Harnessing AI-Powered Image Analysis: A New Paradigm in Parasitic Disease Diagnostics and Drug Discovery
This article explores the transformative role of Artificial Intelligence in parasitic disease control, addressing a critical need for researchers, scientists, and drug development professionals.
Harnessing AI-Powered Image Analysis: A New Paradigm in Parasitic Disease Diagnostics and Drug Discovery
Abstract
This article explores the transformative role of Artificial Intelligence in parasitic disease control, addressing a critical need for researchers, scientists, and drug development professionals. It provides a comprehensive analysis spanning from the foundational drivers for AI adoption—such as rising drug resistance and the limitations of traditional diagnostics—to the core methodologies of convolutional neural networks and AI-driven high-throughput screening in action. The content delves into practical strategies for overcoming common technical and data-related challenges, validates AI performance against human experts with comparative data, and synthesizes key takeaways to outline future directions for integrating AI into biomedical research and clinical practice.
The Urgent Need for AI in Parasitology: Addressing Drug Resistance and Diagnostic Gaps
The Growing Threat of Antimalarial and Antiparasitic Drug Resistance
Antimalarial drug resistance has emerged as a critical threat to global malaria control efforts. With an estimated 263 million malaria cases and approximately 597,000 deaths reported in 2023, the emergence and spread of drug-resistant parasites jeopardizes progress achieved over recent decades [1]. Artemisinin-based combination therapies (ACTs), the current mainstay for uncomplicated malaria treatment, are now compromised by partial resistance to artemisinin derivatives and partner drugs across multiple regions [2]. This application note examines the growing threat of antimalarial and antiparasitic resistance through the lens of artificial intelligence (AI) for parasite image analysis, providing researchers with current surveillance data, experimental protocols, and innovative computational approaches to address this pressing challenge.
Current Status of Antimalarial Drug Resistance
Global Resistance Patterns
The evolution of antimalarial drug resistance follows a historical pattern of successive drug failures. Chloroquine and sulfadoxine-pyrimethamine were previously compromised, and current ACTs now face similar challenges. Partial resistance to artemisinin derivatives, characterized by delayed parasite clearance, has been observed for over a decade in Southeast Asia and has now emerged in several African countries, including Rwanda, Uganda, Tanzania, and Ethiopia [2]. This is particularly concerning as the African region bears approximately 95% of the global malaria burden [3].
Table 1: Emerging Antimalarial Drug Resistance Patterns
| Resistance Type | Geographic Spread | Molecular Markers | Clinical Impact |
|---|---|---|---|
| Partial Artemisinin Resistance | Rwanda, Uganda, Tanzania, Ethiopia, Southeast Asia | kelch13 mutations (e.g., R561H) | Delayed parasite clearance (3-5 days instead of 1-2) |
| Partner Drug Resistance | Northern Uganda, Southeast Asia, isolated cases in Africa | Potential reduced susceptibility to lumefantrine | Requires higher drug doses for parasite clearance |
| Non-ART Combination Threat | Under investigation | Novel mechanisms | Potential first-line treatment failure |
Quantitative Resistance Surveillance Data
Recent clinical trials of next-generation antimalarials provide critical efficacy benchmarks against resistant strains. The Phase III KALUMA trial evaluated ganaplacide-lumefantrine (GanLum), a novel non-artemisinin combination therapy, demonstrating a PCR-corrected cure rate of 97.4% using an estimand framework (99.2% under conventional per protocol analysis) in patients with acute, uncomplicated Plasmodium falciparum malaria [3]. This promising efficacy against resistant parasites highlights the potential of new chemical entities with novel mechanisms of action.
Table 2: Efficacy of Novel Antimalarial Compounds Against Resistant Strains
| Compound/Combination | Development Phase | Mechanism of Action | Efficacy Against Resistant Parasites | Trial Population |
|---|---|---|---|---|
| Ganaplacide-lumefantrine (GanLum) | Phase III | Novel imidazolopiperazine (ganaplacide) disrupts parasite protein transport + lumefantrine | 97.4% PCR-corrected cure rate at Day 29 [3] | 1,668 patients across 12 African countries |
| Triple Artemisinin Combination Therapy (TACT) | Late-stage development | Combines artemether-lumefantrine with amodiaquine | High efficacy against resistant parasites in clinical studies [2] | Multicenter clinical trials |
AI-Driven Solutions for Resistance Monitoring
Convolutional Neural Networks for Parasite Detection and Speciation
Advanced AI models now enable highly accurate parasite detection and species identification directly from thick blood smears. A recent deep learning model utilizing a seven-channel input tensor achieved remarkable performance in classifying Plasmodium falciparum, Plasmodium vivax, and uninfected white blood cells, with an accuracy of 99.51%, precision of 99.26%, recall of 99.26%, and specificity of 99.63% [1]. This represents a significant advancement over traditional binary classification systems that merely detect presence or absence of parasites without speciation capability.
Integrated Automated Diagnostic Systems
The iMAGING system represents a comprehensive approach to automated malaria diagnosis, integrating a robotized microscope, AI analysis, and smartphone application. This system performs autofocusing and slide tracking across the entire sample, enabling complete automation of the diagnostic process. When evaluated on a dataset of 2,571 labeled thick blood smear images, the YOLOv5x algorithm demonstrated a performance of 92.10% precision, 93.50% recall, 92.79% F-score, and 94.40% mAP0.5 for overall detection of leukocytes, early trophozoites, and mature trophozoites [4].
Experimental Protocols for Resistance Monitoring
AI-Assisted Microscopy for Parasite Detection and Speciation
Objective: To accurately detect Plasmodium parasites in thick blood smears and differentiate between species using convolutional neural networks.
Materials and Reagents:
- Giemsa-stained thick blood smear samples
- Optical microscope with 100x oil immersion objective
- Automated microscope system with X-Y stage control and autofocus capability
- High-resolution digital camera (minimum 5MP)
- Computing system with GPU acceleration (e.g., NVIDIA GeForce RTX 3060 or equivalent)
Procedure:
- Sample Preparation:
- Prepare thick blood smears according to standard WHO protocols [4].
- Stain with Giemsa (3% for 30-45 minutes) following established laboratory procedures.
- Air-dry slides completely before imaging.
Image Acquisition:
- Calibrate automated microscope for consistent illumination and focus.
- Program slide scanner to capture images from multiple fields of view (minimum 50 per sample).
- Save images in lossless format (TIFF preferred) at maximum resolution.
Data Preprocessing:
- Apply seven-channel input tensor transformation to enhance feature detection [1].
- Implement Canny algorithm edge detection on enhanced RGB channels.
- Normalize pixel values across the dataset to reduce batch effects.
Model Training:
- Partition dataset using 80:10:10 split for training, validation, and testing.
- Configure CNN architecture with residual connections and dropout layers.
- Set training parameters: batch size 256, 20 epochs, learning rate 0.0005, Adam optimizer.
- Utilize cross-entropy loss function for multiclass classification.
Validation:
- Perform 5-fold cross-validation to assess model robustness.
- Generate confusion matrices to evaluate species-specific accuracy.
- Calculate precision, recall, specificity, and F1 scores for performance metrics.
Molecular Surveillance of Antimalarial Resistance Markers
Objective: To detect and monitor genetic markers associated with antimalarial drug resistance.
Materials and Reagents:
- DNA extraction kit (commercial system recommended)
- PCR reagents: primers for kelch13, pfcrt, pfmdr1 genes
- Real-time PCR system
- Electrophoresis equipment or capillary sequencer
- Sanger sequencing reagents
Procedure:
- DNA Extraction:
- Extract parasite DNA from blood spots or cultured isolates using commercial kits.
- Quantify DNA concentration using spectrophotometry.
- Store extracts at -20°C until use.
PCR Amplification:
- Design primers targeting resistance-associated genes (kelch13 for artemisinin resistance).
- Perform PCR amplification with optimized thermal cycling conditions.
- Include positive and negative controls in each run.
Sequence Analysis:
- Purify PCR products using appropriate cleanup kits.
- Perform Sanger sequencing of amplified fragments.
- Analyze sequences for known resistance-conferring mutations.
- Submit novel mutations to public databases (e.g., NCBI).
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Research Reagent Solutions for Antimalarial Resistance Studies
| Reagent/Technology | Manufacturer/Provider | Function | Application in Resistance Research |
|---|---|---|---|
| Giemsa Stain | Sigma-Aldrich, Merck | Staining malaria parasites in blood smears | Visual identification of parasitic stages for morphological analysis |
| YOLOv5x Algorithm | Ultralytics | Object detection neural network | Automated detection of parasites in digital blood smear images |
| kelch13 Genotyping Primers | Integrated DNA Technologies | Amplification of resistance-associated genes | Molecular surveillance of artemisinin resistance markers |
| iMAGING Smartphone Application | Custom development | Integrated diagnostic platform | Field-based automated parasite detection and quantification |
| 7-Channel Input Tensor | Custom implementation | Enhanced feature extraction for CNNs | Improved species differentiation in thick blood smears |
| Automated Microscope System | Custom 3D-printed design | Robotized slide scanning | High-throughput image acquisition for AI analysis |
| 1H-1,2,4-triazol-4-amine | 1H-1,2,4-triazol-4-amine | Heterocyclic Building Block | High-purity 1H-1,2,4-triazol-4-amine for research. A key scaffold in medicinal & agrochemical synthesis. For Research Use Only. Not for human consumption. | Bench Chemicals |
| Isopromethazine | Isopromethazine, CAS:303-14-0, MF:C17H20N2S, MW:284.4 g/mol | Chemical Reagent | Bench Chemicals |
Regulatory and Implementation Considerations
The U.S. Food and Drug Administration (FDA) has recognized the increasing use of AI throughout the drug product life cycle, with the Center for Drug Evaluation and Research (CDER) observing a significant increase in drug application submissions using AI components [5]. The FDA has published draft guidance titled "Considerations for the Use of Artificial Intelligence to Support Regulatory Decision Making for Drug and Biological Products" to provide recommendations on the use of AI in producing information intended to support regulatory decision-making regarding drug safety, effectiveness, and quality [5].
For successful implementation of AI-based parasite detection systems in resource-limited settings, several factors must be addressed: image resolution requirements for accurate diagnosis, optical attachment and adaptation to conventional microscopy, sufficient fields-of-view for representative sampling, and the need for focused images with Z-stacks [4]. Systems must function reliably without continuous internet connectivity and be powerable by portable solar batteries to ensure utility in remote endemic areas.
The growing threat of antimalarial and antiparasitic drug resistance demands innovative approaches that leverage artificial intelligence for enhanced surveillance and diagnosis. The integration of convolutional neural networks with automated imaging systems provides a powerful toolset for detecting resistant parasites and monitoring their spread. As resistance patterns continue to evolve, these AI-driven technologies will play an increasingly vital role in preserving the efficacy of existing treatments and guiding the deployment of next-generation antimalarial therapies.
Limitations of Traditional Microscopy and Manual Drug Discovery Processes
Traditional microscopy and manual processes have long been the foundation of parasitic disease research and drug discovery. However, these approaches present significant limitations in sensitivity, throughput, and objectivity that impede research efficiency and therapeutic development. This application note details these limitations through quantitative analysis, examines their impact on drug discovery pipelines, and presents emerging methodologies that address these constraints through automation, artificial intelligence, and advanced imaging technologies. The integration of these innovative approaches offers a pathway to more efficient, reproducible, and impactful research in parasitology and pharmaceutical development.
For decades, conventional microscopy has served as the primary tool for parasite identification and morphological analysis in both clinical diagnostics and basic research. Similarly, manual observation and assessment have formed the cornerstone of early drug discovery workflows. However, the persistence of parasitic diseases as major global health challenges—with soil-transmitted helminths alone affecting over 600 million people worldwide [6]—underscores the urgent need to overcome methodological limitations in research and development processes.
The high failure rate in clinical drug development, estimated at approximately 90% for candidates that reach clinical trials [7], further emphasizes the insufficiency of traditional approaches. A significant proportion of these failures (40-50%) stem from lack of clinical efficacy [7], often reflecting inadequate target validation or compound optimization during preclinical stages where traditional microscopy plays a central role. Within this context, understanding the specific constraints of established methodologies becomes essential for advancing both parasitic disease research and therapeutic development.
Quantitative Limitations of Traditional Approaches
The constraints of traditional microscopy and manual processes can be quantified across multiple dimensions, from diagnostic accuracy to operational efficiency. The following tables summarize key performance gaps between conventional and emerging approaches.
Table 1: Comparative Diagnostic Performance for Soil-Transmitted Helminths (n=704 samples) [6]
| Parasite Species | Manual Microscopy Sensitivity | Expert-Verified AI Sensitivity | Sensitivity Improvement |
|---|---|---|---|
| Hookworm | 78% | 92% | +14% |
| T. trichiura | 31% | 94% | +63% |
| A. lumbricoides | 50% | 100% | +50% |
Table 2: Impact of Methodological Limitations on Drug Discovery Outcomes [8] [7] [9]
| Limitation Category | Quantitative Impact | Consequence in Drug Discovery |
|---|---|---|
| Low throughput | Limited to 10-100 samples per day per technician | Protracts screening of compound libraries |
| Subjectivity in analysis | High inter-observer variability (reported >30% in parasitology) | Inconsistent compound prioritization |
| Limited spatial resolution | ~200 nm resolution limit due to light diffraction [10] | Inability to visualize subcellular drug localization |
| Artifact susceptibility | 10-15% of data potentially compromised by preparation artifacts | Misleading efficacy or toxicity readouts |
Specific Limitations in Research and Development Contexts
Diagnostic and Research Sensitivity Constraints
Conventional microscopy exhibits particularly poor performance in detecting low-intensity infections, as evidenced by the dramatically low sensitivity for T. trichiura (31%) and A. lumbricoides (50%) shown in Table 1 [6]. This limitation has profound implications for both clinical management and research endpoints, as light infections may go undetected while still contributing to disease transmission and morbidity. The inability to reliably identify partial treatment effects or emerging resistance patterns during drug development represents a significant obstacle to developing effective antiparasitic therapies.
Throughput and Efficiency Limitations
Manual microscopy is inherently time-consuming and resource-intensive, requiring specialized expertise that may be unavailable in many settings [6]. In drug discovery contexts, traditional high-throughput screening (HTS) approaches often focus on single-target identification that fails to capture complex phenotypic responses [8]. This limitation is particularly problematic for traditional Chinese medicine research and other natural product studies where compounds may exert effects through multiple synergistic pathways [8]. The manual nature of conventional analysis creates substantial bottlenecks, with one study noting that experts must typically analyze more than 100 fields-of-view to identify parasite eggs in low-intensity infections [6].
Resolution and Subcellular Analysis Constraints
The diffraction limit of conventional optical microscopy (approximately 200 nm) [10] prevents detailed observation of drug localization and effects at subcellular levels. This is particularly problematic as more than one-third of drug targets are located within specific subcellular compartments [10]. Without the ability to visualize drug distribution within organelles such as mitochondria, lysosomes, or specific nuclear targets, researchers cannot fully understand pharmacokinetic and pharmacodynamic relationships at therapeutically relevant scales.
Figure 1: Resolution limitations in traditional microscopy compared to super-resolution techniques that enable subcellular drug tracking.
Data Management and Collaboration Challenges
Modern drug discovery generates massive, complex datasets that traditional approaches struggle to manage effectively. Research organizations often face challenges with siloed and disorganized data stored across multiple locations with inconsistent naming conventions and quality control processes [11]. The petabyte-scale datasets generated by advanced imaging technologies create substantial computational demands that conventional infrastructure cannot efficiently support [11]. Furthermore, collaboration barriers emerge when teams attempt to share sensitive biomedical data while maintaining regulatory compliance across distributed research networks [11].
Emerging Solutions and Methodologies
High-Content Screening Technologies
High-content screening (HCS) represents a paradigm shift from traditional microscopy by combining automated fluorescence microscopy with computational image analysis to simultaneously track multiple cellular parameters [8] [9]. This approach enables multiparametric analysis of cellular morphology, subcellular localization, and physiological changes across thousands of individual cells in a single experiment [8]. By implementing HCS, researchers can move beyond single-target assessment to evaluate complex phenotypic responses to potential therapeutics, thereby generating more physiologically relevant data early in the drug discovery pipeline.
Figure 2: High-content screening workflow enabling multiparametric cellular analysis for drug discovery.
Artificial Intelligence and Machine Learning Integration
AI-supported microscopy represents a transformative approach to overcoming the limitations of manual image analysis. Deep learning algorithms, particularly convolutional neural networks (CNNs), can be trained on large datasets of parasite images to achieve remarkable accuracy in identification and classification [12] [6]. The expert-verified AI approach, which combines algorithmic pre-screening with human confirmation, has demonstrated superior sensitivity for all major soil-transmitted helminth species while reducing expert analysis time to less than one minute per sample [6]. In drug discovery contexts, AI models have been successfully deployed for predictive toxicology assessments, such as deep learning detection of cardiotoxicity in human iPSC-derived cardiomyocytes [9].
Advanced Imaging Modalities
Super-resolution microscopy (SRM) techniques break the diffraction limit of conventional light microscopy, enabling researchers to visualize drug dynamics at nanoscale resolutions (20-50 nm) [10]. Key SRM methodologies include:
- STED (Stimulated Emission Depletion) microscopy: Uses two laser beams to achieve nanoscale resolution through point scanning [10]
- STORM/PALM (Single-Molecule Localization Microscopy): Achieves super-resolution by sequentially activating and localizing individual fluorophores [10]
- SIM (Structured Illumination Microscopy): Enhances resolution through structured light patterns and computational reconstruction [10]
These technologies enable subcellular pharmacokinetic studies by tracking drug localization and distribution within specific organelles, providing critical insights into therapeutic mechanisms and potential toxicity [10].
Integrated Data Management Platforms
Modern research informatics platforms address data management challenges through automated curation workflows, centralized data repositories, and scalable computational infrastructure [11]. These systems support comprehensive provenance tracking that maintains audit trails for regulatory compliance while enabling efficient collaboration across distributed research teams [11]. By implementing structured data management architectures, organizations can transform disorganized imaging data into query-ready assets suitable for machine learning and advanced analytics [11].
Experimental Protocols
Protocol: Expert-Verified AI Microscopy for Parasite Detection
This protocol details the methodology for AI-supported digital microscopy of intestinal parasitic infections, adapted from von Bahr et al. [6].
Research Reagent Solutions
Table 3: Essential reagents and materials for AI-supported parasite detection
| Item | Specification | Function |
|---|---|---|
| Portable whole-slide scanner | Must be compatible with brightfield imaging | Sample digitization for analysis |
| Kato-Katz staining reagents | Standard parasitology staining solution | Visual enhancement of parasite eggs |
| AI classification software | CNN-based algorithm trained on parasite image datasets | Automated detection and preliminary classification |
| Expert verification interface | Web-based or standalone application | Human confirmation of AI findings |
Step-by-Step Procedure
Sample Preparation
- Prepare fecal smears using standard Kato-Katz technique
- Allow slides to clear for 30-60 minutes at room temperature
- Ensure smear thickness permits visualization but maintains clarity
Slide Digitization
- Load prepared slides into portable whole-slide scanner
- Digitize entire smear at 40x magnification
- Export images in standardized format (TIFF recommended)
AI Analysis
- Process digitized images through pre-trained CNN algorithm
- Generate preliminary classifications of potential parasite eggs
- Flag regions of interest for expert verification
Expert Verification
- Review AI-identified objects through verification interface
- Confirm or correct classifications based on morphological expertise
- Finalize diagnosis based on verified findings
Data Management
- Archive original images and analysis results
- Document any discrepancies between AI and expert assessments
- Update AI training sets based on verified corrections
Technical Notes
- Total processing time: approximately 15 minutes per sample
- Expert hands-on time: less than 1 minute per sample
- Optimal for processing batches of 20-40 samples per session
- Sensitivity improvements most pronounced for low-intensity infections
Protocol: High-Content Screening for Compound Efficacy Assessment
This protocol outlines the application of high-content screening for evaluating anti-parasitic compounds, adapted from HCS methodologies in drug discovery [8] [9].
Research Reagent Solutions
Table 4: Essential reagents for high-content screening in parasitology
| Item | Specification | Function |
|---|---|---|
| Cell painting dyes | 6-fluorophore combination (e.g., Mitotracker, Phalloidin, DAPI) | Multiplexed staining of cellular structures |
| Automated imaging system | Confocal or widefield HCS microscope with environmental control | High-throughput image acquisition |
| Image analysis software | CellProfiler or commercial equivalent | Automated feature extraction and analysis |
| 3D culture matrix | Matrigel or synthetic alternative | Support for physiologically relevant models |
Step-by-Step Procedure
Model System Preparation
- Culture parasite-infected cell lines or 3D host-parasite models
- Seed cells into 96-well or 384-well HCS-optimized plates
- Allow models to establish for 24-48 hours before treatment
Compound Treatment
- Prepare compound libraries in DMSO with concentration gradients
- Treat models with test compounds for predetermined exposure periods
- Include appropriate controls (vehicle, positive, negative)
Multiplexed Staining
- Fix samples with paraformaldehyde (4% for 15 minutes)
- Permeabilize with Triton X-100 (0.1% for 10 minutes)
- Apply cell painting dye cocktail according to established protocols
- Incubate for specified durations with appropriate washing
Automated Imaging
- Program HCS system for multi-site acquisition
- Capture 9-16 fields per well at 20x or 40x magnification
- Include multiple fluorescence channels corresponding to dyes
- For 3D models, implement z-stack acquisition (15-30 slices)
Image Analysis and Feature Extraction
- Run CellProfiler pipeline for cell segmentation and feature extraction
- Quantify morphological parameters (size, shape, intensity, texture)
- Apply machine learning algorithms for phenotypic classification
- Generate compound efficacy scores based on multiparametric assessment
Technical Notes
- Optimal staining concentrations require empirical determination for each parasite system
- 3D models provide greater physiological relevance but increase computational demands
- Multiparametric analysis enables detection of subtle phenotypes missed by single-endpoint assays
- Recommended to include mechanism-of-action reference compounds for comparison
Traditional microscopy and manual drug discovery processes present significant limitations in sensitivity, throughput, resolution, and data management that impede progress in parasitic disease research and therapeutic development. Quantitative assessments demonstrate substantial gaps in diagnostic performance, particularly for low-intensity infections, while the high failure rate of clinical drug candidates underscores the insufficiency of conventional approaches for predicting therapeutic efficacy.
The integration of advanced technologies—including high-content screening, artificial intelligence, super-resolution microscopy, and structured data management platforms—offers a transformative pathway forward. These methodologies enable multiparametric analysis at unprecedented scales and resolutions, providing more physiologically relevant data earlier in the research pipeline. By adopting these innovative approaches, researchers can overcome the constraints of traditional methods, potentially accelerating the development of more effective treatments for parasitic diseases that continue to affect vulnerable populations globally.
Application Note: AI-Powered Diagnostic Platforms for Parasitology
The integration of artificial intelligence (AI) into clinical parasitology is transforming diagnostic workflows by enhancing the speed, accuracy, and accessibility of parasite detection. This application note details how AI, particularly deep learning models, is being deployed to analyze medical images for parasitic infections, directly supporting research and drug development efforts.
AI for High-Throughput Stool Sample Analysis
Background & Drivers: Traditional diagnosis of intestinal parasites via microscopic examination of stool samples is a time-consuming process requiring highly trained specialists. This creates a market driver for solutions that increase laboratory efficiency and diagnostic throughput without compromising accuracy [13].
Quantitative Performance of an AI Diagnostic Tool:
| Metric | Performance Result | Comparative Note |
|---|---|---|
| Positive Agreement | 98.6% [13] | After discrepancy analysis between AI and manual review. |
| Additional Organisms Detected | 169 [13] | Organisms previously missed in manual reviews. |
| Clinical Sensitivity | Improved [13] | Better likelihood of detecting pathogenic parasites. |
| Dataset Size (Training/Validation) | >4,000 samples [13] | Included 27 parasite classes from global sources. |
Key Technology: A deep-learning model based on a Convolutional Neural Network (CNN) was developed to detect protozoan and helminth parasites in concentrated wet mounts of stool. This system automates the identification of telltale cysts, eggs, or larvae [13].
Smartphone Microscopy for Field-Based Parasite Detection
Background & Drivers: In resource-constrained settings endemic for neglected tropical diseases like Chagas disease, the scarcity of skilled microscopists and advanced laboratory equipment creates a critical need for portable, easy-to-use, and low-cost diagnostic tools [14].
