Advanced FEA Methods for Modeling Difficult Stool Consistencies in Biomechanical Research
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for applying Finite Element Analysis (FEA) to model complex stool consistencies and their interaction with biological systems.
Advanced FEA Methods for Modeling Difficult Stool Consistencies in Biomechanical Research
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for applying Finite Element Analysis (FEA) to model complex stool consistencies and their interaction with biological systems. It covers foundational biomechanics, advanced methodological protocols for model creation, troubleshooting for convergence and accuracy, and rigorous validation techniques. By synthesizing current research and best practices, this guide aims to enhance the predictive power of computational models in gastrointestinal drug development, pelvic floor rehabilitation, and the design of medical devices for bowel management.
Understanding Stool Biomechanics and the Role of FEA
Stool consistency is a critical parameter in gastrointestinal research, serving as a key indicator of digestive health, intestinal transit time, and the effectiveness of therapeutic interventions. For researchers and drug development professionals, accurately defining and measuring this property is essential for studies on functional bowel disorders, novel drug formulations, and advanced biomechanical modeling. The assessment landscape spans from simple visual classification tools to sophisticated quantitative rheological methods, each with distinct applications in experimental and clinical settings. This technical support center provides targeted guidance on navigating these methodologies, with particular emphasis on their application in Finite Element Analysis (FEA) research involving difficult stool consistencies.
Core Classification System: The Bristol Stool Form Scale
The Bristol Stool Form Scale (BSFS) is a diagnostic medical tool developed in 1997 by Dr. Kenneth Heaton at the Bristol Royal Infirmary to classify human feces into seven distinct categories based on their physical appearance [1] [2]. This scale serves as a validated visual assessment method that correlates with intestinal transit time and has become the standard classification system in both clinical practice and research environments [1] [3]. Researchers and clinicians utilize the BSFS as a non-invasive, rapid assessment tool for evaluating bowel function, diagnosing conditions such as irritable bowel syndrome (IBS) and constipation, and monitoring treatment outcomes in pharmaceutical development [1] [2].
The BSFS categorizes stools from Type 1 (separate hard lumps) to Type 7 (watery, no solid pieces), with Types 3 and 4 generally considered ideal as they indicate normal transit time and are easy to pass without straining [1] [4]. Types 1 and 2 indicate constipation (slow transit), while Types 5-7 suggest diarrhea or rapid intestinal transit [3] [4]. The scale provides researchers with a common vocabulary for characterizing stool consistency across studies and has been validated in multiple languages, including Spanish, Brazilian Portuguese, and Polish, enhancing its utility in international research collaborations [2].
Technical Limitations in Research Applications
Despite its widespread adoption, the BSFS presents significant limitations for precise scientific research, particularly in studies requiring quantitative measurements for FEA modeling. The primary constraint is its subjective nature, which introduces inter-rater and intra-rater variability that can compromise data reliability [5]. One study demonstrated that the correlation between BSFS scores and objectively measured stool consistency was significantly stronger when scores were assigned by experts (rrm = -0.789) compared to subject self-assessment (rrm = -0.587), highlighting the potential for subjective bias [5].
Additionally, the BSFS exhibits limited granularity, as it categorizes stools into only seven broad types despite the continuous spectrum of stool consistency found in biological systems [5]. This lack of resolution becomes particularly problematic when researching "difficult consistencies" - extremely hard (Type 1) or watery (Type 7) stools that present challenges for both patients and experimental protocols. Furthermore, the scale provides no direct quantitative data on mechanical properties essential for FEA, such as compressive yield stress, viscosity, or solids diffusivity [5] [6]. These limitations have driven the development of complementary quantitative measurement technologies that can provide the precise, continuous data required for advanced computational modeling.
Quantitative Measurement Techniques
Texture Analysis for Direct Mechanical Measurement
Texture analyzers represent a significant advancement in objective stool consistency measurement, providing direct mechanical quantification that surpasses the limitations of visual scales. These instruments measure the force required to deform a stool sample under controlled conditions, generating continuous numerical data suitable for statistical analysis and modeling applications [5].
Table 1: Texture Analysis Protocol for Stool Consistency Measurement
| Parameter | Specification | Application Notes |
|---|---|---|
| Instrument | TA.XTExpress Texture Analyser (Stable Micro Systems Ltd.) | Compatible with various penetrometer probes |
| Probe Type | Cylindrical (ø 6 mm) | Optimal for minimal sample disturbance |
| Probe Speed | 2.0 mm/s | Controlled penetration rate |
| Penetration Depth | 5 mm | Standardized measurement depth |
| Measured Value | Gram-force required for penetration | Direct indicator of mechanical resistance |
| Sample Storage | Refrigeration at 4°C if not measured immediately | Preserves original consistency properties |
| Measurement Environment | Room temperature (20-25°C) | Standardized testing conditions |
The protocol developed for the TA.XTExpress Texture Analyser demonstrates a strong negative correlation with stool water content (rrm = -0.781), validating its accuracy as a direct measurement tool [5]. This method can detect consistency variations across the entire clinical range, from hard constipated stools to watery diarrhea, with sensitivity superior to visual assessment alone. The log-transformed stool consistency values obtained from this method show normal distribution, making them suitable for parametric statistical analysis in research settings [5].
Rheological Characterization for FEA Modeling
Rheological measurements provide essential parameters for FEA simulations of stool movement through the digestive system and during defecation. These techniques characterize the flow and deformation behavior of stool under various stress conditions, generating data critical for accurate biomechanical modeling [6].
Research on the compressional rheology of fresh feces has identified key parameters that influence dewatering behavior and mechanical properties. The gel point (φg), which represents the solids concentration where the material develops a networked structure, ranges between 6.3 and 15.6% total solids (TS) concentration for fresh feces [6]. This is significantly higher than the gel point observed for wastewater sludge, indicating that passive gravity-driven processes can effectively thicken fresh fecal material - a finding with implications for both sanitation technology and understanding physiological water absorption in the colon.
Table 2: Key Rheological Parameters of Fresh Feces for FEA Modeling
| Parameter | Value Range | Significance for FEA |
|---|---|---|
| Gel Point (φg) | 6.3-15.6% TS | Defines transition from fluid-like to solid-like mechanical behavior |
| Passive Sedimentation Rate | 3 to 10% TS in <0.5 h | Important for modeling liquid separation processes |
| Filtration Characterization | Lengthy cake filtration times with short compression times | Informs on dewatering kinetics and resistance to flow |
| Effect of Conductivity | Increased conductivity hinders dewatering rate | Models impact of ionic composition on mechanical properties |
| Compressive Yield Stress | Varies with solids concentration | Critical parameter for deformation modeling under load |
The compressional rheology of fresh feces exhibits more favorable dewatering characteristics compared to wastewater sludge, supporting higher final cake solids concentrations and improved dewatering kinetics [6]. These rheological properties are significantly influenced by environmental factors, particularly conductivity, which decreases dewaterability - an effect mitigated by implementing solid-liquid separation earlier in the process [6].
Troubleshooting Guides for Difficult Stool Consistencies
Handling Extremely Hard Stools (BSFS Types 1-2)
Problem: Sample Fragmentation and Non-representative Sampling Hard, lumpy stools (BSFS Types 1-2) present challenges for homogeneous sampling and mechanical testing due to their heterogeneous composition and structural integrity.
Solution:
- Pre-hydration Protocol: For texture analysis, carefully apply a standardized mist of physiological saline (0.9% NaCl) to the sample surface and allow equilibrium for 10 minutes before testing to create a more uniform surface without altering bulk properties.
- Multiple Point Measurement: Implement a grid-based measurement approach with a minimum of 5 penetration tests at different locations on the sample surface. Record the mean and coefficient of variation - a CV >25% indicates significant heterogeneity that must be accounted for in data interpretation.
- Cryogenic Grinding: For compositional analysis, flash-freeze samples in liquid nitrogen and use a cryogenic mill to create homogeneous powder while preserving molecular integrity. This enables representative sub-sampling for parallel analyses.
- Centrifugal Partitioning: For chemical extraction, use accelerated solvent extraction systems with increased pressure and temperature cycles to improve extraction efficiency from the dense, low-hydration matrix.
Managing Watery Stools (BSFS Types 6-7)
Problem: Liquid-phase Separation and Analyte Dilution Watery stools lack sufficient structural integrity for standard mechanical testing and undergo rapid phase separation, compromising sample representativeness.
Solution:
- Rapid Preservation: Immediately add preservation buffers (e.g., RNAlater for molecular analysis or formaldehyde-based fixatives for microscopic examination) upon sample collection to maintain analyte distribution.
- Vacuum Filtration Concentration: Use graded filtration systems with sequential membrane pores (20μm, 5μm, 0.8μm) to concentrate solid components while preserving the fractionated materials for separate analysis.
- Inline Turbidity Monitoring: Implement real-time turbidity sensors, as demonstrated in automated stool sampling systems, to characterize liquid stools without physical manipulation [7]. Calibrate turbidity readings against total solids concentration for quantitative assessment.
- Centrifugal Concentration: Standardize centrifugation protocols (e.g., 10,000 × g for 15 minutes at 4°C) to pellet solid components while retaining the aqueous phase for parallel analysis of soluble markers.
Addressing Subjectivity in Visual Classification
Problem: Inter-rater Variability in BSFS Scoring Subjective classification introduces significant variability, particularly in multi-center trials where consistent categorization is essential for reliable data.
Solution:
- Digital Image Analysis: Implement standardized imaging protocols with color calibration cards and scale references. Use machine learning algorithms trained on expert-classified images to reduce classification variance.
- Expert Consensus Training: Before study initiation, conduct calibration sessions using standardized image libraries until all raters achieve >90% agreement with expert consensus scores.
- Multi-parameter Assessment: Supplement BSFS classification with simple objective measures such as sample spread diameter on a standardized surface and water content via rapid moisture analysis to validate visual classifications.
Frequently Asked Questions
Q1: How can we minimize contamination and cross-over between sequential stool samples in automated collection systems?
A1: Automated systems should incorporate zero dead-leg valves and clean-in-place procedures demonstrated to reduce bacterial carryover between samples by 1-3 log reductions [7]. System design should minimize stagnant volumes and include rinse cycles between samples. For high-sensitivity molecular applications, implement PCR inhibition testing to detect potential cross-contamination.
Q2: What is the optimal preservation method for stool samples intended for both microbiological and rheological analysis?
A2: Rheological properties are best measured on fresh samples within 30 minutes of collection. When parallel analyses are required, partition the sample immediately: allocate portion for texture analysis (test immediately), preserve portion in RNAlater for molecular work (4°C overnight then -80°C), and freeze a portion at -80°C for compositional analysis. Note that preservation methods inevitably alter mechanical properties.
Q3: How does stool water content correlate with objectively measured consistency values?
A3: Texture analyzer measurements show a strong negative linear correlation with stool water content (rrm = -0.781) [5]. However, this relationship is not perfectly linear across the entire consistency range, as water-holding capacity of insoluble solids and microbial composition also influence mechanical properties.
Q4: What factors contribute to the variability in rheological properties between samples?
A4: Key factors include: (1) total solids concentration, (2) dietary fiber composition and particle size, (3) microbial biomass and composition, (4) electrolyte concentration, and (5) mucosal content. Studies show that increased conductivity significantly hinders dewatering rate, suggesting ionic composition markedly influences stool rheology [6].
Q5: How can we improve patient adherence to stool sampling protocols in clinical trials?
A5: Studies indicate that disgust and embarrassment are major barriers to adherence [7]. Implementation of hands-free sampling systems that integrate with standard toilet hardware significantly improves acceptability [7]. Additionally, clear communication about the clinical value of the research and privacy protections enhances participant cooperation.
Experimental Protocols
Protocol 1: Direct Consistency Measurement via Texture Analysis
Objective: To quantitatively measure stool consistency using a texture analyzer, generating numerical values for research applications and validation of subjective scales.
Materials:
- TA.XTExpress Texture Analyser (Stable Micro Systems Ltd.) or equivalent
- Cylindrical probe (6 mm diameter)
- Standardized sample containers (60 mm diameter)
- Precision balance (±0.01 g)
- Physiological saline (0.9% NaCl)
- Disposable spatulas and forceps
Procedure:
- Collect stool sample in a clean, dry container. Process within 30 minutes of passage.
- Weigh sample container and record tare weight. Transfer approximately 50g of stool to container, avoiding selective sampling of heterogeneous specimens.
- Level the sample surface gently with a spatula without compression, creating a uniform testing surface.
- Mount cylindrical probe to texture analyzer and calibrate according to manufacturer specifications.
- Program analyzer with these parameters: pre-test speed 1.0 mm/s, test speed 2.0 mm/s, post-test speed 10.0 mm/s, penetration distance 5 mm, trigger force 5g.
- Position sample under probe and initiate test cycle.
- Record maximum force (g) required to achieve 5 mm penetration.
- Repeat measurement at 3 additional locations on sample surface if sufficient material exists.
- Calculate mean consistency value and coefficient of variation.
- Clean probe thoroughly with laboratory detergent and 70% ethanol between samples.
Validation: The log-transformed values should demonstrate a strong negative correlation with expert BSFS scores (expected rrm ≈ -0.789) and water content [5].
Protocol 2: Rheological Characterization for FEA Parameters
Objective: To determine key rheological parameters of stool samples for finite element analysis modeling.
Materials:
- Rheometer with parallel plate geometry (40 mm diameter)
- Temperature control unit
- Moisture analysis balance
- Centrifuge with swing-bucket rotor
- Precision sieves (500 μm, 250 μm)
Procedure:
- Prepare sample by homogenizing gently and passing through a 500 μm sieve to remove large particulate matter while preserving matrix structure.
- Determine initial solids content by drying 2g aliquot at 105°C for 24 hours.
- Load approximately 3mL of sample between rheometer plates, setting gap to 2 mm.
- Perform amplitude sweep test (0.1-100% strain, 1 Hz) to determine linear viscoelastic region.
- Conduct frequency sweep test (0.1-10 Hz) within linear region to characterize mechanical spectrum.
- Perform flow curve measurement (0.1-100 s⁻¹ shear rate) to model viscosity function.
- For compression testing, use a separate aliquot in a confined cell to determine compressive yield stress as a function of solids concentration.
- Fit data to appropriate rheological models (Herschel-Bulkley for flow curves, power law for viscoelastic properties).
Data Analysis: Calculate gel point (solids concentration where G' > G''), yield stress, flow behavior index, and consistency coefficient for incorporation into FEA simulations.
Research Reagent Solutions
Table 3: Essential Materials for Stool Consistency Research
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| TA.XTExpress Texture Analyser | Direct mechanical measurement of stool consistency | Provides quantitative consistency values in gram-force; validated against BSFS [5] |
| Parallel Plate Rheometer | Characterization of viscoelastic properties | Essential for obtaining FEA parameters such as viscosity and yield stress |
| RNAlater Stabilization Solution | Preservation of nucleic acids for parallel molecular analysis | Enables correlation of microbiome data with mechanical properties |
| Physiological Saline (0.9% NaCl) | Sample hydration control | Standardizes surface conditions for texture analysis without altering bulk properties |
| Graded Filtration Membranes | Size-fractionation of stool components | Separates particulate matter for individualized analysis of different fractions |
| Zero Dead-Leg Valves | Prevention of cross-contamination in automated systems | Critical for maintaining sample integrity in sequential sampling [7] |
| Turbidity Sensors | Real-time assessment of liquid stools | Enables characterization of watery samples without physical manipulation [7] |
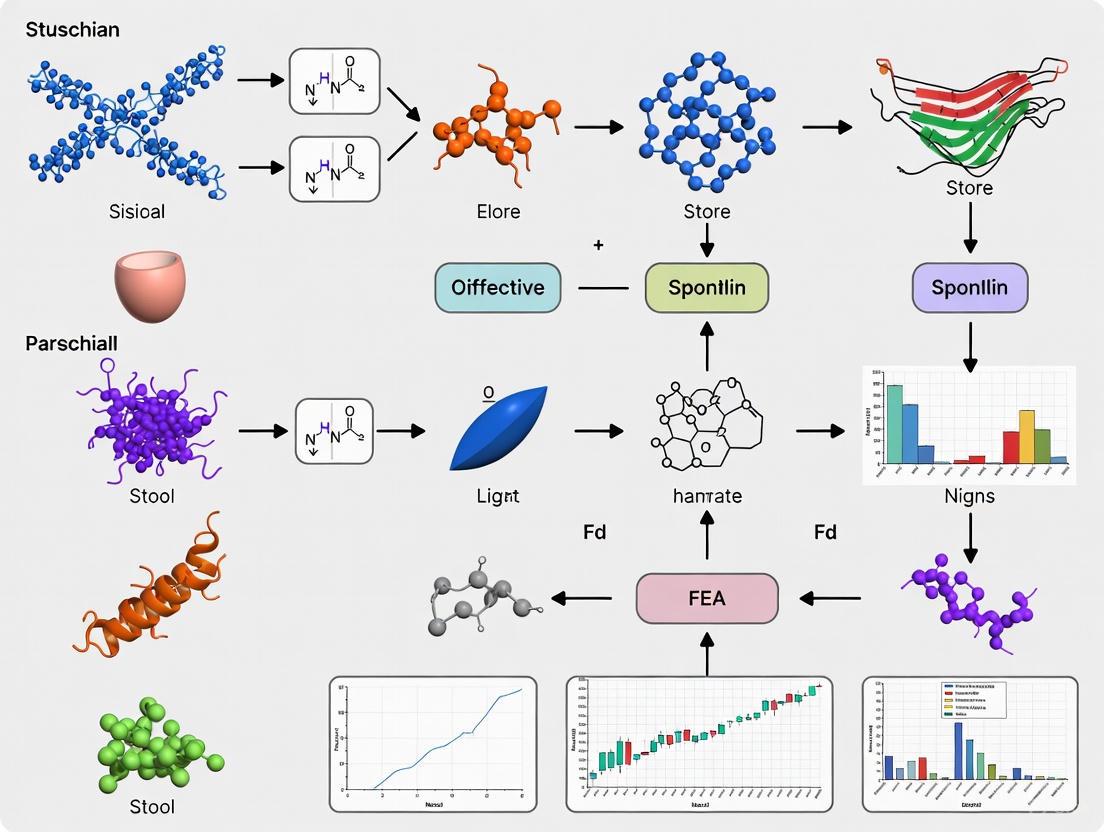
Workflow Visualization
The comprehensive assessment of stool consistency requires integration of both qualitative classification and quantitative measurement approaches. While the Bristol Stool Form Scale provides a rapid, clinically validated assessment tool, advanced research—particularly FEA modeling of difficult stool consistencies—demands the precise, continuous data provided by texture analysis and rheological characterization. The methodologies and troubleshooting guides presented here enable researchers to navigate the challenges associated with heterogeneous biological materials, generating reliable data for computational modeling and therapeutic development. As research in this field advances, the integration of automated sampling technologies with multi-parameter assessment will further enhance our understanding of stool biomechanics and its implications for gastrointestinal health and disease.
