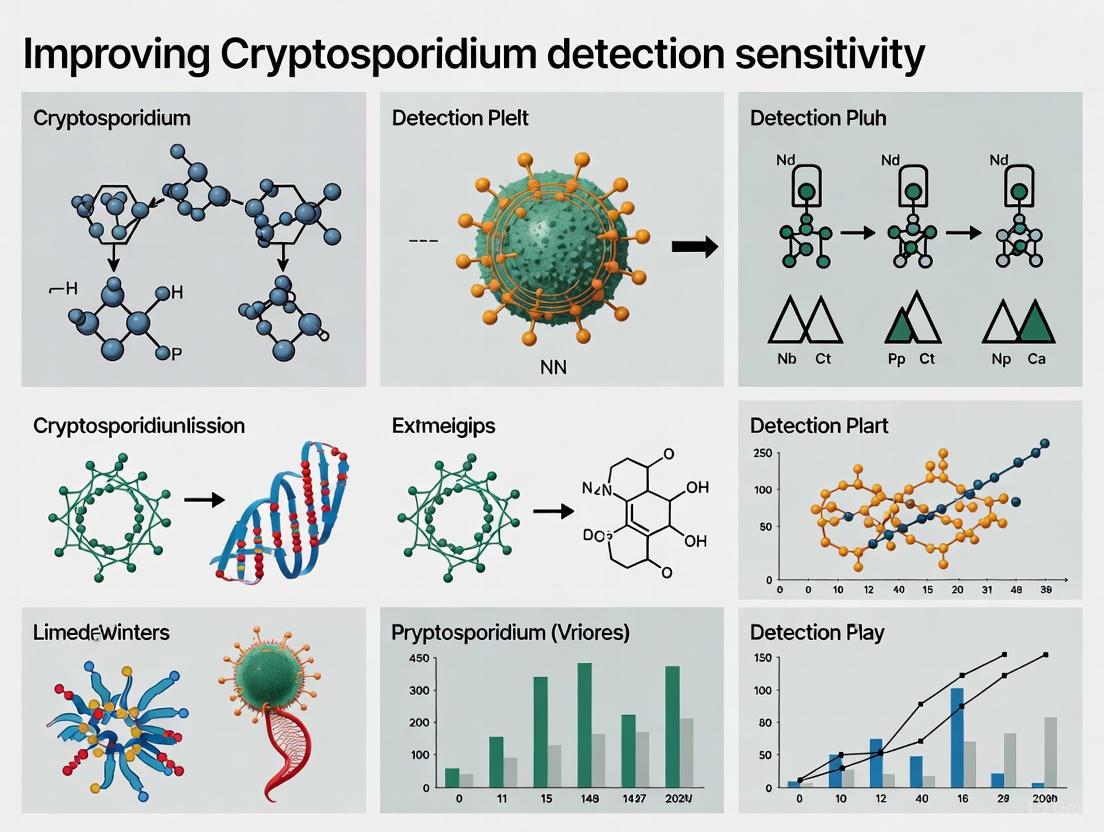
Advancing Cryptosporidium Detection: Strategies for Enhanced Sensitivity in Clinical and Research Settings
Cryptosporidium, a significant cause of diarrheal disease, has been historically underestimated due to the insensitivity of conventional diagnostic methods.
Advancing Cryptosporidium Detection: Strategies for Enhanced Sensitivity in Clinical and Research Settings
Abstract
Cryptosporidium, a significant cause of diarrheal disease, has been historically underestimated due to the insensitivity of conventional diagnostic methods. This article synthesizes recent evidence demonstrating how the shift to molecular techniques, such multiplex PCR panels, has dramatically improved detection rates and revealed the true endemicity of cryptosporidiosis. Tailored for researchers and drug development professionals, we explore the limitations of traditional microscopy and antigen tests, provide a comparative analysis of modern PCR methods, and detail optimized DNA extraction protocols. Furthermore, we discuss validation frameworks and troubleshooting strategies to maximize detection sensitivity for diverse Cryptosporidium species, ultimately aiming to support more accurate surveillance, outbreak control, and therapeutic development.
Unmasking a Hidden Pathogen: Why Traditional Cryptosporidium Detection Fails
The Global Health Burden of Cryptosporidiosis and the Impact of Underdiagnosis
Cryptosporidium, an obligate enteric protozoan parasite, is a leading cause of diarrheal illness worldwide, posing a significant threat to young children, immunocompromised patients, and individuals in resource-limited settings [1]. Despite its significant global health impact, cryptosporidiosis remains substantially underdiagnosed and underreported, creating a critical gap between its true burden and recorded incidence [2] [3]. This underascertainment stems from a complex interplay of factors including inadequate surveillance systems, suboptimal diagnostic practices, and varying clinical awareness across different healthcare settings [2]. For researchers dedicated to improving the sensitivity of Cryptosporidium detection, understanding this landscape is paramount. The development of novel diagnostic approaches must be contextualized within the realities of field conditions, resource constraints, and the biological peculiarities of this resilient pathogen. This article explores the global burden of cryptosporidiosis, analyzes the roots and consequences of underdiagnosis, and provides a technical toolkit to advance detection research, ultimately contributing to more accurate disease mapping and effective public health interventions.
The Global Health Burden of Cryptosporidiosis
The global impact of cryptosporidiosis is profound, with morbidity and mortality rates that underscore its significance as a public health priority, particularly in vulnerable populations.
Morbidity, Mortality, and Geographic Distribution
Cryptosporidiosis manifests as acute gastroenteritis, characterized by watery diarrhea, abdominal pain, and can lead to life-threatening complications in specific patient groups [3]. The burden is disproportionately high in developing countries, especially in sub-Saharan Africa, South America, and Asia, where it is a leading cause of moderate-to-severe gastrointestinal morbidity in children younger than 5 years [1] [4]. A study on the global burden of gastrointestinal disease found that Cryptosporidium spp. accounted for over 1 million deaths and more than 71 million disability-adjusted life years (DALYs) between 2005 and 2015, with nearly half of the fatalities occurring in children under five [1]. The Global Enteric Multicenter Study (GEMS) identified Cryptosporidium as responsible for an estimated 7.5 million annual cryptosporidiosis cases in regions with the highest mortality rates among young children [4].
In immunocompromised hosts, such as individuals with HIV/AIDS, cancer, or transplant recipients, the parasite causes a chronic, prolonged, and often fatal form of the disease, making it one of the riskiest opportunistic infections for these patients [3]. The parasite is also a significant concern in outbreak settings in developed nations, with a historic 1993 waterborne outbreak in Milwaukee affecting approximately 400,000 residents [1].
Table 1: Global Health Impact of Cryptosporidiosis
| Metric | Impact Figure | Affected Population | Source/Context |
|---|---|---|---|
| Annual Child Deaths | ~200,000 | Children globally | [4] |
| Total Deaths (2005-2015) | >1 million | All age groups, global | [1] |
| Annual Cases (High-Mortality Regions) | 7.5 million | Children under 5 | GEMS Study [4] |
| Disability-Adjusted Life Years (DALYs, 2005-2015) | >71 million | All age groups, global | [1] |
| Waterborne Outbreak (Single Incident) | ~400,000 | Milwaukee residents | 1993 outbreak [1] |
Long-Term Consequences in Children
Beyond acute diarrhea and mortality, cryptosporidiosis has devastating long-term sequelae, particularly in children. Infections are strongly associated with malnutrition, growth shortfalls (stunting), and poor neurological development [2] [4]. Even symptomatic infections with C. parvum in young children are often heavy and associated with growth shortfalls [2]. The parasite creates a vicious cycle: diarrhea and enteric inflammation lead to malnutrition, which in turn increases susceptibility to future Cryptosporidium infections and other pathogens, further impairing a child's developmental trajectory [4].
The Challenge of Underdiagnosis
The true incidence of cryptosporidiosis is believed to be significantly higher than reported cases, with estimates suggesting the actual frequency of infection may be 100-fold higher than official figures [3]. This underdiagnosis is multi-factorial.
Limitations in Diagnostic Practices and Standards
A primary driver of underdiagnosis is the lack of international standard methods for diagnosis and widespread reliance on suboptimal diagnostic techniques [1]. Microscopy, often considered the "gold standard," is limited by its labor-intensive nature, requirement for skilled technicians, and inadequate sensitivity, leading to false negatives [1] [5]. Furthermore, expertise in stool microscopy is declining in modern clinical laboratories [1].
Diagnostic practices are also hampered by inconsistent testing criteria. In many countries, screening is not routine and is often dependent on clinician request or specific patient criteria, such as age or immune status [1] [3]. For instance, some protocols recommend testing only patients under a specific age threshold (e.g., 10 or 15 years) for sporadic cases, which can miss a large proportion of infections in adults, as evidenced by an outbreak in Galway, Ireland, where 40% of infections occurred in patients over 15 [1]. This age bias significantly impacts reported age distribution and underestimates the burden in adult populations [1].
Biological and Environmental Factors
The biology of Cryptosporidium and the environments it contaminates also complicate detection.
- Low Infectious Dose & High Shedding: The low infectious dose (10–30 oocysts) means even minimal environmental contamination can cause disease, while infected individuals can shed vast numbers of oocysts (up to 10^9 per bowel movement) for weeks after symptoms cease, facilitating spread but complicating source identification [2].
- Environmental Resilience: The oocysts are small, environmentally robust, and highly resistant to common water disinfectants like chlorine, making them persistent in water supplies and difficult to eradicate [2] [3].
- Non-Specific Symptoms: The watery diarrhea caused by Cryptosporidium is clinically similar to that caused by other bacterial, viral, and parasitic enteric pathogens, leading to misdiagnosis if proper pathogen-specific testing is not conducted [3].
Table 2: Key Factors Contributing to the Underdiagnosis of Cryptosporidiosis
| Category | Factor | Impact on Diagnosis |
|---|---|---|
| Diagnostic Practices | Reliance on insensitive microscopy | High false-negative rate, need for skilled technicians |
| Lack of standardized international protocols | Inconsistent testing and reporting across regions | |
| Use of restrictive testing criteria (e.g., age limits) | Misses infections in demographic groups outside criteria | |
| Declining microscopy expertise | Reduced diagnostic accuracy in clinical labs | |
| Clinical Presentation | Non-specific symptoms (watery diarrhea) | Misattribution to other more common enteric pathogens |
| Asymptomatic infections | Cases go entirely unreported and undetected | |
| Pathogen Biology | Intermittent shedding of oocysts | Single stool sample may yield false negative; requires multiple samples |
| Resistance to common disinfectants (e.g., Chlorine) | Increased environmental persistence and exposure risk |
Technical Guide: Advancing Detection Sensitivity
For researchers aiming to improve diagnostic sensitivity, understanding and optimizing current and emerging methodologies is crucial. The field is gradually shifting from traditional microscopy to molecular and immunoassay-based techniques.
Research Reagent Solutions for Cryptosporidium Detection
A critical step in enhancing detection is the selection of appropriate reagents and materials. The following table details key components used in advanced detection workflows.
Table 3: Essential Research Reagents for Cryptosporidium Detection and Analysis
| Reagent / Material | Primary Function | Application in Research/Diagnostics |
|---|---|---|
| Immunomagnetic Separation (IMS) Beads | Coated with anti-Cryptosporidium antibodies to selectively capture and concentrate oocysts from complex samples. | Sample preparation for water testing; purifies oocysts prior to downstream analysis (microscopy, PCR). [5] |
| Fluorochrome-labeled Monoclonal Antibodies (e.g., MERIFLUOR, EasyStain) | Bind specifically to surface antigens on oocysts/cysts for visualization via immunofluorescence. | Gold-standard for detection in water samples (EPA Method 1623) and clinical DFA tests; allows for differentiation from debris. [5] |
| PCR Primers (e.g., COWP, SSU rRNA genes) | Amplify Cryptosporidium-specific DNA sequences via Polymerase Chain Reaction. | Molecular detection and identification; nested PCR targeting COWP gene is highly sensitive. [6] |
| ColorSeed / EasySeed | Internal process control containing inactivated oocysts that fluoresce differently from wild types. | Quality control; added to samples to monitor and validate the entire detection process (from filtration to staining), confirming test efficacy. [5] |
| CRISPR/Cas Components | Enable precise genetic modification or nucleic acid detection. | Emerging research: creating tractable parasites for study [1] and developing novel, highly specific diagnostic assays. |
Comparative Analysis of Diagnostic Methodologies
Evaluating the performance characteristics of different diagnostic methods is key to selecting and improving assays.
Table 4: Comparison of Cryptosporidium Detection Methods
| Method | Target | Advantages | Disadvantages / Limitations | Reported Sensitivity (Example) |
|---|---|---|---|---|
| Microscopy with Staining (Ziehl-Neelsen, Auramine) | Oocyst morphology | Low cost, widely available. | Labor-intensive, requires expertise, low sensitivity, poor species differentiation. | Variable, generally low [1] [3] |
| Immunofluorescence Assay (IFA/DFA) | Oocyst surface antigens | Higher sensitivity & specificity than basic stains, considered gold standard for water testing. | Requires fluorescent microscope, antibody cost. | Higher than conventional stains [5] |
| Enzyme Immunoassay (EIA) | Soluble fecal antigens | Higher throughput, easier to perform, good for screening. | Cannot determine species, less sensitive than DFA/PCR. | Good for clinical screening [5] |
| PCR (Standard) | Cryptosporidium DNA | High specificity, potential for species identification. | Requires lab infrastructure, risk of inhibition. | ~10^3 to 10^4 oocysts [6] |
| Nested PCR | Cryptosporidium DNA | Very high sensitivity and specificity. | High contamination risk, more time-consuming. | 1 to 100 oocysts (COWP gene most sensitive) [6] |
| Real-Time PCR | Cryptosporidium DNA | Quantification, fast, reduced contamination risk. | Requires expensive equipment, complex reagent design. | Highly sensitive, comparable to nested PCR [5] |
Workflow for Molecular Detection and Subtyping in Water
Detecting Cryptosporidium in water matrices requires concentrating the parasite from large volumes followed by sensitive detection and identification methods. The following workflow outlines a standard and advanced pathway for water analysis.
This workflow highlights the critical steps, from processing large water volumes to final identification. The molecular path is essential for outbreak investigation and transmission studies, as it allows researchers to identify the specific species and subtypes (e.g., C. hominis IeA11G3T3) responsible for infections, which is not possible with standard microscopy [5] [7].
Troubleshooting Common Issues in Detection
Researchers often encounter specific challenges when working with Cryptosporidium detection. This FAQ addresses common problems and proposes solutions.
FAQ 1: How can I improve the sensitivity of PCR for detecting low oocyst numbers?
- Problem: Standard single-round PCR lacks the sensitivity for environmental samples with very low oocyst counts.
- Solution: Implement a nested PCR protocol. Research demonstrates that nested PCR, particularly using primer sets targeting the Cryptosporidium oocyst wall protein (COWP) gene, significantly enhances sensitivity, enabling detection of as few as 1 to 10 oocysts compared to 10^3-10^4 for standard PCR [6]. Always include appropriate controls (positive, negative, and extraction) to monitor for contamination, a major risk with nested PCR.
FAQ 2: What is the best way to control for assay efficiency when testing complex samples like water or stool?
- Problem: Inhibitory substances in sample matrices can lead to false-negative results in both molecular and microscopy-based assays.
- Solution: Use an internal process control such as ColorSeed. This product contains inactivated oocysts that fluoresce a different color (red) than wild-type oocysts (green) in DFA tests. By spiking it into every sample, you can validate that the entire process—from filtration and IMS to staining and microscopy—has worked efficiently, confirming that negative results are true negatives [5].
FAQ 3: Our lab primarily uses microscopy. How can we transition to molecular methods confidently?
- Problem: Declining microscopy expertise and the desire for higher throughput and sensitivity are driving a shift to molecular methods, but validation is challenging.
- Solution: Phase in molecular methods alongside your existing microscopy protocol for a period of parallel testing. Begin with validated commercial PCR kits or establish in-house assays targeting well-characterized genes like SSU rRNA or gp60 [6] [5]. Utilize proficiency panels or archived clinical samples to compare the sensitivity and specificity of the new molecular method against your current standard, ensuring a smooth and validated transition.
FAQ 4: Why is species/subtype identification important, and how is it achieved?
- Problem: Genus-level detection provides limited epidemiological insight into transmission dynamics.
- Solution: Species and subtype identification is crucial for tracking outbreaks and understanding zoonotic versus anthroponotic transmission. This is achieved molecularly. After a positive PCR, techniques such as restriction fragment length polymorphism (RFLP) analysis or Sanger sequencing of the gp60 gene are used for subtyping [5] [7]. Multi-locus sequence typing (MLST) provides even higher resolution for tracking emerging subtypes, such as the recently dominant C. hominis IeA11G3T3 [7].
Cryptosporidiosis represents a severe and ongoing global health challenge, disproportionately affecting children and immunocompromised individuals. The chasm between its true burden and reported cases, driven by significant underdiagnosis, undermines effective public health responses and resource allocation. For the research community, this highlights an urgent need and a clear opportunity. Advancing beyond traditional diagnostic limitations through the adoption and refinement of sensitive molecular techniques, robust reagent systems, and standardized workflows is critical. By improving detection sensitivity and specificity, researchers can provide a more accurate picture of the epidemiology of Cryptosporidium, which is the foundational step toward developing better treatments, control measures, and prevention strategies to alleviate the global burden of this neglected disease.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary limitations of microscopy for Cryptosporidium detection? Microscopy, particularly using modified acid-fast stains like Ziehl-Neelsen, faces significant limitations in sensitivity and operator dependency. Its sensitivity can be as low as 75-84% compared to molecular methods, and it often fails to detect infections with low oocyst shedding ( [8] [9]). The method is time-consuming, requires experienced personnel to accurately identify oocysts, and can yield false positives due to misinterpretation of other objects like yeast cells ( [10] [11] [9]). Furthermore, microscopy cannot differentiate between Cryptosporidium species, which is crucial for outbreak investigation and understanding transmission dynamics ( [10] [11]).
FAQ 2: How reliable are antigen-based tests for Cryptosporidium? The reliability of antigen tests (ELISA, Immunochromatographic tests) is variable. While they often show high specificity (98-100%), their sensitivity can be unacceptably low. One study reported sensitivities of 63.6% for EIA, 40.9% for ELISA, and 22.7% for an immunochromatographic test (ICT) when compared to PCR ( [12]). Another evaluation of a rapid test showed sensitivity dropped from 74% to 62% when microscopy was extended to find samples with very low oocyst numbers ( [8]). This indicates that antigen tests may miss a substantial number of true infections, especially in cases of low parasite burden.
FAQ 3: Why is PCR considered superior to conventional methods for detection? PCR is considered superior due to its high sensitivity and specificity, often reaching 100% in clinical trials ( [10] [11]). It can detect Cryptosporidium at very low oocyst concentrations (as low as 1-10 oocysts per gram of fecal sample) and is capable of genotyping the parasite directly from clinical samples ( [13] [11] [14]). This allows researchers to distinguish between species like C. hominis and C. parvum, providing vital data for molecular epidemiology and source tracking during outbreaks ( [10] [14]).
Troubleshooting Guides
Issue 1: Low Sensitivity in Microscopic Examination
Problem: Consistent failure to detect low-intensity infections, leading to false-negative results.
Solution:
- Protocol Enhancement: Implement a formalin-ether or formol-ether sedimentation concentration step prior to staining. This increases the yield of oocysts from fecal debris. Centrifuge at higher speeds (up to 1200 x g) for better oocyst recovery, though this may not be suitable if also checking for helminth eggs ( [9] [15]).
- Alternative Staining: Use fluorescent stains like auramine-phenol. This method is more sensitive than modified acid-fast staining and is recommended as a rapid screening tool. Positive results can be confirmed with Ziehl-Neelsen stain ( [9] [15]).
- Extended Examination: If using acid-fast stains, scan slides for an extended period (>10 minutes) as low-density infections can be missed with routine screening times ( [8]).
Issue 2: Variable Performance and False Negatives in Antigen Tests
Problem: Immunoassays (EIA, ELISA, ICT) produce false-negative results, particularly with different Cryptosporidium species or low oocyst counts.
Solution:
- Confirmatory Testing: Do not rely on a single antigen test as the sole diagnostic method. Any negative result from a rapid test in a high-prevalence population or from an immunocompromised patient should be confirmed by a more sensitive method, such as PCR or immunofluorescence microscopy ( [12] [8]).
- Understand Kit Limitations: Be aware that commercial antibodies are often raised against C. parvum. Species with variable oocyst wall epitopes (e.g., C. muris, C. andersoni) may fluoresce less intensely or not be detected at all, leading to false negatives ( [12] [9]).
Issue 3: Overcoming PCR Inhibition in Fecal Samples
Problem: PCR amplification is inhibited by substances in fecal samples, leading to false-negative results.
Solution:
- Optimized DNA Extraction: Use a robust DNA extraction method. The glass beads DNA extraction method has demonstrated higher sensitivity (100%) compared to a freeze-thaw method using liquid nitrogen (83%) ( [13]).
- Inhibition Control: Include an internal control in each PCR reaction. Spiking sample DNA with a known amount of control DNA can help identify reactions where inhibition is occurring ( [10] [14]).
- Additive Use: Incorporate additives like polyvinylpolypyrrolidone (PVPP) during the initial extraction phase. PVPP has been shown to reduce PCR inhibition by binding polyphenolic compounds ( [11]).
