Advancing Parasitology Diagnostics: A Comprehensive Guide to Real-Time PCR for Intestinal Protozoa
This article provides a comprehensive resource for researchers and scientists on the implementation of real-time PCR (qPCR) for detecting pathogenic intestinal protozoa.
Advancing Parasitology Diagnostics: A Comprehensive Guide to Real-Time PCR for Intestinal Protozoa
Abstract
This article provides a comprehensive resource for researchers and scientists on the implementation of real-time PCR (qPCR) for detecting pathogenic intestinal protozoa. It covers the foundational rationale for moving beyond traditional microscopy to molecular methods, detailing specific assay designs—including singleplex, duplex, and triplex protocols—for targets like Giardia duodenalis, Cryptosporidium spp., Entamoeba histolytica, and Dientamoeba fragilis. The content explores automated high-throughput platforms, troubleshooting for common issues like inhibitor management and DNA extraction, and presents validation data comparing commercial versus in-house tests against reference standards. By synthesizing recent multicentre and validation studies, this guide aims to support robust assay development, improve diagnostic accuracy, and inform drug efficacy testing in clinical and research settings.
The Molecular Shift: Why qPCR is Replacing Microscopy for Intestinal Protozoa Diagnosis
The Global Burden and Diagnostic Challenge of Intestinal Protozoa
Intestinal protozoan pathogens represent a significant and persistent global health challenge, contributing substantially to diarrheal morbidity and mortality worldwide. These infections disproportionately affect resource-limited settings where poor sanitation and inadequate water infrastructure facilitate transmission [1]. This application note, framed within a broader thesis on real-time PCR protocols for intestinal protozoa research, provides a comprehensive overview of the disease burden, conventional diagnostic limitations, and advanced molecular solutions for detecting these pathogens, with detailed experimental protocols for researchers and scientists.
The global impact of these infections is staggering. Recent meta-analyses reveal that protozoan pathogens are responsible for approximately 7.5% of diarrheal cases globally, with the highest prevalence observed in the Americas and Africa [1]. Collectively, intestinal protozoan parasites infect nearly 3.5 billion people worldwide and contribute to an estimated 1.7 billion annual diarrheal episodes [2] [3]. Among the most clinically significant enteric protozoa, Cryptosporidium spp., Giardia duodenalis, and Entamoeba histolytica account for an estimated 500 million annual diarrheal cases worldwide, contributing significantly to childhood morbidity, malnutrition, and developmental delays [1].
Global Epidemiology and Health Impact
The burden of intestinal protozoan infections reveals striking geographical and demographic disparities. Children under five in low- and middle-income countries (LMICs) are disproportionately affected, where these pathogens are responsible for 10-15% of diarrheal deaths and are increasingly recognized as contributors to long-term growth faltering and cognitive impairment [1]. Cryptosporidium alone causes approximately 200,000 deaths annually, with the highest burden in sub-Saharan Africa and South Asia [1].
Table 1: Global Prevalence and Impact of Major Intestinal Protozoa
| Parasite | Global Prevalence/Incidence | Key Health Impacts | High-Risk Populations |
|---|---|---|---|
| Giardia duodenalis | 280 million symptomatic cases annually [3] | Watery diarrhea, bloating, malabsorption, chronic malnutrition [1] | Children in developing countries [4] |
| Cryptosporidium spp. | 1-4% worldwide; up to 10% in children in low-income regions [1] | Severe watery diarrhea; life-threatening in immunocompromised patients [1] | Children under 5, immunocompromised individuals [1] [5] |
| Entamoeba histolytica | About 1-2% true infections (10% carry Entamoeba species) [1] | Amoebiasis - bloody diarrhea, dysentery, liver abscess [1] | Populations in Central/South America, parts of Asia [1] |
| Blastocystis spp. | 50-60% in developing countries [5] | Often asymptomatic; potential association with irritable bowel syndrome [5] | General population; role in health/disease debated [4] |
The epidemiology of these infections is influenced by complex transmission patterns involving environmental, climatic, and anthropogenic factors. Climate change is altering transmission dynamics, with studies linking increased rainfall intensity to Cryptosporidium outbreaks and drought conditions to Giardia proliferation [1]. Urbanization has introduced new transmission patterns, with dense informal settlements creating ideal conditions for person-to-person spread [1].
Diagnostic Challenges and Limitations of Conventional Methods
Accurate diagnosis of intestinal protozoa remains challenging, particularly in resource-limited settings. Conventional microscopy, while widely used for its cost-effectiveness and simplicity, presents significant limitations:
- Low Sensitivity and Specificity: Microscopy-based surveillance misses 30-50% of cases detectable by molecular methods [1]. The sensitivity of light microscopy for Cryptosporidium with modified acid-fast stain is only 54.8% [4].
- Inability to Differentiate Species: Microscopy cannot differentiate pathogenic E. histolytica from non-pathogenic E. dispar and E. moshkovskii [4]. Similarly, Blastocystis consists of at least seven morphologically identical but genetically different organisms [4].
- Technical Expertise Requirements: Microscopy requires highly trained personnel, and results are subjective with inter-observer variability [5] [3].
- Time-Consuming Nature: Comprehensive microscopic examination is labor-intensive and requires experienced examiners for optimal interpretation [4].
These diagnostic challenges lead to underestimation of the true disease burden, inappropriate treatment, and impaired disease surveillance. Immunodiagnostic methods such as ELISA, while offering improved speed, still demonstrate variable sensitivity and specificity compared to molecular methods [4].
Molecular Diagnostics: Real-Time PCR Solutions
Molecular diagnostics, particularly real-time PCR (qPCR), have revolutionized the detection of intestinal protozoa by offering enhanced sensitivity, specificity, and species-level differentiation. Molecular methods enable accurate detection of protozoan infections that are often missed by conventional techniques [6] [5] [3].
Advantages of qPCR for Intestinal Protozoa Detection
- Enhanced Sensitivity and Specificity: qPCR demonstrates significantly higher sensitivity compared to microscopy and antigen-based tests [3].
- Species-Level Differentiation: qPCR can distinguish morphologically identical species such as E. histolytica and E. dispar [5] [4].
- Quantification Capabilities: Provides quantitative data on parasite load, potentially correlating with disease severity [7].
- High-Throughput Capacity: Enables processing of large sample volumes efficiently [3].
- Detection of Mixed Infections: Multiplex assays allow simultaneous detection of multiple pathogens in a single reaction [7].
Table 2: Research Reagent Solutions for Protozoan Detection by qPCR
| Reagent/Equipment | Function/Application | Examples/Specifications |
|---|---|---|
| Primers/Probes | Target-specific amplification and detection | Custom designs for E. histolytica 16S-like SSU rRNA, G. duodenalis gdh, Cryptosporidium 18S rRNA [7] |
| DNA Extraction Kits | Nucleic acid purification from stool samples | QIAamp DNA Mini Kit, QIAamp DNA Fast Stool Mini Kit (Qiagen) [7] |
| qPCR Master Mix | Amplification reaction components | 2× TaqMan Fast Universal PCR Master Mix [3] |
| qPCR Instruments | Amplification and detection platform | ABI 7900HT Fast Real-Time PCR System, CFX Maestro [3] [5] |
| Standard Plasmids | Quantification standards | Recombinant plasmids (PUC19 vector) with target inserts [7] |
Experimental Protocol: Duplex qPCR for Intestinal Protozoa
The following protocol adapts methodologies from recent studies for detecting intestinal protozoa using qPCR [6] [5] [7]:
Sample Collection and DNA Extraction
Sample Collection:
- Collect fresh stool samples or preserve in appropriate media (e.g., Para-Pak, S.T.A.R Buffer).
- Note: Preserved samples may yield better DNA quality [3].
DNA Extraction:
- Use commercial DNA extraction kits (e.g., QIAamp DNA Mini Kit, MagNA Pure 96 System).
- Mix 350 µL of stool transport buffer with approximately 1 µL of fecal sample.
- Incubate for 5 minutes at room temperature, then centrifuge at 2000 rpm for 2 minutes.
- Transfer 250 µL of supernatant for automated or manual DNA extraction.
- Include an internal extraction control to monitor extraction efficiency.
- Store extracted DNA at -20°C until analysis [3] [7].
qPCR Assay Setup
Reaction Composition:
Thermal Cycling Conditions:
Controls:
- Include positive controls (quantified standard plasmids)
- Negative controls (no-template and extraction controls)
- Internal amplification controls to detect inhibition [7]
Primer and Probe Design Considerations
- Target genetically conserved regions with species-specific variations (e.g., 18S rRNA, gdh genes).
- Ensure GC content of approximately 50% and melting temperature of ~58°C.
- Verify specificity using BLAST analysis against non-target species.
- For multiplex assays, use probes with distinct fluorophores with non-overlapping emission spectra [5] [7].
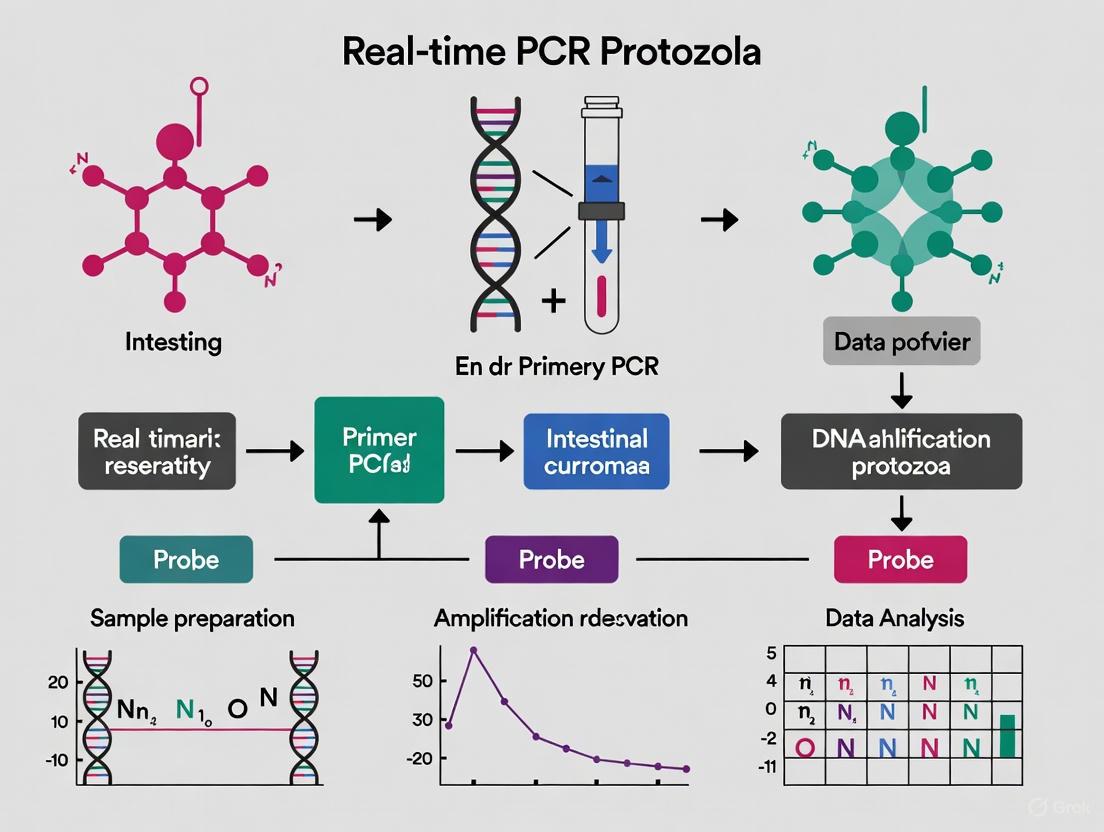
Workflow Visualization: Molecular Detection of Intestinal Protozoa
The following diagram illustrates the comprehensive workflow for detecting intestinal protozoa using molecular methods:
Application in Research and Drug Development
Molecular diagnostics for intestinal protozoa play a crucial role in pharmaceutical research and drug development. Accurate detection methods are essential for:
- Clinical Trial Monitoring: qPCR provides sensitive assessment of treatment efficacy in anti-protozoal drug trials [6] [5].
- Epidemiological Studies: Accurate prevalence data informs public health interventions and resource allocation [1] [8].
- Transmission Dynamics: Molecular typing helps elucidate transmission routes and zoonotic potential [1] [4].
Recent studies have applied these methods to evaluate potential anti-protozoal compounds. For instance, a study on Pemba Island, Tanzania, utilized qPCR to assess emodepside's efficacy against intestinal protozoa, demonstrating the application of these methods in clinical research [6] [5].
Intestinal protozoan infections remain a significant global health challenge, particularly in resource-limited settings and among vulnerable populations. The development and implementation of robust molecular diagnostic methods, particularly real-time PCR protocols, are essential for accurate disease surveillance, clinical management, and drug development research. The protocols outlined in this application note provide researchers with detailed methodologies for detecting these important pathogens, contributing to improved understanding and control of intestinal protozoan diseases worldwide.
Future directions in this field include the development of point-of-care molecular tests, standardized multiplex assays for a broader range of pathogens, and integration of molecular diagnostics into routine surveillance programs in endemic areas.
Despite its long-standing role as a reference method in parasitology, conventional microscopy for intestinal protozoa diagnosis is hampered by significant limitations in sensitivity, specificity, and dependence on expert operators [9] [3]. These constraints are particularly critical in research settings and drug development programs, where diagnostic accuracy directly impacts experimental outcomes and therapeutic efficacy assessments. This application note delineates these limitations through quantitative data analysis and establishes the foundation for integrating advanced molecular methodologies into intestinal protozoa research workflows aligned with your thesis on real-time PCR protocols.
Quantitative Performance Analysis
Comparative Diagnostic Sensitivity
Multiple studies demonstrate significantly higher detection rates for molecular methods compared to conventional microscopy across major intestinal protozoa.
Table 1: Comparative Sensitivity of Microscopy Versus Molecular Methods
| Parasite | Microscopy Sensitivity | PCR Sensitivity | Study Characteristics | Citation |
|---|---|---|---|---|
| Giardia intestinalis | 38.0% (9/24) | 100% (24/24) | 889 samples, Danish patients | [10] |
| Cryptosporidium spp. | 0% (0/16) | 100% (16/16) | 889 samples, Danish patients | [10] |
| Dientamoeba fragilis | Not detectable | 100% (167/167) | 889 samples, Danish patients | [10] |
| Blastocystis sp. | 30.0% (19/64) | Gold standard | Compared to culture (64 positive) | [10] |
| Multiple Protozoa | 28.7% (286/995) | 90.9% (909/995) | 3,495 samples, prospective study | [11] |
Species Differentiation Capability
Microscopy cannot reliably differentiate morphologically identical species with divergent clinical significance, a critical limitation for pathogen-specific research.
Table 2: Microscopy Limitations in Species Differentiation
| Microscopic Identification | Molecular Differentiation | Clinical/Research Significance | Citation |
|---|---|---|---|
| Entamoeba histolytica/dispar/moshkovskii | E. histolytica (pathogenic) | Causes amoebic dysentery, requires treatment | [9] [12] |
| E. dispar (non-pathogenic) | Considered a commensal, no treatment needed | [5] [9] | |
| Various amoebae | E. moshkovskii (potentially pathogenic) | Pathogenicity still under investigation | [9] |
Experimental Protocols
Standard Microscopy Protocol for Intestinal Protozoa
Principle: Visual identification of protozoan trophozoites, cysts, and oocysts through morphological examination of concentrated stool samples.
Materials:
- Fresh stool sample (multiple samples recommended)
- Formalin-ethyl acetate concentration reagents
- Microscope slides and coverslips
- Light microscope with 10×, 40×, and 100× objectives
- Iodine and other staining solutions
Procedure:
- Sample Collection: Collect three stool samples on alternate days to account for intermittent shedding [9].
- Concentration: Process samples using formalin-ethyl acetate concentration technique (FECT) or similar method [10] [11].
- Slide Preparation: Prepare wet mounts from concentrated sediment with and without iodine staining.
- Microscopic Examination:
- Systematically scan entire coverslip area (22 × 22 mm) at 100× and 400× magnification
- Identify protozoa based on size, shape, nuclear characteristics, and motility
- Examine multiple fields to detect low-intensity infections
- Interpretation: Differentiate pathogenic from non-pathogenic species based on morphological criteria.
Limitations: This protocol is labor-intensive, requires 30-45 minutes per sample, and depends heavily on technician expertise [9] [3]. Sensitivity remains limited even with multiple samples.
Real-Time PCR Protocol for Intestinal Protozoa
Principle: Multiplex real-time PCR detection of protozoan DNA from stool samples, enabling species-specific identification and differentiation.
Materials:
- Stool sample (200 mg) in appropriate transport medium
- DNA extraction kit (e.g., MagnaPure LC.2, MagNA Pure 96)
- Multiplex PCR master mix (e.g., SsoFast master mix, AllPlex GI-Parasite Assay)
- Real-time PCR instrument (e.g., CFX96, ABI 7900HT)
- Species-specific primers and probes
Procedure:
- DNA Extraction:
- PCR Setup:
- Prepare reaction mix containing:
- PCR buffer
- BSA (2.5 µg)
- Primers and probes (species-specific concentrations)
- Internal control primers/probe
- Aliquot 5-10 µL DNA template
- Prepare reaction mix containing:
- Amplification:
- Cycling conditions: 3 min at 95°C; 40 cycles of 15 s at 95°C, 30-60 s at 60°C
- Fluorescence detection at each cycle
- Analysis:
- Set threshold to 200 RFU
- Cq values <40 considered positive
- Verify internal control amplification
Advantages: This protocol detects 2.5-3× more positive samples compared to microscopy, differentiates pathogenic species, and processes multiple samples simultaneously [10] [11] [12].
Diagram: Molecular vs. Conventional Diagnostic Workflows - This diagram contrasts the streamlined, automated PCR workflow requiring a single sample against the labor-intensive, multi-sample microscopy approach, highlighting key performance advantages.
The Scientist's Toolkit
Research Reagent Solutions
Table 3: Essential Reagents for Intestinal Protozoa Research
| Reagent/Kit | Primary Function | Research Application | Citation |
|---|---|---|---|
| AllPlex GI-Parasite Assay | Multiplex PCR detection of 6 protozoa | Simultaneous detection of major intestinal pathogens | [11] [12] |
| MagnaPure LC.2/Nimbus | Automated nucleic acid extraction | Standardized DNA purification, reduced cross-contamination | [9] [12] |
| S.T.A.R. Buffer | Stool transport and DNA stabilization | Preserves nucleic acids during storage and transport | [3] |
| Phocine Herpes Virus | Internal extraction control | Monitors PCR inhibition and extraction efficiency | [9] |
| Seegene Viewer Software | PCR result interpretation | Automated analysis of multiplex PCR data | [12] |
| Prothrombin (18-23) | Prothrombin (18-23) | Human Peptide Fragment | Prothrombin (18-23) peptide for coagulation research. High purity, For Research Use Only. Not for human or veterinary diagnosis or therapy. | Bench Chemicals |
| tert-Buty-P4 | tert-Buty-P4 | Superbase Reagent | For Research Use | tert-Buty-P4 is a potent, non-ionic phosphazene superbase for deprotonation and catalysis. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
Conventional microscopy exhibits critical limitations for intestinal protozoa research, with sensitivity rates of 30-75% compared to 90-100% for molecular methods, inability to differentiate pathogenic species, and substantial dependence on technical expertise [10] [9] [11]. These constraints directly impact research quality, particularly in drug development studies requiring precise endpoint measurements. The integration of validated real-time PCR protocols, as detailed in this application note, addresses these limitations through standardized, sensitive, and species-specific detection methods essential for rigorous scientific investigation of intestinal protozoa.
Fundamental Principles and Advantages of Real-Time PCR Technology
Fundamental Principles of Real-Time PCR
Real-time PCR, also known as quantitative PCR (qPCR), is a powerful molecular biology technique that allows for the detection and quantification of nucleic acids in real-time during the polymerase chain reaction, as opposed to at the end of the process like in conventional PCR [13] [14]. The core principle revolves around monitoring the amplification of a targeted DNA molecule as the reaction occurs, providing both qualitative and quantitative data [15].
The Quantification Cycle (Cq) and Amplification Curves
The quantitative capability of real-time PCR is based on the direct relationship between the initial amount of target nucleic acid and the point in the amplification process when a fluorescent signal is first detected above a background threshold [13] [15].
- Amplification Curve Phases: A typical real-time PCR amplification curve features three phases: the linear (ground) phase, the exponential (logarithmic) phase, and the plateau phase [13]. The exponential phase is the most critical for quantification because the reaction components are not yet limiting, and the amplification is most efficient [13].
- Threshold Cycle (Ct)/Quantification Cycle (Cq): This is the fractional PCR cycle number at which the reporter fluorescence exceeds a minimum detectable level, known as the threshold [13]. A sample with a high starting concentration of the target will produce a detectable signal and thus a low Cq value earlier in the amplification process. Conversely, a low initial concentration will result in a high Cq value [14] [15]. This inverse relationship is the foundation for quantification.
Detection Chemistries: Fluorescent Reporters
Real-time PCR systems use fluorescent reporters to monitor amplification, which can be broadly classified into two categories [13]:
- DNA-Binding Dyes: Dyes like SYBR Green I fluoresce brightly when bound to double-stranded DNA [14]. As the PCR product (amplicon) accumulates with each cycle, more dye binds, leading to an increase in fluorescence intensity. While cost-effective and easy to use, a key disadvantage is their lack of specificity, as they will bind to any double-stranded DNA, including non-specific amplicons and primer-dimers [14] [16].
- Sequence-Specific Probes: This category includes hydrolysis probes (e.g., TaqMan probes), molecular beacons, and hybridization probes [13]. These oligonucleotides are designed to be complementary to a specific sequence within the target amplicon and are labeled with a fluorophore and a quencher. For example, in a TaqMan assay, the 5' to 3' exonuclease activity of the DNA polymerase cleaves the probe during amplification, separating the fluorophore from the quencher and generating a fluorescent signal [14] [16]. This mechanism ensures that fluorescence is generated only if the specific target sequence is amplified, providing a high degree of specificity.
Table 1: Comparison of Major Fluorescent Detection Methods in Real-Time PCR.
| Feature | SYBR Green | TaqMan Probes |
|---|---|---|
| Principle | Binds non-specifically to dsDNA | Sequence-specific probe hydrolysis |
| Specificity | Lower; detects any amplicon | High; only the specific target is detected |
| Cost | Lower | Higher |
| Complexity | Simpler; only primers needed | More complex; requires probe design |
| Multiplexing | Not possible | Possible with different colored dyes |
Reverse Transcription Quantitative PCR (RT-qPCR)
To detect and quantify RNA targets (e.g., mRNA for gene expression or RNA viruses), the method is coupled with a reverse transcription step. This combined technique is known as reverse transcription quantitative PCR (RT-qPCR) [17] [15]. The RNA is first transcribed into complementary DNA (cDNA) using a reverse transcriptase enzyme. This cDNA then serves as the template for the subsequent real-time PCR amplification [13] [17]. RT-qPCR can be performed as a one-step or two-step reaction [13] [17].
- One-Step RT-qPCR: The reverse transcription and PCR amplification are performed sequentially in a single tube. This is faster, reduces pipetting steps and contamination risk, and is ideal for high-throughput applications [17].
- Two-Step RT-qPCR: The reverse transcription and PCR amplification are performed in separate tubes with individually optimized reaction conditions. This allows a single cDNA synthesis reaction to be used for multiple qPCR assays targeting different genes and provides more flexibility [13] [17].
Advantages Over Conventional PCR and Microscopy
Real-time PCR offers several significant advantages that make it a gold standard in research and diagnostics [14] [15].
- Quantification: It provides accurate, quantitative data over a broad dynamic range (up to 10^7-fold), enabling precise measurement of gene expression, viral load, or parasite burden [13] [15]. Conventional PCR is, at best, semi-quantitative [14].
- Speed and Throughput: The reaction is monitored in real-time, eliminating the need for post-PCR processing like gel electrophoresis. This speeds up analysis and facilitates high-throughput testing in 96- or 384-well formats [14] [15].
- Sensitivity and Specificity: The technique is extremely sensitive, capable of detecting down to a few copies of a target nucleic acid [15]. When using sequence-specific probes, it achieves high specificity by requiring three specific binding events (two primers and one probe) [16].
