Beyond Single Pathogens: Overcoming Sanger Sequencing Limitations in Complex Co-Infections
The accurate identification of co-infections remains a significant challenge in clinical diagnostics and therapeutic development.
Beyond Single Pathogens: Overcoming Sanger Sequencing Limitations in Complex Co-Infections
Abstract
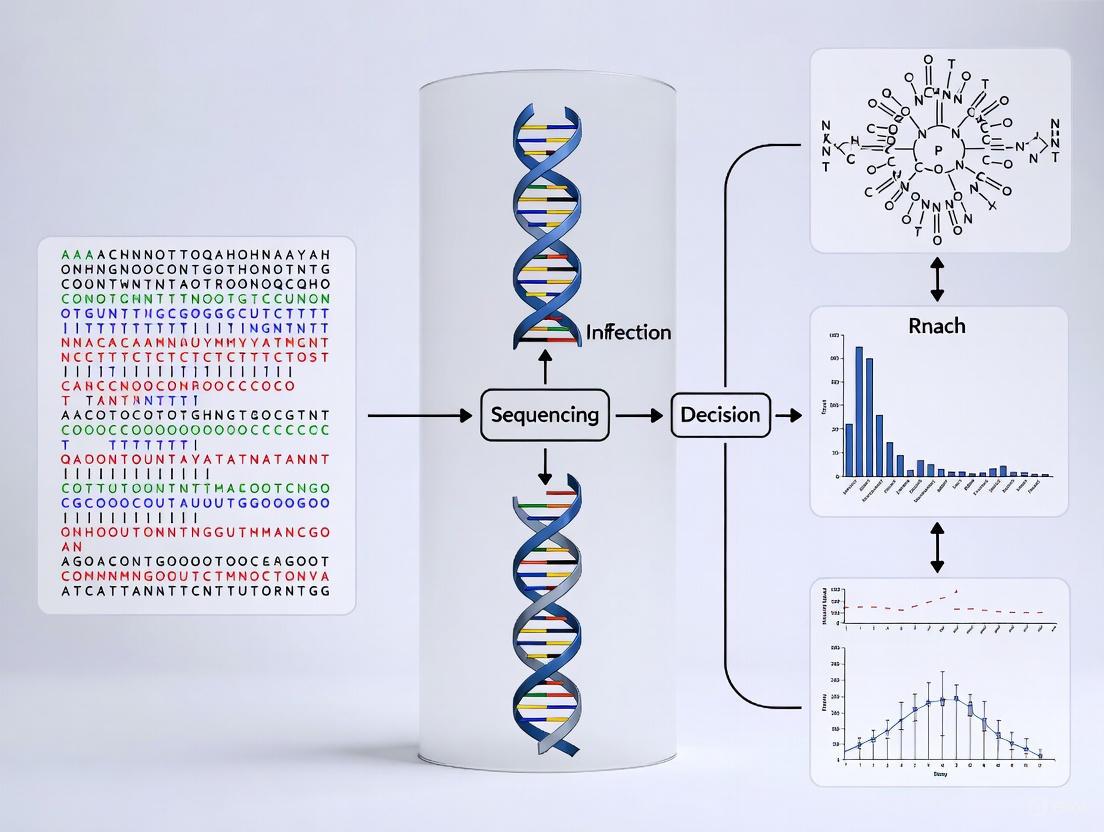
The accurate identification of co-infections remains a significant challenge in clinical diagnostics and therapeutic development. Sanger sequencing, while a gold standard for single-pathogen detection, has inherent limitations in complex microbial communities, including low throughput and an inability to detect low-frequency variants. This article explores the critical transition from traditional Sanger sequencing to advanced metagenomic next-generation sequencing (mNGS) for comprehensive co-infection analysis. We examine the foundational principles of each technology, present methodological workflows for mNGS application, address key troubleshooting and optimization strategies and provide a comparative validation of these techniques using recent clinical data. Aimed at researchers and drug development professionals, this review synthesizes evidence to guide the selection and implementation of advanced genomic tools for overcoming diagnostic bottlenecks and improving patient outcomes in polymicrobial infections.
The Co-Infection Diagnostic Challenge: Why Sanger Sequencing Falls Short
Polymicrobial infections (PMIs), characterized by the simultaneous presence of multiple microbial species at an infection site, represent a significant and often underappreciated challenge in clinical practice and infectious disease research. Worldwide, PMIs account for an estimated 20–50% of severe clinical infection cases, with biofilm-associated and device-related infections reaching 60–80% in hospitalized patients [1]. These complex infections contribute substantially to morbidity and mortality, with vulnerable populations including neonates, the elderly, and immunocompromised patients showing case-fatality rates 2-fold higher than monomicrobial infections in similar settings [1].
The clinical landscape of PMIs is diverse, encompassing diabetic foot infections, intra-abdominal infections, pneumonia, cystic fibrosis lung infections, and biofilm-associated device infections [1] [2]. The Indian subcontinent is considered a particular PMI hotspot where high comorbidities, endemic antimicrobial resistance, and underdeveloped diagnostic capacity elevate the risks of poor outcomes [1]. Understanding the prevalence, impact, and diagnostic challenges of these complex infections is essential for improving patient care and outcomes.
The Diagnostic Bottleneck: Limitations of Conventional Methods
The Culture Problem
Traditional culture-based diagnostic methods, while foundational to microbiology, exhibit critical limitations that contribute to diagnostic gaps in PMIs. These methods often suffer from low sensitivity, particularly for slow-growing, low-abundance, or unculturable pathogens, resulting in false negatives and incomplete pathogen profiles [1]. Conventional techniques typically focus on a narrow spectrum of anticipated pathogens, overlooking potentially significant co-infecting organisms and their contributions to disease pathogenesis [1].
Epidemiological data show that conventional culture-based diagnostic methods tend to detect only fast-growing, dominant microbes, often missing other slow-growing, anaerobic, or hard-to-culture organisms [1]. This incomplete detection has significant clinical implications, as the complex interplay between co-infecting microbes substantially alters disease pathophysiology, severity, and therapeutic response, heightening the risk of morbidity, prolonging hospitalization, and inflating healthcare costs [1].
The Sanger Sequencing Limitation in Co-infections Research
While Sanger sequencing has been a gold standard for genetic analysis, it faces particular challenges in the context of polymicrobial infections. The method struggles with mixed templates, which are characteristic of PMIs, leading to ambiguous results and detection failures.
Table 1: Common Sanger Sequencing Challenges in Polymicrobial Infection Research
| Challenge | Identification in Chromatogram | Possible Causes | Recommended Solutions |
|---|---|---|---|
| Failed Reactions | Trace is messy with no discernable peaks or sequence reads "NNNNN" | Template concentration too low or poor quality DNA; bad primer | Adjust DNA concentration to 100-200ng/µL; clean up contaminants; verify primer quality [3] |
| Double Sequence/Mixed Template | Two or more peaks at same location from beginning of trace | Multiple templates in reaction; colony contamination; multiple priming sites | Ensure single colony purity; use single primer per reaction; clean up PCR products thoroughly [3] |
| Sequence Degradation | High quality data that suddenly terminates or intensity drops dramatically | Secondary structure (hairpins) in template; long stretches of G/C nucleotides | Use "difficult template" protocol with alternate dye chemistry; design primers after or toward problematic region [3] |
| Background Noise | Discernable peaks with background noise along bottom | Low signal intensity due to poor amplification; low template concentration | Optimize template concentration; ensure high primer binding efficiency; check for primer degradation [3] |
Modern Solutions: Advanced Technologies for PMI Detection
Metagenomic Next-Generation Sequencing (mNGS)
Metagenomic next-generation sequencing offers a powerful alternative to conventional methods for PMI detection. Unlike culture-based methods, metagenomics allows for unbiased, culture-independent identification of entire microbial communities, including bacteria, viruses, fungi, and parasites within clinical samples [1]. This high-throughput approach can detect pathogens missed by conventional diagnostics and provide detailed taxonomic and resistance gene profiles [1].
A comparative study of lower respiratory tract infections demonstrated the significant advantage of mNGS over conventional culture methods in detecting co-infections. In 184 bronchoalveolar lavage fluid samples, mNGS identified 66 samples with co-infections, compared to 64 by Sanger sequencing, and only 22 by conventional culture [4]. The same study showed that in 91.30% (168/184) of cases, identical results were produced by both mNGS and Sanger sequencing, validating the reliability of mNGS while highlighting its greater comprehensiveness [4].
Long-Read Sequencing Technologies
Emerging long-read sequencing technologies, such as Oxford Nanopore Technologies (ONT), provide additional advantages for resolving complex polymicrobial infections. These technologies enable unfragmented genome assembly, which is particularly valuable for detecting co-infections and resolving complex microbial communities [5] [6].
In a study on avian haemosporidian parasites, Nanopore sequencing effectively resolved cryptic co-infections through complete mitogenome assembly, "overcoming ambiguities inherent to Sanger sequencing" [5]. The extended read lengths allow for better discrimination between similar sequences and more accurate phylogenetic resolution of closely related species within mixed infections.
Targeted Amplicon Sequencing
For many clinical applications, targeted amplicon sequencing (such as 16S rRNA gene sequencing for bacteria or ITS sequencing for fungi) provides a cost-effective middle ground between comprehensive metagenomics and targeted Sanger sequencing [7]. This approach allows for broader detection of microbial communities while maintaining deeper sequencing coverage of specific taxonomic groups.
However, this method has limitations, including the inability to differentiate prokaryotes at the species taxonomic level reliably and generally being restricted to genus-level classification [7]. The accurate taxonomic identification also depends heavily on the quality and completeness of reference databases, which often contain unidentified and/or poorly annotated sequences [7].
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q: Why does Sanger sequencing fail to detect multiple pathogens in a mixed infection? A: Sanger sequencing operates on the principle of single-template amplification. When multiple templates are present, the sequencing reaction becomes confused, resulting in overlapping signals that appear as mixed peaks in the chromatogram. This fundamental limitation makes it unsuitable for detecting polymicrobial infections without prior separation and individual analysis of each pathogen [3].
Q: What are the key indicators of polymicrobial infection in Sanger sequencing chromatograms? A: The primary indicator is the presence of double peaks or multiple overlapping peaks at single nucleotide positions, particularly when this pattern persists throughout the sequence read. Other indicators include high background noise, sudden sequence termination, and poor-quality scores that cannot be explained by template quality alone [3].
Q: How does mNGS overcome the limitations of Sanger sequencing for PMI detection? A: mNGS sequences all DNA fragments in a sample simultaneously, then uses bioinformatics to map these fragments to reference databases, allowing identification of multiple organisms without prior targeting. This culture-independent, unbiased approach can detect unexpected pathogens, difficult-to-culture organisms, and mixed infections that would be missed by both conventional culture and Sanger sequencing [1] [4].
Q: What is the turnaround time for mNGS compared to traditional methods? A: While conventional culture can take 24-72 hours and Sanger sequencing typically requires 24-48 hours after culture isolation, mNGS can provide results within 24-48 hours total from sample receipt. Emerging technologies like CRISPR-based multiplex assays and sensitive biosensors show potential for reducing this turnaround time to under 2 hours while maintaining high accuracy (>95%) [1].
Research Reagent Solutions for Polymicrobial Infection Studies
Table 2: Essential Research Reagents and Materials for Advanced PMI Detection
| Reagent/Material | Function | Application Notes |
|---|---|---|
| DNA Extraction Kits (for complex samples) | Isolation of high-quality DNA from diverse sample types | Choose kits that efficiently lyse all microbial cell types (bacterial, fungal, viral) and remove PCR inhibitors [4] |
| Multiplex PCR Primers | Amplification of multiple target sequences simultaneously | Designed to target conserved regions flanking variable areas of phylogenetic marker genes (16S, 18S, ITS) [7] |
| Metagenomic Sequencing Kits | Library preparation for NGS | Include fragmentation, adapter ligation, and amplification steps optimized for mixed microbial communities [4] |
| Bioinformatic Analysis Software | Taxonomic classification and resistance gene profiling | Platforms like IDseqTM-2, MYcrobiota provide automated analysis pipelines for NGS data [7] [4] |
| MALDI-TOF Mass Spectrometry | Rapid microbial identification from culture isolates | Requires pure cultures but provides rapid species identification; limited for mixed samples [4] |
Methodologies and Workflows for PMI Research
Comparative Method Workflow for Respiratory Pathogen Detection
Detailed mNGS Protocol for BALF Samples
Based on the comparative analysis of LRTI pathogens [4], the following protocol can be implemented for comprehensive PMI detection:
Sample Collection and Processing: Collect bronchoalveolar lavage fluid (BALF) using standard clinical procedures. Process samples within 2 hours of collection or store at -80°C until processing.
Nucleic Acid Extraction: Extract DNA using commercial kits designed for complex samples. Include mechanical lysis steps to ensure efficient disruption of all microbial cell types.
Library Preparation: Utilize commercially available metagenomic sequencing kits (e.g., Respiratory Pathogen Multiplex Detection Kit). The process includes:
- DNA fragmentation to appropriate size (200-500bp)
- End repair and adapter ligation
- PCR amplification with barcoded primers
- Library quantification and quality control
Sequencing: Perform high-throughput sequencing using platforms such as VisionSeq 1000 or comparable systems. Aim for at least 10 million reads per sample to ensure adequate coverage of low-abundance pathogens.
Bioinformatic Analysis: Process raw sequencing data through automated analysis pipelines (e.g., IDseqTM-2) that include:
- Quality filtering and host sequence removal
- Alignment to comprehensive pathogen databases
- Taxonomic classification and abundance estimation
- Antimicrobial resistance gene detection
Result Interpretation: Integrate mNGS findings with clinical data to distinguish pathogens from colonizing organisms. Establish threshold criteria for positive identification based on read counts and clinical relevance.
Validation Framework for PMI Detection Methods
To ensure reliability of polymicrobial infection detection, implement a validation framework that includes:
Analytical Sensitivity: Determine limit of detection for each target pathogen in mixed samples using spiked controls.
Specificity Testing: Verify minimal cross-reactivity between different microbial targets in multiplex assays.
Reproducibility Assessment: Perform inter-run and intra-run replicates to establish precision metrics.
Clinical Correlation: Compare method performance against clinical presentation and outcome data.
The clinical imperative for accurately diagnosing polymicrobial infections is clear, given their significant prevalence and impact on patient outcomes. While conventional methods like culture and Sanger sequencing remain important tools in clinical microbiology, their limitations in detecting mixed infections necessitate the adoption of more comprehensive approaches like metagenomic next-generation sequencing.
The future of PMI diagnosis lies in the strategic integration of multiple technologies—leveraging the speed and specificity of targeted methods with the comprehensiveness of untargeted approaches. Emerging methods including CRISPR-based multiplex assays, artificial intelligence-based metagenomic platforms, and sensitive biosensors with point-of-care applicability show potential in reducing turnaround times to under 2 hours with accuracy exceeding 95% [1].
As these technologies continue to evolve and become more accessible, they promise to transform our approach to complex infections, enabling more targeted therapies, improved antimicrobial stewardship, and ultimately, better patient outcomes across diverse healthcare settings.
For decades, Sanger sequencing has remained the gold standard method for DNA sequencing, providing high-quality data for specific, targeted regions. In clinical microbiology, it is invaluable for identifying bacterial and fungal pathogens from clinical samples, particularly when traditional culture methods fail. This technique is highly effective for confirming the identity of a single pathogen. However, a significant limitation arises in cases of polymicrobial infections, where Sanger sequencing produces overlapping electropherogram signals that are impossible to interpret, complicating the diagnosis of co-infections [8] [9]. This technical support center is designed to help researchers overcome common experimental hurdles and understand the context in which Sanger sequencing is most effectively applied.
Troubleshooting Common Sanger Sequencing Issues
FAQ: Addressing Typical Data Quality Problems
1. My sequencing reaction failed, and the trace data contains mostly N's. What happened? A failed reaction with a messy trace and no discernable peaks is often due to issues with the template DNA [10].
- Low template concentration: This is the most common reason. Ensure your template concentration is between 100-200 ng/µL, accurately measured on an instrument like a NanoDrop [10].
- Poor DNA quality: Contaminants like salts, ethanol, or phenol can inhibit the sequencing reaction. Re-clean your DNA sample to ensure a 260/280 OD ratio of 1.8 or greater [10] [11].
- Bad primer: Verify that your primer is of high quality, not degraded, and designed to bind efficiently to a single site on your template [10].
2. The beginning of my sequence trace is noisy, but it clears up further down. Why? Noise or mixed sequence at the start of a trace is frequently caused by primer dimer formation. The primer self-hybridizes due to complementary bases on the primer itself. You can analyze your primer sequence using free online tools to ensure it is unlikely to form dimers [10].
3. Why does my high-quality sequence data suddenly stop? Sharp termination of good sequence data is usually a sign of secondary structure in the DNA template, such as hairpins formed by GC-rich regions. The sequencing polymerase cannot pass through these structures. Some core facilities offer alternate sequencing chemistries (e.g., "difficult template" protocols) that can sometimes help the polymerase read through these regions [10].
4. What are the broad, blobby peaks that appear around base 80 in my chromatogram? These are known as "dye blobs," and they represent aggregates of unincorporated dye terminators that co-migrate with DNA fragments during capillary electrophoresis. They appear as broad C or T peaks and can interfere with base calling. While cleanup protocols are designed to remove these dyes, no method is 100% effective. To avoid this issue, design primers so that your region of interest is at least 100 bases away from the primer binding site [12].
5. My sequence has good quality initially but then becomes mixed (shows double peaks). What does this mean? Double sequences can have a couple of causes [10]:
- Colony contamination: If you sequenced a bacterial colony, you may have accidentally picked more than one clone, resulting in a mixture of templates.
- Multiple priming sites: Your primer may be binding to more than one location on your template. Redesign your primer to ensure a single, unique annealing site.
Data Quality Metrics and Interpretation
Understanding the quality metrics embedded in your Sanger results is crucial for evaluating your data objectively. The following table summarizes key metrics to examine [12].
Table 1: Key Quality Metrics for Sanger Sequencing Data
| Metric | Description | Ideal Value/Range | Interpretation |
|---|---|---|---|
| Quality Value (QV) | A per-base score logarithmically related to the error probability (e.g., QV=20 means a 1% error rate). | ≥ 20 | Higher scores indicate more confident base calls. |
| Quality Score (QS) | The average QV for all assigned bases in the trace. | ≥ 40 | Indicates overall high-quality sequence. |
| Average Signal Intensity | The strength of the fluorescent signal, measured in relative fluorescence units (RFU). | > 1,000 RFU | Low values (<100) indicate noisy data; very high values (>10,000) can cause oversaturation. |
| Continuous Read Length (CRL) | The longest stretch of bases with a running average QV of 20 or higher. | > 500 bases | Common benchmark for high-quality data from plasmids or long PCR products. |
Sanger Sequencing in Clinical Research: A Protocol for Pathogen ID
The protocol below, adapted from recent clinical studies, outlines a standard methodology for identifying pathogens from clinical samples using broad-range PCR followed by Sanger sequencing [9].
Objective: To identify bacterial and fungal pathogens from culture-negative clinical samples (e.g., blood, CSF, tissue) via amplification and sequencing of conserved genomic markers.
Methodology:
DNA Extraction:
- Extract total DNA from 400 µL of clinical sample (e.g., whole blood, cerebrospinal fluid) using a commercial DNA extraction kit, such as the DNA Quick Miniprep kit.
- Determine DNA concentration and purity using a fluorescent assay (e.g., Qubit dsDNA BR assay) [9].
PCR Amplification:
- Use primers targeting conserved genomic regions:
- Reaction Setup: Use 1 µL of extracted DNA template, 2 µL of each primer (10 pmol/µL), and 47 µL of a master mix like GoTaq Green Master Mix.
- Cycling Conditions: Initial denaturation at 95°C for 5 min; 25 cycles of [95°C for 5 s, 60°C for 15 s, 72°C for 15 s]; final extension at 72°C for 5 min [9].
Gel Electrophoresis and Purification:
- Confirm successful amplification and specificity by running 5 µL of the PCR product on a 2% agarose gel.
- Purify the correct PCR band from the gel using a Gel DNA Recovery kit [9].
Sanger Sequencing:
- Submit the purified amplicon for Sanger sequencing using the BigDye Terminator cycle sequencing kit on a platform such as the Applied Biosystems 3500 Genetic Analyzer [9].
Data Analysis:
- Visually inspect the chromatograms for quality using software like Geneious Prime.
- Compare the obtained sequence to a reference database (e.g., NCBI BLAST) for pathogen identification [9].
Experimental Workflow Diagram
The end-to-end process for pathogen identification via Sanger sequencing is outlined below.
Research Reagent Solutions
Table 2: Essential Reagents for Pathogen Identification via Sanger Sequencing
| Reagent/Kit | Function | Example Product |
|---|---|---|
| DNA Extraction Kit | Isolates total genomic DNA from various clinical sample types. | DNA Quick Miniprep Kit [9] |
| PCR Master Mix | Provides enzymes, dNTPs, and buffer for robust amplification of target genes. | GoTaq Green Master Mix [9] |
| Gel DNA Recovery Kit | Purifies the specific DNA amplicon from an agarose gel post-electrophoresis. | Zymoclean Gel DNA Recovery Kit [9] |
| Cycle Sequencing Kit | Performs the chain-termination sequencing reaction with fluorescently labeled ddNTPs. | BigDye Terminator Kit [9] |
| Reference Material | Validates the entire workflow, from extraction to sequencing, ensuring accuracy. | WHO WC-Gut RR, NML Metagenomic Controls [8] |
The Limitation in Co-infections and the Rise of NGS
The primary strength of Sanger sequencing—generating a single, high-quality sequence from a pure template—becomes its critical weakness in complex samples. When multiple pathogens are present, the PCR amplification generates a mixture of templates. Since Sanger sequencing is a bulk sequencing method, it produces a consensus signal from all amplified products, resulting in unreadable, overlapping chromatograms [8]. This makes it impossible to identify the individual species in a polymicrobial infection.
Comparative Data: Sanger vs. mNGS for Co-infections A 2025 study on Lower Respiratory Tract Infections (LRTI) directly compared the performance of Sanger sequencing, metagenomic Next-Generation Sequencing (mNGS), and culture, using clinical samples. The results clearly illustrate the limitation of Sanger sequencing in detecting multiple pathogens [13].
Table 3: Comparison of Pathogen Detection in Bronchoalveolar Lavage (BALF) Samples [13]
| Method | Samples with Identical Results (All 3 Methods) | Samples with Co-infections Detected | Key Advantage |
|---|---|---|---|
| Microbial Culture | 49.41% (85/172) | 22 samples | Gold standard for viable, common bacteria. |
| Sanger Sequencing | 49.41% (85/172) | 64 samples | Good for single pathogen identification; faster than culture. |
| mNGS | 49.41% (85/172) | 66 samples | Superior for detecting co-infections and rare/unculturable pathogens. |
This data shows that while Sanger sequencing is a powerful tool, its utility is confined to specific clinical questions. For complex cases where co-infections are suspected, long-read sequencing technologies like Oxford Nanopore Technology (ONT) are now being implemented. ONT can sequence the entire ~1500 bp 16S rRNA gene and, crucially, resolve individual sequences from a mixed sample, providing species-level identification of all pathogens present [8] [5]. The diagram below illustrates this paradigm shift in diagnostic sequencing.
Troubleshooting Guides
Issue 1: Low Throughput Slows Down Screening for Multiple Pathogens
Problem: My project involves screening clinical samples for a panel of 20 potential bacterial pathogens. Using Sanger sequencing serially for each target is impractically slow.
Explanation: Sanger sequencing processes only a single DNA fragment per run, making it a low-throughput technique [14]. This "one reaction, one fragment" principle is fundamentally mismatched for projects requiring analysis of multiple genes or samples simultaneously [15] [16].
Solution: Implement a targeted Next-Generation Sequencing (NGS) panel. This approach sequences hundreds to thousands of genes in a single, massively parallel run [15]. The table below summarizes the throughput comparison.
