Definitive Diagnosis of Parasitic Diseases: From Traditional Methods to Next-Generation Tools for Researchers and Developers
This article provides a comprehensive overview of the evolving landscape of parasitic disease diagnostics, tailored for researchers, scientists, and drug development professionals.
Definitive Diagnosis of Parasitic Diseases: From Traditional Methods to Next-Generation Tools for Researchers and Developers
Abstract
This article provides a comprehensive overview of the evolving landscape of parasitic disease diagnostics, tailored for researchers, scientists, and drug development professionals. It explores the limitations of conventional techniques and delves into advanced molecular, nanobiosensor, and multi-omics approaches that are enhancing sensitivity and specificity. The content further addresses critical challenges in assay optimization and standardization, while also examining the regulatory frameworks and comparative efficacy of novel tools. The synthesis aims to inform R&D strategy and accelerate the development of next-generation diagnostic solutions for global health.
The Diagnostic Imperative: Understanding the Global Burden and Limitations of Conventional Parasitology
The Global Health and Economic Impact of Parasitic Infections
Parasitic infections constitute a profound and persistent global health challenge, imposing a significant burden on human populations, healthcare systems, and economies worldwide. These infections, caused by diverse organisms including protozoa, helminths, and ectoparasites, are particularly prevalent in tropical and subtropical regions with resource-limited settings and poor sanitation [1]. The World Health Organization (WHO) estimates that more than a quarter of the world's population is infected with intestinal parasitic infections alone, resulting in approximately 450 million illnesses annually, with the highest burden occurring among children [2]. This whitepaper provides a comprehensive technical analysis of the health and economic impacts of parasitic diseases, framed within the critical context of advanced diagnostic research, which is essential for accurate disease surveillance, effective treatment, and the development of control strategies.
The relationship between parasitic infections and their definitive diagnosis represents a fundamental nexus in global public health. Accurate diagnosis not only guides individual patient management but also enables the precise quantification of disease burden, informs resource allocation, and monitors the effectiveness of intervention programs. For researchers, scientists, and drug development professionals, understanding the full scope of the problem is a necessary precursor to innovating solutions. This document synthesizes the most current data on epidemiological reach and economic consequences, while simultaneously detailing the advanced diagnostic methodologies that are reshaping the field of parasitology.
Global Health Burden of Parasitic Infections
Epidemiological Reach and Mortality
The global health impact of parasitic infections is staggering, both in terms of morbidity and mortality. These diseases disproportionally affect the most vulnerable populations, including children, immunocompromised individuals, and those in low- and middle-income countries.
Table 1: Global Burden of Major Parasitic Infections
| Parasite/Disease | Global Prevalence/Incidence | Annual Mortality | Population at Risk | Key Affected Populations |
|---|---|---|---|---|
| Malaria (Plasmodium spp.) | 249 million cases [2] | >600,000 [2] | Nearly half the global population [2] | Children under 5 (account for ~80% of deaths) [2] |
| Soil-Transmitted Helminths | 1.5 billion infected [3] | Not specified (Morbidity focus) | Not specified | Children in endemic areas [3] |
| Schistosomiasis | Not specified | Not specified | Not specified | Communities with limited access to safe water and sanitation |
| Intestinal Protozoa (e.g., Giardia, Cryptosporidium) | 450 million ill as result of intestinal infections [2] | Not specified | Global, with higher burden in areas of poor sanitation [2] | Children, travelers, immunocompromised individuals [1] |
| Visceral Leishmaniasis | Up to 400,000 new cases annually [2] | ~50,000 (2010 estimate) [2] | >65 countries [2] | Endemic areas of Brazil, India, East Africa, Southern Europe [2] |
Beyond the raw numbers of infection and death, the Disability-Adjusted Life Year (DALY) metric provides a more complete picture of the disease burden by combining years of life lost due to premature mortality and years lived with disability. For example, malaria was responsible for a staggering 46 million DALYs in 2019, reflecting its devastating impact on healthy life [2]. Vector-borne diseases, which include many parasitic illnesses transmitted by mosquitoes, ticks, and other ectoparasites, account for more than 17% of all human infectious diseases globally, causing over 700,000 deaths annually [2].
Morbidity and Co-infections
The morbidity associated with parasitic infections extends across a wide spectrum, from acute, life-threatening illness to chronic conditions that cause long-term disability and impair cognitive and physical development. Helminth infections, for instance, are a leading cause of iron-deficiency anemia, growth retardation, and stunted cognitive development in children [4]. The impact of co-infections with other pathogens presents an additional layer of complexity. A 2025 meta-analysis revealed that the global prevalence of parasitic coinfection in people living with viruses is substantial, estimated at 21.34% for helminths and 34.13% for protozoa in virus-infected individuals [4]. These co-infections can alter immune responses, exacerbate disease severity, and complicate diagnosis and treatment. For instance, HIV infection drives immunocompromise that predisposes individuals to severe opportunistic parasitic infections, while helminth-induced Th2-type immune responses can inhibit Th1-type antiviral defense mechanisms [4].
Economic Impact of Parasitic Diseases
The economic burden of parasitic infections is multifaceted, encompassing direct healthcare costs, indirect costs due to lost productivity, and long-term macroeconomic effects on human capital and national economies.
Direct and Indirect Costs
The direct costs include expenses for diagnosis, treatment, and hospitalization, while indirect costs arise from lost labor productivity due to illness, disability, and premature death. For example, the Parasitic Diseases Therapeutic Market is anticipated to grow from $9.39 billion in 2025 to $19.78 billion by 2033, reflecting the substantial and growing economic activity directed at managing these diseases [5]. This market growth is driven by increasing disease prevalence, advancements in treatment, and heightened awareness.
The economic impact is not limited to human health. Plant-parasitic nematodes, such as root-knot nematodes (Meloidogyne spp.), cause massive agricultural losses, estimated at $125 to $350 billion per year in global crop yields [2]. The rice root-knot nematode (M. graminicola) alone is responsible for annual rice yield losses of 15% in Asia, threatening food security [2].
Macroeconomic Burden
The macroeconomic burden, measured by the impact on a country's gross domestic product (GDP), can be profound, particularly in endemic countries. A 2025 study on schistosomiasis estimated its macroeconomic burden in 25 endemic countries at INT$ 49,504 million (uncertainty interval: 48,668–50,339) for the period 2010-2050 [6]. This model considered the impact of mortality and morbidity on labor supply, age and gender differences in education and work experience, and treatment costs on capital accumulation. The burden was inequitably distributed, with Egypt, Brazil, and South Africa bearing the largest absolute economic burdens [6]. This represents a loss equivalent to 0.0174% of the total GDP of these 25 countries, underscoring the long-term economic drag exerted by a single neglected tropical disease.
Table 2: Estimated Macroeconomic Burden of Schistosomiasis in Select Endemic Countries (2025 Study)
| Country | Estimated Economic Burden (International Dollars, Millions) |
|---|---|
| Egypt | 11,400 |
| Brazil | 9,779 |
| South Africa | 6,744 |
| 25 Endemic Countries (Total) | 49,504 |
The Critical Role of Definitive Diagnosis in Mitigating Impact
Limitations of Conventional Diagnostic Methods
Accurate diagnosis is the cornerstone of effective parasitic disease control, yet traditional methods have significant limitations that hinder their effectiveness, particularly in resource-poor settings. Conventional techniques such as microscopy, serological testing, histopathology, and culturing have been the diagnostic mainstay for decades [7]. While often effective, these methods can be time-consuming, require a high level of technical expertise, and have limited sensitivity and specificity, especially in cases of low parasite burden or chronic infection [7] [3]. The reliance on these tools in endemic regions with poor infrastructure and limited access to healthcare facilities has historically led to underdiagnosis and inaccurate burden estimates, thereby impeding effective control and eradication efforts [8].
Advanced Diagnostic Methodologies and Protocols
The field of parasitic disease diagnosis is being revolutionized by technological advancements that offer unprecedented sensitivity, specificity, speed, and field-deployability. These innovations are crucial for generating the precise data needed to truly understand and mitigate the global impact of these infections.
Molecular Diagnostics
Molecular methods have dramatically enhanced the detection and identification of parasites.
- Polymerase Chain Reaction (PCR) and Its Variants: These techniques amplify and detect parasite-specific DNA sequences, offering high sensitivity and the ability to differentiate between species and strains. Multiplex PCR allows for the simultaneous detection of multiple parasites in a single reaction, which is invaluable for diagnosing co-infections [8]. Digital PCR (dPCR), a newer technology, provides absolute quantification of parasite load without the need for a standard curve, proving useful for monitoring treatment efficacy and detecting low-level infections [8].
- Isothermal Amplification (e.g., LAMP, RPA): Techniques like Loop-Mediated Isothermal Amplification (LAMP) amplify DNA at a constant temperature, eliminating the need for sophisticated thermal cyclers. This makes them ideal for rapid, field-adjustable tools for use in primary care settings or remote laboratories [7] [8].
- Next-Generation Sequencing (NGS): NGS technologies allow for the comprehensive analysis of parasite genomes, enabling species identification, detection of drug-resistance markers, and investigation of complex parasite populations and transmission dynamics [7] [8].
Immunological and Biomarker-Based Advances
Advanced serological methods have moved beyond basic antibody detection.
- Rapid Diagnostic Tests (RDTs) and Lateral Flow Immunoassays (LFIA): These point-of-care (POC) tests provide results in minutes from a drop of blood, serum, or other samples. They are crucial for rapid screening and management, particularly for diseases like malaria [7] [8].
- Enzyme-Linked Immunosorbent Assay (ELISA) and Chemiluminescent Immunoassays (CLIA): These plate-based assays are used for the high-throughput detection of parasite-specific antigens or host antibodies. They are fundamental tools for seroepidemiology studies [8].
- Biomarker Detection: Research is focused on identifying and detecting specific biomarkers, including parasite-specific antigens, host-derived antibodies, cytokines, and metabolites, to distinguish between active and past infections, monitor disease progression, and assess treatment response [7] [8].
Imaging and Artificial Intelligence
Advanced imaging technologies, augmented by artificial intelligence (AI), are increasing the speed and accuracy of diagnosis.
- AI-Based Image Recognition: AI algorithms are being trained to automatically detect and identify parasites in digital images of blood smears, stool samples, and histopathology slides. This can reduce reliance on human expertise, decrease diagnostic time, and improve consistency [3] [8].
- Advanced Staining and Imaging Techniques: Improved staining methods enhance the contrast and visibility of parasites in samples, while advanced imaging systems can automate the scanning of slides, flagging potential parasites for technologist review [8].
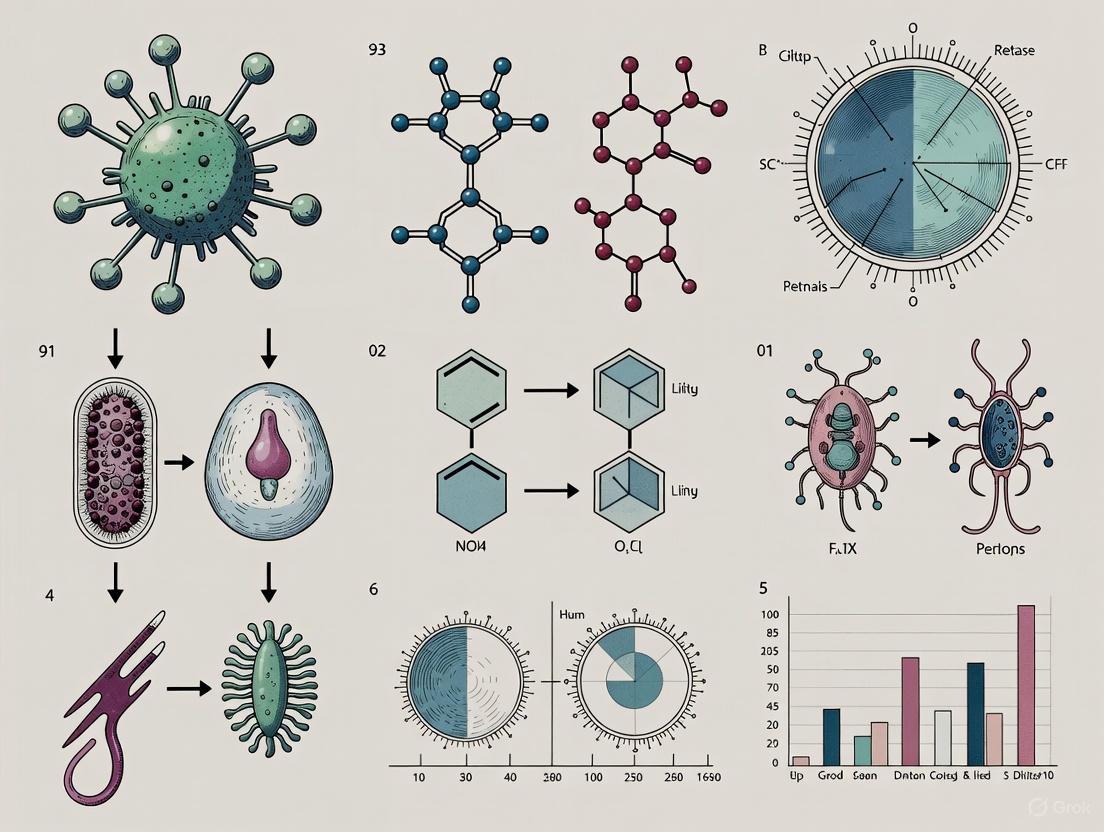
The following workflow diagram illustrates the integrated application of these modern diagnostic approaches in a research and clinical setting:
Integrated Diagnostic Workflow for Parasitic Infections
CRISPR-Cas and Nanotechnology
The latest innovations are pushing the boundaries of diagnostic sensitivity and portability.
- CRISPR-Cas Diagnostics: This technology utilizes the programmability of CRISPR-Cas systems to detect parasite-specific DNA or RNA sequences with exceptional specificity. It offers the potential for ultra-sensitive, rapid, and field-deployable diagnostic tests [8].
- Nanotechnology: The application of nanoparticles in diagnostics is leading to the development of highly sensitive nano-biosensors. These devices can detect minute quantities of parasite biomarkers (nucleic acids, antigens) and are being integrated into POC platforms for use in low-resource settings [8].
Multi-Omics Integration
A holistic approach integrating data from genomics, transcriptomics, proteomics, and metabolomics (multi-omics) is providing a comprehensive understanding of parasite biology, host-parasite interactions, and disease mechanisms. This integrated data is invaluable for identifying new therapeutic targets and discovering novel diagnostic biomarkers [7] [8].
The Scientist's Toolkit: Key Research Reagent Solutions
The advancement of diagnostic research and development relies on a suite of specialized reagents and materials. The following table details essential components used in modern parasitology diagnostics.
Table 3: Key Research Reagent Solutions for Parasitic Disease Diagnostics
| Research Reagent / Material | Function and Application in Diagnostics |
|---|---|
| Specific Primers and Probes | Short, synthetic DNA sequences designed to bind to and amplify unique genomic regions of target parasites in PCR, qPCR, and dPCR assays. |
| Recombinant Parasitic Antigens | Purified proteins produced from cloned parasite genes; used as capture/detection targets in immunoassays (ELISA, RDTs) and for assessing host immune responses. |
| Monoclonal and Polyclonal Antibodies | Antibodies raised against specific parasitic antigens; function as critical detection reagents in immunoassays like LFIA, ELISA, and CLIA. |
| CRISPR-Cas Enzymes & Guide RNAs | The core components of CRISPR-based diagnostics; the guide RNA directs the Cas enzyme to a specific parasite DNA/RNA sequence, triggering a detectable signal upon binding. |
| Functionalized Nanoparticles | Gold nanoparticles, magnetic beads, or quantum dots coated with antibodies or DNA probes; used as signal amplifiers or capture agents in biosensors and rapid tests. |
| Next-Generation Sequencing Kits | Commercial kits containing all necessary enzymes, buffers, and adapters for preparing parasite DNA/RNA libraries for sequencing on NGS platforms. |
| Cell Culture Media for Parasites | Specialized nutrient media required for in vitro cultivation of certain parasites (e.g., Leishmania, Trypanosoma), essential for antigen production and drug testing. |
| Fenuron-d5 | Fenuron-d5, CAS:1219802-06-8, MF:C9H12N2O, MW:169.239 |
| 1-Octen-3-ol - d3 | 1-Octen-3-ol |
Parasitic infections remain a formidable global challenge, inflicting severe health consequences and imposing a substantial economic burden that stifles development, particularly in endemic regions. The data presented herein underscores the vast epidemiological reach of these diseases, from malaria affecting hundreds of millions to the chronic disability caused by soil-transmitted helminths and schistosomiasis. The economic toll, quantified in billions of dollars of lost productivity and healthcare costs, highlights the urgent need for sustained and increased investment in control and elimination efforts. The path to mitigating this multifaceted impact is inextricably linked to advancements in diagnostic technology. The transition from traditional, often insensitive methods to sophisticated molecular, immunoassay, and nanotechnology-based platforms is revolutionizing the field. These innovations enable definitive diagnosis, accurate species identification, detection of co-infections, and monitoring of drug resistance, which are all critical for effective patient management, precise disease surveillance, and the development of new therapeutics. For researchers, scientists, and drug development professionals, a deep understanding of both the scale of the problem and the cutting-edge tools available to address it is paramount. Continued research and development into more sensitive, specific, affordable, and field-deployable diagnostic solutions, integrated within a One Health framework, are essential for achieving lasting progress against parasitic diseases and alleviating their profound impact on global health and economies.
For decades, the diagnosis of parasitic infections has relied fundamentally on a triad of conventional techniques: microscopy, serology, and culture. Despite the emergence of sophisticated molecular methods, these traditional approaches have formed the historical gold standards and continue to serve as the backbone of diagnostic parasitology, particularly in resource-limited settings where the burden of parasitic diseases is highest [9] [10]. These methods are efficient, comparatively cheap, and sometimes still provide information that newer molecular methods cannot replicate [11]. The enduring relevance of these techniques lies in their direct ability to visualize parasites, detect the host's immune response, or isolate the causative organism, thereby providing a definitive diagnosis. However, the diagnostic process is complicated by the fact that many parasitic diseases do not produce characteristic symptoms, requiring not just the detection of a parasite but also the establishment of a causal relationship between its presence and the clinical disease [3] [12]. This in-depth technical guide examines the principles, methodologies, and applications of these cornerstone techniques within the broader context of definitive diagnosis for research and drug development.
Microscopy: The Visual Gold Standard
Principles and Historical Significance
Microscopy represents the oldest and most foundational tool in parasitology. Its inception in the 17th century, pioneered by Antonie van Leeuwenhoek, revolutionized the field by enabling the visualization of the microscopic world of parasites [9]. Before its advent, parasitic infections were often misunderstood and misdiagnosed [9]. The core principle of microscopic diagnosis is the direct morphological identification of parasites, their eggs (ova), larvae, or cysts in various clinical specimens. This method remains the gold standard for diagnosing many parasitic infections due to its directness, low cost, and ability to provide a quantitative assessment of parasite burden [10] [13]. Despite its advantages, microscopy requires significant expertise, as the accurate differentiation of parasite species relies on a detailed understanding of morphological characteristics, and its sensitivity can be limited by factors such as parasite load and sample quality [3] [14].
Key Methodologies and Workflows
Microscopic diagnosis encompasses several standardized protocols, tailored to the parasite and the specimen type.
- Direct Wet Mount Examination: Fresh specimens (e.g., stool, blood) are examined under a microscope, often using saline or iodine. This allows for the observation of motile trophozoites (e.g., in amoebiasis), larvae, or cysts [13]. Iodine staining helps visualize nuclear details within cysts.
- Concentration Techniques: Methods like formol-ether sedimentation are used to concentrate parasites from a larger sample volume, thereby increasing the test's sensitivity. This is particularly useful for identifying light infections [13].
- Stained Smears: Thin and thick blood smears are critical for diagnosing blood-borne parasites like Plasmodium species (malaria). The smears are stained with Giemsa or other Romanowsky stains to highlight the parasite's morphology within red blood cells [10]. Similarly, permanent stains (e.g., iron-hematoxylin) are used on stool samples to enhance the visualization of intestinal protozoa [13].
The following workflow outlines a typical diagnostic process for an intestinal parasitic infection using microscopy:
Experimental Protocol: Direct Wet Mount and Concentration for Intestinal Parasites
Objective: To identify cysts, ova, or trophozoites of intestinal parasites in a stool sample.
Materials:
- Fresh stool specimen
- Microscope slides and coverslips
- Normal saline (0.9%)
- Lugol's iodine
- Centrifuge and centrifuge tubes
- Formalin (10%) and ethyl acetate
- Disposable pipettes
Procedure:
- Direct Saline and Iodine Wet Mount:
- Emulsify a small portion of stool (about 2 mg) in a drop of saline on a microscope slide.
- Prepare a second emulsification in a drop of Lugol's iodine on a separate slide.
- Apply coverslips and examine systematically under low (10x) and high (40x) magnification. Use 100x oil immersion for detail if needed.
- Look for motile trophozoites (in saline), cysts, and eggs. Iodine stains glycogen and nuclei.
- Formol-Ether Sedimentation Concentration:
- Suspend 1-2 g of stool in 10 mL of 10% formalin in a centrifuge tube. Mix thoroughly and filter through a sieve.
- Add 3 mL of ethyl acetate to the filtrate. Stopper the tube and shake vigorously.
- Centrifuge at 500 x g for 10 minutes. The debris will form a plug between the formalin and ethyl acetate layers.
- Free the debris plug by ringing it with an applicator stick and carefully decant the supernatant.
- Use a swab or pipette to transfer sediment to a slide for examination as above.
Interpretation: Identify parasites based on characteristic size, shape, and internal structures (e.g., number of nuclei in cysts, appearance of eggshells) [13].
Serology: Detecting the Host's Immune Response
Principles and Diagnostic Value
Serological techniques indirectly detect parasitic infections by measuring the host's humoral immune response (antibodies) or, increasingly, circulating parasite antigens [3] [11]. These methods are indispensable for diagnosing tissue-invasive parasites that are not readily found in stool or blood, such as Echinococcus spp. (hydatid disease) or Toxoplasma gondii [10] [1]. A significant advantage of antigen-detection tests is their ability to confirm active infection, whereas antibody tests can struggle to distinguish between past exposure and current, active disease [9] [10]. Furthermore, cross-reactivity between antigens from related parasite species can sometimes reduce test specificity [9]. Despite these challenges, the high throughput and automation potential of serological assays like ELISA make them a mainstay in clinical laboratories.
Key Methodologies and Workflows
Serodiagnostics have evolved from early complement fixation tests to modern, highly automated immunoassays.
- Enzyme-Linked Immunosorbent Assay (ELISA): This workhorse technique can be configured to detect either antibodies or antigens. It involves immobilizing a capture molecule (antigen for antibody detection, or antibody for antigen detection) on a solid phase. An enzyme-conjugated secondary antibody produces a colorimetric signal proportional to the target's concentration [11] [10]. Variations like the Falcon Assay Screening Test (FAST-ELISA) and Dot-ELISA offer rapid, simpler alternatives [10].
- Immunofluorescence Assay (IFA): Often considered a gold standard in serology, IFA uses fixed whole parasites or antigen substrates on a slide. The patient's serum is applied, and any bound antibody is detected with a fluorochrome-labeled anti-human immunoglobulin, visualized under a fluorescence microscope [10].
- Rapid Diagnostic Tests (RDTs): These are lateral flow immunochromatographic assays that provide results in minutes, making them ideal for point-of-care settings. They are widely used for detecting malaria antigens (Plasmodium histidine-rich protein 2, aldolase) or other parasitic antigens [15] [10].
The decision pathway for employing serological methods is outlined below:
Experimental Protocol: Indirect ELISA for Antibody Detection
Objective: To detect parasite-specific IgG antibodies in a human serum sample.
Materials:
- Microtiter plate coated with purified parasite antigen
- Test and control human serum samples
- Blocking buffer (e.g., PBS with 1% BSA or 5% skim milk)
- Wash buffer (PBS with 0.05% Tween 20)
- Enzyme-conjugated secondary antibody (e.g., Horseradish Peroxidase-anti-human IgG)
- Substrate solution (e.g., TMB/Hâ‚‚Oâ‚‚)
- Stop solution (e.g., 1M Hâ‚‚SOâ‚„)
- ELISA plate reader
Procedure:
- Blocking: Add blocking buffer to the antigen-coated wells and incubate (e.g., 1 hour at 37°C) to prevent nonspecific binding. Wash the plate three times with wash buffer.
- Primary Antibody Incubation: Add diluted test and control sera to the wells. Incubate (e.g., 1 hour at 37°C). Wash thoroughly.
- Secondary Antibody Incubation: Add the enzyme-conjugated anti-human IgG at the recommended dilution. Incubate (e.g., 1 hour at 37°C). Wash thoroughly.
- Detection: Add substrate solution to each well. Incubate in the dark for a fixed time (e.g., 15-30 minutes) until color develops.
- Stop Reaction and Read: Add stop solution to terminate the enzyme reaction. Immediately read the absorbance at the appropriate wavelength (e.g., 450 nm for TMB) using a plate reader.
Interpretation: A sample's optical density (OD) is compared to the cutoff value (often determined from negative controls). An OD above the cutoff indicates the presence of specific antibodies [11] [13].
Culture: Isolating the Pathogen
Principles and Applications in Parasitology
While culture is a cornerstone of bacteriology and mycology, its application in diagnostic parasitology is more limited but remains crucial for specific protozoan infections. The principle involves providing the necessary nutrients, temperature, and atmospheric conditions to support the growth and multiplication of parasites in vitro [11]. Culture is highly sensitive for certain parasites like Entamoeba histolytica and Leishmania spp., and it provides a source of organisms for further analysis, such as isoenzyme typing (zymodeme analysis) or drug sensitivity testing [10] [1]. However, culture methods are not available for most helminths, are often labor-intensive, require specialized media, and can take days to weeks to yield results, limiting their routine use [11].
Key Methodologies
- Xenic Culture: This method cultivates the parasite in the presence of an unknown consortium of other microorganisms. Robinson's medium, for example, is used for the xenic culture of Entamoeba histolytica from stool samples.
- Axic Culture: This involves cultivating the parasite in a sterile environment without any other living organisms. This is the standard for Leishmania and Trypanosoma cultures, often using media like NNN (Novy-MacNeal-Nicolle) medium or Schneider's Insect Medium, supplemented with fetal bovine serum.
- Cell Culture: Some parasites, such as Toxoplasma gondii, are efficiently cultivated in mammalian cell monolayers (e.g., human foreskin fibroblasts), which act as a host cell for the intracellular parasite.
Comparative Analysis of Conventional Techniques
The following tables summarize the key characteristics, advantages, and limitations of each conventional technique, along with common specimen requirements.
Table 1: Comparison of Conventional Diagnostic Techniques
| Technique | Principle | Key Advantage | Primary Limitation | Ideal Use Case |
|---|---|---|---|---|
| Microscopy | Direct morphological identification | Low cost; gold standard for many parasites; quantitative | Low sensitivity in light infections; requires expertise | Routine screening for intestinal/blood parasites [3] [13] |
| Serology | Detection of host antibodies or parasite antigens | High throughput; automatable; good for tissue parasites | Cannot always distinguish active from past infection (antibody tests) | Diagnosing invasive disease (e.g., echinococcosis, toxoplasmosis) [10] [1] |
| Culture | In vitro propagation of parasite | High sensitivity for some protozoa; provides isolate for further study | Not available for most parasites; slow; technically demanding | Confirmation & typing of Entamoeba histolytica, Leishmania [10] [1] |
Table 2: Specimen and Method Selection for Common Parasites
| Parasite | Disease | Primary Specimen(s) | Gold Standard/Common Conventional Method |
|---|---|---|---|
| Plasmodium spp. | Malaria | Blood | Microscopy (Giemsa-stained thick & thin smears) [10] |
| Entamoeba histolytica | Amoebiasis | Stool, Liver abscess aspirate | Microscopy (wet mount, stained smears); Culture [13] |
| Giardia lamblia | Giardiasis | Stool, Duodenal contents | Microscopy (wet mount, concentration) [3] [12] |
| Leishmania spp. | Leishmaniasis | Tissue aspirate, Bone marrow | Microscopy (smears); Culture (NNN medium) [10] |
| Echinococcus spp. | Hydatidosis | Serum, Cyst fluid | Serology (ELISA, Immunoblot) [10] |
| Strongyloides stercoralis | Strongyloidiasis | Stool, Serum | Microscopy (larvae identification); Serology (ELISA) [10] [1] |
The Research Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Conventional Parasitology
| Reagent/Material | Function | Application Example |
|---|---|---|
| Giemsa Stain | Stains nuclei (purple) and cytoplasm (blue) of parasites | Differentiation of Plasmodium species in blood smears [10] |
| Formalin (10%) | Preservative; fixes parasites; disinfects | Preservation of stool samples for concentration techniques [13] |
| ELISA Kits (Antigen/Antibody) | High-throughput detection of immune response or parasite markers | Seroprevalence studies; diagnosis of toxoplasmosis, cysticercosis [10] [13] |
| Culture Media (e.g., NNN, Robinson's) | Supports in vitro growth and propagation of parasites | Isolation and maintenance of Leishmania or Entamoeba strains [10] |
| Fluorochrome-Lagged Antibodies | Binds to primary antibody for visual detection | Confirmatory testing in Immunofluorescence Assays (IFA) [10] |
| 5-Chloro-AB-PINACA | 5-Chloro-AB-PINACA|CAS 1801552-02-2|Research Chemical | 5-Chloro-AB-PINACA is a synthetic cannabinoid receptor agonist (SCRA) for pharmacological research only. Not for human or veterinary use. Buy now for your studies. |
| 9-Norketo FK-506 | 9-Norketo FK-506, CAS:123719-19-7, MF:C₄₃H₆₉NO₁₁, MW:776.01 | Chemical Reagent |
Microscopy, serology, and culture have collectively formed the unshakeable foundation of diagnostic parasitology. While the field is rapidly advancing with the integration of molecular diagnostics and artificial intelligence [9] [14], these conventional techniques retain their status as historical gold standards. They continue to be vital for routine diagnosis, epidemiological surveillance, and primary research, especially in regions where parasitic diseases are endemic. A comprehensive diagnostic strategy often involves a synergistic approach, leveraging the strengths of these traditional methods while acknowledging their limitations. For researchers and drug development professionals, a firm grasp of these core techniques is essential for designing robust experiments, validating new diagnostics, and ultimately contributing to the global effort to control and eliminate parasitic diseases.
Parasitic diseases present a profound and persistent global health challenge, affecting hundreds of millions of people worldwide and imposing significant economic burdens, particularly in developing regions [7] [16]. The World Health Organization estimates that nearly one-quarter of the world's population is affected by parasitic infections, with soil-transmitted helminths alone infecting approximately 1 billion people [9] [17]. These infections result in devastating health consequences including malnutrition, anemia, impaired cognitive and physical development in children, and increased susceptibility to other diseases [9]. In the face of this substantial disease burden, accurate and timely diagnosis represents the critical first step toward effective treatment, control, and potential eradication of these complex pathogens.
The diagnostic landscape for parasitic infections has evolved significantly over centuries, yet fundamental limitations continue to hamper effective disease management [9]. Traditional techniques including microscopy, serological assays, histopathology, and culturing have formed the diagnostic backbone for decades [7]. While these methods have provided invaluable service in parasite identification, they suffer from three interconnected critical limitations that undermine their effectiveness: excessive time consumption, profound dependency on specialized expertise, and inadequate sensitivity and specificity [7] [12] [17]. These limitations become particularly problematic in resource-limited settings where parasitic diseases are most prevalent, creating a diagnostic paradox where the regions most burdened by these infections have the least access to reliable diagnostic capabilities [7] [8].
This technical analysis examines the core limitations of conventional parasitic diagnostic methodologies within the broader context of definitive diagnosis research. By quantifying these constraints through experimental data and exploring emerging technological solutions, we provide a comprehensive framework for researchers and drug development professionals to advance the next generation of diagnostic platforms for parasitic diseases.
Quantitative Analysis of Conventional Diagnostic Limitations
The performance constraints of traditional diagnostic methods can be precisely quantified through experimental data and clinical studies. The following analysis examines the specific limitations related to time efficiency, expertise dependency, and analytical sensitivity/specificity across major diagnostic platforms.
Table 1: Performance Limitations of Conventional Parasite Diagnostic Methods
| Diagnostic Method | Time Requirement | Expertise Dependency | Reported Sensitivity | Key Limitations |
|---|---|---|---|---|
| Kato-Katz Microscopy | 15-30 minutes/sample [17] | High (parasitology expertise required) [12] | 50-62% (1 sample, S. mansoni); 75-85% (hookworm, 3 samples) [17] | Low sensitivity for light infections, day-to-day egg output variation [17] |
| Wet Mount Microscopy | 20-40 minutes/sample [18] | High (morphological differentiation skills) [14] [12] | 89.5% (compared to reference) [18] | Observer-dependent, limited by parasite load [18] |
| Rapid Diagnostic Tests (RDTs) | 10-20 minutes [7] | Low to moderate | Variable; cross-reactivity issues [9] | Limited antigen targets, inability to distinguish active infection [12] |
| ELISA/Serology | 2-4 hours (batch processing) [14] | Moderate (technical training required) | Limited by cross-reactivity [9] | Cannot distinguish past vs. current infection [9] |
Table 2: Impact of Repeated Sampling on Diagnostic Sensitivity
| Number of Stool Samples | S. mansoni Sensitivity (%) | Hookworm Sensitivity (%) |
|---|---|---|
| 1 sample | 50-62% [17] | ~50% [17] |
| 2 samples | ~80% [17] | ~75% [17] |
| 3 samples | Not reported | ~85% [17] |
| 4 samples | Not reported | ~95% [17] |
The data reveal several critical patterns. First, microscopy-based methods exhibit significant time investments per sample, creating processing bottlenecks in high-volume settings [18]. Second, the sensitivity of the widely-used Kato-Katz technique shows strong dependence on both parasite species and sampling effort, with hookworm diagnosis requiring up to four samples to achieve >90% sensitivity [17]. This sampling burden directly impacts time efficiency and compliance in field studies and clinical trials. Third, the expertise requirement for morphological identification remains a substantial barrier to reliable diagnosis, particularly in non-endemic regions where technologist proficiency may be limited [12].