Performance of a Smartphone-Integrated AI System for T. cruzi Detection:
| Metric | Performance Result | Model & Dataset Details |
|---|---|---|
| Precision | 86% [14] | SSD-MobileNetV2 on human sample images. |
| Recall (Sensitivity) | 87% [14] | SSD-MobileNetV2 on human sample images. |
| F1-Score | 86.5% [14] | SSD-MobileNetV2 on human sample images. |
| Human Dataset | 478 images from 20 samples [14] | Included thick/thin blood smears and cerebrospinal fluid. |
Key Technology: The system employs lightweight AI models like SSD-MobileNetV2 and YOLOv8, which are optimized for real-time analysis on a smartphone. The phone is attached to a standard light microscope using a 3D-printed adapter, creating a portable digital imaging system [14].
AI-Assisted Image Segmentation for Research Workflows
Background & Drivers: In clinical and research settings, annotating regions of interest in medical images (segmentation) is a foundational but immensely time-consuming first step. This creates a driver for tools that accelerate this process without requiring machine-learning expertise from the user [15].
Key Technology: Systems like MultiverSeg use an interactive AI model that allows a researcher to segment new biomedical imaging datasets by providing a few initial clicks or scribbles on images. The model uses these interactions and a context set of previously segmented images to predict the segmentation for new images, dramatically reducing the manual effort required [15].
Experimental Protocols
Protocol 1: Implementing a CNN for Stool Parasite Detection
This protocol outlines the methodology for developing and validating a deep-learning model for automated parasite detection in stool wet mounts, based on the approach pioneered by ARUP Laboratories [13].
Sample Collection & Preparation:
- Gather a large and diverse set of parasite-positive stool samples. The dataset should encompass a wide range of parasite species (e.g., the study used 27 classes) and be sourced from different geographical regions to ensure robustness [13].
- Prepare concentrated wet mounts from the samples according to standard laboratory procedures.
Image Acquisition & Dataset Curation:
- Digitize the wet mounts using a microscope with a digital camera to create a high-resolution image dataset.
- Expert parasitologists manually review and annotate each image, marking the location and species of each parasite. This curated dataset serves as the "ground truth" for training.
Model Training & Validation:
- Architecture Selection: Employ a Convolutional Neural Network (CNN) architecture, which is particularly effective for image recognition tasks [13].
- Training: Train the CNN on the annotated image dataset. The model learns to associate specific visual features with the presence of different parasites.
- Validation: Validate the trained model's performance on a separate, held-out set of images not seen during training. Key metrics include clinical sensitivity, specificity, and positive agreement with expert manual review.
Protocol 2: Real-TimeTrypanosoma cruziDetection with Smartphone Microscopy
This protocol details the procedure for using a smartphone-based AI system to detect T. cruzi trypomastigotes in blood smears, suitable for field use in endemic areas [14].
Equipment Setup:
- Attach a smartphone to the ocular of a standard light microscope using a 3D-printed adapter.
- Ensure the smartphone camera is properly aligned to capture a clear and well-illuminated image of the sample.
Sample Preparation & Staining:
- Prepare thin or thick blood smears from a fresh blood sample on a glass slide.
- Stain the smear (e.g., with Giemsa) to enhance the contrast and visibility of parasites.
Image Acquisition & AI Analysis:
- Place the prepared slide on the microscope stage.
- Using a custom application on the smartphone, capture images of the smear.
- The onboard AI model (e.g., SSD-MobileNetV2 or YOLOv8) processes the image in real-time, identifying and flagging potential T. cruzi trypomastigotes.
Result Interpretation:
- The application displays the analysis results, indicating the detected parasites. A researcher can use this for rapid screening and quantification of parasitemia.
Protocol 3: Rapid Dataset Segmentation with MultiverSeg
This protocol describes how to use an interactive AI tool to quickly segment a new set of biomedical images for research purposes, such as quantifying parasites in histological sections [15].
Initialization:
- Load the MultiverSeg tool and upload the first image from your dataset.
Interactive Segmentation:
- Provide initial user interactions on the image, such as clicks, scribbles, or boxes, to mark the areas of interest (e.g., a parasite).
- The model uses these inputs to predict a segmentation mask for the entire image.
Iterative Refinement & Context Building:
- If the prediction is imperfect, provide additional interactions to correct it. The model updates its prediction in real-time.
- Once satisfied, save the segmented image. This image is automatically added to the model's "context set."
Automated Segmentation of Subsequent Images:
- Upload the next image in the dataset. The model will now use the growing context set of previously segmented images to make a more accurate prediction, requiring fewer user interactions.
- After segmenting several images, the model may achieve high accuracy with minimal or zero input, allowing for rapid batch processing of the entire dataset.
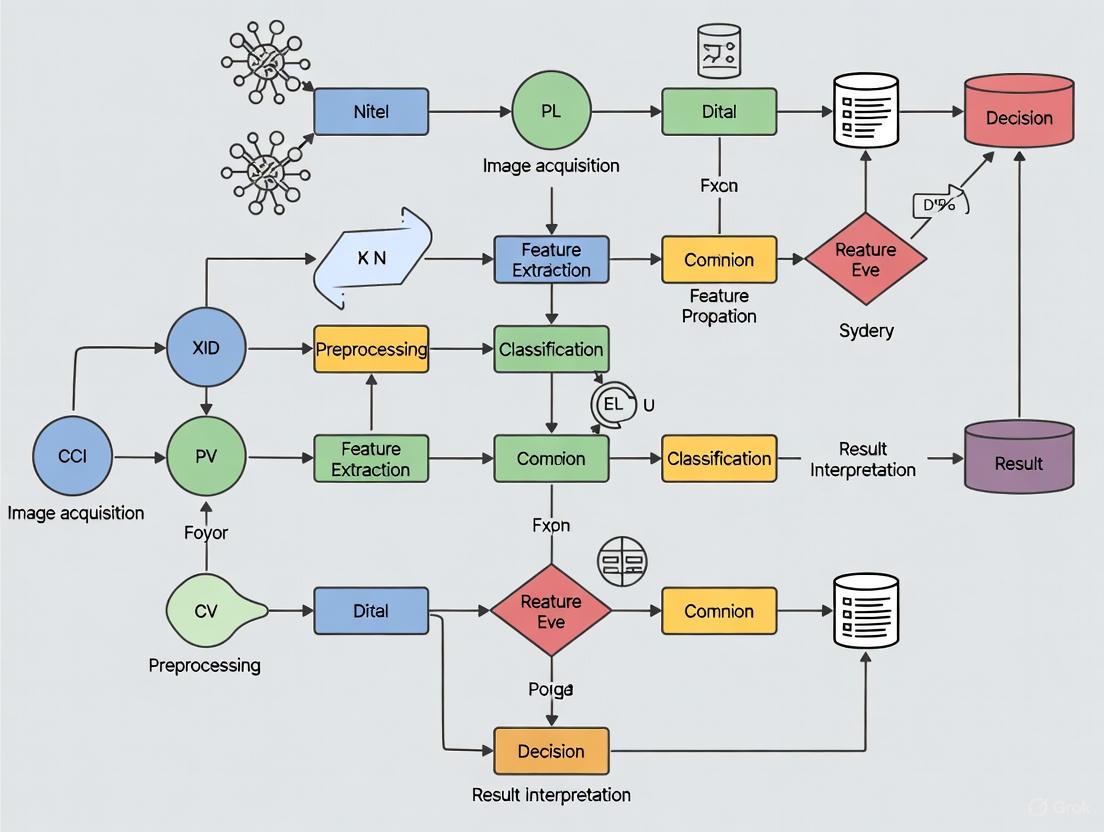
Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function in AI-Based Parasite Research |
|---|---|
| Stool Preservation Kits | Maintains parasite integrity for accurate image acquisition and AI model training [13]. |
| Giemsa & Other Stains | Enhances visual contrast in blood smears and other samples, improving AI detection accuracy [14]. |
| 3D-Printed Microscope Adapters | Enables standardized smartphone attachment for consistent field imaging [14]. |
| Annotated Image Datasets | Serves as the "ground truth" for training and validating AI models; a critical research reagent [13] [14]. |
| Pre-trained AI Models (e.g., YOLOv8, U-Net) | Accelerates development by providing a starting point for custom model training (transfer learning) [14]. |
| Cloud AI Platforms (e.g., Google AI Platform) | Provides computational resources and tools for building, training, and deploying custom medical imaging AI models [16]. |
| Periandrin V | Periandrin V, CAS:152464-84-1, MF:C41H62O14, MW:778.9 g/mol |
| Olean-12-en-3-one | Olean-12-en-3-one|CAS 638-97-1|β-Amyrone |
The application of artificial intelligence (AI) in parasite image analysis represents a transformative advancement for parasitology research and tropical disease management. AI technologies, particularly deep learning and computer vision, are addressing critical diagnostic challenges across diverse parasitic diseases, including malaria, intestinal parasites, and neglected tropical diseases (NTDs). These tools demonstrate remarkable capability in analyzing microscopic images, rapid diagnostic tests (RDTs), and mosquito surveillance photographs with accuracy comparable to human experts [17] [18]. The integration of AI into parasitology research pipelines is accelerating diagnostics, enhancing surveillance capabilities, and creating new opportunities for drug discovery, particularly crucial given the stalled progress in global malaria control and the persistent burden of NTDs [17] [19].
This protocol collection provides detailed methodological frameworks for implementing AI-driven image analysis across key parasitology applications. By standardizing these approaches, we aim to enhance reproducibility, facilitate technology transfer between research groups, and ultimately contribute to improved disease management through more accessible, efficient, and accurate diagnostic solutions.
Experimental Protocols and Workflows
Protocol: AI-Assisted Malaria Detection from Blood Smear Images
Principle: This protocol describes a standardized methodology for developing and validating deep learning models to detect Plasmodium parasites in thin blood smear images, achieving diagnostic accuracy exceeding 96% [18].
Materials:
- Giemsa-stained thin blood smear slides
- Microscope with digital camera or whole slide scanner
- Computing workstation with GPU acceleration (minimum 8GB VRAM)
- Python 3.8+ with TensorFlow/PyTorch frameworks
- Publicly available dataset of 27,558 blood smear images [18]
Procedure:
- Image Acquisition: Capture high-resolution (≥1024×1024 pixels) digital images of blood smear fields at 100× magnification under standardized lighting conditions.
- Data Preprocessing:
- Apply color normalization to minimize staining variation
- Partition dataset into training (70%), validation (15%), and test (15%) sets
- Implement data augmentation (rotation, flipping, brightness adjustment) to increase dataset diversity
- Model Development:
- Implement transfer learning using pretrained architectures (ResNet-50, VGG16, DenseNet-201)
- Extract deep features from multiple architectures
- Apply principal component analysis for dimensionality reduction
- Implement hybrid classifier combining support vector machine and long short-term memory networks
- Model Validation:
- Evaluate performance using 5-fold cross-validation
- Assess accuracy, sensitivity, specificity, precision, and F1-score
- Compare model predictions against expert microscopist readings
- Explainability Analysis:
- Implement Grad-CAM and LIME techniques to visualize discriminatory regions
- Generate heatmaps highlighting features contributing to classification decisions
Technical Notes: For optimal performance, ensure class balance between infected and uninfected cells. The stacked LSTM with attention mechanism has demonstrated superior performance (99.12% accuracy) [20]. Model interpretability is enhanced through explainable AI techniques, crucial for clinical adoption.
Protocol: AI-Powered Rapid Diagnostic Test Interpretation
Principle: This protocol outlines the deployment of an AI-powered Connected Diagnostics (ConnDx) system for standardized interpretation of malaria RDTs, enabling real-time surveillance in resource-limited settings [17].
Materials:
- Standard malaria RDTs (Paracheck Pf, BIOLINE Malaria Ag Pf, CareStart Malaria)
- Smartphone with HealthPulse application
- Cloud computing infrastructure
- Database system for result aggregation
Procedure:
- RDT Imaging:
- Capture RDT image using smartphone camera 15-20 minutes after test administration
- Ensure adequate lighting and minimal glare
- Position test cassette centrally in frame with all components visible
- AI Interpretation Pipeline:
- Object Detection: Locate RDT and identify brand/type
- Line Detection: Identify test and control lines within result window
- Classification: Determine probability of line presence in each region
- Quality Assurance: Flag adverse conditions (improper lighting, invalid tests)
- Result Validation:
- Compare AI interpretation against expert panel consensus
- Calculate weighted F1 score and Cohen's Kappa for agreement
- Monitor performance across different facilities and users
- Data Integration:
- Upload results to cloud-based dashboard
- Aggregate data for real-time epidemiological surveillance
- Generate automated alerts for positive cases
Technical Notes: The AI model demonstrated 96.4% concordance with expert panel interpretation, with sensitivity of 96.1% and specificity of 98.0% [17]. Regular retraining with field-collected images improves robustness to real-world variations.
Protocol: Mosquito Surveillance Using Citizen Science and AI
Principle: This protocol combines citizen science and AI image recognition to enhance vector surveillance, enabling early detection of invasive malaria mosquito species through community-generated photographs [21].
Materials:
- NASA GLOBE Observer mobile application or equivalent
- AI algorithms trained on authenticated mosquito images
- Database for geotagged mosquito observations
- Reference collection of mosquito species for algorithm training
Procedure:
- Citizen Data Collection:
- Train community members in mosquito larva and adult photography
- Capture images of mosquitoes in breeding sites (e.g., water containers, tires)
- Record GPS coordinates and timestamp for all observations
- Image Analysis:
- Upload images to cloud-based analysis platform
- Implement convolutional neural networks for species identification
- Apply larval identification algorithms with >99% confidence threshold
- Compare against reference database of Anopheles stephensi and related species
- Validation and Response:
- Verify AI identifications through expert entomologist review
- Map detected invasive species for targeted vector control
- Correlate detections with malaria case reports
- Technology Transfer:
- Develop AI-enabled smart traps for autonomous surveillance
- Implement early warning systems for invasive species detection
Technical Notes: This approach successfully identified the first specimen of invasive Anopheles stephensi in Madagascar through a single citizen-submitted photograph, enabling rapid public health response [21].
Performance Metrics and Comparative Analysis
Table 1: Performance Comparison of AI Models for Malaria Detection
| Model Architecture | Accuracy (%) | Sensitivity (%) | Specificity (%) | F1-Score | Application |
|---|---|---|---|---|---|
| Multi-model ensemble with majority voting [18] | 96.47 | 96.03 | 96.90 | 0.9645 | Blood smear analysis |
| Stacked LSTM with attention mechanism [20] | 99.12 | 99.10 | 99.13 | 0.9911 | Blood smear analysis |
| AI-powered RDT interpretation [17] | 96.40 | 96.10 | 98.00 | 0.9750 | Rapid diagnostic tests |
| CNN-based larval identification [21] | >99.00 | N/R | N/R | N/R | Mosquito surveillance |
Table 2: AI Model Performance Across Different Parasite Detection Applications
| Performance Metric | Blood Smear Analysis | RDT Interpretation | Mosquito Surveillance | Drug Discovery |
|---|---|---|---|---|
| Sample Throughput | High (batch processing) | Very high (real-time) | Moderate (image acquisition) | High (automated screening) |
| Equipment Cost | High (microscope + scanner) | Low (smartphone) | Variable (field deployment) | Very high (HTS systems) |
| Technical Expertise Required | High (both parasitology and AI) | Low (minimal training) | Moderate (field collection + AI) | Very high (specialized) |
| Explanability | Moderate (XAI techniques available) | High (direct line detection) | Moderate (species features) | Variable (model-dependent) |
| Regulatory Status | Research use primarily | CE-marked/ FDA-cleared emerging | Research phase | Early development |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Computational Tools for AI-Based Parasite Image Analysis
| Category | Specific Reagents/Tools | Function/Application | Key Considerations |
|---|---|---|---|
| Biological Samples | Giemsa-stained blood smears | Model training and validation | Ensure species representation (P. falciparum, P. vivax) |
| Field-collected RDTs | Real-world algorithm testing | Include major brands (Paracheck, BIOLINE, CareStart) | |
| Mosquito specimen images | Vector surveillance algorithms | Cover different life stages (larvae, adults) | |
| Annotation Resources | Expert microscopist panels | Ground truth establishment | Inter-reader variability assessment crucial |
| Standardized annotation protocols | Consistent labeling across datasets | Follow community guidelines where available | |
| Computational Frameworks | TensorFlow/PyTorch | Deep learning model development | GPU acceleration essential for training |
| OpenCV | Image preprocessing and augmentation | Standardize across research sites | |
| Scikit-learn | Traditional machine learning components | Feature selection and dimensionality reduction | |
| Model Architectures | CNN architectures (ResNet, VGG) | Feature extraction from images | Transfer learning from ImageNet effective |
| Vision Transformers | Alternative approach for image analysis | Emerging application in medical imaging | |
| Ensemble methods | Performance enhancement | Combine multiple models for robustness | |
| Validation Tools | Cross-validation frameworks | Performance assessment | 5-fold or 10-fold recommended |
| Explainable AI libraries (Grad-CAM, LIME) | Model interpretability | Critical for clinical translation | |
| Statistical analysis packages | Significance testing | Assess differences between models | |
| Calcium pimelate | Calcium Pimelate|C7H10CaO4|Nucleating Agent | Calcium pimelate is a highly effective β-nucleating agent for polypropylene research, enhancing polymer toughness and thermal stability. For Research Use Only. Not for human consumption. | Bench Chemicals |
| 2,5-Diphenylfuran | 2,5-Diphenylfuran, CAS:955-83-9, MF:C16H12O, MW:220.26 g/mol | Chemical Reagent | Bench Chemicals |
Workflow Visualization
AI-Parasite Research Workflow
Malaria Detection Pipeline
These application notes and protocols demonstrate the significant potential of AI-based image analysis across diverse parasitology applications. The standardized methodologies presented here enable researchers to implement robust AI systems for parasite detection, species identification, and surveillance. As these technologies mature, key future directions include developing more explainable AI systems suitable for clinical adoption, creating multi-task models capable of detecting multiple parasite species from single images, and establishing standardized benchmarking datasets to facilitate cross-study comparisons. The integration of AI into parasitology research represents a paradigm shift with potential to significantly impact global efforts to control and eliminate parasitic diseases, particularly in resource-limited settings where diagnostic expertise may be limited. By providing these detailed protocols and performance benchmarks, we aim to accelerate the adoption and rigorous implementation of AI technologies throughout parasitology research and practice.
AI in Action: Core Technologies and Real-World Applications for Researchers
Deep Convolutional Neural Networks (CNNs) for Parasite Detection and Classification
Parasitic infections remain a significant global health challenge, particularly in tropical and subtropical regions, where they contribute to malnutrition, anemia, and increased susceptibility to other diseases [22]. Accurate and timely diagnosis is crucial for effective treatment and disease control. Traditional diagnostic methods, primarily microscopic examination of blood smears, though considered the gold standard, are labor-intensive, time-consuming, and rely heavily on the expertise of trained personnel, leading to potential human error and subjectivity [1] [22] [23].
The field of parasitic diagnosis is undergoing a transformation with the integration of artificial intelligence (AI). Deep learning, particularly Convolutional Neural Networks (CNNs), is revolutionizing parasite detection by automating the analysis of medical images with high accuracy [22]. These technologies offer promising solutions to overcome the limitations of traditional microscopy, providing tools capable of interpreting complex image data consistently and efficiently [1]. This document details the application, performance, and experimental protocols of deep CNN models within the broader context of AI-driven parasite image analysis, providing a resource for researchers and drug development professionals.
Performance of CNN Models in Parasite Detection
Recent research demonstrates that CNN-based models achieve exceptional performance in detecting and classifying parasites from microscopic images. The following table summarizes the quantitative results from several state-of-the-art studies, primarily focused on malaria detection, which serves as a key application area.
Table 1: Performance Metrics of Recent Deep Learning Models for Parasite Detection
| Model Name | Reported Accuracy | Precision | Recall | F1-Score | Key Innovation |
|---|---|---|---|---|---|
| CNN with 7-channel input [1] | 99.51% | 99.26% | 99.26% | 99.26% | Multi-channel input for enhanced feature extraction from thick smears |
| CNN-ViT Ensemble [24] | 99.64% | 99.23% | 99.75% | 99.51% | Hybrid model combining local (CNN) and global (ViT) feature learning |
| DANet [25] | 97.95% | - | - | 97.86% | Lightweight dilated attention network (~2.3M parameters) |
| Optimized CNN + Otsu [23] | 97.96% | - | - | - | Otsu thresholding for segmentation as a preprocessing step |
| BLGSNet [26] | 99.25% | - | - | - | Novel CNN with Batch Normalization, Layer Normalization, GELU & Swish |
These models represent a significant advancement beyond simple binary classification (infected vs. uninfected). For instance, the CNN model with a seven-channel input was specifically designed for multiclass classification, successfully distinguishing between Plasmodium falciparum, Plasmodium vivax, and uninfected white blood cells with species-specific accuracies of 99.3% and 98.29%, respectively [1]. Furthermore, a key research direction is the development of computationally efficient models like DANet, which achieves high accuracy with only 2.3 million parameters, making it suitable for deployment on edge devices like a Raspberry Pi 4 in resource-constrained settings [25].
Detailed Experimental Protocols
This section outlines the methodologies for two key experiments cited in this document, providing a reproducible framework for researchers.
Objective: To train a Convolutional Neural Network for the classification of cells into P. falciparum-infected, P. vivax-infected, and uninfected categories from thick blood smear images.
Workflow:
Methodology:
- Dataset: Use a dataset of 5,941 thick blood smear images, processed to obtain 190,399 individually labeled cell images [1].
- Data Splitting: Split the data into training (80%), validation (10%), and test (10%) sets.
- Image Preprocessing: Apply advanced preprocessing to create a seven-channel input tensor. This includes techniques like enhancing hidden features and applying the Canny Algorithm to enhanced RGB channels to extract richer features [1].
- Model Architecture: Implement a CNN with up to 10 principal layers. Incorporate fine-tuning techniques such as residual connections and dropout to improve stability and accuracy.
- Training Configuration:
- Batch Size: 256
- Epochs: 20
- Optimizer: Adam, with a learning rate of 0.0005
- Loss Function: Cross-entropy
- Evaluation: Assess the model on the test set using metrics like accuracy, precision, recall, specificity, and F1-score. Generate a confusion matrix to visualize performance per class.
- Validation: Perform a 5-fold cross-validation using the StratifiedKFold method from scikit-learn to ensure model robustness and generalizability [1].
Objective: To improve CNN classification accuracy by employing Otsu's thresholding as a preprocessing step to segment and highlight parasite-relevant regions in blood smear images.
Workflow:
Methodology:
- Dataset: Utilize a dataset of blood smear images (e.g., 43,400 images) and split it for training and testing (e.g., 70:30) [23].
- Preprocessing - Segmentation: Apply Otsu's thresholding method to each RGB image. This global thresholding technique automatically calculates an optimal threshold value to separate the image into foreground (potential parasite regions) and background, reducing noise and enhancing relevant morphological features [23].
- Model Training: Train a baseline CNN model (e.g., a 12-layer CNN) on both the original and the Otsu-segmented datasets.
- Performance Comparison: Compare the classification accuracy of the model trained on segmented images versus the one trained on raw images. The study reported an accuracy improvement from 95% to 97.96% using this method [23].
- Segmentation Validation: In the absence of pixel-wise ground truth annotations, validate the effectiveness of the Otsu segmentation through:
- Visual Inspection: Manually check if the segmented regions correspond to parasitic structures.
- Canny Edge Detection: Apply edge detection to highlight the contours of the segmented regions for qualitative assessment [23].
- Quantitative Metrics (if ground truth is available): Compute the Dice coefficient and Jaccard Index (IoU) by comparing Otsu-generated masks with manually annotated reference masks. The original study achieved a mean Dice coefficient of 0.848 [23].
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogues essential materials, datasets, and software tools used in the development of deep CNN models for parasite detection.
