, ultimately advancing the implementation of robust clinical assays.
The validation of modern molecular assays against established gold standards, such as microscopy, demands rigorous analytical optimization to ensure accuracy, sensitivity, and reliability. This process hinges on three fundamental pillars: the strategic design of primers and probes, the precise measurement and control of amplification efficiency, and the effective management of reaction inhibitors. These elements collectively determine whether a molecular test can outperform or effectively supplement traditional methods by providing faster, more sensitive, and more specific detection of pathogens or genetic markers.
The following sections provide a detailed, evidence-based comparison of optimization strategies, supported by experimental data and protocols. This guide is structured to equip researchers with the practical knowledge to refine their molecular assays, particularly in contexts like validating new diagnostic tests against conventional microscopy for disease diagnosis [70].
Primer and Probe Design: Principles and Comparison
Optimal primer and probe design is the first critical step in developing a robust molecular assay. Poorly designed oligonucleotides can lead to non-specific amplification, primer-dimer formation, and reduced sensitivity, ultimately compromising assay performance.
Core Design Principles
The table below summarizes the key design parameters for PCR primers and hydrolysis probes, as recommended by industry standards [71].
Table 1: Key Design Parameters for PCR Primers and Probes
| Parameter | PCR Primers | qPCR Probes | Rationale |
|---|---|---|---|
| Length | 18–30 bases | 20–30 bases (single-quenched) | Balances specificity and binding energy. |
| Melting Temperature (Tm) | 60–64°C (ideal 62°C) | 5–10°C higher than primers | Ensures probe binds before primers for efficient hydrolysis. |
| Difference between Primer Tms | ≤ 2°C | Not Applicable | Allows simultaneous binding of both primers. |
| GC Content | 35–65% (ideal 50%) | 35–65% | Provides sequence complexity; avoids extreme structures. |
| Specific Sequence Warnings | Avoid ≥ 4 consecutive Gs | Avoid G at 5' end | Prevents quadruplex formation (primers) and fluorophore quenching (probes). |
| Complementarity Checks | ΔG > -9 kcal/mol for self-dimers, hairpins, and heterodimers. | Minimizes secondary structures and off-target interactions. |
Advanced Considerations and Comparative Performance
Beyond these core principles, advanced strategies can further enhance performance. For multi-template PCR, used in high-throughput sequencing and metagenomics, sequence-specific amplification biases can severely skew results. Recent work demonstrates that deep learning models (1D-CNNs) can predict a sequence's amplification efficiency based solely on its sequence, achieving an AUROC of 0.88. This approach identified adapter-mediated self-priming as a key mechanism behind poor amplification, challenging traditional design assumptions [72].
Furthermore, assay format influences design. The PathCrisp assay, which combines loop-mediated isothermal amplification (LAMP) with CRISPR/Cas12a detection, requires a different design philosophy. Its LAMP component uses six primers targeting eight distinct regions of the NDM gene, while its CRISPR component relies on a specific single-guide RNA (sgRNA) for detection. This combined approach demonstrated 100% concordance with PCR-Sanger sequencing but with greater sensitivity and a faster turnaround of approximately 2 hours [12].
Table 2: Comparison of Amplification Assay Characteristics
| Assay Type | Typical Amplicon Length | Key Design Consideration | Reported Sensitivity |
|---|---|---|---|
| Standard qPCR | 70–150 bp (up to 500 bp possible) | Amplicon should span an exon-exon junction to avoid gDNA amplification [71]. | Varies with optimization; gold standard for quantification [73]. |
| Multi-template PCR (for NGS) | Library-dependent | Homogeneous efficiency across templates is critical; deep learning can predict poor amplifiers [72]. | Non-homogeneous amplification can drown out ~2% of sequences [72]. |
| LAMP-CRISPR (PathCrisp) | Target-dependent (NDM gene) | Requires design of 6 LAMP primers and a specific CRISPR sgRNA [12]. | Detected as few as 700 copies of the NDM gene from clinical isolates [12]. |
Amplification Efficiency: Quantification and Impact
Amplification efficiency (E) is a quantitative measure of how effectively a target sequence is duplicated in each PCR cycle. It is foundational for accurate data interpretation, especially in quantitative real-time PCR (qPCR).
Defining and Calculating Efficiency
The ideal amplification efficiency is 100% (E=1.0), representing a perfect doubling of product every cycle. Efficiency is most accurately calculated from a standard curve of serial dilutions. The slope of the trend line of Ct (threshold cycle) versus log concentration is used in the equation: E = -1 + 10^(-1/slope). An ideal slope of -3.32 corresponds to 100% efficiency [74].
An alternative method that does not require a standard curve calculates the starting template quantity (R0) directly from the amplification profile using the formula: R0 = RCt × (1 + E)^–Ct, where RCt is the fluorescence at the threshold cycle. This method involves calculating a unique amplification efficiency (E) for each sample by performing linear regression on the log-linear phase of its amplification plot [73].
Causes and Implications of Abnormal Efficiency
Efficiencies consistently below 90% typically indicate poor reaction optimization, suboptimal primer design, or the presence of inhibitors. Perhaps counterintuitively, efficiencies exceeding 100% are a common artifact and often signal the presence of polymerase inhibitors in the more concentrated samples of a dilution series. In this scenario, inhibitors are diluted out along with the template, causing ΔCt values between dilutions to be smaller than expected, which flattens the standard curve's slope and inflates the calculated efficiency [74].
The impact of even small efficiency variations is profound due to the exponential nature of PCR. A template with an efficiency just 5% below the average will be underrepresented by a factor of two after only 12 cycles. After 26 cycles, a 5% difference can result in one sample having twice as much product as another that started with the same initial concentration [72] [73].
Managing Amplification Inhibitors
Inhibitors are substances that co-purify with nucleic acids and disrupt enzymatic reactions, leading to false negatives, reduced sensitivity, and skewed quantitative results.
Inhibitors can originate from the sample itself (e.g., hemoglobin from blood, polysaccharides from plants, bile salts from feces) or from the nucleic acid extraction process (e.g., phenol, ethanol, or SDS) [74]. In clinical settings, samples like sputum for tuberculosis testing are particularly prone to inhibition.
Strategies for Inhibition Management
Several proven strategies can mitigate the effects of inhibitors:
- Sample Dilution: Diluting the sample is a simple and effective way to reduce inhibitor concentration below a critical threshold [74].
- Nucleic Acid Purification: Using silica-column based purification or agent purification can remove many common inhibitors. Spectrophotometric measurement (A260/A280 ratio) can assess sample purity, with ratios above 1.8 for DNA and 2.0 for RNA indicating acceptable purity [74].
- Alternative Polymerase Systems: Using specialized polymerase enzymes or master mixes formulated to be more tolerant of inhibitors can be highly effective [74].
- Simplified Extraction Protocols: For point-of-care applications, simplified protocols such as crude extraction via heating, as used in the PathCrisp assay, can circumvent the need for complex, inhibitor-prone purification kits while still delivering results [12].
Experimental Protocols for Key Validations
Protocol: Calculating Amplification Efficiency from Amplification Plots
This protocol allows for efficiency calculation without a standard curve [73].
- Run qPCR: Perform the real-time PCR assay under optimized conditions.
- Determine Background and Maximum Fluorescence: Calculate the background noise (Rnoise) as the standard deviation of fluorescence from cycles 1-10. Determine the maximum fluorescence (Rmax) of the amplification plot.
- Find the Linear Range Midpoint: Calculate the midpoint (M) of the logarithmic signal range using the formula: M = Rnoise × √(Rmax / Rnoise).
- Perform Linear Regression: Using a 10-fold fluorescence range around M, perform a linear regression of log(fluorescence) versus cycle number. The slope of this line is used to calculate efficiency: E = 10^(1/slope) - 1.
Protocol: PathCrisp LAMP-CRISPR Assay for NDM Detection
This two-step protocol demonstrates an optimized, inhibitor-resistant method [12].
- Crude DNA Extraction: Boil a bacterial colony or culture sample for 10 minutes, then centrifuge. The supernatant contains the crude DNA template.
- Isothermal Amplification:
- Reaction Setup: Combine 1 µl of crude DNA extract with 5 µl of 2x LAMP reaction buffer, 0.4 µl of Bst 1.0 enzyme, and LAMP primers (0.2 µM outer primers, 1.6 µM inner primers, 0.4 µM loop primers).
- Incubation: Incubate the reaction at 60°C for 1 hour.
- CRISPR/Cas12a Detection:
- Detection Mix Preparation: Pre-incubate 26 nM sgRNA, 26 nM Cas12a enzyme, and 200 nM ssDNA-FQ reporter in 1x NEBuffer 2 at room temperature for 10 minutes.
- Detection: Add 10 µl of the LAMP product to the detection mix and incubate at 37°C. Monitor fluorescence in real-time (excitation 480 nm, emission 520 nm). A positive signal is indicated by a rapid increase in fluorescence.
Visualizing Workflows and Relationships
Assay Optimization Workflow
This diagram outlines the iterative process of molecular assay optimization, highlighting how primer design, efficiency evaluation, and inhibitor management are interconnected.
Why qPCR Efficiency Exceeds 100%
This causal diagram illustrates the mechanism by which inhibitors in a sample can lead to an artifactual calculation of amplification efficiency exceeding 100%.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Reagent Solutions for Molecular Assay Optimization
| Reagent/Material | Function/Purpose | Example Use Case |
|---|---|---|
| WarmStart Multi-Purpose LAMP/RT-LAMP Master Mix (with UDG) | Isothermal amplification with UDG to prevent carryover contamination [12]. | PathCrisp assay for NDM gene detection [12]. |
| AltR L.b. Cas12a (Cpf1) Ultra | CRISPR effector enzyme for specific nucleic acid detection via collateral cleavage [12]. | Post-amplification detection in PathCrisp assay [12]. |
| ssDNA-FQ Reporter (e.g., /56-FAM/TTATT/3IABkFQ) | Fluorescent reporter molecule; cleavage produces detectable signal [12]. | Real-time fluorescence detection in CRISPR-based assays [12]. |
| Double-Quenched Probes (e.g., with ZEN/TAO) | qPCR probes with internal quenchers for lower background and higher signal-to-noise [71]. | Standard qPCR assays requiring high sensitivity [71]. |
| Inhibitor-Tolerant Polymerase Master Mixes | Specialized enzyme blends resistant to common PCR inhibitors [74]. | Amplification from complex samples (blood, sputum, soil). |
| NEBuffer 2.1 | Optimized reaction buffer for CRISPR/Cas enzyme activity [12]. | Maintaining optimal Cas12a trans-cleavage activity [12]. |
In the validation of molecular assays, microscopy often serves as a gold standard for providing spatial context and direct visual confirmation. However, the journey from raw image data to quantitative insights is fraught with technical challenges. As microscopy technology diversifies and becomes more complex, the problem of accurate image quantification has emerged as a major roadblock across biological and biomedical research. All researchers face universal challenges in transforming microscopy images into reliable answers, regardless of their specific scientific questions or the images they generate. These difficulties can arise at multiple stages—from initial file handling and image pre-processing to object segmentation and final measurement. This guide objectively compares current solutions and methodologies, providing researchers with experimental frameworks for validating their image analysis workflows against the rigorous demands of molecular assay development.
Current Landscape of Image Analysis Solutions
The bioimage analysis software ecosystem contains diverse tools with varying capabilities, approaches, and performance characteristics. Understanding this landscape is essential for selecting appropriate methodologies for assay validation.
Table 1: Comparison of Image Analysis Tools and Approaches
| Tool/Approach | Primary Methodology | Automation Level | Dimensionality | Key Performance Metrics |
|---|---|---|---|---|
| TrueSpot | Automated threshold selection algorithm | Fully automated | 2D & 3D image stacks | Higher precision and recall vs. Big-FISH, RS-FISH [75] |
| Cellpose | Deep learning-based segmentation | User-adjustable parameters | 2D | Cell segmentation from brightfield images [76] |
| Custom Python Pipeline (skimage, Cellpose) | Traditional image analysis + deep learning | Semi-automated with manual review | 2D multi-channel | Background subtraction, fluorescence quantification [76] |
| Fractal Dimension Analysis | Box-counting algorithm | Manual threshold setting | 2D & 3D | Chromatin pattern differentiation [77] |
The performance disparities between these tools highlight a critical consideration for researchers: the tradeoff between automation and control. TrueSpot addresses the fundamental challenge of threshold selection—a traditionally subjective step that introduces variability—through its automated algorithm that adapts to varying background noise and signal intensity [75]. Conversely, tools like Cellpose integrated into custom Python pipelines offer more transparent parameter adjustment, enabling researchers to maintain oversight at the cost of increased manual intervention [76].