Comparative Performance Data
The table below summarizes the performance characteristics of different Cryptosporidium detection methods as reported in the literature.
Table 1: Comparison of Cryptosporidium Detection Methods
| Method | Reported Sensitivity | Reported Specificity | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Microscopy (ZN stain) | 75.8% - 83.7% [16] [10] | 98.9% - 99.3% [10] [16] | Low reagent cost; indicates active infection [8] [9] | Low sensitivity; operator-dependent; no genotyping [10] [9] |
| Immunofluorescence (DFA) | Higher than ZN stain [9] | High [9] | High sensitivity & specificity combination [9] | Requires fluorescent microscope; more expensive [9] |
| Antigen Test (ELISA/EIA) | 40.9% - 95.35% [12] [16] | 75.9% - 100% [12] [8] | Faster than microscopy; batch processing [10] [9] | Highly variable sensitivity; species-dependent [12] [9] |
| Antigen Test (RDT/ICT) | 22.7% - 74% [12] [8] | 100% [12] | Very rapid; easy to use [8] | Poor sensitivity, misses low-shed infections [12] [8] |
| PCR | 100% [10] [11] | 100% [10] [11] | Highest sensitivity; enables genotyping [10] [14] | Higher cost; requires specialized equipment [10] [11] |
Table 2: Performance of Three Commercial Immunoassays in Animal Samples (n=79) [12]
| Test Type | Sensitivity | Specificity | Notes |
|---|---|---|---|
| Enzyme Immunoassay (EIA) | 63.6% | 75.9% | Questionable samples considered positive. |
| Enzyme-Linked Immunosorbent Assay (ELISA) | 40.9% | 78.9% | Questionable samples considered positive. |
| Immunochromatographic Test (ICT) | 22.7% | 100% | Questionable samples considered positive. |
Experimental Protocols
Detailed Protocol 1: PCR Detection with Glass Bead DNA Extraction
This protocol is adapted from methods that showed high sensitivity for detecting Cryptosporidium in fecal samples [13].
- Sample Preparation: Homogenize 100 mg of stool sample with 0.5 mm glass beads, 1.0 mm zircon beads, and 300 μL of lysis solution in a homogenizer at 6500 rpm for 90 seconds.
- DNA Extraction: Extract genomic DNA from the homogenate using a commercial DNA extraction kit. The glass beads method is superior to freeze-thaw for breaking oocyst walls.
- Nested PCR (First Round):
- Target: 18S SSU rRNA gene.
- Reaction Mix: 50 μL total volume, containing 5 μL of DNA sample, 0.2 μM primers, and 5U Taq DNA polymerase.
- Cycling Conditions:
- Initial Denaturation: 95°C for 5 min
- 35 Cycles: 95°C for 1 min, 61°C for 1 min, 72°C for 2 min
- Final Elongation: 72°C for 7 min
- Nested PCR (Second Round):
- Use 1-5 μL of the primary PCR product as a template.
- Use internal primers and repeat the cycling conditions, but with an annealing temperature of 57°C.
- Analysis: Evaluate the secondary PCR product by electrophoresis on an agarose gel and visualize under UV light. A ~350 bp band indicates a positive result.
Detailed Protocol 2: Modified Acid-Fast Staining (Ziehl-Neelsen)
This is the conventional method for oocyst detection, but its limitations must be acknowledged [8] [9].
- Smear Preparation: Prepare a thin smear of concentrated or unconcentrated stool on a glass slide. Air dry and fix with absolute methanol for 10 minutes.
- Staining: Flood the slide with carbol fuchsin stain and allow it to sit for 15 minutes. Rinse gently with deionized water.
- Decolorize: Apply 1% acid-alcohol for 15 seconds to 1 minute, then rinse. This is a critical step that requires optimization based on smear thickness.
- Counterstain: Flood the slide with 0.5% methylene blue counterstain for 30 seconds to 4 minutes. Rinse and air dry.
- Microscopy: Examine under oil immersion (100x objective). Cryptosporidium oocysts stain bright red against a blue-green background. A minimum of 5-10 minutes of examination per slide is recommended.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for Cryptosporidium Research
| Item | Function/Application | Example Use |
|---|---|---|
| Glass Beads (0.5mm) | Mechanical disruption of tough oocyst walls for DNA release. | Used in optimized DNA extraction protocols for PCR [12] [13]. |
| Polyvinylpolypyrrolidone (PVPP) | Binds polyphenolic compounds in feces that inhibit PCR. | Added to fecal suspensions before DNA extraction to reduce PCR inhibition [11]. |
| Biotinylated Monoclonal Antibodies | Specific capture and detection of oocysts. | Used in immunoassays and advanced biosensor development [17]. |
| Formalin-Ethyl Acetate | Sedimentation solution for concentrating parasites from stool. | Used in the formalin-ethyl acetate sedimentation method to increase oocyst yield prior to microscopy [9] [15]. |
| Primers targeting 18S SSU rRNA | Amplification of a conserved and specific genetic marker. | Used in nested PCR protocols for highly sensitive detection and genotyping of Cryptosporidium [12] [13]. |
| Tripropylborane | Tripropylborane | High-Purity Organoboron Reagent | Tripropylborane for research: An organoboron compound for organic synthesis & cross-coupling. For Research Use Only. Not for human or veterinary use. |
| 5-Phenylisatin | 5-Phenylisatin, CAS:109496-98-2, MF:C14H9NO2, MW:223.23 g/mol | Chemical Reagent |
Workflow Diagram: Method Selection for Cryptosporidium Detection
The following diagram outlines a decision-making workflow for selecting a detection method based on research objectives and resources.
Diagram 1: Method selection workflow for Cryptosporidium detection.
Prior to 2021, cryptosporidiosis was considered a rare and primarily travel-associated disease in Denmark. This perception shifted dramatically with the adoption of gastrointestinal syndromic PCR panels in local hospitals, which revealed a previously hidden endemic situation [18]. This case study examines how the transition from traditional microscopy to molecular testing uncovered the true scope of Cryptosporidium transmission in Denmark, transforming public health understanding of this enteric pathogen.
The Danish experience provides a powerful example of how diagnostic evolution can directly impact disease surveillance and public health priorities. Between 2010 and 2024, comprehensive analysis of identified cases revealed striking patterns: after 2021, case numbers increased substantially, with Cryptosporidium detected in >2% of patients tested during seasonal peaks (August-October) [18].
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: Why did Cryptosporidium cases in Denmark increase so dramatically after 2021? A: The increase was primarily attributable to improved detection capabilities rather than a true epidemic. The adoption of gastrointestinal syndromic PCR panels in several Danish hospitals significantly enhanced testing sensitivity and scope [18]. These molecular tests were applied to more patients, including those without recent travel history, revealing an endemic situation that had previously been underestimated.
Q2: What are the key advantages of molecular methods over microscopy for Cryptosporidium detection? A: Molecular methods, particularly PCR and nested PCR, offer several advantages:
- Higher sensitivity: Capable of detecting as few as 1-10 oocysts compared to 10,000-50,000 for microscopy [11] [19]
- Species differentiation: Can distinguish between C. parvum, C. hominis, and other zoonotic species [18] [19]
- Reduced operator dependence: Less affected by variations in technical expertise [1]
- Automation potential: Adaptable to high-throughput screening [1]
Q3: What factors might cause false-negative results in PCR-based Cryptosporidium detection? A: Common issues include:
- PCR inhibition from fecal components like hemoglobin derivatives and bile acids [19]
- Inefficient oocyst disruption during DNA extraction [19]
- Insufficient DNA recovery from low oocyst numbers [20]
- Primer mismatches with uncommon Cryptosporidium species [19]
Q4: How can researchers optimize oocyst recovery from environmental samples? A: Sucrose flotation methods have demonstrated superior analytical sensitivity, capable of detecting as few as 10 oocysts. Combining this with spin column DNA extraction and PCR-hybridization provides a robust detection system for environmental samples [20].
Troubleshooting Guides
Problem: Inconsistent PCR results with low oocyst numbers
| Possible Cause | Solution | Verification Method |
|---|---|---|
| PCR inhibition from fecal samples | Add polyvinylpolypyrrolidone (PVPP) during extraction; use dilution schemes [11] | Include internal positive control; test spiked samples [20] |
| Inefficient oocyst disruption | Incorporate freeze-thaw cycles (5+ cycles) or bead beating [19] [21] | Compare DNA yield with/without disruption step |
| Suboptimal primer selection | Use nested PCR targeting COWP gene for enhanced sensitivity [19] | Test primer sets against serial oocyst dilutions |
Problem: Inability to differentiate Cryptosporidium species
| Solution | Protocol | Expected Result |
|---|---|---|
| Implement GP60 gene sequencing | Amplify GP60 region, sequence products, and compare to reference sequences [22] | Identification of subtype families and zoonotic potential |
| Use real-time PCR with melting curve analysis | Perform real-time PCR followed by melting curve analysis for species discrimination [20] | Distinct melting temperatures for different species |
| Apply fragment analysis | Use fluorescently labeled primers for microsatellite analysis [23] | High-resolution genotyping with 100% concordance to sequencing |
Experimental Protocols & Methodologies
Nested PCR for Enhanced Cryptosporidium Detection
This protocol, adapted from methods used in sensitivity comparisons, detects low oocyst numbers in clinical and environmental samples [19].
Principle: Two rounds of PCR amplification using outer and inner primer sets targeting the Cryptosporidium oocyst wall protein (COWP) gene provide enhanced sensitivity and specificity.
Reagents:
- Lysis buffer (e.g., ASL buffer from QIAquick stool mini kit)
- Proteinase K
- Primers: Outer set (Cry-15/Cry-19); Inner set (cowpnest-F1/cowpnest-R2)
- PCR master mix with Taq polymerase
- Agarose gel electrophoresis materials
Procedure:
- DNA Extraction:
- Suspend 10^7 oocysts in ASL lysis buffer
- Incubate at 70°C for 30 minutes
- Extract DNA using commercial kits per manufacturer's instructions [19]
Primary PCR:
- Prepare 50μL reaction with: 5μL template DNA, 10mM Tris-HCl (pH 8.3), 2.5mM MgCl₂, 200μM dNTPs, 25pmol each outer primer, 2.5U Taq polymerase
- Cycling: Initial denaturation 94°C/5min; 30 cycles of 94°C/50s, 55°C/30s, 72°C/50s; Final extension 72°C/10min
Nested PCR:
- Use 2μL of purified primary PCR product as template
- Reaction composition similar to primary PCR but with inner primers
- Cycling: Same as primary PCR but with annealing at 52°C
Analysis:
- Electrophorese 10μL nested PCR product on 1.5% agarose gel
- Visualize 311bp product under UV light [19]
Expected Results: This nested PCR approach can detect as few as 1 oocyst, significantly enhancing sensitivity over single-round PCR (10^3-10^4 oocysts) [19].
Sucrose Flotation Method for Oocyst Recovery
This method optimizes oocyst recovery from environmental samples prior to molecular detection [20].
Principle: Differential density separation concentrates oocysts while reducing PCR inhibitors.
Reagents:
- Sucrose flotation solution (specific gravity 1.18)
- PBS (pH 7.2)
- Washing buffer
- DNA extraction reagents
Procedure:
- Sample Processing:
- Homogenize 1g soil/feces or 10mL water sample
- Centrifuge at 1500 × g for 10 minutes
- Resuspend pellet in 10mL PBS
Flotation:
- Mix sample with equal volume sucrose solution
- Centrifuge at 1000 × g for 10 minutes
- Carefully transfer top layer to new tube
Washing:
- Add 10mL PBS to recovered fraction
- Centrifuge at 1500 × g for 10 minutes
- Repeat washing step twice
DNA Extraction:
- Proceed with DNA extraction using commercial kits
- Include internal positive control to detect PCR inhibition [20]
Performance: This method provides the greatest analytical sensitivity, detecting as few as 10 oocysts in feces and soil, and even fewer in water samples [20].
Data Presentation: Comparative Method Performance
Detection Sensitivity of Diagnostic Methods
Table 1: Comparison of Cryptosporidium detection methods and their performance characteristics
| Method | Detection Limit | Species Identification | Hands-on Time | Cost/Test | Best Application |
|---|---|---|---|---|---|
| Microscopy (acid-fast) | 10^4-10^5 oocysts [11] | No | 15-30 minutes [11] | ~$0.30 [11] | Resource-limited settings |
| Immunofluorescence | 10^3 oocysts [15] | No | 20-40 minutes | ~$2.50 | Clinical diagnostics |
| Conventional PCR | 10^3-10^4 oocysts [19] | Limited | 60-90 minutes | ~$2.57 [11] | Batch screening |
| Nested PCR (COWP) | 1-10 oocysts [19] | Yes | 90-120 minutes | ~$4.00 | Research, outbreak tracing |
| Real-time PCR | 10-100 oocysts [20] | Yes | 60-90 minutes | ~$5.00 | High-throughput testing |
Cryptosporidium Species Distribution in Denmark
Table 2: Species diversity of Cryptosporidium identified in Danish cases (2010-2024) after implementation of molecular testing [18]
| Species | Percentage of Cases | Zoonotic Potential | Clinical Significance |
|---|---|---|---|
| C. parvum | 56.9% | High (cattle) | Moderate-severe diarrhea |
| C. hominis | 11.3% | Low (human-adapted) | Moderate-severe diarrhea |
| C. mortiferum | 2.5% | Unknown | Associated with diarrhea |
| C. meleagridis | 1.7% | Medium (birds) | Diarrhea, extraintestinal cases |
| C. felis | 1.2% | Medium (cats) | Diarrhea, immunocompromised hosts |
| C. erinacei | 0.8% | Medium (hedgehogs) [23] | Diarrhea |
| Other/Unknown | 25.6% | Variable | Variable |
Visualizations
Molecular Detection Workflow
Diagnostic Transition Impact
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential reagents and materials for Cryptosporidium detection research
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Sucrose flotation solution (sp. gr. 1.18) | Oocyst concentration from environmental samples | Superior recovery compared to NaCl flotation [20] |
| PVPP (Polyvinylpolypyrrolidone) | PCR inhibitor removal | Add during DNA extraction to reduce false negatives [11] |
| COWP gene primers (cowpnest-F1/R2) | Nested PCR amplification | Highest sensitivity for C. parvum detection [19] |
| GP60 gene sequencing primers | Subtyping and species identification | Essential for molecular epidemiology [22] |
| Internal positive control DNA | PCR inhibition monitoring | Critical for validating negative results [20] |
| Commercial DNA extraction kits | Nucleic acid purification | Spin column methods provide consistent yield [20] |
| Modified acid-fast stain | Microscopic visualization | Traditional method with variable sensitivity [15] |
| Immunofluorescence antibodies | Microscopic detection | Higher sensitivity than acid-fast stains [15] |
| Ammonia soap | Ammonium Oleate|CAS 544-60-5|For Research | Ammonium Oleate is the ammonium salt of oleic acid, used as a surfactant and emulsifier in research. This product is for research use only (RUO). Not for personal use. |
| Cefoxitin Dimer | Cefoxitin Dimer|RUO|Analytical Standard | Cefoxitin Dimer for Research Use Only. An impurity of the antibiotic Cefoxitin. Not for human or veterinary diagnostic or therapeutic use. |
The Danish experience demonstrates that diagnostic methodology directly shapes understanding of disease epidemiology. The transition to molecular testing revealed that cryptosporidiosis is a common, endemic disease in Denmark with surprising species diversity, rather than a rare travel-associated infection [18]. This paradigm shift underscores how technological advancements in pathogen detection can radically alter public health priorities and resource allocation.
For researchers, the key lessons include:
- Molecular methods, particularly nested PCR targeting the COWP gene, provide superior sensitivity for Cryptosporidium detection [19]
- Genetic diversity analysis at the GP60 locus can serve as an indicator of disease incidence and transmission dynamics [22]
- Comprehensive testing algorithms should account for the wide heterogeneity of Cryptosporidium species in human infections [18]
Future directions should focus on developing point-of-care molecular tests that maintain the sensitivity of laboratory-based PCR while offering rapid results for clinical decision-making. The integration of genetic data with epidemiological surveillance will continue to refine our understanding of Cryptosporidium transmission patterns and inform targeted intervention strategies.
The Wide Heterogeneity of Cryptosporidium Species and Its Diagnostic Implications
Cryptosporidium is a protozoan parasite causing the diarrheal disease cryptosporidiosis. The genus encompasses remarkable species diversity, with nearly 40 valid species exhibiting marked differences in host range [24]. This heterogeneity presents significant challenges for detection, diagnosis, and epidemiological tracking. While Cryptosporidium parvum and C. hominis remain the primary human pathogens, numerous other species including C. meleagridis, C. felis, C. canis, C. ubiquitum, C. mortiferum, and C. erinacei can also infect humans [18] [15]. The recent implementation of enhanced detection methods in Denmark revealed a surprising diversity of Cryptosporidium species in human infections, with C. parvum (56.9%), C. hominis (11.3%), C. mortiferum (2.5%), C. meleagridis (1.7%), C. felis (1.2%), and C. erinacei (0.8%) all identified in clinical samples [18]. This wide heterogeneity complicates diagnostic approaches and necessitates techniques that can identify multiple species simultaneously.
Frequently Asked Questions (FAQs)
Q1: Why is species-level identification of Cryptosporidium important for public health?
Species-level identification is crucial for understanding transmission dynamics and implementing effective control measures. Different Cryptosporidium species have varying host ranges, virulence characteristics, and potential zoonotic significance. For instance, C. hominis is primarily anthroponotic (transmitted between humans), while C. parvum has a wide host range with calves being a major reservoir for human infections [15] [24]. Identifying the specific species involved in outbreaks helps pinpoint contamination sources and guides appropriate public health interventions. Recent research from Denmark demonstrated that most cases had no history of travel outside the country, suggesting endemic transmission previously unrecognized due to diagnostic limitations [18].
Q2: What are the main methodological challenges in Cryptosporidium detection and species identification?
The main challenges include: (1) low parasite concentrations in environmental and clinical samples; (2) presence of PCR inhibitors in stool and environmental matrices; (3) inefficient DNA extraction methods; (4) the small size (4.2-5.4 µm) and variable staining characteristics of oocysts; and (5) the genetic diversity among species requiring broad-range detection assays [15] [25]. Additionally, resolving infections are accompanied by increasing numbers of non-acid-fast "ghost" oocysts that can lead to false-negative results in microscopy-based methods [15].
Q3: How have molecular diagnostics changed our understanding of Cryptosporidium epidemiology?
The adoption of syndromic gastrointestinal PCR testing and other molecular methods has dramatically improved Cryptosporidium detection. In Denmark, implementation of these methods after 2021 led to a substantial increase in identified cases, with Cryptosporidium detected in >2% of tested patients during seasonal peaks (August-October) [18]. Molecular methods have revealed that cryptosporidiosis is endemic in many regions where it was previously considered rare, and have uncovered a much greater diversity of circulating species than previously recognized through traditional microscopy [18].
Q4: What are the current limitations in Cryptosporidium research and drug development?
Significant limitations include: (1) the intractability of the parasite for continuous in vitro culture; (2) limited technical tools for genetic manipulation; (3) the lack of consistently effective treatments for vulnerable populations (only nitazoxanide is FDA-approved but has variable efficacy); and (4) insufficient understanding of species-specific virulence mechanisms [26] [27]. These challenges have hampered drug development, though recent advances in cell culture models, genetic manipulation techniques, and promising new drug candidates are stimulating progress in the field [26].
Troubleshooting Common Experimental Issues
Low Oocyst Recovery from Stool Samples
Problem: Inconsistent or low oocyst recovery from stool specimens during concentration procedures.
Solution:
- Use formalin-ethyl acetate sedimentation as the recommended concentration method [15]
- Increase centrifugation speed or time (500 × g for 10 minutes) to improve oocyst recovery [15]
- Process multiple stool specimens from the same patient, as oocyst shedding can be variable [15]
- For molecular methods, avoid formalin-based fixatives as they adversely affect nucleic acids; instead, use potassium dichromate (2.5% w/v) or other appropriate preservatives [15]
Validation: Include positive control samples with known oocyst concentrations to monitor recovery efficiency across batches.
PCR Inhibition in Environmental Samples
Problem: Inhibition of molecular detection in complex matrices like soil, water, and produce samples.
Solution:
- Evaluate multiple DNA extraction methods and select optimal ones for specific matrices [25]
- Implement droplet digital PCR (ddPCR) which is less affected by PCR inhibitors compared to real-time PCR [25]
- Use appropriate dilution schemes to reduce inhibitor concentrations while maintaining target detectability
- Incorporate internal amplification controls to detect inhibition
Data: A recent study evaluating 11 DNA extraction methods found that performance varied significantly by matrix, with two spin-column kits optimal for water and another better for soil and produce [25]. The same study demonstrated that ddPCR detected Cryptosporidium in 13.6% of water, 23.3% of soil, and 34.7% of fresh produce samples that were negative by real-time PCR [25].
Species Identification Discordance Between Methods
Problem: Discrepancies in species identification between microscopy, immunoassays, and molecular methods.
Solution:
- Use molecular methods (PCR-based approaches) as the reference standard for species identification [15]
- Employ multi-locus genotyping schemes for more accurate speciation and subtyping
- For microscopy, use multiple staining techniques (acid-fast, immunofluorescence) to improve sensitivity
Explanation: Different Cryptosporidium species have overlapping morphological characteristics, making definitive identification by microscopy impossible. Immunoassays may have variable sensitivity across species. Molecular methods provide the most reliable species identification and are increasingly used in reference diagnostic laboratories [15].
