Formalin-Ethyl Acetate Concentration Technique (FECT): A Comprehensive Guide for Enhanced Stool Parasitology
This article provides a comprehensive analysis of the Formalin-Ethyl Acetate Concentration Technique (FECT), a cornerstone diagnostic method in clinical parasitology.
Formalin-Ethyl Acetate Concentration Technique (FECT): A Comprehensive Guide for Enhanced Stool Parasitology
Abstract
This article provides a comprehensive analysis of the Formalin-Ethyl Acetate Concentration Technique (FECT), a cornerstone diagnostic method in clinical parasitology. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of fecal concentration, delivers a detailed procedural methodology, and addresses common troubleshooting scenarios. Furthermore, it synthesizes recent validation studies comparing FECT's performance against alternative diagnostic methods, including emerging AI-powered microscopy, and discusses its critical role in public health interventions and antimicrobial development. The content is informed by current peer-reviewed literature and established guidelines from leading health authorities to ensure scientific rigor and practical applicability.
Principles and Rationale of Stool Concentration in Parasite Diagnosis
The Critical Role of FECT in Global Intestinal Parasitic Infection (IPI) Control
Global Burden of Intestinal Parasitic Infections
Intestinal parasitic infections pose a significant global health challenge, affecting over a billion people worldwide [1]. These infections are among the most common infections globally, with an estimated 3.5 billion people affected and more than 200,000 deaths annually [2]. The World Health Organization reports that approximately 1.5 billion people, representing 24% of the world's population, are infected with soil-transmitted helminths alone [1]. Developing countries, particularly those in tropical and subtropical regions, bear the highest burden of these infections [3].
The impact of IPIs extends beyond morbidity and mortality, significantly affecting physical and intellectual development while exacerbating nutritional deficiencies in early childhood [3]. A recent systematic review and meta-analysis revealed that the pooled prevalence of IPIs among colorectal cancer patients was 19.67% globally, with parasitic infections associated with a significantly higher likelihood of developing colorectal cancer [4]. Food handlers have been identified as potential carriers, with studies in Ethiopia showing a 33.5% prevalence of intestinal parasites among this group [5].
Table 1: Global Prevalence and Impact of Common Intestinal Parasites
| Parasite Category | Representative Species | Global Prevalence/Impact | Primary At-Risk Populations |
|---|---|---|---|
| Soil-transmitted helminths | Ascaris lumbricoides, Trichuris trichiura, Hookworms | 1.5 billion people affected [1] | Children in developing countries [3] |
| Intestinal protozoa | Giardia lamblia, Cryptosporidium spp., Entamoeba histolytica | 352 million infections [2] | Immunocompromised individuals, children [1] |
| Zoonotic parasites | Toxoplasma gondii, Leishmania species | Up to 1/3 of world population infected with T. gondii [6] | Pet owners, immunocompromised patients [6] |
FECT Diagnostic Performance and Advantages
The Formalin-Ethyl Acetate Concentration Technique has established itself as a superior diagnostic method for intestinal parasitic infections compared to direct microscopic examination. Recent hospital-based cross-sectional studies demonstrate that FECT detected parasites in 75% of cases, significantly outperforming both Formol-Ether Concentration (62%) and direct wet mount techniques (41%) [3]. This enhanced detection capability is particularly valuable in settings where accurate diagnosis directly impacts treatment decisions and public health interventions.
The technical superiority of FECT lies in its concentration mechanism, which enhances the detection of low-level infections that might be missed by direct methods [2]. The process involves emulsifying stool specimens in formalin, which fixes the parasites, followed by the addition of ethyl acetate which acts as an extractor of fats, oils, and other debris. Subsequent centrifugation yields a clean sediment concentrate rich in parasitic elements, substantially improving microscopic detection [7]. This method is especially effective for identifying protozoan cysts, helminth eggs, and larvae, with studies showing particular efficacy in detecting Blastocystis hominis, Entamoeba histolytica, and Giardia lamblia [3].
FECT's practical advantages extend beyond diagnostic sensitivity to encompass operational benefits that make it particularly suitable for resource-limited settings. The technique requires minimal infrastructure and is cost-effective compared to molecular methods, while simultaneously providing better quantitative capabilities through the calculation of eggs per gram (EPG) of feces to determine infection intensity [7]. Furthermore, the use of formalin for fixation allows specimens to be preserved for extended periods, facilitating batch processing and transportation from remote collection sites to central laboratories [2].
Table 2: Comparative Performance of Stool Examination Techniques
| Diagnostic Method | Detection Rate | Key Advantages | Limitations |
|---|---|---|---|
| Direct Wet Mount | 41% [3] | Rapid, low cost, requires minimal equipment | Low sensitivity, requires immediate examination |
| Formol-Ether Concentration (FEC) | 62% [3] | Better detection than direct mount, preserves specimens | Lower sensitivity compared to FECT |
| FECT | 75% [3] | Highest sensitivity, quantitative capability (EPG), safe and feasible for rural settings [3] [7] | Requires centrifugation, more processing time |
| Molecular Methods | >90% sensitivity (varies) [2] | High sensitivity and specificity, species differentiation | High cost, requires specialized equipment and training |
| Deep-Learning-Based | Up to 98.93% accuracy [2] | Automated detection, high throughput, reduced human error | Requires technical infrastructure, initial setup costs |
Standardized FECT Protocol for Stool Specimens
Reagents and Materials
The following research reagent solutions and materials are essential for implementing the Formalin-Ethyl Acetate Concentration Technique:
Table 3: Essential Research Reagents and Materials for FECT Protocol
| Item | Specification/Concentration | Primary Function |
|---|---|---|
| Formalin | 10% solution in water | Fixation and preservation of parasitic elements |
| Ethyl Acetate | Laboratory-grade, 3 mL per sample | Extraction of fats, oils, and debris from stool specimens |
| Saline Solution | 0.85% NaCl or 0.9% NaCl | Suspension medium and diluent |
| Gauze | Two layers or specialized strainers | Filtration of large particulate matter |
| Centrifuge Tubes | Conical, 15 mL capacity | Container for concentration process |
| Centrifuge | Capable of 2,500 rpm | Separation of parasitic elements from debris |
| Microscope Slides and Coverslips | Standard glass slides | Preparation for microscopic examination |
| Iodine Solution | Lugol's or similar | Staining for enhanced visualization of structures |
Step-by-Step Procedure
Specimen Preparation: Emulsify approximately 1-2 grams of fresh stool in 7 mL of 10% formalin in a clean conical centrifuge tube. For fixed specimens, begin at step 3. Vigorously shake the specimen to ensure homogeneous suspension [7].
Fixation: Allow the formalin-stool mixture to stand for 10 minutes at room temperature to ensure complete fixation of parasitic elements [3].
Filtration: Strain the mixture through two layers of gauze or a specialized sieve into a new 15 mL conical centrifuge tube to remove large particulate matter and fiber [7].
Solvent Addition: Add 3 mL of ethyl acetate to the formalin solution [3]. Securely cap the tube and mix thoroughly by shaking vigorously for 15-20 seconds, venting carefully to release pressure.
Centrifugation: Centrifuge the mixture at 2,500 rpm for 5 minutes [7]. This step creates four distinct layers: a sediment containing parasitic elements at the bottom, a formalin layer, a fecal debris plug, and an ethyl acetate layer at the top.
Supernatant Removal: Carefully decant the top three layers (ethyl acetate, debris plug, and formalin), leaving the sediment undisturbed at the bottom of the tube [7].
Sediment Preparation: Re-suspend the remaining sediment with 1 mL of 10% formalin or saline solution by tapping the tube or using a vortex mixer at low speed [7].
Microscopic Examination: Transfer two drops of the final suspension to a glass slide, cover with a coverslip, and examine systematically under the microscope. Begin with 10× magnification for initial screening, followed by 40× magnification for detailed morphological assessment of parasitic elements [3].
Limitations and Future Directions in Parasitology Diagnostics
Despite its widespread utility, FECT presents several limitations that impact its effectiveness in comprehensive parasitology diagnostics. The technique demonstrates variable sensitivity for detecting protozoan parasites due to their smaller sizes and shared morphological characteristics, potentially leading to misidentification [2]. Additionally, FECT requires a well-equipped laboratory with centrifugation capabilities, consistent reagent quality, and trained personnel, which may not be readily available in all endemic settings [3]. The method's dependence on operator skill introduces inter-technician variability, with studies showing differences in detection rates between experienced parasitologists and less-trained personnel [2].
Emerging technologies are addressing these limitations through innovative approaches. Deep learning-based systems represent a significant advancement, with models like DINOv2-large demonstrating remarkable accuracy (98.93%), precision (84.52%), and sensitivity (78.00%) in intestinal parasite identification [2]. These artificial intelligence systems leverage convolutional neural networks and vision transformers to automate detection, reducing operator dependency and increasing throughput. Object detection approaches like YOLOv8-m have shown particular promise in identifying multiple parasites in a single image, potentially addressing the challenge of mixed infections [2].
The future of IPI control lies in integrated diagnostic strategies that combine the accessibility of conventional methods like FECT with the precision of advanced technologies. Molecular techniques such as PCR offer higher sensitivity and specificity for specific protozoan identification but remain impractical for routine use in resource-limited settings due to cost and technical requirements [1]. The developing field of hybrid diagnostics envisions a tiered approach where FECT serves as an initial screening tool in peripheral laboratories, with referral of challenging cases to centralized facilities equipped with molecular or AI-based systems [2]. This integrated model maximizes population coverage while maintaining diagnostic accuracy for treatment and surveillance purposes.
The Formalin-Ethyl Acetate Concentration Technique remains a cornerstone in the global effort to control intestinal parasitic infections, particularly in resource-limited settings where these infections are most prevalent. Its demonstrated superiority over direct examination methods, combined with its cost-effectiveness and practicality, ensures its continued relevance in both clinical and public health contexts. As diagnostic technologies evolve, FECT maintains its position as an essential component of integrated approaches to parasitology diagnostics, serving as a reliable bridge between traditional methods and emerging innovations in the ongoing effort to reduce the global burden of intestinal parasitic infections.
Within parasitological diagnostics, microscopic examination of stool specimens remains a cornerstone procedure for detecting intestinal parasites. The sensitivity of this examination is significantly enhanced through concentration techniques, which separate parasitic elements from fecal debris. The two principal methodological approaches—sedimentation and flotation—leverage the physical properties of specific gravity to achieve this goal. This application note delineates the core principles, comparative efficacies, and detailed protocols for these techniques, framed within ongoing research aimed at refining the formalin-ethyl acetate concentration technique (FECT) for stool specimens.
Core Principles and Physicochemical Basis
Concentration techniques are indispensable for diagnosing infections with low parasite burden, where direct smear examination may yield false-negative results. These methods are fundamentally based on differences in specific gravity between parasitic structures (cysts, ova, larvae) and fecal debris.
Sedimentation Principle: Sedimentation techniques utilize a liquid medium with a specific gravity lower than that of the target parasites. When subjected to centrifugal force, the parasitic forms, being denser, settle at the bottom of the tube, while lighter debris remains suspended or is separated. The formalin-ethyl acetate (FEA) method is a diphasic sedimentation technique. Formalin preserves parasitic structures, while ethyl acetate acts as a solvent to extract fats, dissolved sugars, and other debris, forming a plug at the top of the tube that is discarded. Sedimentation is considered easier to perform and less prone to technical errors, and it is recommended for the recovery of a broad spectrum of parasites, including operculated eggs and most trematode eggs that do not float well [8] [9].
Flotation Principle: In contrast, flotation techniques employ a solution with a specific gravity higher than that of the parasites. During centrifugation, the parasitic forms rise to the surface of the solution, where they can be collected for examination. Common flotation solutions include zinc sulfate and Sheather's sugar. The main advantage of this approach is the production of a cleaner material, facilitating microscopic examination. However, a significant disadvantage is that the walls of eggs and cysts can often collapse in hypertonic solutions, hindering identification. Furthermore, some parasite eggs do not float in standard flotation media [8] [10].
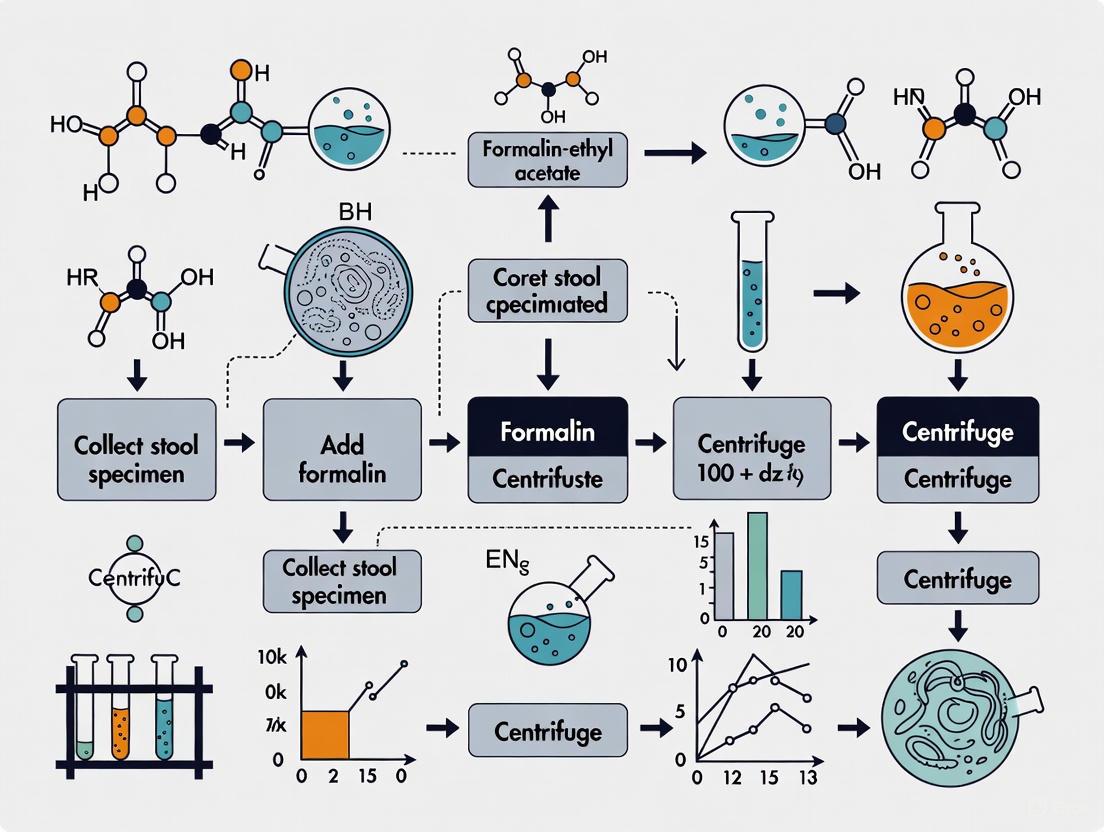
The following diagram illustrates the fundamental workflow and decision-making process in selecting a concentration method.
Comparative Efficacy: Quantitative Data Analysis
The choice between sedimentation and flotation significantly impacts diagnostic sensitivity. A summary of comparative studies is presented in the table below.
Table 1: Comparative Analytical Sensitivity of Sedimentation and Flotation Techniques for Various Parasites
| Parasite | Study / Context | Sedimentation Method | Flotation Method | Key Finding | Statistical Significance (P-value) |
|---|---|---|---|---|---|
| Cryptosporidium spp. | Large human outbreak (n=703) [11] | Formalin-Ethyl Acetate + MCK stain: 18.4% positive | Sheather Sucrose Flotation: 18.1% positive | High agreement between tests; discrepancies in low-density infections. | P < 0.0001 |
| Canine Intestinal Parasites (n=254) [10] | Centrifugation-Sedimentation | Centrifugation-Flotation | Flotation more accurate for Ancylostoma, T. canis, T. vulpis, Giardia. | P < 0.01 | |
| General Parasite Recovery [12] | Formalin-Ethyl Acetate Sedimentation | Zinc Sulfate Flotation | Sedimentation superior for selected ova; Flotation better for protozoan cysts, H. nana, hookworm. | Not Specified | |
| Intestinal Helminths (n=693) [13] | Formalin-Ethyl Acetate (FECT) | Crude Formalin Concentration (FC) | FECT superior for hookworm, Trichuris trichiura, small liver flukes. | Not Specified (sensitivity significantly higher) | |
| Giardia lamblia [11] | Formalin-Ethyl Acetate + Trichrome: 17.9% positive | Sheather Sucrose Flotation: 6.0% positive | Sedimentation significantly more effective for recovering Giardia. | Not Specified |
Experimental Protocols
Detailed Protocol: Formalin-Ethyl Acetate Sedimentation (CDC Standard)
The formalin-ethyl acetate sedimentation technique is a widely adopted standard for general parasitology due to its broad efficacy [8] [13].
Table 2: Research Reagent Solutions for Formalin-Ethyl Acetate Sedimentation
| Reagent/Material | Function / Explanation |
|---|---|
| 10% Buffered Formalin | Preservative that fixes and preserves parasitic structures (cysts, ova, larvae) for microscopy. |
| Ethyl Acetate | Solvent that dissolves fats, removes debris, and reduces odor. A safer substitute for diethyl ether. |
| Saline (0.85%) or 10% Formalin | Used to resuspend and dilute the fecal sample and the final sediment for examination. |
| Conical Centrifuge Tubes | Tubes designed for efficient pelleting of sediment during centrifugation. |
| Gauze or Strainer (e.g., FPC) | Filters out large, coarse fecal debris while allowing parasite eggs and cysts to pass through. |
Workflow:
- Homogenization: Mix approximately 500 mg to 5 ml of fecal specimen with 10 ml of 10% formalin [8] [13].
- Filtration: Strain the emulsified suspension through wet gauze or a commercial fecal parasite concentrator (FPC) into a 15 ml conical centrifuge tube [8].
- Washing: Add saline or formalin to bring the volume to 15 ml. Centrifuge at 500 × g for 10 minutes. Decant the supernatant [8].
- Solvent Extraction: Resuspend the sediment in 10 ml of 10% formalin. Add 4 ml of ethyl acetate, stopper the tube, and shake vigorously for 30 seconds [8] [13].
- Final Concentration: Centrifuge at 500 × g for 10 minutes. Four layers will form: a plug of debris and ethyl acetate at the top, a formalin layer, and the sediment containing parasites at the bottom.
- Sample Preparation: Free the debris plug, decant the top layers, and use a swab to clean the tube walls. Resuspend the final sediment in a small volume of formalin or saline for wet mount examination or staining [8].
Detailed Protocol: Centrifugal Flotation (Zinc Sulfate)
The zinc sulfate flotation is particularly effective for recovering protozoan cysts and some helminth eggs [12].
Workflow:
- Preparation: Emulsify 1-2 g of feces in 10 ml of water and strain as in the sedimentation protocol.
- Washing: Centrifuge the filtrate at 500 × g for 10 minutes. Decant the supernatant.
- Flotation: Resuspend the sediment in a small volume of zinc sulfate solution (specific gravity 1.18-1.20). Add more zinc sulfate to fill the tube to the brim, forming a positive meniscus.
- Coverslip Placement: Place a coverslip on top of the tube to contact the meniscus.
- Centrifugation: Centrifuge at 500 × g for 10 minutes.
- Collection: Carefully remove the coverslip, which will have a drop of fluid adherent to it containing the concentrated parasites, and place it on a microscope slide for examination.
Critical Technical Note: The centrifugal force and time are critical parameters. A modified protocol increasing force to 500 × g and time to 10 minutes demonstrated a significant increase in the recovery of Cryptosporidium oocysts compared to the standard method (400 × g for 2 minutes), raising sensitivity from 86% to 99% [14].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Parasite Concentration Techniques
| Category | Item | Specific Function in Parasitology |
|---|---|---|
| Preservatives & Solutions | 10% Buffered Formalin | Primary fixative and preservative for parasitic morphology; inactivates pathogens. |
| Ethyl Acetate | Lipid solvent for debris extraction in sedimentation; less flammable than ether. | |
| Zinc Sulfate Solution (SG 1.18-1.20) | High-specific gravity medium for flotation of cysts and light eggs. | |
| Sheather's Sugar Solution | High-viscosity flotation medium for delicate oocysts (e.g., Cryptosporidium). | |
| Consumables | Conical Centrifuge Tubes | Facilitates tight pellet formation and efficient separation of layers. |
| Gauze or Commercial Filtration Systems | Removes large particulate matter to prevent obstruction during microscopy. | |
| Coverslips and Microscope Slides | Standard substrates for preparing diagnostic wet mounts. | |
| Instrumentation | Clinical Centrifuge | Imparts controlled centrifugal force for rapid sedimentation or flotation. |
| Compound Microscope | Essential tool for the visualization and identification of concentrated parasites. | |
| Juniperanol | Juniperanol | Juniperanol (CAS 332855-75-1), a lab reagent for research use only (RUO). Explore its potential in metabolic disease studies. Available for fast delivery. |
| 1-butyl-1H-indol-4-amine | 1-Butyl-1H-indol-4-amine | 1-Butyl-1H-indol-4-amine for research. C12H16N2, MW 188.27. Study indolyl compounds in chemical synthesis. For Research Use Only. Not for human or veterinary use. |
Both sedimentation and flotation techniques are vital in the parasitology laboratory. The formalin-ethyl acetate sedimentation method offers robustness and broad-spectrum efficacy, making it an excellent single concentration technique for routine diagnostics. Flotation methods, particularly with zinc sulfate, provide superior cleanliness for detecting specific parasites like protozoan cysts. The choice of method should be guided by the target parasites, available resources, and technical expertise. However, for the most comprehensive detection, especially in research settings or when screening for a wide array of parasites, the use of both techniques in tandem is considered the most sensitive approach, though it may be impractical for some high-throughput laboratories [10]. Ongoing research continues to refine these classical methods, optimizing parameters like centrifugal force to maximize diagnostic yield [14].
Within clinical laboratory science, the processing of stool specimens for the diagnosis of intestinal parasitic infections is a fundamental procedure. The formalin-ether concentration technique (FECT) has long been considered a gold standard for parasite recovery. However, the use of diethyl ether (ether) in this method presents significant safety challenges due to its high flammability and volatility. This application note details the distinct advantages of substituting diethyl ether with ethyl acetate, framing the discussion within the context of the formalin-ethyl acetate concentration technique. We provide a comprehensive safety and efficacy comparison, supported by quantitative data and detailed protocols, to guide researchers, scientists, and laboratory professionals in adopting this safer, equally effective alternative.
Comparative Analysis: Ethyl Acetate vs. Diethyl Ether
The selection of a solvent for diagnostic concentration techniques requires a careful balance of efficacy, safety, and practical handling. The following analysis directly compares ethyl acetate and diethyl ether across these critical parameters.
Table 1: Physicochemical and Safety Comparison of Ethyl Acetate and Diethyl Ether
| Property | Ethyl Acetate | Diethyl Ether | Practical Implication for Use |
|---|---|---|---|
| Flammability | Flammable | Highly Flammable (Flash point: -49°F / -45°C) [15] | Ethyl acetate poses a significantly lower fire risk in the laboratory setting. |
| Volatility | Less volatile, slower evaporation | Highly volatile, rapid evaporation [15] | Ethyl acetate is easier to handle and less prone to creating hazardous vapor concentrations. |
| Health Hazards | Lower toxicity; irritation with exposure | Respiratory irritant; can cause dizziness, nausea, and loss of consciousness [15] | Ethyl acetate provides a safer working environment for laboratory personnel. |
| Peroxide Formation | Does not form explosive peroxides | Can form explosive peroxides upon storage when exposed to air and light [15] | Eliminates a major storage and handling hazard associated with diethyl ether. |
| Environmental & Disposal | Considered a greener solvent [16] | Contributes to air and water pollution if not disposed of properly [15] | Ethyl acetate aligns with green chemistry principles in the laboratory. |
Table 2: Diagnostic Efficacy in Parasite Recovery from Stool Specimens
| Parasite | Comparative Efficacy (Ethyl Acetate vs. Diethyl Ether) | Supporting Data |
|---|---|---|
| Hookworm | Ethyl Acetate is Superior | FECT was superior to FC in detecting hookworm [13]. |
| Trichuris trichiura | Ethyl Acetate is Superior | FECT was superior to FC in detecting T. trichiura [13]. |
| Small Liver Flukes | Ethyl Acetate is Superior | FECT was superior to FC in detecting small liver flukes [13]. |
| Ascaris lumbricoides | Comparable Efficacy | No significant difference was found, possibly due to high egg density [13]. |
| General Parasite Recovery | Comparable | Ethyl acetate was found comparable in the quantitative recovery of parasite eggs, cysts, and larvae [17]. |
Experimental Protocol: Formalin-Ethyl Acetate Concentration Technique (FECT)
The following detailed methodology is adapted for the use of ethyl acetate and is validated for the processing of fresh human stool specimens [13] [17].