Experimental Protocols for Workflow Validation
Protocol 1: Automated Signal Puncta Quantification with TrueSpot
Application Context: Validation of gene expression assays using RNA-FISH or immunofluorescence.
Methodology Details:
- Image Acquisition: Collect fluorescent images using standardized parameters across experimental conditions. For 3D analysis, acquire z-stacks with appropriate step sizes [75].
- Software Setup: Access TrueSpot through its graphical interface or command line. For high-throughput processing, utilize computer cluster capabilities [75].
- Processing Parameters: The tool automatically sets detection thresholds using multiple approaches to distinguish true signals from background noise without manual intervention [75].
- Data Extraction: TrueSpot outputs quantified signal puncta with precision and recall metrics, enabling direct comparison between experimental conditions [75].
- Validation: Compare results with manual counts from a subset of images to verify accuracy, particularly for novel assay conditions.
Protocol 2: Cell Segmentation and Fluorescence Quantification
Application Context: Cellular response assays in yeast or mammalian cells.
Methodology Details:
- Image Preparation: Acquire multi-position, multi-channel 2D data in .nd2 format or similar. Ensure brightfield and fluorescence channels are properly aligned [76].
- Cell Segmentation: Employ Cellpose for segmenting cells from brightfield images. Adjust segmentation parameters based on cell type and morphology [76].
- Quality Control: Use the napari package to visually inspect segmentation accuracy and adjust parameters as needed [76].
- Fluorescence Quantification: Calculate fluorescence intensities within segmented cell regions using skimage and basic Python modules. Compute background signal from areas outside segmented regions and subtract from fluorescence measurements [76].
- Data Analysis Options:
- Total fluorescence per cell
- Pixel-level fluorescence intensity values
- Statistical comparison using Kolmogorov-Smirnov test for distribution analysis [76]
Protocol 3: Nuclear Chromatin Pattern Characterization
Application Context: Epigenetic assay validation and nuclear organization studies.
Methodology Details:
- Sample Preparation: Fix cells with 4% formaldehyde solution, stain with 2.5 μM Hoechst, and mount with antifade reagent [77].
- Image Acquisition: Use confocal microscopy with diffraction-limited resolution (approximately 250 nm in xy focal plane). Set pixel size to 100 nm following Nyquist-Shannon rule [77].
- Fractal Dimension Analysis:
- Crop individual nuclei from larger images
- Equalize intensity distribution (saturated pixels set to 0.35%)
- Binarize image using manual threshold at peak fluorophore intensity
- Apply box-counting algorithm to calculate fractal dimension [77]
- Additional Parameters:
Workflow Visualization
Image Analysis Workflow with Key Challenge Points
Research Reagent Solutions for Image Analysis Workflows
Essential materials and computational tools form the foundation of reliable image analysis. The table below details key resources for implementing the experimental protocols described.
Table 2: Essential Research Reagents and Computational Tools
| Category | Specific Item | Function/Application | Example Use Cases |
|---|---|---|---|
| Cell Lines | HeLa, HepG2 | Nuclear chromatin pattern studies | Differentiation of chromatin organization between cell types [77] |
| Fluorescent Labels | Hoechst | Nuclear DNA staining | Chromatin distribution analysis in fixed cells [77] |
| Analysis Software | TrueSpot | Automated signal puncta detection | RNA-FISH, immunofluorescence quantification [75] |
| Analysis Software | Cellpose | Deep learning-based cell segmentation | Cell boundary identification in brightfield images [76] |
| Analysis Software | Fiji/ImageJ | Fundamental image processing and analysis | Fractal dimension calculation, edge detection [77] |
| Computational Environment | Python Jupyter Notebook | Custom analysis pipeline development | Multi-channel fluorescence intensity analysis [76] |
| Specialized Buffers | ProLong Glass Antifade | Sample preservation for fluorescence microscopy | Maintaining signal intensity during imaging [77] |
The evolution of image analysis tools represents a paradigm shift in how researchers approach microscopy data, moving from subjective manual quantification toward automated, reproducible workflows. TrueSpot's automated thresholding addresses one of the most significant sources of variability, while deep learning tools like Cellpose demonstrate the power of AI-assisted segmentation. Custom Python pipelines offer flexibility for specialized applications, and quantitative parameters like fractal dimension provide new avenues for characterizing subcellular patterns. For researchers validating molecular assays, the integration of these tools creates a robust framework for establishing microscopy as a reliable gold standard. By implementing standardized protocols, leveraging automated tools where appropriate, and maintaining rigorous validation checkpoints, the scientific community can overcome persistent challenges in image analysis and generate more reproducible, quantitatively accurate data for drug development and basic research.
In the validation of molecular assays against microscopy gold standards, instrument calibration transitions from a routine maintenance task to a fundamental component of research integrity. The convergence of advanced optical systems and computational imaging has redefined the limits of detection and resolution in life sciences. Calibration ensures that the data generated by increasingly sophisticated instruments accurately reflects biological reality rather than optical artifacts or electronic noise. This guide provides a systematic comparison of calibration methodologies and their performance impact across different detection system types, with a specific focus on the critical parameters of wavelength, focal height, and gain optimization. Within the framework of assay validation, proper calibration forms the bedrock upon which reliable correlations between molecular data and morphological gold standards are built, enabling researchers and drug development professionals to make confident decisions based on their experimental results.
Comparative Analysis of Detection System Calibration Approaches
The table below summarizes the performance characteristics of three dominant detection system types, highlighting how their calibration requirements impact key performance metrics relevant to assay validation.
Table 1: Performance Comparison of Detection System Types
| System Type | Optimal Resolution After Calibration | Key Calibration Parameters | Throughput/Field of View | Best Suited Assay Validation Context |
|---|---|---|---|---|
| SPI Super-Resolution Microscopy | 116 ± 9 nm (after deconvolution) [78] | Multifocal alignment, TDI sensor synchronization, WB deconvolution [78] | Up to 1.84 mm²/s (5,000-10,000 cells/s) [78] | High-throughput subcellular analysis requiring correlation of molecular data with sub-diffraction-limited structures |
| Computational Imaging (FPM/SIM) | Varies with synthetic NA (e.g., 10x with FPM) [79] | Illumination angle sequencing, phase retrieval algorithms, aperture synthesis [79] | Large FOV with synthetic aperture [79] | Cost-effective resolution enhancement for 2D and 3D quantitative phase imaging |
| High-Precision Astrometric Systems | Sub-microarcsecond precision (for exoplanet detection) [80] | Focal plane pixel grid calibration, line of sight distortion mapping [80] | Targeted star fields with gigapixel focal planes [80] | Specialized applications requiring extreme geometric fidelity; provides conceptual framework for nanoscale precision |
The selection of an appropriate detection system must align with the specific requirements of the assay validation workflow. For instance, Super-resolution Panoramic Integration (SPI) microscopy demonstrates how coordinated calibration of multiple parameters enables unprecedented combination of resolution and throughput, making it particularly valuable for validating molecular markers across large cell populations while maintaining subcellular resolution [78].
Experimental Protocols for Core Calibration Procedures
Protocol 1: Wavelength Calibration and Spectral Accuracy Verification
Objective: To ensure accurate wavelength detection across the instrument's spectral range, critical for multiplexed assays and fluorescence validation.
- Reference Standard Selection: Use certified reference materials (CRMs) with known, stable emission spectra (e.g., rare-earth-doped glasses or fluorescent dyes with characterized peaks) [81].
- Data Acquisition: Acquire emission spectra of the reference standard across the intended wavelength range. For imaging systems, capture flat-field images at multiple discrete wavelengths if using monochromatic illumination [81].
- Peak Identification and Mapping: Identify the centroid positions of known emission peaks in the acquired data. Plot these measured positions against their certified values.
- Calibration Function Generation: Fit a regression model (linear or higher-order, depending on system design) to the peak mapping data. This function translates measured pixel or channel values to true wavelengths.
- Validation: Verify calibration accuracy using a different CRM than the one used for calibration. The mean error should fall within the manufacturer's specifications for the instrument.
Protocol 2: Focal Plane Calibration and Flat-Fielding
Objective: To correct for spatial non-uniformity in illumination and detection pathways, and to ensure consistent focus across the entire field of view.
- Uniform Source Application: Image a uniformly fluorescent sample or a calibrated reflectance slide. For systems without physical standards, computational methods like Fourier ptychography microscopy (FPM) can synthesize a flat-field reference [79].
- Flat-Field Image Calculation: Acquire multiple images of the uniform source and average them to create a master flat-field image that maps pixel-to-pixel sensitivity variations.
- Application to Experimental Data: Divide raw experimental images by the normalized flat-field image. This corrects for vignetting, uneven illumination, and varying pixel sensitivity.
- Focal Height Optimization: For automated systems, perform a z-stack through the focal plane of a sample with well-defined features (e.g., fluorescent beads). Determine the optimal focal height by identifying the z-position that maximizes sharpness metrics (e.g., gradient energy) or minimizes the point-spread function (PSF) width [80].
- Mapping Focal Height: For large fields, this process may be repeated at multiple XY positions to create a focal map that the system can use to maintain consistent focus during stage movement.
Protocol 3: Gain and Linearity Calibration for Quantitative Accuracy
Objective: To establish the linear response of the detection system across its dynamic range, essential for quantitative comparisons in assay validation.
- Reference Material Series: Use a dilution series of a stable fluorescent dye with known concentration or a set of neutral density filters with certified optical densities.
- Signal Acquisition: Measure the signal intensity for each reference point in the series, ensuring that exposure times and gain settings are consistent and within the linear range of the detector.
- Linearity Curve Fitting: Plot the measured signal intensity against the known relative intensity or concentration. Fit a linear regression model to the data.
- Linearity Assessment: Calculate the coefficient of determination (R²). An R² value >0.99 is typically expected for quantitative work. The deviation from linearity at the upper end of the range indicates the saturation point of the detector.
- Gain Calibration: Repeat the process at different gain settings to characterize the relationship between gain and signal output, allowing for appropriate gain selection based on signal strength and required dynamic range.
System Architecture and Calibration Workflow
The following diagram illustrates the integrated relationship between hardware components and computational processing in a modern calibrated detection system, highlighting how raw data is transformed into quantitatively accurate biological information.
System Calibration and Data Flow
This architecture demonstrates that modern calibrated instruments function as integrated physical-digital systems. The calibration inputs directly shape the computational processing to correct for physical layer imperfections, ensuring the final output faithfully represents the biological sample rather than instrument-specific artifacts [79].
The Researcher's Toolkit: Essential Calibration Materials
Successful implementation of the described protocols requires access to appropriate physical and computational tools. The table below details essential research reagent solutions and their specific functions in the calibration workflow.
Table 2: Essential Research Reagent Solutions for Detection System Calibration
| Reagent/Kit | Primary Function | Key Application in Calibration | Compatibility Notes |
|---|---|---|---|
| Certified Reference Materials (CRMs) | Wavelength accuracy verification | Provide known spectral peaks for establishing pixel-to-wavelength mapping [81] | Available for UV-Vis-NIR ranges; ensure compatibility with detection system |
| Uniform Fluorescent Slides/Beads | Flat-field correction | Generate even illumination field to correct for pixel-to-pixel sensitivity variations and vignetting | Choose fluorophores matching common laser lines or broad spectrum for white light systems |
| Fluorescent Microsphere Standards | Point-spread function (PSF) characterization | Enable measurement of system resolution and optimization of focal height [78] [80] | Sub-diffraction sized beads (e.g., 100 nm) for super-resolution systems; larger beads for conventional microscopy |
| Neutral Density Filter Set | Detector linearity assessment | Create known attenuation series to verify detector response across dynamic range | Certified optical densities preferred; ensure spectral flatness for specific application |
| Stable Fluorescent Dye Series | Gain and linearity calibration | Provide concentration series for establishing quantitative response curve | Ensure photostability; consider environmental factors (temperature, pH) affecting fluorescence |
| Multifocal Alignment Specimens | 3D and multi-plane calibration | Verify alignment and registration across multiple focal planes in systems like SPI [78] | Often custom-designed for specific instrument architectures |
In the rigorous framework of validating molecular assays against microscopy gold standards, comprehensive instrument calibration is not optional but fundamental. The optimization of wavelength accuracy, focal height, and gain parameters directly determines the reliability with which molecular data can be correlated with morphological information. As detection systems continue to evolve toward higher throughput and resolution—exemplified by techniques like SPI microscopy that achieve sub-diffraction resolution while imaging thousands of cells per second [78]—the calibration methodologies that underpin their operation must advance with equal sophistication. By implementing the systematic calibration protocols and comparisons outlined in this guide, researchers and drug development professionals can ensure their instruments perform as precision scientific tools capable of generating data that faithfully represents biological truth, thereby strengthening the validity of their conclusions in both basic research and clinical application contexts.