Comparative Performance of Diagnostic Methods
Table 1: Comparison of Cryptosporidium Detection Methods
| Method | Sensitivity | Species Identification | Time to Result | Best Use Cases |
|---|---|---|---|---|
| Microscopy (acid-fast) | Low to moderate [15] | No [15] | 1-2 hours | Initial screening, resource-limited settings |
| Immunofluorescence | High [15] | No (but highly specific) [15] | 1-2 hours | Clinical diagnostics, high sensitivity required |
| Enzyme Immunoassays | Moderate [15] | No [15] | 1-3 hours | Batch testing, clinical laboratories |
| Real-time PCR | High [15] | Yes (with specific assays) [15] | 3-6 hours | Reference laboratories, species identification |
| Digital PCR | Very High [25] | Yes (with specific assays) [25] | 3-6 hours | Inhibitor-rich samples, low oocyst loads |
Table 2: Major Cryptosporidium Species of Human Health Concern
| Species | Primary Host | Zoonotic Potential | Key Characteristics |
|---|---|---|---|
| C. parvum | Multiple mammals, especially calves [24] | High [24] | Major cause of human cryptosporidiosis; zoonotic transmission important |
| C. hominis | Humans [15] | Low (primarily human-to-human) [15] | Second major cause of human disease; anthroponotic |
| C. meleagridis | Birds [15] | Yes [15] | Third most common human pathogen; avian reservoir |
| C. felis | Cats [15] | Yes [15] | Opportunistic human pathogen; immunocompromised at risk |
| C. mortiferum | Unknown | Presumed | Recently identified in human cases in Denmark [18] |
| C. erinacei | Hedgehogs [18] | Yes [18] | Emerging human pathogen; hedgehog reservoir |
Experimental Protocols
Protocol: Modified Acid-Fast Staining for Oocyst Detection
Principle: Cryptosporidium oocysts retain carbol fuchsin dye after acid-alcohol decolorization, appearing bright red against a blue-green counterstain [15].
Materials:
- Stool specimen (fresh or preserved in 10% buffered formalin)
- Microscope slides and coverslips
- Modified acid-fast stain (carbol fuchsin, acid-alcohol, methylene blue or malachite green counterstain)
- Centrifuge and concentration supplies
Procedure:
- Concentrate stool specimen using formalin-ethyl acetate sedimentation at 500 × g for 10 minutes [15]
- Prepare smear from sediment on microscope slide and air dry
- Flood slide with carbol fuchsin and stain for 5-15 minutes
- Rinse gently with distilled water
- Decolorize with acid-alcohol for 30 seconds to 2 minutes until runoff is clear
- Counterstain with methylene blue or malachite green for 1-2 minutes
- Rinse, air dry, and examine under oil immersion (1000× magnification)
Interpretation: Cryptosporidium oocysts appear as bright pink to red spherical structures 4.2-5.4 µm in diameter. Some oocysts may appear as "ghosts" (unstained) in resolving infections [15].
Troubleshooting: Variable staining can occur. Include positive and negative controls with each batch. Over-decolorization may result in false negatives, while under-decolorization may cause background staining.
Protocol: Molecular Detection Using Real-Time PCR
Principle: Amplification of Cryptosporidium-specific DNA sequences with fluorescence detection, allowing for both detection and species identification [15] [25].
Materials:
- DNA extraction kit (selected based on sample matrix) [25]
- Real-time PCR instrument
- Species-specific primers and probes
- PCR reaction mix
- Positive controls (different Cryptosporidium species)
- Negative controls
Procedure:
- DNA Extraction:
PCR Setup:
- Prepare master mix according to manufacturer's instructions
- Add species-specific primers and probes
- Include internal amplification control to detect inhibition
- Aliquot into reaction plates and add template DNA
- Run in real-time PCR instrument with appropriate cycling conditions
Analysis:
- Determine cycle threshold (Ct) values for samples
- Compare to standard curve for quantification (if quantitative)
- Identify species based on specific probe detection
Validation: A recent study demonstrated detection limits as low as 5 oocysts in some matrices, with ddPCR showing superior resistance to inhibitors compared to real-time PCR [25].
Research Reagent Solutions
Table 3: Essential Research Reagents for Cryptosporidium Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Staining Reagents | Modified acid-fast stain, Auramine-rhodamine fluorescent stain [15] | Microscopic visualization and detection of oocysts |
| Immunological Reagents | Immunofluorescence antibody kits, Enzyme immunoassays [15] | High-sensitivity detection; species detection with specific antibodies |
| Molecular Biology Kits | DNA extraction kits (various for different matrices), PCR master mixes [25] | Nucleic acid purification and amplification for detection and speciation |
| Cell Culture Systems | Novel in vitro culture models [26] | Parasite propagation; drug screening; pathogenesis studies |
| Genetic Tools | Genetic modification systems [26] | Gene function studies; molecular pathogenesis research |
Detection Workflow and Species Distribution
Diagram 1: Comprehensive Cryptosporidium Detection Workflow. This workflow integrates traditional and molecular methods to optimize detection sensitivity and species identification. IFA: Immunofluorescence Assay; ddPCR: droplet digital PCR.
Diagram 2: Cryptosporidium Species Distribution in Human Cases. Data from recent Danish surveillance study showing relative frequency of different species. The wide heterogeneity necessitates diagnostic approaches capable of detecting multiple species [18].
The wide heterogeneity of Cryptosporidium species presents both challenges and opportunities for diagnostic approaches. Traditional microscopy-based methods, while useful for initial screening, lack the sensitivity and specificity required for accurate species identification, which is crucial for understanding transmission dynamics and implementing targeted control measures [15]. The adoption of molecular methods has dramatically improved detection capabilities, revealing previously unrecognized endemicity and species diversity in various regions [18].
Future directions in Cryptosporidium diagnostics should focus on: (1) developing multiplexed detection platforms capable of identifying multiple species simultaneously; (2) improving extraction and detection methods for complex matrices like soil and food; (3) establishing standardized genotyping schemes for comparative epidemiology; and (4) integrating novel technologies like digital PCR that offer enhanced sensitivity and resistance to inhibitors [25]. Additionally, the research community would benefit from expanded reagent resources, including species-specific antibodies and molecular controls for less common Cryptosporidium species.
As detection methods continue to improve, our understanding of Cryptosporidium heterogeneity and its implications for public health will undoubtedly expand, potentially revealing additional species and transmission pathways. This knowledge will be essential for developing more effective prevention strategies and targeting interventions to the most significant sources and pathways of human infection.
The Modern Diagnostic Toolkit: Implementing High-Sensitivity Detection Methods
Syndromic multiplex PCR testing represents a transformative approach to infectious disease diagnosis by allowing the simultaneous detection of multiple pathogens—bacteria, viruses, parasites, and fungi—from a single patient sample using a single test. This method targets the comprehensive group of pathogens that could be causing a specific clinical syndrome, such as gastrointestinal infections, rather than testing for one pathogen at a time. For researchers focusing on enteric pathogens like Cryptosporidium, this technology offers a powerful tool for rapid, sensitive, and comprehensive screening, fundamentally advancing detection capabilities and epidemiological research. [28] [29] [30]
Frequently Asked Questions (FAQs)
1. How does syndromic multiplex PCR improve the detection of Cryptosporidium compared to traditional methods? Traditional methods for detecting Cryptosporidium, such as microscopic examination for ova and parasites, are limited by variable sensitivity and often require multiple samples and experienced technologists to achieve acceptable yield. In contrast, syndromic multiplex PCR panels are nucleic acid amplification tests (NAATs) that detect the organism's DNA with superior analytical sensitivity. They can identify Cryptosporidium and other co-infecting pathogens in about an hour, bypassing the challenges of organism viability and morphological ambiguity associated with conventional techniques. [28] [31] [30]
2. What are the key considerations for sample preparation and handling to ensure optimal sensitivity? Proper sample preparation is critical for assay performance. For stool samples, approximately 30 mg should be transferred into molecular grade water and homogenized before loading into nucleic acid extraction cartridges. Processing should begin within 2-3 hours after collection. Each run should include a negative control (deionized water) to monitor for contamination, and an internal control targeted to human DNA should be used to assess DNA extraction efficiency and rule out PCR inhibition. [32]
3. Our lab is observing inconsistent results with the Cryptosporidium target. What could be causing this? Inconsistent detection can stem from several factors:
- Inhibitors in Stool Samples: Complex biological samples like stool can contain PCR inhibitors. Using an internal control is essential to identify inhibition issues.
- Low Pathogen Load: If the organism concentration is near the assay's limit of detection (LOD), results may be variable. Ensure sample homogeneity and consider testing reproducibility around the LOD.
- Nucleic Acid Degradation: Improper sample storage or repeated freeze-thaw cycles can degrade DNA, leading to reduced sensitivity. [32] [33]
4. How can we validate the performance of a new multiplex PCR panel for our Cryptosporidium research? A comprehensive validation should include:
- Limit of Detection (LOD): Empirically determine the lowest number of organisms detectable with high confidence (e.g., ≥95% positivity rate) using spiked clinical samples and probit analysis.
- Analytical Specificity: Test against a panel of related non-target pathogens (e.g., other parasites like Cyclospora cayetanensis and Giardia duodenalis) to ensure no cross-reactivity.
- Clinical Performance: Compare the panel's results against a reference method (e.g., standard PCR or microscopy) to calculate relative sensitivity and specificity. [32]
5. Can these panels distinguish between different species or genotypes of Cryptosporidium? Most commercially available syndromic gastrointestinal panels, such as the BioFire FilmArray GI Panel, report Cryptosporidium as a genus-level detection. They are not typically designed to differentiate between species like C. parvum and C. hominis. For genotyping and subtyping required for detailed outbreak investigations or population genetics, subsequent sequencing of cultured isolates or PCR-positive samples is necessary. [28]
Troubleshooting Guides
Guide 1: Addressing Low Sensitivity or False Negatives
| Symptom | Possible Cause | Recommended Action |
|---|---|---|
| Failure of Internal Control | PCR inhibitors in sample | Dilute the sample and re-extract nucleic acids. Ensure proper homogenization. [32] |
| Target not detected in known positive sample | Nucleic acid degradation | Avoid repeated freeze-thaw cycles. Store samples at recommended temperatures (-80°C for long-term). [33] |
| Pathogen load below LOD | Concentrate the sample before extraction if possible. Verify assay's stated LOD for the target. [32] | |
| Primer/probe mismatch | Verify the panel's target region aligns with circulating strains in your geographical area. [33] | |
| THALLIUM(I)HYDROXIDE | THALLIUM(I)HYDROXIDE, CAS:1310-83-4, MF:Cl6Na2Os | Chemical Reagent |
| Cinepazet maleate | Cinepazet Maleate|For Research | Cinepazet Maleate is a vasodilator for cardiac disease research. This product is for Research Use Only (RUO) and not for human or veterinary diagnosis or treatment. |
Guide 2: Addressing Specificity Issues and Contamination
| Symptom | Possible Cause | Recommended Action |
|---|---|---|
| False positive for a target | Amplicon or sample carryover contamination | Implement strict unidirectional workflow. Use UV hoods for PCR setup and clean workspaces with DNA-degrading solutions. [32] |
| Detection of unexpected targets | Non-specific amplification | Verify the analytical specificity of the assay. Check for genetic similarities between reported targets and non-target organisms. [32] |
| Positive in negative control | Contaminated reagents | Prepare fresh aliquots of all reagents. Use dedicated equipment for reagent preparation. [32] |
Performance Data and Protocols
Table 1: Performance Metrics of a Representative Multiplex qPCR Stool Panel
Data based on a clinical evaluation of a novel syndromic panel. [32]
| Metric | Result for Stool Samples |
|---|---|
| Relative Sensitivity | 94% |
| Relative Specificity | 98% |
| Time to Result | ~3 hours for 10 samples |
| Sample Throughput | 10 samples per run |
Table 2: Representative Limits of Detection (LOD) for Key GI Parasites
LOD can vary based on sample type and specific assay. Values are for illustration. [32] [33]
| Pathogen | Approximate LOD (in clinical sample) |
|---|---|
| Cryptosporidium spp. | 10 - 100 pathogens/mL |
| Giardia duodenalis | 10 - 100 pathogens/mL |
| Entamoeba histolytica | 10 - 100 pathogens/mL |
Experimental Protocol: Determining Limit of Detection (LOD)
Objective: To empirically determine the LOD of Cryptosporidium in a syndromic PCR panel using spiked clinical samples.
Materials:
- Negative stool matrix (confirmed via reference method)
- Quantified Cryptosporidium reference standard (e.g., from ATCC)
- Phosphate-buffered saline (PBS)
- The syndromic PCR panel and required equipment
Method:
- Prepare Dilutions: Serially dilute the reference standard in PBS to create concentrations from 100 to 10^4 genomes/mL.
- Spike Matrix: Spike the negative stool matrix with each dilution to create samples with known concentrations.
- Run Replicates: Test each dilution 12 times in the same run to establish a preliminary LOD in the matrix.
- Probit Analysis: Prepare and test clinical samples containing 0, 0.1xLOD, 0.5xLOD, LOD, and 10xLOD concentrations. Analyze data using probit analysis to determine the concentration at which 95% of the test results are positive. [32]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Syndromic PCR
| Reagent / Material | Function in the Workflow |
|---|---|
| Negative Stool Matrix | Serves as a negative control and dilution matrix for analytical studies and LOD determination. [32] |
| Quantified Pathogen Standards | Used for assay calibration, creating standard curves, and determining analytical sensitivity and LOD. [32] |
| Internal Control (IC) | A non-target nucleic acid (e.g., phage DNA) spiked into each sample to monitor nucleic acid extraction efficiency and detect PCR inhibition. [32] |
| Primer/Probe Sets | Target-specific oligonucleotides for the multiplex PCR reaction. The design is crucial for specificity and avoiding primer-dimers. [34] |
| Nucleic Acid Extraction Kits | Reagents for the automated or manual isolation of high-quality, inhibitor-free DNA and RNA from complex stool samples. [32] |
| Ranatuerin-2AVa | Ranatuerin-2AVa Peptide |
| Methylsilatrane | Methylsilatrane, CAS:2288-13-3, MF:C7H15NO3Si, MW:189.28 g/mol |
Workflow and Troubleshooting Diagrams
Diagram 1: Syndromic PCR Wet-Lab Workflow
Diagram 2: Logical Troubleshooting Framework
Cryptosporidium is a protozoan parasite responsible for gastroenteritis, presenting significant detection challenges in clinical and research settings. The selection of an appropriate genetic target is fundamental to developing a sensitive and specific PCR assay. Among the numerous molecular targets available, the 18S rRNA gene is consistently identified as displaying the best inherent sensitivity due to its multi-copy nature in the genome, while also providing sufficient sequence variation between species for reliable identification [35] [36]. Other commonly used targets include the Cryptosporidium oocyst wall protein (COWP) gene and the LIB13 locus, each offering distinct advantages for specific applications from broad screening to precise species differentiation [37].
This technical resource center provides researchers with evidence-based comparisons of these genetic loci, detailed methodological protocols, and troubleshooting guidance to enhance the sensitivity and specificity of Cryptosporidium detection assays.
Comparative Analysis of Genetic Targets
Key Genetic Loci and Their Characteristics
The table below summarizes the primary genetic targets used in Cryptosporidium PCR detection, highlighting their respective advantages and limitations:
| Genetic Locus | Key Characteristics | Best Applications | Sensitivity Notes | Species Differentiation Capability |
|---|---|---|---|---|
| 18S rRNA | Multi-copy gene (~5 copies/genome), highly conserved with variable regions [36] [38] | Primary detection, broad-spectrum identification [36] | Highest sensitivity; detects 1-10 oocysts/g feces with efficient extraction [13] [38] | Identifies all Cryptosporidium species; sequencing required for differentiation [37] [36] |
| COWP | Single-copy gene, species-specific sequence variations [37] | Species-specific detection, PCR-RFLP typing [37] | Lower sensitivity than 18S rRNA due to single-copy nature [37] | Differentiates species via restriction fragment analysis or specific probes [37] |
| LIB13 | Single-copy locus with significant sequence divergence [37] | Specific identification of C. parvum and C. hominis [37] | High specificity but may miss other species [37] | Direct differentiation of C. parvum and C. hominis with specific probes [37] |
| TRAP-C2 | Single-copy gene [13] | Experimental studies, subsidiary target [13] | Lower sensitivity compared to 18S rRNA [13] | Limited data; less commonly used for differentiation [13] |
Analytical Performance Comparison
Recent multicenter evaluations provide critical quantitative data on assay performance:
| Target Locus | Assay Format | Limit of Detection | Species Identification Method | Diagnostic Specificity |
|---|---|---|---|---|
| 18S rRNA | Real-time PCR [35] [36] | 200-300 oocysts/g stool [35] [37] | Sequencing or specific MGB probes [37] [36] | 100% (for genus detection) [37] |
| 18S rRNA | Nested PCR [38] | Equivalent to 1 oocyst/g feces [38] | Sequencing of PCR products [38] | 100% [38] |
| LIB13 | Duplex real-time PCR (C. parvum & C. hominis) [37] | 2-8 oocysts per PCR reaction [37] | Specific TaqMan MGB probes [37] | 100% for target species [37] |
Experimental Protocols
18S rRNA Nested PCR for Maximum Sensitivity
Principle: This protocol uses two rounds of PCR amplification to achieve exceptional sensitivity for detecting all Cryptosporidium species [38].
Reagents and Equipment:
- DNA extraction kit (QIAamp DNA Stool Mini Kit or equivalent)
- Thermal cycler
- PCR reagents: Thermostable DNA polymerase, dNTPs, MgClâ‚‚, reaction buffers
- Primers (20 μM working solutions):
- Outer forward: Cry18S-S2: 5'-GGTGACTCATAATAACTTTACGG-3'
- Outer reverse: Cry18S-As2: 5'-ACGCTATTGGAGCTGGAATTAC-3'
- Inner forward: Cry18S-S1: 5'-TAAACGGTAGGGTATTGGCCT-3'
- Inner reverse: Cry18S-As1: 5'-CAGACTTGCCCTCCAATTGATA-3'
Procedure:
- DNA Extraction:
Primary PCR:
- Prepare 50 μL reaction containing:
- 20 mM (NHâ‚„)â‚‚SOâ‚„
- 75 mM Tris-HCl (pH 8.8)
- 1 mM MgClâ‚‚
- 0.2 mM dNTP mix
- 1.2 Units thermostable DNA polymerase
- 20 μM each outer primer (Cry18S-S2/As2)
- 1 μL template DNA [38]
- Cycling conditions:
- Initial denaturation: 94°C for 5 minutes
- 35 cycles of: 94°C for 1 minute, 60°C for 1.5 minutes, 72°C for 2 minutes
- Final extension: 72°C for 10 minutes [38]
- Prepare 50 μL reaction containing:
Nested PCR:
- Prepare 50 μL reaction as above, using inner primers (Cry18S-S1/As1)
- Use 1 μL of primary PCR product as template
- Use identical cycling conditions as primary PCR [38]
Analysis:
- Electrophorese 5-10 μL nested PCR product on 1% agarose gel
- Visualize expected 240 bp band under UV light [38]
Multiplex Real-Time PCR for Detection and Differentiation
Principle: This streamlined protocol simultaneously detects all Cryptosporidium species while differentially identifying C. parvum and C. hominis in a single assay [37].
Reagents and Equipment:
- Real-time PCR instrument (e.g., Rotorgene 6000)
- TaqMan environmental master mix 2.0
- Primers and MGB probes:
- Genus detection (SSU rRNA): CRU18SF, CRU18SR, CRU18STM (FAM-labeled)
- C. parvum (LIB13): CRULib13F, CRULib13RCp, CRULib13TMCp (VIC-labeled)
- C. hominis (LIB13): CRULib13F, CRULib13RCh, CRULib13TMCh (VIC-labeled) [37]
Procedure:
- Reaction Setup:
- Prepare two separate duplex reactions for each sample:
Reaction 1 (Genus + C. parvum):
- 12.5 μL TaqMan environmental master mix 2.0
- 900 nM each primer (CRU18SF, CRU18SR, CRULib13F, CRULib13RCp)
- 100 nM CRU18STM probe (FAM)
- 150 nM CRULIB13Cp probe (VIC)
- 2 μL DNA template
- Nuclease-free water to 25 μL [37]
Reaction 2 (C. hominis + Internal Control):
- 12.5 μL TaqMan environmental master mix 2.0
- 900 nM each primer (CRULib13F, CRULib13RCh at 300 nM)
- 100 nM CRULIB13Ch probe (VIC)
- 1 μL primer/probe mix for internal control (FAM-labeled)
- 5 μL of 1:20 diluted internal control DNA
- 2 μL DNA template
- Nuclease-free water to 25 μL [37]
Thermal Cycling:
- Hold: 95°C for 10 minutes
- 55 cycles of: 95°C for 15 seconds, 60°C for 60 seconds
- Collect fluorescence in FAM, VIC, and ROX channels during each 60°C phase [37]
Interpretation:
- Positive genus detection: FAM fluorescence crosses threshold in Reaction 1
- Species identification: VIC fluorescence in respective reactions
- Inhibition: Failure of internal control in Reaction 2 [37]
Troubleshooting Guides and FAQs
Common PCR Problems and Solutions
| Problem | Potential Causes | Solutions |
|---|---|---|
| Low or no product yield | PCR inhibitors, poor primer design, insufficient template, incorrect annealing temperature [39] | Dilute template 1:100, redesign primers with 40-60% GC content, optimize annealing temperature, use PCR enhancers [39] [40] |
| Non-specific amplification | Low annealing temperature, excessive primers, high Mg²⺠concentration [39] | Increase annealing temperature incrementally (2°C steps), optimize primer concentration (0.05-1 μM), titrate Mg²⺠[39] [40] |
| Inconsistent results between replicates | PCR inhibitors in stool, inefficient DNA extraction, pipetting errors [35] | Implement mechanical grinding (Bead-beater), use column-based extraction, prepare master mixes [35] [36] |
| Failed species differentiation | Probe degradation, suboptimal reaction conditions, rare genetic variants [37] | Prepare fresh probe aliquots, verify probe specificity, sequence 18S rRNA amplicon as backup [37] |
Frequently Asked Questions
Q: Which genetic target provides the highest sensitivity for primary Cryptosporidium detection? A: The 18S rRNA gene consistently demonstrates the highest sensitivity due to its multi-copy nature (approximately 5 copies per genome), enabling detection of as few as 1-10 oocysts per gram of feces when combined with efficient DNA extraction methods [38] [36]. This makes it the preferred target for initial screening and maximum sensitivity requirements.