- Reduced Contamination Risk: Because the reaction tubes remain sealed after the run, the risk of cross-contamination with amplicons from previous reactions is greatly minimized [13].
- Superiority to Microscopy: For intestinal protozoa diagnosis, real-time PCR offers higher sensitivity and specificity than traditional bright-field microscopy. It can differentiate between morphologically identical species (e.g., pathogenic Entamoeba histolytica and non-pathogenic Entamoeba dispar), is less labor-intensive, and provides objective, automated readouts [5] [12].
Application in Intestinal Protozoa Research: Protocols and Data
The application of real-time PCR has revolutionized the detection and study of intestinal protozoa, providing a tool for precise species identification and burden assessment that is critical for both clinical diagnostics and research.
Experimental Protocol: Duplex qPCR for Entamoeba Species
The following protocol is adapted from a 2025 study implementing real-time PCR assays for diagnosing intestinal protozoa infections [5].
1. Sample Collection and DNA Extraction:
- Collect human stool samples and preserve appropriately (e.g., freezing at -20°C or -80°C).
- Extract genomic DNA from approximately 50-100 mg of stool specimen using a commercial DNA extraction kit. Automated nucleic acid extraction systems, such as the Microlab Nimbus IVD, are recommended for consistency and throughput [12].
2. Primer and Probe Design:
- Design primers and hydrolysis probes to target conserved, specific genomic regions. For a duplex assay detecting E. histolytica and E. dispar simultaneously, ensure each probe is labeled with a distinct fluorophore (e.g., FAM and HEX).
- The study targeting the 18S ribosomal RNA gene used these primers and probes [5]:
- Forward Primer: AGG ATT GGA TGA AAT TCA GAT GTA CA
- Reverse Primer: TAA GTT TCA GCC TTG TGA CCA TAC
- Probe for E. histolytica: TGA TTG AAT GAG TTG CTT CAA GAT GGA GT (e.g., labeled with FAM)
- Probe for E. dispar: A distinct, sequence-specific probe (e.g., labeled with HEX)
3. qPCR Reaction Setup:
- Prepare a 10 µL reaction mixture containing [5]:
- 1X qPCR Master Mix (includes DNA polymerase, dNTPs, MgClâ‚‚)
- Primers (0.5 µM each)
- Probes (concentration as per manufacturer's optimization)
- 2-5 µL of template DNA
- The study utilized a 10 µL reaction volume to reduce reagent costs [5].
4. Thermal Cycling:
- Perform amplification on a real-time PCR instrument with the following typical cycling conditions [14] [5]:
- Initial Denaturation: 95°C for 2-5 minutes
- 40-45 Cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 60 seconds (data collection at this step)
5. Data Analysis:
- Analyze the amplification curves and assign Cq values using the instrument's software.
- Determine the presence of the target based on a Cq value below a predetermined threshold (e.g., 45) [12]. Quantification is achieved by comparing Cq values to a standard curve of known copy numbers.
Diagram 1: Workflow for real-time PCR detection of intestinal protozoa from stool samples.
Performance Data in Protozoal Detection
Real-time PCR demonstrates exceptional performance in detecting intestinal protozoa compared to traditional methods like microscopy and antigen testing.
Table 2: Diagnostic Performance of a Multiplex Real-Time PCR Assay for Intestinal Protozoa (compared to conventional methods) [12].
| Parasite | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Entamoeba histolytica | 100 | 100 |
| Giardia duodenalis | 100 | 99.2 |
| Dientamoeba fragilis | 97.2 | 100 |
| Cryptosporidium spp. | 100 | 99.7 |
A 2025 study in Tanzania further highlights the utility of qPCR in epidemiological research, where it was used to detect a high prevalence of protozoa, with Entamoeba histolytica and E. dispar found in 31.4% of patient samples [5]. The ability to distinguish the pathogenic E. histolytica (which accounted for one-third of these positives) from the non-pathogenic E. dispar is a critical advantage for appropriate patient management and accurate burden of disease studies [5] [12].
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of real-time PCR for intestinal protozoa research requires a set of key reagents and instruments.
Table 3: Essential Research Reagent Solutions for Real-Time PCR-based Protozoa Detection.
| Item | Function/Description | Example/Note |
|---|---|---|
| qPCR Master Mix | A pre-mixed solution containing thermostable DNA polymerase, dNTPs, MgClâ‚‚, and optimized buffer. | Often includes a reference dye for normalization. |
| Sequence-Specific Primers & Probes | Oligonucleotides designed to uniquely amplify and detect the target protozoan DNA. | Hydrolysis probes (TaqMan) are preferred for specificity in multiplex assays [5]. |
| DNA Extraction Kit | For purifying high-quality, inhibitor-free genomic DNA from complex stool matrices. | Automated systems (e.g., Hamilton Microlab Nimbus) enhance reproducibility [12]. |
| Positive Control Plasmid/DNA | A quantified standard containing the target sequence, essential for generating a standard curve for quantification and validating assay performance. | A plasmid clone of the target gene fragment. |
| Real-Time PCR Instrument | A thermal cycler integrated with an optical system to excite fluorophores and detect fluorescence in real-time. | Instruments from Bio-Rad (CFX96) and others. |
| Nuclease-Free Water | A pure, contaminant-free water used to make up reaction volumes, preventing enzymatic degradation of reagents. | Critical for maintaining reaction integrity. |
| 5,5/'-DINITRO BAPTA | 5,5/'-DINITRO BAPTA, CAS:125367-32-0, MF:C22H22N4O14, MW:566.43 | Chemical Reagent |
| Acetylurethane | Acetylurethane, CAS:2597-54-8, MF:C5H9NO3, MW:131.13 g/mol | Chemical Reagent |
Pathogen Profiles and Clinical Significance
Intestinal protozoan parasites are significant global causes of diarrheal diseases, contributing to substantial morbidity and mortality worldwide. This section details the key biological and clinical characteristics of the four major pathogenic targets.
Table 1: Comparative Profile of Key Intestinal Protozoan Pathogens
| Parameter | Giardia duodenalis (lamblia) | Cryptosporidium spp. | Entamoeba histolytica | Dientamoeba fragilis |
|---|---|---|---|---|
| Classification | Diplomonadida (Excavata) [18] | Apicomplexa (Diaphoretickes) [18] | Amoebozoa (Amorphea) [18] | Trichomonadina (Excavata) [18] |
| Primary Site of Infection | Duodenum, Jejunum, Ileum [18] | Duodenum, Jejunum, Ileum [18] | Colon [18] | Colon [18] |
| Global Incidence (Annual, Estimates) | ~280 million symptomatic cases [3] | Not fully quantified; major cause of childhood diarrhea [19] | ~100 million [18] | Common, but not fully quantified [18] |
| Key Clinical Presentation (Acute) | Persistent diarrhea, malabsorption, flatulence [18] [3] | Mild-to-acute diarrhea, nausea, abdominal pain, low-grade fever [18] | Diarrhea, abdominal pain; can progress to dysentery [18] [3] | Abdominal pain, diarrhea, nausea, vomiting, anal pruritus [3] |
| Key Clinical Presentation (Chronic/Severe) | Malabsorption, loose stools, cramping, liver or pancreatic inflammations [18] | Severe diarrhea, vomiting, volume depletion; biliary/respiratory involvement in immunocompromised [18] | Fever, sepsis, liver abscesses, skin lesions [18] | Weight loss, anorexia [3] |
| At-Risk Populations | Young children in poor sanitary conditions, malnourished individuals [18] | Immunocompromised (e.g., HIV), malnourished individuals, children [18] | Individuals in endemic areas with poor sanitation [18] | Not specified in search results |
| First-Line Treatment | Metronidazole [18] | Nitazoxanide (for immunocompetent) [18] | Not specified in search results | Not specified in search results |
Molecular Detection via Real-Time PCR: Protocols and Workflows
Molecular diagnostics, particularly real-time PCR (qPCR), have surpassed traditional microscopy in sensitivity and specificity, enabling precise species-level differentiation crucial for clinical management and research [5] [3]. This section outlines standardized protocols for detecting these pathogens.
Nucleic Acid Extraction
Robust DNA extraction is critical, as the robust wall structure of protozoan cysts and oocysts can impede DNA yield [3].
- Sample Preparation: Mix 350 µL of Stool Transport and Recovery (S.T.A.R) Buffer with approximately 1 µL of fecal sample using a sterile loop. Incubate for 5 minutes at room temperature and centrifuge at 2000 rpm for 2 minutes [3].
- Supernatant Collection: Carefully transfer 250 µL of the supernatant to a fresh tube [3].
- Automated Extraction: Use the MagNA Pure 96 System with the "MagNA Pure 96 DNA and Viral NA Small Volume Kit" for automated nucleic acid purification. Add an internal extraction control (50 µL) to the sample prior to extraction to monitor extraction efficiency and PCR inhibition [3].
- Elution: Elute the purified DNA in a final volume suitable for downstream PCR applications (e.g., 50-100 µL) [3].
qPCR Assay Configuration
Both commercial multiplex and in-house singleplex assays are used for detection.
- Commercial Multiplex Assays: Platforms like the AusDiagnostics test allow for the simultaneous detection of multiple targets in a single reaction, improving workflow efficiency [3].
- In-House Singleplex/Multiplex Assays: Custom-designed assays provide flexibility. A recommended approach uses two duplex qPCR assays: one for Entamoeba dispar + Entamoeba histolytica and another for Cryptosporidium spp. + Chilomastix mesnili, alongside singleplex assays for Giardia duodenalis and Blastocystis spp. [5].
Table 2: Primer and Probe Sequences for In-House qPCR Detection
| Organism | Target Gene | Primer/Probe | Sequence (5' to 3') | Reaction Concentration |
|---|---|---|---|---|
| Giardia duodenalis | Small subunit ribosomal RNA [5] | Forward Primer | GCT GCG TCA CGC TGC TC [5] | 0.5 µM [5] |
| Reverse Primer | GAC GGC TCA GGA CAA CGG T [5] | 0.5 µM [5] | ||
| Cryptosporidium spp. | Small subunit ribosomal RNA [5] | Forward Primer | ACA TGG ATA ACC GTG GTA ATT CT [5] | 0.5 µM [5] |
| Reverse Primer | CAA TAC CCT ACC GTC TAA AGC TG [5] | 0.5 µM [5] | ||
| Entamoeba histolytica | Small subunit ribosomal RNA [5] | Forward Primer | AGG ATT GGA TGA AAT TCA GAT GTA CA [5] | 0.5 µM [5] |
| Reverse Primer | TAA GTT TCA GCC TTG TGA CCA TAC [5] | 0.5 µM [5] | ||
| Entamoeba dispar | 18S ribosomal RNA gene [5] | Forward Primer | AGG ATT GGA TGA AAT TCA GAT GTA CA [5] | 0.5 µM [5] |
| Reverse Primer | TAA GTT TCA GCC TTG TGA CCA TAC [5] | 0.5 µM [5] |
qPCR Reaction Setup and Thermocycling
- Reaction Mixture (In-House Example):
- 5 µL of extracted DNA template
- 12.5 µL of 2x TaqMan Fast Universal PCR Master Mix
- Primer and probe mix (final concentration as specified in Table 2)
- Nuclease-free water to a final volume of 25 µL [3]
- Thermocycling Conditions (In-House Example):
- Initial Denaturation: 95°C for 10 minutes (1 cycle)
- Amplification: 45 cycles of:
- 95°C for 15 seconds (denaturation)
- 60°C for 1 minute (annealing/extension) [3]
The following workflow diagram summarizes the key stages of the qPCR detection process.
The Scientist's Toolkit: Essential Research Reagents
A standardized set of reagents and tools is fundamental for ensuring reproducible and reliable results in protozoan research and diagnostics.
Table 3: Key Research Reagent Solutions for Protozoan Detection
| Item | Function/Description | Example Product/Note |
|---|---|---|
| Sample Transport Medium | Preserves nucleic acid integrity during sample storage and transport. | S.T.A.R. Buffer [3] / Para-Pak media [3] |
| Nucleic Acid Extraction Kit | Automated, high-throughput purification of DNA from complex stool samples. | MagNA Pure 96 DNA and Viral NA Small Volume Kit [3] |
| qPCR Master Mix | Contains DNA polymerase, dNTPs, buffers, and optimized components for efficient amplification. | 2x TaqMan Fast Universal PCR Master Mix [3] |
| Primers & Hydrolysis Probes | Sequence-specific oligonucleotides for target amplification and detection. Fluorescently labeled probes with a quencher. | See Table 2 for sequences [5]; Dyes/Quenchers selected based on detector capabilities [5] |
| Internal Extraction Control | Non-target nucleic acid added to samples to monitor extraction efficiency and PCR inhibition. | Critical for identifying false negatives [3] |
| Positive Control Template | Plasmid or genomic DNA containing the target sequence to validate qPCR assay performance. | Essential for run validation and ensuring primer/probe functionality |
| Commercial Multiplex PCR Kit | Pre-optimized assays for simultaneous detection of multiple pathogens, enhancing workflow efficiency. | AusDiagnostics intestinal protozoa test [3] |
| 5-Fluoro-1-indanone | 5-Fluoro-1-indanone, CAS:700-84-5, MF:C9H7FO, MW:150.15 g/mol | Chemical Reagent |
| Choline chloride-15N | Choline chloride-15N Stable Isotope|287484-43-9 |
:::info The provided protocols and reagent lists serve as a foundational framework. Specific conditions, such as primer concentrations and cycling parameters, may require optimization for different laboratory setups and clinical sample types. :::
From Theory to Bench: Designing and Implementing qPCR Assays for Protozoan Detection
Within the research framework of real-time PCR (qPCR) protocols for intestinal protozoa, the selection of an appropriate assay configuration—singleplex, duplex, or triplex—is a critical determinant of experimental success. These configurations refer to the simultaneous amplification of one, two, or three distinct target sequences in a single reaction, respectively [20]. The shift from traditional, lower-throughput methods like microscopy to molecular techniques is driven by the need for greater sensitivity, specificity, and objectivity in detecting protozoa such as Entamoeba histolytica, Giardia lamblia, and Cryptosporidium spp. [11] [5] [7]. This application note provides a detailed comparison of these qPCR strategies and outlines optimized protocols for their implementation in intestinal protozoa research, providing scientists with the tools to make informed design choices.
Comparative Analysis of qPCR Configurations
The choice between singleplex and multiplex assays involves a direct trade-off between simplicity and throughput. The following table summarizes the core characteristics, advantages, and challenges of each configuration.
Table 1: Strategic Comparison of Singleplex, Duplex, and Triplex qPCR Configurations
| Feature | Singleplex qPCR | Duplex qPCR | Triplex qPCR |
|---|---|---|---|
| Targets per Reaction | One | Two | Three |
| Primary Advantage | Simplicity; no competition for reagents; lack of ambiguity in results [20] | Balanced throughput; internal control for normalization; cost and time savings over singleplex [20] [5] | Maximum efficiency for multi-target screening; highest savings in reagents, samples, and time [20] [7] |
| Key Challenge | Lower throughput; higher reagent consumption; potential well-to-well variation | Requires dye/probe compatibility and careful optimization to prevent competition [20] | Highest complexity; increased risk of reagent competition and signal interference [20] |
| Dye/Probe Requirements | One fluorescent dye (e.g., SYBR Green) or probe (e.g., FAM) [20] | Two spectrally distinct probes (e.g., FAM and VIC) [20] [5] | Three spectrally distinct probes [7] |
| Ideal Application | Absolute quantification; assay development/validation; low-target-number studies | Pathogen detection with internal control; co-infection studies; validated two-target panels [5] | High-throughput screening of defined pathogen panels [7] [21] [22] |
| Optimization Focus | Standard curve generation; efficiency calculation | Primer limiting for dominant targets; balancing reaction efficiencies [20] | Extensive validation against singleplex; rigorous cross-reactivity testing [20] [7] |
Experimental Protocols for Intestinal Protozoa Detection
Development of a Triplex qPCR forE. histolytica,G. lamblia, andC. parvum
This protocol is adapted from a study that established a sensitive and specific triplex assay for three major intestinal protozoa [7].
1. Primer and Probe Design:
- Target Genes: Design specific primers and TaqMan probes for:
- E. histolytica: 16S-like SSU rRNA gene (GenBank X56991.1)
- G. lamblia: gdh gene (GenBank KM190761.1)
- C. parvum: 18S rRNA gene (GenBank NC_006987.1)
- Bioinformatics Validation: Confirm specificity using BLAST and Primer-BLAST against non-target sequences.
- Probe Labeling: Label each probe with a spectrally distinct fluorophore (e.g., FAM, HEX/VIC, Cy5) and a compatible quencher.
Table 2: Example Primer and Probe Sequences for Triplex qPCR [7]
| Organism | Target Gene | Primer/Probe | Sequence (5' to 3') |
|---|---|---|---|
| Entamoeba histolytica | 16S-like SSU rRNA | Forward Primer | AGCAGGATTGGATGAAATTCAGATGTACA |
| Reverse Primer | TAAGTTTCAGCCTTTGTGACCATAC | ||
| Probe | (e.g., FAM)-TGACCACCAATAGTATTC-(MGBNFQ) | ||
| Giardia lamblia | gdh | Forward Primer | GCTGCGTCACGCTGCTC |
| Reverse Primer | GACGGCTCAGGACAACGGT | ||
| Probe | (e.g., HEX)-TGCCTGCGCTCGGCT-(MGBNFQ) | ||
| Cryptosporidium parvum | 18S rRNA | Forward Primer | ACATGGATAACCGTGGTAATTCT |
| Reverse Primer | CAA TACCCTACCGTC TAAAGCTG | ||
| Probe | (e.g., Cy5)-ACTCGACTTTATGGAA GGGTTGTAT-(MGBNFQ) |
2. Reaction Setup:
- Master Mix: Use a hot-start TaqMan master mix suitable for multiplexing.
- Reaction Volume: 25 µL total volume.
- Reagent Concentrations: Optimize primer and probe concentrations (typical final concentration range: 0.1–0.5 µM for primers, 0.1–0.3 µM for probes).
- Template DNA: Add 2–5 µL of extracted DNA.
- qPCR Cycling Conditions:
- Initial Denaturation: 95°C for 5 min
- 45 Cycles of:
- Denaturation: 95°C for 15 sec
- Annealing/Extension: 60°C for 1 min
3. Validation and Analysis:
- Standard Curve: Generate using serial dilutions of quantified plasmids containing the target insert. The assay should demonstrate a linear dynamic range from at least 5 × 10² to 5 × 10⸠copies/µL with PCR efficiency >90% and R² > 0.99 [7].
- Limit of Detection (LOD): Determine the lowest copy number detectable in 95% of replicates.
- Specificity: Test against a panel of related non-target parasites (e.g., Entamoeba coli, C. baileyi, Plasmodium spp.) to ensure no cross-reactivity.
- Reproducibility: Assess intra- and inter-assay coefficients of variation (CV), which should be less than 2% [7].
Implementing a Duplex qPCR Assay
Duplex assays are highly effective for distinguishing pathogenic from non-pathogenic species or including an internal control.
Example: Duplex for E. histolytica and E. dispar [5]
- Principle: These species are morphologically identical but differ clinically. A duplex qPCR allows for their precise differentiation.
- Design: Use species-specific primers and probes labeled with different dyes (e.g., FAM for E. histolytica, HEX for E. dispar) targeting the 18S rRNA gene.
- Protocol:
- Reaction Volume: Can be scaled down to 10 µL to reduce costs [5].
- Components: Similar to the triplex protocol, but with two targets.
- Critical Step: Validate that the amplification efficiencies of both targets are similar and that there is no inhibition between reactions.
Optimization Strategy for Multiplex Assays
A key challenge in multiplexing is competition for reagents, which can cause one target to amplify preferentially and starve another [20].
- Primer Limiting: If one target (e.g., a highly abundant endogenous control) amplifies earlier and exhausts reagents, significantly reduce its primer concentration. This forces it to plateau earlier, preserving reagents for the other target(s) [20].
- Experimental Validation: Before full-scale use, test 5–6 samples from both experimental and control groups in both multiplex and singleplex configurations. The results (Cq values) should be comparable between the two formats. If they disagree, further optimization is required [20].
Diagram 1: Multiplex qPCR development workflow.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of qPCR assays relies on a suite of reliable reagents and tools.
Table 3: Essential Reagents and Materials for Protozoan qPCR
| Item | Function/Description | Example Products/Protocols |
|---|---|---|
| Specific Probes | Essential for multiplexing; bind specifically to target DNA and emit a unique fluorescent signal, allowing discrimination of multiple targets in one well [20]. | TaqMan Probes (FAM, VIC, HEX, Cy5 labels) [20] [7] |
| Commercial Multiplex Kits | Integrated solutions containing pre-optimized master mixes and reagents for detecting common protozoan panels. | AllPlex GI-Parasite Assay (Seegene) [11] [22], Other marketed panels [7] |
| DNA Extraction Kits | Critical for obtaining inhibitor-free, high-quality DNA from complex stool samples. Automated systems enhance throughput and reproducibility [11] [22]. | QIAamp DNA Stool Mini Kit (Qiagen) [7], STARMag Universal Cartridge (Seegene) on Hamilton STARlet [22] |
| Automated Liquid Handlers | Robots that perform nucleic acid extraction and PCR setup, reducing human error, cross-contamination, and hands-on time, especially for high-throughput labs [11] [22]. | Hamilton STARlet [11] [22] |
| Standard Plasmids | Quantified plasmids containing the target sequence; used to generate standard curves for absolute quantification and determine assay efficiency, LOD, and linear dynamic range [7]. | Cloned PUC19 vectors with target inserts [7] |
| In Silico Design Tools | Software for designing specific primers and probes and checking for off-target binding. | Primer Express (Applied Biosystems) [7], BLAST, Oligo 7 [23] |
| 1-Decanol, 2-octyl- | 1-Decanol, 2-octyl-, CAS:45235-48-1, MF:C18H38O, MW:270.5 g/mol | Chemical Reagent |
| FRG8701 | FRG8701, CAS:108498-50-6, MF:C22H30N2O4S, MW:418.6 g/mol | Chemical Reagent |
The strategic selection of singleplex, duplex, or triplex qPCR configurations directly impacts the efficiency, cost, and reliability of intestinal protozoa research. Singleplex assays remain the gold standard for simplicity and absolute quantification, while duplex and triplex configurations offer powerful solutions for high-throughput screening and complex diagnostic panels. The successful implementation of multiplex assays hinges on careful experimental design, thorough validation against singleplex methods, and the use of optimized protocols and reagents. By adhering to the detailed methodologies outlined in this document, researchers can confidently advance the detection and study of intestinal protozoa.
Within the framework of developing robust real-time PCR (qPCR) protocols for intestinal protozoa research, the selection of appropriate genetic targets is a foundational step that critically influences the sensitivity, specificity, and overall diagnostic utility of the assay. While microscopic examination remains a common diagnostic tool, its limitations in sensitivity and inability to differentiate between morphologically identical species or genotypes have driven the adoption of molecular methods [24] [3]. This document provides a detailed application note for researchers, scientists, and drug development professionals, focusing on the comparative performance of key genetic markers—including rRNA, gdh, and tpi—for the detection and genotyping of intestinal protozoa, with a primary emphasis on Giardia duodenalis. The protocols and data summarized herein are designed to inform assay development for both clinical diagnostics and epidemiological studies.
Comparative Performance of Genetic Targets
The choice of genetic target significantly impacts qPCR assay performance. Comparative studies have evaluated various genes for their efficacy in detection and genotyping. The table below summarizes the diagnostic accuracy of different qPCR assays for Giardia duodenalis as reported by a head-to-head comparative study [25].