Reproducibility forms the cornerstone of reliable scientific research, particularly in molecular diagnostics where results directly influence patient care and drug development. The harmonization of protocols and the implementation of robust controls and reference standards are critical strategies to mitigate inter-laboratory variability. This is especially pertinent when validating novel molecular assays against established gold-standard methods, such as microscopy. The Clinical Laboratory Improvement Amendments (CLIA) mandate that clinical laboratories establish performance specifications for their tests, a process that underscores the necessity for standardized procedures to ensure accuracy and reliability [82]. Without such standardization, even technologically advanced assays can yield inconsistent results, undermining their clinical utility. This guide explores the tangible impact of protocol harmonization on reproducibility by comparing data from disparate testing environments and detailing the experimental methodologies that underpin these findings.
The Reproducibility Challenge in Biomarker Detection
The journey from a sample to a result in molecular diagnostics is complex, involving numerous steps where variability can be introduced. This is evident across various technologies, from serological assays to multiplex immunofluorescence (mIF) and next-generation sequencing (NGS).
- Pre-analytical Variables: For tissue-based tests, factors such as tissue fixation, processing, and storage can significantly impact results. In NGS workflows, the use of formalin-fixed, paraffin-embedded (FFPE) samples often leads to sequence artifacts, while in liquid biopsies, the choice of blood collection tubes can affect sample quality [83] [84].
- Analytical Variables: The core analytical protocol itself is a major source of variability. The concentration of reagents, incubation times and temperatures, and the age of critical components like red blood cells in serological assays have been identified as key parameters affecting inter-laboratory results [85]. In mIF, antibody selection and optimization are crucial, as overly high concentrations can lead to off-target staining [84].
- Post-analytical Variables: The interpretation of data, especially with complex outputs from NGS or multiplexed assays, can vary. The use of different bioinformatics pipelines for variant calling in NGS introduces another layer of variability that requires standardization through in silico datasets with known variants [83].
Table 1: Common Sources of Variability in Molecular Assays
| Stage | Source of Variability | Impact on Assay |
|---|---|---|
| Pre-Analytical | Tissue fixation & storage [84] | Nucleic acid degradation; sequence artifacts [83] |
| Blood collection tube type [83] | Contamination with genomic DNA in liquid biopsies [83] | |
| Analytical | Reagent concentration & age [85] | Altered assay sensitivity and signal intensity |
| Incubation time & temperature [85] | Affects binding kinetics and final titer or concentration | |
| Antibody specificity & dilution [84] | Non-specific binding, high background, false positives | |
| Post-Analytical | Bioinformatics algorithms [83] | Inconsistent variant calling, especially at low allele frequencies |
Protocol Harmonization: A Data-Driven Solution
The process of protocol harmonization involves developing and adhering to a consensus methodology across multiple laboratories. A prime example is the work done by the FLUCOP consortium to standardize the Hemagglutination Inhibition (HAI) assay, a long-established technique for assessing influenza immunity [85].
Experimental Protocol: Achieving HAI Assay Harmonization
The following is a summary of the key experimental steps undertaken to identify sources of variability and develop a consensus HAI protocol [85]:
- Protocol Survey: A comprehensive survey was distributed to multiple laboratories to collect information on 62 different aspects of their HAI protocols, revealing significant variability in critical steps.
- Identification of Key Parameters: Using a Design of Experiment (DOE) approach, six key parameters were identified for systematic testing: turkey RBC (TRBC) concentration, TRBC age, duration and temperature for serum/virus incubation, and duration and temperature for serum/virus/TRBC incubation.
- Fractional Factorial DOE: A fractional factorial (2^6-3) DOE was used to efficiently test the impact of high and low settings for these six parameters, resulting in 8 distinct experimental run conditions plus two controls (consensus SOP and in-house protocol).
- Reagent Standardization: All participating laboratories used common stocks of critical reagents, including reassortant viral strains.
- Data Analysis: Each laboratory conducted 20 independent experiments, testing a panel of 30 serum samples. The geometric coefficient of variation (%GCV) was calculated to quantify inter-laboratory variability for each set of run conditions.
Quantitative Impact of Harmonization
The implementation of a consensus protocol with common reagents had a dramatic effect on reducing variability. The data below compare the inter-laboratory variability, measured as %GCV, when using in-house protocols versus the harmonized FLUCOP protocol [85].
Table 2: Impact of Protocol Harmonization on HAI Assay Variability Data derived from [85]
| Influenza Virus Strain | Inter-laboratory %GCV (In-House Protocols) | Inter-laboratory %GCV (Consensus Protocol & Common Reagents) |
|---|---|---|
| H1N1 | 50% - 117% | 22% - 54% |
| H3N2 | 50% - 117% | 22% - 54% |
| B/Victoria lineage | 50% - 117% | 22% - 54% |
| B/Yamagata lineage | 50% - 117% | 22% - 54% |
This data demonstrates that harmonization can reduce variability by more than half, ensuring that results are comparable and meaningful across different sites. Similar principles are applied in other fields; for instance, in multiplex immunofluorescence, standardizing and automating staining and imaging protocols is vital for obtaining reproducible results in translational research [84].
The Critical Role of Controls and Reference Standards
In conjunction with protocol harmonization, the use of well-characterized controls and reference standards is indispensable for achieving reproducibility. These materials allow laboratories to calibrate their measurements, verify assay sensitivity, and monitor performance over time.
Types of Reference Materials
- Cell Line-Derived Reference Standards: These are increasingly used in oncology diagnostics because they offer the genomic complexity of patient samples and are renewable and reproducible. They can be formulated as FFPE blocks to mimic patient samples fully, controlling the workflow from DNA extraction to final result [83]. For example, commercially available materials can contain over 370 variants across 150 cancer genes at defined variant allele frequencies (VAFs), enabling laboratories to establish the sensitivity of their assays [83].
- Biological Standards: For serological assays, pooled human sera from vaccination campaigns have been shown to be effective as biological standards, helping to normalize results across different laboratories and protocols [85].
- In Silico Data Sets: To standardize the post-analytical phase in NGS, datasets with known variants and allele frequencies serve as controls for bioinformatics pipelines, ensuring robustness and precision in variant calling [83].
Experimental Protocol: Validation of a Novel Molecular Assay
The development and validation of any new molecular assay, including comparisons to a gold standard like microscopy, require a rigorous process. The following workflow outlines key steps, incorporating CLIA guidelines for laboratory-developed tests [82] and principles from assay validation [86].
Diagram 1: Assay Validation Workflow. This outlines the key stages in validating a molecular assay against a gold standard, from initial development to final implementation.
Detailed Experimental Steps for Method Comparison:
- Define Performance Specifications: Before testing begins, establish the target performance characteristics for the assay. For a qualitative test, this includes analytical sensitivity (Limit of Detection), analytical specificity, precision, and accuracy [82].
- Sample Selection: Test a sufficient number of clinical samples (e.g., a minimum of 40) that represent the expected range of the analyte, including positive, negative, and low-positive samples [82].
- Run Comparative Tests: Test all samples using both the new molecular assay and the gold-standard method (e.g., microscopy). This should be done over at least 5 operating days to account for daily variability [82].
- Statistical Analysis:
- Documentation: Compile a comprehensive validation report detailing all experiments, results, and the conclusion that the test is fit for its intended clinical or research purpose [86].
Case Study: Molecular Diagnostics for Leprosy
The challenge of validating new molecular tests against a microscopy gold standard is clearly illustrated in leprosy diagnostics. Microscopy of intradermal scrapings for the Mycobacterium leprae bacillus is a traditional confirmatory test but has limitations in sensitivity, particularly in paucibacillary cases [21].
Serological point-of-care tests (POCTs) using PGL-I antigen offer a rapid, field-friendly alternative but are primarily sensitive for multibacillary leprosy, creating a diagnostic gap [21]. To address this, molecular techniques like quantitative PCR (qPCR) and loop-mediated isothermal amplification (LAMP) have been developed to detect M. leprae DNA with high specificity and sensitivity [21].
The validation of these molecular tests involves a direct comparison with microscopy and clinical examination. The high sensitivity of qPCR allows it to confirm cases where microscopy is negative, thus acting as a more reliable reference method. Furthermore, the integration of these molecular methods with user-friendly POCT technologies is a key goal for developing future tests that are both accurate and applicable in resource-limited settings [21]. This case underscores the ongoing need for harmonized protocols and universal standards to ensure that new, more sensitive molecular assays can be reliably validated and deployed against older, established methods.
The Scientist's Toolkit: Essential Reagents for Reproducible Research
The following table lists key reagents and materials crucial for ensuring reproducibility and standardization in experimental workflows.
Table 3: Key Research Reagent Solutions for Assay Standardization
| Item | Function & Importance in Standardization |
|---|---|
| Cell Line-Derived Reference Standards (e.g., OncoSpan FFPE [83]) | Provides a renewable, reproducible source of known genomic variants in a biologically relevant matrix; essential for establishing assay sensitivity and monitoring performance across runs and sites. |
| Phenolic Glycolipid-I (PGL-I) Antigens [21] | Semi-synthetic, M. leprae-specific antigens critical for standardizing serological assays (ELISA, lateral flow tests) for leprosy diagnosis and monitoring. |
| Recombinant Protein Antigens (e.g., LID-1 [21]) | Recombinantly expressed fusion proteins offer high specificity and consistency for serological test development, improving upon native antigens. |
| Common Reagent Stocks (e.g., viral strains, RBCs [85]) | Central provision of critical reagents (viruses, cells, etc.) to all participating laboratories is a foundational step in harmonization studies to reduce inter-lab variability. |
| In Silico Data Sets [83] | Digital reference materials with verified variants; used to standardize and validate bioinformatics pipelines for NGS data analysis, ensuring consistent variant calling. |
| DNA Restoration Kits [83] | Used to repair common errors in FFPE-derived DNA (e.g., nicks, deamination), improving sequencing library quality and helping to discern true mutations from artifacts. |
The journey toward impeccable reproducibility in molecular diagnostics is multifaceted, relying on a synergistic approach between rigorous protocol harmonization and the strategic use of controls and reference standards. Empirical data from serology and other fields consistently shows that consensus protocols can reduce inter-laboratory variability by more than 50%, transforming data from being merely indicative to being truly reliable [85]. Furthermore, the adoption of commutable reference materials, such as cell line-derived standards, provides a non-subjective benchmark for assessing assay performance [83].
For researchers and drug development professionals, the implication is clear: investing time and resources in the upfront validation of assays—using detailed, statistically powered comparison studies against gold standards—is not a regulatory hurdle but a scientific necessity. As molecular technologies continue to evolve toward point-of-care applications [21] [87], the principles of standardization and control will remain the bedrock upon which trustworthy diagnostic and therapeutic decisions are made.
Proving Performance: Designing Robust Validation and Comparative Studies
The validation of molecular assays, particularly when benchmarked against a microscopy gold standard, is a critical process in clinical diagnostics and biomedical research. It ensures that new, often faster or more automated methods are as reliable and accurate as established techniques. This process is guided by standardized frameworks that provide structure, rigor, and credibility. The Clinical Laboratory Improvement Amendments (CLIA) represents a regulatory framework for clinical laboratories in the United States, establishing mandatory quality standards [88] [89]. The International Organization for Standardization (ISO), particularly through standards like ISO 15189 for medical laboratories and ISO 11781 for molecular methods, provides internationally recognized benchmarks for quality and competence [90] [88]. Finally, the ACCE Model, developed by the Centers for Disease Control and Prevention (CDC), offers a specialized, systematic process for evaluating genetic tests, focusing on four primary components: Analytic validity, Clinical validity, Clinical utility, and Ethical, legal, and social implications [91] [92].
These frameworks, while distinct in their origin and application, provide the essential scaffolding for validating molecular assays. This guide provides a detailed comparison of these frameworks, equipping researchers and drug development professionals with the knowledge to select and apply the appropriate model for their validation projects.
Core Characteristics and Applicability
The following table outlines the fundamental attributes of each framework, highlighting their primary focus and scope of application.