Q: When should I consider using the COWP gene instead of 18S rRNA? A: The COWP gene is particularly valuable for species differentiation through PCR-RFLP or as a confirmatory target when 18S rRNA sequencing reveals ambiguous results [37]. However, its single-copy nature generally provides lower sensitivity compared to 18S rRNA, making it less suitable for primary detection of low-level infections [37].
Q: How can I overcome PCR inhibition from stool components? A: Effective strategies include: (1) Using mechanical disruption with ceramic beads during DNA extraction [36]; (2) Incorporating an internal control to detect inhibition [37]; (3) Diluting template DNA 1:10 to 1:100 [40]; (4) Using inhibitor-resistant polymerases or additives like BSA (10-100 μg/mL) [41].
Q: What is the advantage of a multiplex real-time PCR approach for Cryptosporidium? A: Multiplex real-time PCR simultaneously detects the Cryptosporidium genus (via 18S rRNA) and differentiates the two most clinically relevant species, C. parvum and C. hominis (via LIB13 locus), significantly improving workflow efficiency and reducing turnaround time compared to sequential testing or post-PCR analysis methods [37].
Q: How does DNA extraction method impact detection sensitivity? A: Extraction efficiency critically impacts sensitivity. Multicenter evaluations demonstrate that methods combining mechanical grinding (e.g., Boom technique with bead beating) and column-based purification provide superior yields compared to non-mechanical methods or magnetic silica approaches [35] [36]. The optimal method should effectively rupture durable oocyst walls while purifying DNA from PCR inhibitors.
Workflow Visualization
Cryptosporidium PCR Detection Workflow: This diagram illustrates the optimal pathway for molecular detection of Cryptosporidium, highlighting critical decision points for target selection and methodology based on detection goals.
The Scientist's Toolkit: Essential Research Reagents
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| DNA Extraction Kits | QIAamp DNA Stool Mini Kit, NucliSENS easyMAG [38] [36] | Efficient lysis of durable oocysts and purification from PCR inhibitors; mechanical disruption essential [36] |
| PCR Enzymes | Hot-start Taq polymerases, High-fidelity enzymes [39] [40] | Reduce non-specific amplification; essential for complex stool samples [39] |
| PCR Additives | BSA (10-100 μg/mL), DMSO (1-10%), Betaine (0.5-2.5 M) [41] | Counteract PCR inhibitors; improve amplification efficiency from difficult samples [41] |
| Primer/Probe Sets | 18S rRNA primers (CRU18SF/R), LIB13 probes (C. parvum/hominis) [37] [36] | Genus-specific detection and species differentiation; MGB probes enhance specificity [37] |
| Inhibition Controls | Exogenous internal control DNA [37] | Critical for identifying PCR failure due to inhibitors in complex samples [37] |
| Quantification Standards | Plasmid standards containing target sequences [37] [36] | Enable accurate quantification of oocyst loads in clinical and environmental samples [36] |
| 4-Aminochroman-3-ol | 4-Aminochroman-3-ol|Research Chemical | |
| 2-Nitroanthraquinone | 2-Nitroanthraquinone, CAS:605-27-6, MF:C14H7NO4, MW:253.21 g/mol | Chemical Reagent |
Frequently Asked Questions (FAQs) on Bead-Beating for DNA Extraction
Q1: Why is bead-beating particularly important for Cryptosporidium and similar resilient pathogens? Cryptosporidium oocysts have a tough wall that makes them difficult to disrupt. Bead-beating is a mechanical lysis method that is highly effective for breaking open such resilient biological samples. Unlike chemical or enzymatic methods alone, the rapid agitation with grinding media (beads) physically impacts and disrupts these sturdy structures, which is crucial for liberating sufficient DNA for sensitive downstream detection [42] [25]. This is a key step in improving the sensitivity of detection assays.
Q2: What are the common signs of a sub-optimized bead-beating protocol? Common issues that indicate a need for protocol optimization include:
- Low DNA Yield: This often points to incomplete cell lysis. The solution is to increase bead-beating time or speed, or to use a more appropriate bead size and type [43] [44].
- Degraded DNA: This can result from excessive heat generation during the bead-beating process. This can be mitigated by using a homogenizer with a pulsing feature (alternating short bursts with rest periods on ice) to dissipate heat, or by performing the bead-beating cryogenically (at very low temperatures) [42] [45].
- Inconsistent Results Between Samples: This can be caused by leaking tubes or uneven filling of disruption containers, which impedes the consistent motion of beads. Always use screw-cap tubes with 'O' rings and ensure containers are not overfilled [44].
- Inhibition in Downstream PCR: This can be due to co-purification of inhibitors like humic acids from environmental samples (e.g., soil or water) or from carryover of salts and ethanol from the purification process. Additional purification steps, such as the use of polyvinyl polypyrrolidone (PVPP) or size-exclusion chromatography, may be required to remove these contaminants [46].
Q3: How do I choose the right beads for my sample? The choice of beads is critical for lysis efficiency. The key factors are the sample's resiliency and the target microorganism.
- Size: Smaller beads (e.g., 0.1 mm) are generally more effective for disrupting bacterial cells, while larger beads (e.g., 0.5 mm to 3/8") are better for tougher samples like fungal spores, tissues, or soil [45] [44].
- Material: Common materials include glass (silica), ceramic (zirconium), and steel. Zirconium beads are often preferred for their high density and efficiency.
- Sample Type Guide:
- Cryptosporidium oocysts, soil, seeds: Use larger, dense beads (e.g., 0.5 mm zirconium or ceramic).
- Bacterial cells (e.g., from water): Use small beads (e.g., 0.1 mm zirconium/silica) [44].
- Soft tissues (e.g., liver): Softer samples may be homogenized effectively with a single larger grinding ball [42].
Q4: My downstream digital PCR (dPCR) is sensitive to inhibitors. How can bead-beating and purification be optimized for this? Digital PCR, while generally more tolerant to inhibitors than real-time PCR, can still be affected. For the most sensitive detection of low-abundance targets like Cryptosporidium, a study found that combining optimized bead-beating with a spin-column-based DNA extraction method yielded the best results for environmental samples. The research demonstrated that ddPCR was less prone to be affected by PCR inhibitors present in complex matrices like soil and water, and it successfully detected Cryptosporidium in field samples where real-time PCR failed [25]. Ensuring thorough washing steps during purification to remove inhibitors is paramount.
Troubleshooting Common Bead-Beating Problems
The following table outlines specific issues, their causes, and verified solutions.
| Problem | Possible Cause | Solution |
|---|---|---|
| Low DNA Yield [43] [44] | Incomplete lysis; Inefficient binding of DNA to purification matrix | Increase bead-beating duration or speed; Optimize binding conditions (e.g., ensure correct salt/alcohol concentration); Use a smaller, more effective bead size. |
| Degraded DNA [43] | Excessive heat from prolonged beating; Harsh sample handling | Use the homogenizer's pulse feature (e.g., 1.5 min beats with 1 min on ice); Perform bead-beating in a cold room or using a Cryoblock. |
| Inhibition in Downstream PCR [46] | Co-purification of contaminants (e.g., humic acid, proteins) | Add purification steps: use PVPP or CTAB during extraction; Perform additional wash steps with 70-80% ethanol; Use a purification method proven for your sample matrix. |
| Sample Leakage & Cross-Contamination [44] | Use of inappropriate tube caps or seals | Always use screw-cap tubes with 'O' rings; For plates, use tight-fitting polypropylene strip caps instead of silicone mats. |
| Poor Representation of Microbial Community [45] | Overly harsh lysis destroying some cell types | For complex communities (bacteria and fungi), a protocol without bead-beating or with enzymatic supplementation (e.g., MetaPolyzyme) may provide a more balanced profile. Optimization is required. |
Research Reagent Solutions for Bead-Beating
This table lists essential materials and their functions for setting up a bead-beating protocol.
| Item | Function & Application |
|---|---|
| Zirconium Beads (0.1 mm) | Optimal for efficient lysis of bacterial cells due to high density and small size [44]. |
| Zirconium Beads (0.5 mm) | Effective for disrupting tougher samples like fungal cells, soil, and environmental biofilms [45]. |
| Lysis Tubes with Beads | Pre-filled tubes save time, ensure consistency, and reduce contamination risk. Available for various tube sizes (e.g., 2 ml, 5 ml) and deep-well plates [42]. |
| High-Throughput Homogenizer (e.g., GenoGrinder) | Instruments capable of oscillating deep-well plates or multiple tubes simultaneously for processing hundreds of samples daily with a linear or figure-eight motion [42]. |
| Benchtop Homogenizer (e.g., HT Mini) | Compact devices based on a dental amalgamator design, ideal for rapid disruption of a small number of samples (1-6 tubes) at high speed [42]. |
| Proteinase K | Enzyme used in lysis buffer to digest proteins and degrade nucleases, enhancing DNA yield and quality [43]. |
| PVPP (Polyvinyl Polypyrrolidone) | Additive used to adsorb and remove humic acid contaminants from soil and environmental DNA extracts, reducing PCR inhibition [46]. |
| Magnetic Beads or Spin-Columns | For post-lysis nucleic acid purification. Magnetic beads are automation-friendly, while spin-columns can be optimal for certain sample types as per comparative studies [25] [47]. |
Experimental Protocol: Optimized Bead-Beating for Environmental Samples with High Inhibitor Content
This protocol is adapted from methods successfully used to detect Cryptosporidium in water, soil, and produce samples, which are notorious for PCR inhibitors [25] [46].
Objective: To efficiently release DNA from resilient oocysts and cysts in environmental matrices while minimizing co-extraction of substances that inhibit downstream molecular detection.
Materials:
- High-throughput homogenizer (e.g., GenoGrinder 2010)
- 2 ml screw-cap disruption tubes pre-filled with 0.5 mm zirconium beads
- Lysis buffer (e.g., from a commercial kit, or a custom buffer containing GuHCl, EDTA, Triton X-100)
- Proteinase K
- Phenol:Chloroform:Isoamyl Alcohol (25:24:1)
- Polyethylene Glycol (PEG) 8000
- Ice bath
- Centrifuge
Step-by-Step Method:
- Sample Preparation: Concentrate or weigh the environmental sample (e.g., 10 g of soil, 100 mL of water filtered). For soil, a pre-wash may be necessary to remove loose debris.
- Loading Tubes: Transfer the sample into a 2 ml disruption tube. Add lysis buffer and Proteinase K. Ensure the total volume does not exceed 2/3 of the tube's capacity to allow for bead movement [44].
- Bead-Beating: Secure the tubes in the homogenizer. Process at a high speed (e.g., 1500 rpm) for 3-5 minutes. Use a pulsed protocol: 1.5 minutes of beating followed by 1 minute of rest on ice, repeated twice. This controls heat and improves lysis efficiency [42] [45].
- Initial Separation: Centrifuge the tubes at ≥10,000 g for 1 minute to pellet debris and beads.
- Nucleic Acid Extraction: Transfer the supernatant to a new tube.
- Inhibitor Removal: Add PVPP to the supernatant, vortex, and centrifuge to pellet the PVPP and bound inhibitors [46].
- Precipitation: To the cleaned supernatant, add 0.6 volumes of isopropanol and 0.1 volumes of 3M sodium acetate. Incubate at -20°C for 1 hour. Alternatively, use PEG/NaCl precipitation [46].
- Pellet and Wash: Centrifuge at high speed (e.g., 14,000 rpm) for 15 minutes to pellet the DNA. Wash the pellet with 1 ml of 70% ethanol. Centrifuge again, discard the supernatant, and air-dry the pellet.
- Resuspension: Resuspend the purified DNA in nuclease-free TE buffer or water.
Workflow Visualization
The following diagram illustrates the logical flow of the optimized bead-beating protocol, highlighting critical steps for success.
This table summarizes key performance data from cited studies to inform your method selection, particularly for sensitive detection applications.
| Method / Parameter | LoD (Limit of Detection) / Key Finding | Application & Notes | Source |
|---|---|---|---|
| Real-time dPCR | Lower LoD than both end-point dPCR and qPCR | SARS-CoV-2 detection: Real-time data collection allowed removal of false-positive signals, lowering the limit of blank (LoB) and LoD. | [48] |
| Droplet Digital PCR (ddPCR) | Detected Cryptosporidium in 13.6% (water) to 34.7% (produce) of field samples. | Cryptosporidium in agriculture: More sensitive and inhibitor-tolerant than real-time PCR, which failed to detect any positives in the same samples. | [25] |
| Bead-Beating + Enzymatic Lysis (MLBE) | Provided a balanced profile for combined bacterial and fungal microbiome analysis. | Mock microbial communities: Bead-beating alone (MLB) skewed the fungal community profile; enzymatic supplementation improved recovery. | [45] |
| Modified PCR Protocol (Pre-amplification) | Allowed 16S rRNA amplification from 24 additional low-bacterial-load samples. | Low biomass samples: Using a small percentage of primers without sequencing adapters increased sensitivity without altering community composition. | [49] |
FAQs: Navigating Detection Challenges
1. Our current microscopy methods are well-established for Cryptosporidium. Why should we invest in molecular techniques for species-level identification?
While conventional staining and immunofluorescence microscopy are excellent for genus-level detection, they lack the resolution to distinguish between different Cryptosporidium species and genotypes [15] [5]. Molecular methods are essential because different species have varying public health implications. For instance, identifying C. mortiferum (2.5%), C. felis (1.2%), or C. erinacei (0.8%) in human cases, as recently documented in Denmark, points to specific zoonotic transmission routes that require different investigative and control measures compared to the more common C. parvum or C. hominis [18]. Molecular identification is no longer just for research; it's becoming critical for understanding local transmission dynamics and implementing targeted public health interventions.
2. We keep getting false negatives in our cryptosporidiosis screening, particularly from formed stools. How can we improve sensitivity?
This is a common challenge, as oocyst shedding can be intermittent and variable in density. The solution involves a multi-pronged approach:
- Test Multiple Samples: Always collect and test at least three consecutive stool specimens from a single patient [15] [5].
- Upgrade Your Detection Method: Switch from traditional acid-fast staining to Direct Fluorescent-Antibody (DFA) testing or Enzyme Immunoassays (EIA). DFA, in particular, has greater sensitivity and specificity for initial detection [15] [5].
- Implement a Sensitive Molecular Confirmation: For definitive species identification, use Polymerase Chain Reaction (PCR)-based methods. Techniques like UDG-supplemented Loop-Mediated Isothermal Amplification (UDG-LAMP) have demonstrated high sensitivity and specificity, effectively detecting infections even in cases where microscopy fails [50].
3. Our PCR results are sometimes contaminated with amplicons from previous runs. How can we prevent this?
Carryover contamination is a significant risk in molecular diagnostics. An effective solution is to incorporate Uracil DNA Glycosylase (UDG) into your LAMP or PCR protocol. This technique involves using dUTP in the reaction mix instead of dTTP. The UDG enzyme then enzymatically degrades any PCR products (amplicons) containing uracil from previous reactions before the new amplification cycle begins, effectively eliminating carryover contamination without affecting the native DNA template [50].
4. We need to test large volumes of water for low numbers of oocysts. What is the standard method for concentration and detection?
The environmental testing of water for Cryptosporidium is a specialized process governed by standardized protocols like US EPA Method 1623 or the UK's "Blue Books" [5]. The workflow is complex and involves multiple steps to concentrate and isolate the oocysts from large water volumes (up to 1,000 liters) before detection can occur. The following workflow outlines this multi-stage process:
5. What are the key differences in sample preparation for clinical versus environmental samples?
The table below summarizes the critical differences in handling these distinct sample types.
| Aspect | Clinical Samples (Stool) | Environmental Samples (Water) |
|---|---|---|
| Sample Volume | Small (grams) | Very large (10 - 1,000 liters) [5] |
| Primary Goal | Diagnosis of infection | Monitoring of public water supplies [5] |
| Concentration | Formalin-ethyl acetate sedimentation [15] | Filtration followed by centrifugation and IMS [5] |
| Preservation | 10% buffered formalin; avoid if doing PCR [15] | Refrigeration; process within 96 hours [5] |
| Key Challenge | Intermittent shedding; test 3 samples [5] | Extremely low oocyst count; requires high-volume processing [5] |
Troubleshooting Common Experimental Issues
Problem: Inconsistent or Weak Signal in Acid-Fast Staining
- Possible Cause: The staining procedure is highly sensitive to the condition of the oocysts. Resolving infections often contain increasing numbers of non-acid-fast "ghost" oocysts that will not stain properly [15].
- Solution:
- Ensure samples are fresh or properly preserved.
- Increase centrifugation speed or time (e.g., 500 x g for 10 minutes) during formalin-ethyl acetate sedimentation to maximize oocyst recovery [15].
- Confirm staining results with a known positive control.
- Consider transitioning to DFA or EIA methods for more consistent and reliable detection [15] [5].
Problem: Low Nucleic Acid Yield from Oocysts for Molecular Work
- Possible Cause: The robust oocyst wall makes it difficult to extract high-quality genetic material.
- Solution:
- Incorporate a mechanical disruption step, such as bead beating, into your DNA extraction protocol to ensure the oocyst wall is effectively broken.
- Use commercial DNA extraction kits specifically validated for Cryptosporidium or other tough-to-lyse organisms.
- For water samples, the IMS step is critical for purifying and concentrating oocysts away from PCR inhibitors present in environmental samples [5].
Problem: Inability to Distinguish Between Species After Positive Genus-Level Test
- Possible Cause: Standard diagnostic tests (DFA, EIA) and water testing protocols are designed to identify the genus Cryptosporidium, not individual species [5].
- Solution: Implement a molecular genotyping method. The standard approach involves:
- DNA Extraction: From purified oocysts or positive stool samples.
- PCR Amplification: Target genetic loci such as the 18S rRNA gene, GP60, or other species-specific markers.
- Analysis: Perform Restriction Fragment Length Polymorphism (RFLP) analysis or sequencing of the PCR amplicon [5]. Real-time PCR assays capable of distinguishing species are also available [5].
Research Reagent Solutions
This table lists key reagents and their functions for advanced Cryptosporidium detection and typing.
| Reagent / Kit | Function / Application | Key Feature |
|---|---|---|
| MERIFLUOR Cryptosporidium/Giardia | Direct Fluorescent-Antibody (DFA) test for microscopic detection [5] | High sensitivity and specificity; considered a gold standard |
| UDG-LAMP Reagents | Isothermal molecular detection of C. parvum, C. hominis, and C. meleagridis [50] | High sensitivity, rapid, prevents carryover contamination |
| Immunomagnetic Separation (IMS) Kits | Concentration and purification of oocysts from water and complex samples [5] | Critical for removing PCR inhibitors prior to molecular analysis |
| ColorSeed / EasySeed | Internal process control for water testing methods [5] | Validates entire recovery and detection process; approved by regulatory bodies |
| Cryptosporidium Genotyping Kit (e.g., Invitrogen) | Real-time PCR-based differentiation of species/genotypes [5] | Can distinguish between infective and non-infective species |
Detailed Experimental Protocols
Protocol 1: UDG-LAMP for Sensitive Detection in Clinical Specimens
This protocol is adapted from a study that successfully detected Cryptosporidium in AIDS patients with high sensitivity, overcoming the limitations of acid-fast staining [50].
Principle: LAMP amplifies DNA with high specificity and efficiency under isothermal conditions. The incorporation of UDG prevents false positives from amplicon carryover.
Workflow:
- Specimen Collection: Collect stool samples and preserve appropriately. Formalin-based fixatives are not recommended if molecular testing will be performed [15].
- DNA Extraction: Use a commercial stool DNA extraction kit. Include a mechanical lysis step (bead beating) to break the oocyst wall.
- UDG-LAMP Reaction Setup:
- Prepare the LAMP reaction mix containing dUTP instead of dTTP.
- Add UDG enzyme to the mix.
- Add the extracted DNA template.
- Incubation: Incubate the reaction at a constant temperature (typically 60-65°C) for 45-60 minutes.