Frequently Asked Questions (FAQs)
Q1: What are the key biomechanical properties to measure when studying stool consistency? The three core properties are hardness, viscosity, and flow dynamics. Hardness refers to the material's resistance to deformation, viscosity describes its resistance to flow, and flow dynamics encompass how the material moves and behaves during defecation. Quantitative measurements of these properties are crucial for creating accurate computer models, such as those used in Finite Element Analysis (FEA), to simulate defecation and understand related disorders [8] [5] [9].
Q2: How does stool consistency directly impact defecatory function? Stool consistency significantly alters the biomechanics of defecation. Harder stools require greater expulsion pressure and a longer duration to evacuate. Research using simulated feces of different consistencies found that a harder probe required a maximum bag pressure of 140 cmH₂O and 18 seconds for evacuation, compared to 107 cmH₂O and 9 seconds for a softer probe [8]. This increased mechanical demand can contribute to symptoms like straining, which is associated with stools that are 1.88-fold harder [5].
Q3: What is the relationship between the Bristol Stool Form Scale (BSFS) and direct mechanical measurements? While the BSFS is a widely used visual classification tool, direct mechanical measurements provide more objective and quantitative data. Studies show a strong correlation between BSFS scores and directly measured stool consistency, though with considerable variance, especially for normal stool forms (BSFS 3-5) [5]. Technician-scored BSFS also tends to be more accurate than self-reported scores [10]. Therefore, for precise FEA research, direct mechanical measurement is recommended to supplement BSFS classification.
Q4: What experimental methods are available for direct measurement of stool consistency? The primary method is mechanical analysis using a texture analyzer (e.g., TA.XTExpress). In a standard protocol, a cylindrical probe is pushed into the stool surface at a defined speed (e.g., 2.0 mm/s) to a set depth (e.g., 5 mm), and the resistance force (in gram-force) is recorded [5]. Other technologies include penetrometers and viscometers [5], as well as novel devices like "Fecobionics"—a simulated feces probe that measures pressure and bending angles during evacuation [8].
Troubleshooting Guides
Guide 1: Resolving Material Model Instabilities in FEA of Stool Mechanics
Problem: Your Finite Element Analysis (FEA) simulation of stool deformation is failing to converge or producing unrealistic results.
Solution: This often stems from an improperly defined material model. Stool is a complex, non-linear biological material.
- Step 1: Select an Appropriate Constitutive Model. Avoid overly simple linear elastic models. For soft stools (BSFS 5-7), consider a hyperelastic model like Neo-Hookean or Ogden that can handle large deformations. For harder stools (BSFS 1-2), a plastic or viscoelastic model may be more appropriate to capture permanent deformation and time-dependent behavior [9].
- Step 2: Calibrate Model Parameters with Experimental Data. Use data from texture analysis or rheological studies to inform your model's parameters. For example, the log-transformed consistency values for human stools typically range from ~1.4 ln(gf) for soft stools to ~5.0 ln(gf) for hard stools [5].
- Step 3: Check Element Formulation and Mesh. Use elements suitable for large strain and incompressible material behavior (e.g., C3D8H in Abaqus). Refine the mesh in areas of high stress concentration [11].
Guide 2: Addressing High Variance in Stool Consistency Measurements
Problem: Measurements of stool consistency from your samples show high variability, making it difficult to establish clear trends.
Solution: Implement standardized protocols for sample handling and measurement.
- Step 1: Standardize Sample Preparation. Stool samples should be measured shortly after defecation (within a few hours) and should be analyzed at a consistent temperature to prevent changes in water content and rheology [5].
- Step 2: Perform Multiple Measurements. Do not rely on a single measurement per sample. Take multiple readings from different lumps throughout the length of a specimen and use the median value to account for internal heterogeneity [5].
- Step 3: Control for Subject Factors. Document and account for factors known to affect consistency, such as straining during evacuation (which is linked to harder stools) and time of day (morning stools may be softer) [5]. Using technician-scored BSFS instead of self-reported scores can also reduce variance [10].
Quantitative Data Tables
Table 1: Stool Consistency Measurements by Bristol Stool Form Scale (BSFS)
This table summarizes quantitative stiffness data measured directly from stool samples using a texture analyzer, correlated with BSFS types [5].
| BSFS Type | Description | Log-Transformed Consistency (ln g/probe), Mean ± SD | Number of Samples |
|---|---|---|---|
| 1 or 2 | Hard Stool | 4.956 ± 0.593 | 21 |
| 3, 4, or 5 | Normal Stool | 3.176 ± 0.877 | 217 |
| 6 or 7 | Soft Stool | 1.394 ± 0.562 | 14 |
Table 2: Defecation Parameters for Simulated Feces of Different Consistencies
This table shows key biomechanical parameters measured during the evacuation of simulated feces ("Fecobionics" probes) of different stiffness [8].
| Probe Hardness (Shore) | Approx. BSFS | Defecation Duration (seconds) | Maximum Bag Pressure (cmH₂O) |
|---|---|---|---|
| 0A | Type 2-4 | 9 (8-12) | 107 (96-116) |
| 10A | Type 2-4 | 18 (12-21) | 140 (117-162) |
| 40A | Harder than normal | Not Significantly Different from 10A | Not Significantly Different from 10A |
Note: Data presented as median (quartiles). Significant differences were primarily observed between the 0A and 10A probes.
Experimental Protocols
Protocol 1: Direct Measurement of Stool Consistency using a Texture Analyzer
Objective: To obtain a quantitative, mechanical measure of stool hardness.
Materials:
- Texture Analyzer (e.g., TA.XTExpress, Stable Micro Systems Ltd.)
- Cylindrical probe (e.g., 6 mm diameter)
- Fresh stool sample
- Sample container
Methodology:
- Sample Preparation: Transfer the fresh stool sample to a standardized container. Ensure the surface is relatively level.
- Instrument Setup: Configure the texture analyzer with the cylindrical probe. Set the test speed to 2.0 mm/s and the target penetration depth to 5 mm.
- Measurement: Position the probe above the sample surface and initiate the test. The probe will descend and penetrate the stool.
- Data Recording: The instrument records the force (in gram-force) required to achieve the 5 mm depth. This value is the primary measure of consistency.
- Replication: Repeat the measurement at several different locations on the same stool sample to account for heterogeneity. Calculate the median consistency value for the sample [5].
- Data Transformation: For statistical normalization, use the natural log-transformed value (ln g/probe) for analysis [5].
Protocol 2: Evaluating Defecatory Function using Simulated Feces (Fecobionics)
Objective: To assess anorectal function and flow dynamics during a simulated defecation event.
Materials:
- Fecobionics device (a probe with pressure sensors and motion sensors)
- Lubricant
Methodology:
- Preparation: Select a Fecobionics probe of desired consistency (e.g., 0A, 10A, 40A shore hardness). Lightly lubricate the probe.
- Insertion: Insert the probe into the rectum of the study participant.
- Distension: After a brief rest, slowly fill the device's internal bag with water or air until the participant reports a definite urge to defecate. Record this volume (urge volume).
- Evacuation: The investigators then leave the room, and the participant evacuates the device in privacy, mimicking a natural defecation.
- Data Acquisition: The device records multiple parameters in real-time, including pressures at the front, rear, and inside the bag, as well as the bending angle (anorectal angle) during evacuation [8].
- Analysis: Key outcome measures include defecation duration, maximum pressures generated, and the rectoanal pressure gradient (RAPG).
Research Reagent Solutions
Table 3: Essential Materials for Stool Biomechanics Research
| Item | Function/Brief Explanation |
|---|---|
| Texture Analyzer (TA.XTExpress) | Provides direct, quantitative measurement of stool consistency (hardness) by measuring the force required to deform a sample [5]. |
| Fecobionics Probe | An electronic, simulated feces device that integrates pressure sensors and motion sensors to measure anorectal function and flow dynamics during a physiologically realistic evacuation [8]. |
| Bristol Stool Form Scale (BSFS) | A standardized visual tool for the initial classification of stool form into one of seven types. It is a common reference in both clinical and research settings [12] [5] [10]. |
| Silicone Resins (Varying Hardness) | Used to fabricate Fecobionics probes or other simulated stools with standardized, reproducible mechanical properties (e.g., 0A, 10A, 40A shore hardness) for controlled experiments [8]. |
Workflow and Relationship Diagrams
Diagram 1: Stool Biomechanics Research Workflow
Diagram 2: Key Property Interrelationships
Technical Support Center
Troubleshooting Finite Element Analysis in Pelvic Floor Research
This section addresses common computational challenges encountered when developing finite element models for investigating bowel dysfunction.
Table 1: Common FEA Errors and Solutions
| Error / Warning Message | Potential Root Cause | Solution / Diagnostic Action |
|---|---|---|
| Model fails to converge to a solution [11] | Insufficiently constrained model (rigid body modes), contact issues, or inappropriate material model [11]. | Check constraints to ensure all rigid body motions are eliminated. Review contact definitions and parameters [11]. |
| "Elements are distorted" or "Negative Jacobian" [11] | Excessive deformation causing poor-quality elements or an unstable material model [11]. | Refine the mesh in areas of high deformation. Run a preliminary analysis with smaller load steps [13]. |
| Inaccurate stress/strain results (e.g., stress exceeds failure threshold without simulated failure) [13] | Use of an overly simplified linear elastic material model that does not account for material failure [13]. | Implement a more advanced material model that includes damage or plasticity [13]. |
| Solver stops with a "Zero pivot" warning [11] | Under-constrained model or poorly defined contact, leading to numerical instability [11]. | Check for and eliminate any potential rigid body motions. Review contact pairs for initial overclosures or gaps [11]. |
| Solution is strongly mesh-dependent | The mesh is too coarse to capture the necessary physics, such as stress concentrations. | Perform a mesh sensitivity study to ensure results do not change significantly with further mesh refinement [13]. |
| Model validation fails (simulation does not match dynamic MRI data) [14] [15] | Incorrect boundary conditions, material properties, or anatomical inaccuracies in the 3D model [14]. | Re-check the assignment of all boundary conditions and material properties. Verify the geometric accuracy of the model against medical images [14] [15]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between the Finite Element Method (FEM) and Finite Element Analysis (FEA)? [16] A: The Finite Element Method (FEM) is the mathematical technique used to break down complex systems into smaller, simpler elements and solve the underlying differential equations. Finite Element Analysis (FEA) is the broader process of applying this method to predict an object's behavior and interpret the results. [16]
Q2: How can I validate that my pelvic floor model is biomechanically accurate? [14] [15] A: Model validity can be verified by comparing simulation outputs to actual physiological data. One effective method is to simulate maneuvers like the Valsalva and compare the resulting changes in anatomical angles (e.g., Anorectal Angulation - ARA) and organ displacements against those observed in dynamic MRI scans from the same subject. Geometric deviations should ideally be controlled within 10%. [14] [15]
Q3: My model involves complex interactions between muscles and organs. What type of analysis should I use? A: For simulating physiological processes like bowel movement or Valsalva, which involve large deformations and changing contacts, a dynamic analysis is typically required as it accounts for variation over time. [16] For simulating the effect of sustained muscle tonus, a static analysis might be appropriate. [16]
Q4: Can FEA simulate the effects of different rehabilitation treatments? [15] A: Yes. The effects of physical rehabilitation methods (e.g., exercise, electrical stimulation) can be simulated by proportionally altering the material properties of the targeted muscles in the model. For example, increasing the elastic modulus of a muscle simulates increased strength and stiffness gained through training, allowing researchers to quantify the impact on functional angles like the Retrovesical Angle (RVA) and ARA. [15]
Q5: What are the critical limitations of FEA that I must consider? [16] A: The accuracy of FEA results is entirely dependent on the quality of the inputs—a principle often called "garbage in, garbage out." The model's predictions are only as good as the accuracy of the geometry, material properties, boundary conditions, and loading applied. The results should always be reviewed with a critical, domain-knowledge perspective to assess their physical plausibility. [16] [13]
Experimental Protocols & Methodologies
Detailed Protocol: Developing a Subject-Specific Pelvic Floor Finite Element Model [14]
Medical Image Acquisition:
- Participants: Recruit eligible volunteers (e.g., >60 years) with normal pelvic floor function and no dysfunction. Informed consent and ethical approval are mandatory. [14]
- Scanning: Collect both Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) data. CT provides high-resolution bone geometry, while MRI optimally differentiates soft tissues (muscles, fascia, organs). [14]
- Dynamic Sequences: Perform dynamic MRI capturing specific physiological maneuvers (e.g., Kegel, Valsalva) to provide data for subsequent model validation. [14]
3D Geometric Model Reconstruction:
- Data Import: Import DICOM images from CT and MRI scans into medical image processing software (e.g., Mimics). [14]
- Segmentation: Manually outline and threshold the relevant anatomical structures in each cross-sectional image. This includes bones, pelvic floor muscles (e.g., levator ani), core muscles (e.g., abdominals, back, hip), and organs (bladder, urethra, rectum). Consensus between experienced radiologists is recommended. [14]
- 3D Generation: Use the software's "calculate 3D" function to create initial rough 3D geometry from the segmented masks. Apply smoothing functions to refine the model edges. [14]
Finite Element Model Preparation:
- Surface Generation: Export the 3D geometry and import it into reverse engineering software (e.g., Geomagic Studio) to generate a solid, watertight 3D model suitable for meshing. [14]
- Meshing: Import the solid model into FEA software (e.g., Abaqus) and discretize it into finite elements (mesh). Refine the mesh in areas of expected high stress or deformation. [13]
- Material Assignment: Define material properties (e.g., linear elastic, hyperelastic) for different tissues based on literature or experimental data. [13]
- Boundary Conditions & Loading: Apply realistic constraints to the model (e.g., fixing the sacrum) and simulate loading conditions (e.g., intra-abdominal pressure during Valsalva). [14]
Table 2: Quantitative Validation Metrics for Pelvic Floor Models [15]
| Metric | Full Name & Description | Typical Validation Threshold |
|---|---|---|
| ARA | Anorectal Angulation: The angle between the longitudinal axis of the anal canal and the posterior rectal wall. A key indicator for fecal control. | Deviation from imaging-based measurements < 10% [15] |
| RVA | Retrovesical Angle: The angle between the base of the bladder and the long axis of the urethra. Used to assess urinary control. | Deviation from imaging-based measurements < 10% [14] |
| Waist Circumference Change | The change in abdominal circumference during a Valsalva maneuver. | Deviation from imaging-based measurements < 10% [15] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Pelvic Floor FEA Research
| Item / Resource | Function / Application in Research |
|---|---|
| Medical Image Processing Software (e.g., Mimics) | Used to create 3D geometric models from DICOM-formatted CT and MRI scans through segmentation and thresholding. [14] |
| Reverse Engineering Software (e.g., Geomagic Studio) | Converts the rough 3D geometry generated from segmentation into a smooth, high-quality surface model suitable for finite element meshing. [14] |
| FEA Software (e.g., Abaqus) | The core simulation environment for meshing the geometry, assigning material properties, applying boundary conditions, solving the finite element equations, and post-processing results. [14] [11] |
| Post-Processing Tool (e.g., ParaView) | An open-source tool for advanced visualization and analysis of simulation results, such as stress distributions and deformation animations. [13] |
| Linear Elastic Material Model | A simple material model defining tissues with a constant Young's modulus and Poisson's ratio. Often a starting point for analysis. [13] |
| Hyperelastic Material Model | A complex material model used for simulating soft tissues (like muscles and organs) that undergo large, reversible deformations. [13] |
| Dynamic Analysis | An analysis type used to simulate physiological events that change over time, such a Valsalva maneuver or muscle contraction. [16] |
Workflow and Relationship Visualizations
Finite Element Analysis Workflow
Linking Stool Consistency to FEA and Treatment
FEA Technical Support Center
Frequently Asked Questions (FAQs)
1. What are the key considerations when modeling biological soft tissues? Biological soft tissues are typically hydrated porous hyperelastic materials. They consist of a complex solid skeleton with fine voids filled with fluid. A key consideration is the mechanical interaction between the solid and fluid phases, which can be analyzed using finite element methods (FEM) based on mixture theory [17].
2. My simulation shows unrealistic stress patterns. What could be wrong? Unrealistic stress patterns often result from incorrect boundary condition definitions. A common mistake is treating tissue boundaries as rigid or freely permeable, whereas in reality, many tissues are surrounded by deformable membranes that control transmembrane flows. Ensure your model's boundary conditions accurately reflect the physiological membrane properties [17].
3. How do I model fluid-structure interaction in biological systems? The Immersed Finite Element Method (IFEM) is effective for fluid-structure interaction problems. In IFEM, a Lagrangian solid mesh moves on top of a background Eulerian fluid mesh, greatly simplifying mesh generation. The continuity between fluid and solid subdomains is enforced via velocity interpolation and force distribution [18].
4. What are common pitfalls in modeling hydrated tissues? A frequent pitfall is neglecting the stress relaxation phenomenon caused by interactions between elastic tissue deformation, pore water pressure gradients, and fluid movement. For large deformations of hydrated porous hyperelastic material, use formulations that account for fluid trapped by impermeable membranes, which can cause tissue swelling [17].
5. How can I validate my FEA model for biological materials? Validation should include compression tests comparing simulated results with experimental data. For hydrated tissues, verify that your simulation shows appropriate stress relaxation behavior and fluid-induced swelling around contact areas when surrounded by impermeable membranes [17].