Table 1: Core Characteristics of CLIA, ISO, and ACCE Frameworks
| Feature | CLIA | ISO Standards | ACCE Model |
|---|---|---|---|
| Full Name | Clinical Laboratory Improvement Amendments [89] | International Organization for Standardization (e.g., ISO 15189, ISO 11781) [90] [88] | Analytic validity, Clinical validity, Clinical utility, Ethical, legal, and social implications [91] |
| Nature | U.S. Federal Regulation (Mandatory for clinical labs) [88] | International Standard (Voluntary, but often required for accreditation) [88] | Model Process for Evaluation (Structured guideline) [91] [92] |
| Primary Focus | Quality control, proficiency testing, and regulatory compliance for laboratory testing [88] [89] | Overall quality management system and technical competence [88] | Evidence-based review of genetic tests across multiple domains [91] |
| Defined QC Practices | Yes, specifies requirements for QC procedures and frequency [93] | Yes, but often less specific on frequency, leading to more variable implementation [93] | Not a QC framework; focuses on pre-implementation evaluation |
| Typical Application | All U.S. clinical laboratories performing human diagnostic testing [94] [89] | Medical and food testing laboratories worldwide seeking accreditation [90] [88] | Evaluation of emerging genetic tests prior to clinical implementation [92] |
Regulatory vs. Voluntary Implementation
A key distinction lies in the enforceability of these frameworks. CLIA is a mandatory regulatory requirement for all clinical laboratories in the United States; non-compliance can result in penalties and the revocation of a laboratory's license to operate [88]. In contrast, ISO 15189 accreditation is a voluntary process, though it is often pursued to demonstrate a high level of quality and to gain international recognition [88]. The ACCE model is neither a regulation nor an accreditation standard, but rather an analytical toolkit. It is a structured process used by evaluators, such as payers or policy makers, to systematically assess the value and limitations of a genetic test [92].
Focus and Philosophical Approach
The philosophical approach of each framework also differs. CLIA is primarily focused on regulatory compliance, ensuring that laboratories meet minimum federal standards for testing quality through defined rules for quality control, proficiency testing, and personnel [88] [89]. ISO standards emphasize a holistic quality management system and continuous improvement, requiring laboratories to demonstrate not just technical competence but also effectiveness in all processes, from sample collection to result reporting [88]. The ACCE model is fundamentally an evidence-based review framework. It is designed to answer a standard set of 44 questions to comprehensively evaluate a test's analytical performance, its clinical correlation, its net benefit to patient outcomes, and its associated ethical issues [91] [92].
Experimental Protocols and Data Requirements
Method Validation and Verification
A critical step in bringing a new molecular assay into the laboratory is establishing its performance. The concepts of validation and verification are central to both CLIA and ISO standards, with nuanced differences.
CLIA Requirements: Under CLIA, laboratories introducing a new test method must perform method verification to confirm that they can meet the manufacturer's stated performance specifications. This process, required before reporting patient results, must verify several key performance characteristics [89]:
- Accuracy: The closeness of agreement between a test result and an accepted reference value.
- Precision: The closeness of agreement between independent test results obtained under stipulated conditions (e.g., repeatability).
- Reportable Range: The range of values over which the test can provide quantitative results without modification.
- Reference (Normal) Range: The range of test values expected for a healthy population.
This verification is typically accomplished using proficiency testing samples, patient specimens with known values, or commercial control materials. For quantitative assays, a common rule of thumb is to use at least 20 specimens spanning the reportable range [89].
ISO Standards (ISO 16140 series): ISO standards, particularly the ISO 16140 series for microbiology, provide a more detailed and structured two-stage pathway [95]:
- Method Validation: This first stage proves a method is "fit-for-purpose." It often involves a method comparison study and an interlaboratory study to generate performance data. For food testing, a method validated across 5 different food categories is considered valid for a "broad range of foods" [95].
- Method Verification: This second stage requires a laboratory to demonstrate it can competently perform a previously validated method. This involves an implementation verification using the same samples from the validation study, followed by a (food) item verification using challenging samples relevant to the laboratory's specific scope [95].
Proficiency Testing and Quality Control
Ongoing monitoring of assay performance is mandated by CLIA and ISO, though practices can differ.
CLIA Proficiency Testing (PT): CLIA requires laboratories to enroll in approved PT programs, where they analyze unknown samples and report results back to the PT provider for grading. The 2025 CLIA updates introduced stricter acceptance criteria for many analytes. For example, the allowable total error for creatinine was tightened from ± 0.3 mg/dL or ± 15% to ± 0.2 mg/dL or ± 10%, and for potassium from ± 0.5 mmol/L to ± 0.3 mmol/L [96]. These updated criteria, fully implemented in 2025, raise the bar for laboratory performance.
Comparative QC Practices: A 2025 global survey highlights practical differences in how CLIA and ISO labs manage quality control. CLIA labs are more likely to run QC once per day, aligning with the CLIA minimum requirement, whereas ISO labs more frequently run QC twice or three times daily. The survey also found that CLIA-accredited laboratories report a higher frequency of out-of-control events (over 44% daily) compared to ISO 15189 labs (just over 29%) [93].
The ACCE Evaluation Protocol
The ACCE model employs a structured, question-driven review process that is distinct from routine QC. A "Rapid-ACCE" process has been developed to complete evaluations within months, averaging about 100 hours of analyst time [92]. The protocol involves:
- Defining the Disorder, Test, and Clinical Scenario: A one-page document and conceptual flow diagram are created and refined with a panel of experts [92].
- Systematic Evidence Review: An analyst performs a structured literature review and meta-analysis to answer the 44 core ACCE questions. This includes gathering both published and "gray" unpublished data from laboratories and experts [92].
- Expert Consensus and Review: A series of teleconferences with content experts are held to review data summaries, clarify qualitative issues, and reach consensus. A draft report is then sent to independent reviewers for comment [92].
Table 2: ACCE Model Components and Evaluation Focus
| ACCE Component | Evaluation Focus | Example Questions (from the 44 total) |
|---|---|---|
| Analytic Validity | How accurately and reliably the test measures the target analyte (e.g., specific DNA sequence). | What is the analytic sensitivity (detection limit) and specificity? What is the assay's reproducibility? [91] [92] |
| Clinical Validity | How well the test correlates with the clinical phenotype or disorder. | What is the clinical sensitivity and specificity? What is the prevalence of the mutation in different populations? [91] [92] |
| Clinical Utility | The risks and benefits of using the test in clinical practice. | Does the test result lead to an improved health outcome? What are the financial and health impacts of alternative courses of action? [91] [92] |
| Ethical, Legal, and Social Implications (ELSI) | The broader societal issues related to the test. | What informed consent processes are required? How is privacy and confidentiality protected? [91] [92] |
Visualization of Framework Structures and Workflows
Relationship Between Validation Frameworks
The following diagram illustrates how the CLIA, ISO, and ACCE frameworks interact and relate to each other within the ecosystem of test development and implementation.
The ACCE Model Evaluation Workflow
The ACCE model follows a rigorous, iterative process for evaluating a genetic test, as detailed in the workflow below.
The Scientist's Toolkit: Essential Reagents and Materials
Successful validation of a molecular assay against a microscopy gold standard requires a suite of high-quality reagents and materials. The following table details key components for a typical validation study involving PCR-based detection of a specific DNA sequence, as referenced in standards like ISO 11781 [90].
Table 3: Essential Research Reagents for Molecular Assay Validation
| Reagent/Material | Function in Validation | Key Considerations |
|---|---|---|
| Reference Standard | Serves as the "gold standard" (e.g., microscopy) against which the new molecular assay is compared. Provides known positive and negative samples. | Purity, accuracy, and traceability are critical. Must be well-characterized and accepted as a reference method in the field. |
| Target DNA Controls | Used to establish analytic validity. Positive controls contain the target sequence; negative controls confirm absence of contamination. | Should cover a range of concentrations to determine linearity and limit of detection. Should include near-cutoff values. |
| PCR Master Mix | Provides the core components (polymerase, dNTPs, buffer) for the DNA amplification reaction. | Lot-to-lot consistency is vital for precision studies. Must be suitable for the assay type (e.g., qualitative real-time PCR). |
| Sequence-Specific Primers & Probes | Designed to bind to and amplify/detect the specific DNA target of interest (e.g., from a genetically modified organism or allergenic species). | Specificity is paramount to avoid cross-reactivity. Efficiency should be validated as part of the assay development. |
| Internal Control | A non-target sequence added to or co-amplified with the sample to identify PCR inhibition and confirm reaction validity. | Must be distinguishable from the primary target and not interfere with its amplification. |
| Certified Reference Material (CRM) | A material with a defined and traceable amount of the target analyte, used for calibrating equipment and verifying method accuracy. | Obtained from a recognized national or international standards body. Essential for establishing metrological traceability. |
The choice of a validation framework is not a one-size-fits-all decision but depends on the test's stage of development, its intended use, and the regulatory environment. CLIA provides the non-negotiable, regulatory bedrock for daily operations in U.S. clinical labs, with clearly defined QC and PT rules that were recently updated in 2025 to be more stringent [96] [94]. ISO standards, particularly ISO 15189 and those in the 16140 series, offer a comprehensive quality management system that emphasizes technical competence and continuous improvement, often leading to more robust but variable QC practices [93] [95]. The ACCE model stands apart as a powerful, pre-implementation tool for conducting systematic, evidence-based reviews of genetic tests, forcing a critical appraisal of not just analytical performance but also clinical value and ethical ramifications [91] [92].
For researchers validating a molecular assay against a microscopy gold standard, these frameworks are complementary. The ACCE model can guide the initial, comprehensive evaluation of the assay's merits. Once deemed ready for use, the assay must be implemented and maintained in a laboratory environment governed by the rigorous, day-to-day quality mandates of CLIA and/or the holistic quality system of ISO. Understanding the distinct role and requirements of each framework is essential for ensuring the delivery of accurate, reliable, and clinically meaningful diagnostic results.
The validation of new molecular diagnostic assays against established gold-standard methods is a critical process in medical science. For many infectious diseases, such as malaria and vaginitis, microscopy remains the traditional benchmark for diagnosis [9] [97]. However, newer molecular methods like polymerase chain reaction (PCR) and isothermal amplification techniques offer potential improvements in sensitivity, specificity, and throughput. When evaluating these new assays, researchers must select an appropriate statistical study design—concordance analysis, equivalence testing, or non-inferiority testing—each serving a distinct purpose and answering a different research question. The choice depends on whether the goal is to demonstrate analytical similarity, clinical interchangeability, or that a new method retains an acceptable level of performance while offering other advantages like speed or cost-effectiveness. This guide compares these study designs within the context of validating molecular assays against microscopy gold standards, providing researchers with the framework and tools necessary for robust experimental evaluation.
Comparative Framework: Study Designs and Their Applications
Key Study Designs and Statistical Hypotheses
Table 1: Comparison of Superiority, Non-Inferiority, and Equivalence Trial Designs
| Study Design | Primary Research Question | Null Hypothesis (H₀) | Alternative Hypothesis (H₁) | Typical Application in Assay Validation |
|---|---|---|---|---|
| Superiority | Is the new assay better than the comparator? | The new assay is not better than the comparator. | The new assay is superior to the comparator. [98] | Demonstrating a new molecular test has significantly higher sensitivity than microscopy. |
| Non-Inferiority | Is the new assay not worse than the comparator by a clinically acceptable margin? | The new assay is inferior to the comparator. [99] | The new assay is not inferior to the comparator. [98] [100] | Validating a faster/cheaper diagnostic that is at least as good as the gold standard. |
| Equivalence | Is the new assay similar to the comparator within a set margin? | The new assay is different from the comparator (outside the margin). [99] | The new assay is equivalent to the comparator (within the margin). [98] | Showing a new automated platform performs similarly to a manual gold-standard method. |
Choosing the Right Design: A Conceptual Workflow
The selection of an appropriate study design is a foundational step that shapes the entire validation process. The following workflow outlines the key decision points based on the assay's intended claim and the clinical context.
The Equivalence and Non-Inferiority Framework
Defining the Margin of Clinical Significance (Δ)
The most critical step in designing either an equivalence or non-inferiority study is the a priori specification of the margin of clinical significance, denoted as delta (Δ) [98] [99]. This margin defines the maximum clinically acceptable difference between the new assay and the gold standard that would render the two assays "similar" or confirm that the new one is "not unacceptably worse."
- Statistical Interpretation: In a non-inferiority design, if the outcome is measured on a scale where a higher value is better (e.g., sensitivity), the new assay is considered non-inferior if the lower bound of the confidence interval for the difference (New - Gold Standard) is greater than -Δ [99]. For equivalence, the entire confidence interval must lie between -Δ and +Δ [101].
- Clinical Justification: The Δ margin cannot be chosen arbitrarily; it must be justified based on clinical reasoning and historical data [99]. For example, in a diagnostic study, Δ could be set to a 5% difference in sensitivity, as a loss of detection beyond this point would be considered clinically unacceptable.