Principle
The technique uses the solvent properties of ethyl acetate to extract fat and debris from a formalin-fixed stool suspension. During centrifugation, ethyl acetate, with its lower specific gravity than water, forms a layer above the formalin, trapping debris at the interface. Parasitic elements, such as eggs, cysts, and larvae, are sedimented free from obscuring material for easier microscopic identification [13].
Materials and Reagents
Table 3: Research Reagent Solutions and Essential Materials
| Item | Function / Specification |
|---|---|
| Ethyl Acetate | Solvent for extraction of fats and debris; must be reagent grade. |
| 10% Formalin Solution | Fixative and preservative for stool specimens. |
| Conical Centrifuge Tubes (15mL recommended) | Tubes for sample processing and centrifugation. |
| Moulded Strainer or Gauze (0.6 mm x 0.6 mm sieve) | Removal of large particulate debris from the stool suspension. |
| Saline Solution (0.85%) | Re-suspension of the final sediment for microscopy. |
| Centrifuge | Capable of achieving 500 g. |
| Microscope Slides and Coverslips | Preparation of wet mounts for examination. |
Step-by-Step Procedure
- Specimen Emulsification: Transfer approximately 500 mg of fresh stool into a clean centrifuge tube containing 10 mL of clean water. Mix vigorously until the faecal material is fully suspended [13].
- Filtration: Decant the suspension through a moulded strainer or gauze into a second clean centrifuge tube to remove large, undigested particles [13].
- Centrifugation: Centrifuge the filtered suspension at 500 g for 5 minutes. Carefully decant and discard the supernatant [13].
- Formalin Fixation: Re-suspend the sediment with 10 mL of 10% formalin solution. Allow the mixture to stand for at least 10 minutes for fixation. If the specimen was previously formalinized, begin the protocol from this step [13].
- Solvent Addition: Add 4 mL of ethyl acetate to the formalinized suspension. Stopper the tube securely and shake it vigorously for at least 30 seconds to ensure thorough emulsification. Release the pressure carefully by loosening the stopper [13] [17].
- Second Centrifugation: Recentrifuge the tube at 500 g for 5 minutes. This will result in four distinct layers:
- Top Layer: Ethyl acetate.
- Plug Layer: Debris and extracted material at the interface.
- Middle Layer: Formalin solution.
- Bottom Layer: Sediment containing the concentrated parasitic elements.
- Separation: Free the debris plug from the sides of the tube with an applicator stick. Carefully decant the top three layers (ethyl acetate, debris plug, and formalin) in one smooth motion. Exercise care to prevent the plug from remixing with the sediment [17].
- Preparation for Microscopy: Re-suspend the remaining sediment with a few drops of saline solution or the remaining formalin from the sides of the tube. Using a pipette, transfer one or two drops of the sediment to a microscope slide, apply a coverslip, and examine systematically under appropriate magnification [13].
Workflow Visualization
Critical Notes on Technique and Troubleshooting
Successful implementation of the FECT requires attention to detail, particularly when transitioning from diethyl ether.
- Interface Plug Management: The debris plug formed with ethyl acetate can be more tenacious than with diethyl ether. It is critical to thoroughly free this plug from the tube walls with an applicator stick before decanting to prevent it from sliding back and contaminating the sediment [17].
- Microscopic Clarity: Wet mounts prepared from ethyl acetate concentrates may occasionally be obscured by insoluble liquid bubbles, which are likely residual ethyl acetate. Allowing the slide to stand for a minute or gently tapping the coverslip can help dissipate these bubbles before examination [17].
- Specimen Integrity: The technique does not distort or alter the morphology of parasite eggs, cysts, or larvae, ensuring accurate identification by experienced microscopists [17].
The formalin-ethyl acetate concentration technique presents a significant advancement in laboratory safety without compromising diagnostic accuracy. Ethyl acetate eliminates the severe flammability and peroxide formation hazards inherent to diethyl ether, creating a safer workplace and simplifying storage and disposal protocols. Extensive clinical comparison studies confirm that ethyl acetate is quantitatively comparable to diethyl ether in the recovery of intestinal parasites, proving superior for certain helminths like hookworm and Trichuris trichiura. The adoption of ethyl acetate is a clear and responsible step forward for clinical diagnostics and research in parasitology.
Within the framework of research on the formalin-ethyl acetate concentration technique (FECT), the precise identification of parasitic forms concentrated from stool specimens is a critical determinant of diagnostic accuracy and subsequent research validity [13]. The FECT, a sedimentation-based method, separates parasites from fecal debris through a series of steps involving formalin fixation and ethyl-acetate extraction, ultimately concentrating parasite forms in the sediment for microscopic examination [8]. This protocol enhances the detection of helminth eggs, larvae, and protozoan cysts present in low numbers, making it superior to simpler formalin-based concentration methods for most intestinal helminths [13]. This application note provides a detailed morphological and procedural guide for researchers and scientists identifying these parasitic forms within the context of FECT-based studies.
Morphological Characteristics of Key Parasitic Forms
The definitive diagnosis of gastrointestinal parasitic infections relies on the microscopic identification of various parasitic stages. Their morphological characteristics, as detailed below, enable differentiation.
Intestinal Protozoa: Trophozoites and Cysts
Protozoa such as Entamoeba histolytica and Giardia duodenalis exist in two primary forms: the motile, vegetative trophozoite and the dormant, infective cyst. The following tables summarize the key diagnostic features for identification in permanently stained smears, which are essential for differentiating pathogenic from non-pathogenic species [18] [19].
Table 1: Differential Morphology of Intestinal Amoebae-Trophozoites
| Species | Size (Length) | Motility | Nuclear Characteristics | Cytoplasmic Inclusions |
|---|---|---|---|---|
| Entamoeba histolytica | 10-60 µm; invasive form >20µm | Progressive, with hyaline, finger-like pseudopods | Fine, uniformly distributed peripheral chromatin; small, discrete karyosome | May contain ingested red blood cells (indicative of pathogenicity) |
| Entamoeba coli | 15-50 µm; usual range 20-25µm | Sluggish, non-progressive, with blunt pseudopods | Coarse, irregular peripheral chromatin; large, discrete, often eccentric karyosome | Bacteria, yeasts, other materials; coarse, vacuolated cytoplasm |
| Endolimax nana | 6-12 µm | Sluggish, usually non-progressive | No peripheral chromatin; large, irregular, blot-like karyosome | Bacteria; granular, vacuolated cytoplasm |
| Dientamoeba fragilis | 5-15 µm | Pseudopods are angular, serrated, hyaline | Nucleus often binucleated; large karyosomal cluster of 4-8 granules | Bacteria; finely granular cytoplasm |
Table 2: Differential Morphology of Intestinal Amoebae-Cysts
| Species | Size (Diameter) | Mature Cyst Nuclei | Chromatoid Bodies | Other Cytoplasmic Inclusions |
|---|---|---|---|---|
| Entamoeba histolytica | 10-20 µm | 4 | Present; elongated bars with bluntly rounded ends | Diffuse glycogen mass; stains reddish-brown with iodine |
| Entamoeba coli | 10-35 µm | 8 | Present, but less frequent; splinter-like with pointed ends | Diffuse glycogen mass; stains reddish-brown with iodine |
| Endolimax nana | 5-10 µm | 4 | Not present | Occasionally diffuse mass |
| Iodamoeba bütschlii | 5-20 µm | 1 | Not present | Compact, well-defined glycogen mass; stains dark brown with iodine |
Table 3: Differential Morphology of Flagellates and Ciliates
| Species | Stage | Size (Length) | Shape & Motility | Distinguishing Features |
|---|---|---|---|---|
| Giardia duodenalis | Trophozoite | 10-20 µm | Pear-shaped; "falling leaf" motility | Sucking disk; 2 nuclei; 4 pairs of flagella; median bodies |
| Cyst | 11-14 µm | Oval | 4 nuclei; axonemes; median bodies; thick cyst wall | |
| Chilomastix mesnili | Trophozoite | 6-24 µm | Pear-shaped; stiff, rotary motility | Prominent cytostome; spiral groove |
| Balantidium coli | Trophozoite | - | - | Motile with cilia; large macronucleus |
| Cyst | - | - | Spherical; macronucleus visible |
Helminths: Eggs and Larvae
Helminth eggs and larvae possess distinct morphologies that can be used for species identification during microscopic examination of concentrated specimens [19]. Key features include size, shape, shell thickness and ornamentation, and internal contents.
Table 4: Characteristics of Common Helminth Eggs and Larvae
| Parasite | Stage | Size (Range) | Shape & Description | Key Identifying Features |
|---|---|---|---|---|
| Ascaris lumbricoides | Egg | 45-75 µm x 35-50 µm | Round or oval; thick, mammillated coat (fertile) | Brownish; outer albuminous layer often decorticated |
| Hookworm | Egg | 55-75 µm x 36-40 µm | Oval, thin-shelled | Colorless; contains a developing embryo (usually 4-16 cell stage) |
| Trichuris trichiura | Egg | 50-55 µm x 20-25 µm | Barrel-shaped with polar plugs | Brownish; thick shell |
| Strongyloides stercoralis | Larva | - | - | Rhabditiform larvae (and sometimes filariform) in fresh stool |
Experimental Protocol: Formalin-Ethyl Acetate Concentration Technique (FECT)
The following is the standard FECT protocol as utilized by the CDC and validated in comparative studies [8] [13]. This technique is recommended for general diagnostic laboratories because it is easier to perform and less prone to technical errors than flotation techniques, which can collapse the walls of eggs and cysts [8].
Research Reagent Solutions
Table 5: Essential Reagents for FECT and Staining
| Reagent/Material | Function/Application |
|---|---|
| 10% Formalin | Fixes and preserves parasite morphology; primary preservative. |
| Ethyl Acetate | Solvent that extracts fats, dissolves debris, and reduces odor; replaces the more flammable ether. |
| 0.85% Saline Solution | Isotonic solution for resuspending the final sediment to maintain organism integrity. |
| Polyvinyl Alcohol (PVA) | Preservative for stool specimens intended for permanent staining; fixes trophozoites and provides a medium for adhesion to the slide. |
| Wheatley's Trichrome Stain | Permanent polychromatic stain for protozoal cysts and trophozoites in PVA-preserved samples. |
| Kinyoun's Carbol Fuchsin / Malachite Green | Components of the modified acid-fast stain for identifying coccidian oocysts (e.g., Cryptosporidium, Cyclospora). |
| Chromotrope 2R-based Stain | Specialized stain for detecting microsporidial spores in fecal and other clinical specimens. |
Step-by-Step FECT Procedure
- Specimen Mixing and Filtration: Mix the fresh or formalin-preserved stool specimen thoroughly. Strain approximately 5 mL of the fecal suspension through wetted cheesecloth or a specialized fecal parasite concentrator (with ~0.6 mm x 0.6 mm sieve openings) into a 15 mL conical centrifuge tube. Add 0.85% saline or 10% formalin through the debris on the gauze to bring the volume to 15 mL [8] [13].
- Primary Centrifugation: Centrifuge at 500 × g for 10 minutes. Decant the supernatant completely [8].
- Formalin Resuspension and Ethyl Acetate Addition: Resuspend the sediment in 10 mL of 10% formalin and mix thoroughly. Add 4 mL of ethyl acetate to the tube. Stopper the tube securely and shake it vigorously in an inverted position for 30 seconds. After shaking, carefully remove the stopper [8].
- Secondary Centrifugation: Centrifuge at 500 × g for 10 minutes. This step will result in four distinct layers: a plug of fatty debris at the top (ethyl acetate and debris), a layer of formalin, a sediment of fecal material, and the concentrated parasitic organisms at the very bottom of the sediment [8].
- Supernatant and Debris Removal: Free the debris plug from the sides of the tube by ringing it with an applicator stick. Decant the top three layers (ethyl acetate, debris, and formalin). Use a cotton-tipped applicator to carefully wipe any remaining debris from the inner sides of the centrifuge tube [8].
- Final Suspension: Add a few drops of 10% formalin or saline to the remaining sediment and mix to resuspend the concentrated parasitic material. This final suspension is ready for microscopic examination via wet mounts or preparation for permanent staining [8].
The following workflow diagram illustrates the key procedural steps and decision points in the FECT protocol and subsequent analysis:
Diagram 1: FECT and Downstream Analysis Workflow. This diagram outlines the formalin-ethyl acetate concentration technique (FECT) for stool specimens, from initial processing to final microscopic analysis.
Downstream Microscopic Analysis
- Wet Mount Examination: Use 1-2 drops of the concentrated sediment to prepare wet mounts with and without iodine. The iodine stain enhances the visibility of nuclear features in protozoan cysts and glycogen masses [18] [8]. Systematically examine the entire coverslip area under 10x and 40x objectives to detect helminth eggs, larvae, and protozoan cysts.
- Permanent Stained Smears: For definitive identification of protozoa, especially trophozoites and cysts, prepare smears from the concentrate (or from PVA-preserved specimen) and stain with Wheatley's trichrome stain or iron hematoxylin [20] [19]. This provides a permanent record and allows for the detailed observation of internal structures.
- Special Stains for Coccidia and Microsporidia: If these organisms are suspected, specific stains must be employed. A modified acid-fast stain (e.g., Kinyoun's) is used to identify oocysts of Cryptosporidium spp. (stain pinkish-red), Cystoisospora, and Cyclospora [20] [19]. For the smaller microsporidial spores, the chromotrope stain or the Quick-Hot Gram-Chromotrope stain is required for detection, where spores stain pinkish-red [20].
Validation and Comparative Performance of FECT
The implementation of FECT as a routine diagnostic tool is supported by empirical evidence demonstrating its superior sensitivity compared to simpler concentration methods. A comparative study of 693 faecal samples showed that FECT was significantly superior to a crude formalin concentration (FC) method in detecting hookworm, Trichuris trichiura, and small liver flukes [13]. The enhanced clearing of debris and fat by ethyl acetate results in a cleaner sediment, facilitating the detection of parasites, particularly in low-burden infections. This improved diagnostic accuracy is crucial for both patient-level management and for informing public health policies and deworming strategies in endemic areas [13].
Specimen preservation is a critical foundation for reliable diagnostic and research outcomes in microbiology and parasitology. The accurate morphological analysis of biological samples, particularly stool specimens for intestinal parasite detection, is heavily dependent on the choice of fixative and adherence to precise processing timelines. Within the broader context of formalin-ethyl acetate concentration technique (FECT) research, optimal preservation ensures the integrity of parasite eggs, larvae, cysts, and trophozoites, enabling precise identification and quantification. This protocol details standardized procedures for specimen preservation and processing, emphasizing the FECT method, which has demonstrated superior diagnostic accuracy for detecting intestinal helminth infections compared to crude formalin concentration methods [13]. The formalin-ethyl acetate technique improves detection by extracting fats and debris through the organic solvent ethyl acetate, resulting in a cleaner sediment background for microscopic examination and significantly enhancing the visualization of parasitic elements [21] [13].
Fixative Comparison and Selection
Choosing the appropriate fixative is a critical first step in specimen preservation, as it directly impacts morphological quality and compatibility with downstream diagnostic applications. No single fixative is ideal for all purposes; selection requires careful consideration of advantages and limitations against diagnostic needs.
Table 1: Comparative Analysis of Common Stool Specimen Fixatives
| Fixative | Key Advantages | Key Limitations | Primary Applications |
|---|---|---|---|
| 10% Formalin | All-purpose; long shelf life; good for helminth eggs/larvae; suitable for concentration procedures and immunoassays [22]. | Unsuitable for permanent trichrome stains; inadequate for protozoan trophozoite morphology [22]. | Routine concentration techniques; immunoassay testing. |
| Formalin-Ethyl Acetate (FECT) | Superior debris removal; improved detection for hookworm, Trichuris trichiura, and small liver flukes [13]. | More time-consuming than FC; requires additional materials [13]. | Gold-standard concentration technique for enhanced parasite detection. |
| Merthiolate-Iodine-Formalin (MIF) | Simultaneously fixes and stains organisms; useful for field surveys [22]. | Iodine causes distortion; not suitable for permanent stains or immunoassays [22]. | Field surveys and rapid assessment. |
| Low-Viscosity Polyvinyl-Alcohol (LV-PVA) | Excellent for protozoan trophozoites/cysts; enables permanent stained smears [22]. | Contains toxic mercuric chloride; poor for helminth eggs/larvae; not for concentration [22]. | Permanent staining for protozoan identification. |
| Total-Fix | No formalin, mercury, or PVA; suitable for concentration, stains, and immunoassays from a single vial [23]. | Proprietary formulation; staining consistency may vary compared to traditional fixatives [23]. | Multi-purpose preservation for modern laboratory workflows. |
| Sodium Acetate-Acetic Acid-Formalin (SAF) | Suitable for concentration and permanent stains; no mercury [22]. | Requires adhesive for smear preparation; permanent stain quality inferior to PVA [22]. | Laboratories seeking a non-mercury alternative. |
For comprehensive parasitology surveys, the CDC recommends preserving specimens in both 10% formalin and PVA to leverage their complementary advantages [22]. Furthermore, research into natural alternatives like honey, jaggery, and aloe vera has emerged, though these may present challenges such as shorter shelf life and mold formation compared to conventional chemical fixatives [24].
Formalin-Ethyl Acetate Concentration Technique (FECT): A Detailed Protocol
This protocol describes the FECT procedure, which is recognized for its superior diagnostic accuracy in detecting intestinal helminths, including hookworm and Trichuris trichiura [13].
Principle
The FECT uses formalin to preserve parasitic elements and ethyl acetate as an organic solvent to extract fats, debris, and undigested food materials from the fecal sample. This process concentrates parasitic organisms in the sediment while significantly reducing obscuring background material, thereby facilitating clearer microscopic identification [21] [13].
Specimen Collection and Preservation
- Collection: Collect stool in a clean, leak-proof, dry container. Take care to avoid contamination with water, urine, or soil [22].
- Preservation: Preserve the specimen immediately after collection. For optimal results, add one volume of stool to three volumes of 10% formalin in a labeled container and mix thoroughly to ensure full emulsification [22]. If commercial collection kits are used, follow the manufacturer's instructions [23].
- Transport: Seal containers securely. If necessary, preserved specimens can be stored for several months before processing [22].
Materials and Reagents
- 10% formalin solution
- Ethyl acetate
- Saline solution (0.85%)
- Conical centrifuge tubes (15 mL)
- Fecal strainer or gauze
- Centrifuge
- Microscope slides and coverslips
- Disposable pipettes
Step-by-Step Procedure
- Emulsification: For preserved samples, mix the formalin-fixed specimen thoroughly. If using fresh stool, emulsify approximately 500 mg (or 0.5 mL) of feces in 10 mL of 10% formalin [13].
- Filtration and Primary Sedimentation:
- Pour the emulsified sample through a fecal strainer into a conical centrifuge tube to remove large particulate matter.
- Centrifuge at 500 × g for 2 minutes [13].
- Decant the supernatant completely.
- Ethyl Acetate Extraction:
- Resuspend the sediment in the residual fluid or add fresh 10% formalin up to 10 mL.
- Add 4 mL of ethyl acetate to the tube. Securely cap the tube and shake it vigorously for at least 30 seconds to ensure thorough mixing [13].
- Centrifuge at 500 × g for 5 minutes. This step will result in four distinct layers: an ethyl acetate plug at the top, a layer of debris, the formalin solution, and the concentrated sediment at the bottom.
- Sediment Recovery:
- Free the debris plug from the tube walls using an applicator stick.
- Carefully decant the top three layers (ethyl acetate, debris, and formalin), taking care not to disturb the sediment pellet.
- Use a cotton-tipped applicator to wipe residual debris from the inner walls of the tube.
- Microscopic Examination:
- Resuspend the final sediment in a few drops of saline or formalin.
- Transfer one or two drops to a clean microscope slide, place a coverslip over it, and examine systematically under the microscope.
Research Reagent Solutions
Table 2: Essential Reagents and Materials for FECT
| Item | Function/Application | Specifications/Notes |
|---|---|---|
| 10% Formalin | Primary fixative preserving parasite morphology [22]. | Aqueous solution; long shelf life; suitable for helminth eggs and larvae. |
| Ethyl Acetate | Organic solvent for extracting fats and debris [13]. | Less flammable and hazardous alternative to diethyl ether. |
| Total-Fix | Single-vial, multi-application fixative [23]. | Proprietary, non-formalin, non-mercury fixative for concentration, stains, and immunoassays. |
| Low Melt Agarose | Sample mounting for specialized imaging [25]. | Used for plant samples in light sheet microscopy; requires filter sterilization for optical clarity. |
| Saline (0.85%) | Resuspension medium for final sediment [13]. | Isotonic solution for creating wet mounts for microscopy. |
| Conical Centrifuge Tubes | Container for concentration steps [13]. | 15 mL capacity; enables effective layer separation during FECT. |
| Fecal Strainer | Removal of large particulate matter [13]. | Mesh opening ~0.6 mm; allows parasite eggs to pass while retaining debris. |
Quality Control and Methodological Enhancements
Rigorous quality control is essential for reliable diagnostic results. For the FECT, this includes standardized centrifugation speeds and times to ensure consistent sediment recovery [13]. Microscopic examination should follow a systematic reading procedure, with slides examined by experienced technologists to ensure accurate identification [13].
Recent research has provided insights for methodological improvements. A 2024 study identified that the interaction between cellulose in fecal matter and ethyl acetate is crucial for effective bulk flotation. The study found that adding acid residues can dissolve cellulose from leafy structures that trap oil droplets, thereby improving fecal bulk float and subsequent visualization of parasite eggs [21].
The formalin-ethyl acetate concentration technique represents a significant advancement in stool specimen processing, providing superior diagnostic sensitivity for intestinal helminth infections compared to older formalin-based methods. Successful implementation relies on strict adherence to standardized protocols for specimen preservation, processing timelines, and quality control measures. Ongoing research continues to refine these methods, with developments in understanding flotation mechanics and the introduction of safer, effective fixatives promising to further enhance diagnostic accuracy and laboratory safety.
Standardized FECT Protocol: Step-by-Step Laboratory Procedure
Specimen Collection, Transport, and Macroscopic Examination
The diagnostic accuracy of intestinal parasitic infection (IPI) identification is fundamentally dependent on the initial pre-analytical phases of specimen collection, transport, and macroscopic examination. These stages form the critical foundation for all subsequent laboratory procedures, including the highly sensitive formalin-ethyl acetate concentration technique (FECT) [3] [9]. In the context of research on the FECT for stool specimens, proper specimen integrity is paramount, as the technique's superior recovery rate of parasitic elements can be compromised by suboptimal collection or handling [13]. This protocol outlines detailed methodologies to ensure specimen quality, thereby enhancing the reliability of downstream parasitological analyses crucial for researchers, scientists, and drug development professionals engaged in Neglected Tropical Disease (NTD) research and diagnostic innovation.
Specimen Collection and Transport Procedures
Adherence to standardized protocols for specimen collection and transport is essential to maintain the morphological integrity of parasites, which directly influences diagnostic sensitivity and the validity of research outcomes [26] [9].