Table 1: Diagnostic accuracy of qPCR screening assays for Giardia duodenalis using Latent Class Analysis (LCA)
| Target Gene | Estimated Sensitivity (%) | Estimated Specificity (%) | Key Findings and Application Notes |
|---|---|---|---|
| 18S rRNA | 100.0 | 100.0 | Highest diagnostic accuracy; well-suited for sensitive screening purposes. |
| bg (beta-giardin) | 31.7 | 100.0 | High specificity but lower sensitivity; may require confirmation with another target. |
| gdh (glutamate dehydrogenase) | 17.5 | 92.3 | Lowest sensitivity and specificity among compared targets; not recommended as a primary screening target. |
For genotyping G. duodenalis into its major assemblages (A and B), assays targeting different genes also show variable performance [25]:
Table 2: Performance of duplex qPCR assays for discriminating Giardia duodenalis Assemblages A and B
| Target Gene | Probe Type | Sensitivity (%) | Specificity (%) | Agreement Kappa |
|---|---|---|---|---|
| bg | Standard Probe | 100.0 | 100.0 | 90.1% (near-perfect) |
| bg | LNA Probe | 96.4 | 84.0 | 74.8% (substantial) |
| tpi | Standard Probe | 82.1 | 100.0 | 74.8% (substantial) |
The high prevalence of mixed assemblage infections, as high as 46% in some patient cohorts, further underscores the need for robust, assemblage-discriminating assays [26]. Beyond Giardia, multi-parallel qPCR systems have been successfully implemented for detecting a range of intestinal protozoa, including Entamoeba histolytica, Cryptosporidium spp., Blastocystis spp., and Dientamoeba fragilis [6] [27].
Detailed Experimental Protocols
DNA Extraction from Stool Samples
Principle: Efficient mechanical and chemical lysis of resilient cyst/oocyst walls is critical for high-quality DNA yield [24].
Protocol:
- Sample Preparation: Suspend approximately 200 mg of stool specimen in sterile transport buffer (e.g., S.T.A.R. Buffer) or phosphate-buffered saline (PBS). For formalin-fixed or potassium dichromate-preserved samples, wash three times with distilled water or TE buffer (10 mM Tris/HCl, 1 mM EDTA, pH 8) to remove preservatives [28].
- Mechanical Lysis: Resuspend the pellet in 250 µL TE buffer with ~200 mg of sterile glass powder (cover glass #1). Perform three lysis cycles, each consisting of:
- 3-minute incubation at 4°C.
- 3-minute vigorous vortexing.
- Centrifugation at 21,380 x g for 2 minutes [24].
- Nucleic Acid Extraction: Transfer the supernatant to a new tube and proceed with a commercial silica-membrane-based DNA extraction kit (e.g., QIAamp DNA Stool Mini Kit, Machery-Nagel NucleoSpin Tissue Kit), following the manufacturer's instructions with an extended inhibitor removal incubation step (3 minutes) [29] [24] [3].
- DNA Quantification and Storage: Quantify DNA using a fluorometer (e.g., Qubit). Assess purity and integrity via spectrophotometry (A260/280 ratio ~1.8) and agarose gel electrophoresis. Store eluted DNA at -20°C or -80°C [26] [24].
Real-Time PCR for Detection and Genotyping ofGiardia duodenalis
Principle: This protocol describes a SYBR Green-based real-time PCR for the simultaneous detection and genotyping of G. duodenalis using assemblage-specific primers for the tpi and gdh genes [26].
Reaction Setup:
- Total Reaction Volume: 20 µL
- Reaction Mix:
- 10 µL of 2x Maxima SYBR Green qPCR Master Mix
- 2 µL of primer mix (containing forward and reverse primers at working concentration)
- 2-5 µL of template DNA (containing ~500 ng of DNA)
- Nuclease-free water to 20 µL
Table 3: Primer sequences for Giardia duodenalis genotyping
| Gene | Assemblage | Primer Sequence (5' → 3') | Amplicon Size (bp) |
|---|---|---|---|
| tpi A | A | Forward: TCGTCATTGCCCCTTCCGCCReverse: CAGTTGAGGATAGCAGCG | 77 |
| tpi B | B | Forward: GATGAACGCAAGGCCAATAAReverse: AAGAAGGAGATTGGAGAATC | 77 |
| gdh A | A | Forward: CCGGCAACGTTGCCCAGTTTReverse: TCCGAGTTCAAGGACAAGT | 180 |
| gdh B | B | Forward: CGTATTGGCGTCGGCGGTReverse: CTATCAGACCAGAGGCCACA | 133 |
Thermal Cycling Conditions (Rotor-Gene PCR System):
- Initial Denaturation: 95°C for 10 minutes (1 cycle)
- Amplification: 40-45 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing: 59°C for 30 seconds
- Extension: 72°C for 30 seconds
- Melt Curve Analysis: Perform after amplification to verify PCR specificity.
Analysis: Include positive controls (known G. duodenalis assemblage A and B DNA) and negative controls (nuclease-free water) in each run. A sample is considered positive for a specific assemblage if its amplification curve crosses the threshold within the cycle limit and shows the correct melt curve peak [26].
Workflow and Decision Pathway
The following diagram illustrates the logical workflow for the molecular detection and genetic characterization of intestinal protozoa, from sample collection to final interpretation.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and their functions for establishing the described molecular protocols.
Table 4: Essential research reagents and materials for molecular detection of intestinal protozoa
| Item | Function/Application | Example Product/Note |
|---|---|---|
| DNA Extraction Kit | Nucleic acid purification from complex stool matrices; critical for removing PCR inhibitors. | QIAamp DNA Stool Mini Kit (QIAGEN), NucleoSpin Tissue Kit (Machery-Nagel) [29] [26] [24] |
| qPCR Master Mix | Provides enzymes, dNTPs, and buffer for efficient, specific amplification in real-time PCR. | Maxima SYBR Green qPCR Master Mix (Thermo Scientific) [26] |
| Assemblage-Specific Primers | For specific detection and differentiation of Giardia assemblages (e.g., A, B) or other protozoan genotypes. | Custom oligonucleotides targeting tpi, gdh, or bg genes [26] [25] |
| Positive Control DNA | Essential for validating assay performance and ruling out PCR failure. | Genomic DNA from known Giardia assemblages A and B [26] |
| Automated Nucleic Acid Extractor | Standardizes and improves throughput of the DNA extraction process. | MagNA Pure 96 System (Roche) [3] |
| Real-Time PCR System | Platform for running qPCR assays and analyzing amplification data. | Rotor-Gene Q (QIAGEN), ABI 7900HT (Applied Biosystems) [26] [3] |
| Asoprisnil ecamate | Asoprisnil ecamate, CAS:222732-94-7, MF:C31H40N2O5, MW:520.7 g/mol | Chemical Reagent |
| Mollugogenol A | Mollugogenol A, CAS:22550-76-1, MF:C30H52O4, MW:476.7 g/mol | Chemical Reagent |
Within the framework of thesis research focused on develoing real-time PCR (qPCR) protocols for the detection of intestinal protozoa, the extraction of high-quality DNA from stool samples is a critical first step. The presence of PCR inhibitors and the robust structural nature of parasite cysts and oocysts present significant technical challenges that can lead to false-negative results if not properly addressed [30]. This application note provides a detailed, optimized protocol for nucleic acid extraction and subsequent qPCR setup, incorporating recent comparative data to guide method selection for superior sensitivity in parasite detection.
DNA Extraction from Stool Samples
Principle
The goal of this protocol is to achieve comprehensive mechanical and chemical lysis of a wide range of intestinal parasites—from fragile protozoa like Blastocystis sp. to helminths with tough eggshells like Ascaris lumbricoides—while simultaneously removing co-purified PCR inhibitors present in the fecal matrix [30]. The protocol below is adapted from the CDC-approved procedure and incorporates a bead-beating step, which has been demonstrated to significantly enhance DNA yield and detection rates [31] [30].
Materials and Equipment
- Sample: Fecal specimen, divided into aliquots and stored at -80°C without preservative, or preserved in 70% ethanol or potassium dichromate [31].
- Primary Kit: QIAamp PowerFecal Pro DNA Kit (Qiagen) or FastDNA Kit (MP Biomedicals) [31] [30].
- Mechanical Lysis Equipment: Tissue homogenizer (e.g., FastPrep-24 or similar) and lysing matrix tubes containing silica beads [31].
- Reagents:
- Phosphate Buffered Saline (PBS), pH 7.2
- EDTA solution, 0.5 M, pH 8.0
- Polyvinylpyrrolidone (PVP) [31]
- Lab Consumables: Microcentrifuge tubes, pipette tips, and a microcentrifuge.
Step-by-Step Procedure
Step 1: Sample Preparation and Washing
- Label a 1.5 mL microcentrifuge tube.
- Centrifuge a 300-500 µL aliquot of stool specimen at 14,000 × g at 4°C for 5 minutes. Carefully discard the supernatant.
- Resuspend the pellet in 1 mL of PBS-EDTA. Centrifuge again at 14,000 × g at 4°C for 5 minutes and discard the supernatant.
- Repeat the wash step two more times for a total of three washes [31].
- After the final wash, resuspend the pellet in PBS-EDTA to a final volume of approximately 300 µL.
Step 2: Bead-Beating and Lysis
- Transfer the 300 µL of washed sample into a lysing matrix tube containing silica beads.
- Add the following reagents to the tube:
- 400 µL of CLS-VF (Cell Lysis Solution)
- 200 µL of PPS (Protein Precipitation Solution)
- PVP to a final concentration of 0.1% to 1% (to bind polyphenolic inhibitors) [31].
- Tightly close the tube and secure it in the tissue homogenizer.
- Process the sample at a speed of 5.0-5.5 for 10-30 seconds to ensure complete disruption of tough parasite walls [31] [30].
Step 3: DNA Binding and Purification
- Centrifuge the lysed sample at 14,000 × g for 5 minutes at room temperature.
- Transfer 600 µL of the supernatant to a new, clean 1.5 mL tube, avoiding the pellet and debris.
- Add 600 µL of Binding Matrix to the supernatant and mix gently by inverting the tube for 1 minute.
- Incubate the mixture at room temperature for 5 minutes to allow DNA to bind to the matrix.
- Centrifuge at 14,000 × g for 1 minute. Pour off the supernatant.
- Resuspend the pellet (binding matrix with DNA) in 500 µL of SEWS-M (Salt/Ethanol Wash Solution) by pipetting up and down.
- Centrifuge at 14,000 × g for 1 minute and discard the supernatant.
- Perform a quick spin (10 seconds) and remove any residual wash solution with a fine tip.
Step 4: DNA Elution
- Add 50-100 µL of DES (DNA Elution Solution) or TE buffer to the pellet. Resuspend thoroughly by pipetting.
- Incubate at room temperature for 2-5 minutes.
- Centrifuge at 14,000 × g for 2 minutes.
- Carefully transfer the supernatant, which contains the purified DNA, to a clean, labeled tube.
- Store the extracted DNA at 4°C for immediate use or -20°C for long-term storage.
Troubleshooting and Quality Control
- Inhibitor Removal: If PCR inhibition is suspected, further purify the eluted DNA using an inhibitor removal column, such as the OneStep PCR Inhibitor Removal Kit [32].
- Sample Consistency: For watery stools, use tips with cut ends to pipet both liquid and particulate matter. For viscous samples, use less starting material to avoid overloading the purification column [32].
- DNA Quality Assessment: Evaluate DNA concentration and purity using a spectrophotometer. Optimal 260/280 absorbance ratios are close to 1.8 [33].
Reaction Setup for Real-Time PCR
Primer and Probe Design
For the detection of intestinal protozoa, primers and probes should target conserved, multi-copy genes. The small subunit ribosomal RNA (18S rRNA) gene is a common and reliable target [5]. The table below provides examples of tested primer and probe sequences for key protozoan parasites.
Table 1: Example qPCR Primers and Probes for Intestinal Protozoa
| Organism | Target Gene | Forward Primer (5'->3') | Reverse Primer (5'->3') | Probe Sequence (5'->3') | Reaction Volume |
|---|---|---|---|---|---|
| Giardia duodenalis | Small subunit rRNA | GCT GCG TCA CGC TGC TC | GAC GGC TCA GGA CAA CGG T | (FAM)-TGC CGC CGG CGC (BHQ1) | 10 µL [5] |
| Entamoeba histolytica | 18S ribosomal RNA | AGG ATT GGA TGA AAT TCA GAT GTA CA | TAA GTT TCA GCC TTG TGA CCA TAC | (CY5)-TGA CGG ATA CAG ACT GCA TTG GAA TC-(BHQ2) | 10 µL [5] |
| Cryptosporidium spp. | Small subunit rRNA | ACA TGG ATA ACC GTG GTA ATT CT | CAA TAC CCT ACC GTC TAA AGC TG | (HEX)-ACT CGA CTT TAT GGA AGG GTT GTA T-(BHQ1) | 10 µL [5] |
| Blastocystis spp. | Small subunit rRNA | GGT CCG GTG AAC ACT TTG GAT TT | CCT ACG GAA ACC TTG TTA CGA CTT CA | (FAM)-TCG TGT AAA TCT TAC CAT TTA GAG GA-(BHQ1) | 10 µL [5] |
qPCR Master Mix Setup
A typical 10 µL reaction volume can be used to reduce costs while maintaining sensitivity [5]. The reaction components are listed below.
- Table 2: qPCR Reaction Components
| Component | Final Concentration/Amount | Positive Control | No-Template Control (NTC) |
|---|---|---|---|
| 2x qPCR Master Mix | 5.0 µL | 5.0 µL | 5.0 µL |
| Forward Primer | 0.15 - 0.5 µM | 0.15 - 0.5 µM | 0.15 - 0.5 µM |
| Reverse Primer | 0.15 - 0.5 µM | 0.15 - 0.5 µM | 0.15 - 0.5 µM |
| Probe | 0.1 - 0.3 µM | 0.1 - 0.3 µM | 0.1 - 0.3 µM |
| Nuclease-Free Water | To 10 µL | To 10 µL | To 10 µL |
| Template DNA | 2.0 µL | 2.0 µL (known positive) | - |
qPCR Cycling Conditions
The following cycling conditions are recommended. Parameters may require optimization for different thermocyclers.
- Table 3: Standard qPCR Cycling Protocol
| Step | Cycles | Temperature | Time | Purpose |
|---|---|---|---|---|
| Initial Denaturation | 1 | 95°C | 3-5 minutes | Polymerase activation and initial denaturation |
| Amplification | 40-45 | 95°C | 10-15 seconds | Denaturation |
| 60°C | 30-60 seconds | Primer annealing and extension (acquire fluorescence) |
Comparative Data and Method Selection
A 2022 comparative study evaluated four DNA extraction methods for the detection of diverse intestinal parasites via PCR. The results strongly support the use of kits incorporating bead-beating.
Table 4: Comparison of DNA Extraction Method Efficiencies [30]
| DNA Extraction Method | Description | PCR Detection Rate | Relative Performance Notes |
|---|---|---|---|
| Phenol-Chloroform (P) | Conventional chemical lysis | 8.2% | Lowest detection rate; failed to detect most parasites. |
| Phenol-Chloroform + Beads (PB) | Chemical lysis with mechanical bead-beating | 24.7% | Improved yield but high inhibitor carryover. |
| QIAamp Fast DNA Stool Mini Kit (Q) | Silica column-based | 47.1% | Good performance for some parasites. |
| QIAamp PowerFecal Pro DNA Kit (QB) | Silica column with bead-beating | 61.2% | Highest detection rate; effective for all parasites tested. |
The data conclusively shows that the QIAamp PowerFecal Pro DNA Kit (QB), which integrates a bead-beating step, is the most effective method for the molecular diagnosis of intestinal parasites, yielding the highest PCR detection rate [30]. Another study confirmed that the QIAamp PowerFecal Pro DNA Kit produces microbiome profiles comparable to the previously widely-used QIAamp DNA Stool Mini Kit with a bead-beating step, while also providing more consistent DNA quality [33].
The Scientist's Toolkit
Table 5: Essential Research Reagent Solutions
| Item | Function/Application |
|---|---|
| Lysing Matrix Tubes (Silica Beads) | Provides mechanical disruption (bead-beating) for breaking tough parasite cell walls, cysts, and oocysts [31] [30]. |
| Inhibitor Removal Technology (e.g., PVP, proprietary buffers) | Binds to and removes PCR inhibitors commonly found in stool, such as bile salts, complex polysaccharides, and polyphenolic compounds [31] [32]. |
| Silica-Based Binding Matrix | Selectively binds nucleic acids in the presence of chaotropic salts, allowing for purification and removal of contaminants [31] [34]. |
| Multiplex qPCR Assay Master Mix | Enables simultaneous detection of multiple parasite targets in a single reaction, improving speed and cost-effectiveness [5] [21]. |
| DNA/RNA Shield | A sample preservation reagent that stabilizes microbial community composition at the time of collection and prevents degradation [32]. |
| Non-8-ene-1-thiol | Non-8-ene-1-thiol|95%|For Research Use |
| 7-Bromohept-1-yne | 7-Bromohept-1-yne, CAS:81216-14-0, MF:C7H11Br, MW:175.069 |
Workflow Diagrams
Within the field of intestinal protozoa research, accurate and efficient pathogen detection is fundamental to understanding infection dynamics, disease burden, and treatment efficacy. Traditional diagnostic methods, particularly microscopy, are hampered by challenges in distinguishing morphologically identical species and often lack the sensitivity required for robust surveillance [5]. The adoption of multiplex real-time PCR (qPCR) represents a significant advancement, allowing for the simultaneous detection of multiple pathogens in a single reaction. This application note details the validation and implementation of high-throughput, automated solutions for multiplex panels, providing a structured framework for researchers and drug development professionals to ensure diagnostic accuracy and reliability in their studies on intestinal protozoa.
Performance Data of Validated Multiplex Assays
The transition to molecular methods is driven by the need for higher specificity and sensitivity, especially for distinguishing between pathogenic and non-pathogenic protozoa such as Entamoeba histolytica and Entamoeba dispar [5]. The following tables summarize key performance metrics from validation studies relevant to the field.
Table 1: Analytical Sensitivity and Specificity of Representative Multiplex Assays
| Pathogen/Target | Assay Type | Limit of Detection (LOD) | Specificity | Clinical Sensitivity | Reference |
|---|---|---|---|---|---|
| Entamoeba histolytica/dispar | Duplex qPCR | Not Specified | 100% (Species-level differentiation) | 31.4% Prevalence in cohort | [5] |
| Cryptosporidium spp. + C. mesnili | Duplex qPCR | Not Specified | 100% (Species-level differentiation) | Reliable detection in 74.4% of samples | [5] |
| Giardia duodenalis | Singleplex qPCR | Not Specified | 100% | High prevalence in region | [5] |
| 15 HPV Genotypes | Multiplex qPCR | Varies by genotype | 100% | 98% | [35] |
| SARS-CoV-2, IAV, IBV, RSV, hADV, MP | Multiplex FMCA-PCR | 4.94 - 14.03 copies/µL | 100% (No cross-reactivity) | 98.81% agreement with RT-qPCR | [36] |
Table 2: Throughput and Economic Comparison of PCR Platforms
| Platform / Assay Characteristic | High-Throughput System (e.g., SmartChip) | Standard Tube-Based Multiplex qPCR | Commercial Multiplex Panel (BioFire FilmArray) |
|---|---|---|---|
| Reaction Volume | 100-200 nL | 10-25 µL | Not Specified |
| Samples per Run (Max) | 768 | 96 - 384 | 1 per module |
| Total Assays per Day | >10,000 | Hundreds to low thousands | Multiple with multiple modules |
| Hands-on Time | ~30 minutes | Varies | Minimal per sample |
| Cost per Sample | Significantly reduced | Moderate | Higher |
| Key Advantage | Extreme throughput & reagent savings | Flexibility in panel design | All-in-one, simple workflow |
Experimental Protocol: Validation of a Duplex qPCR for Intestinal Protozoa
This protocol is adapted from a study that implemented duplex qPCR assays for detecting Entamoeba histolytica/dispar and Cryptosporidium spp./Chilomastix mesnili, providing a template for validating multiplex panels in intestinal protozoa research [5].
Sample Preparation and Nucleic Acid Extraction
- Sample Collection: Collect fresh stool samples from patients or animal models. Preserve samples appropriately if immediate processing is not feasible.
- Nucleic Acid Extraction: Use commercially available automated (e.g., QIAcube, [37]) or manual nucleic acid extraction kits. The protocol in [5] utilized a 10 µL reaction volume, indicating small-scale extraction elution volumes (e.g., 50-100 µL) are suitable to maintain template concentration.
- Quality Control: Include an internal control, such as the human beta-globin gene [35] or a sample process control, during extraction to monitor for inhibition and confirm successful nucleic acid isolation.
Primer and Probe Design
- Target Selection: Identify highly conserved genomic regions. For protozoa, small subunit ribosomal RNA genes are common targets [5].
- Specificity Check: Use tools like NCBI BLAST to ensure primer/probe sequences are unique to the target pathogen and do not cross-react with related species or host DNA.
- Multiplexing Configuration: Label probes with distinct fluorophores (e.g., FAM, HEX, ROX) that are compatible with your real-time PCR instrument's detection channels. For the duplex assay targeting E. histolytica/dispar, species-level differentiation was achieved with specific probes [5].
qPCR Reaction Setup and Thermal Cycling
- Reaction Master Mix: Prepare a master mix containing the appropriate buffer, dNTPs, polymerase, and primers/probes. The referenced study used a 10 µL reaction volume [5].
- Thermal Cycling Conditions: A typical two-step cycling protocol is effective:
- Reverse Transcription: 50°C for 5-15 minutes (if detecting RNA).
- Initial Denaturation: 95°C for 30 seconds to 2 minutes.
- Amplification (40-45 cycles):
- Denaturation: 95°C for 5-15 seconds.
- Annealing/Extension: 60°C for 30-60 seconds (acquire fluorescence at this step).
- Platform: This protocol can be performed on standard real-time PCR systems (e.g., Bio-Rad CFX96) or scaled for high-throughput on systems like the SmartChip, which uses 100-200 nL reactions and can complete a run in under four hours [38].
Data Analysis and Interpretation
- Threshold and Baseline: Set the fluorescence threshold in the exponential phase of amplification across all replicates and adjust the baseline according to the instrument's software recommendations.
- Cycle Threshold (Ct): Determine the Ct value for each reaction. A sample is considered positive if the Ct value is below a pre-defined cut-off (e.g., Ct < 40).
- Melting Curve Analysis (if using SYBR Green): If a dye-based assay is used, perform melting curve analysis post-amplification to verify amplicon specificity by its unique melting temperature (Tm).
Workflow Diagram: High-Throughput Multiplex PCR Validation
The following diagram illustrates the logical workflow for validating and running a high-throughput multiplex PCR assay, from initial design to final data analysis.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of high-throughput multiplex PCR relies on a suite of specialized reagents and tools. The table below details essential components for developing and running these assays.
Table 3: Essential Reagents and Materials for Multiplex PCR Assays
| Item | Function/Description | Example from Literature |
|---|---|---|
| Primers & Probes | Specifically designed to target conserved genomic regions of pathogens; probes are labeled with fluorophores (e.g., FAM, HEX) for multiplex detection. | Designed for E6/E7 region of HPV [35]; for small subunit ribosomal RNA of protozoa [5]. |
| Multiplex PCR Master Mix | Optimized buffer containing DNA polymerase, dNTPs, and MgClâ‚‚ designed to support simultaneous amplification of multiple targets without competition or inhibition. | 4X CAPITAL qPCR Probe Master Mix [35]; TB Green Premix Ex Taq II [39]. |
| Automated Nucleic Acid Extraction Kit | Reagents for purifying high-quality DNA/RNA from complex samples like stool, crucial for sensitivity and reproducibility. | QIAamp Viral RNA Kit on QIAcube [37]; MPN-16C RNA/DNA extraction kit [36]. |
| Internal Control Template | Non-target nucleic acid (e.g., phage RNA, human beta-globin) spiked into the reaction to monitor for PCR inhibition and extraction efficiency. | Human beta-globin gene used in HPV assay [35]; Phocine distemper virus (PDV) used in arbovirus assay [40]. |
| Positive Control Plasmids | Plasmid DNA containing the target sequence for each pathogen in the panel, used for standard curve generation and LOD determination. | Mixed plasmids with viral target fragments for precision testing [36]. |
| High-Throughput Platform | Automated system for nanoliter-scale dispensing and cycling, enabling massive parallelization (e.g., SmartChip System). | SmartChip Real-Time PCR System for >10,000 assays/day [38]. |
| 2-Chloropentan-1-ol | 2-Chloropentan-1-ol | 139364-99-1 | C5H11ClO Building Block | Get high-purity 2-Chloropentan-1-ol (CAS 139364-99-1), a versatile C5H11ClO scaffold for organic synthesis. For Research Use Only. Not for human or veterinary use. |
| Acetoxime benzoate | Acetoxime benzoate, CAS:942-89-2, MF:C9H9NO2, MW:163.176 | Chemical Reagent |
Intestinal protozoa infections represent a significant global public health challenge, contributing substantially to gastrointestinal morbidity and malnutrition, particularly in regions with poor sanitation and limited access to clean water [5]. Traditional bright-field microscopy, while cost-effective and widely used, faces considerable limitations in sensitivity and specificity, along with an inherent inability to distinguish between morphologically identical species, such as the pathogenic Entamoeba histolytica and non-pathogenic Entamoeba dispar [5]. The development of real-time PCR (qPCR) assays has revolutionized parasitology diagnostics by providing a tool for specific, sensitive, and quantitative detection of parasitic DNA [41] [42]. This case study details the implementation of novel qPCR assays, including the first molecular detection of Chilomastix mesnili by qPCR, and their application in a clinical study on Pemba Island, Tanzania, framed within a broader thesis on advanced molecular protocols for intestinal protozoa research [5] [43].