- Result Interpretation: Analyze results via gel electrophoresis or by using fluorescent intercalating dyes for real-time monitoring.
Protocol 2: Genotyping by PCR-RFLP/Sequencing
This protocol is used for identifying Cryptosporidium at the species level, which is crucial for understanding transmission cycles.
Workflow:
- DNA Extraction: As described in Protocol 1.
- PCR Amplification: Amplify a target gene region, such as the 18S rRNA gene, using Cryptosporidium-specific primers.
- Analysis (Choose One):
- RFLP: Digest the purified PCR product with appropriate restriction enzymes. Separate the fragments on an agarose gel. The resulting banding pattern is species-specific [5].
- Sequencing: Purify the PCR product and submit for Sanger sequencing. Compare the obtained sequence to databases like CryptoDB.org for species identification [51].
The following flowchart illustrates the decision-making process for selecting the right detection and identification method based on your research goals and available resources:
Beyond the Basics: Overcoming Technical Hurdles for Maximum Sensitivity
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My PCR results for Cryptosporidium are consistently negative despite high clinical suspicion. What are the most likely pre-analytical causes? The most likely causes relate to sample integrity and the presence of PCR inhibitors. Cryptosporidium oocysts can be shed intermittently, and a single, small stool sample may not contain detectable levels [21]. Furthermore, stool is a complex matrix rich in PCR inhibitors. Ensure you are collecting multiple samples (ideally three, on separate days) and using a DNA extraction kit validated for stool samples, such as the QIAamp DNA Stool Mini kit, which includes steps to remove inhibitors [52] [53]. For maximum sensitivity, consider incorporating a DNA capture protocol with biotinylated probes to selectively enrich Cryptosporidium DNA before PCR [52].
Q2: How does storage temperature and time affect the detection of Cryptosporidium antigens and DNA? The stability of the target (antigen vs. DNA) differs. For antigen detection tests like ELISA, intact oocysts are the target. Freezing and thawing can lyse oocysts, potentially releasing antigens but also possibly degrading them. One study found that ELISA had higher sample-to-sample variability compared to qPCR, which may be influenced by storage conditions affecting oocyst integrity [53]. For molecular methods, DNA is relatively stable. Samples for DNA extraction are often frozen at -80°C [53]. However, repeated freeze-thaw cycles should be avoided as they can fragment DNA. The key is consistency; establish and adhere to a standard operating procedure for storage.
Q3: What is the minimum sample volume or weight required for reliable detection? While requirements can vary by specific test, research protocols provide a guide. For DNA extraction from stool, protocols often use 200 mg of solid stool or 200 μL of liquid stool [53]. Another study using a DNA capture method processed samples lysed from an initial stool specimen [52]. Using less than the recommended amount can drastically reduce sensitivity, as you may not capture enough oocysts for detection, especially in low-shedding cases.
Q4: Why might there be a discrepancy between my ELISA and PCR results? Discrepancies are common and arise from the fundamental differences in what each test detects.
- PCR is more sensitive: Multiple studies directly comparing ELISA and PCR consistently demonstrate that PCR is more sensitive, often detecting 1-2 logs fewer oocysts [52] [53]. A negative ELISA with a positive PCR is a frequent finding, especially in samples with low oocyst counts.
- ELISA detects antigens, PCR detects DNA: ELISA requires intact oocysts and specific antigens. PCR can detect DNA from both intact and disintegrated oocysts [53]. This is a critical consideration when monitoring treatment efficacy, as PCR may detect non-viable organisms and show prolonged "shedding" after successful treatment.
- Species-specificity: Some ELISA tests may have variable reactivity to different Cryptosporidium species, potentially leading to false negatives with non-parvum/hominis species [54].
Troubleshooting Common Scenarios
| Scenario | Possible Root Cause | Solution |
|---|---|---|
| Low DNA yield from stool samples. | Inefficient oocyst lysis and DNA release prior to extraction. | Incorporate a mechanical disruption step, such as bead beating with 212-300 μm glass beads for 3 minutes, before the standard extraction protocol [52] [53]. |
| Inhibition of PCR amplification. | Co-purification of PCR inhibitors (e.g., bilirubin, complex carbohydrates) from stool. | Use a DNA extraction kit designed for stool. Include an internal control (e.g., Phocine herpes virus - PhHV) in your qPCR to identify inhibition. If present, dilute the DNA template or use a DNA clean-up kit [53] [37]. |
| High variability in duplicate qPCR runs. | Inconsistent sample homogenization before processing. | Ensure the stool sample is thoroughly mixed before aliquoting for DNA extraction. Liquid stools should be vortexed; solid stools should be emulsified in a suitable buffer [53]. |
| Unexpected negative results with antigen tests. | Oocyst degradation due to improper storage or transport. | Ensure samples are refrigerated and tested promptly. Avoid freeze-thaw cycles for antigen tests. Confirm the test's specificity for the Cryptosporidium species in your sample [54]. |
Performance Data of Diagnostic Methods
The following table summarizes the analytical sensitivity of various diagnostic methods as reported in the literature, which is critical for evaluating pre-analytical protocols.
Table 1: Comparative Analytical Sensitivity of Cryptosporidium Detection Methods
| Method Category | Specific Technique | Reported Analytical Sensitivity | Key Pre-Analytical Considerations |
|---|---|---|---|
| Molecular | Conventional PCR (18S rRNA) | ~200 oocysts per gram of feces processed [37] | Requires effective DNA extraction and inhibitor removal. |
| Molecular | qPCR with conventional DNA extraction | 10^3 - 10^4 cysts/oocysts [52] | Sample volume and homogenization are critical. |
| Molecular | qPCR with Dual Probe Capture DNA extraction | 10^1 - 10^2 cysts/oocysts [52] | Dependent on probe hybridization efficiency; more complex workflow. |
| Immunological | ELISA (ProSpecT Microplate Assay) | 10^3 - 10^4 cysts/oocysts [52] | Requires intact oocysts; avoid freeze-thaw. |
| Microscopy | Modified Acid-Fast / Auramine Staining | ~8 oocysts/mL in water samples [55] | Requires skilled microscopist; sample concentration improves sensitivity. |
Detailed Experimental Protocol: Dual Probe Capture and qPCR
This protocol, adapted from a published study, details a method to significantly improve the sensitivity of Cryptosporidium detection in stool samples by enriching target DNA before PCR [52].
1. Sample Lysis and Initial Processing
- Suspend stool sample in a lysis buffer (e.g., Qiagen ASL buffer).
- Mechanically disrupt the sample by bead beating with 212-300 μm glass beads for 3 minutes.
- Boil the lysate for 5 minutes to further disrupt oocysts.
- Centrifuge at high speed (e.g., 20,000 × g) to pellet debris.
- Treat the supernatant with RNase (e.g., 2.5 μg) to remove RNA.
- Perform a chloroform extraction and ethanol precipitation to partially purify nucleic acids.
- Reconstitute the nucleic acid pellet in a hybridization buffer (e.g., 100μL Qiagen PCR buffer with 4 mM MgCl₂).
2. Dual Probe Hybridization and Capture
- Add biotinylated capture oligonucleotides (e.g., 125 pmol of each probe) to the purified nucleic acid.
- Denature the mixture at 95°C for 5 minutes to separate DNA strands.
- Anneal and hybridize the probes to their target 18S rRNA sequences at 53°C for 5 minutes.
- Incubate the hybridization mix with streptavidin-coated magnetic beads (e.g., Dynabeads M-280) on a rotator at room temperature. The biotinylated probe-DNA complexes will bind to the beads.
3. Washing and Elution
- Separate the bead-bound complex using a magnet.
- Wash the beads twice with a wash solution to remove non-specifically bound material.
- Perform a final wash in a low-salt buffer (e.g., Tris 10mM pH 8.0).
- Elute the captured DNA from the beads by heating at 80°C for 20 minutes in a low-EDTA elution buffer (e.g., Tris 10mM/EDTA 10mM pH 8.0).
4. Multiplex Real-Time PCR
- Use the eluted DNA as a template in a multiplex qPCR assay.
- A typical 25 μL reaction may contain:
- iQ Multiplex Powermix
- 7.5 pmol of each Scorpion probe
- 30 pmol of each forward and reverse primer
- Cycling conditions:
- 95 °C for 10 min (initial denaturation)
- 40 cycles of: 95 °C for 15 s, 51 °C for 15 s, 72 °C for 20 s
- 75 °C for 10 min (final extension)
Workflow Visualization
Optimized Cryptosporidium Detection Workflow
Dual Probe DNA Capture Process
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Sensitive Cryptosporidium Detection Research
| Reagent / Kit | Function / Application | Example Use Case |
|---|---|---|
| Biotinylated Capture Oligonucleotides | Sequence-specific enrichment of target Cryptosporidium 18S rRNA gene from complex samples. | Dual probe capture protocol to improve PCR sensitivity by 1-2 logs [52]. |
| Streptavidin-Coated Magnetic Beads | Solid-phase matrix to isolate biotinylated probe-DNA complexes. | Used in conjunction with capture probes to physically separate target DNA from inhibitors [52]. |
| QIAamp DNA Stool Mini Kit | DNA purification from stool with built-in inhibitor removal technology. | Standard DNA extraction for PCR-based detection of enteric pathogens [52] [53]. |
| Inhibitor Removal Buffers (e.g., InhibitEX) | Binds and removes PCR inhibitors from stool samples during DNA extraction. | Essential pre-treatment step to prevent false-negative PCR results [53]. |
| Internal Control (e.g., Phocine Herpes Virus - PhHV) | Exogenous control added to sample to distinguish true negatives from PCR inhibition. | Spiked into every sample during extraction to monitor for inhibition in qPCR [53]. |
| Multiplex PCR Master Mix | Allows simultaneous amplification of multiple targets in a single reaction. | Enables concurrent detection of Cryptosporidium, Giardia, and an internal control [52]. |
| Cryptosporidium spp. Real-time PCR Assays | Specific primers and probes for detection and differentiation of Cryptosporidium species. | Identifying C. hominis vs. C. parvum for epidemiological studies [37] [56]. |
| 4-Decyn-3-one | 4-Decyn-3-one|High-Purity Research Chemical | 4-Decyn-3-one is a high-purity alkyne ketone for research use only (RUO). Explore its applications in organic synthesis and as a building block. Not for personal use. |
The detection and genetic characterization of Cryptosporidium, a significant waterborne protozoan pathogen, are crucial for public health surveillance and outbreak control. However, Polymerase Chain Reaction (PCR) based detection methods, essential for their sensitivity and specificity, are frequently compromised by inhibitory substances present in complex sample matrices. These inhibitors, originating from clinical (feces, blood) or environmental (water, soil) samples, can severely reduce amplification efficiency, leading to false-negative results and compromised data [57] [21] [58]. For researchers and diagnostics professionals, understanding and mitigating PCR inhibition is therefore not merely a technical exercise but a fundamental requirement for ensuring the reliability and accuracy of Cryptosporidium detection and genotyping efforts. This guide outlines the core mechanisms of inhibition and provides evidence-based strategies to overcome these challenges within a research and development context.
FAQs: Understanding PCR Inhibition
What are PCR inhibitors and where do they come from in Cryptosporidium research?
PCR inhibitors are a diverse group of organic or inorganic substances that interfere with the biochemical processes of nucleic acid amplification [59]. In the context of Cryptosporidium diagnostics, common inhibitors and their sources include:
- Humic and Fulvic Acids: These are degradation products from plant and organic matter, commonly found in water and soil samples, which are frequent sources of Cryptosporidium oocysts [57]. They are known to bind directly to DNA or the DNA polymerase enzyme [60].
- Complex Polysaccharides and Bile Salts: These are prevalent in human and animal fecal samples, a primary specimen for clinical diagnostics of cryptosporidiosis [59].
- Hemoglobin and Hematin: These are derived from blood, which may be present in some clinical stool samples or from sample processing methods [57] [60].
- IgG, Lactoferrin, and Heparin: These are intrinsic components of blood samples or anticoagulants used in sample collection [57].
How do I detect the presence of PCR inhibitors in my samples?
A common and effective method to test for inhibition is through sample dilution [59]. In a quantitative PCR (qPCR) assay, if a diluted sample (e.g., 1:10) results in a lower cycle threshold (Ct) value than the undiluted sample, this is a strong indicator that the original sample contained inhibitors. The dilution reduces the inhibitor concentration, thereby restoring amplification efficiency. Furthermore, the use of an Internal Amplification Control (IAC) is a highly recommended strategy for diagnostic applications [60]. An IAC is a non-target DNA sequence added to the PCR reaction. If the IAC fails to amplify while the sample is negative for the target, it confirms that the reaction is inhibited, helping to prevent false-negative interpretations.
Why is inhibition a particular problem for Cryptosporidium detection?
Cryptosporidium oocysts are often found in environmentally challenging matrices like water, soil, and feces, which are rich in the inhibitory substances listed above [58]. Furthermore, the oocyst itself has a tough wall that requires robust DNA extraction methods, such as bead beating or freeze-thaw cycles, to break it open and release DNA for PCR [13] [21]. These very methods can also co-extract and liberate PCR inhibitors from the sample matrix, creating a significant challenge for subsequent molecular detection.
What is the impact of using digital PCR (dPCR) compared to qPCR for inhibited samples?
Digital PCR (dPCR) has been demonstrated to be more resilient to the effects of many PCR inhibitors than qPCR [57]. In qPCR, inhibitors skew the quantification by affecting the amplification kinetics (Cq values), whereas dPCR relies on end-point, binary (positive/negative) measurements for quantification. This makes dPCR quantification less dependent on amplification efficiency. Additionally, the partitioning of the sample in dPCR may reduce the local concentration of inhibitors in individual reaction droplets, thereby facilitating amplification in partitions where the inhibitor-to-template ratio is low [57].
Troubleshooting Guide: Strategies to Overcome PCR Inhibition
A multi-faceted approach is most effective for combating PCR inhibition. The following workflow outlines a systematic strategy, from sample collection to amplification.
Best Practice 1: Optimize DNA Extraction and Purification
The choice of DNA extraction method is arguably the most critical step in determining the success of downstream PCR amplification.
- Mechanical Lysis: For tough-walled oocysts, mechanical disruption methods are superior. A comparative study on Cryptosporidium-spiked fecal samples found that a glass beads-based DNA extraction method achieved 100% sensitivity, significantly outperforming a freeze-thaw method with liquid nitrogen, which had a sensitivity of 83% [13]. The glass beads method also demonstrated a lower limit of detection (1 oocyst/g of fecal sample vs. 10 oocysts/g for freeze-thaw) [13].
- Specialized Purification Kits: Commercial kits designed for inhibitor removal are highly effective. These often use spin-column technology with proprietary matrices that bind inhibitory substances like humic acids, tannins, and melanins, allowing pure DNA to pass through [59]. Kits specifically formulated for fecal or soil samples (e.g., Zymo Research Quick-DNA Fecal/Soil Microbe Kits) are recommended for Cryptosporidium work [59].
- Direct PCR Methods: For samples with high DNA content, a "direct PCR" approach that minimizes or omits DNA purification can be used. This avoids DNA loss during purification but requires the use of highly inhibitor-tolerant DNA polymerases [57].
Best Practice 2: Optimize PCR Composition and Conditions
If inhibition persists after DNA extraction, optimizing the PCR reaction itself can provide a solution.
- Select Inhibitor-Tolerant Polymerases: The selection of DNA polymerase is crucial. Many modern polymerases are engineered for high inhibitor tolerance through mutagenesis or fusion strategies. Using polymerase blends that combine different enzyme properties can also synergistically enhance resistance to inhibitors [57] [60].
- Employ PCR Additives: The addition of certain compounds to the PCR mix can counteract inhibitors.
- Adjust Reaction Chemistry: Fine-tuning the reaction buffer, particularly the concentration of MgClâ‚‚, which is a critical cofactor for DNA polymerase, can restore amplification efficiency in partially inhibited reactions [61].
Quantitative Comparison of DNA Extraction Methods for Cryptosporidium
The table below summarizes key data from a study directly comparing two DNA extraction methods for detecting Cryptosporidium oocysts in fecal samples [13].
Table 1: Performance comparison of DNA extraction methods for Cryptosporidium detection via PCR
| DNA Extraction Method | Sensitivity | Limit of Detection | Key Findings |
|---|---|---|---|
| Glass Beads | 100% | 1 oocyst/g of fecal sample | Superior method for breaking oocyst wall and releasing DNA with minimal co-purification of inhibitors. |
| Freeze-Thaw (Liquid Nitrogen) | 83% | 10 oocysts/g of fecal sample | Less effective at DNA extraction, leading to higher false-negative rates. |
Mechanisms of Common PCR Inhibitors
Understanding how different inhibitors act can inform the choice of mitigation strategy.
Table 2: Common PCR inhibitors in Cryptosporidium research and their mechanisms of action
| Inhibitor Category | Example Sources | Primary Mechanism of Action |
|---|---|---|
| Humic Substances | Soil, water, surface waters [57] | Binds to DNA polymerase, blocking its active site; can also interact with nucleic acids [60]. |
| Heme Compounds | Blood, fecal samples [57] | Degrades DNA polymerase or interferes with its activity; can also quench fluorescence [60]. |
| Complex Polysaccharides | Feces, plant material [59] | Can impede diffusion and enzyme access by increasing viscosity; may bind to nucleic acids. |
| Metal Chelators | EDTA (anticoagulant) [57] | Chelates Mg²⺠ions, which are essential cofactors for DNA polymerase activity [59]. |
| Dyes and Tannins | Textiles (indigo), plant material [59] | Can bind to proteins (polymerase) or nucleic acids, interfering with their function. |
The Scientist's Toolkit: Research Reagent Solutions
The following table lists key reagents and their roles in overcoming PCR inhibition for sensitive Cryptosporidium detection.
Table 3: Essential research reagents for combating PCR inhibition
| Reagent / Kit | Function / Purpose | Application Context |
|---|---|---|
| Glass Beads (e.g., 0.5mm) | Mechanical cell lysis | Efficiently breaks tough Cryptosporidium oocyst walls to release DNA [13]. |
| Inhibitor Removal Kits | Binds and removes inhibitors | Purifies DNA from complex matrices like feces and soil (e.g., Zymo Research OneStep PCR Inhibitor Removal Kit) [59]. |
| Inhibitor-Tolerant Polymerase Blends | Robust DNA amplification | Maintains activity in the presence of common inhibitors (e.g., Phusion Flash [57]). |
| Bovine Serum Albumin (BSA) | Binds to inhibitors | Added to PCR mix to sequester inhibitors, preventing them from affecting the polymerase [61] [60]. |
| Betaine | Reduces secondary structure; counteracts inhibition | PCR additive that can enhance amplification efficiency and specificity in challenging samples [61]. |
| Internal Amplification Control (IAC) | Quality control for reaction failure | Distinguishes between true target-negative results and false negatives due to PCR inhibition [60]. |
The Role of Sample Concentration Techniques in Enhancing Yield
FAQs: Troubleshooting Sample Concentration forCryptosporidiumDetection
1. My sample concentration for Cryptosporidium is resulting in low oocyst recovery. What are the primary factors I should investigate?
Low oocyst recovery is often related to the choice and execution of the concentration method. First, ensure you are using an appropriate technique for your sample type (e.g., stool, water, soil). For stool samples, the Modified Formalin-Ether Concentration Technique (M-FECT) has been shown to provide enhanced detection of Cryptosporidium oocysts compared to standard methods [62]. If using filtration for water samples, be aware that the efficiency can vary with filter type and water turbidity. Finally, confirm your centrifugation parameters—using the correct Relative Centrifugal Force (RCF) and duration is critical for forming a pellet without damaging oocysts [63] [64].
2. I am dealing with PCR inhibition in downstream molecular detection after concentration. How can I overcome this?
PCR inhibition is a common challenge when concentrating samples, as inhibitors can also be co-concentrated. These inhibitors can include:
- Organic substances: Polysaccharides, humic acids, hemoglobin, melanin, and collagen [40].
- Inorganic substances: Metal ions that compete with magnesium, or EDTA that chelates magnesium [40]. To overcome this:
- Dilute the template: A 10- to 100-fold dilution of your DNA template can often reduce inhibitor concentration sufficiently for amplification [40].
- Use inhibitor-resistant polymerases: Select DNA polymerases formulated for higher tolerance to impurities [40].
- Choose an advanced detection method: Droplet Digital PCR (ddPCR) has been demonstrated to be less affected by PCR inhibitors compared to real-time PCR, leading to higher detection rates in complex environmental matrices like soil and water [25].
- Purify the DNA: Implement a DNA cleanup kit or ethanol precipitation step after extraction to remove impurities [40].
3. What is the difference between RPM and RCF, and why is it critical for concentration by centrifugation?
- RPM (Revolutions Per Minute) is a measure of the rotor's rotational speed.
- RCF (Relative Centrifugal Force or g-force) describes the actual gravitational force applied to the particles in the sample.
RCF is the scientifically meaningful value because it accounts for the rotor's radius, which varies between centrifuge models. Using only RPM can lead to inconsistent results if methods are transferred between different centrifuges. The force that causes particles like Cryptosporidium oocysts to sediment is the RCF. The formula to convert between them is:
RCF = 1.118 × 10â»âµ × r × (rpm)²
where r is the radial distance in centimeters [63]. For reproducible protocols, always specify and use RCF.