Troubleshooting Guides
Problem: Convergence issues in hyperelastic material analysis
- Symptoms: Solver fails to converge, excessive distortion errors
- Possible Causes:
- Overly large load increments causing element distortion
- Inappropriate hyperelastic material model parameters
- Insufficient mesh refinement in high-strain regions
- Solutions:
- Reduce load increments and use automatic stabilization
- Validate material parameters with experimental data
- Implement adaptive meshing in critical regions [18]
Problem: Inaccurate pore pressure distribution in hydrated tissues
- Symptoms: Unrealistic fluid flow patterns, incorrect stress relaxation
- Possible Causes:
- Incorrect permeability definitions
- Improper boundary conditions for fluid flow
- Neglecting membrane control of transmembrane flows
- Solutions:
- Implement nonlinear finite element formulation of mixture theory with pore water pressure and solid displacement as nodal unknowns
- Use Neumann boundary conditions to control fluid flow rate across membranes [17]
Problem: Fluid-structure interaction instabilities
- Symptoms: Oscillations in solution, solver divergence
- Possible Causes:
- Poorly coupled fluid and solid domains
- Inadequate time step selection
- Insufficient numerical stabilization
- Solutions:
- Apply the Immersed Finite Element Method (IFEM) with RKPM delta function for improved coupling
- Use stabilized equal-order finite element formulation to prevent numerical oscillations
- Implement GMRES iterative algorithm with matrix-free techniques for efficiency [18]
Quantitative Data for FEA of Biological Materials
Table 1: Key Parameters for Modeling Hydrated Biological Tissues
| Parameter | Typical Range | Description | Application Context |
|---|---|---|---|
| Fluid (Pore) Pressure (p) | Variable | Pressure of fluid within tissue voids | Appears in Cauchy stress tensor: σ = -pI + σᴱ [17] |
| Effective Stress (σᴱ) | Material-dependent | Stress induced by solid deformation | Corresponds to classical consolidation theory [17] |
| Solid Displacement (uˢ) | Problem-dependent | Movement of solid skeleton | Primary unknown in nonlinear FEM formulations [17] |
| Fluid Velocity (vᶠ) | Flow-dependent | Movement of fluid phase | Governs transmembrane flow in tissues [17] |
Table 2: Finite Element Formulations for Biological Tissues
| Formulation Type | Nodal Unknowns | Advantages | Limitations |
|---|---|---|---|
| Nonlinear Mixed FEM | Pressure, Solid displacement | Effective for large deformations | May require stabilization [17] |
| Penalty FEM | Solid displacement, Fluid velocity | Handles hyperelastic solid phase | Less accurate for complex flows [17] |
| Three-Field Mixed FEM | Solid displacement, Fluid velocity, Pressure | Improved performance over two-field | Increased computational cost [17] |
| Immersed FEM (IFEM) | Fluid velocity, Solid displacement | Simplified mesh generation | Complex implementation [18] |
Experimental Protocols
Protocol 1: Compression Test of Hydrated Porous Hyperelastic Tissue
Purpose: To characterize mechanical behavior of hydrated biological tissues under compression.
Methodology:
- Sample Preparation: Prepare hydrated tissue sample surrounded by a flaccid impermeable membrane.
- Compression Setup: Position a platen to compress part of the top surface of the tissue.
- Simulation Parameters:
- Use nonlinear finite element formulation with pore water pressure and solid displacement as nodal unknowns
- Apply Neumann boundary conditions to control fluid flow across the membrane
- Model solid phase as hyperelastic material
- Data Collection:
- Monitor stress relaxation over time
- Measure tissue swelling around the platen
- Record pore water pressure gradients [17]
Protocol 2: Fluid-Structure Interaction Analysis using IFEM
Purpose: To simulate interaction between deformable structures and surrounding fluid.
Methodology:
- Domain Setup:
- Create Eulerian fluid mesh spanning entire computational domain
- Generate Lagrangian solid mesh on top of fluid mesh
- Coupling Implementation:
- Use RKPM delta function for velocity interpolation and force distribution
- Apply stabilized equal-order finite element formulation for fluid
- Solution Procedure:
- Employ Newton-Raphson method for nonlinear systems
- Implement GMRES iterative algorithm with matrix-free techniques
- Calculate residuals based on matrix-free techniques [18]
Signaling Pathways and Workflows
Diagram 1: FEA Analysis Workflow for Biological Materials
Diagram 2: Biological Tissue Modeling Approach
Research Reagent Solutions
Table 3: Essential Materials for FEA of Biological Materials
| Research Reagent | Function | Application Context |
|---|---|---|
| Nonlinear FEM Software Platform | Provides computational framework for analysis | Essential for implementing mixed finite element formulations [17] |
| Hyperelastic Material Model Library | Defines stress-strain relationships for biological tissues | Critical for accurate solid phase representation [17] |
| Porous Media Flow Solver | Models fluid flow through tissue voids | Necessary for hydrated tissue analysis [17] |
| Fluid-Structure Interaction Module | Handles coupling between fluid and solid domains | Required for IFEM applications [18] |
| Mesh Generation Tools | Creates Lagrangian and Eulerian meshes | Fundamental for domain discretization [18] |
| RKPM Delta Functions | Enables velocity interpolation and force distribution | Key component for IFEM coupling [18] |
| Stabilized Formulation Algorithms | Prevents numerical oscillations | Important for solutions without excessive numerical dissipation [18] |
Building Robust FEA Models for Stool-Tissue Interaction
Frequently Asked Questions (FAQs)
FAQ 1: What are the key medical imaging modalities for creating anatomical models, and how do they compare?
The primary modalities for creating high-resolution anatomical models are Magnetic Resonance Imaging (MRI) and Computed Tomography (CT). Their data is often integrated with other sources to build comprehensive models [19].
Table 1: Comparison of Key Medical Imaging Modalities for Model Creation
| Modality | Primary Use & Strengths | Key Contributions to Model Creation | Common Clinical Applications in Modeling |
|---|---|---|---|
| MRI | Excellent for visualizing soft tissues, organs, and the central nervous system without ionizing radiation [19]. | Provides high-resolution data on anatomy and physiological processes; essential for digital replication [19]. | Cardiovascular system simulation, brain modeling, soft tissue tumors [19]. |
| CT | Ideal for capturing detailed bony structures and anatomy; provides high-contrast images of dense tissues [20]. | Offers high spatial resolution for precise geometric reconstruction of bones and other structures [19]. | Spinal anomalies, craniofacial reconstructions, skull base tumors [20]. |
| PET | Functional imaging that shows metabolic activity [19]. | Documents physiological processes and can identify abnormalities for dynamic modeling [19]. | Earlier disease detection, monitoring treatment responses in oncology [19]. |
| Ultrasound | Real-time, dynamic imaging [19]. | Provides dynamic data for real-time simulation and monitoring [19]. | Not specified in available literature. |
FAQ 2: My 3D model files are too large and slow to process. What are the common causes and solutions?
Large file sizes and slow processing are frequent bottlenecks. Here are the main causes and strategies to address them:
- Cause: Excessive Spatial Resolution. Using a higher image resolution than necessary for your model's purpose drastically increases data volume and computational load [19].
- Solution: Determine the appropriate voxel size for your research question. For a macro-scale anatomical model, a lower resolution might be sufficient and will significantly reduce computational demands [19].
- Cause: Complex Model Geometry. Anatomical structures with intricate details (e.g., trabecular bone, vascular networks) naturally result in models with high polygon counts [21].
- Solution: Utilize model simplification and reduction techniques. Consider using Reduced-Order Models (ROM) to decrease computational complexity while preserving essential model behavior [19].
- Cause: Software and Hardware Limitations. Standard workstations may lack the necessary memory and processing power [21].
- Solution: Leverage High-Performance Computing (HPC) resources or cloud-based platforms designed for complex simulations. Using a Graphics Processing Unit (GPU) for rendering and computation can also dramatically improve performance [19].
FAQ 3: How do I ensure my 3D anatomical model is accurate and validated?
A robust Verification, Validation, and Uncertainty Quantification (VVUQ) process is critical for ensuring model fidelity [19]. The following workflow, implemented by leading clinical institutions, outlines a rigorous path from scan to validated model:
Key steps in this workflow include:
- Quality Control Checks: Every step, from image processing to final model printing, should have checks to ensure the model accurately represents the source data [20].
- Direct Comparison: The final patient-specific 3D model must be exactly what a surgeon would find in the operating room, validated against the original imaging [20].
- Adherence to Standards: The manufacturing process should follow national standards (e.g., ASTM) to ensure accuracy and safety [20].
FAQ 4: What technical barriers exist when integrating multimodal data (like MRI and CT) into a single model?
Integrating data from multiple sources presents several technical challenges [19]:
- Multimodal Integration Complexity: Fusing data from different imaging modalities (e.g., MRI with CT) and other sources (genomic, wearable sensors) is technically complex due to differing formats, resolutions, and physical meanings [19].
- Data Scarcity and Incompleteness: It is often difficult or impossible to directly measure all physiological parameters needed for a complete model, leading to gaps in data [19].
- Computational Demands: Integrating and running simulations with large, multimodal datasets requires significant computational resources [19].
Solutions involve using AI-driven data augmentation to fill data gaps and real-time model optimization techniques to manage computational load [19]. Machine learning models, particularly foundational models pre-trained on large datasets, can help create robust models even with incomplete data [19].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Medical Image Processing and Model Creation
| Tool Category | Specific Examples / Algorithms | Primary Function |
|---|---|---|
| Machine Learning for Segmentation | Convolutional Neural Network (CNN), Generative Adversarial Network (GAN) [19]. | Automates the identification and outlining of anatomical structures in medical images. |
| Simulation & Modeling | Finite Element Modeling (FEM), Computational Fluid Dynamics (CFD) [19]. | Performs biomechanical and fluid flow simulations on the anatomical model. |
| 3D Modeling & Printing Software | Standard Tessellation Language (STL) files [19]. | Creates and edits virtual 3D models and prepares them for 3D printing. |
| Data Integration & Analysis | Principal Component Analysis (PCA), Graph Neural Network (GNN) [19]. | Analyzes and integrates multimodal data sets for a comprehensive model. |
Advanced Troubleshooting: From Image to Biomechanical Model
The process of creating a biomechanical model, such as for studying stool consistency, relies on a multi-stage pipeline. The diagram below illustrates the logical flow from data acquisition to a functional, validated simulation, highlighting areas where troubleshooting is most critical.
Troubleshooting Key Stages:
Stage: Image Segmentation
- Problem: Automated segmentation fails on soft tissues with low contrast.
- Solution: Utilize advanced ML models like Hypergraph Convolutional Neural Networks (HGCNN) or Generative Adversarial Networks (GANs) which can better handle ambiguous boundaries and learn from complex data relationships [19]. Manually correct segmentation errors before proceeding.
Stage: Mesh Generation
- Problem: The generated mesh is non-manifold or contains too many elements for efficient simulation.
- Solution: Use meshing software that allows for control over element size and type. Implement mesh refinement in areas of high stress or geometric complexity and mesh coarsening in areas of low interest. Validate mesh quality before simulation.
Stage: Material Property Assignment
- Problem: Material properties for biological tissues are unknown or highly variable.
- Solution: This is a key challenge. Conduct a sensitivity analysis to understand how model outputs depend on material parameters. Use inverse analysis techniques, where simulation results are matched to experimental data (if available) to estimate property values.
Frequently Asked Questions (FAQs)
Q1: What are the main categories of mesh simplification algorithms, and how do they differ? Mesh simplification algorithms are primarily divided into two categories:
- Geometry-driven algorithms: These focus solely on the 3D geometry of the model (vertices, edges, faces) to reduce complexity. Common methods include vertex clustering, vertex decimation, and edge folding. They strive for geometric fidelity but often ignore appearance attributes like color and texture, which can lead to suboptimal results for textured models [22].
- Appearance attribute-driven algorithms: These algorithms consider both the geometry and appearance attributes (such as texture, color, and lighting) during the simplification process. An extension of the Quadric Error Metric (QEM) that incorporates appearance attributes falls into this category. They are better at preserving the visual appearance of the simplified model [22].
Q2: During the simplification of a textured 3D model, my results show significant texture distortion and deformation. How can I mitigate this? Texture distortion often occurs when simplification is treated only as a post-processing step without integrating the original 3D reconstruction data. To mitigate this:
- Integrate the Reconstruction Pipeline: Utilize the recovered 3D scene structure and calibrated images from the reconstruction process. Construct a reference 3D model scene and use it to generate a reference image set for texture remapping. This helps maintain texture fidelity after simplification [22].
- Use Advanced Error Metrics: Employ algorithms that include constraints for texture preservation. For instance, one method involves segmenting the surface mesh based on topology and appearance and deriving an error metric that minimizes texture distortion [22]. Another algorithm constrains vertices with sharp features and uses Mahalanobis distance to manage multiple constraints effectively, preserving structural details [23].
Q3: How can I validate the accuracy of a simplified 3D model? The accuracy of a simplified model can be quantitatively and qualitatively assessed using several metrics:
- Geometric Fidelity: Use distances like the Hausdorff distance to measure the maximum geometric deviation between the original and simplified model [23].
- Visual Inspection: Compare rendered images of the original and simplified models from multiple viewpoints [22].
- Performance Metrics: Evaluate the simplification time and the improvement in rendering frame rate after simplification [23].
- Mechanical Validation (for FEA models): Compare simulated outcomes from your finite element model (e.g., internal pressure, organ deformation) with actual physiological data captured via dynamic MRI during maneuvers like Kegel exercises or Valsalva [24] [14].
Q4: My 3D reconstructed models have a complex mesh structure that puts great pressure on real-time rendering. What is an effective simplification strategy? For complex models like buildings, a strategy based on triangle folding can be effective. To compensate for the potential loss of model details, introduce more constraints for error control. Specifically:
- Constrain vertices with obvious sharp features to keep the model's structure from deforming.
- Calculate the Mahalanobis distance of each introduced constraint factor to manage the higher algorithm complexity that comes with multiple constraints. This approach helps preserve detailed features and the model's overall visual effect while significantly reducing the mesh count [23].
Troubleshooting Guides
Problem 1: High Texture Distortion Post-Simplification
| Symptom | Possible Cause | Solution |
|---|---|---|
| Blurred or misaligned textures on the simplified model. | The simplification algorithm is purely geometry-driven and does not account for texture information [22]. | Switch to an appearance attribute-driven simplification algorithm [22]. |
| Stretched or warped texture patterns. | Texture coordinates are not correctly updated after edge collapse or vertex removal operations [22]. | Implement a post-simplification texture coordinate update step that adjusts coordinates based on the new mesh geometry [22]. |
| Consistent texture artifacts across multiple LODs. | The original, high-resolution texture is being used on a very coarse mesh, causing over-sampling. | Implement a texture content simplification method that downsamples the reference image based on the mesh simplification parameters [22]. |
Workflow for Mitigating Texture Distortion: The following diagram illustrates a proposed workflow that integrates 3D reconstruction with simplification to minimize texture issues.
Problem 2: Model Geometry is Poorly Preserved After Simplification
| Symptom | Possible Cause | Solution |
|---|---|---|
| Loss of sharp edges and fine structural details. | The simplification error metric does not adequately penalize the removal of perceptually important features [23]. | Introduce constraints that specifically protect vertices and edges with high curvature or sharp features [23]. |
| The overall shape of the model is deformed. | The simplification algorithm is too aggressive, and the tolerance for geometric error is set too high. | Adjust the simplification parameters to reduce the allowable error threshold for each simplification step. Use a more conservative simplification rate. |
| Irregular surface or "holes" in the mesh. | The simplification process violates the mesh's topological structure. | Use an algorithm that includes topological checks to ensure the manifold property of the mesh is maintained after each operation. |
Problem 3: Long Processing Times for Complex Model Simplification
| Symptom | Possible Cause | Solution |
|---|---|---|
| Simplification of a high-polygon model takes hours. | The algorithm has high computational complexity, often O(n log n) or worse, for models with millions of polygons. | Pre-process the model by segmenting it into regions based on geometric or texture similarity. This allows for more efficient, localized simplification [22]. |
| System runs out of memory during simplification. | The data structures holding the mesh and error metrics are too large for available RAM. | Implement out-of-core processing techniques that work on portions of the mesh at a time, or use more efficient data structures like progressive meshes. |
Experimental Protocols
Protocol 1: QEM-Based Simplification with Texture Fidelity
This protocol is adapted from a method that integrates 3D reconstruction data to preserve textures [22].
1. Objective: To simplify a 3D mesh while minimizing texture distortion and reducing texture data volume. 2. Materials:
- Original 3D mesh model
- Set of calibrated images from the reconstruction process 3. Methodology:
- Step 1: Construct Reference 3D Model Scene. Using the original mesh and calibrated images, construct a reference 3D scene with high-quality texture mapping.
- Step 2: Generate Reference Image Set. Back-project the reference 3D model scene using the known view poses (external camera parameters) to generate a consistent set of reference images.
- Step 3: Mesh Simplification. Apply a Quadric Error Metric (QEM) algorithm to simplify the mesh geometry. The cost of edge collapse operations can be modified to consider texture deviation.
- Step 4: Texture Remapping and Simplification. For the simplified mesh, perform texture remapping using the reference image set as the data source. Adaptively downsample the texture resolution based on the mesh simplification parameters to reduce data size. 4. Validation:
- Qualitatively compare the texture quality of the original and simplified models.
- Quantitatively measure the geometric error (e.g., using Hausdorff distance) and the reduction in texture data size [22] [23].
Protocol 2: Building Model Simplification Using Triangle Folding
This protocol is based on a simplification algorithm designed for complex 3D building models [23].
1. Objective: To reduce the number of triangular meshes in a complex 3D building model without affecting its overall visual effect. 2. Materials:
- A 3D building model with a large number of triangular meshes. 3. Methodology:
- Step 1: Identify Feature Vertices. Calculate the sharp features of the model's vertices. Vertices with values exceeding a threshold are identified as feature vertices to be constrained.
- Step 2: Calculate Constraint Factors. Introduce multiple constraint factors (e.g., related to curvature, edge length, dihedral angle) to control the simplification error.
- Step 3: Compute Mahalanobis Distance. To manage the complexity introduced by multiple constraints, calculate the Mahalanobis distance for the constraint factors. This helps in evaluating the overall error while considering the correlation between different constraints.