Statistical Procedures and Analysis
The standard statistical method for testing equivalence is the Two One-Sided Tests (TOST) procedure [99]. This procedure effectively tests whether the observed difference between the two assays is significantly less than +Δ and significantly greater than -Δ.
- Confidence Interval Approach: A common implementation of TOST uses a (1 - 2α) × 100% confidence interval for the difference between the two assays. For a standard α of 0.05, a 90% confidence interval is constructed. If this entire interval falls within the range (-Δ, Δ), equivalence is concluded at the 5% significance level [99].
- Non-Inferiority Testing: As a one-sided test, non-inferiority is established if the lower bound of the (1 - 2α) × 100% confidence interval (e.g., the lower bound of a 90% CI) is above -Δ [99].
Table 2: Interpretation of Confidence Intervals in Different Study Designs
| Observed Confidence Interval (CI) | Superiority Conclusion | Non-Inferiority Conclusion | Equivalence Conclusion |
|---|---|---|---|
| CI is entirely above 0 | Superiority shown | Non-inferiority shown | Equivalence not shown (assay is superior) |
| CI includes 0 but is entirely above -Δ | Superiority not shown | Non-inferiority shown | Equivalence not shown (needs two-sided check) |
| CI is entirely within (-Δ, +Δ) | Superiority not shown | Non-inferiority shown | Equivalence shown |
| CI includes or is below -Δ | Superiority not shown | Non-inferiority not shown | Equivalence not shown |
Experimental Protocols for Molecular Assay Validation
Sample Selection and Preparation
A robust validation study requires a well-characterized sample set that reflects the intended use of the assay.
- Sample Types and Sourcing: Studies may use clinical isolates from hospitalized patients [12], samples from symptomatic patients [9], or experimentally infected laboratory specimens [97]. Ethical approvals and informed consent are mandatory for human-derived samples [12].
- Gold Standard Comparator: The comparator method must be rigorously performed. For microscopy, this includes preparing Giemsa-stained blood smears for malaria parasites [97] or Gram staining and Nugent scoring for vaginitis [9].
- Blinding: To prevent bias, samples should be blinded and tested independently with the new assay and the gold-standard method.
Protocol Example: Validating a Molecular Assay for Malaria
The following workflow summarizes a detailed protocol from a study validating a portable qPCR system for detecting Plasmodium species in mosquito samples, a process that can be adapted for other targets [97].
Protocol Example: Validating a CRISPR-Based Diagnostic Assay
Advanced molecular assays often combine multiple techniques. The PathCrisp assay for detecting the NDM resistance gene uses a two-step process [12]:
- Isothermal Amplification:
- Reaction Setup: A LAMP reaction is prepared using a master mix, Bst polymerase, and specifically designed inner and outer primers targeting the conserved region of the NDM gene.
- Amplification: The reaction is incubated at 60°C for one hour to amplify the target DNA isothermally.
- CRISPR-Based Detection:
- Complex Formation: A detection mix is prepared by pre-incubating engineered sgRNA with the Cas12a enzyme and an ssDNA reporter molecule labeled with a fluorophore and quencher.
- Detection: The amplified product is added to the detection mix. If the target is present, the Cas12a-sgRNA complex binds and activates, cleaving the reporter and producing a fluorescent signal. Fluorescence is measured in real-time at 520 nm.
Essential Reagents and Research Solutions
Table 3: Research Reagent Solutions for Molecular Validation Studies
| Reagent / Solution | Function / Purpose | Example Use Case |
|---|---|---|
| DNAzol Reagent | A ready-to-use reagent for the isolation of DNA from biological samples; enables field-compatible DNA extraction without traditional column-based kits. [97] | Crude DNA extraction directly from whole blood or homogenized mosquito tissues in resource-limited settings. [97] |
| LAMP Master Mix | A pre-mixed solution containing a strand-displacing Bst polymerase, buffers, and dNTPs optimized for loop-mediated isothermal amplification (LAMP). | Isothermal amplification of target pathogen DNA (e.g., NDM gene) without the need for a thermal cycler. [12] |
| CRISPR/Cas12a System | A gene-editing-derived system comprising the Cas12a nuclease and custom single-guide RNA (sgRNA); used here for its collateral cleavage activity upon target recognition. | Highly specific detection of amplified LAMP products, triggering a fluorescent readout for pathogen identification. [12] |
| TaqMan Probes | Hydrolysis probes labeled with a fluorescent reporter and quencher used in qPCR assays; fluorescence increases as the probe is cleaved during amplification. | Sensitive and specific quantification of Plasmodium DNA in real-time qPCR platforms, both standard and portable. [97] |
| ssDNA-FQ Reporter | A single-stranded DNA oligonucleotide labeled with a fluorophore (FAM) and a quencher (Iowa Black); serves as the substrate for activated Cas12a. | Generating a fluorescent signal in CRISPR-based detection assays when collateral trans-cleavage occurs. [12] |
Data Presentation and Analysis in Practice
Quantitative Results from Published Studies
Table 4: Performance Data from Molecular Diagnostic Validation Studies
| Study & Assay | Target / Purpose | Gold Standard Comparator | Sensitivity | Specificity | Key Quantitative Finding |
|---|---|---|---|---|---|
| PathCrisp-NDM [12] | Detection of NDM gene in CRE isolates | PCR with Sanger sequencing | 100% Concordance | 100% Concordance | Detected as few as 700 copies of the NDM gene from clinical isolates. |
| Aptima BV Assay [9] | Diagnosis of Bacterial Vaginosis (BV) | Consensus Gram stain & Nugent score | 97.5% | 96.3% | Demonstrated high agreement with the reference method in symptomatic patients. |
| bCUBE qPCR [97] | Detection of P. falciparum in mosquitoes | Microscopy | Strong correlation (R² = 0.993) with standard qPCR | Not explicitly stated | Detected as few as 0.5 parasites/µl of blood and one oocyst in mosquito guts. |
Performing Concordance Analysis
Concordance studies are often the first step in method comparison. The analysis typically involves:
- 2x2 Contingency Tables: Results are cross-tabulated to calculate overall percent agreement, positive percent agreement (sensitivity), and negative percent agreement (specificity) against the gold standard.
- Cohen's Kappa (κ): This statistic measures the agreement between two tests beyond what is expected by chance alone. A κ value above 0.8 is generally considered excellent agreement.
Selecting the correct study design—superiority, non-inferiority, or equivalence—is paramount for the statistically sound and clinically meaningful validation of new molecular diagnostics. This choice is dictated not by statistical convenience but by the precise research question and the intended claim about the new assay's performance. A rigorous validation study, built upon a well-justified margin of clinical significance, a robust experimental protocol, and clear data analysis, provides the evidence necessary for the scientific community to confidently adopt new diagnostic tools. As molecular technologies continue to evolve towards point-of-care applications, the principles outlined in this guide will remain foundational for assessing their value against established microscopic and molecular gold standards.
In the field of molecular diagnostics, accurately determining a test's performance specifications is not merely a regulatory formality but a fundamental requirement for ensuring reliable patient results. When validating molecular assays against established gold standards like microscopy, three analytical metrics are particularly crucial: the Lower Limit of Detection (LOD), which defines the lowest analyte concentration an assay can reliably detect; linearity, which confirms the assay's quantitative proportionality across its measuring range; and Coefficient of Variation (CV) values, which quantify assay precision [82] [102]. These parameters form the foundation for verifying that a new molecular method provides the sensitivity, reliability, and accuracy required for clinical or research use. The Clinical Laboratory Improvement Amendments (CLIA) mandate that laboratories establish these performance specifications for laboratory-developed tests (LDTs) to ensure accurate and precise results prior to clinical implementation [82]. This guide objectively compares how different molecular assay platforms and technologies perform against these critical metrics, providing researchers and drug development professionals with experimental data and protocols for rigorous assay validation.
Comparative Performance Data of Molecular Assays
The following tables summarize key performance metrics for a selection of molecular assays, illustrating the range of analytical performance achievable across different platforms and technologies.
Table 1: Comparison of LOD and Linear Range for Various Molecular Assays
| Assay / Technology | Target / Application | Reported LOD | Linear Range | Reference Method |
|---|---|---|---|---|
| IntelliPlex Lung Cancer Panel DNA [6] | EGFR p.Thr790Met mutation | 3.17% VAF | LOD to >25% VAF (5 points) | Comprehensive Genomic Profiling (CGP) NGS |
| P. falciparum 18S rRNA qPCR [37] | Malaria parasites in whole blood | 0.3 parasites/μL | 0.25 to 2,500 parasites/μL | Microscopy & Flow Cytometry |
| ValidPrime qPCR Assay [102] | Single-copy human genome target | ~1-2 molecules (statistical) | 1 to 2048 molecules/reaction | NIST-calibrated DNA |
| Microscopy (Thick Blood Smear) [37] | Malaria parasites | ~4–20 parasites/μL | Not quantifiable | N/A (Gold Standard) |
Table 2: Precision (CV) and Accuracy Data from Assay Validations
| Assay / Technology | Precision (CV) | Accuracy / Concordance | Key Validation Findings |
|---|---|---|---|
| IntelliPlex Lung Cancer Panel [6] | Not explicitly stated | 98.15% overall accuracy vs. NGS | 98% agreement for DNA, 100% for RNA with NGS |
| P. falciparum qPCR Assay [37] | Intra- and Inter-assay CV <10% | Specificity: 100% | Robust, precise, and accurate for CHMI studies |
| Laboratory-Developed Tests (CLIA) [82] | Minimum 40 data points over 20 days | Typically ≥40 specimens over 5 days | Requirements for precision and accuracy studies |
Experimental Protocols for Determining Key Metrics
Protocol for Determining Limit of Detection (LOD)
The LOD is the lowest concentration of an analyte that an assay can detect with a stated probability, typically 95% [103] [104]. The following sequential dilution protocol is a standard approach for its determination.
Materials Required:
- Primary stock solution of the target analyte at a known, high concentration
- Appropriate matrix for serial dilutions (e.g., nuclease-free water, negative plasma, wild-type DNA)
- All standard reagents for the assay (primers, probes, master mix, enzymes)
- Platform-specific consumables (reaction plates, tubes)
Procedural Steps:
- Primary Dilution Series: Prepare a broad-range serial dilution (e.g., 1:10 dilutions) of the target analyte, from a concentration that is consistently detected (e.g., 1000 copies/reaction) down to a level expected to be below the LOD (e.g., 1 copy/reaction). Run each dilution in a small number of replicates (e.g., n=3) [103].
- Result Tabulation: Record the detection rate (number of positive replicates / total replicates) at each concentration. This identifies an approximate concentration range for the LOD (e.g., between 10 and 100 copies/reaction) [103].
- Secondary Dilution Series: Create a finer secondary dilution series (e.g., 1:2 or 1:3 dilutions) centered on the approximate LOD range. Use a larger number of replicates (n=10 to n=20) at each concentration to ensure statistical robustness [82] [103].
- LOD Calculation: The LOD is defined as the lowest concentration at which the analyte is detected in ≥95% of the replicates [103]. For greater precision, statistical models like probit regression analysis on 60 data points collected over 5 days can be used to calculate the 95% detection point [82].
Figure 1: Experimental workflow for determining the Limit of Detection (LOD) via serial dilution.
Protocol for Establishing Linearity
Linearity defines the range over which an assay's response is directly proportional to the concentration of the analyte [82] [105].
Materials Required:
- Calibrated standard material at known, high concentration
- Appropriate matrix for serial dilutions
- All standard assay reagents
Procedural Steps:
- Preparation of Linear Dilutions: Create a series of 7-9 samples with concentrations spanning the entire anticipated measuring range of the assay, extending 20-30% beyond the expected reportable range. Prepare 2-3 replicates for each concentration [82].
- Assay Execution: Run the complete dilution series in the assay platform.
- Data Analysis: Plot the measured value (e.g., Cq value for qPCR, or VAF for NGS) against the expected concentration (logarithmic scale may be used for qPCR). Perform regression analysis [82] [37].
- Interpretation: The assay is considered linear across the range if the coefficient of determination (R²) is ≥ 0.98 [37]. The slope of the line is used to calculate amplification efficiency in qPCR [37].
Protocol for Determining Coefficient of Variation (CV)
The CV quantifies the precision (repeatability and reproducibility) of an assay, expressed as a percentage (standard deviation/mean × 100) [37].
Materials Required:
- At least three distinct samples representing high, low, and near the LOD concentrations of the analyte [82].
- All standard assay reagents.
Procedural Steps:
- Sample Selection: Choose samples at a minimum of three concentrations (high, low, and near the LOD) [82].
- Replication Experiment:
- Statistical Calculation: Calculate the standard deviation (SD) and mean for each concentration level. Then compute the CV as (SD / Mean) × 100% [37].