Experimental Protocols for Assessing Diagnostic Limitations
Kato-Katz Sensitivity Quantification Protocol
The Kato-Katz technique represents the gold standard for soil-transmitted helminth diagnosis in epidemiological studies, yet its limitations must be systematically quantified for proper interpretation of results [17].
Materials:
- Kato-Katz templates (40-50 mg)
- Cellophane strips soaked in glycerol-malachite green
- Microscope slides
- Light microscope
Procedure:
- Place approximately 100mg of sieved stool sample on the template
- Transfer sample to microscope slide using template
- Cover with glycerol-soaked cellophane strip
- Press gently to create uniform smear
- Allow 30-60 minutes for clearing before examination
- Examine entire smear under microscope at 100x magnification
- Count eggs for each helminth species separately
- Calculate eggs per gram (EPG) using conversion factor based on template volume
Sensitivity Analysis:
- Collect multiple samples over consecutive days (minimum 2, ideally 3-4)
- Apply zero-inflated negative binomial statistical model to account for false negatives
- Calculate sensitivity as function of infection intensity: Sensitivity = 1 - (1 - p)â¿ where p is probability of detection per sample and n is number of samples [17]
Limitations:
- Sensitivity drops significantly at low infection intensities (<100 EPG)
- Day-to-day variation in egg output affects reproducibility
- Species-dependent clearance rates affect visibility
Automated Microscopy Validation Protocol
Automated microscopy systems like SediMAX2 offer potential solutions to expertise dependency in conventional microscopy [18].
Materials:
- SediMAX2 automated microscopy system
- SAF (sodium acetate-acetic acid-formalin) fixative
- Disposable cuvettes
- Centrifuge
Procedure:
- Fix stool samples in SAF fixative
- Concentrate by centrifugation at 500g for 5 minutes
- Dilute sediment with saline solution (1:20)
- Load 20μl into SediMAX2 disposable cuvettes
- System automatically centrifuges, acquires, and stores 60 high-definition images per sample
- Review stored images for parasitic structures
- Compare results with conventional wet mount examination
Validation Metrics:
- Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV)
- Determine kappa coefficient for inter-method agreement
- Assess time reduction compared to conventional microscopy
Performance Data:
- Reported sensitivity: 89.51%
- Reported specificity: 98.15%
- PPV: 99.22%
- NPV: 77.94%
- Kappa: 0.81 (almost perfect agreement) [18]
Emerging Solutions and Technological Frameworks
Next-generation diagnostic platforms aim to address the critical limitations of conventional methods through technological innovation. The following frameworks visualize the evolving diagnostic landscape and its relationship to the identified constraints.
Diagram 1: Diagnostic evolution addressing core limitations
Diagram 2: Nanobiosensor architecture for parasitic detection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Advanced Parasite Diagnosis
| Reagent Category | Specific Examples | Research Application | Performance Characteristics |
|---|---|---|---|
| Nanomaterials | Gold nanoparticles (AuNPs), Quantum dots (QDs), Carbon nanotubes (CNTs), Graphene oxide (GO) [14] | Signal amplification in biosensors | AuNPs for PfHRP2 detection; QDs for DNA probe labeling; CNTs functionalized with antibodies [14] |
| CRISPR Components | Cas proteins, gRNA, Reporter molecules [7] [8] | Nucleic acid detection | High specificity for parasite DNA/RNA; portable detection systems [8] |
| Molecular Assay Components | Primers, Probes, Isothermal amplification reagents [7] [8] | PCR, LAMP, multiplex assays | Enhanced sensitivity over microscopy; species differentiation [9] [8] |
| Immunological Reagents | Recombinant antigens, Monoclonal antibodies, ELISA kits [12] | Serodiagnosis, antigen detection | Limited by cross-reactivity; unable to distinguish active infection [9] [12] |
| Automated Imaging Consumables | SediMAX2 cuvettes, SAF fixative [18] | Automated microscopy | 89.5% sensitivity, 98.2% specificity vs. conventional microscopy [18] |
| α-Ergocryptine-d3 | α-Ergocryptine-d3|Deuterated Ergot Alkaloid|CAS 1794783-50-8 | α-Ergocryptine-d3 is a deuterated stable isotope-labeled ergot alkaloid. It serves as a critical internal standard for precise bioanalytical research. This product is for Research Use Only (RUO). Not for human or veterinary use. | Bench Chemicals |
| C.I. Acid Yellow 232 | C.I. Acid Yellow 232 | High-purity C.I. Acid Yellow 232 for industrial research. A metal complex dye for wool, leather, and nylon. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
The critical limitations of time consumption, expertise dependency, and inadequate sensitivity/specificity in parasitic disease diagnosis represent both a formidable challenge and a catalyst for innovation. Quantitative analysis reveals that conventional methods suffer from fundamental constraints that impact their utility in both clinical and research settings, particularly in resource-limited regions where parasitic diseases are most prevalent [17] [18]. The experimental protocols detailed herein provide frameworks for systematically evaluating these limitations and validating potential solutions.
Emerging technological platforms including nanobiosensors, CRISPR-based detection systems, automated microscopy, and AI-assisted diagnosis offer promising pathways to overcome these diagnostic constraints [7] [14] [8]. These platforms leverage advances in nanotechnology, molecular biology, and computational analytics to deliver rapid, sensitive, and operator-independent diagnostic capabilities [14] [9]. The research reagent toolkit provides essential components for developing and implementing these next-generation solutions.
For researchers and drug development professionals, addressing these diagnostic limitations is paramount for advancing both therapeutic interventions and eradication campaigns. Improved diagnostics enable more accurate patient stratification, therapeutic monitoring, and epidemiological surveillance—all critical components of comprehensive parasitic disease control strategies. By integrating the technological frameworks and experimental approaches outlined in this analysis, the scientific community can accelerate progress toward definitive diagnosis and effective management of parasitic diseases globally.
The Urgent Need for Innovation in Endemic and Resource-Limited Settings
Parasitic infections pose a critical global health challenge, disproportionately affecting nearly a quarter of the world's population in tropical and subtropical regions [9]. These diseases, including malaria, schistosomiasis, and leishmaniasis, contribute significantly to the global burden of neglected tropical diseases (NTDs), with the World Health Organization identifying 13 of 20 NTDs as parasitic in origin [9]. The profound health impacts include malnutrition, anemia, impaired cognitive development in children, and increased susceptibility to other infectious diseases, thereby perpetuating cycles of poverty and hindering socioeconomic development in endemic regions [9]. In 2022 alone, malaria caused an estimated 249 million cases and over 600,000 deaths globally [14]. The economic burden is equally staggering, with India alone losing approximately $1.94 billion to malaria control in 2014, while visceral leishmaniasis drains 11% of annual household expenditures in affected areas of Bihar [9].
The accurate and timely diagnosis of parasitic infections is fundamental to treatment, control, and elimination efforts. Precise diagnosis enables targeted therapy, helps prevent the development of drug resistance, facilitates surveillance, and allows for monitoring treatment response [9]. However, endemic and resource-limited settings face profound challenges in diagnostic capacity, including limited access to laboratory infrastructure, technical expertise, and reliable electricity. These constraints are compounded by the complex life cycles of many parasites, which can involve multiple hosts and environmental reservoirs, creating additional complications for detection and control [9]. The emergence of drug resistance in parasites further intensifies the need for diagnostic methods that can guide appropriate treatment regimens [9]. This whitepaper examines the limitations of conventional diagnostic approaches and explores innovative technologies that promise to revolutionize parasitic disease management in the most vulnerable populations.
Limitations of Conventional Diagnostic Methods
Traditional diagnostic methods for parasitic infections have remained largely unchanged for decades and present significant limitations in both accuracy and practicality for resource-limited settings. These conventional approaches primarily include microscopic examination, serological assays, and basic molecular techniques, each with distinct constraints that affect their utility in endemic areas.
Microscopy and Serological Constraints
Microscopy, long considered the "gold standard" for parasitic diagnosis, requires expert operators for reliable results, as several parasite eggs and morphological forms can be difficult to distinguish visually [14]. The sensitivity of microscopy is highly dependent on parasite burden and technician skill, leading to potential misdiagnosis in low-intensity infections [14]. Serological assays such as enzyme-linked immunosorbent assay (ELISA), immunoblotting, and immunofluorescence assays (IFA) detect either parasite antigens or host antibodies [14]. While these methods offer better sensitivity than microscopy for some infections, they face substantial limitations including cross-reactivity between related parasite species, inability to distinguish between past exposure and active infection, and variable performance across different geographic regions due to parasite genetic diversity [9] [10]. Furthermore, these tests often cannot be used to monitor treatment response, as antibodies may persist long after successful parasite clearance [10].
Challenges in Resource-Limited Settings
The infrastructure requirements of conventional diagnostic methods present nearly insurmountable barriers in many endemic regions. Microscopy requires reliable electricity, high-quality microscopes, reagents, and trained personnel that may be unavailable in remote areas [8]. Similarly, standard ELISA procedures necessitate well-equipped laboratory environments with consistent power supply, refrigeration capabilities, and technical expertise [8]. The time-consuming nature of these methods, from sample preparation to result interpretation, creates additional bottlenecks in clinical settings with high patient volumes. Transportation of samples from remote collection sites to centralized laboratories introduces further delays in diagnosis and treatment initiation, compromising patient outcomes and impeding public health control efforts [19]. These limitations collectively underscore the critical need for innovative diagnostic solutions that maintain accuracy while overcoming the practical constraints of endemic settings.
Innovative Diagnostic Technologies
The evolving landscape of parasitic disease diagnostics includes several promising technological approaches that offer solutions to the limitations of conventional methods. These innovations span molecular, nanomaterial, and imaging-based platforms, each with distinct advantages for resource-limited settings.
Advanced Molecular Techniques
Molecular diagnostics have transformed parasitic disease detection through enhanced sensitivity and specificity. Digital PCR (dPCR) represents a significant advancement over quantitative real-time PCR (qPCR), offering absolute quantitation without requiring standard curves and demonstrating higher resilience to inhibitors present in stool samples [20]. dPCR has shown particular utility for malaria screening and schistosomiasis elimination programs due to its superior sensitivity in detecting low parasite densities [20]. Loop-mediated isothermal amplification (LAMP) provides an alternative nucleic acid amplification method that operates at constant temperatures, eliminating the need for thermal cyclers and making it suitable for field applications [10]. CRISPR-Cas systems have recently been adapted for parasitic diagnosis, leveraging the precision and programmability of these platforms to create highly specific and sensitive detection tools that can be deployed in point-of-care formats [8]. These systems can identify parasite-specific nucleic acid sequences with high specificity, offering rapid, portable, and cost-effective diagnostic solutions [8].
Nanotechnology and Biosensors
Nanobiosensors represent a revolutionary approach to parasitic detection, integrating nanotechnology with biological recognition elements to create highly sensitive diagnostic platforms [14]. These devices utilize various nanomaterials including gold nanoparticles, quantum dots, carbon nanotubes, and graphene oxide, each providing unique advantages for pathogen detection [14]. Nanobiosensors can detect parasite antigens, genetic material, or specific biomarkers like excretory-secretory products and microRNAs with exceptional sensitivity, often identifying targets at concentrations undetectable by conventional methods [14]. The detection mechanisms employed in these platforms include:
- Electrochemical nanobiosensors that measure electrical signal changes when parasitic antigens or DNA bind to nanoparticle surfaces [14]
- Optical nanobiosensors utilizing surface plasmon resonance (SPR) and fluorescence resonance energy transfer (FRET) to detect binding events through changes in optical properties [14]
- Magnetic nanobiosensors that employ magnetic nanoparticles to isolate and concentrate target molecules from complex clinical samples like blood [14]
These nanobiosensors offer rapid, accurate, and cost-effective results while enabling miniaturization and integration with point-of-care platforms [14].
Artificial Intelligence and Advanced Imaging
The integration of artificial intelligence (AI), particularly convolutional neural networks and deep learning algorithms, is revolutionizing parasitic diagnosis by enhancing the accuracy and efficiency of detection [9]. AI-based image recognition systems can automate the interpretation of microscopic images, reducing reliance on expert microscopists and increasing throughput [8]. These systems are being trained to identify various parasite life cycle stages in blood, stool, and tissue samples with accuracy comparable to or exceeding human experts [9]. Advanced imaging technologies combined with improved staining techniques further enhance visualization of parasitic elements, while portable imaging devices equipped with AI algorithms bring diagnostic capabilities directly to remote communities [8]. The integration of telemedicine platforms with these automated imaging systems creates additional opportunities for expert consultation and quality assurance in low-resource settings.
Table 1: Performance Comparison of Diagnostic Technologies for Parasitic Infections
| Technology | Sensitivity | Specificity | Time to Result | Infrastructure Requirements | Cost |
|---|---|---|---|---|---|
| Microscopy | Low to Moderate | Moderate | 30-60 minutes | Microscope, trained technician | Low |
| ELISA | Moderate | Moderate to High | 2-4 hours | Plate reader, incubator | Moderate |
| Conventional PCR | High | High | 3-6 hours | Thermal cycler, electrophoresis | High |
| dPCR | Very High | Very High | 2-3 hours | dPCR platform, microfluidic chip | Very High |
| LAMP | High | High | 1-2 hours | Water bath/block heater | Moderate |
| Nanobiosensors | Very High | Very High | <30 minutes | Minimal (varies by type) | Low to Moderate |
| AI-Microscopy | Moderate to High | Moderate to High | <30 minutes | Microscope, computing device | Moderate |
Table 2: Nanobiosensor Applications for Major Parasitic Diseases
| Parasite | Disease | Nanomaterial | Target Biomarker | Detection Mechanism |
|---|---|---|---|---|
| Plasmodium spp. | Malaria | Gold nanoparticles (AuNPs) | PfHRP2 antigen | Electrochemical |
| Leishmania spp. | Leishmaniasis | Quantum dots (QDs) | kDNA | Fluorescence |
| Echinococcus granulosus | Cystic Echinococcosis | Carbon nanotubes (CNTs) | Anti-EgAgB antibodies | Immunosensor |
| Schistosoma spp. | Schistosomiasis | Graphene oxide (GO) | Soluble egg antigen (SEA) | Electrochemical |
| Taenia spp. | Taeniasis/Cysticercosis | Metallic nanoparticles | Parasite antigens | Optical |
Experimental Protocols and Methodologies
Digital PCR for Low-Parasite Density Detection
Principle: dPCR partitions a sample into thousands of nanoliter-sized reactions, with each partition containing zero or one target DNA molecule. After endpoint amplification, the fraction of positive partitions is counted to provide absolute quantification of the target without a standard curve [20].
Protocol for Malaria Detection:
- DNA Extraction: Use commercial kits (QIAamp DNA Blood Mini Kit) to extract DNA from 200μL whole blood. Include negative and positive controls.
- Reaction Mix Preparation: Prepare 20μL reactions containing 1X dPCR master mix, 900nM primers, 250nM probe targeting Plasmodium 18S rRNA gene, and 5μL template DNA.
- Partitioning: Load reaction mix into dPCR cartridge (Bio-Rad QX200 system) for droplet generation (approximately 20,000 droplets per sample).
- Amplification: Perform PCR cycling: 95°C for 10min (enzyme activation), then 40 cycles of 94°C for 30s (denaturation) and 55°C for 60s (annealing/extension).
- Reading and Analysis: Transfer plate to droplet reader, which counts positive and negative droplets for each sample. Calculate parasite concentration using the formula: Copies/μL = -ln(1-p)*V, where p=fraction of positive partitions and V=partition volume [20].
Troubleshooting: Inhibitor-resistant polymerases are recommended for stool samples. DNA load optimization (1-10ng/μL) is critical to avoid saturation [20].
Gold Nanoparticle-Based Immunosensor for Malaria Antigen Detection
Principle: This lateral flow assay utilizes AuNPs conjugated with antibodies against Plasmodium falciparum histidine-rich protein 2 (PfHRP2). Antigen presence causes accumulation of AuNPs at test line, producing a visible color change [14].
Protocol:
- AuNP Synthesis and Functionalization:
- Prepare 15nm AuNPs by reducing tetrachloroauric acid with trisodium citrate.
- Adjust AuNP solution to pH 8.5 with K₂CO₃.
- Add anti-PfHRP2 monoclonal antibodies (10μg/mL final concentration) and incubate 1h at room temperature.
- Block with 1% BSA for 30min to prevent non-specific binding.
- Centrifuge at 12,000g for 15min to remove excess antibody and resuspend in storage buffer.
Lateral Flow Strip Assembly:
- Apply conjugated AuNPs to glass fiber pad (conjugate pad).
- Spray capture antibody (different anti-PfHRP2 clone) and control antibody on nitrocellulose membrane as test and control lines, respectively.
- Assemble components (sample pad, conjugate pad, membrane, absorbent pad) on backing card and cut into 4mm strips.
Testing Procedure:
- Add 100μL whole blood or serum to sample well.
- Allow migration for 15min.
- Visual interpretation: both control and test lines visible = positive; only control line visible = negative [14].
Quality Control: Include known positive and negative controls with each batch. Control line must always appear for valid test.
Diagram 1: Malaria Nanosensor Workflow. The lateral flow strip components and result interpretation for PfHRP2 detection.
CRISPR-Cas Based Detection of Parasitic DNA
Principle: Cas12a or Cas13 enzymes complexed with guide RNAs specific to parasite DNA or RNA exhibit collateral nuclease activity upon target recognition, cleaving reporter molecules to generate fluorescence [8].
Protocol for Trypanosoma cruzi Detection:
- Nucleic Acid Extraction: Use boil-and-spin method (10μL blood boiled 10min, centrifuged 2min at 10,000g) or commercial kits for DNA extraction.
- RPA Pre-amplification: Prepare 50μL recombinase polymerase amplification (RPA) reaction with:
- 29.5μL rehydration buffer
- 5μL template DNA
- 420nM forward and reverse primers targeting T. cruzi repetitive sequence
- 14mM magnesium acetate
- Incubate 15-20min at 39°C
- CRISPR Detection:
- Prepare 20μL reaction containing:
- 1X Cas12 buffer
- 50nM LbCas12a enzyme
- 60nM gRNA (specific to amplified T. cruzi sequence)
- 500nM fluorescent reporter (ssDNA with 5'-FAM, 3'-BHQ)
- 5μL RPA product
- Incubate 15-30min at 37°C
- Visualize with UV light or portable fluorometer [8]
- Prepare 20μL reaction containing:
Interpretation: Fluorescence indicates positive detection. Include no-template and negative sample controls.
Diagram 2: CRISPR-Cas Parasite Detection. The workflow from sample preparation to signal generation through collateral cleavage activity.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Advanced Parasitic Diagnostics Development
| Reagent/Material | Function | Example Applications | Technical Considerations |
|---|---|---|---|
| Gold Nanoparticles (15-40nm) | Signal generation in lateral flow assays; plasmonic sensing | Malaria (PfHRP2 detection), Leishmania antigen detection | Size affects color intensity; must be conjugated with specific antibodies [14] |
| Quantum Dots (CdSe/ZnS) | Fluorescent labels for biosensors | Leishmania DNA detection, parasite imaging | High quantum yield; size-tunable emission; potential cytotoxicity concerns [14] |
| CRISPR-Cas Enzymes (Cas12a, Cas13) | Nucleic acid detection through collateral cleavage | Trypanosoma cruzi, Plasmodium species detection | Requires specific PAM sequences; gRNA design critical for specificity [8] |
| Recombinase Polymerase Amplification (RPA) Kits | Isothermal nucleic acid amplification | Field-based parasite DNA/RNA detection | Works at 37-42°C; faster than PCR; sensitive to inhibitor interference [8] |
| Magnetic Nanoparticles (Fe₃O₄) | Sample preparation; target concentration | Parasite DNA extraction from blood/stool; antigen capture | Surface functionalization with silanes/carboxyl groups for antibody binding [14] |
| Screen-Printed Electrodes | Electrochemical sensing platforms | Multiplex parasite detection; biomarker quantification | Carbon, gold, or platinum surfaces; enable miniaturization of diagnostic devices [14] |
| Monoclonal Antibodies (Parasite-Specific) | Capture and detection agents | ELISA, lateral flow assays, immunosensors | Must be validated for cross-reactivity; critical for test specificity [10] |
| 2-(Vinyloxy)ethanol | 2-(Vinyloxy)ethanol, CAS:764-48-7, MF:C4H8O2, MW:88.11 g/mol | Chemical Reagent | Bench Chemicals |
| Siderochelin C | Siderochelin C|CAS 93973-61-6|RUO | Siderochelin C is a ferrous-ion chelating siderophore for iron metabolism research. For Research Use Only. Not for human or diagnostic use. | Bench Chemicals |
Implementation Challenges and Future Directions
The translation of innovative diagnostic technologies from research laboratories to field implementation in endemic settings faces several significant challenges that must be addressed to realize their full potential.
Technical and Infrastructural Hurdles
Nanobiosensor mass production requires standardization and quality control measures that are currently lacking, with batch-to-batch variation in nanomaterial synthesis posing a particular challenge [14]. The interference from biological matrices (hemoglobin in blood, bilirubin in stool) can affect assay performance and must be mitigated through robust sample processing methods [14]. The development of multiplex detection capabilities for co-infections (e.g., malaria and schistosomiasis) presents technical challenges in assay design and signal discrimination but is essential for comprehensive patient care in endemic areas [14]. Device stability under tropical conditions of high temperature and humidity represents another critical consideration, requiring specialized packaging and reagent formulations to maintain performance throughout supply chains and storage [19].
Accessibility and Integration Pathways
The World Health Organization has established the Diagnostics Technical Advisory Group (DTAG) for neglected tropical diseases to address priority areas in diagnostic development and identify gaps in access to available tools [19]. Target Product Profiles (TPPs) developed by WHO outline the desired characteristics of diagnostics for specific diseases, guiding research and development toward practical field applications [19]. Successful integration of new technologies requires:
- Development of sample-to-answer systems that minimize manual processing steps
- Connectivity solutions for result reporting and surveillance in low-infrastructure settings
- Local training programs for device operation and maintenance
- Sustainable supply chains for reagents and consumables
- Implementation of quality assurance systems to maintain testing accuracy [19]
Future development priorities include the creation of multiplex nanobiosensors using polymer nanofibers or hybrid nanoparticles for simultaneous detection of multiple pathogens, along with integration of lab-on-a-chip technology for true point-of-care testing [14]. The combination of AI-assisted image analysis with portable imaging devices presents another promising direction for increasing accessibility to expert-level diagnostic capabilities in remote settings [9]. Multi-omics approaches integrating genomic, proteomic, and metabolomic data offer potential for discovering novel biomarkers that could further enhance the sensitivity and specificity of next-generation diagnostic platforms [8]. Through coordinated efforts between researchers, product developers, endemic country health systems, and global health organizations, these innovative diagnostic technologies can transform the management and control of parasitic diseases in the world's most vulnerable populations.
Next-Generation Diagnostic Technologies: Principles and Workflows for Modern Laboratories
The definitive diagnosis of parasitic diseases represents a critical frontier in medical research and public health. Traditional diagnostic methods, such as microscopy and serology, are often hampered by limitations in sensitivity and specificity, particularly in cases of low-level or cryptic infections. The emergence of molecular assays has fundamentally transformed this landscape, providing researchers and clinicians with powerful tools for precise pathogen detection and identification. These nucleic acid-based technologies, including Polymerase Chain Reaction (PCR), Real-Time PCR (also known as quantitative PCR or qPCR), and Next-Generation Sequencing (NGS), enable the direct detection of parasitic DNA or RNA with unparalleled accuracy. Their integration into parasitology research has not only accelerated the pace of discovery but also refined our understanding of parasite biology, epidemiology, and host-pathogen interactions, thereby forming the cornerstone of modern diagnostic and drug development pipelines.
Within the context of a broader thesis on definitive diagnosis, molecular assays provide the foundational data required for understanding disease dynamics, tracking resistance patterns, and validating therapeutic targets. This technical guide delves into the principles, methodologies, and applications of these core technologies, providing researchers and drug development professionals with a comprehensive framework for their implementation in parasitic disease research.
Fundamental Principles and Evolution
The evolution of molecular diagnostics in parasitology has progressed from simple amplification to sophisticated quantification and massive parallel sequencing. Polymerase Chain Reaction (PCR) serves as the foundational technique, enabling the exponential in vitro amplification of specific target DNA sequences from minute starting quantities. This process, catalyzed by a thermostable DNA polymerase, allows for the detection of parasite DNA even in early or low-parasite-burden infections [21].
Building upon this, Real-Time PCR (qPCR) incorporates fluorescent detection systems to monitor the accumulation of amplification products in real time during each cycle of the PCR. This innovation transforms PCR from a qualitative tool into a robust quantitative assay. The key quantitative parameter is the Ct (threshold cycle) value, which is the cycle number at which the fluorescent signal exceeds a background threshold. A lower Ct value correlates directly with a higher starting concentration of the target nucleic acid [22] [23]. Two primary chemistries are employed for detection in qPCR:
- TaqMan Probes (Hydrolysis Probes): These are sequence-specific oligonucleotides labeled with a fluorescent reporter dye at the 5' end and a quencher at the 3' end. When intact, the quencher suppresses the reporter's fluorescence. During amplification, the 5'→3' exonuclease activity of the DNA polymerase cleaves the probe, separating the reporter from the quencher and generating a fluorescent signal proportional to the amount of amplicon synthesized [22] [24].
- SYBR Green I Dye: This is an inexpensive intercalating dye that fluoresces brightly when bound to double-stranded DNA (dsDNA). While cost-effective, it binds non-specifically to any dsDNA, including non-specific products and primer-dimers, necessitating careful assay optimization and post-amplification melt curve analysis to verify reaction specificity [22] [24].
The most transformative advancement has been Next-Generation Sequencing (NGS), also known as Massively Parallel Sequencing. Unlike PCR-based methods that interroga te predefined targets, NGS enables unbiased, high-throughput sequencing of millions to billions of DNA fragments simultaneously [25] [21]. This hypothesis-free approach allows for comprehensive pathogen detection, discovery of novel parasites, and detailed investigation of parasite population genetics and resistance markers without prior knowledge of the sequences present [26] [27].
Quantitative and Performance Comparison
The following tables provide a consolidated summary of the technical capabilities and performance characteristics of these molecular assays, based on current research and application data.
Table 1: Comparative overview of core molecular technologies for parasite identification
| Feature | PCR + Sanger Sequencing | Quantitative PCR (qPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Primary Function | Target amplification & sequence confirmation | Quantitative nucleic acid detection | Massive parallel sequencing & discovery |
| Quantitative Output | No | Yes (Relative quantification) | Yes (Read counts for relative quant.) |
| Sequence Discovery | Limited (single target) | No | Yes (unbiased) |
| Multiplexing Capacity | 1 target per reaction | 1 to 5 targets per reaction [23] | 1 to >10,000 targets [23] |
| Typical Turnaround Time | ~1-3 hours (PCR) + ~8 hours (Sequencing) [23] | 1 - 3 hours [23] | Several hours to days [23] |
| Sensitivity | Low-frequency mutation detection limited to ~5% [21] | High; can detect low parasitemia [28] | Very high; can detect low-abundance pathogens [27] |
| Key Applications | Variant analysis, CRISPR editing confirmation, species ID | Gene expression, pathogen load monitoring, drug efficacy studies | Pathogen discovery, strain typing, resistance marker screening, metagenomics |
Table 2: Performance of diagnostic methods in a malaria case study (Northwest Ethiopia, 2025) Data derived from a comparative study using multiplex qPCR as a reference standard on peripheral and placental blood samples [28].
| Diagnostic Method | Sensitivity (Peripheral Blood) | Specificity (Peripheral Blood) | Sensitivity (Placental Blood) | Specificity (Placental Blood) |
|---|---|---|---|---|
| Microscopy | 73.8% | 100% | 62.2% | 100% |
| Rapid Diagnostic Test (RDT) | 67.6% | 96.5% | 62.2% | 98.8% |
| Multiplex qPCR (Reference) | 100% | 94.8% | 100% | 94.8% |
This study highlights a critical challenge in parasitology: the significant proportion of submicroscopic infections that are missed by conventional methods but detected by molecular tools like qPCR. These subpatent infections can cause adverse clinical outcomes, underscoring the importance of sensitive molecular diagnostics for definitive diagnosis [28]. The study also demonstrated that a pooled testing strategy with multiplex qPCR obviated about half the reactions and associated costs, presenting a resource-efficient strategy for epidemiological surveillance [28].
Experimental Protocols for Parasite Identification
Protocol 1: Multiplex Real-Time PCR for Plasmodium Detection
This detailed protocol is adapted from a recent comparative study conducted in northwest Ethiopia, which validated the superior performance of multiplex qPCR for detecting malaria parasites in pregnant women [28].
1. Sample Collection and DNA Extraction:
- Collect peripheral blood samples (e.g., 200 µL) in EDTA tubes. For placental malaria studies, collect placental blood samples post-delivery.
- Extract genomic DNA from all samples using a commercial DNA extraction kit. Ensure that extraction includes negative control (nuclease-free water) and positive control (DNA from a known Plasmodium-positive sample) to monitor extraction efficiency and potential contamination.
2. Multiplex qPCR Reaction Setup:
- The multiplex assay targets genus-specific sequences for Plasmodium and may include species-specific targets (e.g., P. falciparum, P. vivax).
- Reaction Mix (20-25 µL total volume):
- 1X TaqMan Universal PCR Master Mix (contains DNA polymerase, dNTPs, and optimized buffer).
- Forward and Reverse Primers (each at a final concentration of 200-500 nM). Primer sequences are designed to target conserved regions within the Plasmodium genome.
- TaqMan Hydrolysis Probes: Use probes for different targets (e.g., Plasmodium genus, P. falciparum) labeled with distinct reporter dyes (e.g., FAM, VIC) at the 5' end and a non-fluorescent quencher (NFQ) with a minor groove binder (MGB) at the 3' end. Probes are typically used at 100-200 nM final concentration.
- 2-5 µL of template DNA.
- Adjust to final volume with nuclease-free water.
3. qPCR Amplification and Data Acquisition:
- Perform amplification on a real-time PCR instrument with the following typical cycling conditions:
- Initial Denaturation: 95°C for 10 minutes (to activate the hot-start polymerase).
- 45-50 Cycles of:
- Denaturation: 95°C for 15 seconds.
- Annealing/Extension: 60°C for 1 minute (fluorescence data collection at this step).
- The instrument's software will collect fluorescence data for each dye channel at every cycle.
4. Data Analysis and Interpretation:
- Set the fluorescence threshold in the exponential phase of the amplification plot above the baseline noise. The software will automatically assign a Ct value to each reaction.
- A sample is considered positive for a specific target if its Ct value is less than a predetermined cut-off (e.g., Ct < 40) and shows a characteristic sigmoidal amplification curve. Negative controls should have no amplification (Ct undetermined). The use of a multiplex format allows for the simultaneous differentiation of Plasmodium species in a single reaction [28].
Protocol 2: Targeted Next-Generation Sequencing for Parasite Metagenomics
This protocol outlines a targeted NGS approach for the identification and characterization of parasites from clinical samples, which is particularly useful for detecting mixed infections and unknown pathogens [26] [27].
1. Library Preparation:
- Nucleic Acid Extraction: Extract total nucleic acid (DNA and RNA) from the sample (e.g., blood, stool, tissue). For RNA viruses, include a reverse transcription step to generate cDNA.
- Library Construction: Prepare sequencing libraries by fragmenting the extracted DNA/cDNA, followed by end-repair, A-tailing, and ligation of platform-specific adapter sequences containing unique molecular indices (barcodes) to allow for sample multiplexing. For comprehensive analysis, use a metagenomic approach without targeted enrichment. For deeper coverage of specific parasites, use hybridization capture with biotinylated RNA baits designed against a panel of parasite genomic regions, or employ a highly multiplexed PCR amplicon approach.
2. Cluster Generation and Sequencing:
- The adapter-ligated library is loaded onto a sequencing flow cell where each fragment is clonally amplified in situ through bridge amplification or exclusion amplification, forming clusters.
- Sequencing-by-Synthesis: Run the flow cell on the NGS platform (e.g., Illumina). The instrument sequentially adds fluorescently labeled, reversibly terminated nucleotides. As each nucleotide is incorporated into the growing DNA strand, its specific fluorescent signal is imaged, determining the sequence of each cluster base-by-base [25] [21].
3. Bioinformatic Analysis:
- Demultiplexing: Assign raw sequence data (in FASTQ format) to individual samples based on their unique barcodes.
- Quality Control and Trimming: Filter reads based on quality scores and remove adapter sequences.
- Taxonomic Classification: This is a critical step for parasite identification. Two primary strategies are employed:
- Reference-Based Alignment: Map the high-quality reads to a curated database of reference parasite genomes using aligners like BWA or Bowtie2.
- De Novo Assembly and Annotation: For novel pathogens or complex samples, assemble reads into longer contiguous sequences (contigs) without a reference genome using tools like SPAdes. These contigs are then compared against public databases (e.g., NCBI NR) using BLAST for identification.
- Reporting: Generate a report detailing the identified parasite species, their relative abundance based on read counts, and any detected markers of interest (e.g., drug resistance mutations).
Visualizing Workflows and Logical Relationships
Molecular Assay Selection Pathway
The following diagram illustrates a decision-making pathway for selecting the appropriate molecular assay based on research objectives, sample number, and target scope.
TaqMan qPCR Probe Detection Mechanism
This diagram details the molecular mechanism of the TaqMan probe hydrolysis assay, a cornerstone of specific target detection and quantification in qPCR.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of molecular assays for parasite identification relies on a suite of specialized reagents and materials. The following table catalogs key components essential for the experiments described in this guide.