- Step 4: Perform Triangle Folding. Execute the triangle folding simplification operation, prioritizing operations with the smallest Mahalanobis distance error. 4. Validation:
- Use the Hausdorff distance to quantitatively evaluate geometric deviation.
- Record the simplification time and the resulting frame rate during rendering for performance evaluation [23].
Research Reagent Solutions
This table details key software and data components essential for experiments in 3D reconstruction and model simplification.
| Item Name | Function/Benefit | Application Context |
|---|---|---|
| Mimics (Materialise NV) | Medical image analysis software used to import MRI/CT DICOM data and generate initial 3D geometry models through thresholding and segmentation [24] [14]. | Creating 3D models from medical scans for Finite Element Analysis, such as modeling the pelvic floor for biomechanical studies [24] [14]. |
| Geomagic Studio (3D Systems Inc) | Reverse engineering software used to convert a 3D image (e.g., from Mimics) into a accurate, water-tight solid 3D model suitable for simulation and analysis [24] [14]. | Refining 3D models for FEA; processing the pelvic floor model by gridding and surface fitting [24] [14]. |
| Abaqus (Dassault Systèmes) | A software suite for finite element analysis and computer-aided engineering. It is used to simulate the mechanical behavior of the 3D model under various conditions [24] [14]. | Performing biomechanical simulations; analyzing stress and strain in a pelvic floor model during different physiological states [24] [14]. |
| Quadric Error Metric (QEM) | A powerful algorithm for mesh simplification that calculates the error of potential edge collapse operations as the sum of squared distances to a set of associated planes. It is efficient and produces high-quality results [22]. | General-purpose mesh simplification for reducing polygon count while preserving geometric details. Can be extended to consider texture attributes [22]. |
| Reference Image Set | A set of images generated by back-projecting a textured 3D model. It provides a consistent, high-fidelity source for texture remapping after mesh simplification [22]. | Integrated 3D reconstruction and simplification pipelines to avoid texture distortion and achieve texture content simplification [22]. |
FAQs on Material Model Selection and Troubleshooting
1. How do I choose between a Linear Elastic and a Hyperelastic model?
The choice depends on the material you are modeling and the expected amount of deformation.
- Linear Elastic models follow Hooke's Law, where stress is directly proportional to strain. Use this model for materials like metals, ceramics, or rigid structures that undergo small deformations (typically less than 1%) [25].
- Hyperelastic models are designed for materials like rubber, soft biological tissues, or polymers that can experience extremely large, reversible deformations (often in the range of 100% to 700% strain). They use a strain energy density function to capture the nonlinear relationship between stress and strain [25] [26]. For soft tissues, which are often inhomogeneous and multiphasic, hyperelastic models are a foundational component in describing their complex, nonlinear behavior [27].
2. My FEA simulation with a Hyperelastic material won't converge. What should I check?
Convergence issues with hyperelastic materials are common and can be addressed by checking the following:
- Material Parameters: Ensure the parameters for your hyperelastic model (e.g., Mooney-Rivlin, Ogden) are accurately derived from experimental test data. An incorrect strain energy function can lead to non-physical results [28].
- Element Formulation: Use appropriate element types. For nearly incompressible materials like elastomers and soft tissues, hybrid elements (which often have an "H" in their name, like C3D8H in Abaqus) should be used to handle the incompressibility constraint [28].
- Contact Definitions: If your model involves contact, an ill-conditioned system can cause divergence. Check for initial penetrations and consider adjusting contact stiffness. Switching from Bonded to Frictional contact and using an "Adjust to Touch" interface treatment can improve convergence [29].
- Mesh Refinement: Perform a mesh sensitivity study. A mesh that is too coarse may not capture the large deformation gradients, while an excessively fine mesh increases computation time. The solution should not change significantly with further mesh refinement [30].
- Load Stepping: Nonlinear problems require the load to be applied in small increments. Reduce the initial time step size and increase the minimum number of substeps to allow the solver to converge [29].
3. What is the difference between a phenomenological and a micro-mechanical hyperelastic model?
Hyperelastic models are generally categorized based on their theoretical foundation [28]:
- Phenomenological Models: These are based on continuum mechanics and ideal elastomer properties. They mathematically fit the observed stress-strain data without considering the underlying microstructure. Examples include:
- Neo-Hookean
- Mooney-Rivlin
- Yeoh
- Ogden
- Micro-Mechanical Models: These models derive from the statistical mechanics of polymer chains, linking the macroscopic behavior to the network microstructure. Examples include:
- Arruda-Boyce
- Hybrid Models: These combine aspects of both phenomenological and micro-mechanical approaches. An example is the van der Waals model.
4. When is a Poroelastic model necessary, and what are its challenges?
A poroelastic model is essential for simulating saturated porous materials where the interaction between a solid matrix and interstitial fluid governs the mechanical response.
- When to Use: It is critical for tissues like articular cartilage and the intervertebral disc, which have a porous solid matrix saturated with fluid. Their nonlinear, time-dependent behavior (e.g., creep, stress relaxation) is governed by fluid flow and pressurization [27].
- Challenges: Developing these models is complex due to the tissue's inhomogeneous, multiphasic, and anisotropic (direction-dependent) structure. Users must be aware of the capabilities and limitations of these approaches to adequately simulate a specific biological phenomenon [27].
Comparison of Hyperelastic Models
The table below summarizes key hyperelastic models to guide your selection. The accuracy of a model is defined by how closely its predicted stress matches stresses derived from mechanical tests [28].
| Model Name | Category | Typical Use Cases | Key Characteristics |
|---|---|---|---|
| Neo-Hookean [28] | Phenomenological | Simple rubber components, preliminary analysis. | The simplest model; depends only on the first deviatoric invariant ((I_1)). |
| Mooney-Rivlin [28] | Phenomenological | Rubber-like materials, elastomers. | An extension of Neo-Hookean; includes a term with the second deviatoric invariant ((I_2)), often more accurate. |
| Yeoh [28] | Phenomenological | Carbon-black filled rubber, materials with large deformation. | Good for describing behavior at large strains and with limited experimental data. |
| Ogden [28] | Phenomenological | Very large deformations, complex stress states. | Models the response in terms of principal stretches; can be very accurate over a wide strain range. |
| Arruda-Boyce [28] | Micro-Mechanical | Polymers, elastomers. | An eight-chain model based on the statistical mechanics of polymer chains; accounts for network stretching. |
Experimental Protocol for Characterizing Soft Materials
This protocol outlines a general methodology for obtaining material parameters for hyperelastic models, which is also relevant for calibrating models for certain soft biological specimens.
1. Objective: To perform mechanical tests on a soft material specimen (e.g., rubber, tissue-engineered sample) to generate stress-strain data for calibrating a hyperelastic material model in FEA software.
2. Materials and Reagents:
- Universal Testing Machine: Equipped with a load cell and environmental chamber if needed.
- Specimen Grips: Suitable for the test type (e.g., clamps for tensile tests, compression plates).
- Digital Image Correlation (DIC) System: Optional, for full-field strain measurement.
- Software: For machine control, data acquisition, and curve-fitting of hyperelastic models.
3. Procedure:
- Specimen Preparation: Prepare specimens according to relevant standards (e.g., ASTM D412 for rubber, custom geometries for tissue samples). Measure and record the exact dimensions of each specimen.
- Mechanical Testing: Perform at least two of the following three fundamental tests to capture different deformation modes. A strain rate of 1.0 mm/min is typical for quasi-static characterization [31].
- Uniaxial Tension: Clamp the specimen ends and extend it until failure or a target strain.
- Uniaxial Compression: Place the specimen between two plates and compress it.
- Planar Shear (or Biaxial Tension): Stretch a thin sheet of material along two perpendicular axes. This is highly valuable for capturing anisotropic behavior.
- Data Collection: Record force-displacement data for all tests. If using DIC, capture the full-field strain map.
- Data Processing:
- Convert force-displacement data into engineering or true stress-strain curves.
- Import the experimental stress-strain curves into your FEA software's material calibration module.
- Use the software's curve-fitting tool to fit various hyperelastic models (e.g., Mooney-Rivlin, Ogden, Yeoh) to the experimental data. The software will calculate the model parameters that provide the best fit.
4. Validation:
- Develop a simple FEA model of the test itself (e.g., a single element test or a model of the specimen).
- Assign the calibrated hyperelastic material to the model.
- Run the simulation and compare the FEA-predicted force-displacement response with the original experimental data. A good agreement, such as an average error of ~10% for modulus, validates the procedure [32].
Research Reagent and Material Solutions
The table below lists key materials and their functions in experimental mechanics and FEA, relevant to the field of material model development.
| Item | Function in Experiment/Simulation |
|---|---|
| Silicone Elastomers | Used as model materials for validating hyperelastic constitutive models due to their consistent, rubber-like properties. |
| Ti6Al4V Alloy Powder | Metal powder used in Powder Bed Fusion (e.g., EBAM, SLM) to fabricate porous lattice structures for mechanical testing and model validation [31]. |
| Formalin-Ethyl Acetate Solution | Used in the Formalin-ethyl acetate centrifugation technique (FECT) for stool sample preservation and parasite concentration, creating a specimen for mechanical analysis [33]. |
| Hybrid Finite Elements | Specialized elements (e.g., C3D8H in Abaqus) used to model incompressible or nearly incompressible materials like hyperelastic polymers and soft tissues [28]. |
Workflow for Material Model Selection and Troubleshooting
The diagram below outlines a logical pathway for selecting a material model and addressing common convergence problems.
Frequently Asked Questions (FAQs)
Q1: What are the primary clinical outcome measures that can be validated through a pelvic floor FEA model? The retrovesical angle (RVA) and anorectad angulation (ARA) are key clinical metrics used to quantitatively validate the effectiveness of a finite element model of the pelvic floor. These angles are known to approach their normal physiological ranges when the model correctly simulates enhanced urinary and defecation control ability, for instance, after simulating targeted rehabilitation training. Comparing the model's output of RVA and ARA against clinical data is a standard method for verifying the model's biofidelity [34].
Q2: How can I objectively define "difficult stool consistencies" as a material in my FEA software? "Difficult stool consistencies," such as those representing constipation, are not single-point definitions but exist on a continuum. You can define them using the Bristol Stool Scale (BSS) and correlate this with quantitative minimal pressure (MP) values. Stool consistency can be directly measured as the gram-force required for a cylindrical probe to penetrate the stool sample by a specific depth. The following table summarizes this relationship, demonstrating that lower BSS types (indicating harder stools) correspond to exponentially higher minimal pressure values [35].
Table 1: Relationship Between Bristol Stool Scale and Measured Stool Hardness
| Bristol Stool Scale (BSS) Type | Description | Minimal Pressure (MP) Value Range |
|---|---|---|
| BSS 1-2 | Hard Stools (Constipation) | High MP, exponentially increasing as BSS decreases [35] |
| BSS 3-5 | Normal Stools | Intermediate MP, large variance within these categories [35] |
| BSS 6-7 | Soft/Loose Stools (Diarrhea) | Low MP [35] |
Q3: My model is not converging when simulating high intra-abdominal pressure (e.g., Valsalva maneuver). What could be the issue? This is often a problem of material properties and geometric non-linearity.
- Incorrect Tissue Properties: Ensure you are using appropriate hyperelastic material models (like Yeoh or Mooney-Rivlin) for soft tissues such as the levator ani muscle, external anal sphincter, and rectum. Using linear elastic models may not capture the large, nonlinear deformations accurately [34].
- Insufficient Mesh Refinement: The mesh in contact regions and areas of high stress concentration may be too coarse. Use curvature and proximity-based meshing functions to automatically refine the mesh in these complex geometric areas without making the entire model excessively large, which can help with both convergence and result accuracy [36].
Q4: How can I visualize the results of my simulation, such as stress distributions in the pelvic floor muscles? Use a symbol plot (also known as a vector plot). This visualization tool displays arrows on your model where the length represents the magnitude of a tensor or vector result (e.g., stress, strain) and the direction indicates its orientation. For tensor results like principal stress, arrowheads pointing toward the shaft typically represent compression, while arrowheads pointing away represent tension, allowing you to quickly identify areas of high mechanical load [37] [38].
Troubleshooting Guides
Problem: Difficulty in Creating a Geometrically Accurate Pelvic Floor Model from Medical Scans
Solution: Follow a structured workflow for model creation and meshing.
Diagram 1: Pelvic Floor Model Creation
Key Steps:
- Image Acquisition: Obtain high-resolution CT (for bone geometry) and static/dynamic MRI (for soft tissue geometry and motion) scans with the participant in a supine position [34].
- Segmentation and Reconstruction: Use medical modeling software like Mimics to segment the DICOM images and reconstruct a preliminary 3D model of the pelvic floor, abdomen, back, and hip structures [34].
- Geometry Processing: Smooth the initial 3D model to reduce sharp angles and create a geometry suitable for high-quality meshing [34].
- Meshing Strategy: Import the geometry into your FEA software (e.g., Ansys). For complex anatomical structures, use an automatic tetrahedral mesher with adaptive sizing. Determine a global element size based on the smallest feature you need to resolve (e.g., thickness of muscular sheets). Use defeaturing to ignore tiny geometric details that do not contribute to global stiffness [36].
Problem: Uncertainty in Assigning Material Properties to Biological Tissues
Solution: Derive properties from published literature and adjust for the specific demographic (e.g., elderly population). The table below summarizes common material models for key tissues [34].
Table 2: Common Material Models for Pelvic Floor Tissues in FEA
| Anatomical Element | Recommended Material Model | Example Material Constants (from literature) | Function in the Model |
|---|---|---|---|
| Bladder, Urethra, Rectum, External Anal Sphincter, Levator Ani Muscle | Yeoh / Mooney-Rivlin (Hyperelastic) | C10 = 0.071, C20 = 0.202, C30 = 0.048 (Bladder example) [34] | Captures the large-strain, non-linear behavior of soft tissues. |
| Other Pelvic Organs, Muscles, Fat | Hooke (Linear Elastic) | Young's Modulus, Poisson's Ratio [34] | Simplifies materials with less critical mechanical roles. |
| Abdominal, Back, Hip Muscles | Standard Linear Solid Model (Viscoelastic) | Relaxation Modulus, Decay Constant [34] | Accounts for time-dependent and strain-rate dependent responses. |
| Pelvis | Rigid Body | N/A | Fixed structure due to its high stiffness relative to soft tissues [34]. |
Problem: Validating That the Simulation Accurately Represents a Pathological Condition like Constipation
Solution: Implement a two-step validation process linking stool mechanics to pelvic floor biomechanics.
- Define the Input (Stool Properties): Characterize the stool consistency associated with constipation. According to research, stools passed with straining are, on average, 1.88-fold harder (as measured by minimal pressure) than those passed without straining. This quantitative value can be used to define a mechanical load or boundary condition in the rectum [5].
- Validate the Output (Pelvic Response): Compare your model's predictions against established clinical markers. For example, a model simulating defecation of hard stool should show alterations in the anorectad angulation (ARA) and retrovesical angle (RVA) that are consistent with clinical observations in constipated patients. This closes the loop between the mechanical input and the physiological output [34].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Software for Pelvic Floor FEA Research
| Item / Solution | Function in the Research Context |
|---|---|
| 3.0T Magnetic Resonance Scanner | Provides high-resolution static and dynamic MRI data for creating geometrically and kinematically accurate 3D models of the pelvic floor structures [34]. |
| Mimics Software | Industry-standard platform for segmenting 2D medical images (CT/MRI) and reconstructing 3D computer models suitable for FEA [34]. |
| Ansys Mechanical | A comprehensive FEA software suite used for applying material properties, meshing, applying loads and boundary conditions, and solving the simulation [34]. |
| TA.XTExpress Texture Analyzer | A instrument that provides direct, objective measurement of stool consistency (hardness) by quantifying the gram-force required for a probe to indent a stool sample, translating subjective BSS classes into quantitative engineering values [5]. |
| Yeoh and Mooney-Rivlin Hyperelastic Models | Mathematical models implemented in FEA software to describe the stress-strain behavior of biological soft tissues like muscles and organs, which undergo large, nonlinear deformations [34]. |
Solving Common FEA Challenges in Stool Consistency Simulation
FAQ: Frequently Asked Questions
1. What is the most common cause of inaccurate stress results in FEA, and how can it be resolved? The most common cause is an under-refined mesh, particularly in areas with high stress gradients. Resolution involves performing a mesh convergence study [39] [40]. This process requires running multiple simulations while progressively refining the mesh and monitoring key results like stress. The study is complete when these results stabilize and further refinement brings negligible change (e.g., less than 1-5%) [40]. For complex material behaviors, advanced techniques like local mesh refinement can focus computational resources on critical areas without inflating the overall model size [39].
2. How do I choose between solid (3D) and shell (2D) elements for my model? The choice depends on your model's geometry and the physics you need to capture [41] [42].
- Use solid elements for thick, bulky structures where stress varies in all three dimensions [41].
- Use shell elements for thin-walled structures (like sheet metal or a soda can) where the thickness is much smaller than the other dimensions. Shell elements are more efficient and often more accurate for these geometries, as solid elements can create artificially stiff structures or require an excessive number of elements through the thickness [42].
3. What are stress singularities and how should I handle them? Stress singularities are numerical artifacts that produce unreasonably high, non-physical stress values, typically at sharp corners, point loads, or hard constraints [39]. They are a result of the model's idealization rather than real behavior. To handle them:
- Identify them: Be skeptical of very high stresses isolated at a single point that diverge with mesh refinement.
- Mitigate them: Use techniques like adding a small fillet to sharp corners, applying loads over a small area instead of at a point, or using soft constraints instead of hard fixes [39]. The software's stress smoothing tools can also help minimize these effects [39].
4. My model has a complex geometry. Is it better to use a hexahedral (hex) or tetrahedral (tet) mesh? For complex geometries, a tetrahedral mesh is often the most practical choice, as it can be automatically generated on almost any shape [42]. However, hexahedral elements are generally preferred where possible because they can provide higher accuracy with fewer elements [42]. A best practice is to simplify the geometry (e.g., by removing small, non-critical fillets) to make it more amenable to a hex-dominant mesh. If a tet mesh is necessary for complexity, ensure you use a finer mesh and potentially second-order elements to maintain accuracy [42].