Table 1: Throughput and Scalability Comparison
| Feature | Sanger Sequencing | Targeted NGS |
|---|---|---|
| Sequencing Scale | Single DNA fragment per run [14] | Millions of fragments simultaneously per run [15] |
| Suitability | Cost-effective for ~1-20 targets [15] | Cost-effective for high sample volumes and large gene panels (>20 targets) [15] [14] |
| Project Impact | Slow and expensive for multi-target screening | Enables high-throughput screening of multiple samples and targets [15] |
Experimental Protocol: Targeted NGS for Pathogen Detection
- DNA Extraction: Extract nucleic acids from the clinical sample (e.g., bronchoalveolar lavage fluid or sputum) using a standardized protocol [13].
- Library Preparation: Use a targeted enrichment approach, such as amplicon sequencing (e.g., Respiratory Pathogen Multiplex Detection Kit) or hybrid capture (e.g., Haloplex/SureSelect), to selectively amplify or capture the genomic regions of the target pathogens [13] [17].
- Sequencing: Load the prepared library onto a high-throughput sequencer (e.g., Illumina MiSeq or VisionSeq 1000) for massively parallel sequencing [13] [17].
- Bioinformatic Analysis: Analyze the resulting sequencing data using specialized software (e.g., IDseqTM-2) by aligning reads to a pathogen database to determine the presence and abundance of microorganisms [13].
Issue 2: Inability to Detect and Resolve Polymicrobial Co-infections
Problem: I suspect my samples contain mixed infections, but the Sanger sequencing electropherogram shows overlapping signals and is unreadable.
Explanation: In a co-infection, DNA from multiple organisms is amplified together. Sanger sequencing produces a single electropherogram per reaction. When different templates are present, the signal from each base position is a mixture, resulting in overlapping peaks that are impossible to interpret accurately [8]. Its detection limit for minor variants is typically 15-20%, meaning it cannot identify pathogens that make up a small fraction of the sample [18] [19].
Solution: Utilize metagenomic NGS (mNGS) or long-read sequencing (e.g., Oxford Nanopore Technologies). These methods sequence all DNA in a sample without targeting specific organisms and assign sequences to individual pathogens bioinformatically. One study demonstrated that mNGS identified co-infections in 66 BALF samples, significantly outperforming culture (22 samples) and matching the performance of another molecular method [13]. Long-read sequencing is particularly effective for resolving the full-length 16S rRNA gene in mixed samples, overcoming ambiguities inherent to Sanger [5] [8].
Experimental Protocol: 16S rRNA Gene Sequencing with Long Reads for Polymicrobial Infections
- Sample Preparation and DNA Extraction: Lyse samples, including bead-beating for tough cell walls. Extract DNA using a validated kit [8].
- PCR Amplification: Amplify the near-full-length ~1500 bp 16S rRNA gene using universal bacterial primers.
- Library Preparation & Sequencing: Prepare the library using a kit like the Ligation Sequencing Kit and load it on a MinION flow cell for real-time sequencing on the GridION or PromethION platform [8].
- Bioinformatic Analysis: Use a real-time basecalling software (e.g., MinKNOW). Process the data through a pipeline that performs demultiplexing, quality filtering, and taxonomic classification by comparing reads to a 16S database (e.g., SILVA) [8].
Table 2: Detection of Co-infections in Clinical Samples (BALF) [13]
| Method | Number of Samples with Co-infections Identified |
|---|---|
| Metagenomic NGS (mNGS) | 66 |
| Sanger Sequencing | 64 |
| Conventional Culture | 22 |
Issue 3: Failed Detection of Low-Frequency Variants or Minor Populations
Problem: I am trying to identify a rare, drug-resistant subpopulation present at 5% frequency, but Sanger sequencing fails to detect it.
Explanation: Sanger sequencing is an analog technique that produces a consolidated signal from all DNA molecules in a reaction. A variant present in a small fraction of the sample (<15-20%) will not produce a signal strong enough to be distinguished from background noise [18] [19]. Its low sequencing depth (each base is typically sequenced once) provides no statistical power for rare variant detection [16].
Solution: For validating known low-frequency variants, use Blocker Displacement Amplification (BDA) coupled with Sanger sequencing. For discovering unknown rare variants, deep-targeted NGS is required.
- BDA + Sanger: This method uses sequence-specific blockers to inhibit the amplification of the wild-type sequence, thereby dramatically enriching the minor variant. The enriched product can then be confirmed by Sanger sequencing, pushing its effective limit of detection down to ~0.1% [18].
- Deep-Targeted NGS: This digital method sequences each molecule thousands of times, providing high sequencing depth. This allows for the detection of low-frequency variants with high confidence, as the variant allele frequency can be quantified from the read counts [17] [19]. NGS can detect variants with a limit of detection as low as 1% [15] [14].
Experimental Protocol: Confirming Low-Frequency Variants with BDA and Sanger Sequencing [18]
- Assay Design: Use software (e.g., NGSure) to design locus-specific PCR primers and a blocker oligonucleotide that binds perfectly to the wild-type sequence, suppressing its amplification.
- Blocker Displacement Amplification (BDA): Perform qPCR on the sample DNA using the primers and blocker. The blocker is displaced when the variant template is amplified, leading to its preferential enrichment.
- Sanger Sequencing: Purify the BDA product and perform Sanger sequencing.
- Analysis: Compare the sequencing chromatogram from the BDA-enriched sample to an unenriched control. The clear appearance of a variant peak indicates a true positive low-frequency variant.
Frequently Asked Questions (FAQs)
Q1: If NGS is superior, is there any reason I should still use Sanger sequencing? Yes, Sanger sequencing remains the gold standard for confirming single-gene variants discovered by NGS due to its very high accuracy for targeted interrogation [17] [16]. It is also cost-effective and efficient for projects involving a limited number of samples and targets, such as validating plasmid constructs or diagnosing single-gene disorders [15] [14] [19].
Q2: What are the key reagent solutions for implementing a long-read sequencing workflow for co-infections? Table 3: Research Reagent Solutions for 16S rRNA Long-Read Sequencing
| Item | Function | Example/Note |
|---|---|---|
| Characterized Reference Materials | Validates entire workflow accuracy using samples with known microbial composition [8]. | NML Metagenomic Control Materials (MCM2α/β), WHO WC-Gut RR [8]. |
| Bead-Beating Tubes | Ensures mechanical lysis of tough bacterial cell walls for efficient DNA extraction [8]. | Lysing Matrix E tubes [8]. |
| DNA Extraction Kit | Isolates high-quality genomic DNA from clinical samples. | AusDiagnostics MT-Prep, GeneRead DNA FFPE Kit [8]. |
| 16S rRNA PCR Primers | Amplifies the target gene for sequencing from a wide range of bacteria. | Universal bacterial primers targeting ~1500 bp region [8]. |
| Long-Red Sequencing Kit | Prepares the amplified DNA library for loading onto the sequencer. | ONT Ligation Sequencing Kit [8]. |
| Bioinformatic Pipeline | Performs basecalling, demultiplexing, quality filtering, and taxonomic classification. | MinKNOW for basecalling, alignment to SILVA database [8]. |
Q3: My Sanger sequencing of a co-infection sample failed. Could the problem be my DNA extraction method? Possibly. The presence of inhibitors from the clinical sample or inefficient lysis of certain pathogen types (e.g., gram-positive bacteria with tough cell walls) can lead to PCR amplification failure, which will result in a failed Sanger sequence. Incorporating bead-beating during DNA extraction and using internal controls can help mitigate this issue [8].
Q4: Are the limitations of Sanger sequencing primarily due to cost or fundamental technology? The limitations are fundamentally technological. The core chemistry of processing one fragment at a time inherently creates bottlenecks in throughput, detection range, and sensitivity for complex mixtures [15] [14]. While cost is a factor for large projects, it is a consequence of this underlying low-throughput design.
Sanger sequencing remains the gold standard for validating sequencing results due to its high single-base accuracy and long read lengths of 500-800 bp [20]. However, in the critical field of co-infections research—where samples often contain multiple pathogenic organisms—researchers frequently encounter two persistent technical bottlenecks: mixed template sequences and excessive background noise. These artifacts compromise data quality, leading to ambiguous base calls and unreliable sequences that can hinder accurate pathogen identification. This technical support center guide provides targeted troubleshooting protocols to overcome these specific challenges, enabling robust Sanger sequencing data from complex clinical and environmental samples.
FAQ: Addressing Mixed Template Sequences
What causes mixed sequences (multiple peaks) in my chromatograms?
Mixed sequences appear as overlapping peaks of two or more colors at the same position in the chromatogram, indicating that multiple DNA templates are being sequenced simultaneously [21]. In co-infections research, this could genuinely reflect biological reality, but more often stems from technical artifacts.
- Colony Contamination ("Double Picking"): Accidentally picking two or more bacterial colonies during culture leads to sequencing multiple DNA clones [10].
- PCR Primer Contamination: Residual PCR primers from amplification reactions not being thoroughly cleaned up can act as unintended sequencing primers [10] [21].
- Multiple Priming Sites: The sequencing primer binds to more than one location on the template DNA, generating extension products from different sites [10] [22].
- Heterogeneous PCR Products: The initial PCR amplification may contain multiple products of similar size, which are then co-sequenced [21].
- True Biological Co-infections: The sample genuinely contains two or more different pathogen strains or species [13] [5].
How can I resolve mixed template issues?
Table 1: Troubleshooting Steps for Mixed Template Sequences
| Problem Cause | Diagnostic Step | Corrective Action |
|---|---|---|
| Colony Contamination | Inspect original colony plates for closely spaced colonies. | Re-isolate single, well-spaced colonies and prepare new plasmid DNA [10] [21]. |
| Multiple PCR Products | Run PCR product on agarose gel. | Gel-purify the single correct band before sequencing [22] [21]. |
| Residual PCR Primers | Review PCR clean-up protocol. | Implement a rigorous PCR purification protocol using validated kits [10] [21]. |
| Multiple Priming Sites | In silico analysis of primer binding sites. | Redesign sequencing primer to ensure a single, unique binding site [10] [22]. |
| Low Annealing Temperature | Check sequencing reaction thermal cycler protocol. | Increase the annealing temperature in the cycle sequencing reaction to improve specificity [21]. |
Experimental Protocol: Verification of Single Template
To confirm a single template source before sequencing:
- Gel Electrophoresis: After PCR amplification, run the product on a high-percentage agarose gel (e.g., 2-3%). Look for a single, sharp band of the expected size. The presence of multiple or smeared bands indicates a heterogeneous product [21].
- PCR Purification: Use a spin-column-based PCR purification kit according to the manufacturer's instructions. This removes excess salts, dNTPs, and, crucially, the original PCR primers [10].
- Quantification: Accurately measure the DNA concentration using a fluorometer (e.g., Qubit) or spectrophotometer (e.g., NanoDrop). Ensure the 260/280 ratio is ~1.8 for pure DNA [10] [23].
Diagram: A workflow for diagnosing and resolving mixed template sequences in Sanger sequencing.
FAQ: Managing Background Noise
What generates background noise in my sequencing traces?
Background noise manifests as smaller, undefined peaks beneath the primary sequencing peaks, creating a "noisy" baseline that interferes with accurate base-calling [23]. This noise can be categorized and its causes are specific.
- Baseline Noise: Low-intensity, random peaks often caused by poor template quality, contaminants, or instrument issues [23] [22].
- Dye Artifacts ("Dye Blobs"): Broad, unidentified peaks, often around 70-80 bases, caused by unincorporated fluorescent dye terminators that were not fully removed during cleanup [10] [12].
- N+1/N-1 Peaks: Smaller peaks immediately adjacent to the main peak, resulting from incomplete termination by the ddNTPs during the extension reaction [23].
- Weak Signals: Low, poorly resolved peaks due to insufficient template DNA, poor primer binding, or degraded reagents [10] [23].
- Polymerase Slippage: Noise following a homopolymer region (e.g., a run of "AAAAA") due to the polymerase enzyme dissociating and re-associating incorrectly [10].
How can I minimize background noise?
Table 2: Troubleshooting Guide for Background Noise
| Noise Type | Primary Cause | Solution |
|---|---|---|
| High Baseline Noise | Poor DNA quality/purity; multiple priming sites. | Re-purify DNA; ensure 260/280 ratio ≥1.8; redesign primer for unique site [23] [22]. |
| Dye Blobs | Inefficient cleanup of sequencing reaction. | Optimize cleanup protocol; ensure proper vortexing if using magnetic beads; avoid ethanol over-concentration [22]. |
| N+1/N-1 Peaks | Incomplete termination in cycle sequencing. | Use fresh, high-quality BigDye terminator mix; optimize ddNTP concentration [23]. |
| Weak Signals | Low template concentration; degraded primer. | Quantify DNA accurately with fluorometer; use 50-300 ng plasmid DNA; store primers properly [10] [22]. |
| Noise after Homopolymers | Polymerase slippage on repetitive sequences. | Sequence from the opposite strand; use a primer located just after the repetitive region [10]. |
Experimental Protocol: Template Purification for Noise Reduction
A critical step for minimizing noise is using high-quality, pure DNA template.
- Extraction: Use a spin-column-based DNA extraction kit tailored to your sample type (e.g., plasmid, tissue, blood) [23].
- Quality Assessment:
- Use a NanoDrop or similar spectrophotometer. Acceptable purity ratios are 260/280 ≈ 1.8 and 260/230 ≈ 2.0-2.2.
- Run agarose gel electrophoresis to check for DNA integrity (sharp band, no smearing).
- Post-PCR Purification: Always clean up PCR products before sequencing. Use a reliable PCR purification kit to remove enzymes, salts, and excess primers. This step alone can reduce background noise by 80-85% [23].
- Storage: Store purified DNA and primers at -20°C or -80°C to maintain stability.
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Troubleshooting Sanger Sequencing
| Reagent/Material | Function & Role in Troubleshooting |
|---|---|
| High-Fidelity DNA Polymerase | Used in initial PCR; reduces amplification errors and non-specific products that cause noise [23]. |
| Spin-Column PCR Purification Kits | Removes residual primers, dNTPs, and salts from PCR products to prevent mixed templates and dye blobs [10] [23]. |
| BigDye Terminator Kit | The core chemistry for cycle sequencing. Use fresh, in-date reagents for optimal termination and signal strength [22]. |
| BigDye XTerminator Purification Kit | Magnetic bead-based cleanup specifically for BigDye reactions; highly effective at removing unincorporated dyes to reduce noise [22]. |
| Control DNA (e.g., pGEM-pGEM Control) | A known, high-quality DNA template and primer provided in kits to distinguish sample problems from reagent/instrument failures [22]. |
| Hi-Di Formamide | Used to resuspend purified sequencing products before capillary electrophoresis; ensures proper sample denaturation and migration [22]. |
Advanced Data Analysis & Validation
How do I interpret quality metrics in my sequencing data?
Modern sequencing analysis software provides quantitative metrics to objectively assess data quality [12].
- Quality Value (QV): A per-base score where QV = -10 × log(error probability). A QV of 20 indicates a 1% base-calling error rate. Actionable Threshold: Bases with QV < 20 should be visually inspected; those with QV < 10 are often called as 'N' and are unreliable [12].
- Quality Score (QS): The average QV for the entire trace. Interpretation: QS ≥ 40 indicates high-quality data; QS ~30 requires careful review; QS < 20 indicates poor, unreliable data [12].
- Signal Intensity: Measured in Relative Fluorescence Units (RFU). Optimal Range: Peaks between 1,000 and 8,000 RFU. Intensity < 100 RFU is too weak and noisy; > 10,000 RFU can cause sensor oversaturation and "spectral pull-up" [12].
A Framework for Validating Sequences in Co-infections Research
When Sanger sequencing indicates a potential co-infection, a rigorous validation workflow is essential to distinguish technical artifacts from biological reality.
Diagram: A decision framework for validating potential co-infections after initial Sanger sequencing results.
Validation Protocol Using Sanger Sequencing:
- Bidirectional Sequencing: Always sequence the same genomic region from both forward and reverse primers. True mutations or mixed bases will appear in both directions, while artifacts often will not.
- Independent PCR Amplification: Repeat the entire process, starting from a new biological sample or DNA aliquot, through independent PCR and sequencing. This controls for errors introduced in a single reaction.
- Sub-cloning: For persistent mixed signals, clone the PCR product into a plasmid vector. Then, sequence multiple individual colonies. If the mixture is a technical artifact, individual clones will show pure sequences. If it's a true co-infection, different clones will show distinct, pure sequences corresponding to the different strains/species [5].
Sanger sequencing remains an indispensable tool for life science research, but its limitations in analyzing complex, mixed samples must be acknowledged and managed. The troubleshooting guides and FAQs presented here provide a systematic approach to diagnosing and resolving the two most common technical bottlenecks—mixed templates and background noise. By implementing rigorous sample preparation protocols, understanding data quality metrics, and employing confirmatory experimental workflows, researchers can generate reliable, high-quality Sanger data. For the most complex co-infections where Sanger reaches its limits, integrating it with orthogonal methods like mNGS or Nanopore sequencing provides a powerful strategy to validate findings and ensure research integrity [13] [5].
Sanger sequencing has long been the gold standard for DNA sequencing in clinical and research settings due to its high accuracy and reliability [24]. However, a significant diagnostic limitation emerges when analyzing samples containing mixed populations of microorganisms, as occurs in co-infections. This technical support guide examines the specific scenarios where Sanger sequencing fails to detect co-infections, explores the underlying technical mechanisms for these failures, and presents advanced methodological solutions to overcome these limitations in research and drug development settings.
Frequently Asked Questions (FAQs)
1. Why can't Sanger sequencing detect multiple pathogen strains in a single sample?
Sanger sequencing operates on the principle of bulk analysis, where signals from all DNA molecules in a sample are averaged during the sequencing reaction. When multiple pathogen strains are present, their genetic variations at the same nucleotide position produce overlapping fluorescence signals that the sequencing software cannot resolve. This results in ambiguous base calling, often appearing as overlapping peaks in the chromatogram that are typically misinterpreted as noise or sequencing artifacts rather than true biological mixtures [24] [12].
2. What is the minimum variant frequency required for reliable detection by Sanger sequencing?
Sanger sequencing reliably detects genetic variants only when they are present as the dominant population in a sample. The established detection threshold is approximately 15-20% of the total genetic material [25]. Variants present below this threshold typically fail to generate sufficient signal strength for detection. Next-generation sequencing (NGS), in contrast, can detect variants at frequencies as low as 1-5%, providing significantly higher sensitivity for identifying minority variants in mixed infections [25].
3. In which specific research scenarios is this limitation most problematic?
The co-infection detection gap poses significant challenges in several critical research areas:
- Antimicrobial resistance studies: Where emergent resistant subpopulations may be present below the detection threshold [25]
- Viral quasispecies analysis: Particularly in HIV and hepatitis C research, where heterogeneous viral populations are common [25]
- Complex infection models: Including polymicrobial biofilms and multi-pathogen infections [26] [27]
- Vaccine efficacy research: Where monitoring for escape mutants requires sensitive variant detection [26]
4. What are the primary technical factors limiting mixed infection detection?
Three key technical factors constrain detection sensitivity:
- Signal averaging: Fluorescence signals from all templates are combined during capillary electrophoresis
- Base-calling algorithms: Designed to call a single base per position, disregarding mixed signals
- Template concentration bias: PCR amplification preferentially amplifies dominant templates, further reducing minority variant signals [3] [22] [24]
Technical Limitations and Detection Thresholds
Table 1: Comparative Detection Thresholds of Sequencing Technologies
| Technology | Variant Detection Threshold | Optimal Read Length | Co-infection Detection Capability |
|---|---|---|---|
| Sanger Sequencing | 15-20% | 500-1000 bp | Limited to dominant strain |
| Pyrosequencing | 5-10% | 100-500 bp | Moderate for major subpopulations |
| Illumina NGS | 1-5% | 50-300 bp | High sensitivity for mixed infections |
| Ion Torrent NGS | 1-5% | 200-400 bp | High sensitivity for mixed infections |
| PacBio SMRT | 0.1-1% | 10,000-50,000 bp | Excellent for haplotype resolution |
| Oxford Nanopore | 0.1-1% | 10,000-100,000 bp | Excellent for full-length variant assembly |
Table 2: Impact of Detection Thresholds on HIV Drug Resistance Monitoring
| Detection Threshold | Reported PDR Prevalence | Ability to Predict Virologic Failure | Clinical Utility |
|---|---|---|---|
| 1% | 29.74% | Highest sensitivity | Research setting |
| 2% | 22.43% | High sensitivity | Optimal for clinical detection |
| 5% | 15.47% | Moderate improvement | Better than Sanger |
| 10% | 12.95% | Slight improvement | Limited advantage |
| 20% (Sanger) | 11.08% | Baseline | Standard reference |
Troubleshooting Guide: Identifying Co-infection Detection Failures
Problem: Mixed Chromatogram Signals
How to Identify: Double or overlapping peaks at multiple positions throughout the sequencing trace, particularly when the overall sequence quality metrics appear normal [3] [24]. The quality scores (QV) for these positions are typically low (<20), and the base-calling software may assign "N" instead of a specific base [12].
Underlying Cause: The presence of multiple genetic templates with sequence variations at the same position. This occurs during co-infections with genetically distinct strains of the same pathogen or infections with multiple pathogen species [26] [5].
Solutions:
- Employ nested PCR with specific primers to amplify and separate individual strains
- Implement clonal amplification by subcloning PCR products before sequencing
- Transition to NGS platforms that can sequence individual molecules, preserving variant information [26] [25]
Problem: Abrupt Sequence Quality Deterioration
How to Identify: High-quality sequencing data that suddenly becomes noisy or terminates prematurely, particularly in regions with homopolymer repeats or secondary structures [3].
Underlying Cause: Polymerase slippage on repetitive regions or secondary structures in mixed templates, leading to heterogeneous fragment populations that disrupt electrophoretic separation [3] [22].
Solutions:
- Use specialized polymerases designed for difficult templates
- Optimize reaction conditions with additives like DMSO or betaine
- Implement long-read sequencing technologies (PacBio, Oxford Nanopore) that better handle repetitive regions [5] [28]
Problem: Selective Template Amplification
How to Identify: Consistent failure to detect known minority variants despite their confirmed presence through alternative methods.
Underlying Cause: PCR amplification bias during template preparation, where primers preferentially amplify certain templates due to sequence mismatches or secondary structures [24].
Solutions:
- Redesign primers to target conserved regions across potential variants
- Use high-fidelity, proofreading polymerases with minimal amplification bias
- Implement metagenomic sequencing without targeted amplification [27] [28]
Experimental Protocols for Overcoming Detection Limitations
Protocol 1: Clonal Separation for Strain Discrimination
Purpose: To physically separate mixed templates before sequencing to enable individual characterization of each strain in a co-infection.
Materials:
- TOPO TA Cloning Kit or equivalent
- Competent E. coli cells
- Plasmid purification kit
- Strain-specific growth media
Procedure:
- Amplify target gene using standard PCR conditions
- Ligate PCR products into cloning vector following manufacturer's protocol
- Transform competent E. coli cells and plate on selective media
- Pick individual colonies (minimum of 20-50) and culture overnight
- Purify plasmid DNA from each culture
- Sequence inserts using standard Sanger sequencing
- Analyze sequences to identify distinct strains [26]
Protocol 2: NGS-Based Co-infection Analysis
Purpose: To comprehensively characterize all strains present in a co-infction without prior separation.