Chilomastix mesnili, while generally considered a non-pathogenic commensal, serves as an important indicator of fecal contamination of food or water sources, with a prevalence of approximately 13% in developing countries [5]. Recent genetic studies have revealed significant diversity within the genus Chilomastix, with distinct molecular classifications and subtypes identified in humans and animals [44]. The implementation of precise molecular diagnostics for such neglected protozoa is crucial for understanding their epidemiology and genetic diversity, while also monitoring and controlling the burden of intestinal protozoal diseases more effectively [5] [44].
Literature Review and Scientific Rationale
The Diagnostic Shift from Microscopy to Molecular Methods
For decades, microscopic examination of stool specimens has been the reference method for diagnosing intestinal protozoan infections [3]. Although cost-effective, this technique is labor-intensive, requires highly trained personnel, and suffers from subjective interpretation and poor sensitivity, especially in cases of low parasite burden [5] [45] [3]. Crucially, microscopy cannot differentiate between morphologically identical species with varying clinical significance, such as E. histolytica and E. dispar [5] [3]. This distinction is vital as E. histolytica causes amoebiasis, responsible for 40,000–100,000 deaths annually, while E. dispar is considered non-pathogenic [5].
Molecular methods, particularly qPCR, have emerged as powerful alternatives, offering superior sensitivity, specificity, and the ability to provide quantitative data [41] [45] [42]. qPCR operates on the principle of fluorescently monitoring DNA amplification in real-time, with the quantification cycle (Cq) value providing a reliable metric for determining the initial quantity of target DNA [41] [42]. The advantages of qPCR include a wide dynamic range (7–8 Log10), reduced risk of contamination compared to conventional PCR, and the potential for multiplexing several targets in a single reaction [41] [42]. Studies have consistently demonstrated the superior performance of qPCR; for instance, one evaluation found qPCR positive in 73.5% of samples compared to only 37.7% by microscopy [45]. This enhanced detection capability is particularly valuable for identifying coinfections and asymptomatic cases, which are frequently missed by traditional methods [45].
Chilomastix mesnili: A Neglected Protozoan
Chilomastix mesnili is a flagellated protozoan commonly found in the human cecum and colon [46]. Despite its widespread presence, it has been largely neglected in molecular epidemiological studies due to its classification as a non-pathogen [44]. While generally considered a commensal, there have been rare clinical case reports associating it with symptoms in immunocompromised individuals or travelers [44] [46]. A recent genetic diversity study revealed that what is formally named C. mesnili actually comprises multiple monophyletic clusters or subtypes, including a human–non-human primate genotype (ST1) and a human genotype (ST2-1) [44]. This finding underscores the need for precise molecular tools to elucidate the complex ecology and potential pathogenicity of different genetic variants. The development of a specific qPCR for C. mesnili, as described in this case study, marks a significant step forward in the capacity to study this overlooked parasite [5].
Materials and Methods
Research Reagent Solutions
The successful implementation of molecular diagnostics relies on a suite of specific reagents and tools. The table below details the key research reagents and their functions as employed in this study.
Table 1: Essential Research Reagents for Protozoan qPCR
| Reagent/Material | Function/Application | Specification/Example |
|---|---|---|
| Primers & Probes | Specifically bind to and detect target DNA sequences of protozoa. | Designed for 18S rRNA or SSU rRNA genes [5] [44]. |
| DNA Polymerase | Enzyme that synthesizes new DNA strands during PCR amplification. | Hot-start Taq polymerase recommended to prevent non-specific amplification [47]. |
| Master Mix | Pre-mixed solution containing buffers, nucleotides, and MgCl₂. | 2× TaqMan Fast Universal PCR Master Mix [3]. |
| DNA Extraction Kit | Isolates high-quality DNA from complex stool matrices. | QIAamp DNA Stool Mini Kit [45] [48]; MagNA Pure 96 System [3]. |
| Internal Control | Monitors for PCR inhibition and validates extraction efficiency. | Synthetic oligonucleotide or control sequence spiked into the sample [45]. |
| Stool Transport Buffer | Preserves nucleic acids prior to DNA extraction. | S.T.A.R. Buffer [3]; DNAzol reagent [44]. |
Primer and Probe Design and Validation
The core of a specific qPCR assay lies in the careful design of primers and probes. In this study, primers and probes for Blastocystis spp., Cryptosporidium spp., E. histolytica, E. dispar, and Giardia duodenalis were obtained from established sources [5]. For the novel detection of C. mesnili, a bioinformatics approach was employed:
- Sequence Retrieval and Alignment: Eight partial sequences of the small ribosomal subunit (18S rRNA) gene for C. mesnili were retrieved from the NCBI database using BLASTN [5].
- Conserved Region Identification: Highly conserved regions unique to C. mesnili were identified by multiple sequence alignment and checked for specificity against the NCBI database to avoid cross-reactivity with closely related organisms [5] [44].
- Oligonucleotide Design: Primers and probes were designed to meet optimal qPCR criteria: a GC content of ~50%, a length of 20–24 bases, and an estimated melting temperature (Tm) of ~58°C [5]. The specificity of the final sequences was confirmed via individual BLASTN searches [5].
All oligonucleotides were synthesized commercially, and dyes/quenchers were selected based on the detection capabilities of the qPCR instrument (e.g., CFX Maestro) [5]. This rigorous design process ensures high specificity and sensitivity for the target protozoa.
Sample Collection and DNA Extraction
Stool samples were collected from 70 patients on Pemba Island, Tanzania, as part of a clinical trial evaluating the anthelmintic drug emodepside [5] [43]. For optimal DNA recovery, a robust extraction protocol is critical to overcome inhibitors commonly found in stool (e.g., bile salts, complex carbohydrates) [47] [3].
The recommended workflow involves:
- Preservation: Stool samples should be preserved immediately after collection in appropriate buffers like DNAzol or S.T.A.R. Buffer to prevent nucleic acid degradation [44] [3].
- Lysis and Purification: Using a commercial kit (e.g., QIAamp DNA Stool Mini Kit), samples are subjected to mechanical and chemical lysis, followed by purification to remove inhibitors [45] [48]. Incorporating a step with glass beads and agitation in a homogenizer can improve lysis of robust protozoal cysts [45].
- Inhibition Testing: Each extracted sample should be spiked with an internal control to check for PCR inhibitors, which can cause false-negative results [45] [48].
qPCR Reaction Setup and Thermal Cycling
This study implemented a volume-optimized qPCR protocol using a 10 µL reaction volume, enhancing cost-effectiveness without compromising performance [5]. The assays were configured as two duplex reactions (Entamoeba dispar + Entamoeba histolytica and Cryptosporidium spp. + Chilomastix mesnili) and two singleplex reactions (Giardia duodenalis and Blastocystis spp.) [5] [43].
A standard probe-based qPCR reaction mixture includes:
- Template DNA: 2-5 µL of extracted DNA.
- Master Mix: Contains DNA polymerase, dNTPs, and MgClâ‚‚ in an optimized buffer.
- Primers and Probes: At optimized concentrations (e.g., 0.3-0.5 µM for primers) [5].
- Nuclease-free Water: To the final volume.
Thermal cycling conditions typically involve: an initial activation step at 95°C for 10 minutes, followed by 35-45 cycles of denaturation (95°C for 15 seconds), and a combined annealing/extension step (60°C for 1 minute) with fluorescence acquisition [48] [3]. Including positive controls (plasmid DNA or known positive sample) and negative controls (no-template control) in every run is essential for validating the results [47].
Diagram 1: Experimental workflow for qPCR detection of intestinal protozoa, from sample collection to data analysis.
Results and Data Analysis
Diagnostic Performance and Prevalence Data
The implemented qPCR assays demonstrated high reliability, detecting protozoal DNA in 74.4% of the stool samples analyzed from Pemba Island [5]. This detection rate far exceeds what is typically achievable with traditional microscopy. The table below summarizes the prevalence data for the key protozoa targeted in the study.
Table 2: Protozoa Prevalence Detected by qPCR in a Tanzanian Cohort (n=70)
| Protozoan Species | Prevalence (%) | Clinical/Diagnostic Notes |
|---|---|---|
| Any Protozoa | 74.4% | Overall detection rate [5]. |
| Entamoeba histolytica / dispar complex | 31.4% | Combined detection [5]. |
| â–¸ Entamoeba histolytica (Pathogenic) | ~10.5% | One-third of E. histolytica/ dispar complex [5]. |
| Chilomastix mesnili | Not specified | First molecular detection by qPCR; indicator of fecal contamination [5]. |
| Giardia duodenalis | Not specified | High global prevalence; cause of diarrhea [5] [3]. |
| Blastocystis spp. | Not specified | Often asymptomatic; associated with healthy gut microbiome [5]. |
| Cryptosporidium spp. | Not specified | Causes severe diarrhea in immunocompromised individuals [5]. |
The ability of qPCR to differentiate E. histolytica from E. dispar is a key finding. The data revealed that approximately one-third of the infections within the E. histolytica/ dispar complex were attributable to the pathogenic E. histolytica [5]. This level of diagnostic precision is impossible with microscopy and has direct implications for patient management and public health interventions.
Assessment of Therapeutic Efficacy
The qPCR assays were further applied to evaluate the potential antiprotozoal effect of emodepside, a veterinary anthelmintic drug. Analysis of 54 samples collected after treatment with 20, 25, or 30 mg of emodepside or a placebo showed no significant reduction in protozoal load compared to the placebo group [5] [43]. This result highlights the utility of quantitative molecular methods not only for diagnosis and prevalence studies but also for accurately assessing the efficacy of therapeutic interventions in clinical trials.
Discussion
Technical Challenges and Troubleshooting
Despite its advantages, implementing qPCR for intestinal protozoa presents specific challenges that require careful troubleshooting. Common pitfalls and their solutions are summarized below.
Table 3: Common qPCR Pitfalls and Troubleshooting Strategies in Parasitology
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| No Amplification (No Cq) | PCR inhibitors, failed reagent preparation, low DNA concentration. | Check DNA quality/purity; include an internal control; repeat extraction with an inhibitor removal kit; verify master mix preparation [47]. |
| High Cq Values (Late Amplification) | Low parasitic load, degraded DNA, suboptimal reaction conditions. | Increase template volume (within limits); optimize annealing temperature; run a dilution series to check for inhibition [47]. |
| Non-Specific Amplification | Primer-dimer formation, poorly designed primers, contaminated reagents. | Redesign primers using software (e.g., Primer-BLAST); use a hot-start Taq polymerase; include melt curve analysis for SYBR Green assays [47]. |
| Low or High PCR Efficiency | Pipetting errors, inaccurate standard curve, poor primer/probe design. | Re-prepare standard curve with careful serial dilutions; calibrate pipettes; optimize primer/probe concentrations and MgClâ‚‚ levels [41] [47]. |
| False Positives | Contamination (cross-contamination between samples, aerosol). | Use separate pre- and post-PCR areas; include no-template controls (NTCs); use UV decontamination [47] [48]. |
A critical consideration in parasitology is the sample matrix. Stool samples contain a variety of PCR inhibitors, such as heme, bile salts, and complex polysaccharides [47] [45]. Furthermore, the robust cyst walls of protozoa like Giardia and Cryptosporidium can make DNA extraction difficult, potentially leading to false negatives [3]. Therefore, validating and optimizing the DNA extraction protocol for the specific sample type is not just recommended, but essential for obtaining reliable results [45] [3].
Application in Research and Drug Development
The transition to molecular diagnostics like qPCR provides researchers and drug development professionals with a powerful, quantitative tool. The high throughput and objectivity of qPCR make it ideal for large-scale epidemiological studies, enabling a more accurate assessment of the true burden and transmission dynamics of intestinal protozoa [5] [45]. Furthermore, the ability to multiplex—detecting several pathogens in a single reaction—improves efficiency and reduces costs, which is particularly beneficial in resource-limited settings [5] [42].
In drug development, the quantitative nature of qPCR (Cq values correlating to parasite load) is invaluable for monitoring treatment efficacy in clinical trials [5] [41]. As demonstrated in the emodepside study, qPCR can objectively determine whether a compound has a significant effect on pathogen load, a critical endpoint for evaluating potential new therapies, especially in the face of rising resistance to current treatments like nitroimidazoles [5].
This case study successfully demonstrates the implementation of novel qPCR assays for the detection of intestinal protozoa, with the groundbreaking development of a qPCR for Chilomastix mesnili. The applied methodology highlights the substantial advantages of qPCR over traditional microscopy, including superior sensitivity, the capacity for species-level differentiation, and the ability to provide quantitative data essential for both epidemiological research and therapeutic assessment.
The findings from Pemba Island confirm a high prevalence of intestinal protozoa in the region and underscore the necessity for continued monitoring and control efforts. The failed efficacy of emodepside against protozoa, clearly identified by qPCR, points to the need for continued research into new therapeutic agents. The protocols and troubleshooting guides provided herein offer a robust framework for researchers and clinicians aiming to implement these advanced molecular diagnostics in their own work, thereby contributing to more effective control and understanding of neglected intestinal protozoal infections.
Maximizing Assay Performance: Overcoming Technical Hurdles in Protozoan qPCR
Optimizing DNA Extraction from Robust Protozoan Cysts and Oocysts
Within the context of developing robust real-time PCR protocols for intestinal protozoa research, the efficacy of the entire molecular diagnostic pipeline is fundamentally dependent on the initial DNA extraction quality. Protozoan parasites such as Cryptosporidium spp., Giardia duodenalis, and Entamoeba histolytica present a unique challenge for nucleic acid isolation due to their resilient oocyst and cyst walls, which are engineered by nature to protect against environmental degradation [49] [50]. Furthermore, clinical and environmental samples like stool and wastewater contain substances that can inhibit downstream polymerase activity [49] [51]. This application note synthesizes recent research to provide optimized, detailed protocols for maximizing DNA recovery from these robust structures, thereby enhancing the sensitivity and reliability of subsequent real-time PCR assays for drug development and clinical research.
Key Challenges in Protozoan DNA Extraction
The journey to an efficient DNA extraction protocol is fraught with obstacles specific to protozoa. The primary barriers include the structural robustness of the (oo)cyst wall, which is difficult to disrupt by standard lysis methods [50] [52]. This wall must be compromised without degrading the genetic material within. Secondly, the complex matrices from which these parasites are often isolated—such as stool, wastewater, and fresh produce—contain a plethora of PCR inhibitors, including heme, bilirubins, bile salts, and complex carbohydrates [49] [50] [51]. If co-purified with the DNA, these substances can severely impair PCR efficiency. Finally, protozoa often exist in low numbers in samples, necessitating protocols with high recovery rates and low limits of detection to avoid false-negative results in diagnostic and research settings [53] [50].
Comparative Analysis of DNA Extraction Methods
Performance of Commercial Kits and Manual Methods
Researchers have systematically evaluated various DNA extraction methods for their efficiency in recovering protozoan DNA from complex samples. The table below summarizes key findings from comparative studies.
Table 1: Comparison of DNA Extraction Methods for Protozoan Parasites
| Extraction Method | Target Protozoa | Key Findings | Reference |
|---|---|---|---|
| QIAamp DNA Stool Mini Kit (Amended Protocol) | Cryptosporidium, Giardia, E. histolytica | Increased sensitivity for Cryptosporidium from 60% to 100%; theoretical detection limit of ≈2 oocysts/cysts. | [49] |
| QIAamp PowerFecal Pro DNA Kit (QB) | Various intestinal parasites | Highest PCR detection rate (61.2%); effective for parasites with robust structures like Ascaris and Strongyloides. | [51] |
| Phenol-Chloroform (P) | Various intestinal parasites | Provided high DNA yields but lowest PCR detection rate (8.2%), indicating potential for inhibitor co-purification. | [51] |
| ZR Fecal DNA MiniPrep (Z) | Tritrichomonas foetus | Combined with LAMP/PCR, showed highest accuracy (AUC: 0.917); detected a single parasite cell. | [54] |
| Phenol-Chloroform (Custom Protocol) | Cryptosporidium parvum | Determined to be the best method for extracting protozoan DNA from wastewater for ddPCR. | [50] |
Impact of Mechanical Pretreatment
Mechanical disruption is a critical step for breaking down the resilient walls of cysts and oocysts. A 2024 multicenter study focusing on Enterocytozoon bieneusi spores provided granular detail on optimizing the bead-beating step [55].
Table 2: Optimization of Bead-Beating Parameters for E. bieneusi Spores
| Parameter | Options Evaluated | Optimal Condition(s) |
|---|---|---|
| Bead Type | Glass beads; MP Lysing Matrix E; ZR BashingBeads | Mixed small-sized beads (e.g., ZR BashingBeads, MP Lysing Matrix E) showed superior performance over glass beads alone. |
| Grinding Speed | 20 Hz, 25 Hz, 30 Hz | 30 Hz |
| Grinding Duration | 60 s, 180 s | 60 s |
| Key Outcome | A short (60s), high-speed (30 Hz) bead-beating step with commercial mixed beads yielded the lowest Cq values and highest detection rates. |
The study concluded that a strong but short bead-beating using small-sized beads from various materials constituted the optimal mechanical pretreatment for robust microsporidian spores [55].
Detailed Optimized Protocols
Amended Protocol for QIAamp DNA Stool Mini Kit
This protocol, optimized for Cryptosporidium, Giardia, and Entamoeba histolytica from fecal samples, highlights critical amendments to the manufacturer's instructions that significantly improve sensitivity [49].
Workflow Overview:
Materials:
- Sample: 180-220 mg of human stool specimen.
- Kit: QIAamp DNA Stool Mini Kit (Qiagen).
- Equipment: Microcentrifuge, heating block, vortex mixer.
Step-wise Procedure:
- Enhanced Lysis: Add 200 mg of stool to ASL buffer and vortex until homogenous. Critical Amendment: Perform the lysis incubation step at boiling temperature (100°C) for 10 minutes to effectively disrupt the tough oocyst/cyst walls [49].
- Improved Inhibitor Removal: Centrifuge the sample and transfer the supernatant to a new tube containing an InhibitEX tablet. Critical Amendment: Vortex and incubate for 5 minutes (instead of the standard 1 minute) to ensure sufficient time for the tablet matrix to adsorb PCR inhibitors [49].
- Precision Precipitation: After proteinase K treatment and AL buffer addition, add ethanol. Critical Amendment: Use pre-cooled (4°C) absolute ethanol for enhanced and more consistent nucleic acid precipitation [49].
- Binding and Washing: Load the mixture onto the QIAamp spin column, centrifuge, and wash twice with AW1 and AW2 buffers as per the standard kit protocol.
- Concentrated Elution: Critical Amendment: Elute the DNA in a small volume of 50-100 µl of AE buffer or nuclease-free water. This increases the final DNA concentration, improving the likelihood of detection in downstream real-time PCR [49].
Optimized Workflow for Produce and Environmental Samples
Detecting protozoa on leafy greens or in water requires a concentration and purification step prior to DNA extraction. The following protocol is adapted from methods validated for lettuce and wastewater [53] [50] [52].
Workflow Overview:
Materials:
- Sample: 25 g of leafy greens (e.g., lettuce, basil) or 1 L of wastewater.
- Buffers: Glycine buffer (for berries/soft herbs) or Elution Buffer (for lettuce/onions) [53].
- Equipment: Stomacher or orbital shaker, high-speed centrifuge, vacuum manifold, TissueLyser II or similar bead-beater.
Step-wise Procedure:
- Oocyst Elution: Place the produce sample in a stomacher bag with 40-50 ml of an appropriate buffer (e.g., glycine buffer for blueberries, elution solution for strawberries and lettuce). Process using a stomacher (for soft herbs) or orbital shaker (for woody herbs and berries) at high speed for 1-5 minutes to dislodge oocysts [53].
- Concentration: Filter the wash fluid through a 35 μm mesh to remove large debris. The filtrate is then concentrated by centrifugation at 15,000 x g for 60 minutes at 4°C. For wastewater, a combination of centrifugation and filtration can increase recovery by approximately 10% [50] [52].
- Mechanical Lysis: Resuspend the pellet in a lysis buffer. Transfer to a tube containing a mixture of small, dense beads (e.g., ZR BashingBeads). Critical Step: Perform mechanical disruption using a homogenizer like the TissueLyser II at 30 Hz for 60 seconds [55].
- DNA Purification: Following lysis, purify the DNA using a method suited to the sample type. For wastewater, the phenol-chloroform method has been shown to be effective [50]. For food samples, kits like the Quick DNA Fecal/Soil Microbe Microprep kit (ZymoResearch) perform well [55].
- Detection: Use the extracted DNA in a sensitive downstream application like droplet digital PCR (ddPCR) or quantitative PCR (qPCR). The optimized extraction protocol enables the detection of as few as 3-5 oocysts per gram of food sample [53].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Kits for Optimized DNA Extraction
| Reagent / Kit Name | Function / Application | Key Feature |
|---|---|---|
| QIAamp DNA Stool Mini Kit (Qiagen) | DNA extraction from stool samples. | Integrated InhibitEX technology for removal of PCR inhibitors. |
| QIAamp PowerFecal Pro DNA Kit (Qiagen) | DNA extraction from stool and environmental samples. | Includes powerful bead-beating step for disruption of tough cells. |
| ZR Fecal DNA MiniPrep (Zymo Research) | DNA extraction from fecal samples. | High efficiency for samples with low parasite loads; good for Tritrichomonas. |
| Quick DNA Fecal/Soil Microbe Microprep (ZymoResearch) | DNA extraction from soil and feces. | Effective for microsporidian spores; includes bead-beating step. |
| MP Lysing Matrix E / ZR BashingBeads | Mechanical disruption of oocysts/cysts. | Mixed-size beads for efficient cell wall breakage. |
| InhibitEX Tablets (Qiagen) | Adsorption of PCR inhibitors in stool samples. | Critical for reducing false-negative PCR results. |
| Toddacoumaquinone | Toddacoumaquinone, CAS:142878-03-3, MF:C23H18O7, MW:406.4 g/mol | Chemical Reagent |
Optimizing DNA extraction is a non-negotiable prerequisite for successful real-time PCR-based research on intestinal protozoa. The data and protocols detailed herein demonstrate that strategic amendments to commercial kits—specifically, enhanced thermal and mechanical lysis, extended inhibitor removal, and concentrated elution—dramatically improve DNA yield and purity. For researchers developing molecular diagnostics or screening compounds in drug development, adopting these optimized protocols ensures that the analytical sensitivity of their real-time PCR assays is not compromised at the initial, and most critical, sample preparation stage. The consistent application of these refined methods will contribute to more reliable detection, genotyping, and quantification of protozoan parasites in clinical and environmental matrices.
Managing PCR Inhibitors in Stool Samples and Complex Matrices
The application of real-time PCR (qPCR) has revolutionized the detection and differentiation of intestinal protozoa, offering significant advantages in sensitivity and specificity over traditional microscopic examination [5] [3]. However, the complex composition of stool samples presents a formidable challenge to molecular diagnostics, primarily due to the presence of substances that inhibit enzymatic reactions critical to PCR amplification [56] [57]. These inhibitors can lead to false-negative results, reduced sensitivity, and inaccurate quantification, ultimately compromising the reliability of diagnostic and research outcomes for intestinal protozoa such as Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica [3] [11].