5. What does "enforcing common nodes" mean, and when should I use it? "Enforcing common nodes" is a meshing technique for assemblies where the nodes of adjacent parts are perfectly aligned at their interfaces [43]. This method is ideal when you need the most accurate results for forces and stresses at the connection between components, as it perfectly bonds the parts. While it may take slightly longer to generate the mesh, it often results in a shorter solution time and more accurate interfacial results compared to a mesh with independent (non-aligned) nodes [43].
Troubleshooting Guide
| Problem | Symptom | Likely Cause | Solution |
|---|---|---|---|
| Non-convergence | Solver fails to find a solution; analysis aborts. | Poor-quality elements (highly distorted) or an unstable numerical model [44]. | Check and repair mesh quality metrics like Aspect Ratio and Jacobian; simplify geometry [44] [45]. |
| Inaccurate Local Stresses | Stress values keep increasing as the mesh is refined, without stabilizing. | Mesh is too coarse in critical areas or presence of a stress singularity [39]. | Perform a mesh convergence study and apply local mesh refinement; check for and mitigate singularities [39] [40]. |
| Excessively Long Solve Time | Simulation takes impractically long to complete. | Mesh is globally too fine, or inappropriate element type is used [42]. | Use a coarser mesh in non-critical areas; consider using shell elements for thin parts; leverage adaptive meshing [41] [42]. |
| Unbalanced Forces at Interfaces | In an assembly, action-reaction forces at a connection are not equal and opposite. | A coarse mesh with independent (non-aligned) nodes at the component interface [43]. | Enforce "common nodes" at the contact region or apply a local mesh control to refine the interface mesh [43]. |
Key Mesh Quality Metrics
For a reliable simulation, your mesh should be evaluated against standard quality metrics. The table below summarizes key parameters and their target values [44] [45].
| Metric | Description | Ideal Value | Impact of Poor Value |
|---|---|---|---|
| Aspect Ratio | Ratio of the longest to shortest element edge [44]. | < 5 (Close to 1 is ideal) [44] [45]. | Causes numerical errors and inaccuracies in stress/strain calculations [44]. |
| Skewness | Measure of element symmetry deviation from an ideal shape [44]. | 0 - 0.75 (Lower is better) [44]. | Leads to interpolation errors and uneven stress distributions [44]. |
| Jacobian | Evaluates mapping from ideal to actual element shape [44]. | Close to 1 (Values > 0.6 are often acceptable) [44]. | Significant deviation indicates high distortion, compromising accuracy and stability [44]. |
| Warping | Measures out-of-plane curvature of element faces [44]. | Minimal (Primarily a concern for shell elements) [44]. | Leads to inaccuracies in stress interpolation for shell analyses [44]. |
Experimental Protocol: Mesh Convergence Study
A mesh convergence study is essential to ensure your results are independent of the mesh discretization. Follow this detailed methodology [39] [40]:
- Create a Base Mesh: Generate an initial, relatively coarse mesh for your model.
- Run Simulation and Record: Solve the analysis and record the values of key outputs (e.g., maximum stress at your area of interest, natural frequency).
- Refine and Iterate: Systematically refine the mesh globally or in critical regions. Run the simulation again and record the same key outputs.
- Analyze for Stability: Repeat step 3 until the key outputs change by less than a pre-defined tolerance (e.g., 1-5%) between successive refinements [40].
- Establish Baseline: The coarsest mesh that produces results within this tolerance is considered sufficiently refined and can be used for further parametric studies.
The workflow for this protocol is summarized in the following diagram:
The Researcher's Toolkit: Essential Meshing Reagents
This table details the key "reagents" or tools and concepts used in the FEA mesh optimization process.
| Tool / Concept | Function in the "Experiment" |
|---|---|
| Mesh Convergence Study [39] [40] | The core validation protocol to ensure simulation results are accurate and not an artifact of the mesh discretization. |
| Local Mesh Refinement [39] | A targeted technique to increase mesh density in critical regions (e.g., high stress gradients) without unnecessary global computational cost. |
| Aspect Ratio [44] | A key quality metric used to screen for poorly shaped, elongated elements that can degrade solution accuracy. |
| High-Performance Computing (HPC) [46] | Infrastructure that provides the computational power required for solving large, complex, or finely discretized models in a reasonable time. |
| Geometry Simplification [45] [42] | A pre-processing step to remove non-critical features (e.g., tiny fillets, text) that complicate meshing and increase element count without improving result accuracy. |
In finite element analysis (FEA), particularly within Abaqus/Standard, convergence signifies that the numerical calculations for solving nonlinear problems have stabilized, producing accurate results where further iterations don't significantly alter the solution [47]. Achieving convergence is fundamental to the reliability of simulations, especially in complex biomechanical research, such as modeling the pelvic floor's response to different stool consistencies [14].
Nonlinear problems are often solved using Newton's method, an iterative numerical technique. The solution is found incrementally, with each iteration solving a linearized system of equations until the solution meets specified convergence criteria [48] [47]. A failure to converge indicates that the solver cannot find a static equilibrium for the given model and loading conditions.
Common Causes of Convergence Issues
Convergence difficulties in models involving nonlinear materials and contact typically stem from several common modeling issues [47]:
- Inappropriate Constraints: Defining conflicting boundary conditions or contact conditions that lead to singularities or unstable configurations.
- Incorrect Element Choice: Using element types unsuitable for the large deformations or material behaviors present in the analysis.
- Material Model Defects: Defining inadequate material models that do not accurately represent the physical behavior, such as hyperelastic or plastic properties for soft tissues.
- Unstable Physical Systems: Modeling scenarios with inherent instabilities, like buckling or collapse, without using appropriate analysis procedures (e.g., Riks method).
- Improper Increment Size: Setting a time increment that is too large for the solver to resolve the nonlinearities effectively.
The Challenge of Contact
Contact introduces severe discontinuities into the model, where constraints change abruptly as surfaces touch or separate. This is a common source of convergence problems [49]. The recommended approach in Abaqus/Standard is to use general contact with surface-to-surface discretization. This method enhances solution quality, avoids issues like contact snagging, and uses penalty constraint enforcement, which generally offers better convergence characteristics than the node-to-surface approach [49].
Techniques for Improving Material and Contact Convergence
Contact Modeling Best Practices
| Technique | Description | Benefit |
|---|---|---|
| Use General Contact | Employs surface-to-surface discretization and includes supplemental edge and vertex formulations [49]. | Avoids snagging/chattering; provides more robust contact detection. |
| Penalty Enforcement | The default constraint enforcement for general contact; allows small penetrations to calculate contact force [49]. | Improved convergence characteristics compared to kinematic enforcement. |
| Adequate Contact Stabilization | Applies small damping forces to prevent rigid body motions at the start of an analysis [49]. | Helps achieve initial equilibrium, especially in complex assemblies. |
Material and Solution Controls
| Technique | Description | Application Context |
|---|---|---|
| Quasi-Newton Method | An approximation of Newton's method that reduces the frequency of Jacobian matrix reformations [48]. | Best for large models with many iterations per increment or where stiffness changes slowly. |
| Line Search Algorithm | Used in conjunction with quasi-Newton; scales the iteration correction to minimize residuals [48]. | Activated by default with quasi-Newton; improves robustness. |
| Viscous Regularization | Adds a small, strain-rate dependent stress to the material response. | Helps stabilize analyses involving soft, highly deformable materials. |
Adjusting Convergence Criteria
Abaqus/Standard uses default, strict tolerances to ensure a solution is acceptably close to the exact equilibrium [48]. These criteria are based on residuals (out-of-balance forces) and corrections (changes in nodal variables). While adjusting these tolerances is possible, it should be done with extreme caution, as loosening them may accept inaccurate solutions. It is often more productive to address the underlying modeling issue causing the lack of convergence [48].
Troubleshooting Workflow for Convergence Problems
The following diagram outlines a systematic workflow for diagnosing and resolving convergence issues.
Application to Pelvic Floor Biomechanics Research
In finite element analysis of pelvic floor biomechanics, simulating physiological states like the Valsalva maneuver or bowel movement involves large deformations and complex tissue interactions [14]. The consistency of stool—classified as hard, normal, or loose—directly influences the mechanical load on the pelvic structures [50]. Successfully modeling this requires careful attention to convergence.
- Material Models: Pelvic tissues (muscles, fascia, organs) exhibit highly nonlinear, hyperelastic behavior. Using stable material models and potentially viscous regularization is crucial.
- Complex Contact: The model includes numerous contact pairs between organs, muscles, and bones. Employing general contact is essential to manage these interactions robustly [49].
- Validation: The accuracy of the converged model must be validated. This can be done by comparing simulation results, such as internal pressures and organ deformation, against dynamic MRI data captured during actual physiological maneuvers [14].
The Researcher's Toolkit: Essential Reagents & Materials
The table below lists key components used in constructing and analyzing a pelvic floor finite element model.
| Research Reagent / Material | Function in the Experiment / Analysis |
|---|---|
| Abaqus FEA Software | Primary environment for model processing, simulation, and biomechanical finite element analysis [14]. |
| Mimics Software | Used for importing MRI/CT DICOM data and constructing the initial 3D geometry of pelvic organs, bones, and muscles [14]. |
| Geomagic Studio | Reverse engineering software used for refining 3D geometry and generating a solid model suitable for meshing [14]. |
| MRI & CT Scan Data | Provides the foundational imaging data for creating a patient-specific, anatomically accurate model of the pelvic cavity [14]. |
| Hyperelastic/Plastic Material Models | Mathematical models within Abaqus that represent the nonlinear stress-strain behavior of biological soft tissues [47]. |
| General Contact Algorithm | The recommended method in Abaqus/Standard for defining interactions between all model components, critical for robustness [49]. |
Frequently Asked Questions (FAQs)
Q: What is the single most important change I can make to improve contact convergence? A: Switch to using General Contact with its default surface-to-surface discretization and penalty enforcement. This avoids many issues inherent in the older contact pair definitions, such as snagging and chattering [49].
Q: Should I relax the convergence criteria if my model won't converge? A: This should be a last resort. The default tolerances in Abaqus/Standard are designed to ensure an accurate solution. Loosening them might allow a non-equilibrated solution to be accepted as converged, leading to inaccurate results. It is almost always better to identify and fix the root cause of the convergence problem [48].
Q: What is the difference between the Newton method and the Quasi-Newton method? A: The standard Newton method recalculates and factorizes the system's Jacobian (stiffness) matrix every iteration, providing quadratic convergence. The Quasi-Newton method approximates the Jacobian, reforming it less frequently (e.g., every 8 iterations by default). This can save substantial computational cost, especially in large models, but does not provide quadratic convergence [48].
Q: My model involves soft tissues and large deformations. What solution techniques can help? A: First, ensure your material model is appropriate. Then, consider using the Quasi-Newton method in combination with the Line Search algorithm, which is activated by default for Quasi-Newton. This combination can be very effective for problems where the stiffness does not change radically between iterations [48].
Frequently Asked Questions (FAQs)
Q1: What are the key parameters that can be simplified in a stool consistency model without significantly affecting its predictive accuracy for defecatory function? Based on controlled evacuation studies, the bending stiffness (consistency) of simulated stools is a critical parameter. However, research using Fecobionics probes of different consistencies (0A, 10A, 40A) found that while significant differences in defecatory parameters like duration and maximum bag pressure exist between the softest (0A) and mid-range (10A) probes, no further significant changes were observed from 10A to the stiffest (40A) probe for most parameters [8]. This suggests that for modeling purposes, a simplified scale that captures the difference between soft and medium consistencies may be sufficient, without the need for highly granular stiffness values at the harder end of the spectrum [8].
Q2: How can we validate that a simplified Finite Element Analysis (FEA) model remains physiologically accurate? Validation should involve direct comparison with physiological data from human studies. Key metrics to correlate include [8]:
- Defecation Duration: The time taken to evacuate the simulated stool.
- Maximum Bag Pressure: The peak pressure generated during evacuation.
- Bend Angle: The anorectal angle during the process. A model is considered valid if its outputs for these parameters fall within the ranges observed in human subjects evacuating probes of known consistency [8].
Q3: Our model is computationally expensive when simulating a wide range of stool consistencies. How can we optimize this? The evidence indicates that the most significant physiological differences occur between soft and medium consistencies [8]. You can optimize computational resources by:
- Focusing on Critical Thresholds: Prioritize model calibration and simulations around the consistency range where parameter changes are most pronounced (e.g., between 0A and 10A).
- Reducing Granularity: Use a simplified consistency scale with fewer data points, especially at the harder end (e.g., 10A to 40A), where changes in output parameters are minimal [8].
Q4: What is the best experimental method to obtain quantitative data on stool consistency for model input? The use of "Fecobionics" devices with cores made of silicone resins of predefined hardness (e.g., Shore 0A, 10A, 40A) is a validated method [51] [8]. This approach provides a direct, quantitative measure of consistency (often in units of ln gf) that can be directly used as an input parameter in your FEA model, moving beyond subjective qualitative scales [8].
Troubleshooting Guides
Problem: Model fails to show significant differences in defecatory parameters when stool consistency is varied.
- Potential Cause 1: The range of consistencies being tested is too narrow.
- Solution: Ensure your model tests consistencies that span the critical threshold. Experimental data shows the most significant differences are between soft (0A) and medium (10A) consistencies [8].
- Potential Cause 2: The model parameters are not sensitive to changes in material properties.
- Solution: Re-calibrate the material model in your FEA software to ensure it properly reflects the non-linear and viscoelastic properties of biological tissues and simulated stools.
Problem: Simulated defecation times are consistently shorter than those observed in human experiments.
- Potential Cause: The model may not fully account for the physiological reflexes and neural control involved in defecation.
- Solution: Incorporate a feedback mechanism that modulates the contraction forces and relaxation of the anal sphincter and puborectalis muscle in response to the pressure and deformation of the simulated stool, rather than relying solely on passive mechanics.
Problem: Difficulty in translating clinical stool descriptions (e.g., from the Bristol Stool Form Scale) into quantitative model inputs.
- Potential Cause: Subjective clinical scales do not have a direct one-to-one mapping to engineering material properties.
Experimental Protocols for Key Cited Studies
Protocol 1: Investigating the Effect of Stool Consistency on Defecatory Function [8]
- Objective: To determine the impact of simulated stool consistency on key defecatory parameters.
- Materials: Fecobionics probes with silicone cores of different hardness (0A, 10A, 40A), anorectal manometry (ARM) system, balloon expulsion test (BET) equipment.
- Subjects: Recruited healthy adult subjects (e.g., n=12). Subjects with abnormal BET results (>2 minutes) are excluded.
- Procedure:
- Subjects complete constipation and fecal incontinence severity questionnaires.
- Baseline ARM and BET are performed for reference.
- The three Fecobionics probes are inserted into the rectum in a randomized order, with a 20-minute washout period between insertions.
- The device's bag is filled with water until the subject feels a sustained urge to defecate.
- Investigators leave the room, and the subject evacuates the device in privacy.
- Data on defecation duration, maximum pressures in the bag and rear, and the bend angle (anorectal angle) are recorded during evacuation.
- Analysis: Non-parametric statistical tests (e.g., Wilcoxon Signed-Rank) are used to compare median values of the recorded parameters across the three probe consistencies.
Protocol 2: Technician Scoring of Stool Consistency [10]
- Objective: To obtain objective, technician-scored stool consistency data from a healthy population and relate it to dietary and stress factors.
- Materials: Stool sample collection kits, Bristol Stool Form Scale (BSFS).
- Subjects: Healthy adults (e.g., n=364).
- Procedure:
- Participants provide a single stool sample.
- An independent, trained technician scores the stool consistency using the BSFS (1-7) without knowledge of the participant's self-score.
- Participants self-report their stool consistency using the BSFS.
- Dietary intake is assessed using 24-hour recalls, and stress is measured via questionnaires and allostatic load scores.
- Analysis: Statistical and machine learning analyses are conducted to determine the relationship between technician-scored BSFS, self-reported scores, and factors like saturated fat intake and stress hormones.
Table 1: Key Defecatory Parameters vs. Simulated Stool Consistency (Fecobionics Probe Hardness) [8]
| Parameter | 0A Probe (Soft) | 10A Probe (Medium) | 40A Probe (Hard) | Statistical Significance (example) |
|---|---|---|---|---|
| Defecation Duration (seconds) | 9 (8-12) | 18 (12-21) | Not Significantly Different from 10A | P < 0.05 (0A vs. 10A) |
| Maximum Bag Pressure (cmH₂O) | 107 (96-116) | 140 (117-162) | Not Significantly Different from 10A | P < 0.05 (0A vs. 10A) |
| Bend Angle During Evacuation | Significant straightening | Less straightening | Similar to 10A | Differed between 10A and 40A |
| Values presented as median (interquartile range). |
Table 2: Relationship between Stool Consistency, Diet, and Stress in a Healthy Population [10]
| Factor | Hard Stool | Normal Stool | Soft Stool | Statistical Significance |
|---|---|---|---|---|
| Saturated Fat Intake (g/1000 kcal) | 13.8 ± 0.40 | 12.5 ± 0.30 | Not Specified | P = 0.005 (Hard vs. Normal) |
| Allostatic Load Score (a measure of stress) | 3.07 ± 0.18 | 2.49 ± 0.15 | 2.89 ± 0.18 | P = 0.009 (Hard vs. Normal); P = 0.049 (Soft vs. Normal) |
| Values presented as mean ± SEM. |
Research Reagent Solutions
Table 3: Essential Materials for Stool Consistency and Defecatory Function Research
| Item | Function / Description | Example/Reference |
|---|---|---|
| Fecobionics Device | A simulated feces instrument that integrates pressure sensors, motion sensors, and a distensible bag to measure anorectal function during actual evacuation. | [51] [8] |
| Silicone Resins (Varying Hardness) | Used to create the core of the Fecobionics probe, allowing for precise, quantitative control over simulated stool consistency (e.g., Shore 0A, 10A, 40A). | HC9000# Silicone [8] |
| Bristol Stool Form Scale (BSFS) | A standardized, visual scale with 7 types used to classify human stool forms subjectively. | Type 1 (separate hard lumps) to Type 7 (watery) [8] [10] |
| High-Resolution Anorectal Manometry (ARM) | A diagnostic system used to assess the pressure and coordination of the anal and rectal muscles. | Used as a reference test [8] |
| Balloon Expulsion Test (BET) | A test to measure the time taken to expel a water-filled balloon from the rectum, used to identify defecatory disorders. | Normal expulsion time < 2 minutes [8] |
Workflow and Pathway Visualizations
FEA Model Simplification Workflow
Experimental Protocol for Consistency Testing
Validating Material Properties and Load Applications Against Experimental Data
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: What are the most common sources of error when validating finite element analysis (FEA) models against experimental stool consistency data?
