Antigen vs. PCR Testing: A Critical Analysis of Diagnostic Sensitivity and Specificity for SARS-CoV-2 and Respiratory Viruses
This article provides a comprehensive analysis of the diagnostic accuracy of rapid antigen tests (Ag-RDTs) versus polymerase chain reaction (PCR) for SARS-CoV-2 and other respiratory viruses.
Antigen vs. PCR Testing: A Critical Analysis of Diagnostic Sensitivity and Specificity for SARS-CoV-2 and Respiratory Viruses
Abstract
This article provides a comprehensive analysis of the diagnostic accuracy of rapid antigen tests (Ag-RDTs) versus polymerase chain reaction (PCR) for SARS-CoV-2 and other respiratory viruses. Aimed at researchers and drug development professionals, it synthesizes foundational performance data, methodological applications, and optimization strategies from recent real-world evidence and meta-analyses. The review highlights the significant sensitivity gap, particularly at low viral loads, and explores the implications of test selection on clinical outcomes, public health policy, and antimicrobial stewardship. It further discusses the critical need for robust post-market surveillance and validation frameworks to guide the development and deployment of future diagnostic technologies.
The Fundamental Accuracy Gap: Unpacking Sensitivity and Specificity in Antigen and PCR Tests
Molecular diagnostics play a pivotal role in modern disease control, with the polymerase chain reaction (PCR) established as the gold standard for pathogen detection. Its superior performance is particularly evident when compared to rapid antigen tests (RATs), especially in its ability to identify early, low-level infections through multi-target genetic analysis. This guide examines the experimental data and methodologies that underpin PCR's high sensitivity and specificity, providing a objective comparison for research and development professionals.
Analytical Performance: PCR vs. Rapid Antigen Tests
The core advantage of PCR lies in its direct detection of a pathogen's genetic material, allowing for exceptional sensitivity. Rapid antigen tests, which detect surface proteins, are inherently less sensitive, a disparity that becomes pronounced in low viral load scenarios.
The table below summarizes key performance metrics from recent studies.
| Test Type | Average Sensitivity | Average Specificity | Contextual Performance Notes | Source (Virus) |
|---|---|---|---|---|
| PCR (qPCR/ddPCR) | ~91.2% - 97.2% (Clinical Sensitivity) [1] [2] | ~91.0% - 100% (Clinical Specificity) [2] | Sensitivity approaches 100% for analytical detection of 500-5000 viral RNA copies/mL [3]. | SARS-CoV-2, Influenza, RSV [1] [2] |
| Rapid Antigen Test (RAT) | 59% - 69.3% (Overall) [4] [5] | 99% - 99.3% [4] [5] | Sensitivity can drop below 30% in patients with low viral loads [1]. | SARS-CoV-2 [4] [5] |
| RAT (Symptomatic) | 73.0% [5] | 99.1% [5] | Highest sensitivity (80.9%) within first week of symptoms [5]. | SARS-CoV-2 [5] |
| RAT (Asymptomatic) | 54.7% [5] | 99.7% [5] | Performance varies significantly by manufacturer [4] [5]. | SARS-CoV-2 [5] |
This significant sensitivity gap has direct clinical consequences. A large meta-analysis found that point-of-care RATs missed nearly a third of SARS-CoV-2 cases (70.6% sensitivity), while molecular point-of-care tests detected over 92% [1]. For influenza, some RATs detect only about half of all cases, performance considered "barely better than a coin toss" [1].
Multi-Target Detection: Enhancing Assay Robustness and Sensitivity
A key strategy for maximizing PCR's reliability is the simultaneous detection of multiple genetic targets. This approach mitigates the risk of false negatives due to mutations or genomic variations in a single region and is now recommended by global health bodies.
Experimental Data on Multi-Target Assays
Research on Yersinia pestis (the plague bacterium) provides a clear example. A 2024 study developed a droplet digital PCR (ddPCR) assay targeting three genes: ypo2088 (chromosomal), and caf1 and pla (plasmid-borne) [6]. This multi-target approach adhered to WHO guidelines, which recommend at least two positive gene targets for confirmed plague cases [6].
The performance of this multi-target assay was systematically evaluated [6]:
- Limits of Detection (LoD): The assay could detect as few as 6.2 to 15.4 copies of the target genes per reaction.
- Sensitivity in Complex Samples: It reliably detected low concentrations of Y. pestis in spiked soil (10² CFU/100 mg) and mouse liver tissue (10³ CFU/20 mg) samples, demonstrating superior sensitivity compared to a qPCR benchmark.
- Quantitative Linearity: The assay showed excellent quantitative performance across a wide range of bacterial concentrations (10³–10⁶ CFU/sample) with a linear correlation (R² = 0.99).
A similar principle applies to SARS-CoV-2 testing. A 2023 evaluation of five commercial RT-PCR kits found that those targeting more genes generally demonstrated better accuracy and fewer false-positive results [2]. For instance, kits targeting three genes (ORF1ab, N, and S or E) showed higher specificity compared to those targeting only one or two genes [2].
Detailed Experimental Protocol: Multi-Target ddPCR forY. pestis
The following protocol summarizes the key experimental methodology from the 2024 study on Y. pestis detection, which exemplifies a rigorous approach to multi-target assay development [6].
Assay Design and Components
- Target Selection: Three genes were selected to ensure redundancy: the chromosomal gene ypo2088 and the plasmid-borne virulence genes caf1 (pMT1 plasmid) and pla (pPCP1 plasmid).
- Primers and Probes: TaqMan hydrolysis probes and primers were designed for each target. Probes were labeled with distinct fluorophores (FAM for pla, HEX for caf1 and ypo2088) to allow multiplexing in a single reaction.
- Sample Preparation: Bacterial genomic DNA was extracted from cultured Y. pestis using a commercial DNA Mini kit. For simulated clinical samples, mouse liver tissues or soil samples were spiked with known concentrations of Y. pestis (measured in Colony Forming Units, CFU) before identical DNA extraction.
ddPCR Reaction Setup
- Reaction Mix: The 20 μL multiplex ddPCR reaction included:
- 10 μL of supermix for probes.
- Forward and reverse primers for all three genes (each at 900 nM).
- TaqMan probes at optimized concentrations (pla and caf1 at 250 nM, ypo2088 at 500 nM).
- 2 μL of the extracted DNA template.
- Droplet Generation and PCR: The reaction mixture was combined with 70 μL of droplet generation oil in a QX200 droplet generator to create thousands of nanoliter-sized droplets. The droplets underwent PCR amplification in a thermal cycler with the following protocol:
- Enzyme activation at 95°C for 10 minutes.
- 40 cycles of:
- Denaturation: 94°C for 30 seconds.
- Annealing/Extension: 60°C for 1 minute.
- Enzyme deactivation at 98°C for 10 minutes.
Data Acquisition and Analysis
- After amplification, droplets were read in a QX200 droplet reader.
- The reader measures the fluorescence in each droplet, classifying it as positive or negative for each target.
- The software uses Poisson statistics to provide an absolute count of the target DNA copies per microliter of the original reaction, without the need for a standard curve.
The Scientist's Toolkit: Key Research Reagents
The table below details essential reagents and their functions based on the protocols cited.
| Research Reagent / Kit | Primary Function in Assay |
|---|---|
| QIAamp DNA Mini Kit [6] | Extraction and purification of genomic DNA from complex samples (e.g., bacterial cultures, tissues, soil). |
| SuperMix for Probes (No dUTP) [6] | A ready-to-use master mix containing DNA polymerase, dNTPs, and optimized buffers for probe-based ddPCR. |
| TaqMan Hydrolysis Probes [6] | Sequence-specific oligonucleotides with a 5' fluorophore and a 3' quencher. Cleavage during PCR generates a fluorescent signal, enabling target detection and quantification. |
| Droplet Generation Oil [6] | An oil formulation used to partition the aqueous PCR reaction into approximately 20,000 nanoliter-sized droplets for digital PCR. |
| Viral Transport Medium (VTM) [4] | A medium used to preserve the viability of viruses and viral RNA in swab samples during transport and storage. |
| CRISPR-CasΦ System [7] | A novel CRISPR-associated protein used in emerging diagnostic platforms for its collateral cleavage activity, enabling amplification-free, ultrasensitive detection. |
Experimental data consistently confirms that PCR, particularly multi-targeted approaches, remains the gold standard for sensitive and specific pathogen detection. Its ability to amplify and detect multiple genetic regions simultaneously provides a robust defense against false negatives caused by pathogen evolution or low viral loads. While rapid antigen tests offer speed and convenience, their significantly lower sensitivity, especially in asymptomatic individuals or during early infection, limits their utility for confirmatory diagnosis. For researchers and clinicians, the choice of diagnostic tool must align with the required performance: PCR for maximum accuracy, and antigen tests for rapid screening where some sensitivity can be traded for speed.
The widespread adoption of Rapid Antigen Tests (Ag-RDTs) for detecting SARS-CoV-2 has represented a crucial public health tool during the COVID-19 pandemic, offering rapid results without specialized laboratory equipment. However, these tests face a fundamental challenge: inherently lower sensitivity compared to molecular methods like polymerase chain reaction (PCR). This performance gap is not random but stems from core technological and biological constraints. Antigen tests detect the presence of viral proteins, which requires a sufficient concentration of these target molecules in the sample to generate a positive signal. In contrast, PCR tests amplify specific sequences of viral genetic material, enabling the detection of even minuscule amounts of the virus that would be undetectable by antigen assays [8].
This article analyzes the mechanistic basis for this sensitivity trade-off, examining how viral load dynamics, test design parameters, and specimen characteristics collectively influence antigen test performance. For researchers and drug development professionals, understanding these limitations is essential for interpreting test results accurately, developing improved diagnostic platforms, and formulating effective testing strategies that account for the inherent strengths and weaknesses of different methodologies.
Comparative Performance Data: Antigen Tests vs. PCR
Numerous real-world studies and systematic reviews have quantified the performance gap between antigen tests and PCR. The table below summarizes key accuracy metrics from recent research, illustrating how antigen test sensitivity varies significantly across different conditions and patient populations.
Table 1: Diagnostic Accuracy of SARS-CoV-2 Antigen Tests Compared to PCR
| Study Context | Overall Sensitivity | Symptomatic Individuals | Asymptomatic Individuals | Specificity | Source |
|---|---|---|---|---|---|
| Cochrane Systematic Review (2023) | 69.3% (95% CI, 66.2-72.3%) | 73.0% (95% CI, 69.3-76.4%) | 54.7% (95% CI, 47.7-61.6%) | 99.3% (95% CI, 99.2-99.3%) | [5] |
| Brazilian Cross-Sectional Study (2025) | 59% (0.56-0.62) | No significant difference by symptom days | Not Reported | 99% (0.98-0.99) | [4] [9] |
| Systematic Review & Meta-Analysis (2021) | 75.0% (95% CI, 71.0-78.0) | Higher than asymptomatic | Lower than symptomatic | High (specific value not stated) | [10] |
| FDA-Authorized Tests Postapproval (2025) | 84.5% (Pooled from postapproval studies) | Not Reported | Not Reported | 99.6% | [11] |
A critical factor explaining this variable performance is the viral load in the patient sample. Antigen test sensitivity demonstrates a strong inverse correlation with PCR cycle threshold (Ct) values, a proxy for viral load. Data from a large Brazilian study vividly illustrates this relationship:
Table 2: Antigen Test Sensitivity as a Function of Viral Load (PCR Cycle Threshold)
| PCR Cycle Threshold (Ct) Range | Viral Load Interpretation | Antigen Test Sensitivity |
|---|---|---|
| Cq < 20 | High Viral Load | 90.85% |
| Cq 20-25 | Moderate to High | 89% |
| Cq 26-28 | Moderate | 66% |
| Cq 29-32 | Low | 34% |
| Cq ≥ 33 | Very Low | 5.59% |
This dependency on viral load is the primary mechanistic reason for antigen tests' lower overall sensitivity. PCR's ability to amplify target DNA allows it to detect infection across all viral load levels, while antigen tests are inherently limited to detecting the period of peak viral replication [1].
The Core Mechanism: Fundamental Limits of Antigen Detection
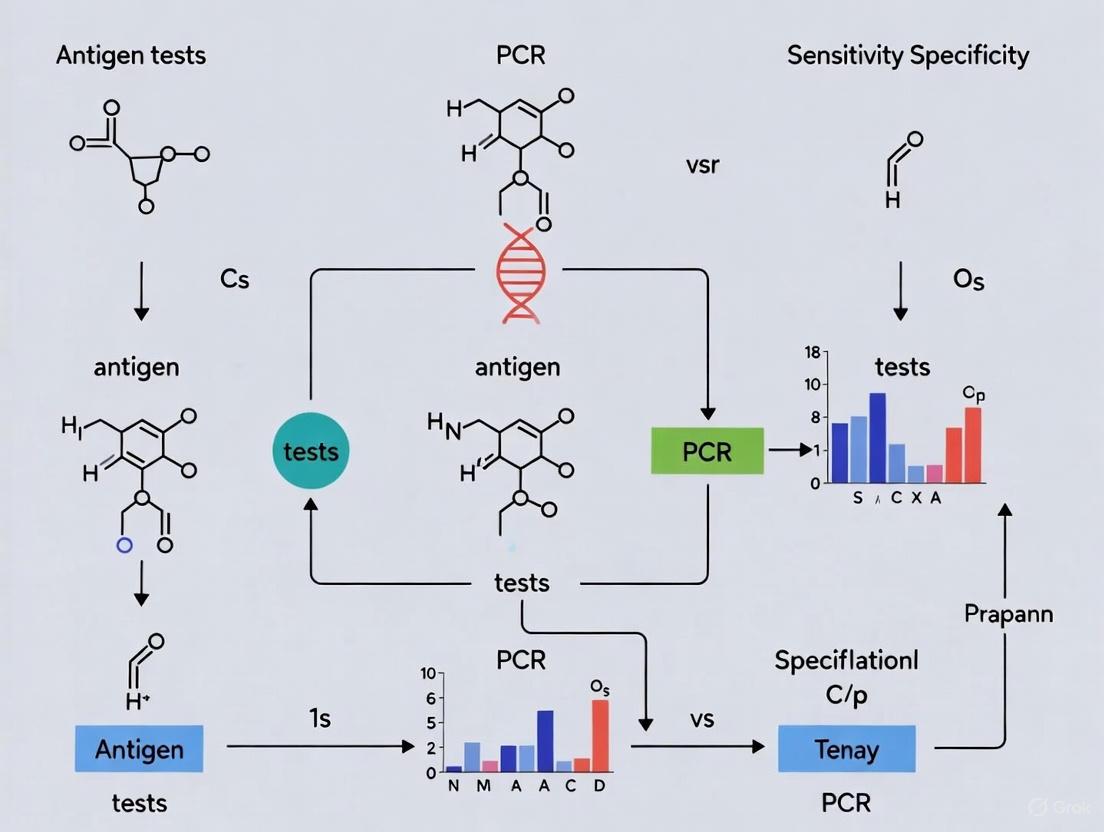
The sensitivity struggle of antigen tests is rooted in their foundational design principle: the direct, non-amplified detection of viral proteins. The following diagram illustrates the fundamental mechanistic disparity between antigen and PCR testing.
The Antigen Detection Pathway and Its Limitations
As shown in the diagram, the antigen test pathway involves viral lysis to release proteins, followed by antigen-antibody binding that is visualized on a test line. The critical limitation is the absence of signal amplification. The test relies on a sufficient number of antigen molecules being present in the sample to create a visible signal (e.g., a colored line) within the short test timeframe [8]. This detection threshold is typically only crossed during the peak viral load phase of an infection, which generally occurs around the time of symptom onset and lasts for a limited window [10]. If the viral protein concentration falls below the test's detection limit—which occurs during the early incubation period, late convalescent phase, or in some asymptomatic cases—the test will return a false negative result, even if the person is infected [1].
The PCR Amplification Advantage
In contrast, the PCR pathway incorporates a powerful amplification step. After converting viral RNA into complementary DNA (cDNA), the process uses enzymatic replication to create billions of copies of a specific target sequence from the original genetic material [8]. This exponential amplification allows the test to detect a very small initial number of viral RNA molecules—theoretically, even a single copy—by making them visible to fluorescent detection systems. This fundamental difference in methodology is why PCR can identify infections at very low viral loads, including during the early and late stages of infection when antigen tests are likely to fail [1].
Factors Influencing Antigen Test Performance
Biological and Clinical Variables
Beyond the core mechanism, several biological and clinical factors significantly influence antigen test sensitivity by affecting the viral antigen concentration in the sample:
- Time from Symptom Onset: Sensitivity is highest in the first week after symptoms begin (around 80.9%) when viral loads typically peak, and drops significantly in the second week (to approximately 53.8%) as the immune system clears the virus and antigen levels decline [5].
- Patient Age: One quantitative antigen test study found a positive correlation between age and test sensitivity (r=0.764 when excluding teenagers), with Presto-negative samples coming from significantly younger patients (median age 39 years) compared to Presto-positive samples (median age 53 years) [12]. This may be related to differences in viral shedding patterns or immune responses across age groups.
- SARS-CoV-2 Variant: While one study found no association between mutant strains and the results of a quantitative antigen test [12], the potential for mutations to alter antigen protein structures remains a theoretical concern that requires ongoing test evaluation.
Specimen Collection and Test Design Factors
- Sample Type and Quality: Nasopharyngeal samples generally yield higher viral loads compared to anterior nasal or saliva samples. Proper collection technique is crucial to obtaining an adequate sample for testing [10].
- Specimen Storage: Freezing specimens prior to antigen testing can impact test performance, potentially reducing sensitivity by altering antigen integrity or antibody binding affinity [10].
- Test Manufacturer and Design: Significant variability exists between different commercial antigen tests. A Cochrane review found that average sensitivities by brand ranged from 34.3% to 91.3% in symptomatic participants, highlighting the impact of assay design, including the antibodies used and the test's analytical limit of detection (LOD) [5].
Experimental Protocols for Performance Evaluation
To generate the comparative data discussed in this article, researchers have employed rigorous experimental protocols. The following methodology is representative of studies evaluating antigen test accuracy against the gold standard of PCR.
Table 3: Key Research Reagent Solutions and Their Functions
| Reagent / Material | Function in Experiment |
|---|---|
| Paired Nasopharyngeal Swabs | Simultaneous sample collection for Ag-RDT and RT-qPCR to enable direct comparison. |
| Viral Transport Medium (VTM) | Preserves virus integrity for transport and subsequent RT-qPCR analysis. |
| Rapid Antigen Test Kits (e.g., TR DPP COVID-19, IBMP TR Covid Ag) | Index test for detecting SARS-CoV-2 nucleocapsid antigens. |
| Viral RNA Extraction Kit (e.g., Loccus Biotecnologia) | Isolates viral genetic material from VTM for PCR amplification. |
| RT-qPCR Master Mix (e.g., GoTaq Probe 1-Step) | Contains enzymes, probes, and buffers for reverse transcription and DNA amplification. |
| RT-qPCR Instrument (e.g., QuantStudio 5) | Thermal cycler that performs precise temperature cycles for amplification and fluorescence detection. |
Detailed Experimental Methodology
1. Study Population and Sample Collection: Studies typically enroll symptomatic individuals presenting for testing. In the Brazilian study, consecutive individuals aged 12 years or older with symptoms suggestive of COVID-19 were included [4] [9]. Two nasopharyngeal swabs are collected simultaneously from each participant by trained healthcare workers to ensure sample parity.
2. Sample Processing and Testing:
- Antigen Testing: One swab is immediately tested using the rapid antigen test according to the manufacturer's instructions, with results typically available in 15-30 minutes [4] [13].
- PCR Testing: The paired swab is stored in Viral Transport Medium (VTM) at -80°C until RNA extraction can be performed. RNA is extracted using commercial kits, and RT-qPCR is performed using approved protocols (e.g., CDC's 2019-nCoV RT-PCR diagnostic protocol) on platforms such as the QuantStudio 5 [4]. Cycle threshold (Ct) values below 35-40 are generally considered positive for SARS-CoV-2.
3. Data Analysis: Statistical analysis involves calculating sensitivity, specificity, positive and negative predictive values, and accuracy with 95% confidence intervals. Results are often stratified by variables such as symptom status, days from symptom onset, and PCR Ct values to understand performance across different subpopulations [4] [5].
The following diagram maps this experimental workflow and the key decision points in the comparative analysis.
The inherent sensitivity limitations of antigen tests are a direct consequence of their fundamental detection mechanism, which relies on the presence of viral proteins above a certain threshold without the benefit of amplification. This mechanistic trade-off is not a design flaw but a defined characteristic that dictates their appropriate application.
For researchers and drug development professionals, these findings have several critical implications. First, diagnostic strategies must account for the predictable performance characteristics of antigen tests, reserving them for scenarios where speed and accessibility are prioritized over ultimate sensitivity, such as rapid screening during the symptomatic phase when viral loads are high. Second, the significant variability in performance between different test brands underscores the necessity of robust post-market surveillance and real-world validation, as manufacturer claims may not always reflect actual performance in clinical practice [11]. Finally, future innovation in rapid diagnostics should focus on novel technologies that can bridge the current performance gap, potentially through integrated isothermal amplification systems or enhanced signal detection methods that can approach PCR-level sensitivity while maintaining the operational advantages of current antigen tests.
The COVID-19 pandemic created an unprecedented global demand for accurate, scalable diagnostic testing. Two primary testing methodologies emerged: antigen-detection rapid diagnostic tests (Ag-RDTs) and quantitative reverse transcription polymerase chain reaction (RT-qPCR) tests. While manufacturers often claim high sensitivity for rapid antigen tests, systematic reviews frequently report considerably lower performance in real-world settings [14]. This discrepancy between controlled evaluations and clinical performance represents a critical challenge for researchers, clinicians, and public health officials relying on these diagnostics.
This guide objectively compares the performance of antigen tests versus PCR across multiple dimensions, including analytical sensitivity, specificity, and the impact of viral load. By synthesizing evidence from meta-analyses and large-scale real-world studies, we provide researchers and drug development professionals with comprehensive experimental data and methodologies to inform diagnostic selection and development.
Performance Comparison: Antigen Tests vs. PCR
Table 1: Overall Performance Characteristics of Antigen Tests vs. PCR
| Test Type | Sensitivity Range | Specificity Range | Overall Accuracy | Key Factors Influencing Performance |
|---|---|---|---|---|
| Antigen Tests (Overall) | 59-86.5% | 94-99.6% | 82-92.4% | Viral load, manufacturer, symptom status |
| PCR (Reference) | ~100% | ~100% | ~100% | Sample quality, extraction efficiency |
| Ag-RDT (High Viral Load, Cq <25) | 90-100% | 94-99.6% | N/R | Sample collection timing |
| Ag-RDT (Low Viral Load, Cq ≥30) | 5.6-31.8% | 94-99.6% | N/R | Viral variants, sample type |
N/R: Not Reported
Substantial evidence confirms that rapid antigen tests perform with high sensitivity (90-100%) when viral loads are high, typically corresponding to PCR cycle threshold (Cq) values below 25 [4] [15]. However, this sensitivity decreases significantly as viral load diminishes. A comprehensive Brazilian study with 2,882 symptomatic individuals demonstrated that antigen test sensitivity dropped from 90.85% at Cq <20 to just 5.59% at Cq ≥33 [4] [9].
Performance variations exist between different antigen test formats. Fluorescence immunoassay (FIA) platforms have demonstrated higher sensitivity (73.68%) compared to lateral flow immunoassay (LFIA) formats (65.79%) in asymptomatic patients [15]. Importantly, a systematic review of FDA-authorized tests found that most maintained stable accuracy post-approval, with pooled sensitivity of 86.5% in preapproval studies versus 84.5% in postapproval settings [14] [11].
Impact of Viral Load on Test Performance
Table 2: Antigen Test Sensitivity Across Viral Load Ranges
| PCR Cycle Threshold (Cq) Range | Viral Load Classification | Antigen Test Sensitivity | Clinical Implications |
|---|---|---|---|
| <20 | High | 90-100% | High detection reliability |
| 20-25 | Moderate to High | 89% | Good detection reliability |
| 26-28 | Moderate | 66% | Moderate detection reliability |
| 29-32 | Low | 34% | Poor detection reliability |
| ≥33 | Very Low | 5.6-27.3% | Minimal detection capability |
The inverse relationship between Cq values (indicating viral concentration) and antigen test sensitivity is well-established [4] [15]. One study demonstrated that while both FIA and LFIA antigen tests achieved 100% sensitivity at Cq values <25, their sensitivity reduced to 31.82% and 27.27% respectively at Cq values >30 [15]. This pattern underscores a fundamental limitation of antigen tests: they detect viral proteins, which are less abundant and only reliably detectable during peak infection.
Variant-Specific Performance
Antigen test performance varies across SARS-CoV-2 variants. Research comparing the Alpha, Delta, and Omicron variants found that the diagnostic sensitivity of FIA was 78.85% for Alpha and 72.22% for Delta, while LFIA showed 69.23% for Alpha and 83.33% for Delta [15]. Notably, both Ag-RDT formats achieved 100% sensitivity for detecting the Omicron variant, suggesting potentially enhanced performance against this variant [15].
Experimental Protocols and Methodologies
Standardized Evaluation Framework
The benchmark testing process for diagnostic assays follows a systematic approach to ensure accurate and comparable results [16]. The methodology involves performance comparison against established standards, repeated measurements to ensure reliability, and validation through statistical analysis.
Real-World Study Designs
Large-scale comparative studies typically employ simultaneous sampling methodologies. For example, in a study of 2,882 symptomatic individuals in Brazil, researchers collected two nasopharyngeal swabs simultaneously from each participant [4] [9]. One swab was analyzed immediately using Ag-RDTs with a 15-minute turnaround time, while the other was stored at -80°C in Viral Transport Medium (VTM) for subsequent RT-qPCR analysis [4]. This paired-sample approach controls for variability in viral load distribution across participants and sampling techniques.