- Interpretation: CV values of <10% are generally considered acceptable for molecular assays, indicating good precision [37]. The total variation should be calculated and evaluated against the assay's required performance.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful assay validation relies on a set of core reagents and materials. The following table details these essential components and their critical functions in the validation process.
Table 3: Key Research Reagent Solutions for Assay Validation
| Reagent / Material | Function in Validation | Application Examples from Research |
|---|---|---|
| Calibrated Standard Reference Material | Serves as the primary calibrator for defining analyte concentration in absolute terms, crucial for LOD and linearity studies. | NIST-calibrated human genomic DNA [102]; Horizon Dx OncoSpan gDNA Reference Standard [6]. |
| Extraction Kits & Automated Systems | Isolate and purify nucleic acids from complex samples; efficiency directly impacts LOD and CV. | QIAsymphony for automated DNA extraction (malaria qPCR) [37]. |
| Assay-Specific Primers & Probes | Bind specifically to the target nucleic acid sequence; their design and quality are paramount for specificity and sensitivity. | ValidPrime assay primers/probes [102]; P. falciparum 18S rRNA primers/probes [37]. |
| Master Mix (qPCR) | Contains enzymes, dNTPs, and buffer necessary for amplification; lot-to-lot consistency is key for robust CV. | TATAA Probe GrandMaster Mix [102]. |
| Negative Control Matrix | The analyte-free background (e.g., healthy donor blood, wild-type DNA) used for preparing dilutions to assess specificity and LOD. | Wild-type DNA sample (NA12878) for LOD dilutions [6]; donor whole blood screened for P. falciparum [37]. |
The rigorous determination of LOD, linearity, and CV is a non-negotiable step in the validation of any molecular assay, especially when establishing performance against a gold standard like microscopy. As demonstrated by the comparative data, well-validated qPCR and multiplexed assays can significantly exceed the analytical sensitivity of traditional methods, enabling earlier detection and more precise quantification. The experimental protocols outlined provide a framework for generating reliable, regulatory-compliant performance data. By systematically applying these validation principles and using the appropriate toolkit of reagents, researchers and drug developers can ensure their assays are fit for purpose, ultimately supporting robust scientific conclusions and reliable diagnostic outcomes.
Statistical Approaches for Comparing Modalities and Calculating Diagnostic Concordance
Diagnostic concordance analysis is a critical statistical process used to establish the validity of a new diagnostic measuring or rating technique or to demonstrate the near-equivalence of multiple techniques [106]. In clinical and research settings, this is particularly crucial when introducing a new method intended to be more readily available, less invasive, or more efficient than an established technique or gold standard [106]. The fundamental question these analyses address is how well the measurements or classifications obtained with a new technique agree with those obtained by an established reference.
Within the specific context of validating molecular assays against microscopy as a gold standard, concordance analysis provides the statistical framework to determine whether the molecular method can reliably replace or complement traditional microscopy. This replacement is only justified if the new method demonstrates sufficient agreement with the established standard for the intended clinical or research purpose [1]. It is vital to recognize that a common but incorrect method of comparing two quantitative techniques is to calculate a simple correlation coefficient, as this measures association rather than agreement [106]. Two techniques can be perfectly correlated yet show consistent, clinically significant differences in their measurements.
Key Statistical Methods for Assessing Concordance
The choice of statistical method for concordance analysis depends primarily on the nature of the data generated by the diagnostic modalities—specifically, whether the output is continuous (numerical along a scale) or categorical (nominal or ordinal classifications).
Analyzing Continuous Data
For quantitative measurements, such as viral load counts or concentrations of a biomarker, several statistical approaches are employed to assess agreement.
Bland-Altman Analysis: This method is considered one of the most informative approaches for comparing two continuous measurement techniques [106] [107]. Also known as the "limits of agreement" approach, it involves calculating the differences between the two measurements for each sample and then plotting these differences against the average of the two measurements [106]. The mean of all differences (( \bar{d} )) indicates the average bias or systematic deviation between the two methods. The standard deviation of the differences (( s{\text{d}} )) quantifies the random variation around this bias. The limits of agreement are calculated as ( \bar{d} \pm 1.96 \cdot s{\text{d}} ), providing a range within which 95% of the differences between the two measurement techniques are expected to fall [106] [107]. The clinical acceptability of these limits is a decision for the researcher or clinician based on the intended use of the test.
Concordance Correlation Coefficient (CCC): Proposed by Lin, the CCC assesses both precision (how closely the data points lie to the best-fit line) and accuracy (how close that best-fit line is to the 45-degree line of perfect agreement) [107]. It is defined as ( \text{CCC} = C{\text{b}} \cdot \rho ), where ( \rho ) is the Pearson correlation coefficient (measuring precision) and ( C{\text{b}} ) is a bias correction factor (measuring accuracy) [107]. The CCC ranges from 0 (no agreement) to 1 (perfect agreement), providing a single summary measure of agreement.
Intraclass Correlation Coefficient (ICC): The ICC is derived from analysis of variance (ANOVA) models and is defined as the ratio of the between-subject variance to the total variance [107]. Like the CCC, it ranges from 0 to 1. The ICC is particularly useful for assessing agreement among multiple raters or methods, and different versions exist to account for fixed or random rater effects [107].
The following table summarizes the core methods for analyzing continuous data:
Table 1: Statistical Methods for Assessing Agreement on a Continuous Scale
| Method | Primary Function | Key Outputs | Interpretation |
|---|---|---|---|
| Bland-Altman Plot [106] [107] | Visualizes agreement and estimates a range of differences. | Mean difference (bias), Limits of Agreement (LOA). | The LOA defines the range where 95% of differences lie. Clinically acceptable LOA indicates good agreement. |
| Concordance Correlation Coefficient (CCC) [107] | Quantifies agreement as a single metric, combining precision and accuracy. | CCC value (0 to 1). | Values closer to 1 indicate stronger agreement. It directly measures deviation from the line of identity. |
| Intraclass Correlation Coefficient (ICC) [107] | Measures reliability or consistency between methods, often from ANOVA. | ICC value (0 to 1). | Values closer to 1 indicate higher reliability and consistency between measurements. |
Analyzing Categorical Data
For data that fall into discrete categories, such as a positive/negative result or a classification like "influenza/flu-like illness/other," different statistical tools are required.
Cohen's Kappa (κ): This statistic measures the agreement between two raters or methods on a categorical scale, correcting for agreement expected by chance alone [106]. A kappa value of 1 indicates perfect agreement, 0 indicates agreement equal to chance, and negative values indicate agreement worse than chance. It is widely used for nominal (non-ordered) categories. As demonstrated in a study comparing standardized versus non-standardized joint examinations, kappa values can be used to show significantly higher concordance for one method over another [108].
Diagnostic Accuracy Metrics: When comparing a new test to a gold standard (e.g., a molecular assay vs. microscopy), standard 2x2 contingency tables are used to calculate fundamental metrics of diagnostic performance [109] [108]. The most critical of these are Sensitivity (the ability to correctly identify positive cases) and Specificity (the ability to correctly identify negative cases). Other derived metrics include Positive Predictive Value (PPV) and Negative Predictive Value (NPV).
McNemar's Test: This is a paired statistical test used to compare the sensitivities or specificities of two diagnostic tests when both tests are applied to the same set of subjects [109]. It is particularly useful because it accounts for the correlated nature of the data. The test focuses on the discordant pairs—the samples where the two tests disagree—to determine if there is a statistically significant difference in the proportions of positive (or negative) results [109].
Table 2: Statistical Methods for Assessing Agreement on a Categorical Scale
| Method | Primary Function | Key Outputs | Interpretation |
|---|---|---|---|
| Cohen's Kappa (κ) [106] [108] | Measures inter-rater agreement for categorical items, correcting for chance. | Kappa statistic (≤1 to 1). | Values >0.8: excellent agreement; 0.6-0.8: substantial; 0.4-0.6: moderate; <0.4: poor agreement. |
| Diagnostic Accuracy Metrics [109] [108] | Quantifies the performance of a new test against a reference standard. | Sensitivity, Specificity, PPV, NPV. | Sensitivity/Specificity closer to 100% indicate better diagnostic performance. |
| McNemar's Test [109] | Determines if there is a significant difference in matched proportions (e.g., sensitivities). | P-value. | A significant p-value (<0.05) suggests a statistically significant difference in the performance of the two tests. |
Experimental Design and Protocols for Validation
A robust validation study comparing a molecular assay to a microscopy gold standard requires careful planning and execution. The following workflow outlines the key stages of this process.
Diagram 1: Validation Study Workflow
Study Planning and Sample Selection
The initial phase involves defining the study's purpose and ensuring the appropriate samples are used.
- Define Performance Specifications: Before beginning, establish the target performance specifications the molecular assay must meet to be considered successful. For a laboratory-developed test, the Clinical Laboratory Improvement Amendments (CLIA) require laboratories to establish their own performance specifications for accuracy, precision, reportable range, and analytical sensitivity and specificity [82] [110]. This defines the "success criteria" for the validation.
- Sample Selection and Size: The sample set must be representative of the future clinical or research application. It should include specimens that cover the entire expected range of the analyte, from low to high concentrations, including negative samples [82] [110]. For quantitative assays, CLSI guidelines suggest using 40 or more specimens tested in duplicate by both the comparative and test procedures over at least 5 operating days to establish accuracy [82]. Including samples with potential interfering substances is also critical for establishing analytical specificity [82].
Data Collection and Analysis Protocol
A rigorous testing protocol is essential to generate reliable, unbiased data for analysis.
- Blinded Testing: To prevent bias, the personnel performing and interpreting the molecular assay should be blinded to the results of the microscopy gold standard, and vice versa [1]. This ensures that the results from one method do not influence the interpretation of the other.
- Paired Measurements: Each specimen must be tested by both the new molecular method and the microscopy gold standard, resulting in a paired dataset [106]. This pairing is a fundamental requirement for statistical analyses like the Bland-Altman plot, McNemar's test, and the calculation of kappa.
- Data Analysis Sequence: First, the nature of the data (continuous or categorical) dictates the primary statistical methods. For continuous data, begin with a Bland-Altman plot to visualize bias and agreement limits, then supplement with a CCC or ICC for a summary measure [106] [107]. For categorical data, construct a 2x2 table to calculate sensitivity and specificity, then use Cohen's kappa to assess agreement beyond chance, and finally, employ McNemar's test if comparing the significance of differences in paired proportions [106] [109].
The Scientist's Toolkit: Essential Reagents and Materials
The successful validation of a molecular assay against microscopy relies on a foundation of high-quality reagents and materials. The following table details key components of the research toolkit.
Table 3: Essential Research Reagent Solutions for Molecular Assay Validation
| Tool/Reagent | Critical Function | Considerations for Validation |
|---|---|---|
| Reference Standard Material | Provides a known quantity of the target analyte to establish accuracy and the reportable range. | Should be traceable to an international standard. Used at multiple concentrations for quantitative linearity studies [82] [110]. |
| Clinical Specimens | Serves as the real-world sample for method comparison. | Must be collected in the appropriate matrix and stored under validated conditions. The panel should cover the full spectrum of expected results [82]. |
| Positive & Negative Controls | Monitors the correct performance of the assay in each run. | Positive controls verify analytical sensitivity; negative controls check for contamination or interference. Required for every batch of tests [110]. |
| Nucleic Acid Extraction Kits | Isifies and purifies the target DNA/RNA from the sample matrix. | The extraction efficiency directly impacts the assay's sensitivity (Limit of Detection). The chosen method must be validated for each sample type [82]. |
| PCR Master Mix & Reagents | Provides the essential enzymes, buffers, and nucleotides for amplification. | Lot-to-lot consistency is critical for maintaining assay precision. Key components for establishing robustness and reproducibility [110]. |
| Primers & Probes | Dictates the specificity of the molecular assay by binding to the unique target sequence. | Careful in silico design (e.g., BLAST analysis) is needed to ensure specificity and avoid cross-reactivity with genetically similar organisms [110]. |
The validation of a new molecular diagnostic assay against an established microscopy gold standard is a multifaceted process that demands a rigorous statistical approach. The core principle is to move beyond simple correlation and instead focus on measures of agreement that are clinically relevant. By strategically applying Bland-Altman analysis, CCC, Cohen's kappa, and diagnostic accuracy metrics within a robust experimental design, researchers can generate compelling evidence regarding the new assay's performance. This evidence-based validation is essential not only for regulatory compliance and publication but, ultimately, for ensuring that new technologies can be trusted to deliver accurate results in patient care and scientific research.