A1: The most common validation errors stem from incorrect material property assignment and improper load simulation. Stool exhibits complex, non-linear mechanical behavior that is highly dependent on water content and composition [52]. If your FEA model uses simplified linear elastic properties or does not account for the strong correlation between water content and mechanical consistency (r~ -0.781), significant errors will occur [52]. Furthermore, applying load conditions that do not replicate the experimental penetrometer protocol (e.g., cylindrical probe, 2.0 mm/s speed, 5 mm depth) will yield non-comparable results [52]. Always ensure your computational load application matches the precise methodology of the physical texture analysis.
Q2: How can I resolve a mismatch between my FEA-predicted deformation and experimental texture analyzer results?
A2: Follow this structured troubleshooting guide:
- Verify Material Properties: Check if the mechanical properties (Young's modulus, hardness) in your model align with experimentally derived values. Stool consistency, measured as gram-force, shows a strong negative correlation with water content [52]. Ensure your model reflects this relationship.
- Check Load Application: Confirm that the force application in your simulation precisely mimics the experimental setup used in texture analysis, including probe geometry, displacement rate, and boundary conditions [52].
- Review Constraints: Incorrect boundary conditions in the FEA model that over- or under-constrain the simulated stool sample are a frequent cause of deformation mismatch. Re-evaluate the constraints against the experimental fixture.
- Assess Mesh Sensitivity: Perform a mesh convergence study. A mesh that is too coarse will not capture stress concentrations and deformation gradients accurately, leading to incorrect results.
Q3: Our experimental data on Ti-alloys shows significant scatter. How should we handle this when using the data for FEA validation?
A3: Scatter in experimental data, especially for complex materials like Ti-alloys, is expected and must be accounted for. When compiling data for validation [53]:
- Use Statistical Aggregates: Do not rely on a single data point. Use averaged values (mean, median) from multiple tests or a statistically significant sample size.
- Report Ranges and Variances: Document the standard deviation or range of properties (e.g., Young's modulus, yield strength) in your validation report. A robust FEA validation should demonstrate that the computational results fall within the experimental scatter range.
- Verify Microstructural Consistency: Ensure the Ti-alloy's phase constituents (α, β, ω, α”) and processing history (e.g., solution-treated and water-quenched) are consistent between the data you are using and the virtual material you are defining in your model [53]. Inconsistent microstructural flags are a major source of property variation.
Troubleshooting Experimental Protocols
Issue: Inconsistent Stool Consistency Measurements with Texture Analyzer
| Symptom | Possible Cause | Solution |
|---|---|---|
| High variance in gram-force readings for samples with similar Bristol Stool Form Scale (BSFS) scores. | Incorrect sample preparation or subject vs. expert rating discrepancy. | Implement a standardized storage and preparation protocol [52]. For rating, rely on a trained expert's BSFS assessment, which correlates much more strongly with direct mechanical measurements (r~ -0.789) than subject self-assessment (r~ -0.587) [52]. |
| Measurements drift over time after sample collection. | Delayed measurement leading to changes in water content and rheology. | Measure samples immediately or within a strictly defined, short timeframe after collection to prevent property alteration [52]. |
| Failure to detect consistency differences in loose stools (BSFS 6-7). | Insufficient sensitivity of the method or probe. | Optimize the protocol. A properly configured texture analyzer can sensitively detect consistency in high-water-content stools (~90%) [52]. |
Quantitative Data for Validation
Table 1: Experimentally Measured Stool Consistency Correlations [52]
| Measurement Method | Correlated With | Correlation Coefficient (r~) | Key Finding for Validation |
|---|---|---|---|
| Texture Analyzer (TAXT) | Stool Water Content | -0.781 | Confirms water content as a valid proxy for material property input in models. |
| Texture Analyzer (TAXT) | Expert BSFS Score | -0.789 | Validates BSFS as a useful, non-invasive preliminary indicator of mechanical behavior. |
| Texture Analyzer (TAXT) | Subject BSFS Score | -0.587 | Highlights the significant error introduced by non-expert classification. |
Table 2: Key Considerations for Ti-Alloy Data Compilation in FEA [53]
| Data Feature | Importance for FEA Validation | Note |
|---|---|---|
| Processing Route | Crucially affects phase composition and mechanical properties. | Most data is for a "standard condition" (ingot metallurgy + solubilization + water quench). Model what you test. |
| Phase Constituents | Directly determines elastic and plastic behavior. | Essential for accurate material model selection (e.g., α, β, α”, ω phases). |
| Oxygen Content | A critical interstitial element that massively affects properties. | Always note oxygen content (wppm) when available; small variations cause large property shifts. |
| Molybdenum Equivalency (MoE) | Indicates β-phase stability, a key microstructural descriptor. | MoE ≥ 10 is typically required to retain metastable β-phase at room temperature [53]. |
Experimental Protocol: Direct Measurement of Stool Consistency
Objective: To mechanically quantify stool consistency using a texture analyzer for the purpose of obtaining validated material properties for FEA input [52].
Equipment:
- TA.XTExpress Texture Analyser (Stable Micro Systems Ltd.) or equivalent.
- Cylindrical probe (ø 6 mm).
- Standardized sample containers.
- Standard balance for water content measurement.
Methodology:
- Sample Collection & Storage: Collect stool samples and adhere to a optimized storage protocol to prevent property changes. Measurement should be performed promptly after collection [52].
- Sample Preparation: Prepare the stool sample according to the developed protocol to ensure a uniform testing surface.
- Instrument Settings:
- Probe Type: Cylindrical, 6 mm diameter.
- Test Speed: 2.0 mm/s.
- Penetration Depth: 5 mm.
- Measured Value: Gram-force (g) required for penetration.
- Data Processing: Log-transform the raw gram-force values (ln g/probe) to achieve a normal distribution for analysis [52].
- Validation: Correl the transformed mechanical data with precisely measured stool water content and expert-rated BSFS scores to validate the measurements.
Research Workflow and Material Toolkit
Table 3: Essential Research Reagent Solutions & Materials
| Item | Function in Research |
|---|---|
| Texture Analyzer (e.g., TA.XTExpress) | The primary instrument for the direct, mechanical quantification of stool consistency (hardness), providing fundamental force-displacement data for material model calibration [52]. |
| Bristol Stool Form Scale (BSFS) | A standardized visual classification tool for the initial, non-invasive assessment of stool samples. Expert-rated BSFS scores show a strong correlation with direct mechanical measurements [54] [52]. |
| High-Throughput Computing (HTC) Resources | Enables large-scale computational simulations and data-driven prediction of material properties, reducing reliance on purely trial-and-error experimental approaches [55]. |
| Compiled Material Database | A structured, open-source database of material properties (e.g., for Ti-alloys) that is essential for comparative analysis, materials selection, and providing benchmark data for FEA validation [53]. |
Ensuring Model Accuracy and Comparative Performance
Frequently Asked Questions (FAQs)
1. What are the most common causes of a discrepancy between FEA-predicted deformation and experimental penetrometry results? Common causes include inaccurate material model definition in the FEA software (e.g., not accounting for the non-linear, viscoelastic, or thixotropic behavior of semisolids) [56], imperfections in the manufactured lattice structures or probes used for testing [57], and a misalignment of the penetrating object during the penetrometry test, which fails to ensure it is perfectly vertical [58].
2. How can I improve the accuracy of my material model for FEA of soft materials? It is crucial to incorporate rheological properties beyond a single yield stress value. Perform rotational, oscillation, and creep tests to fully characterize the viscoelastic and thixotropic nature of your material. Using a three-step thixotropy test can reveal incomplete recovery, which should be reflected in the FEA model [56].
3. Our experimental penetrometry data shows high variability between samples. How can we improve consistency? Adhere strictly to standardized sample preparation protocols. According to pharmacopoeia standards, you must carefully fill containers without forming air bubbles, level the surface, and store all samples at a controlled temperature (e.g., 25 ± 0.5 °C) for a specified duration (e.g., 24 hours) before testing. Applying a defined shear to the samples before filling can also improve consistency [58].
4. What metrics are most effective for quantitatively correlating FEA and penetrometry data? Beyond comparing simple force-displacement curves, effective metrics include:
- Yield Stress: The stress at which the material begins to flow plastically, though its value is highly dependent on the testing and evaluation method [56].
- Deformation Mechanism: For structured materials like lattices, qualitatively compare the deformation patterns (e.g., layer-by-layer fracture vs. shear banding) between simulation and experiment [57].
- Specific Energy Absorption (SEA) & Crushing Force Efficiency (CFE): These are advanced metrics for assessing the energy absorption capabilities of lattice structures under compression [57].
5. How can FEA be used to optimize a penetrometry test for a specific material? FEA can simulate the entire penetrometry process before any physical experiments are conducted. You can model different penetrating object geometries (e.g., cones vs. micro-cones) [58], simulate the effect of varying penetration speeds, and predict stress distribution within the material to identify potential failure points that may not be visible in a standard test [56] [57].
Troubleshooting Guides
Issue 1: FEA Predicts Stiffer Material Behavior Than Experimental Penetrometry Shows
This indicates that your FEA model is overestimating the material's resistance to deformation.
- Potential Cause 1: Incomplete material model.
- Solution: Re-evaluate your material's rheological data. Soft biological or pharmaceutical materials often exhibit time-dependent recovery (thixotropy) that a simple elastic-plastic model cannot capture. Implement a more sophisticated viscoelastic or thixotropic model in your FEA software based on comprehensive rheological testing [56].
- Potential Cause 2: Model does not account for material imperfections.
- Solution: If modeling structured materials (e.g., lattices), introduce stochastic imperfections into the FEA model, such as variations in strut thickness or minor porosity, which are common in additively manufactured samples and reduce overall strength [57].
Issue 2: Poor Repeatability in Experimental Penetrometry Results
High variability between replicate tests undermines the validation process.
- Potential Cause 1: Inconsistent sample preparation and temperature control.
- Solution: Implement a strict, documented sample preparation protocol. Use a temperature-controlled environment for both sample storage and testing, as specified in pharmacopoeial methods [58]. Ensure the penetrating object is also brought to the standard temperature (25 ± 0.5 °C) before the test.
- Potential Cause 2: Operator-dependent setup errors.
- Solution: Verify that the penetrometer's base is perfectly horizontal and that the penetrating object is vertical before each test [58]. Automate the release mechanism for the penetrating object to ensure a consistent, sudden release for each measurement.
Issue 3: FEA Fails to Capture the Correct Deformation Mechanism
The simulation shows a uniform compression pattern, while the experiment shows localized shear banding or layer-by-layer collapse.
- Potential Cause: The FEA model is not capturing the specific architectural failure mechanics.
- Solution: This is common in lattice structure analysis. Refine the FEA mesh to better capture stress concentrations at the nodes and struts. Validate your model against a simple lattice with a known deformation mechanism (e.g., FCC-Z structures typically show layer-by-layer fracture, while BCC-Z structures show shear banding) [57]. Ensure the contact definitions between struts in the simulation are accurately defined.
Quantitative Correlation Data
The following table summarizes key parameters that should be correlated between FEA and experimental results, depending on the material and test type.
Table 1: Key Parameters for FEA-Experiment Correlation
| Parameter | Description | Application Context |
|---|---|---|
| Peak Force / Strength | The maximum force recorded during penetration or compression. | General semisolid penetrometry [58]; Lattice structure compression [57]. |
| Yield Stress | The stress at the elastic limit, highly dependent on test method. | Rheological characterization of semisolids [56]. |
| Deformation Pattern | Qualitative visual comparison of how the material fails. | Critical for lattice structures (e.g., FCC-Z vs. BCC-Z) [57]. |
| Specific Energy Absorption (SEA) | Energy absorbed per unit mass. | Evaluating energy-absorbing structures like lattices [57]. |
| Crushing Force Efficiency (CFE) | Ratio of mean crush force to peak crush force. | Indicates the stability of energy absorption in lattices [57]. |
| Penetration Depth | Depth the object penetrates under a standard force/time. | Standardized pharmacopoeial testing [58]. |
Table 2: Example Deformation Characteristics of Ti6Al4V Lattice Structures (Experimental vs. FEA) [57]
| Lattice Type | Porosity | Experimental Compressive Strength (MPa) | FEA-Predicted Compressive Strength (MPa) | Observed Deformation Mechanism |
|---|---|---|---|---|
| FCC-Z | 50% | 108.5 | 105.2 | Layer-by-layer fracture |
| FCC-Z | 80% | 22.1 | 20.8 | Layer-by-layer fracture |
| BCC-Z | 50% | 85.3 | 81.9 | Shear band formation |
| BCC-Z | 80% | 15.7 | 14.5 | Shear band formation |
Experimental Protocols
Protocol 1: Standardized Penetrometry Test for Semisolids
This protocol is based on the International Pharmacopoeia method for measuring consistency [58].
- Apparatus Setup: Use a penetrometer with a vertical shaft, a horizontal base, a device to ensure the penetrating object is vertical, and a scale showing the depth of penetration in 0.1 mm increments.
- Sample Preparation (Select one method):
- Method A: Carefully fill three containers without introducing air bubbles. Level the surface and store at 25.0 ± 0.5 °C for 24 hours.
- Method B: Store three samples at 25.0 ± 0.5 °C for 24 hours. Apply a defined shear for 5 minutes, then fill the containers.
- Method C: Melt three samples, carefully fill the containers, and store at 25.0 ± 0.5 °C for 24 hours.
- Execution:
- Place one test sample on the base.
- Adjust the penetrating object (e.g., a cone with a total mass of 102.5 g) so its tip just touches the sample surface.
- Release the object and allow it to penetrate freely for 5 seconds.
- Clamp the object and record the penetration depth.
- Repeat for the other two containers.
- Analysis: Express the penetration value as the arithmetic mean of the three measurements, in tenths of a millimetre. If any result differs from the mean by more than 3%, repeat the test with three new samples and report the mean and RSD of all six measurements.
Protocol 2: Correlative FEA Model Setup for Penetrometry Simulation
- Geometry Creation: Create a 3D model of the penetrating object (e.g., cone) and the sample material in the container.
- Material Property Assignment: Input the material model for the sample. For semisolids, this should be based on rheological data (yield stress, viscoelastic properties, etc.) obtained from independent tests [56]. For lattices, use the base material properties (e.g., Ti6Al4V) and the specific lattice architecture [57].
- Meshing: Generate a mappable mesh, refining the mesh around the contact area between the penetrometer and the sample to ensure accuracy [57].
- Boundary Conditions and Contact Definition:
- Fix the bottom and sides of the sample container.
- Apply a vertical displacement to the penetrating object to simulate the penetration.
- Define surface-to-surface contact between the penetrometer and the sample.
- Solution and Validation: Run the simulation and extract data for force and displacement. Compare the resulting force-displacement curve and deformation pattern directly with the experimental data from Protocol 1.
Workflow Visualization
Diagram 1: FEA-Experiment Correlation Workflow
Diagram 2: Key FEA Modeling Steps
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Penetrometry and FEA Correlation Studies
| Item / Reagent | Function / Application | Specification / Notes |
|---|---|---|
| Penetrometer | Measures the penetration depth of a standard object into a semisolid under defined conditions. | Must have a vertical shaft, horizontal base, and a scale graduated in 0.1 mm [58]. |
| Standard Cones | The penetrating object; its shape and mass are critical for reproducible results. | Common cones have a mass of 102.5 g or 7.0 g (micro-cone); geometry must conform to standards [58]. |
| Rheometer | Characterizes the full flow and deformation behavior (viscosity, yield stress, viscoelasticity) of materials. | Provides essential input data for accurate FEA material models [56]. |
| Silicone Resins | Used to create simulated feces or standardized semisolid samples with tunable consistency. | Hardness (e.g., 0A, 10A, 40A shore) can be selected to mimic different stool consistencies [59]. |
| FEA Software | Performs computational simulation of the physical penetrometry test. | Allows for virtual prototyping and understanding of internal stress/strain fields. |
| Ti6Al4V Powder | Material for fabricating lattice structures via Laser Powder Bed Fusion (L-PBF). | Used in studies correlating FEA with compression of porous structures [57]. |
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: What are the most critical steps to ensure my FEA model of biological tissues produces clinically relevant pressure distribution results?
The clinical relevance of your FEA model hinges on three critical steps. First, accurate geometry acquisition using medical imaging techniques like MRI or CT scans is essential for creating a subject-specific model that reflects real anatomy [60] [61]. Second, applying appropriate non-linear, viscoelastic material properties to soft tissues (like fat and muscle) is crucial, as assuming simple linear elasticity will yield inaccurate stress profiles [61]. Third, the model must be rigorously validated against experimental pressure mapping data to ensure the simulated outputs correlate with physical reality; a high correlation coefficient (e.g., R² > 0.8) is a good indicator of a valid model [61].
FAQ 2: My FEA simulation of a seated subject shows unrealistic stress concentrations. What could be the cause and how can I fix it?
Unrealistic stress concentrations, or singularities, are a common issue. The cause is often related to the model's mesh or geometry. To resolve this, first, perform a mesh convergence study by refining your mesh in high-stress regions until the results stabilize, ensuring your solution is not mesh-dependent [60]. Second, check for sharp corners or discontinuities in your geometry, which are uncommon in biological tissues. Slight filletting or smoothing of these areas can create a more realistic stress distribution [60] [62]. Finally, verify the material properties assigned to different tissue layers; overly stiff or simplistic material models can lead to inaccurate load transfer and stress peaks [61].
FAQ 3: How can I model the interaction between a deformable structure (like a residuum) and a rigid socket to analyze interface pressure?