Materials:
- Illumina MiSeq or comparable NGS platform
- DNA library preparation kit
- Bioinformatic analysis software (IDseq, BLAST)
Procedure:
- Extract total DNA/RNA from clinical sample
- Prepare sequencing library following manufacturer's protocol
- Sequence using appropriate NGS platform
- Process raw reads through quality control filters
- Perform de novo assembly of contigs
- Map reads to reference sequences
- Identify strain-specific variations using variant calling algorithms [26] [13]
Diagnostic Workflow Visualization
Diagram 1: Co-infection Detection Workflow Comparison
Research Reagent Solutions
Table 3: Essential Reagents for Advanced Co-infection Studies
| Reagent/Kit | Application | Function in Co-infection Research |
|---|---|---|
| SepsiTest UVD | Direct pathogen DNA isolation | Selective removal of human DNA to enhance microbial signal in mixed infections [27] |
| BigDye Terminator v3.1 | Cycle sequencing | Fluorescent labeling for Sanger sequencing; optimized for difficult templates [22] |
| Micro-Dx Platform | Automated DNA extraction | Standardized processing for culture-independent diagnosis [27] |
| Ion Torrent SS | Semiconductor sequencing | Rapid detection of multiple pathogens without cultivation [28] |
| Vision Respiratory Pathogen Kit | Targeted NGS | Multiplex detection of common respiratory pathogens in co-infections [13] |
| PacBio SMRTbell | Long-read sequencing | Full-length haplotype resolution for strain discrimination [5] [28] |
Advanced Methodologies for Co-infection Resolution
Metagenomic Next-Generation Sequencing (mNGS)
Metagenomic NGS represents a paradigm shift in co-infection detection by eliminating the need for targeted amplification. In comparative studies of lower respiratory tract infections, mNGS demonstrated significantly enhanced detection capabilities for co-infections, identifying 66 co-infected samples in bronchoalveolar lavage fluid compared to 22 detected by culture methods [13]. The unbiased nature of mNGS allows for the detection of unexpected pathogens, fastidious organisms, and novel infectious agents that would be missed by hypothesis-driven testing approaches.
Long-Read Sequencing Technologies
Third-generation sequencing platforms from PacBio and Oxford Nanopore Technologies enable complete resolution of co-infections through ultra-long reads that preserve haplotype information. A study on avian haemosporidian parasites demonstrated that nanopore sequencing successfully resolved cryptic co-infections that were ambiguous by Sanger sequencing, enabling the identification of two novel Haemoproteus lineages and one Plasmodium lineage in a single host [5]. The assembly of unfragmented mitogenomes through long-read sequencing overcomes the phase ambiguity inherent in short-read technologies.
The diagnostic gap in Sanger sequencing's ability to detect co-infections represents a significant limitation in both research and clinical settings. As demonstrated through the technical guidelines presented here, understanding these limitations is the first step toward implementing appropriate methodological solutions. The integration of NGS technologies, particularly metagenomic and long-read sequencing approaches, provides researchers with powerful tools to overcome these challenges and gain a more comprehensive understanding of complex microbial communities in co-infection scenarios. For research and drug development professionals, selecting the appropriate sequencing strategy based on the specific requirements of variant detection sensitivity, throughput, and analytical depth is crucial for successful characterization of co-infections.
Implementing Metagenomic NGS: A Practical Framework for Co-Infection Detection
Untargeted, hypothesis-free sequencing represents a paradigm shift in pathogen detection. Unlike traditional methods that require pre-defined suspects, these approaches use next-generation sequencing (NGS) to comprehensively analyze all nucleic acids in a sample. This guide explores the principles of these powerful methods and provides practical support for researchers overcoming the limitations of Sanger sequencing in co-infections research.
Core Principles: Why Move Beyond Targeted Methods?
The Power of an Unbiased Approach
Hypothesis-free pathogen detection relies on metagenomic next-generation sequencing (mNGS), which uses shotgun sequencing to randomly sample DNA and RNA from clinical specimens. This allows for broad identification of known, unexpected, and even novel pathogens without prior suspicion [29].
Key Advantages Over Conventional Testing
- Unbiased Sampling: Detects nearly any organism, leading to a dramatic paradigm shift in microbial diagnostic testing [29].
- Discovery Capability: Enables identification of unexpected pathogens or discovery of new organisms [29] [13].
- Comprehensive Genomic Data: Provides auxiliary information for evolutionary tracing, strain identification, and prediction of drug resistance [29].
- Solving Co-infections: Particularly valuable for detecting multiple pathogens in a single sample, a scenario where Sanger sequencing often fails [13] [30].
The Critical Limitation of Sanger Sequencing in Co-infections
Sanger sequencing, while a gold standard for single targets, encounters significant limitations in complex samples:
"In mixed cultures or samples with poly-microbial contamination, mixed sequences occur in Sanger sequencing that do not allow reliable pathogen identification" [30].
This fundamental limitation is precisely where mNGS excels, as it can independently sequence thousands to billions of DNA fragments simultaneously [29].
Essential Research Reagent Solutions
Table: Key Reagents for Untargeted Sequencing Workflows
| Item | Function | Considerations |
|---|---|---|
| Nucleic Acid Extraction Kit | Recovers DNA/RNA from diverse sample types (blood, tissue, BALF). | Select kits designed to provide long, intact strands (>1,500 bp) for optimal sequencing [31]. |
| PCR Reagents | Amplifies specific targets or whole genomes for library preparation. | Use high-fidelity polymerases. Hot-Start PCR Kits reduce non-specific amplification [32]. |
| qPCR Master Mix | Quantifies nucleic acid concentration pre-sequencing; verifies findings. | Essential for confirming template quality and quantity before library prep [33]. |
| Library Preparation Kit | Fragments, repairs, and adapts DNA for sequencing on a specific platform. | Platform-specific (e.g., Illumina, Ion Torrent, Nanopore). Critical for efficient sequencing. |
| Sequencing Primers | Initiates the sequencing reaction. | Should be designed to bind at least 60-100 bp away from key regions of interest for optimal Sanger results [12]. |
Workflow & Technology Comparison
The following diagram illustrates the core logical relationship and workflow differences between the targeted Sanger approach and the untargeted mNGS approach for pathogen detection.
Performance Data: mNGS vs. Conventional Methods
Recent studies directly compare the performance of mNGS against standard microbiological culture, using Sanger sequencing as a reference.
Table: Detection performance of mNGS versus culture in respiratory samples [13]
| Sample Type | Total Samples | Identical Results (All Methods) | mNGS & Sanger Results Match | More Pathogens Detected by mNGS | Co-infections Identified (mNGS vs. Culture) |
|---|---|---|---|---|---|
| Sputum | 322 | 52.05% (165/317) | 88.20% (284/322) | 9% (29/322) | Not Specified |
| Bronchoalveolar Lavage Fluid (BALF) | 184 | 49.41% (85/172) | 91.30% (168/184) | 7.61% (14/184) | 66 (mNGS) vs. 22 (Culture) |
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: Is metagenomic sequencing truly "hypothesis-free"?
While often described as "unbiased" or "agnostic," mNGS is not entirely free of underlying assumptions. The experiment depends on hypotheses dictated by the sequencing technology and bioinformatic analysis. For instance, it is inherently biased towards detecting organisms whose nucleic acids can be recovered and whose sequences are present in reference databases [34] [35]. It is more accurate to consider it a "hypothesis-generating" tool that is unbiased by prior pathophysiological assumptions.
Q2: For common lower respiratory infections, is mNGS always necessary?
Not always. For common bacterial pathogens susceptible to culture, conventional methods are often sufficient and more cost-effective. However, mNGS provides significant advantages in detecting rare, fastidious, or difficult-to-culture pathogens and is particularly useful for identifying co-infections, as demonstrated by its ability to find nearly three times more co-infections in BALF samples than culture [13].
Q3: What is the biggest challenge when starting with mNGS?
A key challenge is that microbial nucleic acids in most patient samples are dominated by human host background, often constituting >99% of the sequenced reads. This drastically limits the analytical sensitivity for pathogen detection and requires sufficient sequencing depth to ensure adequate microbial genome coverage [29].
Q4: My Sanger sequencing results in unreadable chromatograms for poly-microbial samples. What is the solution?
This is a classic limitation of Sanger sequencing. When primers amplify multiple different targets, the resulting chromatogram contains overlapping signals from mixed sequences, making it uninterpretable [30]. The solution is to transition to an mNGS approach, which sequences individual DNA fragments independently, thereby resolving the components of a co-infection.
Troubleshooting Guides
Issue 1: Low Pathogen Signal in mNGS Data (High Host Background)
- Problem: The vast majority of sequencing reads are from the host, masking the pathogenic signal.
- Potential Solutions:
- Increase Sequencing Depth: Sequence more deeply to increase the likelihood of capturing rare microbial reads.
- Host Depletion: Employ probe-based or enzymatic methods to selectively remove human host DNA/RNA before library preparation.
- Sample Enrichment: If a specific type of pathogen is suspected (e.g., viruses), use targeted enrichment panels to pull down relevant sequences from the complex mixture.
Issue 2: Interpreting Relevance of Detected Microbes
- Problem: mNGS detects microbial sequences, but not all are clinically pathogenic. Distinguishing contamination, colonization, and true infection is difficult.
- Potential Solutions:
- Use Quantitative Thresholds: Establish minimum thresholds for reporting, such as Reads Per Million (RPM). For example, one study used an RPM threshold of 1 for most bacteria, and a more sensitive 0.1 RPM for tricky pathogens like Mycoplasma pneumoniae and fungi [13].
- Statistical Outliers: Compare the abundance of a suspected pathogen across all samples in a run. One protocol considered a pathogen relevant if its read count was greater than the 4th standard deviation above the mean of all samples [30].
- Correlate with Clinical Data: Always integrate mNGS findings with patient symptoms, other lab results, and imaging.
Issue 3: Inaccurate Base Calls in Sanger Sequencing (For Validation)
- Problem: Even when used for validation, Sanger sequencing can produce poor-quality data, leading to incorrect base calls.
- Potential Solutions:
- Visualize Chromatograms: Always inspect the chromatogram trace file; do not rely solely on the text sequence. Look for sharp, well-spaced peaks [12].
- Check Quality Metrics: Use embedded quality values (QV). A QV of 20 indicates a 1% error probability. Bases with QV < 10 should be considered unreliable [12].
- Optimize Template: Ensure the DNA template submitted for Sanger sequencing is pure, concentrated, and represents a single, specific amplicon. Avoid degenerate primers and always purify PCR products to remove enzymes and unused nucleotides [31].
Accurate pathogen identification is fundamental to infectious disease research and therapeutic development. For decades, Sanger sequencing has served as the gold standard for confirming the identity of microbial isolates, providing high accuracy for single-pathogen detection [36]. However, a significant limitation arises in the context of polymicrobial or co-infections, where multiple pathogens coexist within a single sample. Sanger sequencing struggles to resolve mixed chromatograms resulting from multiple templates, often leading to uninterpretable data and missed secondary pathogens [5]. This technical brief compares the established Sanger workflow with the emerging paradigm of metagenomic next-generation sequencing (mNGS), focusing on their application in co-infections research. We detail protocols, troubleshooting guides, and reagent solutions to empower researchers in selecting the appropriate methodological framework for their investigative needs.
Workflow Comparison: Sanger Sequencing vs. mNGS
The following diagrams and tables summarize the core procedural and performance differences between the two methodologies.
Visual Workflow Comparison
The diagram below illustrates the fundamental differences in process and complexity between Sanger sequencing and mNGS.
Performance Characteristics in Pathogen Detection
Table 1: Quantitative Comparison of Sanger Sequencing and mNGS Performance
| Parameter | Sanger Sequencing | Metagenomic NGS (mNGS) |
|---|---|---|
| Detection Principle | Targeted sequencing of a single, specific PCR amplicon [36] | Untargeted, shotgun sequencing of all nucleic acids in a sample [37] |
| Optimal Use Case | Confirming identity of a single, isolated pathogen | Comprehensive detection of all potential pathogens (bacteria, viruses, fungi, parasites) without prior suspicion [37] |
| Throughput | One target per reaction | Thousands to millions of sequences in parallel [37] |
| Typical Turnaround Time | 1-2 days | 1-3 days [38] |
| Ability to Detect Co-infections | Limited; fails with mixed templates [5] | High; readily identifies multiple pathogens [13] [39] |
| Sensitivity in Clinical Samples | Dependent on prior culture and target concentration | High; can detect low-abundance and unculturable pathogens [13] [38] |
| Quantitative Data | No | Semi-quantitative (e.g., Reads Per Million - RPM) [13] |
| Cost per Sample | Low | High |
Table 2: Empirical Detection Rates in Lower Respiratory Tract Infection Studies
| Method | Sample Type | Positive Detection Rate | Co-infection Identification | Key Findings |
|---|---|---|---|---|
| Sanger Sequencing | 322 Sputum Samples | Used as reference method in study [13] | Limited by design | 88.2% concordance with mNGS in sputa; effective for confirming single targets [13] |
| mNGS | 322 Sputum Samples | 88.20% (284/322) [13] | Significant advantage | Detected more species than Sanger in 9% of cases [13] |
| mNGS | 184 BALF Samples | 91.30% (168/184) [13] | Significant advantage | Identified co-infections in 66 samples, vs. 64 by Sanger and 22 by culture [13] |
| mNGS | 165 LRTI Patients (Multiple Specimens) | 86.7% (143/165) [39] | Significant advantage | Detected 29 kinds of pathogens missed by traditional methods, including viruses and anaerobic bacteria [39] |
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: My Sanger sequencing results for a directly processed clinical sample show mixed base calls and noisy chromatograms. What is the likely cause and solution?
A: This is a classic indicator of a co-infection or polymicrobial sample [5]. Sanger sequencing reactions are designed for a single, pure DNA template. When multiple templates with variations in the target region are present, the overlapping signals create uninterpretable chromatograms.
- Solution A (Sanger Path): Isolate individual pathogens by subculturing the sample on selective media to obtain pure colonies, then sequence each isolate separately. This is time-consuming and may miss unculturable organisms.
- Solution B (mNGS Path): Switch to an mNGS workflow. mNGS is inherently designed to handle mixed templates and will generate individual sequence reads that can be sorted bioinformatically to identify each distinct pathogen present [13] [5].
Q2: For mNGS, how do I determine if a detected microbe is a true pathogen versus background contamination or colonization?
A: This is a critical challenge in interpreting mNGS data. A multifaceted approach is required:
- Use Negative Controls: Include extraction and library preparation controls in every batch. Any pathogen found in both the sample and the control is likely contamination.
- Apply Quantitative Thresholds: Use validated, pathogen-specific thresholds. For example, one study used RPM ≥ 1 for most bacteria and RPM ≥ 0.1 for fungi like Aspergillus fumigatus to define a positive result [13].
- Correlate with Clinical Data: Integrate findings with patient symptoms, immune status, and other lab results (e.g., white blood cell count, procalcitonin). The clinical picture is essential for determining significance.
Q3: The high human host background in my mNGS data from bronchoalveolar lavage fluid (BALF) is limiting pathogen detection sensitivity. How can I improve this?
A: Host nucleic acid is a major confounder in mNGS. Several strategies can mitigate this:
- Sample Pre-treatment: Use commercial host DNA depletion kits (e.g., MolYsis Basic5) which selectively degrade human DNA while leaving microbial cells intact [40].
- Probe-Based Enrichment: Implement targeted enrichment panels using probes that hybridize to and capture pathogen nucleic acids prior to sequencing. One study showed this can boost unique pathogen reads by 34.6-fold and significantly improve genome coverage, especially for viruses [41] [42].
- Specimen Selection: BALF generally has a lower host background compared to sputum.
Essential Research Reagent Solutions
Table 3: Key Reagents and Kits for Sanger and mNGS Workflows
| Reagent / Kit | Function | Application Notes |
|---|---|---|
| Silica Column-based DNA Extraction Kits (e.g., TIANamp Micro DNA Kit [38]) | Extracts nucleic acids from various sample types. | Fundamental for both Sanger and mNGS. For mNGS, ensures broad lysis of diverse microbes. |
| BigDye Terminator Kit | The core chemistry for Sanger cycle sequencing, using fluorescently labeled ddNTPs [36]. | Essential for the Sanger workflow. Requires post-reaction clean-up to remove unincorporated dyes. |
| VAHTS Universal Plus DNA Library Prep Kit for MGI [40] | Prepares DNA fragments for high-throughput sequencing by adding platform-specific adapters. | A key reagent for mNGS library construction on BGISEQ platforms. |
| MolYsis Basic5 [40] | Selectively depletes host (human) DNA from samples prior to extraction. | Critical for improving mNGS sensitivity in samples with high host background, like BALF. |
| Respiratory Pathogen Probe Panels [41] | Biotinylated RNA probes that enrich for targeted pathogen sequences in a library. | Used post-library preparation to significantly increase sensitivity for a pre-defined set of respiratory pathogens. |
| Magnetic Pathogen DNA/RNA Kit [40] | Extracts both DNA and RNA simultaneously. | Necessary for comprehensive mNGS that aims to detect all pathogen types, including RNA viruses. |
Detailed Experimental Protocols
Standard Sanger Sequencing Protocol for Bacterial Identification
This protocol is adapted for identifying a bacterial isolate from a pure culture, typically targeting the 16S rRNA gene [36].
DNA Template Preparation:
- Extract genomic DNA from a pure bacterial colony using a silica column-based kit.
- Quantify DNA using a spectrophotometer (e.g., Nanodrop) or fluorometer. For plasmid templates, a concentration of ~50 ng/μL is recommended; for purified PCR products, ~1-6 ng/μL is sufficient depending on amplicon size [43].
PCR Amplification:
- Set up a PCR reaction with primers targeting the 16S rRNA gene (e.g., 27F and 1492R). Use a high-fidelity PCR master mix.
- Thermal Cycling: Initial denaturation (95°C for 2 min); 35 cycles of: Denaturation (95°C for 30s), Annealing (55°C for 30s), Extension (72°C for 90s); Final extension (72°C for 5 min) [36].
PCR Clean-up:
- Purify the PCR product to remove primers, enzymes, and unincorporated nucleotides. Use a spin column-based purification kit or an enzymatic clean-up method (e.g., ExoSAP-IT) [36].
Cycle Sequencing Reaction:
- Set up the Sanger sequencing reaction using the purified PCR product as template. The reaction includes:
- Template DNA (~1-10 ng)
- Sequencing primer (5 μM, 5 μL)
- BigDye Terminator ready reaction mix
- Sequencing buffer
- Thermal Cycling: Rapid thermal ramp to 96°C; 25 cycles of: Denaturation (96°C for 10s), Annealing (50°C for 5s), Extension (60°C for 4 min) [36].
- Set up the Sanger sequencing reaction using the purified PCR product as template. The reaction includes:
Cycle Sequencing Clean-up:
- Remove unincorporated dye terminators using a spin column, ethanol/EDTA precipitation, or a magnetic bead-based method [36].
Capillary Electrophoresis:
- Load the purified sequencing reaction onto a genetic analyzer (e.g., SeqStudio). The instrument will separate the fragments by size and detect the fluorescent dye as each fragment passes a laser.
Data Analysis:
- The instrument software generates a chromatogram (.ab1 file). Analyze the sequence quality and perform a BLAST search against a public database (e.g., NCBI BLAST) for species identification [36].
Standard mNGS Wet-Lab Protocol for BALF Samples
This protocol outlines the core steps for processing a BALF sample for DNA-based mNGS [13] [40] [38].
Sample Collection and Inactivation:
- Collect BALF aseptically and transport on ice.
- Inactivate: Heat sample at 80°C for 10 minutes to ensure biosafety [38].
Host DNA Depletion (Optional but Recommended):
- Treat the sample with a host depletion kit (e.g., MolYsis Basic5) according to the manufacturer's instructions to increase the relative proportion of microbial nucleic acids [40].
Total Nucleic Acid Extraction:
Library Preparation:
- Fragment DNA via enzymatic or mechanical shearing to a desired size (e.g., 200-300 bp).
- Perform end-repair and ligate sequencing adapters to the fragmented DNA.
- Amplify the library with a limited number of PCR cycles to add index sequences for sample multiplexing [40].
- Quality Control: Assess library concentration using a fluorometer (Qubit) and fragment size distribution using a bioanalyzer (Agilent 2100) [40].
High-Throughput Sequencing:
- Pool multiple, uniquely indexed libraries together.
- Sequence on a high-throughput platform (e.g., Illumina NovaSeq, BGISEQ-500, etc.). A common depth is 10-20 million reads per library for BALF samples [40].
The subsequent bioinformatic analysis, while critical, is a separate complex process involving quality filtering, host sequence subtraction, microbial classification, and interpretation.
For researchers investigating respiratory co-infections, selecting and processing the appropriate specimen type is a critical first step that directly impacts diagnostic accuracy. Traditional Sanger sequencing, while reliable for confirming single pathogens, faces significant limitations in complex co-infction scenarios where multiple organisms may be present. This technical support center provides targeted strategies for optimizing bronchoalveolar lavage fluid (BALF), sputum, and blood specimen processing to overcome these challenges, with a specific focus on methodologies that complement Sanger sequencing's constraints in polymicrobial detection.
Comparative Performance of Respiratory Specimens
Understanding the relative strengths and weaknesses of different specimen types enables researchers to select the most appropriate sample for their experimental goals, particularly when investigating co-infections that Sanger sequencing might miss.
Table 1: Comparative Analysis of Respiratory Specimen Types for Pathogen Detection
| Specimen Type | Detection Sensitivity | Key Advantages | Primary Limitations | Optimal Use Cases |
|---|---|---|---|---|
| BALF | 84.7% sensitivity (mTGS) [44] | Direct sampling from infection site; superior for atypical pathogens | Invasive collection procedure; requires specialized equipment | Gold standard for lower respiratory infections; immunocompromised hosts |
| Sputum | 39.4% sensitivity (culture) [45] | Non-invasive collection; widely accessible | Contamination risk from upper airways; lower pathogen yield | Routine community-acquired pneumonia; follow-up testing |
| Blood | Not quantified in results | Systemic infection detection; sterile sample | Low sensitivity for localized respiratory infections | Sepsis workup; disseminated infections |
Detailed Methodologies for Specimen Processing
Bronchoalveolar Lavage Fluid (BALF) Processing Protocol
Optimized BALF processing significantly enhances pathogen detection rates. The following protocol, validated in recent studies, demonstrates substantial improvement over conventional methods:
Sample Collection: Perform bronchoalveolar lavage via fiberoptic bronchoscopy wedged in the affected bronchopulmonary segment. Instill 100-150 mL sterile saline (5-7 aliquots of 20 mL) with a minimum return of 30% total volume [46]. For pathogen identification, collect 10-20 mL of BALF.
Sample Processing for Molecular Studies:
- Pre-process samples to achieve total cell concentration ≥1×10⁶ cells/mL for host removal [47]
- Extract nucleic acids using magnetic bead-based methods [45] or commercial kits (QIAamp DNA Mini Kit) [46]
- For metagenomic studies, omit host DNA depletion step [44]
- Utilize 800 MB sequencing depth for optimal detection sensitivity [44]
Quality Control Metrics: The optimized meta-genomic Third Generation Sequencing (mTGS) protocol achieves a tenfold increase in sensitivity for detecting Bacillus subtilis, Mycobacterium tuberculosis, Mycobacterium avium, Cryptococcus neoformans, and Human papillomavirus compared to pre-optimized methods [44].
Sputum Specimen Processing Protocol
Proper sputum processing is essential for reliable results:
Sample Qualification: Assess specimen quality via Gram staining. Acceptable samples show <10 squamous epithelial cells and >25 white blood cells per low-power field (10× magnification) or white blood cell to squamous epithelial cell ratio >2.5 [45].
Culture Processing:
- Inoculate sputum specimens onto differential media (blood agar, chocolate agar, MacConkey agar)
- Incubate at 35-37°C for 24-48 hours
- Identify pathogens using colony characteristics, biochemical tests, and mass spectrometry techniques [45]
Molecular Processing:
- Digest samples with dithiothreitol (sputolysin) to homogenize viscosity
- Concentrate via centrifugation
- Extract DNA using standardized kits
- Perform PCR amplification with appropriate controls
Blood Specimen Processing Protocol
While not detailed in the available search results, standard blood processing typically involves:
- Aseptic collection in appropriate blood culture bottles
- Incubation in automated continuous-monitoring blood culture systems
- Subculture of positive bottles to solid media
- Gram staining and preliminary identification of positive cultures
Technical Troubleshooting Guides
Common Sanger Sequencing Issues and Solutions
Table 2: Sanger Sequencing Troubleshooting Guide for Extracted Pathogen DNA
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Failed reactions (mostly N's) | Low template concentration; poor DNA quality; contaminants | Verify concentration (100-200 ng/μL); check 260/280 ratio (~1.8); clean up DNA [3] |
| High background noise | Low signal intensity; multiple priming sites; residual PCR primers | Increase template concentration; redesign primer for single annealing site; purify PCR products [22] [3] |
| Sequence stops abruptly | Secondary structures; GC-rich regions; polymerase blockage | Use specialized protocols for difficult templates; redesign primers past problematic regions [11] [3] |
| Double peaks (mixed sequence) | Multiple templates; colony contamination; multiple priming sites | Ensure single colony pickup; verify primer specificity; purify PCR products from single amplicon [3] |
| Dye blobs (~70 bp) | Unincorporated dye terminators; insufficient cleanup | Optimize purification; ensure proper vortexing with BigDye XTerminator kit [22] [3] |
BALF-Specific Processing Issues
Low Pathogen Yield:
Inhibitors Affecting Downstream Applications:
- Include dilution series in PCR setups
- Use inhibitor-resistant polymerase enzymes
- Implement adequate negative controls to detect suppression
Frequently Asked Questions (FAQs)
Q1: What is the evidence supporting BALF superiority over sputum for pathogen detection? A: Recent studies demonstrate BALF meta-genomic testing achieves 84.7% sensitivity compared to 39.4% for sputum culture [45] [44]. BALF-based testing significantly reduces hospital stays (P=0.0093) and decreases antibiotic usage rates (P=0.0491) [45].