Table 3: Essential research reagents and materials for molecular parasite identification
| Reagent/Material | Function/Description | Key Considerations |
|---|---|---|
| TaqMan Universal PCR Master Mix | A pre-mixed, optimized solution containing hot-start Taq DNA polymerase, dNTPs, MgClâ‚‚, and buffer for robust qPCR amplification [22]. | Provides reproducibility and convenience; essential for multiplex qPCR assays. |
| Sequence-Specific Primers | Synthetic oligonucleotides (typically 18-25 bases) designed to flank and hybridize to the target parasite DNA sequence for amplification. | Specificity is critical; design against conserved genomic regions of the target parasite. |
| TaqMan Hydrolysis Probes | Oligonucleotide probes labeled with a 5' reporter dye (e.g., FAM) and a 3' quencher/MGB. Specificity is conferred by the probe sequence [22] [24]. | MGB probes allow for shorter designs and better discrimination of single-base differences. |
| SYBR Green I Dye | A fluorescent dye that intercalates into double-stranded DNA, allowing for real-time monitoring of PCR product accumulation [22] [24]. | Cost-effective but requires post-amplification melt curve analysis to verify specificity. |
| DNA Library Prep Kit | A suite of enzymes and buffers for fragmenting DNA, repairing ends, adding 'A' tails, and ligating sequencing adapters for NGS. | Selection depends on the NGS platform (e.g., Illumina, PacBio) and application (e.g., WGS, RNA-Seq). |
| Hybridization Capture Baits | Biotinylated oligonucleotides (e.g., RNA baits) designed to enrich sequencing libraries for genomic regions of specific parasites prior to NGS. | Enables targeted sequencing, increasing coverage and cost-effectiveness for defined parasite panels. |
| NGS Flow Cell | The glass slide containing nanoscale wells where clonal amplification and sequencing-by-synthesis occur [25]. | The physical substrate for massively parallel sequencing; capacity varies by instrument model. |
| Dibutyrin | Dibutyrin, CAS:32648-01-4, MF:C11H20O5, MW:232.27 g/mol | Chemical Reagent |
| Fast Yellow AB | Fast Yellow AB, CAS:2706-28-7, MF:C12H11N3NaO6S2, MW:380.4 g/mol | Chemical Reagent |
Molecular assays have irrevocably shifted the paradigm for the definitive diagnosis of parasitic diseases. The technologies of PCR, qPCR, and NGS offer a complementary and powerful arsenal, each with distinct strengths that make them suitable for specific research scenarios. The choice between them is not a matter of superiority but of strategic alignment with the research objective: qPCR for rapid, sensitive quantification of known targets; NGS for unbiased discovery, comprehensive profiling, and handling high target multiplicity; and Sanger sequencing for focused, cost-effective sequence confirmation of limited targets.
As the field advances, the integration of these core technologies with emerging methods like crispr-based diagnostics, digital PCR (dPCR) for absolute quantification, and long-read sequencing for resolving complex genomic regions promises even greater resolution [26] [23]. For researchers and drug development professionals, this evolving molecular toolkit is indispensable for driving forward our understanding of parasitology, enhancing disease surveillance, validating new drug targets, and ultimately achieving the goal of precise and definitive diagnosis.
Loop-mediated isothermal amplification (LAMP) has emerged as a transformative molecular diagnostic technology, particularly for the definitive diagnosis of parasitic diseases in resource-limited settings. LAMP is a nucleic acid amplification technique that operates under isothermal conditions, typically between 60-65°C, eliminating the need for sophisticated thermal cyclers required by conventional polymerase chain reaction (PCR) methods [29] [30]. This innovative platform amplifies target DNA with high specificity, sensitivity, and speed, making it ideally suited for field deployment and point-of-care (POC) diagnosis of parasitic infections that disproportionately affect low-income countries [29] [31]. The technology represents a significant advancement in the global effort to control and eliminate neglected tropical diseases (NTDs), as it combines the accuracy of molecular diagnostics with the practicality needed for implementation in basic healthcare settings.
The burden of parasitic diseases remains substantial throughout the globe, with neglected tropical diseases (NTDs) alone affecting approximately 10% of the world's population [30]. The accurate, species-level diagnosis of these diseases is critical for effective treatment and preventing disease progression. However, traditional diagnostic methods such as microscopy and immunochromatographic tests lack the sensitivity to detect low-density infections and often cannot differentiate between species [31] [32]. Conversely, PCR-based methods, while highly accurate, are often impractical in field settings due to their complexity, equipment requirements, and high running costs [29] [30]. LAMP technology effectively bridges this diagnostic gap by offering a robust, equipment-free alternative that maintains the precision of molecular diagnostics while being adaptable to challenging field conditions [29] [33].
LAMP in Context: Comparison with Existing Diagnostic Modalities
Performance Comparison of Diagnostic Methods
Table 1: Comparison of Diagnostic Methods for Parasitic Diseases
| Method | Sensitivity | Specificity | Equipment Needs | Time to Result | Cost | Personnel Requirements |
|---|---|---|---|---|---|---|
| Microscopy | Low to moderate (e.g., 59% for hookworm) [32] | Variable; requires expert for accuracy [31] | Basic microscope | 30-60 minutes | Low | Skilled technician |
| Rapid Diagnostic Tests (RDTs) | Moderate; decreases with low parasitemia [33] | Generally high (e.g., 99.9% specificity vs LAMP) [33] | None | 15-20 minutes | Low | Minimal training |
| Conventional PCR | High [31] | High [31] | Thermal cycler, electrophoresis equipment | 2-4 hours | High | Skilled technician |
| Real-time PCR | Very high (reference standard) [32] | Very high [31] | Real-time PCR instrument | 1-2 hours | Very high | Skilled technician |
| LAMP | High (e.g., 87.8% for hookworm; detects 3.4x more than RDT in malaria) [33] [32] | High (100% for hookworm, malaria) [32] [34] | Heat block or water bath | 45-60 minutes | Moderate | Minimal to moderate training |
Advantages of LAMP for Field Deployment
LAMP offers several distinct advantages that make it particularly suitable for field-based diagnosis of parasitic diseases. Its isothermal amplification principle eliminates the need for expensive thermocyclers, significantly reducing both equipment costs and power requirements [29] [31]. The technique demonstrates remarkable resistance to inhibitors present in biological samples, which often compromise PCR results, thereby reducing the need for extensive DNA purification [30]. Results can be visualized through simple methods including turbidity measurement, colorimetric changes with dyes like hydroxynaphthol blue or malachite green, or fluorescence under UV light, facilitating interpretation in basic field settings [34].
The robustness of LAMP has been demonstrated across multiple parasitic diseases. In a large-scale field deployment in Zanzibar screening for asymptomatic malaria, LAMP detected 3.4 times more Plasmodium-positive samples than rapid diagnostic tests (1.6% prevalence by LAMP vs. 0.5% by RDT) [33]. Similarly, for hookworm detection, LAMP showed significantly higher sensitivity (87.8%) compared to microscopy (59%) and conventional PCR (83.7%) when using real-time PCR as the reference standard [32]. These performance characteristics, combined with the platform's simplicity, position LAMP as an ideal technology for mass screening programs and surveillance activities in pre-elimination settings for parasitic diseases [29] [33].
Technical Principles of LAMP
Primer Design Strategy
The exceptional specificity of LAMP amplification is achieved through the use of four to six primers that recognize six to eight distinct regions on the target DNA sequence [30] [31]. This multi-primer system consists of two outer primers (F3 and B3), two inner primers (FIP and BIP), and optionally two loop primers (LF and LB) [30]. The inner primers (FIP and BIP) contain two distinct binding sequences connected by a TTTT linker, which facilitates the formation of loop structures essential for the amplification process [30] [35]. The outer primers initiate the reaction by displanging DNA strands synthesized from the inner primers, while the loop primers accelerate the reaction by binding to the loop structures formed during amplification, reducing reaction time by approximately 30 minutes [30].
Primer design follows specific parameters to ensure optimal performance. The target sequence for LAMP amplification is typically 130-260 base pairs in length, situated between the F2 and B2 regions [35]. The melting temperatures (Tm) of the primer regions are carefully balanced, with the F2/B2 regions having a Tm of approximately 60-65°C, and the F1c/B1c regions having a Tm of approximately 65-70°C [35]. The F3 and B3 primers generally have a lower Tm (approximately 55-60°C) than the F2/B2 regions to ensure proper strand displacement during the amplification process [35]. This sophisticated primer design underlies LAMP's exceptional specificity, enabling it to distinguish between closely related species and even detect single nucleotide polymorphisms in applications such as drug resistance monitoring [29] [31].
Amplification Mechanism
The LAMP amplification process occurs through a cyclic mechanism that generates stem-loop DNA structures with inverted repeats of the target sequence. The reaction can be divided into two main phases: an initial non-cyclic step and an exponential amplification phase [30]. In the initial step, all primers contribute to the formation of a dumbbell-shaped DNA structure with loops on both ends. This structure then serves as the starting material for the exponential amplification phase, where the inner and loop primers drive rapid DNA synthesis through a self-priming strand displacement mechanism [30] [35].
During the exponential phase, the FIP primer binds to the loop on the 3' side and initiates strand synthesis, displacing the previously synthesized strand. The displaced strand forms a new stem-loop structure at the opposite end, to which the BIP primer binds to initiate a subsequent round of synthesis [35]. This cyclic process generates long cauliflower-like DNA structures with multiple inverted repeats of the target sequence, resulting in exponential amplification that can produce microgram quantities of DNA in less than an hour [30]. The entire process is catalyzed by a Bst DNA polymerase with strong strand-displacement activity, which operates optimally at isothermal conditions between 60-65°C [30] [31].
Experimental Protocols for Field Deployment
Sample Collection and Preparation
Effective field deployment of LAMP begins with proper sample collection and processing. For blood samples collected in malaria-endemic regions, finger-prick blood (60μL) can be collected using plastic capillary tubes and dispensed into pre-labeled tubes containing DNA extraction buffer (400mM NaCl, 40mM Tris pH 6.5, 0.4% SDS) [33]. For stool samples used in diagnosing soil-transmitted helminths like Ancylostoma duodenale, approximately 200mg of fecal material can be collected from different sites within the stool sample to ensure representative sampling [36] [32]. Studies on Spirometra mansoni detection have demonstrated that sampling location within the stool and storage conditions (temperature, duration) do not significantly affect LAMP detection results, highlighting the method's robustness for field applications [36].
Simplified DNA extraction methods are critical for field-based LAMP applications. The boil and spin method has been successfully implemented in large-scale field studies, where samples are heated at 95°C for several minutes followed by centrifugation to pellet debris [33]. Commercial kits such as the Illumigene Malaria LAMP employ even simpler approaches including simple filtration prep (SFP) and gravity-driven filtration prep (GFP) that rely on chemical lysis and can produce amplifiable DNA within 10 minutes without centrifugation [34]. These simplified methods have demonstrated excellent performance, with the GFP method achieving a detection limit of 0.3 parasites/μL for Plasmodium falciparum [34].
LAMP Reaction Setup and Optimization
Table 2: Standard LAMP Reaction Components and Conditions
| Component | Final Concentration | Function | Optimization Notes |
|---|---|---|---|
| Bst Polymerase | 8-16 units/reaction | DNA synthesis with strand displacement activity | Use in silico designed mutants for improved processivity, fidelity, and inhibitor tolerance [30] |
| dNTPs | 1.0-1.4 mM each | Nucleotide substrates for DNA synthesis | Higher concentrations than PCR may be required [32] |
| Inner Primers (FIP/BIP) | 1.6-2.0 μM each | Primary amplification primers | Critical for reaction efficiency; test ratios of outer:inner primers (1:2 to 1:8) [36] [32] |
| Outer Primers (F3/B3) | 0.2-0.4 μM each | Initiate strand displacement | Lower concentration than inner primers [32] |
| Loop Primers (LF/LB) | 0.8-1.0 μM each | Accelerate reaction | Optional but reduce reaction time by ~30 min [30] |
| MgSOâ‚„ | 4-8 mM | Cofactor for polymerase | Concentration affects specificity; optimize between 4-8mM [36] |
| Betaine | 0.6-1.0 M | Reduces secondary structure in DNA | Enhances amplification efficiency [32] |
| Buffer | 1X (20mM Tris-HCl, 10mM (NH₄)₂SO₄, 10mM KCl, 0.1% Triton X-100) | Reaction environment | pH typically 8.8 at 25°C [32] |
| Temperature | 60-65°C | Isothermal amplification | Optimize based on primer Tm; typically 60-65°C for 45-60 min [30] [32] |
The LAMP reaction setup begins with assembling the master mix containing all necessary components, which can be pre-aliquoted and lyophilized for field use. Reaction optimization should include testing different inner:outer primer ratios (typically between 1:2 to 1:8), magnesium concentration (4-8mM), and temperature (60-65°C) to establish optimal conditions for each specific assay [36] [32]. For field applications, the use of lyophilized reagents in pre-dispensed tubes significantly enhances stability and ease of use, eliminating cold chain requirements [34]. The reaction is typically incubated for 45-60 minutes at the optimal temperature, after which results can be interpreted through various detection methods.
Result Detection and Interpretation
Multiple approaches exist for detecting LAMP amplification products in field settings. Turbidity measurement relies on the precipitation of magnesium pyrophosphate as a byproduct of DNA synthesis, which increases the turbidity of the reaction mixture and can be measured visually or with a simple spectrophotometer [34]. Colorimetric methods employ dyes such as hydroxynaphthol blue or malachite green that change color in response to amplification, allowing visual interpretation without equipment [34]. Fluorescent intercalating dyes like SYBR Green can be used with UV light illumination for result visualization, while lateral flow dipsticks enable detection of labeled amplicons through immunochromatography [30].
The interpretation of LAMP results requires appropriate controls to ensure reliability. Each run should include a positive control (target DNA of known concentration) to verify reaction efficiency, a negative control (nuclease-free water) to detect contamination, and an internal amplification control when possible to identify inhibition [32]. In field studies, result interpretation has been successfully performed by technicians with limited molecular biology experience following brief training sessions, demonstrating the feasibility of deploying this technology in diverse healthcare settings [33].
Performance Data and Field Validation
Analytical and Clinical Performance
Table 3: Field Performance of LAMP for Parasitic Disease Detection
| Parasite/Disease | Sample Type | Reference Method | LAMP Sensitivity | LAMP Specificity | Limit of Detection |
|---|---|---|---|---|---|
| Plasmodium spp. (Malaria) | Whole blood | PET-PCR | 97.1% (GFP method) [34] | 96.5% (GFP method) [34] | 0.3-2.0 parasites/μL depending on sample prep [34] |
| Plasmodium spp. (Asymptomatic malaria) | Whole blood | RDT/Microscopy | Detected 3.4x more positives than RDT (1.6% vs 0.5% prevalence) [33] | 99.9% [33] | Not specified |
| Ancylostoma duodenale (Hookworm) | Stool | Real-time PCR | 87.8% [32] | 100% [32] | 7.47 pg/μL (cat faecal DNA) [32] |
| Spirometra mansoni | Stool, eggs | Specificity panel | 100% (no cross-reactivity) [36] | 100% (no cross-reactivity) [36] | 355.5 fg/μL (egg-derived DNA) [36] |
Field validation studies have demonstrated LAMP's robust performance across various parasitic diseases and settings. In a comprehensive evaluation of the Illumigene Malaria LAMP assay conducted in Senegal, the method showed excellent concordance with reference PET-PCR assays, detecting all human-infecting Plasmodium species without cross-reactivity [34]. The assay performed reliably in a clinical laboratory setting with technicians having limited molecular experience, highlighting its suitability for resource-limited environments [34]. For soil-transmitted helminths, LAMP has shown superior sensitivity compared to traditional microscopy, with a recently developed assay for Ancylostoma duodenale demonstrating perfect specificity (100%) and high sensitivity (87.8%) when compared to real-time PCR [32].
The technology has proven particularly valuable for detecting low-density infections that often escape detection by conventional methods. In a mass screening study of asymptomatic malaria in Zanzibar, LAMP identified a significantly higher number of infected individuals (1.6% prevalence) compared to RDTs (0.5% prevalence), uncovering a reservoir of infection that would have otherwise been missed [33]. This enhanced detection capability is critical for elimination programs, as asymptomatic carriers can sustain transmission cycles even when clinical cases are effectively identified and treated [33].
Essential Research Reagent Solutions
Critical Materials for LAMP Implementation
Table 4: Essential Research Reagents for LAMP-based Parasite Detection
| Reagent/Material | Function | Implementation Notes |
|---|---|---|
| Bst DNA Polymerase | Strand-displacing DNA synthesis | Engineered versions available with improved processivity, fidelity, and inhibitor tolerance [30] |
| Primer Sets (F3, B3, FIP, BIP, LF, LB) | Target-specific amplification | Designed to recognize 6-8 distinct sequences; lyophilized primers enhance field stability [30] [35] |
| dNTP Mix | Nucleotide substrates for DNA synthesis | Higher concentrations (1.0-1.4 mM each) often required compared to PCR [32] |
| MgSOâ‚„ Solution | Essential cofactor for polymerase | Concentration must be optimized (typically 4-8 mM); affects reaction specificity [36] |
| Betaine | Reduces secondary structure in GC-rich regions | Enhances amplification efficiency; typically used at 0.6-1.0 M concentration [32] |
| WarmStart Technology | Prevents non-specific amplification at room temperature | Enables room-temperature setup in field conditions [32] |
| Colorimetric Indicators | Visual result interpretation | Hydroxynaphthol blue, malachite green, or SYBR Green for visualization [34] |
| Lyophilized Reaction Tubes | Stable reagent format for field use | Pre-aliquoted, ambient temperature-stable reagents (e.g., Illumigene, Loopamp kits) [33] [34] |
Successful deployment of LAMP technology in field settings relies on the availability of specialized reagents and materials. The Bst DNA polymerase serves as the core enzyme, with its strand-displacement activity enabling isothermal amplification [30]. Recent advancements include the development of in silico designed Bst mutants with improved processivity, fidelity, stability, and tolerance to amplification inhibitors, further enhancing the robustness of LAMP under challenging field conditions [30]. Primer design software such as Primer Explorer V5 facilitates the development of target-specific assays, with rigorous BLAST analysis required to confirm specificity before implementation [32].
For field applications, lyophilized reagents format is particularly valuable, as demonstrated by commercial kits like the Loopamp MALARIA Pan/Pf Detection Kit and Illumigene Malaria LAMP, which provide pre-dispensed, temperature-stable reaction components [33] [34]. These kits incorporate simplified sample preparation methods that eliminate the need for centrifugation and complex DNA extraction procedures, making them accessible to personnel with minimal molecular biology training [34]. The integration of WarmStart technology prevents non-specific amplification during reaction setup at ambient temperatures, a common challenge in field settings without access to cooled work surfaces [32].
Emerging Trends and Future Perspectives
LAMP technology continues to evolve with several advanced applications enhancing its utility for parasitic disease diagnosis. Multiplex LAMP formats enable simultaneous detection of multiple pathogens or species differentiation in a single reaction, addressing the challenge of polyparasitism common in endemic regions [29]. Reverse Transcription LAMP (RT-LAMP) expands the platform's capability to detect RNA viruses, with potential applications for parasitic diseases with RNA stages in their life cycles [29]. The integration of LAMP with microfluidic platforms creates lab-on-a-chip systems that automate the entire diagnostic process from sample preparation to result detection, potentially enabling high-throughput screening in field settings [29] [30].
The digital LAMP format offers absolute quantification of parasite load by partitioning reactions into thousands of nanoliter droplets, providing valuable data for treatment monitoring and epidemiological studies [29]. For drug resistance monitoring, single nucleotide polymorphism (SNP) LAMP assays have been developed to detect genetic markers associated with treatment failure, such as those conferring artemisinin resistance in malaria parasites [31]. These advanced applications maintain the core advantages of LAMP while expanding its analytical capabilities to address complex diagnostic challenges.
Future development efforts should focus on creating higher throughput, affordable closed systems to minimize contamination risks during large-scale screening [33]. The integration of smartphone-based detection and real-time connectivity would enhance result interpretation, data management, and integration with surveillance systems [30]. As the WHO's 2030 roadmap for NTDs emphasizes improved diagnostics, LAMP platforms are poised to play an increasingly important role in global efforts to control and eliminate parasitic diseases through enhanced detection capabilities in the most affected regions [30] [37].
The definitive diagnosis of parasitic diseases represents a critical challenge in global health, particularly in resource-limited settings where traditional methods often lack the necessary sensitivity and specificity for early detection. This technical guide examines the transformative role of nanobiosensors incorporating metallic nanoparticles and quantum dots (QDs) in revolutionizing parasitic disease diagnosis. These nanotechnology-based platforms demonstrate unparalleled capabilities in detecting parasite-specific antigens and genetic material at ultra-low concentrations, enabling precise early-stage diagnosis essential for effective treatment and disease management. By leveraging the unique physicochemical properties of nanomaterials, these biosensing systems significantly outperform conventional diagnostic techniques, offering rapid, cost-effective solutions that are particularly suitable for point-of-care testing environments. This review comprehensively addresses the underlying principles, material specifications, experimental protocols, and current applications of these advanced diagnostic platforms while contextualizing their development within the broader framework of parasitic disease research.
Parasitic infections including malaria, leishmaniasis, schistosomiasis, and echinococcosis continue to pose substantial global health burdens, with traditional diagnostic techniques such as microscopic examinations, immunological assays like ELISA, and molecular tests including PCR demonstrating significant limitations [14]. These conventional approaches are often constrained by their time-consuming processes, requirement for specialized equipment and trained personnel, and insufficient sensitivity for detecting early or low-level infections [14] [8]. The integration of nanotechnology with biosensing platforms has emerged as a revolutionary approach to overcome these diagnostic challenges, enabling the development of highly sensitive and specific detection systems for parasitic antigens and genetic material.
Nanobiosensors are analytical devices that incorporate nanomaterials such as metallic nanoparticles and quantum dots as integral components to detect biological interactions through various transduction mechanisms [38] [39]. These systems function by converting molecular recognition events, such as antibody-antigen binding or DNA hybridization, into measurable electrical, optical, or electrochemical signals [40]. The exceptional properties of nanomaterials, including their high surface-to-volume ratio, quantum confinement effects, and enhanced reactivity, substantially improve biosensor performance by increasing sensitivity, specificity, and detection limits [38]. This technological advancement is particularly crucial for parasitic disease diagnosis, where early detection of infections can dramatically improve treatment outcomes and disease management strategies.
Fundamental Principles and Nanomaterial Properties
Working Mechanisms of Nanobiosensors
Nanobiosensors operate through specific interactions between target analytes (parasitic antigens or genetic material) and biorecognition elements (antibodies, DNA probes, aptamers), which induce detectable changes in the physicochemical properties of the sensor system [38]. The fundamental working principle involves three key components: a biorecognition element that selectively binds to the target parasite biomarker, a transducer that converts the binding event into a measurable signal, and a signal processing system that quantifies and displays the results [39]. Nanomaterials serve as high-performance interfaces between the recognition elements and transducer, significantly enhancing sensitivity through their large surface area, tunable optical/electronic characteristics, and quantum effects [38].
The detection mechanisms employed in parasitic disease diagnosis primarily include electrochemical, optical, and magnetic approaches. Electrochemical nanobiosensors detect changes in electrical signals when parasitic antigens or DNA attach to electrode surfaces modified with nanomaterials [14]. Optical nanobiosensors utilize the unique plasmonic or fluorescent properties of nanomaterials, employing techniques such as surface plasmon resonance (SPR), localized surface plasmon resonance (LSPR), fluorescence resonance energy transfer (FRET), and surface-enhanced Raman spectroscopy (SERS) [14] [38]. Magnetic nanobiosensors incorporate magnetic nanoparticles to efficiently isolate target molecules from complex biological samples like blood, enabling highly sensitive antigen detection even at minimal concentrations [14].
Properties of Key Nanomaterials
Metallic Nanoparticles: Gold nanoparticles (AuNPs) are extensively utilized in nanobiosensors due to their exceptional biocompatibility, tunable surface chemistry, and unique optical properties, particularly their localized surface plasmon resonance (LSPR) characteristics [38]. The LSPR phenomenon causes strong visible light absorption and scattering when AuNPs undergo-conjugation with biomolecules, resulting in noticeable color changes detectable even by naked eye in some diagnostic formats [14]. Silver nanoparticles (AgNPs) similarly exhibit strong plasmonic effects and are often employed to enhance electrochemical catalysis when incorporated into electrode systems [40]. These metallic nanoparticles can be functionalized with various biological recognition elements including antibodies, DNA probes, and aptamers through thiol chemistry or other conjugation strategies, enabling specific detection of parasitic biomarkers [14] [39].
Quantum Dots: Quantum dots are semiconductor nanocrystals (typically 2-8 nm in size) that exhibit size-tunable fluorescence emission, high quantum yield, and exceptional photostability compared to traditional organic dyes [41]. CdSe QDs typically emit light across 450-650 nm wavelengths, while PbS QDs can generate near-infrared emission at approximately 1000 nm [41]. The fluorescence brightness of core-shell structures like CdSe/ZnS QDs reaches 50-90% quantum yield, enabling detection capabilities at picomolar to femtomolar concentrations essential for identifying low-abundance parasitic biomarkers [41]. Their broad absorption spectra with narrow, symmetric emission peaks facilitate multiplexed detection of several parasitic targets simultaneously without spectral interference [41]. Surface functionalization with various ligands, antibodies, and peptides enables targeted binding to specific parasite biomarkers [41].
Table 1: Key Nanomaterial Properties for Parasite Detection
| Nanomaterial | Key Properties | Detection Mechanisms | Typical Size Range |
|---|---|---|---|
| Gold Nanoparticles (AuNPs) | Biocompatibility, tunable LSPR, strong absorption/scattering | Colorimetric, LSPR, electrochemical | 5-100 nm |
| Quantum Dots (QDs) | Size-tunable fluorescence, high quantum yield, photostability | Fluorescence, FRET | 2-8 nm |
| Carbon Nanotubes (CNTs) | High electrical conductivity, large surface area | Electrochemical, field-effect transistors | 1-100 nm diameter |
| Magnetic Nanoparticles | Superparamagnetism, selective separation | Magnetic isolation, electrochemical | 10-100 nm |
Research Reagent Solutions and Experimental Protocols
Essential Research Reagents
The development and implementation of nanobiosensors for parasitic antigen and genetic material detection requires specialized research reagents and materials. The following table summarizes key components essential for constructing these diagnostic platforms.
Table 2: Essential Research Reagents for Nanobiosensor Development
| Reagent/Material | Function | Specific Examples |
|---|---|---|
| Metallic Nanoparticles | Signal generation, signal amplification | Gold nanoparticles, silver nanoparticles |
| Quantum Dots | Fluorescent labeling, optical detection | CdSe/ZnS core-shell QDs, PbS QDs |
| Biorecognition Elements | Target capture and specificity | Anti-PfHRP2 antibodies (Plasmodium), DNA probes for Leishmania kDNA |
| Surface Functionalization Agents | Bioconjugation, surface modification | Thiol compounds, silanes, EDC/NHS chemistry |
| Transducer Platforms | Signal conversion | Screen-printed carbon electrodes, gold electrodes, optical fibers |
| Signal Enhancement Reagents | Amplification of detection signal | Enzymes (HRP), catalytic nanomaterials |
Experimental Protocol for Parasitic Antigen Detection Using AuNP-Based Biosensors
Objective: To detect Plasmodium falciparum histidine-rich protein 2 (PfHRP2) antigen using gold nanoparticle-based electrochemical biosensor.
Materials and Reagents:
- Citrate-stabilized gold nanoparticles (20 nm diameter)
- Anti-PfHRP2 monoclonal antibodies
- Phosphate buffered saline (PBS, 0.01 M, pH 7.4)
- Screen-printed carbon electrodes (SPCE)
- 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) and N-hydroxysuccinimide (NHS)
- Bovine serum albumin (BSA)
- Clinical samples (blood, serum)
Procedure:
- Electrode Pretreatment: Clean SPCEs by cycling in 0.5 M Hâ‚‚SOâ‚„ from 0 to +1.5 V until stable voltammogram is obtained.
- Antibody Immobilization: Incubate SPCEs with anti-PfHRP2 antibody solution (10 µg/mL in PBS) for 2 hours at 4°C.
- Surface Blocking: Treat electrodes with 1% BSA solution for 1 hour to minimize non-specific binding.
- Sample Incubation: Apply clinical samples (diluted 1:10 in PBS) to functionalized electrodes and incubate for 30 minutes at room temperature.
- Signal Detection: Measure electrochemical response using differential pulse voltammetry in 5 mM [Fe(CN)₆]³â»/â´â» solution with parameters: potential range -0.2 to +0.6 V, pulse amplitude 50 mV, pulse width 50 ms.
- Data Analysis: Quantify PfHRP2 concentration based on reduction in peak current proportional to antigen concentration.
Validation: Compare results with standard ELISA for PfHRP2 detection to determine sensitivity and specificity of the nanobiosensor.
Experimental Protocol for Parasitic Genetic Material Detection Using QD-Based Biosensors
Objective: To detect Leishmania kinetoplast DNA (kDNA) using quantum dot-based fluorescence biosensor.
Materials and Reagents:
- CdTe/ZnS core-shell quantum dots (emission 605 nm)
- DNA probes specific for Leishmania kDNA
- Graphene oxide (GO) sheets
- Tris-EDTA buffer (10 mM Tris, 1 mM EDTA, pH 8.0)
- Hybridization buffer (5× SSC, 0.1% Tween-20)
- Clinical samples (blood, tissue aspirates)
- DNA extraction kit
Procedure:
- DNA Extraction: Isolate total DNA from clinical samples using commercial DNA extraction kit according to manufacturer's instructions.
- Probe Conjugation: Incubate amino-modified DNA probes with carboxyl-functionalized QDs using EDC/NHS chemistry for 4 hours at room temperature.
- Sensor Assembly: Immobilize QD-probe conjugates on GO-coated substrate through π-π stacking interactions.
- Hybridization Reaction: Apply extracted DNA samples to sensor surface and incubate for 1 hour at 42°C in hybridization buffer.
- Signal Measurement: Record fluorescence emission at 605 nm with excitation at 400 nm using fluorescence spectrophotometer.
- Data Analysis: Quantify fluorescence intensity increase proportional to target DNA concentration using standard curve with known kDNA concentrations.
Validation: Compare detection sensitivity with conventional PCR methods, calculating limit of detection (LOD) and dynamic range.
Performance Data and Diagnostic Applications
Quantitative Detection Performance
The integration of metallic nanoparticles and quantum dots in biosensing platforms has demonstrated remarkable improvements in detection sensitivity for parasitic biomarkers. The following table summarizes performance data for selected nanobiosensor applications in parasitic disease diagnosis.
Table 3: Performance Metrics of Nanobiosensors for Parasitic Disease Detection
| Parasite Target | Nanomaterial | Biomarker | Detection Limit | Detection Method |
|---|---|---|---|---|
| Plasmodium spp. | Gold nanoparticles | PfHRP2 antigen | ~10 pg/mL | Electrochemical |
| Leishmania spp. | Quantum dots | kDNA | Femtogram levels | Fluorescence |
| Echinococcus spp. | Carbon nanotubes | EgAgB antigen | ~0.1 ng/mL | Electrochemical |
| Schistosoma spp. | Graphene oxide | Soluble egg antigen | ~1 ng/mL | Optical |
| Taenia spp. | Metallic nanoparticles | Parasite antigens | Sub-nanogram | Electrochemical |
Specific Applications in Parasitic Disease Diagnosis
Malaria Detection: Plasmodium species detection has been significantly enhanced through AuNP-based biosensors targeting the PfHRP2 antigen. These platforms utilize the unique LSPR properties of AuNPs, which undergo measurable shifts upon antigen-antibody binding events [14]. The detection system achieves exceptional sensitivity of ~10 pg/mL, substantially superior to traditional rapid diagnostic tests, enabling early malaria diagnosis when parasite burden is minimal [14]. Additionally, the electrical properties of AuNPs facilitate electrochemical detection schemes that can be integrated into portable, point-of-care devices suitable for resource-limited settings where malaria is endemic [14].
Leishmaniasis Diagnosis: QD-based biosensors have revolutionized leishmaniasis detection through ultrasensitive identification of Leishmania kinetoplast DNA (kDNA) [14]. The system employs CdTe quantum dots labeled with DNA probes specific for conserved kDNA sequences, generating strong fluorescence signals upon hybridization with target parasitic DNA [14] [41]. This approach demonstrates femtogram-level sensitivity, significantly exceeding conventional PCR methods, and can be integrated with microfluidic platforms for automated sample processing and analysis [14] [41]. The photostability of QDs enables prolonged imaging and detection capabilities without signal degradation common with organic fluorophores [41].
Helminth Infections: Nanobiosensors have been successfully developed for major helminth infections including echinococcosis, schistosomiasis, and taeniasis. Carbon nanotubes functionalized with anti-EgAgB antibodies enable specific detection of Echinococcus granulosus antigens at concentrations as low as 0.1 ng/mL [14]. Similarly, graphene oxide-based platforms demonstrate high sensitivity for schistosomiasis through detection of soluble egg antigens, while metallic nanobiosensors effectively identify Taenia species biomarkers even at minimal concentrations [14]. These systems provide crucial diagnostic capabilities in endemic areas where conventional laboratory infrastructure is limited.
Signaling Pathways and Experimental Workflows
The detection mechanisms for parasitic antigens and genetic material involve specific signaling pathways and experimental workflows that can be visualized through the following diagrams:
Diagram 1: Antigen Detection Workflow
Diagram 2: Genetic Material Detection
Challenges and Future Perspectives
Despite the significant advancements in nanobiosensor technology for parasitic disease diagnosis, several challenges remain that require addressing before widespread clinical implementation can be realized. Key limitations include constraints in mass production capabilities, interference from complex biological matrices, and the need for standardization and validation protocols [14]. Additionally, the potential toxicity of certain nanomaterials, particularly quantum dots containing heavy metals, necessitates thorough biocompatibility assessment and the development of effective surface functionalization strategies to mitigate adverse effects [41].