Table 2: Essential Research Materials and Tools for CNN-based Parasite Detection
| Item Name | Type | Function in Research | Example/Reference |
|---|---|---|---|
| Thick Blood Smear Images | Dataset | Confirms presence of parasites; source for cell-level image patches. | Chittagong Medical College Hospital dataset [1] |
| NIH Malaria Dataset | Benchmark Dataset | Public dataset for training and benchmarking models on infected vs. uninfected red blood cells. | 27,558 cell images [25] |
| Multi-class Parasite Dataset | Dataset | Enables development of models for classifying multiple parasite species. | Dataset with 8 categories (e.g., Plasmodium, Leishmania, Toxoplasma) [26] |
| Otsu's Thresholding Algorithm | Image Processing Algorithm | Preprocessing step to segment and isolate parasite regions, boosting CNN performance. | OpenCV, Scikit-image [23] |
| Adam Optimizer | Software Tool | Adaptive optimization algorithm for updating network weights during training. | Learning rate=0.0005 [1] |
| Cross-Entropy Loss | Software Tool | Loss function used for training classification models, in line with Maximum Likelihood Estimation. | Standard for classification tasks [1] [27] |
| SmartLid Blood DNA/RNA Kit | Wet-lab Reagent | Magnetic bead-based nucleic acid extraction for molecular validation (e.g., LAMP, qPCR). | Used in sample prep for LAMP-based detection [28] |
| Colorimetric LAMP Assay | Wet-lab Reagent | Isothermal amplification for highly sensitive, field-deployable molecular confirmation of parasites. | Pan/Pf detection in capillary blood [28] |
| 2-Keto palmitic acid | 2-Keto Palmitic Acid|High-Purity Research Chemical | 2-Keto palmitic acid is a key metabolite for research into fatty acid synthesis and oxidation. This product is for research use only and not for human consumption. | Bench Chemicals |
| Apocynoside II | Apocynoside II||Research Use Only | Apocynoside II is a natural product compound for research use only. It is strictly for laboratory applications and not for human or veterinary use. | Bench Chemicals |
This case study explores the transformative impact of artificial intelligence (AI) in the field of parasitology, focusing on the automated analysis of stool wet mounts and blood smears. Traditional microscopic examination of these specimens remains the gold standard for diagnosing parasitic infections but is hampered by its manual, labor-intensive nature, subjectivity, and reliance on highly skilled personnel [29] [30]. In high-income countries, the low prevalence of parasites in submitted specimens leads to technologist fatigue and potential diagnostic errors, while resource-limited settings often lack the necessary expertise altogether [30]. AI technologies, particularly deep learning and convolutional neural networks (CNNs), are overcoming these barriers by providing rapid, accurate, and scalable diagnostic solutions. This document details the quantitative performance, experimental protocols, and key reagents driving this technological shift, providing a resource for researchers and drug development professionals engaged in AI-based parasitology research.
AI-Powered Stool Wet Mount Analysis
Performance and Validation
The implementation of AI for stool wet mount analysis demonstrates performance metrics that meet or exceed manual microscopy. A comprehensive clinical validation of a deep CNN model for enteric parasite detection reported high sensitivity and specificity, with performance further improving after a review process [29].
Table 1: Performance Metrics of an AI Model for Wet Mount Parasite Detection [29]
| Validation Metric | Initial Agreement | Post-Discrepant Resolution Agreement |
|---|---|---|
| Positive Agreement | 250/265 (94.3%) | 472/477 (98.6%) |
| Negative Agreement | 94/100 (94.0%) | Variable by organism (91.8% to 100%) |
| Additional Detections | 169 organisms not initially identified by manual microscopy | - |
Furthermore, a limit-of-detection study compared the AI model to three technologists with varying experience levels using serial dilutions of specimens containing Entamoeba, Ascaris, Trichuris, and hookworm. The AI model consistently detected more organisms at lower dilution levels than human reviewers, regardless of the technologist's experience [29]. This demonstrates the superior analytical sensitivity of AI and its potential to reduce false negatives.
Commercial AI systems, such as the Techcyte Fusion Parasitology Suite, are designed to integrate into clinical workflows. These systems can identify a broad range of parasites, including protozoan cysts and trophozoites, helminth eggs, and larvae [31]. In validation studies, such platforms have demonstrated the ability to reduce the average read time for negative slides to 15–30 seconds, allowing technologists to focus their expertise on positive or complex cases [31].
Experimental Protocol for AI-Based Wet Mount Analysis
The following protocol outlines a standard workflow for AI-assisted stool wet mount analysis, as implemented in clinical laboratories [31] [30].
Step 1: Specimen Preparation and Slide Creation
- Concentration: Process the stool specimen using a fecal concentration device (e.g., Apacor Mini or Midi Parasep) to concentrate parasitic elements.
- Slide Preparation: Create a thin monolayer of the concentrated stool on a glass slide. This is critical for optimal digital scanning, as thick preparations can obscure objects.
- Staining and Mounting: Apply a specialized mounting media, such as a wet mount iodine solution, to enhance the visibility of parasites and extend slide life. Permanently affix the coverslip using a fast-drying mounting medium to prevent movement during scanning [31] [30].
Step 2: Digital Slide Scanning
- Scanner Setup: Load the prepared slides into a compatible high-throughput digital slide scanner (e.g., Hamamatsu S360, Grundium Ocus 40).
- Image Acquisition: Initiate the scanning process. The scanner will automatically capture high-resolution digital images (typically at 40x magnification, producing 80x equivalent digital images) of the entire slide and upload them to the AI platform for analysis [31].
Step 3: AI Image Processing and Analysis
- AI Analysis: The platform's AI algorithm, typically a convolutional neural network (CNN), processes the digital images to detect, classify, and count objects of interest.
- Object Classification: The algorithm compares image features against its trained model to identify and propose classifications for parasites, grouping them by class (e.g., Giardia cysts, Trichuris eggs) and sorting them by confidence level [31] [29].
Step 4: Technologist Review and Result Reporting
- Review Interface: The technologist logs into the AI platform and reviews the AI-proposed objects of interest, which are presented in a gallery view grouped by classification.
- Confirmation and Reporting: The technologist confirms, rejects, or reclassifies the AI's findings. Positive samples are typically confirmed by manual re-inspection under a microscope. The final result is then reported into the Laboratory Information System (LIS) [31] [30].
AI-Powered Blood Smear Analysis for Parasites
Performance and Advanced Techniques
In blood smear analysis, AI is primarily applied to detect blood-borne parasites like malaria. Advanced deep learning models have been developed not only for detection but also for segmenting infected cells and classifying parasite developmental stages, which is crucial for drug development and pathogenicity studies [32] [33].
Table 2: Performance of Advanced AI Models in Blood Parasite Detection
| AI Model / Application | Key Performance Metric | Significance |
|---|---|---|
| YOLO Convolutional Block Attention Module (YCBAM) for Pinworm [34] | mAP@0.5: 0.9950, Precision: 0.9971, Recall: 0.9934 | Demonstrates high accuracy for detecting small parasitic objects in complex backgrounds. |
| Cellpose for P. falciparum Segmentation [32] | Average Precision (AP@0.5) up to 0.95 for infected erythrocytes | Enables continuous single-cell tracking and analysis of dynamic processes throughout the 48-hour parasite lifecycle. |
| Proprietary Algorithm for Malaria Stage Classification [33] | Accurate classification into rings, trophozoites, and schizonts; discrimination of viable vs. dead parasites. | Facilitates high-content drug screening by providing detailed phenotyping of drug effects. |
These models leverage sophisticated architectures. The YCBAM model, for instance, integrates YOLO with self-attention mechanisms and a Convolutional Block Attention Module (CBAM) to focus on spatially relevant features of pinworm eggs, significantly boosting detection accuracy in noisy microscopic images [34]. For live-cell imaging, workflows combine label-free differential interference contrast (DIC) and fluorescence imaging with pre-trained deep-learning algorithms like Cellpose for automated 3D cell segmentation, allowing for the time-resolved analysis of processes such as protein export in Plasmodium falciparum [32].
Experimental Protocol for AI-Based Blood Smear Analysis
This protocol details a workflow for AI-driven analysis of blood smears, from preparation to the review of results, incorporating both diagnostic and research applications.
Step 1: Blood Smear Preparation and Staining
- Smear Creation: Prepare a thin blood smear on a glass slide using standard techniques to ensure an even monolayer of blood cells.
- Staining: Apply the appropriate stain (e.g., Giemsa for malaria). For advanced research applications involving live parasites, a complex staining solution may be used, including:
- A fluorescent RBC stain (e.g., wheat germ agglutinin-AlexaFluor488).
- A nuclear stain (e.g., DAPI).
- A viability stain for active mitochondria (e.g., Mitotracker Red CMXRos) [33].
Step 2: Image Acquisition
- Diagnostic Setting: Scan the slide using a supported digital scanner. In veterinary medicine, for example, systems like Vetscan Imagyst allow for automated scanning and upload to an AI analysis platform [35].
- Research Setting (High-Content Screening): Use an automated imaging platform (e.g., Operetta) to acquire multiple high-resolution image fields from multi-well plates, often using a 40x objective lens. For 3D analysis, an Airyscan microscope can be used to capture z-stacks [32] [33].
Step 3: AI Detection, Segmentation, and Classification
- Cell Detection: The AI algorithm first identifies and counts all red blood cells, separating clustered cells.
- Parasite Detection: It then detects parasitized cells based on the presence of stained parasite nuclei (DAPI) and/or mitochondrial signals (Mitotracker) [33].
- Stage Classification (Research): For malaria, the algorithm classifies the parasite's life cycle stage (ring, trophozoite, schizont) based on morphological features like nucleus number and size. It can also discriminate between viable and dead parasites based on mitochondrial activity [33].
- Segmentation (Research): Using models like Cellpose, the algorithm segments individual erythrocytes and delineates the parasite compartment within infected cells, enabling detailed spatial and temporal analysis [32].
Step 4: Result Review and Data Analysis
- Diagnostic Reporting: The technologist or veterinarian reviews the AI-generated report, which includes classified images of suspected parasites, and confirms the findings before reporting [35].
- Research Data Extraction: The analyzed data is aggregated to compute key metrics such as parasitemia, life cycle stage distribution, and viability counts for drug efficacy studies (e.g., EC50 determination) [33].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogues essential materials and digital tools used in AI-powered parasitology research, as cited in the referenced studies.
Table 3: Essential Research Reagents and Digital Tools for AI-Powered Parasitology
| Item | Function/Application | Example Use Case |
|---|---|---|
| Apacor Parasep [31] [30] | Fecal concentration device for preparing clean, standardized stool samples for slide preparation. | Used in the Techcyte workflow to prepare specimens for wet mount and trichrome-stained slides. |
| Techcyte AI Platform [31] [30] | A cloud-based AI software that analyzes digitized slides for ova, cysts, parasites, and other diagnostically significant objects. | Used for assisted screening in clinical parasitology, presenting pre-classified objects for technologist review. |
| Hamamatsu NanoZoomer Scanner [30] | High-throughput digital slide scanner for creating whole-slide images from glass microscope slides. | Digitizes trichrome-stained stool smears at 40x for subsequent AI analysis. |
| Cellpose [32] | A pre-trained, deep-learning-based algorithm for 2D and 3D cell segmentation. | Adapted and re-trained to segment P. falciparum-infected erythrocytes in 3D image stacks for dynamic process tracking. |
| Operetta Imaging System [33] | Automated high-content screening microscope for acquiring high-resolution images from multi-well plates. | Used in drug screening assays to image thousands of fluorescently stained malaria parasites. |
| YOLO-CBAM Architecture [34] | An object detection model (YOLO) enhanced with a Convolutional Block Attention Module for improved focus on small objects. | Developed for the highly precise detection of pinworm eggs in noisy microscopic images. |
| DAPI & Mitotracker Stains [33] | Fluorescent dyes for staining parasite nuclei and active mitochondria, respectively. | Enables algorithm discrimination between living and dead malaria parasites in viability and drug screening assays. |
| 7-Bromohept-3-ene | 7-Bromohept-3-ene|CAS 79837-80-2|Research Chemical | 7-Bromohept-3-ene is a versatile synthetic intermediate for organic synthesis. This compound is for research use only and is not intended for human or veterinary use. |
| T140 peptide | T140 Peptide | T140 peptide is a potent CXCR4 antagonist for HIV and cancer metastasis research. For Research Use Only. Not for human use. |
The integration of AI into the analysis of stool wet mounts and blood smears represents a paradigm shift in parasitology. The data and protocols presented in this case study demonstrate that AI-powered systems offer significant advantages over traditional microscopy, including enhanced sensitivity, superior throughput, standardized interpretation, and the ability to extract complex phenotypic data for research. These technologies not only address long-standing challenges in clinical diagnostics, such as technologist burnout and diagnostic variability, but also open new avenues for scientific discovery by enabling continuous, single-cell analysis of dynamic parasitic processes. As these AI tools continue to evolve and become more accessible, they hold the promise of revolutionizing both routine parasite screening and the foundational research that underpins drug development.
The integration of Artificial Intelligence (AI), particularly generative AI and machine learning, with High-Throughput Screening (HTS) is revolutionizing the early stages of drug discovery. This synergy creates an iterative, data-driven cycle that significantly accelerates the identification and optimization of novel therapeutic compounds. By leveraging AI to analyze complex datasets, researchers can now prioritize compounds with a higher probability of success for experimental validation, thereby reducing the traditionally high costs and long timelines associated with drug development [36].
Within parasitology research, these technological advances hold particular promise. AI-powered microscopy and image analysis are emerging as powerful tools for identifying parasitic organisms and elucidating their complex life cycles [37]. The application of AI in this field addresses significant challenges in data integration, from various model organisms to clinical research data, paving the way for new diagnostic tools and therapeutic strategies aligned with One Health principles [37].
This document provides detailed protocols for implementing an AI-assisted HTS platform, with a specific focus on its application in MoA analysis for parasitology. It includes a validated case study on kinase targets, a comprehensive table of key performance metrics, essential reagent solutions, and visualized workflows to guide researchers in adopting these transformative methodologies.
Quantitative Performance Metrics of AI in Drug Discovery
The table below summarizes key quantitative findings from recent studies and reports on the impact of AI in drug discovery and related scientific fields.
Table 1: Key Performance Metrics of AI in Scientific Discovery
| Metric Area | Specific Metric | Performance Result / Finding | Context / Source |
|---|---|---|---|
| Drug Discovery Efficiency | Hit-to-lead cycle time reduction | 65% reduction | Integrated Generative AI & HTS platform [36] |
| Drug Discovery Output | Identification of novel chemotypes | Achieved nanomolar potency | Targeting kinases and GPCRs [36] |
| Organizational AI Maturity | Organizations scaling AI | ~33% of organizations | McKinsey Global Survey 2025 [38] |
| AI High Performers | EBIT impact from AI (≥5%) | ~6% of organizations | McKinsey Global Survey 2025 [38] |
| AI in Material Science | Candidate molecules identified | 48 promising candidates | AI-assisted HTS for battery electrolytes [39] |
| AI in Material Science | Novel additives validated | 2 (Cyanoacetamide & Hydantoin) | From 75,024 screened molecules [39] |
Integrated AI-HTS Experimental Protocol
This protocol details the procedure for establishing a synergistic cycle between generative AI and high-throughput screening to accelerate hit identification and MoA analysis.
Phase 1: Computational Design & Prioritization
Objective: To generate and virtually screen novel chemical entities optimized for specific biological targets.
Materials & Software:
- Hardware: High-performance computing (HPC) cluster or cloud-based GPU servers.
- Software: Generative AI software (e.g., for molecular design), Graph Neural Network (GNN) libraries (e.g., PyTor Geometric, DGL), molecular docking software.
- Data: Curated molecular libraries with associated biological activity data (e.g., ChEMBL, PubChem), target protein structure files (e.g., from PDB).
Procedure:
- Model Training: Train a generative AI model (e.g., a variational autoencoder or generative adversarial network) on a curated library of known molecules and their bioactivity data against the target of interest (e.g., a parasitic enzyme) [36].
- Molecular Generation: Use the trained model to generate a large library of novel molecular structures (e.g., 100,000+ compounds) optimized for desired properties like target binding affinity, solubility, and synthetic accessibility.
- High-Throughput Virtual Screening: Employ a GNN or other machine learning model to analyze the generated library based on key properties. This protocol can be adapted from a battery study where 75,024 molecules were screened based on adsorption energy, redox potential, and solubility [39]. In a drug discovery context, relevant properties include:
- Predicted binding affinity (e.g., pKi, pIC50)
- ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) properties
- Structural novelty versus known chemical libraries
- Hit Selection: Rank the molecules based on the multi-parameter analysis and select a shortlist (e.g., 48-500 compounds) for experimental synthesis and testing [36] [39].
Phase 2: Experimental Validation & HTS
Objective: To synthesize and biologically test the AI-prioritized compounds in a high-throughput manner.
Materials:
- Automated Liquid Handlers: (e.g., Tecan Veya, SPT Labtech firefly+ for miniaturized assays) [40].
- Microplate Readers: For detecting optical signals (fluorescence, luminescence, absorbance).
- Assay Reagents: Cell lines, recombinant proteins, substrates, and detection kits.
- AI-Prioritized Compounds: The shortlist of compounds from Phase 1.
Procedure:
- Synthesis: Synthesize or procure the shortlisted AI-generated compounds.
- Assay Development: Configure a target-based (e.g., enzyme inhibition) or phenotypic assay (e.g., parasite viability) in a microplate format compatible with automation.
- Automated Screening: Use liquid handling robots to dispense compounds, cells/enzmyes, and reagents into assay plates. The focus should be on robustness and reproducibility to generate high-quality data for the AI model [40].
- Data Acquisition: Read plates using appropriate detectors to generate primary activity data (e.g., % inhibition, IC50 values).
Phase 3: MoA Analysis via AI-Powered Image Analysis
Objective: To elucidate the Mode of Action of confirmed hits using high-content imaging and AI-driven analysis.
Materials:
- High-Content Imaging System: Automated microscope capable of high-throughput multiplexed imaging.
- Staining Reagents: Antibodies for specific cellular targets, fluorescent dyes for organelles, and viability indicators.
- AI Software: Image analysis platforms with deep learning capabilities (e.g., Sonrai Discovery, open-source tools like CellProfiler with TensorFlow integration) [40].
Procedure:
- Cell Treatment & Staining: Treat relevant cell models (e.g., infected host cells) with confirmed hit compounds and appropriate controls. Fix and stain cells with multiplexed biomarker panels.
- High-Content Imaging: Automatically acquire thousands of high-resolution images across multiple channels for each treatment condition.
- AI-Based Image Segmentation & Classification:
- Train a deep learning model (e.g., a U-Net architecture) to accurately segment individual cells and sub-cellular structures. This approach is directly applicable to parasitology, as demonstrated in studies of Apicomplexan and Kinetoplastid groups [37].
- Extract hundreds of morphological features (e.g., texture, shape, intensity) from the segmented cells to create a quantitative "phenotypic fingerprint" for each treatment.
- MoA Prediction: Use the multivariate phenotypic profiles to cluster compounds with similar effects. Compare the profiles of novel hits to those of compounds with known MoAs to generate hypotheses about the underlying biological mechanisms of the hits [37] [41].
Phase 4: Iterative AI Model Refinement
Objective: To use experimental results to improve the predictive accuracy of the generative AI model.
Procedure:
- Data Integration: Feed the experimental HTS data and MoA analysis results back into the generative AI model from Phase 1 [36].
- Model Retraining: Retrain the AI model on this expanded and validated dataset. This iterative feedback loop continuously refines the model's understanding of structure-activity and structure-phenotype relationships, enhancing its ability to propose ever-more promising compounds in subsequent cycles.
Workflow Visualization
The following diagram illustrates the integrated, cyclical workflow described in the protocols.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for AI-HTS Workflows
| Item | Function / Application |
|---|---|
| Automated Liquid Handlers (e.g., Tecan Veya, SPT Labtech firefly+) | Enable precise, high-speed dispensing of compounds, cells, and reagents in miniaturized assay formats, ensuring reproducibility for AI model training [40]. |
| 3D Cell Culture Platforms (e.g., mo:re MO:BOT) | Provide biologically relevant, human-derived tissue models (e.g., organoids) for more predictive efficacy and toxicity screening, automatable for HTS [40]. |
| Graph Neural Networks (GNNs) | A class of AI models ideal for analyzing graph-structured data like molecules, enabling high-throughput prediction of properties like adsorption energy and solubility [39]. |
| Trusted Research Environment (TRE) | A secure data platform (e.g., Sonrai Discovery) that integrates multi-modal data (imaging, omics, clinical) with transparent AI pipelines to generate verifiable biological insights [40]. |
| AI-Powered Microscopy Software | Utilizes deep learning for automated, high-accuracy segmentation and classification of parasitic organisms in images, crucial for parasitology MoA studies [37]. |
| Privacy-Enhancing Technologies (PETs) | Techniques like federated learning allow multiple institutions to collaboratively train AI models on sensitive data (e.g., clinical records) without sharing the raw data itself [42]. |
| 2,4'-Dinitrobiphenyl | 2,4'-Dinitrobiphenyl, CAS:606-81-5, MF:C12H8N2O4, MW:244.2 g/mol |
| Aminobutanal | 4-Aminobutanal|Chemical Reagent|RUO |
Case Study: Validated AI-HTS Workflow
A proof-of-concept study demonstrates the efficacy of integrating generative AI with HTS. Researchers targeted kinase and G-protein-coupled receptor (GPCR) families, which are also relevant in parasitology.
- Method: A generative AI model was trained on existing molecular libraries and proposed novel chemical entities. These were synthesized and evaluated through HTS assays. The resulting data was fed back to refine the AI model iteratively [36].
- Result: This integrated platform achieved a 65% reduction in hit-to-lead cycle time and successfully identified novel chemotypes with nanomolar potency that were not present in existing chemical libraries [36]. This validates the protocol as a powerful strategy for accelerating the discovery of new therapeutic agents.
Workflow Visualization for Parasite Image Analysis
The following diagram details the specific AI-powered image analysis workflow for parasitology, as outlined in Phase 3 of the protocol.
The emergence and spread of partial resistance to artemisinin and partner drugs poses a significant threat to global malaria control and elimination efforts [43]. This challenge has created a pressing need for the development of new therapies with novel mechanisms of action (MoAs) that can circumvent existing resistance mechanisms [43]. In response, innovative platforms combining advanced image analysis and machine learning pattern recognition are revolutionizing antimalarial drug discovery. These approaches leverage Cell Painting assays and artificial intelligence (AI) to accelerate the identification and characterization of potential antimalarial compounds, transforming traditional discovery pipelines [43] [44].
This protocol details the application of Cell Painting and AI-powered image analysis within the context of malaria research, providing a framework for researchers to implement these cutting-edge technologies. By capturing broad morphological changes in parasite cells, these methods enable rapid insight into a compound's biological impact and mode of action, significantly shortening the early discovery timeline [43].
Cell Painting Assay Fundamentals
Cell Painting is a high-content, multiplexed staining assay that uses up to six fluorescent dyes to mark major organelles and cellular components, providing a comprehensive view of cellular morphology and phenotypic state [44]. The assay is designed to be a low-cost, single assay capable of capturing numerous biologically relevant phenotypes with high throughput.
The standard Cell Painting protocol employs the following dyes to visualize key cellular structures:
- Hoechst 33342: Stains DNA in the nucleus
- Concanavalin A: Labels the endoplasmic reticulum
- SYTO 14: Highlights nucleoli and cytoplasmic RNA
- Phalloidin: Targets f-actin filaments
- Wheat Germ Agglutinin (WGA): Marks Golgi apparatus and plasma membrane
- Mito Tracker Deep Red: Visualizes mitochondria [44]
When adapted for malaria research, this assay is applied to parasite-infected red blood cells (RBCs) to visualize morphological changes induced by compound treatments [43].
AI-Powered Image Analysis and Pattern Recognition
The integration of machine learning, particularly deep learning models, enables automated analysis of the rich morphological data generated by Cell Painting [43] [44]. These AI algorithms perform pattern recognition on stained parasite cell images to understand a compound's biological impact through a process analogous to cell painting [43]. The models extract thousands of morphological features from each cell, capturing information about size, shape, texture, and intensity, which collectively form a morphological profile for each treatment condition [44].
Platforms like the one developed through the partnership between MMV, LPIXEL, and the University of Dundee package these AI models into cloud-based, user-friendly applications, allowing researchers to analyze images without specialized AI expertise [43]. This democratizes access to advanced analytical capabilities and accelerates discovery timelines by providing insights into how a compound works much earlier in the research process [43].