Q2: How can I improve sequencing results from pathogen DNA extracted from BALF? A: Ensure DNA quality by measuring OD 260/280 ratios (target ~1.8) and OD 260/230 ratios (<0.6) [48]. Use template amounts appropriate for your sequencing platform and application, and verify absence of inhibitors like EDTA, salts, or alcohols [11] [3].
Q3: What are the key considerations when processing samples from immunocompromised patients? A: In connective tissue disease patients, BALF mNGS shows 80.6% sensitivity versus 66.1% for conventional methods [47]. Prioritize detection of opportunistic pathogens like Pneumocystis jirovecii and consider broader pathogen panels.
Q4: How does sequencing technology choice impact co-infection detection capability? A: While Sanger sequencing struggles with mixed templates, metagenomic approaches (mNGS/mTGS) simultaneously detect diverse pathogens in BALF, identifying significantly more microbes than conventional methods (314 vs. 115) [44] [47].
Q5: What quality control measures are essential for reliable sputum processing? A: Implement microscopic qualification to ensure lower respiratory origin, process samples within 1 hour of collection, and use standardized culture media with proper incubation conditions [45].
Research Reagent Solutions
Table 3: Essential Research Reagents for Respiratory Specimen Processing
| Reagent/Kits | Primary Function | Application Notes |
|---|---|---|
| DNA Extraction Kits (Magnetic bead method) [45] | Nucleic acid purification from specimens | Optimal for BALF; ensures removal of inhibitors |
| QIAamp DNA Mini Kit [46] | PCR-quality DNA extraction | Validated for BALF bacterial/fungal detection |
| BigDye Terminator kits [22] | Sanger sequencing reactions | Includes control templates for troubleshooting |
| Host Depletion Reagents [47] | Reduce human DNA in samples | Improves microbial sequencing depth in BALF |
| PCR Purification Kits | Remove primers, dNTPs | Critical for clean Sanger sequencing results [48] |
| Nucleic Acid Size Selection Kits | Fragment selection | Optimizes library preparation for sequencing [44] |
Workflow Visualization: Diagnostic Pathogen Detection
While Sanger sequencing remains valuable for confirming single pathogens, its limitations in co-infection research are effectively addressed through optimized specimen processing strategies and complementary meta-genomic approaches. BALF specimens processed with optimized mTGS protocols demonstrate superior detection capabilities for complex respiratory infections, while proper sputum qualification and processing maintain utility for routine diagnostics. By implementing these standardized methodologies, researchers can significantly enhance detection sensitivity and overcome the fundamental constraints of Sanger sequencing in polymicrobial investigations.
The accurate identification of pathogens in a clinical or research sample is a cornerstone of effective disease diagnosis and treatment. However, this process becomes significantly more complex when a sample contains multiple pathogens, a situation known as co-infection. Traditional methods like Sanger sequencing have historically struggled to resolve co-infections, as they are designed to determine the sequence of a single, dominant DNA template. When multiple organisms are present, the sequencing chromatogram can become mixed and unreadable, a problem known as "double sequencing" where two or more peaks appear at the same location [10]. This limitation can lead to misdiagnosis, incomplete treatment, and a failure to understand the true complexity of an infection.
The advent of High-Throughput Sequencing (HTS), coupled with sophisticated bioinformatics pipelines, has revolutionized this field. These technologies enable the unbiased sequencing of all genetic material in a sample, followed by computational sorting and identification of individual pathogens, even in complex mixtures. This technical support article guides researchers through the transition from Sanger sequencing to modern HTS bioinformatics pipelines for robust pathogen identification, with a special focus on overcoming the challenge of detecting co-infections.
Troubleshooting Sanger Sequencing for Co-infection Research
Sanger sequencing remains a powerful tool for validating results or sequencing single clones. However, its limitations are quickly exposed in co-infection scenarios. The following table outlines common issues that may indicate the presence of a co-infection or other complicating factors.
Table 1: Troubleshooting Sanger Sequencing Problems in Complex Samples
| Problem Identification | Possible Cause | Solution |
|---|---|---|
| Double sequence (mixed peaks) from the beginning of the trace [10] | Colony contamination (more than one clone being sequenced) or multiple priming sites on the template. | Ensure a single colony is picked. Redesign the primer to ensure only one annealing site. |
| Good quality data that suddenly becomes mixed [10] | Expression of a toxic sequence in the vector, leading to deletions/rearrangements and a mixed population. | Use a low-copy vector, grow cells at 30°C, and avoid overgrowing the culture. |
| Poor data following a mononucleotide repeat [10] | Polymerase slippage on a homopolymer stretch, causing frameshifts and a mixed signal. | Design a new primer that sits just after the repeat or sequence toward it from the reverse direction. |
| Sequence gradually dies out [10] | Too much starting template DNA, leading to over-amplification and premature termination. | Lower template concentration to the recommended range (e.g., 100-200 ng/µL for plasmid DNA). |
| Good quality data that comes to a hard stop [10] | Secondary structure (e.g., hairpins) in the template that the polymerase cannot pass through. | Use an alternate sequencing chemistry (e.g., "difficult template" protocols) or design an internal primer. |
| Noisy baseline or "dye blobs" [22] | Excess dye terminators or salts due to inefficient cleanup; can also be caused by contaminants. | Optimize the purification protocol. Ensure thorough vortexing if using magnetic bead-based cleanups. |
Transitioning to HTS Bioinformatics Pipelines
When Sanger sequencing indicates a potential co-infection or when a complex infection is suspected from the start, HTS approaches are necessary. The core workflow involves converting raw sequencing data into actionable diagnostic information through a series of computational steps. The following diagram illustrates the logical flow of a typical bioinformatics pipeline for pathogen detection.
Experimental Protocols for HTS-Based Co-infection Detection
The following are detailed methodologies for key experiments cited in co-infection research, demonstrating the application of HTS and bioinformatics.
Protocol 1: Metagenomic Next-Generation Sequencing (mNGS) for Lower Respiratory Tract Infections (LRTI) [13]
This protocol outlines a prospective, observational study comparing mNGS to standard methods.
- Sample Collection: Collect 184 bronchoalveolar lavage fluid (BALF) and 322 sputum samples from patients with symptoms of LRTI, including severe pneumonia, immunocompromised status, or fever of unknown origin.
- Standard Microbiology: Perform standard microbiological culture on all samples using blood agar, chocolate agar, and McConkey agar. Identify isolates from positive cultures using MALDI-TOF mass spectrometry.
- Nucleic Acid Extraction: Extract nucleic acids from all collected samples.
- Sanger Sequencing: Amplify target regions using pathogen-specific primers. Perform PCR band purification and outsource Sanger sequencing to a professional service. Align obtained sequences using the NCBI BLAST program.
- mNGS Library Preparation and Sequencing:
- Extract DNA from samples.
- Fragment DNA, perform end repair and adapter ligation to construct sequencing libraries.
- Quantify and quality-control libraries.
- Perform high-throughput sequencing on a platform like the VisionSeq 1000.
- Bioinformatic Analysis:
- Compare sequencing data to a curated pathogen database using automated bioinformatic software (e.g., IDseqTM-2).
- Use thresholds for reporting positives (e.g., RPM ≥ 1 for most bacteria, RPM ≥ 0.1 for specific pathogens like Mycoplasma pneumoniae).
- Data Analysis: Compare the detection performance of culture, Sanger sequencing, and mNGS, focusing on the number of pathogens identified and co-infections detected.
Protocol 2: A Metagenomic Pipeline for SARS-CoV-2 Co-infection Identification [49]
This protocol describes a method to identify co-infections with distinct SARS-CoV-2 Variants of Concern (VOCs) using an amplicon sequence variant (ASV)-like approach.
- Sample and Data Selection: Obtain sequencing data from COVID-19 cases with known SARS-CoV-2 lineages, including VOCs (Alpha, Beta, Gamma, Delta, Omicron) and non-VOCs.
- ASV-like Inference: Process sequencing data to infer multiple fragments similar to Amplicon Sequence Variants (ASVs).
- Custom Database Mapping: Map the inferred ASV-like sequences to a custom database containing SARS-CoV-2 genome sequences. ASVs with mutations specific to a VOC will map only to that variant's genome.
- VOC Assignment: For each genome in the database, count the number of mapping ASVs. Assign the sample to a VOC category based on the counts.
- Performance Assessment: Compare the pipeline's VOC class prediction to the expected, known classes to calculate accuracy.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of HTS-based pathogen detection relies on a suite of wet-lab and computational tools.
Table 2: Key Research Reagent Solutions for HTS Pathogen Identification
| Item | Function / Explanation |
|---|---|
| Bronchoalveolar Lavage Fluid (BALF) / Sputum | Clinical sample types rich in respiratory pathogens; used for direct comparison of methods [13]. |
| Nucleic Acid Extraction Kits | Essential for obtaining high-quality, contaminant-free DNA/RNA from complex clinical samples for downstream sequencing. |
| BigDye Terminator Kit | Standard chemistry for Sanger sequencing reactions; includes control DNA (pGEM) and primer for troubleshooting [22]. |
| mNGS Library Prep Kits (e.g., Vision Medicals) | Kits designed to convert extracted nucleic acids into sequencer-ready libraries through fragmentation, end-repair, and adapter ligation [13]. |
| Hi-Di Formamide | Used to prepare Sanger sequencing samples for capillary electrophoresis; helps maintain sample integrity [22]. |
| Bioinformatic Pipelines (e.g., PhytoPipe, IDseq) | Integrated computational workflows that automate quality control, read classification, assembly, and annotation [13] [50]. |
| Curated Pathogen Databases (e.g., NCBI nt, custom SARS-CoV-2) | Reference databases used by classification tools like Kraken2 to assign taxonomic labels to sequencing reads [49] [50]. |
| Simulated HTS Datasets | Artificial sequencing data with a known composition of pathogens; used as benchmarks to validate and compare the performance of bioinformatic pipelines [51]. |
Advanced Topics: Resolving Complex Co-infections with Long-Read Sequencing
For particularly challenging co-infections, such as those involving closely related parasite species or recombinant viruses, newer sequencing technologies offer enhanced resolution.
Case Study: Resolving Avian Haemosporidian Co-infections with Nanopore Sequencing [5]
- Challenge: Microscopy of blood smears from Swinhoe's pheasant suggested a co-infection, but Sanger sequencing was unable to resolve the individual parasite lineages due to mixed signals.
- Solution: Researchers employed Oxford Nanopore Technologies (ONT) sequencing, which produces long reads. This allowed for the unfragmented assembly of the complete mitochondrial genomes of the co-infecting parasites.
- Outcome: The long-read approach successfully resolved the cryptic co-infection, identifying two novel Haemoproteus lineages and one Plasmodium lineage. This overcame the ambiguities inherent to Sanger sequencing and provided a clear picture of haemosporidian diversity in an endangered bird species.
The following diagram illustrates the comparative advantage of a long-read approach in resolving co-infections that confuse traditional methods.
Frequently Asked Questions (FAQs)
Q1: My Sanger sequencing results show double peaks, suggesting a co-infction. What is the first thing I should do? The first step is to ensure this is not a technical artifact. Re-purify your PCR product to remove residual primers and confirm you picked a single bacterial colony. If the problem persists, it strongly indicates a mixed template, and you should transition to an HTS method.
Q2: What is the major advantage of mNGS over multiplex PCR panels for pathogen detection? mNGS is an "unbiased" method that does not require prior knowledge of the suspected pathogens. It can detect unexpected, novel, or difficult-to-culture pathogens, making it exceptionally powerful for diagnosing complex infections where the causative agent is unknown [13].
Q3: How do I know if my bioinformatic pipeline for pathogen detection is accurate? The best practice is to use standardized artificial or semi-artificial HTS datasets for benchmarking. These datasets contain a known quantity and diversity of pathogen sequences, allowing you to calculate critical diagnostic performance metrics for your pipeline, such as analytical sensitivity (ability to detect low levels) and analytical specificity (ability to distinguish between pathogens) [51].
Q4: Are there integrated pipelines available that can detect a wide range of plant pathogens? Yes, pipelines like PhytoPipe are specifically designed for this purpose. PhytoPipe is an integrative Snakemake-based workflow that processes RNA-seq data to detect viruses, viroids, bacteria, fungi, and oomycetes simultaneously by combining quality control, read classification, de novo assembly, and reference-based mapping [50].
Conventional microbiological tests (CMT), including culture and Sanger sequencing, have long been the cornerstone of infectious disease diagnosis. However, these methods face significant limitations in detecting co-infections and rare pathogens. Sanger sequencing, while highly accurate for confirming single pathogens, requires prior knowledge of the suspected microorganism and utilizes targeted primer amplification, making it poorly suited for identifying multiple unknown pathogens in a single test [4] [31]. Metagenomic Next-Generation Sequencing (mNGS) has emerged as a transformative, hypothesis-free tool that sequences all nucleic acids in a clinical sample, enabling the simultaneous detection of bacteria, viruses, fungi, and parasites without prior targeting [52]. This technical support document presents clinical case evidence and troubleshooting guidance for implementing mNGS to overcome the diagnostic challenges posed by complex co-infections.
Clinical Case Studies: mNGS Performance in Real-World Settings
Case Study 1: Lower Respiratory Tract Infections (LRTI) in a Large Cohort
A 2025 comparative analysis of 184 bronchoalveolar lavage fluid (BALF) and 322 sputum samples demonstrated the superior capability of mNGS in identifying co-infections compared to conventional methods.
- Methodology: Samples were fully examined by mNGS, Sanger sequencing, and standard microbiology culture. Sanger sequencing served as the reference method for comparison [4].
- Key Findings on Co-infections: In BALF samples, mNGS identified 66 samples with co-infections, outperforming both Sanger sequencing (64 samples) and conventional culture (22 samples). This highlights mNGS's particular advantage in detecting polymicrobial infections that are frequently missed by traditional cultures [4].
- Performance Metrics: The table below summarizes the detection concordance between methods for sputum and BALF samples.
Table 1: Method Comparison for Pathogen Detection in LRTI [4]
| Sample Type | Identical Results All Three Methods | mNGS & Sanger Sequencing Agreement | Cases Where mNGS Detected More | Cases Where Sanger Detected More |
|---|---|---|---|---|
| Sputa (n=322) | 52.05% (165/317) | 88.20% (284/322) | 9.00% (29/322) | 2.80% (9/322) |
| BALF (n=184) | 49.41% (85/172) | 91.30% (168/184) | 7.61% (14/184) | 2.80% (2/184) |
Case Study 2: Impact on Diagnosis and Management in Suspected LRTI
A 2025 study of 165 patients with suspected LRTI further validated the clinical impact of mNGS, using a variety of samples including BALF, blood, tissue, and pleural effusion.
- Methodology: Researchers compared traditional diagnostic methods (culture, PCR, antigen testing) with mNGS. A multidisciplinary team performed final pathogen diagnosis by integrating all data [39].
- Increased Diagnostic Yield: mNGS showed a significantly higher positive detection rate (86.7%, 143/165) compared to traditional methods (41.8%, 69/165). This led to the identification of the microbial etiology in 88.48% (146/165) of patients [39].
- Detection of Rare and Co-infecting Pathogens: The study confirmed the utility of mNGS in detecting poly-microbial infections and 29 kinds of pathogens that were missed by conventional methods, including non-tuberculous mycobacteria (NTM), Prevotella, anaerobic bacteria, Legionella gresilensis, Orientia tsugamushi, and various viruses [39].
- Therapeutic Impact: Critically, mNGS results directly led to treatment changes in 119 patients (72.13%), with 54 patients (32.73%) able to have their antibiotic regimens reduced, directly supporting antimicrobial stewardship [39].
Case Study 3: Central Nervous System (CNS) Infections
A large 7-year performance study of a clinical mNGS test for cerebrospinal fluid (CSF) underscores its broad utility beyond respiratory infections.
- Methodology: Analysis of 4,828 CSF samples tested with a clinically validated DNA/RNA mNGS assay [53].
- Diagnostic Performance: The test demonstrated 63.1% sensitivity, 99.6% specificity, and 92.9% accuracy for CNS infections. Its sensitivity was significantly higher than indirect serologic testing (28.8%) and direct detection testing from both CSF (45.9%) and non-CSF samples (15.0%) [53].
- Unique Diagnostic Value: Of the 220 infectious diagnoses made in a patient subset, 48 (21.8%) were identified by mNGS alone, justifying its routine use in hospitalized patients with suspected CNS infection of unknown cause [53].
Technical Support: mNGS Implementation Guide
Troubleshooting Guide and FAQs
FAQ: When should mNGS be prioritized over conventional methods like Sanger sequencing? Answer: mNGS is particularly valuable in several key scenarios [4] [52] [54]:
- Critically ill or immunocompromised patients with suspected infection but no definitive diagnosis.
- Suspected poly-microbial infections (co-infections), such as hospital-acquired pneumonia or aspiration pneumonia.
- Suspected rare, fastidious, or slow-growing pathogens that are difficult to culture (e.g., Mycobacterium tuberculosis, fungi, viruses).
- Cases where initial empirical antibiotic therapy has failed and targeted therapy is needed.
FAQ: What is the major interpretative challenge with mNGS results? Answer: The primary challenge is differentiating causative pathogens from colonizing microbes or environmental contaminants [54]. A study on pulmonary infections found that upon clinical evaluation, 47.1% (65/138) of microbial strains initially flagged as potential pathogens by mNGS were reclassified as colonizers [54]. This underscores that mNGS results must always be interpreted in the clinical context of the patient.
FAQ: How can we ensure the quality of mNGS results? Answer: Rigorous quality control is essential. Key steps include [39] [54]:
- Using sterile techniques for sample collection and processing.
- Including negative controls (e.g., sterile water) in each sequencing batch to identify reagent or laboratory contamination.
- Setting bioinformatic thresholds for pathogen identification (e.g., reads per million (RPM) significantly higher than the negative control) [54].
- Utilizing a multidisciplinary team (infectious disease specialists, microbiologists) for final adjudication of results.
Essential Research Reagent Solutions
The table below lists key reagents and materials used in a typical BALF mNGS workflow for pulmonary infection diagnosis, based on the cited studies.
Table 2: Key Research Reagent Solutions for BALF mNGS Workflow [4] [54]
| Reagent / Material | Function in mNGS Workflow |
|---|---|
| Dithiothreitol (DTT) | Mucolytic agent used to homogenize viscous BALF samples prior to nucleic acid extraction [54]. |
| Zirconia Beads & Lysis Buffer | Used in mechanical disruption of microbial cells (bacteria, fungi) to release nucleic acids [54]. |
| TIANamp Micro DNA Kit | Facilitates nucleic acid extraction and purification from the processed sample [54]. |
| KAPA HyperPlus Kit | Used for the preparation of DNA sequencing libraries from the extracted nucleic acids [54]. |
| Respiratory Pathogen Multipplex Detection Kit (Vision Medicals) | A commercial kit system used for integrated mNGS testing, from extraction to analysis [4]. |
| Illumina NextSeq 550Dx / VisionSeq 1000 | Examples of high-throughput sequencing platforms used for clinical mNGS testing [4] [54]. |
Workflow and Decision Pathway Diagrams
The following diagram illustrates the procedural workflow for processing a BALF sample with mNGS and integrating the results for clinical diagnosis, as described in the case studies.
Diagram 1: BALF mNGS Workflow and Integration
This diagnostic approach directly addresses the limitation of Sanger sequencing in co-infections by replacing targeted amplification with comprehensive, unbiased sequencing, followed by sophisticated bioinformatic analysis and crucial clinical interpretation.
Navigating Technical Pitfalls: Optimization Strategies for Reliable mNGS Results
In infectious disease research, particularly in studies of polyclonal infections, the presence of host DNA creates a significant technical challenge for Sanger sequencing. This host DNA background can obscure pathogen signals, leading to failed reactions, ambiguous base calls, and ultimately, inaccurate genotyping of drug-resistant pathogens [55]. The limitation is especially pronounced in high-transmission settings where mixed infections are prevalent, often exceeding 50% of sampled isolates [55]. This technical support center provides targeted troubleshooting guides and FAQs to help researchers overcome these critical limitations, enabling more precise detection and quantification of pathogen variants within complex host-pathogen samples.
FAQs and Troubleshooting Guides
How does host DNA background negatively affect Sanger sequencing of pathogens?
Excessive host DNA in a sample compromises Sanger sequencing in several key ways:
- Reduced Signal Intensity: Host DNA acts as a diluent, reducing the effective concentration of the target pathogen template. This leads to poor signal intensity during capillary electrophoresis, resulting in noisy, low-quality chromatograms that are difficult to interpret [3] [12].
- Competitive Inhibition: During the sequencing reaction, primers may bind non-specifically to host DNA instead of the target pathogen sequence. This competition for reagents (polymerase, nucleotides, labeled terminators) can cause premature reaction termination or complete failure, often indicated by a sequence file full of "N"s [3].
- Complex Mixed Chromatograms: When sequencing primers do bind to host DNA, the resulting signal is a mixture of host and pathogen sequences. This creates complex, unreadable chromatograms with overlapping peaks (double peaks) at a single position, making it impossible to call the pathogen sequence accurately [3] [55].
What are the primary enrichment strategies to mitigate host DNA interference?
A two-pronged strategy, combining wet-lab enrichment techniques with computational deconvolution, is most effective for overcoming host DNA background.
Experimental Enrichment Techniques:
- Target-Specific PCR Amplification: The most common and effective method. Using primers highly specific to the pathogen's genes of interest (e.g., drug resistance genes like Pfdhps or Pfdhfr in malaria) ensures that only the pathogen DNA is amplified millions of times before sequencing, effectively drowning out the host DNA background [55] [13].
- Optimized Nucleic Acid Extraction: Employing extraction protocols or kits designed to preferentially lyse microbial cells or enrich for pathogen nucleic acids can reduce the host DNA load at the initial sample processing stage.
- PCR Condition Optimization: Meticulously optimizing PCR conditions—including annealing temperature, extension time, and primer concentrations—is critical for ensuring efficient and specific amplification of the intended pathogen target, minimizing non-specific host DNA amplification [24].
Computational Solution:
- Chromatogram Deconvolution: For samples that still produce mixed chromatograms due to polyclonal infections or residual host amplification, specialized computational tools can deconvolute the trace files. These tools quantify the proportion of different alleles at each codon position, transforming an ambiguous mixed signal into quantitative data on resistant and sensitive pathogen variants [55].
My sequencing reaction failed entirely (mostly N's in the sequence). Could host DNA be the cause?
Yes. A failed reaction, characterized by a messy trace with no discernible peaks or a .seq file reading "NNNNN," is a classic symptom of several issues, including excessive host DNA. To troubleshoot, systematically investigate the following causes [3]:
- Primary Cause: Low effective template concentration due to host DNA dilution.
- Other Potential Causes:
- Poor Quality Pathogen DNA: Contaminants like salts or phenol can inhibit the sequencing polymerase.
- Too Much Total DNA: Excessive template, even if it's host DNA, can itself kill a sequencing reaction.
- Bad Primer: The primer may be degraded, poorly designed, or have an incorrect sequence.
- Instrument Failure: A blocked capillary on the sequencer, though rare, can cause failure.