Future research directions focus on developing multiplex nanobiosensors using polymer nanofibers or hybrid nanoparticles for simultaneous detection of multiple pathogens [14]. The integration of lab-on-a-chip technology with nanobiosensing platforms will enable automated sample processing and analysis, significantly enhancing point-of-care testing capabilities in resource-limited settings [14] [38]. Furthermore, the convergence of artificial intelligence with nanobiosensor data analysis promises to revolutionize diagnostic accuracy through intelligent pattern recognition and real-time analysis [41]. Emerging materials including two-dimensional transition metal carbides/nitrides (MXenes) and DNA origami-based nanostructures offer new opportunities for developing ultrasensitive and highly specific biosensing platforms with enhanced performance characteristics [38].
The ongoing advancement of nanobiosensor technology is expected to significantly impact the detection, treatment, and management of parasitic infections by providing new avenues for early detection, improved therapeutic monitoring, and enhanced disease surveillance. As these technologies mature and overcome current translational challenges, they hold immense potential to revolutionize parasitic disease diagnosis and ultimately contribute to reduced disease burden in endemic regions worldwide.
Accurate diagnosis of parasitic diseases remains a formidable challenge in global health, particularly in resource-limited settings where these infections are most prevalent. Traditional diagnostic techniques, including microscopy and culturing, are often constrained by requirements for specialized expertise, lengthy processing times, and limited sensitivity [7] [8]. Within this diagnostic landscape, advanced serology and immunoassays have emerged as transformative technologies capable of detecting parasitic antigens and host immune responses with unprecedented precision. These methodologies are revolutionizing the definitive diagnosis of parasitic diseases by providing critical tools that enhance sensitivity, specificity, and operational efficiency [7] [42].
The evolution of immunoassay technologies represents a paradigm shift in parasitic disease management. Conventional methods are increasingly being supplemented or replaced by sophisticated platforms that leverage molecular, nanotechnological, and computational advancements [7] [8]. This technical guide examines the current state of advanced serological applications within parasitology, detailing innovative methodologies, experimental protocols, and emerging trends that are reshaping diagnostic capabilities for researchers, scientists, and drug development professionals.
Technological Innovations in Immunoassays
The diagnostic landscape for parasitic diseases has witnessed remarkable technological advancements that significantly enhance antigen detection and host response characterization. These innovations address critical limitations of traditional assays, particularly in complex biological matrices where interference compounds and low analyte concentrations present substantial challenges.
Next-generation immunoassay systems now incorporate sophisticated pretreatment protocols to improve detection accuracy. The iTACT (Immunoassay for Total Antigen including Complex via preTreatment) method, for instance, employs specialized detergents and denaturants to breakdown antigen complexes and inactivate interfering substances prior to analysis via chemiluminescent enzyme immunoassay (CLEIA) [42]. This approach demonstrated enhanced detection of hepatitis B viral antigens, with applications extending to parasitic disease biomarkers [42]. Similarly, novel assay designs utilizing anti-metatype antibodies enable sandwich assay formats for small-molecule antigens that were previously limited to competitive assays with lower sensitivity [42].
Ultrasensitive detection platforms represent another frontier in immunoassay innovation. Fluxus technology incorporates optical waveguides and microfluidics on miniature chips to enable single-molecule detection, achieving quantification at exceptionally low concentrations across diverse sample types including blood, saliva, and urine [42]. This level of sensitivity is further complemented by the integration of alternative binding molecules such as peptide binders, which can be systematically selected through screening processes to target antigens lacking corresponding antibodies [42].
Table 1: Advanced Immunoassay Platforms for Parasitic Disease Diagnosis
| Technology | Core Principle | Key Advantage | Representative Application |
|---|---|---|---|
| iTACT Method | Sample pretreatment to dissociate complexes | Enhances detection of bound antigens | Hepatitis B antigen monitoring; adaptable for parasitic antigens |
| Fluxus System | Optical waveguides with microfluidics | Single-molecule detection capability | Ultrasensitive biomarker detection in blood, saliva, urine |
| Peptide Binders | Phage display-selected peptides | Targets antigens inaccessible to antibodies | Expanding range of detectable parasitic biomarkers |
| CRISPR-Cas Diagnostics | Nucleic acid detection with Cas proteins | High specificity and portability | Plasmodium, Leishmania detection [8] |
| Nanobiosensors | Nanomaterial-based signal amplification | Exceptional sensitivity at low concentrations | Plasmodium PfHRP2 detection [14] |
The convergence of immunoassays with nanotechnology has produced particularly promising platforms for parasitic disease diagnosis. Nanobiosensors utilizing gold nanoparticles (AuNPs), quantum dots (QDs), and carbon nanotubes functionalized with specific antibodies demonstrate remarkable sensitivity in detecting parasitic antigens and genetic material [14]. For example, AuNP-based sensors successfully identified Plasmodium falciparum histidine-rich protein 2 (PfHRP2), while carbon nanotubes functionalized with anti-EgAgB antibodies showed efficacy in detecting Echinococcus biomarkers [14]. These nanomaterials enhance diagnostic performance through their unique physical and chemical properties, enabling rapid, accurate, and cost-effective detection even at low analyte concentrations [14].
Advanced Experimental Protocols
Automated Chemiluminescent Enzyme Immunoassay (CLEIA) with Pretreatment
The Lumipulse system exemplifies advanced immunoassay automation, integrating sample pretreatment to enhance diagnostic accuracy for complex biological targets. This protocol is particularly valuable for detecting parasitic antigens that may be bound in molecular complexes or obscured by interfering substances [42].
Sample Preparation: Collect serum or plasma samples using standard venipuncture techniques. Centrifuge at 1,500 × g for 10 minutes to remove particulate matter. Aliquot and store at -20°C if not testing immediately [43].
Pretreatment Protocol: Combine 50μL of sample with 100μL of specialized detergent solution containing 1% sodium dodecyl sulfate and 0.1% Triton X-100. Vortex for 30 seconds and incubate at 56°C for 15 minutes to dissociate antigen complexes [42].
Automated Analysis: Load pretreated samples into the Lumipulse instrument alongside reagent cassettes containing capture antibodies, detection antibodies conjugated with alkaline phosphatase, and chemiluminescent substrate (CDP-Star). The system automatically executes the following steps: (1) aliquots 50μL of pretreated sample into reaction vessels; (2) adds 50μL of capture antibody-coated magnetic particles; (3) incubates with agitation for 10 minutes at 37°C; (4) washes twice with phosphate buffered saline with Tween-20 (PBST); (5) adds 50μL of conjugate antibody; (6) incubates for 10 minutes at 37°C; (7) washes three times with PBST; (8) adds 100μL of chemiluminescent substrate; and (9) measures light emission at 430nm [42].
Data Interpretation: Calculate antigen concentration from the standard curve generated using calibrators of known concentration. The pretreatment step typically increases detectable antigen concentrations by 1.5 to 3-fold for complex-bound targets [42].
Nanobiosensor Development for Parasitic Antigen Detection
Nanobiosensors represent the cutting edge of diagnostic sensitivity, leveraging the unique properties of nanomaterials to detect parasitic biomarkers at exceptionally low concentrations.
Nanomaterial Functionalization: Synthesize gold nanoparticles (AuNPs) via citrate reduction method to obtain 20nm particles. Incubate AuNPs with 10μg/mL of anti-parasite monoclonal antibodies in 10mM phosphate buffer (pH 7.4) for 2 hours at room temperature with gentle agitation. Purify functionalized AuNPs by centrifugation at 14,000 × g for 20 minutes and resuspend in storage buffer (10mM Tris-HCl, 0.1% BSA, pH 8.0) [14].
Sensor Assembly: Immerse screen-printed carbon electrodes in the functionalized AuNP solution for 1 hour to create the sensing interface. Wash with deionized water to remove unbound nanoparticles. Block nonspecific binding sites by incubating with 1% bovine serum albumin in Tris-buffered saline (TBS) for 30 minutes [14].
Sample Analysis: Apply 10μL of clinical sample (serum, plasma, or urine) to the sensor surface. Incubate in a humidified chamber for 15 minutes at room temperature. Wash with PBST to remove unbound antigens. For electrochemical detection, measure current changes using square wave voltammetry from -0.2V to +0.6V with a step potential of 0.005V and amplitude of 0.025V [14].
Signal Amplification: For enhanced sensitivity, employ catalytic amplification by adding 50μL of 0.1% hydrogen peroxide and 1mM tetramethylbenzidine in acetate buffer (pH 5.0). Measure the electrochemical reduction signal at -0.2V [14]. This approach can detect parasite-specific antigens at concentrations as low as 10pg/mL, significantly surpassing conventional ELISA sensitivity [14].
Quantitative Performance Comparison
The diagnostic performance of advanced serological assays varies significantly across platforms and target analytes. Understanding these performance characteristics is essential for selecting appropriate methodologies for specific parasitic diseases and research contexts.
Table 2: Performance Metrics of Advanced Serological Assays for Parasitic Disease Diagnosis
| Assay Type | Sensitivity | Specificity | Time to Result | Limit of Detection | Multiplexing Capacity |
|---|---|---|---|---|---|
| Conventional ELISA | 70-85% | 80-90% | 3-4 hours | 1-10 ng/mL | Low (single analyte) |
| Rapid Diagnostic Tests | 75-95% | 85-98% | 15-20 minutes | 5-50 ng/mL | Low to moderate (2-3 analytes) |
| Automated CLEIA | 90-98% | 95-99% | 30-45 minutes | 0.1-1 ng/mL | High (multiple plates) |
| CRISPR-Cas Systems | 95-99% | 97-100% | 60-90 minutes | 1-10 copies/μL | Moderate (2-5 targets) |
| Electrochemical Nanobiosensors | 98-99.5% | 95-99% | 10-20 minutes | 0.01-0.1 ng/mL | High (array formats) |
The performance advantages of advanced serological platforms are particularly evident in their limits of detection and quantitative capabilities. Automated CLEIA systems improve upon conventional ELISA sensitivity by approximately 10-fold, while electrochemical nanobiosensors can achieve up to 100-fold greater sensitivity [42] [14]. This enhanced detection capacity is crucial for identifying low-level parasitic infections, monitoring treatment efficacy, and detecting recurrences at the earliest stages.
Multiplexed immunoassay platforms represent another significant advancement, enabling simultaneous detection of multiple parasitic biomarkers in a single sample. Micro-ELISA systems configured in array formats can quantify numerous antibody isotypes (IgG, IgA, IgM) against multiple parasitic antigens, providing comprehensive immune response profiling [44]. This multiplexing capacity is invaluable for differential diagnosis of parasitic infections with overlapping clinical presentations and for understanding complex host-parasite interactions.
Research Reagent Solutions
The successful implementation of advanced serological assays depends on access to high-quality, well-characterized reagents. These components form the foundation of reliable, reproducible immunoassays for parasitic disease research.
Table 3: Essential Research Reagents for Advanced Serological Assays
| Reagent Category | Specific Examples | Function | Quality Control Parameters |
|---|---|---|---|
| Capture Molecules | Monoclonal antibodies, recombinant antibodies, peptide binders, aptamers | Binds target antigen with high specificity | Affinity constant (>10â¹ Mâ»Â¹), cross-reactivity profile (<1% with common interferents) |
| Signal-Generating Components | Horseradish peroxidase (HRP), alkaline phosphatase (ALP), quantum dots, electrochemiluminescent tags | Generates detectable signal proportional to antigen concentration | Specific activity (≥500 U/mg for HRP), emission spectra (QDs) |
| Solid Phases | Magnetic beads, multiwell plates (e.g., Greiner high-binding), screen-printed electrodes | Provides surface for immunocomplex formation | Binding capacity (>500 ng/cm² IgG), lot-to-lot consistency (CV <10%) |
| Buffer Systems | Carbonate-bicarbonate (pH 9.6), PBS (pH 7.4), TBST, protein-free blockers | Maintain optimal assay conditions and reduce nonspecific binding | pH stability (±0.1), endotoxin levels (<1.0 EU/mL) |
| Reference Materials | International standards, in-house calibrators, positive/negative controls | Enables result standardization and quantification | Stability (≥6 months at -70°C), commutability with clinical samples |
The selection and validation of these reagents require careful consideration of their performance characteristics in the context of parasitic antigen detection. Antibody reagents must demonstrate high specificity with minimal cross-reactivity to related parasite species or host proteins [43]. Similarly, signal-generating components should provide consistent activity with low lot-to-lot variability to ensure reproducible quantitative results across experiments [43]. International reference standards, when available, facilitate assay harmonization and enable meaningful comparisons across research studies and diagnostic platforms.
Integrated Workflow and Pathway Analysis
Advanced serological detection of parasitic infections involves a coordinated sequence of molecular interactions and technical procedures. The following diagram illustrates the core signaling pathway and detection principle for nanobiosensor-based antigen detection.
The experimental workflow for developing and validating advanced immunoassays follows a systematic approach to ensure robust performance. The diagram below outlines the key stages in this process.
The field of advanced serology and immunoassays continues to evolve rapidly, driven by innovations in nanotechnology, materials science, and molecular biology. Emerging trends indicate several promising directions that will further enhance parasitic disease diagnosis in the coming years.
The integration of multi-omics data represents a particularly significant advancement, combining proteomic, genomic, and metabolomic information to provide comprehensive understanding of parasite biology and host-parasite interactions [7] [8]. These integrated approaches facilitate the discovery of novel diagnostic biomarkers and therapeutic targets, potentially enabling more precise stratification of parasitic infections and personalized treatment approaches [7].
Point-of-care testing platforms continue to advance, with lab-on-a-chip technologies and microfluidic systems enabling rapid, accurate detection at or near the patient care site [8] [14]. These developments are especially crucial for resource-limited and endemic areas lacking centralized laboratory facilities, potentially reducing diagnostic delays and improving treatment initiation [8]. The convergence of nanobiosensors with smartphone-based detection systems and portable readers further enhances the field-deployability of these advanced diagnostic platforms [14].
CRISPR-Cas diagnostic systems present another frontier in parasitic disease detection, leveraging the precision and programmability of these molecular tools to identify parasite-specific nucleic acid sequences with exceptional sensitivity and specificity [8]. These systems provide portable, cost-effective detection methods that can be deployed in diverse settings, potentially overcoming limitations associated with traditional molecular techniques [8]. When integrated with immunoassay platforms, CRISPR-based detection creates powerful hybrid systems capable of detecting both parasitic antigens and genetic material.
In conclusion, advanced serology and immunoassays have transformed the diagnostic landscape for parasitic diseases, providing researchers and clinicians with powerful tools for antigen detection and host response characterization. These technologies continue to evolve, offering increasingly sensitive, specific, and accessible diagnostic solutions that promise to improve disease management and patient outcomes worldwide. As these platforms become more sophisticated and widely available, they will play an indispensable role in global efforts to control and eliminate parasitic diseases.
The definitive diagnosis of parasitic diseases, a pressing global health challenge, is being revolutionized by integrated multi-omics approaches. Traditional diagnostic methods, such as microscopy and serology, are often limited by sensitivity, specificity, and an inability to detect emerging pathogens or distinguish active infections from past exposure. This whitepaper details how the synergistic application of genomics, proteomics, and other omics technologies, powered by advanced bioinformatics, is accelerating the discovery of novel biomarkers. These biomarkers are critical for developing new diagnostics, monitoring treatment efficacy, and understanding host-parasite interactions, ultimately paving the way for more effective control of parasitic diseases.
Parasitic diseases affect hundreds of millions of people worldwide, with the greatest burden falling on underdeveloped and developing nations due to significant economic challenges and elevated healthcare expenditures [7]. Accurate and timely diagnosis is a cornerstone of effective disease management and control. For decades, diagnosis has relied on traditional methods including microscopy, serological testing, histopathology, and culturing [7].
While useful, these techniques possess considerable limitations. They can be time-consuming, require a high level of technical expertise, and have constrained application in endemic regions that often suffer from poor infrastructure and limited access to healthcare facilities [7]. Furthermore, methods like the Kato-Katz thick smear, the gold standard for schistosomiasis, can lack the sensitivity for early detection and cannot differentiate between active and past infections [45]. Similarly, for diseases like Chagas disease, the lack of a reliable test to monitor parasitological cure following treatment has been a major obstacle in drug development [46].
These diagnostic blind spots highlight the urgent need for a revolution in parasitology. There is a growing demand for affordable, rapid, and field-adjustable tools that can provide definitive diagnoses and guide therapeutic decisions [7]. Integrated multi-omics approaches are poised to meet this need by providing a comprehensive, unbiased, and systems-level view of both the pathogen and the host response.
The Multi-Omics Framework in Parasitic Disease Research
Integrated multi-omics involves the collective application and combination of various high-throughput "omics" technologies to study complex biological systems. The core premise is that by analyzing multiple layers of biological information—such as the genome, transcriptome, proteome, and metabolome—researchers can achieve a more holistic understanding of pathological processes than any single approach could provide [47].
Core Omics Technologies
The multi-omics framework leverages several advanced technological platforms, each interrogating a different aspect of biology, as detailed in the table below.
Table 1: Core Omics Technologies and Their Applications in Parasitology
| Omics Layer | Description | Key Technologies | Application in Parasitic Diseases |
|---|---|---|---|
| Genomics | Study of the organism's complete set of DNA, including genes and non-coding sequences. | Next-Generation Sequencing (NGS), Whole Genome Sequencing | Identifying parasite species and strains, tracking transmission patterns, discovering drug resistance markers [7]. |
| Transcriptomics | Analysis of the complete set of RNA transcripts produced by the genome under specific conditions. | RNA Sequencing (RNA-Seq) | Understanding parasite gene expression during life cycles, host invasion, and drug exposure; profiling host immune response [48]. |
| Proteomics | Large-scale study of the entire complement of proteins, including their structures and functions. | Mass Spectrometry (LC-MS/MS), Label-free quantification, Tandem Mass Tag (TMT) | Discovering parasite-specific protein biomarkers in host serum/urine; characterizing secretory proteins and vaccine candidates [45] [49]. |
| Metabolomics | Systematic study of unique chemical fingerprints (metabolites) resulting from cellular processes. | NMR Spectroscopy, Mass Spectrometry | Identifying metabolic changes in the host during infection; uncovering parasite-specific metabolic pathways for drug targeting [50]. |
The Integration Workflow
The power of multi-omics lies not just in generating data from each layer, but in their integration. The typical workflow involves sample collection, multi-omics data generation, data integration and analysis, and finally, biomarker validation.
Figure 1: A generalized workflow for integrated multi-omics biomarker discovery. Biological samples are subjected to various omics technologies, and the resulting data are integrated, often using AI-driven approaches, to identify and validate robust biomarkers.
Key Experimental Protocols in Multi-Omics Biomarker Discovery
Proteomics Workflow for Serum Biomarker Identification
The discovery of host- and parasite-derived protein biomarkers in serum is a prominent application of proteomics in parasitology. The following protocol, based on a study of Schistosoma japonicum infection in a rabbit model, outlines a standard label-free LC-MS/MS approach [45].
Figure 2: Detailed workflow for a serum proteomics experiment designed to identify biomarkers of parasitic infection.
Detailed Methodology:
Sample Collection and Preparation:
- Collect peripheral blood (e.g., from the ear vein in rabbit models) and allow it to clot at 37°C for 4 hours.
- Centrifuge at 200×g for 5 minutes to separate serum. Pool equal volumes of serum from biological replicates for each experimental group (e.g., pre-infection, post-infection, post-treatment) to create a representative sample.
- Store the pooled serum at -80°C until analysis [45].
Depletion of High-Abundance Proteins:
- Use a commercial kit (e.g., ProteoExtract Albumin/IgG Removal Kit) to remove highly abundant proteins like albumin and IgG. This step reduces sample complexity and allows for the detection of lower-abundance, potentially more informative, biomarker proteins [45].
Protein Digestion:
- Denature the serum proteins in a buffer containing 8 mM urea/40 mM NH₄HCO₃ with protease inhibitors.
- Reduce disulfide bonds by adding 10 mM dithiothreitol (DTT) and incubating for 60 minutes at room temperature.
- Alkylate the proteins with 20 mM iodoacetamide (IAM) for 45 minutes in the dark to prevent reformation of disulfide bonds.
- Perform a buffer exchange to dilute the urea concentration.
- Add Sequencing Grade Modified Trypsin for proteolytic digestion, which cleaves proteins into peptides for mass spectrometry analysis [45].
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS):
- Separate the resulting peptides using liquid chromatography.
- Analyze the eluted peptides by tandem mass spectrometry, which fragments the peptides to generate spectra for identification [45].
Data Analysis and Bioinformatic Validation:
- Search the acquired MS/MS spectra against relevant protein databases (e.g., host and parasite proteomes) using search engines like MaxQuant or SEQUEST.
- Perform label-free quantification to identify proteins that are significantly changed between different experimental groups.
- Conduct temporal analysis to identify proteins with coherent changes during infection and treatment, which are strong candidates for biomarkers. Use bioinformatics tools for functional enrichment analysis (e.g., Gene Ontology, KEGG pathways) to understand the biological processes implicated [45].
A Multi-Omics Approach for Biomarker Discovery
For a more comprehensive discovery pipeline, a multi-omics approach that integrates genomics and proteomics is increasingly employed.
Methodology:
Genomic Sequencing:
Proteomic Profiling:
- In parallel, conduct proteomic profiling as described in Section 3.1.
- Use the genomic data to create a customized protein sequence database (FASTA file), which improves the accuracy of peptide and protein identification in mass spectrometry data [49].
Data Integration:
- Integrate genomic and proteomic datasets to identify correlations between genetic variants and protein expression levels (e.g., quantitative trait loci mapping).
- Use machine learning algorithms to identify multi-omics signatures that are predictive of infection, species, disease severity, or treatment response. Neural networks and feature selection methods are particularly effective for integrating these diverse and high-volume data types [51].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful multi-omics research relies on a suite of specialized reagents, equipment, and computational resources.
Table 2: Essential Research Reagent Solutions for Multi-Omics Biomarker Discovery
| Category | Item/Kit | Function and Application |
|---|---|---|
| Sample Prep | ProteoExtract Albumin/IgG Removal Kit | Removes high-abundance proteins from serum/plasma to enhance detection of low-abundance biomarkers [45]. |
| Sequencing Grade Modified Trypsin | Proteolytic enzyme used to digest proteins into peptides for mass spectrometric analysis [45]. | |
| Dithiothreitol (DTT) & Iodoacetamide (IAM) | Reducing and alkylating agents, respectively; they break and cap disulfide bonds to prepare proteins for digestion [45]. | |
| Omics Analysis | Next-Generation Sequencers (e.g., Illumina) | Platforms for high-throughput genomic and transcriptomic sequencing [7]. |
| High-Resolution Mass Spectrometers (e.g., Thermo Fisher Orbitrap) | Instruments for precise mass measurement of peptides and metabolites, enabling proteomic and metabolomic profiling [45] [49]. | |
| Data & Bioinformatics | Multi-Omics Data Repositories (e.g., TCGA, OmicsDI) | Public databases providing access to curated multi-omics datasets for analysis and validation [47]. |
| Bioinformatic Pipelines (e.g., MaxQuant, Sequest) | Software tools for processing raw MS/MS data, including protein identification and quantification [45]. | |
| AI/ML Platforms (e.g., Python with Scikit-learn, TensorFlow) | Environments for developing machine learning models to integrate multi-omics data and identify predictive biomarker patterns [51]. | |
| 2-Methyleicosane | 2-Methyleicosane, CAS:52845-08-6, MF:C21H44, MW:296.6 g/mol | Chemical Reagent |
| Kutkoside | Kutkoside | High-purity Kutkoside, an iridoid glycoside fromPicrorhiza kurroa. For cancer and liver disease research (RUO). Not for human consumption. |
Case Studies and Applications in Parasitology
Schistosomiasis: Temporal Serum Proteomics
A 2021 study on Schistosoma japonicum exemplifies the power of proteomics. Researchers performed a label-free quantitative proteomic analysis of rabbit serum collected before infection, at 1 and 6 weeks post-infection, and at 5 and 7 weeks post-treatment with praziquantel. The study identified and quantified 10 parasite-derived proteins and 242 host-derived proteins with significant changes. Temporal analysis revealed coherent changes in proteins involved in receptor-mediated endocytosis, inflammatory response, and acute-phase response (e.g., mannan-binding lectin serine peptidase 1, immunoglobulins, collagen), providing a rich source of potential diagnostic and prognostic biomarkers for the disease [45].
Chagas Disease: A Multi-Parameter Serological Assay
The lack of a test of cure for Chagas disease has long impeded drug development. To address this, DNDi partnered with InfYnity Biomarkers to develop the MultiCruzi assay. This innovative serological assay can detect 15 different antibodies specific to the Trypanosoma cruzi parasite in a single patient blood sample. In a landmark finding, the assay demonstrated a decline in T. cruzi-specific antibodies in patients treated for Chagas disease after 6 and 12 months of follow-up—a first in adult chronic Chagas patients. This multi-parameter biomarker approach shows great promise as a tool for monitoring treatment efficacy and could significantly accelerate the development of new drugs [46].
Integrated multi-omics represents a paradigm shift in the approach to biomarker discovery for parasitic diseases. By moving beyond single-parameter tests to a holistic, systems biology framework, researchers can uncover complex, reproducible biomarker signatures that address the critical limitations of traditional diagnostics. The integration of genomics and proteomics, in particular, provides a powerful lens through which to view the intricate dance between host and parasite.
The future of this field is inextricably linked to advancements in artificial intelligence and machine learning, which are essential for managing the scale and complexity of multi-omics data [51]. Furthermore, the push towards field-ready platforms, such as portable sequencers and rapid diagnostic tests based on discovered biomarkers, will be crucial for translating these technological advances into real-world impact, especially in low-resource settings [52]. As these technologies mature and become more accessible, integrated multi-omics will undoubtedly play a central role in achieving definitive diagnosis and effective control of parasitic diseases worldwide.
Navigating Diagnostic Development: Overcoming Technical and Implementation Hurdles
Addressing Specificity and Cross-Reactivity in Serological and Molecular Assays
The definitive diagnosis of parasitic diseases represents a cornerstone of effective treatment, disease surveillance, and drug development. However, the accuracy of diagnostic outcomes is perpetually challenged by the issues of specificity and cross-reactivity in serological and molecular assays. Specificity refers to an assay's ability to correctly identify a target pathogen without responding to other organisms, while cross-reactivity occurs when antibodies or molecular probes bind to non-target antigens or gene sequences with similar epitopes or structures [53]. Within parasitology, these challenges are exacerbated by the close phylogenetic relationships between many parasites, shared antigenic determinants due to common life cycle stages, and the propensity of some protozoan infections to induce polyclonal B-cell activation [54] [53]. The substantial global health burden of parasitic diseases, with malaria alone causing over 600,000 deaths annually, underscores the critical need for diagnostic tools that deliver unambiguous results [8]. This technical guide examines the fundamental mechanisms behind specificity and cross-reactivity, evaluates current methodological approaches, and presents practical strategies to enhance diagnostic accuracy for researchers, scientists, and drug development professionals working in parasitology.
Fundamental Mechanisms of Antibody-Antigen Interactions
The molecular basis of cross-reactivity lies in the nature of antibody-antigen interactions. An epitope, typically comprising approximately 15 amino acids on the antigen's surface, serves as the antibody binding site, with about 5 of these amino acids contributing most of the binding energy [53]. Conversely, the paratope on the antibody involves approximately 15 variable amino acids that physically contact the epitope [53]. This structural relationship explains why antibodies raised against a specific parasite may recognize different parasites sharing similar epitopes.
Several key factors influence these interactions:
- Polyclonal B-cell proliferation: Certain protozoan infections of the reticuloendothelial system, including human African trypanosomiasis and visceral leishmaniasis, can induce widespread B-cell activation, leading to the production of antibodies with broad reactivity that increase potential cross-reactivity in serological assays [54].
- Low-affinity binding: Under favorable binding conditions, antibodies with low affinity may bind to a broader set of complementary partners, reducing specificity [53].
- Shared epitopes among parasites: Phylogenetically related parasites often conserve antigenic proteins, particularly structural proteins or essential enzymes, creating shared epitopes that antibodies may not distinguish [55].
Table 1: Factors Contributing to Cross-Reactivity in Parasitic Disease Diagnostics
| Factor | Mechanism | Example |
|---|---|---|
| Polyclonal B-Cell Activation | Non-specific antibody production during reticuloendothelial protozoan infections | Reduced specificity of SARS-CoV-2 assays in human African trypanosomiasis (88%) and visceral leishmaniasis (80%) [54] |
| Conserved Antigenic Determinants | Shared epitopes among phylogenetically related parasites | Antigenic similarity between Plasmodium species leading to cross-reactive antibodies in malaria diagnostics |
| Assay Format and Conditions | Variable binding affinities under different reagent concentrations and formats | Up to 5-fold difference in cross-reactivity between ELISA and FPIA formats using identical antibodies [56] |
Cross-Reactivity in Serological Assays: Evidence and Implications
Serological assays remain widely used for parasitic disease diagnosis despite documented challenges with cross-reactivity. A comprehensive assessment of SARS-CoV-2 antibody detection assays among pre-pandemic sera from individuals with parasitic infections revealed specificity concerns particularly pronounced in specific parasitic diseases [54]. The study evaluated three distinct assay formats detecting different analytes: the cPass neutralization antibody detection kit (anti-RBD antibodies), Abbott SARS-CoV-2 IgG assay (anti-nucleocapsid IgG), and Standard Q COVID-19 IgM/IgG combo (anti-nucleocapsid IgM and IgG).
Table 2: Specificity of SARS-CoV-2 Serological Assays in Various Parasitic Infections
| Parasitic Infection | Assay Type | Specificity (%) | 95% CI |
|---|---|---|---|
| Human African Trypanosomiasis | Abbott Architect IgG | 88 | 75-95 |
| Visceral Leishmaniasis | Standard Q IgG | 80 | 30-99 |
| Hyperendemic Malaria (Senegal) | Abbott Architect IgG | 91 | Not specified |
| Hyperendemic Malaria (Senegal) | cPass | 98-99 | Not specified |
| Helminth Infections (Overall) | Multiple Assays | ≥96 | Not specified |
The data demonstrates that specificity varies significantly based on both the parasite and the assay format. Infections causing substantial immune activation, such as human African trypanosomiasis and visceral leishmaniasis, show markedly reduced specificity [54]. Importantly, the majority (>85%) of false-positive reactions occurred with only one assay, suggesting that confirmatory testing with a second, independent assay can dramatically improve diagnostic accuracy [54].
Methodological Approaches to Enhance Specificity
Serological Technique Advancements
Enzyme-Linked Immunosorbent Assay (ELISA) remains a cornerstone of parasitic serology, with continuous refinements enhancing its specificity. The use of recombinant antigens rather than whole parasite lysates has significantly reduced cross-reactivity by focusing on pathogen-specific epitopes [57]. For Toxoplasma gondii detection, recombinants antigens such as GRA2, MAG1, SAG1, and GRA7 have been employed to increase binding specificity of IgG and IgM antibodies [57]. The IgG avidity test represents another important innovation, distinguishing recent from past infections by measuring antibody binding strength, which matures over time [58] [57].
Western blot (immunoblot) continues to serve as an important confirmatory test, particularly for congenital toxoplasmosis diagnosis, by detecting antibodies against specific molecular weight bands of T. gondii antigenic proteins [57]. While commercial Western blot kits are available, they may demonstrate relatively lower sensitivity compared to other diagnostic techniques [57].
Rapid diagnostic tests (RDTs), particularly lateral flow immunoassays, have become invaluable in resource-limited settings. When properly designed with specific antigens, they can approach the specificity of laboratory-based assays. Research has demonstrated that one IgG-detecting RDT showed similarly high specificity to laboratory-based assays for SARS-CoV-2 antibody detection in populations with parasitic infections [54].
Molecular Diagnostics
Molecular methods have substantially addressed many cross-reactivity challenges through precise target sequence recognition. Polymerase chain reaction (PCR) and its variants, including nested PCR, real-time PCR, and multiplex PCR, amplify parasite-specific DNA sequences, virtually eliminating cross-reactivity when primers are carefully designed [8] [57]. Loop-mediated isothermal amplification (LAMP) offers similar specificity with technical simplicity suitable for field applications [57].
Advanced molecular techniques further enhance specificity:
- PCR-restriction fragment length polymorphism (PCR-RFLP): Combines amplification with restriction enzyme digestion to create species-specific banding patterns [57].
- Next-generation sequencing (NGS): Provides comprehensive pathogen identification without cross-reactivity by sequencing all genetic material in a sample [8].
- CRISPR-Cas systems: Leverage the precision of guide RNAs to identify parasite-specific DNA or RNA sequences, enabling highly specific detection with minimal cross-reactivity [8].
Emerging Technologies
Nanotechnology applications in diagnostics utilize the unique properties of nanoparticles to create highly specific detection platforms. Nano-biosensors and magnetic isolation devices functionalized with parasite-specific antibodies or DNA probes can selectively capture and detect pathogens while minimizing non-specific binding [8].
Multi-omics integration combines data from genomics, transcriptomics, proteomics, and metabolomics to identify novel, highly specific biomarker combinations for parasitic detection [8]. This approach moves beyond single-molecule detection to create multifaceted pathogen signatures that dramatically reduce false positives.
Artificial intelligence applied to imaging analysis represents another advancement, with machine learning algorithms trained to recognize parasite-specific morphological patterns in blood smears or tissue samples, reducing observer variability and misidentification [8].
Experimental Protocols for Specificity Assessment
Protocol for Evaluating Cross-Reactivity in Serological Assays
Purpose: To systematically assess cross-reactivity of a serological assay against phylogenetically related parasites and other pathogens known to cause similar clinical presentations.