Patient Preparation and Collection Guidelines
- Patient Instruction: Inform patients or guardians to avoid the use of antibiotics, antiparasitic drugs, mineral oil, bismuth, or barium compounds for at least two weeks prior to specimen collection, as these substances can mask or destroy parasitic structures [3].
- Collection Container: Collect stool samples in a clean, wide-mouth, water-tight plastic container. The container must be properly labeled with at least two patient identifiers (e.g., name, date of birth, unique study ID) at the time of collection [26].
- Specimen Quantity: A sufficient quantity of stool (approximately 4-5 grams or the size of a walnut) should be collected to ensure adequate material for multiple diagnostic techniques and research replicates [26].
- Avoiding Contamination: Caution should be exercised to avoid contamination with water, urine, or soil, as this can introduce foreign organisms that complicate microscopic analysis [9].
Specimen Preservation and Transport
- Timely Transport: Fresh specimens should be transported to the laboratory and examined ideally within 2 hours of passage if being processed without preservatives. This is critical for detecting motile trophozoites of protozoa that degenerate rapidly [9].
- Preservation for Delayed Processing: If immediate transport or processing is not feasible, the specimen must be preserved. The 3:1 ratio of preservative to fecal material is recommended for fixation [9].
- Common Preservative Solutions:
- 10% Buffered Formalin: Excellent for preserving eggs, larvae, cysts, and protozoan trophozoites. It is the preferred preservative for the FECT procedure [3] [13].
- Polyvinyl Alcohol (PVA): Used for both preservation and adhesion of stool smears for permanent staining.
- Sodium Acetate-Acetic Acid-Formalin (SAF): Suitable for concentration procedures and permanent staining [9].
- Temperature Control: Unpreserved specimens must be refrigerated between 3°C and 5°C in an air-tight container during transit to retard bacterial growth and preserve parasitic structures [9].
Macroscopic Examination Procedures
Macroscopic examination provides the first opportunity to assess the specimen and can yield valuable diagnostic clues regarding the patient's condition and potential parasitic infections.
Visual Inspection Protocol
Upon receipt in the laboratory, the specimen should be logged and subjected to a systematic visual inspection without magnification to document the following characteristics [3]:
- Consistency: Document as formed, semi-formed, soft, loose, or watery. Consistency influences the choice of direct examination methods and can correlate with certain pathogens (e.g., motile trophozoites are more likely in watery or loose stools).
- Color: Note any unusual coloration (e.g., pale, black, red).
- Presence of Blood or Mucus: Visually inspect for the presence of gross blood (hematochezia) or mucus. Mucus is often associated with Entamoeba histolytica infection or colonic irritation.
- Adult Parasites: Carefully examine the entire specimen for the presence of adult worms or proglottids. Ascaris lumbricoides adults or Taenia sp. proglottids may be visible to the naked eye [3].
Table 1: Macroscopic Findings and Their Potential Clinical Significance in Parasitology
| Macroscopic Finding | Description | Potential Significance/Associated Parasite |
|---|---|---|
| Consistency | Watery, loose, formed, hard | Determines the likelihood of finding trophozoites (more common in diarrheic stools) versus cysts (more common in formed stools). |
| Color | Black/tarry (melena), red (hematochezia), pale | Melena may indicate upper GI bleeding; pale stools can suggest biliary obstruction. |
| Mucus | Gelatinous, clear or blood-tinged material | Often seen in amebic colitis or other inflammatory conditions of the intestine. |
| Adult Worms | Visible, motile roundworms or tapeworm proglottids | Direct evidence of infection with Ascaris lumbricoides, Enterobius vermicularis, or Taenia species. |
Context within FECT Research
The meticulous execution of collection, transport, and macroscopic examination is a critical prerequisite for maximizing the diagnostic yield of the Formalin-Ethyl Acetate Concentration Technique (FECT). Recent research validates FECT as a superior concentration method with higher sensitivity compared to direct wet mounts and other concentration methods like the Formalin-Ether Concentration (FEC) technique [3] [13].
Quantitative Performance of Diagnostic Techniques
A 2023 hospital-based cross-sectional study directly compared diagnostic performance for intestinal parasite identification, with results summarized in the table below [3].
Table 2: Comparative Detection Rates of Parasitological Examination Techniques (n=110) [3]
| Diagnostic Technique | Total Parasites Detected (n) | Detection Rate (%) |
|---|---|---|
| Direct Wet Mount | 45 | 41% |
| Formalin-Ether Concentration (FEC) | 68 | 62% |
| Formalin-Ethyl Acetate Concentration (FECT) | 82 | 75% |
The FECT method's enhanced performance, evidenced by a 75% detection rate, is attributed to its efficient concentration principle. Ethyl-acetate acts as a solvent to extract fat and debris from the formalin-fixed fecal suspension, concentrating parasitic structures in the sediment after centrifugation [9] [13]. This makes the initial specimen quality non-negotiable; a poorly collected or degraded specimen will result in suboptimal concentration and false-negative results, undermining the technical advantages of FECT.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Stool Specimen Processing and FECT
| Research Reagent / Material | Function and Application |
|---|---|
| 10% Buffered Formalin | Primary fixative and preservative for stool specimens. Kills pathogens, preserves morphological details of cysts, eggs, and larvae, and is the base solution for the FECT method. |
| Ethyl-Acetate Solvent | Key reagent in FECT. Acts as a fat solvent and debris extractor. It forms a plug at the top of the centrifuge tube after spinning, trapping debris for easy removal and leaving a clean sediment of parasites [13]. |
| Conical Centrifuge Tubes | Tubes used during the concentration procedure. Their conical shape facilitates the concentration of parasitic elements into a pellet at the tip for easy sample withdrawal. |
| Fecal Particulate Concentrator (Strainer) | A molded strainer or gauze (e.g., 0.6 mm x 0.6 mm sieve opening) used to filter out large, coarse fecal debris from the liquid suspension before centrifugation, allowing parasite eggs and cysts to pass through [13]. |
| 0.85% Saline Solution | An isotonic solution used to re-suspend the concentrated sediment after centrifugation to create a wet mount for microscopic examination. |
| 1H-Isoindole-1,3-diamine | 1H-Isoindole-1,3-diamine, CAS:53175-37-4, MF:C8H9N3, MW:147.18 g/mol |
| LongipedlactoneB | LongipedlactoneB, MF:C30H40O5, MW:480.6 g/mol |
Workflow for Specimen Processing and FECT
The following diagram illustrates the logical workflow from specimen collection through to the final microscopic analysis, highlighting the central role of macroscopic examination.
Within the formalin-ethyl acetate concentration (FAC) technique for stool specimens, the initial step of homogenization and filtration is critical for subsequent diagnostic accuracy. This phase is designed to prepare a standardized fecal suspension and remove coarse debris, fibrous material, and large undigested particles that can obscure the microscopic identification of parasites [8]. Effective homogenization ensures a representative sample is processed, while filtration directly enhances the quality of the final sediment by reducing confounding background material, thereby improving the clarity and reliability of microscopic examination [27]. This protocol details the standardized methodology for this foundational step, framed within the broader research context of optimizing parasite recovery rates in clinical and research settings.
Experimental Protocols
Detailed Methodology for Homogenization and Filtration
The following procedure is adapted from standardized protocols, including those from the CDC [8], and is designed for processing approximately 1-3 grams of fresh or formalin-preserved stool.
Materials:
- Sterile, wide-mouth plastic container with lid (for collection)
- Disposable gloves and lab coat
- Disposable wooden or plastic applicator sticks
- Filtration Apparatus: This typically consists of a funnel (disposable paper or plastic) and a single layer of wet cheesecloth-type gauze or a specialized sieve with a pore size of 450–500 microns (μ) [3] [27].
- Reagent: 10% Formalin Saline or 10% Formalin solution [3] [8].
- Conical centrifuge tube (15 mL).
- Graduated cylinder or serological pipette.
Step-by-Step Procedure:
Specimen Homogenization:
- Using a disposable applicator stick, transfer approximately 1-3 grams (or 3-5 mL, depending on consistency) of stool into a clean mixing vessel or directly into a 15 mL conical centrifuge tube [3] [27].
- Add 7-10 mL of 10% formalin to the stool specimen. The volume of formalin can be adjusted to achieve a uniform suspension, typically a 1:10 ratio of stool to formalin [3] [8].
- Using a fresh applicator stick, mix the stool and formalin vigorously until a homogenous emulsion is achieved. This ensures that parasitic elements are evenly distributed throughout the sample.
Filtration to Remove Debris:
- Place the wetted gauze or sieve over the mouth of a disposable funnel. The funnel should be seated securely into the open 15 mL conical centrifuge tube.
- Carefully pour the homogenized stool-formalin mixture through the gauze/sieve into the centrifuge tube. The gauze will trap large, undigested particles and debris.
- To maximize yield, rinse any remaining material through the gauze by adding an additional small volume of 10% formalin or 0.85% saline through the debris [8]. Note: The use of distilled water is not recommended at this stage as it may deform or destroy certain parasites like Blastocystis hominis [8].
- The resulting filtrate in the centrifuge tube is a cleaned suspension of stool, now ready for the subsequent concentration steps involving ethyl acetate and centrifugation.
Integrated Workflow of the Full Formalin-Ethyl Acetate Technique
The homogenization and filtration step is the first part of a multi-stage process. The following workflow diagram illustrates its role within the complete FAC protocol, culminating in microscopic examination.
Diagram: Complete FAC workflow with initial Homogenization and Filtration step.
Key Research Data and Comparative Analysis
Performance of FAC in Parasite Detection
Research consistently demonstrates the high sensitivity of the full FAC technique. A recent 2023 hospital-based cross-sectional study with 110 children compared FAC against the Formol-Ether Concentration (FEC) and direct wet mount methods, with the following results [3]:
Table 1: Comparative Detection Rates of Diagnostic Techniques (n=110)
| Diagnostic Technique | Total Positive Samples | Detection Rate |
|---|---|---|
| Formalin-Ethyl Acetate Concentration (FAC) | 82 | 75% |
| Formol-Ether Concentration (FEC) | 68 | 62% |
| Direct Wet Mount | 45 | 41% |
The superior performance of FAC is attributed to its efficient concentration and debris-removal steps, which facilitate the identification of a wider range of parasites, as shown in the breakdown from the same study [3]:
Table 2: Parasite Species Recovered by Each Method
| Parasite Observed | Wet Mount (n=45) | FEC (n=68) | FAC (n=82) |
|---|---|---|---|
| Protozoan Cysts | |||
| ...... Blastocystis hominis | 4 | 10 | 12 |
| ...... Entamoeba histolytica | 13 | 18 | 20 |
| ...... Giardia lamblia | 9 | 12 | 13 |
| Helminth Eggs/Larvae | |||
| ...... Ascaris lumbricoides | 4 | 4 | 7 |
| ...... Strongyloides stercoralis | 1 | 2 | 4 |
| ...... Taenia species | 5 | 7 | 10 |
Impact on Workflow and Morphology
The quality of the initial filtration directly influences the clarity of the final sediment. A comparative study noted that "the wet mount prepared from the sedimentation technique had more background fecal debris in comparison to the Parasep technique," a commercial system that incorporates a built-in filtration stage [27]. Excessive debris can distort parasite morphology, making identification difficult. Furthermore, the integrated homogenization and filtration process contributes to a significant reduction in sample processing time, which is a critical factor in high-throughput laboratories [27].
The Scientist's Toolkit: Research Reagent Solutions
The following table details the essential materials required for the homogenization and filtration step.
Table 3: Key Reagents and Materials for Homogenization and Filtration
| Item | Function/Justification |
|---|---|
| 10% Formalin / Formalin Saline | Acts as a fixative and preservative, stabilizing parasitic morphology and neutralizing biohazards for safe handling [3] [8]. |
| Cheesecloth-Type Gauze or Sieve (450-500 µ) | The primary filtration medium for physically removing large particulate debris while allowing parasitic cysts, eggs, and larvae to pass through [8] [27]. |
| Disposable Paper Funnel | Facilitates the guided transfer of the homogenized specimen through the gauze and into the centrifuge tube, minimizing spillage and cross-contamination [8]. |
| Sterile Wide-Mouth Containers | Ensures safe and easy collection of the original stool specimen without loss of material. |
| Conical Centrifuge Tubes (15 mL) | Used for collecting the filtrate and are suitable for the subsequent concentration steps, including the addition of solvents and centrifugation. |
| KadlongilactoneF | KadlongilactoneF, MF:C30H38O7, MW:510.6 g/mol |
| kadsuphilolE | kadsuphilolE|C34H34O11|Research Chemical |
Within the broader research on the formalin-ethyl acetate concentration technique (FECT) for stool specimens, the steps of formalin fixation and centrifugation are critical pre-analytical variables that directly determine the accuracy and sensitivity of subsequent parasitic diagnostics. This protocol details the optimized parameters for these steps, enabling reliable concentration of helminth eggs, larvae, and protozoan cysts for microscopic identification. Standardizing this workflow is essential for large-scale epidemiological studies, clinical trial participant screening, and evaluating new anthelmintic agents, ensuring data comparability across research institutions and longitudinal studies.
Comparative Performance of Stool Concentration Techniques
The formalin-ethyl acetate concentration technique (FECT) demonstrates superior diagnostic performance compared to other common stool concentration methods.
Table 1: Detection Performance of Different Stool Concentration Techniques
| Parasite Detected | Direct Wet Mount [3] | Formol-Ether Concentration (FEC) [3] | Formalin-Ethyl Acetate Concentration (FECT) [3] | FECT vs. Formalin Concentration (FC) for Helminths [13] |
|---|---|---|---|---|
| Overall Parasite Detection | 41% | 62% | 75% | Superior for hookworm, Trichuris trichiura, and small liver flukes |
| Blastocystis hominis | 9% | 15% | 15% | Not Specified |
| Entamoeba histolytica | 31% | 26% | 24% | Not Specified |
| Giardia lamblia | 20% | 18% | 16% | Not Specified |
| Ascaris lumbricoides | 10% | 6% | 8% | No significant difference (high egg density) |
| Hookworm eggs | 2% | 4% | 4% | Significantly Improved |
| Strongyloides stercoralis | 2% | 3% | 5% | Not Specified |
Detailed Experimental Protocol for FECT
Reagents and Equipment
Research Reagent Solutions:
- 10% Formalin Solution: Serves as a fixative and preservative, immobilizing parasites and killing infectious agents for safe handling [3] [13].
- Ethyl Acetate: Organic solvent that extracts fats, dissolved pigments, and debris from the fecal suspension, concentrating parasitic elements in the sediment [13].
- Diethyl Ether (Alternative): Can be used in place of ethyl acetate, but is highly flammable and more hazardous [13].
- 0.85% Saline Solution: Used for final suspension of the sediment, providing an appropriate medium for microscopic examination [3] [13].
- Gauze or Fecal Strainer (0.6 mm x 0.6 mm sieve): Used to filter out large particulate debris from the fecal suspension [13].
Essential Laboratory Equipment:
- Conical centrifuge tubes (15 mL)
- Centrifuge with swing-bucket rotor
- Microscope slides and coverslips
- Precision balance
- Vortex mixer or applicator sticks for mixing
Step-by-Step Workflow
The following diagram illustrates the complete FECT protocol from sample preparation to microscopic examination:
1. Sample Preparation and Filtration:
- Using a precision balance, weigh approximately 500 mg of fresh stool specimen [13].
- Emulsify the sample in 10 mL of clean water in a 15 mL conical centrifuge tube.
- Vigorously shake the tube to create a homogeneous suspension and filter it through a molded strainer or multiple layers of gauze into a new conical tube to remove large, coarse debris [13] [28].
2. Preliminary Sedimentation:
- Centrifuge the filtered suspension at 500 × g for 5 minutes [13].
- Carefully decant and discard the supernatant, ensuring the sediment at the bottom of the tube is not disturbed.
3. Formalin Fixation:
- Resuspend the resulting sediment in 10 mL of 10% formalin solution [3] [13].
- Fixation occurs upon contact with formalin. The sample can be held in this state if processing must be paused.
4. Ethyl Acetate Extraction and Concentration:
- Add 4 mL of ethyl acetate to the formalin-sediment mixture in the conical tube [13].
- Tightly close the tube cap and vigorously shake it by hand in an inverted position for 30-60 seconds to ensure thorough mixing [3] [13]. This step dissolves and traps interfering substances in the organic solvent layer.
5. Final Centrifugation and Cleanup:
- Centrifuge the tube at 500 × g for 5 minutes [13]. This critical step creates four distinct layers:
- A top layer of ethyl acetate.
- A plug of debris at the interface.
- The formalin solution.
- The concentrated parasite sediment at the bottom.
- Free the debris plug by ringing the sides of the tube with an applicator stick.
- Decant the top three layers (ethyl acetate, debris plug, and formalin) in a single, careful motion [13] [28].
- Use a cotton-tipped applicator to wipe the inner walls of the tube clean of remaining debris.
6. Microscopic Examination:
- Resuspend the final sediment in a few drops of 0.85% saline solution.
- Pipette 1-2 drops onto a microscope slide, apply a coverslip, and examine systematically under the microscope.
- Begin with a 10x objective for initial screening, then switch to a 40x objective for morphological identification of parasites, eggs, larvae, or cysts [3] [13].
Critical Parameters and Troubleshooting
Table 2: Optimized Centrifugation and Fixation Parameters
| Parameter | Optimized Setting | Effect of Deviation | Reference |
|---|---|---|---|
| Centrifugation Speed | 500 × g | Lower speed may yield poor sediment; higher speed may damage fragile forms. | [13] |
| Centrifugation Time | 5 minutes | Insufficient time reduces recovery; excessive time offers no benefit. | [13] |
| Formalin Concentration | 10% | Lower concentration may not preserve all parasites effectively. | [3] [28] |
| Sample Size | 500 mg - 2 g | Smaller samples (<500 mg) reduce sensitivity and detection rate. | [13] [28] |
| Solvent Volume | 3-4 mL Ethyl Acetate | Insufficient volume leads to incomplete debris extraction. | [3] [13] |
The formalin fixation and centrifugation parameters detailed in this application note are foundational to the reliable performance of the FECT protocol. Adherence to the specified reagents, times, and relative centrifugal forces ensures maximum recovery of parasitic elements while removing diagnostic obscuring debris. This standardized protocol provides researchers and drug development professionals with a robust, reproducible, and high-sensitivity tool for intestinal parasite detection in stool specimens, forming a critical step in clinical research and public health interventions.
Within the formalin-ethyl acetate concentration technique (FECT), the addition of ethyl acetate represents a critical juncture that determines the success of both parasite diagnosis and lipidomic analysis. This solvent serves a dual purpose: it efficiently extracts lipid molecules of interest while simultaneously clearing interfering debris from the sample matrix. The procedural consistency of this step directly impacts the sensitivity and specificity of downstream analyses, whether for identifying intestinal parasites in clinical diagnostics or profiling lipid species in research settings. As the broader thesis explores the optimization of FECT for stool specimens, this section specifically details the mechanistic role, standardized protocols, and quantitative performance of ethyl acetate addition across different applications.
Key Functions and Mechanism of Action
Ethyl acetate functions through well-defined physicochemical mechanisms that make it ideal for both debris clearing and lipid extraction. As a solvent of intermediate polarity, it effectively dissolves a wide range of lipid classes while maintaining the integrity of biological structures needed for microscopic identification.
Debris Clearing and Parasite Concentration: In stool specimen processing, ethyl acetate acts as a fat solvent and dehydrating agent. When added to a formalin-fixed fecal suspension and vigorously shaken, it dissolves unwanted fats and organic debris present in the sample. During subsequent centrifugation, these dissolved components form a cohesive plug at the top of the tube, which can be easily discarded. The parasitic elements, including eggs, larvae, and cysts, are sedimented at the bottom of the tube, thus concentrating them for microscopic examination [3] [8] [13]. This process significantly enhances detection sensitivity by purifying and concentrating the target organisms.
Lipid Solubilization and Extraction: In lipidomics, ethyl acetate serves as a green extraction solvent that effectively solubilizes multiple lipid classes. Its chemical properties enable the disruption of lipid-protein complexes and facilitate the partitioning of lipids into the organic phase during liquid-liquid extraction. Studies have demonstrated that methods utilizing ethyl acetate yield quantitative recoveries around 80–90% for most lipid classes from various matrices, including human plasma, serum, and cancer cells [29]. This performance is comparable to traditional chlorinated solvents like methyl-tert-butylether (MTBE) and chloroform, but with improved environmental and safety profiles [29] [30].
Comparative Performance Data
The effectiveness of ethyl acetate-based methods has been quantitatively evaluated against other techniques across different applications. The tables below summarize key performance metrics.
Table 1: Comparative Detection of Intestinal Parasites by Different Concentration Techniques (n=110 samples) [3]
| Parasite Detected | Wet Mount (%) | Formol-Ether (FEC) (%) | Formol-Ethyl Acetate (FAC) (%) |
|---|---|---|---|
| Overall Positivity Rate | 41% | 62% | 75% |
| Blastocystis hominis | 9% | 15% | 15% |
| Entamoeba histolytica | 31% | 26% | 24% |
| Giardia lamblia | 20% | 18% | 16% |
| Ascaris lumbricoides | 10% | 6% | 8% |
| Hymenolepis nana | 1% | 6% | 6% |
| Strongyloides stercoralis | 2% | 3% | 5% |
Table 2: Lipid Extraction Efficiency of Green Solvents vs. Established Methods [29] [31] [30]
| Extraction Method | Primary Solvents | Key Advantages | Reported Lipid Recovery |
|---|---|---|---|
| Automated Green Extraction | Ethyl Acetate, Ethanol | • Lower toxicity• Automated, high-throughput• Reduced operator solvent exposure | ~80-90% for most lipid classes, comparable to MTBE |
| Folch Method | Chloroform, Methanol | • High extraction breadth for diverse lipid classes | Considered a gold standard; high for most classes |
| Bligh & Dyer Method | Chloroform, Methanol | • Rapid• Effective for animal tissues | Similar to Folch for predominant phospholipids |
| MeOH-TBME Method | Methanol, tert-Butyl Methyl Ether | • Avoids chlorinated solvents• Suitable for sphingolipids | Good for lactosyl ceramides; variable for other classes |
Experimental Protocols
Protocol A: Formalin-Ethyl Acetate Concentration for Stool Specimens
This protocol, adapted from the CDC and recent clinical studies, is optimized for the concentration of parasitic elements in stool specimens prior to microscopic examination [3] [8] [13].
Research Reagent Solutions
| Reagent/Material | Function in the Protocol |
|---|---|
| 10% Formalin Solution | Fixes and preserves parasitic structures. |
| Ethyl Acetate | Extracts fats and debris, forming a clean plug. |
| Saline (0.85% NaCl) | Provides an isotonic medium for suspension. |
| Conical Centrifuge Tubes | Vessel for centrifugation and phase separation. |
| Gauze or Strainer | Removes large, coarse particulate matter. |
Step-by-Step Procedure:
- Emulsification and Fixation: Emulsify approximately 1 gram of stool specimen in 7 mL of 10% formalin solution in a centrifuge tube. Fix for 10 minutes.
- Filtration: Strain the suspension through wet gauze (or a commercial fecal concentrator) into a new 15 mL conical centrifuge tube to remove large debris.
- Dilution: Add 0.85% saline or 10% formalin through the debris on the gauze to bring the total volume in the tube to 15 mL.
- First Centrifugation: Centrifuge at 500 × g for 10 minutes. Decant the supernatant completely.
- Resuspension: Resuspend the sediment in 10 mL of 10% formalin and mix thoroughly.
- Ethyl Acetate Addition: Add 4 mL of ethyl acetate to the suspension. Stopper the tube securely.
- Vigorous Shaking: Shake the tube vigorously in an inverted position for at least 30 seconds to ensure thorough mixing of the phases. Carefully release pressure by removing the stopper.
- Second Centrifugation: Recentrifuge at 500 × g for 10 minutes. This step results in four distinct layers: a plug of debris and ethyl acetate at the top, a formalin layer, and the sedimented parasites at the bottom.