Technical Troubleshooting Guides
Guide 1: Troubleshooting Low Yield in Centrifugation
Centrifugation is a fundamental step in most concentration protocols. Suboptimal performance directly reduces yield.
| Problem Area | Common Causes | Recommended Solutions |
|---|---|---|
| Poor Pellet Formation | • Insufficient RCF / time• Using RPM instead of RCF• Incorrect rotor type | • Increase RCF or duration within optimal range for oocysts [64].• Always calculate and use RCF for method consistency [63].• Use a swinging bucket rotor for better pellet visibility or a fixed-angle rotor for shorter path lengths and faster separation [63] [64]. |
| Oocyst Damage | • Excessive RCF• Improper pH or osmolarity of suspension buffer | • Use a refrigerated centrifuge to manage heat generation [64].• Ensure the suspension medium is isotonic and buffered to maintain neutral pH and prevent structural damage [63]. |
Guide 2: Selecting and Optimizing a Concentration Method
The optimal concentration technique depends heavily on the sample matrix. The table below summarizes key methods and their applications.
| Method | Principle | Best For | Key Performance Notes |
|---|---|---|---|
| Modified FECT [62] | Formalin-ether sedimentation and concentration | Stool samples | Provides enhanced detection of Cryptosporidium oocysts from fecal material compared to standard FECT. |
| Membrane Filtration [65] | Physical trapping on a membrane filter | Large volumes of relatively clean water | Efficiency depends on filter pore size and sample turbidity. Followed by back-flushing or scraping to recover oocysts. |
| DEUF (Dead-End Ultrafiltration) [65] | Hollow fiber membranes trap microbes | Large volumes of various water types (turbid surface water to drinking water) | Can process 10–50 L of turbid water or hundreds of litres of drinking water. Highly flexible for field use. |
| Continuous Flow Centrifugation [64] | Continuous feeding and separation | Large volume liquid samples (e.g., culture media, water) | Rapidly processes large volumes without the need for repeated loading/unloading of samples. |
Experimental Protocols for Key Concentration Techniques
Protocol 1: Modified Formalin-Ether Concentration Technique (M-FECT) for Stool
This protocol is adapted from a study that demonstrated enhanced oocyst detection in stool samples [62].
1. Reagents and Materials:
- Formalin (10%)
- Diethyl ether
- Phosphate-Buffered Saline (PBS)
- Centrifuge tubes
- Centrifuge (capable of ~500 x g)
- Vortex mixer
2. Procedure:
- Step 1: Emulsify approximately 1 g of stool in 10% formalin.
- Step 2: Filter the suspension through gauze into a centrifuge tube to remove large debris.
- Step 3: Add an equal volume of diethyl ether to the filtrate in the tube. Securely cap the tube.
- Step 4: Vortex the mixture vigorously for 1 minute.
- Step 5: Centrifuge at 500 x g for 5 minutes. This will result in four layers: an ether plug at the top, a plug of debris, a formalin layer, and a sediment pellet at the bottom.
- Step 6: Carefully decant the top three layers. The sediment pellet contains the concentrated oocysts.
- Step 7: Re-suspend the pellet in PBS for downstream analysis (microscopy or DNA extraction).
Protocol 2: Differential Centrifugation for Cell-Free Culture or Water Samples
This is a general method for pelleting oocysts from liquid samples.
1. Reagents and Materials:
- Refrigerated centrifuge (capable of ~2,500 x g)
- Fixed-angle or swinging-bucket rotor
- Centrifuge tubes
2. Procedure:
- Step 1: Transfer the liquid sample to an appropriate centrifuge tube.
- Step 2: Centrifuge at 2,500 x g for 15 minutes at 4°C. The low temperature helps preserve oocyst integrity.
- Step 3: Carefully decant the supernatant without disturbing the pellet.
- Step 4: Re-suspend the pellet in a small volume of PBS or your chosen buffer. This concentrated sample is now ready for the next step.
The Scientist's Toolkit: Essential Reagents & Materials
| Item | Function in Concentration |
|---|---|
| Formalin (10%) | Preserves morphological integrity of parasites in fecal material and acts as a fixative and disinfectant [66] [62]. |
| Diethyl Ether | Used in sedimentation techniques to separate debris from parasites in the formalin-ether method [62]. |
| Phosphate-Buffered Saline (PBS) | An isotonic and buffered suspension medium; prevents osmotic damage to oocysts and maintains neutral pH during processing [63] [67]. |
| Dialysis Membranes | Semipermeable membranes used in specialized centrifugation and ultrafiltration devices for purification and concentration based on molecular size [68]. |
| Ammonium Sulfate (AS) | A common precipitant in protein purification; used in techniques like centrifugal precipitation chromatography to separate biomolecules based on solubility [68]. |
| Microcentrifuge | A table-top instrument for fast sedimentation of small sample volumes (0.5 µl to 2 ml), often used in DNA cleanup steps post-extraction [63] [64]. |
| Refrigerated Centrifuge | A centrifuge with temperature control (often to -20°C) essential for protecting heat-sensitive biomolecules and oocysts during prolonged or high-speed runs [64]. |
Frequently Asked Questions (FAQs)
Q1: Why might my real-time PCR results for Cryptosporidium be negative when my droplet digital PCR (ddPCR) results from the same sample are positive?
A1: This discrepancy is most commonly due to the presence of PCR inhibitors in the sample, which affect real-time PCR more significantly than ddPCR. Digital PCR is less prone to be affected by PCR inhibitors than real-time PCR [25]. To address this:
- Confirm with Controls: Run a positive control with a known, low concentration of oocysts to observe inhibition in your real-time PCR cycle threshold (Ct) values.
- Dilute the Sample: Try diluting your DNA template to reduce the concentration of inhibitors.
- Change Kits: Re-test using a DNA extraction kit optimized for your specific sample matrix (e.g., soil or produce) [25].
Q2: How can I determine which DNA extraction method is best for my specific sample type (water, soil, produce)?
A2: Extraction performance varies significantly by matrix [25]. You should validate methods using spiked samples. Based on comparative studies:
- For water samples, spin-column kits have demonstrated high performance [25].
- For soil and fresh produce, a different, specific spin-column kit was found to be most effective [25]. Create a validation protocol using samples spiked with a known number of oocysts (e.g., a serial dilution from 12,500 to 5 oocysts) to compare the efficiency and sensitivity of different extraction methods for your lab's specific needs [25].
Q3: What does a "significant discrepancy" between an observed result and an expected value mean in quantitative analysis?
A3: A significant discrepancy indicates a statistically meaningful difference between your measured data and the projected or standard value. This is often calculated as a Percent Discrepancy. To calculate it:
- Find the total discrepancy value (D) by subtracting the expected value (EV) from the observed value (or vice versa, depending on context).
- Apply the formula: Percent Discrepancy (PD) = (D / EV) * 100 [69]. This calculation helps identify errors, manage variations, and is crucial for accurate data interpretation in fields like data analysis and quality control [69].
Troubleshooting Guide: Resolving Conflicting Molecular Detection Results
This guide provides a step-by-step approach to diagnose why you might be getting conflicting results between different detection methodologies, such as real-time PCR and ddPCR.
Start Here: You have obtained conflicting results from two different detection assays.
Step 1: Verify the Source of the Discrepancy
Question: Is the discrepancy consistent across multiple sample replicates?
- If NO: The issue is likely related to random error or sample-specific problems.
- Action: Repeat the experiment with fresh aliquots of the same sample and include more replicates to ensure the result is reproducible.
- If YES: The discrepancy is systematic and requires further investigation. Proceed to Step 2.
Step 2: Analyze Methodological Context
Question: Were the samples processed and analyzed under identical conditions for both methodologies? [70]
Examine the circumstances surrounding each data set. Consider the time period, geographical location, and the population studied [70]. Discrepancies can arise simply because data were collected under different conditions [70].
- Action: Check and document:
- DNA Extraction: Was the same DNA extract used for both assays? If not, variations in extraction efficiency could be the cause.
- Sample Age & Storage: Were the samples stored for different durations before analysis?
- Reagent Lots: Were the same lots of master mix, primers, and probes used?
Step 3: Investigate Technical Inhibition
Question: Could PCR inhibitors be causing the discrepancy in one assay but not the other? [25]
As noted in research, ddPCR is less prone to be affected by PCR inhibitors than real-time PCR [25]. This is a common source of conflict.
- Action:
- Use an Internal Control: Spike your sample with a known quantity of a non-target DNA sequence to check for inhibition.
- Perform a Dilution Series: If the signal intensity increases with dilution in your real-time PCR, it strongly suggests the presence of inhibitors.
Step 4: Evaluate Assay Sensitivity and Optimization
Question: Have both methodologies been fully optimized and validated for the specific sample matrix you are using?
Research shows that detection sensitivity can vary by method and matrix. For example, DNA from as few as five oocysts was occasionally detectable, with performance varying by method [25].
- Action:
- Review Validation Data: Consult the literature or your own validation data to confirm the Limit of Detection (LOD) for each method on your sample type (e.g., soil, water, produce).
- Re-optimize Conditions: If one assay is newer to your lab, you may need to re-optimize primer concentrations, annealing temperatures, or cycle numbers.
Diagram: Troubleshooting Conflicting Results Workflow
The following tables summarize key experimental data from optimized Cryptosporidium detection protocols to serve as a benchmark for your own work.
Table 1: Performance of DNA Extraction Methods and PCR Assays Across Sample Matrices [25]
| Sample Matrix | Optimal DNA Extraction Method | Real-time PCR Sensitivity (Oocyst Count) | ddPCR Sensitivity (Oocyst Count) | Key Finding |
|---|---|---|---|---|
| Distilled Water | Spin-column Kit A | 5 oocysts (occasional) | 5 oocysts (occasional) | Both methods can achieve high sensitivity in pure water. |
| Environmental Water | Spin-column Kit A | Not consistently detected | Detected in 13.6% of samples | ddPCR less affected by environmental inhibitors. |
| Soil | Spin-column Kit B | Not detected | Detected in 23.3% of samples | ddPCR outperforms real-time PCR in complex soil matrices. |
| Fresh Produce | Spin-column Kit B | Not detected | Detected in 34.7% of samples | ddPCR is more reliable for detecting low levels on produce. |
Table 2: Cryptosporidium Contamination Rates in Environmental Samples from Agricultural Settings Using ddPCR [25]
| Sample Type | Sub-category | Contamination Rate | Note |
|---|---|---|---|
| Water | Surface Water | 28.6% | Highest contamination rate among water sources. |
| Soil | Amended with Fertilizer & Manure | 45.0% | Soil amendment practices significantly increase risk. |
| Fresh Produce | Roots | 46.7% | Highest contamination rate among produce types. |
| Fruiting Vegetables | 40.0% | -- | |
| Leafy Greens | 30.15% | -- |
Experimental Protocol: Evaluating DNA Extraction Methods for Cryptosporidium Detection
This protocol is adapted from research focused on improving detection sensitivity [25].
1. Sample Preparation and Spiking
- Materials: Distilled water, environmental water, soil, and fresh produce (e.g., lettuce, spinach).
- Procedure:
- Prepare a total of 188 artificially contaminated samples across all matrices.
- Inoculate each sample with a serial dilution of Cryptosporidium oocysts. The dilution series should range from 12,500 down to 5 oocysts to comprehensively test detection limits [25].
2. DNA Extraction
- Materials: Multiple DNA extraction kits, specifically including different spin-column kits [25].
- Procedure:
- Divide the spiked samples from Step 1.
- Extract DNA from each sample using at least three different extraction methods. The study evaluated 11 methods initially before selecting the top performers [25].
- Record the yield and purity of the extracted DNA.
3. Molecular Detection and Analysis
- Materials: Real-time PCR system, droplet digital PCR (ddPCR) system, primers, and probes specific for Cryptosporidium.
- Procedure:
- Test all extracted DNA samples using both real-time PCR and ddPCR.
- For each method and sample matrix, record the detection rate and the minimum number of oocysts that can be reliably detected.
- Analysis: Compare the results to determine which combination of DNA extraction method and detection assay provides the highest sensitivity for each specific sample matrix (water, soil, produce) [25].
Diagram: Experimental Workflow for Method Evaluation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Cryptosporidium Detection Research
| Item | Function | Example/Note |
|---|---|---|
| Spin-column DNA Extraction Kits | To isolate high-purity DNA from complex sample matrices like soil and produce. | Performance varies by matrix; different kits are optimal for water versus soil/produce [25]. |
| Real-time PCR Master Mix | To amplify and detect target DNA sequences in real-time using fluorescent probes. | Choose mixes with inhibitor-resistant polymers if working with environmental samples. |
| Droplet Digital PCR (ddPCR) Master Mix | To partition samples into nanodroplets for absolute quantification of DNA targets without a standard curve. | More resistant to PCR inhibitors present in environmental samples compared to real-time PCR [25]. |
| Cryptosporidium-specific Primers & Probes | To ensure specific binding and amplification of Cryptosporidium DNA. | Targets are often from the 18S rRNA or oocyst wall protein genes. |
| Phosphate-Buffered Saline (PBS) | To create spiked samples for method validation and calibration in a controlled medium [25]. | Used for creating serial dilutions of oocysts. |
| Positive Control DNA | To confirm that the PCR assays are functioning correctly and to help identify inhibition. | A plasmid containing the target sequence or DNA from a known positive sample. |
Benchmarking Performance: A Data-Driven Approach to Assay Selection
Performance Comparison for Protozoan Detection
Molecular detection of intestinal protozoa, including Cryptosporidium spp., is a critical tool for both clinical diagnostics and research. The table below summarizes key performance metrics from recent comparative studies.
| Parasite Target | Method Type | Sensitivity (%) | Specificity (%) | Notes / Key Findings |
|---|---|---|---|---|
| Giardia duodenalis | In-House Simplex PCR [71] | 96.9 | 93.6 | Performance can be superior to some commercial multiplex kits [71]. |
| Commercial RT-PCR (AusDiagnostics) [72] | Complete agreement with in-house PCR | Complete agreement with in-house PCR | High agreement for fixed fecal specimens [72]. | |
| Cryptosporidium spp. | In-House Simplex PCR [71] | 100 | 99.3 | Highly sensitive and specific in comparative studies [71]. |
| Commercial RT-PCR (AusDiagnostics) [72] | High Specificity | Limited Sensitivity | Inconsistent detection; sensitivity issues potentially from DNA extraction [72]. | |
| Commercial PCR (Various Kits) [71] | Variable | High | Performance depends on the specific kit and Cryptosporidium species [71]. | |
| Entamoeba histolytica | In-House Simplex PCR [71] | 100 | 100 | Essential for accurate diagnosis and differentiation from non-pathogenic species [72] [71]. |
| Commercial Multiplex PCR [71] | Excellent | Excellent | Allows molecular distinction of E. histolytica and E. dispar [71]. |
Interpretation: In-house assays often show high sensitivity and specificity, making them a robust "gold standard" in research settings. Commercial kits, particularly multiplex platforms, offer a standardized, time-saving alternative but may exhibit variable sensitivity for certain parasites like Cryptosporidium [72] [71]. The choice depends on the required balance between performance, throughput, and standardization.
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Why is my PCR assay showing no amplification or low yield for Cryptosporidium DNA?
- Confirm DNA Template Quality and Quantity: Use spectrophotometry or fluorometry to check concentration and purity. Poor quality may require template repurification or concentration [61].
- Optimize PCR Conditions: Adjust critical parameters:
- Check Reagents: Ensure the amount of DNA polymerase and dNTPs is sufficient. Using fresh, diluted working stocks is recommended [61] [74].
Q2: How can I reduce non-specific amplification and primer-dimer formation?
- Employ Hot-Start Polymerases: These enzymes remain inactive at room temperature, preventing non-specific primer extension during reaction setup [61].
- Redesign Primers Carefully: Use design software (e.g., OligoArchitect, Primer-BLAST) to ensure specificity and minimize 3'-end complementarity between primers. Avoid primers that can form stable dimers (ΔG ≥ -2.0 kcal) [73].
- Optimize Primer Concentration: Lowering primer concentration (e.g., to 200-400 nM) can reduce non-specific binding and primer-dimer formation [73].
Q3: What are the best practices for overcoming PCR inhibition from stool samples?
- Use PCR Additives: Incorporate Bovine Serum Albumin (BSA) or betaine into the reaction mix. BSA can bind inhibitors, freeing the polymerase to function [61].
- Optimize DNA Extraction: The efficiency of DNA extraction from robust protozoan oocysts is critical. Automated systems like MagNA Pure are effective, but the protocol may need adjustment for difficult samples [72] [75].
- Purify PCR Reagents: For highly sensitive detection, pre-treat master mixes with restriction enzymes (e.g., Sau3AI) to degrade contaminating bacterial DNA without affecting assay sensitivity [75].
Q4: When should I use a multiplex commercial kit versus an in-house simplex assay?
- Choose Commercial Multiplex Kits for routine screening where time-saving and simultaneous detection of multiple targets (e.g., Giardia, Cryptosporidium, Entamoeba) are priorities [71].
- Choose In-House Simplex Assays for maximum sensitivity and specificity for a single target, or when commercial kits show variable performance for your specific research needs, such as certain Cryptosporidium species [72] [71].
Stepwise PCR Optimization Protocol
For researchers developing or refining in-house PCR assays, follow this systematic optimization workflow to achieve high sensitivity and specificity.
Step 1: Validate Primer Design [73] [76]
- Homology Check: Ensure primers are homologous to the target Cryptosporidium sequence. Use BLAST-like tools to check for off-target binding.
- Avoid Primer-Dimers: Analyze self- and cross-dimer formation using software. The 3'-end dimer should be weak (ΔG ≥ -2.0 kcal).
- Leverage SNPs: For highly conserved genes, design primers based on Single-Nucleotide Polymorphisms (SNPs) unique to the target to differentiate between closely related species or strains [76].
Step 2: Optimize Primer Concentration [73]
- Prepare a matrix of forward and reverse primer concentrations (e.g., 50, 200, 400, 600 nM).
- Run the PCR and select the concentration combination that yields the lowest Cq (threshold cycle) value, high endpoint fluorescence, and a negative no-template control (NTC).
Step 3: Optimize Annealing Temperature (Ta) [73]
- Perform a gradient PCR with a Ta range, for example, from 55°C to 65°C.
- The optimal Ta produces the lowest Cq, a single specific product (verified by melt curve or gel electrophoresis), and high reproducibility between replicates.
Step 4: Validate Final Assay Performance [76]
- Using the optimized conditions, run a standard curve with a logarithmic serial dilution of the target DNA (e.g., 10-fold dilutions).
- The ideal assay should have an amplification efficiency (E) of 100% ± 5% (corresponding to a slope of -3.1 to -3.3) and a correlation coefficient (R²) ≥ 0.99.
The Scientist's Toolkit: Essential Research Reagents
This table outlines key reagents and their critical functions in optimizing PCR assays for sensitive pathogen detection.
| Reagent / Kit | Function / Application | Considerations for Sensitivity |
|---|---|---|
| Hot-Start DNA Polymerase | Reduces non-specific amplification and primer-dimer formation by remaining inactive until high temperatures [61]. | Critical for low-copy target detection; prevents enzyme activity during reaction setup. |
| Bovine Serum Albumin (BSA) | Additive that binds to PCR inhibitors commonly found in complex samples like stool [61]. | Improves robustness and reliability of reactions where DNA extraction may not remove all inhibitors. |
| Automated Nucleic Acid Extraction System | Standardizes and improves the efficiency of DNA purification from samples [72] [75]. | Inefficient DNA extraction from oocysts is a major cause of sensitivity loss [72]. |
| dNTPs | Building blocks for new DNA strands. | Low concentrations can cause no amplification or low yield; ensure fresh, high-quality stocks [61]. |
| Magnesium Chloride (MgClâ‚‚) | Cofactor for DNA polymerase; concentration affects enzyme activity, specificity, and yield [61] [73]. | A key optimization variable; suboptimal concentration is a common cause of PCR failure. |
Experimental Workflow for Comparative Studies
The following diagram outlines a robust methodology for conducting a head-to-head comparison of diagnostic PCR assays, as cited in recent literature.
Step 1: Sample Collection [72] [77]
- Collect a sufficient number of clinical stool samples (e.g., 90-355) from the target population. Include both freshly collected and preserved samples, as preservation can improve DNA stability [72].
Step 2: DNA Extraction [72] [75] [77]
- Use an automated, standardized nucleic acid extraction system (e.g., Roche MagNA Pure) with dedicated stool kits. The efficiency of this step is paramount, especially for breaking down robust oocysts of parasites like Cryptosporidium [72].
Step 3: Parallel PCR Testing [72] [71] [77]
- Test all extracted DNA samples in parallel using:
- The in-house PCR assay(s) to be evaluated.
- One or more commercial PCR kits (simplex or multiplex).
- A reference method (e.g., traditional microscopy or Direct Fluorescent Antibody (DFA)) for comparison [77].
Step 4: Data Analysis and Interpretation [71] [77]
- Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for each method against the reference standard.
- Use statistical tests like Cohen's Kappa to evaluate the level of agreement between methods. Interpret results in the context of your research goals, such as the need for ultimate sensitivity versus high-throughput convenience [71].
Analyzing Limits of Detection (LOD) for Key Cryptosporidium Species
Frequently Asked Questions (FAQs) on LOD and Assay Sensitivity
FAQ 1: What factors most significantly impact the Limit of Detection (LOD) in molecular assays for Cryptosporidium? The LOD is influenced by the entire experimental workflow, not just the amplification method. Key factors include:
- Sample Pre-treatment: Methods to concentrate oocysts from large volume samples (e.g., immunomagnetic separation) or mechanical disruption can greatly improve the recovery of target nucleic acids [78] [9] [79].