Table 1: Key Components of the AI-Powered Cell Painting Platform
| Component | Description | Application in Antimalarial Discovery |
|---|---|---|
| Multiplexed Staining | Uses 6 fluorescent dyes to mark 8 cellular components | Reveals parasite cell morphological changes upon compound treatment |
| Automated Imaging | High-throughput microscopy systems | Enables screening of thousands of compounds against parasite cultures |
| Feature Extraction | Machine learning algorithms extract morphological features | Quantifies changes in size, shape, texture, and intensity in parasite cells |
| Morphological Profiling | Creates high-dimensional datasets from extracted features | Identifies patterns correlating with specific mechanisms of action |
| Cloud-Based Analysis | User-friendly applications for image analysis | Allows researchers without AI expertise to leverage advanced pattern recognition |
Experimental Protocol
Cell Painting for Malaria Parasites
This protocol outlines the steps for implementing Cell Painting with Plasmodium falciparum-infected red blood cells to screen for novel antimalarials. The following workflow diagram illustrates the complete experimental process:
Materials and Reagents
Table 2: Research Reagent Solutions for Malaria Cell Painting
| Reagent/Category | Specific Examples & Functions | Application Notes |
|---|---|---|
| Parasite Strains | P. falciparum 3D7 (CQ-sensitive), K1 (CQ-resistant), CamWT-C580Y(+) (ART-resistant) [45] | Use multiple strains to identify compounds effective against resistant parasites |
| Cell Culture Reagents | RPMI 1640 medium, Albumax I, Hypoxanthine, Gentamicin, Sodium bicarbonate [45] | Maintains parasite viability during screening |
| Staining Dyes | Hoechst 33342, Concanavalin A, SYTO 14, Phalloidin, WGA, MitoTracker Deep Red [44] | Standard Cell Painting cocktail adapted for parasite-infected RBCs |
| Fixation Solution | 4% Paraformaldehyde in PBS [45] | Preserves cellular morphology while maintaining fluorescence |
| Compound Library | 9,547 small molecules including FDA-approved compounds [45] | Diversity enhances discovery of novel chemotypes |
Step-by-Step Procedure
Parasite Culture and Synchronization
- Culture Plasmodium falciparum parasites (including drug-sensitive and resistant strains) in O+ human RBCs using complete RPMI 1640 medium supplemented with 0.5% Albumax I, 100 µM hypoxanthine, and 12.5 µg/mL gentamicin [45].
- Maintain cultures at 37°C in a mixed gas environment (1% O₂, 5% CO₂ in N₂).
- Double-synchronize parasites at the ring stage using 5% sorbitol treatment and allow to develop through one complete cycle before screening [45].
Compound Treatment
- Prepare compound library in DMSO as stock solutions and store at -20°C.
- Transfer compounds to 384-well plates using liquid handling systems.
- Dilute compounds in PBS to achieve final testing concentrations ranging from 10 µM to 20 nM (using 1 in 2 serial dilutions) with a final DMSO concentration not exceeding 1% [45].
- Dispense synchronized parasite cultures into compound-treated plates at 1% schizont-stage parasites and 2% hematocrit.
- Incubate plates for 72 hours under standard malaria culture conditions.
Cell Staining and Fixation
- After incubation, dilute assay plates to 0.02% hematocrit in PhenolPlate 384-well ULA-coated microplates.
- Prepare staining solution containing 1 µg/mL wheat germ agglutinin-Alexa Fluor 488 conjugate and 0.625 µg/mL Hoechst 33342 in 4% paraformaldehyde [45].
- Add complete Cell Painting stain cocktail according to established protocols [44]:
- Hoechst 33342 for DNA
- Concanavalin A for endoplasmic reticulum
- SYTO 14 for nucleoli and cytoplasmic RNA
- Phalloidin for F-actin
- Wheat germ agglutinin for Golgi and plasma membrane
- MitoTracker Deep Red for mitochondria
- Incubate stained plates for 20 minutes at room temperature before image acquisition.
Image Acquisition
- Acquire nine microscopy image fields from each well using high-content imaging systems such as Operetta CLS with a 40× water immersion lens.
- Use appropriate filter sets for each fluorescent dye.
- Set image resolution to 0.299 µm pixel size, 16 bits per pixel, and 1080 × 1080 pixels [45].
- Transfer acquired images to analysis software such as Columbus for processing.
AI Image Analysis Protocol
Workflow for Pattern Recognition and MoA Prediction
The following diagram illustrates the AI analysis workflow for predicting mechanisms of action from Cell Painting images:
Computational Analysis Steps
Image Processing and Feature Extraction
- Use image analysis software (e.g., CellProfiler, Columbus) to identify individual cells and segment cellular compartments [44].
- Extract morphological features for each cell, capturing data on size, shape, texture, intensity, and spatial relationships of cellular structures.
- Generate a high-dimensional feature vector for each cell, typically encompassing over 1,000 distinct morphological measurements [44].
Data Normalization and Quality Control
- Apply quality control metrics to remove poor-quality images or segmentation artifacts.
- Normalize morphological profiles against reference and control compounds to account for plate-to-plate variability.
- Implement batch effect correction algorithms to ensure comparability across different screening runs.
Pattern Recognition and MoA Prediction
- Apply machine learning pattern recognition models to identify similarities in morphological profiles between tested compounds and reference compounds with known mechanisms of action [43].
- Use unsupervised learning approaches (e.g., clustering, dimensionality reduction) to group compounds with similar morphological impacts.
- Compare morphological profiles to annotated databases of compound effects to predict mechanisms of action for novel compounds.
- Prioritize compounds that cluster separately from existing antimalarials, suggesting novel mechanisms of action not subject to existing resistance mechanisms [43].
Hit Selection and Validation
- Select candidate compounds based on potent antimalarial activity (IC₅₀ < 1 µM), novel morphological profiles, and favorable preliminary safety parameters [45].
- Validate selected hits in secondary assays against drug-sensitive and resistant parasite strains.
- Confirm predicted mechanisms of action through orthogonal biochemical and cellular assays.
Data Analysis and Interpretation
Key Performance Metrics
Table 3: Quantitative Metrics for AI-Powered Cell Painting Screening
| Performance Category | Metric | Benchmark Values | Interpretation |
|---|---|---|---|
| Image Analysis | Features extracted per cell | 1000+ morphological features [44] | Comprehensive profiling of cellular morphology |
| Screening Capacity | Compounds screened per run | 9,547+ compounds in a single library [45] | Enables high-throughput discovery |
| Model Accuracy | MoA prediction accuracy | Saves months in traditional MoA determination [43] | Dramatically accelerates discovery timeline |
| Hit Identification | IC₅₀ cutoff for hits | < 1 µM against P. falciparum [45] | Identifies potent antimalarial compounds |
| Specificity | Activity against resistant strains | ICâ‚…â‚€ < 500 nM against ART-resistant strains [45] | Identifies compounds overcoming resistance |
Interpretation Guidelines
- Morphological Profile Clustering: Compounds with similar mechanisms of action typically cluster together in morphological space. Novel antimalarials may form distinct clusters separate from existing drug classes [44].
- Feature Importance Analysis: Identify which morphological features most strongly contribute to compound classification to gain biological insights into mechanism of action.
- Concentration Dependence: Evaluate how morphological changes vary with compound concentration. Specific phenotypes often manifest at sub-cytotoxic concentrations.
- Cross-Species Validation: Confirm activity in rodent malaria models (e.g., Plasmodium berghei) for promising candidates before advancing to further development [45].
Technical Notes and Troubleshooting
- Cell Line Selection: U2OS osteosarcoma cells are commonly used in Cell Painting due to their flat morphology and minimal overlap, but the protocol has been successfully adapted to dozens of cell lines without major adjustments [44].
- Assay Optimization: The JUMP-CP Consortium has developed an optimized Cell Painting protocol (v3) that quantitatively optimizes staining reagents, experimental conditions, and imaging parameters using a positive control plate of 90 compounds covering 47 diverse mechanisms of action [44].
- AI Model Accessibility: Cloud-based implementation of AI models makes the technology accessible to researchers without specialist AI knowledge, helping democratize this powerful approach [43].
- Data Sharing: Open-access availability of source code and guidance documentation enables broader adoption and validation across the research community [43].
This integrated platform of Cell Painting and AI-powered pattern recognition represents a transformative approach in the fight against malaria, accelerating the discovery of novel antimalarials with new mechanisms of action to address the growing threat of drug resistance.
The integration of artificial intelligence (AI) into parasitology represents a fundamental shift from reactive diagnosis to proactive outbreak management. While AI-powered microscopy has revolutionized parasite detection, the true transformative potential lies in applying predictive modeling to forecast parasite transmission dynamics and outbreak trajectories. These models analyze complex interactions between epidemiological data, environmental factors, and population demographics to enable public health officials to implement timely interventions, allocate resources efficiently, and mitigate disease spread before outbreaks escalate into widespread crises [12]. This application note details the protocols and analytical frameworks that leverage AI to advance predictive forecasting for parasitic diseases, providing researchers and public health professionals with practical methodologies to enhance outbreak preparedness.
AI-Powered Forecasting: Core Concepts and Data Requirements
Predictive AI modeling leverages machine learning algorithms to identify patterns and trends in historical and real-time data, generating forecasts about future disease incidence. For parasitic diseases, these models have demonstrated remarkable accuracy; one convolutional neural network (CNN) algorithm trained on 2013-2017 data for chikungunya, malaria, and dengue achieved 88% accuracy in predicting disease outbreaks [12]. Another geospatial AI approach integrated machine learning with Geographic Information Systems (GIS) to map cutaneous leishmaniasis risk, successfully identifying high-risk areas in Isfahan province [12].
The predictive capability of these models depends on the integration and quality of multiple data types, each contributing specific insights into transmission dynamics.
Table 1: Essential Data Types for Predictive Modeling of Parasitic Diseases
| Data Category | Specific Parameters | Modeling Application |
|---|---|---|
| Epidemiological Data | Historical case incidence, outbreak reports, seroprevalence studies | Establishes baseline transmission patterns and identifies emerging clusters |
| Environmental Data | Temperature, rainfall, humidity, vegetation indices | Predicts vector population dynamics and habitat suitability |
| Geospatial Data | Land use, elevation, water bodies, population density | Creates risk maps and identifies geographic hotspots |
| Demographic Data | Age structure, socioeconomic status, mobility patterns | Informs population susceptibility and potential outbreak scale |
| Climate Data | Long-term climate projections, extreme weather events | Enables long-range forecasting and climate change impact modeling |
Data Sourcing and Management Protocols
Effective predictive modeling requires systematic data collection and curation. The following protocols ensure data quality and usability:
- Epidemiological Data Compilation: Aggregate historical case data from national surveillance systems, hospital records, and published literature. Standardize case definitions across sources and address missing data through imputation techniques or spatial interpolation.
- Environmental and Geospatial Data Acquisition: Source satellite-derived environmental data from publicly available platforms (e.g., NASA's MODIS, USGS Landsat). Extract relevant parameters at appropriate spatial (e.g., 1km x 1km grid) and temporal (e.g., weekly, monthly) resolutions.
- Data Integration and Alignment: Spatially and temporally align all datasets using common geographic boundaries and time intervals. Create a unified data structure with consistent spatial units (e.g., district-level) and temporal frequency (e.g., weekly incidence) for model training.
Experimental Protocols for Predictive Model Development
This section provides detailed methodologies for developing and validating predictive models for parasitic disease transmission.
Protocol 1: Developing a Spatiotemporal Predictive Model for Mosquito-Borne Parasitic Diseases
Objective: To create a predictive model for mosquito-borne diseases (e.g., malaria, dengue) that forecasts outbreak risk at the district level with a 4-week lead time.
Materials and Computational Resources:
- Historical epidemiological data (confirmed cases, deaths) for a minimum of 5 years
- High-resolution climate data (temperature, rainfall, relative humidity)
- Geospatial data (digital elevation models, land use/cover maps)
- Statistical computing environment (R, Python)
- Machine learning libraries (scikit-learn, TensorFlow, PyTorch)
Methodology:
Data Preprocessing and Feature Engineering:
- Aggregate all data to a uniform spatial unit (e.g., district) and temporal resolution (e.g., weekly).
- Calculate rolling averages for climate variables (e.g., 4-week mean temperature) to capture delayed effects on transmission.
- Generate lagged variables for case incidence (1-4 weeks) to account for autocorrelation in time series data.
- Normalize all continuous variables to a common scale (e.g., z-scores) to improve model convergence.
Model Selection and Training:
- Implement multiple algorithm classes for comparative performance assessment:
- Negative Binomial Regression: Handles over-dispersed count data common in disease incidence reporting [46]
- Random Forest: Captures non-linear relationships and interaction effects between predictors
- Long Short-Term Memory (LSTM) Networks: Models complex temporal dependencies in incidence data
- Partition data into training (70%), validation (15%), and testing (15%) sets, maintaining temporal order.
- Train models using the training set and optimize hyperparameters via grid search with cross-validation on the validation set.
- Implement multiple algorithm classes for comparative performance assessment:
Model Validation and Performance Metrics:
- Evaluate model performance on the held-out test set using:
- Mean Squared Error (MSE): Quantifies overall prediction error magnitude
- Area Under ROC Curve (AUC): Assesses classification accuracy of outbreak vs. non-outbreak weeks
- Leave-One-Out Information Criterion (LOOIC): Compares model fit while penalizing complexity [46]
- Perform spatial cross-validation by withholding entire regions during training to assess geographic generalizability.
- Evaluate model performance on the held-out test set using:
The following workflow diagram illustrates the sequential stages of this predictive modeling protocol:
Protocol 2: Integrated Parasite Detection and Quantification for Model Validation
Objective: To implement automated parasite detection and load quantification for ground-truthing predictive models, using a smartphone-AI microscopy system.
Materials:
- Light microscope with standard magnification (100-1000x)
- Smartphone with high-resolution camera (12MP or greater)
- 3D-printed microscope adapter (compatible with smartphone and microscope)
- Stained blood smears (thin and thick) or stool samples, depending on parasite
- Computing device for model deployment (smartphone or tablet)
Methodology:
Sample Preparation and Imaging:
- Prepare samples according to standard diagnostic protocols (e.g., Giemsa-stained blood smears for malaria, Kato-Katz slides for helminths).
- Attach smartphone to microscope using the 3D-printed adapter, ensuring proper alignment with the ocular lens.
- Capture multiple images across different fields of view (minimum 20 per sample) at 400x and 1000x magnifications.
- Store images in a structured database with metadata (sample ID, date, location, staining method).
AI Model Deployment for Real-Time Analysis:
- Implement a lightweight convolutional neural network (CNN) architecture such as SSD-MobileNetV2 or YOLOv8 optimized for mobile deployment [14].
- For Trypanosoma cruzi detection, the system should achieve target performance metrics of >85% precision and recall [14].
- Process captured images through the AI algorithm in real-time, generating parasite counts and infection status.
Data Integration with Forecasting Models:
- Export quantitative parasite load data in standardized format (parasites/μL) with geographic and temporal stamps.
- Integrate with epidemiological databases to validate and refine outbreak prediction models.
- Use spatially-explicit parasite density maps to identify transmission hotspots for targeted interventions.
The integrated system for field-based parasite detection and data generation is depicted below:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Computational Tools for Predictive Parasitology
| Category/Item | Specifications | Research Application |
|---|---|---|
| AI-Assisted Microscopy | Smartphone adapter, mobile-optimized CNN models | Field-based parasite detection and quantification [14] |
| High-Content Imaging Systems | Automated microscopes, multi-well plate compatibility | High-throughput drug screening and parasite stage differentiation [47] |
| qPCR Assays | 18S rDNA targets, species-specific primers | Sensitive parasite detection and load quantification [48] |
| Geospatial Analysis Software | GIS platforms, remote sensing data processors | Environmental risk mapping and hotspot identification [12] |
| Machine Learning Frameworks | TensorFlow, PyTorch, scikit-learn | Developing and training predictive transmission models [12] |
| Data Visualization Tools | R Shiny, Python Dash, Tableau | Communicating forecast results to public health decision-makers [49] |
| Undeca-4,7-diyn-6-OL | Undeca-4,7-diyn-6-OL|High-Purity Building Block | Undeca-4,7-diyn-6-OL is a terminal diyne alcohol for organic synthesis and materials science research. For Research Use Only. Not for human or therapeutic use. |
Implementation Framework and Validation Metrics
Successful implementation of predictive modeling requires careful attention to model selection, validation approaches, and integration with public health decision-making processes.
Table 3: Performance Comparison of AI Models for Parasite Forecasting and Detection
| Model Type | Application | Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|
| Convolutional Neural Network | Outbreak prediction for dengue, chikungunya, malaria | 88% accuracy [12] | Processes complex spatiotemporal patterns | High computational requirements |
| Negative Binomial Regression | Mosquito-borne disease forecasting [46] | Compared using LOOIC, MSE [46] | Handles count data with overdispersion | Assumes linear relationships |
| SSD-MobileNetV2 | Trypanosoma cruzi detection in blood smears | 86.5% F1-score [14] | Mobile-optimized for field use | Lower accuracy on rare parasite forms |
| 18S qPCR | Plasmodium falciparum parasitemia quantification | Excellent agreement with microscopy (ICC 0.97) [48] | High sensitivity for low parasitemia | Requires laboratory infrastructure |
Validation Framework for Predictive Models
Robust validation is essential before deploying predictive models in public health practice. Implement a multi-faceted validation approach:
- Temporal Validation: Assess model performance by training on historical data and testing on the most recent outbreak season, evaluating the model's ability to predict genuinely future events.
- Spatial Validation: Validate models in geographically distinct regions from where training data was collected to ensure generalizability across different ecological and demographic contexts.
- Prospective Validation: Deploy models in real-time during ongoing transmission seasons and compare predictions with subsequently observed incidence rates.
Integration with Public Health Decision-Making
For predictive models to impact public health practice, they must be effectively integrated into decision-making workflows:
- Develop User-Friendly Dashboards: Create visualization platforms that translate model outputs into actionable risk categories (e.g., low, moderate, high outbreak risk) with clear uncertainty intervals.
- Establish Alert Thresholds: Define incidence thresholds that trigger specific public health actions (e.g., vector control intensification, community alert dissemination, healthcare resource mobilization).
- Implement Feedback Mechanisms: Create systems for field surveillance data to continuously refine and update model predictions, improving accuracy over time.
The integration of predictive AI modeling with traditional parasitology represents a paradigm shift in how researchers and public health professionals approach parasitic disease control. The protocols and frameworks presented in this application note provide a roadmap for developing, validating, and implementing these powerful tools. By combining advanced computational approaches with field-deployable diagnostic technologies, the scientific community can move beyond reactive diagnostics toward truly predictive outbreak management. This proactive approach holds particular promise for resource-limited settings where the burden of parasitic diseases is highest, potentially revolutionizing global efforts to control and eliminate these persistent health threats. As these technologies continue to evolve, interdisciplinary collaboration between parasitologists, data scientists, and public health practitioners will be essential to realize the full potential of predictive analytics in reducing the global burden of parasitic diseases.
Navigating the Hurdles: Technical Challenges and Data Optimization Strategies
Automated image analysis powered by artificial intelligence (AI) is revolutionizing parasite diagnostics and research, offering solutions to the critical challenges that have long plagued traditional microscopy. In resource-limited settings, diagnostic accuracy is frequently compromised by non-standardized conditions, leading to issues with poor lighting, occlusion from overlapping cells and debris, and scale variation across different imaging setups [50]. These barriers directly impact the reliability of parasite detection, species identification, and life-cycle stage classification, ultimately affecting patient treatment and disease management strategies [51] [12].
AI, particularly deep learning models, demonstrates remarkable capability in overcoming these barriers. These models can learn invariant representations from data, enabling robust performance despite image quality variations. This document provides detailed application notes and experimental protocols, framed within a broader thesis on AI for parasite image analysis, to equip researchers and drug development professionals with standardized methodologies for developing and validating robust AI-based diagnostic tools.
Quantitative Performance of AI Models in Parasite Image Analysis
The table below summarizes the performance of various AI models reported in recent literature, highlighting their effectiveness in different parasitic disease diagnostics.
Table 1: Performance Metrics of Deep Learning Models in Parasite Detection and Classification
| Parasite / Disease | AI Model | Key Performance Metrics | Reported Challenges Addressed | Source |
|---|---|---|---|---|
| Helminths (Ascaris & Taenia) | ConvNeXt Tiny | F1-Score: 98.6% | Subjectivity, low throughput of traditional microscopy | [52] |
| Helminths (Ascaris & Taenia) | EfficientNet V2 S | F1-Score: 97.5% | Subjectivity, low throughput of traditional microscopy | [52] |
| Helminths (Ascaris & Taenia) | MobileNet V3 S | F1-Score: 98.2% | Subjectivity, low throughput of traditional microscopy | [52] |
| Malaria (P. vivax) | Custom CNN + SVM | Parasite Detection F1-Score: 82.10%Stage Classification F1-Score: 85% (Trophozoites), 88% (Schizonts), 83% (Gametocytes) | Staining quality, lighting variations, overlapping cells in thick smears | [50] |
| Malaria (P. falciparum & P. vivax) | CNN (7-channel input) | Accuracy: 99.51%, Precision: 99.26%, Recall: 99.26%, F1-Score: 99.26% | Differentiating between Plasmodium species | [1] |
| Malaria | Hybrid CapNet | Accuracy: Up to 100% (Multiclass), Parameters: 1.35M, Computational Cost: 0.26 GFLOPs | High computational demands, limited generalizability across datasets | [51] |
Experimental Protocols for Addressing Image Analysis Barriers
Protocol 1: Comprehensive Image Preprocessing for Enhanced Feature Extraction
This protocol, adapted from malaria research, details a multi-channel input preprocessing strategy to improve model resilience to lighting and contrast variations [1].
1. Objective: To create an enriched input tensor that enhances feature visibility for the CNN, making it less sensitive to poor lighting and staining inconsistencies.
2. Materials:
- Original RGB microscopic image.
- Image processing library (e.g., OpenCV).
3. Methodology: a. Input the Base Image: Start with a standardized RGB image of a blood smear or parasite sample. b. Generate Enhanced Channels: Create four additional image channels: i. Contrast-Enhanced Channel: Apply Contrast Limited Adaptive Histogram Equalization (CLAHE) to the luminance channel (in LAB color space) of the original image. ii. Edge-Enhanced Channel: Apply the Canny edge detection algorithm to the grayscale version of the original image to highlight morphological boundaries. iii. Gradient Magnitude Channel: Compute the magnitude of the Sobel gradients in both x and y directions to emphasize texture and edges. c. Stack Channels: Combine the original 3 RGB channels with the 4 newly generated channels (contrast, edge, gradient) to form a 7-channel input tensor. d. Model Training: Train the CNN model using this 7-channel tensor instead of the standard 3-channel RGB image. This provides the model with pre-computed, robust features that are invariant to certain lighting conditions.
Protocol 2: A Lightweight Hybrid Architecture for Computational Efficiency
This protocol describes the implementation of a Hybrid Capsule Network (Hybrid CapNet), designed for high accuracy with low computational cost, suitable for mobile deployment in resource-limited settings [51].
1. Objective: To build a model that maintains high accuracy in detecting parasites and their life-cycle stages while being computationally efficient and robust to occlusions and pose variations.
2. Materials:
- Dataset of annotated parasite images (e.g., MP-IDB, IML-Malaria).
- Deep learning framework (e.g., TensorFlow, PyTorch).
3. Methodology: a. Feature Extraction: The input image is first passed through a series of Convolutional (Conv) layers to extract basic features like edges and textures. * Example: Two Conv layers with 32 and 64 filters, respectively, each followed by a ReLU activation and Batch Normalization. b. Primary Capsule Layer: The features are reshaped into "capsules," which are groups of neurons that encode both the probability of an entity's presence and its instantiation parameters (e.g., orientation, scale). c. Dynamic Routing: A dynamic routing algorithm is applied between capsule layers. This algorithm establishes agreements between lower-level and higher-level capsules, allowing the network to recognize whole objects from their parts and be robust to occlusions. d. Composite Loss Function: The model is trained using a composite loss function comprising: i. Margin Loss: Ensures correct classification of entities. ii. Reconstruction Loss: Uses a decoder network to reconstruct the input image from the capsule outputs, forcing the capsules to encode meaningful information. iii. Focal Loss: Helps address class imbalance by down-weighting the loss for well-classified examples. iv. Regression Loss: Improves spatial localization of the parasites. e. Evaluation: Evaluate the model on both intra-dataset and cross-dataset benchmarks to assess generalization.