Materials:
- Test sera from confirmed cases of target parasitic infection (n≥50)
- Sera from patients with related parasitic infections (n≥30 each)
- Sera from healthy endemic controls (n≥100)
- Reference standard (gold standard) assay
- Equipment: ELISA plate reader, microplate washer, incubator
Procedure:
- Coat microplate wells with target antigen (recommended: recombinant antigens for higher specificity) in carbonate-bicarbonate buffer, incubate overnight at 4°C
- Block plates with 5% non-fat milk or BSA in PBS for 2 hours at room temperature
- Add test and control sera in duplicate across dilution series (typically 1:50 to 1:6400)
- Incubate plates for 1 hour at 37°C, then wash 5 times with PBS-Tween
- Add enzyme-conjugated secondary antibody (species-specific) diluted in blocking buffer
- Incubate for 1 hour at 37°C, wash as before
- Add enzyme substrate, incubate for specified time, stop reaction
- Read optical density and calculate results relative to cut-off values
Analysis: Calculate cross-reactivity percentage using the formula:
CR% = (IC50 of target analyte / IC50 of cross-reactant) × 100
where IC50 represents the concentration causing 50% signal inhibition in competitive formats [56]. For non-competitive assays, use the concentration giving equivalent positive signal.
Protocol for Molecular Assay Specificity Validation
Purpose: To verify that molecular detection methods specifically identify target parasites without cross-reacting with genetically similar organisms.
Materials:
- DNA extracts from target parasite and related species
- Clinical samples from patients with confirmed infections
- DNA extraction kit, PCR reagents, thermal cycler, gel electrophoresis system
- Real-time PCR system (if applicable)
Procedure:
- Design primers targeting species-specific genetic regions (e.g., unique ribosomal RNA sequences, repetitive elements, or specific virulence genes)
- Perform BLAST analysis to confirm theoretical specificity against all available sequences
- Extract DNA from reference samples using standardized protocols
- Run PCR amplification with DNA from target and non-target parasites
- Analyze products by gel electrophoresis for expected size confirmation
- For real-time PCR, establish cycle threshold (Ct) values for target and non-target organisms
- Sequence amplification products from representative samples to confirm specificity
Analysis: True specificity is confirmed when amplification occurs only with the target parasite DNA, with no detectable amplification with non-target organisms, even at low Ct values or high template concentrations.
Visualization of Specificity Enhancement Strategies
Diagram 1: Diagnostic Strategy for Enhanced Specificity
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Specificity Optimization
| Reagent/Category | Specific Function | Application Notes |
|---|---|---|
| Recombinant Parasite Antigens | Target specific immunodominant proteins; reduce cross-reactivity from shared epitopes in crude lysates | GRA7, SAG1 for Toxoplasma; MSP1 for Plasmodium; K39 for Leishmania [57] |
| Monoclonal Antibodies | Recognize single epitopes; minimize polyclonal cross-reactivity | Select clones with confirmed species specificity through extensive cross-testing [56] |
| Species-Specific Primers/Probes | Amplify unique genomic regions; essential for molecular specificity | Design targeting multi-copy genes or unique sequences; verify with in silico analysis [57] |
| CRISPR-Cas Systems | Programmable nucleic acid detection with single-base resolution; minimal cross-reactivity | Cas12a, Cas13 systems for parasitic DNA/RNA detection; combined with isothermal amplification [8] |
| Reference Standard Panels | Validate assay performance across parasite species | Should include target parasite, phylogenetically related species, and common co-infections [54] |
| Bismerthiazol | Bismerthiazol, CAS:79319-85-0, MF:C5H6N6S4, MW:278.4 g/mol | Chemical Reagent |
The challenges of specificity and cross-reactivity in serological and molecular assays for parasitic diseases demand multifaceted solutions grounded in understanding fundamental immunological and molecular principles. The evidence demonstrates that assay specificity varies significantly across different parasitic infections, with particular concerns in diseases causing polyclonal B-cell activation such as human African trypanosomiasis and visceral leishmaniasis [54]. Strategic implementation of recombinant antigens, monoclonal antibodies, species-specific molecular targets, and confirmatory testing algorithms can substantially enhance diagnostic accuracy. Emerging technologies including CRISPR-based detection, nanotechnology applications, and multi-omics approaches offer promising avenues for further specificity improvements. For researchers and drug development professionals, rigorous validation using comprehensive reference panels that include target parasites and phylogenetically related species remains essential for assessing true clinical performance. As parasitic diagnostics continue evolving, the integration of multiple methods and targets will be crucial for achieving the specificity required for definitive diagnosis, effective treatment monitoring, and successful drug development programs.
Mitigating Biological Matrix Interference in Complex Patient Samples
The definitive diagnosis of parasitic diseases is a critical public health challenge, particularly in tropical and subtropical regions where these infections significantly impact millions of people [7] [9]. Accurate diagnosis is essential for effective treatment, disease control, and surveillance, yet clinical diagnosis is often complicated as parasitic diseases frequently do not produce characteristic symptoms [3]. The diagnostic process is further confounded by the phenomenon of biological matrix interference, which can compromise the accuracy, reproducibility, and sensitivity of diagnostic tests [59] [60]. Matrix interference occurs when extraneous components within a patient sample—such as proteins, lipids, salts, carbohydrates, or metabolites—interfere with the detection or quantification of a target analyte, leading to ion suppression or enhancement in mass spectrometry, disrupted antibody binding in immunoassays, and ultimately, unreliable clinical data [59] [61] [62].
Within the framework of parasitic disease research, mitigating matrix interference is not merely an analytical exercise but a fundamental prerequisite for achieving reliable diagnosis. The complex life cycles of many parasites and the potential for co-infections necessitate diagnostic tools with the highest possible specificity and sensitivity [9] [3]. Traditional diagnostic methods like microscopy, while foundational, can be time-consuming and require a high level of expertise [7]. The evolution towards more advanced serological and molecular methods, including Enzyme-Linked Immunosorbent Assay (ELISA), Polymerase Chain Reaction (PCR), and tandem mass spectrometry (MS/MS), has remarkably enhanced detection capabilities [7] [9]. However, these advanced techniques are particularly vulnerable to the confounding effects of complex sample matrices such as serum, plasma, urine, and feces [59] [3]. Therefore, understanding and controlling for matrix effects is an invaluable component of diagnostic accuracy, enabling a comprehensive understanding of parasite biology and the discovery of new therapeutic targets and diagnostic biomarkers [7].
Understanding and Detecting Matrix Effects
Matrix effects are primarily caused by endogenous and exogenous substances found in biological samples. Endogenous substances include salts, phospholipids, triglycerides, urea, amines, and metabolites, while exogenous substances can include anticoagulants (like Li-heparin), plasticizers (like phthalates), and mobile phase additives [59]. The composition of these interfering components varies significantly between different biological matrices, as outlined in Table 1, necessitating tailored management strategies for each sample type [59].
Table 1: Common Components in Selected Biological Matrices that Contribute to Matrix Effects
| Components | Plasma/Serum | Urine | Breast Milk |
|---|---|---|---|
| Ions | Na+, K+, Ca2+, Cl-, Mg2+ | Na+, K+, Ca2+, Cl-, NH4+, Sulfates | Calcium, Chloride, Potassium, Sodium, Trace minerals |
| Organic Molecules | Urea, Creatinine, Uric Acid, Glucose, Bilirubin | Urea, Creatinine, Uric Acid, Citrate, Amino Acids | Lactose, Glucose, Urea, Uric Acid, Carotenoids |
| Proteins | Albumins, Globulins, Fibrinogen | Immunoglobulins, Albumin | Albumins, Immunoglobulins, Caseins, Glycoproteins |
| Lipids | Phospholipids, Cholesterol, Triglycerides | - | Triglycerides, Essential Fatty Acids, Phospholipids |
| Others | Water-soluble vitamins | - | Fat-soluble and Water-soluble vitamins |
The mechanisms of interference are technique-dependent. In Liquid Chromatography-Mass Spectrometry (LC-MS/MS), which is widely used for quantitative analysis, matrix components can co-elute with the target analyte and disrupt its ionization in the mass spectrometer, a phenomenon known as ion suppression or, less commonly, ion enhancement [59] [60]. Electrospray Ionization (ESI) is particularly susceptible to this because matrix components can compete for available charges in the liquid phase or alter droplet formation efficiency [59]. In immunoassays, matrix interference can skew results when interfering components prevent the target analyte from binding properly to capture or detection antibodies, leading to inaccurate concentration measurements [61] [62]. Factors such as sample viscosity, pH imbalances, and high salt concentrations can also contribute to these effects [62].
Detection and Assessment Methods
Before mitigation strategies can be applied, it is crucial to detect and quantify the presence and extent of matrix effects. Two primary methods are commonly used for this purpose.
Post-Extraction Spike Method (for LC-MS/MS and Immunoassays): This quantitative method involves comparing the signal response of an analyte spiked into a neat mobile phase or dilution buffer versus the same amount of analyte spiked into a blank, pre-processed sample matrix [60] [62]. The difference in response indicates the extent of the matrix effect. The results are often expressed as percent recovery, calculated with the formula: Percent Recovery = (Spiked Sample Concentration – Sample Concentration) / Spiked Standard Diluent Concentration × 100 [62]. While 100% recovery is ideal, acceptable recovery typically falls between 80-120%; recovery outside this range indicates significant matrix interference [62].
Post-Column Infusion Method (for LC-MS/MS): This qualitative technique involves infusing a constant flow of analyte into the HPLC eluent post-column while injecting a blank, processed sample extract [60]. A dip or rise in the baseline signal of the infused analyte indicates regions in the chromatogram where ion suppression or enhancement is occurring due to co-eluting matrix components [60]. This method helps in developing methods that shift the analyte's retention time away from these interference regions.
Strategies for Mitigating Matrix Interference
A multi-faceted approach is required to effectively manage matrix interference. The following strategies, often used in combination, form the cornerstone of robust analytical methods.
Sample Preparation Techniques
Effective sample preparation is the first line of defense against matrix interference. The goal is to remove interfering components while efficiently recovering the target analyte.
- Dilution: Simple sample dilution can reduce the concentration of interfering components to a level where they no longer significantly impact the assay [61] [62]. This strategy is particularly effective when the analytical method is highly sensitive [60].
- Protein Precipitation (PPT): Commonly used for plasma and serum, PPT involves adding an organic solvent to precipitate proteins, which are then removed by centrifugation. While simple and fast, it may not remove all phospholipids, which are a major cause of ion suppression in LC-MS [63].
- Solid-Phase Extraction (SPE): This technique uses cartridges with various sorbents to selectively isolate and concentrate analytes while washing away impurities. SPE is highly effective for cleaning up samples and can be optimized for specific analyte classes [63]. It is especially useful for preconcentrating analytes from large-volume aqueous samples [63].
- Solid-Phase Microextraction (SPME): SPME uses a fiber coated with a stationary phase to extract volatiles and non-volatiles from liquid or gas matrices, with minimal or no solvent [63]. It is ideal for on-site sample collection and can be automated.
- Liquid-Liquid Extraction (LLE): This method partitions analytes and interferences between two immiscible liquids based on solubility. It is effective for removing salts and polar interferences [63].
- Filtration and Centrifugation: These are fundamental steps for clarifying samples and removing particulate matter that could compromise the analytical instrumentation [64] [63].
- Derivatization: This process chemically modifies the analyte to make it more amenable to analysis by, for example, increasing its volatility for GC or improving its ionization efficiency for MS [63]. It can also be used to "trap" reactive analytes, preventing them from being lost [63].
The following workflow diagram illustrates a logical decision process for selecting and applying these mitigation strategies.
Analytical and Calibration Approaches
Even with diligent sample preparation, residual matrix effects may persist. The following analytical and calibration techniques are critical for compensating these effects.
- Chromatographic Optimization: Modifying chromatographic conditions, such as using a different column chemistry, adjusting the mobile phase gradient, or extending the run time, can separate the analyte from co-eluting matrix components, thereby reducing ionization effects in LC-MS [60].
- Internal Standardization: This is the gold standard for correcting matrix effects in quantitative LC-MS.
- Stable Isotope-Labeled Internal Standards (SIL-IS): These are chemically identical to the analyte but contain heavier isotopes (e.g., ²H, ¹³C, ¹âµN). They co-elute with the analyte and experience nearly identical ionization suppression, allowing for perfect compensation. Nitrogen-15 (¹âµN) and carbon-13 (¹³C) labeled internal standards are often preferred over deuterated standards to eliminate deuterium isotope effects that can cause slight retention time shifts [63] [60].
- Structural Analogues: If a SIL-IS is unavailable or too costly, a co-eluting structural analogue can be used as an internal standard, though it is generally less effective at compensating for matrix effects [60].
- Standard Addition Method: This technique involves spiking the patient sample with known, increasing concentrations of the target analyte and plotting the resulting signal responses [60]. The concentration of the analyte in the original sample is determined by extrapolating the calibration line back to the x-axis. This method is particularly useful for endogenous analytes where a blank matrix is unavailable [60].
- Matrix-Matched Calibration: Creating standard curves by spiking the analyte into the same biological matrix as the experimental samples can help account for matrix effects during calibration [61]. However, it can be challenging to obtain a truly "blank" matrix, and matrix composition can vary significantly between individual samples [60].
Table 2: Key Experimental Protocols for Mitigating Matrix Interference
| Method | Protocol Summary | Key Considerations |
|---|---|---|
| Post-Extraction Spike [60] [62] | 1. Prepare a set of blank matrix samples and process them.2. Spike with a known concentration of analyte post-processing.3. Compare the signal to an equivalent standard in neat solution.4. Calculate % Recovery. | Requires a blank matrix. Acceptable recovery is 80-120%. Simple and quantitative. |
| Standard Addition [60] | 1. Split the patient sample into several aliquots.2. Spike increasing known amounts of analyte into all but one aliquot.3. Analyze all aliquots and plot signal vs. spiked concentration.4. Extrapolate the line to the x-axis to find the original sample concentration. | Does not require a blank matrix. Time-consuming for large sample sets. Ideal for unique matrices. |
| Solid-Phase Extraction [63] | 1. Condition the SPE sorbent with solvent.2. Load the sample onto the cartridge.3. Wash with a solvent to remove impurities.4. Elute the analyte with a strong solvent.5. Evaporate and reconstitute for analysis. | Effective for preconcentration and cleaning. Choice of sorbent is critical for selectivity. Can be automated. |
| Sample Dilution [61] [62] | 1. Prepare a series of sample dilutions using the assay's dilution buffer.2. Analyze the diluted samples.3. Identify the dilution factor where the measured concentration becomes consistent and falls within the assay's dynamic range. | The simplest strategy. Must not dilute the analyte below the limit of quantification. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful management of matrix interference relies on a set of key reagents and materials. The following table details these essential tools.
Table 3: Research Reagent Solutions for Managing Matrix Interference
| Item | Function & Application |
|---|---|
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Co-elutes with the analyte and corrects for ionization suppression/enhancement in LC-MS and variations in sample preparation; the gold standard for quantitative bioanalysis [63] [60]. |
| Solid-Phase Extraction (SPE) Cartridges | Used for selective sample clean-up and preconcentration; available with a wide range of sorbents (e.g., C18, ion-exchange, mixed-mode) to target specific analyte classes and remove interferences [63]. |
| Phospholipid Removal Plates | A specialized form of SPE designed to selectively remove phospholipids from plasma and serum samples, a major source of ion suppression in LC-ESI-MS [59]. |
| Sample Dilution Buffer | A buffered solution used to dilute samples, reducing the concentration of interfering components to a non-influential level; composition is often optimized for specific immunoassays [61] [62]. |
| Blocking Agents (e.g., BSA, Non-fat Milk) | Added to assay buffers to mitigate nonspecific binding in immunoassays, thereby reducing background noise and improving signal-to-noise ratio [61]. |
| Derivatization Reagents | Chemicals used to modify the functional groups of an analyte to improve its chromatographic behavior, volatility, or detectability [63]. |
The accurate and precise diagnosis of parasitic diseases is a cornerstone of global health efforts, directly impacting treatment efficacy, disease surveillance, and the development of new interventions [7] [3]. As the field moves beyond basic microscopy toward sophisticated serological and molecular methods, the challenge of biological matrix interference becomes increasingly central to the validity of research and clinical findings [9]. Mitigating these effects is not a single-step process but a comprehensive strategy that begins with thoughtful sample collection and processing [64], extends through rigorous sample preparation [63], and is finalized with optimized analytical methods and appropriate calibration techniques, notably the use of stable isotope-labeled internal standards [60]. By systematically implementing these practices, researchers and drug development professionals can ensure that the data generated on parasite biomarkers, drug concentrations, and immune responses are a true reflection of biological reality, thereby strengthening the entire chain of evidence in the definitive diagnosis of parasitic diseases.
Strategies for Standardization and Reproducibility Across Laboratory Settings
In the field of parasitic disease research, the definitive diagnosis of pathogens represents a fundamental challenge that relies entirely on reproducible laboratory findings. A reproducibility crisis challenges the validity and reliability of scientific findings across various domains, with particular significance in biological research where experimental complexity is high [65]. For parasitic diseases, clinical diagnosis is often difficult because these pathogens do not produce characteristic symptoms, making laboratory confirmation essential [3]. Correct diagnosis involves not only determining the presence of a parasite but also establishing a causal relationship between parasite invasion and disease symptoms, a process that demands exceptional methodological consistency [3]. Successfully managing these factors ensures that results generated in one laboratory are not only scientifically sound but also consistently attainable by any competent biological laboratory using the same methodology, thereby strengthening the foundation of translational science and accelerating therapeutic development [65].
The diagnostic process for parasitic infections must consider the possibility of coinfection with several parasites simultaneously, requiring diagnostics to be planned with consideration of their frequency in each population and the local epidemiological situation [3]. This complexity underscores why addressing reproducibility requires rigorous adherence to technical standards and systematic process controls. For researchers, clinicians, and drug development professionals working with parasitic diseases, implementing robust standardization strategies transcends mere methodological preference—it represents a professional imperative that directly impacts diagnostic accuracy, treatment efficacy, and ultimately, patient outcomes in populations affected by these widespread infections.
Methodological Standardization: The Foundation of Reliable Diagnostics
Standard Operating Procedures (SOPs) for Parasitology
Defining explicit, step-by-step methods eliminates variation that compromises data quality in parasitic disease research. Methodological standardization serves as the cornerstone for improving reproducibility by mitigating subjective interpretation and non-systematic execution [65]. Standard Operating Procedures (SOPs) must detail every critical step, from sample preparation through final diagnostic analysis, with laboratory personnel treating the SOP as the authoritative reference for all procedures to establish an immutable protocol for the entire workflow [65].
For parasitic disease diagnostics specifically, key elements for robust SOPs should include:
- Instrumentation and calibration: Specify make, model, and serial number of equipment, alongside defined calibration and maintenance schedules for microscopes, PCR machines, and other diagnostic instruments.
- Environmental controls: Document temperature, humidity, and storage conditions for samples and reagents.
- Timing of steps: Establish precise incubation periods, staining durations, and processing times.
- Reagent preparation: Define molarity, solution formulas, preparation dates, and specific lot numbers used in validation of stains, buffers, and molecular biology reagents [65].
Formal guidance from organizations such as the Clinical and Laboratory Standards Institute (CLSI) provides comprehensive quality management and method validation standards, offering an industry-recognized benchmark for procedural rigor [65]. Adopting such guidelines promotes consistent methodological expectations across laboratories, allowing other researchers to replicate diagnostic procedures precisely and assess findings from parasitic disease research with greater confidence.
Experimental Protocols for Parasitic Disease Diagnostics
The experimental protocol functions as a detailed recipe for conducting diagnostic procedures. Each experimenter responsible for discrete data-collection initiatives must write a script sufficiently thorough that a trained researcher unfamiliar with the specific project could execute it correctly using the script alone [66]. For parasitic diagnostics, this becomes particularly important when dealing with the variety of available testing methodologies.
Comprehensive diagnostic protocols for parasitic diseases should encompass several critical phases:
- Pre-analytical phase: Specifies sample collection methods, appropriate containers, preservation techniques, transport conditions, and acceptance/rejection criteria for specimens.
- Analytical phase: Details specific diagnostic procedures, including microscopy techniques (concentration methods, staining protocols), molecular methods (DNA extraction, amplification conditions), immunological assays (ELISA protocols), and quality control measures.
- Post-analytical phase: Defines result interpretation criteria, reporting formats, and reference ranges [67] [3].
For parasitology research, special attention must be paid to specimen-specific considerations. For example, the CDC recommends that three or more stool samples, collected on separate days, be examined for ova and parasite testing to improve detection sensitivity [67]. Protocols should explicitly state such requirements rather than assuming researcher awareness.
Table 1: Key Components of Diagnostic Protocols for Parasitic Diseases
| Protocol Component | Essential Elements | Parasitology-Specific Considerations |
|---|---|---|
| Sample Collection | Container type, preservation method, transport conditions | Multiple samples over separate days for stool exams [67] |
| Microscopy Methods | Staining procedures, magnification, examination time | Concentration techniques, oil immersion examination |
| Molecular Diagnostics | DNA extraction method, primer sequences, amplification conditions | Target genes for specific parasites, inhibition controls |
| Quality Control | Positive/negative controls, competency assessments | Reference specimens, inter-laboratory comparisons |
Research Reagent and Material Management
Reagent Validation and Sourcing in Parasitology
Variability in essential reagents represents a major threat to reproducibility in parasitic disease research. Laboratory personnel must implement stringent qualification and tracking protocols for all critical diagnostic reagents before use in experimental workflows [65]. This is particularly crucial in parasitology, where subtle differences in staining solutions, culture media, or molecular biology reagents can fundamentally alter diagnostic outcomes.
Effective reagent management for parasitic disease diagnostics requires attention to three critical areas:
- Sourcing documentation: Document the supplier, lot number, date of receipt, and storage conditions for every batch of critical reagents including stains, antibodies, primers, and culture media.
- Functional validation: Before using a new batch or lot, perform functional tests using established positive and negative control samples to ensure the reagent performs as expected. For instance, testing a new lot of staining solution against known positive and negative samples confirms diagnostic performance [65].
- Parasite material authentication: Maintain reference parasite strains with periodic authentication through morphological, molecular, or other characteristic identification methods to ensure the integrity of the biological research [65].
Implementing these validation checkpoints drastically reduces the introduction of uncontrolled variables, which in turn elevates the quality of diagnostic data and strengthens the potential for reproducibility across different laboratory settings.
Table 2: Essential Research Reagent Solutions for Parasitic Disease Diagnostics
| Reagent/Material | Function in Parasitology | Validation Requirements |
|---|---|---|
| Staining Solutions (e.g., Trichrome, Kinyoun) | Differentiation of parasitic structures in microscopic examination | Test with known positive and negative control slides each batch |
| Antibodies for Serological Tests | Detection of parasite-specific antigens or antibodies | Verify specificity and sensitivity with reference serum panels |
| PCR Master Mixes and Primers | Amplification of parasite DNA in molecular diagnostics | Validate with control DNA, check for cross-reactivity |
| Culture Media | In vitro propagation of parasites for study | Quality control for growth support with reference strains |
| Fecal Concentration Solutions | Enhancement of parasite detection in stool samples | Compare recovery rates with established methods |
Data Management and Documentation Protocols
Data Integrity and Transparency Standards
Achieving reproducibility extends beyond the bench to the management and interpretation of generated data. A robust data management system ensures data integrity, accessibility, and transparency, which are non-negotiable for high-quality research on parasitic diseases [65]. Poorly organized or inaccessible data archives prevent replication and validation of the original diagnostic findings, particularly problematic when dealing with emerging parasitic infections or evaluating new diagnostic methodologies.
Key principles for data integrity and management in parasitic disease research include:
- Metadata capture: Log all relevant information automatically, including instrument settings, sample identifiers, operator details, and date/time stamps. This contextual information is vital for understanding and recreating the experimental conditions, especially when comparing diagnostic sensitivity across different studies [65].
- Electronic lab notebooks (ELNs): Mandate the use of ELNs to replace paper records, enabling real-time documentation, secure backup, and detailed version control. ELNs establish a traceable chain of custody for all raw data, which is particularly important when documenting rare parasitic findings or unusual morphological characteristics [65] [68].
- Adherence to FAIR principles: Data must be Findable, Accessible, Interoperable, and Reusable. Structuring data according to these principles allows automated systems and other researchers to readily locate, understand, and apply datasets related to parasitic diseases [65].
- Statistical transparency: Define statistical methods and exclusion criteria a priori. Report exact p-values, effect sizes, and raw data distributions. Doing this, rather than just using summary statistics, allows others to re-analyze the data and confirm the conclusions drawn from parasitic disease research [65].
Visual Data Representation for Parasitology Research
Effective data visualization represents a critical component of reproducible research, particularly in parasitology where diagnostic findings may include morphological characteristics, molecular data, and epidemiological patterns. Selecting appropriate comparison charts enhances understanding and facilitates accurate interpretation of complex parasitic disease data [69].
For parasitology research, several visualization approaches prove particularly valuable:
- Bar charts: Ideal for comparing prevalence rates of different parasites across populations or diagnostic yield of different methods [69].
- Line charts: Effective for displaying trends in parasite incidence over time or diagnostic sensitivity across different analyte concentrations [69].
- Microscopy images with scale bars: Essential for documenting morphological findings with appropriate magnification indicators.
- Electrophoresis gel images: Require proper labeling and molecular weight markers for interpretability.
When creating visual representations of data, prioritizing clarity is essential. This involves removing unnecessary elements, ensuring titles and labels for categories and data points are clear and concise, using appropriate scaling that allows for clear differentiation between variables, and maintaining consistency in colors, fonts, and design elements [69].
Quality Assurance and Personnel Competency
Comprehensive Quality Management Systems
Quality assurance (QA) and quality control (QC) in laboratories working with parasitic diseases demand constant vigilance and proactive management. QA defines the processes and standards that prevent errors from occurring (e.g., reagent qualification and SOP generation), while QC focuses on the operational techniques used to detect errors after they happen (e.g., running positive/negative controls and evaluating instrument performance checks) [65]. For parasitic diagnostics, this distinction is crucial—while QA establishes the system for correct diagnosis, QC verifies that each diagnostic procedure performs as expected.
The laboratory must establish scheduled reviews of all SOPs and conduct periodic, documented competency assessments for all personnel on complex or high-variability procedures such as morphological identification of parasites or interpretation of molecular diagnostic results [65]. Only when laboratory professionals consistently execute procedures according to validated standards, and when quality checks yield expected results, does the laboratory truly achieve the level of control necessary for ensuring reproducibility in parasitic disease research. This commitment to documented training and competency verification minimizes the human factor as a source of experimental variation, which is particularly important in parasitology where subjective interpretation can influence diagnostic outcomes.
Personnel Training and Protocol Validation
The skills and consistent execution by laboratory personnel significantly influence reproducibility in parasitic disease diagnostics. Even the most detailed SOPs fail if operators lack the necessary training or deviate from the protocol [65]. A comprehensive training program, paired with meticulous documentation, forms a critical pillar of any quality management system in biological research [65]. Training programs must include initial certifications, annual refreshers, and direct observation of performance for high-variability techniques such as parasite identification.
Documenting training records provides an auditable history of the technical expertise applied to each diagnostic procedure. Furthermore, a culture of quality encourages proactive identification and correction of potential procedural weaknesses [65]. For parasitology specifically, this should include regular testing with blinded proficiency samples to maintain diagnostic skills, particularly for morphological identification of rare parasites or interpretation of ambiguous serological results.
New diagnostic protocols must always be tested and potentially revised before implementation in research studies. The validation process should include:
- Initial self-testing: Researchers run through the protocol themselves to identify gaps in documentation.
- Peer validation: Another lab member performs the procedure using only the written protocol.
- Supervised implementation: A senior researcher observes the protocol in practice with naive samples [66].
This rigorous validation approach ensures that diagnostic protocols for parasitic diseases produce reliable, consistent results across different operators and laboratory settings, ultimately supporting the broader thesis that definitive diagnosis depends on standardized, reproducible methodologies.
Visual Workflows for Standardization and Diagnostic Processes
The following diagrams illustrate key standardization strategies and diagnostic workflows for parasitic disease research, created using DOT language with adherence to the specified color palette and contrast requirements.
Parasitic Disease Diagnostic Workflow with Integrated Quality Control
Quality Management System for Laboratory Standardization
A structured approach to methodological control, reagent validation, data management, and personnel training drives scientific progress in parasitic disease research. Enhancing reproducibility is not merely an aspirational goal but a professional imperative that demands institutional commitment and systematic process implementation from laboratory professionals [65]. Adopting comprehensive quality management principles safeguards the integrity of diagnostic findings and accelerates the translation of discovery into meaningful scientific advances and improved patient care.
The challenges in parasitic disease diagnostics—including non-specific symptoms, possibility of co-infections, and requirement for specialized detection methods—make standardization particularly crucial for this field [3]. By implementing the strategies outlined in this technical guide, researchers can strengthen the reliability of their findings, promote scientific rigor, and contribute to the definitive diagnosis that forms the foundation for effective treatment and control of parasitic diseases worldwide. This commitment to reproducibility ultimately supports the broader thesis that advancing our understanding and management of parasitic infections depends fundamentally on consistent, standardized approaches across laboratory settings.
Challenges in Mass Production, Cost-Effectiveness, and PoC Integration
The definitive diagnosis of parasitic diseases is a cornerstone of global public health, directly impacting the management of illnesses that affect millions, particularly in developing regions [7] [8]. For decades, diagnosis has relied on traditional methods such as microscopy, serological testing, and histopathology. While helpful, these techniques are often time-consuming, require specialized expertise and laboratory infrastructure, and can exhibit limited sensitivity and specificity [7] [8]. The evolution toward Point-of-Care (PoC) testing promises a paradigm shift by enabling rapid, accurate, and early detection of infections at or near the patient site, which is crucial for timely treatment and effective disease control [70] [8].
However, the integration of advanced diagnostic technologies into practical, widespread PoC formats faces significant hurdles. This whitepaper examines the tripartite challenge of mass production, cost-effectiveness, and successful PoC integration for parasitic disease diagnostics. We will explore how innovations in molecular methods, nanotechnology, and artificial intelligence (AI) are pushing the boundaries of sensitivity and specificity, while simultaneously introducing complexities in manufacturing and economic viability [7] [71]. The path from laboratory innovation to a deployable, affordable, and reliable product is fraught with technical and economic constraints that must be addressed to realize the full potential of modern parasitology diagnostics [70].
Technical Hurdles in Mass Production
The scaling of diagnostic technologies from benchtop prototypes to mass-produced devices presents a multitude of intricate challenges. A primary obstacle lies in the integration of complex assays into simple, self-contained, and automated formats that are usable in non-laboratory settings [70]. This often requires sophisticated microfluidics for fluid handling, sample processing, signal amplification, and detection to function seamlessly as a unified system [70]. The manufacturing of these integrated microfluidic devices demands high precision and consistency, which can be difficult to maintain at a large scale.
Furthermore, the incorporation of novel materials and reagents essential for high sensitivity complicates production. For instance, the use of stable affinity reagents like aptamers and engineered antibodies, advanced nanoparticles (e.g., europium chelates, upconverting phosphors, and magnetic nanoparticles), and specialized substrates (e.g., flexible polymers for wearable sensors) introduces supply chain and quality control challenges [70]. These materials must not only perform consistently but also remain stable under variable storage conditions, especially in resource-limited settings where cold-chain logistics may be unreliable [7].
The transition to industrial-scale manufacturing often reveals a stark contrast between prototype and production-line performance. Discrepancies can arise from batch-to-batch variability of biological reagents, imperfections in plastic molding, or the integration of electronic components for readouts and connectivity [70]. As the field moves toward multiplexed panels for detecting co-infections or multi-biomarker profiles, the complexity of the devices—and the difficulty of producing them reliably—increases exponentially [71]. Ensuring that every unit performs with the same high sensitivity and specificity as the laboratory-validated prototype is a formidable task that requires rigorous process control and extensive validation.
Quantitative Cost-Effectiveness Analysis
For any new diagnostic to have a meaningful impact on public health, it must be economically viable for healthcare systems and end-users. Cost-effectiveness analysis (CEA) is the standard methodology used to determine if the value of an intervention justifies its cost, moving beyond simple cost calculation to assign a value to the health outcome achieved [72]. The most widely accepted outcome measure in CEA is the Quality-Adjusted Life Year (QALY), which captures both the quantity and quality of life gained from a medical intervention [72].
The fundamental metric for comparison is the Incremental Cost-Effectiveness Ratio (ICER), calculated as the difference in costs between the new intervention and standard care, divided by the difference in their effectiveness (typically in QALYs) [72]. In the U.S., interventions costing less than $50,000 to $100,000 per QALY are often considered cost-effective, though this threshold varies between countries and healthcare systems [72].
Table 1: Key Components and Considerations for Diagnostic Cost-Effectiveness Analysis
| Component | Description | Considerations in PoC Diagnostics |
|---|---|---|
| Cost Perspective | Healthcare sector vs. Societal | PoC can reduce patient travel time and lost productivity (societal costs) [72]. |
| Cost Elements | Direct (materials, labor) & Indirect (admin, inventory) [73] | High R&D and complex manufacturing increase direct costs; simplified workflows can lower indirect costs [74]. |
| Health Outcomes | Measured in QALYs | Early, accurate PoC diagnosis leads to quicker treatment, better outcomes, and higher QALYs [8] [72]. |
| Discounting | Costs and benefits discounted at 3% annual rate | Reflects the higher value of immediate benefits from rapid PoC results [72]. |
| Time Horizon | Often over the patient's lifetime | PoC can prevent chronic complications of parasitic diseases, yielding long-term savings [72]. |
When evaluating a new PoC diagnostic for a parasitic disease, the analysis must account for its impact on the entire care pathway. A test that is more expensive per unit than traditional microscopy may ultimately be cost-effective if it enables faster treatment initiation, reduces complications, prevents disease transmission, and lowers the overall burden on the healthcare system [8]. The following workflow outlines the key decision points in a cost-effectiveness analysis for a new diagnostic.