- Debris Removal: Free the debris plug from the tube wall with an applicator stick and decant the top three layers (debris plug, ethyl acetate, and formalin).
- Final Preparation: Use a cotton-tipped applicator to wipe residual debris from the tube walls. Resuspend the final sediment in a few drops of 10% formalin or saline for microscopic examination.
Protocol B: Automated Lipid Extraction Using Green Solvents
This protocol outlines a modern, automated approach for the quantitative extraction of lipids from biological matrices using ethyl acetate as a key, less hazardous solvent [29].
Research Reagent Solutions
| Reagent/Material | Function in the Protocol |
|---|---|
| Ethyl Acetate | Primary green solvent for lipid dissolution. |
| Ethanol | Polar solvent to disrupt lipid-protein complexes. |
| Internal Standards | e.g., PC 13:0/13:0, for recovery quantification. |
| Automated Liquid Handler | Ensures precision, reproducibility, and high throughput. |
Step-by-Step Procedure:
- Sample Preparation: Transfer a precise volume of sample (e.g., 50 μL of human plasma or serum) to a designated well on the automated liquid handler platform.
- Internal Standard Addition: Add a known amount of appropriate internal lipid standards to each sample to correct for extraction efficiency and instrumental variability.
- Protein Precipitation & Disruption: Add a volume of ice-cold ethanol to the sample. The automated system mixes the solution vigorously to disrupt protein-lipid complexes and precipitate proteins.
- Lipid Extraction: Add a volume of ethyl acetate to the mixture. The system performs automated, timed mixing to ensure complete partitioning of lipids into the organic solvent phase.
- Phase Separation: The platform executes a centrifugation step to achieve clear phase separation.
- Organic Phase Collection: The automated liquid handler precisely transfers the upper organic phase (containing the extracted lipids) to a new, clean vial or microtiter plate.
- Solvent Evaporation: Evaporate the solvent under a stream of nitrogen gas in a controlled environment.
- Reconstitution: Reconstitute the dried lipid extract in a solvent compatible with downstream analysis, such as a methanol-isopropanol mixture for LC-MS injection.
- Analysis: Proceed with lipidomic analysis via LC-MS/MS. The extraction recovery is calculated by comparing the peak areas of the internal standards to their expected values.
Troubleshooting and Technical Notes
- Incomplete Debris Plug Formation: Ensure vigorous and thorough shaking after ethyl acetate addition. An incomplete plug may result from insufficient mixing, compromising the clarity of the final sediment. Re-shake and re-centrifuge if the plug is not firm [8].
- Low Lipid Recovery Yields: Verify the solvent-to-sample ratio. For automated systems, confirm that the liquid handler is accurately dispensing the ethyl acetate. The use of mechanical pretreatments (e.g., bead beating for microalgae) may be necessary to disrupt robust cell walls before solvent addition [30].
- Solvent Evaporation Considerations: Ethyl acetate has a relatively low boiling point. When evaporating under nitrogen, use a gentle stream and avoid excessive heat to prevent the loss of volatile lipid components.
- Safety and Environmental Considerations: While ethyl acetate is less toxic than chloroform or ether, it remains flammable and should be handled in a well-ventilated area or fume hood. Its classification as a "greener" solvent contributes to a reduced environmental footprint compared to traditional halogenated solvents [29] [30].
The formal-ethyl acetate concentration (FEC) technique, particularly the sedimentation method, is a cornerstone procedure in diagnostic parasitology for enhancing the detection of parasitic elements in stool specimens [8]. This step is critical for separating parasites from fecal debris, thereby concentrating them and significantly increasing the probability of microscopic identification, especially when parasite loads are low [8]. The resulting sediment is a versatile material that serves as the direct substrate for two primary analytical paths: the examination of wet mounts for motile forms and cysts, and the preparation of stained smears for detailed morphological studies and organism identification [8] [20]. This section details the standardized protocols for preparing this essential sediment for its subsequent applications.
Workflow for Sediment Utilization
The sediment obtained from the concentration procedure is the starting point for multiple diagnostic pathways. The diagram below outlines the decision-making process for its use in wet mounts and stained smears.
Diagram 1: Diagnostic pathways for concentrated sediment.
Detailed Experimental Protocols
Protocol for Wet Mount Examination from Sediment
The examination of wet mounts is a rapid technique primarily used for observing motile trophozoites and the internal structures of cysts [8] [32].
Materials:
- Concentrated sediment [8]
- Glass slides and coverslips [32]
- 0.85% saline or distilled water (Note: water may deform Blastocystis hominis) [8]
- Lugol's iodine (optional, for cyst identification) [32]
- Microscope with 10x, 40x, and 100x objectives
Procedure:
- Resuspend Sediment: Using a pipette, gently agitate the concentrated sediment in the centrifuge tube to ensure a homogenous suspension [8].
- Prepare Smear: Place one to two drops of the well-mixed sediment onto a clean glass slide [32].
- Apply Coverslip: Carefully lower a coverslip onto the drop, avoiding air bubbles [32].
- Microscopic Examination:
- Systematically scan the entire smear under 100x magnification, then switch to 400x for detailed observation [32].
- Reduce the light intensity and adjust the condenser to enhance contrast for better visualization of internal structures [32].
- For iodine-enhanced morphology, a drop of Lugol's iodine can be added before applying the coverslip. Note that this will kill motile trophozoites [32].
Critical Considerations:
- Timing: For optimal observation of motile trophozoites, wet mounts should be examined immediately after preparation. Liquid specimens should be examined within 30 minutes of passage, and soft specimens within one hour [8].
- Smear Thickness: The smear should not be too thick. A common quality check is to place the slide on top of printed text; if the letters are not visible through the mixture, it is too thick and requires more diluent or less sediment [32].
Protocol for Stained Smear Preparation from Sediment
Permanent staining is indispensable for the definitive identification of cysts, trophozoites, and other parasitic structures, allowing for detailed observation of internal morphology.
Materials:
- Concentrated sediment [8] [20]
- Glass slides
- Slide warmer or room temperature air-drying setup
- Appropriate stains (e.g., Trichrome, Modified Acid-Fast, Chromotrope) [20]
- Mounting media and coverslips
Procedure:
- Prepare Smear: Insure the sediment is well-mixed. Apply 2 to 3 drops of the sediment to a glass slide, depending on its density [8] [20].
- Fixation:
- Staining: Proceed with the specific staining procedure of choice. The fixed smears can be stained immediately or stored for several months in a protective slide tray for future staining [8].
Common Staining Techniques & Applications:
- Trichrome Stain: The standard for general identification of intestinal protozoa (cysts and trophozoites), human cells, and yeast in permanently stained smears [20].
- Modified Acid-Fast Stain: Used for the identification of oocysts of coccidian parasites like Cryptosporidium spp., Cystoisospora spp., and Cyclospora spp., which stain a pinkish-red against a green background [20].
- Chromotrope Staining: The primary method for differentiating microsporidia spores from background fecal elements, staining the spore walls a pinkish-red color [20].
Performance Data & Comparative Analysis
The effectiveness of the formal-ethyl acetate sedimentation technique in preparing sediment for microscopic analysis is demonstrated by its superior sensitivity compared to direct, unconcentrated methods. The following table summarizes quantitative performance data from comparative studies.
Table 1: Comparative Sensitivity of Diagnostic Methods in Parasite Detection
| Parasite / Context | Diagnostic Method | Detection Rate / Key Finding | Citation |
|---|---|---|---|
| Various Intestinal Parasites | Formalin-Ethyl Acetate Concentration (FAC) | 75% (82/110 samples) | [3] |
| Formalin-Ether Concentration (FEC) | 62% (68/110 samples) | [3] | |
| Direct Wet Mount (Unconcentrated) | 41% (45/110 samples) | [3] | |
| Strongyloides stercoralis | Agar Plate Culture (APC) | 23.52% (290/1233 samples); Highly sensitive reference method | [33] |
| Quantitative FAC (QFEC) | 10.54% (130/1233 samples); Less sensitive than APC for low burdens | [33] | |
| QFEC vs. APC at high burden | 97.8% (45/46) of samples with >50 larvae/gm by QFEC were positive by APC | [33] |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Sediment Preparation and Analysis
| Reagent / Material | Function / Application | Technical Notes |
|---|---|---|
| 10% Formalin | Primary fixative and preservative for stool specimens; used in the sedimentation process. | Preserves protozoan cysts and helminth eggs; suitable for wet mounts, immunoassays, and staining [8]. |
| Ethyl Acetate | Solvent used in the diphasic sedimentation technique. | Replaces the more flammable diethyl ether; acts as a debris extractor and lipid solvent, clearing the final sediment [8]. |
| Polyvinyl Alcohol (PVA) | Coprecipitating fixative and adhesive. | Primarily used for preserving protozoan trophozoites and cysts for permanent stained smears (e.g., Trichrome) [8]. |
| Trichrome Stain | Permanent staining for intestinal protozoa. | Facilitates detection and identification of cysts and trophozoites, providing a permanent record [20]. |
| Modified Acid-Fast Stain (e.g., Kinyoun's) | Differential staining for coccidian parasites. | Identifies oocysts of Cryptosporidium, Cystoisospora, and Cyclospora [20]. |
| Chromotrope 2R-based Stain | Staining of microsporidian spores. | Critical for detecting small (∼1 µm) spores of microsporidia in fecal and clinical specimens [20]. |
| Kadsurindutin H | Kadsurindutin H | Kadsurindutin H is a natural product for research. This product is For Research Use Only (RUO). Not for human or veterinary use. |
| Oxazolidine-2,4-dithione | Oxazolidine-2,4-dithione, MF:C3H3NOS2, MW:133.20 g/mol | Chemical Reagent |
The microscopic examination of stool specimens remains a cornerstone in the diagnosis of parasitic infections, which pose a significant global health burden. Soil-transmitted helminths (STHs) alone infect over 1.5 billion people worldwide, with the highest prevalence in tropical and subtropical regions [34]. The formalin-ethyl acetate concentration technique (FECT) is one of the most widely used methods in clinical and research laboratories for concentrating parasitic elements from stool specimens to facilitate their microscopic identification. This method significantly improves detection sensitivity by removing debris and concentrating parasites, though its efficacy can be affected by various factors related to stool composition and procedural details [35]. Within the broader thesis research on enhancing FECT methodologies, this document provides detailed application notes and protocols for the reliable identification of common helminths and protozoa, serving as an essential resource for researchers, scientists, and drug development professionals engaged in parasitology research and diagnostic innovation.
Morphological Comparison of Intestinal Parasites
Differential Morphology of Intestinal Amebae
Accurate morphological differentiation is fundamental to parasite identification. The tables below summarize key characteristics for the microscopic identification of common intestinal amebae in their trophozoite and cyst stages.
Table 1: Differential Morphology of Intestinal Amebae - Trophozoites [18]
| Species | Size (Length) | Motility Description | Number of Nuclei | Peripheral Chromatin | Karyosomal Chromatin | Cytoplasmic Inclusions |
|---|---|---|---|---|---|---|
| Entamoeba histolytica | 10-60 µm (15-20 µm typical) | Progressive, hyaline, finger-like pseudopods | 1 | Fine, evenly distributed granules | Small, discrete, usually central | RBCs occasionally |
| Entamoeba hartmanni | 5-12 µm (8-10 µm typical) | Usually non-progressive | 1 | Similar to E. histolytica | Small, discrete, often eccentric | Bacteria |
| Entamoeba coli | 15-50 µm (20-25 µm typical) | Sluggish, non-progressive, blunt pseudopods | 1 | Coarse, irregular granules | Large, discrete, usually eccentric | Bacteria, yeasts |
| Endolimax nana | 6-12 µm (8-10 µm typical) | Sluggish, non-progressive, blunt pseudopods | 1 | None | Large, irregular, blot-like | Bacteria |
| Iodamoeba bütschlii | 8-20 µm (12-15 µm typical) | Sluggish, usually non-progressive | 1 | None | Large, central, with achromatic granules | Bacteria, yeasts |
Table 2: Differential Morphology of Intestinal Amebae - Cysts [18]
| Species | Size (Diameter) | Shape | Number of Nuclei (Mature Cyst) | Peripheral Chromatin | Karyosomal Chromatin | Cytoplasmic Inclusions |
|---|---|---|---|---|---|---|
| Entamoeba histolytica | 10-20 µm (12-15 µm typical) | Spherical | 4 | Fine, uniform, evenly distributed | Small, discrete, usually central | Chromatoid bars with rounded ends |
| Entamoeba hartmanni | 5-10 µm (6-8 µm typical) | Spherical | 4 | Similar to E. histolytica | Similar to E. histolytica | Chromatoid bars with rounded ends |
| Entamoeba coli | 10-35 µm (15-25 µm typical) | Spherical | 8 | Coarse, irregular granules | Large, discrete, usually eccentric | Splinter-like chromatoid bodies |
| Endolimax nana | 5-10 µm (6-8 µm typical) | Spherical to oval | 4 | None | Large, blot-like, usually central | Granules occasionally; no distinct chromatoid bodies |
| Iodamoeba bütschlii | 5-20 µm (10-12 µm typical) | Irregular shapes | 1 | None | Large, usually eccentric | Compact, well-defined glycogen mass |
Differential Morphology of Intestinal Flagellates
Table 3: Differential Morphology of Common Intestinal Flagellates - Trophozoites [18]
| Species | Size (Length) | Shape | Motility Description | Number of Nuclei | Number of Flagella | Distinguishing Features |
|---|---|---|---|---|---|---|
| Giardia duodenalis | 10-20 µm (12-15 µm typical) | Pear-shaped | "Falling leaf" | 2 | 8 total (4 lateral, 2 ventral, 2 caudal) | Large sucking disk |
| Chilomastix mesnili | 6-24 µm (10-15 µm typical) | Pear-shaped | Stiff, rotary | 1 | 4 total (3 anterior, 1 in cytosome) | Prominent cytostome, spiral groove |
| Pentatrichomonas hominis | 6-20 µm (11-12 µm typical) | Pear-shaped | Nervous, jerky | 1 | 4-5 anterior, 1 posterior | Undulating membrane full body length |
Detailed Experimental Protocols
Formalin-Ethyl Acetate Concentration Technique (FECT): Standard Protocol
The FECT method is a sedimentation technique that uses formalin to preserve parasitic elements and ethyl acetate to dissolve fats and remove debris, thereby concentrating parasites in the sediment [35].
Materials Required:
- 10% formalin
- Ethyl acetate
- Centrifuge tubes (15 mL conical)
- Gauze or sieve
- Centrifuge
- Applicator sticks
- Microscope slides and coverslips
- Saline solution
- Iodine solution (for temporary staining)
Procedure:
- Specimen Preparation: Emulsify approximately 1-2 grams of fresh stool in 10 mL of 10% formalin in a centrifuge tube. For preserved specimens, use previously fixed material [36] [35].
- Filtration: Strain the suspension through gauze or a sieve into a clean 15 mL conical centrifuge tube to remove large particulate matter.
- Solvent Addition: Add 3-4 mL of ethyl acetate to the filtered suspension. Place the cap on the tube and shake vigorously for 10-15 seconds to ensure thorough mixing [36] [35].
- Centrifugation: Centrifuge at 500 × g for 2-3 minutes. Four distinct layers will form: a thin layer of ethyl acetate at the top, a plug of debris, a formalin layer, and the sediment at the bottom containing the concentrated parasites [35].
- Separation: Loosen the debris plug by ringing it with an applicator stick. Carefully decant the top three layers, leaving the sediment undisturbed.
- Sediment Preparation: Mix the remaining sediment with a small amount of formalin or saline. Transfer one drop to a microscope slide and prepare both saline and iodine-stained wet mounts for examination.
- Microscopic Examination: Systematically examine the entire coverslip area under 100× and 400× magnification. For optimal sensitivity, examine multiple drops of sediment (at least 5 drops recommended) [36].
Optimized FECT Protocol for Enhanced Sensitivity
Recent research has demonstrated that diagnostic sensitivity can be significantly improved by modifying standard FECT procedures:
Multiple Drop Examination:
- The standard protocol of examining two drops of sediment has limited sensitivity, particularly for light-intensity infections [36].
- An optimized approach involves examining at least five drops of sediment, which has been shown to increase detection rates by approximately 15% compared to the standard two-drop method [36].
- In field studies, this optimized protocol detected Opisthorchis viverrini eggs in 25 of 82 individuals (30.5%) who had positive urine antigen tests but were negative by standard FECT [36].
Acid Addition for Problematic Specimens:
- For specimens where fecal bulk fails to float properly after ethyl acetate treatment, recent research indicates that adding small amounts of HCl or acetic acid can improve flotation efficiency [35].
- The acid helps dissolve cellulose fibers in plant material, releasing trapped oil droplets and facilitating better separation [35].
- This modification is particularly valuable for laboratories processing specimens from populations with high-fiber diets.
Urine Antigen Detection Protocol
While not a microscopic technique, antigen detection serves as an important complementary method:
Sample Preparation:
- Collect first-morning midstream urine and centrifuge at 277 × g for 15 minutes at 4°C [36].
- Aliquot clarified supernatant and store at -20°C until testing.
- Pretreat urine samples with an equal volume of 4% trichloroacetic acid (TCA) solution, incubate for 20 minutes at room temperature, then neutralize with an equal volume of 0.244 M carbonate buffer (pH 9.6) [36].
Monoclonal Antibody-Based ELISA:
- Coat polystyrene plates with monoclonal antibody (5 μg/mL) in bicarbonate buffer overnight at 4°C [36].
- After blocking, add pretreated urine samples and incubate at 37°C for 2 hours.
- Add protein A-purified rabbit IgG against crude parasite antigen extract, followed by biotinylated goat anti-rabbit IgG and streptavidin-horseradish peroxidase conjugate [36].
- Develop with OPD substrate, stop with Hâ‚‚SOâ‚„, and read absorbance at 492 nm.
- Calculate antigen concentration from standard curves; positive threshold typically >19.4 ng/mL for Opisthorchis viverrini [36].
Advanced Diagnostic Approaches
Comparative Diagnostic Performance
Table 4: Comparison of Diagnostic Methods for Parasite Detection [36] [34]
| Diagnostic Method | Principle | Sensitivity Range* | Advantages | Limitations |
|---|---|---|---|---|
| FECT (Standard) | Sedimentation and concentration | 58.2% (compared to composite) | Wide availability, preserves morphology | Moderate sensitivity, requires expertise |
| FECT (Optimized) | Multiple sediment examinations | 67.0% (compared to composite) | Improved sensitivity, minimal additional cost | Increased examination time |
| Urine Antigen Detection | Monoclonal antibody-based assay | 98.8% (compared to composite) | High sensitivity, convenient sample collection | Limited parasite targets, requires specific reagents |
| Kato-Katz (Microscopy) | Thick smear and clearing | Varies by parasite species | Quantifies infection intensity, low cost | Low sensitivity for light infections |
| Molecular Methods (PCR) | Nucleic acid amplification | 90-95% for most parasites | High sensitivity and specificity, species differentiation | Higher cost, technical requirements |
*Sensitivity values are representative and may vary by parasite species and infection intensity [36] [34].
Emerging Techniques and Methodological Innovations
Deep Learning in Parasite Microscopy:
- Convolutional Neural Networks (CNNs) are increasingly applied for automated detection and classification of parasites in microscopic images [37].
- Models like U-Net are used for segmentation of red blood cells in malaria diagnosis, while Faster R-CNN detects small cell objects in connected component clusters [37].
- Modified YOLO (You Only Look Once) architectures have been optimized for detecting small objects such as Plasmodium in images captured by smartphone cameras attached to microscope eyepieces [37].
- These approaches show promise for addressing the shortage of skilled microscopists in remote areas, with some models achieving patient-level accuracy exceeding 97% in controlled studies [37].
Antigen Detection Assays:
- Commercial antigen detection tests are available for Cryptosporidium spp., Giardia duodenalis, and Entamoeba histolytica [38].
- Direct fluorescent antibody (DFA) tests are considered the test of choice for cryptosporidiosis and giardiasis, with reported sensitivity and specificity of 99-100% [38].
- Rapid immunochromatographic cartridge tests provide multiple results in a single device with short test times, making them suitable for clinical settings [38].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Essential Research Reagents and Materials for Parasitology Research [36] [18] [38]
| Reagent/Material | Function/Application | Notes |
|---|---|---|
| 10% Formalin | Fixation and preservation of stool specimens | Maintains parasite morphology |
| Ethyl Acetate | Organic solvent for lipid extraction | Reduces debris, cleans background |
| Diethyl Ether | Alternative organic solvent | Similar function to ethyl acetate |
| Saline Solution | Preparation of wet mounts for microscopy | Maintains osmotic balance |
| Iodine Solution | Staining of cysts for structural details | Highlights nuclei and inclusions |
| Trichloroacetic Acid (TCA) | Protein precipitation for antigen detection | Used in urine antigen test preparation |
| Carbonate Buffer | Neutralization of acid-treated samples | For antigen detection assays |
| Monoclonal Antibodies | Target-specific capture/detection in ELISA | Key to specificity in antigen assays |
| Permanent Stains (Trichrome) | Enhanced morphological visualization | Allows detailed structural study |
| Microplate Readers | Absorbance measurement in ELISA | Quantification of antigen levels |
| 1-Methoxybutane-2-thiol | 1-Methoxybutane-2-thiol | 1-Methoxybutane-2-thiol (C5H12OS) is a chemical building block for research. This product is For Research Use Only (RUO). Not for human or personal use. |
| 1,3-Di(pyren-1-yl)benzene | 1,3-Di(pyren-1-yl)benzene, MF:C38H22, MW:478.6 g/mol | Chemical Reagent |
The formalin-ethyl acetate concentration technique remains a fundamental method in parasitology research, particularly when optimized through multiple sediment examinations and procedural refinements. While microscopic examination provides the foundation for parasite identification, integrating these methods with emerging technologies—including antigen detection assays and deep learning approaches—creates a powerful diagnostic and research toolkit. The protocols and application notes detailed herein provide researchers with robust methodologies for advancing studies in parasite biology, drug development, and diagnostic innovation, ultimately contributing to improved control strategies for parasitic infections that continue to affect global health.
Troubleshooting Common FECT Issues and Method Optimization
The formalin-ethyl acetate concentration technique (FECT) remains a cornerstone diagnostic procedure for intestinal parasitic infections in research and clinical laboratories worldwide due to its simplicity, cost-effectiveness, and established protocols [39]. Despite its widespread use, FECT encounters significant sensitivity limitations that can lead to missed infections, particularly in cases of low parasitic load, early-stage infections, or during large-scale screening efforts. These diagnostic delays contribute substantially to morbidity, mortality, and ongoing disease transmission [40]. This application note systematically analyzes the technical causes of low sensitivity in conventional FECT and presents validated solutions and advanced methodologies to enhance detection capabilities for researchers and scientists working in drug development and diagnostic innovation.