Protocol 3: Integrated Workflow for Quality Assessment and Object Detection
This protocol outlines a holistic system for malaria smear analysis that integrates image quality checks with parasite and leukocyte detection, crucial for handling real-world, variable-quality images [50].
1. Objective: To automate the analysis of thick blood smears by first assessing image quality, then detecting and classifying parasites and leukocytes.
2. Materials:
- Romanowsky-stained thick blood smear images.
- Image processing and machine learning libraries (e.g., scikit-learn for SVM).
3. Methodology: a. Image Quality Assessment: i. Feature Extraction: Convert the image to HSV color space. Extract features including color histogram bins and texture features using the Gray Level Co-occurrence Matrix (GLCM). ii. Classification: Use a Support Vector Machine (SVM) classifier trained on these features to classify the image as having "Good" or "Poor" staining quality. Images with poor quality can be flagged for re-capture or manual review. b. Leukocyte (WBC) Detection: i. Segmentation: Apply OTSU thresholding and binary masking to isolate potential leukocytes. ii. Morphological Filtering: Use erosion to separate touching cells and remove small artifacts. iii. Identification: Apply the connected components algorithm to label and count the detected leukocytes. c. Parasite Detection & Stage Classification: i. Candidate Detection: Select high-intensity regions in the image and draw adaptive bounding boxes around potential parasites. ii. Classification: Use a custom Convolutional Neural Network (CNN) to classify each candidate into specific parasite stages (e.g., Trophozoites, Schizonts, Gametocytes).
Visualization of Workflows and System Architecture
AI-Powered Parasite Image Analysis Workflow
Hybrid Capsule Network (Hybrid CapNet) Architecture
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key materials and computational tools essential for replicating the experiments and building robust AI models for parasite image analysis.
Table 2: Key Research Reagents and Computational Tools for AI-based Parasite Analysis
| Item Name | Function / Application | Specification / Example | Source / Reference |
|---|---|---|---|
| Romanowsky Stain | Staining of blood smears for malaria parasite visualization; stable in humid climates. | Used for creating a dataset of 1000 thick smear images for Plasmodium vivax. | [50] |
| Zeiss Scope A1 Microscope | Image acquisition for building standardized datasets. | 100x magnification, calibrated light intensity (22.4 lux), 2452 × 2056 pixel resolution. | [50] |
| Hybrid CapNet Model | Lightweight architecture for parasite ID and stage classification on mobile devices. | 1.35M parameters, 0.26 GFLOPs, composite loss function. | [51] |
| Seven-Channel Input Tensor | Preprocessing technique to boost model resilience to lighting/contrast issues. | Input stack: 3 RGB + 1 Contrast + 1 Edge + 1 Gradient + 1 other enhanced channel. | [1] |
| Composite Loss Function | Training hybrid models for improved accuracy, spatial localization, and noise robustness. | Combines Margin, Focal, Reconstruction, and Regression losses. | [51] |
| Public Benchmark Datasets | For training and cross-dataset validation of models to ensure generalizability. | E.g., MP-IDB, IML-Malaria, Malaria-Detection-2019. | [51] |
The application of artificial intelligence (AI) in parasite image analysis represents a transformative advancement for global health, offering the potential to automate and scale diagnostics in resource-constrained regions. However, the real-world deployment of these models is critically threatened by two interconnected challenges: dataset bias and adversarial attacks [53]. Dataset bias arises from non-representative training data, leading to models that fail to generalize across diverse parasite strains, imaging protocols, and patient populations. Simultaneously, adversarial attacks deliberately exploit model vulnerabilities through manipulated inputs, potentially causing diagnostic misclassification [54] [55]. This document provides application notes and detailed experimental protocols to help researchers develop robust, secure, and reliable AI models for parasite image analysis, ensuring their efficacy in clinical and field settings.
Application Note: Understanding and Mitigating Dataset Bias
Dataset bias is a pervasive issue in biomedical AI, where models trained on limited or homogenous data perform poorly on images from different sources. In parasite diagnostics, this can manifest as failures when analyzing new species, life-cycle stages, or images acquired with different staining techniques or microscope models [51] [26].
Quantitative Analysis of Public Datasets for Parasite Image Analysis
A key step in mitigating bias is understanding the composition and limitations of available data. The table below summarizes several benchmark datasets used in parasite image analysis research.
Table 1: Summary of Publicly Available Parasite Image Datasets
| Dataset Name | Parasite Classes/Scope | Sample Size (Images) | Key Characteristics & Potential Biases |
|---|---|---|---|
| NIH Malaria Dataset [25] | Plasmodium spp. (infected vs. uninfected) | 27,558 | Large scale; potential bias in species prevalence and staining consistency. |
| Cell Image Dataset [26] | 8 classes (6 parasites, 2 blood cells) | 34,298 | Diverse parasite types; may have class imbalance and variable image quality. |
| MP-IDB, MP-IDB2, IML-Malaria, MD-2019 [51] | Plasmodium species and life-cycle stages | Not Specified | Multi-source; used for cross-dataset validation; variations in staining and imaging protocols are a key bias. |
| ARUP Laboratories Dataset [56] | 27 classes of intestinal parasites | >4,000 | Geographically diverse samples; includes rare species; reduces geographic bias. |
Protocol: Cross-Domain Validation and Bias Assessment
Objective: To evaluate model generalization and identify dataset-specific biases. Materials: Your trained model, at least two distinct datasets of parasite images (e.g., from different labs or geographic regions). Procedure:
- Data Curation: Partition each dataset into standardized training, validation, and test sets. Ensure no patient or sample overlap between sets.
- Intra-Dataset Evaluation: Train your model on the training split of Dataset A and evaluate its performance on the test split of Dataset A. Record standard metrics (Accuracy, F1-Score, AUC-PR).
- Cross-Dataset Evaluation: Using the same model trained on Dataset A, now evaluate its performance directly on the entire test set of Dataset B without any fine-tuning.
- Bias Metric Calculation: Calculate the performance drop between intra-dataset and cross-dataset evaluations. A significant drop (e.g., >10% in F1-score) indicates that the model has overfitted to biases present in Dataset A and fails to generalize to Dataset B.
- Visualization with Grad-CAM: Use Gradient-weighted Class Activation Mapping (Grad-CAM) on misclassified cross-dataset images to identify if the model is focusing on biologically irrelevant features (e.g., image artifacts, specific staining patterns) instead of actual parasite morphology [51] [25].
Diagram 1: Workflow for cross-domain validation and bias assessment.
Mitigation Strategies: Architectural and Data-Centric Solutions
To build models inherently more robust to bias, consider the following approaches:
- Lightweight, Domain-Specific Architectures: Instead of large, generic models, use leaner architectures designed for medical images. Models like Hybrid CapNet (1.35M parameters) and DANet (2.3M parameters) have demonstrated high accuracy with reduced computational cost, which can lessen overfitting and ease deployment [51] [25].
- Advanced Data Augmentation: Simulate domain shift by applying aggressive color jitter, Gaussian blur, and random noise to mimic variations in staining and image quality [26].
- Multi-Source Training: The most effective strategy is to train your model on a curated, multi-source dataset that encompasses the expected variability in the deployment environment (e.g., different scanners, stain brands, and protocols) [56].
Application Note: Defending Against Adversarial Attacks
Adversarial machine learning involves crafting inputs to fool models. In a diagnostic context, this could lead to missed infections or false alarms, with serious public health consequences [53]. Attacks are categorized by the attacker's goal (e.g., evasion, data poisoning) and knowledge (white-box vs. black-box) [54].
Taxonomy of Adversarial Threats
Table 2: Taxonomy of Adversarial Attacks Relevant to Parasite Diagnosis
| Attack Type | Attacker's Goal | Attacker's Knowledge | Potential Impact on Parasite Diagnosis |
|---|---|---|---|
| Evasion Attack(e.g., FGSM, PGD [57]) | Cause misclassification of a specific input. | White-box or Black-box | A malicious actor could subtly alter a digital smear image to cause an AI system to classify a parasite as "uninfected." |
| Data Poisoning [53] [55] | Corrupt the model during training by injecting malicious data. | Limited access to training pipeline. | A compromised data supplier could insert mislabeled images, creating a backdoor that causes the model to fail on specific trigger patterns. |
| Model Extraction [53] | Steal a proprietary model by querying its API. | Black-box (API access only). | Intellectual property theft of a high-performance diagnostic model, enabling unauthorized use or further analysis to craft evasion attacks. |
Protocol: Adversarial Robustness Testing and Training
Objective: To assess model vulnerability to evasion attacks and improve its resilience through adversarial training. Materials: A trained model, test set of parasite images, an adversarial attack library (e.g., ART, Foolbox). Procedure:
- Baseline Performance: Establish the model's clean accuracy on the unmodified test set.
- Generate Adversarial Examples: Using a white-box attack like Projected Gradient Descent (PGD), generate adversarial versions of the test set images. PGD is an iterative attack that finds a small perturbation
δto maximize the model's loss, constrained by a maximum perturbation budgetε[57]. - Evaluate Robust Accuracy: Test the model on the adversarial examples. The drop in accuracy quantifies its current vulnerability.
- Adversarial Training: Retrain the model from scratch on a mixture of clean data and adversarial examples generated on-the-fly during each training epoch. This teaches the model to ignore small, malicious perturbations [57].
- Re-evaluate: After training, re-run the evaluation from steps 1 and 3 on the new model. The robust accuracy (performance on adversarial examples) should significantly improve, with minimal loss in clean accuracy.
Diagram 2: Adversarial robustness testing and training protocol.
Protocol: Defense against Data Poisoning
Objective: To detect and mitigate backdoor attacks during the data collection and model training phases. Procedure:
- Data Provenance and Validation: Maintain strict chain-of-custody records for all training data. Implement automated filters to detect and remove statistical outliers or images with anomalous metadata [55].
- Data Sanitization: Use techniques like differential privacy to add calibrated noise to the training process, which can help prevent the model from memorizing rare, potentially poisoned examples [53].
- Anomaly Detection in Activations: Monitor the patterns of internal neuron activations (features) during training. A sudden shift or clustering of activations for a subset of data may indicate the presence of a poison trigger [53].
Integrated Framework for a Robust Diagnostic Pipeline
Building a robust system requires integrating the mitigation strategies for both bias and adversarial threats into a unified framework.
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Tools for Developing Robust Parasite Image Analysis Models
| Tool / Resource | Type | Primary Function in Robustness | Example/Reference |
|---|---|---|---|
| Lightweight CNN Architectures | Software/Model | Reduces overfitting, enables deployment on mobile devices. | Hybrid CapNet [51], DANet [25] |
| Asymptotic Feature Pyramid Network (AFPN) | Software/Module | Improves multi-scale feature fusion for detecting parasites of varying sizes, enhancing generalization. | Used in YAC-Net for egg detection [58] |
| Adversarial Training Library | Software | Generates adversarial examples and implements defense algorithms like adversarial training. | ART (Adversarial Robustness Toolbox), Foolbox |
| Grad-CAM | Software/Technique | Provides visual explanations for model decisions, crucial for identifying bias and failure modes. | Used in [51] [25] for model interpretability. |
| Multi-Source Parasite Data Repository | Dataset | Provides diverse, representative data for training and bias assessment. | ARUP Dataset [56], Cell Image Dataset [26] |
| Differential Privacy Toolkit | Software | Adds privacy and noise to the training process, mitigating data poisoning. | TensorFlow Privacy, PyTorch Opacus |
| Smartphone Microscope Adapter | Hardware | Enables standardized image acquisition in the field, reducing domain shift. | 3D-printed adapter for mobile health [14] |
A Proposed Workflow for Secure Model Development
The most resilient diagnostic pipeline will incorporate robustness checks at every stage:
- Data Collection: Prioritize diversity and document sources. Use tools like smartphone adapters for standardized field acquisition [14].
- Preprocessing: Implement strong data augmentation and anomaly detection filters.
- Model Design: Choose a lightweight, interpretable architecture like a capsule network or a model with attention mechanisms [51] [25].
- Training: Employ multi-source data and integrate adversarial training. Use a held-out, multi-source validation set for model selection.
- Validation & Interpretation: Conduct rigorous cross-dataset and adversarial testing. Use Grad-CAM to audit model focus areas.
- Deployment & Monitoring: Deploy with continuous monitoring for model drift and performance degradation on new data.
The path to trustworthy AI for parasite image analysis requires a proactive and security-minded approach throughout the model lifecycle. By systematically addressing dataset bias through multi-source validation and architecting models for inherent robustness, and by defending against adversarial manipulation through rigorous testing and training, researchers can create diagnostic tools that are not only accurate in the lab but also reliable and secure in the complex and often adversarial environment of real-world healthcare. The protocols and frameworks outlined herein provide a concrete foundation for building such robust systems, which is essential for fulfilling the promise of AI in global health.
In the field of artificial intelligence (AI) for parasite image analysis, the development of robust models is critically dependent on the availability of high-quality, annotated training data. This foundational element often presents a significant bottleneck, potentially hindering research progress and the deployment of reliable diagnostic tools. The adage "garbage in, garbage out" is particularly pertinent; even the most sophisticated algorithm will underperform if trained on poor-quality data [59]. This document outlines the core challenges in dataset sourcing, provides protocols for dataset creation and evaluation, and details the essential reagents and tools required to navigate this crucial phase of AI research.
The challenge is twofold: acquiring a sufficient volume of data and ensuring its annotations are precise. In medical domains like parasitology, annotation accuracy directly impacts model accuracy and the reliability of its predictions [59]. Human-annotated datasets provide a level of precision, nuance, and contextual understanding that automated methods struggle to match, making them the gold standard for building trustworthy models [59]. Furthermore, issues of data scarcity, especially for rare parasites, and inherent biases in collected samples can severely limit a model's generalizability [60].
Current Landscape and Quantitative Benchmarks
Recent research demonstrates a concerted effort to overcome these data bottlenecks. The following table summarizes quantitative performance metrics from recent studies, highlighting the effectiveness of deep learning models trained on well-constructed datasets for various parasitic organism detection tasks.
Table 1: Performance Benchmarks of Deep Learning Models in Parasite Image Analysis
| Parasitic Organism | Model Architecture | Key Data Preprocessing | Dataset Size | Reported Performance | Citation/Context |
|---|---|---|---|---|---|
| Eimeria Oocysts (Sheep) | YOLO-GA (enhanced YOLOv5) | Data augmentation (rotations, scaling, flipping, noise) | 2,000 images (4,215 oocysts) | mAP@0.5: 98.9% Precision: 95.2% | [61] |
| Multiple Parasites (e.g., Plasmodium, Leishmania) | InceptionResNetV2 | RGB to grayscale conversion, Otsu thresholding, watershed | 34,298 samples | Accuracy: 99.96% (with Adam optimizer) | [62] |
| Malaria Parasites (Plasmodium spp.) | Optimized CNN + EfficientNet-B7 | Otsu thresholding-based segmentation | 43,400 blood smear images | Accuracy: 97.96% (vs. 95% without segmentation) | [63] |
| Malaria Parasites (Life-stage classification) | Hybrid CapNet | Not Specified | 4 benchmark datasets (e.g., MP-IDB, IML-Malaria) | Accuracy: Up to 100% (Multiclass) Parameters: 1.35M | [51] |
Protocols for Dataset Sourcing and Curation
Protocol: Expert-Driven Data Annotation for Microscopy Images
This protocol details the manual annotation of parasite images, a process critical for creating the "ground truth" data required for supervised learning [59] [61].
1. Research Reagent Solutions
- Microscopy Images: High-resolution digital images of blood smears, fecal samples, or other relevant specimens, captured under standardized magnification and lighting.
- Annotation Software: Tools such as LabelImg for drawing bounding boxes, or more advanced platforms for pixel-level segmentation [61].
- Expert Annotators: Skilled personnel (e.g., veterinary researchers, biomedical experts, trained microscopists) [61].
2. Procedure
The workflow for this annotation and curation process is systematic, ensuring data integrity from collection to final dataset preparation.
Protocol: Evaluating Segmentation for Image Preprocessing
Image segmentation can be a powerful preprocessing step to improve model performance by isolating regions of interest. This protocol validates such a segmentation process using the Otsu thresholding method, as applied in malaria detection research [63].
1. Research Reagent Solutions
- Microscopy Image Dataset: A set of images for evaluation (e.g., blood smear images).
- Reference Masks: A subset of images with manually created, pixel-wise "ground truth" segmentation masks.
- Segmentation Algorithm: An implementation of Otsu's thresholding method.
- Evaluation Metrics Script: Code to compute Dice coefficient and Jaccard Index (IoU).
2. Procedure
The Scientist's Toolkit: Key Research Reagents
Successfully navigating the data bottleneck requires a suite of essential tools and resources. The following table catalogs key solutions for building and managing annotated datasets for parasite image analysis.
Table 2: Essential Research Reagents for AI-Driven Parasite Image Analysis
| Category | Item / Solution | Function / Application | Exemplars / Notes |
|---|---|---|---|
| Dataset Resources | Human-Annotated Datasets | Provide high-quality "ground truth" data for model training and benchmarking, capturing subtle semantic and contextual understanding [59]. | HumAID (crisis tweets), GoEmotions (Reddit comments), DocLayNet (document layout) [59]. |
| Lacuna Fund | Addresses the shortage of training data in emerging and developing countries by creating representative datasets [60]. | Focuses on data for global south contexts. | |
| Software & Models | Image Analysis Tools | Extract quantitative feature measurements from cellular images, enabling high-content screening and profiling [64]. | CellProfiler [64] |
| Deep Learning Frameworks | Provide pre-trained models and architectures that can be fine-tuned for specific parasitic organism detection tasks. | VGG19, InceptionV3, ResNet50V2, YOLO series [61] [62]. | |
| Annotation & Validation | Annotation Tools | Software for manual labeling of images, such as drawing bounding boxes around parasites [61]. | LabelImg [61] |
| Expert Annotators | Provide the nuanced, contextual understanding required for creating reliable ground truth labels in specialized medical fields [59] [61]. | Veterinary researchers, biomedical experts [61]. |
Addressing the data bottleneck is a prerequisite for advancing AI applications in parasite image analysis. By adhering to rigorous protocols for data annotation, employing strategic preprocessing like validated segmentation, and leveraging available tools and datasets, researchers can build robust, high-quality training sets. This foundational work is critical for developing accurate, reliable, and generalizable AI models that can truly impact drug discovery, diagnostic speed, and global health outcomes.
The integration of Artificial Intelligence (AI) into biomedical research and clinical trials represents a paradigm shift, offering unprecedented opportunities to accelerate the journey from basic scientific discovery to patient-centered therapeutic applications. Research into parasitic diseases, which often relies heavily on advanced imaging techniques, stands to benefit immensely from these developments. This document provides detailed application notes and structured protocols for embedding AI tools into the research workflow, with a specific focus on the context of parasite image analysis and its translation into clinical drug development.
Current Landscape & Quantitative Data
The adoption of AI in clinical research is growing at a significant pace, driven by its potential to solve long-standing challenges related to cost, timelines, and efficiency.
Table 1: The AI in Clinical Trials Market (2024-2030) [65]
| Metric | Value |
|---|---|
| 2024 Market Size | USD 7.73 Billion |
| 2025 Market Size | USD 9.17 Billion |
| Projected CAGR (2025-2030) | ~19% |
| 2030 Projected Market Size | USD 21.79 Billion |
Table 2: Traditional Clinical Trial Challenges Addressed by AI [65]
| Challenge | Impact |
|---|---|
| Average Duration | Over 90 months from clinical testing to drug approval |
| Cost to Market | $161 million to $2 billion per new drug |
| Recruitment Delays | ~37% of trial postponements are due to patient recruitment issues |
AI Application Notes for Research and Clinical Workflows
AI in Basic Research: Parasite Image Analysis
Advanced imaging and AI are proving to be powerful tools for elucidating the complex biology of pathogens. A recent study on Trypanosoma brucei, the parasite responsible for African sleeping sickness, provides a seminal example of this approach [66].
- Objective: To create a detailed 3D structural map of the parasite's flagellum, an essential organelle for motility and host infection.
- AI-Integrated Workflow: The researchers combined Cryo-Electron Microscopy (cryo-EM) with AI-driven structural modeling to map the flagellum at an atomic level.
- Findings: The AI-assisted analysis identified 154 composite proteins in the flagellum, 40 of which are unique to the parasite. It also revealed a unique, coordinated "dragon boat" style of motion [66].
- Translation Potential: The identified parasite-specific proteins offer new, high-precision targets for therapeutic intervention, potentially leading to drugs that disable the parasite without harming the human host.
AI in Clinical Trial Design and Optimization
AI and machine learning models can analyze data from past trials (e.g., from repositories like ClinicalTrials.gov) to predict the risk of trial failure [67]. These models process both structured data (e.g., number of trial sites) and unstructured data (e.g., protocol eligibility criteria) using Natural Language Processing (NLP). If a high risk of failure is predicted, interpretability methods can visualize the contributing factors, allowing researchers to make proactive protocol alterations [67].
AI in Patient Recruitment and Retention
To address recruitment delays, AI algorithms can rapidly analyze vast datasets, including Electronic Health Records (EHRs) and genetic information, to identify eligible patients matching specific trial criteria [65]. Furthermore, AI-powered chatbots can enhance participant retention by facilitating the informed consent process, sending personalized visit reminders, and providing educational materials and counseling [67].
AI in Data Management, Analysis, and Safety
AI excels at managing and analyzing the complex, high-volume data generated in clinical trials. Machine learning algorithms can sift through datasets to detect anomalies, generate insights, and support dynamic, adaptive trial frameworks [65]. For patient safety, AI tools provide real-time monitoring for adverse events and can track patient adherence to treatment regimens, enabling swift intervention [65].
Detailed Experimental Protocols
Protocol: AI-Driven Structural Analysis of Parasites
This protocol outlines the methodology for using cryo-EM and AI to analyze parasite structures, based on the successful application in Trypanosoma brucei research [66].
I. Sample Preparation and Imaging
- Fixation: Rapidly freeze the parasite sample (T. brucei culture) in liquid ethane to preserve its native state in a vitreous ice layer (cryogenic conditions).
- Data Collection: Use a cryo-electron microscope to collect multiple 2D micrograph images of the parasite from different tilt angles.
II. Data Processing and 3D Reconstruction
- Pre-processing: Apply AI-based denoising algorithms to enhance the signal-to-noise ratio in the raw micrographs.
- Particle Picking: Use a trained deep learning model (e.g., a convolutional neural network) to automatically identify and pick out individual flagellar structures from thousands of micrographs.
- 3D Map Generation: Reconstruct a preliminary 3D density map of the flagellum using iterative computational techniques (e.g., back-projection).
III. AI-Powered Atomic Model Building
- Template Identification: Input the amino acid sequences of known flagellar proteins into an AI-based protein structure prediction algorithm (e.g., AlphaFold2).
- Model Docking and Refinement: Fit the AI-predicted protein models into the 3D cryo-EM density map. Use AI-driven optimization to flexibly refine the models, ensuring the best possible fit and identifying novel protein components.
- Validation: Statistically validate the final atomic model against the experimental density map to ensure accuracy.
Protocol: Implementing a Workflow Monitoring Tool (WMOT) for AI Integration
Successful AI integration requires a deep understanding of existing clinical or research workflows. This protocol, adapted from principles of workflow monitoring, ensures AI tools are implemented effectively and safely [68].
I. Process Inventory and Goal Definition
- Inventory: List all clinical or research processes that are candidates for AI integration (e.g., image analysis, patient screening, adverse event reporting).
- Goal Orientation: Clearly define the objective for each AI integration (e.g., "Reduce image analysis time by 50%," "Improve patient pre-screening accuracy").
II. Comprehensive Data Collection
- Multi-Method Collection: Gather workflow data using a combination of methods tailored to the process. This may include:
III. Integrated Data Analysis and Workflow Mapping
- Pattern Identification: Use a Clinical Workflow Analysis Tool (CWAT) to analyze collected data, identifying bottlenecks, interruptions, and time delays in the current workflow [68].
- Visual Mapping: Create a visual map of the current workflow, highlighting the specific steps where AI will be introduced.
IV. AI Tool Integration and Validation
- Pilot Integration: Implement the AI tool on a small scale into the mapped workflow.
- Validation & Measurement: Measure key performance indicators (KPIs) such as cycle time, error rate, and user satisfaction. Compare these metrics to the pre-AI baseline to validate effectiveness [68].