Cost-Effectiveness Decision Pathway
The Manufacturing Cost Analysis Framework
To control the production costs that directly influence cost-effectiveness, manufacturers must adopt a rigorous framework for cost analysis. This process enables organizations to identify, evaluate, and capitalize on savings opportunities across the supply chain [74]. Effective cost analysis provides insight into how factors like inflationary pressures and supply chain disruptions impact component costs, allowing for more informed sourcing and manufacturing decisions [74] [73].
The process can be broken down into three key steps [74]:
- Identify Product Cost Outliers: The first step is to segment components by manufacturing process and material type, then analyze current prices and annual purchase volumes to identify parts with the largest spend. These components are then subjected to a "should-cost" analysis, which involves gathering detailed data on material, batch size, production volumes, and secondary processes to generate a granular cost estimate. Comparing this estimate with actual supplier quotes reveals parts with significant savings potential [74].
- Analyze the Identified Cost Outliers: For each outlier, teams must review the estimates for accuracy, evaluate the potential savings and percentage difference, and build action plans. This involves obtaining a basic cost breakdown from the supplier and comparing it with the internal estimate to identify gaps (e.g., in raw materials, secondary processes, or routings). This gap analysis forms the basis for a fact-based discussion with suppliers. Furthermore, design inefficiencies can be identified by plotting the cost estimate against the finished weight of components to find parts that are more than one standard deviation above a best-fit line [74].
- Act on Cost-Reduction Opportunities: The final stage involves executing cost-reduction plans through either redesign or renegotiation. Engineering teams can collaborate to create cost-effective design iterations, such as simplifying a part to fit a manufacturing process more efficiently. Alternatively, sourcing professionals can approach suppliers with their fact-based "should-cost" estimates to negotiate prices and discover the root cause of cost discrepancies [74].
Table 2: Strategic Approaches to Reduce Production Costs [73]
| Strategy | Methodology | Potential Impact |
|---|---|---|
| Process Audit & Continuous Improvement | Deep dive into every manufacturing process; implement lean principles. | Identifies waste, redundancies, and training gaps; optimizes workflows. |
| Enhanced Visibility via Monitoring | Use of real-time production monitoring software (e.g., MachineMetrics). | Provides actionable data on downtime, bottlenecks, and capacity utilization. |
| Inventory Optimization | Deploy inventory management software to balance safety stock and reorder points. | Reduces carrying costs and prevents production stoppages due to material shortage. |
| Supply Chain Streamlining | Integrate supply chain software with production monitoring systems. | Lowers material costs, reduces idle time, and optimizes production lot sizes. |
| Predictive Maintenance | Leverage machine data and analytics to predict service needs. | Reduces unexpected downtime and maintenance costs by scheduling repairs intelligently. |
Integration Hurdles in Point-of-Care Settings
Successfully integrating a diagnostic into PoC settings extends beyond the technical and economic challenges of manufacturing. The device must align with the practical realities of diverse environments, from remote clinics with minimal infrastructure to home use by untrained individuals. The updated REASSURED criteria define the standard for modern PoC devices: Real-time connectivity, Ease of specimen collection, Affordable, Sensitive, Specific, User-friendly, Rapid and Robust, Equipment-free, and Deliverable to end-users [71].
A significant integration hurdle is user-dependent interpretation. Many rapid tests, like lateral flow assays (LFAs), rely on visual reading of lines, which can lead to false positives or negatives when faint lines are misread by untrained users [71]. To address this, machine learning (ML) algorithms are being integrated into portable readers and smartphone apps to automate result interpretation, reducing human error [71]. For example, convolutional neural networks (CNNs) can analyze images of test strips with high accuracy, determining whether a faint line indicates a positive result, thereby enhancing diagnostic reliability [71].
Another major challenge is achieving the required analytical sensitivity with a simple and rapid format. Laboratory-based methods like PCR are highly sensitive but are difficult to miniaturize and operate at the point of care without complex sample preparation and temperature cycling [70]. Innovations in isothermal amplification (e.g., loop-mediated amplification, LAMP) and CRISPR-Cas systems are paving the way for molecular-level sensitivity in PoC formats [7] [8]. These systems can detect low-abundance nucleic acids of parasites with high specificity and can be integrated into cartridges that automate the assay steps, making them suitable for near-patient testing [8].
Finally, data connectivity and management are becoming increasingly important. A connected PoC device can report results directly to electronic health records, aid in disease surveillance, and provide confirmatory testing guidance [70]. However, this requires robust and low-power data transmission solutions that work in areas with poor network coverage, as well as systems that ensure patient data privacy [71]. The diagram below illustrates the integrated ecosystem required for a successful modern PoC diagnostic, highlighting the synergy between hardware, chemistry, and data analytics.
Modern PoC Diagnostic Ecosystem
The Scientist's Toolkit: Key Research Reagents and Materials
The development of next-generation diagnostics relies on a sophisticated toolkit of reagents and materials that enable high sensitivity, specificity, and integration. The following table details essential components featured in recent advancements.
Table 3: Key Research Reagent Solutions for Advanced Parasitic Diagnostics
| Reagent/Material | Function | Key Characteristics & Examples |
|---|---|---|
| Engineered Affinity Reagents | Target capture and detection; replaces traditional antibodies. | Includes aptamers (stable, synthetic oligonucleotides), Designed Ankyrin Repeat Proteins (DARPins; thermally stable), and single-domain antibodies (high affinity) [70]. |
| Nanoparticles | Signal generation, amplification, and sample preparation. | Europium (Eu) chelates for enhanced fluorescence, magnetic beads for target isolation, upconverting phosphors for low-background signal, and gold nanoparticles for colorimetric LFA strips [70] [8]. |
| CRISPR-Cas Systems | Highly specific nucleic acid detection. | Cas proteins (e.g., Cas12, Cas13) programmed to cleave reporter molecules upon recognition of parasitic DNA/RNA, enabling rapid and sensitive molecular diagnosis [8]. |
| Isothermal Amplification Mix | Amplifies nucleic acids at a constant temperature for PoC use. | Enzymes and primers for techniques like Loop-Mediated Isothermal Amplification (LAMP), eliminating the need for complex thermal cyclers [7]. |
| Functionalized Substrates | Platform for assembling assays; fluidic handling. | Nitrocellulose for lateral flow strips; paper-based substrates with patterned hydrophobic/hydrophilic regions for multi-step assays; flexible polymers for wearable sensors [70]. |
Detailed Experimental Protocol: Evaluating an ML-Enhanced LFA Reader
The following protocol outlines a methodology for developing and validating a machine learning algorithm to improve the accuracy of a lateral flow assay (LFA) for parasitic antigen detection, a key innovation addressing user interpretation hurdles [71].
Objective: To train and validate a convolutional neural network (CNN) to digitally interpret LFA test lines and determine its sensitivity and specificity compared to visual reading by trained and untrained users.
Materials:
- LFA Strips: A batch of strips tested with characterized clinical samples (positive and negative for the target parasite antigen).
- Imaging Device: A standardized imaging setup, such as a smartphone holder with consistent lighting.
- Computing Environment: A computer with Python and deep learning libraries (e.g., TensorFlow, PyTorch).
- Labeled Dataset: Images of LFA strips with ground truth labels (positive/negative) confirmed by a reference method (e.g., PCR).
Methodology:
- Data Acquisition and Preprocessing:
- Capture high-resolution images of the LFA strips using the standardized imaging device.
- Apply preprocessing techniques to the image dataset, including denoising, background subtraction, and normalization to reduce variability and improve model performance [71].
- Manually annotate each image with the correct classification (positive/negative) and, if applicable, the intensity of the test line.
Data Splitting:
- Randomly split the preprocessed dataset into three subsets:
- Training Set (60%): Used to train the CNN model.
- Validation Set (20%): Used to tune model hyperparameters and prevent overfitting during training.
- Blind Testing Set (20%): Used for the final, unbiased evaluation of the model's performance [71].
- Randomly split the preprocessed dataset into three subsets:
Model Optimization and Training:
- Select a CNN architecture (e.g., a pre-trained model for transfer learning).
- Train the model on the training set, using the validation set to monitor performance. The model learns to associate features in the images with the correct classification.
- Optimize model hyperparameters (e.g., learning rate, number of layers) based on performance on the validation set.
Blind Testing and Comparison:
- Use the finalized model to make predictions on the blind testing set, which contains images the model has never seen.
- Compare the ML model's classifications against the ground truth labels to calculate its sensitivity, specificity, and accuracy.
- In parallel, have a cohort of trained laboratory technicians and a cohort of untrained users visually interpret the same strips from the blind testing set.
- Statistically compare the performance metrics (sensitivity, specificity) of the ML model against both user groups.
Expected Outcome: The experiment is designed to demonstrate that the ML-based interpretation achieves a diagnostic accuracy superior to, or at least on par with, trained technicians and significantly better than untrained users, thereby validating its utility for decentralizing testing without sacrificing reliability [71].
The journey toward overcoming the challenges in mass production, cost-effectiveness, and PoC integration for parasitic disease diagnostics is complex yet imperative. The convergence of advanced materials, microfluidic engineering, molecular biology (e.g., CRISPR), and digital technologies (e.g., AI/ML) holds the promise of creating a new generation of REASSURED-compliant diagnostics [71] [8]. However, technological brilliance alone is insufficient. For these innovations to transition from research labs to field-based reality, a holistic approach is necessary. This includes designing for manufacturability and cost from the earliest stages, conducting robust cost-effectiveness analyses to demonstrate value to health systems, and relentlessly focusing on user-centric design for seamless integration into point-of-care workflows. By addressing this triad of challenges in unison, researchers, manufacturers, and public health stakeholders can make the definitive diagnosis of parasitic diseases a rapid, accessible, and affordable reality for all populations in need.
Parasitic infections remain a profound public health challenge, affecting nearly one-quarter of the global population and contributing significantly to the burden of disease in tropical and subtropical regions [9]. These infections result in diverse health issues including malnutrition, anemia, and increased susceptibility to other diseases, thereby hindering development efforts in affected regions [9]. The World Health Organization notes that 13 of the 20 listed neglected tropical diseases are parasitic in origin, underscoring the critical need for improved diagnostic methods [9]. Traditional diagnostic approaches, particularly microscopy, have formed the backbone of parasite detection for decades but face limitations in sensitivity, specificity, and scalability in resource-limited settings [10] [8]. The evolution of diagnostic technologies has progressed through serological methods to molecular approaches, yet the transition from promising proof-of-concept demonstrations to genuinely scalable, field-adjustable tools presents significant scientific and implementation challenges [7] [8]. This technical guide examines the current landscape of parasitic disease diagnostics, analyzes the barriers to field implementation, and provides detailed methodologies for developing solutions that can bridge this critical gap.
Current Diagnostic Landscape: From Conventional to Advanced Methods
The diagnosis of parasitic diseases has evolved significantly over centuries, driven by technological advancements and a deeper understanding of parasite biology [9]. Conventional methods remain widely used but are increasingly supplemented or replaced by more advanced techniques.
Conventional Diagnostic Methods
Microscopy continues to be the most widely used diagnostic method for parasitic infections, particularly in resource-limited settings [10] [8]. Its advantages include low direct costs, immediate applicability, and the ability to detect a broad range of parasites without specialized equipment [75]. However, its sensitivity is highly dependent on parasite burden, technician expertise, and quality of equipment [8]. In the acute infection phase when erythrocyte staining rate is high, thin blood smears may suffice, but thick smears prove essential during subclinical stages or post-acute phases when low parasitemia (<0.1%) challenges detection sensitivity [75].
Serological techniques including Enzyme-Linked Immunosorbent Assay (ELISA), immunofluorescence assays (IFA), and rapid diagnostic tests (RDTs) detect parasite-specific antigens or host antibodies [10] [8]. These methods are valuable for large-scale surveillance but are limited by cross-reactivity between related parasite species and the persistence of antibodies long after active infection has resolved, complicating the distinction between past and current infections [76] [10].
Advanced Molecular Methods
PCR-based methods offer significantly improved sensitivity and specificity compared to conventional methods [10] [8]. Real-time PCR (qPCR) enables both detection and quantification of parasite load, while multiplex PCR allows simultaneous detection of multiple parasites [10] [8]. The limitations include requirement for thermal cycling equipment, trained personnel, and controlled laboratory infrastructure, which restricts application in field-based and point-of-care settings [76].
Isothermal amplification techniques such as Loop-Mediated Isothermal Amplification (LAMP), Recombinase Polymerase Amplification (RPA), and Nucleic Acid Sequence-Based Amplification (NASBA) operate at constant temperatures using minimal instrumentation [76] [8]. These methods are amenable to visual or instrument-free detection formats such as fluorescence, colorimetric changes, or lateral flow strips, making them promising for field deployment [76].
Table 1: Comparison of Diagnostic Methods for Parasitic Diseases
| Method Category | Examples | Sensitivity | Specificity | Infrastructure Requirements | Time to Result | Cost |
|---|---|---|---|---|---|---|
| Conventional | Microscopy, Staining | Low-Moderate | Moderate | Low | 30 mins - 2 hrs | Low |
| Serological | ELISA, IFA, RDTs | Moderate | Moderate-High | Low-Moderate | 15 mins - 4 hrs | Low-Moderate |
| Molecular | PCR, qPCR, Multiplex | High | High | High | 1 - 4 hrs | High |
| Isothermal | LAMP, RPA, NASBA | High | High | Low-Moderate | 15 - 60 mins | Moderate |
| CRISPR-Based | SHERLOCK, DETECTR | Very High | Very High | Low | 30 - 90 mins | Moderate |
The Implementation Gap: Barriers to Field Deployment
The transition from laboratory proof-of-concept to field-deployable tools faces several significant barriers that must be addressed for successful implementation.
Technical and Infrastructure Barriers
Molecular methods such as PCR require stable power, thermal cycling equipment, and controlled laboratory environments, which are often unavailable in remote or resource-limited settings where parasitic diseases are most prevalent [76] [8]. While isothermal amplification techniques reduce instrumentation needs, they still face challenges with nucleic acid extraction, reagent stability, and detection [76]. Many advanced diagnostic methods also require sophisticated sample preparation, trained personnel for operation and interpretation, and cold chain storage for reagents – all significant challenges in field settings [8].
Economic and Sustainability Challenges
The development and manufacturing costs for advanced diagnostic tools can be prohibitive for low-resource settings [77]. Traditional microscopy, while less sensitive, has minimal recurring costs beyond basic supplies and labor [10]. Sustainable implementation requires consideration of total cost of ownership, including maintenance, reagent resupply, and training [77]. Market forces also influence diagnostic development, with the global Ova and Parasite Test Market projected to grow at a CAGR of 5.7% from 2025 to 2032, driven by rising international travel, increasing incidence of parasitic infections, and need for efficient diagnostic methodologies [77].
Emerging Solutions: Towards Field-Adjustable Diagnostic Platforms
CRISPR-Cas Systems for Parasite Detection
CRISPR-Cas systems represent a transformative approach for molecular diagnostics, combining programmability, high specificity, and rapid turnaround [76]. These systems can be coupled with pre-amplification methods (RPA, LAMP) to enhance sensitivity, enabling detection of target sequences at femtomolar to attomolar concentrations [76]. The collateral cleavage activity of Cas12 and Cas13 proteins allows signal amplification that can be detected using simple lateral flow strips or fluorescent readers [76].
CRISPR-Based Detection Workflow
Experimental Protocol: RPA-CRISPR/Cas12a for Parasite Detection
Nucleic Acid Extraction: Use magnetic bead-based extraction kits or boil-and-spin methods for field-compatible DNA extraction from blood, stool, or other clinical samples.
Recombinase Polymerase Amplification (RPA):
- Prepare 50μL reaction containing: 25μL rehydration buffer, 5μL template DNA, 2.1μL forward primer (10μM), 2.1μL reverse primer (10μM), 9.8μL nuclease-free water, and 1μL magnesium acetate (280mM).
- Incubate at 37-42°C for 15-20 minutes.
CRISPR/Cas12a Detection:
- Prepare detection mix: 1μL Cas12a enzyme (1μM), 1.25μL crRNA (4μM), 2.5μL NTP mix, 2.5μL buffer, 0.5μL FQ-reporter (5μM), and 12.25μL nuclease-free water.
- Add 5μL amplified RPA product to detection mix.
- Incubate at 37°C for 10-30 minutes.
Result Visualization:
- Use lateral flow strips: Apply 10μL reaction mixture to sample pad, place in running buffer.
- Alternatively, use portable fluorometer or visual detection under blue light.
This protocol has been adapted for various parasites including Plasmodium species, Trypanosoma cruzi, and Leishmania with detection limits approaching 1-10 copies/μL [76].
Artificial Intelligence and Digital Microscopy
AI-based image recognition represents an innovative approach to overcome limitations of conventional microscopy [9] [75]. Deep learning algorithms, particularly convolutional neural networks (CNNs), can be trained to identify parasite morphological features in blood smears, stool samples, or other clinical specimens [9] [8].
AI-Assisted Parasite Detection
Experimental Protocol: AI-Assisted Microscopy for Babesia Detection
Sample Preparation and Imaging:
- Prepare thin and thick blood smears from capillary blood (ear tips, tail tips).
- Stain with Giemsa or Field's stain using standard protocols.
- Scan slides using portable digital microscope at 1000x magnification.
- Capture multiple images from different fields of view.
Dataset Curation for Model Training:
- Collect at least 5,000 annotated images containing various parasite developmental stages.
- Include diverse samples representing different parasitemia levels (0.1% to 20%).
- Annotate images using bounding boxes or segmentation masks for trophozoites, merozoites, and other forms.
Model Architecture and Training:
- Implement a convolutional neural network (CNN) using architecture such as YOLO (You Only Look Once) or U-Net.
- Use transfer learning from pre-trained models on ImageNet to accelerate training.
- Train with balanced datasets to handle class imbalance between parasite and non-parasite regions.
Field Deployment and Validation:
- Optimize model for mobile deployment using TensorFlow Lite or similar frameworks.
- Integrate with smartphone-based microscope attachments for field use.
- Conduct validation studies comparing AI performance with expert microscopists.
Studies have demonstrated that AI models can achieve sensitivity of 84.6% and specificity of 97.7% for Babesia canis detection using parameters including platelet count (PLT), mean platelet volume (MPV), and percentage of unstained cells (LUC%) [75].
Nanotechnology and Biosensors
Nanotechnology has emerged as a revolutionary tool providing highly sensitive and precise detection of parasitic diseases [8]. Nanoparticles offer versatile platforms for advanced diagnostic tools including nano-biosensors and magnetic isolation devices due to their unique physical, chemical, and biological properties [8].
Table 2: Nanotechnology Applications in Parasite Diagnostics
| Nanomaterial | Application | Detection Mechanism | Target Parasites | Advantages |
|---|---|---|---|---|
| Gold Nanoparticles | Lateral flow assays, Colorimetric detection | Surface plasmon resonance, Color change | Plasmodium, Leishmania | Visual detection, No instrumentation |
| Magnetic Nanoparticles | Sample preparation, Concentration | Magnetic separation | Multiple parasites | Improved sensitivity, Rapid processing |
| Quantum Dots | Fluorescent detection | Photoluminescence | Trypanosoma, Toxoplasma | Multiplexing, High sensitivity |
| Carbon Nanotubes | Electrochemical sensors | Electrical signal change | Various | Label-free detection, Portability |
| Upconversion Nanoparticles | Immunoassays | Near-infrared to visible light | Schistosoma, Filaria | Minimal background, High specificity |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of field-adjustable diagnostic tools requires careful selection of research reagents and materials that balance performance with stability and ease of use.
Table 3: Research Reagent Solutions for Field-Adjustable Diagnostics
| Reagent Category | Specific Examples | Function | Field-Adaptable Alternatives |
|---|---|---|---|
| Nucleic Acid Extraction | Magnetic bead kits, Spin columns | Isolation and purification of DNA/RNA | Boil-and-spin methods, Filter paper collection |
| Amplification Reagents | LAMP, RPA, PCR master mixes | Target amplification | Lyophilized reagents, Room-temperature stable formulations |
| CRISPR Components | Cas12a, Cas13, crRNAs | Specific detection and signal generation | Lyophilized Cas proteins, pre-loaded reaction tubes |
| Signal Detection | Lateral flow strips, FQ-reporters | Visual or instrumental readout | Smartphone cameras, portable fluorometers |
| Sample Preservation | RNA/DNA stabilizers, Transport media | Maintain sample integrity | Chemical preservatives, filter paper, dried blood spots |
| Positive Controls | Synthetic gene fragments, Plasmid controls | Assay validation and quality control | Non-infectious synthetic targets, inactivated parasites |
Quantitative Framework for Diagnostic Assessment
Robust evaluation of diagnostic tools requires comprehensive assessment using standardized metrics and appropriate statistical approaches.
Statistical Considerations for Field Deployment
Sample size determination for monitoring parasitic infections in populations typically follows generic indications, with 10 (ranging from 7 to 20) animals per farm or 10% of the flock being frequent recommendations [78]. For human populations, statistical calculations should consider prevalence estimates, desired confidence level, and test performance characteristics [78].
Diagnostic sensitivity and specificity calculations should follow standard formulas:
- Sensitivity = True Positives / (True Positives + False Negatives)
- Specificity = True Negatives / (True Negatives + False Positives)
Limit of Detection (LOD) determination requires testing dilution series of standardized samples with known parasite concentrations. The LOD is typically defined as the lowest concentration at which ≥95% of replicates test positive [76] [75].
Operational Performance Metrics
Beyond traditional performance characteristics, field-deployable tools should be evaluated against operational metrics:
- Time to result: Target <60 minutes for point-of-care applications
- Stability: Reagents should maintain performance at elevated temperatures (25-40°C) for minimum 4-6 weeks
- Usability: Minimal training requirements (<1 day) for operators with basic technical skills
- Cost: Total cost per test should be compatible with local healthcare budgets
The development of scalable, field-adjustable diagnostic tools for parasitic diseases requires multidisciplinary approaches that address both technological and implementation challenges. CRISPR-based systems, AI-enhanced microscopy, and nanotechnology platforms offer promising pathways toward highly sensitive and specific detection that can function in resource-limited settings. However, successful translation requires early consideration of environmental stability, user-friendly design, manufacturing scalability, and economic sustainability. By adopting integrated development frameworks that engage end-users throughout the design process and rigorously validate tools in real-world conditions, researchers can significantly impact the global fight against parasitic diseases. The continued convergence of molecular biology, materials science, and digital technology holds particular promise for creating next-generation diagnostic tools that are truly accessible where they are most needed.
Evaluating Diagnostic Performance: Regulatory Pathways and Comparative Efficacy Analysis
The definitive diagnosis of parasitic diseases represents a critical challenge in global health, particularly in resource-limited settings where these infections are most prevalent. For decades, traditional microscopy and Enzyme-Linked Immunosorbent Assay (ELISA) have served as cornerstone diagnostic methodologies, providing the fundamental framework for parasitic infection identification and surveillance [9] [8]. Microscopy, despite being the historical gold standard for parasites like Plasmodium species, suffers from significant limitations including operator dependency, low throughput, and diminished sensitivity at low parasite densities [9] [14]. Similarly, while ELISA offers advantages for high-throughput serological testing, it often demonstrates cross-reactivity issues and limited ability to distinguish between past and current infections [9] [8].
The evolving landscape of parasitic disease research demands diagnostic tools with enhanced accuracy, speed, and field-deployability. This technical guide provides a comprehensive benchmarking analysis of emerging diagnostic platforms against traditional methods, with a specific focus on their sensitivity and specificity profiles within the context of parasitic disease research. We present quantitative performance comparisons, detailed experimental methodologies for next-generation assays, and practical resource guidance to inform research and development efforts aimed at overcoming the limitations of conventional diagnostic approaches.
Performance Benchmarking: Quantitative Analysis of Diagnostic Platforms
The following tables summarize the performance characteristics of conventional versus novel diagnostic tools for parasitic diseases, based on current research data. These metrics provide critical insights for researchers selecting appropriate methodologies for specific applications.
Table 1: Overall Performance Metrics of Diagnostic Platforms for Parasitic Diseases
| Diagnostic Platform | Typical Sensitivity Range | Typical Specificity Range | Key Parasitic Applications |
|---|---|---|---|
| Traditional Microscopy | Varies widely by operator; decreases significantly at low parasite density [9] | High for species with distinct morphology [14] | Malaria, Schistosomiasis, Soil-transmitted Helminths [8] |
| Conventional ELISA | Moderate to High [8] | Can be compromised by cross-reactivity [9] | Leishmaniasis, Echinococcosis, Toxoplasmosis [9] [8] |
| Paper-Based ELISA (p-ELISA) | Improved vs. conventional ELISA in some formats; can suffer from high background noise [79] | Improved vs. conventional ELISA in some formats [79] | Point-of-Care (POC) diagnostics for various parasites [79] |
| Nanobiosensors | Very High (detection of biomarkers at low concentrations) [14] | Very High (specific biomarker identification) [14] | Malaria, Leishmania, Echinococcus, Schistosoma detection [14] |
| AI-Based Microscopy Analysis | Up to 99.37% [80] | Implied by high AUC (99.95%) [80] | Automated Plasmodium detection and species identification [80] |
Table 2: Advanced Characterization of Novel Assay Formats
| Assay Format | Detection Limit | Multiplexing Capability | Time to Result |
|---|---|---|---|
| DAS-ELISA (for PCV3) | 3.4 ng/mL (Cap protein) [81] | No (single-analyte) [81] | ~2-3 hours (including incubation steps) [81] |
| Electrochemical Nanobiosensors | Sub-femtomolar possible [82] [14] | Yes (with multiple electrodes/probes) [14] | Minutes to < 1 hour [14] |
| CRISPR-Cas Diagnostics | Attomolar levels for nucleic acids [8] | Limited in current formats [8] | 15-60 minutes [8] |
Experimental Protocols for Next-Generation Assays
Protocol 1: Double Antibody Sandwich ELISA (DAS-ELISA) for Antigen Detection
The DAS-ELISA format provides enhanced specificity for pathogen detection by employing two antibodies targeting different epitopes on the same antigen. The following protocol, adapted for the detection of Porcine Circovirus Type 3 (PCV3) Cap protein, can be modified for parasitic antigen targets [81].
Key Reagents and Materials:
- Capture Antibody: A polyclonal antibody (e.g., produced in rabbit) specific to the target antigen.
- Detection Antibody: A monoclonal antibody (mAb) specific to a different, non-overlapping epitope on the target antigen.
- Coating Buffer: 0.05 M Carbonate-Bicarbonate buffer, pH 9.6.
- Washing Buffer: Phosphate-Buffered Saline (PBS) with 0.05% Tween-20 (PBST).
- Blocking Buffer: PBS with 1-5% Bovine Serum Albumin (BSA) or skim milk.
- Enzyme Conjugate: Horseradish Peroxidase (HRP)-labeled secondary antibody specific to the detection mAb.
- Substrate Solution: Tetramethylbenzidine (TMB) or other chromogenic HRP substrates.
- Stop Solution: 1 M Sulfuric Acid or 2 M Citric Acid.
- Microplate Reader.
Detailed Procedure:
- Plate Coating: Dilute the capture pAb in coating buffer. Add 100 µL per well to a 96-well microplate and incubate overnight at 4°C.
- Washing: Aspirate the coating solution and wash the plate three times with PBST (300 µL per well per wash).
- Blocking: Add 200 µL of blocking buffer to each well. Incubate for 1-2 hours at 37°C. Wash the plate three times as before.
- Sample/Antigen Incubation: Add 100 µL of the test sample (e.g., serum, lysate) or antigen standard to the wells. Incubate for 1 hour at 37°C. Wash three times.
- Detection Antibody Incubation: Add 100 µL of the specific mAb to the wells. Incubate for 1 hour at 37°C. Wash three times.
- Enzyme Conjugate Incubation: Add 100 µL of the HRP-conjugated anti-species secondary antibody. Incubate for 1 hour at 37°C. Wash three times.
- Signal Development: Add 100 µL of TMB substrate to each well. Incubate in the dark for 10-15 minutes at room temperature.
- Reaction Stopping: Add 50 µL of stop solution to each well.
- Signal Measurement: Read the optical density (OD) immediately at 450 nm using a microplate reader.
Validation and Analysis: Calculate the cut-off value (e.g., mean OD of negative controls + 3 standard deviations). Samples with an OD above the cut-off are considered positive. The assay's sensitivity (detection limit) should be determined using a serial dilution of a known antigen standard [81].
Protocol 2: Development and Application of a Gold Nanoparticle (AuNP)-Based Immunosensor
Nanobiosensors utilize nanomaterials as transducers for sensitive detection. This protocol outlines the creation of a colorimetric immunosensor using AuNPs for a parasitic antigen, such as Plasmodium falciparum histidine-rich protein 2 (PfHRP2) [14].
Key Reagents and Materials:
- Chloroauric Acid (HAuClâ‚„) for AuNP synthesis.
- Trisodium Citrate as a reducing/capping agent.
- Detection Antibody: An antibody specific to the target parasitic biomarker.
- Phosphate Buffered Saline (PBS), pH 7.4.
- Sample containing the target antigen.
- Spectrophotometer or plate reader.
Detailed Procedure:
- Synthesis of AuNPs: Prepare a 0.01% solution of HAuClâ‚„ in deionized water and bring it to a boil under reflux. Rapidly add 1% trisodium citrate solution with vigorous stirring. Continue heating and stirring until the solution develops a deep red wine color, indicating AuNP formation. Allow to cool to room temperature. Characterize the AuNPs by UV-Vis spectroscopy (Surface Plasmon Resonance peak ~520 nm) and TEM [14].
- Antibody Functionalization: Adjust the pH of the AuNP solution to around 8-9 using a mild base like potassium carbonate. Add the detection antibody to the AuNP solution dropwise under gentle stirring. The antibody adsorbs onto the AuNP surface via electrostatic interactions. Incubate for 1 hour at room temperature.
- Blocking and Purification: Add a blocking agent (e.g., BSA) to cover any remaining bare AuNP surfaces and prevent non-specific aggregation. Incubate for 30 minutes. Purify the antibody-conjugated AuNPs (Ab-AuNPs) by centrifugation and resuspend in a stable storage buffer (e.g., PBS with BSA) [14].
- Antigen Detection Assay:
- Aggregation-Based Detection: In the presence of the specific antigen, the Ab-AuNPs cross-link, causing aggregation. This shifts the SPR peak to a longer wavelength and changes the solution color from red to blue. Monitor this shift via UV-Vis spectroscopy or visually.
- Lateral Flow Assay (LFA) Integration: The Ab-AuNPs can be used as the detection conjugate in an LFA strip. The antigen in the sample binds to the Ab-AuNPs and is captured at the test line by a second immobilized antibody, producing a colored band.
Validation: Confirm the assay's performance by testing with known concentrations of recombinant antigen to establish a standard curve and determine the limit of detection (LOD). Evaluate specificity by testing against related but non-target antigens [14].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of advanced diagnostic assays requires specific, high-quality reagents. The following table details key materials and their critical functions in the protocols described above.
Table 3: Research Reagent Solutions for Advanced Parasitic Diagnostics
| Reagent/Material | Function/Application | Key Characteristics & Considerations |
|---|---|---|
| Monoclonal Antibodies (mAbs) [81] | Core component for detection in DAS-ELISA, LFAs, and nanobiosensors; targets a single, specific epitope. | High specificity and affinity are critical; epitope mapping ensures the pair for DAS-ELISA bind non-competitively. |
| Polyclonal Antibodies (pAbs) [81] | Often used as the capture antibody in DAS-ELISA; recognizes multiple epitopes on the target antigen. | Can increase the chance of capturing antigen but requires careful purification to minimize background. |
| Gold Nanoparticles (AuNPs) [14] | Signal transducer in nanobiosensors; color change upon aggregation indicates detection. | Size (e.g., 20-40 nm), shape, and surface functionalization (e.g., with antibodies, DNA) dictate performance. |
| Enzyme Conjugates (e.g., HRP) [79] [81] | Catalyzes the conversion of a substrate into a colored (chromogenic), fluorescent, or luminescent product in ELISA. | High specific activity and stability; choice depends on desired sensitivity and detection method. |
| Recombinant Antigens [81] [14] | Used as positive controls, for standard curve generation, and for antibody production/validation. | Must mimic the native protein's immunogenic structure; purity is essential for assay specificity. |
| CRISPR-Cas Enzymes (e.g., Cas12a, Cas13) [8] | Molecular scissors for nucleic acid detection; upon binding target DNA/RNA, exhibit collateral cleavage of reporter molecules. | Programmable guide RNAs confer specificity; ideal for field-deployable, rapid molecular tests. |
Technological Workflows and Logical Pathways
The integration of novel technologies introduces new workflows that differ significantly from traditional methods. The diagram below illustrates the logical pathway for a CRISPR-Cas based diagnostic system, highlighting its potential for rapid, equipment-light detection.
The benchmarking data and protocols presented in this guide underscore a significant paradigm shift in the diagnostic landscape for parasitic diseases. Technologies such as nanobiosensors, CRISPR-Cas platforms, and AI-enhanced imaging consistently demonstrate performance metrics that meet or surpass those of traditional microscopy and ELISA, particularly regarding sensitivity, specificity, and operational efficiency [14] [80] [8]. The move towards multiplexing, point-of-care applicability, and quantitative precision positions these novel tools to address long-standing challenges in both clinical management and research of parasitic infections.
For the research community, the adoption of these advanced methodologies necessitates an investment in understanding their underlying principles and optimal implementation protocols. The continued refinement of these platforms, coupled with the development of standardized reagents and rigorous validation across diverse parasitic targets, will be crucial for realizing their full potential. The future of definitive diagnosis in parasitology lies in the strategic integration of these high-precision tools into a cohesive, accessible, and responsive global health framework.