The inherent complexity of fecal material contributes to this challenge. Stool is a heterogeneous mixture comprising undigested food residues, bilirubin, bile salts, complex carbohydrates, lipids, and various metabolic byproducts [57]. Additionally, the high microbial biomass introduces bacterial polysaccharides and proteins that can interfere with DNA polymerases. Research indicates that PCR inhibitors accumulate with age, found in approximately 17% of stool samples from children aged 6 to 24 months, with this proportion increasing in adult samples [57]. The situation is often exacerbated in diarrheal samples, which may contain higher concentrations of inflammatory cells and blood-derived inhibitors such as heme and immunoglobulin G [57].
Understanding the nature of these inhibitors and implementing robust protocols to overcome their effects is therefore essential for researchers and clinicians working with intestinal protozoa. This application note provides comprehensive strategies for managing PCR inhibitors in stool-based molecular analyses, with specific consideration for protozoan detection in both research and drug development contexts.
Understanding PCR Inhibitors in Stool Matrices
PCR inhibitors in stool samples originate from diverse sources and exhibit varying mechanisms of interference with the amplification process. The primary categories of inhibitors include:
- Polyphenolic Compounds: Humic and fulvic acids resemble DNA in structure and can bind co-valently to nucleic acids or polymerase enzymes, effectively inhibiting enzymatic activity [58] [56]. These compounds are particularly problematic in stool samples due to their persistence through DNA extraction procedures.
- Bile Salts and Bilirubin: These digestive components can disrupt the activity of DNA polymerase by interfering with the enzyme's active site or by destabilizing the primer-template complex [57].
- Complex Carbohydrates: Polysaccharides from dietary fiber or bacterial cell walls co-precipitate with DNA during extraction and can physically block polymerase activity or increase sample viscosity [57].
- Calcium Ions: Present in variable concentrations, calcium can alter the optimal magnesium concentration required for Taq polymerase activity, thereby reducing amplification efficiency [57].
- Bacterial Degradation Products: Endonucleases and other enzymes from bacterial lysis can degrade DNA templates or reagents, while bacterial metabolites may directly inhibit polymerase function [57].
Mechanisms of Inhibition
The mechanisms by which these substances interfere with PCR amplification vary considerably:
- Enzyme Inactivation: Many inhibitors, including polyphenolics and bile salts, directly bind to DNA polymerase, altering its conformation and reducing catalytic efficiency [58].
- Nucleic Acid Binding: Humic substances can coat DNA templates, preventing primer annealing or polymerase binding, while also absorbing UV light and interfering with spectrophotometric DNA quantification [56].
- Chelation of Cofactors: Some inhibitors chelate magnesium ions, which are essential cofactors for DNA polymerase activity, thereby crippling the amplification process [57].
- Degradation of Nucleic Acids: Nucleases present in stool samples can degrade DNA templates before or during the amplification process, leading to complete amplification failure [57].
Table 1: Common PCR Inhibitors in Stool Samples and Their Effects
| Inhibitor Category | Specific Examples | Primary Mechanism of Action | Impact on PCR |
|---|---|---|---|
| Polyphenolic compounds | Humic acids, fulvic acids, tannins | Polymerase binding, template coating | Reduced sensitivity, false negatives |
| Digestive components | Bile salts, bilirubin, cholesterol | Enzyme active site disruption | Delayed Cq values, amplification failure |
| Complex carbohydrates | Polysaccharides, glycogen | Increased viscosity, polymerase blocking | Inconsistent amplification between replicates |
| Metal ions | Calcium | Magnesium chelation | Reduced polymerase efficiency |
| Cellular components | Heme, hemoglobin, immunoglobulins | Polymerase inhibition | Complete or partial inhibition |
Strategies for Inhibitor Management
Sample Collection and Preservation
Proper sample collection and preservation represent the first critical defense against PCR inhibition. Several studies have demonstrated that the choice of preservative significantly impacts downstream DNA quality and amplifiability:
- RNAlater Preservation: This preservative has been shown to yield high DNA quantities while maintaining integrity for amplification, effectively stabilizing samples at ambient temperatures for at least five days [56]. This is particularly valuable for field studies and multi-center trials where immediate freezing is impractical.
- FTA Cards: These chemically-impregnated cards lyse cells on contact and sequester nucleic acids while retaining PCR inhibitors in the matrix, which can be washed away prior to amplification [59]. This method is especially effective for stabilizing samples during transportation and storage.
- Para-Pak Media: Studies on intestinal protozoa detection have demonstrated that stool samples preserved in Para-Pak media yielded better PCR results compared to fresh samples, likely due to better DNA preservation and partial inhibitor neutralization [3].
The selection of an appropriate preservation system should consider the specific protozoan targets, intended storage conditions, and downstream extraction methodologies.
Nucleic Acid Extraction and Purification
The extraction methodology plays a pivotal role in determining both the yield and purity of nucleic acids recovered from stool samples. Comparative studies have identified several effective approaches:
- Silica Membrane-Based Technology: Multiple studies have confirmed the effectiveness of silica membranes in removing PCR inhibitors. One investigation demonstrated that silica membrane purification reduced inhibition rates from 12.5% to 1.1% when applied to clinical samples [60]. These membranes work by selectively binding nucleic acids while allowing inhibitors to pass through during washing steps.
- Magnetic Separation Systems: Automated systems like the MagNA Pure 96 System (Roche) utilize magnetic bead technology for nucleic acid purification and have been successfully implemented in multiplex PCR protocols for intestinal protozoa [3] [11]. These systems offer standardized, high-throughput processing with minimal cross-contamination risk.
- Commercial Stool Kits: Specialized kits such as the Stool total RNA purification kit (Norgen) and QIAamp Stool Mini Kit (Qiagen) have demonstrated superior performance in recovering inhibitor-free DNA, with the Norgen kit providing high RNA purity suitable for sensitive mRNA detection in stool [61] [57].
Table 2: Comparison of Nucleic Acid Extraction Methods for Stool Samples
| Extraction Method | Principle | Inhibitor Removal Efficiency | Suitable Downstream Applications | Considerations |
|---|---|---|---|---|
| Silica membrane columns (QIAamp) | Selective DNA binding to silica gel membrane | High (∼91.5% success rate) [60] | Singleplex and multiplex qPCR, sequencing | Manual processing, scalable |
| Magnetic bead systems (MagNA Pure) | Magnetic separation with silica coating | High | High-throughput multiplex PCR, automation | Higher initial equipment cost |
| FTA filter-based protocol | Cell lysis and DNA entrapment in matrix | High (washes remove inhibitors) [59] | Field collection, transport, PCR | Small sample volume, not for all sample types |
| Phenol-chloroform extraction | Liquid-phase separation | Moderate | Historical data comparison, challenging samples | Labor-intensive, hazardous chemicals |
Specialized Inhibitor Removal Technologies
For samples with persistent inhibition issues despite optimized extraction, dedicated inhibitor removal technologies offer an additional purification layer:
- OneStep PCR Inhibitor Removal Kit: This system utilizes a column slurry specifically optimized to bind and remove polyphenolic compounds, including humic acids, tannins, and melanin. The simple filtration-based workflow can process sample volumes of 50-200μL and achieves 80-90% recovery of PCR-ready DNA [58].
- FTA Filter-Based Purification: This extraction-free approach involves applying samples directly to FTA filters, which lyse cells and capture DNA while allowing inhibitors to be removed through a series of brief washes with specialized buffers. This method has demonstrated sensitivity for detecting as few as 3-10 parasites in seeded samples [59].
- Glass Wool Filtration: For particularly challenging samples, pre-extraction filtration through glass wool columns can remove particulate matter and some hydrophobic inhibitors, improving downstream extraction efficiency, especially for protozoan oocysts [59].
Experimental Protocols for Inhibitor Management
Comprehensive Workflow for Stool Sample Processing
Diagram 1: Complete workflow for managing PCR inhibitors in stool samples
Detailed Protocol: Inhibitor-Resistant DNA Extraction from Stool
Principle: This protocol combines mechanical disruption, chemical lysis, and silica-based purification to maximize DNA yield while minimizing co-purification of PCR inhibitors. The method is adapted from procedures successfully used in intestinal protozoa research [5] [61] [11].
Materials:
- Stool sample (preserved in RNAlater or similar)
- Lysis buffer (commercial or in-house)
- Proteinase K
- Silica membrane columns (QIAamp Stool Mini Kit or equivalent)
- Microcentrifuge
- Water bath or heating block
- Ethanol (96-100%)
- Elution buffer (10 mM Tris-HCl, pH 8.5)
Procedure:
- Sample Homogenization:
- Transfer 180-220 mg of stool to a microcentrifuge tube
- Add 1.4 mL of lysis buffer and vortex thoroughly for 1 minute
- For protozoan cysts/oocysts, include a bead-beating step with 0.1 mm glass beads for 3 minutes
Chemical and Enzymatic Lysis:
- Add 40 μL of Proteinase K (20 mg/mL) and mix by pulse-vortexing
- Incubate at 56°C for 1 hour with occasional mixing
- For resistant protozoa, extend incubation to 2 hours or include a freeze-thaw cycle
Inhibitor Removal and DNA Binding:
- Centrifuge at 17,000 × g for 3 minutes to pellet insoluble debris
- Transfer supernatant to a new tube, avoiding the pellet
- Add 1 volume of ethanol (96-100%) and mix by vortexing
- Apply the mixture to a silica membrane column and centrifuge at 6,000 × g for 1 minute
Washing and Elution:
- Wash with 500 μL of inhibitor removal wash buffer (kit-specific)
- Centrifuge at 6,000 × g for 1 minute and discard flow-through
- Repeat with 500 μL of standard wash buffer
- Perform an additional centrifugation at full speed for 3 minutes to dry the membrane
- Elute DNA with 50-100 μL of elution buffer preheated to 70°C
Quality Control:
- Assess DNA concentration using fluorometry (preferred over spectrophotometry)
- Evaluate inhibitor presence using a spiked internal control or dilution test
- For intestinal protozoa applications, include a positive extraction control with known parasite DNA
Protocol: Post-Extraction Inhibitor Removal
Principle: For samples with residual inhibition after extraction, this secondary purification step specifically targets polyphenolic compounds using specialized resin columns [58].
Materials:
- Extracted DNA in aqueous solution
- OneStep PCR Inhibitor Removal Kit or equivalent
- Microcentrifuge
- Collection tubes
Procedure:
- Sample Preparation:
- Adjust DNA sample volume to 50-100 μL with elution buffer
- For heavily inhibited samples, do not exceed 100 μL input volume
Filtration and Inhibitor Binding:
- Apply sample to the prepared inhibitor removal column
- Centrifuge at 12,000 × g for 1 minute
- Collect flow-through containing purified DNA
Quality Assessment:
- Measure DNA recovery (typically 80-90%)
- Test amplifiability with internal control or reference gene
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagent Solutions for Managing PCR Inhibitors in Stool Samples
| Reagent/Category | Specific Product Examples | Primary Function | Application Notes |
|---|---|---|---|
| Sample Preservation | RNAlater, Paxgene, FTA Cards | Stabilizes nucleic acids, inhibits nucleases | FTA cards ideal for field studies; RNAlater preserves RNA and DNA [56] |
| DNA Extraction Kits | QIAamp Stool Mini Kit (Qiagen), Stool total RNA purification kit (Norgen) | Comprehensive nucleic acid purification | Norgen kit provides high RNA purity; Qiagen offers automation compatibility [61] [57] |
| Inhibitor Removal Resins | OneStep PCR Inhibitor Removal Kit (Zymo Research) | Binds polyphenolic inhibitors | Effective against humic/fulvic acids, tannins; >80% DNA recovery [58] |
| PCR Additives | BSA, Betaine, T4 Gene 32 Protein | Neutralizes residual inhibitors | Enhances amplification efficiency in problematic samples |
| Internal Controls | Commercial ICs, artificially spiked DNA | Detects inhibition in amplification | Essential for validating negative results in diagnostic applications |
Application to Intestinal Protozoa Research
The management of PCR inhibitors is particularly crucial in intestinal protozoa research and drug development, where accurate detection and quantification directly impact experimental outcomes and clinical assessments.
Impact on Protozoa Detection Sensitivity
Studies implementing qPCR for intestinal protozoa have demonstrated that effective inhibitor management significantly enhances detection sensitivity:
- In research on Pemba Island, Tanzania, optimized qPCR assays reliably detected protozoa in 74.4% of stool samples, identifying Entamoeba histolytica and Entamoeba dispar in 31.4% of cases, with one-third of these infections attributed to the pathogenic E. histolytica [5].
- A multicenter evaluation comparing commercial and in-house PCR tests for intestinal protozoa found that molecular methods provided crucial species-level differentiation for Entamoeba histolytica, which is impossible with microscopy alone [3].
- Recent implementation of multiplex PCR panels for routine diagnosis demonstrated superior detection rates for Giardia intestinalis (1.28%), Cryptosporidium spp. (0.85%), and Dientamoeba fragilis (8.86%) compared to microscopic examination [11].
Implications for Drug Development Studies
Effective inhibitor management is paramount in clinical trials assessing anti-protozoal therapeutics, where accurate pre- and post-treatment quantification is essential:
- In a study evaluating emodepside's potential anti-protozoal effects, qPCR implementation enabled precise assessment of parasite burden before and after treatment, ultimately determining that no significant reduction in protozoa occurred following emodepside administration compared to placebo [5].
- The ability to differentiate morphologically identical species, such as pathogenic E. histolytica and non-pathogenic E. dispar, allows for targeted assessment of drug efficacy against specific pathogens [5] [3].
Diagram 2: Impact of inhibitor management on protozoa detection accuracy
Troubleshooting and Quality Control
Detection and Quantification of Inhibition
Implementing robust quality control measures is essential for identifying inhibition and ensuring reliable results:
- Internal Controls: Include non-competitive internal controls in amplification reactions to detect inhibition. The AllPlex Gastrointestinal Panel assay incorporates an internal control that must amplify successfully before results are considered valid [11].
- Dilution Series: Test sample DNA at multiple dilutions (1:1, 1:5, 1:10). A decrease in Cq value with dilution suggests the presence of inhibitors.
- Spike-In Experiments: Add known quantities of control DNA to sample extracts and compare Cq values with buffer controls. Significant Cq shifts (typically >2 cycles) indicate inhibition.
Addressing Persistent Inhibition
For samples demonstrating persistent inhibition despite standard mitigation approaches:
- Increased Wash Steps: Additional wash steps with inhibitor-specific wash buffers can enhance removal of polyphenolic compounds [58].
- Alternative Polymerases: Some DNA polymerases demonstrate greater resistance to specific inhibitors present in stool samples.
- Sample Dilution: Strategic dilution of template DNA can reduce inhibitor concentration below the threshold of interference while maintaining target detectability.
- Magnetic Bead Cleanup: Secondary purification using size-selective magnetic beads can effectively separate inhibitors from nucleic acids based on differential binding properties.
Effective management of PCR inhibitors in stool samples is an essential prerequisite for reliable detection and quantification of intestinal protozoa using molecular methods. The strategies outlined in this application note—including appropriate sample preservation, optimized nucleic acid extraction, dedicated inhibitor removal technologies, and robust quality control measures—provide a comprehensive framework for overcoming the challenges posed by complex stool matrices.
Implementation of these protocols enables researchers and drug development professionals to leverage the full potential of real-time PCR for intestinal protozoa studies, ensuring accurate assessment of pathogen prevalence, species differentiation, and therapeutic efficacy. As molecular diagnostics continue to evolve toward multiplex panels and automated platforms [11], the principles of effective inhibitor management will remain fundamental to generating clinically and scientifically valid results in gastrointestinal pathogen research.
Within the framework of developing robust real-time PCR (qPCR) protocols for intestinal protozoa research, the pre-analytical phase of sample collection and preservation is critically important. Pathogenic intestinal protozoa, including Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, are significant global causes of diarrheal diseases, and their accurate detection via molecular methods is essential for both clinical diagnostics and drug development [3]. While qPCR offers enhanced sensitivity and specificity over traditional microscopy, its performance is fundamentally dependent on the quality and quantity of DNA recovered from stool specimens [5]. The choice between using fresh or fixed stool represents a major decision point, impacting DNA integrity, PCR amplification efficiency, and ultimately, the reliability of experimental and diagnostic outcomes. This application note details the comparative effects of fresh and fixed stool preservation on nucleic acid yield and downstream qPCR results, providing validated protocols to guide researchers and scientists in optimizing their workflows for intestinal protozoa detection.
Comparative Analysis: Fresh vs. Fixed Stool Samples
The decision to use fresh or preserved stool samples has a direct and measurable impact on the success of molecular detection. The table below summarizes the key characteristics of each approach.
Table 1: Comparison of Fresh and Fixed Stool Samples for Molecular Detection of Intestinal Protozoa
| Parameter | Fresh Stool | Fixed Stool (in appropriate preservatives) |
|---|---|---|
| DNA Preservation | Prone to degradation by endogenous nucleases if not processed immediately [3] | Superior DNA preservation; protects from degradation during storage and transport [3] |
| qPCR Performance | Variable; can show lower detection rates for some protozoa [3] | Can yield better PCR results; demonstrated higher overall detection rates in a comparative study [3] |
| Handling & Logistics | Requires immediate processing or freezing; complex logistics [62] [63] | Stable at room temperature; ideal for multi-center studies and storage [62] [63] |
| Inhibitor Removal | May contain PCR inhibitors that are not efficiently removed [64] | Fixation can help prevent PCR inhibition present in fresh specimens [64] |
| Recommended Use | Suitable for immediate processing in a single laboratory. | Essential for studies involving transport, long-term storage, or multi-site collaborations. |
Key Evidence from Comparative Studies
A 2025 multicentre study involving 18 Italian laboratories provided direct, quantitative evidence on this topic. The study compared the performance of commercial and in-house RT-PCR tests on 355 stool samples, of which 230 were freshly collected and 125 were stored in preservation media. The analysis concluded that PCR results from preserved stool samples were better than those from fresh samples, attributing this advantage to better DNA preservation in the former [3]. This finding is crucial for researchers designing experiments, as it demonstrates that fixation can enhance, rather than hinder, molecular detection.
Essential Protocols for Sample Handling and DNA Extraction
The following protocols are synthesized from current literature and guidelines to ensure optimal DNA recovery for intestinal protozoa research.
Specimen Collection and Preservation Protocol
- Collection: Collect stool in a clean, dry, leak-proof container. Take care to avoid contamination with urine, water, or soil [63].
- Preservation: For molecular detection, preserve the specimen as soon as possible after collection.
- Add one volume of stool to three volumes of a molecular-compatible preservative [63].
- Recommended Preservatives: TotalFix, Unifix, modified Zn- or Cu-based PVA, Ecofix, Sodium Acetate-Acetic Acid-Formalin (SAF), absolute ethanol (1:1 dilution), or 2.5% potassium dichromate (1:1 dilution) [62] [63].
- Mix Thoroughly: Ensure the specimen is mixed well with the preservative, especially for formed stools [63].
- Storage and Shipping: Preserved samples can be stored and shipped at room temperature [62]. Unpreserved specimens must be stored frozen and shipped on dry ice [62].
DNA Extraction Protocol
The DNA extraction method is a critical determinant of success, influencing both the yield of target protozoan DNA and the removal of PCR inhibitors present in stool [51].
Table 2: Comparison of DNA Extraction Methods from Stool Samples
| Method | Procedure Summary | Key Findings |
|---|---|---|
| Phenol-Chloroform (P) | Lysis with proteinase K and detergent, incubation, phenol-chloroform extraction, ethanol precipitation [51]. | Provided high DNA yields but the lowest PCR detection rate (8.2%); only detected Strongyloides stercoralis [51]. |
| Phenol-Chloroform with Bead-Beating (PB) | Adds a mechanical lysis step using glass beads to the standard P method [51]. | Higher DNA yield than commercial kits; PCR detection rate superior to P but lower than kit-based methods [51]. |
| QIAamp Fast DNA Stool Mini Kit (Q) | Silica-membrane column-based purification optimized for stool [51]. | Reliable performance; however, a more advanced kit (QB) demonstrated superior results in a comparative study [51]. |
| QIAamp PowerFecal Pro DNA Kit (QB) | Combines mechanical lysis (bead beating) with the power of a silica-membrane technology [51]. | Highest PCR detection rate (61.2%); effective for a wide range of parasites (protozoa and helminths); most effective at removing PCR inhibitors [51]. |
Recommended Protocol: QIAamp PowerFecal Pro DNA Kit (QB) Workflow This protocol is recommended based on its demonstrated superior detection rates [51].
- Pretreatment: Transfer 180-220 mg of stool (preserved or fresh) to a PowerBead Pro tube.
- Lysis and Homogenization:
- Add appropriate lysis buffers to the tube.
- Securely cap the tube and vortex thoroughly to homogenize. Mechanical bead-beating in a vortex adapter is integral to this step for breaking down hardy parasite cysts and oocysts.
- Incubation and Centrifugation: Incubate the lysate at 70°C for 5-10 minutes to further facilitate lysis. Centrifuge to pellet stool debris and the silica beads.
- DNA Binding and Washing:
- Transfer the supernatant to a MB Spin Column.
- Centrifuge to bind DNA to the silica membrane.
- Wash the membrane multiple times with provided wash buffers to remove salts, inhibitors, and other impurities.
- DNA Elution: Elute the purified genomic DNA in a low-salt elution buffer or nuclease-free water. The eluate is now ready for downstream qPCR applications.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Stool DNA Extraction and Protozoan Detection
| Item | Function | Example Products & Notes |
|---|---|---|
| Molecular-Compatible Preservative | Preserves nucleic acids and parasite morphology at room temperature. | TotalFix, Unifix, Ecofix, SAF, modified Zn-PVA [62] [63]. |
| Inhibition-Removing DNA Extraction Kit | Isolates high-quality, PCR-ready DNA while removing co-purified inhibitors. | QIAamp PowerFecal Pro DNA Kit (highly recommended) [51]. QIAamp Fast DNA Stool Mini Kit is an alternative [51]. |
| Automated Nucleic Acid Extractor | Standardizes and streamlines the extraction process, improving reproducibility. | Platforms like the MagNA Pure 96 System (Roche) can be used with appropriate kits [3]. |
| qPCR Master Mix | Provides enzymes, dNTPs, and optimized buffers for sensitive real-time PCR. | TaqMan Fast Universal PCR Master Mix (2X) is commonly used [3]. |
| Protozoa-Specific Primers & Probes | Enables specific detection and differentiation of target pathogens. | Assays for G. duodenalis, Cryptosporidium spp., E. histolytica, E. dispar, and C. mesnili have been implemented [3] [5]. |
Workflow Visualization
The following diagram synthesizes the experimental workflow for processing stool samples to highlight the critical decision points that influence DNA yield and qPCR results.
The evidence clearly demonstrates that sample preservation is not merely a logistical convenience but a critical factor that directly impacts DNA yield and the accuracy of qPCR results for intestinal protozoa. The use of molecular-compatible fixatives, combined with a DNA extraction method that incorporates robust mechanical lysis and inhibitor removal, forms the foundation of a reliable molecular detection pipeline. For researchers and drug development professionals, adhering to these optimized protocols for sample preservation and nucleic acid extraction is essential for generating high-quality, reproducible data that can effectively monitor disease burden and assess the efficacy of novel therapeutic agents.
In the field of intestinal protozoa research, robust and sensitive molecular diagnostics are paramount for accurate disease surveillance, understanding pathogen burden, and evaluating new therapeutic interventions. Real-time quantitative PCR (qPCR) has emerged as a superior alternative to traditional microscopy, offering enhanced sensitivity and the crucial ability to differentiate between morphologically identical species, such as the pathogenic Entamoeba histolytica and non-pathogenic Entamoeba dispar [6] [65]. The full potential of qPCR, however, is only realized through rigorous determination of assay limits of detection (LOD) and strict adherence to protocols that ensure reproducibility. This document outlines critical parameters and detailed protocols for establishing sensitive and reliable qPCR assays, framed within the context of intestinal protozoa research.
Determining the Limit of Detection (LOD)
The LOD is the lowest concentration of a target that can be reliably detected by an assay. Accurate LOD determination is non-negotiable for diagnosing low-level intestinal protozoa infections.
Experimental Protocol for LOD Determination
A. Plasmid DNA Standard Preparation
- Clone Target Sequence: Clone a 120–250 base pair fragment containing the primer and probe binding sites for the protozoan target (e.g., Giardia duodenalis, Cryptosporidium spp.) into a plasmid vector with an antibiotic resistance gene [65].