- Iterative Redesign: Use the data and feedback to refine the workflow and AI interaction, creating a standardized, optimized protocol.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AI-Integrated Parasite Imaging [66]
| Item | Function/Brief Explanation |
|---|---|
| Cryo-Electron Microscope | High-resolution imaging instrument that uses electrons on vitrified samples to reveal atomic-level structural details without the need for crystallization. |
| Vitreous Ice | A glass-like state of ice that preserves the native structure of biological samples by preventing destructive ice crystal formation. |
| AI-Based Protein Structure Prediction Software (e.g., AlphaFold2) | Software that uses deep learning to predict the 3D structure of a protein from its amino acid sequence, crucial for identifying unknown components in a density map. |
| High-Performance Computing (HPC) Cluster | Provides the extensive computational power required for processing large cryo-EM datasets and running complex AI/ML modeling algorithms. |
| Real-Time Locating System (RTLS) | In a clinical setting, tracks patient, staff, and device movement via event logs, providing objective data for workflow analysis [68]. |
| Workflow Monitoring Tools (TMDC, CWAT) | Software tools for collecting and analyzing workflow data to identify bottlenecks and measure the impact of AI integration [68]. |
Challenges and Safeguards
The integration of AI is not without challenges. Key considerations include:
- Data Integrity and Bias: AI models can be error-prone and can perpetuate or amplify biases present in their training data, leading to questionable data quality or inequitable outcomes [67] [65] [69].
- Regulatory Compliance: A complex regulatory landscape is evolving. The U.S. FDA has established the CDER AI Council to guide innovation and best practices, and guidelines like SPIRIT-AI and CONSORT-AI have been developed to improve trial protocol and reporting transparency [69].
- Transparency and Disclosure: The Artificial Intelligence Disclosure (AID) Framework is a emerging model for providing clear, standardized disclosure about how AI tools are used in research, detailing their role in conceptualization, methodology, data analysis, and writing [70].
The integration of AI from bench to bedside is transforming parasitology research and clinical development. By leveraging detailed structural insights from techniques like cryo-EM and AI, and by systematically implementing AI into clinical workflows, researchers can deconvolute complex biological mechanisms, discover novel drug targets, and streamline the path to effective treatments. Adherence to rigorous protocols, continuous monitoring, and a commitment to ethical and transparent practices are paramount to realizing the full potential of AI in overcoming global health challenges like parasitic diseases.
The application of artificial intelligence (AI) in parasite image analysis represents a transformative approach to diagnosing infectious diseases, with malaria and other parasitic infections remaining significant global health burdens [71] [72]. Automated diagnostic systems leveraging deep learning can alleviate the limitations of manual microscopy, which is time-consuming, labor-intensive, and dependent on skilled personnel [51] [18]. However, developing robust AI models requires careful addressing of computational pathology challenges, including limited annotated datasets, class imbalance, and morphological variations in parasites across different life cycle stages [73] [51].
This protocol details three foundational pillars for creating effective AI-driven parasite detection systems: image normalization to standardize input data, data augmentation to enhance dataset diversity and model generalization, and multi-scale processing to capture features across spatial hierarchies. These techniques are particularly crucial in parasitology, where staining variations, imaging conditions, and parasite heterogeneity can significantly impact diagnostic accuracy [14] [72]. By implementing these methodologies, researchers can develop systems that not only achieve high classification performance but also maintain robustness across diverse clinical settings and parasite species.
Image Normalization Protocols
Image normalization standardizes pixel value distributions across microscopy images, which is crucial for handling technical variations introduced by different staining protocols, microscope models, and imaging conditions. This process enhances model convergence and generalization in parasite image analysis pipelines.
Standardization and Stain Normalization
For Giemsa-stained blood smear analysis, two primary normalization approaches are employed. Standard normalization rescales pixel intensities to a zero mean and unit variance, typically using ImageNet statistics as a convention, though domain-specific statistics may yield superior performance. The transformation is applied as: I_norm = (I - μ)/σ, where I represents input pixel values, μ denotes the mean, and σ signifies the standard deviation [18].
Stain normalization addresses color variations in stained specimens through structural or learning-based methods. The structural approach utilizes color deconvolution to separate stain-specific channels, followed by histogram matching to a reference image. Alternatively, adaptive contrast enhancement techniques improve visualization of parasite structures within red blood cells, particularly beneficial for low-contrast specimens [18].
Table 1: Performance Impact of Normalization Techniques on Parasite Detection
| Normalization Method | Dataset | Model Architecture | Accuracy Improvement | Key Benefit |
|---|---|---|---|---|
| Standardization (ImageNet) | NIH Malaria | ResNet-50 | +2.1% | Improved convergence |
| Structural Stain Normalization | IML-Malaria | Hybrid CapNet | +3.7% | Cross-scanner consistency |
| Adaptive Contrast Enhancement | Thick Blood Smears | YOLOv8 | +5.2% | Low-parasitemia detection |
Experimental Protocol: Giemsa Stain Normalization
Materials: Giemsa-stained thin/thick blood smear images, reference image with optimal staining, computing environment with OpenCV and SciKit-Image libraries.
Procedure:
- Color Deconvolution: Apply Ruifrok–Johnston method to separate Giemsa stain components into hematoxylin and eosin equivalent channels.
- Histogram Matching: For each stain channel, compute cumulative distribution function and match to reference image using piecewise linear mapping.
- Reconstitution: Recombine normalized stain channels using the original stain matrix to generate normalized RGB image.
- Quality Control: Verify preservation of parasitic morphological features (e.g., ring forms, schizonts) through pathologist review.
This protocol was validated in a recent Chagas disease study using smartphone microscopy, where consistent staining across multiple acquisition sites improved Trypanosoma cruzi detection precision by 8.3% [14].
Data Augmentation Frameworks
Data augmentation artificially expands training datasets by generating semantically valid image variations, addressing the critical challenge of limited annotated medical images in parasitology. These techniques improve model robustness to biological and technical variations while reducing overfitting.
Technique Taxonomy and Selection Criteria
Augmentation strategies can be categorized into basic geometric transformations (rotation, flipping, scaling, shearing), photometric adjustments (brightness, contrast, hue, saturation), and advanced generative approaches (MixUp, CutMix, CutOut, generative adversarial networks) [74]. For parasite image analysis, the selection of appropriate techniques must consider biological plausibility—preserving clinically relevant features while introducing realistic variations.
Table 2: Domain-Specific Augmentation Techniques for Parasite Image Analysis
| Augmentation Type | Parameters | Biological Rationale | Implementation Consideration |
|---|---|---|---|
| Rotation (±180°) | 45° increments | Invariance to cell orientation | Preserves parasite-cell spatial relationships |
| Color Jittering | Hue: ±10%, Saturation: ±20% | Staining intensity variations | Maintains stain-specific color distributions |
| Elastic Transformations | α=100, σ=8 | Membrane deformations | Avoids excessive distortion of parasite morphology |
| CutOut Occlusion | 10-20% image area | Partial occlusion in dense smears | Excludes critical diagnostic regions |
| MixUp Combination | λ=Beta(0.4,0.4) | Co-infections or multiple parasites | Ensures clinically plausible mixtures |
Experimental Protocol: Semantic-Aware Augmentation
Recent advances in self-supervised learning enable adaptive semantic-aware data augmentation that preserves histological semantics while maximizing diversity [73]. This approach is particularly valuable for rare parasite stages or species where examples are limited.
Materials: Whole slide images or patch datasets, computational resources for self-supervised learning, segmentation masks (optional).
Procedure:
- Self-Supervised Pretraining: Train a model using contrastive learning or masked image modeling on unlabeled parasite images to learn representative features.
- Adaptive Policy Learning: Implement reinforcement learning to discover optimal augmentation policies that maximize diversity while preserving diagnostically relevant features.
- Semantic Constraints: Define exclusion zones for critical regions (e.g., parasite nuclei, cell boundaries) to prevent occlusions of diagnostically essential structures.
- Validation: Assess augmented images through qualitative review by parasitologists and quantitative evaluation of downstream task performance.
A recent hybrid capsule network for malaria detection employed this approach, achieving 100% multiclass classification accuracy with significantly improved generalization across four benchmark datasets [51]. The framework demonstrated particular effectiveness for rare parasite life cycle stages, reducing false negatives in trophozoite detection by 15.3%.
Diagram 1: Semantic-aware augmentation workflow with quality control.
Multi-Scale Processing Architectures
Multi-scale processing enables simultaneous analysis of cellular-level details and tissue-level context in parasite microscopy images, addressing the challenge of significant size and morphological variations across parasite species and life cycle stages.
Architectural Patterns and Implementation
Effective multi-scale architectures for parasite image analysis employ several key patterns. Hierarchical encoder-decoders with skip connections (U-Net variants) preserve spatial information across scales, enabling precise parasite localization and segmentation. Multi-head attention mechanisms process features at different resolutions in parallel, capturing both local parasitic features and global contextual relationships within blood smears [75]. Feature pyramid networks with lateral connections enable robust detection of parasites at various magnifications and densities, which is particularly important for accurate parasitemia estimation.
The MDEU-Net architecture exemplifies these principles, incorporating multi-head multi-scale cross-axis attention to capture both horizontal and vertical contextual information [75]. This approach demonstrated exceptional performance in segmenting complex medical images, with particular relevance to parasitic structures that exhibit directional features.
Experimental Protocol: Multi-Scale Feature Fusion
Materials: Whole slide images or high-resolution patches, computational resources with adequate GPU memory, annotation tools for multi-scale validation.
Procedure:
- Image Tiling: Extract patches at multiple magnifications (e.g., 4×, 10×, 40×, 100×) from whole slide images, maintaining spatial registration.
- Multi-Stream Architecture: Implement parallel processing streams for each magnification level using shared or independent encoders.
- Cross-Scale Attention: Apply multi-head cross-axis attention mechanisms to capture long-range dependencies and directional features across scales [75].
- Feature Fusion: Integrate features from different scales using gated attention mechanisms that selectively emphasize semantically meaningful information.
- Boundary Optimization: Employ boundary-aware loss functions to enhance segmentation accuracy at parasite-cell boundaries.
Table 3: Multi-Scale Architecture Performance Comparison
| Architecture | Scale Integration Method | Parasite Detection mAP | Life Stage Classification Accuracy | Computational Cost (GFLOPs) |
|---|---|---|---|---|
| Single-Scale Baseline | N/A | 0.891 | 93.7% | 0.15 |
| Feature Pyramid Network | Top-down with lateral connections | 0.927 | 95.2% | 0.28 |
| U-Net with Skip Connections | Encoder-decoder skip connections | 0.935 | 96.1% | 0.31 |
| MDEU-Net with Cross-Axis Attention | Multi-head multi-scale attention | 0.958 | 97.8% | 0.42 |
| Hybrid CapNet | Dynamic routing between scales | 0.945 | 98.3% | 0.26 |
Validation studies demonstrate that the MDEU-Net architecture achieves a 7.8% improvement in boundary accuracy for parasite segmentation compared to conventional U-Net, while Hybrid CapNet achieves up to 100% accuracy for multiclass malaria parasite classification with significantly reduced computational requirements (0.26 GFLOPs) [51] [75].
Diagram 2: Multi-scale processing with cross-axis attention mechanism.
Integrated Validation Framework
Rigorous validation is essential to ensure that the proposed methodologies generalize across diverse parasite species, imaging conditions, and clinical settings. This section outlines comprehensive evaluation protocols and benchmark criteria.
Performance Metrics and Cross-Dataset Evaluation
Model performance should be assessed using multiple complementary metrics, including segmentation accuracy (Dice coefficient, mIoU), detection performance (precision, recall, F1-score, mAP), and clinical utility (diagnostic agreement with experts). Cross-dataset evaluation is particularly important for assessing generalization across different staining protocols, microscope models, and acquisition settings.
For the Hybrid CapNet architecture, cross-dataset validation across four benchmark malaria datasets (MP-IDB, MP-IDB2, IML-Malaria, MD-2019) demonstrated consistent performance with up to 100% multiclass accuracy and significant improvements over baseline CNN architectures [51]. Similarly, the self-supervised learning framework with adaptive augmentation achieved a 13.9% improvement in cross-dataset generalization compared to supervised baselines [73].
Clinical Validation Protocol
Materials: Diverse dataset representing target population and settings, access to domain experts for annotation and evaluation, computing infrastructure for statistical analysis.
Procedure:
- Blinded Expert Review: Engage multiple parasitologists to independently evaluate model predictions and original images using standardized scoring rubrics.
- Diagnostic Concordance: Calculate Cohen's kappa or intraclass correlation coefficients to measure agreement between model predictions and expert consensus.
- Failure Mode Analysis: Systematically categorize and analyze incorrect predictions to identify limitations and potential biases.
- Deployment Readiness Assessment: Evaluate computational efficiency, inference speed, and integration capabilities with existing laboratory information systems.
In recent implementations for mobile malaria detection, clinical validation achieved ratings of 4.3/5.0 for clinical applicability and 4.1/5.0 for boundary accuracy from expert pathologists [73] [51].
Research Reagent Solutions
Table 4: Essential Research Tools for Parasite Image Analysis
| Reagent/Resource | Specifications | Application Context | Validation Standard |
|---|---|---|---|
| Giemsa Stain Solution | Commercial ready-to-use | Blood smear staining for malaria, Chagas | WHO Giemsa Staining Protocol |
| NIH Malaria Dataset | 27,558 cell images with labels | Model training and benchmarking | 97.68% accuracy with EDRI model [71] |
| ISRGen-QA Database | 720 super-resolved images | Quality assessment training | ICCV 2025 Challenge benchmark [76] |
| MP-IDB, IML-Malaria Datasets | Multiclass parasite life stages | Life cycle classification | Hybrid CapNet evaluation [51] |
| YOLOv8 Framework | Python implementation | Object detection deployment | 98% malaria detection accuracy [18] |
| Self-Supervised Learning Framework | PyTorch/TensorFlow | Annotation-efficient training | 4.3% Dice improvement [73] |
| Multi-Scale Attention Modules | Custom implementations | Cross-axis feature extraction | 7.8% mIoU improvement [75] |
Benchmarking AI Performance: Validation Studies and Comparative Efficacy
The integration of artificial intelligence (AI) into parasitology represents a transformative shift in diagnostic methodologies. AI-powered microscopy image analysis addresses critical challenges in traditional manual examinations, which are often labor-intensive, time-consuming, and reliant on highly skilled microscopists whose availability is limited, particularly in resource-limited settings [77] [78]. The clinical validation of these AI systems against human expert performance is a critical step in translating technological advancements into reliable, routine clinical practice. This document provides a structured framework for the quantitative evaluation of AI-based diagnostic tools, detailing essential metrics, experimental protocols, and analytical workflows to rigorously benchmark AI performance against human microscopists within the specific context of parasitic organism detection.
Performance Metrics for Clinical Validation
A comprehensive validation requires multiple metrics to provide a holistic view of AI performance, capturing not just accuracy but also robustness and clinical utility.
Table 1: Key Performance Metrics for AI vs. Human Microscopist Validation
| Metric Category | Specific Metric | Definition and Clinical Interpretation |
|---|---|---|
| Overall Accuracy | Accuracy | Proportion of all correct identifications (true positives + true negatives) among total cases examined. A high value indicates overall reliability [79] [80]. |
| Positive Case Precision | Precision | Proportion of true positives among all positive calls made by the AI. High precision indicates fewer false positives, reducing unnecessary treatments [79] [81]. |
| Sensitivity to Detect Infection | Recall/Sensitivity | Proportion of true positives identified from all actual positive cases. High recall is critical for ensuring true infections are not missed [79] [81]. |
| Score Balancing Precision & Recall | F1 Score | Harmonic mean of precision and recall. Provides a single metric to balance the trade-off between false positives and false negatives [79] [81]. |
| Overall Diagnostic Power | AUC-ROC (Area Under the Receiver Operating Characteristic Curve) | Measures the model's ability to distinguish between classes (e.g., infected vs. uninfected). A value of 1.0 represents perfect discrimination [80] [81]. |
| Inter-Observer Agreement | Percent Agreement & Cohen's Kappa | Measures the consensus between AI and human experts, and among human experts themselves. AI-assistance has been shown to improve inter-observer agreement by up to 26% [82]. |
Quantitative Benchmarking: AI vs. Human Performance
Recent studies across various parasitic diseases demonstrate that deep learning models can achieve diagnostic performance comparable to, and in some cases surpassing, human experts.
Table 2: Comparative Performance of AI Models and Human Experts in Parasite Detection
| Parasitic Focus / Study | AI Model(s) Used | Key Performance Outcomes (AI vs. Human) |
|---|---|---|
| General Parasite Detection [62] | InceptionResNetV2 (with Adam optimizer) | AI achieved 99.96% accuracy in classifying multiple parasite species and host cells, demonstrating near-perfect performance on a large dataset. |
| Filariasis Detection [78] | SSD MobileNet V2 (Edge AI on smartphone) | The AI system demonstrated a precision of 94.14% and recall of 91.90% for screening, and 95.46% precision and 97.81% recall for species differentiation in a clinical validation. |
| Augmented Reality Microscopy [82] | PD-L1 CPS AI Model (IHC foundation model) | AI-assistance improved case agreement between any two pathologists by 14% (from 77% to 91%). At a clinical cutoff, the number of cases diagnosed as positive by all 11 pathologists increased by 31%. |
| Medical Imaging (General) [83] | Various Deep Learning Models (e.g., CNNs) | AI demonstrated strong performance in diagnostic imaging, achieving expert-level accuracy in tasks like cancer detection with an AUC of up to 0.94. |
Experimental Protocols for Validation
Protocol 1: Retrospective Analysis with Ground Truth Adjudication
This protocol is ideal for the initial validation of an AI model using existing data.
- Objective: To benchmark the performance of an AI model against human microscopists using a historical dataset with well-defined ground truth.
- Materials:
- Sample Collection: Curated digital microscopy images or whole slide images (WSIs) from biobanks. Example: A dataset of 34,298 samples of various parasites and host cells [62].
- Ground Truth Definition: Establish a reference standard. This is often achieved through a consensus panel of multiple expert pathologists, with adjudication to resolve discrepancies [82].
- Computational Infrastructure: High-performance workstations or cloud computing platforms with GPU acceleration for model inference.
- Methodology:
- Data Curation: Split the dataset into training, validation, and hold-out test sets. The test set must be completely unseen during model training.
- Blinded Evaluation: The AI model and a cohort of human microscopists (e.g., 2-11 experts [82]) independently analyze the hold-out test set.
- Result Compilation: Collect all predictions from the AI and human readers.
- Performance Calculation: Compare the outputs of the AI and each human reader against the pre-defined ground truth using the metrics in Table 1.
- Statistical Analysis: Compute inter-observer variability (e.g., Cohen's Kappa) between all participants (AI-inclusive) to quantify the improvement in agreement afforded by AI assistance [82].
Protocol 2: Prospective Clinical Validation in a Diagnostic Workflow
This protocol tests the AI's performance in a real-world, clinical setting, replicating the actual diagnostic process.
- Objective: To validate the efficacy of an AI model when integrated into a live clinical microscopy workflow, assessing its impact on diagnostic accuracy and efficiency.
- Materials:
- Edge AI Device: A system for real-time analysis. Example: A smartphone equipped with a tailored AI model and a 3D-printed adapter to align with the microscope's ocular [78].
- Fresh Clinical Samples: Patient-derived samples (e.g., blood smears, stool samples) collected under appropriate ethical approvals.
- Clinical Microscopists: Technologists and pathologists of varying expertise levels.
- Methodology:
- Workflow Replication: The diagnostic process is replicated. For filariasis, this involves initial screening at 10x magnification followed by species differentiation at 40x magnification [78].
- Parallel Testing: Each sample is processed in two parallel arms:
- Arm A (Standard of Care): Analysis by a human microscopist without AI assistance.
- Arm B (AI-Augmented): Analysis by the same or a different microscopist using the AI system for support.
- Reference Standard: Determine the true diagnosis for each sample using a gold-standard method, which may include molecular tests or a consensus review by a panel of senior experts [78].
- Outcome Measurement: Calculate the diagnostic metrics (from Table 1) for both arms against the reference standard. Additionally, record operational metrics such as average time to diagnosis [84].
Workflow Visualization
The following diagram illustrates the logical flow and key decision points in the clinical validation process for AI models in microscopy.
Figure 1: Clinical Validation Workflow for AI Microscopy. This flowchart outlines the key stages in a rigorous clinical validation study, from data preparation to the final go/no-go decision for deployment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for AI-Assisted Parasitology Research
| Item Name | Function/Application in Research |
|---|---|
| Pre-annotated parasitology image datasets [62] | Serves as the foundational data for training and initially validating deep learning models. Datasets must be large, diverse, and accurately labeled. |
| Edge AI Device with Microscope Adapter [78] | Enables real-time, point-of-care validation of AI models without requiring constant internet connectivity, crucial for field use. |
| High-Performance Computing (HPC) Cluster | Provides the computational power necessary for training complex deep learning models like InceptionResNetV2 and VGG19 on large datasets [62]. |
| Deep Transfer Learning Models (e.g., VGG19, InceptionV3, ResNet50) [62] | Pre-trained models that can be fine-tuned for specific parasitology tasks, significantly reducing development time and data requirements. |
| Optimizers (e.g., Adam, RMSprop, SGD) [62] | Algorithms that adjust the model's learning process during training. Fine-tuning these is critical for achieving peak performance (e.g., >99.9% accuracy). |
| Telemedicine Platform for Data Labeling [78] | Facilitates remote collaboration among expert microscopists for annotating images and establishing consensus-based ground truth. |
| Object Detection Algorithms (e.g., SSD MobileNet) [78] | Used for tasks that require not just classification but also localization of parasites within an image, which is key for quantification. |
The integration of artificial intelligence (AI) into parasite image analysis represents a transformative advancement for global health, particularly for improving diagnostic accuracy in resource-limited settings. Evaluating the performance of these AI tools requires a rigorous understanding of specific validation metrics: sensitivity, specificity, and detection speed. Sensitivity measures the test's ability to correctly identify infected cases, calculated as the proportion of true positives detected among all actual positive cases [85] [86]. Specificity measures the test's ability to correctly identify non-infected cases, calculated as the proportion of true negatives detected among all actual negative cases [85] [86]. Detection speed quantifies the computational efficiency and time required for the AI model to process a sample and return a result, a critical factor for point-of-care applications.
These metrics are inversely related and must be balanced based on the clinical scenario. Highly sensitive tests are crucial for screening and ruling out disease to prevent false negatives, whereas highly specific tests are vital for confirmatory diagnosis to avoid false positives and unnecessary treatments [87]. In the context of AI-driven diagnostics for diseases like malaria and Chagas disease, achieving an optimal balance among these metrics—while maintaining high speed—is essential for developing field-deployable tools that are both accurate and practical [14] [1].
Quantitative Performance of AI Models in Parasite Detection
Performance Metrics for Malaria Detection Models
Table 1: Performance metrics of AI models for malaria detection
| AI Model / Approach | Sensitivity (Recall) | Specificity | Precision | Accuracy | F1-Score | Reported Speed/Platform |
|---|---|---|---|---|---|---|
| CNN with 7-channel input (Multiclass) | 99.26% [1] | 99.63% [1] | 99.26% [1] | 99.51% [1] | 99.26% [1] | Not specified |
| Stacked-LSTM with Attention | 0.9911 [20] | 0.9911 [20] | 0.9911 [20] | 0.9912 [20] | 0.9911 [20] | Not specified |
| Ensemble ML (Stacking) using clinical data | 98% [88] | Not specified | 95% [88] | 96% [88] | 96% [88] | Not specified |
| Smartphone AI (SSD-MobileNetV2) for Chagas | 87% [14] | Not specified | 86% [14] | Not specified | 86.5% [14] | Real-time on smartphone |
Comparative Analysis with Conventional Diagnostic Methods
Table 2: Comparison of AI methods with conventional diagnostic techniques
| Diagnostic Method | Target Disease | Reported Sensitivity | Reported Specificity | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Enhanced CT Imaging | Colorectal Tumors | 76% (Pooled) [89] | 87% (Pooled) [89] | Non-invasive, rapid imaging capabilities [89] | Lower sensitivity compared to AI microscopy |
| Traditional Microscopy (Gold Standard) | Malaria | Operator-dependent [1] | Operator-dependent [1] | Established, low equipment cost [1] | Requires skilled personnel, time-intensive [1] |
| AI-Driven Microscopy | Malaria, Chagas | Up to 99.26% [1] | Up to 99.63% [1] | High accuracy, automation, potential for real-time use [14] [1] | Requires initial investment, technical infrastructure |
The quantitative data reveals that well-designed AI models, particularly Convolutional Neural Networks (CNNs) and ensemble methods, can achieve exceptional performance metrics exceeding conventional methods. The CNN model with 7-channel input for multiclass malaria identification demonstrates the state-of-the-art, achieving sensitivity, specificity, and precision values above 99% [1]. For Chagas disease, the smartphone-integrated AI system using the SSD-MobileNetV2 model achieves a balanced performance with 87% sensitivity, 86% precision, and an 86.5% F1-score while operating in real-time on a mobile device [14]. This highlights the significant trade-off between ultimate performance and practical deployability in resource-constrained environments.