The Role of FDA's Drug Development Tool (DDT) Qualification Program
The FDA's Drug Development Tool (DDT) Qualification Program represents a formalized pathway to evaluate and qualify methods, materials, or measures that can facilitate drug development and regulatory review [83]. Established under Section 507 of the 21st Century Cures Act of 2016, this program creates a structured framework for the development and regulatory acceptance of tools that can be used across multiple drug development programs for a specific context of use [83] [84]. DDTs include biomarkers for clinical trial enrichment, clinical outcome assessments (COAs) to evaluate clinical benefit, and animal models for efficacy testing, particularly under the Animal Rule for medical countermeasures [83].
The qualification of DDTs is particularly relevant for advancing research in complex disease areas such as parasitic diseases, where definitive diagnosis and treatment monitoring present significant challenges. For parasitic disease researchers, the program offers a mechanism to develop and validate diagnostic, prognostic, and monitoring tools that can be consistently applied across clinical trials, potentially accelerating the development of novel therapeutics for neglected tropical diseases that disproportionately affect global health.
DDT Qualification Process: Structure and Workflow
The DDT qualification process follows a defined three-stage pathway established by the 21st Century Cures Act, building upon the legacy qualification program that FDA had previously implemented voluntarily [84]. This structured approach ensures rigorous scientific evaluation while providing developers with a predictable framework for engagement with regulatory authorities.
Stage 1: Letter of Intent (LOI)
The qualification process begins with the submission of a Letter of Intent to the relevant FDA program (Biomarker Qualification Program, Clinical Outcome Assessment Qualification Program, or Animal Model Qualification Program) [83] [84]. The LOI outlines the proposed DDT, its intended context of use, and preliminary scientific rationale. FDA reviews the LOI within a target timeframe of 3 months to determine whether the proposed tool has sufficient merit to advance to the next stage [85]. As of June 2025, 121 LOIs had been accepted across all DDT qualification programs [86].
Stage 2: Qualification Plan (QP)
If the LOI is accepted, the requester submits a detailed Qualification Plan that comprehensively describes the proposed development plan for the DDT [83]. This includes specific details on the context of use, proposed studies, analytical methods, and statistical analysis plans. In July 2025, FDA published a revised version of the Biomarker Qualification Program Qualification Plan Content Element Outline, providing requesters with comprehensive instructions for preparing QP submissions [83]. The FDA reviews the QP within a target timeframe of 6 months [85]. Currently, 20 QPs have been accepted across all qualification programs [86].
Stage 3: Full Qualification Package (FQP)
The final stage involves submission of a Full Qualification Package containing all necessary data and evidence to support the qualification of the DDT for the specified context of use [84]. This comprehensive package undergoes rigorous review by a multidisciplinary team of FDA staff, with a target review timeframe of 10 months [85]. Upon successful review, FDA issues a qualification decision that is made publicly available along with an executive summary and redacted reviews [84].
The following diagram illustrates the complete DDT qualification workflow and its key components:
The Critical Role of Context of Use
A fundamental concept throughout the DDT qualification process is the context of use (COU), which defines the specific manner and purpose for which the DDT can be relied upon [83]. The COU statement comprehensively describes all elements characterizing the purpose and manner of use, establishing the boundaries within which the available data adequately justify application of the DDT [83]. For parasitic disease research, a clearly defined COU is essential—whether for a diagnostic biomarker to detect specific parasitic infections, a clinical outcome assessment to measure treatment response, or an animal model for evaluating candidate therapeutics.
Program Metrics and Current Status
The DDT Qualification Program has demonstrated substantial activity across its various components. The following table summarizes the current metrics as of August 2025, providing insight into program utilization and outcomes across different tool categories [86]:
Table 1: DDT Qualification Program Metrics (as of June 30, 2025)
| Program Area | Total Projects in Development | LOIs Accepted | QPs Accepted | Newly Qualified DDTs (Past 12 Months) | Total Qualified DDTs to Date |
|---|---|---|---|---|---|
| All DDT Qualification Programs | 141 | 121 | 20 | 1 | 17 |
| Biomarker Qualification Program | 59 | 49 | 10 | 0 | 8 |
| Clinical Outcome Assessment Qualification Program | 67 | 58 | 9 | 1 | 8 |
| Animal Model Qualification Program | 5 | 5 | 0 | 0 | 1 |
| ISTAND Program | 10 | 9 | 1 | 0 | 0 |
Analysis of program performance reveals several important trends. A recent study examining the COA Qualification Program specifically found that only 8.1% of submitted COAs (7 of 86) had achieved qualification, with one tool denied after completing all qualification steps [87] [85]. The study also highlighted that the qualification process typically requires approximately 6 years from initial submission to final qualification, with 46.7% of submissions experiencing review times exceeding FDA's published targets [87] [85].
Regarding utilization in drug development, the same analysis revealed that only three of the seven qualified COAs have been used to support benefit-risk assessments for medicines, primarily as secondary or exploratory endpoints rather than primary endpoints [87] [85]. These qualified COAs have supported regulatory evaluations for 11 medicines across various therapeutic areas, with only one qualified COA included in drug labels [87] [85].
DDTs in Infectious Disease and Diagnostic Applications
The DDT Qualification Program has significant implications for advancing tools for infectious diseases, including parasitic infections. While the search results do not provide specific examples of qualified DDTs for parasitic diseases, several relevant areas of application emerge:
Biomarkers for Parasitic Disease Management
For parasitic diseases, qualified biomarkers could serve critical functions in:
- Early detection of parasitic infections before clinical symptoms manifest
- Disease stratification to identify patients at risk for severe complications
- Treatment response monitoring to assess efficacy of therapeutic interventions
- Predictive enrichment of clinical trials by identifying patients most likely to benefit from investigational therapies
The Biomarker Qualification Program, with 59 projects currently in development, represents a promising pathway for establishing standardized biomarkers for parasitic diseases [86].
Diagnostic Tools and LDT Considerations
The broader regulatory landscape for diagnostic tools includes Laboratory-Developed Tests (LDTs), which are diagnostically validated by individual clinical laboratories [88]. For parasitic diseases, LDTs often serve as important tools when FDA-approved alternatives are limited or unavailable. Examples include:
- Antiviral resistance testing for specific pathogens
- Comprehensive identification of parasitic organisms using advanced methodologies
- Antimicrobial susceptibility testing for parasitic infections [88]
The ongoing regulatory discussion around LDTs highlights the importance of maintaining access to these critical tools while ensuring their safety and efficacy [88].
ISTAND: Pioneering Innovative Approaches
The Innovative Science and Technology Approaches for New Drugs (ISTAND) Program represents an expansion of the DDT qualification paradigm, specifically designed to evaluate novel tools that fall outside the scope of existing qualification programs [89]. Launched to embrace emerging technologies, ISTAND has particular relevance for advancing parasitic disease research through innovative methodologies.
ISTAND Scope and Applications
The ISTAND Program accepts submissions for qualification of novel DDT types that may benefit drug development but do not fit within traditional biomarker, COA, or animal model categories [89]. Examples include:
- Microphysiological systems (tissue chips) for assessing drug safety or efficacy, including a recently accepted organ-on-a-chip technology designed to predict human drug-induced liver injury [89]
- Digital health technologies and wearables for remote patient assessment in decentralized clinical trials
- Artificial intelligence algorithms for patient evaluation, novel endpoint development, or clinical trial optimization [89]
- Tools enabling remote or decentralized trials, such as patient-performed digital photography for dermatology assessments [89]
ISTAND Potential for Parasitic Disease Research
For parasitic disease researchers, the ISTAND Program offers a pathway to qualify innovative tools that could significantly advance the field:
- Point-of-care diagnostic devices for field use in endemic areas
- Digital microscopy platforms with automated parasite detection algorithms
- Remote monitoring technologies for clinical trials conducted in resource-limited settings
- Novel nonclinical assays for evaluating anti-parasitic drug candidates
With 10 projects currently in development and 9 LOIs accepted, ISTAND represents an growing avenue for regulatory qualification of novel approaches [86].
Experimental Considerations for Parasitic Disease DDTs
Researchers developing DDTs for parasitic diseases should consider several critical methodological aspects to enhance the likelihood of successful qualification.
Biomarker Development Methodology
The development of biomarkers for parasitic diseases requires rigorous analytical and clinical validation. Key methodological components include:
Analytical Validation Protocol:
- Specimen Collection and Handling: Standardized procedures for collection, processing, and storage of clinical specimens (e.g., blood, stool, tissue) to preserve biomarker integrity
- Assay Optimization: Determination of optimal assay conditions including temperature, pH, incubation times, and reagent concentrations
- Analytical Performance: Comprehensive assessment of analytical sensitivity (limit of detection), analytical specificity (including cross-reactivity with related parasites), precision (repeatability and reproducibility), and linearity/range
- Quality Control: Implementation of internal quality control procedures and reference standards
Clinical Validation Study Design:
- Patient Cohort Selection: Recruitment of well-characterized patient cohorts representing the spectrum of disease (uninfected, asymptomatic, mild, moderate, and severe infection)
- Control Groups: Inclusion of appropriate control groups, including patients with related parasitic infections (to assess specificity) and non-infected endemic controls
- Longitudinal Sampling: Collection of serial specimens to assess biomarker kinetics during natural history of infection and in response to treatment
- Blinded Assessment: Performance of biomarker testing blinded to clinical status and reference standard results
Clinical Outcome Assessment Development
For COAs targeting parasitic disease symptoms or impacts, development should follow established methodology:
Concept Elicitation Protocol:
- Qualitative Interviews: Conduct semi-structured interviews with patients representing diverse demographic and disease characteristics
- Symptom Characterization: Systematic identification and description of all relevant symptoms, their frequency, severity, duration, and impact on function
- Conceptual Framework: Development of a comprehensive model linking individual symptoms to broader impacts on quality of life and functioning
Cognitive Interviewing Methodology:
- Item Understanding: Assessment of patient comprehension of individual COA items and response options
- Recall Period Evaluation: Determination of appropriate recall period (e.g., 24-hour, 7-day, current) based on symptom variability and patient ability to accurately recall
- Cultural Adaptation: Evaluation of conceptual and linguistic equivalence across different cultural and language groups in endemic regions
Essential Research Reagents and Materials
The development and validation of DDTs for parasitic diseases requires specific research reagents and materials. The following table outlines key solutions and their applications in experimental protocols:
Table 2: Research Reagent Solutions for Parasitic Disease DDT Development
| Research Reagent/Material | Function in DDT Development | Application Examples |
|---|---|---|
| Reference Standard Parasites | Serve as positive controls for assay development and validation | Quantification of analytical sensitivity; cross-reactivity panels |
| Clinical Specimen Panels | Provide well-characterized samples for assay validation | Assessment of clinical sensitivity and specificity; reproducibility testing |
| Species-Specific Monoclonal Antibodies | Enable detection and differentiation of parasitic antigens | Development of immunoassays for specific parasitic infections |
| Target-Specific Molecular Probes | Facilitate development of nucleic acid amplification tests | PCR/RT-PCR assays for parasite detection; quantification of parasite load |
| Culture Media for Parasite Propagation | Support maintenance of parasite life cycles for assay development | Production of parasite antigens; drug susceptibility testing |
| Positive/Negative Control Sera | Provide quality control reagents for serological assays | Determination of assay cutoffs; monitoring of assay performance |
| Protein Extraction and Purification Kits | Enable isolation of parasitic antigens for assay development | Production of native or recombinant antigens for immunoassays |
| Nucleic Acid Extraction Kits | Facilitate isolation of high-quality DNA/RNA from clinical samples | Standardization of pre-analytical procedures across sites |
| Stable Cell Lines Expressing Parasite Antigens | Provide consistent antigen source for assay development | Screening of therapeutic candidates; mechanism of action studies |
The FDA's DDT Qualification Program offers a structured pathway for establishing standardized, regulatory-accepted tools that can accelerate therapeutic development for parasitic diseases. While the program has demonstrated measurable output with 17 qualified DDTs to date and 141 projects in development, analysis suggests opportunities for enhanced efficiency and utilization [86] [87] [85].
For parasitic disease researchers, strategic engagement with the DDT Qualification Program requires:
- Early regulatory engagement to align development plans with qualification requirements
- Precompetitive collaboration through public-private partnerships to pool resources and expertise
- Careful definition of context of use that addresses unmet needs in parasitic disease drug development
- Consideration of innovative approaches through the ISTAND Program for novel tool types
The ongoing evolution of the DDT Qualification Program, including recent updates to submission requirements and the emergence of ISTAND, continues to create new opportunities for advancing the development of tools that can ultimately accelerate the availability of effective treatments for parasitic diseases that burden global health.
The definitive diagnosis of parasitic diseases remains a formidable challenge in global health, particularly in resource-limited settings where these infections are most prevalent. Traditional diagnostic methods, such as microscopy and serology, are often constrained by limitations in sensitivity, specificity, and throughput. This whitepaper provides a comparative analysis of three advanced diagnostic methodologies—Loop-Mediated Isothermal Amplification (LAMP), multiplex assays, and nanobiosensors—evaluating their principles, applications, and performance in the context of parasitic disease research. The integration of these technologies offers a promising pathway toward developing rapid, accurate, and field-deployable diagnostic tools, which is crucial for effective disease management, surveillance, and the achievement of public health objectives.
Parasitic infections such as malaria, schistosomiasis, and leishmaniasis present a significant global health burden, affecting millions of people, particularly in tropical and subtropical regions [8] [9]. The economic impact is profound, with diseases like malaria alone costing economies billions of dollars and hindering development in endemic areas [9]. The diagnosis of these diseases has long relied on traditional techniques including microscopic examination, which requires a high level of expertise and is often insufficient in sensitivity, and serological tests like Enzyme-Linked Immunosorbent Assay (ELISA), which can be hampered by cross-reactivity and an inability to distinguish between past and current infections [90] [9] [91].
The need for rapid, sensitive, and specific diagnostic tools is especially critical in point-of-care (POC) settings, where infrastructure and trained personnel are limited. Molecular diagnostics such as Polymerase Chain Reaction (PCR) have improved sensitivity and specificity but require sophisticated thermocycling equipment and are not easily adaptable to field use [92] [7]. This has driven the development and refinement of advanced platforms like LAMP, multiplex assays, and nanobiosensors. These technologies promise to revolutionize parasitic disease diagnosis by offering isothermal amplification, simultaneous multi-target detection, and ultra-sensitive biomarker recognition, respectively [92] [90] [93]. This review provides a technical guide for researchers and drug development professionals, offering a comparative analysis of these platforms to inform the development of next-generation diagnostic solutions.
Loop-Mediated Isothermal Amplification (LAMP)
Principles and Mechanisms: LAMP is a nucleic acid amplification technique that operates under isothermal conditions, typically between 60–65°C, eliminating the need for complex thermal cycling equipment required by PCR [92]. The reaction utilizes a DNA polymerase with high strand displacement activity and a set of four to six primers that recognize six to eight distinct regions on the target DNA. This complex primer design confers exceptionally high specificity [92]. Amplification can be detected in real-time or at the endpoint via various methods, including turbidity, fluorescence with intercalating dyes, or colorimetric changes with metal indicators [92].
Advantages for Parasitic Diagnosis: The key advantages of LAMP include its rapid reaction time (often 45-60 minutes), high tolerance to inhibitors present in clinical samples, and operational simplicity, making it well-suited for POC applications [92]. Furthermore, the ability to lyophilize or dry (dry-LAMP) reaction components facilitates room-temperature storage and transport, breaking the cold chain requirement [92].
Multiplexing Capabilities (mLAMP): A significant advancement in LAMP technology is its adaptation for multiplex detection. Methodologies such as DARQ (Detection of Amplification by Release of Quenching) and QUASR (Quenching of Unincorporated Amplification Signal Reporters) enable the simultaneous detection of multiple pathogens in a single tube [92].
- DARQ-LAMP: Involves primers modified with a fluorophore and a quencher. Upon amplification, the separation of the fluorophore from the quencher generates a measurable fluorescence signal, allowing for real-time, multiplex quantification [92]. This has been successfully applied for the simultaneous detection of Plasmodium species (P. vivax, P. falciparum) and the human actin gene [92].
- QUASR-LAMP: Uses fluorophore-labeled primers and complementary quencher probes. Post-amplification, the signal is read at endpoint; negative samples result in quenched fluorescence, while positive samples exhibit a fluorescence signal. This method is suitable for colorimetric visualization, potentially aided by smartphone applications [92].
Nanobiosensors
Principles and Mechanisms: Nanobiosensors are analytical devices that integrate nanotechnology with biological recognition elements to detect target analytes at the nanoscale [90] [14]. They typically consist of a biorecognition element (e.g., antibody, DNA probe, aptamer) immobilized on a nanomaterial transducer. Upon binding to a parasitic biomarker (antigen, nucleic acid, etc.), a physicochemical change occurs that is converted into a measurable signal [90] [94].
Key Nanomaterials and Transduction Mechanisms: The performance of nanobiosensors is heavily dependent on the nanomaterials used, which enhance sensitivity and specificity.
- Metallic Nanoparticles: Gold and silver nanoparticles are widely used due to their unique optical properties, such as Localized Surface Plasmon Resonance (LSPR), which is highly sensitive to changes in the local refractive index upon target binding [93].
- Quantum Dots (QDs): These semiconductor nanocrystals are prized for their bright, narrow, and tunable fluorescence emissions. Different QDs can be excited by a single light source, making them ideal for multiplexed assays [95].
- Carbon Nanotubes and Graphene Oxide: These materials offer high electrical conductivity and large surface areas, making them excellent for electrochemical and fluorescence-quenching-based biosensors [90] [14].
Applications in Parasitology: Nanobiosensors have been developed for a range of parasitic infections. For example:
- Plasmodium: Gold nanoparticles (AuNPs) functionalized with antibodies can detect Plasmodium falciparum histidine-rich protein 2 (PfHRP2) [90] [14].
- Leishmania: QDs labeled with DNA probes target kinetoplast DNA (kDNA) for highly sensitive detection [90] [14].
- Schistosoma: Graphene oxide (GO)-based sensors can detect soluble egg antigens (SEA) [90] [14].
Multiplex Assays
Principles and Broader Context: Multiplex assays refer to platforms capable of simultaneously detecting multiple distinct analytes from a single sample. While mLAMP is a specific molecular multiplexing technique, the broader category includes protein-based immunoassays (e.g., multiplex ELISA) and bead-based arrays [95]. The core principle involves spatially separating or using unique labels for different targets to avoid cross-reactivity.
Advantages for Complex Parasitology: The ability to detect co-infections is a major strength, as approximately 30% of human infections may involve multiple pathogens [92]. Multiplexing reduces sample volume requirements, analysis time, and cost per data point while increasing throughput and providing a more comprehensive diagnostic picture [92] [95]. This is crucial for syndromic surveillance and for diseases with similar clinical presentations.
Comparative Performance Analysis
The following table summarizes the key characteristics of these three diagnostic approaches, highlighting their relative strengths and limitations for parasitic disease diagnosis.
Table 1: Comparative Analysis of Advanced Diagnostic Platforms for Parasitic Diseases
| Parameter | LAMP | Multiplex LAMP (mLAMP) | Nanobiosensors |
|---|---|---|---|
| Sensitivity | Very High (detects low copy numbers) [92] | Very High [92] | Extremely High (e.g., femtomolar levels) [90] |
| Specificity | Very High (6-8 primer recognition sites) [92] | Very High (probe-based methods) [92] | Extremely High (target-specific probes) [90] |
| Multiplexing Capacity | Low (in simplex format) | Moderate to High (e.g., DARQ: up to 4 targets) [92] | High (multiple labels, e.g., QDs) [93] [95] |
| Speed & Time-to-Result | Rapid (45-60 min) [92] | Rapid (45-60 min) [92] | Very Rapid (minutes to hours) [90] |
| Ease of Use / Equipment Needs | Low (water bath/block); suitable for POC [92] | Low to Moderate (may require fluorescence reader) [92] | Moderate to High (technical expertise for fabrication/operation) [90] |
| Key Advantage | Isothermal amplification, field-deployable | Simultaneous multi-pathogen detection in a single tube | Ultra-sensitive, direct biomarker detection, miniaturization |
| Key Limitation | Complex primer design, risk of carry-over contamination [92] | Optimization complexity, signal interference [92] | Mass production challenges, biological matrix interference [90] [14] |
Experimental Protocols for Key Methodologies
DARQ-LAMP for Multiplex Parasite Detection
This protocol is adapted from methods used for the simultaneous detection of Plasmodium spp., P. vivax, P. falciparum, and the human actin gene [92].
1. Reagent Preparation:
- Primer Design: Design standard LAMP primer sets (F3, B3, FIP, BIP, LF, LB) for each target gene. For one target, modify the FIP primer at the 5′ end with a quencher (e.g., BHQ-1). Design a complementary oligonucleotide (Fd) to the F1c region of the same FIP, and label its 3′ end with a fluorophore (e.g., FAM). This forms the Quencher Probe Duplex (QPD) [92].
- Reaction Mix: Prepare a master mix containing:
- 1.25 µL of each FIP/BIP primer (for all targets)
- 0.625 µL of each LF/LB primer (for all targets)
- 0.3125 µL of each F3/B3 primer (for all targets)
- 12.5 µL of 2X isothermal amplification buffer
- 1 µL of Bst DNA polymerase (8 U/µL)
- 1 µL of the QPD for each target
- Nuclease-free water to a final volume of 25 µL per reaction.
2. Amplification and Detection:
- Add the master mix to PCR tubes containing the DNA template (e.g., 2 µL of extracted genomic DNA from blood).
- Incubate the reactions at 63°C for 60 minutes in a real-time fluorometer.
- Monitor fluorescence in the respective channels for each fluorophore (e.g., FAM, HEX, Cy5) in real-time.
3. Data Analysis:
- A positive amplification is indicated by a fluorescence signal that exceeds a predetermined threshold. The time to positivity (Tp) can be used for quantification [92].
Quantum Dot-Based Lateral Flow Immunoassay for Protozoan Antigen Detection
This protocol outlines the development of a multiplex nanobiosensor for detecting parasitic antigens, such as those from Leishmania or Schistosoma [90] [95] [14].
1. Conjugation of Detection Probes:
- QD-Antibody Conjugation: Activate carboxylated QDs (emitting at 525 nm, 585 nm, etc.) using EDC (1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide) and NHS (N-Hydroxysuccinimide) chemistry. Mix the activated QDs with anti-target antibodies (e.g., anti-SEA for Schistosoma). Purify the QD-antibody conjugates via centrifugation or filtration [95].
2. Assay Assembly and Execution:
- Test Strip Preparation: On a nitrocellulose membrane, dispense capture antibodies for different parasites at specific test lines (T1, T2). Dispense control antibodies (e.g., anti-species IgG) at the control line (C).
- Sample Application: Apply the clinical sample (e.g., 100 µL of serum) to the sample pad. The sample migrates via capillary action.
- Reaction and Detection: As the sample rehydrates the conjugate pad, it mobilizes the QD-antibody probes. If the target antigen is present, it forms a complex with the QD-probe. This complex is captured at the respective test line, forming a fluorescent band.
- Signal Readout: After 15-20 minutes, scan the test strip using a handheld fluorescence reader or a smartphone-based detector with appropriate filters. The presence of a fluorescent band at a test line confirms a positive result [95].
Visualization of Core Methodologies
DARQ-LAMP Mechanism Workflow
The following diagram illustrates the mechanism of DARQ-LAMP, a key method for multiplexing LAMP assays.
Optical Nanobiosensor Detection Principle
This diagram outlines the general working principle of an optical nanobiosensor for parasitic antigen detection.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for developing and implementing the diagnostic technologies discussed in this review.
Table 2: Essential Research Reagent Solutions for Diagnostic Development
| Reagent/Material | Function/Application | Specific Examples in Context |
|---|---|---|
| Bst DNA Polymerase | Enzyme for isothermal amplification in LAMP; possesses strand displacement activity [92]. | Core enzyme in LAMP and mLAMP assays for parasitic DNA/RNA detection (e.g., for Plasmodium [92]). |
| Fluorophore-Labeled Primers/Probes | Enable real-time or endpoint fluorescence detection in multiplexed assays [92]. | Used in DARQ-LAMP (FAM, BHQ) and QUASR-LAMP for differentiating multiple parasitic targets in one reaction [92]. |
| Quantum Dots (QDs) | Semiconductor nanoparticles as fluorescent labels; narrow emission bands enable multiplexing [90] [95]. | QDs conjugated with antibodies or DNA probes for detecting Leishmania kDNA or Schistosoma antigens in nanobiosensors [90] [14]. |
| Gold Nanoparticles (AuNPs) | Nanomaterial used as a transduction element; colorimetric or LSPR-based detection [93]. | Functionalized with anti-PfHRP2 antibodies for detection of Plasmodium falciparum in lateral flow assays [90] [14]. |
| Functionalized Magnetic Nanoparticles | Used for sample preparation; isolate and concentrate target analytes from complex samples [90]. | Extraction of parasitic nucleic acids or antigens from blood or stool samples prior to LAMP or biosensor detection [90]. |
| Capture Antibodies | Immobilized recognition elements for specific antigen detection in immunoassays and biosensors [95]. | Coated on microplates (QLISA) or test strips (LFA) to capture parasitic antigens (e.g., Echinococcus EgAgB) [90] [95]. |
The definitive diagnosis of parasitic diseases is undergoing a transformative shift, driven by technological innovations in molecular amplification, multiplexing, and nanotechnology. LAMP stands out for its robustness and field-deployability, multiplex assays for their comprehensive profiling capability, and nanobiosensors for their exceptional sensitivity and potential for miniaturization. The choice of technology depends on the specific application requirements, including the need for multiplexing, available infrastructure, and desired turnaround time.
Future advancements will likely focus on integrating these platforms, such as combining LAMP with nanobiosensor detection or incorporating CRISPR-Cas systems for enhanced specificity [7] [8]. Furthermore, the development of multiplex nanobiosensors using hybrid nanomaterials and their integration into lab-on-a-chip platforms represent the frontier of POC diagnostics [90] [93]. Overcoming challenges related to mass production, standardization, and validation in diverse field settings will be crucial for the widespread adoption of these tools. For researchers and drug development professionals, a deep understanding of these comparative technologies is essential for driving innovation and developing the next generation of diagnostic solutions that will ultimately curb the global burden of parasitic diseases.
In the field of parasitic disease research, the pathway from discovering a potential diagnostic biomarker to implementing a clinically useful test requires navigating a complex validation landscape. Two fundamental concepts—analytical validation and clinical utility—form the cornerstone of this process, yet they are often conflated. Analytical validation demonstrates that a test accurately and reliably measures the target analyte, while clinical utility determines whether using the test results improves patient outcomes or clinical decision-making [96] [97]. For parasitic diseases, which affect nearly a quarter of the global population and pose significant challenges in tropical and subtropical regions, this distinction is particularly critical [9]. The context of use—the specific clinical scenario and application—defines the evidence requirements for both analytical and clinical validation [98] [99].
The complex life cycles of parasites, their interaction with host immunity, and the challenges of drug resistance necessitate diagnostic tests with rigorously defined performance characteristics [9] [100]. Without proper analytical validation, even a test targeting a biologically relevant parasite marker cannot yield trustworthy results. Without demonstrated clinical utility, a technically perfect test may not inform treatment decisions, streamline workflows, or ultimately enhance patient care [96]. This technical guide examines the relationship between these concepts within the framework of parasitic disease research and drug development.
Foundational Concepts and Definitions
The Validation Hierarchy: From Technical Performance to Patient Impact
The evaluation of diagnostic tests follows a hierarchical model that establishes whether a test is technically sound, clinically meaningful, and practically beneficial.
Analytical Validity refers to how accurately and reliably an test detects the target analyte. It focuses on the test's technical performance under controlled conditions [101] [97]. Key parameters include accuracy, precision, sensitivity, specificity, and reproducibility, which must be assessed during the method development process [102] [103].
Clinical Validity establishes how accurately the test predicts or correlates with the patient's clinical status. It confirms that the test is clinically meaningful by determining how well the test result associates with the presence, absence, or future development of a specific parasitic disease [101]. This is typically expressed through measures of clinical sensitivity, clinical specificity, and predictive values.
Clinical Utility defines the likelihood that the test will lead to improved patient outcomes by informing clinical management decisions [96] [101]. The National Cancer Institute defines clinical utility as "the likelihood that a test will, by prompting an intervention, result in an improved health outcome" [96]. Beyond direct health outcomes, clinical utility can encompass emotional, social, cognitive, and behavioral benefits that impact patient wellbeing [96].
The relationship between these concepts is sequential yet interdependent. A test must demonstrate adequate analytical validity before its clinical validity can be established, and both are prerequisites for determining clinical utility [96] [99]. The FDA distinguishes between analytical method validation (assessing assay performance characteristics) and clinical qualification (the evidentiary process linking a biomarker with biological processes and clinical endpoints) [98].
The Context of Use as a Defining Framework
The context of use specifies how a test will be employed in clinical practice and defines the necessary evidence for its validation [98] [99]. This context determines the stringency requirements for both analytical and clinical validation. For parasitic diseases, contexts of use may include:
- Mass screening programs in endemic regions
- Diagnostic confirmation in symptomatic patients
- Treatment monitoring and efficacy assessment
- Drug development clinical trials
- Surveillance and eradication programs
The specific context drives the acceptable performance criteria. For example, a test for schistosomiasis intended for mass drug administration monitoring would require different evidence than one designed for treatment efficacy assessment in clinical trials [100]. The FDA's guidance on Next Generation Sequencing tests illustrates how regulatory requirements vary across three levels based on intended use, with companion diagnostics requiring the highest rigor [99].
Analytical Validation: Establishing Technical Reliability
Core Performance Parameters
Analytical validation establishes the fundamental performance characteristics of a diagnostic test through assessment of key parameters. The table below summarizes these essential metrics and their significance in parasitic diagnostic development.
Table 1: Key Parameters in Analytical Method Validation for Parasitic Diagnostics
| Parameter | Definition | Significance in Parasitic Diagnostics |
|---|---|---|
| Accuracy | Closeness of test results to the true value | Ensures correct identification and quantification of parasite load [102] |
| Precision | Repeatability and reproducibility across trials and analysts | Critical for reliable monitoring of treatment response in chronic infections [102] [103] |
| Specificity | Ability to distinguish target parasite from impurities, degradation products, or other organisms | Essential for differentiating morphologically similar parasites or co-infections [102] [9] |
| Sensitivity (Limit of Detection) | Lowest amount of parasite antigen, DNA, or biomarker reliably detected | Determines ability to detect low-level infections and early treatment efficacy [102] [103] |
| Linearity and Range | Ability to produce results proportional to analyte concentration across the measurement interval | Important for correlating parasite burden with disease severity and progression [102] [103] |
| Robustness | Resilience to variations in testing conditions (temperature, pH, reagents) | Crucial for tests deployed in field settings with variable environmental conditions [102] [9] |
Method Development and Workflow
The analytical method development process follows a structured pathway to ensure precision and reliability. In pharmaceutical manufacturing and diagnostic development, this process includes understanding the drug compound or diagnostic target, selecting appropriate analytical techniques, optimizing method parameters, assessing specificity and sensitivity, and conducting preliminary validation [102]. For parasitic diagnostics, this might involve selecting between microscopy, serological assays, molecular techniques, or emerging technologies based on the intended application [9].
The following workflow diagram illustrates the analytical validation pathway from method development through implementation:
Figure 1: Analytical Method Development and Validation Workflow
The lifecycle of an analytical method begins when a pharmaceutical company or laboratory recognizes the need for a new analytical method [103]. Following development, a validation plan is prepared and executed. Once validation confirms the method's suitability for its intended purpose, standard operating procedures are developed for routine execution. The method should be continually monitored throughout its lifecycle, with criteria established for revalidation when changes occur [103].
Clinical Utility: Measuring Impact on Patient Outcomes
Defining Clinical Utility in Parasitic Diseases
Clinical utility represents the ultimate measure of a diagnostic test's value—its ability to improve patient outcomes and enhance clinical decision-making. According to the National Cancer Institute definition, clinical utility refers to "the likelihood that a test will, by prompting an intervention, result in an improved health outcome" [96]. For parasitic diseases, this encompasses multiple dimensions:
- Impact on clinical decision-making: Does the test result guide appropriate treatment selection? For example, determining whether a test for drug-resistant malaria leads to more effective antimalarial prescribing [100].
- Streamlined clinical workflow: Does the test improve efficiency in diagnosis or monitoring? This is particularly relevant in resource-limited settings with high parasitic disease burdens [96] [9].
- Improved patient outcomes: Does test use lead to better survival, reduced morbidity, or enhanced quality of life? In schistosomiasis control programs, this might involve assessing whether a new diagnostic approach contributes to reduced transmission or complication rates [100].
- Cost offsets or avoidance: Does the test reduce overall healthcare costs through earlier diagnosis, targeted treatment, or avoided complications? Economic considerations are crucial for adoption in endemic regions with limited healthcare resources [96].
The Association for Molecular Pathology supports patient-centered definitions of clinical utility that focus on the ability of test results to "diagnose, monitor, prognosticate, or predict disease progression, and to inform treatment and reproductive decisions" [96]. This perspective can be extended to parasitic diseases, where diagnostic results inform mass drug administration strategies, individual treatment regimens, and public health interventions.
Assessment Frameworks and Endpoints
Several established frameworks guide the evaluation of clinical utility. The Fryback and Thornbury hierarchical model includes clinical utility as a key component in evaluating diagnostic efficacy, while the ACCE model (Analytic validity, Clinical validity, Clinical utility, and Ethical, legal, and social implications) developed by the Centers for Disease Control and Prevention defines clinical utility in terms of a test's impact on patient outcomes and value added to clinical decision-making [96].
A workgroup supported by the American Society for Microbiology outlines that diagnostic tests must show improved efficiency in clinical decision-making, streamlined clinical workflow, better patient outcomes, and/or cost offsets to demonstrate clinical utility [96]. For parasitic diseases, relevant endpoints might include:
- Reduction in time to appropriate treatment
- Decreased transmission rates in endemic areas
- Improved targeted use of antiparasitic medications
- Reduction in disease complications (e.g., hepatic fibrosis in schistosomiasis)
- Cost per case averted in mass drug administration programs [100]
The Interdependence: How Analytical Validation Supports Clinical Utility
The Sequential Relationship
The pathway from analytical validation to clinical utility follows a logical sequence where each step builds upon the previous one. A test that fails analytical validation cannot establish clinical validity, and without clinical validity, clinical utility cannot exist [96] [99]. This relationship creates a dependency chain where deficiencies in earlier stages compromise later assessments.