RNA extraction typically employs automated systems such as the Extracta 32 platform using Viral RNA and DNA Kits [4]. PCR confirmation generally follows established protocols like the CDC's real-time RT-PCR diagnostic protocol for SARS-CoV-2, implemented on instruments such as the QuantStudio 5 with GoTaq Probe 1-Step RT-qPCR systems [4] [9].
Advanced Statistical Adjustment Methods
Recent methodological advances address variability in viral load distributions across studies. Bosch et al. (2024) proposed a novel approach that models the probability of positive agreement (PPA) as a function of qRT-PCR cycle thresholds using logistic regression [17]. This method calculates adjusted sensitivity by applying the PPA function to a reference concentration distribution, enabling more uniform sensitivity comparisons across different test products and studies [17].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Diagnostic Test Evaluation
| Reagent/Equipment | Manufacturer/Example | Primary Function | Application Notes |
|---|---|---|---|
| Viral Transport Medium (VTM) | Various | Preserve specimen integrity during transport and storage | Maintains viral viability and nucleic acid stability |
| Automated Nucleic Acid Extractor | Extracta 32 (Loccus Biotecnologia) | Automated RNA/DNA extraction from clinical samples | Increases processing throughput and standardization |
| Viral RNA and DNA Kit | MVXA-P096FAST (Loccus Biotecnologia) | Nucleic acid purification from clinical samples | Compatible with automated extraction systems |
| RT-qPCR Reagents | GoTaq Probe 1-Step RT-qPCR (Promega) | One-step reverse transcription and quantitative PCR | Reduces handling steps and potential contamination |
| Real-time PCR Instrument | QuantStudio 5 (Applied Biosystems) | Quantitative PCR amplification and detection | Enables precise Ct value determination |
| Nasopharyngeal Swabs | FLOQSwabs (Copan) | Clinical specimen collection | Specialized surface coating improves sample recovery |
Discussion and Research Implications
The discrepancy between meta-analysis findings and real-world performance data for antigen tests stems primarily from methodological variations in study design, particularly the distribution of viral loads in sample populations [17]. While manufacturer-reported sensitivities often exceed 80% [9], real-world studies frequently report lower values, such as the 59% overall sensitivity observed in a Brazilian study of 2,882 symptomatic individuals [4]. This discrepancy underscores the importance of standardized post-market surveillance.
Regulatory implications are significant, as evidenced by findings that only 21% of FDA-authorized rapid antigen tests had postapproval studies conducted according to manufacturer instructions [14] [11]. Furthermore, performance variability between test brands can be substantial, with one study reporting 70% sensitivity for the IBMP TR Covid Ag kit compared to 49% for the TR DPP COVID-19 - Bio-Manguinhos test [4] [9].
For researchers and drug development professionals, these findings highlight the necessity of: (1) accounting for viral load distributions when evaluating test performance; (2) implementing standardized benchmarking protocols across studies; and (3) conducting robust post-market surveillance to verify real-world performance. Future diagnostic development should focus on maintaining high specificity while improving sensitivity in low viral load scenarios, potentially through enhanced detection methodologies or multi-target approaches.
The diagnostic performance of rapid antigen tests (Ag-RDTs) for SARS-CoV-2 is fundamentally governed by the viral load present in patient samples, most commonly proxied by quantitative reverse transcription polymerase chain reaction (qRT-PCR) cycle threshold (Ct) values. This inverse relationship between Ct values and antigen test sensitivity represents a critical parameter for researchers, clinical microbiologists, and public health officials interpreting test results and designing testing strategies. Ct values indicate the number of amplification cycles required for viral RNA detection in qRT-PCR, with lower values corresponding to higher viral loads [18]. Antigen tests, which detect viral nucleocapsid proteins rather than nucleic acids, demonstrate markedly variable sensitivity across this viral load spectrum, creating significant implications for their appropriate application in different clinical and public health contexts [19] [4]. Understanding this relationship is essential for optimizing test utilization, particularly when differentiating between diagnostic scenarios requiring high sensitivity versus those where rapid results provide greater utility despite reduced sensitivity.
Quantitative Data: The Inverse Correlation Between Ct Values and Antigen Test Sensitivity
Substantial clinical evidence confirms that antigen test sensitivity declines precipitously as Ct values increase (indicating lower viral loads). This relationship follows a predictable pattern across multiple test brands and study populations, though specific sensitivity thresholds vary between products.
Table 1: Antigen Test Sensitivity Across PCR Ct Value Ranges
| Ct Value Range | Viral Load Category | Reported Sensitivity Ranges | Key Studies |
|---|---|---|---|
| <20 | Very High | 90.9% - ~100% | [4] [13] |
| 20-25 | High | ~80% - 100% | [4] [13] |
| 25-30 | Moderate | 47.8% - Decreases significantly | [4] [13] |
| ≥30 | Low | 5.6% - <30% | [4] [1] |
A comprehensive Brazilian study with 2,882 symptomatic individuals demonstrated this relationship clearly, showing agreement between antigen tests and PCR dropped from 90.85% for samples with Cq <20 to just 5.59% for samples with Cq ≥33 [4]. This trend persists across diverse populations and settings. Research from an emergency department in Seoul confirmed that antigen test positivity rates fell significantly as Ct values increased, with most false-negative antigen results occurring in samples with higher Ct values [18]. Similarly, a manufacturer-independent evaluation of five rapid antigen tests in Scandinavian test centers found that sensitivity variations between tests were substantially influenced by the underlying Ct value distribution of the study population [20].
The correlation between test band intensity and Ct values further reinforces this relationship. One study performing semi-quantitative evaluation of antigen test results found a strong negative correlation (r = -0.706) between Ct values and antigen test band color intensity, with weaker bands observed in samples with higher Ct values [13].
Standardizing Performance Comparisons: Accounting for Ct Value Distribution in Study Design
Cross-study comparisons of antigen test performance are complicated by substantial variations in the Ct value distributions of study populations. Differences in sampling methodologies—such as enrichment for high- or low-Ct specimens—can significantly bias sensitivity estimates and limit generalizability [19].
Statistical Correction Methodology
Researchers have developed statistical frameworks to address this confounding factor by modeling percent positive agreement (PPA) as a function of Ct values and recalibrating results to a standardized reference distribution:
Modeling PPA Function: Using logistic regression on paired antigen test and qRT-PCR results to model the probability of antigen test positivity across the Ct value spectrum [19] [21].
Reference Distribution Application: Applying the derived PPA function to a standardized reference Ct distribution to calculate bias-corrected sensitivity estimates [19].
Performance Standardization: This adjustment enables more accurate comparisons of intrinsic test performance across different studies and commercial suppliers by removing variability introduced by differing viral load distributions [19].
Table 2: Essential Research Reagents and Materials for Antigen Test Performance Studies
| Research Component | Specific Function | Examples/Notes |
|---|---|---|
| Reference Standard | Gold-standard comparator for sensitivity/specificity | qRT-PCR with Ct value reporting [4] [13] |
| Viral Transport Medium (VTM) | Preserve specimen integrity during transport | Used in paired sampling designs [4] [20] |
| Protein Standards | Quantitative test strip signal calibration | Recombinant nucleocapsid protein [21] |
| Inactivated Virus | Analytical sensitivity determination | Heat-inactivated SARS-CoV-2 for LoD studies [21] |
| Digital Imaging Systems | Objective test line intensity measurement | Cell phone cameras with standardized imaging conditions [21] |
This methodology was validated using clinical data from a community study in Chelsea, Massachusetts, which demonstrated that raw sensitivity estimates varied substantially between test suppliers due to differing Ct distributions in their sample populations. After statistical adjustment to a common reference standard, these biases were reduced, enabling more equitable performance comparisons [19].
Experimental Protocols: Assessing Antigen Test Performance Across Viral Loads
Paired Clinical Sample Testing Protocol
The fundamental methodology for establishing the relationship between Ct values and antigen test performance involves concurrent testing of clinical samples with both antigen tests and qRT-PCR:
Sample Collection: Consecutive symptomatic individuals provide paired nasopharyngeal, oropharyngeal, or combined swab specimens [4] [20] [13].
Parallel Testing: One swab is processed immediately using the rapid antigen test according to manufacturer instructions, while the other is placed in viral transport medium for qRT-PCR analysis [4] [20].
Ct Value Determination: RNA extraction followed by qRT-PCR amplification with Ct value recording for positive samples [4] [13].
Data Analysis: Calculate antigen test sensitivity stratified by Ct value ranges and model the relationship using statistical methods such as logistic regression [19] [4].
Laboratory-Based Quantitative Framework
For more rigorous analytical performance assessment beyond clinical sampling, a laboratory-anchored framework can be implemented:
This integrated approach combines analytical measurements with human factors to generate predictive models of real-world test performance. The methodology involves characterizing the test strip signal intensity response to varying concentrations of target recombinant protein and inactivated virus, typically using serial dilutions and digital imaging of test strips to quantify signal intensity [21]. The limit of detection is then statistically characterized using the visual acuity of multiple observers, representing the probability distribution of naked-eye detection thresholds across the user population [21]. Finally, calibration curves are established between qRT-PCR Ct values and viral concentrations, enabling the composition of a Bayesian predictive model that estimates the probability of positive antigen test results as a function of Ct values [21].
Implications for Diagnostic Applications and Public Health Strategy
The deterministic relationship between Ct values and antigen test performance has profound implications for their appropriate utilization across different clinical scenarios.
Diagnostic Strategy Considerations
The Infectious Diseases Society of America (IDSA) guidelines recommend antigen testing for symptomatic individuals within the first five days of symptom onset when viral loads are typically highest, with pooled sensitivity of 89% (95% CI: 83% to 93%) during this period [22]. This sensitivity declines significantly to 54% when testing occurs after five days of symptoms [22]. For asymptomatic individuals, antigen test sensitivity is substantially lower (pooled sensitivity 63%), reflecting the higher proportion of pre-symptomatic or low viral load cases in this population [22].
Molecular testing remains the method of choice when diagnostic certainty is paramount, particularly for immunocompromised patients, hospital admissions, or when clinical suspicion is high despite a negative antigen test [5] [22]. The high specificity of antigen tests (consistently >99%) means positive results are highly reliable and actionable without confirmatory testing across most prevalence scenarios [5] [22].
Transmission Risk Assessment
The correlation between Ct values and antigen test performance has important implications for transmission control. Since antigen tests are most likely to be positive when viral loads are high (typically Ct <25-30), they effectively identify individuals with the highest probability of being infectious [18]. This characteristic makes them valuable tools for rapid isolation of contagious individuals in emergency departments, hospitals, and community settings, despite their lower overall sensitivity compared to PCR [18].
The inverse relationship between Ct values and antigen test sensitivity is a fundamental characteristic that must guide test selection, interpretation, and application across clinical and public health settings. Antigen tests serve as effective tools for identifying contagious individuals during the early, high viral load phase of infection, while PCR remains essential for definitive diagnosis, particularly in low viral load scenarios. Future test development should focus on improving sensitivity across the viral load spectrum while maintaining the speed, accessibility, and cost advantages that make rapid antigen tests valuable components of comprehensive diagnostic and infection control strategies.
Within the critical framework of diagnostic test performance, the high specificity of rapid antigen assays represents a cornerstone of their utility in pandemic control and clinical decision-making. Specificity, defined as a test's ability to correctly identify true negative cases, is the metric that ensures false alarms are minimized and resources are efficiently allocated. While the lower sensitivity of antigen tests compared to polymerase chain reaction (PCR) has been extensively documented, their consistently high specificity deserves focused examination, particularly for researchers and drug development professionals optimizing diagnostic strategies. This guide provides a detailed, data-driven comparison of antigen and PCR test performance, with a specialized focus on the experimental protocols and quantitative evidence underlying the exceptional true-negative rate of antigen assays.
Core Concepts: Specificity, Sensitivity, and Diagnostic Utility
Defining the Diagnostic Metrics
In any diagnostic evaluation, sensitivity and specificity form an interdependent pair of performance characteristics.
- Sensitivity (Positive Agreement): The proportion of actual positives correctly identified by the test. High sensitivity is crucial for ruling out disease.
- Specificity (True-Negative Rate): The proportion of actual negatives correctly identified by the test. High specificity is essential for confirming disease and avoiding false alarms.
The inverse relationship between these metrics often necessitates a balanced approach based on the clinical or public health context. Antigen tests have carved a distinct niche by offering extremely high specificity, making them particularly valuable in situations where a positive result must be trusted to initiate immediate isolation or treatment.
The Technical Foundation of Specificity
The high specificity of antigen tests stems from their core detection mechanism. These lateral flow immunochromatographic assays utilize highly selective monoclonal or polyclonal antibodies that bind to specific viral antigen epitopes, typically the nucleocapsid (N) protein in SARS-CoV-2 [23]. This antibody-antigen interaction is fundamentally designed to minimize cross-reactivity with other pathogens or human proteins, thereby yielding a low false-positive rate. The result is a test that, when positive, provides a highly reliable indication of active infection.
Quantitative Performance Comparison
Extensive real-world studies and meta-analyses have consistently validated the high specificity of antigen tests, even as sensitivity varies more significantly.
Table 1: Overall Diagnostic Accuracy of SARS-CoV-2 Antigen Tests vs. PCR
| Metric | Antigen Test Performance | PCR Test Performance | Contextual Notes |
|---|---|---|---|
| Overall Specificity | 99.3% (95% CI 99.2–99.3%) [5] | Approaching 100% (Gold Standard) [24] [25] | Antigen specificity remains exceptionally high across most brands and settings. |
| Overall Sensitivity | 69.3% (95% CI 66.2–72.3%) [5] | >95% (Gold Standard) [1] | Highly dependent on viral load, symptoms, and timing. |
| Positive Predictive Value (PPV) | Ranges from 81% (5% prevalence) to 95% (20% prevalence) [5] | >99% in most clinical scenarios | Directly tied to disease prevalence; higher prevalence increases PPV. |
| Negative Predictive Value (NPV) | >95% across prevalence scenarios of 5-20% [5] | >99% in most clinical scenarios |
Table 2: Impact of Patient and Testing Factors on Antigen Test Sensitivity
| Factor | Impact on Sensitivity | Effect on Specificity |
|---|---|---|
| Symptomatic Status | 73.0% in symptomatic vs. 54.7% in asymptomatic individuals [5] | Remains high (≈99%) in both groups [5] |
| Viral Load (Ct Value) | 90.85% for Cq < 20 (high load) vs. 5.59% for Cq ≥ 33 (low load) [4] | Specificity is largely independent of viral load. |
| Duration of Symptoms | 80.9% in first week vs. 53.8% in second week [5] | Not reported to significantly affect specificity. |
| Test Brand | Wide variation: 34.3% to 91.3% in symptomatic patients [5] | Most brands maintain specificity >97% [5] [14] |
The data in Table 1 underscores a critical finding: while the sensitivity of antigen tests is variable and often moderate, their specificity is consistently and reliably high, frequently exceeding 99% [5]. This means that in a population with a prevalence of 5%, an antigen test would correctly identify about 95 out of 100 positive results as positive, with a negative predictive value remaining above 95% [5].
Experimental Protocols for Assessing Specificity
For researchers validating diagnostic performance, understanding the standard methodological framework for determining specificity is essential. The following workflow outlines the common comparative design.
Core Methodology Explained
The standard protocol for determining specificity involves a head-to-head comparison with the gold standard, PCR, in a cohort that includes both infected and non-infected individuals.
- Cohort Selection & Sample Collection: Studies typically enroll a diverse cohort, including individuals presenting with symptoms suggestive of infection and asymptomatic individuals, to ensure a representative sample. As detailed in a Brazilian cross-sectional study, paired swabs are collected simultaneously from each participant to eliminate variability [4]. One swab is placed in viral transport medium (VTM) for PCR analysis, while the other is used directly for the rapid antigen test.
- Reference Standard Testing (PCR): The PCR sample undergoes nucleic acid extraction, followed by reverse transcription and amplification using primers and probes specific to viral genes (e.g., N, E, ORF1ab) [24] [23]. The resulting Cycle threshold (Ct) value serves as a quantitative measure of viral load, with lower Ct values indicating higher viral loads [4] [23]. A sample is typically considered positive if the Ct value is below a predetermined cutoff (e.g., 35-40) [13].
- Index Test Processing (Antigen Assay): The antigen test swab is processed according to the manufacturer's instructions, typically involving immersion in a buffer solution and application to the test cassette. The test operates on a lateral flow immunoassay principle, where labeled antibodies bind to the viral antigen, forming a visible line on the test strip [23]. The result is read visually or instrumentally within 15-30 minutes.
- Data Analysis & Specificity Calculation: Results are compiled into a 2x2 contingency table. Specificity is calculated as the number of true negatives (samples negative by both antigen test and PCR) divided by the total number of PCR-negative samples [4] [5]. This provides the proportion of uninfected individuals who were correctly identified by the antigen test.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents and Materials for Diagnostic Test Validation
| Reagent/Material | Critical Function in Validation |
|---|---|
| Paired Swab Kits | Ensures identical sample collection for both index and reference tests, minimizing pre-analytical variability. |
| Viral Transport Medium (VTM) | Preserves viral integrity for PCR testing during transport and storage. |
| RNA Extraction Kits | Isolates high-purity viral RNA from patient samples, a critical step for reliable PCR results. |
| PCR Master Mixes | Contains enzymes (e.g., Taq polymerase), dNTPs, and buffers essential for cDNA synthesis and DNA amplification. |
| Primers & Probes | Short, specific nucleotide sequences that bind to target viral genes, enabling selective amplification and detection. |
| Lateral Flow Test Cassettes | The device containing the nitrocellulose membrane strip with immobilized antibodies for antigen capture and detection. |
| Reference Antigens | Purified viral proteins used as positive controls to verify test functionality and performance. |
Statistical Modeling and Public Health Impact
Interpreting Discordant Results
The high specificity of antigen tests directly informs how to handle discordant results—particularly a positive antigen test followed by a negative PCR test. A model developed for this scenario estimated that in a context of low community prevalence, a patient with this discordant result had only a 15.4% chance of actually being infected [26]. This low probability is a direct consequence of high test specificity; when disease prevalence is low, even a test with an excellent specificity rate will generate a number of false positives that can outweigh the true positives. Therefore, in low-prevalence settings, a negative confirmatory PCR result is highly reliable in indicating that the initial positive antigen test was a false positive [26].
Pathway to Public Health Application
The following diagram illustrates the logical flow from test performance characteristics to public health application, highlighting the role of high specificity.
The body of evidence conclusively demonstrates that high specificity is a robust and reliable feature of rapid antigen assays. While their sensitivity is dependent on viral load and clinical context, the ability of these tests to correctly identify true negatives is consistently excellent. For researchers and public health officials, this performance profile makes antigen tests a powerful tool for specific applications: confirming infection when positive, enabling rapid isolation and contact tracing, and efficiently screening populations in moderate to high prevalence settings. Understanding this "specificity in focus" allows for the strategic deployment of antigen tests within a broader diagnostic ecosystem, where they complement, rather than compete with, the high sensitivity of PCR. Future development should continue to leverage the robust specificity of immunoassay platforms while striving to improve sensitivity at lower viral loads.
Strategic Test Deployment: Matching Methodology to Clinical and Public Health Objectives
The strategic application of SARS-CoV-2 diagnostic tests is a critical component of effective public health response. Within this framework, a clear understanding of the performance characteristics of Antigen-Detecting Rapid Diagnostic Tests (Ag-RDTs) versus the gold standard Nucleic Acid Amplification Tests (NAATs), such as PCR, across different population groups is essential for researchers and clinicians. The World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) provide structured guidance on test utilization, grounded in the fundamental metrics of sensitivity and specificity. Diagnostic sensitivity refers to a test's ability to correctly identify those with the disease (true positive rate), while diagnostic specificity indicates its ability to correctly identify those without the disease (true negative rate) [4]. This guide objectively compares the performance of antigen tests against PCR, synthesizing current guidelines and supporting experimental data to inform decision-making in research and clinical practice.
Official Guidelines: WHO and CDC Testing Frameworks
World Health Organization (WHO) Recommendations
The WHO has established minimum performance requirements for Ag-RDTs to be considered for deployment. These criteria are intentionally structured around the context of use:
- Minimum Performance: Ag-RDTs should meet or exceed ≥80% sensitivity and ≥97% specificity compared to NAAT [20] [13].
- Symptomatic Individuals: Ag-RDTs are primarily recommended for use in individuals presenting with symptoms consistent with COVID-19. Testing should be conducted within the first 5-7 days of symptom onset when viral loads are typically highest [13].
- Asymptomatic Individuals: The WHO advises that Ag-RDTs can be used for testing asymptomatic individuals, particularly as part of serial testing strategies during outbreaks or for contact tracing. However, a negative result in an asymptomatic person may require confirmation with a NAAT due to the higher risk of false negatives [13].
Centers for Disease Control and Prevention (CDC) and IDSA Guidelines
The CDC's guidance and the Infectious Diseases Society of America (IDSA) guidelines provide a nuanced framework that aligns with the WHO's principles, further refining the application based on symptomatic status:
- Symptomatic Individuals (IDSA Recommendation): For symptomatic individuals suspected of having COVID-19, the IDSA panel recommends a single Ag test over no test (strong recommendation, moderate certainty evidence). A positive Ag result, due to its high specificity, can be used to guide treatment and isolation without confirmation. However, if clinical suspicion remains high despite a negative Ag test, confirmation with a NAAT is recommended [22].
- Asymptomatic Individuals: The IDSA guidance notes that the pooled sensitivity of Ag testing in asymptomatic individuals is substantially lower (63%) than in symptomatic populations. This underscores the need for caution when interpreting negative results in this group [22].
- Test Selection Hierarchy: When resources and logistics permit, the IDSA suggests using standard NAAT over Ag tests due to superior sensitivity. The value of rapid Ag testing is highest when timely NAAT is unavailable, as it allows for rapid isolation and contact tracing [22].
Comparative Performance Data: Antigen Tests vs. PCR
The following tables synthesize quantitative data from manufacturer-independent evaluations and guideline summaries, providing a clear comparison of test performance.
| Population | Sensitivity Range | Specificity Range | Key Influencing Factors | Source / Study |
|---|---|---|---|---|
| Symptomatic | 63% - 81% | ≥99% | Timing after symptom onset (highest within first 5 days) | IDSA Guideline [22] |
| Asymptomatic | ~63% | ≥99% | Viral load prevalence; single vs. serial testing | IDSA Guideline [22] |
| Real-World (Symptomatic) | 59% (Overall) | 99% | Test brand, viral load | Brazilian Cohort (n=2882) [4] |
| Real-World (Various Brands) | 53% - 90% | 97.8% - 99.7% | Manufacturer, intended user technique | Scandinavian SKUP Evaluations [20] |
Table 2: Impact of Viral Load on Ag-RDT Performance
| Viral Load Indicator | Ag-RDT Sensitivity | Implications for Test Application |
|---|---|---|
| High Viral Load (Ct < 25) | Very High (e.g., ~90-100% agreement with PCR) | Ag-RDT is highly reliable for detecting infectious individuals [4] [13]. |
| Low Viral Load (Ct ≥ 33) | Very Low (e.g., 5.6% agreement with PCR) | Ag-RDT is likely to yield false negatives; PCR is required for detection [4]. |
| Correlation | Strong inverse correlation between Ct value and antigen test band intensity | Semi-quantitative visual interpretation may offer a crude gauge of infectiousness [13]. |
Key Experimental Protocols and Methodologies
Understanding the data supporting these guidelines requires an overview of the experimental methodologies employed in key studies.
Real-World Diagnostic Accuracy Study
A large-scale, cross-sectional study in Brazil (2022) provides a robust example of real-world Ag-RDT evaluation [4].
- Objective: To determine the real-world accuracy of SARS-CoV-2 antigen tests compared to quantitative RT-PCR (qPCR).
- Participant Cohort: 2,882 symptomatic individuals presenting within the public healthcare system.
- Specimen Collection: Two nasopharyngeal swabs were collected simultaneously from each participant.
- Testing Protocol: One swab was analyzed immediately using one of two Ag-RDT brands (TR DPP or IBMP TR Covid Ag). The other swab was stored in viral transport medium at -80°C for subsequent blinded qPCR analysis using the CDC's RT-PCR diagnostic protocol.
- Data Analysis: Sensitivity, specificity, accuracy, and positive/negative predictive values were calculated. Results were stratified by qPCR cycle threshold (Cq) values as a proxy for viral load.
Multi-Brand Evaluation and User-Friendliness Assessment
The Scandinavian SKUP collaboration performed prospective, manufacturer-independent evaluations of five Ag-RDTs to assess both performance and usability [20].
- Study Setting & Participants: Consecutive enrolment of individuals at COVID-19 test centres in Norway and Denmark. The intended sample size was at least 100 PCR-positive and 100 PCR-negative participants.
- Procedure: Duplicate samples were collected for the Ag-RDT and for RT-PCR. The Ag-RDT was performed immediately by test centre employees, the intended users of the tests.
- User-Friendliness Evaluation: Employees completed a structured questionnaire to rate the tests on criteria such as clarity of instructions, ease of procedure, and result interpretation.
- Analysis: Diagnostic sensitivity and specificity were calculated with 95% confidence intervals. User-friendliness feedback was synthesized into an overall rating.
Signaling Pathways and Experimental Workflows
The following diagram illustrates the logical decision pathway for test application as recommended by health authorities, integrating the critical factors of symptomatic status and test purpose.