Quantitative Analysis of Sensitivity Limitations
Table 1: Comparative Sensitivity of Diagnostic Methods for Parasitic Infections
| Diagnostic Method | Target Pathogen | Reported Sensitivity | Reference Standard | Study Sample Size |
|---|---|---|---|---|
| Standard FECT (2 drops) | Opisthorchis viverrini | 58.2% | Composite reference | 82 antigen-positive cases [36] |
| Optimized FECT (5 drops) | Opisthorchis viverrini | 67.0% | Composite reference | 82 antigen-positive cases [36] |
| Urine Antigen Detection | Opisthorchis viverrini | 98.8% | Composite reference | Field-collected samples [36] |
| Blood Culture | Salmonella enterica | 48.0% | Clinical diagnosis | 100 suspected cases [41] |
| Stool Culture | Salmonella enterica | 32.0% | Clinical diagnosis | 100 suspected cases [41] |
| Direct Blood qPCR (ttr gene) | Salmonella enterica | 82.0% | Clinical diagnosis | 100 suspected cases [41] |
| Enriched Blood qPCR (ttr gene) | Salmonella enterica | 90.0% | Clinical diagnosis | 100 suspected cases [41] |
Table 2: Performance Metrics of Advanced Detection Technologies
| Technology | Pathogens Detected | Accuracy | Sensitivity | Specificity | Key Advantage |
|---|---|---|---|---|---|
| DINOv2-large (AI model) | Intestinal parasites | 98.93% | 78.00% | 99.57% | Self-supervised learning [39] |
| YOLOv8-m (AI model) | Intestinal parasites | 97.59% | 46.78% | 99.13% | Object detection approach [39] |
| Convolutional Neural Network | 27 parasite classes | 98.6% agreement | Superior to manual | High | Detects 169 additional organisms [42] |
| Commercial RT-PCR | Giardia, Cryptosporidium, etc. | High | High | High | Species differentiation [43] |
| In-house RT-PCR | Entamoeba histolytica | High | High | High | Identifies pathogenic species [43] |
Technical Causes of Low Sensitivity
Sample Processing Limitations
The standard FECT protocol examines only two drops of fecal suspension, representing a minute fraction of the total sample. Research demonstrates that this limited sampling volume fails to detect low-intensity infections, with optimized protocols examining five drops identifying 30.5% additional positive cases missed by standard methods [36]. The inhomogeneous distribution of parasites in stool further exacerbates this sampling error, leading to inconsistent detection across replicates.
Operator Dependency and Expertise
Microscopic examination requires substantial expertise for accurate identification, particularly for protozoa with overlapping morphological characteristics. Differentiation between pathogenic Entamoeba histolytica and non-pathogenic Entamoeba dispar is impossible by microscopy alone, requiring molecular confirmation [43]. Survey data indicate that diagnostic delays frequently occur when the appropriate test is not ordered initially or when specialist consultation is delayed [40].
Biological and Technical Constraints
The robust wall structure of protozoan cysts and oocysts complicates DNA extraction for molecular detection [43]. For helminths, prepatent periods (before egg production) and irregular egg laying patterns contribute to false negatives. Additionally, sample preservation methods can affect morphological integrity, with suboptimal fixation distorting key diagnostic features [39].
Integrated Solutions for Enhanced Detection
Protocol Optimization: Modified FECT
Workflow for FECT Optimization
Materials and Reagents
- Fresh stool sample (1-2 g)
- 10% formalin solution
- Ethyl acetate
- Gauze for filtration
- Centrifuge tubes (15 mL conical)
- Centrifuge (capable of 2,500 rpm/769 × g)
- Microscope slides and coverslips
- Light microscope with 10×, 40× objectives
Optimized Procedure
Sample Preparation: Emulsify 2 g of fresh stool in 10 mL of 10% formalin and strain through gauze to remove large particulate matter [36].
Concentration: Add 3 mL of ethyl acetate to the filtered suspension, vortex vigorously for 15 seconds, and centrifuge at 2,500 rpm (769 × g) for 5 minutes [36].
Sediment Examination: Discard the supernatant and resuspend the sediment in 10% formalin. Transfer to a clean tube and homogenize thoroughly.
Multiple Drop Analysis: Place five separate drops of the resuspended sediment on a microscope slide rather than the standard two drops [36].
Systematic Examination: Examine each drop methodically using a consistent scanning pattern at 100× and 400× magnification.
Quality Control: Include positive control samples with known low-intensity infections to validate detection sensitivity.
Advanced Molecular Detection
Molecular Detection Pathways
Enriched Blood qPCR for Salmonella Detection
Principle: This method combines blood culture enrichment with targeted amplification of Salmonella-specific genes (ttr and InvA), significantly improving sensitivity over conventional culture methods [41].
Reagents and Equipment:
- BacT/Alert blood culture bottles (bioMérieux)
- Tryptic Soy Broth (TSB) with 5% bile
- QIAamp DNA extraction kit (Qiagen)
- Primers for ttr and InvA genes [41]
- Maxima SYBR Green qPCR Master Mix
- Real-time PCR system (Applied Biosystems 7500)
Procedure:
- Sample Collection and Enrichment: Inoculate 7 mL of blood into BacT/Alert culture bottle and incubate until positive or for up to 7 days. For direct enrichment, mix 1.5 mL blood with equal volume TSB + 5% bile and incubate 5 hours at 37°C [41].
DNA Extraction: Extract DNA from 350 μL of enriched blood using QIAamp kit according to manufacturer's protocol.
qPCR Setup: Prepare 25 μL reactions containing:
- 12.5 μL Maxima SYBR Green Master Mix
- 1 μL forward primer (20 μM)
- 1 μL reverse primer (20 μM)
- 5 μL DNA template
- 5.5 μL nuclease-free water
Amplification Parameters:
- Initial denaturation: 95°C for 10 min
- 45 cycles of: 95°C for 15 s, 60°C for 30 s, 72°C for 30 s
- Melt curve analysis: 60°C to 95°C
Interpretation: Ct values <37 cycles indicate positive detection [41].
Artificial Intelligence and Automated Detection
Principle: Deep learning algorithms trained on extensive image datasets can identify parasitic elements in stool samples with superior sensitivity and consistency compared to human examiners [39] [42].
Implementation Workflow:
Image Acquisition: Capture digital micrographs of FECT-prepared slides at multiple magnifications.
AI Analysis: Process images through trained convolutional neural networks (CNNs) or vision transformers (ViTs).
Validation: ARUP Laboratories' implementation demonstrated 98.6% positive agreement with manual review while identifying 169 additional organisms missed by technologists [42].
Model Performance: The DINOv2-large architecture achieved 98.93% accuracy, 78.00% sensitivity, and 99.57% specificity for intestinal parasite identification, outperforming human experts in controlled studies [39].
Research Reagent Solutions
Table 3: Essential Research Reagents for Enhanced Parasite Detection
| Reagent/Kit | Application | Key Features | Research Utility |
|---|---|---|---|
| Formalin-Ethyl Acetate | FECT processing | Preserves morphology, concentrates parasites | Standardized sample preparation for comparative studies [36] |
| MagNA Pure 96 DNA Kit | Nucleic acid extraction | Automated, high-throughput | Consistent DNA recovery for molecular studies [43] |
| AusDiagnostics RT-PCR | Protozoan detection | Commercial multiplex | Standardized detection of Giardia, Cryptosporidium, E. histolytica [43] |
| Monoclonal Antibody ELISA | Urine antigen detection | High sensitivity (98.8%) | Non-invasive screening for opisthorchiasis [36] |
| S.T.A.R. Buffer | Stool storage | Preserves nucleic acids | Maintains DNA integrity for molecular work [43] |
| SYBR Green Master Mix | qPCR detection | Sensitive intercalating dye | Flexible pathogen detection with melt curve analysis [41] |
Addressing the sensitivity limitations of conventional FECT requires a multifaceted approach combining protocol optimization, molecular verification, and emerging technologies. The implementation of modified FECT examining five sediment drops increases detection sensitivity by approximately 15%, while integration with antigen detection and PCR-based methods can achieve sensitivities exceeding 90% [36] [41]. Deep learning systems demonstrate particular promise, with DINOv2-large models achieving 98.93% accuracy and identifying additional organisms missed by human technologists [39] [42]. For research applications and drug development programs, adopting these integrated approaches significantly reduces false-negative rates, enabling more accurate prevalence studies, therapeutic efficacy assessments, and ultimately improving patient outcomes through earlier detection and intervention.
Handling Excessive Debris and Poor Sediment Quality
The formalin-ethyl acetate concentration technique (FECT) is a cornerstone sedimentation method in diagnostic parasitology, widely recommended for the detection of intestinal parasites in stool specimens [8]. The procedure functions by concentrating parasitic elements through the differential specific gravity between parasites and fecal debris, utilizing ethyl acetate as an extractor of fats and oils to yield a cleaner sediment for microscopic examination [21] [8]. However, researchers and clinical scientists frequently encounter a significant operational challenge: excessive debris and poor sediment quality that can obscure parasitic forms, thereby reducing diagnostic sensitivity and reliability. This problem is particularly prevalent in certain sample types where fecal bulk fails to float after ethyl acetate treatment, trapping parasite eggs and cysts within a matrix of undigested plant fiber and other particulate matter [21]. This application note delineates the underlying mechanisms of this limitation and provides evidence-based, optimized protocols to enhance sediment quality within the broader context of methodological refinements in FECT-based parasitological research.
Mechanisms and Impact of Suboptimal Sedimentation
Understanding the root causes of poor sedimentation is fundamental to developing effective countermeasures. Recent investigative work has revealed that the interaction between ethyl acetate and cellulose within undigested plant material in stool specimens plays a pivotal role. The proximity of cellulose fibers to ethyl acetate appears to enhance the efficacy of oil extraction from this matrix. However, this process can simultaneously liberate unabsorbed oil droplets that become trapped within the persistent leaf mesophyll structure [21]. This complex interplay results in a fecal bulk that resists proper flotation, leading to a sediment layer contaminated with excessive debris that compromises microscopic visualization.
The impact of suboptimal sedimentation extends beyond mere technical inconvenience. Studies have demonstrated that the diagnostic sensitivity of FECT varies considerably depending on the parasite species and infection intensity. For instance, the technique shows markedly low sensitivity (28.6%) for detecting low-intensity Schistosoma japonicum infections [44]. Similarly, for human strongyloidiasis, the quantitative formalin ethyl acetate concentration technique (QFEC) could only reliably substitute for the more sensitive agar plate culture method when the parasite load exceeded 50 larvae per gram of stool [33] [45]. These limitations are exacerbated when sediment quality is poor, as technicians must examine slides with high debris content, increasing the likelihood of missing scanty parasitic elements and consequently reducing the diagnostic accuracy essential for both clinical trials and epidemiological studies.
Comparative Performance Data
The following tables summarize key comparative studies evaluating FECT against other concentration methods, highlighting its performance limitations and advantages under various conditions.
Table 1: Comparative Sensitivity of FECT for Different Parasite Species
| Parasite Species | Comparative Method | FECT Performance | Key Findings | Reference |
|---|---|---|---|---|
| Schistosoma japonicum | Kato-Katz, Hatching Test | 28.6% sensitivity | Detected disappointingly few positives in low-intensity infections | [44] |
| Strongyloides stercoralis | Agar Plate Culture (APC) | 35.38% positivity agreement | QFEC could substitute for APC only when parasite load >50 larvae/g | [33] [45] |
| Hookworm, Trichuris trichiura, Small Liver Flukes | Formalin-Based Concentration (FC) | Superior detection | FECT was significantly better than crude formalin concentration | [46] |
| Various Helminths and Protozoa | Mini Parasep SF | Comparable yield, better morphology | Parasep offered less debris and reduced distortion of parasite morphology | [27] |
Table 2: Comparison of Concentration Techniques and Workflow Characteristics
| Method | Relative Parasite Recovery | Sediment Cleanliness | Morphology Preservation | Turnaround Time |
|---|---|---|---|---|
| FECT (Standard) | Baseline | Moderate debris | Satisfactory for most helminth eggs | 10-15 minutes/sample [27] |
| Mini Parasep SF | Comparable to FECT [27] | Superior (less background debris) [27] | Better for delicate structures [27] | ~4 minutes/sample [27] |
| CONSED Method | Higher for some pathogens [47] | Information not specified | Better for trophozoites and juveniles [47] | Information not specified |
Experimental Protocols for Sediment Quality Improvement
Acid-Based Modification Protocol for Refractory Specimens
Based on the finding that cellulose-oil interactions impede flotation, the following protocol modification is recommended for specimens with persistent sedimentation issues.
Research Reagent Solutions:
- Formalin (10%): Primary fixative and preservative.
- Ethyl Acetate: Organic solvent for fat and oil extraction.
- Hydrochloric Acid (HCl) or Acetic Acid: Acid residue to dissolve cellulose and loosen the mesophyll cell wall structure [21].
- Saline (0.85%) or 10% Formalin: For suspension and dilution of sediment.
Methodology:
- Initial Processing: Begin with the standard FECT procedure as outlined by the CDC [8], proceeding through the initial straining and centrifugation steps (500 × g for 10 minutes).
- Supernatant Decanting: After the first centrifugation, decant the supernatant thoroughly.
- Acid Addition: To the sediment, add 10 ml of 10% formalin and mix thoroughly. Then, introduce a controlled volume (e.g., 0.5-1 ml) of HCl or acetic acid to the formalin-sediment mixture. The optimal concentration should be determined empirically but should be sufficient to dissolve cellulose without damaging parasitic structures.
- Vigorous Mixing: Stopper the tube and shake vigorously in an inverted position for 30 seconds to ensure thorough interaction between the acid, fecal material, and solvent.
- Secondary Centrifugation: Centrifuge at 500 × g for 10 minutes. The addition of acid residues has been shown to improve fecal bulk float by disrupting the cellulose trap [21].
- Final Processing: Free the debris plug, decant the top layers of supernatant, and proceed with sediment resuspension and examination as per standard protocol [8].
Standardized FECT Protocol with Integrated Quality Control
For general application, the following CDC-recommended protocol should serve as the baseline, from which modifications can be made.
Alternative Concentration Systems
For laboratories handling moderate-to-high sample volumes, commercial closed systems can standardize processing and improve sediment quality. The Mini Parasep SF system incorporates a two-stage filtration matrix within the stool spoon, which is assembled into a conical collection tube [27].
Methodology:
- Transfer two-level scoops (approximately 5 ml) of stool to the Alcorfix-containing mixing chamber.
- Assemble the chamber to the sedimentation cone holding the vertical filtration device.
- Vortex the entire unit briefly for 10-15 seconds to mix contents.
- Invert the unit to allow contents to filter through the filter thimble.
- Centrifuge at 400 × g for 2 minutes.
- Carefully unscrew and discard the mixing chamber and filter thimble.
- Examine the resulting concentrated pellet, which typically exhibits less background debris and better preservation of parasitic morphology [27].
Essential Research Reagent Solutions
Table 3: Key Reagents for FECT Optimization
| Reagent/Material | Function in Protocol | Application Note |
|---|---|---|
| Ethyl Acetate | Extracts fats and oils, reducing fecal sediment and providing a cleaner background for microscopy. | Superior to hexane for oil extraction from cellulose in fecal matrix [21]. |
| Hydrochloric/Acetic Acid | Dissolves cellulose fibers, loosens mesophyll cell wall structure, promotes bulk flotation. | Critical additive for refractory specimens with high cellulose content [21]. |
| Formalin (10%) | Preserves parasitic morphology, serves as suspension medium for centrifugation. | Standard fixative; can be substituted with alcohol-based fixatives (e.g., PROTO-FIX) in alternative systems for better trophozoite preservation [47]. |
| Alcorfix (Alcohol-based Fixative) | Integrated fixative in Parasep system, eliminates formalin use. | Suitable for field settings, provides good morphological preservation for cysts and eggs [27]. |
| CONSED Solution | Sedimentation solution substituted for formalin in CONSED method. | Reported to yield higher recovery of pathogenic species compared to standard FECT [47]. |
Handling excessive debris and poor sediment quality in FECT requires a multifaceted approach grounded in the understanding of the physicochemical interactions between fecal components and processing reagents. The strategic application of acid modification to dissolve interfering cellulose structures presents a direct solution to the problem of non-floating fecal bulk, significantly improving sediment quality for microscopic examination. Furthermore, the adoption of integrated filtration systems like the Mini Parasep SF can streamline workflow while consistently producing cleaner concentrates, advantageous for laboratories with high specimen throughput.
Future research should focus on standardizing acid concentration and exposure time to maximize efficacy while ensuring no deleterious effects on diverse parasitic forms. The integration of artificial intelligence and digital microscopy platforms offers a promising complementary approach. These systems can pre-classify putative parasitic structures even in suboptimal sediments, flagging them for expert review, thereby reducing technologist fatigue and potentially improving diagnostic accuracy in the face of challenging sample quality [2] [48]. By adopting these evidence-based protocols and exploring emerging technologies, researchers and laboratory scientists can significantly enhance the performance of the formalin-ethyl acetate concentration technique, ensuring its continued relevance as a gold standard in parasitological diagnosis.
Optimizing Centrifugation Speed and Time for Maximum Yield
The formalin-ethyl acetate concentration technique (FECT) is a cornerstone diagnostic procedure in parasitology laboratories worldwide, renowned for its cost-effectiveness and superior recovery of intestinal parasites from stool specimens compared to direct smear methods [2]. The principle involves using formalin to fix the specimen and ethyl acetate to dissolve fats and debris, which is then separated via centrifugation, concentrating parasitic elements in the sediment [13]. While the basic protocol is well-established, centrifugation parameters—specifically relative centrifugal force (RCF) and time—are critical variables that significantly impact diagnostic sensitivity. Optimizing these parameters is essential for maximizing yield, particularly for parasites with low shedding rates or in low-intensity infections, which are common in field and clinical settings. This application note provides a detailed, evidence-based protocol for centrifugation optimization to enhance the performance of the FECT procedure.
Comparative Analysis of Centrifugation Parameters
A comparative analysis of published studies reveals significant variations in centrifugation protocols and their resulting diagnostic yields. The standard FECT protocol often specifies a shorter, lower-force centrifugation, but modifications to these parameters have demonstrated marked improvements in sensitivity for specific parasites.
Table 1: Comparison of Centrifugation Protocols and Their Performance
| Centrifugation Protocol | Overall Parasite Detection Rate | Key Parasites with Improved Detection | Reference / Application Context |
|---|---|---|---|
| Standard FECT(500 g for 5 min) | Implemented as a superior routine technique; specific overall rate not provided [13]. | Hookworm, Trichuris trichiura, small liver flukes [13]. | Routine diagnostics in a migrant population on the Thailand-Myanmar border [13]. |
| Modified FECT for Cryptosporidium(500 g for 10 min) | Sensitivity significantly higher than standard method (99% vs. 86%) [14]. | Cryptosporidium oocysts [14]. | Analysis of 73 formalin-preserved stool specimens known to be positive for Cryptosporidium [14]. |
| Formalin-Ethyl Acetate (FAC) Technique(1500 rpm for 5 min; equivalent to ~500 g) | 75% (82/110 samples) [3]. | Superior recovery of dual infections (e.g., E. histolytica cyst with A. lumbricoides) [3]. | Hospital-based study of 110 children with diarrhea [3]. |
The data indicates that a protocol of 500 g for 5 minutes is effective for general helminth detection and has been adopted as a routine standard [13]. However, for more delicate organisms like Cryptosporidium oocysts, a modified protocol using 500 g for 10 minutes is recommended, as it significantly increases sensitivity by recovering a higher number of oocysts [14]. This extended force and time likely ensure that the lighter oocysts are pelleted more completely, reducing false-negative results.
Experimental Protocols for Centrifugation Optimization
Protocol 1: Standard FECT for General Helminth Detection
This protocol is optimized for the detection of common soil-transmitted helminths and is suitable for routine laboratory use [13].
- Specimen Emulsification: Add approximately 500 mg of fresh or formalin-preserved stool to 10 mL of clean water in a 15 mL conical centrifuge tube. Mix vigorously until the faecal material is fully suspended.
- Filtration: Pour the suspension through a single-use fecal strainer (sieve opening size ~0.6 mm x 0.6 mm) into a new 15 mL conical tube. This step removes large particulate debris.
- First Centrifugation: Centrifuge the filtered suspension at 500 g for 5 minutes. Carefully decant the supernatant.
- Formalin-Ethyl Acetate Addition: Re-suspend the sediment in 10 mL of 10% formalin solution. Add 4 mL of ethyl acetate to the tube.
- Vigorous Mixing: Securely cap the tube and shake it vigorously for at least 30 seconds. Vent the tube carefully to release pressure.
- Second Centrifugation: Centrifuge the mixture at 500 g for 5 minutes. This step forms four distinct layers: an ethyl acetate plug at the top, a plug of debris, a formalin layer, and the concentrated sediment containing parasites at the bottom.
- Supernatant Removal: Free the debris plug from the tube walls using an applicator stick. Decant the top three layers (ethyl acetate, debris, and formalin) without disturbing the sediment.
- Sediment Preparation: Use a cotton-tipped applicator to wipe residual debris from the inner wall of the tube. Re-suspend the final sediment in a small volume of saline (0.85% NaCl) for microscopic examination.
Protocol 2: Modified FECT for Enhanced Recovery ofCryptosporidiumOocysts
This modified protocol is specifically designed for the recovery of Cryptosporidium oocysts and other similarly sized, low-density elements, offering higher sensitivity than the standard method [14].
- Steps 1-4: Identical to Protocol 1.
- Step 5 (Second Centrifugation - Modified): Centrifuge the formalin-ethyl acetate mixture at 500 g for 10 minutes [14].
- Steps 6-7: Identical to Protocol 1.
The increased centrifugation time in this modified protocol allows for a more complete sedimentation of the smaller and lighter Cryptosporidium oocysts, which are more prone to remain in suspension during shorter spins.
Workflow Visualization
The following diagram illustrates the logical sequence and key decision points in the FECT procedure, highlighting the two centrifugation optimization paths.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are fundamental to the execution of a reliable FECT protocol. Their consistent quality is critical for reproducible results.
Table 2: Key Research Reagents and Materials for FECT
| Item | Function / Application Note |
|---|---|
| 10% Formalin Solution | Serves as a fixative and preservative, hardening the stool specimen and killing viable parasites to ensure laboratory safety and stabilize morphology for identification [13]. |
| Ethyl Acetate (Analytical Grade) | A solvent that dissolves fats and removes debris from the sample. It forms a separate layer during centrifugation, trapping cleaned debris at the interface, which is subsequently discarded [13]. |
| Conical Centrifuge Tubes (15 mL) | Tubes with a conical base are essential for concentrating the parasitic sediment into a small, easily accessible area for final sampling [3] [13]. |
| Fecal Filtration Strainers | Single-use strainers with a defined pore size (e.g., 0.6 mm x 0.6 mm) are used to remove large, undigested food particles and debris that could interfere with microscopy [13]. |
| Saline Solution (0.85% NaCl) | An isotonic solution used for the final suspension of the sediment, creating an environment that preserves the morphology of parasitic cysts, oocysts, and eggs during examination [3] [13]. |
| 5-Ethynyl-2-nitropyridine | 5-Ethynyl-2-nitropyridine|RUO |
| MappiodosideA | MappiodosideA, MF:C28H38N2O11, MW:578.6 g/mol |
Preservation Artifacts and Their Impact on Parasite Identification
Within the critical practice of diagnosing intestinal parasitic infections, the formalin-ethyl acetate concentration technique (FECT) remains a cornerstone procedure for stool specimen examination, recommended by leading health authorities for its ability to concentrate parasitic structures and remove obscuring fecal debris [8] [9]. However, the diagnostic accuracy of this and related techniques is fundamentally challenged by preservation artifacts—alterations in the morphology and staining characteristics of parasites introduced by chemical preservatives and processing methods. These artifacts can significantly impede the precise identification of pathogens, potentially leading to misdiagnosis. This application note, framed within broader thesis research on FECT, details the common artifacts, provides protocols for their mitigation, and presents quantitative data on how methodological choices impact parasite recovery and identification, serving as an essential guide for researchers and laboratory professionals in the field of parasitology and drug development.
The Scientist's Toolkit: Essential Research Reagent Solutions
The selection of preservatives and concentration reagents is a primary determinant of specimen quality. The table below catalogues key reagents, their functions, and their associated impacts on parasite morphology.