The sequential nature of this relationship means that:
- Analytical validity establishes the foundation - Without accurate measurement of the target analyte, no clinically meaningful interpretation is possible.
- Clinical validity builds the connection - This phase links the test result to the clinical condition, demonstrating that what the test measures matters clinically.
- Clinical utility demonstrates real-world impact - This final step shows that acting on the test result improves outcomes.
For parasitic diagnostics, this sequence might involve first validating a PCR test's ability to detect Schistosoma DNA (analytical validity), then establishing that PCR positivity correlates with active infection (clinical validity), and finally demonstrating that using PCR results to guide treatment reduces complication rates compared to standard practice (clinical utility) [9] [100].
Context-Dependent Performance Requirements
The required stringency of analytical performance depends on the clinical context and intended use. The FDA's tiered approach to Next Generation Sequencing tests illustrates how regulatory requirements vary based on context of use [99]. This concept applies equally to parasitic disease diagnostics.
Table 2: Context-Dependent Requirements for Parasitic Disease Diagnostics
| Context of Use | Analytical Requirements | Clinical Utility Endpoints |
|---|---|---|
| Mass Screening in Endemic Areas | High throughput, good sensitivity, moderate specificity | Reduction in community transmission rates, cost per case identified [9] [100] |
| Confirmatory Diagnosis in Symptomatic Patients | High specificity and positive predictive value | Appropriate treatment initiation, reduced unnecessary drug use [9] |
| Clinical Trial Endpoint | High precision and reproducibility | Demonstration of drug efficacy, correlation with clinical outcomes [98] [100] |
| Drug Resistance Monitoring | High sensitivity for specific mutations | Guidance of effective treatment regimens, prevention of resistance spread [100] |
The relationship between analytical performance and clinical impact can be visualized as follows:
Figure 2: Interdependence of Validation Stages Guided by Context of Use
Case Studies and Experimental Approaches in Parasitic Diseases
Schistosomiasis Control and Drug Development
Schistosomiasis control programs provide a compelling case study for examining the relationship between diagnostic validation and clinical utility. Current mass drug administration programs rely primarily on praziquantel, but diagnostic approaches vary from traditional microscopy to molecular methods [100].
Research on improved drug formulations for schistosomiasis illustrates how clinical utility assessments guide development priorities. Mathematical modeling suggests that drugs with higher efficacy (99% vs current ~85%) or prolonged efficacy would provide the greatest improvement to community-level control, while improved efficacy against juvenile worms offers more modest benefits [100]. These findings directly inform the clinical utility endpoints for new diagnostic tests that might monitor different aspects of treatment response.
Experimental approaches for validating schistosomiasis diagnostics include:
- Comparative sensitivity/specificity studies against gold standard methods
- Longitudinal monitoring of treatment response correlated with clinical outcomes
- Community-level impact assessments measuring changes in transmission dynamics
- Cost-effectiveness analyses comparing new diagnostics to existing approaches
The Evolution of Parasitic Diagnostic Technologies
The field of parasitic diagnosis has evolved from basic microscopy to incorporate serological, molecular, and emerging artificial intelligence-based approaches [9]. Each technological advancement requires re-establishment of both analytical validation and clinical utility.
Molecular diagnostics like PCR and next-generation sequencing offer improved sensitivity and specificity over traditional microscopy for many parasitic diseases [9]. However, these technical improvements do not automatically translate to clinical utility. In resource-limited settings, factors like cost, infrastructure requirements, and turn-around time may limit the clinical utility of technically superior tests. This highlights how the context of use determines whether improved analytical performance translates to enhanced clinical value.
Essential Research Reagents and Materials
The development and validation of parasitic diagnostics requires specific research tools and materials. The following table details key reagent solutions and their functions in diagnostic development.
Table 3: Essential Research Reagent Solutions for Parasitic Diagnostic Development
| Research Reagent | Function in Diagnostic Development | Application Examples |
|---|---|---|
| Reference Parasite Strains | Provide standardized material for assay validation | Quality control, limit of detection studies [9] |
| Clinical Specimens with Defined Status | Establish clinical sensitivity and specificity | Biobanks with microscopy-confirmed positive and negative samples [9] [98] |
| Molecular Biology Reagents | Enable development of nucleic acid-based tests | PCR, qPCR, LAMP assays for parasite detection [9] |
| Immunoassay Components | Support serological test development | Recombinant antigens, monoclonal antibodies, conjugate reagents [9] |
| Cell Culture Systems | Maintain parasite life cycles for assay development | In vitro drug sensitivity testing, antigen production [100] |
The distinction between analytical validation and clinical utility, guided by the context of use, forms a critical framework for advancing parasitic disease diagnostics. Analytical validation ensures that a test measures the target accurately and reliably, while clinical utility demonstrates that using the test improves patient outcomes or clinical decision-making. These concepts are interdependent yet distinct, with the context of use determining the evidence requirements for each.
For researchers and drug development professionals working on parasitic diseases, explicitly defining the context of use at the outset of diagnostic development ensures that validation efforts align with clinical applications. This approach focuses resources on establishing the appropriate level of evidence for both technical performance and clinical impact, ultimately accelerating the development of diagnostics that address the significant global burden of parasitic infections.
The evolving landscape of parasitic diagnostics—from basic microscopy to advanced molecular methods and artificial intelligence—continues to highlight the importance of this distinction [9]. As new technologies emerge, maintaining clear differentiation between analytical validation and clinical utility will remain essential for translating technical innovations into clinically meaningful tools for parasitic disease control and elimination.
Framework for Regulatory Approval and WHO Prequalification of Diagnostic Tests
The definitive diagnosis of parasitic diseases is a critical pillar in global public health, directly impacting the treatment and control of infections that affect billions worldwide, particularly in tropical and subtropical regions. The development of novel diagnostic tests, however, must culminate in regulatory approval and World Health Organization (WHO) prequalification (PQ) to ensure they are safe, effective, and accessible, especially in low- and middle-income countries (LMICs). WHO prequalification is a pivotal service that aims to promote and facilitate access to safe, appropriate, and affordable in vitro diagnostics (IVDs) of good quality [104] [105]. This framework acts as a standardized benchmark for global procurement agencies, such as the Global Fund, and facilitates national regulatory approvals through collaborative procedures. For parasitic diseases—which account for 13 of the 20 WHO-listed neglected tropical diseases (NTDs)—navigating the pathway from research to a prequalified product is a complex but essential endeavor for researchers and drug development professionals [9]. This guide provides a detailed technical examination of the regulatory and prequalification framework, placing it within the critical context of advancing diagnostic research for parasitic infections.
The WHO Prequalification Process for IVDs
The WHO PQ process is a comprehensive assessment that evaluates the quality, safety, and performance of IVDs intended for use in LMICs. The process is underpinned by a risk-based classification system, where diagnostics are categorized according to their potential public health impact and risk to the individual [104]. For parasitic diseases, tests typically fall into higher-risk categories (e.g., Class C), necessitating a more stringent level of scrutiny.
Key Stages of the Prequalification Journey
The PQ pathway is a multi-stage process that requires meticulous preparation and ongoing compliance from manufacturers.
1. Eligibility and Pre-submission: The first step is determining a product's eligibility. WHO publishes Technical Specification Series (TSS) documents for specific disease areas or types of assays. These TSS documents outline the precise requirements for performance characteristics, intended use settings, and target product profiles [104]. For instance, in 2025, WHO has advanced TSS documents for IVDs detecting sexually transmitted infections, which serve as a model for pathogen-specific requirements [106] [105]. A manufacturer must complete a pre-submission form (PQDx_015) to initiate dialogue with the WHO PQ team.
2. Product Dossier Submission and Assessment: The core of the application is the submission of a product dossier. The dossier must be compiled per WHO instructions (PQDx018) and checklist (PQDx049), providing exhaustive evidence on the product's quality, safety, and performance [104]. This includes:
- Manufacturing and Quality Management System (QMS) Information: Demonstration of compliance with ISO 13485:2016 is required [107].
- Performance Evaluation Data: Data from rigorous clinical performance studies and stability testing.
- Risk Management Documentation.
WHO conducts scheduled assessment sessions throughout the year where expert committees review submitted dossiers. For 2025, six such sessions are scheduled, and complete submissions must be received at least 14 days prior to a session [106].
3. Laboratory Evaluation: The WHO PQ program typically subjects IVDs to an independent laboratory evaluation to verify the performance claims made in the dossier. This step is crucial for validating the test's real-world accuracy.
4. Site Inspection: An inspection of the manufacturing site(s) is conducted to assess compliance with the quality management system and good manufacturing practices [104] [107].
5. Prequalification Decision and Listing: Upon successful completion of all stages, the IVD is added to the WHO list of prequalified diagnostics, signaling to global procurers that it meets international standards.
6. Post-Prequalification Requirements: Prequalification is not static. Manufacturers must engage in post-market surveillance and report any significant changes to the product (e.g., in design, manufacturing process, or suppliers) through a formal change assessment process [104]. Documents like PQDx_121 provide guidance on reportable changes.
The following diagram illustrates the key stages of the WHO Prequalification process.
Associated Pathways and Timelines
The standard PQ process can be lengthy. For emergent public health needs, the WHO Emergency Use Listing (EUL) procedure provides an expedited pathway. The EUL allows for the time-limited use of IVDs based on a minimum available set of quality, safety, and performance data, as was utilized for MPOX (monkeypox) detection kits [107] [106].
Another critical pathway for diagnostics that are not yet prequalified is the Expert Review Panel for Diagnostics (ERP-D). The ERP-D assesses the risk-benefit ratio of innovative IVDs with high public health impact, advising procurement agencies on time-limited use. This is particularly relevant for novel diagnostic technologies for neglected parasitic diseases that may not yet have a dedicated TSS [105].
For researchers, understanding the financial and temporal commitment is key. While costs are not always public, WHO does charge prequalification fees (PQDx_299), and manufacturers should account for the need for external expert support to navigate the process [104] [107].
Diagnostic Technologies in Parasitology: From Development to Validation
The evolution of diagnostic technologies for parasitic diseases has been transformative, moving from basic microscopy to sophisticated molecular and serological assays. This progression directly influences the type of data required for a successful regulatory submission.
Table 1: Key Diagnostic Technologies for Parasitic Diseases
| Technology Platform | Target Analyte | Common Parasitic Disease Applications | Key Performance Characteristics | Considerations for Regulatory Submission |
|---|---|---|---|---|
| Rapid Diagnostic Tests (RDTs) / Lateral Flow Immunoassays (LFIAs) | Antigens or host antibodies | Malaria, Schistosomiasis, Leishmaniasis, Chagas disease [8] | Speed (results in 15-20 mins), ease of use, low cost. Sensitivity can vary [8]. | Stability data under diverse climatic conditions is critical. Must demonstrate performance in intended use settings (e.g., community clinics). |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Antigens or host antibodies | Cysticercosis, Strongyloidiasis, Toxoplasmosis [108] [8] | High throughput, quantitative results. Potential for cross-reactivity [9]. | Data must demonstrate specificity against a panel of related parasites. |
| Polymerase Chain Reaction (PCR) & Multiplex PCR | Parasite Nucleic Acid (DNA/RNA) | Malaria, Leishmaniasis, Cryptosporidiosis [9] [8] | High sensitivity and specificity. Can differentiate species and strains. Requires lab infrastructure. | Detailed analytical sensitivity (Limit of Detection) and inclusivity/exclusivity data required. |
| Next-Generation Sequencing (NGS) | Parasite Genomic Material | All, particularly for strain typing, outbreak investigation, and drug resistance analysis [9] [8] | Provides comprehensive genomic data. | Validation of complex bioinformatics pipelines is a key part of the submission. |
| CRISPR-Cas Based Assays | Parasite Nucleic Acid | Emerging for malaria, schistosomiasis [8] | High specificity, potential for POC use. | As a novel technology, extensive data package proving robustness and reproducibility is needed. |
| Automated Microscopy with AI | Parasite morphology in samples | Malaria, intestinal parasites [9] [8] | Increases throughput and consistency of microscopy. | Validation of the AI algorithm with large, diverse datasets is essential to demonstrate accuracy. |
Case Study: Advanced Molecular Detection (AMD) for Schistosomiasis
A prime example of innovation in parasitic diagnostics is the use of AMD for schistosomiasis. The traditional process of manually analyzing hundreds of potential protein targets for immunoassay development was unsustainable, taking approximately 10 days and being prone to human error. By leveraging AMD and advanced bioinformatics, CDC scientists created an automated system that could examine ~500 targets in just a few hours. This dramatic reduction in timeline accelerated the development of new serological tests not only for schistosomiasis but also for other parasitic diseases like cysticercosis and strongyloidiasis [108]. This case highlights the importance of robust, data-driven target selection in the early R&D phase, which forms the foundation of a successful regulatory application.
Experimental Design and Methodologies for Diagnostic Validation
Generating the robust evidence required for WHO PQ demands carefully designed experiments. The following protocols outline key methodologies for establishing the analytical and clinical validity of a new diagnostic test for parasitic diseases.
Protocol 1: Clinical Performance Evaluation (Sensitivity and Specificity)
Objective: To determine the clinical sensitivity and specificity of the index test against a validated comparator (reference standard) in a representative patient population.
Materials:
- Index test kits and all necessary reagents.
- Samples from well-characterized patient cohorts (e.g., known positive and negative for the target parasite).
- Reference standard method (e.g., PCR, expert microscopy, or a previously WHO-prequalified test).
- Appropriate laboratory equipment (pipettes, incubators, readers).
- Data collection forms or electronic data capture system.
Procedure:
- Ethics and Sample Collection: Obtain ethical approval and informed consent. Collect patient samples (e.g., blood, stool, skin lesion specimens) according to standardized procedures that preserve the target analyte.
- Blinding: Ensure that operators performing the index test and the reference standard are blinded to the results of the other test to prevent bias.
- Testing: Perform the index test and the reference standard on all samples independently, strictly following the manufacturers' instructions for use (IFU).
- Data Analysis:
- Construct a 2x2 contingency table comparing the index test results against the reference standard.
- Calculate Sensitivity = (True Positives / (True Positives + False Negatives)) * 100.
- Calculate Specificity = (True Negatives / (True Negatives + False Positives)) * 100.
- Calculate 95% confidence intervals for both estimates.
Regulatory Consideration: A major challenge is imperfect reference standards. If the reference standard (e.g., microscopy) has suboptimal sensitivity, it can lead to biased accuracy estimates. Using latent class analysis or discrepant analysis can help address this, but these approaches must be justified in the submission [109].
Protocol 2: Limit of Detection (LoD) Determination
Objective: To establish the lowest concentration of the parasite that the test can reliably detect.
Materials:
- Cultured parasites or synthetic targets (e.g., recombinant antigen, synthetic DNA).
- Negative sample matrix (e.g., negative human serum, stool).
- Serial dilution equipment.
Procedure:
- Sample Preparation: Create a series of dilutions of the parasite target in the negative sample matrix, covering a range expected to be around the LoD.
- Replication: Test each dilution level multiple times (e.g., 20 replicates) in a single run.
- Testing and Analysis: Perform the index test on all replicates. The LoD is the lowest concentration at which ≥95% of the replicates test positive.
Regulatory Consideration: The LoD should be established using clinically relevant strains of the parasite and in the same sample type as intended for the final test.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Diagnostic Development and Validation
| Research Reagent / Material | Function in Development/Validation | Application Example |
|---|---|---|
| Recombinant Parasitic Antigens | Serve as positive controls and for calibrating immunoassays; used to immunize animals for antibody production. | Development of RDTs for Schistosoma haematobium [108]. |
| Monoclonal and Polyclonal Antibodies | Key recognition elements in immunoassays (e.g., RDTs, ELISA). Specificity is paramount. | Detecting Plasmodium falciparum HRP-II antigen in malaria RDTs. |
| Synthetic Oligonucleotides | Primers and probes for PCR assays; controls for molecular test development. | Designing a multiplex PCR for intestinal protozoa [8]. |
| Characterized Biobanks | Panels of well-defined clinical samples from infected and non-infected individuals used for clinical validation. | Determining clinical sensitivity and specificity against a reference standard [109]. |
| Reference Standards | Well-accepted, validated tests or materials used as a comparator to evaluate the performance of the new index test. | Using quantitative PCR as a reference standard for a new LAMP assay [109]. |
The workflow from research to a validated diagnostic test involves multiple parallel tracks of development and validation, as shown below.
Navigating Global Regulatory Landscapes and Collaborative Procedures
Achieving WHO PQ is a significant milestone, but it does not automatically grant market authorization in individual countries. Navigating the final step to national registration is crucial for patient access.
The Collaborative Registration Procedure (CRP)
To accelerate national registrations, WHO facilitates the Collaborative Registration Procedure. Under the CRP, participating countries' National Regulatory Authorities (NRAs) can leverage the detailed assessment and inspection reports generated by WHO during the PQ process [105]. This reliance mechanism avoids duplication of effort, optimizes resources, and significantly shortens the approval time in participating countries. For example, products can be approved in countries like Zambia, Tanzania, South Africa, and Kenya within 90 days of submission under the CRP [105]. This procedure is a powerful tool for manufacturers to achieve broad geographic distribution efficiently.
Challenges and Recommendations for Researchers
Despite these pathways, challenges persist, particularly for developers targeting parasitic diseases:
- Information Asymmetry: A lack of clarity in procedures and low awareness among applicants can hinder the process [105].
- Quality of Submission: Incomplete dossiers or discrepancies in submitted information are a primary cause of delays [105].
- Local Unmet Needs: Developers must consider the specific needs of LMICs during the product design phase (e.g., stability in high heat and humidity, ease of use) [105].
Recommendations for Success:
- Early Engagement: Interact with the WHO PQ team and relevant NRAs during the development phase to align with current TSS and expectations.
- Robust Study Design: Plan validation studies meticulously from the outset, using appropriate statistical methods and accounting for potential biases like spectrum bias or imperfect reference standards [109].
- Leverage Work-Sharing: Promote and participate in work-sharing initiatives among NRAs in LMICs to further streamline regulatory processes.
The framework for regulatory approval and WHO prequalification of diagnostic tests is a meticulous, evidence-driven pathway that is fundamental to translating research innovation into impactful tools for the definitive diagnosis of parasitic diseases. For researchers and developers, a deep understanding of this framework—from the initial design of validation studies that meet WHO technical specifications to the strategic navigation of post-prequalification collaborative procedures—is not merely a regulatory hurdle but an integral component of the research lifecycle. By integrating these requirements early and planning for the comprehensive data generation needed for a successful product dossier, the scientific community can significantly accelerate the delivery of high-quality, accessible diagnostics to the front lines of the fight against parasitic diseases, ultimately improving global health outcomes.
Conclusion
The definitive diagnosis of parasitic diseases is undergoing a profound transformation, moving from reliance on century-old techniques to a new era of precision medicine. The integration of molecular methods, nanobiosensors, and multi-omics is delivering unprecedented gains in sensitivity, specificity, and speed, which are critical for both clinical management and drug development. However, the path forward requires a concerted effort to overcome hurdles in standardization, cost, and deployment in resource-limited settings. Future success hinges on collaborative innovation—fostering partnerships between academia, industry, and regulators—to refine these advanced tools, develop multiplex point-of-care platforms, and validate biomarkers that can serve as surrogate endpoints in clinical trials. By embracing these innovations, the scientific community can significantly accelerate therapeutic development and ultimately achieve the goal of controlling and eliminating parasitic diseases worldwide.
References
- 1. Approach to Parasitic Infections - Infectious Diseases [https://www.merckmanuals.com/professional/infectious-diseases/approach-to-parasitic-infections/approach-to-parasitic-infections]
- 2. Global impact of parasitic infections and the importance ... [https://www.frontiersin.org/journals/parasitology/articles/10.3389/fpara.2025.1546195/full]
- 3. Effective Laboratory Diagnosis of Parasitic Infections of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11475984/]
- 4. The Global Prevalence of and Factors Associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195843/]
- 5. Parasitic Diseases Therapeutic Market Chart | Size, Growth ... [https://www.linkedin.com/pulse/parasitic-diseases-therapeutic-market-mfmcc/]
- 6. Estimation and prediction on the economic burden of ... [https://pubmed.ncbi.nlm.nih.gov/40524274/]
- 7. Recent Advancements in the Diagnosis of Parasitic Diseases [https://pubmed.ncbi.nlm.nih.gov/41138779/]
- 8. Recent advancements in the diagnosis of parasitic diseases [https://www.sciencedirect.com/science/article/abs/pii/S0166685125000428]
- 9. Parasitic diagnosis: A journey from basic microscopy to cutting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617590/]
- 10. Diagnosis of Parasitic Diseases: Old and New Approaches [https://pmc.ncbi.nlm.nih.gov/articles/PMC2804041/]
- 11. Principles of microscopy, culture and serology-based ... [https://www.sciencedirect.com/science/article/abs/pii/S1357303917301913]
- 12. Effective Laboratory Diagnosis of Parasitic Infections of the ... [https://www.mdpi.com/2075-4418/14/19/2148]
- 13. A Comparative Analysis of Microscopy, Coproantigen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9381307/]
- 14. Nanobiosensors for revolutionizing parasitic infections ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02685-2]
- 15. A faster route to eliminating parasitic infection endemic ... [https://medicine.washu.edu/news/a-faster-route-to-eliminating-parasitic-infection-endemic-to-africa/]
- 16. Challenges in drug discovery targeting TriTryp diseases with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6195035/]
- 17. Estimating sensitivity of the Kato-Katz technique for the ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0005953]
- 18. Automated parasitological diagnosis in clinical ... - Nature [https://www.nature.com/articles/s41598-021-92441-3]
- 19. Control of Neglected Tropical Diseases [https://www.who.int/teams/control-of-neglected-tropical-diseases/interventions/research]
- 20. Digital PCR: a new technology for diagnosis of parasitic ... [https://www.sciencedirect.com/science/article/pii/S1198743X19303167]
- 21. Next Generation Sequencing (NGS) vs. PCR [https://www.cd-genomics.com/resource-ngs-vs-pcr.html]
- 22. 实时è§å…‰å®šé‡PCR原ç†åŠåŸºç¡€çŸ¥è¯† - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/essentials-real-time-pcr.html]
- 23. NGS, qPCR, or Sanger Sequencing: An Assay Selection ... [https://blog.genewiz.com/ngs-qpcr-or-sanger-sequencing-an-assay-selection-guide]
- 24. 定é‡èšåˆé…¶é“¾å应和数å—èšåˆé…¶é“¾å应的检测方法 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/genomics/qpcr/quantitative-pcr-and-digital-pcr-detection-methods?srsltid=AfmBOoqyJKB-OQG7k4c6OgckaXnpzCiU-M7wzB_xvU5BYcP08YE2y57J]
- 25. NGS vs Sanger Sequencing [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-sanger.html]
- 26. 综述:寄生虫病诊æ–的最新进展 [https://www.ebiotrade.com/newsf/2025-10/20251025003002204.htm]
- 27. é‡ç—‡ä¹‹çª—| 脓毒症诊æ–çš„æ–°å¼æ¦å™¨â€”—下一代DNA测åºæŠ€æœ¯ [https://bydrug.pharmcube.com/news/detail/7ae843729fcb121f77566598df3fa428]
- 28. Comparative performance of microscopy, rapid diagnostic ... [https://pubmed.ncbi.nlm.nih.gov/39833795/]
- 29. Loop-mediated isothermal amplification (LAMP) [https://pubmed.ncbi.nlm.nih.gov/41077252/]
- 30. LAMP in Neglected Tropical Diseases: A Focus on Parasites [https://pmc.ncbi.nlm.nih.gov/articles/PMC8000616/]
- 31. Review Loop-Mediated Isothermal Amplification (LAMP): A ... [https://www.sciencedirect.com/science/article/abs/pii/S0166685125000404]
- 32. Development of loop mediated isothermal amplification ... [https://www.nature.com/articles/s41598-025-93995-2]
- 33. Field deployment of loop-mediated isothermal amplification for ... [https://malariajournal.biomedcentral.com/articles/10.1186/s12936-015-0731-2]
- 34. Evaluation of the Illumigene Malaria LAMP: A Robust ... [https://www.nature.com/articles/srep36808]
- 35. A comprehensive guide to loop-mediated isothermal ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1568657/full]
- 36. Development of PCR, qPCR and LAMP methods for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508883/]
- 37. Retrospect, advances and challenges in Chagas disease ... [https://www.sciencedirect.com/science/article/pii/S2667193X24001480]
- 38. Nanobiosensors for Single-Molecule Diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564644/]
- 39. Recent Advancements in Nanobiosensors: Current Trends ... [https://www.mdpi.com/2079-6374/12/10/892]
- 40. Nanobiosensors in neurodegenerative disease diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078979/]
- 41. Quantum dot-infused nanocomposites - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr00440c?page=search]
- 42. Next-generation immunoassays for diagnosis [https://www.nature.com/articles/d42473-024-00342-6]
- 43. Immunoassay Methods - Assay Guidance Manual - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK92434/]
- 44. Performance evaluation of serological assays to determine ... [https://www.sciencedirect.com/science/article/pii/S1386653220303310]
- 45. Proteomics Investigations of Potential Protein Biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8729878/]
- 46. DNDi 2025 Projects of the Year recognize contributions ... [https://dndi.org/news/2025/2025-projects-of-the-year-recognize-contributions-teams-partners-working-innovations-chagas-disease-river-blindness/]
- 47. Multi-omics Data Integration, Interpretation, and Its Application [https://pmc.ncbi.nlm.nih.gov/articles/PMC7003173/]
- 48. Parasite genetics, genomics and proteomics [https://parasitesandvectors.biomedcentral.com/articles/sections/parasite-genetics-genomics-and-proteomics]
- 49. Proteomics on Parasites Services [https://biogenity.com/parasites-proteomics]
- 50. The role of multi-omics in biomarker discovery, diagnosis, ... [https://pubmed.ncbi.nlm.nih.gov/40822515/]
- 51. Machine learning enhances biomarker discovery: From multi [https://esmed.org/MRA/mra/article/view/6888]
- 52. Integrated Multi-Omics Powered Ecosystem | ASM.org [https://asm.org/about-asm/asm-strategic-roadmap/asm-health/intergrated-multi-omics-powered-ecosystem]
- 53. Specificity and Cross-Reactivity - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK2396/]
- 54. Specificity of SARS-CoV-2 Antibody Detection Assays against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8769729/]
- 55. Comparative analyses of parasites with a comprehensive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8901074/]
- 56. Changing Cross-Reactivity for Different Immunoassays ... [https://www.mdpi.com/2076-3417/11/14/6581]
- 57. Trend in serological and molecular diagnostic methods for ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-024-02055-4]
- 58. Diagnostic Techniques: Serological and Molecular Approaches [https://pmc.ncbi.nlm.nih.gov/articles/PMC7157465/]
- 59. Biological Matrix Effects in Quantitative Tandem Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4695332/]
- 60. Strategies for the Detection and Elimination of Matrix ... [https://www.chromatographyonline.com/view/strategies-detection-and-elimination-matrix-effects-quantitative-lc-ms-analysis]
- 61. What is Matrix Interference and How Does It Affect Testing? [https://www.arborassays.com/what-is-matrix-interference/?srsltid=AfmBOoq0HvuDMpewDaqQX45c_DD42Jp5S8NFE-TrxfcNdk2dwM72zwr7]
- 62. Managing Matrix Interference in Immunoassays: Tips and ... [https://www.bio-connect.nl/news/managing-matrix-interference-in-immunoassays-tips-and-solutions/]
- 63. Overview of Methods and Considerations for Handling ... [https://www.chromatographyonline.com/view/overview-methods-and-considerations-handling-complex-samples]
- 64. Sample Collection & Processing Best Practices For Labs [https://qbench.com/blog/sample-collection-processing-best-practices-for-labs]
- 65. Ensuring Reproducibility in Biological Research [https://www.labmanager.com/ensuring-reproducibility-in-biological-research-34610]
- 66. Chapter 15 Experimental protocols | Lab Handbook [https://ccmorey.github.io/labHandbook/experimental-protocols.html]
- 67. Diagnosis of Parasitic Diseases [https://www.cdc.gov/parasites/testing-diagnosis/index.html]
- 68. Top 10 Strategies to Improve Scientific Reproducibility [https://www.labarchives.com/blog/top-10-strategies-to-improve-scientific-reproducibility-with-labarchives-eln-for-research]
- 69. 7 Best Comparison Charts for Effective Data Visualization [https://ninjatables.com/types-of-comparison-charts/?srsltid=AfmBOop_JYFnpwGPL9P-xqeG4KbcTAvY2gfQqgEr7c4kXv2VVRTfTni7]
- 70. Point-of-Care Diagnostics: Recent Developments in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5793870/]
- 71. Machine learning in point-of-care testing: innovations, ... [https://www.nature.com/articles/s41467-025-58527-6]
- 72. Cost-Effectiveness Analysis [https://www.herc.research.va.gov/include/page.asp?id=cost-effectiveness-analysis]
- 73. Reducing Cost of Production - 7 Ways [https://www.machinemetrics.com/blog/reduce-cost-of-production]
- 74. 3 Steps for Effective Manufacturing Cost Analysis [https://www.apriori.com/blog/3-steps-for-effective-manufacturing-cost-analysis/]
- 75. Research progress on diagnostic techniques for different ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1575227/full]
- 76. Review CRISPR-Cas systems: Pioneering next-generation ... [https://www.sciencedirect.com/science/article/abs/pii/S0166685125000441]
- 77. Ova and Parasite Test Market Forecast 2025-2032 [https://www.linkedin.com/pulse/ova-parasite-test-market-forecast-2025-2032-anticipating-zltbf]
- 78. Quantitative Monitoring of Selected Groups of Parasites in ... [https://www.mdpi.com/2076-0817/10/9/1173]
- 79. Advances in paper-based ELISA techniques [https://www.sciencedirect.com/science/article/abs/pii/S016599362400606X]
- 80. Improving Malaria diagnosis through interpretable ... [https://www.nature.com/articles/s41598-025-90851-1]
- 81. Development of a Highly Specific Monoclonal Antibody-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568205/]
- 82. Next-Generation ELISA (ELISA 2.0) Market Research ... [https://www.insightaceanalytic.com/report/next-generation-elisa-market/3241]
- 83. Drug Development Tool (DDT) Qualification Programs [https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tool-ddt-qualification-programs]
- 84. Drug Development Tool (DDT) qualification process [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/drug-development-tool-ddt-qualification-process]
- 85. Has FDA's Drug Development Tools Qualification Program ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181102/]
- 86. Summary Metrics of Drug Development Tool Qualification ... [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/summary-metrics-drug-development-tool-qualification-projects-submitted-fda]
- 87. Has FDA's Drug Development Tools Qualification Program ... [https://pubmed.ncbi.nlm.nih.gov/40320513/]
- 88. FDA proposal threatens access to critical ID diagnostic tests [https://www.idsociety.org/science-speaks-blog/2023/fda-proposal-threatens-access-to-critical-id-diagnostic-tests/]
- 89. ISTAND Program [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/innovative-science-and-technology-approaches-new-drugs-istand-program]
- 90. Nanobiosensors for revolutionizing parasitic infections diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12168311/]
- 91. Diagnosis of parasitic diseases | Research Starters [https://www.ebsco.com/research-starters/consumer-health/diagnosis-parasitic-diseases]
- 92. Multiplexing LAMP Assays: A Methodological Review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11203869/]
- 93. Multiplexed Optical Nanobiosensing Technologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562344/]
- 94. Emerging Applications of Nanobiosensors in Pathogen ... [https://www.mdpi.com/2079-6374/13/10/922]
- 95. Multiplexed Nanobiosensors: Current Trends in Early ... [https://www.mdpi.com/1424-8220/20/23/6890]
- 96. The concept of clinical utility for diagnostic tests [https://www.thermofisher.com/blog/clinical-conversations/the-concept-of-clinical-utility-for-diagnostic-tests/]
- 97. Best Practices for Biomarker Testing Coverage Glossary [https://www.cancercare.org/biomarkertoolkitglossary]
- 98. Validation of Analytical Methods for Biomarkers Employed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2744124/]
- 99. Molecular Diagnostics with Clinical Utility: Their Promise in ... [https://globalforum.diaglobal.org/issue/october-2018/molecular-diagnostics-with-clinical-utility-their-promise-in-advancing-precision-medicine-in-cancer/]
- 100. How improvements to drug effectiveness impact mass drug ... [https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0012624]
- 101. Genetic Tests:Clinical Validity and Clinical Utility - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4084965/]
- 102. Understanding Analytical Method Development and ... [https://www.upm-inc.com/understanding-analytical-method-development-and-validation]
- 103. An Introduction to Analytical Method Development and ... [https://www.sofpromed.com/an-introduction-to-analytical-method-development-and-validation-in-early-phase-clinical-trials]
- 104. Prequalification Guidance - WHO/OMS: Extranet Systems [https://extranet.who.int/prequal/vitro-diagnostics/prequalification-guidance]
- 105. Regulatory Pathways to Promote Access to STI Diagnostics [https://avac.org/resource/report/regulatory-pathways-to-promote-access-to-sti-diagnostics/]
- 106. WHO Prequalification of IVDs: Q1 2025 Newsletter [https://www.linkedin.com/pulse/who-prequalification-ivds-q1-2025-newsletter-irena-prat-wcece]
- 107. WHO Prequalifications for IVDs [https://www.nsf.org/life-sciences/medical-devices/who-pre-qualifications-ivds]
- 108. Improving Parasite Tests | AMD [https://www.cdc.gov/advanced-molecular-detection/php/success-stories/improving-parasite-tests.html]
- 109. A unified framework for diagnostic test development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11632097/]