- Nucleic Acid Extraction: The efficiency of DNA isolation and purification is critical. Studies show that manual extraction methods can yield excellent results, though they are time-consuming. Automated systems like the Nuclisens Easymag have also been identified as effective [79].
- Target Gene and Amplification Method: The choice of target gene (e.g., 18S rRNA, gp60) and the amplification technique (e.g., qPCR, LAMP, HRM) directly affect sensitivity. For instance, targeting an intron-less gene can enhance ultrasensitive detection [78] [80].
FAQ 2: Why might my molecular assay fail to detect low levels of Cryptosporidium oocysts that are visible by microscopy? This discrepancy can occur due to:
- Inhibitors in Sample Matrices: Fecal or water samples often contain substances that inhibit polymerase enzymes in PCR-based reactions, leading to false negatives [9] [81]. Using an appropriate DNA extraction method that includes inhibitor removal steps is crucial.
- Sub-optimal DNA Extraction: If the DNA extraction protocol does not efficiently lyse the robust oocyst wall, the nucleic acid yield will be low, regardless of the oocyst count [79].
- LOD of the Assay: The molecular assay's inherent LOD may be higher than the oocyst count in your sample. For example, an assay with an LOD of 10 oocysts will not detect a sample containing only 5 oocysts [78] [82].
FAQ 3: How can I improve the sensitivity of my Cryptosporidium detection assay without changing the core amplification technology? Sensitivity can be enhanced by optimizing pre-analytical steps:
- Implement Oocyst Concentration: Use methods like formol-ether concentration or immunomagnetic separation to purify and concentrate oocysts from sample debris, thereby increasing the target concentration [9] [82].
- Evaluate DNA Extraction Kits: Systematically test different DNA extraction kits and protocols to find the most efficient one for your specific sample type (e.g., water, stool) [79].
- Use a Multi-Locus Approach: For genotyping, analyze multiple genetic loci (e.g., gp60 and others) to improve the reliability and discriminatory power of your detection [80].
Troubleshooting Guide: Common Experimental Issues and Solutions
Problem: Low Sensitivity or High LOD in a Newly Established LAMP Assay
| Symptom | Possible Cause | Proposed Solution |
|---|---|---|
| High LOD compared to literature. | Inefficient DNA release from oocysts. | Incorporate a direct heat lysis step [78] or a mechanical pre-treatment (e.g., bead beating) to break the tough oocyst wall [79]. |
| Inconsistent results between replicates. | Presence of PCR inhibitors in the sample. | Add an inhibitor removal step to your DNA extraction protocol. Diluting the DNA template can also help, though it may affect sensitivity [81]. |
| Assay fails to detect low oocyst numbers in water. | Lack of sample concentration. | Implement a pre-concentration step such as membrane filtration or flocculation before DNA extraction to capture oocysts from large water volumes [78] [81]. |
Problem: Inability to Differentiate Between Cryptosporidium Species or Subtypes
| Symptom | Possible Cause | Proposed Solution |
|---|---|---|
| gp60 sequencing results are unclear. | Low parasite DNA quantity or quality. | Ensure a high-quality DNA extraction and consider a nested PCR approach to amplify the target before sequencing [80]. |
| Need for a faster alternative to sequencing for subtyping. | Reliance on time-consuming DNA sequencing. | Develop or adopt a High-Resolution Melting (HRM) analysis method post-PCR. HRM can differentiate subtypes based on melting temperature variations in the gp60 gene's polymorphic region [80]. |
| Inadequate discriminatory power for outbreak tracing. | Using a single, non-variable genetic locus. | Move towards a Multi-Locus Variable Number Tandem Repeat Analysis (MLVA) scheme that analyzes several loci simultaneously for superior discrimination [80]. |
Quantitative Data Comparison of Detection Methods
The following table summarizes the Limits of Detection (LOD) for various Cryptosporidium detection methods as reported in the literature. This data is crucial for selecting an appropriate method for your sensitivity requirements.
Table 1: Comparison of Cryptosporidium Detection Method Performance
| Method Category | Specific Technique | Reported Limit of Detection (LOD) | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Molecular (Water) | Direct LAMP (post-magnetic isolation) | 5 oocysts/10 mL tap water [78] | Rapid, avoids commercial DNA kits, uses simple heat lysis [78]. | Requires oocyst concentration; performance may vary with water matrix. |
| Molecular (Stool) | Multiplex PCR (FTD Stool Parasite) | 100% detection achieved with optimal protocol combination [79]. | Can identify multiple parasites simultaneously. | Efficacy is highly dependent on pre-treatment and extraction methods [79]. |
| Molecular (RNA) | Smartphone AuNP biosensor | 5 µM of Cryptosporidium RNA [83] | Label-free, PCR-free, portable, uses smartphone for detection [83]. | Still an emerging technology; may require further validation. |
| Immunoassay (Stool) | CoproStrip RDT | Missed samples with very low oocyst density (1-4 oocysts) [82]. | Rapid (10 min), simple, no need for electricity or skilled microscopist [82]. | Lower sensitivity (62-74%) compared to microscopy; may give false negatives with low parasite burden [82]. |
| Microscopy (Stool) | Modified Ziehl-Neelsen Stain | ~10,000 - 50,000 oocysts/gram for unconcentrated stool [9]. | Low cost, indicates active infection [9] [82]. | Low sensitivity, time-consuming, requires experienced microscopist [9] [82]. |
Experimental Protocol: High-Sensitivity LAMP Detection from Water Samples
This protocol is adapted from a method designed to avoid commercial kit-based DNA isolation [78].
1. Sample Concentration and Oocyst Isolation:
- Collect water samples (e.g., 10 mL).
- Concentrate oocysts using immunomagnetic separation (IMS) with magnetic beads coated with anti-Cryptosporidium antibodies.
- Separate the bead-oocyst complex using a magnetic stand and wash to remove contaminants.
2. Direct Cell Lysis and DNA Release:
- Subject the isolated oocysts to a direct heat lysis step (e.g., 95-100°C for 10-15 minutes) in a lysis buffer to release genomic DNA.
- Centrifuge the lysate briefly, and use the supernatant directly as the template for amplification.
3. Loop-Mediated Isothermal Amplification (LAMP):
- Prepare a LAMP reaction mix containing:
- Isothermal amplification buffer (e.g., 1x)
- Betaine (e.g., 0.8 M)
- MgSOâ‚„ (e.g., 6-8 mM)
- dNTPs (e.g., 1.4 mM each)
- Specific inner primers (FIP/BIP, e.g., 1.6 µM each)
- Specific outer primers (F3/B3, e.g., 0.2 µM each)
- Strand-displacing DNA polymerase (e.g., 8 U)
- Template DNA (from step 2)
- Incubate the reaction at an isothermal temperature (e.g., 60-65°C) for 45-60 minutes.
- Terminate the reaction by heating at 80°C for 5 minutes.
4. Detection of Amplicons:
- Visual inspection for a color change (if using a colorimetric dye) or turbidity (from magnesium pyrophosphate precipitate).
- Alternatively, analyze products using gel electrophoresis.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Cryptosporidium Detection Experiments
| Item | Function/Application | Example from Literature |
|---|---|---|
| Immunomagnetic Beads | Concentration and purification of oocysts from complex samples like water or stool by binding to oocyst-wall antigens [78] [9]. | Used for pre-analytical isolation of oocysts prior to direct heat lysis [78]. |
| Strand-displacing DNA Polymerase | Essential enzyme for LAMP assays. Its strand-displacement activity enables isothermal amplification without the need for thermal denaturation [81]. | Used in LAMP reactions for detecting Cryptosporidium in water samples [78] [81]. |
| gp60 Gene Primers | For nested PCR and subsequent subtyping via sequencing or High-Resolution Melting (HRM) analysis. Targets a highly polymorphic gene for epidemiological studies [80]. | Used for differentiating C. parvum gp60 subtypes based on tandem repeat variations [80]. |
| High-Resolution Melting Dye | Intercalating dye used in real-time PCR instruments to precisely monitor DNA dissociation, allowing discrimination of amplicons with small sequence differences [80]. | Enables subtyping of Cryptosporidium without sequencing by analyzing melting curve differences [80]. |
| Gold Nanoparticles (AuNPs) | Serve as a colorimetric reporter in biosensors. Aggregation state changes (red to blue) upon target binding (e.g., RNA), enabling label-free detection [83]. | Used in a portable smartphone-integrated biosensor for direct Cryptosporidium RNA detection [83]. |
Workflow Diagram: Decision Pathway for Method Selection Based on Sensitivity Needs
The diagram below outlines a logical workflow for selecting an appropriate detection method based on the sensitivity requirements and application context of the researcher.
Cryptosporidium is a critical waterborne protozoan pathogen and a major cause of serious illnesses worldwide, with detection and treatment costing millions of dollars annually [58]. The accurate detection of Cryptosporidium oocysts in fecal and environmental samples presents significant challenges for researchers and clinicians due to the organism's small size (4.2-5.4 µm in diameter) and the potential for confusion with yeast cells in microscopic analysis [15] [84]. The diagnostic landscape encompasses various methodologies, including conventional microscopy, immunodiagnostic techniques, and molecular approaches, each with varying degrees of sensitivity and specificity [84]. Within this context, the Direct Fluorescent Antibody (DFA) assay has emerged as a reference technique that offers the highest combination of sensitivity and specificity for Cryptosporidium detection [84] [85]. This technical support center resource aims to provide researchers, scientists, and drug development professionals with comprehensive troubleshooting guidance and methodological insights for implementing DFA testing within the broader framework of improving detection sensitivity in Cryptosporidium research.
Comparative Diagnostic Performance Data
Quantitative Comparison of Detection Methods
Table 1: Performance comparison of Cryptosporidium detection methods based on recent studies
| Method | Sensitivity | Specificity | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Direct Fluorescent Antibody (DFA) | Highest combination of sensitivity and specificity [84] | Considered gold standard by many laboratories [84] | Cost-effective; high sensitivity and specificity [84] | Requires fluorescent microscopy equipment |
| Modified Acid-Fast Staining | 83% (glass beads method) to 100% (freeze-thaw method) [13] | High specificity [85] | Low cost; allows evaluation of internal oocyst structure [86] | Requires experience; low reproducibility; time-consuming [86] |
| PCR-Based Methods | 100% sensitivity with optimal DNA extraction [13] | 100% specificity with optimal DNA extraction [13] | Species identification; detects non-viable organisms [86] | High cost; complex for routine use [84] |
| Immunochromatographic Test (ICT) | Variable; detected 4 of 7 positive samples in one study [85] | Useful for laboratories with intensive workflow [85] | Rapid results (15-30 minutes); practical use [84] | Limited diagnostic sensitivity; false positives [84] |
| Enzyme Immunoassays (EIA) | Close to immunofluorescence [15] | High specificity [15] | Suitable for batch testing | May miss low-level infections |
Table 2: Detection limits of Cryptosporidium methods in experimental conditions
| Method | Limit of Detection | Experimental Context |
|---|---|---|
| PCR with Glass Beads DNA Extraction | 1 oocyst/g fecal sample [13] | Nested PCR targeting SSU rRNA gene [13] |
| PCR with Freeze-Thaw DNA Extraction | 10 oocysts/g fecal sample [13] | Nested PCR targeting SSU rRNA gene [13] |
| Safranin-Methylene Blue Staining | More sensitive than Ziehl-Neelsen methods [87] | Detected 26 cases vs. 19 by acid-fast methods [87] |
Research Reagent Solutions
Table 3: Essential research reagents for Cryptosporidium detection using DFA
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Merifluor Cryptosporidium/Giardia DFA Kit | Detects surface antigens of Cryptosporidium oocysts [86] | Combined test available for both pathogens |
| Potassium Dichromate (2.5%) | Specimen preservation for molecular testing [15] | Preferred over formalin for DNA preservation |
| Formalin-Ethyl Acetate | Sedimentation concentration method [15] | Increased centrifugation speed (500 x g, 10 min) improves oocyst recovery |
| QIAamp DNA Stool Mini Kit | DNA extraction for PCR confirmation [86] | Enables molecular characterization after DFA screening |
| Acid-Methanol Fixative | Slide preparation for stained methods [87] | Alternative to heat fixation for staining procedures |
Experimental Protocols for DFA Implementation
Standard DFA Protocol for Cryptosporidium Detection
Principle: The DFA method utilizes fluorescein-labeled monoclonal antibodies that specifically bind to surface antigens on Cryptosporidium oocysts, allowing for their visualization under fluorescence microscopy [86].
Materials:
- Merifluor Cryptosporidium/Giardia Direct Immunofluorescence Assay kit or equivalent
- Fluorescence microscope with appropriate filters (FITC excitation/emission)
- Stool samples preserved in appropriate fixatives
- Concentrated specimen prepared by formalin-ethyl acetate sedimentation
- Glass slides, coverslips, and mounting medium
- Positive and negative control slides
Procedure:
- Sample Preparation: Process stool samples using formalin-ethyl acetate sedimentation concentration method with increased centrifugation speed (500 x g for 10 minutes) to maximize oocyst recovery [15].
Slide Preparation: Prepare smears of concentrated fecal material on clean glass slides. Allow to air-dry completely.
Fixation: Fix smears according to manufacturer's instructions, typically with alcohol-based fixatives.
Staining: Apply fluorescein-labeled anti-Cryptosporidium antibody according to manufacturer's recommended volume and incubation time (typically 30 minutes at room temperature in a humidified chamber).
Washing: Gently rinse slides with phosphate-buffered saline or the wash buffer provided in the kit to remove unbound antibody.
Mounting: Apply mounting medium and coverslip to preserve fluorescence.
Microscopy: Examine slides using a fluorescence microscope with appropriate magnification (200-400x). Cryptosporidium oocysts will appear as apple-green fluorescent structures with characteristic size (4.2-5.4 µm) and morphology [15].
Interpretation: Compare with positive and negative controls. True oocysts exhibit uniform fluorescence and typical morphology. Consider using DAPI counterstaining for enhanced visualization of internal structures.
Protocol for Combined DFA-PCR Approach
Principle: This sequential approach leverages the high sensitivity of DFA for initial detection followed by PCR confirmation and species identification, providing both diagnostic accuracy and genetic characterization [84].
Procedure:
- Sample Division: Divide fresh stool samples into three aliquots upon receipt: one for DFA, one for DNA extraction, and one for archival storage at -80°C [86].
DFA Screening: Perform DFA testing as described in section 3.1 on the first aliquot.
DNA Extraction: For DFA-positive samples or those with equivocal results, use the QIAamp DNA Stool Mini Kit or equivalent for DNA extraction from the second aliquot [86]. Note that formalin-based fixatives are not recommended if molecular testing will be performed due to unfavorable effects on nucleic acids [15].
Molecular Characterization: Perform real-time PCR using established primer and probe sequences targeting Cryptosporidium genes. The SSU rRNA gene is particularly suitable as primers for this region are more successful in producing amplification than other targets like the TRAP-C2 gene [13].
Diagram 1: DFA-PCR workflow for enhanced detection
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Why is DFA considered the gold standard for Cryptosporidium detection despite the availability of molecular methods?
DFA offers the highest combination of sensitivity and specificity in a cost-effective format, making it suitable for routine diagnostic use [84]. While PCR methods can provide superior sensitivity under optimal conditions (100% with proper DNA extraction), they require specialized equipment, higher costs, and more technical expertise, limiting their accessibility for many clinical settings [13] [84]. DFA provides visual confirmation of oocyst morphology along with specific antigen detection, serving as an excellent screening method that can be complemented by PCR for species identification.
Q2: What are the common causes of false-negative results in DFA testing, and how can they be minimized?
False negatives can occur due to low oocyst shedding, improper sample collection, inadequate concentration methods, or sample degradation. To minimize these issues:
- Test multiple stool specimens collected on different days as oocyst shedding can be intermittent [15]
- Use formalin-ethyl acetate sedimentation with increased centrifugation speed (500 x g for 10 minutes) to maximize oocyst recovery [15]
- Ensure proper sample preservation using 2.5% potassium dichromate if molecular confirmation is anticipated [15]
- Process samples promptly or store appropriately to prevent degradation
Q3: How does the performance of DFA compare with modified acid-fast staining in clinical practice?
DFA demonstrates superior sensitivity compared to modified acid-fast staining. In one study, DFA detected 6 positive samples out of 51 tested, while modified acid-fast staining identified only 5 positives out of 90 samples [85]. Modified acid-fast staining, while cost-effective and allowing evaluation of internal oocyst structure, requires more experience for accurate interpretation and has lower reproducibility [86]. The staining of Cryptosporidium oocysts can be variable, and in resolving infections, increasing numbers of non-acid-fast "ghost" oocysts may lead to false-negative results [15].
Q4: What is the recommended approach for laboratories with high workflow needing rapid results?
For laboratories with intensive workflow, immunochromatographic tests (ICT) can be useful due to their practical application and rapid results (15-30 minutes) [85]. However, these tests should be interpreted with caution as they often have limited diagnostic sensitivities and potentially high rates of false-positive results [84]. A two-tiered approach using ICT for initial screening followed by DFA confirmation of positive results may provide an optimal balance between workflow efficiency and diagnostic accuracy.
Troubleshooting Common Experimental Issues
Problem: Weak or Faint Fluorescence
- Potential Cause 1: Antibody degradation due to improper storage or repeated freeze-thaw cycles
- Solution: Check expiration dates, ensure proper storage conditions, and avoid repeated freezing and thawing of reagents
- Potential Cause 2: Insufficient incubation time or temperature variations
- Solution: Strictly adhere to manufacturer's recommended incubation protocols and use a humidified chamber to prevent evaporation
Problem: High Background Fluorescence
- Potential Cause 1: Inadequate washing after antibody application
- Solution: Increase wash time or volume, consider adding a brief rinse with distilled water after buffer washing
- Potential Cause 2: Contaminated slides or reagents
- Solution: Use fresh reagents and ensure slides are clean before sample application
Problem: Inconsistent Results Between Replicates
- Potential Cause 1: Uneven sample distribution on slides
- Solution: Ensure proper mixing of samples before slide preparation and use consistent smearing technique
- Potential Cause 2: Variation in sample concentration
- Solution: Standardize the concentration procedure and consistently apply the recommended centrifugation parameters
Problem: Discrepancy Between DFA and PCR Results
- Potential Cause 1: Inhibition of PCR reaction by fecal constituents
- Solution: Include internal controls in PCR reactions and use validated DNA extraction protocols specifically designed for stool samples [86]
- Potential Cause 2: Non-viable or disrupted oocysts that retain antigenicity but not amplifiable DNA
- Solution: Interpret results in clinical context and consider repeat testing on fresh samples if discrepant results occur
Advanced Applications and Research Implications
Enhancing Sensitivity Through Methodological Integration
The integration of DFA with complementary detection technologies represents the most promising approach for advancing Cryptosporidium research sensitivity. Studies have demonstrated that identification of Cryptosporidium infections is most effectively accomplished by the combination of DFA and PCR techniques (p-value: < 0.001) [84]. This integrated methodology leverages the visual confirmation and high throughput capability of DFA with the species discrimination power and sensitivity of molecular methods.
Recent technological advances in nanotechnology, biosensing, and microfluidics offer potential for future development of sophisticated detection tools that could complement or enhance traditional DFA methods [58]. These emerging technologies aim to address limitations of conventional methods, such as long processing times, large sample volumes, and requirements for bulky laboratory equipment, potentially enabling real-time and on-site monitoring in water resources and remote areas [58].
Research Applications in Zoonotic and Environmental Studies
DFA testing plays a critical role in understanding the epidemiology of cryptosporidiosis, particularly in zoonotic transmission studies. Cryptosporidium parvum and C. hominis are the leading causes of human cryptosporidiosis, with zoonotic subtype families of C. parvum commonly associated with cattle, particularly calves [15]. The ability to reliably detect Cryptosporidium in both clinical and environmental samples using DFA provides researchers with a standardized method for comparative studies across host species and geographic regions.
The application of DFA in environmental monitoring represents another significant research application, given that Cryptosporidium is a critical waterborne pathogen [58]. The method's cost-effectiveness and reliability make it suitable for large-scale water quality surveys, though limitations remain in detection threshold for very low-level environmental contamination.
Diagram 2: DFA comparative advantages and research applications
The Direct Fluorescent Antibody assay represents a cornerstone methodology in Cryptosporidium detection that balances diagnostic accuracy with practical implementation. While emerging technologies promise future advances in detection capabilities, DFA currently offers researchers and clinicians the most reliable combination of sensitivity, specificity, and cost-effectiveness for routine use. The method's particular strength lies in its ability to be integrated with molecular techniques in a complementary fashion, providing both immediate diagnostic information and material for subsequent genetic characterization. As research continues toward improving Cryptosporidium detection sensitivity, DFA remains an essential component of the methodological arsenal, particularly for studies requiring standardized, reproducible results across multiple sample types and laboratory settings. Future developments in biosensing and microfluidic technologies may build upon the fundamental principles of antigen-antibody recognition that make DFA so reliable, potentially leading to next-generation detection platforms that preserve the strengths of DFA while addressing its limitations in throughput and quantification.