The Scientist's Toolkit: Key Research Reagents and Materials
For researchers designing studies to evaluate diagnostic test performance, the following reagents and materials are essential.
Table 3: Essential Research Materials for Diagnostic Test Evaluation
| Research Reagent / Material | Function in Experimental Protocol |
|---|---|
| Nasopharyngeal/Oropharyngeal Swabs | Standardized collection of human respiratory specimen for paired testing [4] [13]. |
| Viral Transport Medium (VTM) | Preservation of virus viability and nucleic acid integrity for transport and storage prior to PCR analysis [4] [20]. |
| RNA Extraction Kits | Isolation of high-quality viral RNA from clinical samples, a critical step for RT-PCR [4]. |
| RT-PCR Master Mixes & Assays | Amplification and detection of specific SARS-CoV-2 gene targets (e.g., N, ORF1ab) using fluorescent probes [4] [13]. |
| Quantified SARS-CoV-2 Controls | Standardized virus stocks (e.g., PFU/mL, RNA copies/mL) for determining the limit of detection (LOD) and evaluating variant cross-reactivity [27]. |
| Ag-RDT Test Kits | The point-of-care immunoassays being evaluated, used according to manufacturer's instructions for use (IFU) [20]. |
Point-of-care (POC) testing is defined by its operational context rather than by technology alone—it encompasses any diagnostic test performed at or near the patient where the result enables a clinical decision to be made and an action taken that leads to an improved health outcome [28]. In resource-limited settings (RLS), where access to centralized laboratory facilities is often constrained, the World Health Organization (WHO) has established the "ASSURED" criteria for ideal POC tests: Affordable, Sensitive, Specific, User-friendly, Rapid and robust, Equipment-free, and Deliverable to those who need them [28]. Within this framework, rapid antigen detection tests (Ag-RDTs) have emerged as transformative tools for infectious disease management, offering distinct operational advantages that justify their deployment despite recognized limitations in analytical sensitivity compared to molecular methods.
The fundamental distinction between antigen and molecular testing lies in their detection targets. Antigen tests detect specific proteins on the surface of pathogens using lateral flow immunoassay technology, typically providing results in 10-30 minutes [29]. In contrast, molecular tests (including nucleic acid amplification tests or NAATs) detect pathogen genetic material (DNA or RNA) through amplification techniques like polymerase chain reaction (PCR), offering higher sensitivity but often requiring more complex equipment and longer processing times (15-45 minutes for POC molecular tests) [29]. This comparison guide objectively examines the performance characteristics and operational considerations of these testing modalities within the context of RLS and community settings, supported by experimental data and practical implementation frameworks.
Operational Advantages of Antigen Tests in Resource-Limited Settings
Speed, Simplicity, and Decentralization
The most significant operational advantage of antigen tests in RLS is their rapid turnaround time, which enables clinical decision-making during the same patient encounter. This immediacy eliminates the delays associated with sample transport to centralized laboratories, which can take days in remote settings and often results in patients lost to follow-up [28]. Antigen tests typically produce results within 10-30 minutes without requiring specialized laboratory equipment or highly trained personnel [29]. This simplicity allows deployment at various healthcare levels, including primary health clinics, mobile testing units, and even community-based settings by minimally trained lay providers.
Most antigen tests are CLIA-waived, enabling their use across a broad spectrum of clinical settings without requiring high-complexity laboratory certification [29]. The technical simplicity extends to sample preparation, which is often straightforward—many antigen tests use direct swabs without needing viral transport media or complex processing steps. This equipment-free operation aligns perfectly with the WHO ASSURED criteria, particularly important in settings with unreliable electricity, limited refrigeration capabilities, or inadequate technical support infrastructure [28].
Economic and Logistical Considerations
Antigen tests present compelling economic advantages in resource-constrained environments. Both the per-test cost and equipment requirements are significantly lower than molecular alternatives [29]. For health systems with limited budgets, these cost differentials enable broader testing coverage and more sustainable program implementation. The minimal maintenance requirements and lack of dependency on proprietary cartridges or reagents further reduce the total cost of ownership and eliminate supply chain vulnerabilities that can plague more complex diagnostic systems.
The operational independence of antigen tests from sophisticated laboratory infrastructure makes them particularly valuable for last-mile delivery in remote or conflict-affected areas. Their robustness—including tolerance of temperature variations and extended shelf life—enhances deliverability to marginalized populations [28]. This combination of affordability and deliverability addresses two critical barriers to diagnostic access in RLS, explaining why antigen tests have become foundational to infectious disease control programs for conditions like malaria, HIV, tuberculosis, and SARS-CoV-2 in low-resource contexts [28].
Comparative Performance: Antigen Tests Versus Molecular Methods
Analytical Sensitivity and Specificity
The primary trade-off for the operational advantages of antigen tests is reduced analytical sensitivity compared to molecular methods. Antigen tests generally have moderate sensitivity (50-90%, depending on the pathogen and test brand) while maintaining high specificity (>95%) [29]. Molecular tests, in contrast, typically demonstrate sensitivity >95% and specificity >98% for most pathogens [29]. This performance differential stems from fundamental methodological differences: antigen tests detect surface proteins without amplification, while molecular tests amplify target genetic material, enabling detection of minute quantities of pathogen.
Table 1: Comparative Performance of SARS-CoV-2 Testing Modalities
| Performance Characteristic | Antigen POC Tests | Molecular POC Tests | Laboratory-based RT-PCR |
|---|---|---|---|
| Typical Sensitivity | 59-70.6% [4] [30] | >95% [29] | >95% (reference standard) [30] |
| Typical Specificity | 94-99% [4] [30] | >98% [29] | >99% [30] |
| Turnaround Time | 10-30 minutes [29] | 15-45 minutes [29] | Hours to days (including transport) [28] |
| Approximate Cost | Low [29] | Moderate to High [29] | High (includes infrastructure) [28] |
| Equipment Needs | Minimal [29] | Analyzer required [29] | Sophisticated laboratory equipment [28] |
| Operational Complexity | Usually CLIA-waived [29] | Often CLIA-moderate complexity [29] | High-complexity certification [28] |
| Best Use Case | High-prevalence settings, rapid screening [29] | High-accuracy needs, low-prevalence settings [29] | Confirmatory testing, asymptomatic screening [30] |
Viral Load Dependence and Clinical Utility
The sensitivity of antigen tests demonstrates strong dependence on viral load, as evidenced by their correlation with RT-PCR cycle threshold (Ct) values. A 2025 Brazilian study of 2,882 symptomatic individuals found overall antigen test sensitivity of 59% compared to RT-PCR, but this increased to 90.85% for samples with high viral load (Cq < 20) [4]. Conversely, agreement dropped significantly to 5.59% for samples with low viral load (Cq ≥ 33) [4]. This viral load dependence creates a useful epidemiological property: antigen tests are most likely to detect infections during the peak infectious period, effectively identifying those most likely to transmit disease.
A 2022 meta-analysis of 123 publications further quantified this relationship, finding pooled sensitivity of 70.6% for antigen-based POC tests compared to 92.8% for molecular POC tests [30]. The specificity rates were more comparable—98.9% for antigen tests versus 97.6% for molecular POC tests [30]. This specificity makes false positives relatively uncommon, preserving the positive predictive value in appropriate prevalence settings. When disease prevalence is high, the positive predictive value of antigen testing increases, making rapid antigen results particularly useful during peak seasonal outbreaks [29].
Experimental Protocols and Validation Methodologies
Diagnostic Accuracy Studies
Rigorous evaluation of antigen test performance requires standardized comparative studies against reference molecular methods. The following protocol outlines a typical diagnostic accuracy study design:
Study Population and Sample Collection: Consecutive symptomatic patients meeting clinical case definitions (e.g., suspected COVID-19 with respiratory symptoms lasting <7 days) are enrolled. Two combined oro/nasopharyngeal swabs are collected simultaneously by healthcare workers to minimize sampling variability [13]. One swab is placed in viral transport medium for RT-PCR analysis, while the other is placed in a sterile tube for immediate antigen testing [13].
Laboratory Procedures: The antigen test is performed according to manufacturer instructions, with results interpreted within the specified timeframe (typically 15-30 minutes) [13]. To minimize interpretation bias, a single trained operator evaluates all antigen tests, blinded to RT-PCR results. For the reference standard, RT-PCR is performed using validated kits targeting multiple SARS-CoV-2 genes (e.g., N, ORF1a, ORF1b), with Ct values <35 considered positive [13].
Statistical Analysis: Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) are calculated with 95% confidence intervals using 2x2 contingency tables. Correlation between antigen test band intensity and Ct values can be assessed using Pearson correlation tests [13]. Performance stratification by viral load (Ct value ranges), days since symptom onset, and other clinical variables provides additional insights into test characteristics under real-world conditions.
Quantitative Laboratory-Anchored Framework
Emerging methodologies enable more sophisticated antigen test evaluation through quantitative, laboratory-anchored frameworks that link image-based test line intensities to naked-eye limits of detection (LoD) [21]. This approach involves:
Signal Response Characterization: Digital images of antigen test strips are analyzed to calculate normalized signal intensity across dilution series of target recombinant protein and inactivated virus. The signal intensity is modeled using adsorption models like the Langmuir-Freundlich equation: I = kCᵇ/(1 + kCᵇ), where I is normalized signal intensity, C is concentration, k is adsorption constant, and b is an empirical exponent [21].
Visual Detection Thresholds: The statistical characterization of LoD incorporates observer visual acuity by determining the probability density function of the minimal detectable signal intensity across a representative user population [21]. This acknowledges that real-world performance depends on both test strip chemistry and human interpretation capabilities.
Bayesian Predictive Modeling: A Bayesian model integrates the signal response characterization, visual detection thresholds, and Ct-to-viral-load calibration to predict positive percent agreement (PPA) as a continuous function of qRT-PCR Ct values [21]. This methodology enables performance prediction under real-world conditions before large-scale clinical trials, accelerating test deployment during outbreaks.
Figure 1: Antigen Test Evaluation Framework Integrating Laboratory and User Factors
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagents for Antigen Test Development and Evaluation
| Reagent/Material | Function | Specifications |
|---|---|---|
| Recombinant Antigen Proteins | Serve as reference standards for test development and calibration | High-purity target proteins (e.g., SARS-CoV-2 nucleocapsid) at known concentrations [21] |
| Inactivated Virus Stocks | Mimic natural infection for analytical sensitivity determination | Heat-inactivated virus with known concentration (PFU/mL) [21] |
| Clinical Specimens | Validate test performance with real human samples | Combined oro/nasopharyngeal swabs from symptomatic patients [13] |
| Viral Transport Medium (VTM) | Preserve specimen integrity during transport and storage | Compatible with both antigen testing and RT-PCR reference methods [13] |
| Lateral Flow Test Strips | Platform for antigen detection | Nitrocellulose membrane with immobilized capture and control antibodies [21] |
| qRT-PCR Master Mix | Reference standard for comparative studies | Multiplex assays targeting conserved genomic regions (e.g., N, ORF1ab genes) [4] |
| Digital Imaging System | Objective test result quantification | Standardized lighting conditions and resolution for band intensity measurement [21] |
Discussion: Strategic Implementation in Resource-Limited Settings
Context-Appropriate Test Selection
The choice between antigen and molecular testing in RLS requires careful consideration of clinical context, operational constraints, and epidemiological factors. Antigen tests offer the greatest utility in high-prevalence settings where their positive predictive value is maximized, and for rapid screening during outbreaks when immediate isolation decisions are necessary [29]. Their speed and simplicity make them ideal for triage in overcrowded healthcare facilities and for reaching remote communities without access to laboratory infrastructure.
Molecular tests remain preferred when diagnostic accuracy is paramount, particularly in low-prevalence settings, for confirmatory testing, and in high-risk patient populations (immunocompromised, elderly) where false negatives carry severe consequences [29]. The slightly longer turnaround time of POC molecular tests (15-45 minutes) may be acceptable when clinical management depends on definitive results. Emerging multiplex molecular panels that simultaneously detect multiple pathogens from a single sample provide additional value in cases with overlapping clinical presentations [29].
Hybrid Approaches and Future Directions
Strategic testing algorithms can leverage the complementary strengths of both modalities. A hybrid approach using antigen tests for initial screening with reflexive molecular testing for negative results in high-suspicion cases balances speed, cost, and accuracy [29]. This approach maximizes resource utilization by reserving more expensive molecular testing for cases where it provides the greatest clinical value.
Future developments are likely to narrow the performance gap between antigen and molecular testing. Ultrasensitive digital immunoassays are boosting antigen detection to near-PCR levels, while advances in microfluidics and cartridge-based platforms are making molecular testing faster, simpler, and more affordable [29]. The expansion of multiplex respiratory panels in POC formats will enable rapid differentiation between pathogens with similar symptoms, streamlining both diagnosis and treatment. For resource-limited settings, these technological advances promise to enhance diagnostic capabilities while maintaining the operational advantages that make decentralized testing feasible.
Figure 2: Clinical Decision Algorithm for Test Selection in Resource-Limited Settings
In the diagnostic landscape, the choice between rapid antigen tests and polymerase chain reaction tests often presents a trade-off between speed and accuracy. While antigen tests offer rapid results, their variable sensitivity, particularly in low viral load scenarios, establishes the critical role of PCR as the gold standard for confirmatory testing and guiding targeted antiviral therapies. This guide examines the performance data and procedural frameworks that position PCR as an indispensable tool in clinical practice and drug development.
Diagnostic Performance: A Quantitative Comparison
The fundamental difference between antigen and PCR tests lies in their methodology: antigen tests detect specific viral proteins, while PCR amplifies and detects viral genetic material. This distinction underlies a significant gap in sensitivity, which is crucial for reliable diagnosis.
Table 1: Comparative Diagnostic Accuracy of Antigen and PCR Tests
| Test Characteristic | Rapid Antigen Test (Ag-RDT) | PCR Test |
|---|---|---|
| Overall Sensitivity | 59.0% (95% CI: 0.56-0.62) [4] | 92.8% - 97.2% [1] |
| Sensitivity in Symptomatic | 69.3% - 73.0% [4] [5] | >95% [1] |
| Sensitivity in Asymptomatic | 54.7% (95% CI: 47.7-61.6) [5] | >95% [1] |
| Specificity | 99.3% (95% CI: 99.2-99.3) [5] | >99% [1] |
| Impact of Viral Load | Sensitivity drops to <30% at low viral loads [1] | Maintains high sensitivity across viral loads |
The dependency of antigen test accuracy on viral load is a critical limitation. One study demonstrated that while agreement between antigen and PCR results was high (90.85%) for samples with a high viral load, it decreased dramatically to 5.59% for samples with lower viral loads [4]. This performance chasm underscores the necessity of PCR for confirming negative antigen results in high-stakes situations.
Experimental Protocols and Methodologies
Real-World Evaluation of Antigen Test Performance
A large cross-sectional study provides a template for robustly comparing test performances.
- Objective: To determine the real-world accuracy of SARS-CoV-2 antigen tests compared to qPCR within the Brazilian Unified Health System [4].
- Population: 2,882 symptomatic individuals.
- Sample Collection: Two nasopharyngeal swabs were collected simultaneously from each participant [4].
- Testing Protocol: One swab was analyzed immediately using a rapid antigen test kit (with results in 15 minutes). The other swab was stored in Viral Transport Medium at -80°C for subsequent RT-qPCR testing [4].
- Analysis: Statistical analysis determined sensitivity, specificity, accuracy, and positive/negative predictive values. Performance was also analyzed relative to viral load, as indicated by quantification cycle values from the qPCR assay [4].
Broad-Range PCR for Antimicrobial Stewardship
Beyond viral detection, PCR methodologies are pivotal in managing complex bacterial, fungal, and mycobacterial infections.
- Objective: To explore the clinical utility of Broad-Range PCR (BR-PCR) and its impact on antimicrobial treatment in a hospital cohort [31].
- Methodology: This retrospective evaluation analyzed 359 clinical specimens that underwent BR-PCR testing. The technique uses primers targeting conserved genetic regions, such as the 16S ribosomal RNA gene for bacterial identification, allowing for the detection of a wide spectrum of organisms [31].
- Clinical Utility Assessment: Test results were deemed to have "clinical utility" if they led to an adjustment (de-escalation, discontinuation) or confirmation of the initial antimicrobial regimen [31].
PCR in Antiviral Treatment Decision Pathways
The high sensitivity and specificity of PCR make it the cornerstone for initiating and tailoring antiviral therapy, especially for infections where early intervention is critical.
Diagram: PCR's Role in Antiviral Treatment Decisions
Clinical guidelines explicitly recommend PCR-based testing to guide treatment. For novel influenza A viruses, the CDC recommends initiating antiviral treatment "as soon as possible" for patients who are suspected, probable, or confirmed cases, with confirmation relying on molecular methods like RT-PCR [32]. Similarly, the IDSA guidelines for COVID-19 stress the importance of accurate diagnosis to determine disease severity and guide the use of antivirals and immunomodulators [33].
PCR testing is also fundamental in assessing antiviral efficacy in clinical trials and managing treatment. For instance, mathematical modeling of molnupiravir trials revealed that standard PCR assays might underestimate the drug's true potency because they detect mutated viral RNA fragments, highlighting the need for tailored virologic endpoints in trials for mutagenic antivirals [34].
The Scientist's Toolkit: Key Research Reagents
Successful implementation of PCR testing and development relies on a core set of reagents and instruments.
Table 2: Essential Research Reagents for PCR-Based Diagnostics
| Reagent / Instrument | Function | Example Use Case |
|---|---|---|
| Reverse Transcriptase | Converts viral RNA into complementary DNA for amplification. | Essential for detecting RNA viruses like SARS-CoV-2 and Influenza [35]. |
| Taq Polymerase | Thermally stable enzyme that amplifies the target DNA sequence. | Core component of all PCR reactions, including qRT-PCR [35]. |
| Primers & Probes | Short, specific nucleotide sequences that bind to and label the target genetic material. | Designed to target conserved regions of a virus (e.g., CDC 2019-nCoV primers) [4]. |
| Viral Transport Medium | Preserves viral integrity during sample transport and storage. | Used to store nasopharyngeal swabs for batch PCR testing [4]. |
| Nucleic Acid Extraction Kit | Isolates and purifies DNA/RNA from clinical samples. | Automated extraction (e.g., Loccus Extracta 32) prepares samples for PCR [4]. |
| Real-time PCR Instrument | Amplifies DNA and monitors amplification in real-time using fluorescent probes. | Enables quantitative viral load measurement (e.g., Applied Biosystems QuantStudio 5) [4]. |
The evidence clearly delineates the roles of antigen and PCR testing in modern diagnostics. The convenience of antigen tests is counterbalanced by a significant risk of false negatives, especially in asymptomatic individuals or those with low viral loads. PCR remains the undisputed gold standard due to its superior sensitivity and specificity. Its role is critical not only for confirming diagnoses but also for enabling the precise and timely antiviral treatment decisions that improve patient outcomes and advance drug development. As respiratory pathogens continue to pose global health threats, robust, PCR-based diagnostic infrastructure remains a non-negotiable component of an effective clinical and public health response.
The accurate and timely diagnosis of respiratory pathogens such as Influenza A/B and Respiratory Syncytial Virus (RSV) is a cornerstone of effective clinical management and infection control. While much attention has focused on SARS-CoV-2 diagnostics in recent years, establishing the performance characteristics of testing methods for other clinically significant respiratory viruses remains equally crucial for public health. This guide provides a comparative analysis of two fundamental diagnostic approaches—rapid antigen tests (RATs) and polymerase chain reaction (PCR)-based methods—for detecting Influenza A/B and RSV. The emphasis is placed on their relative sensitivities, specificities, and appropriate use cases within clinical and research settings, supported by recent experimental data. The overarching thesis is that while rapid antigen tests offer advantages in speed and convenience, their variable and often lower sensitivity, particularly at low viral loads, necessitates careful result interpretation and often confirmation with more sensitive molecular methods like PCR.
Performance Comparison: Rapid Antigen Tests vs. PCR
The diagnostic performance of RATs and PCR tests for Influenza A/B and RSV has been extensively evaluated in recent studies. The tables below summarize key quantitative metrics, highlighting the consistent pattern of high specificity but variable sensitivity for RATs, contrasted with the consistently high sensitivity and specificity of PCR-based methods.
Table 1: Comparative Performance of Rapid Antigen Tests (RATs) for Respiratory Virus Detection
| Virus | Study Description | Sensitivity Range | Specificity Range | PPV | NPV | Key Factor / Condition |
|---|---|---|---|---|---|---|
| Influenza A | Three RIDTs vs. RT-PCR [36] | 79.8% - 92.4% | 98.8% - 100% | 98.1% - 100% | 86.9% - 94.5% | Test manufacturer |
| Influenza B | Three RIDTs vs. RT-PCR [36] | 73.7% - 92.1% | 100% | 100% | 97.7% - 99.2% | Test manufacturer |
| Influenza A/B | Combined RDT (SARS-CoV-2/Flu/RSV) vs. Rapid NAAT [37] | 54.3% | >99% | - | - | Overall performance |
| Influenza A/B | ML Ag Combo RDT in pediatric settings vs. rRT-qPCR [38] | 71.43% | 100% | 100% | 92.94% | High viral load (Ct < 20) |
| RSV | Combined RDT (SARS-CoV-2/Flu/RSV) vs. Rapid NAAT [37] | 60.0% | >99% | - | - | Overall performance |
| RSV | ML Ag Combo RDT in pediatric settings vs. rRT-qPCR [38] | 90.06% | 98.33% | 93.45% | 97.38% | High viral load (Ct < 20) |
Table 2: Performance of PCR and Rapid Nucleic Acid Amplification Tests (NAATs)
| Test Type | Pathogen | Sensitivity | Specificity | Key Advantage |
|---|---|---|---|---|
| RT-PCR | Influenza A & B | Reference Method [36] | Reference Method [36] | Gold standard for high sensitivity & specificity |
| Rapid NAAT (ID NOW) | Influenza A&B | Significantly higher than RAT [39] | - | Avoids false negatives; enables timely treatment |
| Point-of-Care PCR (GeneXpert) | SARS-CoV-2, Influenza A/B, RSV | 97.2%, >95%, >95% [1] | - | Maintains high sensitivity at low viral loads |
Experimental Insights and Methodologies
Detailed Experimental Protocols
To critically assess the data in the comparison tables, an understanding of the underlying experimental methodologies is essential. The following protocols are representative of the studies cited.
Protocol 1: Multi-Center Evaluation of Rapid Influenza Diagnostic Tests (RIDTs) [36]
- Study Population & Specimen Collection: A prospective, multi-center study enrolled 291 subjects with acute respiratory infections (symptoms ≤7 days). Nasopharyngeal swabs were collected using flocked swabs and transported in viral transport medium.
- Reference Method: Multiplex real-time RT-PCR was performed using the Influenza A/B Nucleic Acid Detection Kit (Shanghai Berger Medical Technology Co. Ltd.). A cycle threshold (Ct) value ≤38 was defined as positive.
- Index Test: Three commercially available RIDTs (colloidal gold-based) from different manufacturers (Jiangsu Shuo Shi, Tianjin Boao Sais, Aibo Biology) were evaluated. Tests were performed per manufacturers' instructions, with results available in 20 minutes.
- Data Analysis: Sensitivity, specificity, PPV, and NPV were calculated against the RT-PCR reference. Statistical analysis included 95% confidence intervals and Cohen's kappa coefficient for agreement.
Protocol 2: Evaluation of a Combined Rapid Antigen Test [37]
- Specimen Collection: Naso-oropharyngeal swabs were collected from 100 symptomatic patients with acute respiratory tract infections and placed in universal transport medium.
- Reference Method: The Xpert Xpress SARS-CoV-2/Flu/RSV plus test (Cepheid), a rapid, multi-target PCR assay, was used as the reference standard. Ct values were used as a semi-quantitative measure of viral load.
- Index Test: The AllTest SARS-CoV-2/IV-A+B/RSV Antigen Combo Rapid Test was performed within 24 hours of collection according to the manufacturer's instructions. Results were read at 10 minutes by two blinded technicians.
- Data Analysis: Sensitivity and specificity were calculated. Receiver operating characteristic (ROC) analysis was performed, and viral loads (Ct values) of concordant and discordant samples were compared using the Mann-Whitney U test.
The Critical Role of Viral Load and Sample Type
A key finding across studies is that the sensitivity of RATs is highly dependent on viral load. The AllTest combo RDT, for example, achieved 100% sensitivity for SARS-CoV-2, Influenza A/B, and RSV in samples with high viral loads (Ct-values ≤ 25), but sensitivity declined significantly at lower viral loads (higher Ct-values) [37]. This relationship explains why RATs can miss a substantial proportion of infections; one review noted that at low viral loads, RAT sensitivities can plummet below 30%, meaning they miss 7 out of 10 infections [1].
Furthermore, the type of specimen collected directly impacts test performance, especially for RATs. One study demonstrated that using nasopharyngeal (NP) swabs for RATs yielded a sensitivity of 58.9%, which dropped dramatically to 10.3% when oropharyngeal (OP) swabs were used. In contrast, PCR showed a much more robust performance with 89.5% agreement between NP and OP swabs [40]. This underscores that NP swabs are the recommended specimen type for RATs to minimize false-negative results.
Research Reagent Solutions
The following table details key reagents and kits used in the cited studies, which are essential for researchers designing similar diagnostic evaluation studies.