- Quantify and Purity: Precisely quantify the purified plasmid using a spectrophotometer and confirm its sequence.
- Prepare Dilution Series: Perform a ten-fold serial dilution series of the plasmid in a background of carrier DNA (e.g., yeast tRNA) or negative stool DNA to mimic the clinical sample matrix. A minimum of 5 logs of concentration is recommended for a robust standard curve [66].
B. qPCR Amplification and Data Analysis
- Run qPCR: Amplify each dilution in the series using the optimized qPCR assay. A minimum of three technical replicates per dilution is essential for statistical significance [67] [66].
- Generate Standard Curve: Plot the mean quantification cycle (Cq) value for each dilution against the logarithm of the known template concentration.
- Establish LOD: The LOD is defined as the lowest plasmid concentration where the amplification curve consistently reaches the threshold line, displaying a sigmoidal shape, and is detected in at least 95% of replicates [65]. The dynamic range of the assay is the concentration range over which the standard curve remains linear.
Critical Parameters for LOD
- PCR Efficiency: Calculated from the slope of the standard curve (Efficiency % = (10^(-1/slope) - 1) × 100). Optimal efficiency ranges from 90% to 110%, corresponding to a slope of -3.6 to -3.1 [67] [66]. Low efficiency inflates Cq values at low concentrations and compromises sensitivity.
- Linearity (R² Value): The coefficient of determination (R²) should be >0.99, indicating a strong linear relationship between Cq and template concentration, which is crucial for accurate quantification [66].
- Precision: The standard deviation of Cq values for replicates at the LOD should be minimal (ideally ≤0.25) to reliably distinguish a 2-fold change in concentration [66].
- Specificity: The assay must be tested against a panel of genomic DNA from other protozoa and human stool samples from non-infected individuals to ensure no cross-reactivity [65].
Table 1: Key Quantitative Parameters for a Validated qPCR Assay
| Parameter | Target Value | Interpretation |
|---|---|---|
| PCR Efficiency | 90% - 110% | Optimal amplification; slope of -3.6 to -3.1. |
| Standard Curve R² | >0.99 | High degree of linearity and reliable quantification. |
| Precision (Std Dev) | ≤0.25 | Capable of distinguishing 2-fold differences. |
| Dynamic Range | ≥5 logs | Broad range of accurate quantification. |
Ensuring Reproducibility
Reproducibility ensures that qPCR results are consistent within and between laboratories. This is governed by strict adherence to the Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines [68] [69].
Experimental Protocol for a Reproducible qPCR Workflow
The following diagram outlines the critical stages for ensuring a reproducible qPCR workflow in intestinal protozoa detection.
1. Sample Collection and Nucleic Acid Extraction
- Sample: Collect stool samples in appropriate preservatives. For the study on Pemba Island, samples were stored frozen prior to analysis [6] [65].
- Extraction: Use a validated nucleic acid extraction kit suitable for stool samples, which often contain PCR inhibitors. Incorporate an internal control (e.g., human 16S mitochondrial rRNA) to monitor extraction efficiency and the presence of inhibitors [65].
2. Assay Design and Validation
- Design: For protozoa like Chilomastix mesnili, identify highly conserved regions in genomic databases (e.g., NCBI) using BLASTN. Design primers and probes with ~50% GC content, a TM of ~58°C, and a length of 20-24 bases [65].
- Validation: Test primer/probe specificity in silico and wet-lab against a panel of related and non-related organisms. Optimize primer and probe concentrations to achieve the highest signal-to-noise ratio [65].
3. qPCR Setup and Run
- Master Mix: Use a high-quality master mix. Be aware that different master mixes can yield different baseline fluorescence and Cq values for the same sample, preventing direct comparison between mixes [66].
- Reaction Volume: The referenced intestinal protozoa study successfully used a 10 µL reaction volume, which reduces costs [65].
- Passive Reference Dye: Ensure the appropriate concentration of a passive reference dye (e.g., ROX) is used to normalize fluorescence. Low ROX can increase Cq standard deviation, reducing precision [66].
- Controls: Include no-template controls (NTC) to detect contamination, positive controls (plasmid or known positive sample), and inter-plate calibrators to normalize runs.
4. Data Analysis
- Threshold Setting: Set the threshold in the linear phase of the amplification plot, above the baseline but within the exponential phase of all samples [67] [66].
- Cq Determination: The Cq is the cycle at which the amplification curve intersects the threshold. Cq values are relative and can only be directly compared under identical reaction conditions [66].
- Quantification Method: For relative quantification (e.g., comparing gene expression before/after treatment), use the ∆∆Cq method with a stable reference gene. The Livak method assumes PCR efficiencies close to 100%, while the Pfaffl method accounts for efficiency variations [67]. Convert Cq values to efficiency-corrected target quantities for the most accurate reporting [69].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Intestinal Protozoa qPCR
| Item | Function / Rationale |
|---|---|
| Plasmid with Target Insert | Serves as a quantitative standard for generating the calibration curve and determining LOD and PCR efficiency [65]. |
| Validated Primer/Probe Sets | For specific detection of target protozoa (e.g., duplex assays for E. dispar/E. histolytica). Probes should be labeled with compatible fluorophores (e.g., FAM, Texas Red) [65]. |
| qPCR Master Mix | A chemical environment optimized for robust amplification. Choice of master mix directly impacts baseline fluorescence and Cq values [66]. |
| Passive Reference Dye (e.g., ROX) | Normalizes fluorescent signals to account for non-PCR-related fluctuations across the reaction plate, improving well-to-well comparability [66]. |
| Nucleic Acid Extraction Kit | For isolating inhibitor-free DNA/RNA from complex stool matrices. Must include a protocol for stool samples. |
| Internal Amplification Control | Co-extracted and co-amplified control to identify sample-specific inhibition, ensuring negative results are true negatives [65]. |
The accurate detection of intestinal protozoan parasites is fundamental to clinical diagnosis, epidemiological studies, and drug development. Traditional diagnostic methods, particularly microscopy, present significant limitations in sensitivity and specificity, especially for morphologically similar organisms. This application note details advanced molecular protocols for detecting Dientamoeba fragilis and Entamoeba histolytica, framing them within a broader thesis on optimizing real-time PCR for intestinal protozoa research. We provide consolidated performance data, detailed experimental methodologies, and key reagent solutions to aid researchers in implementing these highly sensitive and specific assays in their workflows.
Performance Comparison of Detection Methods
The following tables summarize the quantitative performance of various detection methods as reported in the literature, providing a clear comparison of their sensitivities and specificities.
Table 1: Performance Comparison of Dientamoeba fragilis Detection Methods
| Method Type | Specific Method | Sensitivity | Specificity | Detection Limit | Reference |
|---|---|---|---|---|---|
| Real-time PCR | TaqMan (SSU rRNA target) | 100% | 100% | Not specified | [48] |
| Real-time PCR | 5.8S rRNA target | High (value not specified) | High (value not specified) | Detected in stools stored for 8 weeks at 4°C | [70] |
| Conventional PCR | SSU rRNA target | Lower than real-time | High | ~1 trophozoite equivalent | [48] |
| Microscopy | Iron-hematoxylin stain | Lower than molecular methods | Subject to misidentification | N/A | [48] [71] |
Table 2: Performance Comparison of Entamoeba histolytica Detection Methods
| Method Type | Specific Method | Sensitivity | Specificity | Detection Limit | Reference |
|---|---|---|---|---|---|
| Real-time PCR | Molecular Beacon | Most sensitive (benchmark) | 100% | 0.1 parasite/g of feces | [72] [73] |
| Traditional PCR | Nested PCR | 72% | 99% | Varies | [72] |
| Antigen Detection | TechLab E. histolytica II | 79% | 96% | N/A | [72] |
| Microscopy | Stool examination | 10-60% | Low (cannot differentiate species) | N/A | [72] |
Detailed Experimental Protocols
Real-Time PCR forDientamoeba fragilisDetection
This protocol, adapted from Stark et al. (2006), describes a highly sensitive 5' nuclease (TaqMan) assay for detecting D. fragilis in human stool specimens [48].
DNA Extraction from Stool Specimens
- Specimen: Use fresh fecal specimens (<24 hours old).
- Kit: QIAamp DNA Stool Mini Kit (QIAGEN).
- Procedure: Follow the manufacturer's standard protocol for pathogen DNA isolation. A study found that modified protocols did not significantly improve yield and were less time-efficient [48].
- Inhibition Control: Spike patient fecal samples with a known quantity of cloned target DNA to rule out PCR inhibition.
Primer and Probe Sequences
Target the Small Subunit (SSU) rRNA gene:
- Forward Primer DF3: 5′-GTTGAATACGTCCCTGCCCTTT-3′
- Reverse Primer DF4: 5′-TGATCCAATGATTTCACCGAGTCA-3′
- TaqMan Probe: 5′-6-carboxyfluorescein-CACACCGCCCGTCGCTCCTACCG-6-carboxytetramethylrhodamine-3′
Real-Time PCR Reaction Setup
- Platform: LightCycler (Roche).
- Reaction Volume: 20 µL.
- Reaction Mix:
- 2 µL FastStart Reaction Mix Hybridization Probes (Roche)
- 3 mM MgClâ‚‚
- 0.25 µM each forward and reverse primer
- 0.2 µM dual-labeled fluorescent probe
- 2 µL of extracted DNA template
- Cycling Conditions:
- Initial Denaturation: 95°C for 10 minutes
- 35 Cycles of:
- Denaturation: 95°C for 10 seconds
- Annealing: 58°C for 10 seconds
- Extension: 72°C for 3 seconds
- Readout: Perform in channel F1.
Real-Time PCR for Detection and Differentiation ofEntamoeba histolytica
This protocol, based on a closed-tube real-time PCR assay, sensitively differentiates E. histolytica from the non-pathogenic E. dispar directly from feces [73].
DNA Extraction
- Kit: QIAamp DNA Stool Mini Kit (QIAGEN).
- Procedure: Follow the manufacturer's instructions.
Primer and Probe Sequences forE. histolytica
Target the ribosomal DNA-containing ameba episome.
- Forward Primer (Eh-S26C): 5′-GTA CAA AAT GGC CAA TTC ATT CAA CG-3′
- Reverse Primer (Eh/Ed-AS25): 5′-GAA TTG ATT TTA CTC AAC TCT AGA G-3′
- LC-Red 640-labeled Probe (Eh/Ed-24): LC-Red 640-TCG AAC CCC AAT TCC TCG TTA TCC p
- Fluorescein-labeled Probe (Eh/Ed-25): Fluorescein-GCC ATC TGT AAA GCT CCC TCT CCG A X For *E. dispar, replace the forward primer with Ed-27C: 5′-GTA CAA AGT GGC CAA TTT ATG TAA GCA-3′*
Real-Time PCR Reaction Setup
- Platform: LightCycler (Roche).
- Reaction Volume: 10 µL in a glass capillary.
- Reaction Mix:
- 1 µL FastStart Reaction Mix Hybridization Probes (Roche)
- 1.2 µL MgCl₂ (25 mM)
- 1 µL each sense and antisense primer (10 pmol/µL)
- 0.5 µL each LC-Red 640- and fluorescein-labeled probe (4 pmol/µL)
- 1 µL DNA extract
- H₂O to 10 µL
- Cycling Conditions:
- Initial Denaturation: 95°C for 5 minutes
- 50 Cycles with Touch-Down:
- Denaturation: 95°C for 10 seconds
- Annealing: Stepwise decrease from 62°C to 58°C in first 8 cycles, then 58°C for 10 seconds
- Extension: 72°C for 20 seconds
- Readout: Perform in channel F2/Back-F1. A sample is positive if the software determines a crossing point.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for Protozoan PCR Detection
| Item | Function/Application | Specific Example |
|---|---|---|
| DNA Extraction Kit | Isolation of inhibitor-free DNA from complex stool matrices. | QIAamp DNA Stool Mini Kit (QIAGEN) [48] [72] [73] |
| Real-Time PCR Master Mix | Provides enzymes, dNTPs, and buffer for efficient amplification. | FastStart DNA Master Hybridization Probes Kit (Roche) [48] [73] |
| Commercial Multiplex PCR Kit | FDA-cleared syndromic testing for multiple GI parasites in a single test. | EasyScreen Gastrointestinal Parasite Detection Kit (Genetic Signatures) [74] |
| Inhibition Control | Detects PCR inhibitors in extracted DNA to prevent false negatives. | qPCR Extraction Control Kit (Meridian Bioscience) [75] |
| Cloned Target Plasmid | Used as a positive control and for determining assay sensitivity. | pDf18S rRNA (cloned SSU rRNA gene of D. fragilis) [48] |
Critical Considerations for Assay Design and Validation
Addressing Specificity and Cross-Reactivity
A primary challenge in molecular detection is ensuring specificity and recognizing cross-reactivity, especially when applying human-designed assays to veterinary specimens or in regions with diverse parasite populations.
- Melt Curve Analysis: A 2025 study demonstrated that melt curve analysis is a powerful tool for identifying non-specific amplification. When screening cattle samples for D. fragilis, a 9°C lower melt temperature was observed compared to human positives. Subsequent sequencing confirmed cross-reactivity with Simplicimonas sp. [75].
- Cycle Threshold (Ct) Limit: To reduce false positives from non-specific amplification in later cycles, it is recommended to set a conservative Ct limit, such as reducing the number of PCR cycles to less than 40 [75].
- Confirmatory Sequencing: The identification of new hosts for a parasite should not rely solely on qPCR. Confirmation through DNA sequencing of the PCR product (e.g., of the SSU rDNA) is essential for validation [75].
The Challenge of Variable Shedding
A key factor affecting clinical sensitivity, which is distinct from analytical sensitivity, is the biology of the parasite. D. fragilis exhibits intermittent shedding of trophozoites in stool, meaning infected individuals may not consistently shed the parasite. This necessitates the testing of multiple stool samples over several days to achieve maximum diagnostic yield, a consideration crucial for both clinical trials and patient management [71].
Workflow and Decision Pathway for Assay Implementation
The following diagram illustrates the recommended workflow for implementing and validating a real-time PCR assay for intestinal protozoa, incorporating steps to address critical issues like inhibition and cross-reactivity.
The transition from traditional microscopy to real-time PCR for detecting intestinal protozoa like Dientamoeba fragilis and Entamoeba histolytica represents a significant advancement in diagnostic precision. The protocols and data presented here provide researchers with a robust framework for implementing these sensitive and specific assays. Key to success is a rigorous validation process that includes inhibition controls, melt curve analysis, and confirmatory sequencing to guard against false results. By adopting these optimized molecular approaches, the scientific community can improve diagnostic accuracy, enhance epidemiological understanding, and accelerate development of therapeutics for these important enteric pathogens.
Benchmarking Success: Validating qPCR Assays Against Gold Standards and Commercial Kits
The diagnosis of intestinal protozoan infections, caused by pathogens such as Giardia duodenalis, Cryptosporidium spp., and Entamoeba histolytica, is pivotal for effective treatment and disease control [76] [3]. For decades, traditional microscopy has served as the reference standard in clinical laboratories worldwide, offering a low-cost method for the morphological identification of cysts, trophozoites, and oocysts in fecal specimens [3] [12]. Similarly, immunochromatographic and enzyme-linked immunosorbent assays (ELISAs) have emerged as rapid screening tools for specific antigens [76] [3]. However, these conventional techniques are hampered by significant limitations, including subjective interpretation, an inability to differentiate morphologically identical species, and variable sensitivity and specificity [3] [12] [77].
Molecular diagnostic technologies, particularly real-time PCR (qPCR), are gaining traction in non-endemic areas with low parasitic prevalence due to their enhanced sensitivity and specificity [76] [5]. This application note, framed within a broader thesis on real-time PCR protocols for intestinal protozoa, provides a detailed comparison of these diagnostic methods. It summarizes critical performance data and outlines standardized experimental protocols to guide researchers and scientists in validating and implementing molecular assays for intestinal protozoa research and drug development.
Comparative Performance of Diagnostic Methods
Numerous studies have systematically evaluated the performance of molecular assays against traditional microscopy and antigen tests. The data below highlight the superior sensitivity and specificity of qPCR, particularly for detecting low burdens of infection and for differentiating between pathogenic and non-pathogenic species.
Table 1: Performance of a Commercial Multiplex qPCR (Allplex GI-Parasite Assay) vs. Conventional Methods in an Italian Multicentre Study (n=368 samples) [12]
| Pathogen | Sensitivity (%) | Specificity (%) | Notes |
|---|---|---|---|
| Entamoeba histolytica | 100 | 100 | Crucial for distinguishing from non-pathogenic E. dispar. |
| Giardia duodenalis | 100 | 99.2 | Superior to microscopy and antigen tests. |
| Dientamoeba fragilis | 97.2 | 100 | Detection is difficult with microscopy. |
| Cryptosporidium spp. | 100 | 99.7 | Highly sensitive and specific. |
Table 2: Performance of an Automated High-Throughput Multiplex qPCR in a Canadian Study [22]
| Pathogen | Sensitivity (%) | Specificity (%) | Positive Predictive Value (PPV) (%) | Negative Predictive Value (NPV) (%) |
|---|---|---|---|---|
| Blastocystis hominis | 93.0 | 98.3 | 85.1 | 99.3 |
| Cryptosporidium spp. | 100 | 100 | 100 | 100 |
| Cyclospora cayetanensis | 100 | 100 | 100 | 100 |
| Dientamoeba fragilis | 100 | 99.3 | 88.5 | 100 |
| Entamoeba histolytica | 33.3* | 100 | 100 | 99.6 |
| Giardia lamblia | 100 | 98.9 | 68.8 | 100 |
Sensitivity for *E. histolytica increased to 75% with the inclusion of frozen specimens, indicating sample preservation impacts DNA recovery [22].
Table 3: Summary of Method Advantages and Limitations
| Method | Key Advantages | Key Limitations |
|---|---|---|
| Microscopy | Low cost; detects a broad range of parasites; gold standard for helminths [78] [77]. | Low sensitivity & specificity; unable to differentiate species (e.g., E. histolytica vs. E. dispar); requires high expertise [3] [12]. |
| Antigen Tests | Rapid; simple to use; suitable for screening [76] [3]. | Limited pathogen panel; false positives/negatives reported; cannot differentiate species [3] [12]. |
| qPCR / Molecular Panels | High sensitivity & specificity; species-level differentiation; high-throughput; objective readout [5] [22] [12]. | Higher cost; requires specific equipment; sensitive to PCR inhibitors in stool; DNA extraction critical [76] [79]. |
Experimental Protocols for Molecular Detection
The following section details standardized protocols for the molecular detection of intestinal protozoa, from sample preparation to DNA amplification, as utilized in recent studies.
Sample Collection and DNA Extraction
Sample Handling:
- Collection: Collect fresh stool samples in clean, sterile containers. For optimal DNA preservation, store samples in preservation media such as Para-Pak or S.T.A.R. Buffer [76] [3]. Studies indicate that PCR results from preserved stool samples can be superior to those from fresh samples due to better DNA integrity [76].
- Storage: Immediately freeze and store samples at -20°C or -80°C until processing [3] [12].
DNA Extraction Protocol (Magnetic Separation-Based): [3] This protocol is designed for use with the MagNA Pure 96 System (Roche).
- Homogenization: Mix 350 µL of S.T.A.R. Buffer with approximately 1 mg of fecal sample using a sterile loop.
- Incubation and Centrifugation: Incubate the mixture for 5 minutes at room temperature. Subsequently, centrifuge at 2000 rpm for 2 minutes.
- Supernatant Collection: Carefully transfer 250 µL of the supernatant to a fresh tube. Add 50 µL of an internal extraction control.
- Automated Extraction: Load the samples into the MagNA Pure 96 System and perform DNA extraction using the "MagNA Pure 96 DNA and Viral NA Small Volume Kit" according to the manufacturer's instructions. The final elution volume is typically 100 µL.
Alternative Approach: Several studies successfully used the automated Hamilton STARlet liquid handler with the StarMag Universal Cartridge kit (Seegene) for high-throughput DNA extraction [22].
Real-Time PCR Amplification
A) Commercial Multiplex Assay (Allplex GI-Parasite Assay) [22] [12] This assay detects G. duodenalis, D. fragilis, E. histolytica, B. hominis, C. cayetanensis, and Cryptosporidium spp.
- PCR Master Mix: Prepare a reaction containing 5 µL of 5X GI-P MOM primer mix, 10 µL of RNase-free water, and 5 µL of EM2 (contains DNA polymerase, Uracil-DNA glycosylase, and buffer).
- Reaction Setup: Aliquot 20 µL of the master mix into each PCR tube. Add 5 µL of extracted template DNA, bringing the total reaction volume to 25 µL.
- Thermocycling Conditions: Run on a Bio-Rad CFX96 real-time PCR detection system using the following protocol:
- Denaturation: 95°C for 10 min
- 45 cycles of:
- 95°C for 10 s
- 60°C for 1 min
- 72°C for 30 s
- Result Interpretation: Fluorescence is detected at 60°C and 72°C. A cycle threshold (Ct) value of ≤45 is considered positive [12].
B) In-House Duplex qPCR Assay [5] [6] This protocol describes the implementation of two duplex qPCRs and singleplex assays for a 10 µL reaction volume.
- Reaction Composition: Each 10 µL reaction contains 5 µL of master mix (e.g., 2X TaqMan Fast Universal PCR Master Mix), primers and probes at optimized concentrations (e.g., 0.3-0.5 µM each), and sterile water.
- Thermocycling Conditions:
- Hold Stage: 95°C for 10 min
- PCR Stage (45 cycles): 95°C for 15 s, 60°C for 1 min.
- Primer/Probe Sequences: The table below provides examples of targets and sequences used in published assays.
Table 4: Research Reagent Solutions for qPCR Detection
| Item | Function / Target | Example Specification / Sequence (if provided) |
|---|---|---|
| DNA Extraction Kit | Nucleic acid purification from complex stool samples. | MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche) [3]; StarMag Universal Cartridge kit (Seegene) [22]. |
| PCR Master Mix | Provides enzymes, dNTPs, and buffer for amplification. | TaqMan Fast Universal PCR Master Mix (2X) [3]. |
| Commercial PCR Assay | Multiplex detection of protozoan targets. | Allplex GI-Parasite Assay (Seegene) [22] [12]. |
| Primers & Probe (G. duodenalis) | Target small subunit ribosomal RNA gene. | Forward: GCT GCG TCA CGC TGC TC; Reverse: GAC GGC TCA GGA CAA CGG T; Probe: (See original publication for full sequence) [5]. |
| Primers & Probe (E. histolytica/dispar) | Target 18S ribosomal RNA gene. | Forward: AGG ATT GGA TGA AAT TCA GAT GTA CA; Reverse: TAA GTT TCA GCC TTG TGA CCA TAC [5]. |
| Internal Control | Monitors extraction and amplification efficiency. | Included in commercial kits or designed separately [3]. |
Workflow and Decision Pathway
The following diagram illustrates the integrated diagnostic workflow for detecting intestinal protozoa, comparing traditional and molecular pathways.
The data and protocols presented confirm that real-time PCR assays represent a new standard for the detection of intestinal protozoa in research and clinical settings. Molecular methods consistently demonstrate superior sensitivity and specificity compared to microscopy and antigen tests, while also providing the critical ability to differentiate between pathogenic and non-pathogenic species [76] [5] [12]. The implementation of standardized, high-throughput protocols ensures reliable, objective, and efficient detection of these pathogens. For researchers and drug development professionals, adopting these advanced qPCR protocols is essential for accurate epidemiological studies, clinical trials, and monitoring the efficacy of novel therapeutic compounds against intestinal protozoa.
Within the diagnostic and research landscape for intestinal protozoan infections, real-time PCR (qPCR) has emerged as a transformative technology. It addresses critical limitations of traditional microscopy, which, despite its widespread use, is labor-intensive, requires skilled technicians, and lacks the sensitivity and specificity to differentiate morphologically identical species, such as the pathogenic Entamoeba histolytica from the non-pathogenic E. dispar [80] [3] [12]. Molecular methods are particularly crucial in non-endemic, high-income countries, where low parasite prevalence makes high diagnostic sensitivity essential [80] [11]. The choice between commercial multiplex qPCR assays and laboratory-developed in-house tests presents a significant dilemma for laboratories. This application note, framed within a broader thesis on optimizing real-time PCR protocols for intestinal protozoa, synthesizes data from recent multicentre studies to evaluate the performance, reliability, and practical application of these two approaches for researchers, scientists, and drug development professionals.