Table: Troubleshooting Failed Sequencing Reactions
| Symptom | Possible Cause Related to Host DNA | Other Causes | Solution |
|---|---|---|---|
| Failed reaction, sequence contains mostly N's [3] | Low effective concentration of pathogen template due to dilution by host DNA. | Poor DNA quality; bad primer; instrument failure [3]. | Pre-enrich pathogen DNA via specific PCR; accurately quantify pathogen DNA post-enrichment. |
| Low signal intensity, noisy baseline [3] [22] | Weak signal from pathogen DNA is overwhelmed by baseline noise. | Multiple priming sites; poor purification of PCR product [22]. | Increase target-specific amplification cycles; ensure complete removal of PCR primers before sequencing. |
| Double peaks from the start of the trace [3] | Multiple templates (host and pathogen) are being sequenced simultaneously. | Colony contamination; more than one primer in the reaction [3]. | Use pathogen-specific primers; ensure a single clone is sequenced; provide separate tubes for forward/reverse primers. |
How can I optimize my PCR to specifically enrich for pathogen targets?
Optimizing the PCR prior to sequencing is the most critical step for successful pathogen sequencing from complex samples.
- Primer Design: Design primers to be highly specific to the pathogen gene of interest. Verify their specificity by performing a BLAST search against the host genome to avoid cross-reactivity [24].
- Annealing Temperature Optimization: Perform a temperature gradient PCR to determine the optimal annealing temperature that maximizes yield of the specific pathogen amplicon and minimizes non-specific amplification and primer-dimer formation [24].
- Use of High-Fidelity Polymerases: Employ high-fidelity DNA polymerases with proofreading capabilities. These enzymes minimize errors during amplification, ensuring the sequence data accurately represents the pathogen's genome and is not an artifact of PCR mis-incorporation [24].
- Cleanup: Always purify the PCR product before sequencing to remove excess salts, dNTPs, and, most importantly, the PCR primers themselves. Leftover primers can act as random primers during sequencing, generating high background noise [3] [22].
Are there computational methods to salvage data from mixed host-pathogen samples?
Yes, computational deconvolution is a powerful post-sequencing approach. A 2024 study on malaria demonstrated a method where Sanger chromatograms from mixed infections are deconvoluted at the single amino acid codon level [55].
- Method: This approach does not attempt to resolve the entire chromatogram into two pure sequences. Instead, it independently quantifies the proportion of each nucleotide (and thus each amino acid) at every codon position in the target gene.
- Output: The result is a quantitative percentage for each resistant and sensitive allele present in the mixed infection, providing much richer data for surveillance than a simple "resistant" or "sensitive" binary call [55].
- Application: This cost-effective method is ideal for population-based surveys to characterize the mean fraction of drug-resistant parasites within an individual and across communities, offering an earlier signal of emerging resistance [55].
Experimental Protocols for Key Scenarios
Protocol 1: Targeted Amplification and Sequencing of a Pathogen Drug-Resistance Gene from a Clinical Sample
This protocol is adapted from methodologies used for sequencing Plasmodium falciparum genes from blood samples, which contain high levels of human DNA [55] [13].
1. Sample and Nucleic Acid Extraction:
- Extract total nucleic acid from the clinical sample (e.g., blood, sputum, tissue) using a standard commercial kit.
- Quantify the DNA using a fluorescence-based method (e.g., Qubit) for accuracy, as spectrophotometers can be misled by host DNA contamination.
2. Target-Specific PCR Enrichment:
- Reaction Setup:
- Template DNA: 1-10 µL of extracted DNA (volume depends on concentration).
- Pathogen-Specific Primers: 0.5 µM each [13].
- High-Fidelity PCR Master Mix: 1X final concentration.
- Nuclease-free water to a final volume of 50 µL.
- Cycling Conditions:
- Initial Denaturation: 95°C for 5 minutes.
- 35 Cycles of:
- Denaturation: 95°C for 30 seconds.
- Annealing: Optimize temperature for 30 seconds (see troubleshooting guide above).
- Extension: 72°C for 1 minute per kb.
- Final Extension: 72°C for 7 minutes.
- Hold at 4°C.
3. PCR Product Purification:
- Verify a single amplicon of the correct size by agarose gel electrophoresis.
- Purify the PCR product using a PCR purification kit or by excising the correct band from the gel to remove primers, enzymes, and non-specific products [13].
4. Sanger Sequencing Reaction:
- Use the purified PCR product as the template for the cycle sequencing reaction with BigDye Terminator chemistry or equivalent.
- Template Amount: Use 5-20 ng of a 500-1000 bp PCR product [22].
- Primer: Use the same pathogen-specific primer (3.2 pmol per reaction) for sequencing.
5. Sequencing Product Cleanup and Analysis:
- Purify the sequencing reaction to remove unincorporated dye terminators, which can cause dye blobs [22] [12]. Spin columns or the BigDye XTerminator Kit are effective.
- Run the sample on a capillary electrophoresis sequencer.
- Analyze the chromatogram visually and using quality scores. For mixed infections, apply computational deconvolution software [55].
Protocol 2: Workflow for Resolving Polyclonal Infections via Computational Deconvolution
This protocol outlines the steps for the computational analysis of mixed chromatograms, as described in a 2024 study [55].
- Generate Standard Sanger Sequencing Data: Sequence the enriched PCR product (from Protocol 1) from both forward and reverse directions using standard procedures.
- Obtain Chromatogram Files: Download the
.ab1chromatogram files from the sequencer. Do not rely solely on the text-based.seqfiles, as they lose the mixed base information [24] [12]. - Run Deconvolution Software: Input the chromatogram files into a deconvolution tool designed for this purpose (e.g., the codon-based method described by [55]). The software will analyze the trace data at each position of the target codons.
- Interpret Quantitative Output: The software outputs the relative percentages of each amino acid (e.g., sensitive vs. resistant) at every codon position in the target gene.
- Integrate Data for Surveillance: Use the mean fraction of resistance alleles from multiple individuals to calculate community-level resistance prevalence and heterogeneity.
The following workflow diagram illustrates the integrated experimental and computational process for overcoming host DNA background in pathogen sequencing.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Reagents for Pathogen-Targeted Sequencing
| Item | Function in the Workflow |
|---|---|
| High-Fidelity DNA Polymerase | Amplifies the target pathogen gene with minimal errors, ensuring sequence accuracy and reducing artifacts during PCR enrichment [24]. |
| Pathogen-Specific Primers | Designed to bind exclusively to the pathogen's genome (e.g., drug resistance genes), enabling selective amplification over host DNA [55] [13]. |
| PCR Purification Kit | Removes excess primers, dNTPs, and enzymes from the post-amplification product, preventing them from interfering with the sequencing reaction [3] [22]. |
| BigDye Terminator Kit | The core chemistry for Sanger sequencing, containing fluorescently labeled ddNTPs that terminate DNA synthesis and generate the signal for base calling [22]. |
| BigDye XTerminator Kit | A popular purification method for sequencing reactions that effectively removes unincorporated dye terminators, preventing "dye blob" artifacts in the chromatogram [22]. |
| Computational Deconvolution Software | A specialized algorithm or tool that quantifies the proportion of different alleles in a mixed Sanger chromatogram, converting ambiguous traces into quantitative data [55]. |
Data Presentation: Quantitative Comparisons
Table: Comparison of Sequencing Outcomes With and Without Enrichment
| Metric | Without Pathogen Enrichment | With Pathogen Enrichment & Deconvolution |
|---|---|---|
| Effective Template | Low (diluted by host DNA) [3] | High (concentrated pathogen target) |
| Signal Intensity | Low (< 100 RFU), noisy baseline [12] | High (> 1000 RFU), clean baseline [12] |
| Chromatogram Quality | Mixed peaks (host & pathogen), high background [3] [55] | Clean, single peaks; possible mixed peaks from polyclonal pathogens only [55] |
| Data Output | Binary call ("failed" or "mixed") | Quantitative (% of each allele per codon) [55] |
| Usefulness for Surveillance | Limited, can overestimate resistance by calling mixed as resistant [55] | High, provides mean fraction of resistance alleles in a population [55] |
In the specific context of co-infections research, the limitations of Sanger sequencing are particularly pronounced. This technology struggles to resolve mixed pathogen populations within a single host because it produces a single, consensus sequence from a polymerase chain reaction (PCR) product, making it hypothesis-dependent and poorly suited for identifying rare, novel, or multiple unexpected pathogens [56]. Overcoming these limitations often necessitates a shift to more sensitive next-generation sequencing (NGS) methods. However, this transition introduces a heightened risk of specimen-to-specimen cross-contamination during the more complex library preparation process, which can lead to the false detection of minority variants and compromise the integrity of the research [57]. Therefore, a rigorous, end-to-end contamination control strategy is not merely a best practice but a fundamental requirement for generating reliable genomic data in co-infections studies. This guide outlines a systematic approach to mitigating contamination from the initial sample collection through the final library preparation for sequencing.
Understanding the Limitations: Sanger Sequencing in Co-infections Research
Sanger sequencing, while the gold standard for confirming single targets, has inherent characteristics that make it suboptimal for researching co-infections. The primary challenge is its inability to deconvolute signals from multiple pathogens in a single sample.
- Hypothesis-Dependent and Low Sensitivity for Mixed Infections: Sanger sequencing requires prior sequence knowledge for primer design and is ineffective at detecting unknown pathogens. When multiple organisms are present, the sequencing chromatogram often becomes mixed or unreadable, showing two or more peaks at a single base position, which the software cannot resolve [56] [10]. This results in a failed experiment or misidentification of the dominant pathogen while missing secondary ones.
- Contamination Leading to Misinterpretation: In a Sanger workflow, cross-contamination of samples can lead to "double sequence," where the trace begins clearly but becomes mixed, indicating the presence of more than one template DNA [10]. For co-infections researchers, this is a critical confounder because it becomes impossible to distinguish a true co-infection from an artifact of laboratory contamination.
Table: Key Limitations of Sanger Sequencing in Co-infections Context
| Limitation | Impact on Co-infections Research | Typical Chromatogram Indicator |
|---|---|---|
| Hypothesis-dependent [56] | Cannot detect novel, rare, or unexpected pathogens in a mixed infection. | N/A |
| Mixed template resolution [10] | Fails to produce a clear sequence when multiple pathogens are present, leading to uninterpretable data. | Double or multiple peaks from the beginning or after a specific point. |
| Low sensitivity after antibiotic use [56] | May fail to identify pathogens that are present but not actively culturable. | Failed reaction or weak signal. |
Best Practices from Sample Collection to Library Preparation
Sample Collection and Nucleic Acid Extraction
The foundation of reliable sequencing data is laid at the very first step: sample collection and processing. Proper practices here prevent the introduction of contaminants that can skew results.
- Adherence to Specimen Requirements: Always use validated sample types for the intended test. Ensure specimen containers are labeled with at least two patient identifiers (e.g., name and date of birth) and the collection date to ensure traceability [58].
- Preventing Nucleic Acid Contamination: During extraction, use dedicated, sterile workspace and equipment. For DNA extraction from tissues or cells, methods like protease K digestion followed by phenol-chloroform extraction are effective but require care to avoid cross-over between samples [59]. The quality of the extracted nucleic acids is critical; assess purity using spectrophotometry (OD260/280 ratio of ~1.8-2.0 is ideal) and integrity via gel electrophoresis [59] [60].
Library Preparation for NGS: A Contamination-Controlled Workflow
Transitioning to NGS library preparation requires meticulous technique to manage the high risk of cross-contamination, especially in amplicon-based methods. The following workflow diagram outlines key control points.
- Physical Separation of Pre- and Post-PCR Areas: The most critical control is the physical separation of reagent and sample preparation areas (Pre-PCR) from areas where amplified DNA products are handled (Post-PCR). This prevents amplicon carryover, a major source of contamination [57]. Dedicated equipment, lab coats, and consumables should be used for each area.
- Incorporation of a Negative System Control (NSC): In every library preparation run, include a well containing a non-target nucleic acid control (e.g., MS2 bacteriophage amplicons) [57]. This NSC is processed alongside your samples. Any target sequence detected in the NSC indicates cross-contamination during the liquid handling process. The read depth from the NSC can be used to establish a statistical cut-off for filtering out contamination reads from your actual samples during bioinformatics analysis [57].
- Automated Liquid Handling: To reduce the risk of pipetting errors and specimen-to-specimen contamination, adapt the entire library preparation workflow for a liquid handling platform where possible [57]. Automation ensures consistency and minimizes human error during repetitive transfer steps.
- Rigorous Purification at Each Stage: After the initial targeted amplification PCR, it is essential to clean up the reaction to remove excess primers, salts, and enzymes before proceeding to the indexing PCR [60]. Similarly, purify the final library to remove unligated adapters and primers. This prevents non-specific amplification and ensures optimal sequencing performance. Use bead-based purification kits or gel extraction for this purpose [61].
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Research Reagent Solutions for Contamination Control
| Item | Function | Considerations for Contamination Control |
|---|---|---|
| Dedicated Pre-PCR Reagents | For sample setup and first-round PCR. | Aliquoted into small, single-use volumes to prevent contamination of stock reagents. |
| Nucleic Acid Purification Kits | To clean up PCR products and remove enzymes, salts, and primers. | Critical after initial amplification to prevent carryover into the indexing PCR [60]. |
| Indexed Adapters (Barcodes) | Unique oligonucleotide sequences ligated to fragments for sample multiplexing. | Allows pooling of multiple samples, reducing run-to-run variability and tracking cross-talk [61]. |
| Negative System Control | Non-target DNA/RNA used to monitor cross-contamination. | Must be included in every run to quantify and filter out contamination bioinformatically [57]. |
| UV Decontamination System | For decontaminating work surfaces and equipment. | Used in Pre-PCR areas to degrade any contaminating DNA. |
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: My Sanger sequencing chromatogram is clean at the start but becomes mixed and unreadable. What does this indicate? This pattern typically indicates a mixed template [10]. In co-infections research, this could be a true co-infection. However, you must first rule out colony contamination (if sequencing from a bacterial colony) or PCR contamination. To troubleshoot, re-run the PCR from the original sample with a no-template control. If the mixed signal persists in the sample but not the control, it may be a true co-infection, necessitating confirmation with a method like NGS.
Q2: My NGS run detected a very rare pathogen variant. How can I be sure it's not a contaminant? This is a critical validation step. First, check the results from your Negative System Control (NSC). If the same variant is present in the NSC, it is almost certainly a contaminant. If the NSC is clean, you can apply the contamination rate cut-off calculated from the NSC data to your samples [57]. Any variant with a read depth below this statistically derived threshold should be considered suspect and requires orthogonal confirmation (e.g., by a targeted PCR).
Q3: I am getting consistently poor-quality Sanger sequences with high background noise. What are the most common causes? The number one reason for failed or noisy Sanger sequences is suboptimal template concentration or quality [10] [60].
- Too little DNA: The signal intensity is low, leading to noisy baselines and poor base calling.
- Too much DNA: The reaction can be overwhelmed, leading to short read lengths and early termination.
- Impure DNA: Contaminants like salts, proteins, or residual primers can inhibit the sequencing polymerase.
Solution: Precisely quantify your DNA using a fluorometer or a spectrophotometer like a NanoDrop, ensuring the A260 reading is between 0.1 and 0.8 for accuracy. For plasmids, a concentration of 100-200 ng/µL is often ideal, while PCR products should be purified and typically used at 10-50 ng/µL [59] [10].
Q4: My NGS data shows uneven coverage, with very low reads at the ends of the amplicons. How can I mitigate this? This is a known issue with certain enzymatic library preparation kits, like the Nextera XT, where the transposase has difficulty binding to the very ends of DNA fragments [57]. This can create blind spots in your data. The solution is to modify the PCR primers used for targeted amplification. By adding complete Nextera transposon sequences as overhangs to your target-specific primers, you can generate amplicons that are fully compatible with the kit, resulting in even coverage across the entire genome segment [57].
Overcoming the limitations of Sanger sequencing in co-infections research requires a sophisticated approach that combines advanced NGS technologies with an unwavering commitment to contamination control. By understanding the vulnerabilities of Sanger sequencing and implementing a rigorous, end-to-end strategy—from meticulous sample collection and physical separation of workspaces to the mandatory use of negative controls and automated liquid handling—researchers can confidently generate robust and reliable genomic data. This disciplined framework is essential for accurately characterizing complex microbial communities and advancing our understanding of co-infections.
This technical support center is designed to assist researchers, scientists, and drug development professionals in establishing clinically relevant Reads Per Million (RPM) cut-offs for pathogen reporting using metagenomic next-generation sequencing (mNGS). The content is framed within a broader thesis on overcoming the limitations of Sanger sequencing, particularly in co-infections research where Sanger's single-amplicon approach struggles with complex microbial communities. While Sanger sequencing provides high accuracy for confirming single pathogens, its low throughput makes it inadequate for comprehensive co-infection detection, creating the need for robust mNGS threshold determination protocols.
Understanding RPM Thresholds: Core Concepts
Frequently Asked Questions
What is RPM and why is it used as a threshold metric in mNGS? RPM (Reads Per Million) represents the number of sequencing reads mapped to a specific pathogen per million total reads in a sample. This normalized metric allows for comparison across samples with varying sequencing depths. Unlike Sanger sequencing, which generates a single sequence read per reaction, mNGS generates millions of reads, requiring normalization to distinguish true pathogens from background noise [13].
How do RPM thresholds overcome Sanger sequencing limitations in co-infection research? Sanger sequencing is limited by its inability to detect multiple pathogens in a single reaction and its lower sensitivity for rare pathogens. In contrast, mNGS with appropriate RPM thresholds can identify multiple pathogens simultaneously in a single run. Research shows that in bronchoalveolar lavage fluid samples, mNGS identified co-infections in 66 samples compared to 64 by Sanger sequencing and only 22 by culture methods, demonstrating significant advantage in complex infection scenarios [13].
What factors influence optimal RPM threshold determination? Multiple factors affect optimal RPM thresholds: pathogen type (bacteria, viruses, fungi), sample type (BALF, sputum, blood), host DNA background, sequencing depth, and database completeness. For instance, studies show that optimal thresholds may vary significantly even within similar sample types, with SDSMRN thresholds of 5, SMRN thresholds of 0.25, and RPM ratio thresholds of 8% proving optimal for invasive pulmonary aspergillosis in BALF samples from critically ill patients [62].
Experimental Protocols for Threshold Determination
Receiver Operating Characteristic (ROC) Curve Analysis
Objective: To establish statistically validated RPM thresholds using ROC curve analysis for differentiating true positives from background noise.
Materials and Reagents:
- Known positive control samples (characterized by culture or PCR)
- Known negative control samples
- Nucleic acid extraction kits (e.g., QIAamp Viral RNA Mini Kit) [63]
- mNGS library preparation kit (e.g., Respiratory Pathogen Multiplex Detection Kit) [13]
- High-throughput sequencing platform
Methodology:
- Extract nucleic acids from well-characterized clinical samples using standardized protocols
- Process samples through mNGS workflow including library preparation and sequencing
- Calculate RPM values for known pathogens across all samples
- Generate ROC curves by plotting sensitivity against 1-specificity across a range of RPM thresholds
- Select optimal threshold that maximizes both sensitivity and specificity
- Validate thresholds against an independent sample set
Application Example: This method was successfully applied in norovirus research, where threshold detection based on variations of the P2 domain identified transmission clusters in all tested outbreaks with 80% sensitivity [63].
Comparative Method Validation Protocol
Objective: To validate mNGS thresholds against reference standards including Sanger sequencing and culture methods.
Materials and Reagents:
- Clinical samples (BALF, sputum, etc.)
- Culture media (blood agar, chocolate agar, McConkey agar) [13]
- MALDI-TOF mass spectrometry for isolate identification
- Specific primers for Sanger sequencing [13]
- PCR purification kits
Methodology:
- Split clinical samples for parallel processing by mNGS, Sanger sequencing, and culture
- For Sanger sequencing: Amplify target regions with specific primers, perform gel electrophoresis, excise and purify bands, then sequence [13]
- For mNGS: Process samples through standardized mNGS pipeline
- Compare results across methods using statistical analysis
- Establish concordance rates and adjust RPM thresholds to maximize agreement with reference standards
Application Example: One study demonstrated 91.30% concordance between mNGS and Sanger sequencing in BALF samples, providing a robust validation framework for threshold determination [13].
Troubleshooting RPM Threshold Implementation
Common Challenges and Solutions
Challenge: Low sensitivity despite optimal RPM thresholds Potential Causes and Solutions:
- Insufficient sequencing depth: Increase read depth to improve detection of low-abundance pathogens
- High host DNA background: Implement host DNA depletion strategies during sample preparation
- Database inaccuracies: Curate and update pathogen databases regularly to ensure comprehensive coverage
Challenge: Specificity issues with false positive calls Potential Causes and Solutions:
- Background contamination: Implement rigorous negative controls and establish background subtraction protocols
- Cross-mapping between related species: Adjust thresholds based on genetic similarity between pathogens
- Sample processing contaminants: Monitor and control for environmental contaminants throughout workflow
Challenge: Variable performance across pathogen types Potential Causes and Solutions:
- Differential extraction efficiency: Optimize extraction protocols for different pathogen classes (bacteria, viruses, fungi)
- Genome size variation: Consider genome-size normalized metrics (e.g., RPKM) for improved comparability
- Pathogen-specific biology: Establish separate thresholds for different pathogen categories as demonstrated in studies using thresholds of RPM ≥ 0.1 for Mycoplasma pneumoniae and RPM ≥ 1 for other microorganisms [13]
Research Reagent Solutions
Table 1: Essential Research Reagents for RPM Threshold Studies
| Reagent/Material | Function | Example Product/Specifications |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolation of pathogen nucleic acids from clinical samples | QIAamp Viral RNA Mini Kit [63] |
| mNGS Library Prep Kit | Preparation of sequencing libraries | Respiratory Pathogen Multiplex Detection Kit [13] |
| Culture Media | Reference standard for pathogen detection | Blood agar, chocolate agar, McConkey agar [13] |
| Identification System | Confirmatory pathogen identification | MALDI-TOF mass spectrometry [13] |
| PCR Purification Kits | Cleanup of amplification products | Commercially available PCR spin column kits [48] |
| Specific Primers | Target amplification for Sanger sequencing | Custom-designed primers (18-24 bases, Tm 56-60°C) [11] |
Performance Data and Threshold Specifications
Table 2: Experimentally Determined RPM Thresholds for Various Pathogens
| Pathogen Category | Representative Pathogens | Recommended RPM Threshold | Sensitivity | Specificity | Sample Type |
|---|---|---|---|---|---|
| Fungi | Aspergillus fumigatus | RPM ≥ 0.1 [13] | 21.4-57.1% [62] | 88-92% [62] | BALF |
| Fungi | Pneumocystis jirovecii | RPM ≥ 0.1 [13] | Not specified | Not specified | BALF |
| Bacteria | Mycoplasma pneumoniae | RPM ≥ 0.1 [13] | Not specified | Not specified | Respiratory samples |
| Bacteria | Most bacterial pathogens | RPM ≥ 1 [13] | Not specified | Not specified | Various |
| Viruses | Human adenovirus | RPM ≥ 0.1 [13] | Not specified | Not specified | Respiratory samples |
Table 3: Method Comparison in Clinical Samples
| Method | Co-infection Detection Rate (BALF) | Concordance with Reference Standards | Key Limitations |
|---|---|---|---|
| mNGS | 66/184 samples (35.9%) [13] | 91.30% with Sanger sequencing [13] | Requires optimized thresholds, expensive |
| Sanger Sequencing | 64/184 samples (34.8%) [13] | Reference standard for specific pathogens | Limited to targeted pathogens, poor for co-infections |
| Culture Methods | 22/184 samples (12.0%) [13] | Traditional gold standard | Time-consuming, fastidious organisms not detected |
Workflow Visualization
In infectious disease research and diagnostics, accurately distinguishing between colonization, contamination, and true infection represents a critical interpretive challenge with direct implications for patient management and therapeutic intervention. This distinction becomes particularly complex when investigating co-infections, where multiple pathogens may be present with varying clinical significance. Traditional diagnostic methods, including Sanger sequencing, face substantial limitations in these scenarios, often failing to provide the comprehensive pathogen detection needed for accurate clinical assessment.