Table 3: Key Research Reagents and Kits for Respiratory Virus Detection
| Reagent / Kit Name | Manufacturer | Function / Application |
|---|---|---|
| Influenza A/B Rapid Test Kit (Colloidal Gold) | Jiangsu Shuo Shi Biological Technology Co. Ltd., Tianjin Boao Sais Biotechnology Co. Ltd., Aibo Biology (Hangzhou) Medical Co. Ltd. [36] | Immunochromatographic rapid antigen detection of Influenza A and B viruses. |
| Influenza A/B Nucleic Acid Detection Kit (Fluorescent PCR) | Shanghai Berger Medical Technology Co. Ltd. [36] | Multiplex real-time RT-PCR for gold-standard detection and quantification of Influenza A and B. |
| Xpert Xpress SARS-CoV-2/Flu/RSV plus test | Cepheid [37] | Automated, cartridge-based, rapid molecular test for simultaneous detection of SARS-CoV-2, Influenza A/B, and RSV. |
| AllTest SARS-CoV-2/IV-A+B/RSV Antigen Combo Rapid Test | AllTest Biotech [37] | Combined lateral flow immunoassay for simultaneous, qualitative detection of antigens from SARS-CoV-2, Influenza A/B, and RSV. |
| ID NOW Influenza A&B 2 | Abbott [39] | Rapid, instrument-based, isothermal nucleic acid amplification test (NAAT) for point-of-care detection of Influenza A and B. |
| Wondfo Influenza A and B Antigen Test | Wondfo [40] | Lateral flow immunoassay for rapid antigen detection of Influenza A and B. |
| Universal Transport Medium (UTM) | Copan [37] | For the preservation and transport of viral specimens in nasopharyngeal/oropharyngeal swabs. |
The body of evidence clearly demonstrates a diagnostic performance trade-off. Rapid Antigen Tests (RATs) offer high specificity and speed, making them valuable tools for rapid screening and initial patient triage. A positive RAT result is highly reliable for confirming infection. However, their variable and often modest sensitivity, which is severely compromised at low viral loads and with suboptimal specimen collection, is a major limitation. This leads to a high rate of false negatives, which carries significant risks for clinical management and infection control [1] [37] [40].
In contrast, PCR and rapid NAATs provide superior sensitivity and specificity, maintaining high accuracy across a wide range of viral loads. They are the methods of choice when diagnostic certainty is paramount, such as in hospital settings, for high-risk patients, or when a RAT result is negative but clinical suspicion for influenza or RSV remains high [36] [39].
Therefore, the decision between these tests should be guided by context. RATs are useful for quick, point-of-care answers when prevalence is high and a positive result is likely to be true. In all other scenarios, particularly when ruling out infection is critical, molecular methods like PCR are the more reliable choice. For clinical and research purposes, negative RAT results should be interpreted with caution and confirmed with a PCR test, especially during peak respiratory virus seasons.
The emergence of SARS-CoV-2 created an unprecedented global demand for reliable, scalable, and rapid diagnostic testing. From the pandemic's onset, two principal testing methodologies emerged with complementary characteristics: nucleic acid amplification tests (primarily RT-PCR) and rapid antigen tests (RATs). Reverse transcription-polymerase chain reaction (RT-PCR) represents the gold standard for sensitivity, detecting minute quantities of viral RNA through enzymatic amplification. In contrast, rapid antigen tests (RATs) identify viral proteins through immunoassay formats, offering rapid results and point-of-care deployment but typically with reduced sensitivity. This creates a fundamental trade-off between diagnostic accuracy and operational practicality that continues to challenge public health strategies and clinical decision-making.
The core dilemma facing researchers and clinicians lies in balancing the superior analytical performance of laboratory-based molecular methods against the operational advantages of rapid antigen detection platforms. This cost-benefit analysis extends beyond mere financial considerations to encompass temporal, logistical, and clinical dimensions that collectively determine the optimal testing approach for specific scenarios. Understanding this balance is particularly crucial for drug development professionals and researchers designing clinical trials, where accurate participant screening and monitoring directly impact study validity and therapeutic assessment.
Performance Metrics: Comparative Data Analysis
Extensive evaluation across multiple studies has established clear performance patterns for both testing modalities. The table below summarizes key performance metrics from recent systematic reviews and comparative studies:
Table 1: Overall Diagnostic Performance of RT-PCR vs. Rapid Antigen Tests
| Test Characteristic | RT-PCR | Rapid Antigen Tests | Primary Sources |
|---|---|---|---|
| Pooled Sensitivity | ~80% (clinical context) [3] | 69.3% (95% CI: 66.2-72.3%) [5] | Cochrane Review (2023) |
| Pooled Specificity | 98-99% [3] | 99.3% (95% CI: 99.2-99.3%) [5] | Cochrane Review (2023) |
| Analytical Sensitivity | 500-5000 copies/mL [3] | Varies by brand; significantly lower than RT-PCR | CAP Review (2022) |
| Time to Result | 24-48 hours (including transport) | 15-30 minutes [41] [13] | Multiple studies |
A 2022 meta-analysis of 60 studies confirmed these findings, reporting RAT sensitivity of 69% (95% CI: 68-70) and specificity of 99% (95% CI: 99-99) when using RT-PCR as the reference standard [42]. The diagnostic odds ratio was 316 (95% CI: 167-590), indicating strong overall discriminatory power despite the sensitivity limitations [42].
Impact of Clinical and Virological Factors
Test performance varies substantially based on clinical presentation and viral load. The following table summarizes how these factors affect antigen test sensitivity:
Table 2: Factors Influencing Rapid Antigen Test Sensitivity
| Factor | Sensitivity Impact | Evidence Source |
|---|---|---|
| Symptom Status | 73.0% (symptomatic) vs. 54.7% (asymptomatic) [5] | Cochrane Review (2023) |
| Viral Load (Ct value) | 100% (Ct <25) vs. 31.8-47.8% (Ct >30) [15] [13] | Multiple studies |
| Symptom Duration | 80.9% (≤7 days) vs. 53.8% (>7 days) [5] | Cochrane Review (2023) |
| Variant Type | 100% (Omicron) vs. 78.9-83.3% (Alpha/Delta) [15] | Comparative Study (2024) |
A 2024 comparative evaluation of RT-PCR and antigen tests demonstrated that both fluorescence immunoassay (FIA) and lateral flow immunoassay (LFIA) formats achieved 100% sensitivity at low Ct values (<25), confirming their strong correlation with high viral loads [15]. This relationship is crucial because higher viral loads typically correlate with greater transmissibility, meaning antigen tests effectively identify the most infectious individuals [43].
Experimental Protocols and Methodologies
Standardized Evaluation Framework
Recent comparative studies have employed rigorous methodologies to directly assess test performance. The following experimental workflow illustrates a standardized approach for comparative diagnostic evaluation:
Diagram 1: Diagnostic Evaluation Workflow
Detailed Methodological Approaches
Sample Collection and Handling
In a 2024 comparative study, researchers collected 268 samples tested simultaneously for SARS-CoV-2 using RT-PCR and two antigen detection methods: fluorescence immunoassay (FIA) and lateral flow immunoassay (LFIA) [15]. The standardized collection protocol involved:
- Simultaneous swab collection for all testing modalities to eliminate biological variation
- Viral transport media for RT-PCR samples maintained at 4°C during transport
- Direct processing for antigen tests without specialized transport media
- Viral load quantification via cycle threshold (Ct) values with variant identification using PCR-based assay
This approach minimized pre-analytical variables and enabled direct comparison between methodologies [15].
Laboratory Analysis Procedures
The RT-PCR methodology typically followed this sequence:
- RNA extraction using commercial kits (e.g., Mag-Bind Viral DNA/RNA 96 kit)
- Amplification and detection with approved platforms (e.g., Hologic Panther Fusion, cobas6800)
- Cycle threshold determination with values ≤40 considered positive
- Variant identification through targeted PCR assays for spike protein mutations
For antigen tests, the process was significantly streamlined:
- Direct application of sample to test device
- Lateral flow incubation for 15-30 minutes
- Visual or instrumental readout without specialized equipment
- Result interpretation according to manufacturer guidelines
The 2023 Monaco study exemplified this approach, utilizing the Elecsys SARS-CoV-2 Antigen test on the cobas e801 platform for automated antigen detection, demonstrating how high-throughput antigen testing could be scaled [44].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SARS-CoV-2 Test Evaluation
| Reagent/Kit | Function | Application in Studies |
|---|---|---|
| Viral Transport Media | Preserves sample integrity during transport | Essential for RT-PCR sample stability [41] |
| RNA Extraction Kits | Isolates viral nucleic acid | Critical pre-analytical step for RT-PCR [41] |
| RT-PCR Master Mix | Enzymatic amplification of target sequences | Detects SARS-CoV-2 with high sensitivity [15] |
| Antigen Test Devices | Lateral flow immunoassay platforms | Point-of-care detection (e.g., SD Biosensor) [41] |
| Viral Culture Systems | Propagates infectious virus | Determines correlation with infectivity [43] |
Cost-Benefit Analysis Framework
Operational and Economic Considerations
The fundamental trade-offs between RT-PCR and rapid antigen tests extend beyond raw performance metrics to encompass practical implementation factors:
Diagram 2: Diagnostic Decision Pathways
Clinical and Public Health Implications
The operational characteristics of each testing modality directly impact their appropriate use cases:
Table 4: Use Case Scenarios for SARS-CoV-2 Testing Modalities
| Scenario | Recommended Test | Rationale | Evidence |
|---|---|---|---|
| Symptomatic Individuals | RT-PCR preferred; RAT acceptable with high prevalence | Maximizes detection; RAT adequate with high pretest probability | [5] |
| Asymptomatic Screening | RT-PCR; RAT only with known exposure | Lower sensitivity of RAT problematic without symptoms | [5] |
| High-Risk Settings | RT-PCR for confirmation | Essential for patients eligible for antiviral therapy | [43] |
| Resource-Limited Settings | RAT as first-line | Practical despite sensitivity limitations | [41] |
| Mass Testing Campaigns | RAT for scalability | Enables widespread testing despite performance trade-offs | [41] |
Recent CDC guidance based on 2022-2023 data emphasizes that while "antigen tests continue to detect potentially transmissible infection," clinicians should "consider RT-PCR testing for persons for whom antiviral treatment is recommended" due to the higher sensitivity [43]. This reflects the risk-stratified approach to test selection that has emerged as the standard of care.
The cost-benefit analysis between RT-PCR and rapid antigen testing reveals a consistent pattern: operational advantages come with diagnostic compromises. RT-PCR remains the unchallenged reference for clinical diagnosis when sensitivity is paramount, particularly for vulnerable populations and treatment decisions. Rapid antigen tests, while less sensitive, provide unparalleled speed and accessibility that make them indispensable for public health screening and rapid case identification.
For researchers and drug development professionals, these findings have significant implications. Clinical trial designs must consider the testing modality when enrolling participants or evaluating outcomes, as antigen testing may miss early infections or create false-negative endpoints. Diagnostic manufacturers should focus on improving antigen test sensitivity without sacrificing the core advantages of speed and simplicity, perhaps through novel detection technologies or signal amplification methods.
Future research should prioritize standardized evaluation frameworks that account for emerging variants, diverse populations, and novel testing platforms. The optimal balance between turnaround time and diagnostic accuracy continues to evolve alongside the virus itself, requiring ongoing reassessment of this critical trade-off in both clinical and public health contexts.
Mitigating Diagnostic Limitations: Strategies to Enhance Antigen Test Reliability
This guide provides a comparative analysis of Antigen Tests (Ag-RDTs) and reverse transcription–polymerase chain reaction (RT-PCR) tests, focusing on how sampling strategies critically influence diagnostic yield. The sensitivity of these tests is not static but is profoundly affected by timing relative to symptom onset, viral load in the sample, and the specific variant being detected. The following table summarizes key performance differentiators essential for research and development.
| Performance Characteristic | Antigen Tests (Ag-RDTs) | RT-PCR Tests |
|---|---|---|
| Overall Sensitivity | 47% (compared to RT-PCR) [43] | 100% (reference standard) [15] |
| Sensitivity in High Viral Load (Ct < 25) | ~100% [15] | 100% |
| Sensitivity in Low Viral Load (Ct > 30) | 27-32% [15] | 100% |
| Asymptomatic Case Sensitivity | Lower; FIA shows 73.68% vs. LFIA 65.79% [15] | 100% |
| Variant Specificity | 100% for Omicron; lower for Alpha & Delta [15] | Not significantly affected |
| Time-to-Peak Detection | Peak positive percentage (59%) at 3 days post-symptom onset [43] | Peak positive percentage (83%) at 3 days post-symptom onset [43] |
| Key Strength | Correlates highly with culturable virus (80% sensitivity); ideal for identifying transmissible infection [43] | High sensitivity; detects viral fragments; essential for definitive diagnosis and antiviral treatment initiation [43] |
The accuracy of any diagnostic test is contingent not only on its technological principles but also on the sample it processes. A test's reported sensitivity and specificity are mean values, yet its true performance is dynamic, varying with the context of the sample collected. For SARS-CoV-2, this context includes the patient's viral load, which fluctuates predictably over the course of infection, and the physical characteristics of the sample itself [21]. This guide delves into the experimental data that quantify how timing, technique, and sample type impact the yield of SARS-CoV-2 antigen and PCR tests, providing a framework for researchers to optimize diagnostic protocols and interpret results accurately within the broader thesis of test sensitivity and specificity.
Comparative Test Performance: A Detailed Data Analysis
Performance Relative to Viral Load
The most significant factor affecting antigen test sensitivity is the viral load in the sample, typically inversely measured by RT-PCR Cycle Threshold (Ct) values. A lower Ct value indicates a higher viral load.
Table 2.1: Antigen Test Sensitivity vs. Viral Load (Ct Values)
| Cycle Threshold (Ct) Range | Viral Load Category | Antigen Test Sensitivity (FIA) | Antigen Test Sensitivity (LFIA) |
|---|---|---|---|
| < 25 | High | 100% [15] | 100% [15] |
| 25 - 30 | Medium | Data not available in search results | Data not available in search results |
| > 30 | Low | 31.82% [15] | 27.27% [15] |
Abbreviations: FIA (Fluorescence Immunoassay), LFIA (Lateral Flow Immunoassay).
This data underscores that antigen tests excel at identifying individuals with high viral loads, who are most likely to be contagious. However, their utility is limited in detecting early incubation or late convalescent phases of infection where viral load is lower [15] [43].
Performance Relative to Symptom Status and Timing
The progression of infection and the immune response create a dynamic diagnostic window. One study measuring daily test performance found that the percentage of positive antigen tests peaks at 59.0% three days after symptom onset, which lags behind the peak of culturable virus (52% at two days post-onset) [43]. The presence of symptoms, particularly systemic ones like fever, is a strong indicator of higher viral loads and, consequently, better antigen test performance.
Table 2.2: Antigen Test Sensitivity Based on Clinical Presentation
| Symptom Status on Day of Test | Sensitivity vs. RT-PCR | Sensitivity vs. Viral Culture |
|---|---|---|
| Any COVID-19 Symptom | 56% [43] | 85% [43] |
| Fever Reported | 77% [43] | 94% [43] |
| No Symptoms Reported | 18% [43] | 45% [43] |
Experimental Protocols: Key Studies and Methodologies
Protocol 1: Comparative Evaluation of RT-PCR and Ag-RDTs
This protocol is designed to directly compare the performance of different diagnostic modalities against a gold standard.
- Objective: To compare the performance, variant specificity, and clinical implications of RT-PCR versus antigen-based rapid diagnostic tests (Ag-RDTs) for SARS-CoV-2 detection [15].
- Sample Collection: A total of 268 samples were collected for simultaneous testing with RT-PCR and two types of Ag-RDTs (FIA and LFIA) [15].
- Reference Testing: RT-PCR was performed to confirm the presence of SARS-CoV-2 RNA and to determine the viral load via Cycle Threshold (Ct) values. Variant identification was conducted using a PCR-based assay [15].
- Antigen Testing: Each sample was tested using both FIA and LFIA platforms according to manufacturers' instructions. Results were interpreted and recorded.
- Data Analysis: Diagnostic performance metrics (sensitivity, specificity, PPV, NPV) for the Ag-RDTs were calculated using the RT-PCR results as the reference. Sensitivity was further stratified by Ct value range and viral variant [15].
Protocol 2: A Laboratory-Anchored Framework for Antigen Test Performance
This methodology uses a quantitative, model-based approach to predict real-world test performance without requiring large initial clinical trials.
- Objective: To present a quantitative framework linking laboratory measurements to the probabilistic prediction of Positive Percent Agreement (PPA) as a function of viral load [21].
- Signal Response Characterization: The test's signal intensity is quantitatively evaluated across a dilution series of the target recombinant protein and inactivated virus. A Langmuir-Freundlich adsorption model is fitted to the data to describe the relationship between signal intensity and analyte concentration [21].
- Limit of Detection (LoD) Characterization: The visual acuity of the intended user population is characterized statistically. This involves determining the probability density function of the naked-eye limit of detection in the signal-intensity domain [21].
- Gold Standard Calibration: A calibration curve is established to link qRT-PCR Ct values to viral concentration [21].
- Predictive Modeling: A Bayesian-based predictive model integrates the signal-to-concentration model, the user LoD distribution, and the Ct-to-viral-load calibration. This model outputs a PPA-vs-Ct curve, forecasting the test's sensitivity across a spectrum of viral loads [21].
Optimizing Sampling Strategy: Timing, Technique, and Sample Type
The Critical Impact of Timing
The timing of sample collection is paramount for accurate detection, especially for antigen tests. As viral load rises and falls during infection, so does the probability of detection. The following diagram illustrates the dynamic window of detection for each test type relative to symptom onset and culturable virus.
General Sampling Technique Considerations
Beyond virological timing, the physical sampling technique is crucial. While the provided search results focus on virological factors, principles from other fields like histopathology are instructive. In lung cancer diagnosis, for example, obtaining sufficient tissue is critical for accurate subtyping and molecular testing [45]. Key considerations include:
- Sample Adequacy: Small biopsy samples may have low percentages of tumor cells, complicating diagnosis and advanced testing. Similarly, a nasopharyngeal swab with insufficient cellular material will yield a false negative regardless of test sensitivity [45].
- Handling and Storage: Proper handling of samples immediately after collection is vital to prevent degradation of proteins (for antigen tests) or nucleic acids (for PCR), which directly impacts test yield [46].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials used in the development and optimization of diagnostic tests, as referenced in the studies.
Table 5: Key Research Reagent Solutions
| Reagent / Material | Function in Research & Development |
|---|---|
| Recombinant Viral Protein | Used to generate standard curves for characterizing the signal response and analytical sensitivity of antigen tests without handling live virus [21]. |
| Inactivated Virus | Provides a safe and stable material for determining the Limit of Detection (LoD) and evaluating test performance across variants in a laboratory setting [21]. |
| HotStart PCR Master Mix | A specialized PCR reagent that reduces non-specific amplification and false positives by inhibiting polymerase activity at low temperatures, thereby improving assay specificity and yield [46]. |
| Viral Transport Media (VTM) | A stabilizing solution that preserves the integrity of viral particles and/or nucleic acids in patient samples (e.g., nasopharyngeal swabs) during transport and storage before laboratory testing [43]. |
| Monoclonal Antibodies | Critical components of immunoassays; these highly specific antibodies are used as capture and detection agents in antigen test kits to bind to target viral proteins [47]. |
The utilization of rapid antigen tests (Ag-RDTs) has become a cornerstone in the management and containment of respiratory infectious diseases, most notably COVID-19. These tests offer significant advantages, including a short turnaround time (typically 15-30 minutes), ease of use, and the ability to be deployed at the point-of-care without requiring sophisticated laboratory infrastructure [22] [48]. However, a critical limitation hampers their diagnostic efficacy: inferior sensitivity when compared to molecular reference standards like nucleic acid amplification tests (NAAT), including reverse transcription-polymerase chain reaction (RT-PCR) [22] [1]. This lower sensitivity, particularly in single-test applications, results in a higher rate of false-negative results, which can undermine public health efforts by failing to identify and isolate infectious individuals.
The core of this challenge lies in the fundamental design of antigen tests. Unlike molecular tests that amplify and detect viral RNA, antigen tests are immunoassays designed to detect specific viral proteins, typically the nucleocapsid (N) protein of SARS-CoV-2 [48]. Their performance is intrinsically linked to viral load. As noted by the Infectious Diseases Society of America (IDSA), the pooled Ag test sensitivity is 81% for symptomatic individuals but drops precipitously to 54% when testing occurs more than five days after symptom onset, and is only 63% in asymptomatic individuals [22]. This is because antigen tests are most reliable when the viral antigen concentration in the specimen is high, a state most commonly found during the peak of infection. A recent review in Microorganisms highlighted that at low viral loads, Ag-RDTs can show sensitivities below 30%, meaning they could miss nearly 7 out of 10 infections with low viral loads [1]. This performance characteristic poses a significant risk in clinical and public health settings, as a single negative antigen test cannot reliably rule out an active infection.
To mitigate this limitation, serial testing protocols—the practice of repeating antigen tests over a defined period—have been advocated by health authorities and professional societies. This article provides a comparative analysis of serial antigen testing against single-test applications and alternative molecular diagnostics. It objectively examines the experimental data supporting this strategy, details the underlying methodologies, and discusses its implications within the broader context of diagnostic test sensitivity and specificity for researchers and drug development professionals.
Performance Data: Quantitative Comparison of Testing Strategies
The diagnostic performance of SARS-CoV-2 tests varies significantly based on the testing strategy employed, the population tested, and the viral load present. The following tables synthesize quantitative data from recent studies to facilitate a clear comparison.
Table 1: Performance Characteristics of Single Antigen Tests vs. RT-PCR
| Testing Scenario | Sensitivity | Specificity | Key Study Findings |
|---|---|---|---|
| Symptomatic Individuals (Overall) | 81% (95% CI: 78-84%) [22] | ≥99% [22] | Performance is highest early in infection. |
| Symptomatic (0-5 days post-onset) | 89% (95% CI: 83-93%) [22] | ≥99% [22] | Sensitivity peaks within the first week of symptoms. |
| Symptomatic (>5 days post-onset) | 54% [22] | ≥99% [22] | Sensitivity declines markedly after the first week. |
| Asymptomatic Individuals | 63% [22] | ≥99% [22] | Lower sensitivity due to generally lower viral loads. |
| Real-World Study (Symptomatic) | 59% (95% CI: 56-62%) [4] | 99% (95% CI: 98-99%) [4] | Highlights variability in real-world vs. controlled settings. |
| High Viral Load (Cq <20) | >90% [4] | >99% [4] | Antigen tests are highly accurate when viral load is high. |
| Low Viral Load (Cq ≥33) | 5.59% [4] | >99% [4] | Performance drops drastically at low viral loads. |
Table 2: Comparison of Antigen Tests and Molecular Tests
| Parameter | Rapid Antigen Tests (Ag-RDTs) | Molecular Tests (RT-PCR/NAAT) |
|---|---|---|
| Target Analyte | Viral proteins (e.g., N protein) [48] | Viral RNA [49] |
| Sensitivity | Low to moderate [22] | High [49] |
| Specificity | High (≥99%) [22] | High [49] |
| Turnaround Time | 15-30 minutes [48] | 15 minutes to several days [49] |
| Test Complexity & Cost | Low complexity, low cost [22] | Variable to high complexity, moderate cost [49] |
| Point-of-Care Use | Yes [22] | Most formats are not, though some are allowed [49] |
| Best Correlate of Infectivity | Better correlate of culturable virus [50] | Detects non-viable virus and viral fragments [49] |
The data reveal a clear trend: the sensitivity of a single antigen test is unacceptably low for ruling out infection, particularly in asymptomatic individuals or those with low viral loads. A large real-world cross-sectional study in Brazil of 2,882 symptomatic individuals further reinforced this, showing an overall antigen test sensitivity of only 59% compared to RT-PCR. The study crucially demonstrated that test agreement with RT-PCR was 90.85% for samples with a high viral load (Cq < 20) but plummeted to 5.59% for samples with a low viral load (Cq ≥ 33) [4]. This underscores that the primary weakness of antigen tests is their failure to detect pre-infectious or late-stage infections with low viral burden.
The Serial Testing Solution: Protocols and Experimental Evidence
The rationale for serial testing is rooted in the natural history of viral infection. An individual's viral load is not static; it rises during the incubation and prodromal phases, peaks around symptom onset, and then gradually declines. A single antigen test, if performed during the ascending or trailing edge of this viral load curve, may return a false negative. By testing repeatedly over 24-48 hour intervals, the probability of capturing the individual during their period of peak viral load—and thus obtaining a true positive result—increases substantially [22].
Recommended Serial Testing Protocols
Based on empirical data and modeling studies, public health bodies have formalized specific serial testing recommendations:
- For Symptomatic Individuals: The IDSA guidelines, while noting a lack of direct empirical data, acknowledge modeling that suggests repeat testing increases sensitivity. The U.S. Food and Drug Administration (FDA) has recommended that symptomatic individuals test twice over 48 hours with at least two antigen tests [22].
- For Asymptomatic Individuals: The FDA recommends testing at least three times over 48-hour intervals with antigen tests. This more frequent protocol is designed to compensate for the unknown timing of infection and the typically lower viral loads in asymptomatic cases [22].
Experimental Workflow for Serial Testing Validation
The following diagram illustrates a generalized experimental protocol for validating a serial antigen testing strategy against a gold-standard molecular test.
This workflow is foundational for generating the performance data presented in the previous section. Researchers typically collect paired swabs from participants—one for immediate antigen testing and another in viral transport medium for confirmatory RT-PCR analysis. The antigen test is then repeated according to the protocol under investigation (e.g., at 48 and 96 hours). All results are compared to the RT-PCR benchmark to determine the sensitivity and specificity of the single test versus the serial testing algorithm.
Research Reagent Solutions and Essential Materials
To execute the serial testing protocols and related research, scientists rely on a suite of specific reagents and materials. The table below details key components used in the featured studies.