Table 1: Key Research Reagents in Stool Parasitology
| Reagent Solution | Function in Protocol | Impact on Parasite Identification |
|---|---|---|
| 10% Formalin | Primary fixative and preservative; used in FECT to maintain structural integrity [8]. | Preserves helminth eggs and protozoan cysts well, but can distort nematode juveniles and destroy trophozoites [47]. |
| Ethyl Acetate | Solvent/extractant in FECT; replaces the more flammable diethyl ether to remove fats and debris [8]. | Reduces obscuring debris, improving clarity; generally safer with comparable efficacy to ether [3]. |
| Polyvinyl Alcohol (PVA) | Preservative for adhesion of stool to slides; enables permanent staining for protozoa [8]. | Facilitates critical morphological assessment via trichrome stain, but mercury-based PVA raises environmental and safety concerns [8]. |
| Merthiolate-Iodine-Formalin (MIF) | Combined fixative and staining solution; suitable for field surveys [2]. | Offers convenience but iodine can distort trophozoite morphology, complicating identification [2]. |
| PROTO-FIX | Non-formalin, alcohol-based commercial fixative [47]. | Adequately fixes trophozoites, cysts, eggs, and juvenile worms, reducing distortion seen with formalin [47]. |
| Alcorfix | Alcohol-based fixative integrated in Parasep SF system [27]. | Eliminates need for formalin and mercury; preserves morphology for cysts, oocysts, and eggs [27]. |
| CONSED Solution | Sedimentation solution used as a formalin substitute in concentration methods [47]. | Reported to yield superior parasite recovery, especially for pathogenic species, compared to FECT [47]. |
| 2-Adamantanethiol | 2-Adamantanethiol, MF:C10H16S, MW:168.30 g/mol | Chemical Reagent |
Common Preservation Artifacts and Morphological Impacts
The interaction between parasitic structures and preservatives can lead to a spectrum of artifacts that mimic or obscure key diagnostic features.
Trophozoite Destruction and Distortion: Motile protozoan trophozoites are exceptionally labile. Formalin-based preservatives, while excellent for cysts and eggs, lead to the rapid disintegration of trophozoites, rendering them undetectable in concentrated samples [47] [19]. The MIF technique, while practical, can cause distortion of trophozoites due to the iodine component, complicating species-level identification [2].
Cyst and Egg Wall Alterations: Flotation concentration techniques, which use high-specific-gravity solutions like zinc sulfate, often cause the collapse of cyst and egg walls [8]. Furthermore, in the standard FECT, the walls of some eggs (e.g., Hymenolepis nana, Ascaris lumbricoides, Trichuris trichiura) can appear distorted and entangled in fecal debris, making them difficult to appreciate [27].
Staining Inconsistencies: A critical artifact in the diagnosis of intestinal coccidia is the failure of Cryptosporidium oocysts to retain the modified acid-fast stain after FECT processing, causing them to appear as non-staining "ghosts" and leading to false-negative results [27]. The use of mercury-based PVA can also interfere with some modern staining protocols and molecular assays.
Juvenile Nematode Distortion: As noted in evaluations of commercial systems, specimens preserved in formalin can result in distorted juveniles of nematodes after FECT concentration, complicating the identification of species like Strongyloides stercoralis [47].
Quantitative Comparison of Concentration Techniques
The choice of concentration method and preservative directly influences diagnostic sensitivity. The following tables summarize comparative performance data from recent studies.
Table 2: Comparative Detection Rates of Concentration Methods in Clinical Studies
| Study Population | Method 1 (Detection Rate) | Method 2 (Detection Rate) | Key Findings |
|---|---|---|---|
| 110 children with diarrhea [3] | Formalin-Ethyl Acetate (FAC): 75% | Formalin-Ether (FEC): 62% | FAC demonstrated a higher recovery rate for parasites, including in dual infections. |
| 110 children with diarrhea [3] | Formalin-Ethyl Acetate (FAC): 75% | Direct Wet Mount: 41% | Concentration methods significantly outperform direct smear microscopy. |
| 258 clinical specimens [47] | CONSED Sedimentation: Pathogens found in 15 additional specimens | Formalin-Ethyl Acetate: Pathogen found in 1 additional specimen | The CONSED method missed one pathogen, while the FECT method missed 15. |
| 32 positive specimens [27] | Mini Parasep SF: Parasite yield equal to FECT | Formalin-Ethyl Acetate (FECT): Parasite yield equal to Parasep | Parasep provided equal yield with less debris and better preservation of morphology. |
Table 3: Impact of Technique on Specific Parasite Recovery
| Parasite | Formalin-Ethyl Acetate | CONSED Method | Mini Parasep SF |
|---|---|---|---|
| Entamoeba histolytica | 0 detections [47] | 6 detections [47] | Not Specified |
| Giardia lamblia | 0 detections [47] | 3 detections [47] | Not Specified |
| Trichuris trichiura | 0 detections [47] | 4 detections [47] | Not Specified |
| Coccidian Oocysts | Poor acid-fast staining ("ghosts") [27] | Not Specified | Better morphology & staining [27] |
| Strongyloides stercoralis | Low sensitivity (<50 lpg) [33] [45] | Not Specified | Not Specified |
Detailed Experimental Protocols
Protocol: CDC Formalin-Ethyl Acetate Sedimentation Concentration
This standardized protocol is used to concentrate parasitic structures for microscopic detection [8].
Materials:
- 10% formalin
- Ethyl acetate
- 0.85% saline or distilled water
- Gauze (cheesecloth-type) and funnel
- 15 ml conical centrifuge tubes
- Centrifuge
- Wooden applicator sticks
Methodology:
- Emulsification: Mix the stool specimen thoroughly. Strain approximately 5 ml of the fecal suspension through wetted gauze into a 15 ml conical centrifuge tube.
- Dilution: Add 0.85% saline or 10% formalin through the debris on the gauze to bring the total volume in the tube to 15 ml. Note: Using distilled water may deform Blastocystis hominis [8].
- Primary Centrifugation: Centrifuge at 500 × g for 10 minutes. Decant the supernatant.
- Formalin-Ethyl Acetate Mixing: Resuspend the sediment in 10 ml of 10% formalin. Add 4 ml of ethyl acetate, stopper the tube, and shake vigorously for 30 seconds. Carefully remove the stopper.
- Secondary Centrifugation: Centrifuge at 500 × g for 10 minutes. Four layers will form: an ethyl acetate plug, a plug of debris, a formalin supernatant, and a sediment containing parasites.
- Sediment Harvest: Free the debris plug by ringing the tube sides with an applicator stick. Decant the top three layers. Use a cotton-tipped applicator to wipe debris from the tube sides.
- Preparation for Microscopy: Resuspend the final sediment in a few drops of 10% formalin. The concentrate is now ready for wet mount examination, immunoassay, or special staining.
Protocol: Mini Parasep SF Solvent-Free Concentration
This commercial protocol offers a closed-system alternative that eliminates the use of ether or ethyl acetate [49] [27].
Materials:
- Mini Parasep SF faecal parasite concentrator kit (includes tube with integrated filter and alcohol-based fixative)
Methodology:
- Loading: Transfer two-level scoops (approx. 5 ml) of stool into the mixing chamber containing the Alcorfix fixative.
- Assembly and Mixing: Assemble the sedimentation cone with the integrated vertical filtration device onto the mixing chamber. Vortex the entire unit for 10-15 seconds.
- Filtration and Centrifugation: Invert the unit to filter the contents through the filter thimble (pore size 425μm). Centrifuge at 400-1200 × g for 1-3 minutes [49] [27].
- Discard and Recover: Unscrew and discard the mixing chamber and filter thimble together. The sediment containing the parasites remains in the conical tube.
- Preparation for Microscopy: The sediment can be directly resuspended and used for wet mounts, permanent stains (trichrome, modified acid-fast), or other downstream analyses [27].
Workflow for Assessing Preservation Impacts
The following diagram maps the logical pathway for evaluating preservation artifacts and selecting the appropriate diagnostic technique.
The evidence indicates that preservation artifacts pose a significant, yet manageable, challenge to the accurate identification of intestinal parasites. The traditional FECT, while robust for helminth eggs and protozoan cysts, has documented limitations including trophozoite destruction, staining inconsistencies for coccidia, and morphological distortion. To mitigate these artifacts in research and diagnostic practice, the following is recommended:
- For Broad Routine Use: The FECT remains a reliable and recommended sedimentation technique [8]. However, researchers must be aware of its inherent limitations, particularly when targeting fragile trophozoites or coccidian parasites.
- For Maximizing Sensitivity and Morphology: Emerging solvent-free, closed-system concentrators like the Mini Parasep SF offer a compelling alternative, providing comparable or superior parasite yield with less debris, better morphological preservation, and a significant reduction in processing time and chemical exposure [27].
- For Specific Parasitic Targets: The diagnostic test must be matched to the suspected parasite. For Strongyloides stercoralis, the quantitative FECT is insufficient for low-intensity infections (<50 larvae per gram) and should be supplemented with more sensitive methods like agar plate culture for epidemiological studies [33] [45]. For coccidia, modified acid-fast staining is essential, and its performance can be affected by the prior concentration method [27] [19].
In conclusion, a critical understanding of preservation artifacts and the availability of improved technical protocols empower scientists to make informed choices that enhance diagnostic accuracy, ultimately supporting better patient outcomes and more reliable research data.
The formalin-ethyl acetate concentration technique (FECT) serves as a fundamental diagnostic procedure in parasitology laboratories for detecting intestinal parasites in stool specimens. While effective for many helminths and protozoa, standard FECT protocols require specific adaptations to optimize recovery of particular pathogens such as Cryptosporidium spp. and Blastocystis hominis. This application note details evidence-based modifications to the FECT protocol to enhance detection efficiency for these pathogens, supported by comparative performance data and step-by-step methodologies suitable for research and diagnostic applications.
Pathogen-Specific FECT Adaptations and Performance
Comparative Performance of Diagnostic Methods
Table 1: Comparison of detection methods for Cryptosporidium and Blastocystis
| Pathogen | Method | Sensitivity | Specificity | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Cryptosporidium | Modified Acid-Fast Microscopy | Variable; lower than molecular methods [50] | High [51] | Inexpensive; allows morphological assessment [51] | Labor-intensive; requires trained personnel; low sensitivity [50] |
| Immunofluorescence Microscopy | Higher than acid-fast staining [50] | High [51] | High sensitivity and specificity [51] | Requires fluorescent microscope; more expensive [50] | |
| Antigen Detection (ELISA) | 80-85% (stool); 95% (serum) [52] | 92.72% [52] | High throughput; less training needed [52] | Variable performance between tests [50] | |
| Molecular Methods (PCR) | 100% (laboratory-developed test) [50] | High [50] | Highest sensitivity; species identification [51] [50] | Higher cost; requires specialized equipment [50] | |
| Blastocystis hominis | Direct Microscopy | 36.2% [53] | 99.4% [53] | Rapid; low cost [53] | Low sensitivity; requires experienced technician [53] |
| Culture (Jones' Medium) | 67.6% [53] | 100% [53] | Improves detection vs. microscopy [53] [54] | Requires 2-3 days incubation [53] | |
| PCR | Gold Standard [53] | Gold Standard [53] | Highest sensitivity and specificity; enables subtyping [53] | Highest cost; requires molecular lab [53] |
FECT Modifications for Enhanced Recovery
2.2.1 Cryptosporidium Adaptations
A Modified FECT (M-FECT) protocol significantly improves oocyst recovery through centrifugation adjustments. Standard FECT typically centrifuges at 500 × g for 10 minutes [13], but increasing relative centrifugal force improves sedimentation of small, buoyant Cryptosporidium oocysts (4.2-5.4 µm) [51]. The M-FECT protocol enhances recovery by increasing centrifugation speed or time (500 × g, 10 minutes) to improve oocyst sedimentation [51]. Additionally, a modified formalin-ether concentration technique has been developed specifically for Cryptosporidium that provides enhanced detection in field-collected samples [55].
For laboratories processing specimens for multiple pathogens, a standardized FECT protocol can be employed: homogenize ~500 mg stool in 10 mL water, filter through a strainer, centrifuge (500 × g, 5 minutes), resuspend sediment in 10 mL 10% formalin, add 4 mL ethyl-acetate, shake vigorously for 30 seconds, centrifuge (500 × g, 5 minutes), discard debris plug and supernatant, and examine sediment [13].
2.2.2 Blastocystis hominis Adaptations
For Blastocystis detection, FECT serves as a preliminary concentration step rather than a standalone diagnostic method. The formalin-ether concentration technique (FECT) is used to obtain stool concentrate, which can then be further processed using Ficoll-Paque density gradient centrifugation to isolate Blastocystis cysts [56]. This approach enhances microscopic detection and provides cleaner samples for subsequent culture or molecular analysis.
When processing samples, FECT demonstrates superior capability for detecting Blastocystis cysts compared to direct smear microscopy. This concentration step is particularly valuable given the phenomenon of irregular shedding of Blastocystis in feces, which can lead to false-negative results in single stool examinations [56].
Detailed Experimental Protocols
Modified FECT for Cryptosporidium Detection
Reagents and Materials:
- 10% buffered formalin
- Ethyl-acetate
- Phosphate-buffered saline (PBS)
- Centrifuge tubes with conical bottoms
- Gauze or strainer (0.6 mm × 0.6 mm sieve opening)
- Centrifuge capable of 500 × g
- Optical microscope
Procedure:
- Specimen Preparation: Homogenize 500 mg to 2 g of stool specimen in 10 mL of 10% formalin. For liquid stools, use 1-2 mL directly [50].
- Filtration: Filter the suspension through two layers of wet gauze or a molded strainer into a conical centrifuge tube to remove large debris.
- Centrifugation: Centrifuge at 500 × g for 10 minutes. Decant supernatant completely [51].
- Resuspension: Resuspend the sediment in 10 mL of 10% formalin.
- Solvent Addition: Add 4 mL of ethyl-acetate. Close the tube tightly and shake vigorously for 30 seconds [13].
- Second Centrifugation: Centrifuge at 500 × g for 10 minutes. Four layers will form: ethyl-acetate plug at top, debris layer, formalin layer, and sediment at bottom [51].
- Sediment Recovery: Free the debris plug from tube sides and carefully decant the top three layers. Use a swab to wipe remaining debris from tube walls.
- Microscopic Examination: Resuspend the final sediment in a small amount of saline (100-200 µL). Prepare wet mounts for examination. For Cryptosporidium, use differential interference contrast microscopy or stain with modified acid-fast for oocyst identification [51].
FECT with Culture for Blastocystis Detection
Reagents and Materials:
- Jones' medium with 10% horse serum [53] [56]
- 10% formalin
- Ethyl-acetate
- Ficoll-Paque density gradient medium
- Incubator at 37°C
Procedure:
- Concentration: Perform standard FECT as described in section 3.1, steps 1-7.
- Density Gradient (Optional): For enhanced cyst recovery, resuspend FECT sediment in PBS and layer onto 5 mL Ficoll-Paque. Centrifuge at 1,600 × g for 20 minutes. Recover the cyst layer at the interface [56].
- Inoculation: Inoculate approximately 50-100 mg of concentrated sediment or gradient-purified cysts into Jones' medium supplemented with 10% horse serum.
- Incubation: Incubate at 37°C for 24-72 hours. Anaerobic conditions are not required but may enhance growth [54].
- Examination: Examine cultures at 24, 48, and 72 hours by preparing wet mounts from the culture medium. Identify characteristic vacuolar, granular, or cystic forms using light microscopy. Staining with lactophenol cotton blue or trichrome can enhance morphological differentiation [53].
Quality Control: Include known positive and negative controls with each batch. Monitor culture media for contamination. Subculture every 3-4 days to maintain viable isolates.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential reagents and materials for pathogen-specific FECT
| Reagent/Material | Function | Pathogen Application | Technical Notes |
|---|---|---|---|
| 10% Buffered Formalin | Fixation and preservation of parasite morphology | Both | Maintains structural integrity; not recommended for molecular downstream applications [51] |
| Ethyl-Acetate | Solvent for extraction of fats and debris | Both | Less flammable and hazardous than ether [13] |
| Jones' Medium | Culture medium for in vitro propagation | Blastocystis | Supplement with 10% horse serum; supports growth of vacuolar forms [53] [56] |
| Ficoll-Paque | Density gradient medium for cyst purification | Blastocystis | Enhances cyst recovery from complex stool matrix [56] |
| Modified Acid-Fast Stain | Differential staining of oocysts | Cryptosporidium | Stains oocysts bright red against blue-green background [51] |
| Immunofluorescent Antibodies | Specific detection of surface antigens | Cryptosporidium | Higher sensitivity than acid-fast staining; requires fluorescence microscope [51] [50] |
| Cryptosporidium/Giardia DFA Kit | Direct fluorescent antibody staining | Cryptosporidium | Commercial kit for simultaneous detection; apple-green fluorescence [50] |
| Nuclisens EasyMAG System | Automated nucleic acid extraction | Both | Effective for DNA recovery from stool specimens [50] [57] |
| 18S rDNA PCR Primers | Molecular detection and subtyping | Both | Barcoding region enables subtype identification [53] |
The adaptation of FECT for specific pathogen detection represents a critical advancement in parasitological diagnostics. For Cryptosporidium, protocol modifications focusing on enhanced oocyst recovery through adjusted centrifugation parameters significantly improve detection sensitivity. For Blastocystis hominis, FECT serves as an effective preliminary concentration method that significantly enhances the sensitivity of subsequent culture and molecular techniques.
These optimized protocols provide researchers and clinical laboratory professionals with standardized methodologies that improve diagnostic accuracy while acknowledging the complementary value of traditional and modern detection platforms. The integration of these adapted concentration methods with downstream applications including culture, immunoassays, and molecular diagnostics creates a robust framework for comprehensive parasite detection in both research and clinical settings.
Diagnostic Validation: FECT Performance Against Alternative Methods
Within the ongoing research on the formalin-ethyl acetate concentration technique (FECT) for stool specimens, a critical challenge persists: the accurate diagnosis of intestinal parasitic infections in low-intensity and resource-limited settings. Although intestinal helminths remain among the most prevalent neglected tropical diseases, affecting approximately 1.5 billion people globally, their diagnosis is frequently compromised by the methodological limitations of commonly employed techniques [13]. The diagnostic dilemma is particularly acute in low-transmission settings resulting from successful control programs, where infection intensities have diminished, thereby reducing the sensitivity of conventional microscopy methods [58] [59]. This analysis systematically evaluates the operational characteristics of FECT against direct wet mount and Kato-Katz techniques, providing evidence-based protocols for researchers and drug development professionals seeking to optimize diagnostic accuracy in both clinical and research contexts.
Comparative Diagnostic Performance
The diagnostic sensitivity of copro-microscopic techniques exhibits substantial variation, largely dependent on the parasite species and infection intensity. Table 1 summarizes the comparative performance metrics of FECT, Kato-Katz, and direct wet mount based on aggregated study data.
Table 1: Comparative sensitivity and negative predictive value (NPV) of stool examination techniques
| Diagnostic Method | Overall Sensitivity (%) | Overall NPV (%) | A. lumbricoides Sensitivity (%) | Hookworm Sensitivity (%) | T. trichiura Sensitivity (%) | S. mansoni Sensitivity (%) |
|---|---|---|---|---|---|---|
| FECT | 78.3 | 63.2 | 81.4 | 57.8 | 58.4 | |
| Kato-Katz | 81.0 | 66.2 | 93.1 | 69.0 | 90.6 | 96.1 |
| Direct Wet Mount | 52.7 | 44.0 | 52.0 | 12.5 | 22.1 |
A study conducted in Northwest Ethiopia with 354 fecal specimens demonstrated that Kato-Katz had the highest overall sensitivity (81.0%) and negative predictive value (66.2%), followed by FECT (78.3% sensitivity, 63.2% NPV), while direct wet mount performed substantially worse (52.7% sensitivity, 44.0% NPV) [60]. The detection rates for intestinal parasites using single techniques were 59.0% for Kato-Katz, 57.1% for FECT, and only 38.4% for wet mount [60]. When all three techniques were combined, the detection rate increased to 72.9%, highlighting the limitations of relying on any single method and the necessity of method combination for accurate prevalence estimates [60].
Species-Specific Performance Variations
The diagnostic performance of each technique varies considerably across parasite species, necessitating method selection based on the target pathogen:
- For Ascaris lumbricoides, Kato-Katz demonstrates excellent sensitivity (93.1%), followed by FECT (81.4%), with wet mount performing poorly (52.0%) [60].
- For Trichuris trichiura, Kato-Katz maintains high sensitivity (90.6%), while FECT shows moderate sensitivity (57.8%), and wet mount is markedly insensitive (12.5%) [60].
- For Schistosoma mansoni, Kato-Katz exhibits outstanding sensitivity (96.1%), substantially outperforming FECT (58.4%) and wet mount (22.1%) [60].
- For hookworm species, the agar plate culture (APC) method demonstrates superior sensitivity (86.4%) compared to Kato-Katz (69.0%) [60] [61].
A study in China focusing on low-intensity Schistosoma japonicum infections found that the formalin-ethyl acetate sedimentation technique had a disappointingly low sensitivity of only 28.6%, indicating its limited utility for this specific application [58].
Impact of Infection Intensity on Diagnostic Performance
The sensitivity of diagnostic methods is strongly influenced by infection intensity, as quantified by eggs per gram (EPG) of stool. A Bayesian latent class meta-analysis revealed that the widely used double-slide Kato-Katz method had a sensitivity of 74-95% for soil-transmitted helminths at high infection intensities, but sensitivity dropped substantially to 53-80% in low-intensity settings, with the lowest sensitivity for hookworm and A. lumbricoides [59]. This intensity-dependent performance decline underscores the critical need for more sensitive techniques in post-control settings where infection intensities have diminished.
Table 2: Comparative method performance in different transmission settings
| Diagnostic Method | Overall Sensitivity | High Intensity Settings | Low Intensity Settings | Remarks |
|---|---|---|---|---|
| FLOTAC | 92.7% | Highest | Highest | Superior performance overall |
| Kato-Katz | 74-95% | 53-80% | Sensitivity drops significantly in low intensity | |
| FECT | 78.3% | Better than wet mount | ||
| Mini-FLOTAC | Comparable to Kato-Katz | Comparable to Kato-Katz | Comparable to Kato-Katz | |
| Direct Wet Mount | 42.8% | Lowest sensitivity |
Experimental Protocols
Formalin-Ethyl Acetate Concentration Technique (FECT)
Sample Preparation
- Add approximately 500 mg of fresh stool to 10 ml of clean water and mix thoroughly [13].
- Vigorously shake the suspension and filter through a molded strainer (0.6 mm × 0.6 mm sieve opening) to remove large debris while allowing parasite eggs to pass through [13].
- Centrifuge the filtered suspension at 500 × g for 5 minutes, then discard the supernatant [13].
Ethyl-Acetate Concentration
- Resuspend the sediment with 10 ml of 10% formalin solution [13] [8].
- Add 4 ml of ethyl-acetate to the formalin suspension [8].
- Vigorously shake the mixture for 30 seconds to ensure proper emulsion [8].
- Centrifuge at 500 × g for 5 minutes in a conical centrifuge tube, which results in four distinct layers: an ethyl-acetate layer at the top, a debris plug, a formalin layer, and the sediment containing concentrated parasites at the bottom [13] [8].
Sediment Examination
- Free the debris plug from the tube walls using an applicator stick and decant the top three layers (ethyl-acetate, debris plug, and formalin) [8].
- Use a cotton-tipped applicator to remove remaining debris from the tube sides [8].
- Resuspend the final sediment with 0.85% saline solution or 10% formalin [13].
- Prepare wet mounts (1-2 drops) from the concentrated sediment and examine systematically under microscopy [13].
Kato-Katz Thick Smear Technique
Sample Preparation
- Press fresh stool through a mesh screen (approximately 40-60 mesh) to remove large particulate matter [60] [61].
- Place a template with a 6-8 mm diameter hole (holding approximately 41.7-50 mg of stool) on a clean microscope slide [60] [61].
- Fill the template hole completely with sieved stool and level the surface [60].
Cellophane Preparation and Examination
- Cover the stool sample with a piece of cellophane (previously soaked in glycerol-malachite green or glycerol solution) [60] [61].
- Invert the slide and press firmly against absorbent paper to spread the specimen and remove excess fluid [60].
- For hookworm detection, examine slides within 30-60 minutes of preparation to prevent over-clearing of eggs [61].
- For other helminths, examine slides after 1 hour up to 24 hours, allowing adequate clearing for visualization [61].