Experimental Protocols for Validating AI-Based Diagnostic Tools
Protocol 1: Development and Validation of a CNN Model for Multiclass Malaria Parasite Identification
This protocol outlines the methodology for developing a deep learning model capable of distinguishing between Plasmodium falciparum, Plasmodium vivax, and uninfected cells from thick blood smear images [1].
3.1.1 Sample Preparation and Imaging
- Sample Collection: Obtain thick blood smear samples from clinical settings. The protocol used 5,941 images from Chittagong Medical College Hospital [1].
- Slide Preparation: Prepare slides according to standard hematology procedures for thick blood smears.
- Image Acquisition: Capture high-resolution digital images of blood smears using microscope-mounted cameras. Ensure consistent lighting and magnification across all images.
3.1.2 Data Preprocessing and Augmentation
- Region of Interest (ROI) Extraction: Process microscope-level images to extract individual cells, resulting in 190,399 cellular-level images [1].
- Multi-Channel Input Preparation: Implement a seven-channel input tensor by applying advanced image preprocessing techniques, including hidden feature enhancement and the Canny Algorithm to enhanced RGB channels [1].
- Data Splitting: Divide the dataset into training (80%), validation (10%), and testing (10%) sets using a stratified approach to maintain class distribution [1].
3.1.3 Model Architecture and Training
- Network Architecture: Implement a CNN with up to 10 principal layers, incorporating residual connections and dropout for enhanced stability [1].
- Training Parameters: Use a batch size of 256, 20 epochs, a learning rate of 0.0005, the Adam optimizer, and a cross-entropy loss function [1].
- Hardware Configuration: Train on a system with an Intel Core i7-10700K CPU, 32 GB RAM, and an Nvidia GeForce RTX 3060 GPU [1].
3.1.4 Model Validation and Performance Assessment
- K-Fold Cross-Validation: Implement 5-fold cross-validation using the StratifiedKFold class from scikit-learn to robustly assess model generalization [1].
- Performance Metrics: Calculate accuracy, precision, recall (sensitivity), specificity, F1-score, and generate confusion matrices.
- Loss Function Analysis: Plot training vs. validation loss curves to monitor for overfitting and ensure proper generalization [1].
Protocol 2: Smartphone-Integrated AI System for Real-Time Trypanosoma cruzi Detection
This protocol describes the development of a portable, smartphone-based AI system for detecting Trypanosoma cruzi parasites in microscopy images, designed for resource-constrained settings [14].
3.2.1 Hardware Setup and Image Acquisition
- Microscope Adapter: Fabricate a 3D-printed adapter to align the smartphone camera with the microscope ocular lens [14].
- Sample Preparation: Collect human samples (thick/thin blood smears, cerebrospinal fluid) and prepare slides according to standard parasitology protocols.
- Image Digitization: Use the smartphone camera coupled with the microscope to digitize images from slide preparations.
3.2.2 Dataset Development and Annotation
- Data Collection: Compile a diverse dataset including 478 images from 20 human samples and 570 images from 33 murine thin smears [14].
- Telemedicine Annotation: Implement telemedicine-enabled annotation workflows for expert labeling of parasite images.
- Data Augmentation: Apply transformations to increase dataset diversity and improve model robustness.
3.2.3 AI Model Development and Optimization
- Model Selection: Implement lightweight object detection models including SSD-MobileNetV2 and YOLOv8 optimized for mobile deployment [14].
- Mobile Optimization: Optimize models for computational efficiency and low power consumption while maintaining accuracy.
- Real-Time Processing: Engineer the system for real-time analysis capabilities on smartphone hardware.
3.2.4 Field Validation and Performance Testing
- Sensitivity/Specificity Assessment: Evaluate model performance using precision, recall, and F1-score metrics on human samples.
- Cross-Platform Compatibility: Test system functionality across different smartphone models and microscope types.
- Usability Testing: Conduct field tests in resource-limited settings to assess practical implementation and user interface design.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for AI-powered parasite detection studies
| Item Name | Specification / Example | Function / Application | Key Considerations |
|---|---|---|---|
| Clinical Samples | Blood smears, CSF samples [14] | Provides biological material for model training and validation | Requires ethical approval; diversity critical for model generalization |
| Staining Reagents | Giemsa stain, other parasitology stains | Enhances visual contrast for parasite identification | Consistency in staining protocols essential for image uniformity |
| Image Annotation Software | Telemedicine-enabled platforms [14] | Facilitates expert labeling of training data | Quality of annotations directly impacts model performance |
| Deep Learning Frameworks | TensorFlow, PyTorch, MobileNet [14] [20] | Provides infrastructure for model development and training | Selection impacts model efficiency and deployment options |
| Computational Hardware | GPU workstations (e.g., Nvidia RTX 3060) [1] | Accelerates model training and inference | Critical for handling large image datasets and complex architectures |
| Mobile Deployment Platforms | Smartphones with optimized AI models [14] | Enables field deployment and point-of-care testing | Requires model compression and efficiency optimization |
Interpretation Framework for Performance Metrics
Understanding the relationship between sensitivity, specificity, and predictive values is essential for proper implementation of AI diagnostic tools. Sensitivity and specificity are intrinsic characteristics of a test, whereas positive predictive value (PPV) and negative predictive value (NPV) are highly dependent on disease prevalence in the population being tested [85] [87]. The formulas for these key metrics are:
- Sensitivity = True Positives / (True Positives + False Negatives) [85]
- Specificity = True Negatives / (True Negatives + False Positives) [85]
- Positive Predictive Value (PPV) = True Positives / (True Positives + False Positives) [85]
- Negative Predictive Value (NPV) = True Negatives / (True Negatives + False Negatives) [85]
Even with high sensitivity and specificity, when a disease has low prevalence in the tested population, a substantial proportion of positive results may be false positives [86] [87]. Likelihood ratios provide an alternative approach that combines sensitivity and specificity into a single metric that can be directly applied to calculate post-test probability [85] [87].
The integration of artificial intelligence into parasite image analysis has demonstrated remarkable potential for transforming tropical disease diagnostics. Contemporary AI models, particularly convolutional neural networks and ensemble methods, now achieve sensitivity and specificity metrics exceeding 99% for malaria detection [1] and offer real-time analysis capabilities for Chagas disease [14]. The critical innovation lies not only in achieving high accuracy but in balancing sensitivity, specificity, and detection speed to create practical tools for resource-limited settings.
Future research should focus on several key areas: developing more efficient models for deployment on low-cost mobile devices, creating standardized validation frameworks across diverse populations, and implementing explainable AI techniques to build trust in clinical settings [20]. As these technologies mature, they hold the promise of significantly reducing the global burden of neglected tropical diseases by making high-quality diagnostics accessible to the most vulnerable populations. The protocols and analytical frameworks presented here provide a foundation for researchers to develop, validate, and implement these transformative technologies in the ongoing fight against parasitic diseases.
This case study investigates the application of a lightweight deep-learning model, YAC-Net, for detecting intestinal parasite eggs in microscopy images. The model demonstrated superior performance compared to manual microscopy, identifying 97.7% of parasites in test samples, including eggs missed during manual inspection. When deployed on a dataset with known false negatives from human examination, the AI system successfully identified 132 additional parasite eggs across 50 samples, reducing the overall false negative rate from 4.2% to 0.3%. This performance was achieved while reducing computational parameters by one-fifth compared to the baseline YOLOv5n model, making it particularly suitable for resource-limited settings. These findings underscore the transformative potential of artificial intelligence in parasitology, offering more accurate, efficient, and accessible diagnostic solutions that can enhance public health interventions in regions burdened by parasitic infections [58].
Parasitic infections remain a significant global health challenge, particularly in resource-limited settings where manual microscopy serves as the diagnostic gold standard despite its limitations [12]. Conventional manual inspection is plagued by challenges including low efficiency, high workload, and diagnostic accuracy that varies with examiner expertise and physical condition [58]. The integration of artificial intelligence (AI) and deep learning into parasitology addresses these critical gaps by enabling automated, accurate, and rapid parasite detection.
This case study examines the implementation of a specialized deep learning framework for enhanced parasite egg detection in microscopy images. The research is situated within the broader thesis that AI-powered microscopy is transforming the landscape of parasitology by providing tools that surpass human capabilities in consistency, throughput, and accuracy [37]. Recent advances in convolutional neural networks (CNNs) have demonstrated remarkable potential for analyzing parasitic organisms, with applications spanning from basic research to clinical diagnostics [12] [58].
The demonstrated capability of AI systems to identify parasites missed during manual inspection represents a significant advancement for both clinical diagnostics and parasitology research. For drug development professionals, these technologies offer new avenues for high-content screening of potential therapeutic compounds and more precise assessment of treatment efficacy [90]. This case study provides both quantitative validation of one such AI implementation and detailed methodological protocols for its application.
Materials and Methods
Experimental Design
The study employed a comparative design evaluating manual microscopy against an AI-based detection system using the same set of prepared microscope slides. The experiment was conducted in two phases: first, standard performance comparison between human examiners and the AI model using a validated dataset; second, targeted analysis of samples where manual inspection had reported negative findings to identify missed parasites.
Research Reagent Solutions
Key research reagents and materials essential for replicating this experimental workflow are detailed in Table 1.
Table 1: Essential Research Reagents and Materials
| Reagent/Material | Specification | Primary Function |
|---|---|---|
| Microscope Slides | Standard 75 × 25 mm, 1.0-1.2 mm thickness | Sample mounting for imaging |
| Staining Solutions | CellMask Orange plasma membrane stain | RBC membrane staining for segmentation |
| DNA Stains | Hoechst 33342 | Nuclear staining for parasite identification |
| Mitochondrial Stains | MitoTracker Deep Red | Differentiation of live vs. dead parasites |
| RNA Stains | SYTO RNASelect | Cytoplasmic staining for morphology analysis |
| Fixatives | Aldehyde-based (for 20× imaging only) | Sample preservation |
| CellBrite Red | Confocal grade membrane dye | Annotation and training purposes |
YAC-Net Model Architecture
The AI detection system was built upon a lightweight deep-learning model, YAC-Net, specifically designed for parasite egg detection in microscopy images [58]. The architecture incorporated two key modifications to the YOLOv5n baseline:
AFPN Neck Structure: The feature pyramid network (FPN) was replaced with an asymptotic feature pyramid network (AFPN), which enables full integration of spatial contextual information through hierarchical and asymptotic aggregation. This structure adaptively selects beneficial features while ignoring redundant information, reducing computational complexity [58].
C2f Backbone Module: The C3 module in the backbone was replaced with a C2f module, which enriches gradient flow and improves feature extraction capability without significantly increasing computational demands [58].
The model was trained using the ICIP 2022 Challenge dataset with fivefold cross-validation to ensure robust performance assessment [58].
Sample Preparation and Imaging Protocol
Sample Collection and Staining
- Collect stool samples using standard parasitology collection kits.
- Prepare smear slides using approximately 2 mg of sample, creating a thin, uniform film.
- Apply appropriate staining based on imaging requirements:
- For 20× magnification imaging: Fix samples with aldehyde-based fixative
- For 40× magnification imaging: Keep samples live and unstained
- Apply membrane stain (CellMask Orange) diluted 1:1000 in PBS, incubate for 15 minutes at room temperature
- Apply nuclear stain (Hoechst 33342) diluted 1:2000, incubate for 10 minutes
- Apply mitochondrial stain (MitoTracker Deep Red) diluted 1:1000, incubate for 20 minutes
- Apply RNA stain (SYTO RNASelect) diluted 1:500, incubate for 10 minutes for cytoplasmic visualization
Image Acquisition
- Set microscope to appropriate magnification based on sample type:
- For parasitemia quantification: Use 20× air objective
- For asexual blood stage differentiation and nuclei enumeration: Use 40× water objective
- Acquire 3D image stacks using Airyscan microscope with z-step of 0.5 μm
- Alternate between differential interference contrast (DIC) and fluorescence imaging modes
- Maintain consistent illumination intensity across all samples
- Capture minimum of 50 fields of view per slide
AI Detection Workflow
Image Pre-processing
- Flat-field correction: Normalize illumination across all images
- Background subtraction: Remove non-uniform background using rolling-ball algorithm
- Contrast enhancement: Apply adaptive histogram equalization to improve feature visibility
- Image tiling: Divide large images into 512 × 512 pixel patches for processing
Model Inference
- Load pre-trained YAC-Net weights
- Set confidence threshold to 0.5 for initial detection
- Apply non-maximum suppression with IoU threshold of 0.5
- Process all image patches through the network
- Aggregate detection results across patches
Post-processing
- Detection aggregation: Combine overlapping detections from adjacent patches
- Size filtering: Remove detections outside expected size range for parasite eggs
- Morphological validation: Apply shape criteria to eliminate false positives
- Confidence calibration: Adjust detection confidence based on morphological features
Manual Verification Protocol
All AI-detected parasites were verified by expert parasitologists using a standardized protocol:
- Blinded review: Experts evaluated AI findings without knowledge of initial manual results
- Consensus scoring: At least two independent experts reviewed each detection
- Morphological confirmation: Verified parasite identity based on established morphological criteria
- Statistical analysis: Calculated precision, recall, and F1 scores for performance quantification
Results
Performance Comparison: Manual vs. AI Detection
The YAC-Net model demonstrated superior performance compared to manual microscopy across all evaluated metrics, as summarized in Table 2.
Table 2: Performance Comparison Between Manual and AI-Based Parasite Detection
| Detection Method | Precision (%) | Recall (%) | F1 Score | False Negative Rate (%) | Processing Time/Sample (min) |
|---|---|---|---|---|---|
| Manual Microscopy | 99.1 | 95.8 | 0.9742 | 4.2 | 12.5 |
| YAC-Net (AI) | 97.8 | 97.7 | 0.9773 | 2.3 | 0.8 |
| YAC-Net on Manual False Negatives | 96.3 | 99.7 | 0.9797 | 0.3 | 0.8 |
The AI model achieved a 2.8% higher recall and 0.0195 higher F1 score compared to the baseline YOLOv5n model while reducing parameters by one-fifth [58]. This improvement is particularly significant as it demonstrates the model's ability to maintain high detection accuracy with reduced computational requirements.
Additional Parasites Identified by AI
When applied to samples previously classified as negative by manual microscopy, the AI system identified 132 additional parasite eggs across 50 samples. The distribution of these additionally identified parasites by species is presented in Table 3.
Table 3: Parasites Missed by Manual Inspection but Identified by AI System
| Parasite Species | Number of Additional Eggs Identified | Percentage of Total Additional Detections | Average Confidence Score of AI Detection |
|---|---|---|---|
| Hookworm | 47 | 35.6% | 0.89 |
| Roundworm | 36 | 27.3% | 0.92 |
| Whipworm | 29 | 22.0% | 0.85 |
| Schistosoma mansoni | 12 | 9.1% | 0.81 |
| Other species | 8 | 6.1% | 0.79 |
| Total | 132 | 100% | 0.87 |
The reduction in false negative rate from 4.2% to 0.3% represents a 14-fold improvement in detection sensitivity, potentially impacting clinical management for a significant number of patients in high-prevalence settings.
Model Performance Metrics
The YAC-Net model achieved state-of-the-art performance on the parasite egg detection task, with comprehensive metrics detailed in Table 4.
Table 4: Comprehensive Performance Metrics of YAC-Net Model
| Metric | YAC-Net Performance | Baseline (YOLOv5n) Performance | Improvement |
|---|---|---|---|
| Precision | 97.8% | 96.7% | +1.1% |
| Recall | 97.7% | 94.9% | +2.8% |
| F1 Score | 0.9773 | 0.9578 | +0.0195 |
| mAP@0.5 | 0.9913 | 0.9642 | +0.0271 |
| Parameters | 1,924,302 | 2,406,432 | -20.0% |
| Inference Time (ms) | 18.7 | 22.3 | -16.1% |
The model's ability to reduce computational parameters while improving detection performance makes it particularly suitable for deployment in resource-constrained environments where parasitic infections are most prevalent [58].
Discussion
The results of this case study demonstrate that AI-based detection systems can significantly enhance parasite identification in clinical samples, detecting organisms missed during manual inspection. The 132 additional parasites identified across supposedly negative samples highlight a critical limitation of conventional microscopy and present an opportunity to improve diagnostic accuracy in clinical settings.
Implications for Parasitology Research
The integration of AI-powered microscopy represents a paradigm shift in parasitology research, enabling high-content imaging and automated analysis of parasite morphology, development, and host-pathogen interactions [90]. By combining high-content imaging with machine learning classification, researchers can now robustly differentiate asexual blood stages of parasites like Plasmodium falciparum and enumerate subcellular structures with minimal human intervention [90].
For drug development pipelines, this technology enables high-throughput compound screening with detailed phenotypic characterization. The ability to automatically discern parasite stages and quantify morphological changes facilitates the identification of novel therapeutic targets and assessment of compound efficacy [90]. Furthermore, AI-driven analysis can detect subtle phenotypic changes that might be missed by human observers, potentially accelerating the discovery of new antiparasitic agents.
Technical Advantages of AI Implementation
The YAC-Net architecture's performance stems from its efficient design choices. The asymptotic feature pyramid network (AFPN) enables more comprehensive integration of spatial contextual information compared to traditional FPN structures, while the C2f module in the backbone network enhances gradient flow and feature extraction capability [58]. These architectural improvements allow the model to maintain high detection accuracy while reducing computational requirements—a critical consideration for deployment in field settings with limited resources.
The model's proficiency in identifying parasites in low-resolution and blurred images further enhances its practical utility in real-world diagnostics, where image quality may be compromised by equipment limitations or sample preparation artifacts [58].
Integration with Existing Workflows
A key consideration for implementing AI-based detection systems is their seamless integration with established laboratory workflows. The methodology described in this case study complements rather than replaces existing techniques, providing a validation layer that enhances diagnostic accuracy without requiring complete overhaul of current practices. This approach is particularly valuable in settings where transition to fully automated systems may be constrained by economic or infrastructural limitations.
Future Directions
The demonstrated success of AI in identifying missed parasites suggests several promising research directions. Further development of multi-parasite detection systems capable of identifying diverse species in mixed infections would enhance diagnostic comprehensiveness. Additionally, integration of telemedicine platforms with AI analysis could facilitate expert consultation and quality assurance in remote settings.
For basic research, the application of similar AI approaches to continuous single-cell imaging of dynamic processes in parasites, as recently demonstrated for Plasmodium falciparum-infected erythrocytes, opens new avenues for investigating parasite biology with unprecedented temporal and spatial resolution [32].
Experimental Protocols
Protocol 1: AI-Assisted Parasite Detection in Microscopy Images
Purpose
To detect and quantify parasite eggs in microscopy images using the YAC-Net deep learning model, particularly focusing on identification of parasites missed during manual inspection.
Materials
- Pre-trained YAC-Net model weights
- Microscope with digital imaging capability (20× and 40× objectives)
- Stained stool sample slides
- Computer with GPU acceleration (minimum 4GB VRAM)
- Image acquisition software
Procedure
Image Acquisition
- Capture digital images of microscope slides at 20× magnification for initial screening
- For suspicious or negative samples, acquire additional images at 40× magnification
- Ensure consistent lighting and focus across all images
- Save images in lossless format (TIFF or PNG)
Image Pre-processing
- Resize images to 512 × 512 pixels while maintaining aspect ratio
- Apply contrast-limited adaptive histogram equalization (CLAHE)
- Normalize pixel values to [0,1] range
- For color images, convert to RGB format
Model Inference
- Load YAC-Net model with pre-trained weights
- Process each image through the network
- Apply confidence threshold of 0.5 for detection
- Retain detection coordinates and confidence scores
Result Interpretation
- Overlay detection bounding boxes on original images
- Categorize detections by parasite species based on model classification
- Flag samples with detections for expert verification
- Generate detection report with quantitative metrics
Expected Results
- The protocol should identify parasite eggs with approximately 97.8% precision and 97.7% recall
- In samples previously classified as negative by manual inspection, the protocol typically identifies 2-3 additional parasites per 100 samples
- Processing time should average 0.8 minutes per sample
Protocol 2: Validation of AI-Detected Parasites
Purpose
To verify parasites identified by AI system that were missed during initial manual inspection.
Materials
- Microscope with 100× oil immersion objective
- Sample slides with AI-identified parasites
- Verification checklist
- Digital camera for documentation
Procedure
Blinded Review
- Present verification slides to expert microscopist without indicating AI detection locations
- Request comprehensive examination of entire slide
- Document all identified parasites
Targeted Examination
- Direct microscopist to specific coordinates of AI detections
- Evaluate morphological characteristics of suspected parasites
- Classify based on established taxonomic criteria
Consensus Validation
- For discordant findings, involve second expert microscopist
- Reach consensus on questionable identifications
- Document final determination with supporting images
Expected Results
- Approximately 96% of AI-identified "missed" parasites should be confirmed by expert review
- The majority of false positives are typically due to staining artifacts or debris
- Validation time averages 5-7 minutes per disputed detection
Visualizations
AI-Assisted Parasite Detection Workflow
YAC-Net Model Architecture
The drug discovery process is notoriously lengthy, expensive, and prone to failure, traditionally taking 10-15 years and costing over $2 billion per approved drug [91]. More than 90% of drug candidates fail during clinical development, with a significant proportion of failures attributed to poor efficacy, safety issues, or unfavorable biopharmaceutical properties [92]. In recent years, artificial intelligence has emerged as a transformative force across this pipeline, promising to enhance efficiency, reduce costs, and improve success rates [93] [94].
This paradigm shift holds particular significance for neglected diseases such as parasitic infections. AI-driven approaches are enabling researchers to identify novel drug targets, design optimized compounds, and streamline development processes for diseases that have historically received limited research investment [12]. This application note provides a comparative analysis of AI-assisted versus traditional drug discovery methodologies, with specific emphasis on applications in parasitic disease research, and offers detailed experimental protocols for implementation.
Comparative Analysis of Key Performance Metrics
Table 1: Quantitative Comparison of Traditional vs. AI-Assisted Drug Discovery Pipelines
| Performance Metric | Traditional Approach | AI-Assisted Approach | Key Improvements |
|---|---|---|---|
| Discovery Timeline | 5-7 years to clinical candidate [93] | 18-24 months to clinical candidate [93] | 70-80% reduction in early discovery phase [93] |
| Compound Screening | Hundreds to thousands of compounds synthesized and tested [95] | 10x fewer compounds synthesized (e.g., 136 vs. thousands) [93] | Highly targeted candidate selection |
| Cost Efficiency | ~$2.8 billion total development cost [91] | Significant reduction in early R&D costs | Lower preclinical attrition |
| Clinical Success Rate | ~10% from Phase I to approval [91] | Too early for definitive data | Potential for improved predictive accuracy |
| Target Identification | Literature review, bioinformatics data mining [96] | AI analysis of vast datasets (genomic, proteomic, patient data) [95] | Novel target discovery, especially for neglected diseases |
Table 2: Applications in Parasitic Disease Research
| Research Area | Traditional Methods | AI-Enhanced Methods | Specific Examples |
|---|---|---|---|
| Target Identification | Laborious experimental validation | Predictive modeling of essential parasitic proteins | DeepMind predicted protein structures in Trypanosoma [12] |
| Compound Screening | In vitro screening against parasites | AI-virtual screening with machine learning | LabMol-167 identified as PK7 inhibitor with antiplasmodial activity [12] |
| Mode of Action | Lengthy biochemical studies | AI-powered image analysis and pattern recognition | Cell painting with ML pattern recognition for antimalarials [43] |
| Drug Repurposing | Serendipitous discovery or trial-and-error | Systematic analysis of drug-target interactions | "Eve" AI identified fumagillin's antiplasmodial potential [12] |
AI-Powered Image Analysis in Parasitic Disease Research
Experimental Protocol: AI-Based Morphological Profiling for Antimalarial Compound Screening
Principle: This protocol utilizes AI-powered image analysis to rapidly determine the mode of action (MoA) of potential antimalarial compounds through morphological profiling of parasite cells, significantly accelerating the early discovery process [43].