In the rapidly advancing field of molecular diagnostics, the validation dossier serves as the critical bridge between innovative assay development and regulated clinical implementation. As molecular technologies evolve from traditional microscopy and culture-based methods to sophisticated CRISPR-based systems and next-generation sequencing, the framework for validating these tools against established standards becomes increasingly important [12] [111]. This guide objectively compares the performance of contemporary molecular assays against the microscopy gold standard, providing researchers, scientists, and drug development professionals with experimental data and methodologies essential for constructing comprehensive regulatory submissions.
The validation process demonstrates that a new assay is reliable, accurate, and reproducible for its intended use. Within regulated environments, this documentation must satisfy rigorous requirements from agencies like the FDA, EMA, and other global health authorities [112] [113]. This article examines specific case studies of molecular assays validated against microscopy, details their experimental protocols, and synthesizes their performance data into structured comparisons to inform your own validation strategy.
Case Studies: Molecular Assays Versus Microscopy Gold Standards
Tuberculosis Diagnostics: Orange G3 TBC vs. Microscopy and GeneXpert
Tuberculosis (TB) diagnosis has historically relied on smear microscopy, despite its limitations in sensitivity and biosafety risks for laboratory personnel [111]. A 2025 diagnostic accuracy study evaluated the Orange G3 TBC platform, a PCR-based system featuring a unique biosafe processing design, against both smear microscopy and the WHO-endorsed GeneXpert Ultra system [111].
The study, conducted with 71 clinical samples in Bolivia, demonstrated that while microscopy remains the accessible standard in resource-limited settings, its sensitivity falls significantly short of molecular alternatives. The Orange G3 TBC platform addressed key microscopy limitations by implementing a closed-system design that eliminates airborne transmission risk through sample inactivation at 88°C for 20 minutes [111]. This system also eliminates the subjectivity inherent in microscopic examination, providing objective, fluorometrically-detected results.
Experimental Protocol: Orange G3 TBC Validation
- Sample Collection and Preparation: The study utilized 67 sputum specimens and 4 cerebrospinal fluid samples from patients with presumptive TB. All samples underwent initial smear microscopy before molecular analysis [111].
- Biosafe Nucleic Acid Extraction: The Orange G3 TBC protocol performs sample liquefaction and biological inactivation in a sealed system using a three-way stopcock apparatus, followed by DNA purification via a simplified Boom method [111]. This generates concentrated genetic material free from inhibitors while protecting laboratory staff.
- Amplification and Detection: The platform employs a balanced hemi-nested fluorometric PCR system targeting the IS6110 insertion element of M. tuberculosis. Amplification occurs in a dedicated TB thermocycler-fluorometer with double-stranded DNA detected using a DNA intercalating fluorochrome and custom software [111].
- Comparison Methodology: All samples were tested in a randomized, double-blind manner with both Orange G3 TBC and GeneXpert Ultra systems. Statistical analysis included sensitivity, specificity, predictive values, likelihood ratios, and correlation measures to evaluate performance against the reference standard [111].
NDM-Resistant Infections: PathCrisp as a Culture-Independent Method
For detecting New Delhi metallo-beta-lactamase (NDM) genes in carbapenem-resistant enterobacteriaceae, the PathCrisp assay represents an innovative approach that combines loop-mediated isothermal amplification with CRISPR-Cas12a detection [12]. This system operates at a constant temperature, reducing equipment complexity while maintaining high sensitivity.
Traditional culture-based antimicrobial susceptibility testing requires 2-5 days, creating significant delays in therapeutic decision-making [12]. While not directly compared to microscopy, the PathCrisp system addresses similar limitations in turnaround time and technical complexity found in gold-standard methods. The assay achieves detection sensitivity as low as 700 copies of the NDM gene from clinical isolates, demonstrating 100% concordance with PCR-Sanger sequencing methods [12].
Experimental Protocol: PathCrisp Assay Development
- Oligo Design and Conservation Testing: Researchers downloaded NDM variant gene sequences from databases and aligned them using Clustal Omega. sgRNA was designed in conserved regions, with six LAMP primers designed around the sgRNA target [12].
- Isothermal Amplification: The LAMP reaction utilizes a strand-displacing Bst polymerase with outer, loop, and inner primers. The reaction occurs at 60°C for one hour without requiring thermal cycling [12].
- CRISPR-Based Detection: The detection mix contains sgRNA, Cas12a enzyme, and an ssDNA reporter with fluorophore and quencher. When the Cas12a complex binds its target, collateral trans-cleavage activity releases the fluorophore, generating a detectable signal [12].
- Validation Approach: The assay was tested on 49 carbapenem-resistant enterobacteriaceae clinical isolates and compared with PCR-Sanger sequencing. The method also demonstrated compatibility with crude bacterial extracts obtained through heating, eliminating need for kit-based DNA purification [12].
Comparative Performance Data Analysis
Quantitative Comparison of Diagnostic Assays
Table 1: Performance Metrics of Molecular Assays Versus Reference Standards
| Assay Name | Reference Method | Sensitivity | Specificity | PPV | NPV | Diagnostic Efficiency |
|---|---|---|---|---|---|---|
| Orange G3 TBC | GeneXpert Ultra | 90% | 97% | 82% | 98% | 96% |
| Orange G3 TBC | Smear Microscopy | 94.7% [111] | N/R | N/R | N/R | N/R |
| PathCrisp (NDM detection) | PCR-Sanger Sequencing | 100% Concordance [12] | 100% Concordance [12] | N/R | N/R | N/R |
Table 2: Operational Characteristics Comparison
| Assay Name | Turnaround Time | Equipment Needs | Biosafety Considerations | Sample Processing Features |
|---|---|---|---|---|
| Smear Microscopy | 1-2 hours | Microscope, basic lab equipment | High risk of operator exposure [111] | Direct smear staining, subjective interpretation |
| Orange G3 TBC | Approximately 2-3 hours | Thermocycler-fluorometer | Closed system, sample inactivation at 88°C [111] | Integrated liquefaction, inactivation, and purification |
| PathCrisp | ~2 hours | Constant temperature device [12] | Compatible with crude extracts, reduced handling | No kit-based DNA purification needed |
| Culture-Based AST | 2-5 days [12] | Incubators, purity plates | Requires live culture handling | Elaborate culture-based processing |
Key Advantages of Molecular Assays Documented in Validation Studies
The quantitative data reveals several critical advantages of molecular assays over traditional microscopy that should be highlighted in validation dossiers:
- Enhanced Sensitivity: Molecular methods demonstrate significantly improved detection capabilities for low-abundance targets, with Orange G3 TBC showing approximately 44% higher sensitivity compared to smear microscopy values ranging from 46-78% [111].
- Superior Biosafety: The closed-system design of modern platforms like Orange G3 TBC directly addresses the "risk of transmission to laboratory personnel" associated with smear microscopy [111].
- Rapid Turnaround: Molecular assays provide results in hours rather than days, enabling faster clinical decision-making. PathCrisp reduces detection time for NDM-resistant infections from the 18-24 hours required by systems like VITEK-2 to approximately 2 hours [12].
- Objective Interpretation: Unlike the subjective interpretation inherent in microscopic examination, molecular platforms provide digital readouts (fluorometric signals) that minimize operator-dependent variability [111].
Regulatory Framework and Submission Strategy
Contemporary Regulatory Considerations for 2025
The regulatory landscape for diagnostic assays continues to evolve, with several key trends impacting validation dossier requirements:
- Emphasis on Real-World Evidence: Regulatory agencies are increasingly incorporating RWE into decision-making. The FDA's Advancing Real-World Evidence Program aims to improve the quality and acceptance of RWE-based approaches [112].
- Decentralized Trial Models: Regulatory bodies have updated guidelines to accommodate decentralized clinical trials with remote testing components. Both FDA and EMA have issued specific guidance on conducting trials with decentralized elements [112].
- AI Integration in Regulatory Processes: Agencies are adopting AI tools to enhance efficiency. The FDA has launched "Elsa," a generative AI tool to help employees work more efficiently, reflecting the broader acceptance of advanced technologies in regulatory science [113].
- Streamlined Approval Processes: Initiatives like the FDA's Breakthrough Therapy Designation and the UK's 10-Year Health Plan aim to reduce clinical trial setup times, encouraging development of innovative diagnostics [112] [113].
Dossier Preparation Strategies
Successful regulatory submissions in the current environment require strategic approaches:
- Adopt Zero-Based Redesign: Re-engineer submission processes from the ground up, focusing on critical-path activities. Leading companies have accelerated submissions by 50-65% using this approach [114].
- Leverage Automation and AI: Implement AI-assisted medical writing, which can reduce end-to-end cycling time for clinical study reports by 40% [114].
- Modernize Core Systems: Invest in regulatory-information-management systems that enable seamless workflows and data-centric approaches [114].
- Engage Early with Agencies: Pursue pre-submission meetings to align on study designs and endpoints, as demonstrated by Oncocyte's regulatory strategy for their GraftAssureDx test [115].
Visualizing the Validation Workflow
The following diagram illustrates the key decision points and workflow for validating a molecular assay against a gold standard, incorporating elements from the case studies:
Assay Validation Workflow - This pathway outlines the key stages in validating a molecular assay against established standards, culminating in dossier compilation.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Molecular Assay Validation
| Reagent/Material | Function in Validation | Example from Case Studies |
|---|---|---|
| Strand-Displacing Polymerase | Isothermal amplification without denaturation | Bst 1.0 enzyme in PathCrisp LAMP reaction [12] |
| Cas Protein Complex | Sequence-specific detection with collateral activity | Cas12a enzyme with sgRNA in PathCrisp [12] |
| Fluorophore-Quencher Reporters | Real-time detection of nucleic acid amplification | FAM-labeled ssDNA reporter cleaved by activated Cas12a [12] |
| Target-Specific Primers | Amplification of conserved target regions | Six LAMP primers designed around NDM gene conserved regions [12] |
| Sample Inactivation System | Biosafe processing of infectious materials | Three-way stopcock system with 88°C heating in Orange G3 TBC [111] |
| Silica-Based Purification | Nucleic acid isolation free of inhibitors | Simplified Boom method for DNA purification [111] |
| Custom Bioinformatic Pipeline | Data analysis and variant calling | Customized pipeline for UMA panel analysis [116] |
The case studies examined demonstrate that successful validation dossiers for molecular assays must provide comprehensive evidence of superior performance over gold standards like microscopy, while addressing key limitations related to sensitivity, biosafety, and operational efficiency. The quantitative data from these studies reveals consistent patterns of enhanced diagnostic accuracy, with molecular assays typically achieving sensitivity ratings above 90% compared to microscopy's 46-78% range [111].
When constructing your validation dossier, emphasize not just analytical performance but also practical implementation advantages. These include reduced turnaround times, enhanced biosafety through closed-system designs, and operational efficiency in resource-limited settings [12] [111]. Furthermore, align your submission strategy with evolving regulatory trends, including the use of real-world evidence, engagement with health authorities through pre-submission meetings, and adoption of AI-enhanced documentation processes [112] [114] [113].
By systematically addressing these elements and providing robust comparative data against established standards, your validation dossier will effectively demonstrate the clinical utility and regulatory compliance of your molecular assay, facilitating its pathway to regulatory approval and clinical adoption.
Conclusion
The successful validation of a molecular assay against microscopy is a multifaceted process that extends beyond proving technical equivalence. It requires a deep understanding of foundational principles, meticulous methodological execution, proactive troubleshooting, and a rigorous comparative study design. As demonstrated by advancements in malaria CHMI studies, leprosy POCTs, and resistance gene detection, the future of diagnostics lies in integrating these validated molecular tools with traditional methods. This synergy enhances sensitivity, speeds up turnaround times, and enables new applications like liquid biopsy. Ultimately, a robust validation framework is not a mere regulatory hurdle but a critical step that ensures patient safety, guides effective treatment, and builds the foundation for the next generation of precision diagnostics.