Direct Wet Mount Technique
Fresh Specimen Examination
- Emulsify approximately 20 mg of fresh stool in a drop of 0.85% saline solution on a microscope slide [60].
- Apply a coverslip (22 × 22 mm) and examine immediately under microscopy [62].
- For optimal detection of motile trophozoites, examine liquid specimens within 30 minutes of passage and soft specimens within one hour [8].
- Formed specimens can be examined within 24 hours if refrigerated overnight [8].
Microscopy
- Systematically scan the entire coverslip area at 100× magnification, followed by 400× for morphological details [62].
- For low-intensity infections, examine multiple wet mounts from different parts of the specimen to increase detection probability [60].
Workflow and Diagnostic Pathways
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential research reagents and materials for stool parasitology diagnostics
| Item | Specification/Function | Application Notes |
|---|---|---|
| Ethyl-acetate | Solvent for lipid extraction and debris clearance in FECT | Less flammable alternative to ether; improves sample clarity [13] [8] |
| 10% Buffered Formalin | Preservative and fixative for parasite morphology | Maintains structural integrity of eggs and cysts during processing [8] |
| Cellophane Coverslips | Glycerol-impregnated for Kato-Katz clearancing | Allows optical clearancing of stool matrix for egg visualization [60] |
| Plastic Template | Standardized sample volume (41.7-50 mg) for Kato-Katz | Ensures consistent sample thickness and quantitative accuracy [60] [61] |
| Molded Strainers | Fecal debris filtration (0.6 mm sieve opening) | Removes large particulate matter while preserving parasites [13] |
| Agar Plates | Culture medium for larval development and detection | Essential for hookworm species identification and increased sensitivity [61] |
| Conical Centrifuge Tubes | 15 ml capacity for sedimentation procedures | Facilitates phase separation in concentration techniques [8] |
Discussion and Research Implications
Method Selection Considerations
The comparative sensitivity analysis reveals that method selection must be guided by specific research objectives, target parasites, and available resources. For soil-transmitted helminth mapping and drug efficacy trials where quantitative data is essential, the Kato-Katz technique remains the recommended method despite its limitations in low-intensity settings [59] [61]. For comprehensive parasite detection, particularly in clinical settings where multiple parasite types may be present, FECT provides superior performance compared to direct wet mount, though at the cost of increased processing time and resource requirements [13].
The strikingly low sensitivity of direct wet mount (42.8-52.7%) across multiple studies raises serious concerns about its continued use as a standalone diagnostic method in both clinical and research contexts [60] [59]. The employment of concentration techniques like FECT or spontaneous tube sedimentation for routine laboratory diagnosis would significantly improve accurate detection of parasitic infections, thereby enhancing patient care and strengthening control programs [61].
Future Directions in Diagnostic Development
Recent advancements in molecular diagnostics and proteomic approaches offer promising alternatives to conventional microscopy-based methods. In colorectal cancer screening, fecal immunochemical tests (FIT) have demonstrated superior diagnostic accuracy compared to other fecal protein biomarkers, with significantly better performance for detecting advanced neoplasms [63]. Similar technological innovations are urgently needed in parasitology diagnostics, particularly for low-intensity infections where current microscopy methods show inadequate sensitivity.
The integration of multiple diagnostic approaches, leveraging the complementary strengths of different techniques, represents the most promising pathway forward. For instance, combining FECT's broad detection capabilities with Kato-Katz's quantitative accuracy and APC's high sensitivity for hookworm creates a robust diagnostic algorithm that maximizes detection probability across the spectrum of intestinal helminths [61]. This multifaceted approach is particularly crucial in the current era of integrated neglected tropical disease control programs, where accurate surveillance data informs targeted interventions and monitors their success.
The Formalin-Ethyl Acetate Concentration Technique (FECT) establishes itself as a superior diagnostic method for detecting soil-transmitted helminths (STHs), particularly hookworm and Trichuris trichiura. This application note synthesizes recent comparative studies evaluating FECT against other common copromicroscopic techniques. Data confirms FECT's enhanced sensitivity and reliability in both field surveys and clinical trials, providing researchers and drug development professionals with robust evidence for its application in STH diagnosis and efficacy monitoring.
Soil-transmitted helminths (STHs), including hookworm and Trichuris trichiura, continue to pose a significant global health burden, predominantly affecting tropical and subtropical regions with inadequate sanitation [64] [65]. Accurate diagnosis is the cornerstone of effective control programs, drug efficacy trials, and epidemiological surveys. While numerous diagnostic techniques exist, the Formalin-Ethyl Acetate Concentration Technique (FECT) has emerged as a reference standard due to its ability to be performed on preserved samples and its comparative diagnostic accuracy. This note consolidates recent evidence on FECT's performance, provides a detailed protocol for its implementation, and outlines essential tools for the researching scientist.
Comparative Diagnostic Performance
Recent studies have systematically compared FECT with other common techniques, such as direct wet mount (DWM), Kato-Katz (KK), McMaster methods, and crude formalin concentration (FC). The tables below summarize key performance metrics for detecting hookworm and T. trichiura.
Table 1: Comparative Sensitivity of Diagnostic Techniques for Hookworm Detection
| Diagnostic Technique | Sensitivity (%) | Specificity (%) | Test Efficiency (%) | Agreement with CRS (Kappa, κ) | Citation |
|---|---|---|---|---|---|
| Spontaneous Tube Sedimentation (STS) | 86.5 | - | 95.3 | 0.893 (Perfect) | [66] |
| Richie's Technique | 77.3 | - | 92.1 | 0.816 (Perfect) | [66] |
| Formalin-Ethyl Acetate (FECT) | 72.7* | - | - | - | [64] |
| Kato-Katz (KK) | 63.8 | - | 87.4 | 0.696 (Substantial) | [66] |
| McMaster2 Method | 70.6 | - | - | - | [64] |
| Direct Wet Mount (DWM) | 43.2 | - | 80.2 | 0.498 (Moderate) | [66] |
Note: Sensitivity value for FECT is from a separate study population and is included for context. CRS: Composite Reference Standard.
Table 2: Comparative Sensitivity of Diagnostic Techniques for Trichuris trichiura Detection
| Diagnostic Technique | Sensitivity (%) | Comparative Findings | Citation |
|---|---|---|---|
| McMaster Method | 90.1 | Most sensitive | [64] |
| McMaster2 Method | 89.3 | Highly sensitive | [64] |
| Formalin-Ethyl Acetate (FECT) | Superior | Significantly better detection vs. Crude FC | [13] |
| Crude Formalin Concentration (FC) | Inferior | Significantly poorer detection vs. FECT | [13] |
| Kato-Katz (KK) | Lower (Post-Tx) | Sensitivity decreases in low-intensity infections | [65] |
Detailed FECT Protocol for Soil-Transmitted Helminths
Principle
The FECT is a sedimentation method that leverages the differences in specific gravity between parasitic elements and fecal debris. Ethyl acetate acts as a solvent, extracting fats, oils, and debris into an upper layer, which is subsequently discarded, leaving a cleaned sediment concentrated with helminth eggs, larvae, and protozoan cysts for microscopic examination [13].
Reagents and Equipment
- 10% Formalin Solution
- Ethyl Acetate
- Saline Solution (0.85%)
- Conical Centrifuge Tubes (15 mL)
- Fecal Strainers or Sieves (450–500 µm pore size)
- Centrifuge
- Microscope Slides and Coverslips
- Wooden applicator sticks or disposable loops
Step-by-Step Procedure
- Specimen Preparation: Emulsify approximately 0.5 - 3 g of fresh or formalin-preserved stool in 10 mL of clean water or 10% formalin within a centrifuge tube. Ensure the sample is thoroughly homogenized [64] [13].
- Filtration: Vigorously shake the suspension and pour it through a molded strainer or sieve (e.g., 450–500 µm) into a clean conical centrifuge tube. This step removes large particulate debris [13].
- First Centrifugation: Centrifuge the filtered suspension at 500 g for 5 minutes. Carefully decant and discard the supernatant [13].
- Formalin-Ethyl Acetate Addition: Re-suspend the sediment in 10 mL of 10% formalin. Add 4 mL of ethyl acetate to the tube. Securely cap the tube and shake it vigorously for at least 30 seconds to ensure thorough mixing [27] [13].
- Second Centrifugation: Centrifuge the mixture at 500 g for 5 minutes. This will result in four distinct layers:
- Layer 1 (Top): A plug of ethyl acetate and debris.
- Layer 2: A layer of formalin.
- Layer 3: A sediment of fecal material.
- Layer 4 (Bottom Pellet): The concentrated parasitic elements.
- Supernatant Removal: Free the debris plug from the tube's sides with an applicator stick. Carefully decant the top three layers (ethyl acetate, debris, and formalin) without disturbing the sediment pellet [13].
- Final Preparation: Use a cotton-tipped applicator to wipe any remaining debris from the inner walls of the tube. Re-suspend the final sediment pellet in a few drops of saline (0.85%) or formalin. The volume of the resuspension fluid can be adjusted based on the density of the sediment [27] [13].
- Microscopy: Transfer one or two drops of the re-suspended sediment onto a microscope slide, add a coverslip, and systematically examine the entire area under the coverslip using 10x and 40x objectives. The intensity of infection can be semi-quantified by counting the number of eggs per slide [13].
Quality Control and Notes
- Always process positive control samples periodically if available.
- Examiners reading slides should be blinded to other diagnostic results when performing comparative studies [13].
- The morphology of helminth eggs is generally well-preserved, and background debris is significantly reduced compared to crude formalin methods [27] [13].
Workflow and Logical Diagram
The following diagram illustrates the logical decision-making process for selecting and implementing FECT in a research or diagnostic context, based on study objectives and practical constraints.
FECT Selection Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for FECT
| Item | Function/Application | Key Considerations |
|---|---|---|
| 10% Formalin | Fixative and preservative; stabilizes parasitic morphology for delayed processing. | Enables storage and batch testing; essential for large-scale surveys. [64] [13] |
| Ethyl Acetate | Solvent for lipid removal and debris extraction; cleans the sediment. | Less flammable and hazardous than ether; improves slide clarity. [27] [13] |
| Fecal Strainers (450-500 µm) | Filters coarse debris; allows passage of helminth eggs and cysts. | Standardizes sample preparation; improves concentration efficiency. [13] |
| Conical Centrifuge Tubes | Facilitates sedimentation and separation of layers during centrifugation. | Conical shape is critical for forming a compact parasite pellet. [27] |
| QIAamp PowerFecal Pro DNA Kit | High-quality DNA extraction from stool for downstream PCR. | Superior for breaking helminth eggshells; highest PCR detection rate. [67] |
The consolidated data from recent studies unequivocally supports the superiority of FECT for detecting hookworm and T. trichiura infections. Its enhanced sensitivity over techniques like direct wet mount and crude formalin concentration, coupled with its logistical flexibility for use with fixed samples, makes it an indispensable tool for both field epidemiology and clinical trial settings [66] [13]. While the Kato-Katz technique remains valuable for fresh sample analysis and intensity quantification, and molecular methods like qPCR offer superior sensitivity in low-intensity post-treatment scenarios, FECT provides an optimal balance of sensitivity, practicality, and cost-effectiveness [64] [65]. The standardized protocol and toolkit outlined herein provide a robust framework for researchers and drug development professionals to implement this reliable diagnostic technique, thereby strengthening the accuracy of helminth monitoring and efficacy evaluation programs globally.
Evaluation of Commercial Kits (e.g., Mini Parasep SF) Against Standard FECT
The formalin-ethyl acetate concentration technique (FECT) has long been a cornerstone of parasitological diagnosis, providing a reliable method for detecting intestinal parasites in stool specimens. However, the procedure is labor-intensive, requires multiple steps, and involves handling hazardous chemicals. The development of commercial kits, such as the Mini Parasep SF stool concentrator kit, aims to streamline this process while maintaining diagnostic accuracy. This application note provides a comprehensive evaluation of the Mini Parasep SF kit against the standard FECT, synthesizing current research findings, presenting structured comparative data, and detailing standardized protocols for researchers and laboratory professionals. Evidence from multiple studies indicates that while FECT may hold a slight sensitivity advantage for specific parasites like Opisthorchis viverrini in low-intensity infections, the Mini Parasep SF kit demonstrates comparable performance for most helminthiases while offering significant workflow advantages [68] [69] [70].
Comparative Performance Analysis
Diagnostic Sensitivity and Parasite Detection
Evaluation of diagnostic performance across multiple studies reveals context-dependent outcomes for the Mini Parasep SF kit compared to FECT. The table below summarizes key sensitivity and detection rate comparisons:
Table 1: Comparative Diagnostic Performance of FECT and Mini Parasep SF
| Parasite | FECT Sensitivity/Detection | Mini Parasep SF Sensitivity/Detection | Research Context |
|---|---|---|---|
| Opisthorchis viverrini | 75.5% sensitivity [68]91.0% sensitivity [70] | 67.3% sensitivity [68]41.8% sensitivity [70] | Northeast Thailand (n=150) [68]Low-intensity infections [70] |
| Hookworm | Superior detection [13] | Lower detection rate [13] | Thailand-Myanmar border (n=693) [13] |
| Trichuris trichiura | Superior detection [13] | Lower detection rate [13] | Thailand-Myanmar border (n=693) [13] |
| Minute Intestinal Flukes (MIF) | 30.7% detection rate [69] | 27.3% detection rate [69] | Northeast Thailand subset (n=150) [69] |
| Strongyloides stercoralis | Better detection with FECT/stool kit vs. KK [68] | Better detection with FECT/stool kit vs. KK [68] | Northeast Thailand [68] |
| Co-infections | Performs better than KK [68] | Performs better than KK [68] | Northeast Thailand [68] |
For quantitative measurements of infection intensity (fecal egg counts), results from the Mini Parasep SF kit show a significant positive correlation with both FECT and Kato-Katz methods, indicating its reliability for both qualitative detection and quantitative assessment of parasite burden [68] [69].
Operational and Workflow Considerations
Beyond diagnostic accuracy, practical implementation factors significantly influence method selection in both research and clinical settings.
Table 2: Workflow and Practical Considerations
| Parameter | Formalin-Ethyl Acetate Concentration Technique (FECT) | Mini Parasep SF Stool Kit |
|---|---|---|
| Process Complexity | Multiple steps: straining, centrifugation, solvent addition [27] | Simplified, integrated system [27] |
| Handling Hazard | Exposure to formalin and ethyl acetate [27] | Closed system; formalin-free fixative (Alcorfix) [27] |
| Sample Input | Typically 2g [69] or 500mg [13] | Typically 0.5g [69] or two-level scoops [27] |
| Processing Time | 10-15 minutes per sample [27] | Approximately 4 minutes per sample [27] |
| Centrifugation Time | 5 minutes [69] | 2 minutes [69] [27] |
| Cost Factor | Lower reagent cost | Higher per-test cost; potential savings in labor and time |
The enclosed design of the Mini Parasep SF system enhances laboratory safety by minimizing exposure to hazardous chemicals and infectious materials [27]. The integrated filtration system reduces background debris, resulting in cleaner specimens that facilitate microscopic examination and morphological identification [27].
Experimental Protocols
Standard FECT Protocol
Principle: FECT concentrates parasitic elements through a combination of formalin fixation, ethyl-acetate solvent extraction, and differential centrifugation [69] [13].
Materials:
- 10% formalin solution
- Ethyl-acetate
- Saline (0.85%)
- Conical centrifuge tubes (15ml)
- Gauze or strainer (450-500μm)
- Centrifuge
- Microscope slides and coverslips
- Lugol's iodine solution
Procedure:
- Homogenization and Fixation: Homogenize 2g of fresh stool in 7ml of 10% formalin solution in a centrifuge tube [69].
- Straining: Pour the mixture through two layers of gauze or a specialized strainer into a new 15ml conical centrifuge tube to remove large particulate matter [69] [13].
- Solvent Addition: Add 3ml of ethyl-acetate to the filtered suspension [69]. Securely cap the tube and shake vigorously for 30-60 seconds to emulsify the contents and extract fats [69] [13].
- Centrifugation: Centrifuge at 500g for 5 minutes [69]. This results in four distinct layers: a plug of debris at the top, the ethyl-acetate layer, a formalin layer, and the sediment containing parasites at the bottom.
- Supernatant Removal: Free the debris plug from the tube sides and carefully decant the top three layers (debris, ethyl-acetate, and formalin) without disturbing the sediment [13].
- Sediment Preparation: Resuspend the remaining sediment in a small volume of 10% formalin or saline [69]. Transfer a drop to a microscope slide, add a drop of Lugol's iodine if needed, and examine under a microscope at 100x and 400x magnifications [69].
Mini Parasep SF Stool Kit Protocol
Principle: This integrated system combines fixation, filtration, and concentration into a single device, utilizing an alcohol-based fixative and a vertical filtration matrix to concentrate parasitic elements [69] [27].
Materials:
- Mini Parasep SF stool concentrator kit (includes tubes with integrated filters and Alcorfix fixative)
- Vortex mixer
- Centrifuge
- Microscope slides and coverslips
- Lugol's iodine solution
Procedure:
- Sample Introduction: Using the spoon attached to the kit, transfer approximately 0.5g of stool (or two-level scoops) into the mixing chamber containing the Alcorfix fixative solution [69] [27].
- Assembly and Mixing: Assemble the sedimentation cone with its integrated vertical filtration device onto the mixing chamber. Vortex the entire unit briefly for 10-15 seconds to thoroughly mix the sample with the fixative [27].
- Filtration and Concentration: Invert the assembled device to allow the contents to pass through the filter thimble, which removes large debris. Centrifuge the unit at 400-500g for 2 minutes [69] [27].
- Discard Filtration Components: Carefully unscrew and discard the mixing chamber and the used filter thimble [27].
- Sediment Examination: The concentrated sediment remains in the conical tip of the tube. Resuspend it gently and prepare microscopic slides with and without Lugol's iodine staining. Examine systematically under the microscope at appropriate magnifications [69].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Stool Concentration Techniques
| Item | Function/Application | Considerations for Use |
|---|---|---|
| Mini Parasep SF Stool Kit | Integrated concentration system for parasite detection | Simplifies workflow; reduces chemical exposure; suitable for field studies [69] [27] |
| 10% Formalin Solution | Fixative and preservative for parasitic elements | Hazardous chemical requiring appropriate safety measures [69] [13] |
| Ethyl-Acetate | Solvent for fat extraction and debris removal | Less flammable alternative to diethyl ether [13] |
| Alcorfix | Alcohol-based fixative in Mini Parasep kit | Formalin-free; integrated in device [27] |
| Lugol's Iodine Solution | Staining agent for enhanced visualization of cysts and eggs | Provides contrast for microscopic structures [69] |
| Malachite Green-Glycerol Solution | Cellophane preparation for Kato-Katz method | Used in comparative studies [69] |
| Triton X-100 | Detergent for emulsifying stool samples in kit protocol | Aids in sample processing [69] |
Discussion and Application Guidance
Research Applications and Limitations
The choice between FECT and commercial concentrator kits depends heavily on the specific research context. For studies where maximum sensitivity is paramount, particularly for detecting low-intensity Opisthorchis viverrini infections, FECT remains the preferred method [70]. Its superior performance in this specific scenario is well-documented, with one study reporting 91.0% sensitivity for FECT versus 41.8% for the Mini Parasep SF kit in low-intensity infections [70].
However, for general helminth surveillance and studies where multiple parasites are of interest, the Mini Parasep SF kit demonstrates comparable effectiveness to FECT while offering substantial practical advantages [68] [69]. The kit's performance is particularly notable for detecting co-infections and parasites like Strongyloides stercoralis [68]. Furthermore, the significant reduction in processing time (4 minutes for Mini Parasep versus 10-15 minutes for FECT) makes it highly suitable for high-throughput studies and field settings with limited laboratory infrastructure [27].
Method Selection Framework
Researchers should consider the following factors when selecting a stool concentration method:
- Primary Research Objective: If ultimate sensitivity for specific trematodes is critical, FECT is superior. For general parasite surveys or workflow efficiency, the kit approach is advantageous.
- Sample Throughput: High-volume laboratories may benefit from the faster processing time of commercial kits despite higher per-test costs.
- Safety Environment: Settings with limited ventilation or safety equipment favor the enclosed, formalin-free kit system.
- Operator Expertise: The simplified, standardized procedure of commercial kits reduces technical variability across operators with different experience levels.
- Budget Constraints: While FECT has lower reagent costs, total cost-of-operation analysis should include personnel time and safety measures.
Within the broader thesis of FECT research for stool specimens, commercial kits like the Mini Parasep SF represent a significant evolution in diagnostic methodology. They successfully address key limitations of conventional FECT regarding workflow efficiency, technical complexity, and laboratory safety while maintaining comparable diagnostic performance for most intestinal helminths. The minor reduction in sensitivity for specific parasites in low-intensity infections must be weighed against the substantial operational benefits in the context of the research objectives. Future developments in this field will likely focus on further simplifying diagnostic workflows while enhancing sensitivity through integrated molecular and digital imaging technologies.
Integrating FECT with Immunoassays and Molecular Diagnostics
The Formalin-Ethyl Acetate Concentration Technique (FECT) remains a cornerstone of parasitology diagnostics, particularly in resource-limited settings, due to its proven effectiveness in enriching parasitic elements from stool specimens [3] [2]. However, contemporary diagnostic and research laboratories increasingly rely on immunoassays and molecular techniques for their superior sensitivity and specificity [71] [2]. This creates a critical opportunity for methodological integration. This Application Note details protocols for leveraging FECT as a robust sample preparation step to enhance the performance of downstream immunoassays and molecular diagnostics, providing a standardized framework for researchers and drug development professionals.
Performance Comparison of Diagnostic Techniques
Table 1: Comparative Performance of Stool Examination Techniques
| Technique Category | Specific Method | Key Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|
| Conventional Microscopy | Direct Wet Mount | Detection Rate: 41% [3] | Rapid, low cost, minimal equipment | Low sensitivity, unsuitable for low-level infections |
| Formol-Ether Concentration (FEC) | Detection Rate: 62% [3] | Improved sensitivity over wet mount | - | |
| Formalin-Ethyl Acetate (FECT) | Detection Rate: 75% [3] | Higher recovery rate, safe, feasible in rural settings [3] | Subjective, requires expertise | |
| Advanced Microscopy | Merthiolate-Iodine-Formalin (MIF) | Effective fixation & staining [2] | Long shelf life, good for field surveys | Can distort trophozoite morphology [2] |
| Immunoassay | Label-based (e.g., ELISA) | High sensitivity and specificity [71] | Amenable to automation, quantitative | Requires specific antibody reagents, label interference [72] |
| Label-free Capacitive | Detects NS1 biomarker for dengue [72] | Reagentless, direct detection, POC potential | Emerging technology, requires specialized electrodes | |
| Multiplex Immunoassay (MagArray) | Wider dynamic range vs. ELISA [73] | Simultaneous multi-analyte detection, small sample volume (20 μL) | Platform-specific reagents and equipment | |
| Molecular Diagnostics | PCR-based (e.g., Cepheid Xpert) | High sensitivity & specificity [74] [2] | Automated "lab in a cartridge", rapid results | Higher cost, risk of contamination, requires DNA extraction [2] |
| Artificial Intelligence | DINOv2-large (AI Model) | Accuracy: 98.93%, Sensitivity: 78.00%, Specificity: 99.57% [2] | Automated detection, high throughput, reduces human error | Requires large, curated image datasets for training [2] |
Integrated Experimental Workflows
Core FECT Protocol for Sample Preparation
The following protocol, adapted from standardized procedures, ensures optimal sample preparation for subsequent analyses [7].
Materials:
- Specimen: 2 grams of fresh stool.
- Fixative: 10% Formalin.
- Solvent: Ethyl Accetate.
- Buffer: 0.85% Normal Saline Solution (NSS).
- Equipment: Centrifuge, gauze, sterile wide-mouth containers, conical centrifuge tubes.