Table 3: Key Research Reagent Solutions for Antigen and Molecular Testing
| Reagent / Material | Function / Description | Example Use in Cited Studies |
|---|---|---|
| Viral Transport Medium (VTM) | Preserves viral integrity for transport and subsequent RNA extraction for RT-PCR. | Used to store nasopharyngeal swabs at -80°C prior to RT-PCR analysis [4]. |
| Automated Nucleic Acid Extractor | Automates the purification of viral RNA from patient samples, ensuring consistency and throughput. | Loccus Extracta 32 system was used with a Viral RNA kit for extraction [4]. |
| RT-PCR Master Mix | Contains enzymes, dNTPs, and buffers for the reverse transcription and amplification of viral RNA. | GoTaq Probe 1-Step RT-qPCR system (Promega) used on a QuantStudio 5 instrument [4]. |
| SARS-CoV-2 Primers/Probes | Target specific viral genes (e.g., N, ORF1a, ORF1b, S); bind to and mark viral sequences for detection. | CDC's real-time RT-PCR protocol targeting N gene etc. was utilized [4]. |
| Lateral Flow Immunoassay Cartridge | The device containing the nitrocellulose membrane and reagents for the antigen test. | Commercial tests like Abbott Panbio, Qiagen mö-screen, TR DPP, IBMP TR Covid Ag kit [4] [50] [13]. |
| Monoclonal/Polyclonal Antibodies | Core component of antigen tests; specifically bind to viral target proteins (e.g., N protein). | Target immunodominant epitopes of the N protein; performance can be affected by mutations [48] [50]. |
Limitations and Emerging Challenges in Antigen Testing
Despite the benefits of serial testing, several important limitations must be considered by researchers and clinicians. First, the performance of antigen tests is not uniform across all commercially available products. The Brazilian real-world study found a significant difference between two widely used tests, with one (IBMP TR Covid Ag kit) showing a sensitivity of 70% and the other (TR DPP COVID-19) a sensitivity of only 49% [4]. This highlights that the success of a serial testing protocol is contingent upon the intrinsic analytical performance of the specific test kit used.
A more profound challenge is the emergence of antigen test target failure. A hospital surveillance study in Italy identified SARS-CoV-2 variants characterized by multiple disruptive amino-acid substitutions in the N protein. These mutations, occurring in immunodominant epitopes that function as the target for capture antibodies in antigen tests, led to false-negative antigen results even in samples with high viral loads (low Cq values) [50]. The study fitted a multi-strain model to epidemiological data and concluded that the increased reliance on antigen testing in one Italian region, compared to the rest of the country, likely favored the undetected spread of this antigen-escape variant [50]. This finding underscores a critical risk: widespread antigen testing in the absence of complementary molecular testing for surveillance can create a blind spot, allowing variants with mutations in the target protein to circulate undetected.
Finally, the positive predictive value (PPV) of antigen tests is highly dependent on disease prevalence. In low-prevalence settings, even a test with high specificity can have a suboptimal PPV, leading to a higher proportion of false positives. As one study noted, at a prevalence of 0.1%, the PPV of an antigen test can be below 50% [50]. This necessitates confirmatory molecular testing for positive results in low-prevalence environments, a nuance that must be factored into public health testing algorithms.
Serial antigen testing protocols represent a pragmatic and evidence-based strategy to mitigate the fundamental limitation of single antigen tests: poor sensitivity, particularly at low viral loads. The data are clear that while a single negative antigen test is insufficient to rule out infection, repeated testing at 24- to 48-hour intervals significantly increases the probability of detecting the virus during the window of high viral load, thereby improving overall diagnostic sensitivity.
For researchers and public health officials, the implications are twofold. First, the implementation of antigen testing must be strategically designed, with serial protocols tailored to the population (symptomatic vs. asymptomatic). Second, the reliance on antigen tests should not come at the expense of robust molecular surveillance. The potential for antigenic escape variants, as documented, necessitates the ongoing use of RT-PCR not only for confirmatory diagnosis but also for genomic monitoring. The future of diagnostic preparedness lies in a balanced, multi-modal approach that leverages the speed and accessibility of serial antigen testing for rapid isolation and containment, while relying on the sensitivity and precision of molecular assays for confirmation, surveillance, and the early detection of novel viral variants.
The diagnosis of SARS-CoV-2 infection remains a critical component of public health and clinical management throughout the COVID-19 pandemic. While reverse transcription-polymerase chain reaction (RT-PCR) stands as the reference method for detection, antigen-detection rapid diagnostic tests (Ag-RDTs) have emerged as a vital tool due to their rapid turnaround time, cost-effectiveness, and point-of-care applicability [4] [42]. A critical understanding has emerged that the accuracy of these rapid tests is not static but is significantly influenced by clinical context, particularly the patient's symptomatology and the timing of test administration relative to symptom onset.
This guide objectively compares the performance of antigen tests against PCR, framing the analysis within the broader thesis that clinical presentation is a fundamental variable for interpreting Ag-RDT results. We synthesize experimental data to provide researchers and drug development professionals with a evidence-based framework for evaluating test performance under varying clinical conditions.
The foundational difference between antigen and PCR tests lies in their detection targets: Ag-RDTs identify specific viral proteins, while PCR amplifies and detects viral RNA. This distinction explains the general consensus that PCR is more sensitive, but it fails to capture the nuanced relationship between antigen test performance and clinical status [42] [22].
A large-scale meta-analysis of 60 studies confirmed that the pooled sensitivity of rapid antigen tests was 69% (95% CI: 68–70) compared to RT-PCR, while specificity was notably high at 99% (95% CI: 99–99) [42]. This high specificity means that a positive antigen result is highly reliable and can typically be acted upon without PCR confirmation in most settings [22].
Table 1: Overall Diagnostic Accuracy of Rapid Antigen Tests vs. RT-PCR
| Metric | Estimate | Certainty/Context |
|---|---|---|
| Pooled Sensitivity | 69% (95% CI: 68–70) [42] | Compared to RT-PCR |
| Pooled Specificity | 99% (95% CI: 99–99) [42] | Compared to RT-PCR |
| Diagnostic Odds Ratio (DOR) | 316 (95% CI: 167–590) [42] | Random-effects model |
| Area Under the Curve (AUC) | 97% [42] | Summary Receiver Operating Characteristic (SROC) curve |
However, these overall figures mask critical variations. Performance is substantially different in symptomatic versus asymptomatic individuals and is heavily dependent on the timing of the test.
Table 2: Antigen Test Performance in Symptomatic vs. Asymptomatic Individuals
| Population | Sensitivity | Specificity | Key Determinants |
|---|---|---|---|
| Symptomatic | 81% (95% CI: 78% to 84%) [22] | ≥99% [22] | Timing post-symptom onset; viral load |
| Asymptomatic | 63% [22] | ≥99% [22] | Generally lower viral loads |
The Critical Role of Symptom Status and Timing
The Symptom-Onset Timeline
The relationship between symptom onset and antigen test sensitivity is a cornerstone of accurate interpretation. The Infectious Diseases Society of America (IDSA) guidelines highlight that sensitivity is highest when testing is performed early in the symptomatic phase [22].
- Optimal Window (0-5 Days Post-Symptom Onset): Pooled Ag test sensitivity reaches 89% (95% CI: 83% to 93%) within the first five days of illness, when viral loads are typically at their peak [22].
- After Day 5: Sensitivity plummets to approximately 54% as the active replication phase subsides and viral load decreases [22].
- Peak Infectiousness Correlation: A 2024 CDC study using viral culture as a measure of infectiousness found antigen test sensitivity was 80% (95% CI: 76%–85%) compared to culture, and was highest around the time of peak culture positivity (2-3 days after symptom onset) [43].
The Viral Load Connection
The primary driver behind the timing effect is viral load, which is highest in the early symptomatic phase. Antigen test performance shows a strong inverse correlation with RT-PCR cycle threshold (Ct) values, a common proxy for viral load [4] [51].
A Brazilian cross-sectional study of 2,882 symptomatic individuals found that agreement between antigen tests and RT-PCR was 90.85% for samples with a low Cq (quantification cycle) < 20 (indicating high viral load), but dropped drastically to 5.59% for samples with Cq ≥ 33 (indicating low viral load) [4]. A study of the mö-screen Corona Antigen Test demonstrated a correlation coefficient of -0.706 (p<0.001) between antigen test band intensity and Ct values, confirming that stronger positive signals are associated with higher viral loads [51] [13].
Experimental Data and Protocols
Key Studies and Their Methodologies
Large-Scale Real-World Accuracy Study (Brazil)
- Objective: To evaluate the real-world accuracy of two Ag-RDT kits widely used within the Brazilian Unified Health System compared to qPCR [4].
- Population: 2,882 symptomatic individuals aged ≥12 years presenting with COVID-19 suggestive symptoms.
- Specimen Collection: Two nasopharyngeal swabs collected simultaneously from each participant. One was analyzed immediately with the Ag-RDT, the other stored in Viral Transport Medium at -80°C for RT-PCR testing [4].
- RT-PCR Protocol: RNA extraction was automated (Extracta 32, Loccus Biotecnologia). SARS-CoV-2 detection used the CDC's real-time RT-PCR diagnostic protocol on the QuantStudio 5 instrument (Applied Biosystems) with the GoTaq Probe 1-Step RT-qPCR system (Promega) [4].
- Key Findings: Overall sensitivity (59%), specificity (99%), and accuracy (82%) varied significantly by manufacturer and was strongly dependent on viral load [4].
Household Transmission Study (CDC, 2022-2023)
- Objective: To reevaluate Ag test performance compared to RT-PCR and viral culture during a period of increased population immunity and Omicron variant circulation [43].
- Design: Case-ascertained household transmission study where participants completed daily symptom diaries and collected two nasal swabs daily for 10 days.
- Testing: One swab was used for at-home antigen testing (result self-reported), the other was tested in the lab via automated RT-PCR (Hologic Panther Fusion) and viral culture [43].
- Key Findings: Overall Ag test sensitivity was 47% compared to RT-PCR but 80% compared to viral culture. Sensitivity was highest on days with fever (77% vs. RT-PCR; 94% vs. culture) [43].
Optimal Performance Validation Study (Turkey)
- Objective: To compare the diagnostic accuracy of the mö-screen Corona Antigen Test (Qiagen) with RT-PCR in symptomatic patients [51] [13].
- Population: 200 symptomatic patients with duration of symptoms less than one week.
- Specimen Collection: Two combined oro/nasopharyngeal swabs collected simultaneously by healthcare workers. One placed in viral nucleic acid transport medium for PCR, the other in a sterile tube for antigen testing.
- Testing: Antigen testing followed manufacturer instructions. RT-PCR used the Biospeedy SARS-CoV-2 RT-PCR kit (targeting N, ORF 1a, ORF 1b genes) on a Rotor-Gene (Qiagen) instrument. Ct<35 was positive [51] [13].
- Key Findings: Reported 100% sensitivity and specificity, attributed to combined swab sampling and early symptom phase testing. Found strong correlation (r=-0.706, p<0.001) between antigen band intensity and Ct values [51] [13].
Table 3: Comparative Experimental Data from Key Studies
| Study / Characteristic | Real-World Brazil Study [4] | CDC Household Study [43] | Mö-Screen Validation [51] [13] |
|---|---|---|---|
| Study Design | Cross-sectional | Daily longitudinal, household transmission | Diagnostic accuracy |
| Participant Number | 2,882 | 236 RT-PCR+ | 200 |
| Symptom Status | Symptomatic | Symptomatic & Asymptomatic | Symptomatic (<7 days) |
| Specimen Type | Nasopharyngeal | Nasal | Combined Oro/Nasopharyngeal |
| Reference Standard | RT-PCR (CDC protocol) | RT-PCR & Viral Culture | RT-PCR (Biospeedy kit) |
| Overall Ag Sensitivity | 59% | 47% (vs. RT-PCR), 80% (vs. culture) | 100% |
| Overall Ag Specificity | 99% | Not explicitly stated, but high | 100% |
| Key Correlation | High viral load (Cq<20): 90.85% agreement | Higher sensitivity on fever days | Ct value vs. Ag result (r=-0.706) |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Research Reagent Solutions for Antigen Test Performance Studies
| Item | Function/Description | Example Brands/Types (from cited studies) |
|---|---|---|
| Ag-RDT Kits | Immunochromatographic tests detecting SARS-CoV-2 nucleocapsid protein. | TR DPP COVID-19 Ag (Bio-Manguinhos), IBMP TR Covid Ag kit, mö-screen Corona Antigen Test (Qiagen), Standard Q COVID-19 Ag, Panbio [4] [42] [52] |
| RT-PCR Kits | Gold-standard nucleic acid amplification for detection of SARS-CoV-2 RNA. | CDC 2019-nCoV RT-PCR Diagnostic Panel, Biospeedy SARS-CoV-2 RT-PCR Test (targets N, ORF1a, ORF1b) [4] [51] |
| Viral Transport Medium (VTM) | Preserves virus viability and nucleic acids for transport and storage prior to RT-PCR. | Standard VTM (e.g., in 15 mL Falcon tubes) [4] |
| Viral & Nucleic Acid Transport Systems | Specialized systems for rapid preparation of samples for PCR without manual extraction. | vNat Sample Prep Solutions (Bioeksen) [51] |
| RNA Extraction Kits | Isolate and purify viral RNA from clinical specimens for downstream RT-PCR. | Viral RNA and DNA Kit (Loccus Biotecnologia) [4] |
| Automated Nucleic Acid Extractor | Standardizes and automates the RNA/DNA extraction process. | Extracta 32 (Loccus Biotecnologia) [4] |
| Real-Time PCR Instruments | Platforms for performing and quantifying RT-PCR reactions. | QuantStudio 5 (Applied Biosystems), Rotor-Gene (Qiagen) [4] [51] |
Implications for Research and Clinical Practice
The synthesized data lead to several key conclusions for test utilization and development:
- Actionable Positive Results: The consistently high specificity of Ag-RDTs means that a positive result in a symptomatic individual is highly reliable and should trigger immediate interventions (isolation, treatment) without need for PCR confirmation [22].
- Cautious Interpretation of Negative Results: A negative antigen test does not rule out infection, especially in symptomatic individuals tested later in their illness or with low viral load. The IDSA suggests confirming a negative Ag result with a standard NAAT (e.g., RT-PCR) if clinical suspicion for COVID-19 remains high [22].
- Protocol Standardization is Critical: Variations in specimen collection (nasopharyngeal vs. combined oro/nasopharyngeal), timing, and test brand significantly impact performance metrics, making cross-study comparisons challenging [4] [51].
- Targeted Use Case: Antigen tests are most valuable as a tool for rapid identification of contagious, symptomatic individuals early in their illness, when viral load is high and the risk of transmission is greatest [43] [22].
Antigen tests are a pragmatic and powerful diagnostic tool when their performance characteristics are understood in the context of clinical presentation. The core principle is that symptomatology and timing are not confounding variables but are central to accurate test interpretation. For researchers and clinicians, leveraging this relationship means deploying Ag-RDTs strategically—valuing their speed and high positive predictive value in symptomatic populations while understanding their limitations in low-viral-load scenarios. Future test development should aim to improve sensitivity without sacrificing speed or cost, particularly for earlier detection or use in asymptomatic screening. Ultimately, correlating clinical presentation with test results ensures that Ag-RDTs are used to their maximum potential, providing critical information for both patient care and public health containment strategies.
The continuous evolution of SARS-CoV-2 variants and the dynamic landscape of population immunity present significant challenges for diagnostic test performance. As new variants emerge with distinct genetic and antigenic properties, and as population immunity shifts through vaccination and prior infections, the accuracy and reliability of diagnostic tests must be continually reassessed. This comparison guide examines the performance characteristics of antigen-detection rapid diagnostic tests (Ag-RDTs) versus reverse transcription-polymerase chain reaction (RT-PCR) tests in the context of contemporary viral variants and population immunity. Understanding these factors is crucial for researchers, scientists, and drug development professionals working to optimize testing strategies and develop next-generation diagnostics.
Performance Comparison: Antigen Tests vs. PCR
Table 1: Overall Performance Characteristics of Antigen Tests Compared to RT-PCR
| Performance Metric | Ag-RDT Performance | RT-PCR Performance | References |
|---|---|---|---|
| Overall Sensitivity | 47-59% | ~100% (reference standard) | [4] [43] |
| Overall Specificity | 94-99.7% | ~100% (reference standard) | [15] [20] |
| Sensitivity in Symptomatic | 56-65% | ~100% | [43] [20] |
| Sensitivity in Asymptomatic | 18-31% | ~100% | [43] [20] |
| Positive Predictive Value | 90-99% (20% prevalence) | ~100% | [20] |
| Negative Predictive Value | 57-92.56% | ~100% | [15] [20] |
The data demonstrate significantly lower sensitivity for Ag-RDTs compared to RT-PCR across multiple studies and settings. This performance gap becomes particularly pronounced in asymptomatic individuals and those with low viral loads. The specificity of Ag-RDTs remains consistently high, making positive results reliable in appropriate prevalence settings.
Impact of Viral Load on Test Performance
Table 2: Test Performance Stratified by Viral Load (Cycle Threshold Values)
| Viral Load Category | Ct Value Range | Ag-RDT Sensitivity | PCR Sensitivity | References |
|---|---|---|---|---|
| High Viral Load | Ct < 25 | 90.85-100% | ~100% | [15] [4] [13] |
| Moderate Viral Load | Ct 25-30 | 47.8-73.68% | ~100% | [15] [13] |
| Low Viral Load | Ct > 30 | 5.59-31.82% | ~100% | [15] [4] |
| Very Low Viral Load | Ct ≥ 33 | 5.59-27.27% | ~100% | [15] [4] |
The relationship between viral load and Ag-RDT sensitivity demonstrates a strong correlation, with performance declining dramatically as cycle threshold values increase (indicating lower viral loads). This fundamental limitation of antigen tests has important implications for their appropriate use in different clinical and public health scenarios.
Variant-Specific Performance
Table 3: Test Performance Across SARS-CoV-2 Variants
| Variant | Ag-RDT Sensitivity | PCR Sensitivity | Notes | References |
|---|---|---|---|---|
| Alpha | 69.23-78.85% | ~100% | Variant-dependent performance observed | [15] |
| Delta | 72.22-83.33% | ~100% | Differential performance between Ag-RDT types | [15] |
| Omicron | 100% (specific subvariants) | ~100% | Generally well-detected by Ag-RDTs | [15] |
| JN.1 | Comparable to earlier variants | ~100% | Maintained performance despite mutations | [53] |
| NB.1.8.1 | Expected comparable performance | ~100% | No significant impact anticipated | [53] |
While some variant-specific differences in Ag-RDT performance have been observed, particularly between Alpha and Delta variants, most contemporary Ag-RDTs maintain good detection capabilities across currently circulating variants, including Omicron descendants. This suggests that despite continuous viral evolution, the epitopes detected by these tests remain largely conserved.
Experimental Approaches and Methodologies
Standardized Evaluation Protocols
Independent evaluations of Ag-RDT performance typically follow standardized protocols to ensure comparable results across studies. The Scandinavian evaluation of laboratory equipment for point of care testing (SKUP) provides a robust methodology that has been applied to multiple Ag-RDT assessments [20].
Key Methodological Components:
- Participant Enrollment: Consecutive sampling of symptomatic and asymptomatic individuals presenting at test centers
- Sample Collection: Duplicate nasopharyngeal or combined oro-nasopharyngeal swabs collected simultaneously
- Reference Testing: RT-PCR as gold standard, typically targeting multiple SARS-CoV-2 genes (N, ORF1a, ORF1b)
- Blinded Analysis: Test operators blinded to reference results during Ag-RDT interpretation
- Quality Control: Internal analytical quality control where possible, with daily testing of controls
Sample processing typically occurs within 4 hours of collection, with Ag-RDTs performed according to manufacturer instructions and RT-PCR conducted using automated systems such as the Hologic Panther Fusion [43] [20]. Statistical analyses include sensitivity, specificity, positive and negative predictive values with 95% confidence intervals, often using cluster-robust bootstrapping to account for within-participant correlation in longitudinal studies [43].
Viral Culture as Correlate of Infectiousness
Recent methodologies have incorporated viral culture as an additional reference standard to distinguish between detection of replicating virus versus viral RNA fragments. This approach provides important insights into the practical utility of Ag-RDTs for identifying potentially transmissible infections [43].
Culture Methodology:
- Sample Processing: Nasal swabs in viral transport media, refrigerated ≤72 hours, then stored at -80°C
- Culture Protocol: Inoculation into permissive cell lines with cytopathic effect monitoring
- Outcome Measures: Correlation between Ag-RDT positivity and culture positivity as indicator of infectiousness
Studies using this methodology have found that Ag-RDT sensitivity improves to 80% when compared to viral culture as a reference, suggesting that Ag-RDTs are particularly effective at identifying individuals with actively replicating, potentially transmissible virus [43].
Impact of Population Immunity on Testing
Immune Imprinting and Diagnostic Performance
The concept of immune imprinting describes how initial exposures to SARS-CoV-2 antigens (through infection or vaccination) shape subsequent immune responses. Recent research demonstrates that sequential vaccination and hybrid immunity progressively shift immune imprinting from the prototype strain toward more recent variants [54].
This evolving landscape of population immunity influences testing dynamics in several ways. First, individuals with hybrid immunity may exhibit different viral kinetics, potentially affecting the window of detection for both antigen and molecular tests. Second, the relationship between viral load and infectiousness may be modified by pre-existing immunity, making viral culture correlation increasingly important for assessing test performance in contemporary populations [54] [43].
Protective Thresholds and Population Susceptibility
Recent research has begun to establish quantitative protective thresholds for neutralizing antibodies against specific variants. One study estimated the 50% protective neutralizing antibody titer against XBB.1.9.1 to be 1:12.6, providing a valuable benchmark for assessing population susceptibility [54].
Key Findings on Population Immunity:
- Retrospective analysis revealed that 80.3% of the population fell below the protective threshold against XBB in mid-2023, aligning with subsequent XBB resurgence
- By August 2024, only 33.8% exhibited sub-protective titers against JN.1, explaining the absence of JN.1-driven endemicity despite its dominance
- Modeling projections suggest that decreasing population immunity alone can drive COVID-19 waves even without changes in variant properties [53]
These findings highlight the importance of ongoing monitoring of population immunity to anticipate testing needs and interpret test performance in the context of evolving population susceptibility.
Research Reagent Solutions
Table 4: Essential Research Reagents for Test Performance Evaluation
| Reagent/Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| Reference Standard Tests | Hologic Panther Fusion RT-PCR, Biospeedy SARS-CoV-2 RT-PCR | Gold standard for SARS-CoV-2 detection | [4] [13] |
| Viral Transport Media | Viral Transport Medium (VTM), Viral Nucleic Acid Transport (vNAT) | Sample preservation and transport | [4] [13] |
| Automated Nucleic Acid Extraction | Loccus Extracta 32, Viral RNA and DNA Kit | Standardized nucleic acid isolation | [4] |
| PCR Detection Kits | Biospeedy SARS-CoV-2 RT-PCR, CDC RT-PCR diagnostic protocol | Target amplification and detection | [4] [13] |
| Neutralization Assays | Plaque reduction neutralization test (PRNT), Pseudotype virus neutralization | Immune response quantification | [54] [55] |
| Cell Culture Systems | Permissive cell lines (Vero E6, etc.) | Viral culture for infectivity assessment | [43] |
| Antigen Test Kits | LumiraDx, CLINITEST, NADAL, Flowflex, MF-68 | Rapid antigen detection | [20] |
Implications for Research and Development
The evolving landscape of viral variants and population immunity has significant implications for diagnostic test development and evaluation:
Test Development Considerations
Multiplex Approaches: Future test development should consider multiplex approaches that can detect multiple viral targets or variants simultaneously, addressing the challenge of continuous viral evolution.
Quantitative Antigen Tests: Research into quantitative or semi-quantitative antigen tests could provide better correlation with viral load and infectiousness, addressing the current limitation of binary results.
Variant-Neutral Epitopes: Identification and targeting of conserved epitopes less susceptible to viral mutation could enhance test longevity as new variants emerge.
Evaluation Framework Recommendations
Continuous Performance Monitoring: Establishing systems for ongoing test performance monitoring as new variants emerge is essential, rather than one-time evaluations.
Standardized Methodologies: Development of consensus methodologies for evaluating test performance across variants would enable more direct comparisons between studies.
Integrated Assessment: Future evaluations should integrate assessment of diagnostic performance with correlates of infectiousness (viral culture) and population immunity metrics.
The performance of SARS-CoV-2 diagnostic tests is intrinsically linked to the dynamic interplay between viral evolution and population immunity. While RT-PCR maintains superior sensitivity across all viral loads and variants, Ag-RDTs provide a valuable tool for rapid identification of infectious individuals, particularly those with high viral loads. The strong correlation between Ag-RDT positivity and viral culture results suggests their particular utility in identifying transmissible infection.
As SARS-CoV-2 continues to evolve and population immunity shifts through vaccination and infection, ongoing independent evaluation of test performance remains essential. Researchers and developers should prioritize tests with demonstrated performance across variants and in populations with diverse immune backgrounds. Future test development should aim to address the current limitations in low viral load detection while maintaining the advantages of speed, accessibility, and correlation with infectiousness that make Ag-RDTs valuable in appropriate settings.
The reliability of diagnostic testing, a cornerstone of modern clinical and research practice, hinges on the integrity of the sample analyzed. For researchers and drug development professionals comparing the performance of diagnostic methods, such as antigen tests and PCR, understanding the pre-analytical phase is paramount. Pre-analytical errors—those occurring from test ordering through sample handling—are not merely procedural concerns; they are a significant source of data variability that can compromise sensitivity and specificity calculations, ultimately skewing performance comparisons. This guide objectively examines these pitfalls, supported by experimental data, to ensure that the foundational evidence for your research remains uncompromised.