Colonization refers to the presence of microorganisms on or in the body without causing disease in the person [64]. In contrast, infection involves the invasion of a host organism's bodily tissues by disease-causing organisms, resulting in a disease state through the interplay between pathogens and host defenses [64]. Contamination represents the accidental introduction of microorganisms during sample collection or processing that do not originate from the patient's infection site. The diagnostic challenge intensifies with co-infections, where multiple pathogens interact through complex biological mechanisms that can amplify disease severity [65].
Sanger sequencing, while considered the gold standard for specific pathogen identification, operates as a hypothesis-dependent method that requires prior knowledge of potential pathogens for primer design [56]. This fundamental limitation renders it inadequate for detecting novel, rare, or unexpected pathogens in co-infection scenarios, potentially leading to missed diagnoses and suboptimal treatment approaches [56].
Technical Support Center: Sanger Sequencing Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q: Why does my Sanger sequencing chromatogram show double peaks, suggesting mixed sequences?
A: Double peaks or mixed sequences typically indicate the presence of multiple templates in the sequencing reaction [3]. This can result from:
- Colony contamination: Accidentally picking two or more bacterial colonies during culture, leading to sequencing of different inserts [3]
- Multiple priming sites: The template may have more than one binding site for the primer being used [22]
- PCR carryover: Incomplete cleanup of PCR reactions before sequencing, leaving residual primers or salt contaminants [3]
- True genetic mixture: In co-infection contexts, this may actually represent authentic multiple pathogen presence that Sanger sequencing cannot resolve [56]
Q: What causes poor-quality sequence data with high background noise?
A: Noisy sequences with low signal-to-noise ratios typically stem from:
- Low template concentration: Insufficient DNA template (below 100ng/μL) results in poor amplification [3]
- Poor template quality: Contaminants like salts, ethanol, or proteins inhibit the sequencing reaction [3]
- Low primer binding efficiency: Primers with secondary structures, degradation, or incorrect sequence reduce reaction efficiency [3]
- Secondary structures: Hairpin formations in the template DNA can cause polymerase stuttering [22]
Q: Why does my sequencing reaction terminate early with good initial quality?
A: Abrupt sequence termination after initial good quality data often indicates:
- Secondary structures: Complementary regions forming hairpin structures that the sequencing polymerase cannot pass through [3]
- High GC content: Long stretches of G or C nucleotides can hinder polymerase progression [3]
- Template degradation: Partially degraded DNA templates may lack complete sequences [3]
- Polymerase inhibitors: Residual contaminants from sample preparation that affect enzyme processivity [22]
Troubleshooting Guide for Common Sanger Sequencing Issues
Table 1: Sanger Sequencing Troubleshooting Guide for Co-infection Research
| Problem | Possible Causes | Solutions | Prevention Strategies |
|---|---|---|---|
| Mixed sequences (double peaks) | Multiple templates, colony contamination, multiple priming sites [3] | Re-streak for single colonies, redesign primers, use clone-based sequencing [3] | Strict single-colony picking, verify primer specificity, adequate PCR cleanup |
| High background noise | Low template concentration, poor DNA quality, contaminating salts [3] | Quantify DNA precisely, repurify template, ethanol precipitation [22] | Use nanodrop for quantification, implement rigorous purification protocols |
| Sequence termination | Secondary structures, high GC regions, polymerase inhibitors [3] | Use "difficult template" protocols, sequence from opposite strand, add DMSO [3] | Design primers avoiding known problematic regions, optimize template quality |
| Dye blobs (peaks ~70bp) | Unincorporated dye terminators, contaminants in DNA [22] [3] | Optimize purification, ensure proper vortexing with BigDye XTerminator [22] | Follow manufacturer's protocols precisely, use fresh purification reagents |
| Poor peak resolution | Unknown contaminants, degraded polymer in sequencer [3] | Try alternative cleanup methods, dilute template, request instrument service [3] | Use high-quality purification kits, verify instrument performance regularly |
Sanger Sequencing Limitations in Co-infection Research
Technical Constraints in Pathogen Detection
Sanger sequencing faces significant methodological constraints when applied to co-infection research:
Hypothesis-dependent design: Unlike hypothesis-free metagenomic approaches, Sanger sequencing requires prior knowledge of potential pathogens for specific primer design, making it unsuitable for detecting novel, rare, or unexpected pathogens [56]. This limitation is particularly problematic in clinical settings where the causative agents may not be suspected based on symptomatic presentation alone.
Limited multiplexing capability: Traditional Sanger sequencing processes one DNA fragment per reaction, severely restricting its efficiency for detecting multiple pathogens simultaneously [56]. In co-infection scenarios with diverse pathogen communities, this necessitates multiple separate reactions, increasing cost, time, and sample requirements.
Insufficient sensitivity for minority populations: In mixed infections where pathogen loads vary significantly, Sanger sequencing often fails to detect minority populations that constitute less than 15-20% of the total genetic material [56]. This limited sensitivity can miss clinically relevant co-infecting pathogens that contribute to disease progression.
Inability to provide comprehensive pathogen characterization: Sanger sequencing typically targets specific genetic regions (e.g., 16S rRNA for bacteria) and cannot simultaneously provide information about antimicrobial resistance genes or virulence factors that are crucial for treatment decisions [56].
Impact on Colonization vs. Infection Differentiation
The technical limitations of Sanger sequencing directly impact the ability to differentiate colonization from true infection:
Inability to quantify pathogen load: Sanger sequencing does not provide reliable quantitative data about pathogen abundance, which is often critical for distinguishing colonization (lower load) from active infection (higher load) [64].
Limited resolution for strain typing: Many Sanger sequencing targets lack the discriminatory power to differentiate between pathogenic and commensal strains of the same species, a crucial distinction in determining clinical significance [64].
False negatives in polymicrobial infections: When multiple microorganisms are present, the dominance of one pathogen can mask the presence of others, leading to incomplete pathogen detection and potentially misinterpretation of the clinical scenario [56].
Table 2: Comparison of Pathogen Detection Methods in Co-infection Research
| Parameter | Sanger Sequencing | Metagenomic NGS | Traditional Culture |
|---|---|---|---|
| Hypothesis requirement | Hypothesis-dependent, requires prior knowledge [56] | Hypothesis-free, unbiased [56] | Hypothesis-dependent, requires growth conditions |
| Detection of novel pathogens | Limited to known pathogens with available sequence data [56] | Capable of discovering novel, rare, or unexpected pathogens [56] | Limited to cultivable organisms |
| Turn-around time | 24-48 hours for targeted pathogens [56] | 24-48 hours for comprehensive results [56] | 2-5 days for most bacteria, longer for fastidious organisms |
| Sensitivity in mixed samples | Low sensitivity for minor populations (<15-20%) [56] | High sensitivity for detecting multiple pathogens simultaneously [56] | Variable, depends on relative abundance of organisms |
| Ability to quantify | Limited quantitative capability | Semi-quantitative with appropriate controls | Quantitative with colony counts |
| Antimicrobial resistance detection | Requires separate assays for specific resistance genes | Can detect resistance genes simultaneously with pathogen identification [56] | Requires additional susceptibility testing |
Advanced Methodologies for Enhanced Co-infection Detection
Next-Generation Sequencing Solutions
Next-generation sequencing (NGS) technologies, particularly metagenomic sequencing, overcome many limitations of Sanger sequencing in co-infection research:
Untargeted pathogen detection: Metagenomic NGS sequences all nucleic acids in a sample without requiring prior knowledge of potential pathogens, enabling detection of bacteria, viruses, fungi, and parasites in a single assay [56]. This comprehensive approach is particularly valuable for diagnosing pulmonary infections where diverse pathogen types may be involved [56].
Superior sensitivity for co-infections: Clinical studies demonstrate that metagenomic sequencing identifies approximately 30% more co-infections compared to conventional methods, with improved detection of viruses and fastidious bacteria [56].
Enhanced differentiation of colonization and infection: The semi-quantitative nature of metagenomic sequencing provides data on relative pathogen abundance, helping distinguish colonizing organisms from primary pathogens based on proportional representation in the sample [56].
Rapid turnaround for clinical decision-making: Metagenomic sequencing can provide pathogen identification and antimicrobial resistance profiles within 24-48 hours, comparable to targeted Sanger sequencing but with vastly more comprehensive data [56].
Research Reagent Solutions for Co-infection Studies
Table 3: Essential Research Reagents for Advanced Co-infection Detection
| Reagent/Kit | Function | Application in Co-infection Research |
|---|---|---|
| Broad-range PCR primers | Amplify conserved regions across pathogen groups | Initial screening for bacterial, fungal, or viral presence before sequencing |
| Nucleic acid extraction kits | Isolate DNA and RNA from clinical samples | Obtain high-quality, inhibitor-free nucleic acids for downstream sequencing |
| Host depletion reagents | Remove human nucleic acids to enrich pathogen sequences | Improve sensitivity of pathogen detection in human-derived samples [56] |
| Library preparation kits | Prepare sequencing libraries for NGS platforms | Enable metagenomic sequencing from diverse sample types |
| Bioinformatics pipelines | Analyze sequencing data for pathogen identification | Differentiate true pathogens from contaminants and colonizers [56] |
Experimental Workflows for Co-infection Analysis
Integrated Diagnostic Pathway for Pulmonary Infections
Sanger Sequencing vs. NGS in Co-infection Detection
The critical challenge of differentiating colonization, contamination, and true infection in co-infection research demands technological approaches that overcome the inherent limitations of Sanger sequencing. While Sanger methodology provides specific and accurate data for targeted pathogen identification, its hypothesis-dependent nature, limited multiplexing capability, and insufficient sensitivity for detecting minority populations render it inadequate for comprehensive co-infection assessment.
Metagenomic next-generation sequencing emerges as a transformative technology that addresses these limitations through hypothesis-free, untargeted sequencing of all nucleic acids in clinical samples. This approach enables detection of novel, rare, and unexpected pathogens while providing semi-quantitative data that assists in differentiating colonizing organisms from true pathogens. The integration of metagenomic sequencing with traditional methods and clinical assessment creates a powerful diagnostic pathway for accurate characterization of complex co-infection scenarios.
For researchers and clinicians investigating co-infections, moving beyond Sanger sequencing to embrace metagenomic approaches represents an essential evolution in diagnostic capability. This transition supports more accurate differentiation between colonization and infection, ultimately leading to improved patient management and therapeutic outcomes in complex infectious disease presentations.
For researchers investigating infectious diseases, particularly complex co-infections, Sanger sequencing presents distinct limitations that challenge data accuracy and reproducibility. The technology's fundamental constraint lies in its inability to resolve multiple templates within a single reaction. When multiple pathogen strains or species are present in a clinical sample, Sanger sequencing produces mixed chromatograms characterized by overlapping peaks at variable positions, making accurate base-calling impossible [3] [5]. This technical limitation necessitates robust quality control measures and complementary methodologies to ensure data integrity in co-infection research. This guide provides troubleshooting protocols and alternative approaches to overcome these challenges and generate reliable, reproducible sequencing data.
Troubleshooting Guide: FAQ for Common Sanger Sequencing Issues
FAQ 1: How do I resolve mixed sequencing traces that suggest multiple templates or co-infections?
- Problem Identification: The sequencing trace begins with clean, high-quality peaks but becomes mixed (showing two or more peaks at the same position) partway through the read, or displays mixed peaks from the very beginning [3].
- Potential Causes:
- True biological co-infection: The sample contains multiple pathogen strains or species [5].
- Colony contamination: More than one bacterial clone was picked during sample preparation [3].
- Multiple priming sites: The sequencing primer binds to more than one location on the template DNA [22] [3].
- Incomplete PCR purification: Residual PCR primers in the sample act as unintended sequencing primers [3].
- Solutions:
- Verify with cloning: Clone the PCR product and sequence multiple clones to isolate individual sequences from the mixture.
- Redesign primers: Design new, highly specific primers that bind to a unique region of the target pathogen's genome.
- Improve purification: Use a validated PCR purification kit to remove all residual salts and primers before the sequencing reaction [3].
- Employ NGS: For complex mixtures, use next-generation sequencing (NGS) which is designed to handle multiple templates simultaneously [66] [13].
FAQ 2: What causes sequence data to terminate abruptly or show a sharp drop in signal intensity?
- Problem Identification: The sequence is of high quality but ends suddenly, or the signal intensity drops dramatically at a specific point [3].
- Potential Causes:
- Secondary structures: Hairpins or stem-loop structures in the template DNA can block polymerase progression [3].
- High GC content: Long stretches of G or C bases can cause the polymerase to dissociate [3].
- Template degradation: The DNA template is fragmented or of poor quality.
- Polymerase inhibition: Contaminants in the sample are inhibiting the sequencing enzyme.
- Solutions:
- Use special chemistry: Employ "difficult template" sequencing kits that include additives (e.g., DMSO) or alternative polymerases designed to resolve secondary structures [3].
- Sequence from both strands: Design primers to sequence through the problematic region from the reverse direction.
- Ensure template quality: Check DNA integrity using gel electrophoresis and use a reliable purification method to remove contaminants [67].
- Adjust template concentration: Overloaded template can cause premature termination; ensure concentration is within the optimal range (see Table 1) [22] [3].
FAQ 3: Why is my sequencing data noisy or have a low signal-to-noise ratio?
- Problem Identification: The chromatogram has a noisy baseline with low peak height, making the sequence difficult to read. The quality scores are low [22] [3].
- Potential Causes:
- Low template concentration or quality: Insufficient DNA or poor-quality DNA is the most common cause [3] [67].
- Poor primer binding: The primer may be degraded, have a low melting temperature, or contain a large n-1 population [3].
- Multiple priming events: The primer is binding non-specifically [22].
- Weak signal: The overall signal is too close to the instrument's detection baseline [22].
- Solutions:
- Quantify template accurately: Use a fluorometer or NanoDrop to ensure template concentration is optimal (see Table 1). Avoid spectrophotometers that are inaccurate for low concentrations [3].
- Check primer design and quality: Ensure primers are HPLC-purified, have appropriate melting temperatures, and are specific to a single site. Resynthesize if necessary [22] [67].
- Run a positive control: Use the control DNA (e.g., pGEM) and primer provided in the sequencing kit to verify the reaction chemistry and instrument performance [22].
FAQ 4: How can I address "dye blobs" that obscure data in the first 100 bases?
- Problem Identification: Large, broad peaks (often C, G, or T) appear within the first 100 base pairs, interfering with base calling in this region [22] [3].
- Potential Causes:
- Incomplete cleanup: Unincorporated dye terminators (ddNTPs) remain in the sample [22].
- Insufficient vortexing: When using magnetic bead cleanups like the BigDye XTerminator kit, incomplete mixing is a common cause [22].
- Incorrect reagent ratios: The ratio of cleanup reagents to reaction volume is critical and must be precise [22].
- Solutions:
- Optimize cleanup protocol: For spin columns, ensure sample is dispensed directly onto the purification material. For ethanol precipitation, use the recommended salt and ethanol concentrations [22].
- Use qualified vortexers: If using the BigDye XTerminator kit, use a validated vortexer capable of 2,000 RPM with a 4mm orbital diameter for the recommended time [22].
- Check reagent ratios: Precisely follow the manufacturer's guidelines for the volume of BigDye XTerminator reagent relative to your reaction volume [22].
FAQ 5: What should I do if my sequencing peaks are off-scale or too broad?
- Problem Identification: The peaks are flat-topped ("off-scale") or appear broad and poorly resolved instead of sharp and distinct [22] [3].
- Potential Causes:
- Too much template DNA: Excessive template is the primary cause of over-amplification and off-scale data [22] [3].
- Sample overloading: The amount of DNA injected into the capillary exceeds the detection limit [22].
- Unknown contaminants: Certain contaminants can cause peak broadening [3].
- Deteriorated capillary array: The instrument's capillary array may need replacement [22].
- Solutions:
- Reduce template amount: Re-do the reaction with less template DNA (see Table 1 for guidelines) [22].
- Re-inject with shorter injection time: If the sample is still on the instrument, reduce the injection time and voltage and re-inject [22].
- Try an alternative cleanup method: If contaminants are suspected, dilute the template or use a different DNA purification method [3].
- Contact core facility: If the issue is instrument-wide (affecting all samples in a run), the capillary array may need service [22].
The table below summarizes recommended template quantities for different DNA types to prevent common issues like off-scale data or early termination [22].
Table 1: Recommended Template Quantities for Sanger Sequencing
| DNA Template Type | Quantity for Standard Protocols | Quantity for BigDye XTerminator Protocol |
|---|---|---|
| PCR Product: 100-200 bp | 1–3 ng | 0.5–3 ng |
| PCR Product: 200-500 bp | 3–10 ng | 1–10 ng |
| PCR Product: 500-1000 bp | 5–20 ng | 2–20 ng |
| PCR Product: 1000-2000 bp | 10–40 ng | 5–40 ng |
| PCR Product: >2000 bp | 20–50 ng | 20–50 ng |
| Single-stranded DNA | 25–50 ng | 10–50 ng |
| Double-stranded DNA | 150–300 ng | 50–300 ng |
| Cosmid, BAC | 0.5–1.0 μg | 0.2–1.0 μg |
| Bacterial Genomic DNA | 2–3 μg | 1–3 μg |
Workflow Diagram: From Sample to Sequence
The following diagram illustrates the core Sanger sequencing workflow, highlighting key quality control checkpoints (in orange) that are essential for ensuring reproducibility and accuracy at every stage.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials critical for successful and reproducible Sanger sequencing experiments [22] [3].
Table 2: Essential Reagents and Materials for Sanger Sequencing
| Item | Function | Key Considerations |
|---|---|---|
| BigDye Terminator Kit | Provides the fluorescently-labeled ddNTPs and enzyme for the cycle sequencing reaction. | Check expiration dates. Includes control DNA (pGEM) and primer (-21 M13) for troubleshooting [22]. |
| Sequencing Primers | Binds to a specific site on the DNA template to initiate the sequencing reaction. | Must be HPLC-purified to avoid n-1 fragments. Designed for high specificity and Tm (~50-60°C) [22] [67]. |
| Hi-Di Formamide | Denatures the sequencing product and maintains single-stranded state during capillary injection. | Use fresh, high-quality formamide. Protects samples from degradation [22]. |
| BigDye XTerminator Kit | Purification kit that removes unincorporated dye terminators and salts via a magnetic bead process. | Vortexing is critical. Use a qualified vortexer to ensure complete mixing [22]. |
| PCR Purification Kit | Removes excess primers, dNTPs, and enzymes from PCR products before sequencing. | Essential for preventing false priming and noisy baselines. Follow protocol precisely [3]. |
| Control DNA (pGEM) | A well-characterized DNA template provided in sequencing kits. | Used as a positive control to determine if a failed reaction is due to template quality or reaction failure [22]. |
Advanced Topic: Overcoming Co-infection Limitations with Complementary Technologies
While Sanger sequencing is a powerful tool, its fundamental design for single-template analysis makes it unsuitable for characterizing complex co-infections. Research demonstrates that metagenomic Next-Generation Sequencing (mNGS) can detect a broader range of pathogens in co-infections compared to both culture and Sanger sequencing [13]. One study on lower respiratory tract infections found that mNGS identified more microbial species in 9% of sputa and 7.61% of bronchoalveolar lavage fluid samples compared to Sanger sequencing [13].
For resolving closely related strains within a co-infection, long-read sequencing technologies like Oxford Nanopore Technologies (ONT) are highly effective. ONT can generate uninterrupted sequences that span entire repetitive or complex regions, allowing for the unambiguous resolution of individual haplotypes in a mixed infection [5]. A study on avian haemosporidian parasites successfully used ONT to resolve cryptic co-infections by assembling complete mitochondrial genomes, thereby overcoming the ambiguities inherent to Sanger sequencing [5].
A practical strategy is to use these technologies in a complementary manner. NGS can be employed for the initial, broad detection of all pathogens present in a sample. Once identified, Sanger sequencing can then be used as a highly accurate and cost-effective method to validate specific key findings or to fill in gaps in the consensus sequence, ensuring the final data is both comprehensive and highly accurate [66] [28]. The table below summarizes this comparative approach.
Table 3: Comparing Sequencing Technologies for Co-infection Research
| Feature | Sanger Sequencing | Metagenomic NGS (mNGS) | Long-Read Sequencing (e.g., ONT) |
|---|---|---|---|
| Throughput | Low (single fragment) | Ultra-high (millions of fragments) | High (long fragments) |
| Cost per Sample | Low | High | Moderate to High |
| Ability to Resolve Co-infections | Poor - produces mixed chromatograms | Excellent - detects multiple pathogens simultaneously | Excellent - resolves strain-level variation |
| Best Use Case | Validating known suspects, confirming single strains | Unbiased discovery of all pathogens in a sample | Resolving complex strain mixtures and haplotypes |
| Reference | [3] | [13] | [5] |
Benchmarking Performance: Comparative Analysis of Diagnostic Platforms in Clinical Practice
For researchers investigating polymicrobial infections, traditional diagnostic methods often hit a wall. Conventional culture, long considered the gold standard, has a significant limitation: it can require days to yield results and fails to detect a vast number of fastidious or non-culturable pathogens [68]. Sanger sequencing, while accurate, is inherently low-throughput and requires prior knowledge of the suspected pathogen for targeted amplification, making it poorly suited for discovering unexpected or novel organisms in a mixed infection [68]. This diagnostic blind spot directly impedes research into co-infections, where complex interactions between multiple pathogens can dictate disease progression and treatment outcomes.
Metagenomic Next-Generation Sequencing (mNGS) presents a paradigm shift. This hypothesis-free, culture-independent technique sequences all nucleic acids in a clinical sample, allowing for the broad detection of bacteria, viruses, fungi, and parasites in a single assay [68]. This article provides a head-to-head comparison of these three methods, framing the discussion within the context of overcoming Sanger sequencing's limitations to advance co-infection research.
At a Glance: Comparative Diagnostic Performance
The table below summarizes the key characteristics and performance metrics of the three diagnostic techniques, providing a quick reference for researchers selecting an appropriate method.
Table 1: Diagnostic Method Comparison at a Glance
| Feature | Conventional Culture | Sanger Sequencing | Metagenomic NGS (mNGS) |
|---|---|---|---|
| Core Principle | Growth of viable microorganisms on culture media [13] | Targeted amplification and sequencing of a pre-specified gene region [13] | Untargeted, high-throughput sequencing of all nucleic acids in a sample [68] |
| Throughput | Low | Low | Very High |
| Multiplexing Capability (Co-infections) | Limited; differential growth rates can suppress some species [69] | Very Limited; requires separate assays for each target [68] | Excellent; detects all genomic material present without bias [13] [39] |
| Key Advantage | Gold standard for antimicrobial susceptibility testing (AST) | High accuracy for confirming known pathogens | Unbiased, broad-pathogen detection; novel pathogen discovery [68] |
| Key Limitation | Long turnaround time (2-5 days); cannot culture all pathogens [69] | Requires a priori hypothesis; poorly suited for polymicrobial detection [68] | High cost; complex data analysis; cannot distinguish live from dead organisms [68] |
| Ideal Use Case | AST and confirmation of common, culturable pathogens. | Orthogonal confirmation of a specific pathogen identified by other means. | Hypothesis-free diagnosis, detection of rare/novel pathogens, and comprehensive co-infection profiling [13] [53]. |
Quantitative Face-Off: Detection Rates in Clinical Samples
Recent studies directly comparing these methods on matched clinical samples provide compelling quantitative data on their performance. The following tables highlight findings from two key types of respiratory specimens.
Table 2: Detection Performance in Sputum Samples (n=322) [13]
| Metric | mNGS vs. Sanger Sequencing | mNGS vs. Conventional Culture |
|---|---|---|
| Concordance Rate | 88.20% (284/322) | Data not explicitly stated for direct comparison. |
| Cases Detecting More Microbes | mNGS: 9.00% (29/322)Sanger: 2.80% (9/322) | mNGS demonstrated a significant advantage in detecting co-infections. |
| Triple-Method Concordance | 52.05% (165/317) for mNGS, Sanger, and culture combined. |
Table 3: Detection Performance in BALF Samples (n=184) [13]
| Metric | mNGS vs. Sanger Sequencing | mNGS vs. Conventional Culture |
|---|---|---|
| Concordance Rate | 91.30% (168/184) | Data not explicitly stated for direct comparison. |
| Cases Detecting More Microbes | mNGS: 7.61% (14/184)Sanger: 2.80% (2/184) | mNGS identified co-infections in 66 samples, versus 22 by culture. |
| Triple-Method Concordance | 49.41% (85/172) for mNGS, Sanger, and culture combined. |
A separate 2025 study on Lower Respiratory Tract Infections (LRTI) further reinforced the superior detection rate of mNGS, reporting a positive rate of 86.7% (143/165) for mNGS compared to 41.8% (69/165) for traditional methods combined [39].