Accurate detection of the parasite Cryptosporidium is critical for both clinical diagnosis and public health surveillance. However, the absence of a perfect "gold standard" test complicates the evaluation of new diagnostic methods. This guide explores the core statistical frameworks—including sensitivity, specificity, and Latent Class Analysis (LCA)—used to validate new diagnostic assays for cryptosporidiosis in the absence of a perfect reference standard, thereby improving the sensitivity and reliability of detection in research settings.
Performance Metrics for Diagnostic Tests
Core Definitions
- Sensitivity: The proportion of true positive subjects that are correctly identified by the test. A highly sensitive test is reliable for ruling out disease when its result is negative.
- Specificity: The proportion of true negative subjects that are correctly identified by the test. A highly specific test is reliable for ruling in disease when its result is positive.
- Positive Predictive Value (PPV): The probability that a subject with a positive test result truly has the disease.
- Negative Predictive Value (NPV): The probability that a subject with a negative test result truly does not have the disease.
Quantitative Performance of Diagnostic Assays forCryptosporidium
The following table summarizes the performance of various diagnostic techniques as reported in recent studies:
Table 1: Comparison of Diagnostic Test Performance for Cryptosporidium Detection
| Diagnostic Method | Sensitivity (%) | Specificity (%) | Research Context | Citation |
|---|---|---|---|---|
| Immunochromatography (IC) | 74.1 | 90.0 | Cattle fecal samples [88] | |
| Modified Ziehl-Neelsen (mZN) | 47.2 | 98.3 | Cattle fecal samples [88] | |
| Enzyme-Linked Immunosorbent Assay (ELISA) | 48.0 | 95.7 | Cattle fecal samples [88] | |
| Real-time PCR (SSU rRNA target) | 100.0 | 96.9 | Human stool samples [89] | |
| Real-time PCR (COWP target) | 90.0 | 99.6 | Human stool samples [89] | |
| Real-time PCR (DnaJ target) | 88.8 | 96.9 | Human stool samples [89] | |
| Polymerase Chain Reaction (PCR) | 100.0 | 99.1 | Validation against conventional PCR [37] |
Latent Class Analysis (LCA) for Imperfect Standards
Concept and Workflow
Latent Class Analysis (LCA) is a statistical model used to evaluate diagnostic tests when a gold standard is unavailable. It uses results from multiple imperfect tests to estimate their true sensitivity and specificity by identifying an underlying, unobserved (or "latent") disease status [90].
The following diagram illustrates the workflow and logical relationships in applying LCA for diagnostic test validation:
Experimental Protocol for LCA
A study on detecting Cryptosporidium in asymptomatic livestock provides a template for applying LCA [90] [91]:
- Sample Collection and Tests: Collect fecal samples from the target population (e.g., cattle, sheep). Subject each sample to multiple diagnostic tests, such as:
- Data Compilation: Create a dataset where each row represents a sample and each column represents the result (positive/negative) from a different test.
- Statistical Modeling: Input this data into an LCA model. The model treats the true infection status as a latent variable and uses the patterns of agreement and disagreement between the tests to estimate the sensitivity and specificity of each test.
- Interpretation: The LCA output provides the estimated sensitivity and specificity for each test. Researchers can use these values to determine the most reliable tests and optimal testing algorithms for their specific context.
Frequently Asked Questions (FAQs) on Statistical Validation
Q1: Why can't we use a single, good test as a gold standard for Cryptosporidium detection? No single test is perfect. Microscopy has low sensitivity, requiring a high oocyst concentration (>50,000/mL) for detection [92]. Antigen tests can yield false positives [88], and even PCRs can vary in performance based on the genetic target used [89]. Using an imperfect test as a gold standard introduces incorporation bias, skewing the evaluation of new tests. LCA avoids this by not relying on a single reference [90].
Q2: We are evaluating a new rapid IC test. Our comparison to microscopy shows poor agreement. What should we do? This is a common challenge. Microscopy has low sensitivity (as low as 47% in some studies), so it is a poor comparator [88]. To robustly validate your IC test:
- Adopt a Composite Reference Standard (CRS): Classify a sample as "truly positive" if it is positive by at least 2 out of 3 different methods (e.g., IC, ELISA, and PCR), excluding the test under evaluation. This creates a more robust pseudo-gold standard [88].
- Implement LCA: If resources and sample size allow, LCA provides the most statistically rigorous evaluation without designating a gold standard [90].
Q3: How do I choose which tests to include in an LCA model? Include at least three different tests that are conditionally independent—meaning the chance of one test being wrong is not directly related to another test being wrong. A typical combination for Cryptosporidium includes a microscopy method (e.g., mZN), an antigen test (e.g., IC or ELISA), and a molecular test (e.g., PCR) [90] [88].
Q4: Our new PCR assay is highly sensitive but occasionally detects non-pathogenic species. How do we account for this in validation? High sensitivity alone is not sufficient; specificity is equally critical. This challenge can be addressed by:
- Using a Combination of PCR Targets: Use a highly sensitive PCR (e.g., targeting SSU rRNA) for initial screening, followed by a more specific PCR (e.g., targeting the COWP gene) for confirmation [89].
- Sequencing for Confirmation: Perform sequencing on a subset of PCR-positive samples to confirm the species and verify that the detected Cryptosporidium is a human pathogen [37] [93].
Research Reagent Solutions for Validation Experiments
Table 2: Essential Reagents and Kits for Cryptosporidium Detection Assays
| Reagent / Kit | Function / Target | Application in Validation |
|---|---|---|
| Kinyoun's Carbol-Fuchsin Stain | Acid-fast staining of oocyst walls | Conventional microscopy; one input for LCA models [92] [90]. |
| FITC-labeled Anti-Cryptosporidium mAb | Binds to oocyst wall antigens | Direct Fluorescent Antibody Test (DFAT); a sensitive microscopic method [90]. |
| Commercial IC Kits (e.g., Crypto/Giardia IC) | Detects specific coproantigens | Rapid, point-of-care testing; evaluating ease-of-use vs. performance [92] [88]. |
| PCR Primers (18S rRNA gene) | Amplifies conserved ribosomal RNA gene | Highly sensitive molecular detection; often used as a reference in CRS [90] [89]. |
| PCR Primers (COWP gene) | Amplifies oocyst wall protein gene | Used for confirmatory testing and species differentiation [89] [37]. |
| QIAamp Stool DNA Kit | DNA extraction from stool samples | Critical step for molecular methods; ensures high-quality template for PCR [89]. |
| TaqMan Environmental Master Mix | PCR reaction mix for probe-based assays | Essential reagent for sensitive and specific real-time PCR assays [37]. |
Conclusion
The journey to sensitive Cryptosporidium detection requires a paradigm shift from traditional, low-yield methods to a sophisticated, molecular-based approach. As evidenced by recent surveillance data, this transition is not merely technical but essential for uncovering the true scale of cryptosporidiosis, which has significant implications for public health and patient care. The future lies in the widespread adoption and continuous refinement of PCR-based methods, coupled with robust DNA extraction and rigorous validation. For researchers and drug developers, these advances provide the reliable detection necessary for accurate epidemiological studies, effective outbreak management, and the critical evaluation of novel therapeutics and vaccines. Embracing a One Health perspective that integrates human, animal, and environmental testing will be crucial to fully understanding and controlling the transmission of this resilient pathogen.
References
- 1. Cryptosporidium spp. diagnosis and research in the 21st century - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8390533/]
- 2. Distribution, Public Global and Clinical Impact of the Protozoan... Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC2913630/]
- 3. Cryptosporidium Infection: Epidemiology, Pathogenesis, and Differential Diagnosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6945992/]
- 4. The Most Neglected NTD: Cryptosporidiosis | Global NOW Health [https://globalhealthnow.org/2025-01/most-neglected-ntd-cryptosporidiosis]
- 5. Cryptosporidium/Giardia Detection and Identification ... [https://www.rapidmicrobiology.com/test-method/cryptosporidium-and-giardia-detection-and-identification-methods-2]
- 6. Comparative sensitivity of PCR primer sets for detection of... [https://pubmed.ncbi.nlm.nih.gov/19724705/]
- 7. Molecular analysis of Cryptosporidium species in Western Australian... [https://pubmed.ncbi.nlm.nih.gov/41130355/]
- 8. Performance evaluation of point-of-care test for detection of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4030457/]
- 9. Laboratory diagnosis of cryptosporidiosis - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5991046/]
- 10. Comparison of PCR and microscopy for detection of... [https://pubmed.ncbi.nlm.nih.gov/9542924/]
- 11. Comparison of PCR and Microscopy for Detection of Cryptosporidium parvum in Human Fecal Specimens: Clinical Trial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC104676/]
- 12. , specificity and comparison of three commercially available... Sensitivity [https://www.elsevier.es/es-revista-brazilian-journal-microbiology-490-articulo-sensitivity-specificity-comparison-three-commercially-S1517838216309868]
- 13. The sensitivity of PCR detection of Cryptosporidium oocysts in fecal samples using two DNA extraction methods - PubMed [https://pubmed.ncbi.nlm.nih.gov/15068384/]
- 14. Detecting Cryptosporidium in Stool Samples Submitted to a Reference Laboratory - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7356455/]
- 15. CDC - DPDx - Cryptosporidiosis [https://www.cdc.gov/dpdx/cryptosporidiosis/index.html]
- 16. Comparison of ELISA and Microscopy for Detection of... [https://scialert.net/fulltext/?doi=pjbs.2015.341.345]
- 17. Performance enhancement of real-time detection of protozoan parasite, Cryptosporidium oocyst by a modified surface plasmon resonance (SPR) biosensor - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0141022906001025]
- 18. From rare to recognized: enhanced detection uncovers... [https://pubmed.ncbi.nlm.nih.gov/40609035/]
- 19. Comparative Sensitivity of PCR Primer Sets for Detection of Cryptosporidium parvum - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2735697/]
- 20. Development of a sensitive detection system for Cryptosporidium in environmental samples - PubMed [https://pubmed.ncbi.nlm.nih.gov/16387443/]
- 21. Advancing Cryptosporidium Diagnostics from Bench to Bedside | Current Tropical Medicine Reports [https://link.springer.com/article/10.1007/s40475-015-0055-x]
- 22. Hypothesis: Cryptosporidium genetic diversity mirrors national... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-015-0921-3]
- 23. cambridge.org/core/journals/parasitology/article/abs/ molecular ... [https://www.cambridge.org/core/journals/parasitology/article/abs/molecular-characterization-of-danish-cryptosporidium-parvum-isolates/85BDC26A572182AB5DEF80FC6ED73F92]
- 24. infections in terrestrial ungulates with focus on... Cryptosporidium [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-019-3704-4]
- 25. Optimized Molecular Detection of Cryptosporidium within the... [https://pubmed.ncbi.nlm.nih.gov/40571259/]
- 26. Recent Breakthroughs and Ongoing Limitations in Cryptosporidium Research - PubMed [https://pubmed.ncbi.nlm.nih.gov/30228873/]
- 27. Novel treatment strategies and drugs in development for cryptosporidiosis - PubMed [https://pubmed.ncbi.nlm.nih.gov/30003818/]
- 28. for Gastrointestinal... Multiplex Polymerase Chain Reaction Panels [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541719/]
- 29. What is Syndromic Test? Uses, How It Works & Top... Multiplex [https://www.linkedin.com/pulse/what-syndromic-multiplex-test-uses-how-works-top-companies-lirqf]
- 30. Syndromic Testing: The Right Test, The First Time | BioFire Diagnostics [https://www.biofiredx.com/syndromic-testing/]
- 31. Syndromic diagnostic testing: a new way to approach patient care in the treatment of infectious diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8460095/]
- 32. Syndromic Testing—The Evaluation of Four Novel Multiplex Real-Time Polymerase Chain Reaction Panels [https://www.mdpi.com/2075-4418/15/10/1228]
- 33. Performance Evaluation of Multiplex Molecular Syndromic Panel vs. Singleplex PCR for Diagnosis of Acute Central Nervous System Infections [https://www.mdpi.com/2076-2607/13/4/892]
- 34. How Multiplex Disease Diagnosis | Babirus LLC PCR Improves [https://www.babirus.ae/how-is-multiplex-pcr-improving-disease-diagnosis/]
- 35. Multicentric evaluation of a new real-time PCR assay for quantification... [https://pubmed.ncbi.nlm.nih.gov/23720792/]
- 36. Multicentric Evaluation of a New Real-Time PCR Assay for Quantification of Cryptosporidium spp. and Identification of Cryptosporidium parvum and Cryptosporidium hominis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3719639/]
- 37. and Differentiation of Detection spp. in Human... Cryptosporidium [https://pmc.ncbi.nlm.nih.gov/articles/PMC3067739/]
- 38. A Sensitive and Specific PCR Based Method for Identification of Cryptosporidium Sp. Using New Primers from 18S Ribosomal RNA - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3279906/]
- 39. PCR Basic Troubleshooting Guide [https://www.creative-biogene.com/blog/pcr-basic-troubleshooting-guide]
- 40. Troubleshooting your PCR [https://www.takarabio.com/learning-centers/pcr/faq/troubleshooting]
- 41. Polymerase Chain Reaction: Basic Protocol Plus Troubleshooting and Optimization Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846334/]
- 42. Bead Beating Guide Contents and Introduction [https://opsdiagnostics.com/notes/ranpri/bbguide1.html]
- 43. Sample Preparation for Optimizing : A DNA for... Extraction Guide [https://dpxtechnologies.com/optimizing-sample-preparation-for-dna-extraction/]
- 44. Bacterial Cell Disruption by Bead Beating [https://opsdiagnostics.com/applications/applicationtable/microorganism/bacteria.htm]
- 45. of a Optimization for improving bacterial... DNA extraction protocol [https://pmc.ncbi.nlm.nih.gov/articles/PMC11457918/]
- 46. Optimization of high-yielding protocol for DNA extraction from the forest rhizosphere microbes - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5447523/]
- 47. Magnetic Beads in Nucleic Acid Purification: A Workflow Guide for... [https://gentelbio.com/magnetic-beads-in-nucleic-acid-purification-a-workflow-guide-for-high-yield-dna-and-rna-extraction/]
- 48. Increased sensitivity using real-time dPCR for detection of SARS-CoV-2 - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7888512/]
- 49. Modified PCR protocol to increase sensitivity for determination of bacterial community composition | Microbiome | Full Text [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-020-00958-y]
- 50. An advanced uracil DNA glycosylase-supplemented loop-mediated... [https://pubmed.ncbi.nlm.nih.gov/29366630/]
- 51. Cryptosporidium: Methods and Protocols | SpringerLink [https://link.springer.com/book/10.1007/978-1-4939-9748-0]
- 52. Dual probe DNA capture for sensitive real-time PCR detection of Cryptosporidium and Giardia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3319247/]
- 53. Examination of ELISA against PCR for assessing treatment efficacy against Cryptosporidium in a clinical trial context - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10490871/]
- 54. Sensitivity, specificity and comparison of three commercially available immunological tests in the diagnosis of Cryptosporidium species in animals - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1517838216309868]
- 55. (PDF) Analytical of staining and molecular techniques for... sensitivity [https://www.academia.edu/74976388/Analytical_sensitivity_of_staining_and_molecular_techniques_for_the_detection_of_Cryptosporidium_spp_oocysts_isolated_from_bovines_in_water_samples_a_preliminary_study]
- 56. The transformation of a Cryptosporidium reference microbiology service to tackle the One Health challenge - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272628/]
- 57. in qPCR, dPCR and MPS—mechanisms and solutions... PCR inhibition [https://pmc.ncbi.nlm.nih.gov/articles/PMC7072044/]
- 58. Comprehensive review of conventional and state-of-the-art detection methods of Cryptosporidium - PubMed [https://pubmed.ncbi.nlm.nih.gov/34325293/]
- 59. What Are PCR ? - LubioScience Inhibitors [https://www.lubio.ch/blog/what-are-pcr-inhibitors]
- 60. for Overcoming Strategies in... - Amerigo Scientific PCR Inhibition [https://www.amerigoscientific.com/resource-strategies-for-overcoming-pcr-inhibition-in-diagnostic-analysis.html]
- 61. PCR Troubleshooting: Common Problems and Solutions | MyBioSource Learning Center [https://www.mybiosource.com/learn/pcr-troubleshooting-common-problems-and-solutions/]
- 62. An improved stool concentration procedure for the detection of... [https://pubmed.ncbi.nlm.nih.gov/25193442/]
- 63. Centrifugation - Wikipedia [https://en.wikipedia.org/wiki/Centrifugation]
- 64. Centrifugation; An Overview of Centrifuge Structure, Principle, Types and Techniques [https://www.biotechreality.com/2023/11/centrifugation-an-overview-of-centrifuge-structure-principle-types-and-techniques.html]
- 65. Frontiers | Methods used for concentrating oocysts of Cryptosporidium spp., spores Encephalitozoon spp. and Enterocytozoon spp. and their occurrence in Slovak water samples [https://www.frontiersin.org/journals/environmental-science/articles/10.3389/fenvs.2023.1161465/full]
- 66. Comparison of current methods used to detect Cryptosporidium oocysts in stools - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1438463917304698]
- 67. Quantification of In Vitro and In Vivo Cryptosporidium parvum Infection by Using Real-Time PCR - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1489663/]
- 68. Centrifugal precipitation chromatography - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2817994/]
- 69. Calculate Discrepancy : A Step-by-Step Guide [https://sourcetable.com/calculate/how-to-calculate-discrepancy]
- 70. Resolve Research Discrepancies with These Tips [https://www.linkedin.com/advice/0/youre-facing-conflicting-data-sources-your-research-how-3qsqf]
- 71. Simplex and Multiplex Commercial for the Detection of... PCR Assays [https://www.bohrium.com/paper-details/commercial-simplex-and-multiplex-pcr-assays-for-the-detection-of-intestinal-parasites-giardia-intestinalis-entamoeba-spp-and-cryptosporidium-spp-comparative-evaluation-of-seven-commercial-pcr-kits-with-routine-in-house-simplex-pcr-assays/813266484615708672-7956]
- 72. analysis of Comparative and “ commercial - In †molecular tests... House [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 73. PCR Assay Optimization and Validation [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/pcr/assay-optimization-and-validation]
- 74. & Solutions | Boster Bio PCR Troubleshooting Guide [https://www.bosterbio.com/protocol-and-troubleshooting/pcr-troubleshooting]
- 75. Optimization of Real-Time PCR Assay for Rapid and Sensitive Detection of Eubacterial 16S Ribosomal DNA in Platelet Concentrates - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC254335/]
- 76. An optimized protocol for stepwise optimization of real-time RT-PCR analysis | Horticulture Research [https://www.nature.com/articles/s41438-021-00616-w]
- 77. Investigation of the Frequency of Cryptosporidium spp. in... [https://turkiyeparazitolderg.org/articles/investigation-of-the-frequency-of-lessemgreatercryptosporidiumlessemgreater-spp-in-immunosuppressed-patients-with-diarrhea/doi/tpd.galenos.2025.88700]
- 78. Avoiding commercial kit-based DNA isolation and purification steps... [https://pubs.rsc.org/en/content/articlelanding/2025/sd/d4sd00344f]
- 79. Performance of 30 protocol combinations for the detection of Cryptosporidium parvum in stool samples - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1684118225000064]
- 80. Development of novel methodology for the molecular differentiation of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7724200/]
- 81. Giardia and Cryptosporidium spp. dissemination during wastewater treatment and comparative detection via immunofluorescence assay (IFA), nested polymerase chain reaction (nested PCR) and loop mediated isothermal amplification (LAMP) - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0001706X16300584]
- 82. Performance evaluation of point-of-care test for detection of... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/1756-3305-7-227]
- 83. Portable on-chip colorimetric biosensing platform integrated with... [https://www.nature.com/articles/s41598-021-02580-w?error=cookies_not_supported&code=17eee064-2070-4faf-8c89-4c8cc51c7ad8]
- 84. Enhancing diagnostic accuracy: Direct immunofluorescence assay as... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11445881/]
- 85. Investigation of the Frequency of Cryptosporidium spp. in... [https://pubmed.ncbi.nlm.nih.gov/40340275/]
- 86. Investigation of the Frequency of Cryptosporidium spp. in... [https://turkiyeparazitolderg.org/articles/investigation-of-the-frequency-of-lessemgreatercryptosporidiumlessemgreater-spp-in-immunosuppressed-patients-with-diarrhea/tpd.galenos.2025.88700]
- 87. The development and performance of a simple, sensitive method for the detection of Cryptosporidium oocysts in faeces | Epidemiology & Infection | Cambridge Core [https://www.cambridge.org/core/journals/epidemiology-and-infection/article/development-and-performance-of-a-simple-sensitive-method-for-the-detection-of-cryptosporidium-oocysts-in-faeces/92574AE5633AE9CBF4F2DFC607F47F0D]
- 88. Performance of diagnostic assays used to detect ... [https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-022-03435-w]
- 89. Comparison of Three Real-Time PCR Assays Targeting the ... [https://www.mdpi.com/2076-0817/10/9/1131]
- 90. Comparison of diagnostic techniques for the detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4406248/]
- 91. Comparison of diagnostic techniques for the detection ... [https://www.sciencedirect.com/science/article/pii/S0014489415000296?via%3Dihub#!]
- 92. Comparison of four diagnostic techniques for Cryptosporidium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371275/]
- 93. enhanced detection uncovers Cryptosporidium endemicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291217/]