The Critical Weight of the Pre-Analytical Phase
The total testing process is a continuum, often conceptualized as a brain-to-brain loop, beginning with the test request and concluding with the interpreted result informing a clinical or research decision [56]. Within this process, the pre-analytical phase is the most vulnerable to error.
- Error Prevalence: Studies consistently show that 46% to 68% of all laboratory errors originate in the pre-analytical phase [57] [58]. This dwarfs errors occurring during the analytical phase (7-13%) [57].
- Impact on Results: Errors during this phase can lead to sample rejection or, more insidiously, the generation of erroneous results that are not flagged by laboratory systems. This directly impacts research outcomes, particularly when assessing key metrics like the sensitivity and specificity of a new assay [56].
Table 1: Distribution of Laboratory Errors Across Testing Phases
| Testing Phase | Description | Estimated Frequency of Errors |
|---|---|---|
| Pre-Analytical | Test request, patient preparation, sample collection, handling, transport | 46% - 68% [57] [58] |
| Analytical | Sample analysis on equipment | 7% - 13% [57] |
| Post-Analytical | Result validation, interpretation, and reporting | Remaining percentage |
Common Pre-Analytical Pitfalls and Their Impact on Diagnostic Performance
A nuanced understanding of specific pre-analytical errors is essential for designing robust experiments and accurately interpreting test performance data.
Patient Preparation and Identification
Factors preceding the physical act of venipuncture can significantly alter analyte concentrations or lead to sample misidentification.
- Fasting Status and Circadian Rhythm: Failure to fast for 10-12 hours can cause falsely elevated glucose and triglyceride levels [56] [57]. Furthermore, hormones like cortisol and renin exhibit strong diurnal variation, making collection timing critical [57].
- Medication and Supplement Interference: A prevalent concern is biotin (Vitamin B7), a common component of hair and nail supplements. Biotin can interfere with immunoassays that use a streptavidin-biotin system, leading to falsely high or low results. For reliable results, biotin supplements should be withheld for at least one week before testing [57].
- Patient Misidentification: Approximately 16% of phlebotomy errors involve patient misidentification, while 56% stem from improper tube labeling [56]. Pre-labeling tubes before collection is a high-risk practice that should be avoided [57].
Sample Collection Techniques
The collection process itself is a frequent source of significant errors that degrade sample quality.
- Hemolysis: In-vitro hemolysis, the rupture of red blood cells after collection, accounts for over 98% of hemolyzed samples and is a leading cause of sample rejection [57]. It can be caused by prolonged tourniquet time, using too small a needle, or forcefully transferring blood through a needle. Hemolysis falsely elevates potassium, phosphate, and lactate dehydrogenase and can interfere with spectrophotometric assays [56] [58].
- Contamination: Two primary sources are:
- IV Fluid Contamination: Drawing blood from an arm with a running IV drip dilutes the sample, causing aberrant results for electrolytes, glucose, and complete blood counts [58].
- Anticoagulant Cross-Contamination: Failing to follow the correct order of draw can transfer EDTA from a purple-top (K₂EDTA) tube into a light-blue top (sodium citrate) coagulation tube. EDTA chelates calcium, utterly invalidating coagulation tests like PT and APTT by preventing the clotting cascade from initiating [57] [58].
- Tourniquet Use: Applying a tourniquet for more than 60 seconds can increase potassium by 2.5% and total cholesterol by 5% due to hemoconcentration [58].
Sample Handling, Transport, and Storage
Errors do not stop once the sample is drawn. Improper handling post-collection can degrade the sample before analysis.
- Temperature and Time Delays: Glucose levels in unprocessed blood samples can decrease by 5-7% per hour at room temperature due to ongoing glycolysis [58]. Total bilirubin is photosensitive and will decline if exposed to light [58].
- Delayed Centrifugation: Storing uncentrifuged blood samples for extended periods allows cellular metabolism to continue. This can lead to potassium leaking out of cells and glucose being consumed, dramatically altering results as demonstrated in a case where potassium was reported at a critical 16.8 mmol/L after weekend refrigeration [58].
Table 2: Common Pre-Analytical Errors and Their Effects on Key Analytes
| Error Type | Specific Example | Effect on Test Results |
|---|---|---|
| Patient Preparation | Non-fasting state | Falsely elevated glucose, triglycerides [56] |
| Supplement Interference | Biotin intake | Interference with immunoassays (e.g., thyroid function, troponin) [57] |
| Collection Technique | Hemolysis | Falsely elevated K+, Mg2+, PO4-, LDH, AST; spectral interference [56] [57] |
| Collection Technique | EDTA contamination (into coagulation tube) | Falsely prolonged PT, APTT, TT [58] |
| Sample Handling | Delayed processing/centrifugation | Falsely decreased glucose; falsely increased K+ [58] |
| Sample Handling | Sample drawn from IV line | Dilution of all analytes (e.g., falsely low HGB, aberrant electrolytes) [58] |
The Researcher's Toolkit: Essential Materials and Reagents
The following table details key reagents and materials critical for ensuring sample integrity in diagnostic research, particularly in studies involving immunoassays and molecular biology.
Table 3: Key Research Reagent Solutions for Diagnostic Studies
| Reagent/Material | Function in Research Context |
|---|---|
| Viral Transport Medium (VTM) | Preserves viral integrity in nasopharyngeal swabs for downstream PCR or antigen testing [4] [13]. |
| Colloidal Gold-Labeled Antibodies | The detection conjugate in lateral flow immunochromatographic assays (GICA); binds to target antigen (e.g., SARS-CoV-2 nucleocapsid protein) to produce a visible signal [59]. |
| qRT-PCR Master Mix | Contains enzymes, dNTPs, and buffers essential for the reverse transcription and amplification of viral RNA, enabling detection and quantification via Cycle Threshold (Ct) [4] [59]. |
| Specific Monoclonal Antibodies | Used in both GICA and laboratory immunoassays; these highly specific antibodies are critical for capturing and detecting the target analyte with high specificity [59]. |
| EDTA and Sodium Citrate Tubes | Anticoagulant tubes for specific test types (e.g., EDTA for hematology, citrate for coagulation). Essential for pre-analytical integrity but a source of error if misused or cross-contaminated [57] [58]. |
Visualizing the Pre-Analytical Workflow and Its Impact
A clear workflow diagram helps identify potential failure points in the sample journey. The following diagram maps the key stages and highlights major risks.
Connecting Pre-Analytical Integrity to Test Performance: Antigen vs. PCR
The rigor of the pre-analytical phase is not just a quality control measure; it is a fundamental variable in the accurate assessment of diagnostic test performance, particularly when comparing antigen and PCR tests.
The Gold Standard and the Challenger
- RT-PCR is recognized for its high sensitivity and specificity, detecting viral RNA. However, it requires specialized lab infrastructure, trained personnel, and has a longer turnaround time [59].
- Antigen Tests (e.g., GICA) detect viral proteins, offering rapid results (15-20 minutes) at a lower cost, making them suitable for point-of-care and large-scale screening. Their primary limitation is lower sensitivity, especially in low viral load cases [59] [13].
The Viral Load Dependency
The core of the performance comparison lies in viral load, which is directly affected by pre-analytical handling. PCR's ability to amplify tiny amounts of genetic material makes it exceptionally sensitive. Antigen tests, however, require a higher viral load to generate a visible signal.
Real-world data underscores this relationship. One study of 2,882 symptomatic individuals found that while overall antigen test sensitivity was 59%, it rose to 90.85% in samples with high viral load (Cq < 20) but plummeted to 5.59% in samples with low viral load (Cq ≥ 33) [4]. This demonstrates that antigen test sensitivity is not a fixed value but a function of viral concentration.
The Pre-Analytical Link
A poorly handled sample can diminish viral load, thereby reducing the apparent sensitivity of an antigen test. For instance, improper swab collection, delays in testing, or exposure to degrading conditions can lower the amount of detectable antigen. This pre-analytical degradation would have a less pronounced effect on robust PCR assays, thereby widening the observed performance gap in a manner that is not reflective of the tests' true capabilities under ideal conditions.
Table 4: Comparative Analysis of SARS-CoV-2 Antigen Tests vs. RT-PCR
| Test Characteristic | RT-PCR (Gold Standard) | Rapid Antigen Test (GICA) | Experimental Data & Context |
|---|---|---|---|
| Target Molecule | Viral RNA | Viral Nucleocapsid (N) Protein | [59] |
| Sensitivity (Overall) | ~100% (by definition) | Varies by brand & viral load; ~59% overall in one study | Overall sensitivity of 59% (56-62 CI) reported in a study of 2882 individuals [4]. |
| Sensitivity (High Viral Load) | High | High | A study reported 90.85% agreement for Cq < 20 [4]. Another found 100% sensitivity for Ct < 25 [13]. |
| Sensitivity (Low Viral Load) | High | Low | Agreement dropped to 5.59% for Cq ≥ 33 [4]. |
| Specificity | ~100% (by definition) | Generally High | Consistently reported at 94-100% across studies [4] [59] [13]. |
| Time to Result | Hours to days | 15 - 30 minutes | [59] [13] |
| Key Pre-Analytical Concerns | RNA degradation during storage/transport; sample collection technique. | Rapid antigen degradation; sample collection technique; strict adherence to read-time window. | Sample stability and viral load are critical for antigen test performance [21]. |
For researchers and drug developers, the pre-analytical phase is a critical domain where study validity is won or lost. Errors in sample collection and handling introduce uncontrolled variability that can obscure true diagnostic performance, leading to inaccurate sensitivity and specificity estimates. A deep understanding of these pitfalls—from biotin interference to the order of draw and sample degradation—is not merely procedural but foundational. By implementing rigorous, standardized pre-analytical protocols, the research community can ensure that performance comparisons between diagnostic methods like antigen tests and PCR are accurate, reliable, and truly reflective of the technology being evaluated.
Beyond Manufacturer Claims: Independent Validation and Post-Market Surveillance
The rapid development and deployment of diagnostic tests during the COVID-19 pandemic created an unprecedented natural experiment in regulatory science, revealing critical gaps between pre-approval claims and real-world performance. For researchers and drug development professionals, understanding these discrepancies is essential for advancing diagnostic test validation frameworks. This guide objectively compares the performance of rapid antigen tests (RATs) with the gold standard reverse transcription polymerase chain reaction (RT-PCR), focusing specifically on the transition from controlled pre-approval studies to real-world clinical application.
The fundamental performance challenge stems from differing detection methods: RATs identify viral surface proteins, while PCR amplifies and detects viral genetic material, making it inherently more sensitive [8]. However, as this analysis demonstrates, the magnitude of the performance gap revealed in post-approval studies has significant implications for clinical practice and public health policy, particularly in resource-constrained settings where RATs offer practical advantages of speed and accessibility.
Performance Data Comparison: From Controlled Studies to Real-World Settings
Comprehensive Performance Metrics Table
Table 1: Comparative performance of antigen tests versus PCR across study types
| Test Category | Study Type | Sensitivity Range | Specificity Range | Key Influencing Factors | Sample Size/Studies |
|---|---|---|---|---|---|
| Overall Antigen Tests | Pre-approval (Manufacturer) | 86.5% (pooled average) [11] | 99.6% (pooled average) [11] | Ideal laboratory conditions, standardized procedures | 13 pre-approval studies across 9 brands [11] |
| Post-approval (Real-world) | 84.5% (pooled average) [11] | 99.6% (pooled average) [11] | Viral load, user technique, sample quality, variants | 26 post-approval studies across 9 brands [11] | |
| PCR Tests | Laboratory and real-world | 92.8%-97.2% [1] | ≈100% [1] | Sample collection, transport, laboratory expertise | Multiple clinical validations [1] [60] |
| Specific Antigen Test Brands | Pre- to post-approval comparison | Varies significantly by brand: LumiraDx (-10.9%), SOFIA (-15.0%) [11] | Remained stable across studies | Brand-specific design, manufacturing consistency | 15,500+ individuals across studies [11] |
Viral Load Impact on Test Performance
Table 2: Antigen test sensitivity correlation with viral load (measured by PCR cycle threshold values)
| Viral Load Category | PCR Cycle Threshold (Ct) | Antigen Test Sensitivity | Study Details |
|---|---|---|---|
| High viral load | Ct ≤20 | 100% [61] | PCL Spit Rapid Antigen Test Kit evaluation |
| Ct ≤25 | 82.4%-100% [1] [13] | Various brands including Roche/SDB and mö-screen | |
| Intermediate viral load | Ct 21-25 | 63% [61] | PCL Spit Rapid Antigen Test Kit evaluation |
| Low viral load | Ct >26 | 22% [61] | PCL Spit Rapid Antigen Test Kit evaluation |
| Ct >30 | 47.8% [13] | mö-screen Corona Antigen Test | |
| Very low viral load | Ct ≥33 | 5.59% agreement with PCR [4] | Brazilian real-world study of 2,882 symptomatic individuals |
| Low viral loads (unspecified) | Below 30% [1] | General finding from clinical review |
Experimental Protocols and Methodologies
Systematic Review Methodology for Pre- and Post-Approval Comparison
The most comprehensive comparison of pre-approval versus post-approval performance comes from a systematic review and meta-analysis conducted by Cochrane Denmark and the Centre for Evidence-Based Medicine Odense. This research analyzed 13 pre-approval and 26 post-approval studies across nine different SARS-CoV-2 rapid antigen test brands, encompassing data from over 15,500 individuals [11].
The experimental protocol involved:
- Literature Search Strategy: Comprehensive search of multiple databases for both published and unpublished studies
- Inclusion Criteria: Studies comparing antigen test performance with RT-PCR as reference standard, with separate analysis for pre-approval (submitted for regulatory approval) and post-approval (real-world use according to manufacturer instructions) studies
- Data Extraction: Standardized extraction of true positives, false positives, true negatives, and false negatives for each test brand
- Statistical Analysis: Bivariate meta-analysis to calculate pooled sensitivity and specificity estimates with 95% confidence intervals for both pre-approval and post-approval cohorts
- Heterogeneity Assessment: Investigation of sources of variation in performance, including test brand, study design, and population characteristics
This methodology allowed direct comparison of pre-approval claims with post-approval real-world performance, revealing that while most tests maintained stable accuracy, two widely used brands (LumiraDx and SOFIA) showed statistically significant declines in sensitivity of 10.9% and 15.0% respectively in post-approval settings [11].
Laboratory-Anchored Framework for Performance Prediction
A 2025 study published in JMIR X Med developed a quantitative, laboratory-anchored framework to predict real-world antigen test performance before large-scale clinical trials [21]. This methodology aims to bridge the evidence gap by combining controlled laboratory measurements with real-world variables.
The experimental workflow involves:
- Signal Response Characterization: Measuring test strip signal intensity across dilution series of target recombinant protein and inactivated virus using digital image analysis of test lines
- Limit of Detection (LoD) Determination: Statistical characterization of visual detection limits across a representative user population to establish probability of detection curves
- qPCR Calibration: Establishing correlation between PCR cycle threshold values and viral concentrations to enable cross-method comparisons
- Bayesian Predictive Modeling: Integrating laboratory measurements with user variability to generate continuous probability of positive agreement curves across the range of viral loads
This innovative approach moves beyond binary sensitivity reporting to create more nuanced performance predictions that account for real-world user variability and viral load distribution [21].
Diagram 1: Framework for bridging antigen test evidence gap. This illustrates the integration of laboratory data with real-world variables to predict performance.
Real-World Clinical Validation Protocols
Multiple studies have employed standardized clinical validation protocols to assess antigen test performance in real-world settings. The Brazilian cross-sectional study of 2,882 symptomatic individuals followed this rigorous protocol [4]:
- Study Population: Consecutive symptomatic individuals presenting to public healthcare facilities in Toledo, Brazil
- Sample Collection: Simultaneous collection of two nasopharyngeal swabs - one for immediate antigen testing and one for RT-PCR reference standard
- Test Execution: Antigen tests performed according to manufacturer instructions with 15-minute turnaround time
- PCR Methodology: RNA extraction using Viral RNA and DNA Kit with automated nucleic acid extractor, followed by CDC RT-PCR protocol on QuantStudio 5 instrument
- Data Analysis: Calculation of sensitivity, specificity, positive predictive value, and negative predictive value with 95% confidence intervals, stratified by viral load and demographic factors
This methodology revealed an overall antigen test sensitivity of 59% (56%-62%) compared to PCR, with significant variation between test brands (70% for IBMP kit vs. 49% for Bio-Manguinhos kit) [4].
Key Performance Drivers and Analytical Insights
The Viral Load Dependency
The most significant determinant of antigen test performance is viral load, typically measured by PCR cycle threshold (Ct) values. The relationship is inverse and nonlinear: as Ct values increase (indicating lower viral load), antigen test sensitivity decreases dramatically [1] [4] [61]. This explains the substantial performance differences between pre-approval studies (often enriched with high viral load samples) and real-world applications (covering the full spectrum of viral loads).
At Ct values ≤25 (high viral load), antigen tests approach PCR-level sensitivity, with some studies reporting 100% detection [13] [61]. However, at Ct values >30 (low viral load), detection rates plummet to 5.59%-47.8% [4] [13]. This has profound implications for test utility in different clinical scenarios: antigen tests perform excellently for identifying contagious individuals early in symptom onset when viral loads are typically high, but poorly for detecting late-stage infections or asymptomatic cases with lower viral loads [1] [8].
Impact on Clinical Decision-Making and Public Health
The performance gap between pre-approval claims and real-world performance has direct consequences for clinical management and public health policy:
- Missed Infections: At low viral loads, antigen tests show sensitivities below 30%, potentially missing 7 out of 10 infections with low viral loads [1]. In emergency room settings where 20-30% of patients present with low viral loads, this represents a significant diagnostic gap [1].
- Testing Cascades: Patients initially tested with antigen tests were over four times more likely to undergo additional testing on the same day compared to those starting with molecular PCR tests, increasing healthcare system burden [1].
- Transmission Risk: False negatives in low viral load cases contribute to ongoing community transmission, particularly in hospital settings where nosocomial outbreaks can originate from a single missed case [1].
Diagram 2: Viral load impact on antigen test performance. This shows the inverse relationship between viral load and test sensitivity.
Research Reagent Solutions and Essential Materials
Table 3: Key research reagents and materials for diagnostic test evaluation
| Reagent/Material | Function in Test Evaluation | Application Examples | Performance Considerations |
|---|---|---|---|
| Recombinant Viral Proteins | Standardization of antigen test signal response calibration | Establishing reference curves for test line intensity [21] | Enables quantitative comparison across test platforms without infectious materials |
| Heat-Inactivated Virus | Safe simulation of clinical samples for limit of detection studies | Determining analytical sensitivity under controlled conditions [21] | Maintains structural proteins while eliminating infectivity risk |
| Viral Transport Media | Preservation of sample integrity during storage and transport | Maintaining antigen stability between collection and testing [62] [60] | Composition affects antigen stability and test performance |
| Reference PCR Assays | Gold standard quantification of viral load | CDC RT-PCR protocol, commercially available RT-PCR kits [4] | Must be calibrated with standardized controls for cross-study comparisons |
| Automated Nucleic Acid Extraction Systems | Standardization of RNA extraction for PCR reference testing | Extracta 32 system, other automated extractors [4] | Reduces variability in sample preparation step |
| Digital Image Analysis Tools | Objective quantification of test line intensity | Cell phone camera capture with normalized pixel intensity analysis [21] | Eliminates subjective visual interpretation in laboratory studies |
The evidence gap between pre-approval and real-world performance of rapid antigen tests stems from multiple factors: viral load distribution differences between controlled studies and clinical populations, user variability in test administration and interpretation, and the inherent limitations of lateral flow technology in low viral load scenarios.
For researchers and drug development professionals, these findings highlight the necessity of:
- Enhanced Post-Market Surveillance: Mandatory, systematic post-approval evaluation should be required for diagnostic tests, particularly when widely deployed in non-clinical settings [11]
- Standardized Performance Reporting: Sensitivity should be reported across the full spectrum of viral loads rather than as a single aggregate measure [21]
- Context-Specific Test Recommendations: Recognition that antigen and molecular tests serve complementary roles based on clinical scenario, prevalence, and available resources [1] [8]
Bridging the evidence gap requires more sophisticated evaluation frameworks that integrate laboratory measurements with real-world variables, enabling more accurate prediction of clinical performance before widespread deployment. The methodologies and insights presented in this guide provide a foundation for developing such frameworks, ultimately leading to more reliable diagnostic test performance claims and more effective implementation in clinical and public health practice.
The unprecedented reliance on rapid antigen tests during the COVID-19 pandemic highlighted a critical challenge in diagnostic medicine: significant performance variability exists among commercial test kits that target the same pathogen. While manufacturers provide sensitivity and specificity claims based on controlled studies, independent evaluations consistently reveal that real-world performance often differs substantially from these claims [63]. For researchers, scientists, and drug development professionals, understanding the extent and implications of this variability is paramount when selecting diagnostic tools for clinical trials, surveillance studies, or public health interventions.
This analysis synthesizes findings from multiple independent studies to provide a evidence-based comparison of SARS-CoV-2 rapid antigen test performance. The data demonstrates that sensitivity varies dramatically across brands, between evaluation settings (laboratory versus real-world), and across different viral load levels. These discrepancies underscore the necessity of post-market surveillance and independent validation to ensure test reliability and inform appropriate use cases across healthcare and research settings [11] [20].
Methodological Framework for Test Evaluation
Standardized Evaluation Protocols
Independent evaluations of rapid antigen tests typically employ standardized methodologies to enable fair comparisons across different test brands. The foundational approach involves paired sampling, where two specimens are collected simultaneously from each participant—one for the antigen test being evaluated and one for reverse transcription quantitative polymerase Chain Reaction (RT-qPCR) testing as the reference standard [4] [20].
The Scandinavian evaluation of laboratory equipment for point of care testing (SKUP) provides a representative model for robust test assessment. Their protocol includes:
- Consecutive enrollment of participants presenting at test centers with symptoms suggestive of COVID-19 or with known exposure to confirmed cases
- Duplicate sampling using nasopharyngeal or combined oro-nasopharyngeal swabs
- Immediate processing of antigen tests according to manufacturer specifications
- Blinded interpretation of results to prevent assessment bias
- Viral transport medium preservation of paired samples for RT-qPCR analysis in clinical laboratories
- Statistical analysis calculating sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) with 95% confidence intervals [20]
This methodology ensures that performance metrics reflect real-world conditions while maintaining scientific rigor through standardized comparison to the gold standard RT-qPCR.
Quantitative Framework for Performance Prediction
Recent research has developed more sophisticated, quantitative frameworks for predicting test performance based on laboratory measurements. This approach combines:
- Signal intensity characterization across dilution series of target recombinant protein and inactivated virus
- Statistical modeling of the naked-eye limit of detection (LoD) across a user population
- Calibration of RT-qPCR cycle thresholds against viral concentration
- Bayesian predictive modeling to estimate probability of positive agreement as a function of viral load variables [21]
This methodology enables performance projection before large-scale clinical trials, enhancing the efficiency of test evaluation during public health emergencies.
Figure 1: Comprehensive Framework for Antigen Test Evaluation. This workflow illustrates the integrated laboratory and real-world assessment methodology used in independent test evaluations.
Comparative Performance Data Across Test Brands
Documented Sensitivity Variations in Independent Evaluations
Independent assessments consistently reveal substantial variability in sensitivity across different rapid antigen test brands, often diverging from manufacturer claims. The following table synthesizes performance data from multiple independent studies:
Table 1: Documented Sensitivity Variations Across SARS-CoV-2 Antigen Test Brands
| Test Brand | Reported Sensitivity | Independent Evaluation Sensitivity | Specificity | Study Context |
|---|---|---|---|---|
| IBMP TR Covid Ag kit | Not specified | 70% (95% CI: 69.8%) | 94% | 796 symptomatic individuals, Brazil [4] |
| TR DPP COVID-19 - Bio-Manguinhos | Not specified | 49% (95% CI: 49.0%) | 99% | 2,086 symptomatic individuals, Brazil [4] |
| LumiraDx SARS-CoV-2 Ag Test | >96% (pre-approval) | 10.9% decline post-approval | 99.6% | FDA post-market surveillance [11] |
| SOFIA SARS-CoV-2 Antigen Test | >96% (pre-approval) | 15.0% decline post-approval | 99.6% | FDA post-market surveillance [11] |
| CLINITEST Rapid COVID-19 Antigen Test | Manufacturer claims | 90% (95% CI: 82-95%) | 99.7% | SKUP evaluation, Scandinavia [20] |
| MF-68 SARS-CoV-2 Antigen Test | Manufacturer claims | 53% (95% CI: 42-64%) | 97.8% | SKUP evaluation, Scandinavia [20] |
| Mö-screen Corona Antigen Test | 98.32% (nasopharyngeal) | 100% (combined oro/nasopharyngeal) | 100% | 200 symptomatic patients [13] |
The UK Health Security Agency's systematic evaluation of 86 lateral flow devices found sensitivity ranging from 32% to 83%, with no correlation between manufacturer-reported sensitivity and independently determined performance [63]. This comprehensive assessment underscores the critical importance of independent verification for diagnostic tests used in clinical and public health decision-making.