Procedure:
- Fixation: Emulsify approximately 2 grams of fresh stool in 10 mL of 10% formalin in a centrifuge tube. Fix at room temperature for a minimum of 30 minutes.
- Filtration: After vigorous shaking, filter the suspension through two layers of gauze into a new 15 mL conical centrifuge tube to remove large debris.
- Sedimentation: Centrifuge the filtrate at 2,500 rpm for 5 minutes. Discard the supernatant.
- Wash: Re-suspend the sediment in 7 mL of 0.85% saline and mix thoroughly.
- Solvent Extraction: Add 3 mL of ethyl acetate to the tube. Cap tightly and mix vigorously for 30 seconds.
- Final Concentration: Centrifuge at 2,500 rpm for 5 minutes. Four distinct layers will form: a top layer of ethyl acetate, a plug of debris, a formalin layer, and a sediment pellet.
- Harvest: Carefully remove the top three layers by decanting or with a pipette. The final sediment contains the concentrated parasitic elements.
- Re-suspension: Re-suspend the final sediment in 1 mL of 10% formalin or a buffer compatible with your downstream application (e.g., PBS for immunoassays, lysis buffer for molecular work) [7].
Workflow for Integrating FECT with Downstream Applications
The concentrated sediment from the FECT protocol serves as a unified starting point for various advanced diagnostic techniques. The following diagram illustrates this integrated pathway.
Protocol A: FECT with Multiplex Immunoassay (MagArray Platform)
This protocol leverages the concentrated FECT sediment for highly sensitive, multiplexed protein detection [73].
Materials:
- Chip: MagArray plastic chip cartridge pre-coated with capture antibodies.
- Buffers: Reaction Buffer (1% BSA in PBS), Rinsing Buffer (0.1% BSA, 0.05% Tween-20 in PBS).
- Detection Reagents: Biotinylated detection antibodies, Magnetic Nanotags (MNT).
- Equipment: MagArray MR-110a reader, rocking shaker, vacuum aspiration system.
Procedure:
- Sample Application: Dilute the FECT-concentrated sediment 1:10 in Reaction Buffer. Add 100 µL to the chip well. Cover with tape and incubate on a rocking shaker (350 rpm) for 2 hours.
- Washing: Aspirate the sample and wash the chip three times with 100 µL of Rinsing Buffer.
- Detection: Add 100 µL of detection antibody solution (diluted in Reaction Buffer) to the well. Incubate for 1 hour at room temperature.
- Signal Development: Wash the chip three times as before. Immediately add 100 µL of MNT solution.
- Measurement: Insert the chip into the MagArray reader and start measurement. Data acquisition can be as short as 2 minutes post-MNT addition. The integrated software provides quantitative results [73].
Protocol B: FECT with Molecular Diagnostics (qPCR)
The FECT sediment is an ideal source for pathogen DNA, free from PCR inhibitors present in crude stool [74] [2].
Materials:
- DNA Extraction Kit: Silica-membrane or magnetic-bead based kit.
- PCR Reagents: Master mix, primers, probes.
- Equipment: Real-time PCR system or automated platform like GeneXpert.
Procedure:
- Nucleic Acid Extraction: Use the FECT-concentrated sediment as the input sample for DNA extraction, following the manufacturer's protocol for your chosen kit. The concentration step improves DNA yield by removing non-parasitic debris.
- Amplification & Detection:
- Manual qPCR: Set up reactions using the extracted DNA and run on a standard real-time PCR instrument.
- Automated System: For platforms like Cepheid's GeneXpert, the FECT sediment can be loaded directly into the "lab in a cartridge" for fully automated extraction, amplification, and detection [74].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for Integrated FECT Workflows
| Item | Function/Application | Specific Examples & Notes |
|---|---|---|
| Formalin (10%) | Fixative for FECT; preserves parasitic morphology and inactivates pathogens. | Standardized solution is critical for consistent recovery rates [3] [7]. |
| Ethyl Acetate | Solvent for FECT; extracts fats and dissolved debris from the sample. | Preferred over diethyl ether for enhanced safety [3]. |
| Phosphate Buffered Saline (PBS) | Universal washing and dilution buffer for immunoassays. | Common formulation: 50 mM Phosphate, pH 8.0, 0.15 M NaCl [71]. |
| Blocking Buffers | Reduces non-specific binding in immunoassays. | 1% BSA or 10% host serum in TBS/PBS; casein-based commercial blockers (e.g., Pierce) [71] [73]. |
| Matched Antibody Pairs | Critical for sandwich immunoassays; one for capture, one for detection. | Must be affinity-purified and tested for specificity and lack of cross-reactivity [71]. |
| Magnetic Nanotags (MNT) | Detection label for MagArray platform; enables highly sensitive, wash-free detection. | An alternative to enzymatic (HRP/ALP) or fluorescent labels [73]. |
| DNA Extraction Kits | Isolate high-purity genomic DNA from FECT sediment for PCR. | Silica-membrane or magnetic-bead based kits are effective [2]. |
| Xpert Test Cartridges | Self-contained, automated modules for PCR. | Enable sample-to-answer molecular testing from FECT sediment [74]. |
The integration of the traditional FECT method with modern immunoassays and molecular diagnostics creates a powerful, synergistic workflow for parasitology research and diagnostic development. Using FECT as a universal sample preparation step standardizes input material, removes common inhibitors, and significantly enhances the sensitivity and reliability of downstream applications. The protocols outlined herein provide a clear roadmap for researchers to leverage this integrated approach, facilitating more accurate detection, drug efficacy studies, and ultimately, improved management of intestinal parasitic infections.
The formalin-ethyl acetate concentration technique (FECT) remains the gold standard for diagnosing intestinal parasitic infections (IPIs) in clinical and research settings worldwide [2] [75]. Despite the emergence of molecular techniques, FECT maintains its status due to its proven sensitivity, cost-effectiveness, and simplicity, particularly in resource-limited environments where the burden of parasitic diseases is highest [2]. However, traditional FECT exhibits limitations in detecting low-intensity infections and depends heavily on the expertise of laboratory personnel, introducing potential variability in diagnostic accuracy [75].
Recent advances in artificial intelligence (AI) and deep learning (DL) present a transformative opportunity to augment traditional parasitological diagnostics. These technologies offer the potential for automated, high-throughput, and highly accurate analysis of stool samples, which could standardize diagnostics and improve detection sensitivity, particularly for low-intensity infections that often evade conventional microscopy [2]. This application note details the experimental protocols and validation frameworks for rigorously benchmarking AI and DL models against the established FECT standard, ensuring that these innovative tools meet the rigorous demands of clinical and research parasitology.
Current State and Refinements of the FECT Standard
The conventional FECT procedure, as outlined by the CDC, involves a series of meticulous steps designed to concentrate parasitic elements from stool specimens [8]. The process begins with homogenization of a stool sample in saline, followed by filtration through gauze to remove large debris. The filtered suspension is then centrifuged, and the resulting pellet is resuspended in formalin for fixation. The key concentration step involves the addition of ethyl acetate, followed by vigorous shaking and subsequent centrifugation. This creates a layered system where debris is trapped in an ethyl acetate plug, which is discarded, leaving a cleaned sediment containing parasites for microscopic examination [8].
Advancements in FECT Methodology
Recent research has focused on optimizing FECT to enhance its sensitivity, especially for challenging low-intensity infections. A significant innovation is the "one-step FECT" method, which modifies the traditional protocol by initially preserving one gram of feces in 10% formalin for two days before the addition of ethyl acetate and a shorter, gentler centrifugation step [75]. This modification has demonstrated a marked improvement in diagnostic performance.
Table 1: Performance Comparison of Conventional vs. One-Step FECT for Opisthorchis viverrini Detection
| Diagnostic Method | Sensitivity (%) | Detection Threshold (Eggs per Gram) | Key Advantage |
|---|---|---|---|
| Conventional FECT | 87.9% | 34 e.p.g. | Established gold standard; robust protocol [75] |
| One-Step FECT | 95.6% | 18 e.p.g. | Superior sensitivity for low-intensity infections [75] |
Another study investigated the underlying mechanisms of FECT, revealing that the interaction between ethyl acetate and cellulose fibers in fecal material is crucial for efficient lipid extraction and debris clearance. The addition of acid residues was found to loosen cellulose structures, thereby improving fecal bulk flotation and providing a cleaner background for the visualization of parasite eggs [21].
AI and Deep Learning Models for Parasite Detection
The application of AI in stool diagnostics primarily utilizes two approaches: classification models, which categorize an entire image, and object detection models, which identify and locate multiple parasitic structures within an image.
Performance of State-of-the-Art Models
A comprehensive 2025 validation study compared several advanced DL models against human experts using FECT and Merthiolate-iodine-formalin (MIF) techniques as the ground truth. The models were trained and tested on image datasets derived from modified direct smear preparations [2].
Table 2: Performance Metrics of Deep Learning Models in Intestinal Parasite Identification
| Model | Accuracy (%) | Precision (%) | Sensitivity (%) | Specificity (%) | F1 Score | AUROC |
|---|---|---|---|---|---|---|
| DINOv2-Large | 98.93 | 84.52 | 78.00 | 99.57 | 81.13 | 0.97 |
| YOLOv8-m | 97.59 | 62.02 | 46.78 | 99.13 | 53.33 | 0.76 |
| ResNet-50 | Details in [2] | Details in [2] | Details in [2] | Details in [2] | Details in [2] | Details in [2] |
| YOLOv4-tiny | Details in [2] | 96.25 | 95.08 | Details in [2] | Details in [2] | Details in [2] |
The study concluded that the DINOv2-large model, a self-supervised learning architecture, demonstrated superior overall performance, with high metric values indicating strong potential for reliable automated parasite identification [2]. Object detection models like YOLOv4-tiny also showed high precision and sensitivity, making them suitable for detecting multiple parasites in a single image, which is crucial for diagnosing mixed infections [2].
Experimental Protocols for AI Validation Against FECT
Sample Preparation and Ground Truth Establishment
Protocol: Reference Standard FECT Procedure
- Specimen Processing: Mix the stool specimen thoroughly. Weigh 1 gram of feces and emulsify in 10 mL of 0.85% saline or 10% formalin [8] [75].
- Filtration: Strain the suspension through wetted cheesecloth-type gauze into a 15 mL conical centrifuge tube. Add additional saline or formalin to bring the volume to 15 mL [8].
- Primary Centrifugation: Centrifuge at 500 × g for 10 minutes. Decant the supernatant completely [8].
- Formalin-Ethyl Acetate Concentration: Resuspend the sediment in 10 mL of 10% formalin. Add 4 mL of ethyl acetate, stopper the tube, and shake vigorously for 30 seconds. Centrifuge again at 500 × g for 10 minutes [8].
- Sediment Collection: Free the debris plug from the tube wall with an applicator stick, decant the supernatant layers, and clean the tube walls with a swab. The final sediment, containing the concentrated parasites, is resuspended in a few drops of 10% formalin [8].
- Microscopy and Labeling: Prepare wet mounts from the sediment and examine under a microscope at appropriate magnifications. Experienced microbiologists must identify and manually annotate (label) all parasitic structures (eggs, cysts, larvae) in digital images of the slides. These annotated images serve as the ground truth dataset for AI model training and validation [2].
AI Model Training and Evaluation Workflow
Protocol: AI Model Development and Benchmarking
- Data Curation: Split the ground truth image dataset into a training set (80%) and a testing set (20%). Employ data augmentation techniques (e.g., rotation, flipping, color variation) to increase dataset diversity and improve model robustness [2].
- Model Selection and Training:
- For Classification: Train models like ResNet-50 or DINOv2 to classify images into predefined categories (e.g., "positive for A. lumbricoides," "negative") [2].
- For Object Detection: Train models like YOLOv8 or YOLOv4-tiny to draw bounding boxes around and classify individual parasitic elements within an image [2].
- Performance Benchmarking: Evaluate the trained models on the withheld test set. Compare model predictions against the human-annotated ground truth using the metrics in Table 2 [2].
- Statistical Agreement Analysis: Use Cohen's Kappa to measure the level of agreement between the AI model and human expert classifications. Employ Bland-Altman analysis to visualize any systematic biases in quantitative measures, such as egg counts per gram [2].
Diagram 1: AI Validation Workflow against FECT. This diagram outlines the key steps for validating AI models using FECT as a reference standard.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the validation protocol requires specific laboratory materials and computational resources.
Table 3: Essential Research Reagents and Materials for FECT and AI Validation
| Item | Function/Application | Specifications/Notes |
|---|---|---|
| 10% Formalin | Fixation and preservation of parasitic elements in stool specimens. | Maintains morphology; essential for FECT procedure [8]. |
| Ethyl Acetate | Organic solvent for concentration; extracts fats and debris. | Creates a clean sediment for microscopy [8] [21]. |
| Conical Centrifuge Tubes | Holder for samples during centrifugation and concentration steps. | 15 mL capacity; compatible with standard centrifuges [8]. |
| Microscope & Digital Camera | Visualization and digitization of FECT sediment for analysis. | Must be capable of high-resolution image capture for AI training [2]. |
| GPU Workstation | Computational hardware for training complex deep learning models. | Required for efficient processing of large image datasets [2]. |
| AI Training Platform | Software environment for developing and training AI models. | E.g., CIRA CORE, TensorFlow, or PyTorch [2]. |
Regulatory and Commercial Pathway
The integration of AI into diagnostic devices is an area of active regulatory development. The U.S. Food and Drug Administration (FDA) has published an "Artificial Intelligence/Machine Learning Software as a Medical Device Action Plan" and related guidance documents to outline a regulatory framework for these technologies [76]. Key considerations include:
- Premarket Review: Most AI-enabled diagnostic devices will require premarket review via pathways like 510(k), De Novo, or Premarket Approval (PMA) [76].
- Predetermined Change Control Plans (PCCP): The FDA encourages manufacturers to submit a PCCP, which outlines planned future modifications to the AI model, allowing for iterative improvement under a defined regulatory umbrella [76].
- Clinical Validation: As emphasized in broader AI development principles, prospective validation in real-world clinical settings and, in many cases, randomized controlled trials (RCTs) are increasingly imperative to demonstrate clinical utility, secure regulatory approval, and achieve reimbursement [77].
The commercial landscape is also evolving, with the stool biomarkers test market projected to grow significantly, driven in part by the integration of AI to enhance diagnostic accuracy and efficiency [78].
The validation of AI and deep learning models against the FECT standard represents a critical step toward the future of parasitology diagnostics. Evidence demonstrates that models like DINOv2-large and YOLOv4-tiny can achieve a strong level of agreement with human experts, showcasing particular strength in identifying helminth eggs due to their distinct morphology [2]. The path forward involves a hybrid approach, where AI does not merely replace traditional methods but augments them. This synergy can lead to higher diagnostic throughput, reduced inter-observer variability, and improved detection of low-intensity infections, as highlighted by the enhanced one-step FECT [75]. For researchers and drug developers, adopting the rigorous validation protocols outlined herein is essential for building robust, clinically relevant AI tools that can meet regulatory standards and ultimately reduce the global burden of intestinal parasitic infections.
Conclusion
The Formalin-Ethyl Acetate Concentration Technique remains a vital, highly sensitive, and cost-effective method for the diagnosis of intestinal parasites, forming the gold standard in many laboratory settings. Evidence consistently validates its superiority over direct smear and simple formalin concentration methods, particularly for detecting low-burden and co-infections. Future directions point toward the hybridization of FECT with advanced technologies, including AI-assisted microscopy for automated detection and classification, which can enhance throughput and standardize diagnostics. For researchers and drug development professionals, mastering FECT is fundamental for epidemiological surveillance, assessing intervention efficacy, and validating novel diagnostic and therapeutic agents in the ongoing fight against neglected tropical diseases.
References
- 1. Intestinal Parasitic Infections in 2023 - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10284646/]
- 2. Performance validation of deep-learning-based approach in ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06878-w]
- 3. Evaluation of different concentration techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922389/]
- 4. Global prevalence and correlation of intestinal parasitic ... [https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-025-04144-y]
- 5. Burden and factors influencing intestinal parasitic infections ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11198874/]
- 6. Global impact of parasitic infections and the importance ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1546195/full]
- 7. Faecal examination by the quantitative formalin-ethyl ... [https://bio-protocol.org/exchange/minidetail?id=6562293&type=30]
- 8. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimenproc.html]
- 9. A historical review of the techniques of recovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7269538/]
- 10. Comparison of three concentration methods for the ... [https://www.sciencedirect.com/science/article/abs/pii/S0014489410001542]
- 11. Comparison of sedimentation and flotation techniques for ... [https://pubmed.ncbi.nlm.nih.gov/2416771/]
- 12. Comparison of formalin-ethyl ether sedimentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC273909/]
- 13. Improved Detection of Intestinal Helminth Infections with a ... [https://www.mdpi.com/2414-6366/6/2/51]
- 14. Comparison of 2 centrifugation procedures in the formalin- ... [https://www.sciencedirect.com/science/article/abs/pii/0020751996000574]
- 15. Know All About Diethyl Ether a Detail Guide [https://cloudsds.com/chemical-hazard-and-safety/know-all-about-diethyl-ether-a-detail-guide-cloudsds/]
- 16. Eco-friendly alternatives to conventional solvents [https://www.sciencedirect.com/science/article/pii/S2772826925000859]
- 17. Clinical comparison of ethyl acetate and diethyl ether in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC273973/]
- 18. Morphologic comparison of intestinal parasites [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/morphcomp.html]
- 19. Stool Ova and Parasite Test [https://emedicine.medscape.com/article/2117799-overview]
- 20. Stool Specimens – Staining Procedures [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/staining.html]
- 21. Improvement of the Diagnostic Method for the Detection ... [https://pubmed.ncbi.nlm.nih.gov/39153012/]
- 22. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimencoll.html]
- 23. Total-Fixâ„¢ Fixative, O&P Stool Transport for Parasitology [https://hardydiagnostics.com/280705]
- 24. Rethinking tissue preservation: A review of non-toxic and ... [https://pubmed.ncbi.nlm.nih.gov/40378504/]
- 25. A long term time lapse microscopy technique for ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1601397/full]
- 26. Introduction to Specimen Collection [https://www.labcorp.com/test-menu/resources/introduction-to-specimen-collection]
- 27. A comparative study of formalin-ethyl acetate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5991041/]
- 28. High-throughput detection of parasites and ova in stool using ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-023-06108-1]
- 29. Automated green sample preparation for quantitative ... [https://www.sciencedirect.com/science/article/pii/S2772577424000375]
- 30. Advances in Lipid Extraction Methods—A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8704327/]
- 31. A comparison of five lipid extraction solvent systems for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3679384/]
- 32. Module 2.2: Direct Fecal Smear (Wet Mount) [https://pressbooks.umn.edu/cvdl/chapter/module-2-2-fecal-lab-procedure-1-direct-fecal-smear-wet-mount/]
- 33. Comparison of the Quantitative Formalin Ethyl Acetate ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1081356/]
- 34. Advantages and Limitations of Microscopy and Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9979072/]
- 35. Improvement of the Diagnostic Method for the Detection of Parasite... [https://link.springer.com/article/10.1007/s11686-024-00871-6]
- 36. Comparison of a Urine Antigen Assay and Multiple Examinations with... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10324020/]
- 37. Deep learning for microscopic examination of protozoan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8886013/]
- 38. Stool Specimens – Detection of Parasite Antigens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/antigendetection.html]
- 39. Performance validation of deep-learning-based approach in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317604/]
- 40. Diagnostic delays in infectious diseases - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9424060/]
- 41. Validation of stool and blood analysis compared to Inv A and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12228386/]
- 42. AI System Outperforms Human Detection of Parasites in ... [https://clpmag.com/disease-states/infectious-diseases/gastrointestinal-infections/ai-system-outperforms-human-detection-parasites-stool-samples/]
- 43. Comparative analysis of commercial and “In-House ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 44. Low Sensitivity of the Formol-Ethyl Acetate Sedimentation ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0000386]
- 45. Comparison of the quantitative formalin ethyl acetate ... [https://pubmed.ncbi.nlm.nih.gov/15815023/]
- 46. Improved Detection of Intestinal Helminth Infections with a ... [https://www.shoklo-unit.com/research-activities/publications/1172304]
- 47. Comparison of CONSEDâ„¢ and Formalin-Ethyl Acetate ... [https://www.alphatecsystems.com/comparison-of-consedtm-and-formalin-ethyl-acetate-methods-for-concentrating-intestinal-parasites-and-eggs/]
- 48. Validation of Digital Slide Scanning and a Convolutional ... [https://www.mdpi.com/2075-4418/15/23/2974]
- 49. Concentration method [https://bio-protocol.org/exchange/minidetail?id=2176385&type=30]
- 50. Detecting Cryptosporidium in Stool Samples Submitted to a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7356455/]
- 51. CDC - DPDx - Cryptosporidiosis [https://www.cdc.gov/dpdx/cryptosporidiosis/index.html]
- 52. Anti- Cryptosporidium oocysts polyclonal antibodies for... [https://amb-express.springeropen.com/articles/10.1186/s13568-023-01632-w]
- 53. Detection of Blastocystis in clinical stool specimens using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5991034/]
- 54. In vitro culture of Blastocystis hominis in three liquid media ... [https://www.sciencedirect.com/science/article/pii/S1201971211001913]
- 55. An improved stool concentration procedure for the detection of... [https://pubmed.ncbi.nlm.nih.gov/25193442/]
- 56. Advantage of using colonic washouts for Blastocystis ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/1756-3305-7-162]
- 57. Performance of 30 protocol combinations for the detection ... [https://www.sciencedirect.com/science/article/pii/S1684118225000064]
- 58. Low Sensitivity of the Formol-Ethyl Acetate Sedimentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2638014/]
- 59. Sensitivity of diagnostic tests for human soil-transmitted ... [https://www.sciencedirect.com/science/article/pii/S002075191400143X]
- 60. Comparison of the Kato-Katz, Wet Mount, and Formol-Ether ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4890854/]
- 61. Evaluating the performance of diagnostic methods for soil ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-020-05533-2]
- 62. Journal of Gastrointestinal & Digestive System Open Access [https://www.omicsonline.org/open-access/the-sensitivity-and-specificity-comparison-between-stool-wet-mount-and-katokatz-techniques-for-the-detection-of-intestinal-helmint-2161-069X-1000692-120837.html]
- 63. Comparison of faecal protein biomarkers' diagnostic ... [https://www.nature.com/articles/s41598-022-06689-4]
- 64. Diagnostic sensitivity of formalin-fixed faecal microscopy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12138886/]
- 65. Assessing the diagnostic value of qPCR for Trichuris trichiura [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629931/]
- 66. Evaluation of the diagnostic techniques in the detection ... [https://www.sciencedirect.com/science/article/pii/S2405844024159671]
- 67. Comparative Study of DNA Extraction Methods for the PCR ... [https://www.mdpi.com/2075-4418/12/11/2588]
- 68. Performance of Mini Parasep® SF stool concentrator kit ... [https://pubmed.ncbi.nlm.nih.gov/35761311/]
- 69. Performance of Mini Parasep® SF stool concentrator kit ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-022-05338-z]
- 70. Comparison of stool examination techniques to detect ... [https://www.sciencedirect.com/science/article/abs/pii/S0001706X18311318]
- 71. Immunoassay Methods - Assay Guidance Manual - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK92434/]
- 72. Label-free capacitive assaying of biomarkers for molecular ... [https://www.nature.com/articles/s41596-020-0390-9]
- 73. Multiplex Immunoassay Protocol [https://www.creative-diagnostics.com/multiplex-immunoassay-protocol.htm]
- 74. Molecular Diagnostic Test Menu [https://www.cepheid.com/en-US/tests.html]
- 75. Enhanced detection of Opisthorchis viverrini infection: A comparative... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11647639/]
- 76. Artificial Intelligence in Software as a Medical Device [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-software-medical-device]
- 77. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 78. Stool Biomarkers Test Market Futuristic Trends | AI & ... [https://www.linkedin.com/pulse/stool-biomarkers-test-market-futuristic-trends-qigse/]