Modeling this contact interaction is a core aspect of such analyses. You must define a surface-to-surface contact algorithm within your FEA software, specifying the deformable body (e.g., residuum) and the rigid or deformable body (e.g., socket) [61]. The simulation should replicate the actual donning environment by applying boundary conditions that mimic the real-world fitting, such as displacement constraints or pressure loads [61]. The key output is the interface pressure distribution profile, which helps evaluate subject comfort and identify potential areas for socket design improvement to reduce the risk of tissue injury [61].
FAQ 4: What is the difference between the "Strong" and "Weak" form of a PDE in FEA, and why does it matter for my simulation?
The Strong Form of a partial differential equation (PDE) is its original form, requiring a high degree of smoothness in the solution (e.g., continuous second derivatives) [62]. This can be problematic for complex geometries or materials. The Weak Form is an integral version of the PDE that has weaker continuity requirements, making it more suitable for obtaining approximate solutions for complex real-world problems [62]. The Finite Element Method is fundamentally built on the weak formulation, which is why it is so powerful for analyzing physical phenomena described by PDEs, such as heat transfer or structural mechanics in intricate biological systems [62].
Troubleshooting Guides
Issue: Simulation Diverges or Fails to Converge A guide for when your FEA solver cannot find a solution.
| # | Step | Action | Key Parameter to Check |
|---|---|---|---|
| 1 | Check Material Model | Ensure material properties are physically possible and stable. For soft tissues, use viscoelastic or hyperelastic models instead of linear elastic [61]. | Density, Young's Modulus, Bulk Modulus [61]. |
| 2 | Refine Contact Definition | Review contact parameters, avoid initial penetrations, and adjust penalty stiffness factors. | Contact stiffness, initial gap/penetration. |
| 3 | Adjust Solver Settings | Increase the number of iterations/substeps, switch from static to dynamic solver for difficult contacts. | Time step size, number of iterations. |
Issue: Poor Correlation with Experimental Validation Data A guide for when your FEA results do not match physical measurements.
| # | Step | Action | Key Parameter to Check |
|---|---|---|---|
| 1 | Verify Geometry & Mesh | Confirm the 3D model accurately represents the experimental specimen. A mesh sensitivity analysis is mandatory [60]. | Mesh size and type (e.g., tetrahedral vs. hexahedral) [60]. |
| 2 | Review Boundary Conditions | Ensure the constraints and loads in the simulation precisely match the experimental setup [61]. | Applied forces, fixed constraints, pressure loads. |
| 3 | Calibrate Material Properties | Compare simulated vs. experimental force-displacement data for tissue samples to calibrate material parameters like hyperelastic constants [61]. | C1, C2 constants in Mooney-Rivlin model, bulk modulus (K) [61]. |
Experimental Protocols
Detailed Methodology: Estimating Pressure Distribution in a Prosthetic Socket using FEA [61]
1. Model Construction
- Data Acquisition: Obtain Magnetic Resonance Imaging (MRI) scans of the subject's residuum. Arrange images vertically with a consistent spacing (e.g., 5 mm).
- 3D Geometry Creation:
- Use image processing to identify and segment different tissue types: bone, muscle, and fat.
- Select the bone's center point and create trajectory lines around the residuum's perimeter.
- Connect intersection points to form cross-sections for each image layer.
- Use a "Swept Blend" function in CAD software (e.g., Creo) to link cross-sections and construct a 3D multimaterial model of the residuum.
- Repeat the process to create a 3D model of the prosthetic socket.
- Meshing: Import the geometry into FEA software (e.g., LS-DYNA) and generate a mesh. The element type and size should be selected based on a convergence study.
2. Material Property Assignment
- Model tissues as isotropic, homogeneous materials with viscoelastic properties based on Quasi-Linear Viscoelastic (QLV) theory.
- Use a strain-energy function (W) to define the material behavior [61]:
- ( W = W1 + W2 + W3 )
- The first term, ( W1 = C1(I1 - 3) + C2(I2 - 3) ), models the ground substance as a Mooney-Rivlin material, where ( I1 ) and ( I2 ) are invariants of the deformation tensor, and ( C1 ), ( C2 ) are material constants [61].
- The second term (( W2 )) related to collagen fibers is often ignored if fiber direction is undefined.
- The third term, ( W3 = \frac{1}{2}K[\ln(J)]^2 ), enforces near-incompressibility, where ( J ) is the determinant of the deformation gradient and ( K ) is the bulk modulus [61].
- The reduced relaxation function ( G(t) ) is defined by a Prony series: ( G(t) = \sum{i=1}^{3} Si \exp(-t/Ti) ), where ( Si ) and ( T_i ) are spectral strengths and characteristic times, respectively [61].
3. Simulation Setup and Execution
- Boundary Conditions: Apply constraints to the socket model to mimic its real-world fixation.
- Contact Definition: Define a contact interface between the outer surface of the residuum and the inner surface of the socket.
- Loading: Simulate the donning process by applying displacements or forces that bring the residuum into full contact with the socket.
- Processing: Run the simulation to solve for displacements, strains, and stresses.
4. Validation
- Compare the simulated pressure distribution at the residuum-socket interface against experimental data collected from pressure sensors.
- Calculate statistical correlation coefficients (e.g., R²) to quantify the agreement between the FEA results and experimental measurements. A value of R² > 0.8 indicates a strong correlation [61].
Workflow and Pathway Visualizations
FEA Workflow for Pressure Analysis
FEA Troubleshooting Logic Flow
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials and Software for FEA of Biological Pressure Distribution
| Item Name | Function / Purpose | Specific Example / Note |
|---|---|---|
| Medical Imaging Scanner | Acquires precise 3D anatomical data to construct subject-specific models. | MRI or CT Scanner (e.g., Siemens Magneton Symphony) [61]. |
| CAD Software | Creates and manipulates the 3D geometry of the biological structure and interacting device. | Creo Parametric (PTC Ltd.) [61]. |
| FEA Software | Performs the numerical simulation, solving for stresses, strains, and pressures. | LS-DYNA, ANSYS [61] [63]. |
| Viscoelastic Material Model | Defines the realistic, time-dependent mechanical behavior of soft biological tissues (fat, muscle). | Quasi-Linear Viscoelastic (QLV) Theory with Prony series [61]. |
| Pressure Mapping System | Provides experimental data for validation of FEA results. | Sensor mats or films that measure interface pressure. |
The fidelity of computational models in predicting real-world physiological behavior is paramount, especially in fields like drug development and biomedical device design. A material model is a mathematical representation that defines how a substance behaves under various physical conditions, such as stress, strain, and time. In the context of physiological research, these models range from simplified linear elastic assumptions to highly complex, non-linear, viscoelastic, and poroelastic formulations that attempt to capture the intricate behavior of biological tissues. Selecting an appropriate model is not merely an academic exercise; it directly influences the accuracy of surgical simulations, the safety predictions of implantable devices, and the efficacy of pharmaceutical treatments.
This guide is framed within a specific thesis research context focused on handling difficult stool consistencies using the Finite Element Analysis (FEA) method. This research aims to develop more accurate computational models of defecatory dynamics, a area where traditional material models often fall short. The challenge lies in the fact that human feces exhibit complex, large-deformation mechanical behavior, and an inaccurate constitutive model can lead to misleading simulation results, ultimately hindering the development of effective interventions for conditions like chronic constipation. This technical support center provides troubleshooting guides and detailed methodologies to help researchers navigate these complexities, ensuring their material models yield physiologically relevant and accurate predictions.
Troubleshooting Guides and FAQs
Common Material Model Selection and Implementation Issues
Q1: My Finite Element Analysis (FEA) simulation of soft tissue shows unrealistic stress concentrations and numerical instability. What could be the cause?
- A: This is a frequent challenge, often stemming from an oversimplified material model.
- Incorrect Model Type: Biological tissues like the pelvic floor muscles or stool simulants are typically non-linear and viscoelastic. Using a simple linear-elastic model will not capture their real behavior, where stiffness increases with strain and response is time-dependent [14].
- Solution: Implement a hyperelastic model (e.g., Ogden, Mooney-Rivlin) for large-strain non-linearity and couple it with a viscoelastic component to account for stress relaxation and creep.
- Unrealistic Material Parameters: The parameters for your chosen model may be poorly defined or outside a physiologically plausible range.
- Solution: Conduct a thorough literature review or perform your own mechanical testing on representative samples to calibrate the model. Use sensitivity analysis to identify which parameters most significantly impact your results.
Q2: How can I validate my physiological model to ensure it is a credible representation of the real system?
- A: Validation is a multi-step process that should extend beyond the data used to calibrate (fit) the model.
- Multi-faceted Assessment: As demonstrated in studies of physiological closed-loop controlled (PCLC) medical devices, model accuracy should be assessed using both calibration performance and predictive capability [64].
- Quantitative Metrics: Use metrics like Root-Mean-Squared Error (RMSE) to evaluate goodness-of-fit and the Akaike Information Criterion (AIC) to ensure enhanced performance isn't due to overfitting [64].
- Predictive Validation: Test the model's predictive power under conditions for which it was not calibrated. This can include predicting a subject-specific transient response or using a leave-one-out cross-validation procedure to assess inter-subject variability [64].
Q3: My model, which worked well in a controlled laboratory setting, performs poorly when applied to a broader population. Why?
- A: This often results from a lack of inter-subject variability and insufficient testing against diverse physiological states.
- Limited Training Data: A model trained on data from a homogeneous group or a narrow set of conditions will not generalize well.
- Solution: Incorporate data that captures a wide spectrum of physiological variability. In thermal comfort models, for instance, small datasets and oversimplified experimental conditions are recognized key sources of error [65].
- Ignoring Key Phenomena: The model may be missing a critical physiological phenomenon. For example, in thermal comfort, failing to account for "temporal thermal alliesthesia" (a transient state of psychological comfort) can reduce model accuracy [65].
- Solution: Systematically review the literature to identify and incorporate such domain-specific factors into your model structure or assumptions.
Data Acquisition and Preprocessing Challenges
Q4: The sensor data I am using for model calibration is noisy and contains drift. How can I improve data quality?
- A: Data preprocessing is a critical, yet often overlooked, stage in model development.
- Implement Data Cleaning: Fewer than one-third of physiological modeling studies report applying rigorous data cleaning techniques. You should routinely use:
- Outlier Removal: To exclude physiologically implausible data points.
- Filtering: Apply low-pass filters to remove high-frequency noise.
- Normalization: To standardize data ranges from different sensors or subjects [65].
- Address Sensor Drift: Sensor drift, a change in reading when the input is constant, is a common issue with technologies like IR cameras and thermocouples. Implement drift correction algorithms based on baseline measurements or control experiments [65].
- Implement Data Cleaning: Fewer than one-third of physiological modeling studies report applying rigorous data cleaning techniques. You should routinely use:
Q5: How do I determine the most important features from my physiological data to use in my model?
- A: Not all measured data points are equally informative.
- Perform Feature Extraction: More than half of modeling studies perform feature extraction, which reshapes raw data into more informative inputs. For example, instead of using raw skin temperature, you might calculate its temporal gradient (rate of change) or spatial difference across body parts [65].
- Assess Feature Contribution: To avoid overcomplicating the model, use methods like recursive feature elimination or analysis of SHapley Additive exPlanations (SHAP) values to assess the individual contribution of each feature to the model's accuracy and retain only the most predictive ones [65].
Experimental Protocols for Model Development and Validation
Protocol: Developing and Validating a Finite Element Model of the Pelvic Floor
This protocol outlines the methodology for creating a biomechanically accurate FEA model, adaptable for researching defecatory dysfunction [14].
- Objective: To construct and validate a 3D computer simulation model of the pelvic cavity to understand mechanical characteristics and physiological changes during rehabilitation.
- Ethical Approval: Secure approval from an institutional review board. Participants must provide informed consent.
- Subject Selection: Include participants with normal pelvic floor function and no reported urination or defecation dysfunction. Exclusion criteria typically involve major surgical history or neurological disorders.
- Data Acquisition:
- Medical Imaging: Collect both Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) data from each subject.
- CT Scanning: Provides high-resolution data on pelvic bones (hip bone, sacrum, coccyx).
- MRI Scanning: Essential for distinguishing soft tissues, including pelvic floor muscles (e.g., levator ani), organs (bladder, rectum), and fascia [14].
- Dynamic Maneuvers: During MRI, capture dynamic sequences such as Kegel movements (contraction) and Valsalva maneuvers (straining) to record the range of physiological motion.
- Medical Imaging: Collect both Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) data from each subject.
- Model Establishment:
- Data Import: Import DICOM images from MRI and CT scans into 3D reconstruction software (e.g., Mimics).
- Segmentation: Manually or semi-automatically outline (segment) all relevant anatomical structures in each cross-sectional image. Combine CT-derived bone data with MRI-derived soft tissue data.
- 3D Geometry Generation: Use the software to calculate 3D solid geometry models from the segmented masks and export them in a format suitable for FEA software (e.g., STL).
- Mesh Generation and Material Assignment: Import the 3D geometry into FEA software (e.g., Abaqus). Generate a finite element mesh. Assign appropriate material models (e.g., non-linear, hyperelastic models for soft tissues) to each anatomical structure.
- Model Validation:
- Geometric Verification: Simulate the dynamic maneuvers (Kegel, Valsalva) and compare the model's output—such as internal pressures and organ deformation—against the actual movements observed in the dynamic MRI sequences [14].
- Validation against Independent Data: If available, compare simulation results with physiological data obtained from other sources, such as intra-vaginal or intra-rectal pressure measurements.
Protocol: Quantifying the Effect of Stool Consistency on Defecatory Parameters
This protocol details an experimental method using simulated feces to empirically measure how material consistency affects physiological function, providing critical data for model calibration [66].
- Objective: To test the effect of various fecal consistencies on defecatory parameters using a simulated feces device (Fecobionics).
- Device Preparation:
- Fecobionics Probes: Construct simulated feces probes using silicone resins of different hardness. For example, use shores of 0A, 10A, and 40A to represent a range from normal to constipated stool consistencies, correlating to Bristol Stool Form Scale types 2-4 [66].
- Calibration: Perform mechanical testing (e.g., controlled bending experiments) on the probes to quantitatively define their consistency in units like natural log-transformed grams-force (ln gf).
- Experimental Procedure:
- Subject Recruitment: Recruit healthy adult subjects with normal defecation patterns, confirmed by questionnaires.
- Reference Tests: Perform standard anorectal function tests (e.g., anorectal manometry and balloon expulsion test) for baseline reference.
- Fecobionics Testing: For each subject, test the three probes in a randomized order.
- Insert the lubricated probe into the rectum.
- Fill the device's internal bag with saline until the subject feels a sustained urge to defecate.
- The subject then evacuates the device in privacy, mimicking a natural defecation.
- Data Collection and Analysis:
- Key Parameters: Record defecation duration, maximum internal bag pressure, and anorectal angle (derived from device bending).
- Statistical Analysis: Use non-parametric tests (e.g., Wilcoxon Signed-Rank test) to compare parameters across the different consistency probes. Median and quartiles are typically reported.
Quantitative Data from Stool Consistency Studies
Table 1: Defecatory Parameters vs. Simulated Stool Consistency [66]
| Mechanical Property (Shore Hardness) | Approx. Bristol Scale Type | Defecation Duration (seconds) | Maximum Bag Pressure (cmH₂O) |
|---|---|---|---|
| 0A (Softest) | Type 4 | 9 (8-12) | 107 (96-116) |
| 10A | Type 3 | 18 (12-21) | 140 (117-162) |
| 40A (Hardest) | Type 2 | Not Significant vs. 10A | Not Significant vs. 10A |
Table 2: Key Metrics for Physiological Model Validation [64]
| Validation Metric | Purpose | Interpretation |
|---|---|---|
| Root-Mean-Squared Error (RMSE) | Quantifies the average magnitude of difference between model output and experimental data. | A lower RMSE indicates better calibration performance. A significant reduction (e.g., 9%, P=0.03) shows improvement. |
| Akaike Information Criterion (AIC) | Evaluates the quality of a model relative to others, penalizing for complexity. | A lower AIC suggests a better model. Comparable AIC between models with more parameters indicates no overfitting. |
| Prediction Envelope Proportion | Measures the percentage of experimental data points that fall within the model's prediction range. | A significantly larger proportion (P < 0.02) indicates superior predictive capability in interpolation/extrapolation. |
Research Reagent Solutions and Essential Materials
Table 3: Essential Materials for Biomechanical and Physiological Modeling
| Item | Function/Description | Example Use Case |
|---|---|---|
| Silicone Resins (e.g., HC9000#) | Used to fabricate simulated feces with tunable mechanical properties (hardness, viscosity) [66]. | Creating Fecobionics probes with shore hardness 0A, 10A, 40A for defecation studies. |
| Fecobionics Device | An integrated tool that measures pressure, orientation, and bending during actual evacuation [66]. | Studying anorectal function in a physiologically relevant manner. |
| 3D Reconstruction Software (e.g., Mimics) | Converts 2D medical image data (MRI, CT) into 3D computational geometry [14]. | Generating accurate anatomical models for FEA. |
| Finite Element Analysis Software (e.g., Abaqus) | Solves complex biomechanical problems by simulating the physical behavior of 3D models under loads [14]. | Predicting stress and strain in pelvic floor tissues during simulated defecation. |
| Motion Processing Units (MPUs) | Sensors (gyroscopes, accelerometers) embedded in devices to track 3D orientation and bending [66]. | Measuring the anorectal angle in real-time during Fecobionics evacuation. |
Workflow and Signaling Pathway Diagrams
Diagram 1: Physiological FEA Model Workflow. This diagram outlines the integrated process of developing and validating a physiological Finite Element Analysis model, from data acquisition to final validation.
Diagram 2: Stool Consistency Impact Pathway. This diagram illustrates the logical cause-and-effect relationship between increased stool consistency and the biomechanical outcomes of difficult defecation, as measured in empirical studies.
FAQs: Finite Element Analysis in Pelvic Floor Biomechanics
Q1: What is Finite Element Analysis (FEA) and how is it applied to study bowel control?
Finite Element Analysis (FEA) is a computational technique used to simulate the mechanical properties of an object by dividing it into discrete elements and creating a numerical calculation model to represent its behavior [14]. In studying bowel control, FEA is used to construct a detailed 3D computer simulation model of the pelvic cavity, including structures like the pelvis, bladder, urethra, rectum, levator ani muscle, and supportive ligaments [14] [67]. Researchers can simulate different physiological states, such as the Valsalva maneuver and bowel movement, to investigate the effects of neuromuscular functional changes and quantify the impact of various muscle groups and nerves on continence [14].