Viral Load Dependency as a Key Performance Determinant
A consistent finding across multiple studies is the strong dependency of antigen test sensitivity on viral load, typically measured through RT-qPCR cycle threshold (Ct) values. Lower Ct values indicate higher viral loads and correspond with substantially improved antigen test performance:
Table 2: Antigen Test Sensitivity Stratified by Viral Load (PCR Cycle Threshold Values)
| Ct Value Range | Viral Load Category | Sensitivity Range Across Studies | Representative Study |
|---|---|---|---|
| Ct ≤20 | High | 90.85%-100% | Brazilian study (n=2,882) [4] |
| Ct 21-25 | Intermediate | 63%-81.25% | Multiple studies [4] [13] [61] |
| Ct 26-30 | Low | 22%-47.8% | Multiple studies [4] [13] [61] |
| Ct ≥33 | Very Low | 5.59%-30% | Brazilian study, Garcia-Rodriguez et al. [4] [1] |
This viral load dependency creates particular challenges in asymptomatic screening and early infection detection scenarios where viral loads may be below the reliable detection threshold of many rapid antigen tests. At Ct values above 30 (indicating lower viral loads), rapid antigen tests show sensitivities below 30%, potentially missing 7 out of 10 infections with low viral loads [1].
Figure 2: Antigen Test Performance Degradation with Decreasing Viral Load. Sensitivity drops dramatically as viral load decreases (higher Ct values), creating detection challenges in pre-symptomatic and convalescent phases.
Impact of Setting and User Factors on Test Performance
Pre-approval Versus Post-approval Performance Discrepancies
Regulatory evaluations of diagnostic tests typically rely on pre-approval studies conducted under controlled conditions. However, post-approval assessments conducted in real-world settings frequently reveal different performance characteristics. A systematic review of FDA-authorized SARS-CoV-2 rapid antigen tests found that while most tests maintained stable accuracy post-approval, some brands showed statistically significant declines in sensitivity [11].
The pooled analysis of 13 pre-approval and 26 post-approval studies across nine test brands demonstrated:
- Pre-approval sensitivity: 86.5%
- Post-approval sensitivity: 84.5%
- Absolute difference: 2.0% (not statistically significant)
- Specificity: Remained unchanged at 99.6%
Despite this overall stability, two specific test brands (LumiraDx and SOFIA) demonstrated significant sensitivity declines of 10.9% and 15.0% respectively in post-approval settings [11]. Notably, these brands had reported exceptionally high pre-approval sensitivity (>96%), suggesting that initial studies may have overestimated real-world performance or that later viral variants affected detection capabilities.
The Role of User Technique and Sample Quality
Beyond inherent test characteristics, operator-dependent factors significantly influence test performance. Proper specimen collection technique, timing of test administration relative to symptom onset, and correct interpretation of results all contribute to variability in real-world effectiveness [21] [13].
The SKUP evaluations specifically assessed user-friendliness through questionnaires completed by test center employees. While all evaluated tests received satisfactory ratings for user-friendliness, variations in procedural complexity (such as number of processing steps and clarity of result interpretation) may contribute to performance differences between laboratory and field settings [20].
Sample collection method also impacts sensitivity. One study found that using combined oro/nasopharyngeal swabs yielded 100% sensitivity compared to 98.32% with nasopharyngeal swabs alone as specified in the manufacturer's instructions [13]. This suggests that sample quality and collection technique can partially compensate for inherent test limitations.
Implications for Research and Clinical Practice
Strategic Test Selection Based on Use Case
The documented variability in test performance underscores the importance of context-appropriate test selection. The World Health Organization recommends that antigen tests meet minimum performance requirements of ≥80% sensitivity and ≥97% specificity, and suggests they be used primarily in symptomatic populations where viral loads tend to be higher [13] [20].
For research applications, particularly those involving assessment of infectiousness or transmission risk, tests with demonstrated high sensitivity at low Ct values (high viral loads) may be preferable. For surveillance programs in low-prevalence settings, the SKUP evaluations found positive predictive values can be unacceptably low (16-55% at 0.5% prevalence), suggesting limited utility for general screening in such contexts [20].
The Research Reagent Toolkit for Test Evaluation
Independent evaluation of diagnostic tests requires specialized reagents and equipment to ensure standardized assessment. The following table outlines essential components of the research toolkit for test validation:
Table 3: Essential Research Reagents and Materials for Test Evaluation
| Reagent/Material | Function in Evaluation | Representative Examples |
|---|---|---|
| Viral Transport Medium (VTM) | Preserves specimen integrity during transport and storage | Copan VTM, Viral Nucleic Acid Transport Medium [4] [13] |
| Reference Standard Test | Provides gold standard comparison for accuracy assessment | RT-qPCR tests (CDC protocol, Biospeedy SARS-CoV-2) [4] [13] |
| Automated Nucleic Acid Extraction Systems | Standardizes RNA extraction for reference testing | KingFisher Flex, STARlet Seegene system [4] [64] |
| Inactivated Virus Preparations | Enables controlled sensitivity assessment | Heat-inactivated SARS-CoV-2 [21] |
| Recombinant Target Proteins | Characterizes test line signal response | Recombinant nucleocapsid protein [21] |
| Digital PCR Systems | Provides absolute quantification for method comparison | QIAcuity platform, droplet digital PCR [64] |
The comprehensive analysis of SARS-CoV-2 rapid antigen tests reveals substantial variability in sensitivity across commercial brands, with performance frequently diverging from manufacturer claims. This variability is most pronounced at lower viral loads, creating significant limitations for certain applications including asymptomatic screening and early infection detection.
For the research and clinical community, these findings highlight several critical considerations:
- Independent validation should be prerequisite for test deployment in research studies or clinical programs
- Viral load characteristics of the target population should inform test selection decisions
- Post-market surveillance is essential to identify performance changes with new variants or in different user populations
- Standardized evaluation methodologies enable meaningful comparisons across different test brands
Future diagnostic development should prioritize transparent reporting of performance data across the full spectrum of viral loads and robust design that maintains accuracy despite operator variability. As new pathogens emerge and testing technologies evolve, the lessons from SARS-CoV-2 test evaluation provide a framework for more reliable assessment of diagnostic tools that inform both clinical and public health decision-making.
The COVID-19 pandemic has highlighted a critical challenge in diagnostic testing: while reverse transcription-polymerase chain reaction (RT-PCR) provides exceptional sensitivity for detecting viral RNA, it cannot distinguish between infectious virus and non-viable viral fragments, potentially leading to prolonged isolation periods beyond the window of transmissibility [65] [43] [66]. This limitation has stimulated renewed interest in viral culture as a functional benchmark for determining true infectious potential, as it detects only replication-competent virus [66] [67].
Antigen tests (Ag-RDTs) have emerged as widely deployed tools for rapid diagnosis, but their variable sensitivity compared to PCR has raised concerns about their reliability [1] [4]. However, when evaluated against the more clinically relevant benchmark of viral culture—which correlates directly with transmissibility—antigen test performance appears substantially different [65] [43] [66]. This review synthesizes evidence establishing viral culture as a functional gold standard and examines how antigen tests correlate with infectious SARS-CoV-2, providing researchers and clinicians with a critical framework for interpreting test results in the context of transmission risk.
Viral Culture as the Functional Gold Standard
Technical Basis and Methodology
Viral culture isolates replication-competent SARS-CoV-2 by inoculating patient samples onto permissive cell lines (typically Vero E6 cells) and observing cytopathic effects or detecting viral replication through secondary assays [66] [67]. Unlike molecular methods that amplify viral genetic material, culture detects only intact, viable virus capable of infecting host cells.
Standardized viral culture protocols involve:
- Sample preparation: Nasopharyngeal or nasal swabs in viral transport medium are centrifuged to remove debris [67]
- Cell inoculation: Supernatants are applied to coniferous cell monolayers in biosafety level-3 (BSL-3) facilities [67]
- Incubation period: Typically 5-7 days with monitoring for cytopathic effects [66]
- Confirmation methods: Include immunofluorescence staining for viral proteins or PCR demonstrating increasing viral RNA in culture supernatants [67]
The major limitation of viral culture is its requirement for BSL-3 containment and extended processing time (days versus hours), making it impractical for routine clinical use [67]. However, for research establishing correlates of infectivity, it remains indispensable.
Temporal Dynamics of Infectious Virus Shedding
Longitudinal studies tracking multiple biomarkers reveal distinct timelines for detectability. Viral RNA by RT-PCR remains detectable long after cessation of infectious virus shedding, while antigen detection and viral culture positivity align more closely with the period of potential transmission.
Table 1: Temporal Dynamics of SARS-CoV-2 Detection Methods
| Detection Method | Target | Median Time to Negativity (Days from Symptom Onset) | Maximum Detection Window |
|---|---|---|---|
| Viral Culture | Replication-competent virus | 11 [IQR: 9-13] [66] | Typically 10-14 days [66] |
| Nucleocapsid Antigen | Viral nucleocapsid protein | 13 [IQR: 10-16] [66] | Up to 16 days [66] |
| Spike Antigen | Viral spike protein | 9 [IQR: 7-12] [66] | Up to 12 days [66] |
| RT-PCR | Viral RNA | >19 days [66] | 21-30 days (50% of patients) [66] |
Beyond two weeks from symptom onset, viral growth in culture is rarely positive, while RT-PCR remains detectable in half of patients tested 21-30 days after symptom onset [66]. This discordance highlights the clinical challenge of using PCR alone to determine infection control measures.
Antigen Test Performance Against Culture and PCR
When evaluated against both PCR and viral culture, antigen tests demonstrate intermediate sensitivity—lower than PCR but substantially higher when compared to culture.
Table 2: Antigen Test Performance Compared to Reference Standards
| Reference Standard | Antigen Test Sensitivity | Specificity | Study Details |
|---|---|---|---|
| RT-PCR | 40.9% [65] to 59% [4] | 99%-100% [65] [4] | Various settings and populations |
| Viral Culture | 80% (95% CI: 76%-85%) [43] | Not reported | Household transmission study |
| Viral Culture | 96.2% (95% CI: 85.9%-99.3%) [65] | 91.0% (95% CI: 87.0%-94.0%) [65] | Evaluation of Standard Q COVID-19 Ag test |
This pattern of higher sensitivity against culture than against PCR is consistent across multiple studies. A CDC study conducted from November 2022-May 2023 found antigen test sensitivity was 47% compared to RT-PCR but 80% compared to viral culture [43]. This suggests antigen tests miss RNA detection but identify most culturally viable virus.
Impact of Viral Load on Test Performance
The relationship between antigen test sensitivity and viral load is well-established. Antigen test performance excels when viral loads are high but declines substantially at lower viral loads.
Table 3: Antigen Test Sensitivity by Viral Load (Measured via PCR Cycle Threshold)
| Cycle Threshold (Ct) Range | Antigen Test Sensitivity | Interpretation |
|---|---|---|
| Ct < 25 (High viral load) | 100% [15] [61] | Excellent detection |
| Ct 25-30 (Intermediate viral load) | 31.8%-63% [15] [61] | Variable detection |
| Ct > 30 (Low viral load) | 5.6%-31.8% [15] [4] | Poor detection |
This viral load dependency is functionally significant because higher viral loads correlate strongly with positive cultures. One study found that a Ct value of 18.1 in RT-PCR best predicted positive viral culture (AUC 97.6%) [65]. Both antigen test types (FIA and LFIA) showed 100% sensitivity at Ct values <25, but sensitivity dropped to 27.3%-31.8% at Ct values >30 [15].
The following diagram illustrates the relationship between viral load and detection methods:
Key Determinants of Antigen Test Performance
Symptom Status and Timing
The performance of antigen tests varies significantly based on clinical presentation and timing relative to symptom onset. Symptomatic individuals, particularly early in symptom course, show higher antigen test sensitivity.
A comprehensive study found antigen test sensitivity was 57.9% (95% CI: 46.0%-68.9%) in patients with 1-5 days of symptoms, but dropped to 12.0% (95% CI: 5.0%-25.0%) in asymptomatic individuals [65]. The CDC household transmission study reported antigen test sensitivity reached 65% at 3 days after symptom onset among symptomatic individuals, and peaked at 80% among those reporting fever [43].
SARS-CoV-2 Variants
Emerging evidence suggests antigen test performance may vary across SARS-CoV-2 variants. One study comparing antigen test performance across variants found that both fluorescence immunoassay (FIA) and lateral flow immunoassay (LFIA) antigen tests had 100% sensitivity for detecting the Omicron variant, compared to 78.85% and 69.23% respectively for the Alpha variant [15]. This may reflect higher viral loads associated with Omicron infection [15].
Research Applications and Methodologies
Experimental Workflow for Test Validation
The following diagram outlines a standardized research approach for correlating antigen test performance with viral culture:
Essential Research Reagents and Materials
Table 4: Research Reagent Solutions for Viral Culture and Antigen Test Evaluation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Vero E6 Cells | Permissive cell line for SARS-CoV-2 replication | Essential for viral culture; requires BSL-3 containment [67] |
| Viral Transport Medium (VTM) | Preserves virus viability during transport and storage | Critical for maintaining sample integrity before culture [4] [67] |
| SARS-CoV-2 Nucleocapsid Antibodies | Detect viral nucleocapsid protein in antigen tests | Target for most commercial antigen tests [65] [66] |
| RNA Extraction Kits | Isolate viral RNA for RT-PCR testing | Required for PCR-based quantification [4] |
| Virus Inactivation Reagents | Render virus non-infectious while preserving antigens | Enable safe handling for antigen testing outside BSL-3 [21] |
| Cell Culture Media | Support cell viability during incubation period | Essential for maintaining cells during 5-7 day culture period [67] |
Discussion and Research Implications
The evidence synthesized in this review demonstrates that viral culture provides a functional benchmark for SARS-CoV-2 infectivity that aligns more closely with antigen test performance than with PCR detection. While PCR remains the most sensitive method for identifying infected individuals, the strong correlation between antigen test positivity and viral culture suggests antigen tests may be superior for identifying individuals most likely to transmit infection [65] [43] [66].
From a public health perspective, these findings support the use of antigen tests for guiding isolation decisions, particularly in settings where rapid identification of infectious individuals is critical for outbreak control. The high specificity of antigen tests (typically >97%) means positive results rarely require confirmation in high-prevalence settings [1] [4]. However, the lower sensitivity of antigen tests, particularly in asymptomatic individuals or those with low viral loads, necessitates caution when using negative tests to rule out infection in high-risk scenarios [65] [43].
For the research community, these findings highlight the importance of selecting appropriate reference standards based on the clinical or public health question being addressed. PCR remains the optimal reference for diagnostic sensitivity studies aimed at case identification, while viral culture provides the most relevant benchmark for studies investigating transmission risk and infectivity.
Viral culture serves as a critical functional benchmark for establishing the relationship between antigen test results and infectious potential. Mounting evidence demonstrates that antigen tests strongly correlate with culturable virus, particularly during the period of peak transmissibility early in the course of infection. This correlation persists across SARS-CoV-2 variants and is enhanced in symptomatic individuals.
While PCR detection remains more sensitive for identifying infection, the functional correlation between antigen test positivity and viral culture supports the use of these rapid tests for identifying individuals most likely to transmit SARS-CoV-2. Future test development should continue to utilize viral culture as a reference standard when evaluating the performance of rapid diagnostics intended for infection control purposes. For researchers and clinicians, understanding these relationships is essential for appropriate test selection, interpretation, and application in both clinical and public health contexts.
Independent evaluation serves as a cornerstone in the validation of diagnostic tests, providing unbiased assessments of performance metrics that manufacturer-reported data may not fully capture. Within the context of SARS-CoV-2 testing, this independent verification has proven particularly crucial for rapid antigen tests (Ag-RDTs), where real-world performance often diverges from manufacturer claims under ideal laboratory conditions. The Scandinavian evaluation of laboratory equipment for point of care testing (SKUP) consortium exemplifies this approach through systematic, manufacturer-independent assessments conducted by intended users in real-world settings [20]. These evaluations become especially significant when contextualized within the broader research on the sensitivity and specificity of antigen tests compared to the gold standard reverse transcription-polymerase chain reaction (RT-PCR) methodology.
The COVID-19 pandemic precipitated an unprecedented global testing regime, creating an urgent need for decentralized, accessible diagnostic options. While RT-PCR maintained its position as the gold standard due to its high sensitivity, it required specialized laboratory infrastructure, trained personnel, and incurred significant time delays [51] [13]. Rapid antigen tests emerged as a viable alternative, offering quick results at lower cost without requiring sophisticated equipment, thus playing a pivotal role in pandemic control strategies [4] [51]. However, questions regarding their diagnostic accuracy relative to RT-PCR necessitated rigorous independent evaluation to inform appropriate use cases and limitations, particularly as test performance varied considerably across manufacturers and viral load levels [4] [5] [20].
Independent Evaluation Frameworks: SKUP and SCOPE
The SKUP Consortium Framework
The Scandinavian evaluation of laboratory equipment for point of care testing (SKUP) represents a robust model for manufacturer-independent diagnostic test evaluation. Established as a collaboration between external quality assurance organizations in Norway (Noklus), Sweden (Equalis), and Denmark (DEKS), SKUP aims to improve point-of-care testing quality by providing objective information about diagnostic performance and user-friendliness [20]. This consortium operates on the fundamental principle that evaluations should be conducted under real-life conditions by the intended end-users, providing practical insights that complement controlled laboratory studies.
SKUP's methodology is characterized by several key features: prospective evaluation designs, consecutive participant enrollment, and direct comparison against reference standards (typically RT-PCR for SARS-CoV-2 detection). Their evaluations generally target sample sizes of at least 100 positive and 100 negative results, or a maximum of 500 samples, ensuring sufficient statistical power for reliability [20]. This approach aligns with recommendations from the European Centre for Disease Prevention and Control (ECDC), which emphasizes the importance of evaluations performed among intended users before widespread implementation [20]. The organizational independence of such frameworks ensures freedom from outside interference, with evaluators protected from potential conflicts of interest that might compromise the objectivity of their assessments [68].
The SCOPE Framework for Research Evaluation
Complementing SKUP's focus on diagnostic tests, the SCOPE (Start, Context, Options, Probe, Evaluate) framework provides a systematic, five-stage model for responsible research evaluation [69]. Developed by the International Network of Research Management Societies (INORMS) Research Evaluation Group, SCOPE offers a practical step-by-step process that helps research managers and evaluators plan new evaluations or check existing ones against responsible assessment principles.
The SCOPE framework's stages include: Starting with what an institution values, considering Contextual factors, evaluating Options for assessment, Probing deeply into evidence, and Evaluating the evaluation process itself [69]. This framework has been implemented by numerous institutions worldwide, including the University of Turku, Loughborough University, and the UK Higher Education Funding Bodies, demonstrating its versatility across different evaluation contexts [69]. While originally designed for research assessment, SCOPE's principles of responsible evaluation align closely with the needs of diagnostic test evaluation, particularly in its emphasis on context-aware, value-led assessment practices.
Comparative Performance Data: Antigen Tests vs. RT-PCR
Independent evaluations across multiple studies have consistently demonstrated that rapid antigen tests generally exhibit lower sensitivity but high specificity when compared to RT-PCR. The following table summarizes key findings from recent independent studies:
Table 1: Performance Characteristics of Rapid Antigen Tests vs. RT-PCR
| Study/Evaluation | Sensitivity (%) | Specificity (%) | Sample Size | Population Characteristics |
|---|---|---|---|---|
| SKUP Evaluations (Range) [20] | 53-90 | 97.8-99.7 | 321-679 per test | Symptomatic and asymptomatic with suspected exposure |
| CDC Household Study [43] | 47 (vs. RT-PCR) 80 (vs. culture) | N/R | 236 infected participants | Household contacts with longitudinal sampling |
| Cochrane Review [5] | 69.3 (average) | 99.3 (average) | 117,372 samples | Mixed symptomatic and asymptomatic |
| Brazilian Real-World Study [4] | 59 | 99 | 2,882 | Symptomatic individuals in public health system |
| Pakistan Saliva-Based Test [61] | 67 | 75 | 320 | Predominantly male population |
This aggregated data reveals considerable variation in test performance, underscoring how factors like study population, sampling methods, and test brand influence outcomes. The SKUP evaluations notably documented sensitivities ranging from 53% to 90%, with three of five tests clustering between 70-75% sensitivity – figures that frequently fell short of manufacturer claims [20]. This performance discrepancy highlights the critical importance of independent verification, as healthcare systems and policymakers rely on accurate performance data to make informed testing decisions.
Impact of Viral Load and Symptoms on Test Performance
A consistent finding across independent evaluations is the strong correlation between antigen test sensitivity and viral load, typically measured through RT-PCR cycle threshold (Ct) values. The following table illustrates this relationship across multiple studies:
Table 2: Antigen Test Sensitivity Stratified by Viral Load (Ct Values)
| Study | Ct ≤20 (High Viral Load) | Ct 21-25 (Moderate Viral Load) | Ct >25 (Low Viral Load) | Notes |
|---|---|---|---|---|
| Brazilian Study [4] | 90.85% agreement | Performance decreased with increasing Ct | 5.59% agreement for Ct ≥33 | Significant difference between test brands |
| Pakistan Study [61] | 100% | 63% | 22% (for Ct 26-30) | Using saliva samples |
| Qiagen mö-screen Evaluation [51] | 100% for Ct <25 | 47.8% for Ct 25-30 | Not reported | Combined oro/nasopharyngeal sampling |
Symptom status also significantly impacts test performance. The Cochrane review reported average sensitivity of 73.0% in symptomatic individuals compared to 54.7% in asymptomatic populations [5]. Similarly, the CDC found antigen test sensitivity reached 56% on days when any COVID-19 symptoms were reported, peaking at 77% on days when fever was present, compared to just 18% on asymptomatic days [43]. This pattern reinforces World Health Organization recommendations that antigen tests should be used primarily in symptomatic individuals, ideally within the first week of symptom onset when viral loads tend to be highest [5] [20].
Experimental Protocols in Independent Evaluations
SKUP Evaluation Methodology
The SKUP consortium implemented a standardized protocol for evaluating SARS-CoV-2 antigen tests that exemplifies rigorous independent assessment methodology. The process begins with consecutive enrollment of participants at COVID-19 test centers in Norway and Denmark, including both symptomatic individuals and asymptomatic contacts of confirmed cases [20]. During the peak Omicron wave, inclusion criteria were broadened to "symptomatic and asymptomatic subjects with high probability of SARS-CoV-2 infection" to reflect the high community prevalence [20].
The core testing protocol involves simultaneous duplicate sampling – two swabs collected at the same time by the same healthcare professional. One swab is used immediately for the antigen test according to manufacturer instructions, while the other is placed in viral transport media for RT-PCR analysis at a clinical laboratory [20]. This paired design controls for variability in sampling timing and technique, enabling direct comparison between the index test and reference standard.
SKUP evaluations incorporate user-friendliness assessments through questionnaires completed by test center staff, capturing practical elements like ease of use, clarity of instructions, and result interpretation [20]. This multidimensional approach provides insights beyond pure accuracy metrics, addressing implementation factors critical to real-world utility.
Laboratory Methodologies in Comparative Studies
Independent evaluations typically employ standardized laboratory techniques to ensure result reliability. For RT-PCR testing, common protocols include:
- RNA extraction using commercial kits (e.g., Viral RNA and DNA Kit) with automated extraction systems [4]
- PCR amplification using approved kits (e.g., Biospeedy SARS-CoV-2 RT-PCR test, CDC protocols) on platforms like QuantStudio 5 or Rotor-Gene systems [4] [51]
- Cycle threshold values typically set at 35-36 as the positivity cutoff [51] [61]
For antigen testing, evaluations follow manufacturer instructions precisely while maintaining consistent reading times and interpretation criteria. Some studies implement semi-quantitative assessment of test line intensity, correlating these with Ct values to establish viral load relationships [51] [13]. This approach reveals that faint test lines typically correspond to higher Ct values (lower viral loads), providing useful context for interpreting weak positive results.
Statistical Analysis Approaches
Independent evaluations employ comprehensive statistical methodologies to assess test performance. Standard calculations include:
- Sensitivity and specificity with 95% confidence intervals using standard formulas [70] [20]
- Positive and negative predictive values at various prevalence levels to contextualize clinical utility [70] [20]
- Logistic regression to examine relationships between test results and factors like Ct values, symptom status, and days since symptom onset [4] [61]
These analytical approaches allow evaluators to quantify performance across clinically relevant subgroups and provide nuanced guidance for test implementation in different populations and settings.
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Essential Research Reagents and Materials for Diagnostic Test Evaluation
| Item | Function | Example Products/Brands |
|---|---|---|
| Viral Transport Media | Preserves specimen integrity during transport | Viral Transport Medium (VTM), Viral Nucleic Acid Transport (vNAT) [4] [51] |
| RNA Extraction Kits | Isolates viral genetic material for RT-PCR | GF-1 Viral Nucleic Acid Extraction Kit, MVXA-P096FAST [4] [61] |
| RT-PCR Test Kits | Detects SARS-CoV-2 RNA through amplification | Biospeedy SARS-CoV-2 RT-PCR Test, Bosphore Novel Coronavirus Detection Kit [51] [61] |
| Rapid Antigen Tests | Detects viral nucleocapsid proteins | LumiraDx SARS-CoV-2 Ag Test, Flowflex SARS-CoV-2 Antigen Test, CLINITEST Rapid COVID-19 Antigen Test [20] |
| Nasopharyngeal/Oropharyngeal Swabs | Sample collection from respiratory tract | FLOQSwabs (Copan) [51] [13] |
| PCR Instruments | Amplification and detection of viral RNA | QuantStudio 5 (Applied Biosystems), Rotor-Gene (Qiagen) [4] [51] |
This collection of essential reagents and equipment enables researchers to conduct comprehensive evaluations of diagnostic test performance. The selection of appropriate materials directly impacts evaluation quality, particularly regarding sample integrity, amplification efficiency, and result reliability. Standardized use of these tools across independent studies facilitates more meaningful cross-study comparisons and meta-analyses.