References
- 1. Validation of digital microscopy: Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8761960/]
- 2. A validation study of microscopy versus quantitative PCR for ... [https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-019-0176-3]
- 3. Comparison of microscopy and radiography as gold ... [https://pubmed.ncbi.nlm.nih.gov/10740474/]
- 4. Clinical validation and evaluation of the EasyNAT Malaria ... [https://www.sciencedirect.com/science/article/pii/S1477893925000365]
- 5. Comparison of performance between three SARS‐CoV‐2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9088664/]
- 6. Validation of a rapid biomarker assay for lung cancer using ... [https://www.nature.com/articles/s41598-025-10585-y]
- 7. Validation of a modified CDC assay and performance ... [https://www.sciencedirect.com/science/article/abs/pii/S1386653220304303]
- 8. The Rise of AI-Assisted Diagnosis: Will Pathologists Be ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468387/]
- 9. From microscopy to molecular diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502618/]
- 10. Discrepancy analysis comparing molecular and histology ... [https://www.sciencedirect.com/science/article/pii/S1600613522223193]
- 11. Histology image analysis of 13 healthy tissues reveals ... [https://www.nature.com/articles/s41598-025-11853-7]
- 12. PathCrisp: an innovative molecular diagnostic tool for early ... [https://www.nature.com/articles/s41598-024-84832-z]
- 13. High‐Throughput, Label‐Free and Slide‐Free Histological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8805566/]
- 14. Bridging the Gap: Image Software Quantification vs. ... [https://www.appliedpathology.com/blog/bridging-the-gap-image-software-quantification-vs-pathologist-scoring-in-histopathology]
- 15. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 16. Accuracy, precision, specificity & sensitivity [https://labtestsonline.org.uk/articles/accuracy-precision-specificity-sensitivity]
- 17. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 18. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 19. Understanding the Four Types of Analytical Method ... [https://www.oxford-analytical.co.uk/understanding-the-four-types-of-analytical-method-validation/]
- 20. Roche Digital Pathology Dx whole slide imaging system is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421238/]
- 21. Challenges and advances in serological and molecular tests ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800132/]
- 22. How to verify and validate a clinical microbiology test ... [https://www.sciencedirect.com/science/article/pii/S1198743X24003094]
- 23. How Roche's DP200 and DP600 systems earned FDA ... [https://www.linkedin.com/posts/aleksandra-zuraw-dvm-phd-dacvp_why-accuracy-matters-in-digital-pathology-activity-7386372733116248064-Idzw]
- 24. Navigating method evaluation in clinical laboratories [https://myadlm.org/cln/articles/2024/mayjune/navigating-method-evaluation-in-clinical-laboratories]
- 25. Experts See 17 Laboratory Trends Dominating 2025 [https://clpmag.com/diagnostic-technologies/experts-see-17-laboratory-trends-dominating-2025/]
- 26. Using a Web-Based Application to Define the Accuracy of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0079489]
- 27. Diagnostic concordance and discordance in digital pathology [https://pmc.ncbi.nlm.nih.gov/articles/PMC8223673/]
- 28. The Impact of Expert Pathology Review and Molecular ... [https://www.mdpi.com/2072-6694/16/13/2314]
- 29. Comparison of diagnostic performance of RT-qPCR, RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10170900/]
- 30. Comparison between RT-qPCR and LAMP Methods for a ... [https://www.intechopen.com/chapters/1130226]
- 31. Comparative Evaluation of the LAMP Assay and PCR ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.02089/full]
- 32. Comparison of PCR, Nested PCR, and RT-LAMP for Rapid ... [https://www.mdpi.com/2076-2615/14/16/2432]
- 33. Method development and clinical validation of LAMP ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1533100/full]
- 34. Combinations of PCR and Isothermal Amplification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7672014/]
- 35. Comparison of RT-LAMP and RT-qPCR assays for ... [https://pubmed.ncbi.nlm.nih.gov/38103738/]
- 36. PathCrisp: an innovative molecular diagnostic tool for early ... [https://pubmed.ncbi.nlm.nih.gov/39747369/]
- 37. Quantification of Plasmodium falciparum: validation ... [https://www.frontiersin.org/journals/malaria/articles/10.3389/fmala.2025.1497613/full]
- 38. A validation study of microscopy versus quantitative PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6712708/]
- 39. Performance of rapid diagnostic tests, microscopy, and qPCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11984112/]
- 40. Comparative performance of microscopy, rapid diagnostic ... [https://malariajournal.biomedcentral.com/articles/10.1186/s12936-025-05256-2]
- 41. Implementation and validation of a new qPCR assay to ... [https://pubmed.ncbi.nlm.nih.gov/39656014/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1JKSd2KF3MGtV5lO5sks4qb8ZkLa-sn7rf8rl4cgGi9ahMukW&fc=None&ff=20241214011742&v=2.18.0.post9+e462414]
- 42. Real-time PCR for malaria diagnosis and identification of ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-024-06467-3]
- 43. Rapid Identification of Carbapenemase Genes Directly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523387/]
- 44. Molecular detection of bla VIM and bla NDM in multidrug- ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1672531/full]
- 45. Evaluating the Performance of Two Rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11913027/]
- 46. Rapid detection of carbapenemases in multiresistant Gram ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502678/]
- 47. The molecular detection of carbapenem markers with a two ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1346442/full]
- 48. blaNDM-5 is the predominant variant of blaNDM gene in ... [https://www.sciencedirect.com/science/article/pii/S2213716525002334]
- 49. Performance of serological tests PGL1 and NDO-LID in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6322275/]
- 50. ELISA Test Based on the Phenolic Glycolipid-I (PGL-I) of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9415083/]
- 51. NDO-BSA, LID-1, and NDO-LID Antibody Responses for ... [https://www.frontiersin.org/journals/tropical-diseases/articles/10.3389/fitd.2022.850886/full]
- 52. Identifying Leprosy and Those at Risk of ... - Research journals [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0004934]
- 53. Biotechnological and Immunological Platforms Based on ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.00429/full]
- 54. Detection of antibodies to both M. leprae PGL-I and MMP-II ... [https://www.sciencedirect.com/science/article/pii/S0732889315002382#!]
- 55. Combination of Serological, Antigen Detection, and DNA ... [https://www.nature.com/articles/s41598-020-65419-w]
- 56. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 57. Research progress of CTC, ctDNA, and EVs in cancer liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10850354/]
- 58. Circulating tumor cells: overcoming challenges of detecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123222/]
- 59. Circulating tumor cell markers for early detection and drug ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1494723/full]
- 60. Feasibility of mass cytometry proteomic characterisation ... [https://www.nature.com/articles/s41416-023-02428-2]
- 61. Advances in CTC and ctDNA detection techniques [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-025-02024-7]
- 62. Mass cytometric detection of homologous recombination ... [https://pubmed.ncbi.nlm.nih.gov/40456663/]
- 63. Pre-Analytical Phase - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/pre-analytical-phase]
- 64. Effects of pre-analytical processes on blood samples used in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4471316/]
- 65. Preanalytical Variables and Their Influence on the Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6238383/]
- 66. Comparison and clinical validation of qPCR assays targeting ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008750]
- 67. Evaluation of pre-analytical factors affecting plasma DNA ... [https://www.nature.com/articles/s41598-018-25810-0]
- 68. The impact of preanalytical variables on the analysis of cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1385041/full]
- 69. An Overview of Pre-Analytical Factors Impacting ... [https://www.mdpi.com/2218-1989/14/9/474]
- 70. Evolution of tuberculosis diagnostics: From molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10072981/]
- 71. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 72. Predicting sequence-specific amplification efficiency in ... [https://www.nature.com/articles/s41467-025-64221-4]
- 73. Experimental validation of novel and conventional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC167648/]
- 74. Understanding qPCR Efficiency and Why It Exceeds 100% [https://biosistemika.com/blog/qpcr-efficiency-over-100/]
- 75. New algorithmic tool can improve microscopy image analysis ... [https://medschool.vanderbilt.edu/basic-sciences/2025/10/06/new-algorithmic-tool-can-improve-microscopy-image-analysis-making-improvements-across-fields/]
- 76. Image Analysis | TU-Dresden - iGEM 2025 [https://2025.igem.wiki/tu-dresden/image_analysis]
- 77. Image analysis tools for improved characterization of ... [https://link.springer.com/article/10.1007/s00249-025-01770-y]
- 78. Real-time, high-throughput super-resolution microscopy ... [https://www.nature.com/articles/s41467-025-64368-0]
- 79. Computational optical imaging: on the convergence of ... [https://opg.optica.org/optica/abstract.cfm?uri=optica-12-1-113]
- 80. System Analysis for a high-precision high-accuracy ... [https://arxiv.org/html/2511.07113v1]
- 81. Calibration Programs [https://www.stsci.edu/jwst/science-execution/approved-programs/calibration]
- 82. Validation of Laboratory-Developed Molecular Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2901657/]
- 83. Choosing Reference Standards for Molecular Assay ... [https://clpmag.com/diagnostic-technologies/molecular-diagnostics/choosing-reference-standards-for-molecular-assay-development/]
- 84. Best Practices for Technical Reproducibility Assessment of ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.660202/full]
- 85. Assay Harmonization and Use of Biological Standards To ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8530177/]
- 86. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 87. Molecular point-of-care testing technologies: Current status ... [https://www.sciencedirect.com/science/article/pii/S2950160125000063]
- 88. USA CLIA Standards vs. International ISO 15189 Standards [https://www.linkedin.com/pulse/comparing-quality-management-usa-clia-standards-vs-international-yf26e]
- 89. Clinical Laboratory Improvement Amendments (CLIA) [https://www.aafp.org/family-physician/practice-and-career/managing-your-practice/clia.html]
- 90. ISO 11781:2025 - Molecular biomarker analysis [https://www.iso.org/standard/83912.html]
- 91. ACCE Model Process for Evaluating Genetic Tests [https://archive.cdc.gov/www_cdc_gov/genomics/gtesting/acce/index.htm]
- 92. Rapid ACCE: Experience with a rapid and structured ... [https://www.nature.com/articles/gim200772]
- 93. 2025 Great Global QC Survey: ISO and CLIA labs [https://www.westgard.com/qc-applications/basic-qc-practices/2025-qc-survey-iso-vs-clia.html]
- 94. What 2025 CLIA Updates Mean for Labs and Compliance [https://reesscientific.com/blog/2025-clia-updates-for-labs]
- 95. Method validation and method verification - Introduction - ISO [https://committee.iso.org/sites/tc34sc9/home/essential-information/content-left-area/validation-of-methods/method-validation-and-method-ver.html]
- 96. 2025 CLIA Acceptance Limits for Proficiency Testing [https://www.westgard.com/clia-a-quality/quality-requirements/2024-clia-requirements.html]
- 97. Off-grid field-deployable molecular diagnostic platform for ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06779-y]
- 98. Comparisons of Superiority, Non-inferiority, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5925592/]
- 99. Understanding Equivalence and Noninferiority Testing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3019319/]
- 100. Trial Designs—Non-inferiority vs. Superiority vs. Equivalence [https://www.certara.com/blog/trial-designs-non-inferiority-vs-superiority-vs-equivalence/]
- 101. What is the difference between Superiority vs. Equivalence ... [https://www.statsols.com/articles/what-is-the-difference-between-superiority-vs.-equivalence-vs.-non-inferiority-in-clinical-trial-design]
- 102. Methods to determine limit of detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496743/]
- 103. The How and Why of Limit of Detection [https://bitesizebio.com/44092/how-to-calculate-the-limit-of-detection-for-an-assay-and-why-youd-want-to/]
- 104. Limit of Detection | National Exposure Report [https://www.cdc.gov/environmental-exposure-report/php/about-the-data/limit-of-detection.html]
- 105. Determining LOD and LOQ Based on the Calibration Curve [https://www.sepscience.com/hplc-solutions-126-chromatographic-measurements-part-5-determining-lod-and-loq-based-on-the-calibration-curve-6959]
- 106. Concordance Analysis: Part 16 of a Series on Evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3165924/]
- 107. Methods for evaluating the agreement between diagnostic ... [https://link.springer.com/article/10.1007/s12350-015-0175-7]
- 108. Diagnostic Accuracy and Concordance of Standardized vs. ... [https://www.mdpi.com/2077-0383/14/15/5334]
- 109. 17.4 - Comparing Two Diagnostic Tests | STAT 509 [https://online.stat.psu.edu/stat509/lesson/17/17.4]
- 110. A standardized framework for the validation and verification ... [https://www.nature.com/articles/ejhg2010101]
- 111. Diagnostic accuracy of the novel and biosafe molecular assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553880/]
- 112. Clinical trial regulations in 2025: navigating the constraints [https://clinicaltrialrisk.org/clinical-trial-design/clinical-trial-regulations-navigating-the-constraints/]
- 113. Q3 2025 Newsletter – What's New in Clinical Development ... [https://www.s-cubed-global.com/industry-insights/q3-2025-newsletter-whats-new-in-clinical-development-practices-regulations]
- 114. Faster regulatory submissions for pharma with AI [https://www.mckinsey.com/industries/life-sciences/our-insights/rewiring-pharmas-regulatory-submissions-with-ai-and-zero-based-design]
- 115. Oncocyte Reports Successful 2024; Sets Stage for 2025 ... [https://investors.imdxinc.com/news-releases/2025/03-24-2025-200558408]
- 116. Unique molecular assay (UMA): a next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485320/]