Q2: What are the common outcome indicators used in FEA models to assess defecation ability?
Common quantitative outcome indicators used in FEA models to assess defecation ability include [67]:
- Retrovesical Angle (RVA): The angle between the bladder and the rectum.
- Anorectad Angulation (ARA): The angle of the anorectal junction.
- Stress Distribution: The internal forces within pelvic tissues.
- Strain: The degree of deformation under load. Improvements in urinary and defecation control ability are indicated when ARA and RVA approach their normal ranges through rehabilitation interventions [67].
Q3: How are FEA models of the pelvic floor validated for accuracy?
Two primary methods are used to validate FEA models of the pelvic floor [14]:
- Geometric Verification: Comparing the dynamic effects simulated by the FEA model with actual subject movements captured during dynamic MRI, such as during Kegel movements and Valsalva maneuvers. This includes assessing whether internal pressure and organ deformation align.
- Validation of Results: Ensuring that the model outputs are consistent with known physiological behaviors and established clinical measurements.
Q4: What software and hardware are typically used for such FEA studies?
Typical software and hardware used in pelvic floor FEA studies include [14]:
- Software: Mimics for 3D model building, Geomagic Studio for model refinement, and Abaqus or Ansys for biomechanical finite element analysis and simulation [14] [67].
- Hardware: A computer with an Intel Core i5 processor or better, 64-bit operating system, 16 GB of memory, and adequate storage (500GB hard disk or more).
Q5: How can FEA help in designing rehabilitation programs for bowel dysfunction?
FEA can quantitatively assess the impact of different rehabilitation training methods by simulating changes in muscle material properties. Researchers can model the effects of various interventions—such as pelvic floor muscle training, biofeedback, electrical stimulation, magnetic stimulation, and vibrational stimulation—on key outcome indicators (RVA, ARA, stress, strain) [67]. This helps in identifying the most effective interventions for specific types of dysfunction and in understanding the underlying mechanisms for improving bowel control [14] [67].
Troubleshooting Common FEA Modeling Issues
Problem: Model predictions do not match validation data from dynamic MRI.
- Potential Cause 1: Incorrect material properties assigned to pelvic tissues.
- Solution: Review literature for age-appropriate tissue properties. Pelvic soft tissue mechanical characteristics differ between young and old individuals; ensure appropriate adjustments are made [67].
- Potential Cause 2: Inadequate mesh refinement.
- Solution: Manually refine the mesh, particularly in areas of complex geometry or high-stress gradients, to improve accuracy [68].
Problem: Simulation fails to converge during nonlinear analysis.
- Potential Cause 1: Large deformations or complex contact interactions.
- Solution: Utilize FEA software with robust nonlinear solution capabilities, such as Abaqus, which features automatic time stepping to adjust increments automatically for complex simulations [69].
- Potential Cause 2: Unrealistic boundary conditions or loading.
- Solution: Re-evaluate the applied constraints and loads based on anatomical reality. Prefer displacement boundary conditions over force boundary conditions for better stability [13].
Problem: Difficulty in distinguishing pelvic muscles and fascia in medical images.
- Potential Cause: Similar density of adjacent soft tissues in CT or ultrasound.
- Solution: Use MRI as the primary imaging modality for soft tissues due to its superior contrast, and combine with CT data for bone geometry. Have experienced radiologists collaboratively outline structures in each cross-sectional image to reach a consensus [14].
Quantitative Data Tables
Table 1: Impact of Rehabilitation Training on Key Outcome Indicators
This table summarizes the relative effectiveness of five rehabilitation methods on improving parameters related to bowel control, as suggested by FEA studies. The values are illustrative of trends reported in the literature [67].
| Rehabilitation Method | Effect on Anorectad Angulation (ARA) | Effect on Retrovesical Angle (RVA) | Effect on Pelvic Floor Stress | Effect on Pelvic Floor Strain |
|---|---|---|---|---|
| Targeted Levator Ani Exercise | Significant Improvement | Significant Improvement | Favorable Reduction | Favorable Reduction |
| External Anal Sphincter Training | Significant Improvement | Moderate Improvement | Favorable Reduction | Favorable Reduction |
| General Pelvic Floor Muscle Training | Moderate Improvement | Moderate Improvement | Moderate Reduction | Moderate Reduction |
| Biofeedback Therapy | Moderate Improvement | Moderate Improvement | Moderate Reduction | Moderate Reduction |
| Electrical/Magnetic Stimulation | Mild Improvement | Mild Improvement | Mild Reduction | Mild Reduction |
Table 2: Material Properties for Pelvic Floor FEA Models
Material properties are critical for accurate FEA modeling. The table below lists constitutive models and material constants for key pelvic structures, as compiled from the literature and adjusted for elderly tissue characteristics [67].
| Anatomical Element | Constitutive Model | Material Constants (Examples from Literature) |
|---|---|---|
| Bladder | Yeoh Hyperelastic | C10=0.071, C20=0.202, C30=0.048 |
| Urethra | Mooney-Rivlin Hyperelastic | (Varies based on specific model) |
| Rectum | Mooney-Rivlin Hyperelastic | (Varies based on specific model) |
| Levator Ani Muscle | Yeoh Hyperelastic | (Varies based on specific model) |
| External Anal Sphincter | Mooney-Rivlin Hyperelastic | (Varies based on specific model) |
| Pelvic Bones | Linear Elastic (Rigid Body) | High stiffness to simulate minimal deformation |
Experimental Protocol: Building a Pelvic Floor FEA Model
Step 1: Image Data Acquisition
- Participant Criteria: Recruit a healthy volunteer (e.g., >60 years) with normal pelvic floor function and no history of defecation dysfunction or surgery [67].
- Scanning Protocol:
- CT Scan: Use to capture bone geometry. Scan from the iliac crest to the knee joint. Example parameters: slice thickness of 0.5 mm, resolution of 512 x 512 [67].
- Static MRI: Use for soft tissue geometry. Example parameters: 3D-T2 weighted sequence, 1.0 mm slice thickness, continuous volumetric scanning [14] [67].
- Dynamic MRI: Perform while the participant executes maneuvers (resting, Kegel, Valsalva) to capture pelvic floor dynamics for model validation. Example parameters: sagittal plane, 8 mm slice thickness, 9-10 frames/sec [14] [67].
Step 2: 3D Model Reconstruction
- Data Import: Import DICOM data from MRI and CT into medical image analysis software (e.g., Mimics) [14].
- Segmentation and Thresholding: In collaboration with experienced radiologists, outline organs, bones, and muscles in each cross-sectional image. Use threshold adjustments to select structures while minimizing interference from adjacent tissues [14].
- 3D Image Generation: Use the "calculate 3D" function to generate a 3D solid geometry model. Apply smoothing functions to refine edges and improve mesh quality [14] [67].
Step 3: Finite Element Model Setup
- Geometry Import and Meshing: Import the 3D image into reverse engineering software (e.g., Geomagic Studio) and then into FEA software (e.g., Abaqus, Ansys). Mesh the geometry, primarily using tetrahedral elements [14] [67].
- Material Property Assignment: Assign material properties to different tissues based on published literature, using appropriate constitutive models (e.g., hyperelastic for muscles and organs, linear elastic for bones) [67].
- Applying Boundary Conditions and Loads: Define constraints (e.g., fix pelvis as a rigid body) and simulate physiological loads and maneuvers (e.g., intra-abdominal pressure during Valsalva) [67].
Step 4: Model Validation and Simulation
- Validation: Compare simulation results (e.g., organ displacement, internal pressures) against the dynamic MRI data collected during Kegel and Valsalva maneuvers [14].
- Running Simulations: Once validated, use the model to simulate various scenarios, such as changes in muscle material properties to represent different rehabilitation training effects [67].
Workflow and Relationship Diagrams
Diagram 1: FEA model development workflow.
Diagram 2: FEA convergence troubleshooting logic.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Software for Pelvic Floor FEA
| Item | Function/Application in Research |
|---|---|
| 3.0T MRI Scanner | Provides high-resolution static and dynamic images of pelvic floor structures and movements during maneuvers [67]. |
| 64-Slice Spiral CT Scanner | Captures detailed geometry of pelvic bones, which have higher density and resolution in CT images [67]. |
| Mimics Software | Medical image processing software used to segment MRI and CT data and reconstruct initial 3D geometric models [14]. |
| Geomagic Studio | Reverse engineering software used to process the initial 3D image into a solid model suitable for finite element analysis [14]. |
| Abaqus FEA Software | A general-purpose FEA software used for simulating complex, nonlinear biomechanical behavior, including tissue deformation and contact [14] [69]. |
| Ansys FEA Software | Another major FEA software platform capable of structural and biomechanical simulations, used for numerical analysis of the model [67]. |
| Hyperelastic Material Models (Yeoh, Mooney-Rivlin) | Mathematical models used to accurately represent the nonlinear, large-strain behavior of soft biological tissues like muscles and organs [67]. |
Conclusion
The integration of sophisticated FEA methodologies provides an unparalleled tool for quantifying and predicting the biomechanical behavior of difficult stool consistencies. A rigorous approach encompassing accurate geometric modeling, appropriate material definitions, and thorough validation is paramount for generating clinically relevant insights. Future directions should focus on developing more advanced multiphysics models that couple stool mechanics with neural control and microbiome data. For researchers in drug development, these validated models offer a powerful platform for in silico testing of pharmaceuticals aimed at altering stool consistency, ultimately accelerating innovation and improving patient outcomes in managing bowel dysfunction.
References
- 1. Bristol Stool scale: Stool types and what they mean [https://www.medicalnewstoday.com/articles/bristol-stool-scale]
- 2. Bristol stool scale [https://en.wikipedia.org/wiki/Bristol_stool_scale]
- 3. Bristol Stool Chart: Types of Poop [https://www.webmd.com/digestive-disorders/poop-chart-bristol-stool-scale]
- 4. Bristol Stool Chart | Faecal | Continence Foundation of ... [https://www.continence.org.au/bristol-stool-chart]
- 5. Direct measurement of stool consistency by texture analyzer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7840686/]
- 6. On the compressional rheology of fresh faeces [https://www.sciencedirect.com/science/article/pii/S0043135421007223]
- 7. A hands-free stool sampling system for monitoring ... [https://www.nature.com/articles/s41598-022-14803-9]
- 8. Consistency of Feces Affects Defecatory Function - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11238102/]
- 9. Biomechanical constitutive modeling of the gastrointestinal ... [https://www.sciencedirect.com/science/article/pii/S0264127522001976]
- 10. Technician-Scored Stool Consistency Spans the Full ... [https://www.sciencedirect.com/science/article/pii/S0022316622001924]
- 11. Troubleshooting Finite-Element Modeling with Abaqus [https://link.springer.com/book/10.1007/978-3-030-26740-7]
- 12. AI‐Driven Defecation Analysis by Smart Healthcare Toilet [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376671/]
- 13. Learn Finite Element Analysis | The Complete Guide for FEA [https://www.simscale.com/blog/learn-finite-element-analysis-fea/]
- 14. Finite Element Analysis of Pelvic Floor Biomechanical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11179018/]
- 15. Finite element-based prioritization of pelvic floor muscles ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1663545/full]
- 16. What is Finite Element Analysis (FEA)? [https://www.ansys.com/simulation-topics/what-is-finite-element-analysis]
- 17. Finite element analysis of biological soft tissue surrounded by ... [https://tbiomed.biomedcentral.com/articles/10.1186/s12976-018-0094-9]
- 18. Immersed finite element method and its applications to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2830735/]
- 19. Current progress of digital twin construction using medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370374/]
- 20. 'Digital twins': 3D models enhance neurosurgical care [https://www.mayoclinic.org/medical-professionals/neurology-neurosurgery/news/digital-twins-3d-models-enhance-neurosurgical-care/mac-20587959]
- 21. 3D modelling in anatomy teaching: state of the art and pilot ... [https://www.sciencedirect.com/science/article/pii/S2214854X25000639]
- 22. A Model Simplification Algorithm for 3D Reconstruction [https://www.mdpi.com/2072-4292/14/17/4216]
- 23. Simplification algorithm of 3D building model based on ... [https://www.sciencedirect.com/science/article/pii/S2589004224021953]
- 24. Finite Element Analysis of Pelvic Floor Biomechanical ... [https://www.researchprotocols.org/2024/1/e56333]
- 25. Hyperelastic Materials vs Linear Elastic | ED [https://engineeringdownloads.com/hyperelastic-materials-vs-linear-elastic/]
- 26. What is the difference between a hyperelastic material ... [https://support.functionbay.com/en/faq/single/87/difference-hyperelastic-material-elastic-material-recurdyn]
- 27. Finite element modeling of soft tissues [https://pubmed.ncbi.nlm.nih.gov/24529470/]
- 28. Comparative Analysis of Various Hyperelastic Models and ... [https://www.mdpi.com/2411-9660/7/6/135]
- 29. Convergence issues with material model changes [https://innovationspace.ansys.com/forum/forums/topic/convergence-issues-with-material-model-changes/]
- 30. Convergence In FEA - What Should We Look Out For? [https://www.fidelisfea.com/post/convergence-in-fea-what-should-we-look-out-for]
- 31. Finite Element Analysis on Initial Crack Site of Porous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8659206/]
- 32. A validated finite element analysis procedure for porous ... [https://www.sciencedirect.com/science/article/pii/S0264127520300794]
- 33. Performance validation of deep-learning-based approach in ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06878-w]
- 34. Quantifying the effects of five rehabilitation training ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11233532/]
- 35. The Importance of Objective Stool Classification in Fecal 1H ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8002301/]
- 36. The FEM mesh of the future - mastering complexity ... [https://blog.cadfem.net/en/the-fem-mesh-of-the-future-mastering-complexity-automating-the-mesh]
- 37. 27.1 Understanding symbol plotting [https://classes.engineering.wustl.edu/2009/spring/mase5513/abaqus/docs/v6.6/books/usi/pt05ch27s01.html]
- 38. D.8 Displaying and customizing a symbol plot [http://130.149.89.49:2080/v2016/books/gsa/ap04s08.html]
- 39. Ansys Mechanical in 2025R1: Advanced Techniques for ... [https://blog.cadfem.ai/ansys-mechanical-in-2025r1/]
- 40. Create a Better Mesh for Accurate CFD or FEA: 5 Tips [https://www.simscale.com/blog/tips-high-quality-mesh/]
- 41. What Is Mesh in Finite Element Analysis (FEA)? [https://sdcverifier.com/structural-engineering-101/meshing-in-finite-element-analysis/]
- 42. 3 Steps to Improve FEA Models [https://www.ansys.com/blog/how-to-improve-fea]
- 43. SOLIDWORKS Simulation: How Common and ... [https://hawkridgesys.com/blog/common-nodes-meshing-solidworks-simulation]
- 44. The Fundamentals of Mesh Quality in FEA [https://sdcverifier.com/structural-engineering-101/the-fundamentals-of-mesh-quality/]
- 45. SOLIDWORKS Simulation Meshing Guide [https://www.mlc-cad.com/solidworks-help-center/solidworks-simulation-meshing-guide/]
- 46. Best Practices To Optimize Infrastructure for ... [https://www.ansys.com/blog/best-practices-to-optimize-infrastructure-ansys-simulations]
- 47. Issues| FEA Abaqus Problem- 2025 Convergence Convergence [https://caeassistant.com/blog/abaqus-convergence-issues/]
- 48. 7.2.3 Convergence criteria for nonlinear problems [https://classes.engineering.wustl.edu/2009/spring/mase5513/abaqus/docs/v6.6/books/usb/pt03ch07s02aus43.html]
- 49. and Contact in Convergence /Standard | SIMULIA - Dassault... Abaqus [https://blog.3ds.com/brands/simulia/contact-convergence-abaqus-standard/]
- 50. Does the consistency of stools define a distinct patient cohort ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530747/]
- 51. Consistency of Feces Affects Defecatory Function - PubMed [https://pubmed.ncbi.nlm.nih.gov/38533644/]
- 52. Direct measurement of stool consistency by texture ... [https://www.nature.com/articles/s41598-021-81783-7]
- 53. A compilation of experimental data on the mechanical ... [https://www.nature.com/articles/s41597-022-01283-9]
- 54. Clinical efficacy of non-pharmacological treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12160061/]
- 55. Digitized material design and performance prediction ... [https://www.frontiersin.org/journals/materials/articles/10.3389/fmats.2025.1599439/full]
- 56. Contribution to the rheological testing of pharmaceutical semisolids [https://pubmed.ncbi.nlm.nih.gov/29315014/]
- 57. An experimental and FEA investigation of deformation ... [https://www.sciencedirect.com/science/article/abs/pii/S0997753825000919]
- 58. The International Pharmacopoeia Twelfth Edition - Pharmacopoea... [https://digicollections.net/phint/en/d/Jb/10.4.2.html]
- 59. Consistency of Feces Affects Defecatory Function [https://www.jnmjournal.org/journal/view.html?uid=1902&vmd=Full]
- 60. Finite Element Methods for Modeling the Pressure ... [https://www.mdpi.com/2076-3417/12/12/6160]
- 61. Analysis of Pressure Distribution in Transfemoral Prosthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6956391/]
- 62. What Is FEA | Finite Element Analysis? (Ultimate Guide) [https://www.simscale.com/docs/simwiki/fea-finite-element-analysis/what-is-fea-finite-element-analysis/]
- 63. Finite Element Analysis of Pressure Vessels [https://www.nationalboard.org/index.aspx?pageID=164&ID=214]
- 64. Accuracy assessment methods for physiological model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8087034/]
- 65. A Structured Review of Physiological-Based Thermal ... [https://www.sciencedirect.com/science/article/abs/pii/S0378778825014203]
- 66. Consistency of Feces Affects Defecatory Function [https://www.jnmjournal.org/journal/view.html?doi=10.5056/jnm22177]
- 67. Quantifying the effects of five rehabilitation training ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1392448/full]
- 68. FAQs About Structural Analysis (FEA) [https://www.simscale.com/blog/faqs-about-structural-analysis-fea/]
- 69. Abaqus Finite Element Analysis | SIMULIA [https://www.3ds.com/products/simulia/abaqus]