Implications for Research and Clinical Practice
Independent evaluations have revealed critical limitations in rapid antigen tests that directly impact their appropriate clinical use. The consistently demonstrated lower sensitivity compared to RT-PCR, particularly in asymptomatic individuals and those with low viral loads, necessitates careful consideration of how and when these tests should be deployed [5] [20] [43]. The SKUP evaluations found that at a hypothetical disease prevalence of 0.5%, positive predictive values (PPVs) ranged from just 16% to 55%, calling into question the utility of antigen tests for general screening in low-prevalence settings [20].
These performance characteristics have direct implications for clinical practice and public health policy. The CDC recommends that persons in the community eligible for antiviral treatment should seek more sensitive RT-PCR testing, as antigen tests' lower sensitivity might lead to false-negative results and delayed treatment initiation [43]. Similarly, the Infectious Diseases Society of America guidelines recommend nucleic acid amplification tests over antigen tests for symptomatic individuals or when the implications of missing a COVID-19 diagnosis are significant [5].
From a research perspective, the consistent gap between manufacturer-reported performance and independently verified results underscores the necessity of robust post-market surveillance for diagnostic tests. The SKUP model provides a template for such evaluations, emphasizing real-world conditions and intended users to generate clinically relevant performance data [20]. This approach should be extended beyond SARS-CoV-2 to other infectious diseases where rapid diagnostics play a crucial role in clinical management and public health control measures.
Independent evaluation frameworks like SKUP and SCOPE provide indispensable methodologies for validating the real-world performance of diagnostic tests. The evidence generated through these rigorous assessments reveals critical insights that manufacturer data alone cannot provide, particularly regarding the variable sensitivity of rapid antigen tests across different viral loads and patient populations. In the context of SARS-CoV-2, these evaluations have demonstrated that while antigen tests offer practical advantages through speed and accessibility, their diagnostic limitations necessitate thoughtful implementation strategies that account for their optimal use cases.
The consistent findings across multiple independent studies – showing higher antigen test sensitivity in symptomatic individuals, those with high viral loads, and during early symptom onset – provide an evidence-based foundation for test utilization policies. As new variants emerge and population immunity evolves, continued independent evaluation remains essential to monitor test performance and inform appropriate use. The frameworks and methodologies described herein offer a model for such ongoing assessment, ensuring that diagnostic strategies remain grounded in rigorous, independent evidence rather than manufacturer claims alone.
The COVID-19 pandemic created an unprecedented global demand for accurate, scalable, and rapid diagnostic tests, revealing critical strengths and vulnerabilities in diagnostic validation pipelines during public health emergencies. The two most important methods for detecting SARS-CoV-2—Antigen-detection Rapid Diagnostic Tests (Ag-RDTs) and quantitative Reverse Transcription Polymerase Chain Reaction (RT-qPCR) tests—presented distinct operational profiles that influenced pandemic control strategies globally [4]. While antigen tests offered rapid turnaround times suitable for point-of-care testing, they demonstrated generally lower sensitivity compared to RT-qPCR tests, which detected viral genetic material with higher sensitivity but required specialized infrastructure, technical expertise, and longer processing times [4]. This diagnostic dichotomy framed a central challenge in pandemic management: balancing speed against accuracy while maintaining robustness against an evolving pathogen.
The performance characteristics of these tests became paramount as countries implemented testing-based containment strategies. Diagnostic accuracy, particularly the proportion of correct results (both true positives and true negatives), required rigorous evaluation not just in controlled laboratory settings but in real-world implementation contexts [4]. The lessons learned from SARS-CoV-2 diagnostic testing now provide a critical foundation for building more robust validation frameworks capable of responding to future pandemic threats with greater efficiency, accuracy, and adaptability.
Comparative Performance: Antigen Tests Versus PCR in Real-World Settings
Diagnostic Accuracy Across Test Modalities
Real-world performance data reveals significant differences in operational characteristics between antigen and molecular tests. The following table summarizes key performance metrics from recent comparative studies:
Table 1: Comparative Performance of Antigen Tests vs. PCR in Diagnostic Accuracy
| Study Reference | Sample Size | Sensitivity | Specificity | PPV | NPV | Test Type |
|---|---|---|---|---|---|---|
| Brazilian Cross-Sectional Study [4] | 2882 | 59% (0.56-0.62) | 99% (0.98-0.99) | 97% | 78% | Antigen (Overall) |
| Brazilian Study - IBMP Kit [4] | 796 | 70% | 94% | 96% | 57% | Antigen (Specific Brand) |
| Brazilian Study - Bio-Manguinhos [4] | 2086 | 49% | 99% | N/R | N/R | Antigen (Specific Brand) |
| Mö-Screen Evaluation [13] | 200 | 100% | 100% | 100% | 100% | Antigen (Specific Brand) |
| Padua Hospital Study [50] | 1387 | 68.9% | 99.9% | N/R | N/R | Antigen (Abbott) |
| PCR (Gold Standard) [4] | N/A | ~100% | ~100% | ~100% | ~100% | Molecular |
The variation in antigen test performance, particularly between different manufacturers, highlights the critical importance of rigorous validation and brand-specific evaluation before deployment in public health responses [4]. This variability underscores the necessity of standardized assessment protocols that can be rapidly implemented during emergent health crises.
Impact of Viral Load on Test Performance
Viral load, typically measured through Cycle quantification (Cq) values in PCR testing, represents a crucial determinant of antigen test performance. The relationship between viral load and antigen test accuracy reveals fundamental operational limitations:
Table 2: Antigen Test Performance Stratified by Viral Load (Cq Values)
| Cq Value Range | Viral Load Category | Antigen Test Agreement with PCR | Implications for Detection |
|---|---|---|---|
| < 20 | High | 90.85% | Excellent detection of contagious individuals |
| 20-25 | Moderate | 81.25% | Good detection in symptomatic cases |
| 26-28 | Low | Declining performance | Increased false negative risk |
| 29-32 | Very Low | Significantly reduced | High false negative rate |
| ≥ 33 | Extremely Low | 5.59% | Minimal detection capability |
This viral load dependency creates an important epidemiological trade-off: while antigen tests demonstrate high accuracy in detecting cases with high viral loads (who are most likely to be infectious), they miss a substantial proportion of cases with lower viral loads [4] [50]. This performance characteristic must be carefully considered when designing testing strategies for different public health objectives, whether for isolation of infectious individuals versus comprehensive surveillance.
Experimental Protocols for Diagnostic Validation
Standardized Comparative Study Design
Robust validation of diagnostic tests during emergencies requires methodologically sound comparative studies. The following protocol exemplifies a rigorous approach for evaluating antigen test performance against the gold standard PCR:
Sample Collection Methodology: Simultaneous collection of two nasopharyngeal swabs from symptomatic individuals. One swab is placed in viral transport medium (VTM) for PCR analysis and frozen at -80°C, while the other is tested immediately with the antigen test [4] [13]. This paired-sample design controls for variation in viral load across sampling sites and times.
PCR Validation Protocol: RNA extraction using validated kits (e.g., Loccus Biotecnologia Viral RNA and DNA Kit) in automated nucleic acid extractors (e.g., Extracta 32). Subsequent testing employs CDC-approved real-time RT-PCR diagnostic protocols using systems such as QuantStudio 5 with GoTaq Probe 1-Step RT-qPCR systems [4]. Samples are typically considered positive at Cq values <35, though lower thresholds may be applied depending on the clinical context [13].
Antigen Test Execution: Rapid immunochromatographic tests performed according to manufacturer specifications, with results typically available within 15-30 minutes [4] [13]. To maintain consistency, all antigen tests should be performed by trained personnel following standardized interpretation criteria, with blinding to PCR results to prevent assessment bias.
Statistical Analysis: Calculation of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and overall accuracy with 95% confidence intervals using statistical software such as RStudio [4]. Stratified analysis by symptom onset, vaccination status, age, and viral load (Cq values) provides crucial insights into context-dependent performance.
Validation Framework for Emergency Use
The validation process for diagnostic tests, whether laboratory-developed tests (LDTs) or commercial assays, must balance rigor with speed during public health emergencies. The following workflow outlines a comprehensive validation approach:
Diagram 1: Diagnostic Test Validation Workflow
This validation framework emphasizes several critical components:
Preliminary Considerations: Define the purpose of the assay, as all subsequent validation steps flow from this determination. Consider sample type (tissue, whole blood, CSF), potential inhibitors, and whether qualitative or quantitative results are needed [71]. The biological, technical, and operator-related factors that affect the assay's ability to detect the target in the specific sample-type must be evaluated.
Reference Materials and Sample Numbers: For LDTs, secure well-characterized positive control samples, typically 50-80 positive and 20-50 negative specimens (approximately 100 total) [71]. When genuine clinical samples are scarce, construct test samples by spiking various concentrations of the analyte into a suitable matrix. Include paired control specimens with low analyte concentrations, with and without known inhibitors.
Ongoing Quality Assurance: Establish continuous monitoring of internal and external positive controls to maintain the validated status of the assay [71]. Monitor for viral mutations that may affect primer/probe binding efficiency and necessitate test updates. Evaluate new buffers, enzymes, extraction kits, and probe chemistry as they become available.
Limitations and Challenges in Diagnostic Testing
Pre-Analytical and Analytical Vulnerabilities
Diagnostic accuracy depends heavily on factors beyond the test's inherent design, including pre-analytical variables that introduce vulnerabilities into testing pipelines:
Sample Collection Timing: Antigen test sensitivity is highest within the first 5-7 days of symptom onset when viral loads peak [4] [13]. Testing outside this window substantially increases false-negative rates, potentially missing cases that would be detected by more sensitive PCR methods.
Operator Competence and Workflow: Commercial test performance established in controlled settings may not translate to real-world implementation due to variations in staff competence, workflow systems, equipment maintenance schedules, and physical workspace configurations [71]. These operational factors can fundamentally affect assay performance but are rarely addressed in emergency use authorizations.
Genetic Drift and Antigen Escape: SARS-CoV-2 variants with mutations in the nucleocapsid (N) protein have demonstrated the ability to escape detection by antigen tests targeting this protein [50]. One study identified multiple disruptive amino-acid substitutions (including P365S, R209I, D348Y, M234I, and A376T) mapping within immunodominant epitopes that function as the target of capture antibodies in antigen tests [50]. This creates a selective pressure that may favor undetected spread of antigen-escape variants when antigen testing predominates without molecular confirmation.
Predictive Value Limitations in Dynamic Epidemics
The predictive values of diagnostic tests—crucial for clinical decision-making—demonstrate significant dependency on disease prevalence and uncertainty in prevalence estimates:
Prevalence Dependency: Positive Predictive Value (PPV) decreases substantially as disease prevalence declines, even when test sensitivity and specificity remain constant [72] [50]. At very low prevalence (0.1%), the PPV of antigen tests can fall below 50%, meaning most positive results are false positives [50]. This creates operational challenges in low-transmission settings where antigen tests may generate more misleading than helpful results.
Uncertainty in Prevalence Estimates: During emerging epidemics, incidence rates are highly uncertain due to variable pathogen penetration across communities, heterogeneous testing patterns, and asymptomatic transmission [72]. This uncertainty translates directly to unreliability in PPV and NPV estimates, complicating test interpretation and public health guidance.
Robustness Trade-Offs: Optimal estimates of PPV and NPV have zero robustness to uncertainty in prevalence (the "zeroing" property) [72]. A trade-off exists between robustness and error—requiring zero error in PPV provides zero robustness to prevalence uncertainty, while accepting modest error (e.g., 0.3) substantially increases robustness. This mathematical reality necessitates cautious interpretation of predictive values during evolving outbreaks.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Diagnostic Test Validation
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| Viral Transport Medium (VTM) | Preserves viral integrity during transport and storage | Standard VTM with protein stabilizers and antimicrobial agents |
| Automated Nucleic Acid Extraction Systems | Isolate viral RNA/DNA from clinical samples | Extracta 32 system; Viral RNA and DNA Kits (e.g., MVXA-P096FAST) |
| Real-Time PCR Instruments | Amplify and detect viral genetic material | QuantStudio 5; Rotor-Gene systems |
| PCR Master Mixes | Provide enzymes and reagents for amplification | GoTaq Probe 1-Step RT-qPCR system; manufacturer-specific mixes |
| Positive Control Materials | Verify test performance and sensitivity | Quantified viral RNA; inactivated virus; synthetic controls |
| External Quality Assessment Panels | Inter-laboratory comparison and proficiency testing | WHO international standards; commercially available panels |
| Reference Antigen Tests | Comparator for new test validation | WHO-listed tests meeting Target Product Profile (≥80% sensitivity, ≥97% specificity) |
This toolkit represents the essential components for establishing robust validation pipelines during emergency responses. The availability of well-characterized reagents, standardized protocols, and quality control materials forms the foundation for reliable diagnostic test performance assessment [71] [73].
Validation Frameworks for Future Pandemic Preparedness
Integrated Multi-Strain Surveillance System
The emergence of antigen-escape variants during the COVID-19 pandemic highlights the critical need for integrated surveillance systems that combine diagnostic testing with genomic sequencing:
Diagram 2: Integrated Surveillance for Variant Detection
This surveillance framework addresses a critical vulnerability identified during COVID-19: genomic surveillance systems that rely solely on antigen testing to identify samples for sequencing will systematically bias against detecting antigen-escape variants [50]. An integrated approach ensures that:
- Discordant Results Trigger Sequencing: Samples showing PCR-positive/antigen-negative results undergo prioritized genomic analysis to identify potential antigen-escape mutations [50].
- Representative Sampling: Sequencing selection includes random sampling from all positive cases, not just those identified through antigen testing, preventing systematic surveillance gaps.
- Adaptive Testing Strategies: Public health policies maintain flexibility to incorporate molecular testing for confirmatory purposes, particularly when emerging variants are suspected or prevalence patterns suggest diagnostic escape.
Temporal Validation Framework for Diagnostic Models
The highly dynamic nature of pandemics requires diagnostic validation frameworks that explicitly account for temporal evolution and dataset shift:
Multi-Time Period Partitioning: Divide data from multiple years into distinct training and validation cohorts to evaluate performance consistency across different phases of an epidemic [74]. This approach detects performance degradation as pathogens evolve and population immunity changes.
Temporal Characterization: Systematically track the evolution of patient demographics, symptoms, viral load distributions, and test performance metrics over time [74]. This monitoring identifies meaningful shifts in test operation characteristics that may necessitate recalibration or replacement.
Feature Importance Monitoring: Implement data valuation algorithms to identify features with stable predictive power versus those demonstrating temporal volatility [74]. In diagnostic contexts, this might include monitoring the stability of specific viral gene targets or the relationship between symptom patterns and test accuracy.
Longevity Assessment: Evaluate the trade-off between data quantity and recency by testing models trained on expanding time windows versus more recent data only [74]. This determines the optimal retraining frequency for diagnostic algorithms in rapidly evolving pandemic scenarios.
The COVID-19 pandemic provided a rigorous real-world validation of diagnostic technologies under pressure, revealing both remarkable adaptability and significant vulnerabilities in global diagnostic preparedness. The comparative performance data between antigen and PCR tests underscores that diagnostic choices must be context-dependent, balancing speed, sensitivity, scalability, and cost based on specific public health objectives. No single diagnostic modality will optimally serve all needs during a pandemic response.
The lessons learned highlight several critical requirements for future diagnostic validation pipelines: (1) standardized yet adaptable validation protocols that can be rapidly implemented during emergencies; (2) integrated surveillance systems that combine rapid testing with genomic sequencing to detect diagnostic escape variants; (3) robust frameworks for interpreting predictive values under conditions of prevalence uncertainty; and (4) temporal validation approaches that monitor and adapt to pathogen evolution and population dynamics.
Building on these foundations, future pandemic preparedness efforts must prioritize diagnostic pipelines that are not only accurate but also resilient, adaptable, and integrated within comprehensive public health response systems. The scientific toolkit and validation frameworks outlined here provide a roadmap for developing such robust diagnostic capabilities, potentially transforming our response to the inevitable emerging pathogens of the future.
Conclusion
The choice between antigen and PCR tests is not a simple binary but a strategic decision contingent on the clinical or public health objective. While PCR remains the undisputed gold standard for sensitivity, its operational limitations create a vital niche for rapid antigen tests, particularly in high-prevalence, high-transmission scenarios where speed and accessibility are paramount. The key to effective deployment lies in a clear understanding of antigen tests' limitations, especially their dramatically reduced sensitivity in asymptomatic individuals or during early/low-viral-load infection. Future directions must prioritize the development of novel technologies that bridge the performance-speed gap, the establishment of mandatory post-market surveillance to ensure real-world accuracy, and the creation of integrated diagnostic algorithms that leverage the complementary strengths of both methodologies to enhance pandemic preparedness and patient care.
References
- 1. Antigen testing vs PCR: less haste, more speed please [https://www.cepheid.com/en-US/insights/insight-hub/respiratory-health/2025/09/antigen-testing-vs-pcr-less-haste-more-speed-please.html]
- 2. Evaluation of RT-PCR assays for detection of SARS-CoV-2 ... [https://www.nature.com/articles/s41598-023-28275-y]
- 3. How Good are COVID-19 (SARS-CoV-2) Diagnostic PCR ... [https://www.cap.org/member-resources/articles/how-good-are-covid-19-sars-cov-2-diagnostic-pcr-tests]
- 4. Real-world accuracy of SARS-CoV-2 antigen detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12036026/]
- 5. Accuracy of Point-of-Care Rapid Antigen Tests for ... [https://www.aafp.org/pubs/afp/issues/2023/0400/cochrane-poc-rapid-antigen-tests-for-diagnosis-of-covid-19.html]
- 6. Development and evaluation of a multi-target droplet digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11095742/]
- 7. Ultrasensitive detection of clinical pathogens through a ... [https://www.nature.com/articles/s41467-025-59219-x]
- 8. PCR vs. rapid COVID-19 test: What's the difference? [https://www.osfhealthcare.org/blog/pcr-vs-rapid-covid-19-test-whats-the-difference]
- 9. Real-world accuracy of SARS-CoV-2 antigen detection ... [https://www.bjid.org.br/en-real-world-accuracy-sars-cov-2-antigen-detection-articulo-S1413867025000236]
- 10. Factors that Influence the Reported Sensitivity of Rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8524138/]
- 11. FDA Rapid Antigen COVID Tests Hold Up After Approval ... [https://globalbiodefense.com/2025/07/23/fda-covid-rapid-antigen-test-accuracy-review/]
- 12. Factors affecting the sensitivity of quantitative severe acute ... [https://www.sciencedirect.com/science/article/pii/S1341321X2300096X]
- 13. Comparison of a Commercial SARS-CoV-2 Rapid Antigen ... [https://www.idcmjournal.org/sars-cov-2-rapid-antigen-vs-pcr]
- 14. Preapproval and postapproval diagnostic test accuracy of ... [https://www.sciencedirect.com/science/article/pii/S1198743X25003490]
- 15. Comparative evaluation of RT-PCR and antigen-based ... [https://pubmed.ncbi.nlm.nih.gov/38683014/]
- 16. A Guide to Measuring and Optimizing System Performance [https://www.linkedin.com/pulse/benchmark-testing-guide-measuring-optimizing-system-performance-bvt9c]
- 17. Improving Real-world Antigen Test Sensitivity Estimation ... [https://www.medrxiv.org/content/10.1101/2024.10.25.24316137v1.full-text]
- 18. Diagnostic performance of rapid antigen tests for SARS ... [https://www.sciencedirect.com/science/article/abs/pii/S0735675723004898]
- 19. Estimating Antigen Test Sensitivity via Target Distribution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536919/]
- 20. Diagnostic performance and user-friendliness of five rapid ... [https://jlpm.amegroups.org/article/view/10318/html]
- 21. Real-World Performance of COVID-19 Antigen Tests [https://xmed.jmir.org/2025/1/e68376]
- 22. COVID-19 Guideline, Part 5: Antigen Testing [https://www.idsociety.org/practice-guideline/covid-19-guideline-antigen-testing/]
- 23. Comparative Analysis of RT-PCR and a Colloidal Gold ... [https://www.mdpi.com/2075-4418/15/11/1362]
- 24. Polymerase Chain Reaction (PCR) - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK589663/]
- 25. PCR Testing Explained: Applications, Benefits & Role [https://www.cpgr.org.za/pcr-testing-explained-applications-benefits-role-cpgr/]
- 26. Model for Interpreting Discordant SARS-CoV-2 Diagnostic Test Results - Volume 30, Number 2—February 2024 - Emerging Infectious Diseases journal - CDC [https://wwwnc.cdc.gov/eid/article/30/2/23-0200_article]
- 27. Comparison of the analytical and clinical sensitivities of 34 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502672/]
- 28. Evaluating Diagnostic Point-of-Care Tests in Resource-Limited Settings - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4016042/]
- 29. Antigen vs. Molecular: Benefits, Limitations, and Practical Considerations [https://www.physiciansofficeresource.com/articles/point-of-care-testing/antigen-vs-molecular/]
- 30. Performance of point-of care molecular and antigen-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9660861/]
- 31. Clinical Utility of Broad-Range PCR Testing and Impact ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11672430/]
- 32. Interim Guidance on the Use of Antiviral Medications for ... [https://www.cdc.gov/bird-flu/hcp/clinicians-evaluating-patients/interim-guidance-treatment-humans.html]
- 33. IDSA Guidelines on the Treatment and Management of ... [https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/]
- 34. Molnupiravir clinical trial simulation suggests that polymerase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578382/]
- 35. PCR Test: What It Is, How It Works & Results [https://my.clevelandclinic.org/health/diagnostics/21462-covid-19-and-pcr-testing]
- 36. Comparative Evaluation of Three Rapid Influenza Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11733857/]
- 37. Diagnostic Performance of a Combined Rapid Antigen Test for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12265398/]
- 38. Evaluation of Influenza A/B, SARS-CoV-2, and RSV Antigen ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.20944/preprints202511.0742.v1]
- 39. Comparison of rapid nucleic acid amplification tests and ... [https://www.sciencedirect.com/science/article/pii/S0735675725006333]
- 40. Performance evaluation of influenza a rapid antigen test ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11234145/]
- 41. Performance of SARS-CoV-2 rapid antigen test compared with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8088036/]
- 42. Diagnostic Accuracy of Rapid Antigen Tests for COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9021531/]
- 43. SARS-CoV-2 Viral Shedding and Rapid Antigen Test ... [https://www.cdc.gov/mmwr/volumes/73/wr/mm7316a2.htm]
- 44. Diagnostic accuracy of non-invasive SARS-CoV-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096796/]
- 45. Optimizing Tissue Sampling for the Diagnosis, Subtyping, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4170137/]
- 46. Free Guide: Top 5 PCR Optimization Tips - Yeasen [https://www.yeasenbio.com/blogs/molecular-biology/free-guide-top-5-pcr-optimization-tips]
- 47. Rapid Antigen Testing Market Size, Trends & Demand ... [https://www.futuremarketinsights.com/reports/rapid-antigen-testing-market]
- 48. The evolution of rapid antigen detection systems and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8234251/]
- 49. COVID-19 检测专家指南 [https://healthmatters.nyp.org/an-experts-guide-to-covid-19-testing-in-chinese/]
- 50. Impact of antigen test target failure and testing strategies ... [https://www.nature.com/articles/s41467-022-33460-0]
- 51. Comparison of a Commercial SARS-CoV-2 Rapid Antigen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11687234/]
- 52. Diagnostic performance of rapid antigen test for COVID-19 ... [https://www.sciencedirect.com/science/article/pii/S187603412100157X]
- 53. SARS-CoV-2 and NB.1.8.1 variant assessment - ECDC [https://www.ecdc.europa.eu/en/news-events/epidemiological-update-sars-cov-2-and-nb181-variant-assessment]
- 54. Immune imprinting toward SARS-CoV-2 XBB [https://www.nature.com/articles/s41392-025-02484-5]
- 55. Humoral immunity to current variants of SARS-CoV-2 in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505990/]
- 56. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 57. Preparation for blood tests: what can go wrong before the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377977/]
- 58. THE PREANALYTICAL ERRORS: A CONTINUOUS… [https://ascls.org/the-preanalytical-errors/]
- 59. Comparative Analysis of RT-PCR and a Colloidal Gold ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154499/]
- 60. RT-qPCR Testing and Performance Metrics in the COVID- ... [https://www.mdpi.com/1422-0067/25/17/9326]
- 61. Comparison of Rapid Antigen Test with RT-PCR for COVID ... [https://romj.org/2024-0210]
- 62. Real-world clinical performance of commercial SARS-CoV-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8127520/]
- 63. Evaluation of SARS-CoV-2 lateral flow device sensitivity [https://www.sciencedirect.com/science/article/pii/S2589537025003864]
- 64. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 65. The Usefulness of Antigen Testing in Predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9045251/]
- 66. Duration of viral infectiousness and correlation with ... [https://www.sciencedirect.com/science/article/pii/S1386653223000422]
- 67. Clinical comparison and agreement of PCR, antigen, and viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9300048/]
- 68. IDB | Independent Evaluation [https://www.iadb.org/en/who-we-are/independent-evaluation]
- 69. SCOPE Framework for Research Evaluation [https://inorms.net/scope-framework-for-research-evaluation/]
- 70. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 71. Validating Real-Time Polymerase Chain Reaction (PCR) Assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC7834634/]
- 72. Interpreting PPV and NPV of Diagnostic Tests with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11294685/]
- 73. COVID-19 antigen diagnostic test pipeline [https://www.path.org/who-we-are/programs/diagnostics/covid-dashboard-covid-19-antigen-diagnostic-test-pipeline/]
- 74. Diagnostic framework to validate clinical machine learning ... [https://www.nature.com/articles/s43856-025-00965-w]