Experimental Protocols for Method Comparison
To ensure the validity of a head-to-head comparison study, consistent and standardized protocols for sample processing and analysis are critical.
Sample Collection and Processing
- Sample Types: The compared methods can be applied to various samples, including bronchoalveolar lavage fluid (BALF), sputum, tissue, cerebrospinal fluid (CSF), and joint fluid [13] [53] [70].
- Specimen Handling: For culture, samples are inoculated onto appropriate culture media (e.g., blood agar, chocolate agar, McConkey agar) immediately upon receipt [13]. For molecular methods (mNGS and Sanger), nucleic acid extraction is the first step. The extracted nucleic acid is then divided for parallel analysis by Sanger sequencing and mNGS [13].
- Targeted PCR Amplification: Design and use specific primers for the pathogens of interest.
- PCR Product Purification: Clean up the amplification products to remove primers and enzymes.
- Sequencing and Analysis: Perform cycle sequencing and analyze the obtained sequences using a alignment tool like NCBI BLAST for pathogen identification.
- Nucleic Acid Extraction: Isolate total DNA and/or RNA from the specimen.
- Library Preparation: Fragment the nucleic acids, perform end-repair, and ligate sequencing adapters. This may involve a reverse transcription step for RNA.
- High-Throughput Sequencing: Sequence the prepared libraries on a platform such as an Illumina or VisionSeq 1000 sequencer.
- Quality Control & Host Depletion: Filter out low-quality sequences and human host reads.
- Alignment and Classification: Map the remaining high-quality sequencing reads to comprehensive microbial genome databases.
- Result Interpretation: Use pre-established thresholds (e.g., Reads Per Million - RPM) to differentiate potential pathogens from background noise or contamination. The criteria may vary by pathogen; for example, an RPM ≥ 0.1 might be used for Mycoplasma pneumoniae, while an RPM ≥ 1 is used for other bacteria [13].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Reagents and Materials for mNGS-based Pathogen Detection
| Reagent / Material | Function in the Workflow | Key Considerations for Researchers |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolate total DNA and/or RNA from complex clinical samples. | Select kits optimized for your sample type (BALF, tissue, etc.) and capable of handling low biomass. |
| Library Prep Kits | Prepare sequencing libraries from extracted nucleic acids by fragmenting, repairing ends, and adding platform-specific adapters. | Choose between DNA-only or dual DNA/RNA kits based on your research question. |
| Pathogen Database | A curated genomic database of bacterial, viral, fungal, and parasitic genomes for classifying sequencing reads. | Database comprehensiveness and regular updates are critical for detection sensitivity and discovering divergent species. |
| Bioinformatic Pipelines (e.g., IDseq) | Software for quality control, host read subtraction, microbial alignment, and abundance reporting [13]. | Pipelines must be robust against contamination and provide clear metrics (e.g., RPM) for interpretation. |
| Negative Controls (e.g., Sterile Water) | Essential for identifying background contamination introduced during sample processing or reagents [39]. | Must be included in every sequencing run to distinguish true pathogens from contaminants. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Our mNGS results detected multiple organisms. How do we determine which are true pathogens and not contamination or colonization? A: This is a common challenge. Use a multi-faceted approach:
- Consult Controls: Always run negative controls. Organisms present in both the sample and the control are likely contaminants.
- Use Quantitative Thresholds: Employ metrics like Reads Per Million (RPM) or genome coverage. While not perfect, higher relative abundance can support clinical relevance [13].
- Correlate with Clinical Data: Integrate patient symptoms, immune status, and other lab results (e.g., white blood cell count in CSF).
- Orthogonal Confirmation: Use a targeted method like PCR or Sanger sequencing to confirm the presence of key pathogens identified by mNGS [53].
Q2: Why did our microbial culture fail to detect anything, while mNGS returned a positive result? A: Several factors can cause this discrepancy, which are often the very reasons to employ mNGS:
- Prior Antibiotic Use: This is a leading cause. Even a single dose can render pathogens non-viable and unculturable, but their DNA remains detectable by mNGS [70].
- Fastidious or Non-Culturable Pathogens: The pathogen may have specific growth requirements not met by standard culture media (e.g., viruses, atypical bacteria, fungi) [13] [39].
- Low Microbial Load: The pathogen may be present in quantities below the detection limit of culture but detectable by the sensitive mNGS assay.
- Sample Transport Conditions: Improper transport can kill fragile microbes, affecting culture but not mNGS.
Q3: What are the primary sources of contamination in an mNGS workflow, and how can we minimize them? A: Contamination can originate from:
- Laboratory Environment and Personnel: Use strict aseptic techniques and dedicated equipment.
- Molecular Biology Reagents: Kits themselves can contain microbial DNA. This is why using negative controls is non-negotiable [68].
- Sample Cross-Contamination: During collection or processing.
- Mitigation Strategies: Include routine cleaning of workspaces, using ultrapure reagents, processing samples in a laminar flow hood, and bioinformatically subtracting organisms identified in negative controls.
Q4: For a research project with budget constraints, is there a role for a combined diagnostic approach? A: Absolutely. A synergistic approach is often the most cost-effective and scientifically robust strategy.
- First Line: Use conventional culture for its low cost and ability to provide AST for common bacteria.
- Second Line: Employ mNGS in cases of culture-negative infections, suspected polymicrobial infections, or in immunocompromised hosts where the pathogen spectrum is wide [13] [39].
- Final Confirmation: Use Sanger sequencing as an orthogonal method to validate key findings from mNGS, especially for novel or unexpected pathogens.
The evidence clearly demonstrates that mNGS outperforms both Sanger sequencing and conventional culture in detecting polymicrobial and difficult-to-culture infections due to its unbiased, high-throughput nature [13] [39]. However, it does not render the older methods obsolete. Instead, mNGS serves as a powerful complement, effectively overcoming the key limitation of Sanger sequencing—its inability to efficiently handle co-infections without a prior hypothesis.
The future of microbial diagnostics in research lies in integrated, synergistic approaches. By combining the broad, discovery power of mNGS with the cost-effectiveness of culture and the confirmatory precision of Sanger sequencing, researchers can construct a complete and accurate picture of the microbial landscape in co-infections, ultimately accelerating the development of more effective therapeutic interventions.
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary limitation of Sanger sequencing in detecting co-infections? Sanger sequencing produces a consensus sequence and struggles to resolve mixed signals in a chromatogram. When two or more pathogen strains are present, their sequences can overlap at the same genomic position, resulting in overlapping peaks (double peaks) in the electropherogram. This makes it difficult to distinguish between a true co-infection and technical artifacts, often leading to ambiguous or unreadable results [71] [8].
FAQ 2: How do next-generation sequencing (NGS) methods overcome this limitation? Unlike Sanger sequencing, NGS methods, such as metagenomic NGS (mNGS) or targeted NGS (tNGS), are high-throughput, generating millions of individual sequence reads from a sample. This allows for the detection of multiple, distinct pathogen genomes within a single sample by identifying and quantifying unique sequences, thereby providing unambiguous evidence of co-infections [56] [26] [72].
FAQ 3: What is the documented sensitivity of mNGS for detecting co-infections in respiratory illnesses? In a 2025 study on Lower Respiratory Tract Infections (LRTIs), mNGS demonstrated a significant advantage in identifying co-infections. The study examined 184 bronchoalveolar lavage fluid (BALF) samples and found that mNGS identified co-infections in 66 samples, outperforming Sanger sequencing (64 samples) and conventional culture, which only identified 22 co-infected samples [13].
FAQ 4: Are there quantitative metrics comparing the sensitivity of mNGS to traditional culture? Yes. A 2025 diagnostic study compared mNGS against culture using clinical diagnosis as the gold standard. The results, summarized in the table below, show that mNGS has a significantly higher sensitivity, making it far more effective for pathogen detection [73].
Table 1: Diagnostic Performance of mNGS vs. Culture for Lower Respiratory Tract Infections
| Diagnostic Method | Sensitivity | Specificity | Area Under the Curve (AUC) |
|---|---|---|---|
| Metagenomic NGS (mNGS) | 93.3% | 54.9% | 0.744 |
| Traditional Culture | 55.6% | 71.8% | 0.636 |
Troubleshooting Guides
Issue 1: Ambiguous or Unreadable Sanger Chromatograms Suggesting Co-infection
Problem: The Sanger sequencing chromatogram shows numerous positions with overlapping peaks, making the sequence impossible to interpret confidently. It is unclear if this is due to a true co-infection, a heterozygous host genetic site, or a PCR artifact [71].
Solution:
- Verify with Re-amplification: Repeat the PCR and sequencing process from the original sample to rule out one-time PCR errors or contamination.
- Employ NGS for Confirmation: The most definitive solution is to use a targeted NGS (tNGS) or mNGS approach on the same sample. tNGS is highly effective for this, as it can detect multiple pathogens simultaneously with a high positive rate for co-infections, reported to be as high as 49.03% in some studies [72]. This will conclusively identify the presence and identity of multiple pathogens.
- Use Cloning as an Intermediate Step: If NGS is not available, a traditional method is to clone the PCR amplicons into a vector and then perform Sanger sequencing on multiple individual clones. This can separate the different sequences present in the mixture, though it is more labor-intensive and time-consuming than NGS.
Issue 2: Low Abundance Pathogen in a Co-Infection is Not Detected
Problem: Standard methods like culture or PCR fail to detect a pathogen that is present at low levels alongside a dominant pathogen.
Solution:
- Utilize mNGS: Metagenomic NGS is highly sensitive and culture-free, allowing it to detect rare, novel, and fastidious pathogens that are often missed by conventional methods. It is particularly useful for intracellular pathogens like Pneumocystis jirovecii and Mycoplasma pneumoniae [13] [73].
- Apply Targeted NGS (tNGS): tNGS uses probes to enrich for specific pathogens, which increases the sequencing depth and sensitivity for the targeted organisms. One study achieved a high pathogen detection rate of 97.08% using tNGS, making it excellent for identifying known pathogens in a co-infection, even at low levels [72].
Experimental Protocols & Data
Protocol 1: Metagenomic NGS (mNGS) for Comprehensive Pathogen Detection
This protocol is adapted from methodologies used in recent clinical studies for detecting pathogens in bronchoalveolar lavage fluid (BALF) [13] [73].
- Sample Preparation: Process sample (e.g., BALF, sputum) by mechanical disruption using bead-beating to lyse tough cell walls.
- Nucleic Acid Extraction: Extract total DNA and/or RNA using a commercial kit (e.g., TIANamp Micro DNA Kit).
- Library Preparation: Fragment the nucleic acids, perform end-repair, and add sequencing adapters. For RNA viruses, include a reverse transcription step to create cDNA.
- High-Throughput Sequencing: Sequence the library on a platform such as an Illumina NextSeq or a VisionSeq 1000.
- Bioinformatic Analysis:
- Quality Control: Remove low-quality reads and adapter sequences using tools like Fastp.
- Host Depletion: Map reads to a human reference genome (e.g., GRCh38) using Bowtie2 and remove matching reads.
- Pathogen Identification: Align the remaining non-host reads to comprehensive microbial genome databases using specialized software (e.g., IDseqTM-2, Kraken2).
Protocol 2: Differentiating Co-infection from Intra-host Variation using NGS
This protocol is critical for determining whether mixed signals represent a co-infection with distinct strains or minor genetic variations within a single dominant strain [26] [74].
- Deep Sequencing: Perform NGS on the sample to achieve high coverage (>100x) across the target genome.
- Variant Calling: Use a bioinformatic pipeline (e.g., CLC Genomics Workbench, BWA/GATK) to identify single-nucleotide variants (SNVs) and their respective allele frequencies.
- Linkage Analysis: Analyze if the minor variants (e.g., at 30% frequency) are randomly distributed or linked together on the same sequencing reads.
- Co-infection Evidence: Finding multiple SNVs with similar allele frequencies that appear together on the same reads suggests two or more full-length, distinct genomes.
- Intra-host Variation Evidence: If minor variants are isolated and not linked, they likely represent a quasispecies within a single major strain.
Table 2: Key Metrics for Differentiating Co-infection from Intra-host Variation
| Feature | Co-infection with Distinct Strains | Intra-host Variation (Quasispecies) |
|---|---|---|
| Allele Frequencies | Two or more sets of variants with stable, substantial frequencies (e.g., ~50%/50%, ~70%/30%). | A dominant strain with many low-frequency variants (<5%). |
| Variant Linkage | Multiple minor variants are physically linked on the same sequencing reads, forming a distinct haplotype. | Minor variants are not linked and appear independently on different reads. |
| Genome Coverage | Even coverage across the entire genome for all major haplotypes. | Even coverage from the dominant strain, with low-frequency variants having poor coverage. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for Co-infection Detection Studies
| Item | Function / Application | Example Product / Specification |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolates total DNA and RNA from diverse clinical samples, crucial for capturing all potential pathogens. | TIANamp Micro DNA Kit (TIANGEN Biotech) [73] |
| Library Prep Kit | Prepares sequencing libraries from extracted nucleic acids for NGS platforms. | Nextera XT Kit (Illumina); Respiratory Pathogen Multiplex Detection Kit (Vision Medicals) [13] [73] |
| Targeted Enrichment Probes/Primers | For tNGS; enriches sequences from a predefined set of pathogens, increasing sensitivity and cost-efficiency. | Custom multiplex PCR primer panels (e.g., from KingCreate Biotech) [72] |
| Metagenomic Control Material | Validates and standardizes the entire mNGS/tNGS workflow, ensuring accuracy and reproducibility. | NML Metagenomic Control Materials (MCM2α/β); WHO International Reference Reagents [8] |
| Bioinformatic Software | Analyzes NGS data by removing host sequences and identifying microbial reads. | IDseqTM-2, Fastp, Bowtie2, BWA [13] [73] [72] |
The limitations of conventional microbiological tests (CMTs), including Sanger sequencing and culture-based methods, present a significant challenge in co-infections research. These methods offer specificity but have a limited scope, require a priori knowledge of suspected pathogens, and struggle with fastidious or rare organisms that are difficult to culture [75] [7]. Metagenomic Next-Generation Sequencing (mNGS) provides a culture-independent, hypothesis-free approach that simultaneously detects a wide spectrum of pathogens—bacteria, viruses, fungi, and parasites—from a single sample, making it particularly powerful for identifying polymicrobial infections that traditional methods often miss [75] [56].
Performance Comparison: mNGS vs. Conventional Methods
Clinical studies consistently demonstrate the superior detection capabilities of mNGS in diagnosing pulmonary and other infectious diseases.
Table 1: Diagnostic Performance of mNGS vs. Conventional Methods in Recent Clinical Studies
| Study Focus | mNGS Positive Rate | Conventional Method Positive Rate | Key Findings |
|---|---|---|---|
| Pulmonary Infections [75] | 86% | 67% | mNGS detected 59 bacteria, 18 fungi, 14 viruses, and 4 special pathogens, far exceeding the 28 total pathogens found by CMTs. |
| Severe Community-Acquired Pneumonia (SCAP) [76] | 92.6% | 74.7% | mNGS-guided therapy led to a significant reduction in mortality (28.0% vs. 43.9%) and shorter ventilation time. |
| Lower Respiratory Tract Infections (LRTI) [77] | 86.7% | 41.8% | mNGS identified 29 kinds of pathogens missed by traditional methods, including non-tuberculous mycobacteria (NTM) and anaerobic bacteria. |
Table 2: Pathogen Detection Spectrum: mNGS vs. Conventional Methods
| Pathogen Category | Examples of Pathogens Detected by mNGS | Common Limitations of Conventional Methods |
|---|---|---|
| Atypical Bacteria | Mycoplasma pneumoniae, Chlamydia psittaci, Legionella species [75] [56] | Fastidious growth requirements, slow culture times, or lack of specific PCR testing. |
| Viruses | Adenoviruses, herpesviruses, human rhinoviruses, SARS-CoV-2 [75] [56] | Requires specific primer/probe design for PCR; unknown viruses evade detection. |
| Fungi | Pneumocystis jirovecii, Talaromyces marneffei, Aspergillus fumigatus [75] [56] | Difficult to culture due to specific growth needs or low fungal burden. |
| Anaerobic Bacteria | Prevotella species and other anaerobes [77] | Specialized collection and culture conditions required; often perish during transport. |
| Parasites | Spirometra erinaceieuropaei [56] | Rarely suspected and not covered by routine diagnostic panels. |
Experimental Protocol: mNGS Workflow for Pathogen Identification
The following workflow details the standard mNGS procedure used in the cited clinical studies for pathogen identification from Bronchoalveolar Lavage Fluid (BALF) and other samples.
Sample Collection and Nucleic Acid Extraction
- Sample Types: Bronchoalveolar lavage fluid (BALF) is most common; sputum, blood, and tissue biopsies are also used [76] [56] [77].
- Procedure: Collect samples using sterile techniques. For BALF, instill sterile saline into the subsegmental bronchi via bronchoscopy and retrieve the fluid [76]. Process samples promptly (e.g., within 4 hours) to minimize degradation and contamination [77].
- DNA Extraction: Use commercial kits (e.g., TIANamp Micro DNA kit) following manufacturer protocols to achieve high-quality, high-quantity DNA [76].
Library Preparation and Sequencing
- Library Prep: Construct DNA libraries using commercial kits (e.g., MGIEasy Cell-free DNA Library Preparation Kit). This involves DNA fragmentation, end repair, adapter ligation, and PCR amplification [76].
- Quality Control: Assess library quality using instruments like the Agilent 2100 Bioanalyzer and quantify DNA with Qubit fluorometry [76].
- Sequencing: Load qualified libraries onto high-throughput sequencers. Studies cited used the MGISEQ-2000 platform for 50bp single-end sequencing [76]. Other common platforms include Illumina (e.g., NovaSeq 6000) and Oxford Nanopore Technologies (e.g., GridION) [78] [79].
Bioinformatic Analysis
The bioinformatics pipeline is critical for converting raw sequencing data into actionable microbiological information.
Table 3: Key Steps in mNGS Bioinformatic Analysis
| Analysis Step | Tool/Method Example | Purpose |
|---|---|---|
| Quality Control & Pre-processing | Custom pipelines (e.g., CZ ID) | Remove low-quality reads, adapter sequences, and duplicate reads [78]. |
| Host Sequence Removal | Burrows-Wheeler Alignment (BWA) against hg19 | Filter out human reads to enrich for microbial data [76]. |
| Microbial Classification | Alignment to curated microbial databases (NCBI, SILVA, GreenGenes) | Assign reads to specific pathogens (bacteria, viruses, fungi, parasites) [7] [76]. |
| Background Subtraction | Comparison to negative control samples (Z-score calculation) | Distinguish true pathogens from environmental or reagent contamination [78]. |
Troubleshooting Common mNGS Challenges
Q: A high percentage of reads are removed during host filtering. Is my sample inadequate?
- A: Not necessarily. The percentage of host reads depends heavily on the sample type. Sterile fluids like CSF routinely have >99% of reads removed during host filtering, while stool samples have a much lower percentage. This is expected and reflects the biological reality of the sample [78].
Q: How can I distinguish true pathogens from background contamination?
- A: Always include negative control samples (e.g., sterile water) processed alongside your clinical samples. Use these to create a background model [78]. Calculate a Z-score for each detected taxon:
Z = (rPM_sample - Mean_rPM_controls) / StandardDeviation_rPM_controls[78]. A high Z-score indicates the organism is significantly more abundant in your sample than in the controls. Rely on aggregate scores that combine relative abundance and Z-score information to rank microbial matches [78].
Q: My sequencing run failed initialization due to a pH error. What should I do?
- A: For Ion PGM systems, pH errors can occur if nucleotide pH is out of range or due to a minor measurement glitch. Press "Start" to restart the measurement. If it fails again, check the pH of all reagents and the error message, then contact technical support [80].
Q: My DNA is highly degraded. Will mNGS still work?
- A: Degraded DNA can lead to sequencing failure. Always check DNA integrity via gel electrophoresis before submission. For irretrievable samples, sequencing may be attempted, but resequencing of failed samples may not be offered [79].
Essential Research Reagent Solutions
Table 4: Key Reagents and Materials for mNGS Experiments
| Reagent/Material | Function | Example Product |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolves total DNA/RNA from clinical samples, crucial for yield and purity. | TIANamp Micro DNA Kit (Tiangen Biotech) [76] |
| DNA Library Prep Kit | Fragments DNA, repairs ends, and ligates adapters for sequencing. | MGIEasy Cell-free DNA Library Preparation Kit (MGI Tech) [76] |
| External RNA Controls (ERCC) | Spike-in controls to monitor sequencing efficiency and detect bias. | ERCC Spike-In Mix (Thermo Fisher Scientific) [78] |
| Sequencing Chip & Kit | Platform-specific consumables that determine read length and output. | MGISEQ-2000 sequencing kit [76], Ion Torrent Chips [80] |
| Bioinformatic Databases | Curated genomic reference databases for accurate taxonomic classification. | NCBI RefSeq, SILVA, GreenGenes [7] [76] |
mNGS has proven to be a transformative tool in clinical microbiology, effectively overcoming the critical limitations of Sanger sequencing and culture-based methods, especially in the context of complex co-infections. By providing a rapid, unbiased, and comprehensive snapshot of the microbial landscape, it enables researchers and clinicians to identify rare, fastidious, and unexpected pathogens, thereby guiding precise antimicrobial therapy and improving patient outcomes [75] [76] [56]. As standardization improves and costs decrease, mNGS is poised to become an integral part of the diagnostic and research arsenal for infectious diseases.
For researchers and drug development professionals, accurate pathogen identification is crucial for diagnosing infections and developing effective treatments. Sanger sequencing has long been a gold standard in clinical diagnostics due to its reliability and accuracy for analyzing specific DNA regions [24]. However, a significant limitation emerges when dealing with polymicrobial infections, or co-infections. In these samples, Sanger sequencing produces uninterpretable chromatograms due to overlapping signals from multiple pathogens, limiting its diagnostic sensitivity [81] [8]. This technical support center provides troubleshooting guidance and solutions for researchers facing these challenges, with a focus on practical implementation considerations.
Comparative Performance: Sanger Sequencing vs. Next-Generation Sequencing
Quantitative Detection Rates in Clinical Samples
Recent studies directly comparing Sanger sequencing with Next-Generation Sequencing (NGS) for pathogen identification reveal notable performance differences, particularly in complex samples.
Table 1: Detection Rate Comparison Between Sanger and NGS Sequencing
| Study Focus | Sanger Positivity Rate | NGS Positivity Rate | Sample Type | Key Finding |
|---|---|---|---|---|
| Pathogen detection in culture-negative samples [81] | 59% (60/101 samples) | 72% (73/101 samples) | Tissue, joint fluid, pleural fluid | ONT detected more samples with polymicrobial presence (13 vs. 5) |
| Lower Respiratory Tract Infections (LRTI) [4] | Reference method | 88.2% concordance (284/322 sputa) | Sputum and BALF samples | mNGS offered comprehensive detection, especially for co-infections |
Analysis of Co-infection Detection Capability
The core limitation of Sanger sequencing in co-infection research is its inability to deconvolute signals from multiple microorganisms in a single sample.
Table 2: Co-infection Detection Capability
| Method | Ability to Resolve Co-infections | Underlying Reason | Example from Literature |
|---|---|---|---|
| Sanger Sequencing | Limited | Produces uninterpretable chromatograms with overlapping peaks in polymicrobial samples [81] [8] | Identified 64 co-infections in BALF samples [4] |
| Nanopore NGS (ONT) | High | Generates thousands of individual sequence reads that can be classified to specific pathogens [81] | Identified 66 co-infections in the same sample set [4] |
| Metagenomic NGS (mNGS) | High | Enables unbiased sequencing and identification of all nucleic acids in a sample [4] | Detected rare and difficult-to-culture pathogens [4] |
Troubleshooting Guides and FAQs for Sanger Sequencing
Common Technical Issues and Solutions
Q: My Sanger sequencing chromatogram shows noisy, uninterpretable data with overlapping peaks. What is the cause and solution?