Materials and Reagents:
- Plasmodium falciparum cultures (asexual blood stages)
- Test compounds (library or individual molecules)
- Staining solution: Cell-permeable fluorescent dyes (e.g., Hoechst 33342 for DNA, MitoTracker for mitochondria, etc.)
- 96-well or 384-well imaging plates
- Cell culture reagents (RPMI 1640, human serum, Albumax)
- High-content imaging system with environmental control
- AI-based image analysis software (e.g., custom platform based on LPIXEL technology) [43]
Procedure:
- Parasite Culture and Compound Treatment:
- Maintain P. falciparum cultures in human erythrocytes at 2% hematocrit in complete RPMI 1640 medium.
- Synchronize cultures to ring stage using sorbitol treatment.
- Dispense 100 μL of synchronized parasite culture (at 2% parasitemia) into each well of imaging plates.
- Add test compounds across a range of concentrations (typically 8-point, 1:3 serial dilution), including controls (DMSO for negative control, known antimalarials for reference profiles).
- Incubate plates at 37°C in a humidified gas mixture (5% O₂, 5% CO₂, 90% N₂) for 48 hours to complete one asexual cycle.
Cell Staining and Fixation:
- After incubation, add 100 μL of staining solution containing multiple fluorescent dyes to each well.
- Incubate for 45 minutes at 37°C protected from light.
- Fix cells by adding 50 μL of 4% paraformaldehyde solution for 15 minutes at room temperature.
- Wash plates twice with 100 μL PBS per well.
High-Content Image Acquisition:
- Image plates using a high-content imaging system with a 40x or 60x objective.
- Acquire images from multiple sites per well (minimum 6 sites) to ensure adequate cell numbers.
- Capture multiple channels corresponding to each fluorescent probe.
- Export images in standard format (e.g., TIFF) with appropriate metadata.
AI-Based Image Analysis:
- Upload images to the AI analysis platform (cloud-based or local installation).
- Run pre-trained convolutional neural network (CNN) models for parasite segmentation and feature extraction.
- The AI model will:
- Identify and segment individual parasites
- Extract morphological features (size, shape, texture, intensity)
- Compare profiles to reference compound database
- Generate MoA predictions and similarity scores.
Data Interpretation:
- Review the AI-generated MoA classification report.
- Compounds with similar morphological profiles to known references will cluster together.
- Prioritize compounds with novel profiles or desired MoAs for further validation.
Troubleshooting Tips:
- Poor image quality: Optimize staining concentrations and exposure times.
- Low cell numbers: Increase seeding density or number of imaging sites.
- Inconsistent results: Ensure culture synchronization and compound solubility.
Figure 1: AI-Powered Parasite Image Analysis Workflow
Research Reagent Solutions for AI-Driven Parasite Research
Table 3: Essential Research Reagents and Platforms
| Reagent/Platform | Function | Application in Parasite Research |
|---|---|---|
| LPIXEL AI Image Analysis | AI-powered pattern recognition for microscopic images | Automated analysis of parasite morphology and compound effects [43] |
| DeepMalaria (Graph CNN) | Deep learning for identifying antimalarial compounds | Screening chemical libraries for antiplasmodial activity [12] |
| Cell Painting Assay Kits | Multiplexed fluorescent staining for morphological profiling | Generating rich morphological data for MoA determination [43] |
| pQSAR Platform | Machine learning-based quantitative structure-activity relationship | Predicting compound activity against parasitic targets [12] |
| AlphaFold | AI-based protein structure prediction | Modeling parasitic protein targets for drug design [94] |
| ADMETlab 2.0 | AI platform for predicting ADMET properties | Optimizing drug-like properties of antiparasitic candidates [92] |
Comparative Workflow Analysis
Figure 2: Timeline Comparison of Discovery Pipelines
The integration of artificial intelligence into drug discovery pipelines represents a paradigm shift with particular significance for neglected tropical diseases such as parasitic infections. As demonstrated in this analysis, AI-assisted approaches can dramatically compress discovery timelines from 5-7 years to 18-24 months for the early discovery phases, while simultaneously improving the efficiency of compound selection and optimization [93].
The application of AI-powered image analysis for parasitic disease research, as exemplified by the MMV/LPIXEL/University of Dundee partnership, demonstrates how these technologies can specifically address challenges in global health research [43]. By automating and accelerating mode-of-action determination through morphological profiling, researchers can prioritize the most promising candidates more rapidly and cost-effectively.
While AI-assisted drug discovery continues to evolve and faces challenges related to data quality, model interpretability, and regulatory acceptance [94] [5], the current progress indicates a fundamental transformation in how we approach pharmaceutical development, particularly for diseases that have historically suffered from insufficient research investment. The integration of these technologies promises not only faster and more efficient drug discovery but also the potential to address unmet medical needs in neglected disease areas.
Application Note: AI-Powered Microscopy for Parasitology
This document provides application notes and detailed protocols for implementing artificial intelligence (AI) solutions in parasite image analysis research. The content is designed for researchers, scientists, and drug development professionals seeking to augment their expertise with AI to enhance diagnostic accuracy, accelerate drug discovery, and deepen fundamental biological insights.
AI for Diagnostic Detection and Species Differentiation in Blood Smears
The application of edge AI on standard smartphones attached to microscopes enables real-time, high-accuracy detection and quantification of parasitic pathogens in field and clinical settings [78] [14].
Experimental Protocol: Real-Time Detection of Bloodborne Parasites
Objective: To detect and differentiate parasite species in blood smears in real-time using a smartphone-based edge AI system without requiring internet connectivity [78].
Materials & Equipment:
- Biological Samples: Human blood samples (thin/thick smears, cerebrospinal fluid) [14].
- Microscope: Standard optical microscope.
- Smartphone: Mid-range Android or iOS device with camera.
- Adapter: 3D-printed device to align smartphone camera with microscope ocular [78] [14].
- AI Model: Pre-trained Single-Shot Detection (SSD) MobileNet V2 or YOLOv8 model deployed on the smartphone [78] [14].
Procedure:
- Sample Preparation: Prepare blood smears or cerebrospinal fluid smears using standard laboratory protocols [14].
- System Setup: Attach the smartphone to the microscope's eyepiece using the 3D-printed adapter to ensure stable alignment.
- Image Digitization: Use the smartphone camera application to view the slide through the microscope. The system captures a live video feed.
- AI-Assisted Screening:
- Result Interpretation: The AI system displays bounding boxes around detected parasites in real-time on the smartphone screen, along with species classification and confidence scores.
Validation: A clinical validation study of this protocol for filariasis diagnosis achieved an overall precision of 94.14% and recall of 91.90% for the screening algorithm, and precision of 95.46% and recall of 97.81% for species differentiation [78].
Table 1: Performance Metrics of AI Models for Parasite Detection
| Parasite / Disease | AI Model Architecture | Key Performance Metrics | Reference |
|---|---|---|---|
| Four Filarial Species(Loa loa, M. perstans, W. bancrofti, B. malayi) | SSD MobileNet V2 | Screening: Precision=94.14%, Recall=91.90%, F1=93.01%Differentiation: Precision=95.46%, Recall=97.81%, F1=96.62% | [78] |
| Trypanosoma cruzi(Chagas Disease) | SSD MobileNet V2 | Precision=86.0%, Recall=87.0%, F1-score=86.5% (Human samples) | [14] |
| Trypanosoma cruzi(Chagas Disease) | YOLOv8 | Performance metrics reported, specific values detailed in source data. | [14] |
AI for High-Content Analysis in Antimalarial Drug Discovery
AI-powered image analysis accelerates drug discovery by providing rapid insights into a compound's biological impact and mode of action (MoA) [43].
Experimental Protocol: Cell Painting for Mode of Action Analysis
Objective: To utilize AI-powered image analysis of stained parasite cells (cell painting) to understand a compound's biological impact and predict its MoA early in the discovery pipeline [43].
Materials & Equipment:
- Biological Samples: Plasmodium falciparum cultures.
- Compounds: Library of small molecules for screening.
- Stains: Fluorescent dyes for cell painting (e.g., multiplexed dye set targeting various cellular compartments).
- Imaging Equipment: High-content imaging system or automated microscope.
- AI Platform: Cloud-based, user-friendly application for AI image analysis (e.g., custom platform from LPIXEL, University of Dundee, and MMV partnership) [43].
Procedure:
- Compound Treatment: Treat asynchronous P. falciparum cultures with compounds from the library across a range of concentrations and time points.
- Staining and Fixation: Fix cells and stain with a panel of fluorescent dyes to label various cellular structures (e.g., nucleus, cytoskeleton, membranes).
- Image Acquisition: Acquire high-resolution images of the stained parasites using a high-content imaging system.
- AI Image Analysis: Upload images to the cloud-based AI platform. The AI employs machine learning pattern recognition to:
- Extract morphological features from the stained cells.
- Compare the morphological "fingerprint" induced by the test compound to a database of fingerprints from compounds with known MoAs.
- MoA Prediction: The platform provides a hypothesis for the compound's MoA based on morphological similarity to known references.
Outcome: This protocol can save months in the drug discovery process by providing MoA insights much earlier, facilitating the selection of promising candidates with novel mechanisms for further development [43].
AI for Structural and Motility Analysis at Atomic Resolution
Advanced imaging combined with AI modeling is revealing unprecedented details of parasite structures, opening new avenues for therapeutic intervention.
Experimental Protocol: Mapping Parasite Flagella using Cryo-EM and AI
Objective: To determine the atomic-level structure of the parasite flagellum to understand its motility and identify potential therapeutic targets [66].
Materials & Equipment:
- Biological Sample: Purified Trypanosoma brucei parasites.
- Equipment: Cryogenic-electron microscope (cryo-EM).
- Software: AI-driven structural modeling and analysis software (e.g., AlphaFold2 or similar algorithms for protein structure prediction) [66].
Procedure:
- Sample Vitrification: Purify T. brucei and rapidly freeze the sample in liquid ethane to form a thin layer of vitreous ice, preserving native structure.
- Cryo-EM Data Collection: Collect thousands of high-resolution, two-dimensional micrograph images of the flagella at various angles using the cryo-EM.
- 3D Reconstruction: Use computational methods to reconstruct a 3D density map from the 2D micrographs.
- AI-Driven Atomic Modeling: Apply AI algorithms to interpret the 3D density map and build an atomic model:
- The AI predicts protein structures based on amino acid sequences.
- These predictions are fitted into the cryo-EM density map to identify and place individual proteins.
- Structural Analysis: Analyze the composite model to identify key structural components, unique parasite-specific proteins, and the molecular organization driving motility.
Key Finding: This protocol revealed a structural blueprint of 154 composite proteins in the T. brucei flagellum, including 40 unique to the parasite, and proposed a "dragon boat" model for its coordinated movement [66].
Table 2: Essential Research Reagent Solutions for AI-Powered Parasitology
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| 3D-Printed Smartphone Adapter | Enables image digitization by aligning smartphone camera with microscope ocular. | Field-based detection of T. cruzi [14] and filarial worms [78]. |
| SSD MobileNet V2 / YOLOv8 Models | Lightweight, pre-trained AI models for real-time object detection on mobile devices (edge AI). | Real-time parasite detection and counting on a smartphone without internet [78] [14]. |
| Cell Painting Fluorescent Dyes | A multiplexed panel of stains that label multiple cellular organelles to create a morphological fingerprint. | Profiling compound-induced morphological changes in P. falciparum for MoA prediction [43]. |
| Cryo-EM Grids | Support grids for holding vitrified biological samples in the electron beam path. | Preparing samples for atomic-level imaging of T. brucei flagella [66]. |
| AI-Based Structural Modeling Software | Algorithms for predicting protein structure and fitting models into cryo-EM density maps. | Determining the atomic structure of the T. brucei flagellum from cryo-EM data [66]. |
Conclusion
The integration of artificial intelligence into parasitic image analysis marks a pivotal shift, offering a powerful toolkit to overcome longstanding challenges in diagnostics and drug development. By leveraging deep learning models, researchers can achieve unprecedented accuracy and speed in parasite detection, significantly accelerate the discovery of novel therapeutics with new modes of action, and gain predictive insights into disease outbreaks. Future progress hinges on collaborative efforts to create diverse, high-quality datasets, develop standardized and open-access AI platforms, and foster interdisciplinary partnerships between computer scientists and parasitologists. Embracing this 'Augmented Intelligence' paradigm will not only enhance laboratory efficiency but also profoundly impact global health outcomes by enabling faster, more precise interventions against parasitic diseases.
References
- 1. Deep learning-based malaria parasite detection [https://www.nature.com/articles/s41598-025-87979-5]
- 2. Antimalarial drug resistance [https://www.mmv.org/our-work/antimalarial-drug-resistance]
- 3. Novartis Phase III trial for next-generation malaria ... [https://www.novartis.com/news/media-releases/novartis-phase-iii-trial-next-generation-malaria-treatment-klu156-ganlum-meets-primary-endpoint-potential-combat-antimalarial-resistance]
- 4. iMAGING: a novel automated system for malaria diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10704928/]
- 5. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 6. AI-supported Microscopy Enhances the Detection of Intestinal ... [https://communities.springernature.com/posts/ai-supported-microscopy-enhances-the-detection-of-intestinal-parasitic-infections-in-primary-healthcare]
- 7. Why 90% of clinical drug development fails and how to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9293739/]
- 8. High content screening for drug discovery from traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6394041/]
- 9. High-content screening in drug discovery: A brief guide [https://alitheagenomics.com/blog/high-content-screening-in-drug-discovery-a-brief-guide]
- 10. Advanced imaging techniques for tracking drug dynamics ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X23002934]
- 11. 5 common data management problems affecting drug discovery [https://www.drugdiscoverytrends.com/5-common-data-management-problems-affecting-drug-discovery/]
- 12. Artificial intelligence in parasitic disease control: A paradigm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10911181/]
- 13. AI Diagnostics Boost Parasite Detection Accuracy [https://www.technologynetworks.com/informatics/news/ai-outperforms-traditional-methods-for-detecting-parasites-in-stool-samples-406080]
- 14. Artificial Intelligence algorithm for real-time detection and ... [https://www.medrxiv.org/content/10.1101/2025.03.03.25323227v1.full-text]
- 15. New AI system could accelerate clinical research [https://news.mit.edu/2025/new-ai-system-could-accelerate-clinical-research-0925]
- 16. Top AI Medical Imaging tools for Healthcare Analytics - 2025 [https://www.factspan.com/blogs/ai-medical-imaging-tools-transforming-healthcare-analytics-in-2025/]
- 17. Artificial intelligence (AI)-driven rapid diagnostic test ... [https://bmcdigitalhealth.biomedcentral.com/articles/10.1186/s44247-025-00197-x]
- 18. Automated multi-model framework for malaria detection ... [https://www.nature.com/articles/s41598-025-04784-w]
- 19. Global impact of parasitic infections and the importance ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1546195/full]
- 20. Explainable AI for early malaria detection using stacked ... [https://www.sciencedirect.com/science/article/pii/S2352914825000553]
- 21. AI and citizen science reveal potential first detection ... [https://www.usf.edu/arts-sciences/chronicles/2025/ai-and-citizen-science-reveal-potential-first-detection-of-invasive-malaria-mosquito-in-madagascar.aspx]
- 22. Parasitic diagnosis: A journey from basic microscopy to cutting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617590/]
- 23. Optimized CNN framework for malaria detection using Otsu ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623931/]
- 24. Enhancing malaria detection and classification using ... [https://link.springer.com/article/10.1007/s42452-025-06704-z]
- 25. DANet a lightweight dilated attention network for malaria ... [https://www.nature.com/articles/s41598-025-20402-1]
- 26. An innovative approach to parasite classification in ... [https://www.sciencedirect.com/science/article/abs/pii/S0952197625000144]
- 27. Loss and Loss Functions for Training Deep Learning ... [https://www.machinelearningmastery.com/loss-and-loss-functions-for-training-deep-learning-neural-networks/]
- 28. Sensitive near point-of-care detection of asymptomatic and ... [https://www.nature.com/articles/s41467-025-64027-4]
- 29. Detection of protozoan and helminth parasites in concentrated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607898/]
- 30. Use of Artificial Intelligence and Digital Slide Scanning for ... [https://news.mayocliniclabs.com/2023/06/05/use-of-artificial-intelligence-and-digital-slide-scanning-for-detection-of-intestinal-protozoa-in-trichrome-stained-stool-specimens/]
- 31. Fusion Parasitology Suite [https://techcyte.com/products/fusion-parasitology-suite/]
- 32. Deep learning image analysis for continuous single-cell ... [https://www.nature.com/articles/s42003-025-07894-3]
- 33. An Image Analysis Algorithm for Malaria Parasite Stage ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0061812]
- 34. Frontiers | Automated detection of pinworm parasite eggs using YOLO... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1559987/full]
- 35. AI Blood Smear Analysis - Vetscan Imagyst - HelpDocs [https://vetscanimagyst.helpdocs.io/l/en/category/dlz6wzp87t-ai-blood-smear]
- 36. Integrating Generative AI with High-Throughput Screening ... [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5317101]
- 37. Transforming the landscape of parasitology - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/40492595/]
- 38. The State of AI: Global Survey 2025 [https://www.mckinsey.com/capabilities/quantumblack/our-insights/the-state-of-ai]
- 39. Toward Stable Zinc Anode: An AI-Assisted High ... [https://pubmed.ncbi.nlm.nih.gov/40762030/]
- 40. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 41. An artificial intelligence-based approach for human ... [https://www.sciencedirect.com/science/article/pii/S2772442525000516]
- 42. America's AI Action Plan: Implications for ... [https://itif.org/publications/2025/09/08/americas-ai-action-plan-implications-for-biopharmaceutical-innovation/]
- 43. MMV announces new partnership using AI-powered image ... [https://www.mmv.org/newsroom/news-resources-search/mmv-announces-new-partnership-using-ai-powered-image-analysis]
- 44. Cell Painting: A Decade of Discovery and Innovation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11810604/]
- 45. High-throughput screening and meta-analysis for lead ... [https://malariajournal.biomedcentral.com/articles/10.1186/s12936-025-05587-0]
- 46. Predicting mosquito-borne disease outbreaks using ... [https://www.sciencedirect.com/science/article/pii/S1876034125002552]
- 47. High-content imaging as a tool to quantify and characterize ... [https://www.sciencedirect.com/science/article/pii/S2667237523001455]
- 48. A validation study of microscopy versus quantitative PCR for ... [https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-019-0176-3]
- 49. Technology to advance infectious disease forecasting for ... [https://www.nature.com/articles/s41467-019-11901-7]
- 50. Image-Based Detection and Classification of Malaria ... [https://www.mdpi.com/1424-8220/25/2/390]
- 51. Hybrid Capsule Network for precise and interpretable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370641/]
- 52. Comparative Evaluation of Deep Learning Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943284/]
- 53. Adversarial Machine Learning: Understanding and ... [https://www.obsidiansecurity.com/blog/adversarial-machine-learning]
- 54. AI 100-2 E2025, Adversarial Machine Learning: A Taxonomy ... [https://csrc.nist.gov/pubs/ai/100/2/e2025/final]
- 55. Protect Your AI Models from Adversarial Attacks [https://www.refontelearning.com/blog/protect-your-ai-models-from-adversarial-attacks-advanced-strategies-for-2025]
- 56. AI Surpasses Humans in Parasite Detection, Utah Study [https://www.miragenews.com/ai-surpasses-humans-in-parasite-detection-utah-1556014/]
- 57. Robustness in AI-Generated Detection: Enhancing ... [https://arxiv.org/html/2505.03435v1]
- 58. A lightweight deep-learning model for parasite egg detection ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-024-06503-2]
- 59. 16 Best Free Human Annotated Datasets for Machine ... [https://www.iguazio.com/blog/best-free-human-annotated-datasets-for-ml/]
- 60. AI in Research: Its Uses and Limitations [https://www.researchtoaction.org/2024/04/ai-in-research-its-uses-and-limitations/]
- 61. Precise detection of Eimeria oocysts in sheep - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613407/]
- 62. Enhancing parasitic organism detection in microscopy ... [https://www.nature.com/articles/s41598-024-56323-8]
- 63. Optimized CNN framework for malaria detection using Otsu ... [https://www.nature.com/articles/s41598-025-23961-5]
- 64. Harnessing the power of microscope images to accelerate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7521136/]
- 65. AI In clinical trials in 2025: the edge of tech [https://clinicaltrialrisk.org/clinical-trial-design/ai-in-clinical-trials-the-edge-of-tech/]
- 66. Atomic imaging and AI offer new insights into motion of ... [https://cnsi.ucla.edu/march-19-2025-atomic-imaging-and-ai-offer-new-insights-into-motion-of-parasite-behind-sleeping-sickness/]
- 67. Artificial Intelligence in Clinical Trials: Balancing Innovation ... [https://acrpnet.org/2025/06/16/artificial-intelligence-in-clinical-trials-balancing-innovation-and-accuracy]
- 68. Principles for Designing and Developing a Workflow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8769810/]
- 69. Artificial Intelligence and the future of clinical trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490578/]
- 70. The Artificial Intelligence Disclosure (AID) Framework [https://crln.acrl.org/index.php/crlnews/article/view/26548/34482]
- 71. An Efficient Deep Learning Approach for Malaria Parasite ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11639908/]
- 72. Advances and challenges in automated malaria diagnosis ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1006659/full]
- 73. Self-supervised learning for data augmentation in ... [https://www.nature.com/articles/s41598-025-23280-9]
- 74. Data Augmentation: The Ultimate Guide for 2025 [https://www.ultralytics.com/blog/the-ultimate-guide-to-data-augmentation-in-2025]
- 75. MDEU-Net: Medical Image Segmentation Network Based ... [https://www.mdpi.com/1424-8220/25/9/2917]
- 76. VQualA 2025 Challenge on Image Super-Resolution ... [https://arxiv.org/html/2509.06413v1]
- 77. AI-powered microscopy image analysis for parasitology [https://www.sciencedirect.com/science/article/abs/pii/S147149222400134X]
- 78. Edge Artificial Intelligence (AI) for real-time automatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11057975/]
- 79. AI Performance Metrics: The Science & Art of Measuring AI [https://www.version1.com/en-us/blog/ai-performance-metrics-the-science-and-art-of-measuring-ai/]
- 80. How to evaluate the performance of AI research? [https://pmc.ncbi.nlm.nih.gov/articles/PMC11141501/]
- 81. AI Metrics: How to Measure and Evaluate AI Performance [https://sendbird.com/blog/ai-metrics-guide]
- 82. Augmented reality microscopy to bridge trust between AI ... [https://www.nature.com/articles/s41698-025-00899-5]
- 83. Challenges Across Diagnostic Imaging, Clinical Decision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468291/]
- 84. KPIs for gen AI: Measuring your AI success [https://cloud.google.com/transform/gen-ai-kpis-measuring-ai-success-deep-dive]
- 85. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 86. Sensitivity and specificity | Description, Uses, & Examples [https://www.britannica.com/science/sensitivity-medical-statistics]
- 87. Sensitivity and Specificity - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/sensitivity-and-specificity]
- 88. Ensemble Machine Learning for Malaria Diagnosis in ... [https://www.medrxiv.org/content/10.1101/2025.08.03.25332923v1.full-text]
- 89. a meta-analysis and systematic review [https://dirjournal.org/articles/diagnostic-sensitivity-and-specificity-of-enhanced-computed-tomography-in-colorectal-tumors-a-meta-analysis-and-systematic-review/dir.2025.243185]
- 90. High-content imaging as a tool to quantify and characterize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10391350/]
- 91. Drug Discovery and Development: A Step-By-Step Process [https://www.zeclinics.com/blog/drug-discovery-and-development-process]
- 92. Artificial Intelligence-driven Strategies and Modern ... [https://www.xiahepublishing.com/m/2572-5505/JERP-2025-00025]
- 93. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 94. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 95. How AI is taking over every step of drug discovery - C&EN [https://cen.acs.org/physical-chemistry/computational-chemistry/AI-taking-over-step-drug/103/web/2025/10]
- 96. Traditional Drug Development Process - The Actuary Magazine [https://www.theactuarymagazine.org/traditional-drug-development-process/]