Performance Comparison: Commercial vs. In-House qPCR
The relative performance of commercial and in-house qPCR assays has been directly compared in several studies, with key metrics summarized in Table 1.
Table 1: Comparative Performance of qPCR Assays from Multicentre Studies
| Target Parasite | Assay Type | Sensitivity (%) | Specificity (%) | Notes | Study (Citation) |
|---|---|---|---|---|---|
| Giardia duodenalis | Commercial (AusDiagnostics) | 100 | 100 | Complete agreement with in-house PCR | [3] |
| In-House (Padua Hospital) | 100 | 100 | Complete agreement with commercial PCR | [3] | |
| Commercial (Allplex GI-Parasite) | 100 | 99.2 | Compared to conventional methods | [12] | |
| Cryptosporidium spp. | Commercial (AusDiagnostics) | High Specificity | Limited Sensitivity | Inadequate DNA extraction suspected | [3] |
| In-House (Padua Hospital) | High Specificity | Limited Sensitivity | Inadequate DNA extraction suspected | [3] | |
| Commercial (Allplex GI-Parasite) | 100 | 99.7 | Compared to conventional methods | [12] | |
| Entamoeba histolytica | Commercial (AusDiagnostics) | Critical for accurate diagnosis | Critical for accurate diagnosis | Superior to microscopy for species differentiation | [3] |
| In-House (Padua Hospital) | Critical for accurate diagnosis | Critical for accurate diagnosis | Superior to microscopy for species differentiation | [3] | |
| Commercial (Allplex GI-Parasite) | 100 | 100 | Compared to conventional methods | [12] | |
| Dientamoeba fragilis | Commercial (AusDiagnostics) | High Specificity | Limited Sensitivity | Inconsistent detection | [3] |
| In-House (Padua Hospital) | High Specificity | Limited Sensitivity | Inconsistent detection | [3] | |
| Commercial (Allplex GI-Parasite) | 97.2 | 100 | Compared to conventional methods | [12] |
A pivotal 2025 Italian multicentre study analyzing 355 stool samples found that for Giardia duodenalis, both the commercial AusDiagnostics test and an in-house assay demonstrated complete agreement and high performance [3]. However, for other protozoa like Cryptosporidium spp. and Dientamoeba fragilis, both molecular methods exhibited high specificity but limited sensitivity, which the authors attributed to challenges in DNA extraction from the robust (oo)cyst walls of these parasites [3]. The study concluded that molecular assays are particularly critical for the accurate diagnosis of Entamoeba histolytica, where microscopy fails [3].
In contrast, a separate 2025 multicentre evaluation of the Allplex GI-Parasite Assay (Seegene) reported exceptional performance across the board, with sensitivities of 97.2-100% and specificities of 99.2-100% for all targeted protozoa (G. duodenalis, E. histolytica, D. fragilis, Cryptosporidium spp.) when compared to a composite of conventional methods [12]. This suggests that some commercial multiplex assays have achieved a high level of optimization and reliability.
Comparative Analysis of Commercial Multiplex Kits
Beyond the comparison with in-house tests, studies have also directly evaluated the performance of different commercial kits against each other. A 2019 study compared four commercial multiplex qPCR assays using a reference DNA panel, finding significant variation in diagnostic performance [80] [81].
Table 2: Performance of Commercial Multiplex qPCR Kits for Key Protozoa
| Commercial qPCR Kit | Cryptosporidium hominis/parvum Sensitivity | Giardia duodenalis Sensitivity | Key Findings | Study (Citation) |
|---|---|---|---|---|
| RIDAGENE (R-Biopharm) | 87.5% | Not Specified | Best performance for Cryptosporidium; 100-fold better detection limit. | [80] [81] |
| FTD Stool Parasites (Fast Track) | 53.1% | 100% | Poor for Cryptosporidium; superior for Giardia (10-fold better detection limit). | [80] [81] |
| Gastroenteritis Panel (Diagenode) | 78.1% | 97.9% | Did not detect E. histolytica. | [80] [81] |
| Allplex Panel (Seegene) | 71.9% | 68.1% | Lower sensitivity for Giardia in this particular evaluation. | [80] [81] |
The study concluded that diagnostic performance varied substantially based on the method and the targeted pathogen. Factors such as test sensitivity/specificity, cost, workflow, and the patient population must be carefully considered when selecting a platform [80] [81].
Detailed Experimental Protocols
To ensure reproducibility and facilitate the adoption of these methods, detailed protocols for in-house assay development and commercial kit validation are provided below.
Protocol 1: Development and Validation of a Triplex In-House qPCR
This protocol is adapted from a study that developed a triplex qPCR for the simultaneous detection of E. histolytica, G. lamblia, and C. parvum [7].
1. Primer and Probe Design:
- Target Genes:
- E. histolytica: 16S-like SSU rRNA gene (GenBank X56991.1)
- G. lamblia: gdh gene (GenBank KM190761.1)
- C. parvum: 18S rRNA gene (GenBank NC_006987.1)
- Design Parameters: Use software (e.g., Primer Express). Confirm specificity via BLAST. Aim for a GC content of ~50%, length of 20-24 bases, and Tm of ~58°C [7].
- Sequences: See Table 3 for sequences from the study.
Table 3: Primer and Probe Sequences for Triplex qPCR [7]
| Organism | Target | Primer/Probe | Sequence (5' to 3') |
|---|---|---|---|
| E. histolytica | 16S-like SSU rRNA | Forward | CGC AGC TCA GAC TGT AAT TCC T |
| Reverse | GCT GGC ACC AGA CTT GTC T | ||
| Probe | FAM-AGG AAT TAA GTA CCT TTG CTG CT-BHQ1 | ||
| G. lamblia | gdh | Forward | GCT GCG TCA CGC TGC TC |
| Reverse | GAC GGC TCA GGA CAA CGG T | ||
| Probe | HEX-CGC TGC CGT CGC TGG A-BHQ1 | ||
| C. parvum | 18S rRNA | Forward | ACA TGG ATA ACC GTG GTA ATT CT |
| Reverse | CAA TAC CCT ACC GTC TAA AGC TG | ||
| Probe | CY5-ACT CGA CTT TAT GGA AGG GTT GTA T-BHQ2 |
2. DNA Extraction:
- Use commercial kits such as the QIAamp DNA Stool Mini Kit or similar, following the manufacturer's instructions [7] [3]. Automated systems like the MagNA Pure 96 System can also be employed for high-throughput and consistency [3].
3. qPCR Reaction Setup:
- Reaction Volume: 25 µL
- Reaction Mix: 12.5 µL of 2x TaqMan Fast Universal PCR Master Mix, 0.5-0.9 µM of each primer, 0.1-0.3 µM of each probe, 5 µL of DNA template, and nuclease-free water to volume [7].
- Cycling Conditions:
- Hold: 95°C for 10 min
- 45 Cycles: 95°C for 15 sec, 60°C for 1 min (data collection)
4. Validation and Analysis:
- Standard Curves: Generate using plasmids containing target sequences. The assay should demonstrate a limit of detection (LOD) of around 500 copies/µL, with amplification efficiency >95% and R² >0.99 [7].
- Analysis: Use software (e.g., Bio-Rad CFX Manager) to analyze amplification curves. A cycle threshold (Ct) below 40 is typically considered positive [11].
Protocol 2: Multicenter Validation of a Commercial qPCR Assay
This protocol outlines the procedure for evaluating a commercial kit, as used in the study of the Allplex GI-Parasite Assay [12].
1. Sample Collection and Storage:
- Collect stool samples from patients suspected of enteric parasitic infection.
- Preserve samples by freezing at -20°C or -80°C until batch testing.
2. DNA Extraction (Automated):
- Sample Preparation: Suspend 50-100 mg of stool in 1 mL of lysis buffer (e.g., Qiagen ASL buffer). Vortex and incubate for 10 min at room temperature. Centrifuge at 14,000 rpm for 2 min.
- Nucleic Acid Extraction: Use an automated system like the Microlab Nimbus IVD. The system automatically processes the supernatant from the previous step and sets up the PCR reaction, ensuring minimal manual handling and cross-contamination [12].
3. qPCR Setup and Run:
- Kit: Allplex GI-Parasite Assay (targets: G. duodenalis, D. fragilis, E. histolytica, B. hominis, Cyclospora cayetanensis, Cryptosporidium spp.)
- Platform: CFX96 Real-time PCR system or equivalent.
- Procedure: Follow the manufacturer's instructions. The automated Nimbus system directly aliquots the prepared DNA into the PCR mix.
- Cycling and Analysis: Run the pre-programmed cycling protocol. Analyze results using the Seegene Viewer software. A positive result is typically defined by a Ct value <45 [12].
4. Discrepancy Analysis:
- In case of discordant results between the commercial PCR and reference methods, retest the sample with both the qPCR and the traditional method (e.g., microscopy, antigen testing) to resolve the outcome [12].
Experimental Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for a multicentre evaluation comparing commercial and in-house qPCR assays, from sample collection to data interpretation.
Diagram 1: Workflow for Multicentre qPCR Evaluation. This chart outlines the parallel pathways for comparing traditional and molecular diagnostic methods, culminating in a performance analysis that informs assay selection.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of qPCR assays, whether commercial or in-house, relies on key reagents and instruments. The table below details essential components as utilized in the cited studies.
Table 4: Essential Reagents and Instruments for Intestinal Protozoa qPCR
| Item Category | Specific Examples | Function & Application Notes | Citation |
|---|---|---|---|
| Commercial qPCR Kits | RIDAGENE Parasitic Stool Panel (R-Biopharm); Allplex GI-Parasite (Seegene); FTD Stool Parasites (Fast Track); Gastroenteritis/Para-site Panel I (Diagenode) | Multiplex detection of major protozoa. Performance varies by manufacturer and target pathogen. | [80] [12] |
| DNA Extraction Kits | QIAamp DNA Stool Mini Kit (Qiagen); MagNA Pure 96 DNA Kit (Roche) | Critical for breaking down robust (oo)cyst walls and removing PCR inhibitors present in stool. | [7] [3] |
| Automated Extraction/PCR Setup | Microlab Nimbus IVD (Hamilton); MagNA Pure 96 System (Roche) | Ensures high-throughput, reproducibility, and reduced risk of cross-contamination. | [11] [12] |
| qPCR Instruments | CFX96 (Bio-Rad); ABI 7900HT (Applied Biosystems); Rotor-Gene 6000 (Qiagen) | Platforms for amplification and fluorescence detection. Must be compatible with the assay chemistry. | [80] [7] [3] |
| Target-Specific Primers/Probes | Custom designs for E. histolytica 16S-like rRNA, G. duodenalis gdh, C. parvum 18S rRNA | Core components of in-house assays. Specificity and optimization are paramount. | [5] [7] |
| Positive Controls | Recombinant plasmids with cloned target genes; characterized positive stool samples | Essential for assay validation, run control, and determining limit of detection (LOD). | [7] |
The diagnosis of intestinal protozoan infections is critical for public health, particularly in resource-limited settings and for vulnerable populations. Traditional diagnosis via microscopic examination, while cost-effective, is limited by poor sensitivity, an inability to differentiate morphologically identical species, and a dependency on high technical expertise [5] [12]. Molecular methods, particularly real-time PCR (qPCR), have emerged as superior tools, offering enhanced sensitivity, specificity, and throughput [22]. This document details the key performance metrics—sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and throughput—of modern qPCR assays for detecting intestinal protozoa, providing application notes and protocols for researchers and scientists in the field.
Performance Metrics of qPCR Assays for Intestinal Protozoa
The following tables summarize the performance characteristics of various qPCR assays as validated in recent studies.
Table 1: Performance Metrics of the Seegene Allplex GI-Parasite Assay (Validation Study from Public Health Ontario Laboratories on 461 Unpreserved Fecal Specimens) [22]
| Protozoan Pathogen | Sensitivity (%) | Specificity (%) | Positive Predictive Value (PPV %) | Negative Predictive Value (NPV %) |
|---|---|---|---|---|
| Blastocystis hominis | 93.0 | 98.3 | 85.1 | 99.3 |
| Cryptosporidium spp. | 100 | 100 | 100 | 100 |
| Cyclospora cayetanensis | 100 | 100 | 100 | 100 |
| Dientamoeba fragilis | 100 | 99.3 | 88.5 | 100 |
| Entamoeba histolytica | 33.3* | 100 | 100 | 99.6 |
| Giardia lamblia | 100 | 98.9 | 68.8 | 100 |
| Note: Sensitivity for *Entamoeba histolytica increased to 75% with the inclusion of 17 frozen specimens.* |
Table 2: Performance Metrics of the Seegene Allplex GI-Parasite Assay (Multicentric Italian Study on 368 Samples) [12] [82]
| Protozoan Pathogen | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Entamoeba histolytica | 100 | 100 |
| Giardia duodenalis | 100 | 99.2 |
| Dientamoeba fragilis | 97.2 | 100 |
| Cryptosporidium spp. | 100 | 99.7 |
Table 3: Throughput and Workflow Efficiency of Molecular vs. Conventional Methods
| Metric | Conventional Microscopy | Multiplex qPCR (e.g., AllPlex GIP) |
|---|---|---|
| Analytical Turnaround Time | Prolonged (multiple staining, reading) | Reduced by ~7 hours per batch [22] |
| Sample Processing | Low-throughput, manual | High-throughput, automated [22] [11] |
| Detection in First Sample | Often requires multiple samples [12] | Highly likely on first sample [11] |
Experimental Protocols
Protocol: Implementation of a Duplex qPCR Assay for Intestinal Protozoa
This protocol is adapted from a study that implemented two duplex qPCR assays for detecting Entamoeba dispar + Entamoeba histolytica and Cryptosporidium spp. + Chilomastix mesnili, alongside singleplex assays for Giardia duodenalis and Blastocystis spp. [6] [5].
3.1.1 Primer and Probe Design
- Source: Primers and probes for Blastocystis spp., Cryptosporidium spp., E. histolytica, E. dispar, and G. duodenalis can be obtained from established diagnostic centers or literature [5].
- Novel Targets: For novel targets like Chilomastix mesnili, retrieve sequence data (e.g., small ribosomal subunit) from the NCBI database.
- Design Parameters: Identify highly conserved regions using tools like BLASTN. Design primers and probes with a GC content of ~50%, length of 20-24 bases, and a melting temperature (TM) of approximately 58°C.
- Specificity Check: Confirm the uniqueness of all primer and probe sequences via individual BLASTN searches against the NCBI database [5].
3.1.2 Reagent Setup
- Prepare a master mix for a 10 µL reaction volume.
- Use a final primer concentration of 0.3-0.5 µM, as optimized for each target.
- Select appropriate fluorophores and quenchers compatible with your real-time PCR detection system (e.g., CFX Maestro) [5].
3.1.3 qPCR Amplification
- Use standard cycling conditions for TaqMan-based assays: an initial denaturation step (e.g., 95°C for 2-5 minutes), followed by 45 cycles of denaturation (e.g., 95°C for 10-15 seconds) and a combined annealing/extension step (e.g., 60°C for 30-60 seconds) [5] [12].
Protocol: Validation of a Commercial Multiplex qPCR Assay
This protocol outlines the procedure for using and validating the automated Seegene Allplex GI-Parasite Assay [22] [12].
3.2.1 Sample Preparation and DNA Extraction
- Sample Collection: Inoculate a swab of fresh, unpreserved stool into a FecalSwab tube containing Cary-Blair transport media. Vortex for 10 seconds to homogenize [22].
- Automated Nucleic Acid Extraction: Load samples onto an automated liquid handling platform (e.g., Hamilton STARlet or Microlab Nimbus IVD). Perform extraction using the manufacturer's recommended kit (e.g., STARMag 96 × 4 Universal Cartridge kit). The protocol typically uses 50 µL of stool suspension, eluting DNA in a final volume of 100 µL [22] [12].
3.2.2 PCR Setup and Amplification
- Reaction Mix: Aliquot the PCR master mix. For the Allplex assay, this includes the 5X GI-P MOM primer mix, RNase-free water, and EM2 (containing DNA polymerase, Uracil-DNA glycosylase, and dNTPs) [22].
- Setup: Combine 20 µL of master mix with 5 µL of extracted DNA in a PCR tube. This step is fully automated on platforms like the Hamilton STARlet or Microlab Nimbus [22] [12].
- Amplification: Run the real-time PCR on a compatible thermocycler (e.g., Bio-Rad CFX96). Use the following cycling conditions as an example:
- Analysis: Interpret results using the manufacturer's software (e.g., Seegene Viewer). A cycle threshold (Ct) value of ≤40-45 is typically considered positive [12] [11].
Workflow and Pathway Diagrams
The following diagram illustrates the high-level workflow for the multiplex qPCR diagnostic process, from sample receipt to result interpretation, highlighting key decision points and parallel paths for molecular and traditional methods.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Kits for Intestinal Protozoa qPCR
| Item | Function/Description | Example Product/Supplier |
|---|---|---|
| Multiplex PCR Assay Kit | Contains pre-optimized primer-probe mixes for simultaneous detection of multiple protozoan targets. | Allplex GI-Parasite Assay (Seegene Inc.) [22] [12] |
| Automated Nucleic Acid Extraction Kit | Reagents for bead-based extraction of DNA from complex stool samples on automated platforms. | STARMag 96 × 4 Universal Cartridge Kit (Seegene Inc.) [22] |
| Stool Transport Medium | Preserves nucleic acids and ensures sample homogeneity for downstream DNA extraction. | FecalSwab with Cary-Blair Media (COPAN Diagnostics) [22] [11] |
| Internal Control | Non-competitive control added to each sample to monitor extraction efficiency and PCR inhibition. | Included in commercial multiplex kits [11] |
| Automated Liquid Handler | Instrument for high-throughput, reproducible nucleic acid extraction and PCR setup. | Hamilton STARlet, Microlab Nimbus IVD [22] [12] |
| Real-Time PCR Thermocycler | Instrument for DNA amplification with fluorescence detection for real-time, quantitative analysis. | Bio-Rad CFX96 [22] [12] |
The accurate detection of enteric protozoan parasites is a cornerstone of public health, particularly in the realms of patient diagnosis, outbreak investigation, and drug development. Traditional diagnostic methods, primarily microscopy, are hampered by challenges including significant technical expertise, prolonged turnaround times, and limited sensitivity and specificity [11] [82]. The advent of real-time PCR (qPCR) has revolutionized this field, offering a more objective, higher-throughput alternative capable of distinguishing morphologically identical species, such as the pathogenic Entamoeba histolytica from the non-pathogenic Entamoeba dispar [5] [82].
However, the transition from in-house, single-laboratory qPCR assays to robust, standardized diagnostic tools requires rigorous validation. Multi-laboratory validation (MLV) studies are the gold standard for this process, providing independent verification of a method's performance across different instruments, operators, and environmental conditions. These studies are indispensable for ensuring that results are reproducible, reliable, and comparable across sites—a fundamental requirement for large-scale epidemiological studies and clinical trials. This application note details the protocols and quantitative outcomes of MLV studies for qPCR assays targeting intestinal protozoa, providing a framework for researchers and drug development professionals to ensure the highest standards of data integrity.
Performance Comparison of Validated Molecular Assays
The following tables summarize the key performance metrics from recent multi-laboratory and single-laboratory validation studies for various PCR-based assays detecting intestinal protozoa. These data provide a benchmark for expected outcomes in validation workflows.
Table 1: Summary of Multi-Laboratory Validation Study for Cyclospora cayetanensis Detection in Fresh Produce
| Parameter | Mit1C qPCR Method [83] | 18S qPCR (Reference Method) [83] |
|---|---|---|
| Overall Detection Rate (200 oocysts) | 100% (78/78) | 100% (78/78) |
| Overall Detection Rate (5 oocysts) | 69.23% (99/143) | 61.54% (88/143) |
| Specificity | 98.9% | 100% |
| Between-Laboratory Variance | Nearly zero | Not Specified |
| Relative Level of Detection (LODâ‚…â‚€) | 0.81 (95% CI: 0.600, 1.095) | 1 (Reference) |
Table 2: Performance of the AllPlex GI-Parasite Assay in Clinical Stool Samples
| Target Protozoa | Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Study |
|---|---|---|---|---|---|
| Giardia duodenalis | 100 | 99.2-100 | 68.8-100 | 99.3-100 | [22] [82] |
| Cryptosporidium spp. | 100 | 99.7-100 | 100 | 100 | [22] [82] |
| Dientamoeba fragilis | 97.2 | 100 | 88.5 | 100 | [82] |
| Entamoeba histolytica | 33.3-100 * | 100 | 100 | 99.6 | [22] [82] |
| Blastocystis hominis | 93 | 98.3 | 85.1 | 99.3 | [22] |
| Cyclospora cayetanensis | 100 | 100 | 100 | 100 | [22] |
Note: The sensitivity for *E. histolytica improved from 33.3% with fresh specimens to 75% when frozen specimens were included in the analysis, highlighting the impact of sample preservation [22].*
Experimental Protocols for Key Validation Procedures
Protocol 1: Multi-Laboratory Validation of a Novel qPCR Method
This protocol is adapted from an MLV study for detecting Cyclospora cayetanensis in fresh produce, which can be adapted for clinical stool samples [83].
1. Study Design and Sample Preparation: - Participating Laboratories: Engage a minimum of 10-13 independent laboratories with relevant expertise. - Test Samples: Prepare a large batch of homogeneous, blind-coded samples. These should include: - Uninoculated samples: To assess specificity and false-positive rates. - Low-inoculum samples: Spiked with a low number of target organisms (e.g., 5 oocysts) near the expected limit of detection (LOD) to evaluate sensitivity. - High-inoculum samples: Spiked with a high number of target organisms (e.g., 200 oocysts) to confirm robust detection. - Reference Method: A well-characterized reference method (e.g., the 18S qPCR method for C. cayetanensis) must be run in parallel by all laboratories for comparison.
2. DNA Extraction and qPCR Setup: - Standardized Reagents: Provide all participating labs with identical kits for nucleic acid extraction and PCR amplification to minimize variability. - Automated Extraction: Utilize automated nucleic acid extraction platforms (e.g., Hamilton MICROLAB STARlet or Nimbus IVD) to improve reproducibility [11] [82]. - qPCR Amplification: Perform amplification on standardized real-time PCR instruments (e.g., Bio-Rad CFX96). The reaction mix should contain: - 5 µL of extracted DNA template. - 12.5 µL of 2x Master Mix. - 2.5 µL of specific primer/probe mix. - 5 µL of RNase-free water to a final volume of 25 µL [22] [84]. - Cycling Conditions: 95°C for 10 min, followed by 45 cycles of 95°C for 10 s, 60°C for 1 min, and 72°C for 30 s [22].
3. Data Analysis and Acceptance Criteria: - Data Collection: Collate cycle threshold (Ct) values and qualitative results (positive/negative) from all laboratories. - Statistical Analysis: Calculate overall detection rates, sensitivity, specificity, and the relative level of detection (RLOD) compared to the reference method. A method is considered equivalent if the confidence interval for the RLOD includes 1 [83]. - Assessment of Reproducibility: Analyze between-laboratory variance; a value close to zero indicates high reproducibility.
Protocol 2: In-House Validation of a Multiplex qPCR Assay
This protocol outlines the key parameters to validate before initiating an MLV study, as demonstrated in the development of novel assays [22] [84].
1. Analytical Specificity and Cross-Reactivity Testing: - Test Panel: Assemble a comprehensive panel of genomic DNA from target protozoa and phylogenetically related or clinically relevant non-target organisms (e.g., helminths, bacteria, human DNA). - Procedure: Run the qPCR assay with each non-target DNA sample. The assay must not generate a positive signal for any non-target organism to confirm specificity [84].
2. Limit of Detection (LOD) Determination: - Sample Preparation: Serially dilute a characterized positive control (e.g., oocysts/cysts counted by microscopy or optical density) in a negative stool matrix. - Replication: Test each dilution in a minimum of 12-20 replicates. - Analysis: The LOD is defined as the lowest concentration at which ≥95% of replicates test positive [22] [84].
3. Diagnostic Accuracy Assessment: - Sample Collection: Use a well-characterized panel of clinical samples with known status determined by a reference method (e.g., microscopy, antigen testing, or a previously validated PCR). - Blinded Testing: Perform the novel qPCR assay on the panel in a blinded manner. - Statistical Calculation: Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) by comparing the new assay's results to the reference standard [22] [82].