- Possible Cause 1: Polymicrobial Sample. This is a fundamental limitation when your sample contains multiple bacterial species. The sequencing reaction incorporates terminators from all templates, creating mixed signals [81] [24].
- Solution: Switch to a Next-Generation Sequencing approach like 16S rRNA gene amplicon sequencing using Oxford Nanopore Technologies (ONT). NGS generates reads for individual bacteria, allowing identification of all pathogens in polymicrobial samples [81] [8].
- Possible Cause 2: Low Signal Intensity. Poor amplification can cause background noise, often due to low template concentration or poor primer binding [22] [3].
- Solution: Ensure your template DNA concentration is accurate (recommended between 100-200 ng/μL) and use high-quality primers with good binding efficiency [3].
Q: The sequencing data starts strong but terminates early. Why does this happen?
- Cause: This often indicates secondary structures (e.g., hairpins) or long stretches of mononucleotides (e.g., polyA) in the template DNA that the sequencing polymerase cannot pass through [22] [3].
- Solutions:
- Use an alternative sequencing chemistry designed for difficult templates (e.g., "difficult template" protocols) [11] [3].
- Design a new sequencing primer that sits just beyond the problematic region or sequences toward it from the reverse direction [3].
- For poly(A) regions, some researchers use a mixture of oligo dT primers with a C, A, or G as a 2-base anchor [22].
Q: My chromatogram shows double peaks from the start, suggesting a mixed sequence. What went wrong?
- Causes and Solutions:
- Multiple Templates: Ensure only a single template is present in the reaction. In cloning workflows, confirm that only one colony was picked and sequenced [3].
- Multiple Priming Sites: Verify that your sequencing primer has only one binding site on the template DNA [22] [3].
- Unpurified PCR Product: Residual PCR primers in your template can act as secondary priming sites. Always clean up PCR products before sequencing using spin columns [48] [3].
Decision Workflow for Pathogen Identification
The following diagram outlines a systematic workflow for selecting the appropriate sequencing method based on sample type and research question, particularly in the context of suspected co-infections.
Experimental Protocols for Method Validation
Protocol: Implementing ONT 16S rRNA Gene Sequencing for Co-infections
This protocol is adapted from clinical studies that successfully implemented long-read sequencing to overcome Sanger limitations [81] [8].
DNA Extraction:
- Use a bead-beating step (e.g., with Lysing Matrix E tubes) for thorough cell lysis, especially for tissue samples [8].
- For tissue samples, pre-process by emulsifying with tissue lysis buffer and proteinase K for 2 hours at 56°C before bead-beating [8].
- Validate extraction efficiency using well-characterized whole-cell reference materials if available [8].
16S rRNA Gene PCR:
Library Preparation and Sequencing (ONT):
- Prepare DNA libraries using the SQK-SLK109 protocol from Oxford Nanopore Technologies with reagents from New England Biolabs [81].
- Sequence on a GridION or MinION device with FLO-MIN104/R9.4.1 flow cells.
- Use super-accurate basecalling with the following read filtering: minimum Q-score of 10, minimum bases 200, maximum bases 500 [81].
Bioinformatic Analysis:
- Process ONT data using the EPI2ME platform's Fastq 16S workflow or an in-house pipeline using the k-mer alignment (KMA) tool.
- Map reads to a curated database built from the NCBI RefSeq and SILVA databases for accurate taxonomic assignment [81].
Protocol: Validation and Quality Control Framework
For laboratories seeking to implement NGS for clinical diagnostics, a robust validation framework is essential.
- Use Characterized Reference Materials: Employ metagenomic control materials containing genomic DNA from mixtures of clinically relevant bacteria at variable concentrations to assess PCR and sequencing efficiency and accuracy [8].
- Establish Quality Control Measures: Implement a rigorous quality control process for sequencing data, including the use of control DNA templates (e.g., pGEM) and primers to distinguish between template quality issues and sequencing reaction failures [22].
- Data Interpretation: The clinical significance of identified microorganisms should be evaluated by a senior microbiologist, considering clinical data, recent microbiological history, and response to antibiotic therapy [81].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Sequencing-Based Pathogen Identification
| Item | Function/Application | Example/Specification |
|---|---|---|
| High-Fidelity DNA Polymerase | Minimizes PCR errors during target amplification for sequencing [24] | Polymerases with proofreading capabilities |
| Metagenomic Control Materials (MCM) | Validates PCR and sequencing efficiency/accuracy using DNA from multiple known microbes [8] | MCM2α and MCM2β materials with DNA from 14 clinically relevant bacteria |
| DNA Purification Kits | Removes contaminants (salts, proteins, residual primers) that inhibit sequencing reactions [11] [48] | Commercially available PCR purification spin column kits |
| ONT Sequencing Kit | Prepares DNA libraries for long-read nanopore sequencing [81] | SQK-SLK109 kit (Oxford Nanopore Technologies) |
| Spectrophotometer | Accurately quantifies DNA concentration and checks purity via 260/280 and 260/230 ratios [11] [3] | NanoDrop instrument |
| WHO International Reference Reagents | Assesses DNA extraction efficiency and bias using whole-cell standards [8] | WHO WC-Gut RR (NIBSC 22/210) |
The choice between Sanger and NGS sequencing involves a critical trade-off between cost, turnaround time, and diagnostic completeness. While Sanger sequencing remains a cost-effective and accurate method for identifying single pathogens [24] [82], its limitations in co-infection research are profound. The implementation of NGS, particularly long-read technologies like ONT, provides a powerful solution to overcome these limitations, enabling comprehensive pathogen detection and significantly improving sensitivity for polymicrobial samples [81] [8] [4]. As NGS protocols become more standardized and cost-effective, their adoption in routine diagnostic and research workflows is poised to grow, ultimately leading to more precise diagnoses, targeted treatments, and enhanced antimicrobial stewardship.
In the diagnosis of infectious diseases, particularly in cases of polymicrobial infections, no single methodological approach provides a complete picture. Traditional Sanger sequencing, while a workhorse in clinical diagnostics, encounters significant limitations when faced with co-infections, often resulting in ambiguous or uninterpretable data due to mixed sequencing signals [8]. This technical support article outlines the inherent challenges of using Sanger sequencing for complex infections and establishes robust diagnostic algorithms that integrate complementary technologies, such as metagenomic Next-Generation Sequencing (mNGS) and long-read nanopore sequencing, to overcome these barriers. The following guide provides troubleshooting for common Sanger sequencing failures and details standardized protocols for advanced methodologies, providing researchers and drug development professionals with a framework for achieving unambiguous, species-level resolution in co-infection research.
The Limitation of Sanger Sequencing in Co-infections
Sanger sequencing is fundamentally designed to read a single, pure DNA template. In a co-infection, where multiple pathogen genomes are present in a single sample, the sequencing reaction incorporates terminators from all templates simultaneously. This generates overlapping peaks in the chromatogram after the point where the sequences of the different organisms begin to diverge, a phenomenon known as "mixed sequence" or "double sequence" [3]. The resulting electropherogram becomes messy and unreadable, preventing accurate base calling and organism identification.
Troubleshooting Guide: Sanger Sequencing FAQs
This section addresses specific issues encountered when Sanger sequencing fails due to sample complexity.
FAQ 1: My sequencing chromatogram becomes mixed and unreadable partway through the trace. What is the cause and how can I resolve it?
- Problem Identification: The sequence trace begins with high-quality, clean peaks but then becomes mixed (showing two or more peaks at a single position) and unreadable downstream [3].
- Possible Causes and Solutions:
- Colony Contamination: If two or more bacterial clones are picked accidentally, you end up sequencing more than one DNA insert. Ensure that only a single colony is selected and sequenced [3].
- Mixed PCR Product: The initial PCR amplification may have contained multiple templates. Gel-purify the PCR product of interest to ensure a single, clean band before sequencing [22].
- Toxic Sequence in DNA: In cloned samples, the inserted gene may be expressed and toxic to the E. coli host, leading to deletions or rearrangements and a mixed population. This can be mitigated by using a low-copy vector and avoiding overgrowing the cells [3].
FAQ 2: My sequencing reaction failed completely, returning a trace full of N's. What are the most common reasons?
- Problem Identification: The sequencing data contains mostly N's (undefined bases) and the trace is messy with no discernible peaks [3].
- Possible Causes and Solutions [3] [22]:
- Low Template Concentration/Degraded DNA: This is the number one reason for reaction failure. Verify DNA concentration and quality (260/280 OD ratio of ~1.8). Use a fluorometer for accurate low-concentration measurement.
- Poor Primer Binding: Ensure the primer is of high quality, not degraded, and designed for a unique site on the template.
- PCR Primers Not Removed: Residual PCR primers from the amplification step can act as unwanted sequencing primers. Always clean up PCR products before sequencing using a validated purification kit [22].
FAQ 3: The sequencing data is of good quality but terminates abruptly. Why does this happen?
- Problem Identification: The sequence is high quality but suddenly stops or the signal intensity drops dramatically [3].
- Possible Causes and Solutions:
- Secondary Structure: The DNA template may form hairpin structures (e.g., regions with high GC content) that the sequencing polymerase cannot pass through [3].
- Solution: Use an alternate sequencing chemistry (e.g., "difficult template" protocols) or design a new primer that sits directly on or just beyond the problematic region to sequence through it [3].
Establishing Integrated Diagnostic Algorithms
To overcome the limitations of Sanger sequencing, a multi-method approach is necessary. The following workflows and protocols leverage the strengths of different sequencing technologies.
Algorithm 1: Resolving Co-infections with Long-Read Sequencing
Nanopore sequencing is highly effective for resolving cryptic co-infections by generating long, continuous reads that can be assigned to individual pathogen genomes, enabling unfragmented mitogenome assembly [5].
Table 1: Key Research Reagent Solutions for Nanopore 16S rRNA Gene Sequencing
| Reagent/Material | Function in the Protocol |
|---|---|
| Lysing Matrix E Tubes | Mechanical disruption of cells for comprehensive DNA extraction from tough-to-lyse pathogens [8]. |
| AusDiagnostics MT-Prep | Automated nucleic acid extraction system for consistent and high-quality DNA yields [8]. |
| 16S rRNA PCR Primers | Amplification of the hypervariable regions of the bacterial 16S rRNA gene for taxonomic identification [8]. |
| Oxford Nanopore Ligation Kits | Prepares the amplified DNA library for loading onto the nanopore sequencer by adding sequencing adapters [8]. |
| Metagenomic Control Material (MCM2α/β) | Characterized DNA mix from multiple microbes used to validate and monitor PCR and sequencing efficiency and accuracy [8]. |
Experimental Protocol: Standardized 16S rRNA Gene Sequencing using Oxford Nanopore Technology [8]
Sample Processing:
- Emulsify tissue samples with Tissue Lysis Buffer and Proteinase K. Incubate at 56°C for 2 hours.
- Subject all samples to mechanical bead-beating using Lysing Matrix E tubes on a TissueLyser (50 oscillations/second for 2 minutes).
DNA Extraction:
- Extract nucleic acids using the AusDiagnostics MT-Prep system or equivalent, following manufacturer's instructions. Elute in a final volume of 100 µL.
Library Preparation and Sequencing:
- Amplify the near-full-length 16S rRNA gene using universal bacterial primers.
- Purify the PCR amplicons.
- Prepare the sequencing library using an ONT Ligation Sequencing Kit (e.g., SQK-LSK114).
- Load the library onto a MinION flow cell (e.g., R10.4.1) and sequence for up to 72 hours, basecalling in real-time.
Algorithm 2: Comprehensive Pathogen Detection with mNGS
For unbiased pathogen detection without prior amplification, mNGS sequences all nucleic acids in a sample, making it particularly useful for detecting rare, novel, or difficult-to-culture pathogens [13].
Table 2: Comparative Performance of Diagnostic Methods in Lower Respiratory Tract Infections [13]
| Methodology | Detection of Co-infections in BALF | Key Advantage | Best Use Case |
|---|---|---|---|
| Microbial Culture | 22 / 184 samples | Low cost; allows for antibiotic susceptibility testing. | Detection of common, culturable bacterial pathogens. |
| Sanger Sequencing | 64 / 184 samples | Gold standard for single-pathogen confirmation. | Targeted identification from a pure isolate or single-pathogen sample. |
| Metagenomic NGS (mNGS) | 66 / 184 samples | Comprehensive, culture-free detection of diverse pathogens (bacterial, viral, fungal). | Complex cases, immunocompromised hosts, and culture-negative infections. |
Experimental Protocol: Metagenomic NGS for BALF and Sputum Samples [13]
Nucleic Acid Extraction:
- Extract DNA directly from bronchoalveolar lavage fluid (BALF) or sputum samples using a validated pathogen DNA extraction kit. The extraction must be rigorous to handle a wide variety of organism types.
Library Preparation and Sequencing:
- Fragment the extracted DNA.
- Perform end-repair and adapter ligation to construct sequencing libraries.
- Amplify the library with tagged primers.
- Sequence the libraries on a high-throughput platform (e.g., VisionSeq 1000).
Bioinformatic Analysis and Criteria for Positivity:
- Compare sequencing reads against a curated pathogen database using automated software (e.g., IDseqTM-2).
- Use pre-defined thresholds for reporting positives. For example:
- Mycoplasma pneumoniae, Aspergillus fumigatus: RPM ≥ 0.1
- Most other bacteria: RPM ≥ 1 (where RPM is Reads Per Million) [13].
Navigating the challenges of co-infection diagnostics requires a deliberate and integrated approach. While Sanger sequencing remains a reliable tool for confirming single pathogens, its limitations in mixed infections are profound and well-documented. By establishing diagnostic algorithms that incorporate the power of long-read sequencing for unambiguous resolution of polymicrobial communities and the breadth of mNGS for comprehensive pathogen detection, researchers and clinical scientists can significantly advance the accuracy and efficiency of infectious disease research and patient management. The troubleshooting guides and standardized protocols provided here serve as a foundational toolkit for implementing these robust methodologies.
Conclusion
The limitations of Sanger sequencing in detecting co-infections are effectively addressed by metagenomic NGS, which provides a comprehensive, unbiased approach to pathogen identification. While Sanger sequencing maintains its value for targeted analysis of single pathogens, mNGS offers superior capability for detecting polymicrobial infections, rare pathogens, and low-abundance organisms that significantly impact patient management. The integration of mNGS into diagnostic workflows represents a paradigm shift in clinical microbiology, enabling more accurate etiological diagnosis and targeted therapeutic interventions. Future directions should focus on standardizing mNGS protocols, reducing costs, developing sophisticated bioinformatics tools for automated analysis, and validating clinical utility through large-scale prospective studies. For researchers and drug development professionals, embracing these advanced genomic technologies is crucial for advancing our understanding of complex infectious diseases and developing more effective antimicrobial strategies.
References
- 1. Polymicrobial Infections: A Comprehensive Review on ... [https://www.mdpi.com/2813-9054/70/4/39]
- 2. Polymicrobial Infections and Biofilms: Clinical Significance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9774821/]
- 3. Sanger sequencing troubleshooting guide - Research at Yale [https://research.yale.edu/sanger-sequencing-troubleshooting-guide]
- 4. Comparative Analysis of Metagenomic Next-Generation ... [https://www.mdpi.com/2076-2607/13/3/682]
- 5. Characterization of co-infections of haemosporidian ... [https://www.sciencedirect.com/science/article/pii/S2667114X25000731]
- 6. Overcoming challenges in metagenomic AMR surveillance ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1614301/full]
- 7. Understanding and overcoming the pitfalls and biases of next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6520317/]
- 8. Standardization of 16S rRNA gene sequencing using ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1517208/full]
- 9. Sanger Sequencing Implementation in Clinically Ill Patients ... [https://www.scirp.org/journal/paperinformation?paperid=118671]
- 10. Sanger DNA Sequencing: Troubleshooting [https://dnacore.mgh.harvard.edu/new-cgi-bin/site/pages/sequencing_pages/seq_troubleshooting.jsp]
- 11. Sanger sequencing FAQs [https://www.genewiz.com/public/resources/faqs/faqs-dna-sequencing]
- 12. Analyzing Sanger Sequencing Data [https://blog.genewiz.com/analyzing-sanger-sequencing-data]
- 13. PMC Search Update - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944894/]
- 14. Sanger Sequencing vs. Next-Generation Sequencing (NGS) [https://www.cd-genomics.com/resource-sanger-sequencing-vs-next-generation-sequencing.html]
- 15. NGS vs Sanger Sequencing [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-sanger.html]
- 16. Advantages and Limitations of Sanger Sequencing [https://geneticeducation.co.in/advantages-and-limitations-of-sanger-sequencing/]
- 17. Sanger Validation of High-Throughput Sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7738558/]
- 18. Confirming putative variants at ≤ 5% allele frequency ... [https://www.nature.com/articles/s41598-021-91142-1]
- 19. Sanger Sequencing - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/sanger-sequencing]
- 20. The Future of Sanger Sequencing: Technical Development ... [https://www.cd-genomics.com/blog/sanger-sequencing-technology-innovation/]
- 21. Mixed DNA Templates [https://www.nucleics.com/DNA_sequencing_support/DNA-sequencing-mixed-template.html]
- 22. Sanger Sequencing Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/capillary-electrophoresis-applications-support-center/sanger-sequencing-support/sanger-sequencing-support-troubleshooting.html]
- 23. Sanger Sequencing Analysis 102: Background Noise In ... [https://geneticeducation.co.in/background-noise-in-sanger-sequencing/]
- 24. Mastering DNA chromatogram analysis in Sanger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10643650/]
- 25. HIV-1 Drug Resistance Detected by Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10893194/]
- 26. Detection and characterization of two co-infection variant ... [https://www.nature.com/articles/srep24519]
- 27. Direct 16S/18S rRNA Gene PCR Followed by Sanger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10575125/]
- 28. Current Uses and Future Perspectives of Genomic ... [https://www.mdpi.com/2079-6382/12/11/1580]
- 29. Clinical Metagenomic Next-Generation Sequencing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6345613/]
- 30. Next-generation sequencing for hypothesis-free genomic ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-019-1448-0]
- 31. Guidelines for Sanger sequencing and molecular assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7649556/]
- 32. Troubleshooting qPCR: Common Issues and Solutions for ... [https://www.visiblegenetics.com/troubleshooting-qpcr-common-issues-and-solutions-for-accurate-pathogen-detection/]
- 33. PCR/qPCR Troubleshooting Quick Reference [https://biopathogenix.com/pcr-qpcr-troubleshooting-quick-reference/]
- 34. Genome-Wide Association Studies: hypothesis-“free” or “ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2971665/]
- 35. Hypothesis-Free? No Such Thing | The Scientist [https://www.the-scientist.com/hypothesis-free-no-such-thing-45190]
- 36. How to Conduct Sanger Sequencing [https://www.thermofisher.com/us/en/home/life-science/sequencing/sequencing-learning-center/capillary-electrophoresis-information/how-conduct-fragment-analysis0.html]
- 37. Application of metagenomic next-generation sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11604630/]
- 38. Metagenomic next-generation sequencing promotes ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1388765/full]
- 39. Diagnostic value of metagenomic next-generation ... [https://www.nature.com/articles/s41598-025-23695-4]
- 40. Comparative analysis of metagenomic and targeted next ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1451440/full]
- 41. Empirical assessment of the enrichment-based ... [https://www.nature.com/articles/s41598-024-75120-x]
- 42. Metagenomic sequencing with spiked primer enrichment for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7047537/]
- 43. Sample Preparation - GENEWIZ from Azenta Life ... [https://www.genewiz.com/public/resources/sample-submission-guidelines/sanger-sequencing-sample-submission-guidelines/sample-preparation]
- 44. Optimisation and clinical validation of a metagenomic third ... [https://www.sciencedirect.com/science/article/pii/S2352396425001963]
- 45. Comparison of bronchoalveolar lavage fluid mNGS and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174430/]
- 46. Methodological comparison of bronchoalveolar lavage ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.1168812/full]
- 47. Diagnostic value of bronchoalveolar lavage fluid ... [https://www.nature.com/articles/s41598-025-02472-3]
- 48. FAQs Sanger Sequencing [https://eurofinsgenomics.eu/en/eurofins-genomics/product-faqs/sanger-sequencing/]
- 49. Metagenomic pipeline for identifying co-infections among ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9172093/]
- 50. PhytoPipe: a phytosanitary pipeline for plant pathogen ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05589-2]
- 51. Simulated High Throughput Sequencing Datasets [https://pmc.ncbi.nlm.nih.gov/articles/PMC11428249/]
- 52. Metagenomic Next-Generation Sequencing in Infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384723/]
- 53. Seven-year performance of a clinical metagenomic next- ... [https://www.nature.com/articles/s41591-024-03275-1]
- 54. Experience of implementing metagenomic next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11926336/]
- 55. Sanger sequencing and deconvolution of polyclonal infections [https://pmc.ncbi.nlm.nih.gov/articles/PMC11031737/]
- 56. Advantages and challenges of metagenomic sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9527156/]
- 57. Contamination-controlled high-throughput whole genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5022032/]
- 58. Specimen requirements and shipping [https://www.preventiongenetics.com/ClinicalTesting/specimenRequirements]
- 59. Sanger Sequencing: Experimental Design and Sample ... [https://www.cd-genomics.com/blog/sanger-sequencing-sample-prepation-experimental-design/]
- 60. Sanger Sequencing Best Practices - A guide to sample ... [https://genome.center.uconn.edu/cgi-services/sequencing-best-practices-a-guide-to-sample-preparation-and-troubleshooting/]
- 61. Library Preparation for Next-Generation Sequencing [https://krakensense.com/blog/library-preparation-for-next-generation-sequencing]
- 62. Comparison of different criteria of metagenomic next- ... [https://www.sciencedirect.com/science/article/pii/S0732889323002444]
- 63. Identifying SNP threshold from P2 sequences for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11153907/]
- 64. Colonization and infection - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4074726/]
- 65. Mechanistic Models of Virus–Bacteria Co-Infections in ... [https://www.mdpi.com/2076-0817/14/8/830]
- 66. Next Generation Sequence Testing: Essential 2025 Guide [https://lifebit.ai/blog/next-generation-sequence-testing/]
- 67. 3 Essential Tips for Accurate Sanger Sequencing Results [https://internationaljournalofresearch.com/2025/08/21/3-essential-tips-for-accurate-sanger-sequencing-results/]
- 68. Understanding the Promises and Hurdles of Metagenomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7108102/]
- 69. A 'Culture' Shift: Application of Molecular Techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6447436/]
- 70. Microbial culture vs. mNGS: diagnostic variations in ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1611332/full]
- 71. Mastering DNA chromatogram analysis in Sanger ... [https://www.sciencedirect.com/science/article/pii/S1687157X23010077]
- 72. tNGS-based detection of respiratory pathogens in a single ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1663234/full]
- 73. Clinical utility of metagenomic next-generation sequencing ... [https://www.nature.com/articles/s41598-025-03564-w]
- 74. Systematic detection of co-infection and intra-host ... [https://www.nature.com/articles/s41467-023-43391-z]
- 75. DNA Test Detects Over Three Times of Lung Pathogens ... [https://www.bgi.com/global/news/study-dna-test-detects-over-three-times-of-lung-pathogens-than-traditional-methods]
- 76. Next-generation sequencing guides the treatment of severe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11637351/]
- 77. Diagnostic value of metagenomic next-generation sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618669/]
- 78. Guide to mNGS Data Analysis [https://chanzuckerberg.zendesk.com/hc/en-us/articles/13770737266196-Guide-to-mNGS-Data-Analysis]
- 79. MicrobesNG - Frequently Asked Questions [https://microbesng.com/microbesng-faq/]
- 80. NGS Sequencing Support-Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-support/ngs-support-troubleshooting.html]
- 81. Next Generation Sequencing Improves Diagnostic 16S ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418051/]
- 82. Application of next-generation sequencing to identify different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10859930/]