Workflow Diagram: Multi-Laboratory Validation Process
The following diagram illustrates the end-to-end workflow for conducting a multi-laboratory validation study, from initial planning to final analysis and reporting.
Multi-Lab Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
The successful implementation and validation of qPCR assays for intestinal protozoa rely on a core set of reagents and materials. The following table details essential components and their functions.
Table 3: Essential Research Reagents for qPCR-Based Detection of Intestinal Protozoa
| Reagent / Material | Function & Importance | Example Products / Targets |
|---|---|---|
| Commercial Multiplex PCR Kits | Provides pre-optimized master mixes and primer-probe sets for simultaneous detection of multiple pathogens, ensuring consistency across labs. | AllPlex GI-Parasite Assay (Seegene) [11] [22] [82] |
| Automated Nucleic Acid Extraction Systems | Standardizes the DNA extraction process, reducing human error, cross-contamination, and variability between technicians and sites. | Hamilton STARlet, Hamilton Nimbus IVD [11] [22] [82] |
| Stool Transport and Lysis Buffers | Preserves nucleic acid integrity during sample storage and transport, and facilitates the breakdown of tough protozoal (oo)cyst walls for efficient DNA release. | FecalSwab (Cary-Blair media), ASL Buffer (Qiagen) [11] [22] [82] |
| Target-Specific Primers and Probes | Binds to unique genomic sequences to ensure specific amplification and detection of the target protozoa, allowing for species-level differentiation. | Targets: E. histolytica 18S rRNA, Cryptosporidium SSU rRNA, C. cayetanensis Mit1C gene [5] [83] |
| Positive and Negative Control Materials | Verifies the correct performance of the entire qPCR process, from extraction to amplification, and is critical for validating each run. | Genomic DNA from cultured organisms, cloned plasmid controls, confirmed negative stool [22] [84] |
Multi-laboratory validation is a non-negotiable step in the journey from a promising in-house qPCR assay to a standardized, reliable tool for research and diagnostics. The protocols and data presented herein demonstrate that rigorously validated multiplex qPCR assays consistently outperform traditional microscopy in the detection of key intestinal protozoa like Giardia duodenalis, Cryptosporidium spp., and Dientamoeba fragilis [22] [82]. The high sensitivity, specificity, and reproducibility achieved through these studies provide the scientific community with confidence in the generated data, which is paramount for advancing our understanding of parasite epidemiology, assessing the efficacy of new therapeutic agents, and ultimately improving public health outcomes. By adhering to these structured validation frameworks, researchers and drug developers can ensure that their molecular methods are fit-for-purpose and yield comparable results across the global scientific landscape.
The Emerging Role of Digital PCR (dPCR) for Absolute Quantification and Enhanced Sensitivity
The diagnosis of intestinal protozoa infections, a major public health challenge in regions with poor sanitation, has long relied on traditional methods like bright-field microscopy [6] [65]. While cost-effective, microscopy is limited by subjective readout, an inability to distinguish morphologically identical species, and insufficient sensitivity and specificity [65]. The adoption of real-time PCR (qPCR) has marked a significant advancement, providing higher specificity and sensitivity, and enabling species-level differentiation crucial for pathogens like Entamoeba histolytica and the non-pathogenic Entamoeba dispar [6] [65].
Digital PCR (dPCR) represents a paradigm shift in molecular diagnostics. As a third-generation PCR technology, it enables absolute quantification of nucleic acids without the need for standard curves [85] [86] [87]. By partitioning a sample into thousands of individual reactions and applying Poisson statistics, dPCR calculates the exact concentration of the target molecule [86] [87]. This offers superior accuracy, consistency, and precision, particularly for quantifying low viral loads and detecting co-infections, making it a powerful tool for intestinal protozoa research and drug development [85].
Comparative Advantages of dPCR
Technical Superiority over qPCR and Microscopy
dPCR offers several critical advantages over qPCR and microscopy for protozoan research:
- Absolute Quantification: dPCR provides a direct count of target DNA molecules (in copies/μL), eliminating the variability introduced by the standard curves required in qPCR [85] [87]. This is vital for accurately assessing pathogen load, a key metric in understanding infection severity and treatment efficacy.
- Enhanced Sensitivity and Precision: The partitioning step in dPCR mitigates the effects of PCR inhibitors and sample matrix complexities, which are common challenges when working with stool samples [85]. This results in superior accuracy, especially for samples with low pathogen concentrations [85] [87]. A study on Hepatitis D virus (HDV) found that 31% of samples testing negative by RT-qPCR were positive by RT-dPCR, demonstrating its higher sensitivity for low-level targets [87].
- Robustness in Complex Matrices: Respiratory virus research has shown that dPCR offers greater consistency and precision than Real-Time RT-PCR, particularly in quantifying intermediate viral levels in complex sample matrices like nasopharyngeal swabs [85]. This robustness is directly transferable to the analysis of stool samples for intestinal protozoa.
Practical Implications for Protozoa Research and Drug Development
The technical benefits of dPCR translate into tangible improvements in research and diagnostic outcomes as shown in the table below.
Table 1: Impact of dPCR on Key Research and Diagnostic Applications
| Application Area | Impact of dPCR |
|---|---|
| Species-Level Differentiation | Enables precise discrimination of morphologically identical species (e.g., E. histolytica vs. E. dispar), crucial for accurate diagnosis and understanding pathogenesis [6] [65]. |
| Drug Efficacy Trials | Provides absolute quantification to accurately measure changes in pathogen load before and after treatment, offering a robust metric for evaluating new therapeutics [6]. |
| Detection of Low-Level Infections | High sensitivity allows for the identification of persistent or subclinical infections that may be missed by other methods, impacting epidemiology and control efforts [87]. |
| Comprehensive Pathogen Detection | Multiplexing capability allows for the simultaneous detection of multiple protozoa in a single reaction, improving speed and cost-effectiveness for surveillance [6] [86]. |
Experimental Application: dPCR for Intestinal Protozoa
Published Precedent and Research Context
A 2025 study on Pemba Island, Tanzania, effectively demonstrates the utility of advanced molecular diagnostics in intestinal protozoa research [6] [65]. The researchers implemented duplex qPCR assays to detect Entamoeba dispar + Entamoeba histolytica and Cryptosporidium spp. + Chilomastix mesnili, alongside singleplex assays for Giardia duodenalis and Blastocystis spp. [65]. This approach reliably detected protozoa in 74.4% of patient samples and provided crucial prevalence data for the region [6]. The study also highlighted the need for more sensitive tools, as it found no significant antiprotozoal effect of the investigational drug emodepside, a conclusion that could be further verified with the enhanced precision of dPCR [6] [65].
Proposed dPCR Protocol for Protozoan Detection
The following protocol is adapted from validated dPCR workflows for pathogen detection [87] and optimized for intestinal protozoa, leveraging the foundational qPCR assays from the Pemba Island study [65].
Protocol: Absolute Quantification of Intestinal Protozoa using dPCR
1. Sample Collection and DNA Extraction
- Sample Type: Collect fresh stool samples from patients. For biobanking, store at -80°C.
- DNA Extraction: Use a standardized kit optimized for stool samples, such as the QIAamp DNA Stool Mini Kit (Qiagen). Include negative extraction controls (molecular grade water) and positive controls (plasmid with target sequence) with each batch [65] [87].
- DNA Elution: Elute DNA in a consistent volume of RNase-free water (e.g., 60 μL) [87].
2. dPCR Reaction Setup
- Platform: This protocol is designed for a nanowell-based system (e.g., QIAcuity, Qiagen) or a droplet-based system (e.g., QX200, Bio-Rad). Adjust volumes according to manufacturer specifications.
- Reaction Mix (for one reaction):
- Primer/Probe Sets: Utilize previously published and validated sequences for protozoa. For example, the primers and probes for E. histolytica, E. dispar, Cryptosporidium spp., G. duodenalis, and Blastocystis spp. can be implemented as described in the Pemba Island study [65]. The assay for Chilomastix mesnili represents the first molecular detection by qPCR and can be adapted for dPCR [6] [65].
- Multiplexing: To maximize efficiency, develop duplex or triplex assays by combining primer/probe sets labeled with different fluorophores (e.g., FAM, HEX/VIC) [65].
3. dPCR Run Conditions
- Partition the reaction mixture according to the platform's protocol (e.g., ~26,000 nanowells for QIAcuity or ~20,000 droplets for QX200) [85] [86].
- Use the following thermal cycling conditions, optimized from protozoa qPCR protocols [65]:
- Enzyme activation: 95°C for 5-10 minutes
- 40-45 cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing/Extension: 60°C for 1 minute
- Hold: 4°C or 98°C (for droplet stability)
4. Data Analysis
- Use the instrument's native software (e.g., QIAcuity Suite Software) to analyze the endpoint fluorescence and determine the number of positive and negative partitions.
- The software will automatically apply Poisson statistics to calculate the absolute concentration of the target DNA in copies/μL of the reaction mix [86] [87].
- Convert the result to a clinically relevant unit (e.g., copies/gram of stool) using the following calculation:
Concentration (copies/g) = [Measured concentration (copies/μL) × Total DNA elution volume (μL)] / Mass of stool sample (g)
The following workflow diagram summarizes the key steps of this dPCR protocol:
dPCR Workflow for Protozoa Detection
Performance Data and Validation
Quantitative Comparison of dPCR and qPCR
The superior performance of dPCR is evident in direct comparisons with qPCR. The table below summarizes key performance metrics from clinical studies on viral and protozoan targets.
Table 2: Performance Comparison of dPCR versus qPCR
| Parameter | dPCR Performance | qPCR Performance | Research Context |
|---|---|---|---|
| Quantification Method | Absolute (copies/μL); no standard curve [86] [87] | Relative (Ct value); requires standard curve [85] | Fundamental difference in approach |
| Sensitivity | 31% more positive samples identified in low-concentration HDV cohort [87] | Missed low-level viremia later detected by dPCR [87] | Clinical plasma samples |
| Limit of Detection (LOD) | 0.7 copies/mL for HDV RNA [87] | 14 IU/mL for a commercial HDV kit [87] | Analytical sensitivity |
| Precision & Consistency | Superior accuracy for high/medium viral loads; greater consistency [85] | Variability due to sample matrix effects and standard curves [85] | Respiratory virus samples stratified by Ct value |
| Effect of Inhibitors | Reduced susceptibility due to partitioning [85] | More susceptible, leading to reduced efficiency [85] | Complex sample matrices (e.g., stool, sputum) |
Validation and Quality Control
For dPCR to be implemented in research and potential clinical settings, rigorous validation is essential.
- Limit of Detection (LOD) and Quantification (LOQ): Determine these by running a dilution series with a high number of replicates. One study used 20-50 replicates per dilution to establish an LOD of 0.7 copies/mL and LOQ of 10 copies/mL for HDV [87].
- Conversion to International Units: To align with existing standards, a conversion factor can be calculated using the World Health Organization (WHO) International Standard. For example, a conversion factor of 0.77 (copies/mL to IU/mL) was established for HDV [87].
- RNA Extraction Kit Comparison: Evaluate different nucleic acid extraction kits for their recovery and precision. Performance should be assessed across multiple days and by different operators to determine intermediate precision [87].
Essential Research Reagent Solutions
Successful implementation of dPCR for intestinal protozoa research depends on a suite of reliable reagents and tools.
Table 3: Key Research Reagent Solutions for dPCR-based Protozoa Detection
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| Primer & Probe Sets | Species-specific detection of target protozoan DNA. | Validated sets for E. histolytica, G. duodenalis, etc. [65]. Fluorophores (FAM, HEX) must match instrument filters. |
| dPCR Supermix | Provides optimized buffer, enzymes, and dNTPs for amplification in partitions. | dPCR Supermix for Probes (Bio-Rad); QIAcuity NP Probe PCR Kit (Qiagen). |
| Nucleic Acid Extraction Kit | Islands high-purity, inhibitor-free DNA from complex stool matrices. | QIAamp DNA Stool Mini Kit (Qiagen); other kits validated for stool. |
| International Standard | Calibrates dPCR results to internationally accepted units (IU). | WHO International Standard (e.g., for HDV, used for conversion factor) [87]. |
| Positive Control Plasmid | Contains target sequence for assay development, optimization, and run control. | Custom-designed plasmids with a 120-250 bp insert of the target sequence [65]. |
Implementation and Outlook
Current Challenges and Considerations
Despite its advantages, the adoption of dPCR faces hurdles. The high capital and per-sample costs remain a significant barrier, particularly in resource-limited settings where intestinal protozoa are endemic [88]. While dPCR excels in sensitivity, its throughput limitations compared to high-throughput qPCR platforms can be a constraint for large-scale epidemiological studies [88]. Furthermore, transitioning from research to clinical diagnostics requires extensive assay validation and regulatory compliance (e.g., IVDR, FDA) to ensure reliability and reproducibility [86].
Future Directions in Protozoa Research
dPCR is poised to significantly advance intestinal protozoa research. Its unparalleled sensitivity makes it an ideal tool for monitoring treatment efficacy in clinical trials, as it can detect minute changes in pathogen load that might be missed by other methods [6] [87]. The technology's ability to provide absolute quantification will also refine our understanding of asymptomatic carriage and subclinical infections, clarifying the role of parasites like Blastocystis spp. in gut health [65]. Finally, the move towards multiplexed and automated dPCR systems will increase diagnostic speed and cost-effectiveness, making comprehensive parasite screening more accessible [88] [86]. The relationship between these core applications and the technology's evolution is summarized below.
dPCR Drives Key Research Applications
Conclusion
The integration of real-time PCR into the diagnostic pipeline for intestinal protozoa represents a significant advancement, offering unparalleled sensitivity, specificity, and species-level differentiation crucial for accurate prevalence studies and drug efficacy trials. While challenges in DNA extraction and assay standardization persist, the consistent validation of both in-house and commercial multiplex platforms confirms their utility in clinical and research laboratories. Future directions point toward the wider adoption of fully automated, high-throughput systems and the exploration of even more sensitive technologies like digital PCR. For biomedical research, these refined molecular tools are indispensable for monitoring treatment outcomes, understanding true infection burdens, and ultimately controlling the spread of these pervasive pathogens.
References
- 1. Burden and Distribution of Protozoan Pathogens in Diarrhea ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494489/]
- 2. Global prevalence of intestinal protozoan parasites among ... [https://www.sciencedirect.com/science/article/abs/pii/S0956713522006594]
- 3. Comparative analysis of commercial and “In-House ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06879-9]
- 4. Diagnostic Methods of Common Intestinal Protozoa [https://pmc.ncbi.nlm.nih.gov/articles/PMC9606991/]
- 5. Implementation of real-time PCR assays for diagnosing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11978536/]
- 6. Implementation of real-time PCR assays for diagnosing ... [https://pubmed.ncbi.nlm.nih.gov/40198454/]
- 7. Development and Preliminary Application of a Triplex Real ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.888529/full]
- 8. Worldwide prevalence of protozoans and helminths among ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-24074-4]
- 9. Molecular Biology Can Change the Classic Laboratory ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.02191/full]
- 10. Comparison of Microscopy and PCR for Detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3264173/]
- 11. Improvement of the diagnosis of intestinal protozoa using a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077082/]
- 12. Evaluation of Allplex™ GI-Parasite Assay—A Multiplex ... [https://www.mdpi.com/2414-6366/10/8/234]
- 13. Real-Time Polymerase Chain Reaction: Current Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9778061/]
- 14. Real-Time PCR (qPCR): Principle, Process, Markers, Uses [https://microbenotes.com/real-time-pcr-principle-process-markers-advantages-applications/]
- 15. How Does qPCR Work? (Technology Basics) [https://biosistemika.com/blog/qpcr-technology-basics/]
- 16. Real-Time Polymerase Chain Reaction - an overview [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/real-time-polymerase-chain-reaction]
- 17. Basic Principles of RT-qPCR [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/spotlight-articles/basic-principles-rt-qpcr.html]
- 18. Comparative Pathobiology of the Intestinal Protozoan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6789772/]
- 19. Getting to the guts of the matter: The status and potential ... [https://www.sciencedirect.com/science/article/abs/pii/S002075191300177X]
- 20. Multiplex vs. Singleplex qPCR: What Do I Need To Know? [https://www.thermofisher.com/blog/behindthebench/multiplex-vs-singleplex-qpcr-what-do-i-need-to-know/]
- 21. Detection of intestinal protozoa in paediatric patients with ... [https://www.sciencedirect.com/science/article/pii/S1198743X14641835]
- 22. Validation of an Automated High-Throughput Multiplex ... [https://www.mdpi.com/2673-947X/5/1/8]
- 23. Singleplex real-time PCR and duplex PCR platform for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312404/]
- 24. Standardization of molecular techniques for the detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9084511/]
- 25. Comparative Evaluation of Real-Time Screening PCR ... [https://www.mdpi.com/2076-2607/10/7/1310]
- 26. Molecular detection and genotyping of Giardia lamblia in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617593/]
- 27. Molecular detection and genotyping of intestinal protozoa ... [https://peerj.com/articles/8554/]
- 28. Molecular characterization of intestinal protozoa in two poor ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-015-0714-8]
- 29. Comparison of Two Target Genes for Detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1317193/]
- 30. Comparative Study of DNA Extraction Methods for the PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9689707/]
- 31. Extraction of Parasite DNA from Fecal Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/dnaextraction.html]
- 32. How To Extract DNA From Feces [https://www.zymoresearch.com/blogs/blog/everybody-poops-how-to-extract-dna-from-feces?srsltid=AfmBOoqPBSp-wl1vh_9P35QntP1CtVPCf2smcUjFYrpXy3mDB6o0nwQD]
- 33. Evaluation of fecal DNA extraction protocols for human gut ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-020-01894-5]
- 34. A rapid and high-yield method for nucleic acid extraction [https://www.nature.com/articles/s41598-025-95226-0]
- 35. Development and validation of a multiplex qPCR method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11889745/]
- 36. Development and clinical validation of a novel multiplex ... [https://www.nature.com/articles/s41598-025-16434-2]
- 37. Comparative Analysis of Five Multiplex RT-PCR Assays in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8876857/]
- 38. High-throughput real-time PCR [https://www.takarabio.com/applications/molecular-diagnostics/solutions/high-throughput-real-time-pcr?srsltid=AfmBOooF99pTCr9zpe800bRkNwti0S46SGPxRS1HotWs5bUnw4AJ0PH6]
- 39. Development and validation of high throughput real-time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8324608/]
- 40. Technical validation of a multiplex real-time PCR for ... [https://www.sciencedirect.com/science/article/pii/S0166093425000679]
- 41. A Basic Guide to Real Time PCR in Microbial Diagnostics [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.00108/full]
- 42. A Basic Guide to Real Time PCR in Microbial Diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC5288344/]
- 43. Implementation of real-time PCR assays for diagnosing intestinal ... [https://colab.ws/articles/10.1007%2Fs00436-025-08483-3]
- 44. Genetic diversity of genus Chilomastix: molecular ... [https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-025-00725-5]
- 45. Performance of Real-Time Polymerase Chain Reaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5508894/]
- 46. Detection of Chilomastix mesnili in Common Marmoset ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6737374/]
- 47. Common Pitfalls and How to Troubleshoot Your Results - qpcr [https://qpcr.odoo.com/blog/news-2/qpcr-in-parasitology-common-pitfalls-and-how-to-troubleshoot-your-results-3]
- 48. Evaluation of Three Diagnostic Methods, Including Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1351980/]
- 49. DNA Extraction from Protozoan Oocysts/Cysts in Feces for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4096637/]
- 50. Development and evaluation of a molecular based protocol ... [https://www.sciencedirect.com/science/article/abs/pii/S0014489422000108]
- 51. Comparative Study of DNA Extraction Methods for the PCR ... [https://www.mdpi.com/2075-4418/12/11/2588]
- 52. Metagenomic detection of protozoan parasites on leafy ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1566579/full]
- 53. Optimization and validation of methods for isolation ... [https://www.sciencedirect.com/science/article/pii/S2405676615300299]
- 54. Comparison Study of Four Extraction Methods Combined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9143749/]
- 55. Multicenter comparative study of Enterocytozoon bieneusi ... [https://www.nature.com/articles/s41598-024-66154-2]
- 56. Fecal collection, ambient preservation, and DNA extraction ... [https://www.sciencedirect.com/science/article/abs/pii/S0167701207003843]
- 57. Application of PCR-Based Techniques for the Identification ... [https://www.mdpi.com/2036-7449/16/5/75]
- 58. OneStep PCR Inhibitor Removal Kit [https://www.zymoresearch.com/products/onestep-pcr-inhibitor-removal-new-kit?srsltid=AfmBOoqhzyodgCgVs0nzxGZAchG4dZhgWZIhB3eYCfDf95wb7YK1zbEB]
- 59. Extraction-Free, Filter-Based Template Preparation for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC86779/]
- 60. Removal of PCR Inhibitors by Silica Membranes [https://pmc.ncbi.nlm.nih.gov/articles/PMC88425/]
- 61. Selection of optimal extraction and RT-PCR protocols for ... [https://www.nature.com/articles/s41598-024-78680-0]
- 62. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/moleculardx.html]
- 63. CDC - DPDx - Diagnostic Procedures - Stool Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimencoll.html]
- 64. An improved PCR-based method for detection and ... [https://www.sciencedirect.com/science/article/abs/pii/S0001706X04002062]
- 65. Implementation of real-time PCR assays for diagnosing ... [https://link.springer.com/article/10.1007/s00436-025-08483-3]
- 66. Real-Time PCR: Understanding Ct [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-pcr-understanding-ct.html]
- 67. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOooK-k7z3qIlJFPwQPWHo1zfVM4P1gpRZjO7RjpZu0MEAZ-iXuHW]
- 68. MIQE Guidelines | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/why-choose-taqman-assays/publish-real-time-pcr-results.html]
- 69. MIQE 2.0: Revision of the Minimum Information for ... [https://pubmed.ncbi.nlm.nih.gov/40272429/]
- 70. Real-time PCR for the detection of Dientamoeba fragilis in ... [https://pubmed.ncbi.nlm.nih.gov/17587544/]
- 71. Detection of Dientamoeba fragilis in fresh stool specimens ... [https://www.sciencedirect.com/science/article/abs/pii/S0020751904001936]
- 72. Real-Time-PCR Assay for Diagnosis of Entamoeba ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1153781/]
- 73. Real-Time PCR for Detection and Differentiation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC154634/]
- 74. Dientamoeba fragilis laboratory diagnosis [https://geneticsignatures.com/us/our-products/gastrointestinal-infections/d-fragilis-laboratory-diagnosis/]
- 75. Diagnostic dilemma: application of real-time PCR assays ... [https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-025-06730-1]
- 76. Comparative analysis of commercial and "In-House ... [https://pubmed.ncbi.nlm.nih.gov/40751255/]
- 77. Parasitic diagnosis: A journey from basic microscopy to cutting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617590/]
- 78. Detection of protozoan and helminth parasites in concentrated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607898/]
- 79. Performance of 30 protocol combinations for the detection ... [https://www.sciencedirect.com/science/article/pii/S1684118225000064]
- 80. Comparative performance evaluation of four commercial multiplex real-time PCR assays for the detection of the diarrhoea-causing protozoa Cryptosporidium hominis/parvum, Giardia duodenalis and Entamoeba histolytica - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6453453/]
- 81. Comparative performance evaluation of four commercial multiplex real-time PCR assays for the detection of the diarrhoea-causing protozoa Cryptosporidium hominis/parvum, Giardia duodenalis and Entamoeba histolytica | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0215068]
- 82. Evaluation of Allplex™ GI-Parasite Assay—A Multiplex Real ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390207/]
- 83. Multi-laboratory validation of a modified real-time PCR ... [https://www.sciencedirect.com/science/article/pii/S0740002025000073]
- 84. Development, Optimisation and Validation of a Novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9693193/]
- 85. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 86. dPCR vs. ddPCR: Why Precision Matters in Cell and Gene ... [https://www.roslinct.com/insights/dpcr-vs-ddpcr/]
- 87. Droplet Digital PCR: A Powerful Tool for Accurate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12080313/]
- 88. Digital PCR Market Size, Forecast Report [https://www.mordorintelligence.com/industry-reports/digital-pcr-market]